Purchase 2 mg imodium fast delivery
Tosetto A chronic gastritis radiology buy imodium with american express, Castaman G, Rodeghiero F: Bleeding scores in inherited bleeding disorders: Clinical or research tools Mezzano D, Quiroga T, Pereira J: the level of laboratory testing required for diagnosis or exclusion of a platelet function disorder using 20. Borhany M, Pahore Z, Ul Qadr Z, et al: Bleeding disorders in the tribe: Result of consanguineous in breeding. Loewen P, Dahri K: Risk of bleeding with oral anticoagulants: An updated systematic review and performance analysis of clinical prediction rules. Mikhail S, Kouides P: Von Willebrand disease in the pediatric and adolescent population. Peyvandi F, Garagiola I, Menegatti M: Gynecological and obstetrical manifestations of inherited bleeding disorders in women. Schmaier the clinical laboratory evaluation is an integral part of the diagnosis and management of patients with hemostatic/thrombotic disorders. A clinical hematologist when challenged by patients with hemostatic/ thrombotic disorders is as good as the laboratory that serves him or her for diagnosis and management. This chapter provides a critical practical approach to the diagnosis and management of bleeding and clotting disorders. The latter activity is a new use of laboratory resources for what until the present era has mostly been a diagnostic facility. Physiologic hemostasis is the sum of protein (coagulation, fibri nolytic, and anticoagulation) and cellular (platelets, endothelial cells, and leukocytes) elements working in concert to staunch the bleeding at sites of vascular injury without occlusive thrombosis. For example, a patient with Glanz mann thrombasthenia has abnormal platelet function but normal blood coagulation studies. The cellular elements, platelets, endothelial cell, and leukocytes localize physiologic hemostasis and provide proteins and peptides that contribute to the process. The role of the anticoagu lation system is to regulate all the enzymes of the coagulation and fibrinolytic systems so that no excess clotting or bleeding occurs. Thus the present approach to patients with bleeding disorders is to evaluate the plasma proteins of the hemostatic, fibrinolytic, and anticoagula tion systems and platelet number and function that contribute to this process. Although the material just presented has become a cohesive hypothesis for physiologic coagulation activation, clinical laboratory testing of the proteins of coagulation is not based on this current understanding-it follows the Ratnoff and Davies hypothesis. The clinical laboratory assays used to examine the proteins of the coagulation system are based on the original surfaceactivated coagu lation cascade hypothesis. Thus the clini cian must understand the distinction between physiologic coagula tion, fibrinolysis, and anticoagulation contributing to hemostasis and the diagnostic tests that are used to measure these systems. Understanding these assays is an approach to recognizing a potential bleeding abnormality in a patient. In addition to diagnosis of a bleeding disorder, the coagula tion laboratory has the potential to assist the physician in patient management by monitoring changes in the degree of activated blood coagulation. When faced with a bleeding patient, the hematologist must use an analytic diagnostic approach to determine the cause of the bleed ing. When approaching the diagnosis of a coagulation protein defect in a patient, understanding the mechanism is paramount. Any coagu lation protein defect can be a true protein deficiency, an abnormal protein that cannot participate in its physiologic function(s), or an inhibitor directed against the active site of the protein or one that induces enhanced clearance of the protein. In general, inhibitors to a coagulation protein are immunoglobulins, although abnormal pro duction of endogenous heparin, fibronectin, or cryoglobulins has been reported as the source of acquired inhibitors to coagulation proteins. Last, enhanced clearance of coagulation proteins usually occurs as a result of an antibodyprotein complex that is recognized as foreign and thus removed from the circulation. Thus clinical labora tory testing, when available, should focus on measuring the presence of the protein by antigen and its functionality by a variety of assays. Soft tissue petechiae, purpura, or ecchymoses characterize von Willebrand disease or platelet number or functional disorders. History and physical examination are important components of the hemostatic workup (see Chapter 130) but are inadequate for specific diagnosis of bleeding or clotting disorders. Thus the clinical labora tory is essential for definitive diagnosis of a blood coagulation protein defect leading to bleeding. Thrombin also proteolyzes fibrinogen to form fibrin monomer, which then polymerizes into a fibrin clot. When all three assays are performed simultaneously on a sample of plasma, the results indicate almost all of the diagnostic categories for a blood coagulation protein bleeding state. It is most useful to perform a diagnostic evaluation at one time with a complete panel of assays rather than a series of piecemeal studies. Patient conditions usually are dynamic, so piecemeal evaluations often miss evolving clinical states. To perform this assay, equal parts of a negatively charged surface and phospholipid mixture and patient plasma are incubated for more than 5 minutes. This latter mechanism is the basis of the activated partial thromboplastin time, a major screening test for hemostatic disorders. To perform this assay, tissue thromboplastin (tissuederived or recombinant human tissue factor), phospho lipid, and patient plasma are incubated for more than 5 minutes. The plasma then is recalcified by the addition of calcium chloride to 30 mM, and the time required for clot formation is measured. To perform this assay, purified thrombin is added to plasma, and the time to clot formation is measured. It is important to realize that the coagulation proteins need to decrease to different levels before the various screening assays show an abnormality. The sensitivity of the screening tests for detection of specific abnormalities varies with the factor being tested, the commercial reagent used in the assay, and the equipment platform for measurement. In the coagulation cascade hypothesis, coagulation proteins are classified as members of the intrinsic system, the extrinsic system, or the common pathway. In these assays, a sequence of proteolytic reactions takes place, leading to thrombin formation and its proteolysis of fibrinogen. Proteolysis of fibrinogen results in clot formation with precipitation of soluble proteins that are detected by either increased impedance or turbidity or decreased optical clarity, based on the instrumentation used to measure the result. Furthermore, because a series of reactions must occur to result in the final clot formation, any substance. Knowing what each test measures, the clinician can use the fol lowing approach to evaluate bleeding risk in patients who have pro longed values in one or more of these assays (Table 1311). It also is important to recognize these protein defects so that patients do not undergo unnecessary plasma replacement therapy. Individuals can have acquired disorders that inhibit specific coagu lation factors and increase their risk for bleeding. The clinical labora tory phenotype of these patients depends on the protein to which the coagulation protein inhibitor is directed. Inhibitor titer is determined by the degree of dilution of test plasma to obtain a factor level of 50% normal. A complete discussion on performance and interpretation of this assay is seen in Schmaier and Miller. Anticoagulation, unless the patient is faking medical illness, and massive transfusion are excluded by history. The reptilase time uses a snake venom enzyme to "clot" fibrinogen by liberating only fibrinopeptide A. Acquired deficiencies or inhibitors are also seen in a number of medical conditions. This coagulation test pattern is characteristic of a specific inhibitor to a coagulation protein. Another acquired inhibitor that influences coagulation protein reactions is the lupus anticoagulant (see Chapter 143). This inhibitor represents antibodies directed to epitopes of proteins bound to certain phospholipids. Detection of the degree of interference depends on the nature of the commercial reagent. Characteristically a lupus anti coagulant will have a greater effect on a coagulation assay as the reagents, not protein, in the assay are diluted out. After incubation for more than 5 minutes, the time to clot is initiated by recalcification with calcium chloride.
Cheap imodium 2 mg mastercard
Gogarten W treating gastritis diet generic 2mg imodium overnight delivery, Vandermeulen E, Van Aken H, et al: Regional anaesthesia and antithrombotic agents: Recommendations of the European Society of Anaesthesiology. Decousus H, Leizorovicz A, Parent F, et al: A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prandoni P, Bruchi O, Sabbion P, et al: Prolonged thromboprophylaxis with oral anticoagulants after total hip arthroplasty: A prospective controlled randomized study. Bergqvist D, Lowe G: Venous thromboembolism in patients undergoing laparoscopic and arthroscopic surgery and in leg casts. Azarbal A, Rowell S, Lewis J, et al: Duplex ultrasound screening detects high rates of deep vein thromboses in critically ill trauma patients. Prevention of venous thromboembolism in the acute treatment phase after spinal cord injury: A randomized, multicenter trial comparing low-dose heparin plus intermittent pneumatic compression with enoxaparin. Niemi T, Armstrong E: Thromboprophylactic management in the neurosurgical patient with high risk for both thrombosis and intracranial bleeding. Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep vein thrombosis in elective cancer surgery: A doubleblind randomized multicentre trial with venographic assessment. Eufrasio P, Parada B, Moreira P, et al: Surgical complications in 2000 renal transplants. Poli D, Zanazzi M, Antonucci E, et al: Renal transplant recipients are at high risk for both symptomatic and asymptomatic deep vein thrombosis. Hocher B, Slowinski T, Hauser I, et al: Association of factor V Leiden mutation with delayed graft function, acute rejection episodes and long-term graft dysfunction in kidney transplant recipients. Fischereder M, Schneeberger H, Lohse P, et al: Increased rate of renal transplant failure in patients with the G20210A mutation of the prothrombin gene. Heidenreich S, Junker R, Wolters H, et al: Outcome of kidney transplantation in patients with inherited thrombophilia: Data of a prospective study. Ripert T, Menard J, Schoepen Y, et al: Preventing graft thrombosis after renal transplantation: A multicenter survey of clinical practice. Kucher N, Koo S, Quiroz R, et al: Electronic alerts to prevent venous thromboembolism among hospitalized patients. Baser O, Supina D, Sengupta N, et al: Impact of postoperative venous thromboembolism on Medicare recipients undergoing total hip replacement or total knee replacement surgery. Schiffman Galen described the spleen as the "organ of mystery," with functions related to mood and good or ill humors. The complexities of splenic function continue to be the focus of research and observation. Although the spleen is not necessary to life because many of its functions overlap with or can be assumed by other organs, it is an important part of immune and hematologic systems and part of many disease processes. The spleen efficiently phagocytoses erythrocytes, recycles iron, recognizes and destroys pathogens, and induces adaptive immune responses. An appreciation for the subtleties of its anatomy and function is important for the physician evaluating patients with many hematologic, immunologic, hepatic, and infectious diseases. By the ninth week of gestation, layers of the left dorsal mesogastrium condense and blood vessels appear. Lymphocytes appear during the fourth month, and red and white pulp can be identified by the sixth month. Germinal centers do not develop during fetal life, but primitive inactive follicles are evident at birth. In mice, a homeobox gene, Tlx1 (formerly known as Hox11), which controls the genesis of the splanchnic mesodermal plate, is essential for development of the spleen. The spleen is capable of supporting hematopoiesis during fetal life and, in a variety of pathologic states, postnatally. The circulation of primitive hematopoietic stem cells in peripheral blood during prenatal life through birth makes it difficult to distinguish hematopoiesis arising from stem cells in the spleen as opposed to the incidental presence of hematopoietic cells within the circulation. The splenic artery arises from the celiac axis, enters the capsule at the hilum, and branches into trabecular arteries. The trabecular arteries then branch into central arteries and enter the white pulp. The periarterial lymphatic sheath consists of a cuff of T lymphocytes, plasma cells, and macrophages around the central arteries. B-lymphocyte clusters appear in follicles along the periarterial lymphatic sheath at arterial branch points. On the cut surface of the normal spleen, white pulp is visible as white nodules 1 to 2 mm in diameter. The nodules are fully developed at birth, increase in size in childhood (especially with immunizations and infections), peak at puberty, and involute in adulthood. Immunologically normal, uninfected adults normally have no evident germinal centers. A mantle zone of B lymphocytes surrounds the follicle, or secondary germinal center. Antigen trapping and processing take place in the marginal zone of the white pulp. The red pulp of the spleen consists of vascular sinuses, the cords of Billroth, and the terminal branches of the penicilliary arteries. Intact leukocytes, erythrocytes, and platelets are able to squeeze through the potential spaces between these cells and between the ring fibers. Processes of the reticular cells of the cords of Billroth are outside the sinus walls. Venous sinus endothelial cells contain a plasma membrane-associated network of stress fibers composed of actin and myosin-like filaments. These filaments may cross the plasma membrane and insert into the mesh-like basement membrane. As the fibers tense, they create fenestrations through which erythrocytes must pass if they hope to continue their journey. Cells infected by parasites or simply worn from age become trapped by the fibers and will not continue in the circulation. Circulation of blood through red pulp lined with endothelial cells represents a closed circulation, which is rapid. Circulation into the cords, or open circulation, is slower and permits the macrophages lining the cord to remove damaged or aged cells. Accessory spleens are present in up to a third of the population and result from failure of precursor cells to fuse during embryologic development. They often receive blood flow from the splenic artery and are located near the spleen but can be distant and confused with a tumor when noted on imaging studies or even physical examination. They can develop similar conditions as the spleen proper and may result in continued abnormalities even after splenectomy. Functions the functions of the spleen and their anatomic locations are summarized in Table 162-1. The Red Pulp Splenic macrophages dominate the function of the red pulp and are responsible for filtering blood, removing bacteria, and recycling iron. Arterial blood pools in the splenic cords before entering the splenic sinuses and returning to systemic circulation. Arterial blood is delivered to the cords of the red pulp through an open system of reticular fibers, fibroblasts, and macrophages without an endothelial lining. Blood then passes from the cords into the efferent venous sinuses, which are lined with endothelium with a discontinuous structure. Stress fibers extend beneath the basal plasma membrane and run parallel to the axis of the endothelial cells. These cords direct the blood into sinuses through slits modulated in size by the stress fibers. In many animals, these stress fibers and the splenic capsule are contractile and enable the spleen to serve as a reservoir of red cells and reduce blood viscosity when the animal is at rest. In humans, however, there is no evidence that the spleen serves such a function or is capable of significant changes in volume with rest and exercise. To return to the circulation, cells must pass through the slits between venous sinus endothelial cells. This surface is probably an important site for the culling and pitting of aged or damaged cells.
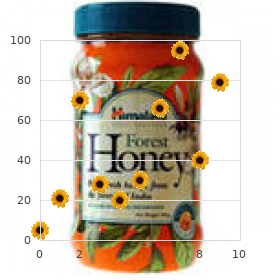
| Comparative prices of Imodium | ||
| # | Retailer | Average price |
| 1 | AutoZone | 457 |
| 2 | J.C. Penney | 967 |
| 3 | Barnes & Noble | 689 |
| 4 | IKEA North America | 522 |
| 5 | Belk | 876 |
| 6 | OSI Restaurant Partners | 935 |
| 7 | PetSmart | 578 |
| 8 | The Home Depot | 367 |
Buy imodium
The overall maternal mortality for uterine rupture is less than 1% gastritis what to avoid order imodium line, but if rupture occurs in the antepartum patient at home, it is likely to be higher. The perinatal mortality for uterine rupture ranges from 1% to 15%, again depending on where the patient is when the uterine rupture occurs. In women with a prior low transverse cesarean delivery, it is estimated to occur in 0. However, in women with a prior classical cesarean delivery (vertical uterine incision), the incidence of uterine dehiscence or rupture is estimated to be 6 to 12%. Risk factors for uterine rupture are conditions that predispose to a weakened uterine wall, including uterine scars, overdistension, inappropriate and aggressive use of uterotonic agents, maternal congenital uterine anomalies, and abnormal placentation (Table 5-7). There is an increased incidence of both velamentous cord insertion and vasa previa in pregnancies that result from in vitro fertilization, particularly in twin pregnancies. Nonreassuring fetal testing, abnormal abdominal contour, cessation of uterine contractions, disappearance of fetal heart tones, and regression of the presenting fetal part are other signs of uterine rupture. Whenever bleeding accompanies rupture of the membranes in labor, especially if there are associated fetal heart rate decelerations, fetal bradycardia, or a sinusoidal fetal heart rate pattern, the obstetrician should have a high index of suspicion for a ruptured vasa previa. In cases of large rupture extensions, repair may not be feasible and the patient may require a hysterectomy. Patients are usually discouraged to attempt future pregnancies given the high risk of recurrent rupture. Trial of labor would be avoided in any subsequent pregnancy, and the patient would commonly be delivered via repeat cesarean section either at week 36 after confirmation of fetal lung maturity or at 37 weeks with out testing for fetal lung maturity. With advancing capabilities of ultrasound, velamentous insertion of the umbilical cord and succenturiate placental lobes can be diagnosed in the antepartum period. Further, with the use of color Doppler, vasa previa may also be diagnosed antepartum, but the sensitivity and specificity of these diagnoses are yet to be determined and are likely related to the experience of the sonographer and/ or sonologist and ultrasound equipment available. However, several small prospective studies have demonstrated that the majority of cases of vasa previa in asymptomatic women can be diagnosed prenatally through a policy of routinely evaluating the placental cord insertion when an ultrasound examination is performed, and considering vaginal sonography with color Doppler if the placental cord insertion cannot be identified, or if there is a low-lying placenta or a suspected succenturiate placental lobe. These studies found that sonographic identification of placental cord insertion was accurate, sensitive, and added little or no extra time to the duration of the obstetric sonographic examination. In the prenatally diagnosed cases, the neonatal survival of infants without congenital malformations was approximately 97%. This is dramatic when compared to the 45% neonatal survival rate when the diagnosis was not made prenatally. If the resulting mixture is pink, it indicates fetal blood; a yellow-brown color is seen with maternal blood. However, when acute bleeding occurs from a ruptured vasa previa, emergent delivery is frequently indicated, and there may be no time to test for fetal blood cells. Because the vessels course unprotected through the membranes before inserting on the placental margin, they are vulnerable to rupture, shearing, or laceration. In addition, these unprotected vessels may cross over the internal cervical os (vasa previa), making them vulnerable to compression by the presenting fetal part or to being torn when the membranes are ruptured. Although vasa previa is rare, perinatal mortality is high (approximately 40% to 60%) and increases if the membranes are also ruptured. The condition is important because, when the membranes rupture, spontaneously or artificially, the fetal vessels running through the membranes have a high risk of concomitant rupture, frequently resulting in fetal exsanguination and death. Because the fetal blood volume is only about 80 to 100 mL/kg, loss of even small amounts of blood could prove disastrous to the fetus. Additionally, pressure on the unprotected vessels by the presenting fetal part could lead to fetal asphyxia and death. Unprotected fetal vessels and vasa previa may occur with a succenturiate lobe of the placenta. In this case, the bulk of the placenta is implanted in one portion of the uterine wall, but a small lobe of the placenta is implanted in another location. The vessels that connect these two portions of the placenta are unprotected and may course over the cervix and present as a vasa previa. Risk factors for fetal vessel rupture include abnormal placentation leading to a succenturiate lobe as well as multiple gestations that increase the risk of velamentous insertion. Even when the neonate has lost considerable blood, immediate transfusion may be lifesaving. One study suggests that women with prenatally diagnosed vasa previa be offered elective delivery by cesarean at about 35 weeks of gestation, or earlier, if fetal lung maturity is documented. This is earlier than the 39 weeks that is generally recommended for elective cesarean delivery. The mean age of delivery for the cases not diagnosed prenatally in this series was approximately 38 weeks. The risks associated with prematurity at 35 weeks of gestation must be weighed against the risk of a dismal outcome should the membranes rupture, especially because approximately 8% of women at term will have ruptured membranes before the onset of labor. Unfortunately, membrane rupture, even in a hospital, often results in infants with low Apgar scores and who require transfusions, suggesting significant morbidity. If patients with known vasa previa elect to undergo a trial of labor, artificial rupture of membranes is contraindicated. Patients with these conditions usually present with spotting rather than frank bleeding. The diagnosis is usually made by speculum examination, Papanicolaou test, cultures, or colposcopy as indicated. Other than advanced maternal neoplasia, which is associated with poor maternal outcome, most nonobstetric causes of antepartum hemorrhage require relatively simple management and have good outcomes. Infections may be treated with appropriate agents, cervical polyps can be removed, and benign neoplasms usually require simple treatment. Previa occurs more often in patients with prior placenta previa, uterine scars, or multiple gestations. The classic presentation of placenta previa is painless vaginal bleeding in the third trimester and it is usually diagnosed via ultrasound. Patients are delivered by cesarean section in the case of unstoppable preterm labor, large hemorrhage, nonreassuring fetal testing, or at week 36 with mature lung indices. When the placenta invades into the myometrium, it is known as placenta increta, whereas when it invades through the myometrium and to the serosa, it is known placenta percreta. Placental abruption accounts for 30% of all third-trimester hemorrhages and is seen more often in women with chronic hypertension, with preeclampsia, using cocaine or methamphetamines, or with a history of abruption. Women can be delivered vaginally if they are stable; cesarean delivery is necessary in the unstable patient or when fetal testing is nonreassuring. Uterine rupture is a rare obstetric catastrophe, but is seen in 1 in 200 laboring women with a prior cesarean delivery. Maternal and fetal morbidity and mortality are increased in the setting of uterine rupture. Uterine rupture requires immediate laparotomy, delivery of the fetus, and either repair of the rupture site or hysterectomy. Fetal vessel rupture is a rare obstetric complication and is usually associated with multiple gestation and/or a velamentous cord insertion. Fetal vessel rupture is associated with a perinatal mortality of up to 60% of cases. Nonobstetric causes of antepartum hemorrhage include cervical and vaginal lacerations, hemorrhoids, infections, and neoplasms. Nonobstetric causes of antepartum hemorrhage generally require simple management and have good outcomes. No vaginal bleeding, leakage of fluid, no discharge, just starting to feel fetal movement. Past surgical history was significant for two prior low-transverse cesarean sections at term, first cesarean section for breech at 39 weeks secondary to failed external cephalic version in 2007 and second for repeat cesarean section at 39 weeks in 2009. On ultrasound, the fetus is noted to have normal anatomy, normal amniotic fluid index, and an anterior placenta that is noted to be completely covering the internal os of the cervix. What is this patient most at risk for at delivery given her history and ultrasound findings Complete pelvic rest for the remainder of the pregnancy or until previa resolves c. Bed rest and pelvic rest for the remainder of the pregnancy or until previa resolves. What further imaging, if any, might be helpful in the diagnosis of placenta accreta in this patient Attempt to tocolyze the patient and give a steroid course for fetal lung maturity b. On ultrasound, the fetus is noted to have an anterior placenta with a posterior succenturiate lobe. On sterile vaginal examination, the patient is initially found to be 2 cm dilated, 50% effaced, and 23 station.
Cheap imodium on line
The earliest and most prominent cell type in human and mouse atherosclerotic lesions are monocytes and macrophages gastritis diet ���� cheap 2 mg imodium with mastercard. Initial monocyte entry into the arterial intima is in response to poorly understood cues related to endothelial cell dysfunction. The adherent monocytes then diapedese through disrupted endothelial junctions and enter the intima. The ultimate fate of monocytes within the intima is probably determined in part by lineage commitment programs carried by the entering monocytes and in part by local environmental cues. Most, however, seem to polarize toward the so-called M1 inflammatory macrophage phenotype. In addition to monocytes, small numbers of lymphocytes, particularly T cells, also enter the intima, where they contribute to plaque formation by secreting cytokines and other mediators. The net effect is formation and accumulation of lipid-laden foam cells and proinflammatory immune cells, which together form plaque. Although abundant data from animal models and correlative human studies support the oxidative stress hypothesis, considerable controversy remains because large- and medium-sized interventional trials of antioxidant therapy in humans have generally failed to prevent the complications of atherosclerosis. Another potential problem with the antioxidant clinical trials is that the choice of antioxidants may have been flawed. Recent studies showed that tocopherols, in addition to having activity as antioxidants, have important cell-signaling functions mediated by specific cellular receptors. Therapy with formulations containing primarily -tocopherol may downregulate endogenous -tocopherol levels, leading to imbalance in natural tocopherol signaling pathways. Furthermore, tocopherols are lipid-based structures that are themselves subject to oxidation, producing lipid peroxides that can actually promote further oxidative stress. In experimental animals, transplantation of atherosclerotic aortae from hypercholesterolemic animals into normal recipients induces migration of lipidladen macrophages out of the vessel wall and plaque regression. Lymphocytes infiltrating from the circulation and mast cells from the adventitia also contribute to the inflammatory milieu and matrix remodeling. Animal studies suggest that platelets may facilitate monocyte recruitment, acting as a bridge between the endothelium and circulating monocytes. Sophisticated single-cell imaging studies in mice showed that monocytes continue to traffic through the "shoulders" of even advanced stage lesions. Plaque generally grows in an eccentric pattern within the intima and in certain instances can create significant obstruction to blood flow. In such cases, as oxygen demand increases, tissue ischemia results, leading to angina and/or lower extremity claudication. Recent in vivo studies using sophisticated imaging techniques, such as intravascular ultrasound, however, demonstrate that in most cases, the vessel wall remodels as plaque grows. Of note, such studies along with careful histopathologic examinations, have led to the concept that the "quality" of the plaque may be more important than its quantity in predicting cardiovascular outcomes. Some plaques, particularly those with thick fibrous caps and cellular cores seem to be "stable". Rupture refers to the sudden loss of integrity of the fibrous cap with release of plaque material into the lumen, often followed by acute occlusive thrombosis. Erosion is a more subtle concept referring to loss of endothelial cells at the shoulder of the lesion or minimal leakage of plaque through a partially disrupted cap. Plaque erosion may lead to subocclusive thrombus formation and/or intraplaque hemorrhage and thrombosis. Repeated cycles of erosion and intraplaque hemorrhage/ thrombosis may account for the apparent stepwise growth of some lesions. Understanding factors that contribute to plaque vulnerability is an extremely important topic of research, but one that is difficult to model in animals. Some key features that have emerged are the degree of angiogenesis within the plaque, the balance of matrix-degrading enzymes and enzyme inhibitors, the level of apoptosis of cells within the plaque, and the deposition of calcium within the plaque. In response to chemokines, monocytes continue to enter plaque, perhaps accompanied by platelets. Cholesterol loading of macrophages induces apoptosis and apoptotic cells accumulate because of dysfunction of normal efferocytotic clearance pathways. These cells produce collagen and other matrix components, contributing to plaque growth and formation of a fibrous cap. To support plaque growth, an angiogenic response is elicited from vasa vasora within the adventitia. On the left is a cross-section cartoon image of an artery containing a large eccentric plaque (orange). The atheromatous lesion is extending into the arterial lumen and would be visible on an angiogram as an obstructing lesion. On the right is a lesion of similar mass, but its formation was accompanied by significant vessel wall remodeling so that the lesion extends mainly into the vessel wall, preserving the lumen. On the left is a cross-section cartoon image of an artery with a plaque containing abundant smooth muscle cells and foam cells and a thick fibrous cap. On the right is a similar-size plaque, but with a thin fibrous cap that has ruptured allowing plaque contents to extrude into the lumen. This plaque contains smooth muscle cells and foam cells, as in the stable plaque on the left, but there is abundant angiogenesis, along with apoptotic and necrotic cells. In animal models, treatment with antiangiogenic agents significantly slows plaque growth. In some diseases states, such as diabetes, accelerated atherosclerosis may reflect a "microvascular" disease of the vasa vasorum. Integrity of the fibrous cap is maintained by a balance between collagen synthesis by smooth muscle cells and fibroblasts and collagenolysis by matrix-degrading enzymes. The latter is maintained by a balance between enzymes and their endogenous inhibitors. These enzymes are tightly regulated by a network of activators and inhibitors and in settings in which activation exceeds inhibition, excessive matrix degradation may occur. A prominent feature of advanced atherosclerotic lesions is the presence of apoptotic cells, mostly of macrophage and smooth muscle cell origin. The nature of the proapoptotic signals within plaque is incompletely understood, but excess intracellular cholesterol can initiate the endoplasmic reticulum stress response leading to apoptosis. In most inflammatory sites, apoptotic leukocytes are quickly removed by phagocytes in a process known as efferocytosis. The efferocytotic macrophages are generally thought to be of the M2, antiinflammatory type; thus their engagement by apoptotic cells not only removes the apoptotic cell from the microenvironment, but also directly contributes to downregulation of the inflammatory state by inducing secretion of antiinflammatory cytokines and effectors. In atherosclerotic plaque, this process seems to be inefficient so that apoptotic cells accumulate, contributing to the lipid load and releasing potentially toxic contents. Although therapeutic interventions to stabilize vulnerable plaque or prevent plaques from becoming vulnerable have not yet materialized, several imaging approaches have been studied in attempt to develop useful biomarkers to identify vulnerable plaque and therefore to identify patients who might benefit from aggressive antithrombotic and lipid-lowering therapeutic interventions. As described in later chapters in this section, treatment and prevention strategies using aggressive antiplatelet, anticoagulant, fibrinolytic, and/or mechanical approaches have been remarkably effective at reducing major cardiovascular events, but tremendous unmet need still exists, particularly in the areas of primary and secondary prevention of thrombosis. The pathophysiologic mechanisms underlying acute arterial thrombosis center on two key concepts: (1) exposure of prothrombotic materials to the local circulation as a consequence of plaque rupture acts as a thrombotic trigger, and (2) advanced atherosclerosis is associated with a systemic prothrombotic state that accelerates or enhances pathologic thrombosis. Platelets accumulate at the rupture site and are activated by plaque components, such as collagen, forming an aggregate that, if large enough, can obstruct blood flow. Similar findings were seen in platelets from mouse models of hyperlipidemia, such as the apoE-null strain, which was fed a high-fat diet. Of note, the time to form occlusive thrombi after arterial injury in vivo was accelerated in hyperlipidemic mice compared with controls. In that context, much attention has been paid to identifying and characterizing receptors on the platelet surface that recognize specific classes of lipids and lipoproteins. Epidemiologic studies have also associated levels of soluble phospholipase A2 with cardiovascular risk. In addition to platelet hyperreactivity, it is also quite likely that systemic activation of the coagulation cascade contributes to the prothrombotic state associated with advanced atherosclerosis. This is consistent with studies showing that atherosclerosis is associated with increased risk for venous thromboembolic disorders, as well as arterial thrombosis. They are 200 to 1000 nm in size and possess different antigenic properties depending on the cell from which they are derived. In mice, the contact activating system and intrinsic coagulation cascade have been shown to participate in arterial thrombosis after injury and to have proatherogenic properties. Given these observations, there has been renewed interest in exploring the use of antiinflammatory agents and antithrombotic agents to slow the progress of atherosclerosis. Specific antioxidant approaches based on fundamental understanding of the oxidation processes relevant to atherosclerosis remain viable as well. Thus bidirectional cross-talk between the inflammation and coagulation systems serves to enhance each other and to promote atherosclerosis.
Buy imodium 2 mg online
Fetal mortality occurs in about 35% of all clinically relevant antepartum placental abruptions and can be as high as 50% to 80% in cases of severe placental abruption gastritis diet 21 2 mg imodium with amex. The cause of fetal demise is usually due to hypoxia resulting from decreased placental surface area and maternal hemorrhage. Although relatively uncommon, placental abruption is a major cause of fetal and neonatal mortality. The high mortality associated with abruptio placentae has been demonstrated to be due to its strong association with preterm birth, with more than 50% of the excess perinatal deaths among abruptio-associated pregnancies accounted for by premature delivery. While the incidence of placental abruption increases with the number of gestations (triplets. The predisposing and precipitating factors for placental abruption are listed in Table 5-5. The most common factor associated with increased incidence of abruption is hypertension, whether it is chronic, the result of preeclampsia, or maternal ingestion of cocaine or methamphetamine. In cases of abruptions that are severe enough to cause fetal death, 50% are due to hypertension: 25% of these are from chronic hypertension and 25% are from preeclampsia. The risk of abruption in future pregnancy is 10% after one abruption and 25% after two prior abruptions. Only 2% to 25% of abruptions are diagnosed by ultrasound (evidenced by a retroplacental clot). However, because abruption can present clinically in a similar fashion to placenta previa with vaginal bleeding, ultrasonography is routinely performed to rule out previa in cases of suspected abruption. The diagnosis of abruption may be confirmed by inspection of the placenta at delivery. The presence of a retroplacental clot with overlying placental destruction confirms the diagnosis. Conversely, neither hypotension nor anemia is obligatory even with extreme concealed hemorrhage. However, about 30% of placental separations are small with few or no symptoms and are identified only after inspection of the placenta at delivery. It has historically been taught that painful uterine bleeding signifies placental abruption, whereas painless uterine bleeding is indicative of placenta previa. The differential diagnosis is usually not this straightforward, and labor accompanying previa may cause pain suggestive of placental abruption. Alternatively, pain from abruption may mimic normal labor, or it may be painless, especially with a posterior placenta. Consumptive Coagulopathy Placental abruption is one of the most common causes of clinically significant consumptive coagulopathy in obstetrics. In approximately one-third of women with an abruption severe enough to kill the fetus, there are measurable changes in coagulation factors. In cases where the fetus survives, severe coagulation defects are seen less commonly. In general, if serious coagulopathy develops, it is usually evident by the time abruption symptoms appear. The major mechanism of consumptive coagulopathy in the setting of abruption is activation of intravascular coagulation with varying degrees of defibrination. Procoagulants are also consumed in the retroplacental clots, although the amounts Physical Examination On physical examination, a patient with placental abruption will often have vaginal bleeding and a firm, tender uterus. On tocometer, small frequent contractions are usually seen along with tetanic contractions. On fetal monitoring, nonreassuring fetal heart tracing is frequently seen secondary to hypoxia. Overt thrombocytopenia may or may not accompany severe hypofibrinogenemia initially, but commonly becomes evident after repeated blood transfusions. Vaginal delivery is preferred as long as bleeding is controlled and there are no signs of fetal distress. Vaginal delivery is also preferred in the case of intrauterine fetal demise in the setting of severe placental abruption. Because the uterus is typically hyperactive and persistently hypertonic in patients with an abruption, a rapid labor and delivery should be expected. If the fetal heart rate tracing is nonreassuring, delivery should occur for fetal indications. However, most abruptions are small and noncatastrophic, and do not therefore necessitate immediate delivery. Treatment of placental abruption varies depending on gestational age and the status of the mother and fetus. Emergency cesarean delivery is chosen by most clinicians if vaginal delivery is not imminent and the fetus is of viable gestational age. With massive external bleeding, intensive resuscitation with blood products, crystalloid fluids, and prompt delivery to control hemorrhage are lifesaving for the mother and, hopefully, for the fetus. If the diagnosis is uncertain and the fetus is alive but without evidence of compromise, then close observation can be practiced in facilities capable of immediate intervention. Blood loss due to placental abruption is commonly grossly underestimated because of to concealed bleeding. Additionally, patients should also be transfused fresh frozen plasma and occasionally cryoprecipitate in similar ratios as found in massive transfusion protocols for trauma. In the preterm pregnancy, betamethasone may be given to promote fetal lung maturity and some providers tocolyze to assist in prolonging the pregnancy to week 34 for pregnancies complicated by suspected abruption with no evidence of fetal compromise. More than 90% of all uterine ruptures are associated with a prior uterine scar either from cesarean section or other uterine surgery. Uterine ruptures without a prior uterine scar may be related to an abdominal trauma. The primary maternal complications from a ruptured uterus include hemorrhage and hypovolemic shock. Close observation in triage with continuous fetal monitoring and repeat sterile vaginal exam in 2 to 4 hours b. Admission to L & D triage, continuous fetal monitoring, and start oxytocin augmentation 2. Admission to L & D triage and repeat cesarean delivery without a trial of labor d. None of the above pulse rate is 120 bpm, she appears to be in significant pain, is unable to answer questions, and her abdomen feels rigid. What does this patient now have as a result of her abruption and significant blood loss Further imaging to rule out placenta accreta (or increta/percreta) can be helpful in cases such as this where the diagnosis is unclear on ultrasound. Further imaging reveals complete anterior previa with evidence of placental invasion into the bladder. She denies contractions but on the tocometer is noted to have contractions every 2 to 4 minutes. A sterile speculum examination is performed and her cervix is dilated to approximately 2 cm. Of note, she does not desire future fertility and would like a tubal ligation after delivery, if possible. Vignette 1 Question 4 Answer A: the most appropriate management plan if the patient continues to labor would be to tocolyze her so as to prolong the pregnancy long enough to administer a steroid course to improve prior to completion of the steroid course. It is reasonable to attempt to tocolyze at this early gestation as long as the patient remains hemodynamically stable with minimal vaginal bleeding. However, if the patient bleeds significantly, she may need to be delivered prior to completion of the steroid course. Although in some cases it is reasonable to allow a patient to have a trial of labor after two cesarean sections, it is not appropriate in a patient with a complete placenta previa, as it would result in significant hemorrhage and likely both maternal and fetal compromise. Because the patient has had two prior cesarean sections, has complete placenta previa, and is now experiencing hematuria, this is concerning for a placenta percreta with invasion into the bladder. With the progression of pregnancy, more than 90% of low-lying placentas identified early in pregnancy will appear to move away from the cervix and out of the lower uterine segment. However, placenta previa occurs in as many as 1% to 4% of women with a prior cesarean section. If placenta previa persists, it can be complicated by an associated placenta accreta (placenta previa accreta) in approximately 5% of cases.
Syndromes
- Severe headache
- Refraction test
- Blockage in the nose caused by a crooked, bent, or deformed nasal septum (the structure that separates the nostrils)
- Acute bilateral obstructive uropathy
- Audiometry
- Cervical polyps
- Blockage of blood vessels in the leg
- Are all the fontanelles bulging?
Purchase imodium visa
Warfarin accumulates in the liver atrophic gastritis symptoms uk cheap imodium online visa, where the two isomers are metabolized via distinct pathways. Whether this approach will increase the efficacy and/or safety of warfarin therapy is uncertain. In addition to genetic factors, the anticoagulant effect of warfarin is influenced by diet, drugs, and various disease states. A wide variety of drugs can alter absorption, clearance, or metabolism of warfarin. Because of the variability in the anticoagulant response to warfarin, coagulation monitoring is essential to ensure that a therapeutic response is obtained. Consequently, less sensitive thromboplastins will prompt the administration of higher doses of warfarin to achieve a target prothrombin time. This is problematic because higher doses of warfarin increase the risk for bleeding. Furthermore, every laboratory must establish the mean normal prothrombin time with each new batch of thromboplastin reagent. To accomplish this, the prothrombin time must be measured in fresh plasma samples from at least 20 healthy volunteers using the same coagulometer that is used for patient samples. A minimum 5-day course of parenteral anticoagulation is recommended to ensure that the levels of prothrombin have been reduced into the therapeutic range with warfarin. Because warfarin has a narrow therapeutic window, frequent coagulation monitoring is essential to ensure that a therapeutic anticoagulant response is obtained. Bleeding complications may be mild, such as epistaxis or hematuria, or more severe, such as retroperitoneal or gastrointestinal bleeding. These patients should be given 5 to 10 mg of vitamin K by slow intravenous infusion. For life-threatening bleeds, or if patients cannot tolerate the volume load, prothrombin complex concentrates can be used. Those with gastrointestinal bleeding often have underlying peptic ulcer disease or a tumor. This is of particular concern at delivery, when trauma to the head during passage through the birth canal can lead to intracranial bleeding. Because of these potential problems, warfarin is rarely used in pregnancy, particularly in the first and third trimesters. Special Problems Patients with a lupus anticoagulant or those who need urgent or elective surgery present special challenges. Skin Necrosis A rare complication of warfarin, skin necrosis usually is seen 2 to 5 days after initiation of therapy. Well-demarcated erythematous lesions form on the thighs, buttocks, breasts, or toes. Examination of skin biopsy specimens taken from the border of these lesions reveals thrombi in the microvasculature. Warfarin-induced skin necrosis is seen in patients with congenital or acquired deficiencies of protein C or protein S (see Chapters 128, 129, and 142). Initiation of warfarin therapy in these patients produces a precipitous fall in plasma levels of proteins C or S, thereby eliminating this important anticoagulant pathway before warfarin exerts an antithrombotic effect through lowering of the functional levels of factor X and prothrombin. Why the thrombosis is localized to the microvasculature of fatty tissues is unclear. Treatment involves discontinuation of warfarin and reversal with vitamin K, if needed. Because of the potential for skin necrosis, patients with known protein C or protein S deficiency require overlapping treatment with a parenteral anticoagulant when initiating warfarin therapy. Dabigatran the active moiety of dabigatran etexilate, dabigatran targets the active site of thrombin and blocks its procoagulant activities. Mechanism of Action Dabigatran etexilate is a prodrug with an oral bioavailability of 6% to 7%. Once absorbed, the drug is rapidly biotransformed by esterases to dabigatran, the levels of which peak 1 to 2 hours after oral administration. Dosing For thromboprophylaxis after hip or knee replacement surgery, dabigatran is given once daily at a dose of 220 or 150 mg; a half-dose is given on the day of surgery. In patients with atrial fibrillation, dabigatran is given at a dose of 150 mg or 110 mg twice daily. A dose of 75 mg twice daily is used in the United States for patients with a creatinine clearance of 15 to 30 mL/min, whereas the 150 mg twicedaily dose is recommended for those with a creatinine clearance over 30 mL/min; the 110-mg twice-daily dose is not licensed in the United States (see Chapters 147 and 149). For treatment of venous thromboembolism, dabigatran is given at a dose of 150 mg twice daily (see Chapter 144). Pregnancy Warfarin crosses the placenta and can cause fetal abnormalities or bleeding. The fetal abnormalities include a characteristic embryopathy, which consists of nasal hypoplasia and stippled epiphyses. The risk for embryopathy is highest if warfarin is given in the first trimester of pregnancy. Central nervous system abnormalities also can occur with exposure to coumarins at any time during pregnancy. Compared with warfarin, Chapter 151 Antithrombotic Drugs 2115 there may be a small increase in the risk for myocardial infarction with dabigatran. This increase translates into 2 additional myocardial infarcts for every 1000 patients treated. Unactivated prothrombin complex concentrates do not reverse the anticoagulant effects of dabigatran. The dose is reduced to 15 mg once daily for those with a creatinine clearance of 15 to 49 mL/min. For treatment of venous thromboembolism, rivaroxaban is started at a dose of 15 mg twice daily for 3 weeks and the dose is then reduced to 20 mg once daily thereafter. When used as an adjunct to antiplatelet therapy in stabilized patients with acute coronary syndrome, rivaroxaban is given at a dose of 2. Side Effects Rivaroxaban is well tolerated and is not associated with dyspepsia or hepatic toxicity. Although prothrombin complex concentrate reverses the anticoagulant effects of rivaroxaban, its utility for treatment of bleeding is uncertain. Indications In many countries, dabigatran is licensed for prophylaxis after hip or knee replacement surgery. Although not inferior to once-daily lowmolecular-weight heparin for this indication, once-daily dabigatran was inferior to twice-daily low-molecular-weight heparin for thromboprophylaxis after elective knee replacement surgery. At the 150-mg twice-daily dose, dabigatran was superior to warfarin for reduction in both hemorrhagic and ischemic stroke. In those over the age of 75 years, there is more gastrointestinal bleeding with this dose of dabigatran than with warfarin. However, the dose was selected because pharmacokinetic data revealed similar drug exposure in those with reduced renal function as produced by the 150-mg twice-daily dose in those with a creatinine clearance over 30 mL/min. Although drug exposure is similar, the half-life of dabigatran is prolonged to several days in those with impaired renal function. For treatment of venous thromboembolism, dabigatran is not inferior to warfarin and is associated with reduced major plus clinically relevant nonmajor bleeding. Dabigatran is started after a 5- to 7-day course of heparin or low-molecular-weight heparin. Current licensed indications for rivaroxaban include (1) thromboprophylaxis after hip or knee replacement surgery, situations in which the drug is usually given for 2 and 4 weeks, respectively, and (2) as an alternative to warfarin for stroke prevention in atrial fibrillation. The drug also is licensed in some countries for treatment of deep venous thrombosis and is under consideration for treatment of pulmonary embolism and for secondary prevention in stabilized patients with acute coronary syndromes. Rivaroxaban An oral factor Xa inhibitor, rivaroxaban is an active drug that targets the active site of factor Xa even when the enzyme is incorporated in the prothrombinase complex. Apixaban Another oral factor Xa inhibitor, apixaban is licensed in many countries, but not the United States, for thromboprophylaxis after hip or knee replacement surgery. It is under consideration for licensing as an alternative to aspirin or warfarin for stroke prevention in atrial fibrillation. Mechanism of Action Rivaroxaban has an oral bioavailability of 80%, and plasma levels peak 2 to 3 hours after drug administration.
Purchase 2 mg imodium with amex
There is little data on the current prevalence of thrombocytopenia in patients under active antiviral treatment gastritis diet ������� buy discount imodium line. Direct infection of megakaryocytes results in defective platelet production and megakaryocytic apoptosis. Epidemiologic studies suggest that the pathogenesis of thrombocytopenia is partially dependent on disease burden. An open label trial of interferon- in a cohort of predominately homosexual men documented responses in 9 of 16 (56%) patients, with responses occurring as early as 2 weeks after the initiation of treatment. Such rapid responses preclude the possibility that improvement in the platelet count is due solely to suppression of concomitant hepatitis C virus infection. Major bleeding is rare, and only a few cases of fatal hemorrhage have been reported. This life-threatening disorder is characterized by thrombocytopenia and microangiopathic (fragmentation) hemolytic anemia. The original description of this disorder emphasized a classic pentad of fever, thrombocytopenia, microangiopathic hemolytic anemia, renal failure, and neurologic abnormalities. However, most patients present with only one or two manifestations of the original pentad, and isolated thrombocytopenia may be the initial finding. Therefore it is essential that the evaluation of thrombocytopenia include a careful review of the peripheral blood smear. Corticosteroids such as prednisone (1 mg/kg/day) also can be given with the exchanges. Patients who relapse can be treated with repeat exchange combined with immunosuppressive therapy including agents such as vincristine or rituximab. Recent data suggest that the primary event leads to unregulated complement activation due to either inhibitors of complement regulatory protein such as complement H or congenital abnormalities in complement regulation. Many patients will respond to aggressive plasma exchange, but complete remissions are rare. However, 53% of the thrombotic events occurred in individuals without history of recent hospitalization. The development of a thromboembolic event was associated with statistically increased mortality in all groups. There is a well-documented association between acute and chronic inflammation and activation of the hemostatic system. Oral anticoagulants can be started immediately upon achieving therapeutic heparin levels, and under optimal circumstances heparin treatment can be completed and the patient discharged from the hospital within 5 to 7 days. In patients in whom maintaining therapeutic levels is difficult, home monitoring using devices approved by the U. However, the decision to extend anticoagulation to prevent recurrence of thrombosis must be weighed against the significant risk for bleeding in this population. Abnormalities of glucose metabolism and serum lipids are commonly observed with protease inhibitor therapy. Insulin resistance is associated with acquired defects in the fibrinolytic system, including increased levels of plasminogen activator inhibitor and tissue plasminogen activator. Similar fibrinolytic abnormalities have been observed in patients with documented insulin resistance who are treated with protease inhibitors. The majority of reported hemostatic abnormalities appear primarily to affect the protein C and S inhibitory mechanisms. Chen M, Chien-Ching H, Fang C, et al: Reconstituted immunity against persistent parvovirus B19 infection in a patient with acquired immunodeficiency syndrome after highly active antiretroviral therapy. Roberts Parasitic diseases are not common in medical, let alone hematologic, practice in North America or Europe. Although some significant parasitic diseases are transmitted in temperate climates, the majority of parasites of significance to human health are endemic in the tropical world. This reflects not only socioeconomic circumstances but also the origin of our species in tropical Africa, where the human host, parasites, and also vectors have established complex relationships over evolutionary timescales. Even here, there are marked variations in practice in North America and Europe, where the United Kingdom reports more cases of imported malaria than the United States and indeed has a 10-fold greater incidence of malaria per capita, reflecting the increased frequency of travel to and from endemic areas compared to North American populations. Malaria, leishmaniasis, trypanosomiasis, and babesiosis may present directly or indirectly to hematologists. This account will concentrate on the biologic, clinical, and hematologic features of these infections and the hematologic aspects or complications of their treatment. Comprehensive accounts of the general medical aspects of these diseases are provided in many recent textbooks. Recently a fifth species, Plasmodium knowlesi, has been shown to cause human infection in some parts of Southeast Asia (for review see reference 5). In endemic areas, a significant proportion of the mortality and morbidity is due to anemia. In Europe and North America, malaria is not infrequently a clinical problem in travelers or recent arrivals from malaria-endemic areas, and hematologists may be involved in the diagnosis and management of the disease. Moreover, in nonendemic areas, malaria may cause a fatal transfusion-transmitted infection, and detection of blood donors who may be carrying the disease represents a major challenge for blood services. Epidemiology Approximately 1000 million people live in areas of endemic or epidemic malaria. The global mortality and morbidity have been revised to 350 million cases and 1 million deaths per year following an evaluation of the prevalence of infection in Southeast Asia. Within these limits transmission does not occur above 1500 m in arid regions or in the Central and South Pacific (due to the absence of suitable vectors). The intensity of transmission determines the distribution of clinical symptoms in different age-groups. Finally, if the rate of transmission is very low, few cases of malaria are seen in any age-group and such populations would have little natural immunity. In such areas, a sudden increase in vectorial capacity (through the accidental introduction of efficient vectors or higher density, biting, or survival of the resident vectors), more rapid parasite sporogony, or migration of infected or nonimmune populations can result in epidemics where large numbers fall ill in all age-groups. The transition from high to low transmission has been classified by holoendemicity, hyperendemicity, mesoendemicity, and hypoendemicity. These categories can be related epidemiologically to age-specific rates of parasite prevalence or splenomegaly and theoretically to the reproductive ratio of malarial infection. Sickle cell trait and thalassemia traits protect from infection and are truly polymorphic characteristics in many parts of the world. Understanding the genetic epidemiology has provided the foundation of population genetics and has provided classic examples of principles of genetic selection in vivo-for example, balancing selection for sickle cell trait and negative epistasis for sickle cell trait and -thalassemia. In endemic areas, these genetic diseases represent major public health problems (for review see references 9 and 10). Areas are colored according to malaria endemicity (prevalence): light green, hypoendemic (areas in which childhood infection prevalence is less than 10%); medium green, mesoendemic (areas with infection prevalence between 11% and 50%); dark green, hyperendemic and holoendemic (areas with an infection prevalence of 50% or more); unclassified areas (yellow) represent only 6% of the global population at risk and are due to discrepancies in recent data. Grey areas are a combined mask of areas outside of the transmission limits and areas of population density less than 1 person/km2. Ligands are expressed at the surface of the infected red blood cell that mediate adhesion to host receptors on venular endothelium. These trophozoites no longer circulate throughout the body but are sequestered in the peripheral circulation. Nuclear division begins, at approximately 30 hours, to form schizonts, containing up to 32 merozoites. At 48 hours, the red blood cell is ruptured to release the merozoites into the circulation to continue further cycles of asexual multiplication. The erythrocytic cycle of schizogony may achieve a 10-fold increase in parasitemia in vivo and a patent or microscopically detectable infection 6 days after the liver stage is completed.
Cheap imodium 2 mg visa
Interestingly gastritis symptoms causes and treatment order imodium 2 mg line, it was demonstrated that high cholesterol levels (>240 mg/ dL) impair the antithrombotic effect of low-dose aspirin in a microvascular injury model. The risk of bleeding is increased even with doses of aspirin as low as 10 to 30 mg/day20; the protective effect of resistant coatings is unproved. Because low doses have been shown to be effective in preventing thrombosis, it is likely that the risk of bleeding can be reduced while maintaining an antiplatelet effect. The life span of platelets is 8 to 10 days, and every day nearly 10% to 12% of the platelets are replaced by new platelets. The capacity of the bone marrow to produce new platelets, the aspirin dosage, the aspirin exposure time (spot doses or regular use), and individual parameters may be different among individuals. The major limitations of flow cytometry analysis are the cost and need for expert interpretation. Citrated blood passes through an aperture within a coated membrane at the end of the cartridge, and the time for occlusion of this aperture is measured. VerifyNow is another cartridge-based system designed to assay platelet aggregation in the presence of antiplatelet drugs; the aspirin response is assessed by aggregation in response to arachidonic acid. Clinical resistance is a definition applied to patients who experienced a new thrombotic event while receiving regular and effective-dose aspirin therapy. Because arterial thrombosis is a multifactorial process, the inhibition of one pathway of platelet activation may be insufficient to prevent thrombosis. In some patients, aspirin may not produce the expected effects on one or more screening laboratory tests. They investigated these patients on regular aspirin therapy, after withdrawal of aspirin for 7 days, and after an observed ingestion of 325 mg of aspirin. After being observed to take the 325 mg aspirin, however, all patients but one displayed inhibition of aggregation. The likelihood that aspirin will cause bleeding is increased in the presence of other hemostatic defects. The risk of bleeding is increased if aspirin is given simultaneously with warfarin in high-intensity anticoagulation regimens (international normalized ratio, 3. Approximately 15% of the absorbed prodrug is converted to its active form in the liver by the cytochrome P450 system. At lower doses of clopidogrel, the full pharmacologic effect requires 4 to 7 days, often doubling the bleeding time. When a rapid therapeutic effect is desired, clopidogrel can be given with a loading dose of 300 to 600 mg. At these doses, clopidogrel significantly impairs platelet function within 90 minutes of administration. The causes of clopidogrel resistance are many and include noncompliance; drug interactions (proton pump inhibitors may affect clopidogrel metabolism); and various genetic polymorphisms that control clopidogrel absorption, metabolic activation, and biological activity. Prasugrel Prasugrel is a third-generation oral thienopyridine that is converted to its active form in the liver much more efficiently than is clopidogrel. Three groups of patients are at particularly high risk of bleeding: those older than 75 years of age, those weighing less than 60 kg, and patients with history of stroke or transient ischemic attack. Platelets contain two P2Y receptors, P2Y1 and P2Y12, complexed to the heterotrimeric G proteins Gq and Gi2, respectively. P2Y12, coupled to inhibition of adenylyl cyclase, mediates the amplification of the aggregation response and increases thrombus stability. Ticagrelor is given orally and is metabolized by the liver cytochrome P450 system to the active metabolite, which has a half-life of approximately 12 hours. Ticagrelor has some advantages over thienopyridines such as rapid action, reversible and consistent antiplatelet effect with only a small increase in the risk of bleeding, and efficacy in patients with genetic resistance to clopidogrel. The drug was recently approved in the United States for the treatment of acute coronary syndromes. Dual therapy with aspirin and clopidogrel improves the clinical benefit of antiplatelet therapy, but aggregation is still able to proceed through the action of other agonists such as thrombin. Although these agents share many similarities in their pharmacodynamics and therapeutic effects, they also have a number of clinically important pharmacokinetic differences. This explains why patients with thrombocytosis may require larger weight-adjusted doses of abciximab to attain a therapeutic antiplatelet effect65 and why patients with lower platelet counts treated with the usual dose of abciximab display more profound platelet inhibition. Abciximab is not excreted in the urine and is probably metabolized by the reticuloendothelial system at the time platelets (with bound abciximab) are cleared from the circulation. The dose of abciximab does not have to be adjusted in patients with renal impairment. Although a daily platelet turnover rate of 10% would predict that no abciximab would be detected in blood after 10 days of its administration, platelet-bound abciximab has been observed up to 3 weeks after its initial administration, suggesting platelet-to-platelet redistribution of the drug or release of new platelets from megakaryocytes that had previously bound the drug. Without platelet transfusions, platelet aggregation generally returns to baseline levels within 12 to 24 hours after discontinuing abciximab. Eptifibatide differs pharmacokinetically from abciximab in several important ways. Platelet aggregation returns to normal in approximately 4 hours, with the bleeding time normalizing within 1 hour. However, its half-life is even shorter than that of eptifibatide (2 hours), and its antiplatelet effect is reversed rapidly after discontinuation of infusion. It is therefore essential that a platelet count be obtained 2 to 4 hours after initiating treatment. Most patients with severe thrombocytopenia respond well to platelet transfusions and their platelet counts usually recover within 5 days, although they may take more than 1 week to do so. Many patients require readministration of abciximab, raising the possibility that antibodies against the drug will complicate therapy. The safety of readministration was studied systematically in the ReoPro Readministration Registry. However, thrombocytopenia tended to be profound, relatively refractory to platelet infusion, and more often delayed. It is therefore recommended that clinicians obtain a second platelet count 24 hours after the readministration of abciximab and that they maintain a high index of suspicion for the delayed development of abciximab-induced thrombocytopenia. Bleeding complications are quite common, especially in the inguinal area, where the femoral artery has been breached during procedures. Patients on antiplatelet therapy can be divided into two groups according to the risk of thrombotic complications. Low-risk patients include those receiving single antiplatelet therapy (usually low-dose aspirin) for primary prophylaxis of arterial disease. The high-risk group includes patients having had a recent (within 3-6 months) myocardial infarction, stroke, or peripheral arterial thrombosis and patients who have had recent implantation of a coronary stent. Endothelization of bare metal stents requires 4 to 6 weeks but could take up to 1 year for drug-eluting stents. Approximately 6% to 8% of patients taking combined antiplatelet therapy for coronary artery disease also receive oral anticoagulants due to cardiac rhythm or valve problems. Aspirin and clopidogrel irreversibly inhibit platelets; restoration of normal platelet hemostasis thus requires a few days after cessation of the drug. Hypoxia, hypercoagulability, and inflammatory responses caused by the operation are also associated with stent thrombosis and adverse cardiac events in these patients. If surgery is required, it is recommended that both aspirin and clopidogrel be continued. Caffeine, at a dosage of 250 mg orally three times a day for 1 week, was demonstrated to reduce platelet aggregation in healthy subjects. Although anagrelide inhibits platelet aggregation in vitro, it surprisingly also inhibits megakaryocyte maturation and proliferation and causes thrombocytopenia in humans by a mechanism that is poorly understood. Several reports of sildenafil-associated bleeding have appeared, including epistaxis,84,85 hemorrhoidal bleeding,86 spontaneous intracranial hemorrhage,87 and acute variceal bleeding. Despite the potent inhibition of platelet aggregation by prostacyclin in vitro, the effects on the bleeding time are minimal and inconsistent. These drugs are used for pulmonary arterial hypertension and peripheral artery disease.
Quality 2mg imodium
Obstetricians also use the term grand multip gastritis omeprazole order imodium on line amex, which refers to a woman whose parity is greater than or equal to 5. A myriad of physiologic changes occur in a pregnant woman, which affect every organ system. In a patient who has regular menstrual cycles and is sexually active, a period delayed by more than a few days to a week is suggestive of pregnancy. Pregnancy dating can be confirmed and should be consistent with the examination of the uterine size at the first prenatal appointment. Approximately 5% to 15% of women may be oligo-ovulatory, meaning they ovulate beyond the usual 14th day of the cycle. The increase in cardiac output is first due to an increase in stroke volume and is then maintained by an increase in heart rate as the stroke volume decreases to near prepregnancy levels by the end of the third trimester. Systemic vascular resistance decreases during pregnancy, resulting in a fall in arterial blood pressure. This decrease is most likely due to elevated progesterone, leading to smooth muscle relaxation. There is a decrease in systolic blood pressure of 5 to 10 mm Hg and in diastolic blood pressure of 10 to 15 mm Hg that nadirs at week 24. Because ultrasound dating of pregnancy decreases in accuracy as the pregnancy progresses, determining and confirming pregnancy dating at the first interaction between a pregnant woman and the health care system is imperative. A woman who presents to the emergency department may not return for prenatal care, so dating should be confirmed at that visit. Pregnancy dating is particularly important because a number of decisions regarding care are based on accurate dating. This gradient facilitates oxygen delivery to the fetus and carbon dioxide removal from the fetus. This has been termed morning sickness even though it can occur anytime throughout the day. Hyperemesis gravidarum refers to a severe form of morning sickness associated with weight loss (5% of prepregnancy weight) and ketosis. During pregnancy, the stomach has prolonged gastric emptying times and the gastroesophageal sphincter has decreased tone. Together, these changes lead to reflux and possibly combine with decreased esophageal tone to cause ptyalism, or spitting, during pregnancy. The large bowel also has decreased motility, which leads to increased water absorption and constipation. Renal the kidneys increase in size and the ureters dilate during pregnancy, which may lead to increased rates of pyelonephritis. There is a slight decrease in the concentration of platelets, probably secondary to increased plasma volume and an increase in peripheral destruction. Although in 7% to 8% of patients the platelet count may be between 100 and 150 million/mL, a drop in the platelet count below 100 million/mL over a short time is not normal and should be investigated promptly. Pregnancy is considered to be a hypercoagulable state with an increase in the number of thromboembolic events. The increased rate of thromboembolic events in pregnancy may also be secondary to the other elements of Virchow triad, that is an increase in venous stasis and vessel endothelial damage. Eventually, the placenta takes over progesterone production and the corpus luteum degrades into the corpus albicans. Progesterone causes relaxation of smooth muscle, which has multiple effects on the gastrointestinal, cardiovascular, and genitourinary systems. Musculoskeletal and Dermatologic the obvious change in the center of gravity during pregnancy can lead to a shift in posture and lower back strain, which worsens throughout pregnancy, particularly during the third trimester. Numerous changes occur in the skin, including spider angiomata and palmar erythema secondary to increased estrogen levels and hyperpigmentation of the nipples, umbilicus, abdominal midline (the linea nigra), perineum, and face (melasma or chloasma) secondary to increased levels of the melanocytestimulating hormones and the steroid hormones. Pregnancy is also associated with carpal tunnel syndrome, which results from compression of the median nerve. The caloric requirement is increased by 300 kcal/day during pregnancy and by 500 kcal/day when breastfeeding. Thus, pregnancy is not the caloric equivalent of eating for two; more accurately, it is approximately eating for 1. Overweight women are advised to gain less, between 15 and 25 lb; underweight women are advised to gain more, 28 to 40 lb. Unfortunately, a large proportion of women gain more than the recommended amount, which contributes to a number of complications in pregnancy plus postpartum weight retention and downstream obesity. It is the responsibility of each prenatal care provider to review diet and exercise during pregnancy. The increased estrogen is produced primarily by the placenta, with the ovaries contributing to a lesser degree. Unlike estrogen production in the ovaries, where estrogen precursors are produced in ovarian theca cells and transferred to the ovarian granulosa cells, estrogen in the placenta is derived from circulating plasma-borne precursors produced by the maternal adrenal glands. Fetal well-being has been correlated with maternal serum estrogen levels, with low estrogen levels being associated with conditions such as fetal death and anencephaly. Many patients develop iron deficiency anemia because of the increased demand on hematopoiesis both by the mother and the fetus. These are designed to compensate for the increased nutritional demands of pregnancy. Furthermore, any patient whose hematocrit falls during pregnancy is advised to increase iron intake with oral supplementation (Table 1-2). It should occur early in the first trimester, between 6 and 10 weeks, although occasionally patients will not present for their initial prenatal visit until later in their pregnancy. Finally, a complete medical, surgical, family, and social history should be obtained. They include a series of outpatient office visits that involve routine physical examinations and various screening tests that occur at different points in the prenatal care. Important issues of prenatal care include initial patient evaluation, routine patient evaluation, nutrition, disease states during the pregnancy, and preparing for the delivery. Accurate dating is crucial for all subsequent obstetrical evaluations and interventions. A urine pregnancy test should be sent if the patient is not entirely certain she is pregnant. While there is some debate over the use of routine toxoplasma titers, they are often ordered as well. In addition to this battery of tests, there are a variety of other screens offered to high-risk patients (Table 1-4). Maternal blood pressure decreases during the first and second trimesters and slowly returns to baseline during the third trimester; elevation may be a sign of preeclampsia. Maternal weight is followed serially throughout the pregnancy as a proxy for adequate nutrition. Also, large weight gains toward the end of pregnancy can be a sign of fluid retention and preeclampsia. Measurement of the uterine fundal height in centimeters corresponds roughly to the weeks of gestation. At each visit, the patient is asked about symptoms that indicate complications of pregnancy. These symptoms include vaginal bleeding, vaginal discharge or leaking of fluid, and urinary symptoms. In addition, after 20 weeks, patients are asked about contractions and fetal movement. Vaginal bleeding is a sign of possible miscarriage or ectopic pregnancy in the first trimester and of placental abruption or previa as the pregnancy advances. Vaginal discharge may be a sign of infection or cervical change, whereas leaking fluid can indicate ruptured fetal membranes. While irregular (Braxton Hicks) contractions are common throughout the third trimester, regular contractions more frequent than five or six per hour may be a sign of preterm labor and should be assessed. First-Trimester Visits During the first trimester, patients-particularly nulliparous women-need to be familiarized with pregnancy.
Purchase 2mg imodium with mastercard
Developmental hemostasis is the term applied to the evolution of the hemostatic and fibrinolytic systems through infancy and childhood gastritis medicine over the counter cheap imodium 2mg line. The template bleeding time is reported to be normal in neonates, but this is an unreliable test in neonatology and is not recommended for bleeding evaluations. Investigations into neonatal hemostatic pathology are limited by the lack of normal reference values for the neonatal population and the difficulties associated with obtaining clean blood samples for testing. The hemostatic system evolves throughout childhood and most rapidly during the neonatal period. Changes in the plasma concentrations of proteins involved in blood coagulation lead to a dynamic group of reference ranges for preterm and term infants. Although different from adult values, these reference ranges are neither abnormal nor pathologic. The relative rarity of hemorrhagic or thrombotic complications in this population argues that the neonatal coagulation system is physiologically replete. Blood Coagulation Proteins the synthesis of fetal and neonatal coagulation proteins begins at approximately 10 weeks of gestation, and plasma concentrations of these proteins increase with gestational age. The physiologic ranges for coagulation factors in healthy newborns who have received intramuscular vitamin K after delivery are shown in Table 152-2. The concept of developmental hemostasis is now widely accepted, and her seminal papers describing the reference ranges for healthy premature and full-term neonates are still widely quoted. Thus prior publications of defined reference ranges for neonates may not be relevant because coagulation assay results vary depending on the type of analyzer and reagents used. Although the absolute values are reagent- and analyzer-specific, the changes in functional protein levels lead to corresponding changes in global tests of coagulation. However, samples from premature infants and 2120 Regulation of Thrombin Despite decreased and delayed thrombin generation, neonates have excellent hemostasis. Thrombin regulation in neonatal plasma is similar to that in plasma from adults who are receiving therapeutic doses of anticoagulants. The concentration of thrombin generated in neonatal plasma is proportional to the available prothrombin concentration, whereas the rate of thrombin generation depends on the level of other procoagulant proteins. Neonatal fibrin clots bind less thrombin than clots formed in adult plasma, in part because of lower levels of thrombin generation. Reduced thrombin generation and less fibrin-bound thrombin may protect neonates from thrombosis. Plasminogen levels are lower in neonates than in adults, and fetal plasminogen binds to cellular receptors with lower affinity because of its increased sialic acid and mannose content. Neonates with severe plasminogen deficiency have only a minimal increased risk for thrombosis, and most of their clinical findings are the result of impaired extravascular fibrinolysis. Imbalance in the fibrinolytic system, whether hereditary or acquired, can lead to thrombotic or bleeding complications. The efficacy and safety of fibrinolytic therapy may be influenced by age-dependent differences in the fibrinolytic system. Data are lacking on the optimal doses of fibrinolytic agents for the pediatric population, especially for neonates. The contribution of differences between the neonatal and adult fibrinolytic systems to the protection from thromboembolic complications in childhood remains to be elucidated. Platelets the platelet count and mean platelet volume in neonates are similar to those in adults as is platelet ultrastructure. Neonatal platelets exhibit reduced phospholipid metabolism, calcium mobilization, granule secretion, and aggregation in response to agonists compared with adult platelets. Platelet function is reduced at birth, which may reflect the platelet activation and degranulation that occurs during labor and delivery. Flow cytometric studies using monoclonal antibodies directed against platelet activation markers indicate that platelets from cord blood or from neonates on the first postnatal day are hyporeactive compared with adult platelets. In neonates the 2-macroglobulin concentration is twofold higher than that in adults. The overall capacity of newborn plasma to inhibit thrombin is similar to that of adult plasma due in part to the increased binding of thrombin by 2-macroglobulin. Regulation of thrombin generation is accomplished by upstream inhibition of the clotting proteins in the prothrombinase and tenase complexes (see Chapters 128 and 129). Plasma concentrations of protein C are low at birth and gradually increase to adult levels by 6 months of age. Although the total concentration of protein S is low at birth, the functional activity of protein S is comparable to that in adults because low levels of C4b-binding protein result in more free protein S. The interaction of protein S with activated protein C in neonatal plasma may be limited by the elevated levels of 2macroglobulin. Free tissue factor pathway inhibitor levels are lower than in adults, despite total tissue factor pathway inhibitor levels being similar in neonatal and adult plasma. The Fibrinolytic System Although the levels of some of the components of the fibrinolytic system in neonates are different from those in adults, the clinical relevance of this finding is probably minimal. The fibrinolytic system regulates fibrin deposition by generating plasmin, which solubilizes fibrin. At birth the fibrinolytic system has all the key components, but there are important age-related differences in the quantity and quality of the fibrinolytic proteins and enzymes. Despite lower levels of fibrinolytic components, the newborn fibrinolytic system is still effective. The whole-blood clotting time and euglobulin clot lysis time are global assays of fibrinolytic activity but reflect only part of the physiologic fibrinolytic potential. Maneuvers that induce the release of endogenous fibrinolytic components, such as venous occlusion, desmopressin infusion, or exercise, provide more sensitive measures in vivo fibrinolytic activity. Circulating levels of endothelial cell adhesion markers vary with age, implying dynamic expression and/or secretion of these proteins as a function of age. In sick infants, acquired factor deficiencies or thrombocytopenia are frequently to blame, but rare congenital factor deficiencies can also manifest with neonatal bleeding. Thromb Haemost 95:362, 2006; and Andrew M, Paes B, Milner R, et al: Development of the human coagulation system in the full-term infant. Initial empirical therapy consists of platelet and/or factor supplementation, which is often administered while diagnostic studies are under way. Evaluation of the Bleeding Neonate Neonatal, peripartum, maternal, and family history are each important in the evaluation of a newborn with hemorrhagic complications. Maternal history of prior pregnancies, medications, and illnesses can provide clues to the hemostatic disorder in the neonate. The family history, such as parental ethnicity and consanguineous marriage, may help to identify congenital bleeding disorders. Maternal infection, drug use, or immune thrombocytopenia can lead to neonatal thrombocytopenia. Wellappearing newborns are more likely to have localized bleeding or ecchymoses because of thrombocytopenia from a transplacental antibody, vitamin K deficiency, or a rare inherited factor deficiency. Neonatal Thrombocytopenia the following factors are important to consider when evaluating neonates with thrombocytopenia: congenital or acquired, sick or well, maternal antibody or drug, and platelet size. The estimated prevalence of thrombocytopenia is in the range of 1% to 5% of all newborns. With severe thrombocytopenia, platelet transfusion may be necessary to treat or decrease the risk for bleeding. Causes of neonatal thrombocytopenia include decreased platelet production, increased platelet consumption, and/or hypersplenism. In wellappearing newborns, thrombocytopenia is usually immune mediated and related to maternal transplacental immunoglobulin G antibodies or drugs. Platelet production can be impaired with hypoxic-ischemic injury, perhaps because fetal megakaryocytes are particularly sensitive to hypoxia. Newborns from pregnancies complicated by intrauterine growth restriction or pregnancy-induced hypertension frequently exhibit transient mild to moderate thrombocytopenia.