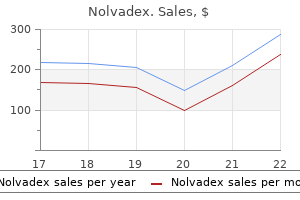
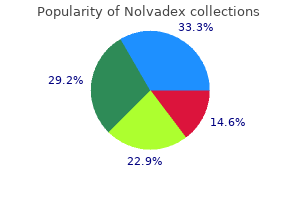
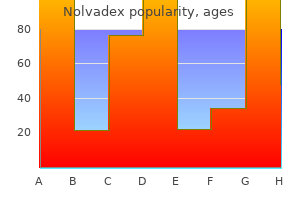
Purchase discount nolvadex on-line
During treatment with hydrocortisone with maximum doses appropriate for stress menstrual taboos generic 10mg nolvadex mastercard, fludrocortisone replacement is not required. Some patients cannot tolerate fludrocorti sone and must substitute NaCl tablets to replace renal sodium loss. Without waiting for the results, treat ment is initiated immediately with hydrocortisone phos phate or hydrocortisone sodium succinate 1 00-300 mg intravenously along with saline solution. Thereafter, hydrocortisone is continued as intravenous infusions of 50- 1 0 0 mg every 6 hours for the first day. The dosage may then be reduced according to the clinical picture and labo ratory test results. Since bacterial infection frequently precipitates acute adrenal crisis, broad-spectrum antibiotics should be administered empirically while waiting for the results of initial cultures. The patient must also be treated for electro lyte abnormalities, hypoglycemia, and dehydration, as indicated. When the patient is able to take food by mouth, hydro cortisone is administered orally in doses of 10-20 mg every 6 hours, and the dosage is reduced to maintenance levels as needed. Most patients ultimately require hydrocortisone twice daily (1 0-20 mg in am; 5 - 1 0 mg in pm). Mineralocor ticoid replacement is not needed when large amounts of hydrocortisone are being given, but as its dose is reduced it is usually necessary to add fludrocortisone acetate, 0. Some patients never require fludrocortisone or become edematous at doses of more than 0. Once the crisis has passed, the patient must be evaluated to assess the degree of permanent adrenal insufficiency and to establish the cause, if possible. However, one retrospective Swedish study of 1 675 patients with Addison disease found an unexpected increase in all cause mortality, mostly from cardiovascular disease, malig nancy, and infection. For example, patients with adreno leukodystrophy or Allgrove syndrome may suffer from neurologic disease. Patients with adrenal tuberculosis have a serious systemic infection that requires treatment. Adre nal crisis can occur in patients who stop their medication or who experience stress such as infection, trauma, or sur gery without appropriately higher doses of corticosteroids. Patients who take excessive doses of corticosteroid replace ment can develop Cushing syndrome, which imposes its own risks. However, some patients feel residual fatigue, despite glucocorticoid and mineralocorticoid replacement. Also, patients with Addison disease are deficient in epinephrine, but replacement epinephrine is not available. Fatigue may also be an indication of suboptimal dosing of medication, electrolyte imbalance, or concurrent hypothyroidism or diabetes mellitus. However, if adrenal crisis is unrecog nized and untreated, shock that is unresponsive to fluid replacement and vasopressors can result in death. Psychological morbidity and impaired quality of life in patients with stable treatment for primary adrenal insufficiency: cross-sectional study and review of the litera ture. Adrenal insufficiency in pregnancy: challenging issues in diagnosis and management. Prognosis the life expectancy of patients with Addison disease is reasonably normal, as long as they are compliant with their medications and knowledgeable about their condition. General Considerations the term Cushing "syndrome" refers to the manifestations of excessive corticosteroids, commonly due to supraphysi ologic doses of corticosteroid drugs and rarely due to spontaneous production of excessive corticosteroids by the adrenal cortex. Cushing disease is caused by a benign pituitary adenoma that is typically smaller than 5 mm and usually located in the anterior pitu itary (98%) or in the posterior pituitary (2%). Ectopic locations include the lungs (55%), pancreas (9%), mediastinum-thymus (8%), adrenal (6%), gastrointestinal tract (5%), thyroid (4%), and other sites (1 3%). Benign adrenal adenomas are generally small and produce mostly cortisol; adrenocortical carcinomas are usually large when discov ered and can produce excessive cortisol as well as andro gens but may be nonsecretory. Bilateral primary pigmented adrenal macronodular adrenocortical disease is a rare cause of Cushing syndrome in children and young adults. Bilateral primary pigmented adrenal macronodular adre nocortical disease may be an isolated condition or part of the Carney complex, an autosomal dominant condition with additional features consisting of myxomas of the heart and skin with spotty skin pigmentation and facial freckles. Muscle atrophy causes weakness, with dif ficulty standing up from a seated position or climbing stairs. Patients may also experience backache, headache, hypertension, osteoporosis, avascular necrosis of bone, acne, superficial skin infections, and oligomenorrhea or amenorrhea in women or erectile dysfunction in men. Patients may have thirst and polyuria (with or without glycosuria), renal calculi, glaucoma, purple striae (espe cially around the thighs, breasts, and abdomen), and easy bruisability. Mental symptoms may range from diminished ability to concentrate to increased lability of mood to frank psychosis. However, some adrenal carcinomas are smaller and the histopatho logic diagnosis can be difficult. Some adrenal carcinomas have microscopic metastases that can only be inferred from the presence of detectable cortisol levels following removal of the primary adrenal tumor. Laboratory Findings Glucose tolerance is impaired as a result of insulin resis tance. Polyuria is present as a result of increased free water clearance; diabetes mellitus with glycosuria may worsen it. Patients with Cushing syndrome often have leukocytosis with relative granulocytosis and lymphopenia. Tests for Hypercortisolism the biochemical evaluation for Cushing syndrome can be difficult, since test results are often misleading or conflict ing. The dexamethasone suppression test is the easiest screening test for Cushing syndrome. However, 8% of established p atients with pituitary Cushing disease have dexameth asone-suppressed cortisol levels less than 2 mcgldL (55 nmol! Therefore, when other clinical criteria suggest hypercortisolism, further evaluation is warranted even in the face of normal dexamethasone-suppressed serum cortisol. Antiseizure drugs (eg, phenytoin, phenobarbital, primidone) and rifampin accelerate the metabolism of dexamethasone, causing a lack of cortisol suppression by dexamethasone. Early in the course of the disease, patients frequently complain of fatigue or reduced endurance but may have few, if any, of the physical stigmata described below. An abnormally high 24-hour urine free cortisol (or free cortisol to creatinine ratio of greater than 95 meg cortisol! In preg nancy, urine free cortisol is increased, while 17 -hydroxy corticosteroids remain normal and diurnal variability of serum cortisol is normal. Late-night salivary cortisol assays are useful due to the inconvenience of obtaining a midnight blood specimen for serum cortisol. Late-night salivary cortisol levels that are consis tently greater than 250 ng/dL (7. The late-night salivary cortisol test has a relatively high sensitivity and specificity for Cushing syn drome, but false-positive and false-negative tests occur. L) are indicative of Cushing syndrome and distinguish it from other conditions associated with a high urine free cortisol (pseudo-Cushing states). Requirements for this test include being in the same time zone for at least 3 days, being without food for at least 3 hours, and having an indwelling intravenous line established in advance for the blood draw. Differential Diagnosis Alcoholic patients can have hypercortisolism and many clinical manifestations of Cushing syndrome. Depressed patients also have hypercortisolism that can be nearly impossible to distinguish biochemically from Cush ing syndrome but without clinical signs of Cushing syn drome. Cushing syndrome can be misdiagnosed as anorexia nervosa (and vice versa) owing to the muscle wasting and extraordinarily high urine free cortisol levels found in anorexia. Patients with severe obesity frequently have an abnormal dexamethasone suppression test, but the urine free cortisol is usually normal, as is diurnal variation of serum cortisol. Patients with familial cortisol resistance have hyperandrogenism, hypertension, and hypercorti solism without actual Cushing syndrome. Some adolescents develop violaceous striae on the abdomen, back, and breasts; these are known as "striae distensae" and are not indicative of Cushing syndrome. Patients with familial partial lipodystrophy type I develop central obesity and moon facies, along with thin extremi ties due to atrophy of subcutaneous fat. It must be collected properly in a plastic tube on ice and processed quickly by a laboratory with a reliable, sensitive assay. Although the overwhelming major ity of adrenal incidentalomas are benign adrenal adeno mas, the differential diagnosis includes adrenal carcinoma, pheochromocytoma, metastases, lymphoma, myelolipoma, infection, and cysts.
Purchase 20mg nolvadex visa
Treatment of small cell lung cancer: diagnosis and management of lung cancer womens health rights order generic nolvadex, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Symptoms and Signs Symptoms are uncommon but include cough, hemoptysis and, in advanced cases, dyspnea and hypoxemia. Relative contraindications to resection of pulmonary metastases include (1) malignant melanoma primary, (2) requirement for pneumonectomy, and (3) pleural involvement. Unfavorable prognostic fac tors also include shorter disease-free interval from primary tumor treatment to presentation of metastases and a larger number of metastases. Retrospective data from the International Registry of Lung Metastases report an overall 5 -year survival rate of 36% and 1 0-year survival rate of 26% after complete resection of pulmonary metastases. Patients who are not surgical can didates but have solitary or limited metastatic disease to the lungs may be candidates for stereotactic radiotherapy, radioablation, or cryotherapy. For patients with unresect able progressive disease, chemotherapy tailored to the pri mary tumor can be offered, and diligent attention to palliative care is essential (see Chapter 5). Survival after radiofrequency ablation i n 122 patients with inoperable colorectal lung metastases. Risk factors for survival after lung metastasec tomy in colorectal cancer patients: a systematic review and meta-analysis. Pulmonary metastasectomy: what is the prac tice and where is the evidence for effectiveness Appro priate studies should be ordered if there is a suspicion of any primary cancer, such as breast, thyroid, testis, colorectal, or prostate, for which specific treatment is available. Occasionally, cytologic studies of pleural fluid or pleural biopsy reveals the diagnosis. To determine a primary diagnosis, immunohistochemi cal staining should be done on the biopsy specimen. I maging Chest radiographs usually show multiple spherical densities with sharp margins. The size of metastatic lesions varies from a few millimeters (miliary densities) to large masses. The lesions are usually bilateral, pleural or subpleural in location, and more common in lower lung zones. Lymphangitic spread and solitary pulmo nary nodule are less common radiographic presentations of pulmonary metastasis. Mammography should be consid ered in women to search for possible primary breast cancer. Treatment Once the diagnosis has been established, management consists of treatment of the primary neoplasm and any pulmonary complications. Surgical resection of a solitary pulmonary nodule is often prudent in the patient with known current or previous extrapulmonary cancer. Local resection of one or more pulmonary metastases is feasible in a few carefully selected patients with various sarcomas and carcinomas (such as testis, colorectal, and kidney). About three-fourths of pleural mesothelio mas are diffuse (usually malignant) tumors, and the remaining one-fourth are localized (usually benign). Numerous studies have confirmed the association of malignant pleural mesothe lioma with exposure to asbestos (particularly the amphi bole form). The lifetime risk to asbestos workers of developing malignant pleural mesothelioma is as high as 10%. The latent period between exposure and onset of symptoms ranges from 20 to 40 years. The clinician should inquire about asbestos exposure through mining, milling, manufacturing, shipyard work, insulation, brake linings, building construction and demolition, roofing materials, and other asbestos products (pipes, textiles, paints, tiles, gaskets, panels). Although cigarette smoking significantly increases the risk of bronchogenic carcinoma in asbestos workers and aggravates asbestosis, there is no association between smoking and mesothelioma. Treatment Chemotherapy is the mainstay of treatment, with surgery only included in multimodality treatment if there is local ized disease that can be surgically resected and no evidence of mediastinal nodal involvement. For localized disease, surgi cal options include pleurectomy and decortication (surgical stripping of the pleura and pericardium from apex of the lung to diaphragm) or extrapleural pneumonectomy (a radical surgical procedure involving removal of the ipsilat era! Limited nonrandomized data have shown that a trimodality approach for localized dis ease with extrapleural pneumonectomy, adjuvant radiation, and (neoadjuvant or adjuvant) chemotherapy can prolong survival in highly selected patients. This small randomized study, comparing extrapleural pneumonectomy with no extrapleural pneu monectomy after induction chemotherapy in 50 patients, showed that extrapleural pneumonectomy offers no sur vival benefit and may cause more harm. In advanced dis ease, palliative chemotherapy with cisplatin and pemetrexed can achieve response rates of 30-40%, extend median overall survival to 12 months, and improve quality of life. Other alternative chemotherapy regimens include gem citabine, anthracyclines, or vinorelbine. Drainage of pleural effusions, pleurodesis, radiation therapy, and even surgical resection may offer palliative benefit in some patients. Sym ptoms and Signs the average interval between onset of symptoms and diag nosis is 2-3 months; the median age at diagnosis is 72-74 years in Western countries. Symptoms include the insidi ous onset of shortness of breath, nonpleuritic chest pain, and weight loss. Physical findings include dullness to per cussion, diminished breath sounds and, in some cases, digital clubbing. The histologic variants of malignant pleural mesothelioma are epithelial (50-60%), sarcomatoid (1 0%), and biphasic (30-40%). Since distinction from benign inflammatory conditions and metastatic adenocar cinoma may be difficult, immunohistochemical stains are important to confirm the diagnosis. I maging Radiographic abnormalities consist of nodular, irregular, unilateral pleural thickening and varying degrees of unilat era! Sixty percent of patients have right sided disease, while only 5% have bilateral involvement. Prog nosis Most patients die of respiratory failure and complications of local extension. Tumors that are predominantly sarcomatoid are more resis tant to therapy and have a worse prognosis, with median survivals less than 1 year. Poor prognostic features include poor performance status, non-epithelioid histology, male gender, nodal involvement, elevated lactate dehydrogenase, high white blood cell count, low hemoglobin, and high platelet count. Complications Malignant pleural mesothelioma progresses rapidly as the tumor spreads along the pleural surface to involve the peri cardium, mediastinum, and contralateral pleura. The tumor may eventually extend beyond the thorax to involve abdominal lymph nodes and organs. Evidence for an association with long term use of oral contraceptives is inconclusive. While sulfo nylurea and insulin use may increase the risk ofhepatocellular carcinoma, consumption of coffee, vegetables, white meat, fish, and n-3 polyunsaturated fatty acids; aspirin use; and statin and metformin use in diabetic patients appear to be protective. The fibrolamellar variant of hepatocellular carci noma generally occurs in young women and is character ized by a distinctive histologic picture, absence of risk factors, unique genomic profiles, and indolent course. Hepatoblastoma, the most common malignant liver tumor in infants and young children, occurs rarely in adults. Symptoms and Signs the presence of a hepatocellular carcinoma may be unsus pected until there is deterioration in the condition of a cir rhotic patient who was formerly stable. The sudden appearance of ascites, which may be bloody, suggests portal or hepatic vein thrombosis by tumor or bleeding from a necrotic tumor. Physical examination may show tender enlargement of the liver, occasionally with a palpable mass. In Africa, the typical presentation in young patients is a rapidly expand ing abdominal mass. Auscultation may reveal a bruit over the tumor or a friction rub when the tumor has extended to the surface of the liver. Laboratory Findings Laboratory tests may reveal leukocytosis, as opposed to the leukopenia that is frequently encountered in cirrhotic patients. Anemia is common, but a normal or elevated hematocrit value may be found in up to one-third of patients owing to elaboration of erythropoietin by the tumor. Sudden and sustained elevation of the serum alka line phosphatase in a patient who was formerly stable is a common finding. Alpha-fetoprotein levels are elevated in up to 70% of patients with hepatocellular carci noma in Western countries (although the sensitivity is lower in blacks and levels are not elevated in patients with fibrolamellar hepatocellular carcinoma); however, mild elevations (1 0-200 ng/mL [1 0-200 mcg/L]) are also often seen in patients with chronic hepatitis. Serum levels of des gamma-carboxy prothrombin are elevated in up to 90% of patients with hepatocellular carcinoma, but they may also be elevated in patients with vitamin K deficiency, chronic hepatitis, and metastatic cancer.
Purchase nolvadex 10mg online
Ampullary carci noma may present with jaundice due to bile duct obstruc tion or bleeding menstruation gas bloating order nolvadex pills in toronto. Imatinib induces disease control in up to 85% of patients with metastatic disease with a progres sion-free survival of 20-24 months and median overall sur vival of almost 5 years. Emerging agents for the treatment of advanced, imatinib-resistant gastrointestinal stromal tumors: current status and future directions. Risk factors for gastrointestinal stromal tumor recurrence in patients treated with adjuvant imatinib. The standard diagnosis, treatment, and follow up of gastrointestinal stromal tumors based on guidelines. Gastrointestinal stromal tumors: management of metastatic disease and emerging therapies. Small I ntesti nal Lymphomas Lymphomas may arise primarily in the gastrointestinal tract or involve it secondarily in patients with disseminated disease. In Western countries, primary gastrointestinal lymphomas account for 5% of lymphomas and 20% of small bowel malignancies. Enteropathy-associated T cell lymphomas appear to be increasing in incidence in the United States. In the Middle East, lymphomas may arise in the setting of immunoproliferative small intestinal disease. Other types of intestinal lymphomas include primary intestinal follicular cell lymphoma, mantle cell lymphoma, and Burkitt lymphoma (see Chapter 1 3). Protein-losing enteropathy may result in hypoalbuminemia, but other signs of malabsorp tion are unusual. Treatment depends on the tumor histologic subtype and stage of disease (see Chapter 1 3). Surgical resection of primary intestinal lymphoma, if feasible, may be appropri ate for localized tumors. Patients with more extensive disease generally are treated according to the tumor histology. S mall I ntestinal Adenoca rci nomas these are aggressive tumors that occur most commonly in the duodenum or proximal jejunum. The incidence is rare, with approximately 6000 new diagnoses per year in the United States. General Considerations Gastrointestinal carcinoid tumors are generally slow grow ing neuroendocrine tumors that account for approximately one-third of tumors arising in the small bowel. Gastroin testinal carcinoid tumors most commonly occur in the small intestine (45%) but are also found in the rectum (20%), appendix (1 7%), and colon (l l %), with the remain der occurring in the stomach (less than 10%; see Gastric Carcinoid Tumors above). Carcinoid tumors may contain a variety of hormones, including serotonin, somatostatin, gastrin, and substance P, each of which may or may not be secreted. Small intestinal carcinoids most commonly arise in the distal ileum within 60 em of the ileocecal valve. Although many carcinoids behave in an indolent fashion, the overall 5 -year survival rates for patients with locoregional and metastatic small bowel car cinoids are approximately 65% and 35%, respectively. The risk of metastatic spread increases when the tumor is 1 em or larger and when it is larger than 2 em with invasion beyond muscularis propria. However, in patients with appendiceal carcinoid tumors larger than 2 em, approximately 90% develop nodal and distant metas tases; right hemicolectomy is recommended in these cases. Rectal carcinoids are usually detected incidentally as submucosal nodules during proctoscopic examination and often locally excised by biopsy or snare polypectomy before the histologic diagnosis is known. Endorectal ultrasound is usually recommended to assess the size, presence and depth of invasion, and presence of lymph node metastases. Rectal carcinoids smaller than 1 em virtually never metas tasize and are treated effectively with local endoscopic or transanal excision. Hence, a more extensive cancer resection operation is warranted in fit patients with rectal carcinoid tumors larger than 1-2 em or with high risk features (such as invasion of muscularis propria or evidence of nodal involvement), or both. The manifestations include facial flush ing, edema of the head and neck (especially with bronchial carcinoid), abdominal cramps and diarrhea, broncho spasm, cardiac lesions (pulmonary or tricuspid stenosis or regurgitation in 1 0-30%), and telangiectases. Laboratory Findings Serum chromogranin A (CgA) is elevated in the majority of neuroendocrine tumors, although its sensitivity for small, localized carcinoid tumors is unknown. Somatostatin receptor scintigraphy, which is positive in up to 90% of patients with metastatic carcinoid, is routinely used in staging. Treatment & Outcomes Small intestinal carcinoids generally are indolent tumors with slow spread. Patients with disease confined to the small intestine should be treated with surgical excision. Even patients with meta static disease may have an indolent course with a 5 -year survival of 43%. Conventional cytotoxic chemotherapy agents do not achieve significant responses in carcinoid tumors and have not been associated with improved outcomes. Radiolabeled somatostatin analogs are used in Europe but are currently under investigation in the United States as another treatment modality for patients with somatostatin receptor positive advanced carcinoid tumors. Sym ptoms and Signs Most lesions smaller than 1-2 em are asymptomatic and difficult to detect by endoscopy or imaging studies. Through local extension or metastasis to mesenteric lymph nodes, carcinoids engender a fibroblastic reaction with contraction and kinking of the bowel or encasement of mesenteric vessels. Small intestinal carcinoids may present with abdominal pain, bowel obstruction, bleeding, or bowel infarction. Appendiceal and rectal carcinoids usu ally are small and asymptomatic but large lesions can cause bleeding, obstruction, or altered bowel habits. More than 90% of patients with carcinoid syndrome have hepatic metastases, usually from carcinoids of small bowel origin. About 10% of patients with carcinoid syndrome have primary bronchial or ovarian tumors without hepatic metastases. In patients with carcinoid syndrome, the somatostatin analog octreotide, 1 50-250 meg subcutaneously three times daily or administered as a long-acting intramuscular depot formulation administered monthly, inhibits hor mone secretion from the carcinoid tumor. This results in dramatic relief of symptoms of carcinoid syndrome, includ ing diarrhea or flushing, in 90% of patients for a median period of 1 year. In selected patients with refractory carcinoid syndrome, resection of hepatic metastases may provide dramatic improvement. Hepatic artery occlusion, liver directed debulking procedures, and chemotherapy also may provide symptomatic improvement in some patients with hepatic metastases. Widespread involvement may be best treated by systemic chemotherapy using single-agent therapy or combinations of pegylated-doxorubicin (Doxil), paclitaxel, vincristine, bleomycin, or etoposide. Efficacy of adjuvant chemotherapy for small bowel adenocarcinoma: a propensity score-matched analysis. Endoscopically identified well-differentiated rectal carcinoid tumors: impact of tumor size on the natural history and outcomes. Epidemiology and classification of gastroen teropancreatic neuroendocrine neoplasms using current cod ing criteria. A selective approach to the surgical management of periampullary cancer patients and its outcome. Update on the role of somatostatin analogs for the treatment of patients with gastroenteropancreatic neuroendocrine tumors. Small bowel stromal tumors: different clinico pathologic and computed tomography features in various anatomic sites. Advanced small bowel adenocarcinoma: molecu lar characteristics and therapeutic perspectives. General Considerations Colorectal cancer is the second leading cause of death due to malignancy in the United States. Colorectal cancer will develop in approximately 6% of Americans and 40% of those will die of the disease. In 2014, there were an esti mated 96,830 new cases of colon cancer and 40,000 new cases of rectal cancer in the United States, with combined estimated 50,3 1 0 deaths. During this same period, the percent of patients 50 years or older who were screened for colorectal cancer has increased to 66. Colorectal cancers are almost all adenocarcinomas, which tend to form bulky exophytic masses or annular constricting lesions. Polyps that are "advanced" (ie, polyps at least 1 em in size, adeno mas with villous features or high-grade dysplasia, or ser rated polyps with dysplasia) are associated with a greater risk of cancer. Activation of oncogenes such as K-ras and B-raf is present in a subset of colorectal cancers with prognostic and therapeutic implications discussed further below.
Generic 10 mg nolvadex overnight delivery
Gastrointestinal symptoms include anorexia women's health weight loss pills cheap 20 mg nolvadex with amex, nausea, heartburn, vomiting, abdominal pain, weight loss, constipation, and obstipation. Cal cium may precipitate in the corneas ("band keratopathy"), in extravascular tissues (calcinosis) and in small arteries, causing small vessel thrombosis and skin necrosis (calciphylaxis). Normocalcemic primary hyperparathyroid ism Patients with normocalcemic primary hyperparathyroid ism generally have few symptoms. However, on average, such patients have higher blood pressures (systolic blood pressure 1 0 mm Hg higher and diastolic blood pressure 7 mm Hg higher) than controls. Also, affected patients can have very subtle symptoms, such as mild fatigue, that may not be appreciated as abnormal. Hyperpa rathyroidism during preg nancy-Pregnant women having mild hyperparathyroidism with a serum calcium below 1 1. How ever, the majority ofwomen with more severe hypercalcemia during pregnancy experience complications such as neph rolithiasis, hyperemesis, pancreatitis, muscle weakness, and cognitive changes. About 80% of fetuses experience complications of maternal hyperparathyroidism, including fetal demise, preterm delivery, and low birth weight. Parathyroid carcinoma is a rare cause of hyperparathy roidism, accounting for less than 1 % of hyperparathyroid ism. About 90% of parathyroid carcinomas are functional and present with serum calcium levels greater than or equal to 14. However, some cases present with smaller tumors, less severe hypercalcemia, and benign appearing histologic features. Distant metastases arise most commonly in the lungs but also in bones, liver, brain, and mediastinum. Although parathyroid carcinoma is typically indolent, an increasing tumor burden is associated with critically severe hypercalcemia and death. Secondary and tertiary hyperparathyroidism usually occurs in patients with chronic kidney disease, in which hyperphosphatemia and decreased renal production of 1,25-dihydroxycholecalciferol (1,25 [0H]p 3) initially pro duce a decrease in ionized calcium. The parathyroid glands are stimulated (secondary hyperparathyroidism) and may enlarge, becoming autonomous (tertiary hyperparathy roidism). Secondary hyperparathyroidism predictably develops in patients with a deficiency in vitamin D. Serum calcium levels are typically in the normal range, but may rise to become borderline elevated with time, with tertiary hyperparathyroidism due to parathyroid glandular hyperplasia. Sym ptoms and Signs In the developed world, hypercalcemia is typically discov ered incidentally by routine chemistry panels. Many patients are asymptomatic or have mild symptoms that may be elicited only upon questioning. Parathyroid adeno mas are usually so small and deeply located in the neck that they are almost never palpable; when a mass is palpated, it usually turns out to be an incidental thyroid nodule. Skeletal manifestations-Hyperparathyroidism causes a loss of cortical bone and a gain of trabecular bone. Parathyroid carcinoma-Parathyroid carcinoma must always be suspected in patients with a serum calcium greater than or equal to 14. Laboratory Findings the hallmark of primary hyperparathyroidism is hypercal cemia, with the serum adjusted total calcium greater than 10. The urine calcium excretion may be high or normal (averaging 250 mg/g creatinine) but it is usually low for the degree of hypercalcemia. There is an excessive loss of phosphate in the urine in the presence of hypophosphate mia (25% of cases), whereas the serum phosphate may be high in kidney disease, which causes secondary hyperpara thyroidism. Vitamin D deficiency is common in patients with hyperparathyroidism, and it is prudent to screen for vitamin D deficiency with a serum 25-0H vita min D determination. Serum 25-0H vitamin D levels below 20 mcg/L (50 nmol/L) can aggravate hyperparathy roidism and its bone manifestations; vitamin D replace ment may be helpful in treating such patients with hyperparathyroidism. Patients with apparent hyperparathyroidism should be screened for familial benign hypocalciuric hypercalcemia with a 24-hour urine for calcium and creatinine. Such individuals require monitoring, since hypercalcemia develops in about 19% of patients over 3 years of follow-up. Imaging Parathyroid imaging is not necessary for the diagnosis of hyperparathyroidism, which depends on serum parathy roid and calcium levels. Imaging is performed for most patients prior to parathyroid surgery and is particularly important for patients who have had prior neck surgery. The visualization of an apparent parathyroid adenoma helps secure the diagnosis when there is occasional diag nostic difficulty and often allows for minimally invasive surgery. Ultra sound has a sensitivity of 79% for single adenomas but only 35% for multiglandular disease. However, false-positive scans are common, caused by thyroid nod ules, thyroiditis, or cervical lymphadenopathy. It can also be helpful for patients who have had prior neck surgery and for those with ectopic glands. For patients with apparently asymptomatic hyperparathyroid ism, the presence or absence of calcium nephrolithiasis can be a deciding factor about whether to have parathyroidec tomy surgery. B one radiographs are usually normal and are not required to make the diagnosis of hyperparathyroidism. There may be demineralization, subperiosteal resorption of bone (especially in the radial aspects of the fingers), or loss of the lamina dura of the teeth. There may be cysts throughout the skeleton, mottling of the skull ("salt-and pepper appearance"), or pathologic fractures. Patients with renal osteodystrophy may have ectopic calcifications around joints or in soft tissue. Such patients may exhibit radiographic changes of osteopenia, osteitis fibrosa cystica, or osteosclerosis, alone or in combination. Complications Pathologic long bone fractures are more common in patients with hyperparathyroidism than in the general population. Urinary tract infection due to stone and obstruction may lead to kidney disease and uremia. If the serum calcium level rises rapidly, clouding of sensorium, kidney disease, and rapid precipitation of calcium through out the soft tissues may occur. Pseudogout may complicate hyperparathyroidism both before and after surgical removal of tumors. In tertiary hyperparathyroidism due to chronic kidney disease, high serum calcium and phosphate levels may cause disseminated calcification in the skin, soft tissues, and arteries (calciphylaxis); this can result in painful isch ernie necrosis of skin and gangrene, cardiac arrhythmias, and respiratory failure. The actual serum levels of calcium and phosphate have not correlated well with calciphylaxis, but a calcium (mg/dL) x phosphate (mg/dL) product over 70 is usually present. Differential Diagnosis Artifactual hypercalcemia is common, so a report of hypercalcemia should always prompt a confirmatory serum calcium level that is drawn after an overnight fast along with a serum protein, albumin, and triglyceride while ensuring that the patient is well-hydrated. Hypercal cemia may be due to high serum protein concentrations; in the presence of very high or low serum albumin concentra tions, an adjusted serum calcium or a serum ionized cal cium is more dependable than the total serum calcium concentration. Spurious elevations in serum calcium have also been reported with severe hypertriglyceridemia, when the calcium assay uses spectrophotometry. Hypercalcemia of malignancy occurs most frequently with breast, lung, pancreatic, uterine, and renal cell carci noma, and paraganglioma. Many other hematologic cancers, such as mono cytic leukemia, T cell leukemia and lymphoma, and Burkitt lymphoma, have also been associated with hypercalcemia. Sarcoidosis and other granulomatous disorders, such as tuberculosis, berylliosis, histoplasmosis, coccidioidomy cosis, leprosy, and foreign-body granuloma, can cause hypercalcemia. Excessive calcium or vitamin D ingestion can cause hypercalcemia, especially in patients who concurrently take thiazide diuretics, which reduce urinary calcium loss. Hypercalcemia is reversible following withdrawal of cal cium and vitamin D supplements. If hypercalcemia per sists, the possibility of associated hyperparathyroidism should be considered. Serum levels of 25-hydroxycholecalciferol (25 [0H] D 3) are helpful to con firm the diagnosis. A brief course of corticosteroid therapy may be necessary if hypercalcemia is severe. Familial benign hypocalciuric hypercalcemia can be easily mistaken for mild hyperparathyroidism. It is a com mon autosomal dominant inherited disorder (prevalence: 1 in 1 6,000) caused by a loss-of-function mutation in the gene encoding the calcium sensing receptor.
Buy cheap nolvadex 20mg online
Most meniscus injuries occur with acute injuries (usually in younger patients) or repeated microtrauma pregnancy photography generic nolvadex 20 mg on line, such as squatting or twisting (usually in older patients). Symptoms and Signs the patient may have an antalgic (painful) gait and diffi culty with squatting. Meniscus tears rarely lead to the immediate swelling that is commonly seen with fractures and ligament tears. However, it is often unclear whether the pain is coming from the meniscus tear or the arthritis. Provocative tests, including the McMurray test, the modified McMurray test, and the Thessaly test, can be performed to confirm the diagnosis (Table 4 1 -9). Most symptomatic meniscus tears cause pain with deep squat ting and when waddling (performing a "duck walk"). High signal through the meniscus (bright on T2 images) represents a meniscal tear. Arthroscopic partial meniscectomy ver sus sham surgery for a degenerative meniscal tear. The pain affects any or all of the anterior knee structures, including the medial and lateral aspects of the patella as well as the quadriceps and patellar tendon insertions. The patella engages the femoral trochlear groove with approximately 30 degrees of knee flexion. Forces on the patellofemoral j oint increase up to three times body weight as the knee flexes to 90 degrees (eg, climbing stairs), and five times body weight when going into full knee flexion (eg, squatting). Abnormal patellar tracking during flexion can lead to abnormal articular cartilage wear and pain. When the patient has ligamentous hyperlaxity, the patella can sublux out of the groove, usually laterally. Patellofemoral pain is also associ ated with muscle strength and flexibility imbalances as well as altered hip and ankle biomechanics. Treatment Conservative treatment can be used for degenerative tears in older patients. A randomized con trolled trial showed that physical therapy compared to arthrosopic partial meniscectomy had similar outcomes at 6 months. However, 30% of the patients who were assigned to physical therapy alone underwent surgery within 6 months. Another randomized study has shown that arthroscopic surgery has no benefit over sham operation for patients who have meniscus tears in osteoarthritic knees. A 20 1 3 randomized controlled study has further demonstrated no benefit for arthroscopic meniscectomy with sham operation for patients with degenerative menis cal tears. Acute tears in young and active patients with signs of internal derangement and without signs of arthritis on imaging can be best treated arthroscopically with meniscus repair or debridement. Symptoms and Signs Patients usually complain of pain in the anterior knee with bending movements and less commonly in full extension. Pain from this condition is localized under the kneecap but can sometimes be referred to the posterior knee or over the medial or lateral inferior patella. Symptoms may begin after a trauma or after repetitive physical activity, such as running and jumping. On physical examination, it is important to pal pate the articular surfaces of the patella. For example, the clinician can use one hand to move the patella laterally, and use the fingertips of the other hand to palpate the lateral undersurface of patella. Patellar mobility can be assessed by medially and laterally deviating the patella (deviation by one-quarter of the diameter of the kneecap is consider normal; greater than one-half the diameter suggests exces sive mobility). The apprehension sign suggests instability of the patellofemoral joint and is positive when the patient becomes apprehensive when the patella is deviated laterally. When to Refer If the patient has symptoms of internal derangement suspected as meniscus injury. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. The patellar grind test is performed by grasping the knee superior to the patella and pushing it downward with the patient supine and the knee extended, pushing the patella inferiorly. The patient is asked to con tract the quadriceps muscle to oppose this downward translation, with reproduction of pain or grinding being the positive sign for chondromalacia of the patella. There are two common presentations: (1) Patients whose liga ments and patella are too loose (hypermobility); (2) and patients who have soft tissues that are too tight leading to excessive pressure on the j oint. Evaluation of the quadriceps strength and hip stabiliz ers can be accomplished by having the patient perform a one-leg squat without support. Patients who are weak may display poor balance, with dropping of the pelvis (similar to a positive hip Trendelenburg sign) or excessive internal rotation of the knee medially. Normally, with a one-leg squat, the knee should align over the second metatarsal ray of the foot. Radiographs may show lateral deviation or tilting of the patella in relation to the femoral groove. When to Refer Patients with persistent symptoms despite a course of con servative therapy. Posterolateral hip muscle strengthening versus quadriceps strengthening for patellofemoral pain: a comparative control trial. Conservative For symptomatic relief, use of local modalities such as ice and anti-inflammatory medications can be beneficial. If the patient has signs of patellar hypermobility, physical therapy exercises are useful to strengthen the quadriceps (especially the vastus medialis obliquus muscle) to help stabilize the patella and improve tracking. There is consistent evidence that exercise therapy for patellofemoral pain syndrome may result in clinically important reduction in pain and improvement in functional ability. Lower quality research supports that hip and knee exercises are better than knee exercises alone. Strengthening the quadriceps and the pos terolateral hip muscles such as the hip abductors that control rotation at the knee should be recommended. Support for the patellofemoral joint can be provided by use of a patellar stabilizer brace or special taping techniques (McConnell tap ing). Correcting lower extremity alignment (with appropri ate footwear or over-the-counter orthotics) can help improve symptoms, especially if the patient has pronation or high arched feet. If the patient demonstrates tight peripatellar soft tissues, special focus should be put on stretching the ham strings, iliotibial band, quadriceps, calves and hip flexors. Surgical Surgery is rarely needed and is considered a last resort for patellofemoral pain. Mechanical symp toms-such as swelling, grinding, catching, and locking suggest internal derangement, which is indicated by damaged cartilage or bone fragments that affect the smooth range of motion expected at an articular joint. Symptoms include pain with bending or twisting activities, and going up and down stairs. Knee joint corticosteroid inj ections are options to help reduce pain and inflammation and can provide short- term pain relief, usually lasting about 6 - 1 2 weeks. Viscosupple mentation by injections of hyaluronic acid-based products is controversial. Platelet-rich plasma injections contain high concentration of platelet -derived growth factors, which regulate some biologic processes in tissue repair. How ever, 9 of the 10 studies had a high risk of bias, and the underlying mechanism of biologic healing is unknown. Joint replacement surgeries are effective and cost-effective for patients with significant symptoms or functional limitations, provid ing improvements in pain, function, and quality of life. Minimally invasive surgeries and computer-assisted navigation during opera tion are being investigated as methods to improve tech niques (eg, accurate placement of the hardware implant) and to reduce complication rates; however, maj or improve ments have yet to be demonstrated. The most commonly recommended radiographs include bilateral weight-bearing 45-degree bent knee posteroante rior, lateral, and patellofemoral j oint views (Merchant view). Radiographic findings include diminished width of the articular cartilage causing j oint space narrowing, sub chondral sclerosis, presence of osteophytes, and cystic changes in the subchondral bone. There fore, a cure for the diseased joint is not possible, although symptoms or structural issues can be addressed to try to maintain activity level.
Angelica officinalis (Angelica). Nolvadex.
- Dosing considerations for Angelica.
- Premature ejaculation, when applied directly to the skin of the penis in combination with other medicines.
- How does Angelica work?
- Upset stomach (dyspepsia), when a combination of angelica and five other herbs is used (Iberogast, Medical Futures, Inc).
- Intestinal cramps and gas, nerve pain, arthritis-like pain, fluid retention, menstrual disorders, promoting sweating, and increasing urine production (diuretic).
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96304
Discount nolvadex 20mg overnight delivery
After rechecking blood lipids breast cancer nail decals proven 20mg nolvadex, the dose is increased and divided over three meals until the goal of3-4. It is not known whether routine monitoring of liver enzymes results in early detection and thus reduced severity of hepatocel lular hepatitis with jaundice. Although niacin may increase blood sugar in some patients, clinical trials have shown that niacin can be safely used in diabetic patients. Bile Acid-Binding Resins the bile acid-binding resins include cholestyramine, cole sevelam, and colestipol. Treatment with these agents reduces the incidence of coronary events in middle-aged men by about 20%, with no significant effect on total mor tality. The resultant reduction in the enterohepatic circulation causes the liver to increase its production of bile acids, using hepatic cholesterol to do so. The triglyceride level tends to increase slightly in some patients treated with bile acid-binding resins; they should be used with caution in those with elevated triglyc erides and probably not at all in patients who have triglyc eride levels above 500 mg/dL. The usual dose of cholestyramine is 1 2-36 g of resin per day in divided doses with meals, mixed in water or, more palatably, juice. They may interfere with the absorption of fat-soluble vitamins (thereby complicating the management of patients receiving warfarin) and may bind other drugs in the intestine. Other serious, but extremely uncommon, side effects include liver failure and muscle disease including myositis and rhabdomyolysis. Some patients experience muscle pain even when the serum creatine kinase levels are nor mal. Manufacturers of statins recom mend monitoring liver enzymes before initiating therapy and as clinically indicated thereafter. Muscle disease is more common with statins and fibrates and niacin as well as with erythromycin, antifungal medications, nefazadone, and cyclosporine. This dose should only be used in those who have been taking the medication for longer than 1 year without muscle toxicity. N iacin (Nicoti nic Acid) Niacin was the first lipid-lowering agent that was associ ated with a reduction in total mortality. Long-term follow up of a secondary prevention trial of middle-aged men with previous myocardial infarction disclosed that about half of those who had been previously treated with niacin had died, compared with nearly 60% of the placebo group. This favorable effect on mortality was not seen during the trial itself, though there was a reduction in the incidence of recurrent coronary events. A meta-analysis of 10 random ized trials using niacin has also shown a 27% reduction in cardiovascular events. The fibric acid derivatives or fibrates approved for use in the United States are gemfibrozil and fenofibrate. The incidence of the latter two conditions may be higher among patients also taking other lipid-lowering agents. In the largest clinical trial that used clofibrate, there were significantly more deaths-especially due to cancer in the treatment group; it should not be used. Ezetimibe Ezetimibe is a lipid-lowering drug that inhibits the intesti nal absorption of dietary and biliary cholesterol by block ing p assage across the intestinal wall by inhibiting a cholesterol transporter. However, beneficial effects of ezeti mibe monotherapy on cardiovascular outcomes has not been demonstrated. One study has shown that adding ezetimibe to a statin resulted in a small incremental benefit on cardiovascular outcomes. At the end of 7 years of study, patients taking ezetimibe-simvastatin had a 2% absolute reduction in car diovascular events compared to patients taking simvastatin alone. Studies designed to demonstrate a reduction in cardiovascular events have not been pub lished, but analysis of existing studies does suggest a sub stantial reduction in death from cardiovascular disease and myocardial infarction. However, cost effectiveness models suggest that these medications, at current prices, are not cost -effective. Although other medications will also have beneficial effects on lipids, there is little evidence demonstrating the desired effects on cardiovascular disease and all-cause mortality. The use of extended-release niacin with laropip rant (a prostaglandin antagonist) in high-risk patients tak ing a statin also did not reduce the risk of cardiovascular events. An increase in adverse events was also seen when niacin plus laropiprant was added to statins. Safety and efficacy of statin treatment alone and in combination with fibrates in patients with dyslipidemia: a meta-analysis. Effect of ezetimibe on major atherosclerotic disease events and all-cause mortality. Comparative tolerability and harms of individual statins: a study level network meta-analysis of 246,955 partici pants from 1 3 5 randomized, controlled trials. The patho physiology is not certain, since pancreatitis never develops in some patients with very high triglyceride levels. Most patients with congenital abnormalities in triglyceride metabolism present in childhood; hypertriglyceridemia induced pancreatitis first presenting in adults is more com monly due to an acquired problem in lipid metabolism. Although there are no clear triglyceride levels that pre dict pancreatitis, most clinicians treat fasting levels above 500 mg/dL (5 mmol/L). The risk of pancreatitis may be more related to the triglyceride level following consump tion of a fatty meal. Because postprandial increases in tri glyceride are inevitable if fat-containing foods are eaten, fasting triglyceride levels in persons prone to pancreatitis should be kept well below that level. In patients with fasting triglycerides greater than or equal to 500 mg/dL (5 mmol! Evaluation and treatment of hypertriglyceride mia: an Endocrine Society clinical practice guideline. For example, dimin ished energy intake may result from poor dentition or various gastrointestinal disorders. Clin ical Findings Clinical manifestations of protein-energy malnutrition range from mild growth retardation and weight loss to a number of distinct clinical syndromes. Progressive wasting that begins with weight loss and proceeds to more severe cachexia typically develops in most patients with marasmus-like secondary protein-energy malnutrition. In the most severe form of this disorder, most body fat stores disappear and muscle mass decreases, most noticeably in the temporalis and interosseous muscles. Laboratory studies may be unremarkable-serum albumin, for example, may be normal or slightly decreased, rarely decreasing to less than 2. In contrast, owing to its rapidity of onset, kwashiorkor-like secondary protein energy malnutrition may develop in patients with normal subcutaneous fat and muscle mass or, if the patient is obese, even in patients with excess fat and muscle. The serum protein level, however, typically declines and the serum albumin is often less than 2. As with primary protein-energy malnutrition, combinations of the maras mus-like and kwashiorkor-like syndromes can occur simul taneously, typically in patients with progressive chronic disease in whom a superimposed acute illness develops. General Considerations Protein-energy malnutrition occurs as a result of a relative or absolute deficiency of energy and protein. It may be primary, due to inadequate food intake, or secondary, as a result of other illness. For most developing nations, pri mary protein-energy malnutrition remains among the most significant health problems. Kwashiorkor, caused by a deficiency of protein in the presence of adequate energy, is typically seen in weaning infants at the birth of a sibling in areas where foods containing protein are insufficient. Maras mus, caused by combined protein and energy deficiency, is seen where adequate quantities of food are simply not available. In industrialized societies, protein-energy malnutri tion is most often secondary to other diseases. Kwashior kor-like secondary protein-energy malnutrition occurs primarily in association with hypermetabolic acute ill nesses such as trauma, burns, and sepsis. These two syndromes are estimated to be present in at least 20% of hospitalized patients. A substantially greater number of patients have risk factors that could result in them. In both syndromes, protein-energy malnutrition is caused either by decreased intake of energy and protein or. Treatment the treatment of severe protein-energy malnutrition is a slow process requiring great care.
Generic nolvadex 20mg fast delivery
A positive agglutination test (greater than 1:80) develops in the second week after infection and may persist for several years pregnancy and headaches generic 10mg nolvadex. Differential Diag nosis Tularemia must be differentiated from rickettsial and meningococcal infections, cat-scratch disease, infectious mononucleosis, and various bacterial and fungal diseases. Symptoms and Signs the onset is sudden, with high fever, malaise, tachycardia, intense headache, delirium, and severe myalgias. If pneumonia develops, tachypnea, productive cough, blood-tinged sputum, and cyanosis also occur. Axillary, inguinal, or cervical lymph nodes become enlarged and tender and may suppurate and drain. With hematogenous spread, the patient may rapidly become toxic and comatose, with purpuric spots (black plague) appearing on the skin. Primary plague pneumonia is a fulminant pneumoni this with bloody, frothy sputum and sepsis. Laboratory Findings the plague bacillus may be found in smears from aspirates of buboes examined with Gram stain. In convalescing patients, an antibody titer rise may be demonstrated by agglutination tests. Complications Hematogenous spread may produce meningitis, perisple nitis, pericarditis, pneumonia, and osteomyelitis. Gentamicin, which has good in vitro activity against F tularensis, is generally less toxic than streptomycin and probably just as effective. A variety of other agents (eg, fluoroquino lones) are active in vitro but their clinical effectiveness is less well established. The lymphadenitis of plague is most commonly mistaken for the lymphadenitis accompanying staphylococcal or streptococcal infections of an extremity, sexually transmit ted diseases such as lymphogranuloma venereum or syphi lis, and tularemia. The systemic manifestations resemble those of enteric or rickettsial fevers, malaria, or influenza. The pneumonia resembles other bacterial pneumonias, and the meningitis is similar to those caused by other bacteria. Prevention Avoiding exposure to rodents and fleas in endemic areas is the best prevention strategy. Drug prophylaxis may provide temporary protection for persons exposed to the risk of plague infection, particularly by the respiratory route. General Considerations Plague is an infection of wild rodents with Yersinia pestis, a small bipolar-staining gram-negative rod. Either streptomycin (the agent with which there is greatest experience), 1 g every 12 hours intravenously, or gentamicin, administered as a 2-mg/kg loading dose, then 1. Patients with plague pneumonia are placed in strict respiratory isolation, and prophylactic therapy is given to any person who came in contact with the patient. Outbreak of human pneumonic plague with dog-to human and possible human-to-human transmission-Colo rado, June-July 2014. Women may have dysuria, urinary frequency, and urgency, with a purulent urethral discharge. Infection may be asymptomatic, with only slightly increased vaginal discharge and moderate cervicitis on examination. It can progress to involve the uterus and tubes with acute and chronic salpingitis, with scarring of tubes and sterility. In pelvic inflammatory disease, anaerobes and chlamydiae often accompany gonococci. Rectal infection may result from spread of the organism from the genital tract or from anal coitus. Gram stain of urethral discharge in men, especially dur ing the first week after onset, shows gram-negative diplo cocci in polymorphonuclear leukocytes. Nucleic acid amplification tests are the preferred method for diagnosing all types of gonor rhea given their excellent sensitivity and specificity. Cultures should still be obtained when evaluating a treatment failure to assess for antimicrobial resistance. Disseminated Disease Systemic complications follow the dissemination of gono cocci from the primary site via the bloodstream. Two dis tinct clinical syndromes-either purulent arthritis or the triad of rash, tenosynovitis, and arthralgias-are com monly observed in patients with disseminated gonococcal infection, although overlap can be seen. The skin lesions can range from maculopapular to pustular or hemorrhagic, which tend to be few in number and peripherally located. Gonococci are isolated by culture from less than half of patients with gonococcal arthritis. Conjunctivitis the most common form of eye involvement is direct inoculation of gonococci into the conjunctival sac. The purulent conjunctivitis may rapidly progress to panophthalmitis and loss of the eye unless treated promptly. General Considerations Gonorrhea is caused by Neisseria gonorrhoeae, a gram negative diplococcus typically found inside polymorpho nuclear cells. It is transmitted during sexual activity and has its greatest incidence in the 1 5 - to 29-year-old age group. U rethritis and Cervicitis In men, there is initially burning on urination and a serous or milky discharge. One to 3 days later, the urethral pain is more pronounced and the discharge becomes yellow, creamy, and profuse, sometimes blood-tinged. The disor der may regress and become chronic or progress to involve the prostate, epididymis, and periurethral glands with painful inflammation. Treatment of Other I nfections Disseminated gonococcal infection (including arthritis and arthritis-dermatitis syndromes) should be treated with ceftriaxone (1 g intravenously daily) plus azithromycin (1 000 mg orally as a single dose), until 48 hours after improvement begins, at which time therapy may be switched to cefixime (400 mg orally daily) to complete at least 1 week of antimicrobial therapy. Endocarditis should be treated with ceftriaxone (2 g every 24 hours intrave nously) for at least 4 weeks. Pelvic inflammatory disease requires cefoxitin (2 g par enterally every 6 hours) or cefotetan (2 g intravenously every 12 hours) plus doxycycline (1 00 mg every 12 hours). Clindamycin (900 mg intravenously every 8 hours) plus gentamicin (administered intravenously as a 2-mg/kg load ing dose followed by 1. Ceftriaxone (250 mg intramuscularly as a single dose) or cefoxitin (2 g intramuscularly) plus probenecid (1 g orally as a single dose) plus doxycycline (1 00 mg twice a day for 14 days), with or without metronidazole (500 mg twice daily for 14 days) is an effective outpatient regimen. Reactive arthri this (urethritis, conjunctivitis, arthritis) may mimic gonor rhea or coexist with it. Prevention Prevention is based on education and mechanical or chemical prophylaxis. Effective drugs taken in thera peutic doses within 24 hours of exposure can abort an infection. Partner notification and referral of contacts for treatment has been the standard method used to control sexually transmitted diseases. Expedited treatment of sex partners by patient-delivered partner therapy is more effective than partner notification in reducing persistence and recurrence rates of gonorrhea and chlamydia. Treatment Therapy typically is administered before antimicrobial susceptibilities are known. The choice of which regimen to use should be based on the national prevalences of antibi otic-resistant organisms. Nationwide, strains of gonococci that are resistant to penicillin, tetracycline, or ciprofloxacin have been increasingly observed. Treatment for gonorrhea should include a higher dose of intramuscular ceftriaxone in combination with a second drug (azithromycin or doxycy cline) regardless of concern for possible secondary infec tion with chlamydia. For uncomplicated gonococcal infections of the cervix, urethra, and rectum, the recom mended treatment is ceftriaxone (250 mg intramuscu larly) plus azithromycin (1 000 mg orally as a single dose). In cases where an oral cephalosporin is the only option, cefixime, 400 mg orally as a single dose, can be combined with azithromycin as above. When azithromycin is not an option, doxycycline at 100 mg orally twice daily for 7 days can be substituted. Fluoroquinolones are no longer recom mended for treatment due to high rates of microbial resis tance.
Order nolvadex online now
Blood samples for plasma glucose are obtained at 0 and 120 minutes after ingestion of glucose menstrual headaches generic nolvadex 10mg with amex. An oral glucose tolerance test is normal if the fasting venous plasma glu cose value is less than 100 mg/dL (5. A fast ing value of 126 mg/dL (7 mmol/L) or higher or a 2-hour value of greater than 200 mg/dL (1 1. False-positive results may occur in patients who are malnourished, bedridden, or afflicted with an infection or severe emotional stress. Oral glucose tolerance test-If the fasting plasma glu reactions between glucose and other sugars and the free 5. Glycated hemoglobin (hemoglobin A1) measure ments- Hemoglobin becomes glycated by ketoamine amino groups on the alpha and beta chains. Only glycation of the N-terminal valine of the beta chain imparts suffi cient negative charge to the hemoglobin molecule to allow separation by charge dependent techniques. These charge separated hemoglobins are collectively referred to as hemo globin A1 (HbA 1). The major form of HbA1 is hemoglobin A,c (HbA,c) where glucose is the carbohydrate. Office-based immunoassays using capillary blood ive a result in about 9 minutes and this allows for nearly Since glycohemoglobins circulate within red blood cells whose life span lasts up to 120 days, they generally reflect the state of glycemia over the preceding 8 - 1 2 weeks, thereby providing an improved method of assessing dia betic control. Measurements should be made in patients with either type of diabetes mellitus at 3- to 4-month intervals. In patients monitoring their own blood glucose levels, HbA,c values provide a valuable check on the accuracy of monitoring. There is a linear relationship between the HbA,c and the average glucose levels in the previous 3 months. In a study using a combination of intermittent seven-point capillary blood glucose profiles (preprandial, postprandial, and bedtime) and intermittent continuous glucose monitoring data, the change in glucose values was 28. Substantial individual variability exists, however, betwe n HbA1 and mean glucose concentration. For this reason, caution should be exercised in estimating average glucose levels from measured HbA1c. The accuracy of HbA1c values can be affected by hemo globin variants or traits; the effect depends on the specific hemoglobin variant or derivative and the specific assay used. In patients with high levels of hemoglobin F, immu noassays give falsely low values of HbA1c. Intravenous iro and erythropoietin therapy for treatment of anemia in chronic kidney disease also falsely lower HbA1 c levels. Alternative methods such as fructosamine should be con sidered for these patients. A reflec tance photometer or an amperometric system is then used to measure the reaction that takes place on the reagent strip. All are accurate, but they vary with regard to speed, convenience, size of blood samples required, report ing capability, and cost. These blood glucose meters are relatively inexpensive, ranging from $50 to $ 1 00 each. Each glucose meter also comes with a lancet device and disposable 26- to 33-gauge lancets. Most meters can store from 1 00 to 1 000 glucose values in their memories and have capabilities to download the values into a computer spreadsheet for review by the patients and their health care team. Contour Next Link meter, for example, communicates with the MiniMed Medtronic pump). The accuracy of data obtained by home glucose monitoring does require education of the patient in sam pling and measuring procedures as well as in properly cali brating the instruments. The clinician should be aware of the limitations of the self-monitoring glucose systems. The strips have limited lifespans and improper storage (high temperature; open vial) can affect their function. Some of the older meters require input of a code for each batch of strips and failure to enter the code can result in misleading results. Increases or decreases in hematocrit can decrease or increase the mea sured glucose values. The mechanism underlying this effect is not known but presumably it is due to the impact of red cells on the diffusion of plasma into the reagent layer. Meters and the test strips are calibrated over the glucose concentrations ranging from 60 mg/dL (3. L), the difference between the meter and the laboratory value may be as much as 20%. Glucose oxidase-based amperometric systems underesti mate glucose levels in the presence of high oxygen tension. This may be important in the critically ill who are receiving supplemental oxygen; under these circumstances, a glucose dehydrogenase-based system may be preferable. Some meters have been approved for measur ing glucose in blood samples obtained at alternative sites such as the forearm and thigh. There is, however, a 5- to 20-minute lag in the glucose response on the arm with respect to the glucose response on the finger. Forearm blood glucose measurements could therefore result in a falsely lower test results possibly by inhibiting glycation of hemoglobin. Conditions that increase erythrocyte survival such as splenectomy for hereditary spherocytosis will falsely raise HbA1c levels. The advantages of using the HbA1c to diagnose diabetes is that there is no need to fast; it has lower intraindividual variability than the fasting glu cose test and the oral glucose tolerance test; and it provides an estimate of glucose control for the preceding 2-3 months. The diagnosis should be confirmed with a repeat HbA1c test, unless the patient is symptomatic with plasma glucose levels greater than 200 mg/dL (1 1. This test is not appropriate to use in populations with high prevalence of hemoglobinopathies or in conditions with increased red cell turnover. Serum fructosamine-Serum fructosamine is formed by nonenzymatic glyco sylation of s erum proteins (pre dominantly albumin). Since serum albumin has a much shorter half-life than hemoglobin, serum fructos amine generally reflects the state of glycemic control for only the preceding 1 -2 weeks. Reductions in serum albu min (eg, nephrotic state, protein-losing enteropathy, or hepatic disease) will lower the serum fructosamine value. When abnormal hemoglobins or hemolytic states affect the interpretation of glycohemoglobin or when a narrower time frame is required, such as for ascertaining glycemic control at the time of conception in a diabetic woman who has recently become pregnant, serum fructosamine assays offer some advantage. Normal values vary in relation to the serum albumin concentration and are 200-285 mcmol! Substantial individual variability exists, though, when estimating the likely HbA1c value from the fructosamine measurement. Self-monitoring of blood gl ucose-Capillary blood glucose measurements performed by patients themselves, as outpatients, are extremely useful. In type 1 patients in whom "tight" metabolic control is attempted, they are indispensable. Impaired circulation to the fingers (for example, in patients with Raynaud disease) will artificially lower finger-stick glucose measurements (pseudohypoglycemia). The systems manufactured by Medtronic Minimed, DexCom systems, and Abbott Diagnostics (out side the United States), involve inserting a subcutaneous sensor (rather like an insulin pump cannula) that measures glucose concentrations in the interstitial fluid for 3-7 days. The MiniMed system can only be used in conjunction with the Minimed pump and the glucose data are displayed on the screen of the pump. The D exCom system transmits glucose data wirelessly to a separate pager-like evice with a screen. The DexCom system also has the optiOn of dts playing data on smart phones or smart watches or on the screens of several insulin pumps. The systems allow the patient to set "alerts" for low and high glucose values an d rate of change of glucose levels.