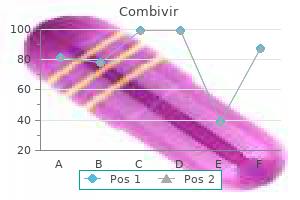
Effective combivir 300mg
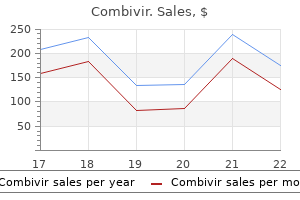
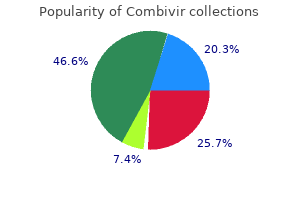
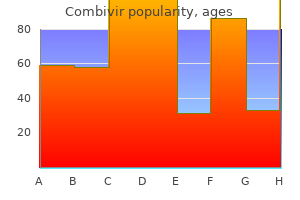
Treatment with radiotherapy or chemotherapy is indicated for relief of cough or dyspnea medications to treat bipolar purchase combivir 300mg without prescription. In general, lung lesions, like other manifestations of Kaposi sarcoma, improve on antiretroviral combination therapy. Typical chest radiograph; note the central nodular densities, with peripheral extension. The chest X-ray shows reticulonodular infiltrates that may vary and disappear spontaneously. Gastrointestinal involvement with ulcers, skin lesions, and lymphadenopathies are also frequent. The disease is diagnosed by direct stain of the sputum, where delicate, gram-labile, branched filaments are detected. Treatment relies on prolonged administration of high doses of trimethoprim-sulfamethoxazole; alternatives are imipenem and the newer fluoroquinolones. Also see Chapter 8 for a discussion of infections that can affect both immu-nocompetent and immunocompromised individuals. The erythematous form of candidiasis consists of brilliant red spots on the tongue or palate. The clinical diagnosis is usually evident; cultures are difficult to interpret, because Candida is found in the mouth of many people without stomatitis. Typically seen as white plaques that detach when scraped, or as red spots on the tongue and palate. Often, Candida stomatitis is associated with esophagitis, which may cause dysphagia and retrosternal pain. If achieving reversal is not possible, some physicians prefer to wait for a relapse, which they then retreat; others favor preventive therapy-for instance, fluconazole 50 mg daily or 150 mg weekly. After years of intermittent treatment or prevention, relapses become more frequent and resistance of Candida is common. Other imidazoles-such as itraconazole solution, voriconazole, or ketoconazole-may remain effective. In other cases, intravenous therapy with amphotericin B at doses of 20-30 mg daily is necessary. Newer agents such as the echinocandins (see Chapter 1) are easier to administer, but expensive. If the lesion persists, a biopsy with viral culture or immunofluorescence is often necessary for diagnosis. Usually, treatment is not necessary, but in resistant cases, topical application of podophyllotoxin can be effective. Acyclovir can also be administered, but usually it causes only temporary regression of the lesions. It produces painless macules or nodules with characteristic purple coloration on the palate, gingivae, or tongue. Cytomegalovirus is less common, causing longitudinal ulcers and viral inclusions on biopsy. Herpes simplex virus type 1 is moderately frequent; type 2 and herpes zoster are less common. However, when esophageal symptoms occur in a patient who does not have clear evidence of Candida stomatitis, other causes must be sought. The lesion can be diagnosed only by biopsy: characteristic viral inclusions are seen in endothelial, epithelial, or smooth muscle cells. This subsection briefly comments on the most frequent causes (also see Chapter 8). In biopsies of the gastrointestinal tract, the submucosa may be filled with characteristic acid-fast microorganisms. Antiretroviral drugs and antibiotics can cause diarrhea (with Clostridium difficile, for example). Colonoscopy shows multiple erosions, and biopsies reveal the characteristic intranuclear inclusions. No treatment has so far proven effective, although oral paromomycin (500-750 mg every 8 hours), macrolides such oral azithromycin (1250 mg daily), oral clarithromycin (500 mg twice daily), and oral albendazole (400 mg daily) can be tried, in addition to symptomatic treatment of diarrhea (loperamide, narcotics). Past treatments were not very effective, and eradication of the organism was usually impossible. Fumagillin (20 mg three times daily for 2 weeks) clears the spores and prevents relapse in most patients (see Chapter 8). Albendazole (400 mg twice daily) is useful in cases of Encephalitozoon intestinalis infection. Such lesions may necessitate admission to hospital and parenteral therapy with high-dose acyclovir. Ulcer on the buttocks resulting from infection with herpes simplex virus 2 (diameter: 5 cm). Screening programs in homosexual patients for this virus have been considered, analogous to those that screen for cervical cancer, as well as vaccination of adolescents have been considered, but are not yet part of routine clinical practice. However, such involvement is usually asymptomatic, and involvement of the gastrointestinal tract without involvement of skin is rare. Occasional complications include bleeding, obstruction, invagination, and perforations. Symptoms of lymphoma are therefore difficult to distinguish from those of opportunistic infections. Chemotherapy is theoretically effective, but often very difficult to administer to these severely immunosuppressed patients. During chemotherapy, perforation with overwhelming peritonitis and sepsis remains a threat. Direct-acting agents, such as boceprevir and telaprevir, are used in combination with pegylated interferon and ribavirin for the first 12 weeks of treatment. They are used in combination with peginterferon and ribavirin for 12 weeks, followed by peginterferon and ribavirin alone for 12-36 weeks. For many coinfected patients with contraindications to interferon, the best option is waiting for interferon-free therapy using a combination of direct-acting agents. At the time of this writing, early results from small series of monoinfected patients look promising; such treatment may become available by 2015. The first signs are usually memory problems, mental slowness, and lack of precision. Clinical examination shows difficulties in comprehension and coordination, abnormal gait, nystagmus, and archaic reflexes. Dementia symptoms are accompanied by apathy and withdrawal that can be mistaken for depression. Magnetic resonance imaging shows an increased T2 signal in the subcortical white matter preferentially in parasagittal regions. Toxoplasma encephalitis usually starts with a focal deficit (hemiplegia, for instance), convulsions, headaches, fever, or confusion. If antibody is absent, or if the patient has taken trimethoprim-sulfamethoxazole prophylaxis, another diagnosis should be considered first. Treat using a combination of sulfadiazine and pyrimethamine, with added folinic acid. If the IgG antibodies are positive and the images are typical, empiric treatment is warranted. Steroids (intravenous dexamethasone 4 mg every 6 hours) may be administered to diminish the cerebral edema.
Combivir 300 mg on-line
A definitive diagnosis requires at least one of the above rabies-specific tests from a skin biopsy symptoms before period order cheapest combivir and combivir, saliva, or brain biopsy. On histology of brain tissue, infection typically appears as encephalitis with Negri bodies, which are eosinophilic neuronal cytoplasmic inclusions. Treatment Once the virus has entered peripheral nerves, administration of Ig and vaccine likely does not prevent central spread, neurologic disease, or mortality. Infectious diseases consultation and the advice of public health authorities are recommended. Vaccination is generally limited to high-risk groups, such as veterinarians, laboratory workers who may come into contact with rabies virus, and international travelers who are likely to come into contact with animals in countries where dog rabies is enzootic and rapid access to post-exposure treatment is limited. Post-exposure prophylaxis Infection with rabies can be prevented with timely postexposure treatment. In 1988, there were more than 350,000 cases world-wide, which dropped dramatically to approximately 1500 reported cases in 2009118. However, due to the ease of world-wide travel, there continues to be importation of cases from endemic areas that may lead to outbreaks in countries thought to previously be free of polio. Outbreaks occurred most often during the summer months, with a higher incidence in temperate climates and areas with poor sanitation. Poliovirus is further subclassified into three different serotypes (types 1, 2, and 3). In some of these patients, poliovirus then causes selective destruction of motor neurons, characterized by the development of motor weakness. Spread of virus to the neighboring motor neurons may occur laterally, Infections of the central nervous system 455 independent of axonal transport or by transneuronal spread. Spinal paralytic poliomyelitis (60% of cases) Classic paralytic polio often begins with severe muscle pain and spasms. Reflexes are initially brisk, but then become absent as neuronal destruction progresses. The paralytic manifestations may be minor (one muscle or group of muscles) or severe (quadriplegia and respiratory failure). The flaccid paralysis of poliomyelitis remains stable for several days or weeks, followed by a slow recovery over months to years. New sprouting and re-innervation of muscle by surviving motor neurons must occur for recovery. Most commonly, the lower cranial nerve nuclei are affected, including those neurons innervating the soft palate and pharynx, resulting in dysphagia, dysphonia, dysarthria, and difficulty handling secretions. Nonpolio enteroviruses are in the differential diagnosis, and the lab should be notified of this when ordering viral cultures. It is difficult to make a definitive diagnosis using serum antibody testing, but the lab can compare acute and convalescent sera. Motor unit action potentials are reduced in number but return during recovery, becoming abnormally large in amplitude, with increased duration and a polyphasic pattern due to reinnervation. Poliomyelitis is confirmed by isolation of the virus from oropharyngeal swabs or stool cultures. Lesions mainly affect the gray matter of the anterior, intermediate, and posterior horns of the spinal cord and motor nuclei of the pons and medulla. Pleconaril is an oral antiviral with activity against enteroviruses122 that has shown mixed results for the treatment of enteroviral encephalitis123. Post-polio syndrome can present complex management issues, with patients experiencing chronic pain, contractures, depression, fatigue, and sleep disorders. The efficacy with three doses is nearly 100%122, and antibodies persist for at least 5 years in the vast majority of patients129. The risk is higher in those with immunodeficiency and it is contraindicated in these patients. Rapid progression occurs following diagnosis, resulting in quadraparesis, severe dementia, seizures, and coma. Disease is localized to the cerebral white matter, although there can also be involvement of the cerebellum, brainstem, and spinal cord. Pathology A definitive diagnosis is made with brain biopsy, and sterotactic biopsy may be required in some circumstances. Histologic examination reveals multiple asymmetric foci of demyelination in differing stages of evolution, found in the cortical and subcortical white matter (450). The enlarged oligodendrocytes show nuclear enlargement and intranuclear hyperchromatic inclusions (451) with homogenous staining. Treatment Several medical therapies have been investigated, including cidofovir140,141, cytarabine142, interferon143, and interleukin-2144, but several trials have been disappointing and there are not enough good clinical data to recommend any of these agents. Organisms do not cause disease in these intermediate hosts, but can become infectious to humans when inhaled. It is not associated with bird guano, but occupies a specific environmental niche in some tropical and subtropical regions, particularly associated with Eucalyptus trees in Australia. These traits allow the organism to evade host immunity, deplete complement, cause cytokine dysregulation, protect cryptococci from temperature changes and antifungals, and inhibit phagocytosis147. The susceptibility to , and severity of, infection are related to the host immunologic status and the size of the fungal inoculum. Approximately 25% of patients present with altered mentation, suggesting clinically apparent encephalitis. Cryptococcosis is known to cause vasculitis and ischemic stroke148, and it should be considered in the differential diagnosis of cerebrovascular disease in the immunocompromised patient. Concomitant pulmonary disease is suggested by cough, shortness of breath, crackles on lung examination, and infiltrates on chest X-ray. Inflammation can be highly variable, including relatively little infiltration to frank granulomas. One must remain aware of immune reconstitution syndrome, leading to an exacerbation of symptoms or development of acute meningeal signs or lymphadenopathy. Cryptococcus gattii is treated with the same antifungal regimens and adjunctive therapy as C. Fungal spores become airborne with disruption of dry soil from construction, wind storms, earthquakes, and other phenomena which disturb the soil. These spherules enlarge, rupture, and release endospores that can gain access to the bloodstream and disseminate to multiple organs, including the meninges of the brain and spinal cord. Classic signs and symptoms of meningitis typically begin within several weeks of exposure, but intervals as long as 2 years have been reported160. Erythema nodosum occurs in 5% of patients overall, and a higher proportion of those with disseminated infection161. There is typically a slight elevation in protein with a profound hypoglycorrhachia. Hydrocephalus is the most common complication, and is seen in up to 50% of patients with coccidioidal meningitis. Serum positivity for antibodies is suggestive, but not 100% specific, and must be interpreted with caution.
Diseases
- Chaotic atrial tachycardia
- Hypotrichosis
- Pyruvate carboxylase deficiency
- Finnish type amyloidosis
- Adrenal hyperplasia
- Multinodular goiter cystic kidney polydactyly
Buy combivir 300mg visa
Procedures requiring the removal of thick bone beyond the capacity of the microdebrider led to the development of a variety of drills and burrs treatment zit buy combivir from india. One major advantage of drills over traditional techniques for bone removal is that the drill requires relatively small amount of force to be applied by the operator, permitting expeditious, yet controlled bone removal. The drills themselves have been designed with a slimmer profile to permit simultaneous use with an endoscope in a narrow surgical field, and to facilitate movement through the nostrils. There is a protective sheath along the shaft of the drill burr to protect against collateral friction damage to adjacent tissues (including soft tissues of the nostril). Some also have a sheath to protect the posterior aspect of the burr offering further protection to adjacent structures. Continuous suction/irrigation has also been designed into handpieces to decrease the number of instruments the endoscopic surgeon must manipulate at one time. Other modifications aimed at addressing some of the unique ergonomic and length concerns for endonasal drilling include longer sheaths, extended drill attachments for the skull base, telescoping drill bits, and angulated handpieces. Like any other instrument, microdebriders have certain limitations that must be recognized if these tools are to be used effectively and safely. This means that the tactile feedback during surgery is markedly diminished with microdebriders. Bhatti et al described two cases of ocular injury, one resulting in restrictive ophthalmoplegia and the other in transection of the medial rectus. There is still opportunity to make great strides in the arena of endoscopic drills. One fact common to all drills is that the number of flutes on the burr determines how aggressively the drill will take down bone. A burr with few deep flutes will cut very aggressively, resulting in the rapid take down of bone. Something that may be counter-intuitive to the novice user is that faster rotational speeds actually improve control, as there is less chance for chatter or tear out. When more control is needed, diamond burrs are also available, which are generally much less aggressive then fluted (cutting) burrs and are good for smoothing bone edges. Diamond burrs are also used in situations where bone needs to be thinned close to important structures, and controlled movements removing small amounts of bone are needed such as along the skull base and orbital apex. This involves thick bone removal beginning in the region of the maxillary line and proceeding anteriorly. Removal of thick bone during orbital decompression (particularly the lateral and inferior walls) and optic nerve decompressions has also been described in the literature as being augmented by the use of an endoscopic drill. The goal is to develop the most ergonomic, superior functioning, endoscopic drill that minimally obstructs the narrow operative field, characteristic of endoscopic rhinologic surgery. In 2004, Jho and Ha published a three-part series on the use of endoscopic drils to access the midline anterior fossa skull base, cavernous sinus, clivus, and posterior fossa. Perhaps the most common contemporary application of endoscopic drilling is in surgery of the frontal sinus. After conservative measures aimed at widening the frontal recess fail, more aggressive techniques targeting the frontal sinus ostium and the floor of the sinus can be pursued. Drills have also had a significant impact on the endoscopic surgery of the orbit and lacrimal system. Endoscopic orbital techniques offer the advantages of enhancing visualization while providing a direct route to the posterior orbit and apex. Radiofrequency Ablation Radiofrequency ablation (coblation) is a technology patented by ArthroCare (Austin, Texas, United States) in 1997, initially intended for use in cartilage ablation during arthroscopy. As some studies suggest that a plasma field is unlikely to be created outside a vacuum, Zinder theorized that the decreased thermal damage during coblation has more to do with vaporization of the saline solution than creation of a plasma field. Advantages and Evidence the most common use of coblation technology in otolaryngology is for tonsillectomy, where some studies have suggested less postoperative pain and a faster recovery. It should be noted that radiofrequency ablation technology has only recently been introduced to the field of rhinologic surgery, which explains the paucity of data regarding this technology in the literature. Coblation technology was initially adapted for use in rhinologic surgery for inferior turbinate reduction. A study by Eloy et al compared blood loss with operative time in patients undergoing coblator-assisted polypectomy with those undergoing a microdebriderassisted polypectomy. The estimated blood loss was 307 mL in the coblation group compared with 627 mL in the microdebrider cohort. A subgroup analysis revealed that the difference in blood loss was only significant, however, in revision cases. They found a decreased operative time when this technique was compared to traditional bipolar cautery for resection, with no statistical increase in complications noted. All surgeries on the sinuses or extending beyond the confines of the sinonasal tract therefore require the controlled take down of varying amounts of bone. Due to the close proximity of important soft tissue structures, it is crucial to take down bone with as little impact on the surrounding soft tissue as possible. Basic Science and Current Technology Ultrasonic aspirators operate on the converse piezoelectric effect, whereby application of an electric charge to certain crystals creates a reversible mechanical deformation (direct piezoelectric effect refers to electricity being generated by mechanical stress on the crystals). The piezoelectric effect was first described by Pierre and Jacques Curie in the late 19th century. The technology was first described within the medical field in its use for phacoemulsification of the lens during cataract surgery by ophthalmologists. Advances in the field now allow aspirators to expeditiously remove bone while still being respectful of nearby soft tissues. There is a stack of piezoelectric discs, or tubular piezoelectric crystal, within the handpiece that expands and contracts when alternating current is applied causing vibration. This high-frequency vibration breaks down hydrogen bonds in tissue proteins, resulting in their denaturation. The actual cutting of tissue is secondary to cavitation, which is the formation, expansion, and subsequent implosion of small vapor bubbles within the tissue, caused by the ultrasonic waves. The resulting emulsified tissue is then removed by continuous irrigation and suction. The technology was designed such that the frequency of vibration can be adjusted and thus optimized for either bone or soft tissue removal. Power can be adjusted on the ultrasonic aspirator, with greater power resulting in increased amplitude of tip stroke and more aggressive take down of bone or soft tissue. Also, to date there have been no studies examining the extent of heat generation or transmission to adjacent structures during prolonged use of this instrument, as would be necessary for tumor or polyp removal. The theory behind the technology is that radiofrequency ablation of the tissue is supposed to decrease thermal spread. Other limitations include a relative 80 Rhinology and Endoscopic Skull Base Surgery aspirators has been described in a variety of neurosurgical procedures, and they have been praised for their ability to minimize damage to soft tissue structures. Greywoode et al described the use of the ultrasonic aspirator for removal of the bony portion of the inferior turbinate, leaving the soft tissues of the inferior turbinate intact. A Limitations this technology, while novel and cutting edge, does not have significant literature supporting rhinologic applications in which it may be advantageous or even preferable. While it theoretically carries benefits over other powered instruments related to its tissue selectivity, the impact of this on actual outcomes has not yet been demonstrated. Another drawback is that the cost of the unit itself is substantial and its use carries the ongoing costs of disposables. Further, this instrument does remove bone more slowly than a highspeed drill and importantly data on heat generation at the tip during bone emulsification are presently lacking. Instrument Advantages and Evidence A novel aspect of this new technology and one of its most advantageous features is the programmable selectivity it provides.
Purchase combivir line
Nearly one-half of patients who are shunted will require shunt revision within 3 years for shunt malfunction or infection treatment molluscum contagiosum cheap 300 mg combivir free shipping. Brainstem auditory evoked responses and somatosensory evoked responses may demonstrate slowing consistent with brainstem or spinal cord compression related to Chiari Type I malformation. Some surgeons open the dura in the posterior fossa and add a graft (duraplasty); others do not manipulate the dura. Some children with syrinxes will present with scoliosis prior to the development of any motor or sensory symptoms. Somatosensory evoked responses may be delayed due to involvement of the cervical or thoracic spinal cord. When the syrinx extends into the brainstem, brainstem auditory evoked responses may be abnormal. The cerebellar tonsils are low-lying, indicating associated Chiari malformation Type I. The onset of visual loss is usually gradual, but in some patients visual loss may occur precipitously, requiring rapid surgical intervention. This sagging causes traction on pain-sensitive structures within the head and leads to headache. Overdrainage by a ventriculo-peritoneal shunt is an important treatable cause of intracranial hypotension syndrome. The headache may or may not be throbbing, it is usually bilateral, and may be frontal, occipital, or holocephalic in location. Other, highly variable symptoms include nausea, vomiting, diplopia, altered hearing, dizziness, neck pain, blurred vision, and radicular pain in the upper extremities. Laughing,coughing,ortheValsalvamaneuvercan exacerbate the headache of intracranial hypotension. H Low-lying tonsils in intracranial hypotension syndrome must be differentiated from Chiari malformation Type I. T It is currently felt that volume depletion due to intracranial hypotension causes a compensatory venous engorgement, thickening of the meninges, and a downward displacement of the brain. The gadolinium enhancement of intracranial hypotension is thick, diffuse, and linear and involves the pachymeninges of both the supra-tentorial and infra-tentorial compartments of the brain. Controlled studies of the efficacy of these remedies are not available and most are of questionable value. When conservative remedies fail including bed rest, relief can usually be obtained with an epidural blood patch using autologous blood. When a meningeal tear can be demonstrated radiologically, surgical repair may be necessary in some cases. Other investigations Lumbar puncture shows an opening pressure of 60 mmH2O or less. Indium-111 is used as a tracer and when a leak is present activity does rise up above the basal cisterns to the cerebral convexities. Prevalence of probable idiopathic normal pressure hydrocephalus in a Norwegian population. Anatomy and physiology Nerve fibers subserving the sense of smell have their cells of origin in the mucous membranes of the upper and posterior parts of the nasal cavity. In the olfactory bulb, the axons of the receptor cells synapse with mitral and tufted cells, the dendrites of which form brush-like terminals or olfactory glomeruli. Anterior commissure 638 Left and right olfactory bulbs Tufted and mitral cells (secondary olfactory cells) Glomeruli Olfactory gland Cribriform plate of skull Basal cell Supporting cell (sustentacular) Primary olfactory cell Primary axon Mucus Aromatic molecule 638 Schematic illustration of olfactory epithelium, bulb, and tract. Fibers in the lateral stria give off collaterals to the anterior perforated substance, and terminate in the primary olfactory cortex, which comprises the anterior olfactory nucleus, the piriform cortex, the anterior cortical nucleus of the amygdaloid complex, and the entorhinal cortex1. Etiology and pathophysiology Loss of, or reduction of, the sense of smell may be caused by local disease in the nose or by a lesion along the olfactory pathway. It may present as impaired taste, because taste depends largely on the volatile particles in foods and beverages, which reach the olfactory receptors through the nasopharynx; the perception of flavor is a combination of smell and taste. However, these patients are able to distinguish the elementary taste sensations (sweet, sour, bitter, and salty). Tip E Olfactory impulses reach the cerebral cortex without relay through the thalamus and this is a unique feature among the sensory systems. After temporal lobectomy there may be ipsilateral deficits in olfactory discrimination. Dysfunction can be a distortion of smell (dysosmia or parosmia), which may be due to foul odors within the nasal cavity in association with nasal infections, or a spontaneous sensation of smell in the absence of a stimulus (phantosmia). From the ganglion, the sensory fibers enter the pons and terminate on three major sensory nuclei that are located in the brainstem from the mesencephalon to the upper cervical spinal cord. V2 C2, C3 V3 C2, C3 C3, C4 C3 C4 Second (maxillary) division or V2 Innervates the skin of the ipsilateral lower eyelid, lateral nose, upper lip, cheek sparing the skin over the angle of the mandible (which is innervated by the C2/C3 nerve roots), the lower half of the cornea, conjunctiva and iris, the mucous membranes of the maxillary sinus, palate, nasopharynx, upper gum, the upper teeth, and the dura of the middle cranial fossa (via middle meningeal artery). V2 enters the skull through the foramen rotundum and then passes in the inferolateral wall of the cavernous sinus to the trigeminal sensory ganglion. Tip E V1 enters the skull through the superior orbital fissure, V2 enters the skull through the foramen rotundum, and V3 enters the skull through the foramen ovale. After the trigeminothalamic tracts synapse in the thalamus, third-order neurons from the thalamus project on the somatosensory cortex. At posterior fossa exploration, many patients are found to have a trigeminal root that is compressed or even grooved by a blood vessel, usually the superior cerebellar artery. Under these conditions, normal impulses elicited by light mechanical stimulation can recruit nearby pain fibers, particularly if they have already been made hyperexcitable by axonal damage. It commonly starts in the dermatomal distribution of the second or third division of the trigeminal nerve; only 5% start in the first division. Trigger points are areas around the nose, lips, or mouth which, when touched, evoke a paroxysm of pain. When sites are inside the mouth patients become hesitant about eating, drinking, and brushing their teeth.
Buy discount combivir 300 mg line
Ca2+ channel blockers enhance neuromuscular blockade produced by both competitive and depolarizing antagonists symptoms 6 weeks proven combivir 300mg. Miscellaneous drugs that may have significant interactions with either competitive or depolarizing neuromuscular blocking agents include trimethaphan, lithium, opioid analgesics, procaine, lidocaine, quinidine, phenelzine, carbamazepine, phenytoin, propranolol, dantrolene, azathioprine, tamoxifen, magnesium salts, corticosteroids, digitalis glycosides, chloroquine, catecholamines, and diuretics. Responses to repetitive or tetanic stimuli are most useful for evaluation of blockade of transmission. Hence, tracheal intubation can be performed before onset of complete block at the adductor pollicis, whereas partial recovery of function of this muscle allows sufficient recovery of respiration for extubation. Preventing Trauma During Electroshock Therapy Electroconvulsive therapy of psychiatric disorders occasionally is complicated by trauma to the patient; the seizures induced may cause dislocations or fractures. Inasmuch as the muscular component of the convulsion is not essential for benefit from the procedure, neuromuscular blocking agents, usually succinylcholine, and a short-acting barbiturate, usually methohexital, are employed. Botulinum toxins and dantrolene act peripherally to reduce muscle contraction; a variety of other agents act centrally to reduce skeletal muscle tone and spasm. Originally approved for the treatment of the ocular conditions of strabismus and blepharospasm and for hemifacial spasms, botulinum toxins have been used to treat spasms and dystonias and spasms associated with the lower esophageal sphincter and anal fissures. Like the bloom of youth, the reduction of wrinkles is temporary; unlike the bloom of youth, the effect of botulinum toxin can be renewed by readministration. Because of its efficacy in managing Control of Muscle Spasms and Rigidity Adverse Effects the important untoward responses of the neuromuscular blocking agents include prolonged apnea, cardiovascular collapse, those resulting from histamine release, and, rarely, anaphylaxis. Related factors may include alterations in body temperature; electrolyte imbalance, particularly of K+; 184 low plasma butyrylcholinesterase levels, resulting in a reduction in the rate of destruction of succinylcholine; the presence of latent myasthenia gravis or of malignant disease such as small cell carcinoma of the lung with Eaton-Lambert myasthenic syndrome; reduced blood flow to skeletal muscles, causing delayed removal of the blocking drugs; and decreased elimination of the muscle relaxants secondary to hepatic dysfunction (cisatracurium, rocuronium, vecuronium) or reduced renal function (pancuronium). Susceptibility to malignant hyperthermia, an autosomal dominant trait, is associated with certain congenital myopathies, such as central core disease. In the case of overdose, a muscarinic cholinergic antagonist (atropine or glycopyrrolate) may be added to prevent undue slowing of the heart (see Synergisms and Antagonisms). Competitive blocking agents, however, are commonly used in pediatric patients; generally, dosage is similar to adults but both rate of block onset and clearance are faster. There are normal changes at the neuromuscular junction in elderly patients that may affect pharmacodynamics of neuromuscular blocking agents. The end result of these changes is decreased efficiency of neuromuscular transmission. General physiological changes in aging patients, including decreases in body water and muscle, increases in total body fat, and decreases in renal and hepatic function, also contribute to the action of neuromuscular blockers. The dosing of succinylcholine is not significantly altered in the geriatric population. Among the competitive blocking agents, initial dose requirements are unchanged, however, the onset of blockade is delayed in an age-related manner, and block is prolonged. For compounds such as atracurium that are not dependent on hepatic or renal blood flow for their elimination, pharmacodynamics and kinetics are largely unaltered. The amino steroids pancuronium, vecuronium, pipecuronium, and rocuronium have even less tendency to release histamine after intradermal or systemic injection (Basta, 1992; Watkins, 1994). Histamine release typically is a direct action of the muscle relaxant on the mast cell rather than anaphylaxis mediated by immunoglobulin E. Unlike the neuromuscular junction, ganglia do not have discrete end plates with focal localization of receptors; rather, the dendrites and nerve cell bodies contain the receptors. The characteristics of nicotinic-receptor channels of the ganglia and the neuromuscular junction are similar. Measurements of singlechannel conductances indicate that the characteristics of nicotinic receptor channels of the ganglia and the neuromuscular junction are similar. In such circumstances, sympathomimetic amines may be given to support the blood pressure. Antihistamines are definitely beneficial to counteract the responses that follow the release of histamine, particularly when administered before the neuromuscular blocking agent. Sugammadex at doses greater than 2 mg/kg is able to reverse neuromuscular blockade from rocuronium within 3 min. Sugammadex clearance is markedly reduced in patients with impaired renal function, Reversal of Effects by Chelation Therapy. Nicotine Nicotine is of considerable medical significance because of its toxicity, presence in tobacco, and propensity for conferring dependence on its users. The chronic effects of nicotine and the untoward effects of the chronic use of tobacco are considered in Chapter 24. Nicotine can increase heart rate by excitation of sympathetic ganglia or by paralysis of parasympathetic cardiac ganglia, and it can slow heart rate by paralysis of sympathetic or stimulation of parasympathetic cardiac ganglia. Finally, nicotine can stimulate secretion of epinephrine from the adrenal medulla, which accelerates heart rate and raises blood pressure. The first group consists of drugs with specificities similar to nicotine: lobeline, tetramethylammonium, and dimethylphenylpiperazinium. The major action of nicotine consists initially of transient stimulation and then a more persistent depression of all autonomic ganglia. Whereas stimulation of the ganglion cells coincides with their depolarization, depression of transmission by adequate doses of nicotine occurs both during the depolarization and after it has subsided. However, the stimulant phase is obscured largely by the rapidly developing paralysis. These include mechanoreceptors that respond to stretch or pressure of the skin, mesentery, tongue, lung, and stomach; chemoreceptors of the carotid body; thermal receptors of the skin and tongue; and pain receptors. Chronic exposure to nicotine in several systems causes a marked increase in the density or number of nicotinic receptors, possibly contributing to tolerance and dependence. Nicotine is thought to act as an intracellular pharmacological chaperone; it is uncharged at physiological pH and readily permeates the plasma membrane. Chronic low-dose exposure to nicotine also significantly increases the t1/2 of nicotinic receptors on the cell surface (Kuryatov et al. The onset of symptoms of acute, severe nicotine poisoning is rapid; they include nausea, salivation, abdominal pain, vomiting, diarrhea, cold sweat, headache, dizziness, disturbed hearing and vision, mental confusion, and marked weakness. A slurry of activated charcoal is then passed through the tube and left in the stomach. Nausea, vomiting, and occasionally diarrhea are observed following systemic absorption of nicotine in an individual who has not been exposed to nicotine previously. However, due to the role of ganglionic transmission in both sympathetic and parasympathetic neurotransmission, the antihypertensive action of ganglionic blocking agents was accompanied by numerous undesirable side effects. Mecamylamine, a secondary amine with a channel block mechanism similar to hexamethonium, is available as an antihypertensive agent with good oral bioavailability. For example, blockade of sympathetic ganglia interrupts adrenergic control of arterioles and results in vasodilation, improved peripheral blood flow in some vascular beds, and a fall in blood pressure. The absorption of quaternary ammonium and sulfonium compounds from the enteric tract is incomplete and unpredictable. This is due both to the limited ability of these ionized substances to penetrate cell membranes and to the depression of propulsive movements of the small intestine and gastric emptying. Although the absorption of mecamylamine is less erratic, reduced bowel activity and paralytic ileus are a danger. Therapeutic Uses; Adverse Effects Cardiovascular Effects Existing sympathetic tone is a critical determinant of the degree ganglionic blockade will lower blood pressure. Changes in heart rate following ganglionic blockade depend largely on existing vagal tone. In humans, only mild tachycardia usually accompanies the hypotension, a sign that indicates fairly complete ganglionic blockade.
Syndromes
- Vomiting
- Blood clots in the legs that may travel to the lungs
- If the medication was prescribed for the patient
- Thickening and scarring of the sac like covering of the heart
- Improved fitness, making it easier to do everyday activities
- Meat, poultry, fish, dry beans, eggs, and nuts -- eat at least 3 servings
Trusted combivir 300 mg
For smaller pituitary lesions that are off the midline and for those larger tumors extending laterally into the cavernous sinus medicine 5852 discount combivir 300 mg mastercard, the contralateral nasal cavity may present a better angle of initial approach. The tumor is then removed with a combination of suction and neurosurgical spatulas and ring curettes with different angulations. Tumor tissue is usually easily differentiated from normal yellow pituitary tissue. Once the bulk of the tumor is removed, the endoscope is inserted into the sella to facilitate more detailed exploration, and angled endoscopes may be used to examine the crevices of the sella. The diaphragm of the sella and normal pituitary tissue often tend to descend into the void created by tumor removal. This can obscure visualization, especially in the lateral and posterior or superior recesses of the cavity. To improve visualization in this setting, we have developed the technique of "hydroscopy," using normal saline irrigation under several centimeters water pressure attached to the endoscopes. The pressure of the saline expands the soft tissue boundaries of the sella including the diaphragm, washes out small bits of residual tumor, improves visualization, and facilitates inspection of the cavity and ensures as complete a removal of tumor tissue as possible. At the end of the procedure, hemostasis is obtained using a hemostatic substance such as microfibrillar collagen, which is then irrigated out. Caution must be exercised as carotids can be dehiscent in up to 22% of sphenoid sinuses. The sella is then entered with a chisel or high-speed drill depending on the thickness of the sellar face and the opening enlarged with a Kerrison rongeur. Occasionally, bleeding can be encountered from anterior intercavernous connections; this is controlled with microfibrillar collagen, pressure, or bipolar cautery. Patients are generally discharged home on antibiotics and hormonal replacement as necessary and nose blowing or sneezing is avoided. At the first postoperative visit approximately 3 weeks later, endoscopy is performed to confirm appropriate healing. Postoperative leaks were managed with lumbar drain (n = 14) or endoscopic repair (n = 6). One patient with a large arachnoid cyst had two unsuccessful repair procedures after failure of conservative management and eventually required lumboperitoneal shunting. One of the 11 patients had a history of chronic rhinosinusitis and previous endoscopic sinus surgery. The nasal anatomy in our approach remains essentially undisturbed, thereby allowing for the sinuses to continue functioning. Only one patient had persistent chronic rhinosinusitis, and this was a pre-existing condition and was not exacerbated by the surgery. Two neurological complications occurred in the same series,20 pneumocephalus and cranial neuropathy (1. One patient suffered bilateral abducens palsy in the immediate postoperative course. This patient subsequently had a recurrence of his nonsecreting pituitary adenoma, had revision surgery and experienced no cranial neuropathy after the revision surgery. The authors compared outcomes after purely endoscopic resection versus traditional microscopeaided resection. They examined retrospective data on 25 patients surgically treated for a pituitary lesion, with all procedures performed by the same senior neurosurgeon who was initially unfamiliar with the endoscopic endonasal approach. Internal view of the sella after removal of the pituitary Outcomes Senior et al20 examined the mortality rate in their series of 176 consecutive patients and found a mortality rate of 0. Most mortality reported in the literature is because of medical complications such as pulmonary embolus or cardiac events. Mortality related to the surgery itself is most often secondary to incomplete resection of large, suprasellar tumors that develop significant edema and irreversible neurological insult. The wide range is likely because of the small numbers of patients in some of the other series. The rate of vascular complications including intracranial hemorrhage, cerebral vascular accident, epistaxis, and intraoperative hemorrhage was 5. Epistaxis controlled with pressure, cauterization, or anterior packing occurred in six resections (3. One patient with a conchal sphenoid early in the series had significant cavernous bleeding from an anterior communicating sinus that resulted in aborting the procedure. Another patient taking an antiplatelet medication (clopidogrel) perioperatively had 900 mL of blood loss and required blood transfusion. There were no episodes of massive epistaxis, cavernous sinus thrombosis, carotid injury, subdural, or subarachnoid hematoma in any of the 193 procedures. Of the patients who had pre- and postoperative imaging studies, 14 (66%) of 21 endoscopically treated patients had gross total resection; 4 patients had two or more operations, and 10 (66%) of 15 patients reported complete symptom resolution at followup. The first nine patients who were treated endoscopically had a mean surgical time of 3. The difference in length of operation between the first nine and the last eight patients treated endoscopically was significantly different. They estimated that the learning curve for endoscopic resection should be 17 or less procedures. Other factors examined included intraoperative blood loss, length of stay, and tumor histology and were similar between the three groups. Kabil et al23 performed a retrospective study of 300 patients who underwent fully endoscopic endonasal pituitary adenoma resection during a 6-year period. Data on outcomes were collected and compared with mean values calculated from several transseptal transsphenoidal reports. From a total of 300 pituitary adenomas treated endoscopically, 139 (46%) were hormonally active, whereas 161 (54%) were nonfunctioning. Remission, being defined as no hormonal or radiologic evidence of recurrence within the time frame of the followup, was demonstrated in 127/134 (95%) of enclosed and 144/166 (87%) of invasive adenomas. A comparison of fully endoscopic endonasal versus transseptal transsphenoidal remission results revealed an improved outcome using the fully endoscopic endonasal technique for all hormonesecreting tumor types: adrenocorticotropic hormone (86 vs. The authors also noted a marked reduction in complications related to the endoscopic procedure, indicating that the fully endoscopic endonasal technique is a safe and effective method for the removal of pituitary adenomas providing more complete tumor removal and reducing complications. The use of the natural ostium preserves a functional sphenoid cavity that can be easily monitored postoperatively. The use of this minimally invasive approach has been shown to decrease the length of patient hospital stay, and the two-team approach using an otolaryngological team working in conjunction with a neurosurgical team has a short learning curve and has been shown to have a low rate of postoperative complications. Pioneers in the development of transsphenoidal surgery: Theodor Kocher, Oskar Hirsch, and Norman Dott. The Pituitary Body and Its Disorders: Clinical States Produced by Disorders of the Hypophysis Cerebri. Harvey Cushing and Oskar Hirsch: early forefathers of modern transsphenoidal surgery. Partial Hypophysectomy for acromegaly: with remarks on the function of the hypophysis. Computerassisted neurosurgical navigational system for transsphenoidal surgery-technical note. Preliminary comparison of the endoscopic transnasal vs the sublabial transseptal approach for clinically nonfunctioning pituitary macroadenomas. The one-nostril transnasal transsphenoidal extramucosal approach: the analysis of surgical technique and complications in 529 consecutive cases. Comparison of endoscopic and microscopic removal of pituitary adenomas: single-surgeon experience and the learning curve. Transnasal transsphenoidal hypophysectomy: choice of approach for the otolaryngologist. Wang Endonasal approaches to the skull base are classified based on their orientation in sagittal and coronal planes. In the posterior (inferior) coronal plane, the endonasal approach extends laterally below the petrous bone to the medial jugular tubercle and jugular bulb. For centrally located lesions, an endonasal approach provides maximal access with minimal manipulation of normal neural and vascular structures.
300mg combivir otc
Group two includes patients with more advanced disease or revision surgery with limited landmarks medications for ibs buy combivir 300 mg low cost, in which image guidance was not necessary but may be beneficial. Image guidance is recommended for patients in group three, as these patients have disease processes encroaching upon or involving the anterior skull base, pterygomaxillary fossa, infratemporal fossa, or extensive polypoid disease. Open skull base surgery advanced quickly in the 1970s as techniques for surgical exposure and skull base reconstruction using pedicled and free tissue flaps were consistently used. For 40 years, pituitary tumors were removed through a sublabial approach with fluoroscopic guidance. In the 1950s and 1960s, fluoroscopic imaging allowed for the identification of microsurgical instruments in the sphenoid sinus and sella for pituitary surgery. In the 1980s, endoscopic sinus surgery was introduced in the United States and since that time, improvements in endoscopic telescopes and camera systems have allowed sinus surgery to be visualized over video monitoring systems. Repeat scans of the operating field were taken intraoperatively to confirm probe tip positions, which was very impractical. This method of image acquisition intraoperatively was abandoned for neurosurgical purposes. However, this still presented complications because the frame of reference in neurosurgery was most often soft tissue, which often became an unreliable source after initiating surgery. When coupled together, this technique has been beneficial in situations where anatomy has been altered, such as disease progression, pneumatization anomalies, fibro-osseous lesions, or other bony lesions. Tabaee et al published the first comparative study looking at the quality of life after endoscopic sinus surgery performed with and without image guidance. Additionally, the study found no statistical significance in incidence of complications or need for revision surgery. Studies indicate that increased operative time is the biggest complaint of image-guided systems. Sindwani and Metson analyzed 33 patients who had either undergone osteoplastic frontal sinus obliteration using image guidance or obliteration via traditional techniques. Although the numbers are small, statistical significance was obtained, suggesting that image guidance increased the safety of this complex procedure. The question as to when it is appropriate to use imageguided systems will probably never be answered with level 1 evidence. To appropriately power such a randomized study with significance would require anywhere between 3000 and 30,000 patients. Sources of registration error with image guidance systems during endoscopic anterior cranial base surgery. Intraoperative imageguided surgery of the lateral and anterior skull base in patients with tumors or trauma. Quality of life and complications following image-guided endoscopic sinus surgery. Summary Image-guided sinus surgery has evolved into a valuable adjunct for rhinologic and skull base conditions. Further comparative studies with and without image guidance would be helpful to answer two important questions. Does image guidance improve the safety of functional endoscopic sinus surgery and endonasal skull base surgery Does image guidance improve the quality of the surgery performed and improve long-term benefits Krempl meatus from the pyriform aperture anteriorly often to the choana posteriorly. The inferior turbinate bone is a thin, curved bone that articulates with the maxilla at the lateral nasal wall. The nasal septum and inferior turbinates are covered with pseudostratified ciliated (respiratory) epithelium with numerous mucous-producing goblet cells. Beneath the epithelium is the lamina propria, which is rich with seromucinous glands and cavernous vascular tissue with large venous sinusoids. The septal blood flow is supplied by branches from the ethmoidal, sphenopalatine, greater palatine, and labial arteries. Knowledge of each branch is important for proper injection of local anesthetics and vasoconstrictors before surgery. Septal abnormalities and turbinate hypertrophy can often prohibit the introduction of endoscopic instruments, and limit good visualization during surgical management of sinus and skull base pathology. Septal surgery is also often required to achieve other important objectives: maximizing nasal tip and dorsal stability, establishing an adequate and long-lasting airway for the patient, and removing any sinus outflow obstructions. While conventional closed septoplasty is a standard surgical approach for many otolaryngologists, conservative and endoscopic techniques are becoming more prominent. This chapter reviews techniques for both approaches as well as turbinate reduction, which commonly accompanies septal deviation surgery. Anatomy the nasal septum is the vertical midline structure that extends posteriorly from the columella and divides the nose into roughly symmetric halves. The bony and cartilaginous septal floor is anatomically stabilized in a groove of the maxillary crest. The inferior turbinates are paired structures consisting of bone and soft tissue that run the length of the inferior Perpendicular plate Vomer Preoperative Patient Evaluation Nasal airway obstruction remains the most common indication for surgery of the nasal septum and turbinates. Turbinate and rarely septal mucosal abnormalities can result in turbulent nonlamellar nasal airflow and the subjective sensation of nasal obstruction. This can cause inflammatory cell infiltration of the lamina propria, reactive engorgement of the venous sinusoids, and subepithelial edema. Examples of such processes include infectious rhinosinusitis and allergic rhinitis. Secondary changes to the lymphatic and venous drainage, and to the connective tissue within the lamina propria after prolonged inflammation, lead to more permanent hypertrophy of these structures. This renders more resistance to topical decongestants and anti-inflammatory medications such as steroids. Nasal airflow and/or sinus outflow tracts can also be disrupted by anatomic abnormalities such as septal deviation, spur, fracture, or dislocation from the maxillary crest. These may be caused by former nasal trauma, previous surgery, or congenital factors. When nasal airway obstruction persists despite maximal medical management, such as nasal steroids and topical antihistamines, surgical treatment is indicated. A proper history and physical examination with nasal fiberoptic evaluation is used to rule out other potential causes of nasal obstruction that may need to be addressed. Maxillar y crest 87 88 Rhinology and Endoscopic Skull Base Surgery Allergic rhinitis, rhinitis medicamentosum, polyps, neoplasms, concha bullosa, adenoid hypertrophy, choanal and pyriform stenosis, severe nasal dorsal deformity, lateral nasal wall collapse, and poor tip support should be properly diagnosed and managed. The region of septal deflection should also be noted during the examination as this will guide proper surgical planning and technique. A more caudal deviation may prompt a traditional closed approach to the septum, for example, while an isolated more posterior deviation or spur may be better addressed endoscopically. Complex cases should prompt an open and honest discussion with the patient concerning the higher risk for complications and reasonable expectations. Patients should also be informed preoperatively about what to expect after surgery and the common and most severe complications that can occur. Plane of dissection Cartilage Surgical Technique Septoplasty Traditional Closed Headlight Approach Septoplasty can be performed with appropriately administered local anesthesia and sedation, however, the procedure is usually performed under general anesthesia. The most important surgical preparations in either situation are the use of a topical decongestant (oxymetazoline, neosynephrine, or 4% cocaine solution) and submucoperichondrial injection of a local anesthetic mixture containing epinephrine (1:100,000 being the most common concentration). Under headlight illumination, a #15 scalpel is used to make either a hemitransfixion incision at the caudal edge of septal cartilage or a Killian incision just rostral to it. Establishing the correct plane helps minimize blood loss and prevent septal tears. A nasal speculum is placed in the incision with intermittent use of a Frazier suction to improve visualization. A Woodson elevator and floor of nose tunnel helps prevent tears raising the flap around bony spurs and the septal-maxillary crest junction. Much of this elevation may need to be performed without direct visualization because of anatomic constraints. If so, maintaining contact between the tip of the Cottle or Woodson elevator and the septal cartilage is important to ensure that the proper plane of dissection is maintained. Caudal cartilaginous deformities can either be reshaped by scoring the cartilage with a knife on the opposite side of the deflection, or they can be resected being sure to leave at least 1 to 1. Resected cartilage can be carved and placed as a caudal strut to improve the stability of the nasal tip, to increase nasal projection, or to help correct a caudal deflection. Alternatively, cartilage can be banked between submucoperichondrial flaps before closure for potential future procedures if needed. Significant dorsal deflections are important to recognize and address as they can be a significant source of "memory" and redeviation of caudal cartilage.
Discount combivir 300 mg
Pupillary reflexes Light reflex the normal pupil contracts briskly in the eye to which the light is directed (direct response) and also in the opposite eye (consensual response) symptoms 9 days after iui order 300mg combivir with mastercard. Shining a light into either eye fails to evoke a direct or consensual response in the affected eye, because of the defect in the efferent arc of the reflex. However, shining a light in the eye ipsilateral to the lesion (the affected eye) evokes a consensual reaction in the eye contralateral to the lesion (the unaffected eye) because of the preserved afferent pathway. Accommodation reflex Any lesion involving the pupilloconstrictor muscle fibers will impair the reaction of accommodation. Increased age and parasympathetic and sympathetic neuropathies are associated with a reduced ratio. Reduced sweating below the knee in a peripheral neuropathy (723), and reduced sweating following a sympathectomy (724). Sweating Autonomic neuropathies affecting sympathetic efferent fibers are associated with impaired sweating. The quantitative sudomotor axon reflex test is a test of post-ganglionic sympathetic sudomotor function. This test is limited if the patient is nervous and resting skin blood flow is minimal. This is because of the denervation supersensitivity of the constrictor muscle of the pupil. History, examination Underlying and associated disorders, such as diabetes mellitus and amyloidosis (see above), need to be excluded. However, these tests are not commercially performed in Australia and many other countries. It increases circulating effective blood volume and has a mild sympathetic effect. Have caution with long-term use, where domperidone up to 10 mg three times per day in adults is preferable. Tip E There is a range of pharmacologic and physical treatments for symptomatic management of autonomic neuropathies. Anatomy A peripheral nerve consists of a cell body and about six fascicles, each of which contains many myelinated and unmyelinated axons. Each fascicle has small nutrient blood vessels which are integral to its function (725). A motor unit consists of an anterior horn cell, its axon, the neuromuscular junctions, and all of the muscle fibers innervated by the axon. Collagen tissue, elastic fibers, and fatty tissue that bind individual fascicles together, providing protection from compression. The sensory modalities include proprioception, position sense, and touch sensation. They branch into arterioles that pen etrate the perineurium to form capillary anastomoses in the fascicles. However, in onethird of cases, a cause is not discovered and the polyneuropathy is considered idiopathic. A stimulus is given at different points along the nerve, in a distal to proximal fashion. When the response reaches the corresponding anterior horn cells, a second action potential is propagated in an orthodromic direction along the entire length of one or more of the same motor axons. The Fwaves, on the other hand, have different latencies and morphologies due to activation of different motor units with subsequent stimulations. Recordings are visualized on a computer screen and heard through a speaker system. Spontaneous activity: positive sharp waves with a few fibrillations in the first dorsal interosseous. Spontaneous activity Electric activity recorded from muscle at rest after inser tion activity has subsided. Positive sharp waves and fibrillations may also be observed in certain primary muscle disorders, presumed to be due to muscle membrane instability (730). Fasciculations are random and spontaneous twitch ing of a group of muscle fibers or a motor unit that is often grossly visible in a limb or the tongue. A fascicula tion potential is a recording often associated with clinical fasciculations. Complex repetitive discharges are activity that origi nates from a reverberating circuit that has developed within contiguous myofibers. These can occur in a variety of nerve disorders, but are most commonly associated with radiationinduced nerve injury. In neurogenic recruitment, with axon loss there is a reduced number of motor units available to recruit. The remaining motor units need to fire at a greater frequency in order to compensate for this loss. Thus, a single motor axon may be supplying many more muscle fibers than it had prior to the nerve insult. Laboratory tests Recommended screening blood tests for the evaluation of polyneuropathy include glucose, vitamin B12 with metabolites (methylmalonic acid with or without homocysteine), and serum protein immunofixation elec trophoresis. Nerve biopsy Nerve biopsy can be used as a diagnostic measure to fur ther delineate the specific form of neuropathy. The indications for nerve biopsy are mostly confined to evaluation for suspected vasculitic neuropathies, leukemic infiltration, or amyloid. Heredi tary neuropathies may be considered, however, and molecular genetic testing is available in most cases. Theories include a metabolic pro cess, microangiopathic ischemia, or an immunologic disorder.
Buy 300mg combivir fast delivery
Amyloid- (A) deposition seems to be the neuropathologic factor most strongly influenced by genetic factors medications requiring aims testing proven combivir 300 mg. Recent evidence suggests that soluble oligomers of A constitute the neurotoxic factor, rather than the A plaques deposited in the extracellular space. Impaired learning (encoding) of new verbal and visual information is evident on neuropsychologic assessment. This impairment in antegrade episodic memory is thought to correlate with the deposition of tangles in the transentorhinal region, which result in deafferentation of the hippocampal complex. There may, however, be focal cortical neurologic signs including aphasia, agraphia, dyscalculia, apraxia (ideomotor and dressing), agnosia for objects or faces, and neglect or sensory inattention. These may mark the onset of disease, but generally appear after presentation of memory impairment. Psychiatric features may include paranoia and other personality or behavioral changes. If hallucinations are present, they are typically persecutory or of deceased family members. On physical examination, primitive reflexes and other frontal release signs may be observed at any stage, but are more evident in later stages of disease. However, as the disease progresses muscular rigidity (paratonia) may be evident, in addition to reduced gait speed and stride. A physical finding, such as unilateral motor or sensory abnormalities or parkinsonian features, suggests another process. A score of 24 or less is generally considered abnormal, but this test should only be used as a screening assessment and not a diagnostic test4. A change in the role of the patient is also an important clue: if the patient normally deals with family finances, yet one of the family members has found the need to take over those finances, this represents a loss in functioning. Often patients will report a restriction in their driving radius, providing a clue that they are unsure of themselves with regard to driving. Recent developments in tracers have produced agents that can be used to assess amyloid plaque pathology in living patients. Genetic testing In the individual with cognitive impairment, genetic testing can be used to determine whether the disease is genetically transmissible. The aggregated neurofibrils are visualized as paired helical filaments on electron microscopy. Loss is widespread (hippocampus, entorhinal cortex, association areas of neocortex, and nucleus basalis of Meynert [the substantia innominata] and locus ceruleus) and predominantly a loss of cholinergic, noradrenergic, and dopaminergic neurons. The drug can also be administered in the morning and may be appropriate in patients with insomnia or vivid dreams. The drug should be used with caution in patients with supraventricular conduction abnormalities, peptic ulcers, and obstructive airway disease. The patient should be maintained on the highest dose tolerated, up to a maximum of 6 mg twice daily. To offset some of the gastrointestinal side-effects, this drug is now available in patch form. Galantamine is available in 4 mg and 8 mg, with a liquid preparation (4 mg/ml), which is useful for titration. The dose can be titrated from 4 mg twice daily to 8 mg twice daily over 4 weeks according to tolerance and benefit, but patients with hepatic impairment should be started with 4 mg daily. A long-acting form of galantamine is now also available that can be given once a day. A calming, supportive, and reassuring voice that is nonconfrontational works best. Acute behaviors on top of chronic behaviors may relate to an underlying medical condition and, as such, physical symptoms or iatrogenic factors should be sought out and corrected. Newer antipsychotic agents such as risperidone, olanzapine, and quetiapine, have very few anticholinergic or extrapyramidal side-effects, and appear to be at least as effective as conventional neuroleptics for those symptoms that might be treatable by neuroleptics. However, these drugs now carry a black box warning in that they have been associated with a higher risk of sudden death and/or stroke in elderly patients with dementia. First-line therapy is education of the caregivers in how to deal with difficult behaviors expressed by the patient. It is still not clear whether challenging the brain with puzzles such as crossword puzzles, Sudoku, word jumbles, word searches, or a variety of other brain exercises that are promoted commercially, are beneficial. However, as the disease progresses, the impairment becomes more generalized to involve all cognitive domains. It has been complicated by the recognition that several diseases once thought to be distinct entities. Most commonly, patients present with difficulty generating or recalling familiar words. Diagnosis Diagnosis is made on medical history, detailed neurologic examination, and neuropsychologic pattern of deficits consistent with one of the above syndromes. Macroscopic changes include atrophy, with decreased brain weight and frontotemporal atrophy that is most severe in the mesial and temporal area (531). Family members should be counseled on how to manage behavioral improprieties, impulsivity, and so on. Support groups for family members should be offered as a mechanism to learn behavioral management techniques. Early speech therapy and assistive devices may be useful in patients with predominant language difficulties. Benefit may not be significant and hallucinations and worsening behavior should be monitored. Since recognition, it has undergone several modifications and refinements in the clinical diagnostic criteria, guided by a consortium of investigators. Cognitive impairment is persistent and progressive, but characterized by pronounced fluctuation, varying between lucid intervals and episodic confusion. Overall, rest tremor is uncommon and axial features (postural instability, gait difficulty, facial immobility) are most common. Patients often recognize that these are hallucinations, rather than believing they are real. Progressive cognitive decline of sufficient magnitude to interfere with normal social or occupational function is the central required feature. Prominent or persistent memory impairment may not necessarily occur in the early stages but is usually evident with progression. Deficits on tests of attention, executive function, and visuospatial ability may be especially prominent. The symptoms of these disorders have significant overlap, and they are often hard to differentiate from one another clinically32. Alpha-synuclein immunocytochemistry is potentially the most sensitive and specific technique for detecting and quantifying Lewy bodies and Lewy neurites.
Cheap 300 mg combivir
They are in fact the most common subtype of the Schneiderian papillomas symptoms stomach flu order combivir with a mastercard, with the exophytic fungiform and cylindrical cell comprising the other types. Grossly, they appear as fleshy, gray-tan mucosal lesions that can be more vascular than a typical inflammatory nasal polyp. While the stroma may have a variable amount of inflammation, fibrosis, and edema, there is an absence of seromucous glands and the basement membrane is preserved. Karkos et al in 2009 found that T2-weighted images could be helpful in distinguishing tumor from inflammatory tissue. Note the area of bony hyperostosis on the lateral maxillary sinus wall (a possible area of tumor attachment). The authors experience that the combination of the two is invaluable for preoperative planning. Knowing what inspissated secretions versus solid mass is, it will often be the differentiator between a purely endoscopic procedure and the need for an adjunctive external incision. The T2-weighted images demonstrate tumor within the sphenoid sinus but with no invasion of the cavernous sinus or carotid artery. In addition to identifying the presence of a nasal mass or polyp, the endoscope may facilitate a biopsy of the suspected tissue under local anesthetic. This is especially important for patient consent and counseling, particularly if there is any evidence of dysplasia or malignancy. However, clinical biopsies should only be performed if the accessible tissue is not hypervascular and there is clearly no evidence of intracranial extension. If the patient is not amenable for a clinic biopsy, a frozen section may be performed at the beginning of the surgical case. For bilateral nasal polyps, we do not routinely conduct clinical biopsies unless the tissue is grossly abnormal on endoscopy. Note the bony dehiscence of the right lateral wall overlying the cavernous carotid artery. Tumors involving the ostiomeatal complex, ethmoid sinuses, and/or the medial portion of the maxillary sinus (with or without involvement of the nasal cavity). Tumors with any extranasal/extrasinus extension to involve adjacent structures such as the orbit, intracranial compartment, or the pterygomaxillary space. This will help identify the site of tumor attachment while minimizing blood loss and decreasing trauma to the surrounding normal tissues. However, once the site of origin or pedicle is identified, a submucoperiosteal en bloc dissection of the diseased mucosa and tumor should be undertaken. This enables pathologists to fully evaluate the site of origin as one contiguous piece, helping to maintain orientation if dysplasia or malignancy is found. Biopsies are taken of the surrounding mucosa to ensure that complete tumor clearance has been achieved. Finally, after elevating the diseased mucosa, it is important to address the underlying areas of bone. These are the potential sites of bony attachment or invasion, which can be irregular in nature. As such, we recommend using a diamond drill bit to burr down these areas to minimize the risk of recurrence. If these general principles cannot be accomplished endoscopically, the use of an adjunctive open or external approach should be considered. An external procedure is rarely needed for tumor within the maxillary sinus, but is of use for tumors involving the frontal sinus in which the site of attachment is out of reach or attached to dura of the anterior skull base. Finally, it is important to remember that if concurrent malignancy is discovered, standard oncologic surgical principles should be maintained such that negative tumor margins are achieved. The rest of the chapter outlines the specific details of endoscopic surgery for each of the involved sinuses. It attempts to describe the extent of tumor involvement both in the nasal cavity and in the paranasal sinuses. Endoscopic Surgery for Inverted Papilloma medial maxillectomy is accomplished by first removing the posterior two-third of the inferior turbinate, and then resecting the medial wall of the maxillary sinus down to the nasal cavity floor with either cutting instruments or a drill. The extent of medial maxillectomy and the need for nasolacrimal duct section again depends on the site of tumor attachment. While the medial wall may not be directly involved with tumor, the medial maxillectomy is often necessary for adequate access and instrumentation within the sinus. Given the angulation, a particularly challenging area for endoscopic surgery is the anterior wall of the maxillary sinus. To address this location, we routinely resect the medial maxillary wall anteriorly to the pyriform aperture. This can be done with a variety of instruments, including the backbiter and angled drills. Resection of the medial maxillary wall will require resection of the nasolacrimal duct. By resecting this area, we are ensuring complete tumor removal as well as improving our visualization and ability to instrument the anterior, anterolateral, and anteromedial maxillary walls. This is essentially a modified version of the endonasal Denker operation that has been previously described by Tomenzoli et al. Because a nasolacrimal duct section is performed concurrently, we routinely marsupialize the nasolacrimal sac at the end of the case to prevent postoperative epiphora. As an alternative, a transseptal approach through the contralateral nostril or a septal dislocation procedure has also been described to allow for greater instrumentation and access of the anterior and lateral maxillary sinus wall. As such, the historical approach to remove tumors in this location was a medial maxillectomy via a lateral rhinotomy approach. At this point in the surgery, it is often advantageous to switch to an angled 30- or 70-degree endoscope to fully visualize the site of tumor attachment. Again, the key aspect of surgical removal is to debulk the tumor until it is possible to visualize the site of attachment. Perhaps more importantly, the resulting sphenoid sinus opening will be large enough for long-term surveillance. Care must be taken to review the preoperative films closely and to examine for bony dehiscences over the carotid and optic nerve. Careful use of the bipolar cautery may be used to debulk the papilloma in the case of a dehiscent carotid or optic nerve. Historically, the osteoplastic flap was necessary to ensure complete tumor extirpation. From the most recent series by Lombardi et al, 6 out of 11 patients with frontal sinus involvement were managed exclusively by an endoscopic approach. An adjuvant osteoplastic flap was required in the remaining five patients because of extensive mucosal involvement either in a large frontal sinus or in a supraorbital ethmoid cell. With current instrumentation, the ability to fully remove diseased mucosa and drill down the underlying bone in these areas is severely restricted. However, if the tumor involves the frontal sinus proper, the treating surgeon must be prepared to convert to an osteoplastic flap if it is felt that a modified Lothrop procedure will not provide the necessary access for tumor control. One special situation that may arise is if there is a dehiscence of the posterior table of the frontal sinus. Recently, there have been several reviews, which have highlighted the superiority of the endoscopic approach. A "contemporary" cohort of studies from 1992 to 2004 was selected whereby the majority of cases was performed with an endoscopic approach. This was then compared with a "historical" cohort of studies whereby strictly external approaches were used. Endoscopic Surgery for Inverted Papilloma It was found that the contemporary cohort of 32 studies had a statistically significant lower recurrence rate of 15% versus 20% in the historical group of 13 studies (p < 0. Interestingly, when the contemporary cohort was examined, patients treated endoscopically also had a lower recurrence rate of 12% compared with 20% in patients that were treated nonendoscopically (p < 0. More importantly, many authors agree that the risk of recurrence appears to be related to the completeness of tumor removal during the primary surgery. While the risk of malignancy appears to be low, the challenge has always been to achieve a thorough resection to minimize the risk of recurrence. From the available literature, it appears that with the appropriate indications and techniques, endoscopic surgery should be the first line of treatment for the vast majority of tumors. However, surgeons must be prepared to perform advanced endonasal procedures including medial maxillectomy and extended frontal sinus dissections.