Discount 16 mg betahistine mastercard
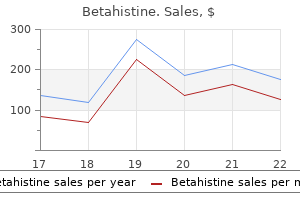
Sonographically medicine zantac buy betahistine 16 mg without prescription, the lungs appear brightly echogenic, the bronchi are dilated, the diaphragm is flattened or everted, and the heart is compressed. In one review of 118 cases, associated anomalies were identified in more than 50 percent (Sanford, 2012). In some cases, the obstructed airway spontaneously perforates, which potentially confers a better prognosis. Heart Cardiac malformations are the most common class of congenital anomalies, and their overall prevalence is 8 in 1000 births (Cragan, 2009). Almost 90 percent of cardiac defects are multifactorial or polygenic in origin, another 1 to 2 percent result from a single-gene disorder or gene-deletion syndrome, and 1 to 2 percent stem from exposure to a teratogen such as isotretinoin, hydantoin, or maternal diabetes. Based on data from population-based registries, approximately 1 in 8 liveborn and stillborn neonates with a congenital heart defect has a chromosomal abnormality (Dolk, 2010; Hartman, 2011). Of chromosomal abnormalities associated with cardiac anomalies, trisomy 21 accounts for more than 50 percent of cases. Traditionally, detection of congenital cardiac anomalies is more challenging than for anomalies of other organ systems. This may be particularly true for ductal-dependent lesions-those requiring prostaglandin infusion after birth to keep the ductus arteriosus open (Franklin, 2002; Mahle, 2001; Tworetzky, 2001). Basic Cardiac Examination Standard cardiac assessment includes a four-chamber view, evaluation of rate and rhythm, and evaluation of the left and right ventricular outflow tracts. Examination of the cardiac outflow tracts aids detection of abnormalities that might not be appreciated in the four-chamber view. These include tetralogy of Fallot, transposition of the great vessels, and truncus arteriosus. Diagram demonstrating measurement of the cardiac axis from the four-chamber view of the fetal heart. The arrow with asterisk marks the interventricular septum becoming the opposing aortic wall. The four-chamber view is a transverse image of the fetal thorax at a level immediately above the diaphragm. It allows evaluation of cardiac size, position in the thorax, cardiac axis, atria and ventricles, foramen ovale, atrial septum primum, interventricular septum, and atrioventricular valves. The atria and ventricles should be similar in size, and the apex of the heart should form a 45degree angle with the left anterior chest wall. Abnormalities of cardiac axis are frequently encountered with structural cardiac anomalies and occur in more than a third (Shipp, 1995). The left ventricular outflow tract view is a transverse image just above the diaphragm and demonstrates that the ascending aorta arises entirely from the left ventricle. The interventricular septum is shown to be in continuity with the anterior wall of the aorta, and the mitral valve in continuity with the posterior wall of the aorta. Ventricular septal defects and outflow tract abnormalities are often visible in this view. In this four-chamber view of a 22week fetus, a defect (arrow) is noted in the superior (membranous) portion of the interventricular septum. The left-ventricular outflow tract view of the same fetus demonstrates a break (arrow) in continuity between the interventricular septum and the anterior wall of the aorta. The right ventricular outflow tract view shows the right ventricle giving rise to the pulmonary artery. Together, the left and right outflow tract views demonstrate the normal perpendicular orientation of the aorta and pulmonary artery, and the comparable size of these great arteries. Structures visible in the right ventricular outflow tract view include the right ventricle and the main pulmonary artery, which subsequently branches into the right and left pulmonary arteries. Fetal Echocardiography this is a specialized examination of fetal cardiac structure and function designed to identify and characterize abnormalities. Guidelines for its performance have been developed collaboratively by the American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine, American Society of Echocardiography, and American College of Radiology. Echocardiography indications include suspected fetal cardiac anomaly, extracardiac anomaly, or chromosomal abnormality; fetal arrhythmia; hydrops; thick nuchal translucency; monochorionic twin gestation; first-degree relative to the fetus with a congenital cardiac defect; in vitro fertilization; maternal anti-Ro or anti-La antibodies; exposure to a medication associated with cardiac defects; and maternal metabolic disease associated with cardiac defects-such as pregestational diabetes or phenylketonuria (American Institute of Ultrasound in Medicine, 2013a). Components of Fetal Echocardiography Basic imaging parameters Evaluation of atria Evaluation of ventricles Evaluation of great vessels Cardiac and visceral situs Atrioventricular junctions Ventriculoarterial junctions Scanning planes, gray scale Four-chamber view Left ventricular outflow tract Right ventricular outflow tract Three-vessel and trachea view Short-axis view, low (ventricles) Short-axis view, high (outflow tracts) Aortic arch Ductal arch Superior and inferior vena cavae Color Doppler evaluation Systemic veins (vena cavae and ductus venosusa) Pulmonary veins Foramen ovale Atrioventricular valvesa Atrial and ventricular septae Aortic and pulmonary valvesa Ductus arteriosus Aortic arch Umbilical artery and vein (optional)a Cardiac rate and rhythm assessment aPulsed-wave Doppler sonography should be used as an adjunct to evaluate these structures. Cardiac biometry and functional assessment are optional but should be considered for suspected structural/functional abnormalities. This is the most common congenital cardiac anomaly and is found in approximately 1 in 300 births (Cragan, 2009; Dolk, 2010). A defect may be appreciated in the membranous or muscular portion of the interventricular septum in the four-chamber view, and color Doppler demonstrates flow through the defect. Imaging of the left ventricular outflow tract may show discontinuity of the interventricular septum as it becomes the wall of the aorta. It has a prevalence of approximately 1 in 2500 births and is associated with trisomy 21 in more than half of cases (Christensen, 2013; Cragan, 2009; Dolk, 2010). The endocardial cushions are the crux of the heart, and defects jointly involve the atrial septum primum, interventricular septum, and medial leaflets of the mitral and tricuspid valves. Approximately 6 percent of cases occur with heterotaxy syndromes, that is, those in which the heart and/or abdominal organs are on the incorrect side. During ventricular systole, the lateral leaflets of the mitral and triscuspid valves come together in the midline. But the atrioventricular valve plane is abnormal, a common atrium (A) is observed, and there is a visible defect (arrow) in the interventricular septum. During diastolic filling, opening of the atrioventricular valves more clearly demonstrates the absence of their medial leaflets. This anomaly is found in approximately 1 in 4000 births (Cragan, 2009; Dolk, 2010). Sonographically, the left side of the heart may appear "filled-in" or the left ventricle may be so small and attenuated that a ventricular chamber is difficult to appreciate. There may be no visible left ventricular inflow or outflow, and reversal of flow may be documented in the aortic arch. Color Doppler depicts flow from the right atrium to the right ventricle only, and left ventricular filling is not visible. The left ventricular outflow tract view demonstrates marked narrowing of the aorta (Ao). Postnatal treatment consists of a three-stage palliative repair or cardiac transplantation. Still, morbidity remains high, and developmental delays are common (Lloyd, 2017; Paladini, 2017). This is a ductal-dependent lesion for which neonatal administration of prostaglandin therapy is essential. This anomaly occurs in approximately 1 in 3000 births (Cragan, 2009; Dolk, 2010; Nelson, 2016). It includes a ventricular septal defect; an overriding aorta; a pulmonary valve abnormality, typically stenosis; and right ventricular hypertrophy. Due to the location of the ventricular septal defect, the four-chamber view may appear normal. This image shows a ventricular septal defect with an overriding aorta in a fetus with tetralogy of Fallot. Following postnatal repair, the 20-year survival rates exceed 95 percent (KnottCraig, 1998). These affected fetuses are at risk for hydrops and for tracheomalacia from compression of the trachea by an enlarged pulmonary artery. Approximately 50 percent of cases are associated with tuberous sclerosis, an autosomal dominant disease with multiorgan system manifestations. Cardiac rhabdomyomas appear as well-circumscribed echogenic masses, usually within the ventricles or outflow tracts. They may be single or multiple; may grow in size during gestation; and occasionally, may lead to inflow or outflow obstruction. In cases without obstruction or large tumor size, the prognosis is relatively good from a cardiac standpoint, because the tumors tend to regress after the neonatal period. M-Mode Motion-mode or M-mode imaging is a linear display of cardiac cycle events, with time on the x-axis and motion on the y-axis. If an abnormality of heart rate or rhythm is identified, M-mode imaging permits separate evaluation of atrial and ventricular waveforms. Thus, it is particularly useful for characterizing arrhythmias and their response to treatment (Chap.
Syndromes
- Urinalysis
- Need for follow-up surgery, especially in growing children
- Loss of consciousness
- Hyperthyroidism
- Are taking NSAIDs prescribed by your health care provider, including celecoxib (Celebrex) or nabumetone (Relafen).
- Kidney stones
- Underactive thyroid gland
- Fatigue
- Problems at home, school, and with peer relationships
Buy cheap betahistine 16mg on line
One unusual feature of the pregnancy-induced changes in renal excretion is the remarkably increased amounts of some nutrients lost in the urine medicine of the future generic 16mg betahistine amex. Amino acids and water-soluble vitamins are excreted in much greater amounts (Shibata, 2013). Renal Function Tests Of renal function tests, serum creatinine levels decline during normal pregnancy from a mean of 0. Creatinine clearance in pregnancy averages 30 percent higher than the 100 to 115 mL/min in nonpregnant women. This is a useful test to estimate renal function, provided that complete urine collection is made during an accurately timed period. During the day, pregnant women tend to accumulate water as dependent edema, and at night, while recumbent, they mobilize this fluid with diuresis. This reversal of the usual nonpregnant diurnal pattern of urinary flow causes nocturia, and urine is more dilute than in nonpregnant women. Failure of a pregnant woman to excrete concentrated urine after withholding fluids for approximately 18 hours does not necessarily signify renal damage. In fact, the kidneys in these circumstances function perfectly normally by excreting mobilized extracellular fluid of relatively low osmolality. Chesley (1963) calculated that about a sixth of pregnant women will spill glucose in the urine. That said, although common during pregnancy, when glucosuria is identified, a search for diabetes mellitus is pursued. Hematuria is common after difficult labor and delivery because of trauma to the bladder and urethra. Proteinuria is typically defined in nonpregnant subjects as a protein excretion rate of more than 150 mg/d. Because of the aforementioned hyperfiltration and possible reduction of tubular reabsorption, proteinuria during pregnancy is usually considered significant once a protein excretion threshold of at least 300 mg/d is reached (Odutayo, 2012). Higby and coworkers (1994) measured protein excretion in 270 normal women throughout pregnancy. Mean 24-hour excretion for all three trimesters was 115 mg, and the upper 95-percent confidence limit was 260 mg/d without significant differences by trimester. The three most commonly employed approaches for assessing proteinuria are the qualitative classic dipstick, the quantitative 24-hour collection, and the albumin/creatinine or protein/creatinine ratio of a single voided urine specimen. The pitfalls of each approach have been reviewed by Conrad (2014b) and Bramham (2016) and their colleagues. The principal problem with dipstick assessment is that it fails to account for renal concentration or dilution of urine. For example, with polyuria and extremely dilute urine, a negative or trace dipstick could actually be associated with excessive protein excretion. The 24-hour urine collection is affected by urinary tract dilatation, which is discussed in the next section. The dilated tract may lead to errors related both to retention-hundreds of milliliters of urine remaining in the dilated tract-and to timing-the remaining urine may have formed hours before the collection. To minimize these pitfalls, the patient is first hydrated and positioned in lateral recumbency-the definitive nonobstructive posture-for 45 to 60 minutes. During the final hour of collection, the patient is again placed in the lateral recumbent position. But, at the end of this hour, the final collected urine is incorporated into the total collected volume (Lindheimer, 2010). Last, the protein/creatinine ratio is a promising approach because data can be obtained quickly and collection errors are avoided. Disadvantageously, the amount of protein per unit of creatinine excreted during a 24-hour period is not constant, and the thresholds to define abnormal vary. Nomograms for urinary microalbumin and creatinine ratios during uncomplicated pregnancies have been developed (Waugh, 2003). Ureters After the uterus completely rises out of the pelvis, it rests on the ureters. Above this level, elevated intraureteral tonus results, and ureteral dilatation is impressive (Rubi, 1968). This unequal dilatation may result from cushioning provided the left ureter by the sigmoid colon and perhaps from greater right ureteral compression exerted by the dextrorotated uterus. The right ovarian vein complex, which is remarkably dilated during pregnancy, lies obliquely over the right ureter and may also contribute to right ureteral dilatation. Moderate hydronephrosis on the right (arrows) and mild hydronephrosis on the left (arrowheads) are both normal for this 35-week gestation. Van Wagenen and Jenkins (1939) described continued ureteral dilatation after removal of the monkey fetus but with the placenta left in situ. The relatively abrupt onset of dilatation in women at midpregnancy, however, seems more consistent with ureteral compression. Ureteral elongation accompanies distention, and the ureter is frequently thrown into curves of varying size, the smaller of which may be sharply angulated. They are usually single or double curves that, when viewed in a radiograph taken in the same plane as the curve, may appear as acute angulations. Another exposure at right angles nearly always identifies them to be gentle curves. Despite these anatomical changes, complication rates associated with ureteroscopy in pregnant and nonpregnant patients do not differ significantly (Semins, 2014). Subsequently, however, increased uterine size, the hyperemia that affects all pelvic organs, and hyperplasia of bladder muscle and connective tissues elevate the trigone and thicken its intraureteric margin. Continuation of this process to term produces marked deepening and widening of the trigone. The bladder mucosa is unchanged other than an increase in the size and tortuosity of its blood vessels. Bladder pressure in primigravidas increases from 8 cm H2O early in pregnancy to 20 cm H2O at term (Iosif, 1980). To compensate for reduced bladder capacity, absolute and functional urethral lengths increased by 6. Concurrently, maximal intraurethral pressure rises from 70 to 93 cm H2O, and thus continence is maintained. Still, at least half of women experience some degree of urinary incontinence by the third trimester (Abdullah, 2016a). Indeed, this is always considered in the differential diagnosis of ruptured membranes. Near term -particularly in nulliparas, in whom the presenting part often engages before labor -the entire base of the bladder is pushed ventral and cephalad. As a result, difficulties in diagnostic and therapeutic procedures are greatly accentuated. Moreover, pressure from the presenting part impairs blood and lymph drainage from the bladder base, often rendering the area edematous, easily traumatized, and possibly more susceptible to infection. Pyrosis (heartburn) is common during pregnancy and is most likely caused by reflux of acidic secretions into the lower esophagus. Although the altered stomach position probably contributes to its frequency, lower esophageal sphincter tone also is decreased. In addition, intraesophageal pressures are lower and intragastric pressures higher in pregnant women. Concurrently, esophageal peristalsis has lower wave speed and lower amplitude (Ulmsten, 1978). Gastric emptying time is unchanged during each trimester and compared with nonpregnant women (Macfie, 1991; Wong, 2002, 2007). During labor, however, and especially after administration of analgesics, gastric emptying time may be appreciably prolonged. As a result, one danger of general anesthesia for delivery is regurgitation and aspiration of either food-laden or highly acidic gastric contents. They are caused in large measure by constipation and elevated pressure in rectal veins below the level of the enlarged uterus. Hepatic arterial and portal venous blood flow, however, increase substantively (Clapp, 2000). Some laboratory test results of hepatic function are altered in normal pregnancy (Appendix, p. Total alkaline phosphatase activity almost doubles, but much of the rise is attributable to heat-stable placental alkaline phosphatase isozymes. Total body albumin levels rise, however, because of pregnancy-associated increased plasma volume.
Buy betahistine visa
The apnea technique symptoms of a stranger safe 16mg betahistine, popular in the earlier era, is now outdated and considered extremely risky. It involves performing the procedure rapidly within a span of 4 min, which is the upper limit for brain hypoxia to occur. Even in expert hands, mortality with this procedure is very high, almost close to 100 percent, and understandably so, very few surgeons now perform this hazardous procedure except in poorly equipped settings. Use the suction and forceps with the right hand while the endoscope is transferred to the left hand. In esophagoscopy, endotracheal intubation may be undertaken, but an emergency tracheotomy may sometimes be required. In long-standing cases, preoperative antibiotics and chest physiotherapy may be required in addition. If respiratory distress is absent, an elective procedure may be done after relevant investigations. Contrast studies with a water-soluble dye such as Gastrografin may be done safely in the case of a suspected esophageal injury. Rigid endoscopy is always preferable to flexible endoscopy in the removal of a foreign body because of better control of the airway. There is better illumination, natural color, and wide-angle viewing, and instrumentation is possible for suction and biopsies of suspicious lesions if any, along with the removal of the foreign body. In esophagoscopy, the cricopharynx, mid-esophagus, and lower esophagus must be thoroughly examined. The region of the hypopharynx may be especially tricky to visualize and requires specific procedures to avoid missing a foreign body [2]. Though these have been described for the detection of hidden malignancies, a knowledge of the same would help in the detection of small foreign bodies or those with almost the same color as the mucosa, for example, dentures. A second look must be taken to ensure completeness of removal and to rule out aspiration of pus or mucus. Cases of severe impaction may require thoracotomy or even gastrotomy, after pushing the foreign body into the stomach. Larger tears must be explored by an open approach such as neck exploration or thoracotomy. References 163 Foreign bodies may get impacted in the soft tissues of the head and neck or inside the spaces and crevices of the upper aerodigestive tract in cases of facial injuries. A preliminary clinical examination must rule out this possibility prior to fixation of facial fractures with wiring or plating, especially if the patient is not in a position to provide historical details. Vomiting, bleeding, cough, hemoptysis, and respiratory distress are common complications of foreign bodies thus missed. Removal of the fixation by cutting the wires, and an elective tracheotomy to safeguard the airway, must be undertaken in order to search for such foreign bodies. Such areas of calcification can be mistaken for a foreign body when a suggestive history is present. Simple passage of balloon catheters, enzymatic dissolution, and unscientific procedures should be strictly avoided. Conclusion Foreign body impaction, both by ingestion and inhalation, is a common occurrence for the otolaryngologist and can pose life-threatening injuries. It may be considered a form of internal injury which is invisible and presents in an indirect manner but must be expediently managed. A 10-year-old child complains of ear pain and impaired hearing after being involved in a fist fight 2 days earlier. Examination reveals a soft fluctuant swelling over the right pinna, and the eardrum has a dark discoloration. A fist fight suggests a blunt trauma to the head and face from the frontal or, in this case, lateral aspect. The discoloration of the drum is due to a hemotympanum, but the opposite ear needs to be examined carefully to rule out otitis media with effusion, which is common in allergic rhinitis. Lab tests must exclude common conditions such as anemia, diabetes, and bleeding disorders from the point of view of incipient surgical intervention and overall prognosis. Serial audiograms should exclude an ossicular discontinuity or fixation due to fibrosis and ankylosis. A 35-year-old housewife presents with acute-onset earache and difficulty in hearing after a domestic quarrel in which her husband slapped her. This is a case of blast trauma with transmission of a pressure wave from the environment into the vibrating apparatus of the ear. It causes a shearing force across the surface of the tympanic membrane with rupture of its vessels and minor bleeding which stops spontaneously. Sometimes ossicular discontinuity may occur due to dislocation or subluxation of the ear ossicles. Very rarely such an impact might even cause sensorineural damage and irreversible hearing loss. Tinnitus may be a significant accompanying symptom and could be temporary or permanent. Such a perforation is usually moderate in size and elliptical in shape, with irregular or jagged edges. For this, a baseline audiometry is first performed, followed by the placement of a small piece of moistened sterile cigarette paper to seal the perforation and repeating the audiogram. Correction of the hearing and abolition of tinnitus, if any, would prove the diagnosis of traumatic perforation. Because this is a fresh injury, fibroblasts grow from the edges of the perforation and facilitate healing. Even if a patch test is not done, the edges of the perforation should be examined carefully under the microscope and may be found to be curled inward. These are then everted under vision so that regeneration of epithelium can take place in an outward direction. Otherwise, squamous epithelium from the ear canal may grow into the middle ear cavity. A 50-year-old man is brought to A&E in an unconscious state and bleeding from the left ear as result of a motor vehicle accident. This patient has suffered a head injury, and therefore attention must be drawn to this first before anything else. The head injury in this case is likely to be severe, and airway compromise would be imminent. Furthermore, if the patient is not breathing spontaneously, he must be connected to a ventilator as soon as possible. The vital parameters must be optimized by the insertion of an intravenous line, urinary catheter and nasogastric tube, and any other means for artificial life support if required. The primary and secondary survey must exclude injury to other systems such as the thorax, abdomen, pelvis, and lower limbs. The middle and inner ear, as well as the facial nerve, are difficult to assess at this juncture. Lab investigations must be sent accordingly and would at the minimum include a complete hemogram with coagulation profile, blood gases, serum electrolytes, and renal function tests. Injuries to other systems would require appropriate imaging such as X-rays, ultrasound, and Doppler studies. Such an extensive avulsion is rarely viable if sutured back in place, but primary repair may be carried out in the absence of facilities for a microvascular flap repair. The wound is copiously irrigated with saline and dilute hydrogen peroxide to get rid of blood clots, dried crusts, dirt, and other contaminants and the wound carefully examined to rule out traces of embedded materials like glass, metal, or wood. Burns, if any, should be carefully handled and the edges of the wound freshened or resurfaced. Primary suturing of the wound edges is then performed with fine nonabsorbable monofilament or polyfilament material.
Purchase betahistine online now
For patients who experience milrinone toxicity medications used for anxiety buy generic betahistine 16mg, the drug is discontinued and if the patient remains hypotensive we add a low dose vasopressin infusion. Epinephrine is a beta-adrenergic drug that possesses beta-1 and beta-2 properties. At higher doses it can produce systemic vasoconstriction via its effect on alpha receptors. It should be used cautiously (or avoided when possible) in patients with elevated pulmonary artery resistance because it is a potent pulmonary artery constrictor. In many centers epinephrine has replaced dopamine as the beta-adrenergic drug of choice in neonates recovering after congenital heart surgery. First, it is clear that dopamine increases systemic oxygen consumption in some neonates after surgery while epinephrine does not. Second, its use has been linked to the development of postoperative junctional ectopic tachycardia. Arginine vasopressin is a potent pressor agent used in a variety of vasodilatory shock conditions. Cardiopulmonary bypass can be associated with the development of vasodilatory hypotension often refractory to other pressor agents. Vasopressin can increase blood pressure under those conditions and improve systemic organ perfusion. Vasopressin does not increase heart rate and this is of considerable benefit for some neonates already pushed to their maximum heart rates. Also, as opposed to other pressors routinely used postoperatively, vasopressin does not increase pulmonary vascular resistance. Acute myocardial injury and low cardiac output states are not uncommon after neonatal surgery and for those patients refractory to medical therapy, mechanical support is a viable option. We have found lactate trending to be extremely useful in predicting survival after congenital heart surgery. A lactate of 10 or greater that does not begin to diminish in a predictable pattern strongly suggests the patient will not survive without support. It is acceptable to consider mechanical support if the amount of inotropic support is excessive. Drugs such as epinephrine have been shown to cause cardiac apoptosis at high doses. At this time, implantable ventricular assist devices, such as the Berlin Heart (Berlin GmbH, Berlin, Germany), are restricted for use in those patients being bridged to transplant. Despite the ability to improve tissue oxygenation, mechanical support is associated with a number of serious complications including neurologic injury and bleeding. Discussions regarding end of life care or transplant should begin at this point if they have not started earlier. Patients with single ventricle physiology and systemic to pulmonary artery shunts have to perfuse both the pulmonary and systemic circulations through the arterial cannula. The required flow rates of the mechanical circuit are higher than flow rates required in those patients with two ventricles. We try to avoid excessive agitation and irritability during the extubation period. Dexmedetomidine, an alpha-2 adrenergic agnostic, has sedative, anxiolytic, and analgesic properties. It can be given to intubated patients, be continued as the patient is bridged through extubation, and even after extubation. It is relatively hemodynamically safe, with bradycardia being the major cardiovascular effect. Its effects in the conduction system have made it a useful drug for the management of postoperative tachyarrhythmia. While experience in newborns has been limited, it is a useful drug in the postoperative period and may become a cornerstone of postoperative management in the future. Postoperative Arrhythmias Arrhythmias in patients recovering after congenital heart surgery are not infrequent, although their incidence appears to be decreasing. Postoperative arrhythmias are associated with significant increases in morbidity, length of hospital stay, and mortality. Mitigating the causative factors associated with postoperative arrhythmias and recognizing and treating them promptly and correctly will have a positive impact on postoperative outcomes. Postoperative tachycardias occur in a number of different cardiac repairs and the incidence and severity is directly related to type of repair, surgical technique, hemodynamic status, electrolyte imbalances, agitation, pain, and temperature of the postoperative patient. Fever and increased circulating catecholamines (intrinsic or iatrogenic) can result in tachyarrhythmias. Once the patient has arrived in the critical care unit, the focus should be on optimizing hemodynamics and reducing oxygen demand along with maintaining normal electrolyte values. The management of these patients should begin with eliminating any postoperative fever. Drug therapy is begun if mild cooling and elimination or decreasing the catecholamines being administered has not resulted in a significant decrease in heart rate. Its administration has been associated with hypotension but this can usually be managed by slowing the infusion rate or giving a bolus of calcium. Some have advocated utilizing a continuos infusion of amiodarone although in our center we give 2-3 mg/kg/hour until the arrhythmia has been adequately controlled. This regimen minimizes the total amount of amiodarone a patient receives and so helps to diminish some of the side effects of amiodarone. There can be atrial flutter or atrial ectopic tachycardia in patients with pre-existing atrial pathology, such as neonates with Ebstein anomaly or in neonates who have had extensive surgery involving the atrium, such as total anomalous pulmonary venous connection. The rapid onset and termination of re-entrant arrhythmias can often be clearly distinguished in the graphic trends. It is recommended that adenosine is used with caution in the postoperative patient. Conversion from a hemodynamically stable rhythm to a more malignant one is well documented in the literature. Atrial overdrive pacing (via atrial pacing wires or a transesophageal pacing wire) or electrical cardioversion might be reasonable alternatives or even the preferred treatment of choice in the most unstable patients. The hemodynamics are almost always adversely affected by this rhythm, although at slower rates ventricular tachycardia can be tolerated for some time. The incidence of ventricular tachycardia increases with operations that include coronary surgery, such as arterial switch and the Ross procedure, and those operations that include ventriculotomies. Lidocaine bolus followed by a continuos infusion can be used, although treatment with procainamide or amiodarone can be more efficacious. Postoperative bradyarrhythmias frequently include sinus node disfunction or complete heart block. For those patients who experience hemodynamically significant changes related to decreased heart rate, pharmacologic treatment with a catecholamine is usually sufficient. Temporary atrial pacing wires notoriously fail to sense atrial activity efficiently. Endotracheal suctioning is a frequent trigger for pulmonary vasoconstriction events. Ventilation needs to be optimized, as well as sedation, medication, and pain management. A strong case can be made for allowing time to pass to achieve somatic growth in low birth weight babies and to allow for brain maturation in those patients who are born preterm. However, aberrant physiologic conditions, such as ventricular volume overload conditions or Box 69. Norwood Operation severe cyanosis, make waiting for surgical correction or palliation dangerous or impractical. Also, patients who are unable to be weaned from mechanical ventilation are unlikely to benefit from waiting for somatic growth. The decision to operate or wait on the preterm or low birth weight neonate needs to be made on a case-by-case basis. Variations of this operation are used to palliate a number of neonates who have in Table 69.
Betahistine 16 mg with visa
Fetal plasma levels medicine etodolac buy discount betahistine on line, however, are only about 3 percent of those in maternal plasma. Before approximately 110 days, there is no vascularization of the fetal anterior pituitary from the hypothalamus. In some women with gestational trophoblastic disease, biochemical and clinical evidence of hyperthyroidism sometimes develops (Chap. This once was attributed to formation of chorionic thyrotropins by neoplastic trophoblasts. The thyroid-stimulatory activity in plasma of firsttrimester pregnant women varies appreciably from sample to sample. For example, acidic isoforms stimulate thyroid activity, and some more basic isoforms stimulate iodine uptake (Kraiem, 1994; Tsuruta, 1995; Yoshimura, 1994). Some examples are multifetal pregnancy, erythroblastosis fetalis associated with fetal hemolytic anemia, and gestational trophoblastic disease. The reason for the elevation is not clear, but reduced placental maturity has been speculated. Human Placental Lactogen Biosynthesis this is a single, nonglycosylated polypeptide chain with a molecular weight of 22,279 Da. Because of these similarities, it was called human placental lactogen or chorionic growth hormone. Thus, its role in pregnancy is believed to be mediated through actions in maternal rather than in fetal tissues. For example, increased maternal insulin resistance ensures nutrient flow to the fetus. It also favors protein synthesis and provides a readily available amino acid source to the fetus. To counterbalance the greater insulin resistance and prevent maternal hyperglycemia, maternal insulin levels are increased. It may serve an important function in fetal vasculature formation (Corbacho, 2002). Other Placental Protein Hormones the placenta has a remarkable capacity to synthesize numerous peptide hormones, including some that are analogous or related to hypothalamic and pituitary hormones. In contrast to their counterparts, some of these placental peptide/protein hormones are not subject to feedback inhibition. For each, there is an analogous hormone produced in the human placenta (Petraglia, 1992; Siler-Khodr, 1988). Other proposed biological roles include induction of smooth-muscle relaxation in vascular and myometrial tissue and immunosuppression. Some evidence suggests that urocortin 2 expression is induced at term and induces expression of proinflammatory markers and prostaglandin F receptor expression in the placenta and myometrium (Voltolini, 2015). Trophoblast ghrelin expression peaks at midpregnancy and is a paracrine regulator of differentiation or is a potential regulator of human growth hormone variant production, described next (Fuglsang, 2005; Gualillo, 2001). Relaxin Expression of relaxin has been demonstrated in human corpus luteum, decidua, and placenta (Bogic, 1995). This peptide is synthesized as a single, 105-amino-acid preprorelaxin molecule that is cleaved to A and B molecules. Two of the three relaxin genes-H2 and H3-are transcribed in the corpus luteum (Bathgate, 2002; Hudson, 1983, 1984). Relaxin, along with rising progesterone levels, may act on myometrium to promote relaxation and the quiescence of early pregnancy (Chap. In addition, the production of relaxin and relaxin-like factors within the placenta and fetal membranes may play an autocrine-paracrine role in postpartum regulation of extracellular matrix remodeling (Qin, 1997a,b). One important relaxin function is enhancement of the glomerular filtration rate (Chap. It also contributes to fetal mineral homeostasis in bone, amnionic fluid, and the fetal circulation (Simmonds, 2010). It functions as an antiobesity hormone that decreases food intake through its hypothalamic receptor. In the placenta, leptin is synthesized by both cytotrophoblasts and syncytiotrophoblast (Henson, 2002). Relative contributions of leptin from maternal adipose tissue versus placenta are currently not well defined, although recent evidence highlights a key regulatory role of placental leptin in placental amino acid transport and fetal growth (Rosario, 2016a). Fetal leptin levels correlate positively with birthweight and likely function in fetal development and growth. Studies suggest that reductions in leptin availability contribute to adverse fetal metabolic programing in intrauterine growth-restricted offspring (Nusken, 2016). It also is found in sympathetic neurons innervating the cardiovascular, respiratory, gastrointestinal, and genitourinary systems. Neuropeptide Y has been isolated from the placenta and localized in cytotrophoblasts (Petraglia, 1989). Inhibin and Activin these glycoprotein hormones are expressed in male and female reproductive tissues and belong to the transforming growth factor- family (Jones, 2006). Inhibin is a heterodimer made up of one -subunit and one of two distinct subunits, either A or B. For example, elevation in inhibin A levels in the second trimester is indicative of fetal Down syndrome. Further, low inhibin levels early in pregnancy may indicate pregnancy failure (Prakash, 2005; Wallace, 1996). Elevations in circulating inhibin and activin levels are reported in women with preeclampsia (Bersinger, 2003). Surgical removal of the corpus luteum or even bilateral oophorectomy during the 7th to 10th week does not decrease excretion rates of urinary pregnanediol, the principal urinary metabolite of progesterone. Before this time, however, corpus luteum removal will result in spontaneous abortion unless an exogenous progestin is given (Chap. After approximately 8 weeks, the placenta assumes progesterone secretion, resulting in a gradual increase in maternal serum levels throughout pregnancy. By term, these levels are 10 to 5000 times those found in nonpregnant women, depending on the stage of the ovarian cycle. First, cholesterol is converted to pregnenolone within the mitochondria, in a reaction catalyzed by cytochrome P450 cholesterol side-chain cleavage enzyme. Pregnenolone leaves the mitochondria and is converted to progesterone in the endoplasmic reticulum by 3-hydroxysteroid dehydrogenase. Although the placenta produces a prodigious amount of progesterone, the syncytiotrophoblast has a limited capacity for cholesterol biosynthesis. Radiolabeled acetate is incorporated into cholesterol by placental tissue at a slow rate. Because of this, the placenta must rely on an exogenous source, that is, maternal cholesterol, for progesterone formation. This mechanism differs from placental production of estrogens, which relies principally on fetal adrenal precursors. Although there is a relationship between fetal well-being and placental estrogen production, this is not the case for placental progesterone. The metabolic clearance rate of progesterone in pregnant women is similar to that found in men and nonpregnant women. During pregnancy, the plasma concentration of 5-dihydroprogesterone disproportionately rises due to synthesis in syncytiotrophoblast from both placenta-produced progesterone and fetus-derived precursor (Dombroski, 1997). Thus, the concentration ratio of this progesterone metabolite to progesterone is elevated in pregnancy. Progesterone also is converted to the potent mineralocorticoid deoxycorticosterone in pregnant women and in the fetus. The concentration of deoxycorticosterone is strikingly higher in both maternal and fetal compartments (see Table 5-1). The extraadrenal formation of deoxycorticosterone from circulating progesterone accounts for most of its production in pregnancy (Casey, 1982a,b). Production of both progesterone and estrogens in the maternal ovaries drops significantly by the 7th week of pregnancy.
Aminocarnitine (L-Carnitine). Betahistine.
- Treating male infertility caused by inflammation of some reproductive organs and tissues (prostate, seminal vesicles, and epididymis).
- Dosing considerations for L-carnitine.
- Improving symptoms and complications of heart disease and heart failure (chest pain, heart attack, and others).
- Improving low birth weight.
- Increasing red blood cell count in people with serious kidney disease.
- Eating disorders, fatigue, diabetes, high cholesterol, blood disorders, circulatory problems in the legs, leg ulcers, attention deficit-hyperactivity disorder (ADHD), Lyme disease, autism, Rett syndrome, and other conditions.
- How does L-carnitine work?
- Improving athletic ability.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96985
Buy cheap betahistine 16 mg on line
Unlike elective surgery medications qd discount 16mg betahistine with amex, it is almost impossible to prevent contamination and risk of infection when dealing with trauma, except in certain cases of iatrogenic trauma. Antimicrobial drugs may be used by surgeons for the prevention of wound infection and also for its treatment. The instances in which trauma surgeons need to be cognizant of antibiotic use, especially in the case of wound infection prophylaxis, lie in several parameters. The most important one is to determine the benefits of prophylactic antibiotic use against its inherent risks. Another crucial factor in determining risk is the status of the wound, in other words, whether it is clean, contaminated, clean-contaminated, or dirty, as is popularly practiced. The extent or magnitude of the operative procedure, in other words the amount and depth of tissue involved, plays a major role in selecting an antibiotic for prophylaxis or whether or not prophylaxis is required at all. The further choice of the antibiotic depends on whether the tissue concerned is compatible for the antibiotic, for example, quinolones such as ciprofloxacin penetrate cartilage well, whereas clindamycin is suitable for the salivary glands. The time of scheduling of the surgery and also its duration are further determinants of the use of a prophylactic antibiotic. It is best administered as close as possible to the time of taking the first incision, and a procedure of long duration may require more than one dose of prophylaxis. In many developing countries, public sector hospitals dispense antibiotics depending upon the availability of current stock and government policies pertaining to that region, which may or may not be along recommended and expected guidelines. Doctors are not uniform in their use of antibiotics, in many instances owing to ignorance and absence of a culture of evidence based practice. Dogma and profiteering by individual doctors and pharmacists also play no mean role in the emergence of antimicrobial resistance. More than anything, it is in the treatment of trauma that many of these considerations must be borne in mind because the patient is often forced to seek treatment in a place that is unfamiliar, and much of these factors might be overlooked. Wound infection then becomes a much more challenging problem to deal with than the mere management of the acute trauma itself. A useful way to deal with this is to opt for a topical preparation whenever applicable. Trainees of various levels of skill and experience and the influx or migration of medical professionals from different ethnicities, cultures, and philosophies mean that chaos and confusion often rule in many trauma services and trauma centers. The concept of damage control surgery has resulted in staggered and multiple operative procedures, often at the hands of different providers, complicating care and making the provision of trauma services extremely exasperating for most patients. While the decision to withhold or withdraw life support is a medical one, political and cultural factors may play a major role and confound the situation greatly. This is always desirable but at the same time unpredictable in certain situations and also dependent on various factors surrounding the trauma episode. At times, tissue regeneration can go haywire and result in unsightly scarring and loss of function, as seen in facial deformity and airway stenosis. Experimental studies are now focused on the recognition of agents that are crucial to tissue repair and renewal and the use of antagonistic agents that could help to keep florid and uncontrollable repair processes under check. While the use of this is tested and tried in malignancies like renal cell and colon carcinoma, research is on for use of the same in trauma and various other diseases. Most research in trauma is in the area of experimental basic research on the one hand and minimally invasive observational research on the other because the authority to waive consent or use delayed consent is not available to trauma service providers. This naturally deters useful and practical research, such as that into newer modalities of treatment like devices, procedures, and even drugs. Institutional mandate for ethical review makes any research beyond retrospective case series and audits cumbersome, and taking the research protocol through all the necessary steps is daunting for most trauma practitioners. Conclusion Even though trauma is unpredictable, sudden, and very often life-threatening, specific principles and guidelines must always be borne in mind. These must be applied as per the demands of a particular situation, all the time keeping in mind the medicolegal problems which may prove daunting in many cases. Platelet preparations for use in facial rejuvenation and wound healing: a critical review of current literature. Effect of neural-induced mesenchymal stem cells and platelet rich plasma on facial nerve regeneration in an acute nerve injury model. Controlled release of hepatocyte growth factor from a bovine acellular scaffold for vocal fold reconstruction. Once trauma has occurred and a wound has formed, the natural tendency of the body is to aid in its healing. Other important factors are whether contamination by impacted foreign bodies or debris is present or bacterial infection due to microorganisms has occurred. The general condition of the patient and the state of the immune system are important factors for prognosis. Habits such as smoking or alcohol abuse could cause further problems such as vascular compromise due to microangiopathy or major vessel disease causing arterial or venous insufficiency and poor nutritional status causing malnutrition and deficiency of vitamins, minerals, and micronutrients. The position of a dependent part and the use of trusses, collars, or bulky bandages could further worsen venous congestion, vascular insufficiency, and the tendency to develop a pressure or decubitus ulcer. Healing by primary intention occurs when the edges of the wound are opposed precisely. Healing by secondary intention occurs when the wound edges cannot be opposed, and therefore the wound is left open. Inflammatory reactions and hyperemia or increased vascular flow causes proliferation of granulation tissue which later undergoes epithelization and contracts, resulting in a visible or obvious scar. A combination of the above two may be understood as healing by tertiary intention. In this the wound edges may not be opposed, and the site may require cleaning, dressing, and debridement until granulation tissue starts to appear and the wound starts to contract. At this point, the edges could be brought closer together and sutured so as to hasten the healing process and optimize the resulting scar. Wound healing can be understood better with the knowledge of skin tissue anatomy and physiology and adequate blood flow through the tissue at all times. The vascular components are made up of red blood cells, neutrophils, platelets, macrophages, and reticulocytes. The lining of the blood vessels also contributes by way of endothelial cells and vascular smooth muscle. The tissue components are the dermis with fibroblasts and myofibroblasts; the adnexal organs such as dermal papilla cells surrounding the hair follicles and the outer root sheath cells; the epidermal elements composed of melanocytes, keratinocytes, and Langerhans cells; the subcutaneous adipose tissue and fat cells; and last but not the least, the neuroendocrine regulation of blood circulation through neurons and hormones. This is the scaffold which serves as the foundation for the migration and adherence of more fibroblasts, and this is responsible for the formation of the dermal matrix that helps in the production of collagen types 1 and 3. This is also evident histologically by the appearance of alpha smooth muscle actin as seen with its increased propensity to take up stain. In experimental animals such as mice, this has been observed to occur between 15 and 30 days after injury. The stage of remodeling then follows, and this eventually restores the elasticity of the skin up to 80% of the normal. This is mainly due to the continuous replacement of type 3 collagen by type 1 collagen until the normal ratio of 1:4 (type 3 to 1) has been achieved. So the natural healing process is capable of restoring almost full structure and function to the injured site. The first step in trauma management is obviously immediate treatment of the wound. Again, factors such as nature and extent of injury are crucial in order to decide how to proceed with wound management. The wound may have to be cleansed and debrided to allow a thorough exploration and to determine what needs to be done further. At this stage, even a working diagnosis must be made that would define the line of treatment to be followed, for example, "a single incised wound over the auricle with exposure of cartilage" or "an external deformity of the nose with fracture of the nasal bones and septal hematoma. Relevant investigations may have to be undertaken, such as basic blood and laboratory tests, and plain X-rays at the minimum. Loss of tissue should be restored wherever possible to maintain cosmetic and esthetic appearance, and physiological function, but not at the expense of compromised viability and risk of infection and necrosis.
Order betahistine discount
The diagnosis being considered may depend on the timing of the onset of symptoms from birth symptoms 4dpo cheap betahistine 16 mg free shipping. The baby may still be in the hospital as a result of premature birth or management of involvement of other organ systems such as diaphragmatic hernia, hydrocephalus, intestinal malrotation, or suboptimal feeding pattern, and a heart murmur is detected resulting in cardiology consultation. Many cardiac defects associated with significant left to right shunt, such as a large ventricular septal defect, patent ductus arteriosus, atrioventricular canal, truncus arteriosus, and aorticopulmonary window, develop symptoms after the postnatal drop in pulmonary resistance. Physical Examination If faced with a critically ill neonate, a concise sequence of physical examination can expedite placement of intravenous or umbilical vessel lines, possible intubation and mechanical ventilation, and performance of echocardiogram, electrocardiogram, and chest roentgenogram. This sequence of physical examination is directed towards confirmation of the suspected diagnosis and determining its severity and the presence of any associated problems. This sequence includes determining the weight and gestational age of the child, a cursory inspection of the face and limbs for major anomalies, inspecting the cardiac impulse, auscultating the heart for cardiac sounds, clicks, and murmurs, auscultating the lungs, palpating the abdomen for any organomegaly, palpating the femoral pulses, auscultating the head and liver for any bruit, and setting up the vital signs monitoring that can determine the heart rate and rhythm, oxygen saturation, respiratory rate, and blood pressure. When the neonate is not critically ill, the temptation to immediately listen to the heart with a stethoscope should be avoided. The recorded weight, length, temperature, respiratory rates, heart rates, and oxygen saturation should be noted. Small and large for gestational age babies have increased risks for the presence of cardiac defects. A general survey is then performed that includes inspection of the head, torso, and limbs for any major anomaly, respiratory effort, color, skin perfusion, motor activity, and responsiveness to tactile stimuli. A sluggish refill may be normal soon after birth, but is also present in poor cardiac output. Acrocyanosis, a benign bluish or cyanotic discoloration of the hands, feet, and face, is common in the first 24 hours after birth. Cyanosis of the lips and oral mucosa, a sign of central cyanosis, is a sign of low oxygen saturation if persistent beyond the first few hours after birth. The head is examined for any facial dysmorphism seen in genetic or chromosomal anomalies with associated cardiac defect. The anterior fontanel is auscultated for any bruit of a cerebral arteriovenous malformation. Certain cardiovascular lesions can result in respiratory distress: pulmonary sling, vascular ring, and tetralogy of Fallot, with absent pulmonary valve syndrome where there maybe markedly dilated pulmonary arteries. This should start with visual inspection and palpation of the cardiac impulse and for the presence of a thrill. A prominent cardiac impulse at the right may suggest the presence of dextrocardia, left-sided pneumothorax, or left diaphragmatic hernia. Auscultation is then performed, which begins with identifying the first and second heart sounds. The first heart sound is more pronounced at the apex; the second heart sound more pronounced at the base. In spite of a fast heartbeat, the splitting of the second sound may be identified. A loud pulmonary component of the second sound may be present in pulmonary hypertension. A single second sound may be present in truncus arteriosus, tetralogy of Fallot with severe pulmonary stenosis or pulmonary atresia, aortic atresia, and in transposition of great arteries and double outlet right ventricle where the aortic and pulmonary valves have an anteroposterior relationship. A systolic ejection click is a high-pitched sound following the first sound heard in stenosis of the truncal valve and aortic or pulmonary valve. Heart murmurs result from turbulence in blood flow across valves, chambers, septal defects, and vessels. A closing ductus arteriosus is heard as transient soft systolic murmur at the left upper chest. A systolic murmur heard at birth may be a sign of a semilunar valve or truncal valve stenosis, or significant atrioventricular valve regurgitation. Ventricular septal defect usually manifests with a murmur only after the drop in pulmonary resistance. Further Reading 55 Lesions such as transposition of great vessels, tetralogy of Fallot with pulmonary atresia, aortic atresia, and persistent pulmonary hypertension may not be associated with a murmur but manifest with overt cyanosis or poor perfusion. A generalized shallow pulse is seen in low cardiac output conditions such as severe dilated cardiomyopathy, supraventricular tachycardia, and complete heart block. If the right brachial artery and the femoral artery pulses are not palpable, an aberrant right subclavian artery below the coarctation may be present. A wide pulse pressure may be seen in an older premature baby with a patent ductus arteriosus and in high cardiac output failure such as neonatal thyrotoxicosis and arteriovenous malformation. The abdomen should be palpated for hepatomegaly associated with right heart failure, and auscultated for bruit from an arteriovenous malformation. The presence of anasarca or hydrops may be signs of arteriovenous malformation, complete heart block, long-standing tachydysrhythmia, or severe cardiomyopathy. A structured sequence of history-taking and physical examination can provide information needed for evaluation of the severity of neonatal cardiac illness and for selecting the appropriate diagnostic and treatment strategy. Central cyanosis should be differentiated from acrocyanosis or peripheral cyanosis, which is a benign bluish discoloration of the hands, feet, or face. This is thought to be from vasospasm of the cutaneous arterioles with sluggish capillary blood flow, oftentimes triggered by cold, and does not require treatment. Central cyanosis is clinically observable in the presence of >3 gm/dL of desaturated hemoglobin in the arterial blood and >5 gm/dL in capillary blood. If cardiac disease is strongly suspected and echocardiography is not available, a hyperoxia test may be performed. In pulmonary disease, PaO2 usually increases to >100 mmHg, whereas infants with cyanotic heart disease show little change in PaO2. Likewise, PaO2 >100 mmHg can be seen in certain forms of cyanotic heart disease with high pulmonary blood flow such as truncus arteriosus and tricuspid atresia with a large ventricular septal defect. Simultaneous measurement of the oxygen saturations of the right hand and a foot is another method that provides a clue for the presence of critical congenital heart disease that warrant further diagnostic examination. This screening method is advocated by the American Academy of Pediatrics and recommended for routine Visual Guide to Neonatal Cardiology, First Edition. Any infant with a positive screen should have a diagnostic echocardiogram, which would involve an echocardiogram within the hospital or birthing center, transport to another institution for the procedure, or use of telemedicine for remote evaluation. Stabilization is important if infant is not in a facility where echocardiography can be performed. Centers for Disease Control and Prevention (2017) Screening for critical congenital heart defects. The manifestations include rapid respirations, grunting, chest retractions, alar flaring, cyanosis, and even slow and shallow breathing or terminal apnea. A detailed history and physical examination, chest X-ray, complete blood count with hematocrit, blood sugar, arterial blood gas, and oxygen saturations should be determined. An electrocardiogram is valuable if there is persistent tachycardia or bradycardia. The timing of appearance of respiratory distress can provide clues to the kind of cardiac disease involved. Pulmonary parenchymal disorders are the most common causes of respiratory distress in the neonate but other etiologies should also be considered (Box 8. A cardiovascular etiology may be seen with a heart murmur, abnormal cardiac silhouette and vascular markings on chest X-ray, difficult ventilation and oxygenation, and differential cyanosis on pulse oximetry of the right hand and a foot. In some pulmonary parenchymal or airway diseases, a separate associated cardiovascular disorder is seen. An echocardiogram should be performed if there is suspicion of cardiovascular disease. In obstructive lesions of the left heart, there is significant impediment in blood flow to the systemic circulation, resulting in manifestations of pulmonary edema and respiratory distress. Tachypnea can be observed in coarctation of the aorta, critical aortic stenosis, and severe mitral stenosis in addition to systemic hypoperfusion. A large communication between systemic and pulmonary circulations may result in overperfusion of the lungs.
Purchase betahistine 16mg line
Fetuses with bladderoutlet obstruction may be candidates for vesicoamnionic shunt placement (Chap medications and mothers milk 2016 purchase betahistine mastercard. Medication Oligohydramnios has been associated with exposure to drugs that block the reninangiotensin system. Fetal skull bone hypoplasia and limb contractures have also been described (Schaefer, 2003). In neonates, their use may result in acute and chronic renal insufficiency (Fanos, 2011). Even in their absence, rates of stillbirth, growth restriction, nonreassuring heart rate pattern, and meconium aspiration syndrome were higher than in nonaffected pregnancies. One review of trials encompassing more than 3200 high-risk and low-risk pregnancies compared outcomes according to which definition was used (Nabhan, 2008). Rates of cesarean delivery, neonatal intensive care unit admission, umbilical artery pH <7. In this group, there was a doubling of the labor induction rate and a 50-percent increase in the cesarean delivery rate for fetal distress. Pulmonary Hypoplasia When diminished amnionic fluid is first identified before the mid-second trimester, particularly before 20 to 22 weeks, pulmonary hypoplasia is a significant concern. Severe oligohydramnios secondary to a renal abnormality generally has a lethal prognosis. Oligohydramnios that results from membrane rupture in the second trimester is reviewed in Chapter 42 (p. In a pregnancy complicated by oligohydramnios and fetal-growth restriction, close fetal surveillance is important because of associated morbidity and mortality (Chap. However, evidence of fetal or maternal compromise will override potential complications from preterm delivery. However, it was not clear whether this translated into better pregnancy outcomes (Gizzo, 2015). It is not considered treatment for oligohydramnios per se, although the decelerations are presumed secondary to umbilical cord compression resulting from lack of amnionic fluid. Amnioinfusion is not the standard of care for other etiologies of oligohydramnios and is not generally recommended. That said, higher rates of preterm delivery, cesarean delivery for a nonreassuring fetal heart rate pattern, and fetalgrowth restriction were found. Magann and associates (2011) concluded that evidence is insufficient to support fetal testing or delivery in this setting. Fetal Diagn Ther 32(4):251, 2012 American College of Obstetricians and Gynecologists: Ultrasound in pregnancy. J Matern Fetal Neonatal Med 22(4):315, 2009 Erez O, Shoham-Vardi I, Sheiner E, et al: Hydramnios and small for gestational age are independent risk factors for neonatal mortality and maternal morbidity. J Matern Fetal Neonatal Med 24(S1):50, 2011 Frank Wolf M, Peleg D, Stahl-Rosenzweig T, et al: Isolated polyhydramnios in the third trimester: is a gestational diabetes evaluation of value Gynecol Endocrinol 33(11):849, 2017 Gizzo S, Noventa M, Vitagliano A, et al: An update on maternal hydration strategies for amniotic fluid improvement in isolated oligohydramnios and normohydramnios: evidence from a systematic review of literature and meta-analysis. Gynecol Obstet Invest 35:91, 1993 Guron G, Friberg P: An intact renin-angiotensin system is a prerequisite for normal renal development. Ultrasound Obstet Gynecol 47:674, 2016 Khan S, Donnelly J: Outcome of pregnancy in women diagnosed with idiopathic polyhydramnios. Eur J Obstet Gynecol Reprod Biol 199:175, 2016 Panting-Kemp A, Nguyen T, Chang E, et al: Idiopathic polyhydramnios and perinatal outcome. The fatal result is usually due to the transmission of toxins, and occasionally the specific micro-organisms from the mother to the child. Poisoning with phosphorus, lead, illuminating gas, and other substances may lead to similar results. Whitridge Williams (1903) Other than referring to fetal deformities that might impede vaginal delivery, little is written in the first edition of this book regarding teratogens and fetal malformations. This is despite the fact that birth defects are common, and 2 to 3 percent of all newborns have a major congenital abnormality detectable at birth (Cragan, 2009; Dolk, 2010). There are undoubtedly medications that pose significant risk to the developing embryo or fetus (Table 12-1). However, 80 percent of birth defects do not have an obvious etiology, and of those with an identified cause, nearly 95 percent of cases have chromosomal or genetic origins (Feldkamp, 2017). Known and unknown causes of 5504 birth defects from a population-based review of 270,878 births. This is because so many pregnant women are prescribed medications and because safety data are often lacking. Investigators from the National Birth Defects Prevention Study found that women take an average of two to three medications per pregnancy and that 70 percent use medication in the first trimester (Mitchell, 2011). A teratogen may be defined as any agent that acts during embryonic or fetal development to produce a permanent alteration of form or function. Thus, a teratogen may be a medication or other chemical substance, a physical or environmental factor such as heat or radiation, a maternal metabolite as in diabetes or phenylketonuria, or an infection such as cytomegalovirus. A hadegen- after the god Hades-is an agent that interferes with organ maturation and function, and a trophogen alters growth. Substances in the latter two groups typically affect development in the fetal period or after birth, when exposures are often more difficult to document. In most circumstances, the term teratogen is used to refer to all three types of agents. Criteria for Determining Teratogenicity the guidelines shown in Table 12-2 were proposed by Shepard (1994) as a framework for discussion and have proven useful for more than 25 years. This is preferably done by a geneticist or dysmorphologist because various genetic and environmental factors may produce similar anomalies. It is easiest to prove causation when a rare exposure produces a rare defect, when at least three cases with the same exposure have been identified, and when the defect is severe. Although almost all drugs cross the placenta, transport must be of sufficient quantity to directly influence embryonic or fetal development or to alter maternal or placental metabolism to exert an indirect effect. Placental transfer depends on maternal metabolism; on specific characteristics of the drug, such as protein binding and storage, molecular size, electrical charge, and lipid solubility; and on placental metabolism, such as by the cytochrome P450 enzyme system. In early pregnancy, the placenta also has a relatively thick membrane that slows diffusion. The preimplantation period is the 2 weeks between fertilization and implantation and is known as the "all or none" period. As the zygote undergoes cleavage, an insult damaging a large number of cells typically causes embryonic death. However, if only a few cells are injured, compensation may be possible and allow normal development (ClaytonSmith, 1996). From animal data, insults that appreciably diminish the cell number in the inner cell mass may produce a dose-dependent diminution in body length or size (Iahnaccone, 1987). The embryonic period extends from the second through the eighth week postconception. It encompasses organogenesis and is thus the most crucial period with regard to structural malformations. Because birth defects and medication exposures are both common, they may be temporally but not causally related. Because initial evaluation of teratogen exposure is often retrospective, it may be hampered by recall bias, inadequate reporting, and incomplete assessment of the exposed population. Potential confounding factors include varying dosages, concomitant drug therapy, and comorbid maternal disease(s). Familial and environmental variables can also influence development of birth defects. Thus, an important criterion for teratogenicity is that two or more high-quality epidemiological studies report similar findings. In fact, the Teratology Society (2005) states that establishment of causation in teratology-related litigation requires human data. Failure to employ these tenets and criteria has contributed to erroneous conclusions regarding the safety of some widely used drugs. This antiemetic was a combination of doxylamine and pyridoxine, with or without dicyclomine, and was safe and effective for nausea and vomiting in early pregnancy. More than 30 million women used this drug worldwide, and the 3-percent congenital anomaly rate among exposed fetuses was not different from the background rate (McKeigue, 1994). Despite considerable evidence that this combination of an antihistamine and a B-vitamin is not teratogenic, Bendectin was the target of numerous lawsuits, and the financial burden of defending these forced its withdrawal from the marketplace.
Discount betahistine online
Without corrective surgery this is universally fatal with most neonates dying within 30 days symptoms 0f food poisoning purchase betahistine overnight delivery. Genetic associations have been described, including trisomies 13 and 18 [4, 5], Turner syndrome (45 X0), and Jacobsen syndrome (terminal 11q deletion). The ascending aorta is usually rudimentary but gives rise to the coronary arteries. In virtually all cases, the ascending aorta and transverse aortic arch are abnormal. When there is antegrade aortic flow, the ascending aorta may be larger but still hypoplastic. The transverse arch is usually hypoplastic, and there may be discrete coarctation. This may not be important with neonatal management but becomes relevant when considering further palliative interventions. Most patients have normal pulmonary venous drainage, but abnormalities can become relevant when considering surgical treatment. In addition to ascending aorta and transverse arch hypoplasia, other arch abnormalities can be seen, such as an anomalous right subclavian artery. Physiology Following delivery, in order to maintain the cardiac output, there must be adequate flow across the arterial duct and atrial septum. Ductal patency is maintained with prostglandin E2 infusion, which can be instituted immediately after birth if a fetal diagnosis has been made. If the arterial duct constricts prior to diagnosis, systemic flow will be reduced, resulting in impaired organ perfusion, acidosis, shock, and even death if untreated. An inadequate or restrictive atrial communication can be diagnosed by fetal echocardiography [8], requiring appropriate delivery and immediate postnatal treatment. Immediately after birth, the pulmonary and systemic vascular resistances are similar, and blood flow between the pulmonary and systemic circulations is balanced. As pulmonary vascular resistance falls, pulmonary blood flow increases at the expense of systemic flow. When pulmonary blood flow increases this is described as "pulmonary overcirculation". Early clinical indicators of this include high systemic oxygen saturations, tachypnea, and low diastolic pressure, eventually progressing to reduced peripheral perfusion, hypotension, acidosis, and shock. Measures that reduce the pulmonary vascular resistance, such as oxygen administration, should be avoided. When pulmonary overcirculation is evident, it may be necessary to control ventilation, manipulate pulmonary resistance with permissive hypercapnia, and use inotropic support. After birth, the patient may present during routine screening; for example, with clinical signs or abnormal four-limb oxygen saturations. However, presentation often occurs as cardiovascular collapse after arterial duct closure. If there is some forward flow through the left heart or a small arterial duct, a murmur may be heard. Oxygen saturations can also be reduced with differential saturations if there is forward flow across the aortic valve. The chest X-ray may be normal or show pulmonary plethora and cardiomegaly, depending upon the balance of the circulation and cardiac function. The most commonly employed method is subjective visual assessment, but this has significant limitations, and its value depends on operator experience [11]. Others may not wish for active intervention post-delivery and opt for compassionate comfort care. Cardiac transplantation in the neonate remains an option but is severely limited by organ availability and therefore not considered a viable treatment option in many countries. This consists of an aortic reconstruction where the pulmonary artery, having been disconnected from the branch pulmonary arteries, is anastomosed to the aortic arch with augmentation using homograft tissue (formation of the neo-aorta). An alternative strategy to the Norwood procedure as a primary palliation has been utilized more recently. The procedure is performed via a sternotomy but has the advantage of avoiding the need for cardiopulmonary bypass. This may be of particular advantage to babies of low birth weight or those who have had cardiovascular collapse. It may also provide an interim solution in those patients with a borderline left heart in whom it is hoped a full biventricular repair may be possible [12]. When children will not achieve a biventricular circulation, a Norwood procedure will ultimately need to be performed, whether this is as a stand-alone procedure or combined with a superior cavopulmonary connection. After the Norwood procedure or a hybrid, children will have common mixing of their circulations. After birth, acute collapse from circulatory imbalance can be life-threatening, and some infants will not survive to undergo their first palliation. Given the precarious nature of the circulation following a Norwood or hybrid procedure, children are at risk for sudden death prior to the superior cavopulmonary connection. The mechanism of this may be acute shunt occlusion, a loss of circulatory balance resulting in pulmonary overcirculation, and/or progressive myocardial dysfunction. Procedure-related mortality for the superior cavopulmonary connection and completion of Fontan is low. Exercise intolerance is common, and other Fontan complications such as arrhythmias, thrombosis, protein losing enteropathy, and plastic bronchitis can also be seen. Incidence Aortic stenosis is more common in childhood and adolescence than in infancy. Incidence increases with age to become the second most common congenital heart disease after ventricular septal defect in the third decade of life. The commissures of the aortic valve may be fused, rendering the orifice small and at times eccentric. The valve is commonly bicuspid in aortic stenosis and the leaflets are asymmetric in 40% of cases. A small percentage of patients with bicuspid aortic valve will develop aortic stenosis, while the majority will not. Therefore, most patients with aortic stenosis are born with this lesion and it is not a result of progression of bicuspid aortic valve. Fusion between aortic valve cusps resulting in a right-to-left commissural fusion is noted to have a worse prognosis in bicuspid aortic than anteroposterior commissures in developing aortic stenosis. Eccentric orifices have a worse prognosis than central orifices in developing aortic stenosis. Pathophysiology Aortic stenosis causes a pressure gradient across the aortic valve, thus elevating left ventricular pressures. This will lead to hypertrophy of the left ventricle later in life and eventually can cause strain of the left ventricle from hypoxia as a result of increase in muscle mass with reduced coronary blood flow. The ascending aorta can become dilated because of the forceful jet of blood as it crosses the aortic valve. Patients with bicuspid aortic valve are known to develop aortic root dilation; this may not be associated with aortic stenosis and the etiology in these cases is not clear but may be related to abnormal wall architecture of the ascending aorta. Aortic regurgitation, occasionally noted with aortic stenosis, will hasten the development of left ventricular dilation and failure as it causes volume overload to the left ventricle on top of the pressure overload caused by aortic stenosis [1]. Natural History Mild cases usually do not progress, while moderate and severe cases usually progress in severity. Sudden death can occur in any patient with aortic stenosis but mainly in more severe and symptomatic patients. A heart murmur is the most common presenting sign suggesting aortic valve disease. Symptoms are limited to patients with severe aortic stenosis caused by reduced cardiac output manifesting as easy fatigability (poor feeding in neonates), shortness of breath, pallor and sweating with exertion, and cool and clammy extremities.
Order betahistine line
It is possible that the child has put a small part or battery of the toy car into his mouth medications you cant take while breastfeeding purchase betahistine 16mg with visa, and this has either entered the airway or the esophagus of the baby. A battery causes severe inflammation of the mucosa, which could involve the airway even if the foreign body has entered the digestive tract. The drooling and refusal of feeds are explained by this and also the crankiness and incessant crying. There is also the possibility of it being in the airway but not occluding the lumen completely. The initial choking or cough may have gone unnoticed, and the child may be already fatigued by the respiratory distress and is therefore listless. Routine laboratory investigations are usually not required as this is a dire emergency. A 50-year-old lady presents to the outpatient department with hoarseness of voice and dyspnea on exertion. She had suffered a stroke 6 months ago and had been hospitalized and treated in intensive care for a month. An otolaryngologist is usually not called in except for evaluation of a complaint of dysphagia, if any. Upon recovery and discharge of the patient, otolaryngological follow-up is thus never done unless the patient has a particular complaint. Vocal cord injury due to endotracheal intubation is more common than usually believed. The cord may get dislocated, or a granuloma may develop at the site of mucosal injury. Stenosis is common at the site of the endotracheal tube cuff due to increased pressure and lack of adequate deflation. A 50-year-old lady presents to the clinic complaining of inability to close the mouth. She reveals that it happened while yawning and has occurred several times in the past. This is because of less muscular strength and gradual effacement of the temporomandibular joint because of increasing age and loss of dentition. The history of recurring episodes is thus common in such patients, and the most common trigger is a forceful or deep yawn. Anterior dislocation is more common because the glenoid fossa is shallower anteriorly. Although many of these interactions are incompletely understood, a number of maternal, placental, and fetal conditions that disrupt normal fetal cardiac development and/or function have been identified. Systemic inflammatory response to these antibodies is thought to lead to the fetal myocardial and conduction system injury and fibrosis. Pacemaker placement is indicated in infants with hydrops or other evidence of poor cardiac output. Infection Maternal infections have been implicated in fetal structural heart defects and myocarditis. It has been reported that any febrile illness in the first trimester can increase the risk for congenital heart defects [2]. Maternal parvovirus B19 infection is a rare cause of fetal anemia (and non-immune hydrops) as well as myocarditis [7]. Maternal Factors Metabolic Pregestational maternal diabetes is associated with up to a fivefold risk of structural cardiac malformations [1]. While most of these infants are asymptomatic, some with severe hypertrophy develop congestive heart failure because of reduced ventricular compliance and/or severe left ventricular outflow tract obstruction and may require supportive care. Maternal phenylketonuria confers a 10- to 15-fold higher risk of structural heart defects when maternal phenylalanine levels are >15 mg/dL [4]. Cardiac defects more commonly seen are hypoplastic left heart syndrome, coarctation of the aorta, and tetralogy of Fallot. The development of hypertrophy is associated with maternal hemoglobin A1C levels >6 g/dL in the latter part of gestation and generally resolves slowly after birth. Endocardial fibroelastosis involving the left ventricle is seen (b) by fetal echocardiography, as echo-bright areas of atrial and ventricular endocardium (arrows) and (c) autopsy specimen. Heart block is usually not reversible once it occurs; cardiomyopathy, associated with high rates of death or transplantation in the first year of life, may be treated in utero or in the neonatal period with dexamethasone and intravenous immunoglobulin with improvement in survival [18]. Familial 25 Cardiac Teratogens Anticonvulsants, lithium, retinoic acid, selective serotonin reuptake inhibitors, and angiotensin converting enzyme inhibitors have been linked to structural cardiac defects if fetal exposure occurs during the first trimester. In general, this is reversible within a few days of discontinuation of the medication [8]. If ductal constriction continues, severe right ventricular dysfunction, tricuspid regurgitation, and hydrops can develop. Delivery may be indicated and these infants are at an increased risk for neonatal pulmonary hypertension. However, in some diseases such as Marfan syndrome, the cardiac phenotype may not manifest until childhood or later and therefore may not be detectable in fetal or neonatal life without genetic testing. Fetal and neonatal familial cardiomyopathies represent more severe forms of these diseases and generally portend poor prognosis. Rarely, fetuses with metabolic abnormalities, such as glycogen storage diseases and cytochrome oxidase deficiency, can exhibit hypertrophic cardiomyopathy in the prenatal or perinatal period. Other genetic diseases may have variable penetrance Twins Cardiac malformations are more common in twin than in singleton pregnancies, and monozygotic twins are at a higher risk than dizygotic twins. The left ventricular myocardium has a "spongy" appearance (a, arrows) with large non-compacted to compacted layer dimension, which can be demonstrated clearly by application of color Doppler over the area of interest (b). This neonate presented with poor cardiac output and the diagnosis was confirmed on gross and histologic examination of the explanted heart at the time of orthotopic heart transplantation soon after these images were obtained. Though rarely obstructive, in this particular case there was moderate obstruction to the left ventricular outflow tract seen by color Doppler from the subcostal coronal image (lower right). These tumors can be detected in the mid-gestation fetus, and often enlarge at an alarming rate through the remainder of gestation, but will regress postnatally. These lesions are complex histologically and may appear on ultrasound as homogeneous, cystic, or mixed type lesions. Compression of the heart and large veins can lead to impaired cardiac filling and hydrops. Myocardial function may appear preserved yet some studies have demonstrated reduced function over time. Congenital diaphragmatic hernia can lead to pulmonary hypoplasia and compression of the heart. Small left-sided cardiac structures and myocardial thinning have been described, though the left heart structures normalize in size after birth in the majority of cases [14]. Occasionally, hypoplastic left heart syndrome may be associated with a left-sided diaphragmatic hernia. The disorder occurs most often in the second trimester and presents as polyhydramnios in the "recipient" twin and oligohydramnios in the other, the "donor. In addition to heart failure resulting in hydrops and fetal demise, the recipient is at increased risk for acquired structural heart defects, most commonly right ventricular outflow tract obstruction [9]. Placental "insufficiency" seen in association with intrauterine growth restriction is manifested by increased vascular resistance in the placenta and decreased oxygenated umbilical venous flow to the fetus. The fetal heart faces increased afterload and there is reduced oxygen delivery to fetal tissue resulting in preferential perfusion of the myocardium and brain (decreased cerebral vascular resistance and increased coronary flow are features [17]). Though pericardial teratomas and their accompanying pericardial effusions are often well-tolerated, large teratomas can also have a compressive effect and lead to hydrops in the fetus or severe compromise in the newborn necessitating urgent surgery for decompression and/or removal of the tumor. These diverse conditions result in increased cardiac workload (preload) for the fetal heart. Although the fetus may be able to generate several times a normal cardiac output before decompensation, the passive nature of the fetoplacental circulation is highly sensitive to small elevations in venous pressure. This, in combination with high capillary permeability and low fetal oncotic pressure, leads to extravasation of fluid into various compartments resulting in pericardial and pleural effusions, ascites, skin edema, polyhydramnios, and placental edema. Space-Occupying Thoracic Lesions Thoracic lesions can affect the position and occasionally the function and development of the heart. These anomalies can continue to progress throughout gestation resulting in significant hemodynamic consequences.