Purchase 800mg mesalamine visa
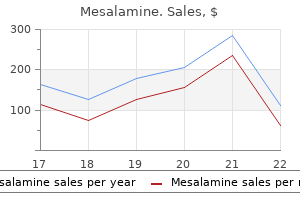
A randomized comparison of reversed and in situ vein grafts to crural arteries demonstrated no significant patency or limb salvage differences treatment xdr tb guidelines purchase cheap mesalamine on-line, except for veins less than 3mm in distended diameter. To facilitate the use of vein as the conduit, the grafts should be as short as possible. No other patent arterial segments were available as targets for revascularization, and no autologous vein available for a bypass. Any technical error in graft preparation, tunneling, or anastomotic construction will result in failure. Magnification and microsurgical instruments are often required, and care must be taken to treat outflow arteries atraumatically and to preserve all outflow branches, even the small ones that are unnamed. Completion arteriography (cinefluoroscopy) is also essential, as with all infrapopliteal bypasses, to assure good anastomotic configuration and bypass flow rates. If spasm or decreased flow is noted, vasodilators (nitroglycerin, papaverine) may be helpful. Although these techniques can work well in the short term, long-term results are unclear, and it remains to be determined how these results will compare with bypass operations. Newer Techniques for Redo Procedures After Failed Bypasses It is well known that infrainguinal revascularization procedures, both endovascular and open surgical, are associated with progressive failure due to a diminished luminal caliber, followed by thrombosis. This is due to both intimal hyperplasia, which is largely a reaction to vascular injury and progression of the arteriosclerotic process. This may be due to healing of the original gangrenous or ulcerated lesion and greater blood flow is required to achieve healing than to maintain it. Alternatively the maintenance of a healed foot after a revascularization failure may be, due to improved collateral blood flow or absence of the trauma or infection that initially contributed to the gangrene or ulceration. Management strategies for patients with failed revascularization procedures should be influenced by the understanding that critical ischemia might not recur. Only if critical ischemia is present should a secondary intervention be undertaken, because secondary procedures are generally more difficult and have worse results than primary procedures. The one exception is when a primary procedure is determined by physical examination, symptoms, or noninvasive testing to be in a failing mode. A full description of all possible redo procedures that are indicated when a primary bypass (with vein or prosthetic) fails is beyond the scope of this chapter and is available elsewhere. First, endovascular interventions should always be considered as the first option in patients requiring a redo procedure, even if the original revascularization was a bypass. Improved technology that was previously unavailable may provide sufficient increased blood flow to maintain foot viability. Second, redissection of previously dissected arteries, particularly in the groin, should be avoided because they are difficult to perform and prone to an increased risk of infection. If a totally new bypass is required, as is usually the case when a failed vein graft cannot be freed of clot, alternate or new approaches to patent arteries should be used. Fourth, if the failed bypass is a prosthetic conduit, an effort should be made to restore patency percutaneously using mechanical thrombectomy devices and lytic agents. This is, often facilitated if the proximal anastomotic hood of the original graft can be seen angiographically to facilitate guidewire passage. Only if interventional procedures fail should reoperation be undertaken; this is generally required when the proximal or distal organized thrombotic plug cannot be lysed or removed by percutaneous means. The graft is opened longitudinally and the liquefied clot is removed gently with balloon catheters. Fluoroscopy with contrast injections is used to identify any inflow or anastomotic lesions and similarly any outflow lesions. A double-lumen balloon catheter is then passed over the guidewire across the anastomosis, the balloon is inflated with dilute contrast, and under fluoroscopic control the balloon is withdrawn gently to remove free clot. If so, a 9 French hemostatic sheath is placed into the graft, and bleeding around the sheath is controlled with doubled Silastic loops. The dilator is removed and an adherent clot removal catheter (Edwards Laboratory) is passed within the sheath under fluoroscopic control. The sheath is retracted and the wires of the clot removal catheter are deployed within the graft, under fluoroscopic control to engage the adherent plug and remove it without injuring the adjacent artery 42 Angiography should be used to demonstrate the absence of residual. Multiple Redo Procedures Some patients are subject to repetitive failure of lower extremity revascularization procedures, including bypasses. Some believe that patients who have failure of two or more bypasses in the same lower extremity should, if they redevelop critical ischemia, undergo a major amputation. Lipsitz and colleagues43 have recently demonstrated the value of repetitive redo bypasses, performed over several years, in preserving the limb of these patients. They observed that the duration of patency following more than three bypasses was substantial and resulted in more than 3 years of extended limb salvage in more than 50% of the patients who would otherwise have required an amputation. Moreover, these repetitive bypasses should be performed only when the patient would otherwise require an immediate major amputation. Conclusions All surgical treatment efforts should be used to salvage the threatened foot in elderly, high-risk patients who will not walk well after one major amputation and certainly will not after bilateral amputations. Although the surgical methods to save limbs and maintain limb salvage may be time consuming and technically demanding, and although they require a continuing commitment on the part of the vascular surgeon, they are gratifying to those who perform them. They are particularly rewarding to patients who are able to maintain an ambulatory life style in the presence of advanced atherosclerosis. True or false: Multiple reinterventions and redo bypasses are often indicated and worthwhile after a failed primary vein bypass. True or false: Heavily calcified, incompressible tibial arteries are unsuitable for use in limb salvage arterial bypasses. True or false: Studies have clearly shown that in situ vein bypasses are superior to reversed vein bypasses. True or false: the standard arteriogram for femoropopliteal occlusive disease should visualize all arteries from the renal arteries to the forefoot. When is bypass to a tibial artery at the ankle level or in the foot indicated for disabling intermittent claudication True or false: Toe amputation or foot debridement should never be combined with arterial revascularization. True or false: the presence of pedal pulses is evidence of sufficiently good circulation in the foot that a toe amputation for infection is likely to heal. True or false: In patients with a failed infrainguinal bypass and a threatened limb, there is a poor chance of saving the foot by performing a secondary revascularization. Changing arteriosclerotic disease patterns and management strategies in lower limb threatening ischemia. Successful conservative therapy of severe limb threatening ischemia: the value of nonsympathectomy Surgery. Ultimate salvage for the patient with limb-threatening ischemia- realistic goals and surgical considerations. Progress in limb salvage by reconstructive arterial surgery combined with new or improved adjunctive procedures. Diagnosis and management of failing lower extremity arterial reconstructions prior to graft occlusion. The superficial femoral and popliteal arteries as inflow sites for distal bypasses. Bypasses to plantar arteries and other tibial branches: an extended approach to limb salvage. Short vein grafts: a superior option for arterial reconstruction to poor or compromised outflow tracts. Direct approaches to the middle and distal portions of the deep femoral artery for use as sites of origin or termination for secondary bypasses. Percutaneous transluminal angioplasty of the infrapopliteal arteries: results in 53 patients. Impact of nonoperative therapy on the clinical management of peripheral arterial disease. A ten-year experience with one hundred fifty failing or threatened vein and polytetrafluoroethylene arterial bypass grafts. Is percutaneous balloon angioplasty appropriate in the treatment of graft and anastomotic lesions responsible for failing vein bypasses. Open surgical revascularization for wound healing: past performance and future directions. Balloon angioplasty versus implantation of Nitonol stents in the superficial femoral artery N Engl J Med.
Purchase mesalamine 400mg fast delivery
Long-term renal function preservation after renal artery stenting in patients with progressive ischemic nephropathy medicine wheel order 400mg mesalamine otc. Atherosclerotic renal arterial stenosis: clinical outcomes of stent placement for hypertension and renal failure. Stent-supported angioplasty of severe atherosclerotic renal artery stenosis preserves renal function and improves blood pressure control: long-term results from a prospective registry of 456 lesions. The management of renal artery atherosclerosis for renal salvage: does stenting help Endovascular management of atherosclerotic renovascular disease: early results following primary intervention. Percutaneous transluminal renal angioplasty versus surgical reconstruction of atherosclerotic renal artery stenosis -a prospective randomized study J Vasc Surg. Percutaneous transluminal angioplasty of the renal artery: results and long-term follow-up. Percutaneous transluminal renal angioplasty in renovascular hypertension due to atheroma or fibromuscular dysplasia. Impact of Renal Artery Angulation on Procedure Efficiency During Fenestrated and Snorkel/Chimney Endovascular Aneurysm Repair. Autogenous tissue revascularization technics in surgery for renovascular hypertension. Use of the splenic and hepatic artery for renal revascularization in patients with atherosclerotic renal artery disease. The contemporary role of extra-anatomical surgical renal revascularization in patients with atherosclerotic renal artery disease. Preservation of renal function with surgical revascularization in patients with atherosclerotic renovascular disease. Operative management of renovascular hypertension: results after a follow-up of fifteen to twenty-three years. Atherosclerotic lesions usually affect the origin or the proximal 2 to 3cm of the mesenteric arteries, frequently with associated plaque in the aorta and renal arteries. The differential diagnosis includes vasculitis, systemic lupus, Buerger disease, spontaneous dissections, fibromuscular dysplasia, neurofibromatosis, radiation arteritis, coarctation, mesenteric venous stenosis or occlusion, and drug-induced arteriopathy from the use of cocaine or ergot. In the resting state 20% of the cardiac output passes through the mesenteric arteries; but during the digestive process there is a hyperemic postprandial response and the output increases to 150%. Asymptomatic mesenteric stenosis tends to have a benign course, although 15% to 50% of patients with acute mesenteric ischemia from in situ thrombosis of preexisting lesions have no previous signs or symptoms. An excessive delay in proceeding with definitive revascularization or prolonged use of parenteral nutrition alone has been associated with clinical deterioration, bowel infarction, or risk of sepsis from catheterrelated complications. Treatment goals are to relieve symptoms, restore normal weight, and prevent bowel infarction. The indication for prophylactic revascularization in patients with asymptomatic lesions remains controversial. This may be considered in patients with severe three-vessel disease, especially if access to medical care is difficult for those who live in remote or underserved areas. Revascularization may also be considered in asymptomatic patients with severe three-vessel disease undergoing open surgical aortic reconstructions. The technical difficulty of endovascular procedures can be anticipated by the presence of severe eccentric calcification, flush occlusion, and in dealing with patients who have longer lesions, small vessels, and tandem lesions affecting branches. These anatomic features are associated with worse technical results, increased risk of arterial complications. Open reconstruction has also been used in younger patients with nonatherosclerotic lesions and in those who have failed percutaneous intervention or have had multiple recurrent in-stent restenoses. Preprocedure Evaluation Preoperative evaluation should focus on a critical review of surgical risk, nutritional status, and anatomic factors that affect the choice of reconstruction. Optimization of clinical and nutritional status should be sought as long as no significant delay is caused. Optimal medical therapy in these patients ideally should include cessation of cigarette smoking, acetylsalicylic acid, beta-blocker, and lipid-lowering medication. Patients who present with deterioration of symptoms should be admitted, started on intravenous heparin, and treated urgently within 24 to 48 hours. Patients with iodinated contrast allergy should be premedicated with a steroid preparation. Gentle bowel preparation may be used prior to open reconstruction but should be avoided in those with severe or subacute ischemia. Technique of Endovascular Revascularization Arterial access can be obtained using either the femoral or brachial approach, preferentially with ultrasound guidance and a micropuncture set. Choice of access is based on physician preference, the presence of mesenteric occlusion, and angle of origin. Diagnostic angiographies are usually done as part of the intervention and rarely indicated to establish the diagnosis. Brachial access offers more catheter support in patients with very acute origins and occlusions. Diagnostic angiography is done using a 5 French flush catheter positioned approximately at the level of T12. A complete diagnostic study should include an abdominal aortogram with anteroposterior and lateral views to define the location, severity and extent of visceral artery involvement and to identify, concomitant lesions in the aorta or the renal or iliac arteries. If the brachial access is selected, a 90-cm hydrophilic sheath is positioned in the descending thoracic aorta. Choice of catheter shape for selective catheterization is dependent on access site, angle of origin, and individual preference. The initial selective angiography should demonstrate the area of stenosis and the distal runoff branches for comparison with postintervention views. In patients with questionable lesions, pressure gradients can be measured using pressure wire, "pull-back," or a simultaneous pressure measurement technique. Embolic protection may be useful in selected patients who present with acute or subacute symptoms, particularly those with occlusions, long lesions (>30mm length), severe calcification, or thrombus. Predilatation is recommended only if there is tight stenosis, occlusion, or severe calcification, or to gauge the size of stents. A balloon-expandable stent with diameter from 5 to 8mm is used in more than 95% of cases, allowing precise deployment and greater radial force. The stent should cover slightly more than the entire length of the lesion and should go 1 to 2mm into the aortic lumen. Ideally the stent should be flared gently into the aorta to prevent missing the ostia and to facilitate recatheterization if needed. Occasionally a self-expandable stent is used if the treated segment is tortuous or long, extending across proximal jejunal branches. A 6 or 7 French main pulmonary artery catheter is positioned in the descending thoracic aorta. This technique requires a stiff support system to cross the lesion and to deliver the stent. In most cases primary stenting is recommended because of elastic recoil and restenosis, which occurs with angioplasty of ostial lesions. Routine use of two-vessel stenting is not recommended, since it adds cost and potential risk of complications without any evidence of better outcomes. The technique requires a stiffer support system to cross the lesion and deliver the stent. Attempting difficult recanalization from the femoral approach adds time, contrast, and catheter manipulations and is fraught with failure. It is important to avoid the, subintimal plane owing to the risk of dissection or disruption; it is best achieved using straight-tipped guidewires. Our preference has been to use an embolic protection device with a two-wire technique routinely in cases of total occlusion. The occluded superior mesenteric artery stump is engaged with the coaxial system (A). The lesion is crossed using a guidewire and catheter (B), followed by predilatation (C) and stent placement (D).
Order mesalamine with amex
In lymphedema-distichiasis venous varicosities symptoms joint pain fatigue discount mesalamine online american express, ptosis, cleft palate, congenital heart disease, spinal extradural cysts, and other abnormalities are also commonly found. Wartlike (verrucous) skin changes are commonly seen in advanced cases of chronic, long-standing lymphedema. It may be necessary to rule out other problems that can cause or contribute to limb swelling, especially venous occlusion or chronic reflux. The left limb has a perioperative iliofemoral deep venous thrombosis and secondary lymphedema from surgical disruption of the nodes and lymphatics. In diagnosing lymphedema and assessing response to therapy both qualitative and, 16 quantitative assessments of lymphedema are useful. Volumetric methods assess changes in the size of the extremity and compare them with the contralateral extremity that is unaffected and not at risk for lymphedema. In addition to volume changes, tissue properties are altered by the pathologic process, and a number of methods have been developed for the evaluation of tissue elasticity and electric conductivity. Lymphangiography involves the cannulation of a distal lymphatic vessel via a surgical incision. It is now rarely used, as it is painful, technically difficult to perform, and in some cases may cause sterile lymphangitis and worsen lymphatic obstruction. In normal subjects, transport to the abdominal level occurs in an hour or less, but when lymphatic obstruction is present, the colloid never ascends the lymphatics and becomes trapped in the interstitial spaces of the distal limb, producing a "dermal back-flow" pattern. Isotope quickly reaches ilioinguinal lymph nodes via a single lymphatic channel on the right. Marked dermal backflow is noted on the left without reaching the ilioinguinal lymph nodes. By 6 hours, isotope transit from the injection site is completed on the right; dermal backflow persists on the left. Early lymphedema is more amenable to interventions; thus early detection plays an important role. Duplex ultrasound scanning and venography help assess the possible contribution of venous pathology to edema. After 10 minutes, the spread of the medium from the point of maximum congestion is assessed with fluorescent light microscope and compared with the spread from the symmetrical point of the contralateral extremity Considerable. This test is safer, quicker, and simpler compared with lymphangiography and lymphoscintigraphy and may gain wider, 44-46 acceptance as a more practicable alternative. In diagnosing protein-losing enteropathy albumin-labeled (99mTc) scintigraphy may be, used. Several immunohistochemical markers may aid the examination of the lymphatic system. Myxedema associated with thyroid dysfunction, cardiac or renal failure, hypoproteinemia, and chronic dependency may resemble lymphedema or can aggravate otherwise mild cases of lymphedema. Obesity (including morbid obesity and lipedema) is frequently seen in conjunction with or mistaken for lymphedema. Rationale for Treatment Lymphedema is generally an incurable, chronic disease that often requires lifelong care, but is almost never life-threatening. The natural history of the disease is characterized by progression both in terms of the amount of lymphedema and its grades. This progression is slower for primary cases compared with secondary ones, and slower for arms than for legs. The rationale for therapy directed at pain relief, functional improvement, or appearance seems obvious; therapy intended to prevent future complications is less intuitive but often of greater importance. However, the ensuing complications may be devastating when patients develop cellulitis or lymphangitis that ravages the remaining lymphatics and leaves the limb dysfunctional with severe lymphedema. Even more devastated are patients who develop angiosarcoma, a condition that usually leads to the rapid loss of the limb and life (5-year survival time 10% to 16%; mean survival of 19 to 31 months). It is easy to conclude that a young, healthy patient with severe, disabling, painful, cosmetically disfiguring lymphedema warrants treatment. Other decisions may not be so easy What about the young woman whose swelling is so mild that she notices it only. In these instances, the "cost" of treating lymphedema (given the mild symptoms, bad prognosis, or advanced age) must be weighed against the likely "benefits. Cost is, determined not only by the dollars spent on therapy but also by less tangible factors such as the time devoted to therapy (which may be substantial), the inconvenience of certain treatment measures. There is no one right answer, and therefore therapy must be individualized for each patient. Differences in treatment rationale and patient demographics define the variety of institutional practices. Goals of Therapy the goals of therapy may seem obvious-to reduce the size of the limb and thus to minimize functional impairment, pain, cosmetic disfigurement, and the chance of longterm complications. However, how much fluid needs to be removed from a lymphedematous limb to achieve these goals, and what degree of reduction is feasible Even in this era of evidence-based medicine, lymphedema treatment remains more art than science. Effective therapy is often a balancing act-the more aggressively the edema is controlled, the more intense (and often lifestyle-altering) the treatment is. The patient and the physician may have vastly different ideas about the ultimate goals of therapy. Treatment Options There is no universal consensus on the best approach to lymphedema treatment, so protocols vary among institutions. Attempts have been made by the International Society of Lymphology and the International Union of Phlebology to amalgamate the spectrum of these diverse diagnostic and treatment approaches into consensus documents. Diuretics are generally not recommended due to the risk of increased fibrosis and worsening fluid accumulation. Benzopyrones (coumarins) are thought to increase proteolysis by macrophages and used to be touted as drugs that can help patients with lymphedema. Evacuation of the excessive fluid from the extremities affected by lymphedema can be accomplished by maximizing the evacuation through the remaining lymphatic vessels; alternatively new conduits for lymphatic outflow can be created to replace defective, ones. It is often combined with other techniques, such as compression bandaging as part of decongestive therapy and may vary in its effectiveness, depending, on the degree of fibrosis. It is more effective in the early stages of lymphedema when collateral lymphatic flow rerouting is more easily achievable and before the more pronounced fat tissue changes and fibrosis develop. It is geared toward augmenting the contractility of lymphatic vessels and increasing lymphatic flow through cutaneous lymphatics (thus improving lymphatic fluid evacuation from deeper tissues). Randomized controlled studies have been performed, some demonstrating a 40% to 60% decrease in the excess limb volume. However, follow-up is generally limited and the individual results are variable, which may be due to the differences in the stage of the disease. Some of the newer pumps encase the trunk and limbs, and are composed of individually inflatable chambers that can be programmed to mimic lymphatic massage. The concept of compression therapies to enhance lymphatic flow through existing lymphatic channels as well as to stimulate the formation of new channels is very intuitive. Lymphatic pumps are used for several short sessions a day or for prolonged periods. Normal lymphatic pressures are significantly lower than venous or arterial pressures in the same extremity. However, to stimulate creation of new lymphatic channels in more fibrotic tissues of advanced lymphedema, higher pressures may be needed. The exact pressures, duration, frequency and other application parameters of the lymphatic compression pumps, depend on the lymphedema stage, are not well studied, and will have to be elucidated in current and future clinical trials. By sequentially activating each cell in a predetermined order, the pump can be programmed to simulate lymphatic massage. Gravity may also be used to improve passive drainage through limb elevation and is helpful, especially in the early stages of lymphedema. The durations of the intense initial and then maintenance lymphedema treatments are not well established, and symptomatic recurrence may occur within several months of initiating maintenance therapy 80. Functional outcomes and quality of life measures are the ultimate end-point metrics of lymphedema therapy Functional outcomes, such as strength and range of motion, may. Even regular, progressive exercises appear to be safe and beneficial in patients with secondary lymphedema.
Buy mesalamine 800mg with visa
Up to three-quarters of patients with popliteal aneurysms present with symptoms medicine prescription order mesalamine 400 mg mastercard, including claudication, chronic embolization with ischemia, acute limb ischemia from embolism or thrombosis, or swelling and pain from aneurysm expansion and compression. Rupture can occur into the popliteal vein and is associated with a high rate of limb loss. Diagnosis A popliteal aneurysm should be suspected in any patient in whom the popliteal pulse is widened and easily palpated, in any patient with an acutely ischemic limb despite a femoral pulse, or in any patient with evidence of distal embolic occlusion of the infrapopliteal arterial tree. Many popliteal aneurysms are calcified on plain radiographs of the popliteal fossa. Arteriography is currently rarely necessary for elective operative repairs, but is essential for patients with acute thrombosis and limb threatening ischemia. Indications for Aneurysm Repair Current recommendations for repair of popliteal aneurysms include aneurysm size 1. This recommendation is based on the high incidence of thromboembolic complications associated with these lesions, as detailed earlier, and the low morbidity and mortality associated with repair. Treatment Repair of a popliteal artery aneurysm can be accomplished by either open or endovascular repair. Which approach is used depends on a number of factors including patient comorbidities, runoff vessel patency popliteal artery tortuosity and length of, vessel involvement. Open repair of popliteal artery aneurysms was first accomplished by aneurysm ligation with above-knee to below-knee bypass through a medial approach. Since both approaches are effective, which one is employed for a given patient is dependent on surgeon experience, aneurysm size, and proximal and distal extent of the aneurysm. Extension of aneurysmal degeneration into the superficial femoral artery or infra-geniculate arterial tree precludes a posterior open approach. In this anatomic situation, the proximal and/or distal anastomoses of the arterial reconstruction are best approached medially When popliteal aneurysms are large. The posterior approach has the benefit of complete aneurysm decompression, which does not always occur with medial ligation and bypass. There have been reports of higher rates of nerve damage from a posterior approach, particularly with large extensive aneurysms; however, a recent meta-analysis found no statistically significant difference between the two approaches with respect to nerve damage. In such patients, bypass is often not possible or is subject to a high failure rate, due to poor runoff. In this situation, the use of pre-repair thrombolytic therapy can frequently establish patent runoff and improve the microcirculation, thereby allowing for successful bypass or stent-grafting. Following acute thrombosis of a popliteal artery graft patency and limb salvage rates after initial thrombolysis have been, reported to be superior to early operative intervention alone. Since then, numerous reports have been published on the use of stent-grafts in this arterial location. These studies report shorter operative time and hospital stay and less perioperative morbidity 12,25-32 For endovascular stent-graft. Stentgrafts have also been used successfully in the treatment of ruptured popliteal aneurysms. In a series of 51 popliteal aneurysms reported by Shortell and colleagues,36 results were dependent on the clinical presentation and the status of the runoff vessels. Patients with limb-threatening ischemia had a graft patency of 69% at 1 year, whereas all electively performed grafts in asymptomatic patients were patent at 1 year. After 3 years, runoff dictated patency; grafts with good runoff had a patency rate of 89%, whereas poor runoff was associated with a 3-year patency rate of only 30%. Numerous, more recent reports of large series of popliteal aneurysms have confirmed these earlier results. Forty percent were asymptomatic, 39% had chronic ischemia, and 21% had acute ischemia. The 30-day thrombosis rate was 1% in asymptomatic limbs, 4% in limbs with chronic ischemia, and 9% in limbs with acute ischemia. There were three deaths and six early amputations, all in the acute ischemia group. Within that group, limbs treated with preoperative thrombolysis had better limb salvage (96%) than those limbs treated with surgery alone (69%). Two percent of aneurysms required reintervention for aneurysm enlargement, and all these limbs had been treated with ligation and bypass. In 2015, a retrospective review of 234 open popliteal artery aneurysm repairs in 196 patients evaluated long-term patency this study found primary patency. In the vast majority of surgical series described above, the Edwards technique was used. However, as experience has accumulated, it became evident that late aneurysm expansion and even rupture can occur. In 2003, Ebaugh and colleagues43 reported the Northwestern experience with 57 popliteal aneurysms treated with aneurysm ligation and bypass. Beseth and Moore22 reported on 30 popliteal aneurysms that were treated through a posterior approach using a short prosthetic interposition graft repair. Aneurysms that extended proximal to the adductor canal were excluded from the posterior approach, and all aneurysms had one or more patent tibial artery runoff vessels. Ravn and colleagues24 analyzed the Swedish Vascular Registry which contained 717 popliteal aneurysms. There was no difference in patency between vein and prosthetic graft when the posterior approach was used, but there was better patency with vein using the medial approach (90% vs. Emergency procedures and the use of prosthetic graft were associated with higher amputation rates. Postoperative aneurysm expansion was demonstrated in 33% when the medial approach was used, but in only 8. Zaraca and colleagues45 found that the posterior approach was possible in 78% of aneurysms using proximal extension above the adductor canal as the primary contraindication to posterior repair. A 2016 meta-analysis by Phair and colleagues19 compared the posterior and medial approach for open repair. Primary outcomes were major perioperative complications, primary patency secondary patency and limb loss. A total of seven studies from 2007 to , 2015 with a total of 1427 patients were evaluated. There were 338 that underwent a posterior approach and 1089 that underwent a medial approach. There was no statistical difference in nerve damage, 30-day complications, 30-day limb loss, or 30-day primary patency When looking at 30-day secondary patency results suggested superiority of the. Because of the inferior results of endovascular or open repair once acute thromboembolic complications have occurred, attention has focused on the reestablishment of runoff preoperatively through the use of thrombolytic therapy Most. Hoelting and associates46 described 24 patients with acute ischemia secondary to popliteal artery aneurysm thrombosis. Nine patients were treated with preoperative thrombolysis and underwent successful bypass. For three patients, lysis was incomplete but established sufficient runoff so that successful bypass could be performed. These authors also reviewed the literature and reported an amputation rate of approximately 27% in 455 patients treated with bypass alone, compared with approximately 20% in 14 patients in whom only thrombolytic therapy was used. In 30 patients in whom thrombolytic therapy was combined with bypass, no limb was lost. Varga and colleagues suggested that thrombolysis is of value in restoring distal runoff before bypass in the presence of limbthreatening ischemia. Carpenter16 reported on seven limbs with popliteal aneurysm thrombosis and complete thrombosis of all runoff vessels. These patients were treated with preoperative thrombolysis, with 100% limb salvage and superior graft patency compared to similar patients not treated with preoperative thrombolysis. Early experience of popliteal artery aneurysms with stent-grafts demonstrated technical success, but patency was considerably lower than that achieved with aneurysm ligation and bypass. However, Tielliu47 in 2005 reported on 57 popliteal aneurysms treated (five emergently) with stent-grafting.
Mesalamine 800mg discount
Modern duplex scanners use complex scan probes made up of many elements in an array but the principle of focal sampling is the same top medicine buy mesalamine visa. Although qualitative interpretation is helpful in some patient examinations, quantitative measurements provide objective testing. Spectral analyzers are used to determine the main frequency components obtained from a given vessel. Sonograms display the different frequency contents detected at each point in time. The computational algorithm used to perform the conversion of the amplitude of received frequencies to a frequency over time display is called a fast Fourier transform. This process involves the grouping of frequencies based on quantity for each time unit. This is then converted to a frequency (or proportional velocity) versus time plot where the intensity of the curve (Doppler waveform) corresponds to the amplitude or amount of any given frequency this has implications in the interpretation of spectral broadening. Duplex Ultrasound During the 1960s, B-mode ultrasound imaging (B = bright mode, a static image of the tissue) was used for visualization of soft tissue structures. In general, experience shows that when high-quality imaging is obtained, the diagnostic accuracy is very high; however, in patients with advanced atherosclerosis, it is difficult to obtain optimal studies, and diagnostic accuracy is lower. A common problem is incomplete imaging of the vessel wall as a result of calcification, which is present in varying degrees in up to half of patients studied. The extent of interference may be limited, but in some vessels there is no visualization of substantial portions of the artery Although calcified plaques stand out. A major source of error is that recent thrombus may have the same echo density as flowing blood, so that an occluded vessel may look normal on the ultrasound image. To overcome the limitations of ultrasound imaging, the research team at the University of Washington developed the duplex scanner (also called duplex ultrasound), combining a real-time B-mode ultrasound image system with a pulsed wave Doppler detector. The device can study calcified vessels by analyzing the Doppler velocity signal distal to the areas of calcification. In the past 20 years, there has been extensive improvement in duplex scanners in terms of both image resolution and Doppler signal processing. Color Flow Imaging An important later development was the color-coded Doppler system. If the returning ultrasound signal has no change in phase or frequency the amplitude information is used to create the gray-scale image at that point, in the matrix. If there is a change in phase or frequency the information is analyzed in, terms of velocity A color is assigned to represent an approximate mean velocity occurring. The magnitude of the velocity is represented by the hue of the color: a dark shade indicates slow flow, and a lighter shade or white indicates high flow. The aggregate of the color representation from the sample volumes detecting motion produces a realtime representation of the flow patterns within the vessels superimposed on the grayscale image of the stationary tissue. An additional tool is color-coding of the Doppler power (as opposed to velocity) detected. Power is proportional to the square of the velocity; therefore, this measurement provides more sensitive detection of very slow flow or flow in small vessels. A good example of the benefit of power imaging is the detection of an internal carotid string sign. Squaring the velocity eliminates the positive or negative value, so that power values have no directional representation. Most examinations are performed with colorcoding of velocities limited to a portion of the image (area B). Within this portion of the matrix, ultrasound pulses from sample volumes with a change in frequency are interpreted as velocity data. Most of the early tests provided indirect measurement by detecting distal changes in blood flow characteristics produced by advanced stenosis. Common features of the indirect methods are that they detect only lesions that are sufficiently advanced to reduce mean blood flow, and they cannot separate a tight stenosis from an occlusion because the physiologic changes in the distal bed may be indistinguishable. These methods achieved a variable degree of clinical use in the 1970s and 1980s, but were ultimately replaced by duplex scanning. The color image demonstrates the reverse velocity detected in the carotid bulb, as a result of the pattern of flow separation at the bifurcation. Although such arteries can be studied with a conventional scanner, the application of color flow and power Doppler simplifies the examination. The scan usually identifies the pathologic regions, but with advanced atherosclerosis, it is often difficult to get an adequate image to accurately estimate the degree of stenosis. Much of the classification of stenosis is based on interpretation of the Doppler signal. There are two sets of criteria that have been used for many years, and although some laboratories have made modifications or adjustments, the basic principles continue to be applied. Contemporary scanners have improved our ability to find small residual flow channels, especially using power Doppler imaging. Overall, low-grade plaques are best assessed with the image, whereas advanced lesions are best evaluated with the Doppler information. Duplex scanning has been adopted as the standard for carotid disease diagnosis and screening. These studies have shown rates of 92% to 96% accuracy in the identification of severe stenosis. Of particular importance is the fact that experienced laboratories make few errors in separating severe stenosis from occlusion. Although the majority of attention has been focused on the carotid circulation, laboratories routinely investigate the status of the vertebral arteries as well. The examination seeks two types of problems: stenosis in the vertebral artery itself and the abnormal flow produced by subclavian steal, which has both an occlusion of the proximal subclavian artery and reversal of flow in the vertebral artery In the majority of cases of. In some cases of severe occlusive disease, there is sufficient asymmetry in the waveforms of the two vertebral arteries to point to the problem side. Because of its deeper location, the left vertebral artery is more difficult to study than the right. Ackerstaff and associates8 found that the status of the ostium could be studied satisfactorily in about 80% of patients. When adequate evaluation of the prevertebral portion was possible, a sensitivity of 80% and a specificity of 97% were achieved in the detection of reductions greater than 50% in diameter. Most clinical cases of subclavian steal are demonstrated by a reverse flow in the vertebral artery on the affected side. Von Reutern and Pourcelot9 demonstrated that in some cases of subclavian stenosis there is distortion of the waveform rather than complete reversal of flow. Such cases can be assessed more fully by recording the Doppler signal after arm exercise or the induction of reactive hyperemia. In the presence of advanced subclavian stenosis, this stress test produces full reversal of flow. Plaque Characteristics In addition to estimating the severity of a stenosis, ultrasound can be used to study the plaque itself. Most investigators merely distinguish between homogeneous- and heterogeneous-appearing plaques and describe the surface as either smooth or irregular. More elaborate approaches to the description of morphology are being evaluated, but no single approach has been widely adopted. A large number of transient ischemic attacks and strokes are caused by thromboembolization from plaques in the carotid bifurcation. In most situations, a duplex scan is the initial workup, identifying the location and severity of lesions in the carotid system. Many centers use the ultrasound study as the definitive test on which to base the decision to treat. Having an experienced vascular laboratory with a validated record of high accuracy in carotid scanning is the critical element in using duplex scanning as the definitive test. Many asymptomatic patients are being referred to vascular laboratories for the evaluation of cervical bruits. Although some of these patients have bruits radiating from the heart or the great vessels, in a considerable number the sound originates from the carotid bifurcation. Duplex scanning can provide accurate separation according to category of stenosis (see Tables 14. Patients with severe stenosis are considered at increased risk of stroke and are evaluated for optimal medical and/or surgical treatment for stroke risk reduction.
Archangel (White Dead Nettle Flower). Mesalamine.
- Dosing considerations for White Dead Nettle Flower.
- How does White Dead Nettle Flower work?
- Swelling (inflammation) of the upper airways, sore throat, skin inflammation, vaginal discharge, and other conditions.
- Are there safety concerns?
- What is White Dead Nettle Flower?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96362
Discount mesalamine 400 mg fast delivery
Detachable coils for repair of extraparenchymal renal artery aneurysms: an alternative to surgical therapy Ann symptoms xanax treats discount mesalamine 800 mg otc. Stent-assisted coil embolization of widenecked renal artery bifurcation aneurysms. Endovascular management of complex renal artery aneurysms using the multilayer stent. Aneurysmectomy with arterial reconstruction of renal artery aneurysms in the endovascular era: a safe, effective treatment for both aneurysm and associated hypertension. Repair of complex renal artery aneurysms by laparoscopic nephrectomy with ex vivo repair and autotransplantation. Ruptured renal artery aneurysm during pregnancy: successful ex situ repair and autotransplantation. Reconstruction for renal artery aneurysm: operative techniques and long-term results. Favorable outcomes with in situ techniques for surgical repair of complex renal artery aneurysms. Ex vivo renal artery repair with kidney autotransplantation for renal artery branch aneurysms: long-term results of sixtyseven procedures. Isolated renal artery dissection: presentation, evaluation, management and pathology Mayo Clin Proc. Surgical treatment of renal artery dissection in 25 patients: indications and results. Spontaneous dissection of renal artery: long-term results of extracorporeal reconstruction and autotransplantaion. Management of isolated nontraumatic renal artery dissection: report of four cases. Evalluation of characteristics, associations and clinical course of isolated spontaneous renal artery dissection. Spontaneous dissection of branch renal artery-Is conservative management safe and effective Spontaneous renal artery dissection: longterm outcomes after endovascular stent placement. Isolated renal artery thrombosis because of blunt trauma abdomen: a report of a case with review of the literature. Delayed endovascular treatment of renal artery dissection and reno-vascular hypertension after blunt abdominal trauma. Weaver Peripheral arterial aneurysms are less common than aortic aneurysms, but can cause significant morbidity and occasionally lead to death; however, the most common serious complication is end-organ loss or dysfunction. The peripheral aneurysms discussed in this chapter will be the most common ones, including those of the lower extremity arteries below the inguinal ligament, including the femoral artery as well as the, extracranial carotid arteries, and the upper extremity arteries distal to and including the subclavian artery the focus will be on true peripheral artery aneurysms, although the. Iatrogenic and mycotic peripheral aneurysms are discussed separately at the end of the chapter, with a focus on management and traumatic peripheral aneurysms are discussed in Chapter 48. Peripheral Aneurysms the most common cause of nonmycotic peripheral arterial aneurysms is atherosclerosis and all peripheral aneurysms are uncommon when compared to aortic aneurysms. In descending order, the relative frequency of these aneurysms is popliteal, femoral, subclavian or axillary and carotid. Atherosclerotic peripheral aneurysms are frequently, associated with synchronous aortic, iliac, or splanchnic aneurysms. Reports on distal aneurysms involving the brachial, radial, ulnar, deep femoral, and tibial or peroneal arteries are limited to small series or case reports. Although true aneurysms have been reported in these areas, for the most part, forearm, hand, tibial, and peroneal aneurysms are secondary to trauma or are mycotic in origin. Atherosclerotic aneurysms tend to occur primarily in men older than 50 years of age, and aneurysms caused by trauma are also more common in men, but occur at a younger age. Aneurysms secondary to thoracic outlet syndrome are most commonly seen in middleaged women (75%). Unlike aortic aneurysms, which tend to rupture, peripheral aneurysms most commonly thrombose or give rise to distal arterial emboli and since there are rarely warning signs before embolization, the mere presence of a peripheral aneurysm often suggests the need for repair. The two primary objectives of treatment are exclusion of the aneurysm and restoration of arterial continuity and in most cases, both objectives, can be achieved. In the rare aneurysm that is not surgically accessible, exclusion alone may be required in this situation. Additional considerations include relieving associated compressive symptoms from the aneurysm and minimizing the risk of late aneurysm expansion. Because most patients with peripheral aneurysms do not often have extensive atherosclerotic occlusive disease, the results of reconstructive vascular procedures are usually excellent. In some cases, however, prior embolization from the aneurysm can lead to obliteration of some, or all, of the distal arterial bed, leading to less satisfactory results. Dent and colleagues showed an association between femoral and popliteal aneurysms and other aneurysms of atherosclerotic origin. Among patients with a common femoral aneurysm, 95% had a second aneurysm, 92% had an aorta-iliac aneurysm, and 59% had bilateral femoral aneurysms. Natural History the natural history of femoral aneurysms, like popliteal aneurysms, is associated with a significant incidence of thromboembolic events. Deep femoral aneurysms, however, are thought to be particularly prone to rupture, with reported rates of 13% to 45%. While the incidence of deep femoral aneurysms is much lower, more than half will present with complications and greater than 80% will have associated aneurysms in other vascular beds. Femoral aneurysms should be considered in any patient with an acute lower extremity arterial occlusion or with evidence of embolic disease affecting the foot and leg. Femoral aneurysms are easily diagnosed by ultrasonography and some authors have suggested the routine use of ultrasonography to look for femoral and popliteal aneurysms in men with aortic aneurysms. Indications for Aneurysm Repair Conventional recommendations for the treatment of femoral aneurysms include all symptomatic aneurysms of any size, aneurysms with intramural thrombus, aneurysms greater than 2. A more recent study by Lawrence and the Vascular Low-Frequency Disease Consortium8 has brought into question the current recommendations for repair based on a size of 2. In their multivariate analysis they found that size 4cm or greater and intraluminal thrombus were indications for repair and significantly associated with complications in patients managed nonoperatively (P =. Location of the femoral aneurysm (common, profunda, superficial) was not significantly associated with complications. One caveat to this recommendation is that the presence of thrombus was a predictor of symptomatic progression and an indication for repair at a smaller size. When the deep femoral artery is involved, the graft may be sewn end to end to the superficial femoral artery and the origin of the deep femoral artery implanted into the, side of the graft. Releasing the inferior border of the inguinal ligament, dividing the inguinal ligament, or making a separate retroperitoneal incision can assist in gaining proximal control of the external iliac artery Additionally proximal endovascular balloon control. In addition, stents and stent-grafts in this area may complicate future arterial access. Furthermore, coverage of the profunda femoris orifice by the stent-graft excludes a critical thigh vessel from antegrade flow. Repair of a deep femoral artery aneurysm is dictated by the patency of the superficial femoral artery and the distal extent of the aneurysm. Although, approximately 50% of deep femoral aneurysms can be safely ligated, in-line repair should be performed when technically feasible. Repair can be accomplished with an interposition graft of saphenous vein, but prosthetic grafts are also acceptable in the absence of vein conduit. Usually superficial femoral artery aneurysms are an extension of a popliteal aneurysm. Open repair can be accomplished by either aneurysm resection and interposition grafting or aneurysm ligation and bypass. Stent-grafting can be applied anywhere along the superficial femoral artery as long as there are adequate landing zones. Outcomes When femoral aneurysms are treated before complications arise, the results are excellent. The 18 asymptomatic patients with femoral aneurysms in the series by Cutler and Darling all had excellent early and late results (no graft occlusions).
Syndromes
- Genetic disorder
- Muscle aches
- 24-hour urine for cortisol and creatinine
- 1 mL = 1 cc
- Symptoms that last more than 3 weeks
- Chest x-ray
- Trypsin and chymotrypsin in stool
- Acute respiratory distress syndrome (ARDS)
Order mesalamine 400mg without prescription
As a therapeutic intervention 247 medications buy line mesalamine, lytic therapy may be the best alternative in certain clinical situations. In many other cases, it is just one aspect of the overall care of patients with thrombotic complications of peripheral vascular disease. This article provides an overview of the fibrinolytic system and the available agents. This information can be translated into guidelines to help clinicians select patients who may benefit from thrombolytic therapy Methods, dosages, complications, and promising. In 1906 Morawitz observed that postmortem blood destroys fibrinogen and fibrin in normal blood. The term fibrinolysis had been coined by Dastre in 1893 to describe the disappearance of fibrin in unclottable blood obtained from dogs subjected to repeated hemorrhage. Charles Dotter was the first to describe intraarterial drug delivery into thrombus for thrombolysis. The interplay of components, activators, and inhibitors are becoming more appreciated. The potential to harness the fibrinolytic system for therapeutic means has emerged in the past few decades, and results from prospective clinical trials are now available, providing guidelines to patient selection and therapy For the vascular. In addition, careful attention and observation of the patient, renal dysfunction, systemic effects, and often the limb undergoing treatment are required. Fibrinolytic System the complex and intricate relationships among all components of the fibrinolytic system are only partially understood. However, much progress has been made, mostly owing to recognition of the importance of the fibrinolytic system as a homeostatic system. This same process has been harnessed for a therapeutic effect in cases of clinical thrombosis. This baseline fibrinolytic activity is probably under local and central control mechanisms. The feedback loop that prevents systemic fibrinolysis involves both inhibitors at the activator level and specific inhibitors of the proteolytic enzyme plasmin. The final common pathway in the fibrinolytic system is the conversion of the proenzyme plasminogen to the active enzyme plasmin. At least four forms occur in plasma, based on variations in the N-terminal and the degree of glycosylation. Lys-plasminogen, containing mostly lysin in the N-terminal, results from limited proteolysis of the Glu form; it has a shorter half-life and is found in higher concentrations in thrombus, most likely secondary to its higher affinity for fibrin. The kringle portion of plasminogen is a nonprotease, or heavy chain, consisting of five homologous domains. The function of these kringles is thought to be of paramount importance in the binding of plasminogen and plasmin to fibrin, 2-antiplasmin, and other macromolecules. Aminocaproic acid and tranexamic acid induce this change from the closed structure to the open structure. Because of this change, plasminogen is far more readily cleaved to the active enzyme plasmin by plasminogen activators. Concentrations of lysine analogs, such as tranexamic acid and aminocaproic acid, that actually promote the more active, open conformation of Glu-plasminogen also prevent its binding to fibrin and therefore exhibit an antifibrinolytic effect. Circulating fibrinogen is composed of three polypeptide chains known as the, and chains. These chains are bonded together by disulfide bonds, which are also linked to a second identical chain, thus making fibrinogen a dimer of trimers. Thrombin, the common pathway of the coagulation cascade, removes several amino acid peptides from the end terminal of the chain, the chain (fibrinopeptide B), to form fibrin. Plasmin catalyzes the hydrolysis of these bonds, producing peptides that can be assayed in circulation. Specifically those produced after the cleavage of fibrinogen consist of, truncated polypeptides collectively known as X fragments. X fragments can be incorporated into both newly forming and existing thrombi, causing them to be more fragile. Several fragments are specifically produced by the action of plasmin on fibrin, as opposed to fibrinogen. Unique fragments such as D-dimers can be assayed, documenting fibrinolysis as opposed to fibrinogenolysis. Plasminogen can also cause the release of kinin from high-molecular-weight kininogen. In addition, it can directly and indirectly activate prekallikrein, again inducing kinin formation. These inhibitors control the activity of the activators in plasma and possibly at the cellular level. When pharmacologic dosages of these agents are administered, the inhibitor activity is suppressed. It is estimated that one-third to one-half of the initial pharmacologic dosage of urokinase, for example, becomes inactivated shortly after administration. This protease inhibitor is a single-chain glycoprotein that inhibits plasminogen in two steps: a fast reversible binding step, followed by the formation of a covalent complex involving the active site of plasmin. This complex system is capable of maintaining a balanced equilibrium between clotting and lysis, so that blood fluidity is ensured. It is important to recognize that although plasmin is highly selective for fibrin, it also digests fibrinogen and other plasma proteins. Circulating plasmin inhibitors prevent this otherwise disordered lytic action and preclude free circulating plasmin under normal conditions. A link between lipoprotein metabolism and fibrinolytic function has been suggested by the demonstration of significant homology between the amino acid sequence of apolipoprotein A and the structure of plasminogen. Thus a prothrombotic function by virtue of interference with the numerous physiologic functions of plasminogen has been suggested in patients with increased levels of apolipoprotein A. Apolipoprotein A has also been found to competitively inhibit the binding of plasminogen to fibrinogen and to the plasminogen receptor on endothelial cells. From the foregoing discussion, it is evident that the fibrinolytic (plasminogenplasmin) system plays a vital role in biological homeostasis. In addition, it has a pivotal role in certain disease states, ranging from atherosclerosis to carcinogenesis. From a therapeutic standpoint, drugs capable of converting plasminogen to plasmin achieve their lytic effect to a great extent by overwhelming circulating plasmin inhibitors and generating an abundance of plasmin (exogenous fibrinolysis). Circulating plasmin not only produces the desired fibrinolysis but also proceeds to digest circulating fibrinogen. A more desirable situation results in the activation of thrombus-bound plasminogen (endogenous fibrinolysis) by these agents. Thrombus-bound plasminogen is, to a certain extent, protected from circulating inhibitors and thus proceeds with fibrin digestion much more effectively Current investigations are concentrated on producing. With better understanding of the complexity of the fibrinolytic system, it is possible that these benefits can be realized. Thrombolytic Agents the use of thrombolytic agents has clearly resulted in a significant improvement in the outcome of patients with acute cardiac ischemia, myocardial infarction, and cerebral infarction. It has also resulted in a modification in the treatment algorithm for patients with peripheral arterial occlusion. Thrombolytic therapy is an important treatment option for patients with vascular occlusive disease. The agents can be grouped by their mechanism of action-those that directly convert plasminogen to plasmin versus those that are inactive zymogens and require transformation to an active form before they can cleave plasminogen. In addition, thrombolytic agents can be classified by their pharmacologic actions-those that are fibrin specific. First-Generation Thrombolytic Drugs First-generation thrombolytic agents-namely streptokinase and urokinase-are highly, effective at thrombolysis, but their potency is limited by the fact that they are not fibrin specific. They also convert circulating plasminogen to plasmin, but because circulating plasminogen and the plasminogen in thrombus are in equilibrium, the plasminogen in thrombus would be depleted, thus limiting the efficacy of the agent.
Purchase 400 mg mesalamine overnight delivery
A urinary catheter medicine while breastfeeding generic mesalamine 800 mg free shipping, as well as a peripheral arterial catheter, should be placed for monitoring intravascular volumes and hemodynamic status. Patients who have profound acidosis, hemodynamic instability or clinical, evidence of peritonitis should be taken immediately to the operating suite for abdominal exploration. In these advanced cases, correction of acidosis may not be possible until the ischemic bowel has been removed or revascularized. Perioperative morbidity and mortality in these patients is significant, with the reported mortality ranging from 20% to 50%. If lysis is not accomplished within 4 hours of commencing thrombolytic therapy or if peritoneal signs develop, the infusion should be discontinued and immediate surgical exploration should be performed. Successful endovascular therapy defined as successful return of bowel perfusion, resulted in fewer laparotomies, (69% vs. Those who failed endovascular treatment had the same elevated 50% mortality rate as the open surgical group. Ryer and colleagues at the Mayo Clinic recently reported a series of 93 patients who underwent emergency arterial revascularization for acute mesenteric ischemia from 1990 to 2010. There was no significant difference in outcomes between open and endovascular revascularization. There was no significant difference in outcomes among patients treated in the 1990s (n = 45 patients) and the 2000s (n = 48 patients) with the overall 30-day mortality being 22%. If the use of a prosthetic graft was required in the presence of necrotic bowel, grafts were soaked in rifampin and excluded with omentum prior to performing an enterectomy. Seventy-six percent underwent open surgery and 24% underwent endovascular treatment. An advantage of this approach is that the increased "pushability" allowed by sheath access in close proximity to the obstruction can facilitate treatment of some occlusive lesions that cannot be successfully treated via antegrade access. This method is a viable alternative to open bypass and may also be considered as a bridge to more durable open revascularization following recovery. When an aortic dissection involves the origin of one or more of the visceral vessels, endovascular repairs have been attempted through stent placement55,56 and balloon fenestration of the dissection septum. Regardless of the cause, most patients with acute arterial occlusion require early surgical exploration and reestablishment of mesenteric flow to prevent or minimize bowel infarction. A generous midline incision should be made, and the extent of mesenteric ischemia and necrosis should be assessed. If the entire small bowel is gangrenous, enterectomy with lifelong hyperalimentation is the only option. If the process is more segmental, portions of frankly ischemic and nonviable intestine should be resected and controlled while further exploration is continued. After locating all infarcted segments, the cause of the intestinal ischemia should be sought. To achieve adequate exposure, the transverse colon is retracted superiorly and the, fourth portion of the duodenum is mobilized to the ligament of Treitz. Balloon-tipped embolectomy catheters are inserted retrograde, and the embolus is extracted. Embolectomy catheters should also be passed distally to ensure that no fragmentation of the clot or discontinuous thrombosis has occurred. Transverse arteriotomies are closed primarily with interrupted fine monofilament sutures to ensure that the vessel is not stenosed. If a longitudinal arteriotomy is required, closure is best accomplished with a vein patch. Appropriately selected longitudinal arteriotomies can also be used for distal anastomoses of bypass grafts if thrombectomies are unsuccessful in obtaining arterial inflow. Balloon-tipped catheter extraction of a mesenteric embolus is performed through a transverse arteriotomy. Primary closure of the arteriotomy is then completed transversely or with a vein patch to prevent stricture. Segments that previously demonstrated equivocal viability may improve with revascularization, and resection may be avoided; lengths of bowel that are obviously nonviable must be removed. Bowel continuity can be restored primarily or stomas may, be exteriorized if the patient is unstable. In most instances, a second-look operation should be performed at 24 to 36 hours to assess the cumulative effects of reperfusion. Planning for this reexploration allows the surgeon to minimize the amount of bowel resected primarily and to ensure that the final bowel anastomoses are performed with viable bowel. If there is a high likelihood of bowel resection, an autologous conduit should be used for the bypass. If bowel necrosis is present and a suitable autogenous vein is not available for conduit, then a prosthetic graft may be soaked in rifampin antibiotic solution prior to use. In syndromes of nonocclusive ischemia, the primary therapy is selective arterial administration of vasodilating agents such as papaverine. Such treatment must be coupled with the cessation of agonists or other vasoconstrictors. Heparin should also be administered to prevent thrombosis in the cannulated vessel, but the drug must be infused through a peripheral intravenous catheter to avoid precipitation when mixed with papaverine. If a patient demonstrates signs of continued bowel ischemia or necrosis, as evidenced by peritonitis or guarding, surgical exploration is required. All necrotic bowel should be resected while arterial infusions of vasodilators continue. The room temperature should be elevated, and the bowel should be kept in moist laparotomy pads to minimize vasoconstriction during exploration. Most patients should undergo a second-look operation in 24 to 48 hours to reassess bowel viability. Unfortunately venous, thrombectomy is of limited durability and has not proved effective in most instances. The extent of bowel resection should be generous, and repeated exploratory laparotomy is often required to ensure that adequate bowel resection has been performed. Because many patients succumb despite these measures, a more aggressive stance toward early surgical thrombectomy or fibrinolysis has been advocated by some. Although the detection of frankly necrotic bowel is not difficult, the determination of viability in marginally perfused bowel is more challenging. Simple indicators of viability include visible peristalsis as well as a pink and normal color of the serosa. If any question remains, the bowel should be reassessed at a minimum of 30 minutes after revascularization. Administration of intravenous fluorescein followed by illumination with a Wood ultraviolet light will confirm perfusion of the bowel. The primary limitation of fluorescein is that it is eventually absorbed in fat; therefore it can be administered only once before it diffuses throughout all tissue and loses its specificity Unfortunately. Long-term patient outcomes after acute intestinal ischemia are strongly dependent on the timeliness of diagnosis, the underlying lesion, and the associated cardiovascular status. In a comprehensive report by Klempnauer and colleagues of 90 patients suffering from intestinal ischemia, 31 patients survived and were discharged from the hospital. The worst survival (20% at 5 years) was seen in patients who suffered mesenteric arterial thrombosis, and the best survival was seen in patients with emboli or nonocclusive ischemia (about 70%). Only one patient who survived the first episode of arterial thrombosis died because of recurrent bowel ischemia. The lesions usually represent extensions of aortic atheroma rather than intrinsic disease of the mesenteric arteries. Risk factors parallel those of atherosclerosis in general, including a positive family history smoking, hypertension, and hypercholesterolemia. The pain is characteristically dull and crampy occurring primarily in the epigastrium or midabdomen. The discomfort, results from activation of visceral afferent nerves that respond to distension and ischemia but that poorly localize pain. The pain occurs 15 to 45 minutes after eating, with increasing severity according to the size and nature of the meal. The temporal relationship between pain and food ingestion often leads to "food fear " (sitophobia), a classic but variable complaint. Many patients become so emaciated that they undergo extensive evaluations for occult neoplasms.
Discount mesalamine 400mg otc
Surgical or endovascular revascularization in patients with critical limb ischemia: influence of diabetes mellitus on clinical outcome permatex rust treatment purchase discount mesalamine. Primary everolimuseluting stenting versus balloon angioplasty with bailout bare metal stenting of long infrapopliteal lesions for treatment of critical limb ischemia. The impact of isolated tibial disease on outcomes in the critical limb ischemic population. Improved outcomes are associated with multilevel endovascular intervention involving the tibial vessels compared with isolated tibial intervention. Angiographic patency and clinical outcome after balloon-angioplasty for extensive infrapopliteal arterial disease. Subintimal angioplasty as the first-choice revascularization technique for infrainguinal arterial occlusions in patients with critical limb ischemia. Subintimal angioplasty of isolated infragenicular vessels in lower limb ischemia: long-term results. Cutting balloon angioplasty versus standard balloon angioplasty for failing infra-inguinal vein grafts: comparative study of short- and mid-term primary patency rates. Cutting balloon angioplasty of the popliteal and infrapopliteal vessels for symptomatic limb ischemia. Drug-Coated Balloons for Revascularization of Infrapopliteal Arteries: A Meta-Analysis of Randomized Trials. Endovascular therapy as the primary approach for limb salvage in patients with critical limb ischemia: experience with 443 infrapopliteal procedures. Angioplasty or primary stenting for infrapopliteal lesions: results of a prospective randomized trial. Primary stent-supported angioplasty for treatment of below-knee critical limb ischemia and severe claudication: early and one-year outcomes. Below-knee bare nitinol stent placement in high-risk patients with critical limb ischaemia and unlimited supragenicular inflow as treatment of choice. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery Multicenter Study of. Value of antiplatelet therapy in preventing thrombotic events in generalized vascular disease. Current medical therapies for patients with peripheral arterial disease: a critical review. Because of its relatively less invasive nature, the open technique for lumbar sympathectomy is still performed, but with rapidly decreasing frequency 7,8 Indications for both thoracic and lumbar sympathectomies have. Earlier indications such as claudication, uncomplicated primary Raynaud syndrome, or scleroderma are not used. Historical Background Although Jabouley suggested sympathetic denervation for vasospastic disorders as early as 1899, periarterial sympathectomy was introduced by Leriche only in 1913 for ischemic lesions caused by vasospasm. Adson and Brown14 were the first to perform cervicothoracic sympathectomy in 1929. Using the single-scope technique, thoracoscopic sympathectomy was popularized by Kux15 in Austria as early as 1954. Anatomy and Physiology the peripheral nervous system includes both somatic and autonomic components. The somatic efferent motor nerves control the voluntary striate muscles and the afferent nerves transmit somatosensory information to the brain. The autonomic nervous system transmits information from the abdominal viscera as well as the smooth and cardiac muscles and the exocrine glands. Autonomic nerves are composed of the sympathetic and parasympathetic nervous systems. Anatomy the sympathetic nervous system consists of the central autonomic network-which includes the brain stem, diencephalons, and cortex-and the peripheral sympathetic pathways. The peripheral sympathetic pathway consists of preganglionic and postganglionic neurons. Information from the brain stem and hypothalamus descends through the lateral funiculus of the spinal cord to the preganglionic sympathetic fibers. The preganglionic sympathetic neurons originate in the anteromedial column of the thoracolumbar cord, between T1 and L2. These myelinated white nerve fibers travel in the ventral root of the spinal cord to the paravertebral sympathetic ganglia, where they synapse onto the postganglionic unmyelinated gray fibers. It is likely that each preganglionic axon innervates about 10 postganglionic neurons. The regional activity of the sympathetic chain is the product of reflex arcs between somatic afferent fibers and preganglionic efferent fibers. For sympathetic denervation of the upper limbs, interruption of the sympathetic chain from T2 to T4 is required. Although the stellate ganglion has some innervation to the upper limbs, resection of the stellate ganglion results in Horner syndrome (ptosis, myosis, and enophthalmos). Because of this associated morbidity the stellate ganglion is not removed surgically the nerves of Kuntz. Resection of T2 and T3 ganglia (sympathectomy) is thought to be essential to achieve good and durable sympathetic denervation of the arms. The preganglionic fibers may bypass the paravertebral ganglia to synapse with more distal intermediate ganglia or may cross over to innervate the contralateral side as well. Therefore, as mentioned previously a complete sympathectomy includes division of the, preganglionic fibers and excision of the relay ganglia T2 and T3 and the intercommunicating fibers (the nerve of Kuntz). Several authors advocate T4 and T5 resection, especially in patients who undergo the operation for axillary hyperhidrosis. The nerve of Kuntz, originating at the level of T2, provides direct communicating fibers to the brachial plexus. Atkinson and colleagues2 advocate performing sympathotomy by severing all visualized sympathetic branches between the T1 (and C8) ganglion and the T2 ganglion so as to minimize axonal and potential neuronal injury which may increase side effects, particularly compensatory postsympathectomy hyperhidrosis. These include the celiac, aortorenal, and superior and inferior mesenteric ganglia located in the abdominal cavity on the top of, and around the aorta. The primary function of the peripheral sympathetic nervous system is to prevent heat loss by reducing the blood flow to the skin and subcutaneous tissue of the limbs. The increased activity of the postganglionic sympathetic nerves, mediated by norepinephrine, results in decreased blood flow because of stimulation of the vasoconstrictor fibers innervating the blood vessels. There is increased sweating caused by stimulation of the sudomotor fibers innervating the exocrine glands (an activity mediated by acetylcholine, adenosine, and other neuropeptides) as well as piloerection mediated through the activity of the pilomotor fibers that innervate the erector pili muscles. As a result of sympathetic denervation, the blood flow to the skin increases, there is a loss of sweating and piloerection, and the hands after thoracic sympathectomy/sympathotomy and the feet after lumbar sympathectomy become warm, pink, and dry Sympathectomy also results in decreased pain in the ischemic limb, likely. The pain tolerance is better because of decreased tissue concentration of norepinephrine and reduced spinal augmentation of pain transmission to cerebral centers. The maximal effect of the sympathectomy/sympathotomy is immediate, although vasodilation will be less after 1 week because of compensatory mechanisms. Blood flow changes recorded at 6 months following sympathectomy are minimal because of incomplete denervation, regeneration of fibers, and hypersensitivity of the receptors to circulating catecholamines. Several authors have investigated the effect of sympathectomy on blood flow of the limbs. Cronenwett and colleagues17 found no increase of nutrient capillary perfusion as a result of sympathectomy Using intradermal xenon clearance, Moore and Hall18 observed. Rutherford and Valenta19 failed to confirm increased muscle flow as a result of sympathectomy Dalessandri and. It is evident that the effect of sympathectomy on cutaneous blood flow is transient, but this period may be sufficient to heal superficial ulcerations. The more lasting effects of sympathectomy are on sweating, abnormal vasomotor tone, and pain relief.