Discount 40mg pepcid mastercard
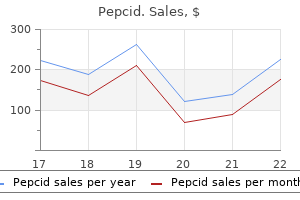
Skin conditions such as scleromyxedema, necrobiotic xanthogranuloma, and cryoglobulinemia should be considered in the differential diagnosis when patients present with cutaneous lesions medicine norco generic pepcid 40 mg amex. This should distinguish benign from clinically relevant conditions that need immediate intervention. A good understanding of conditions associated with monoclonal gammopathy is essential. Immunoglobulin free light assay will help identify cases with only free light chain production, but negative protein electrophoresis. Alternatively, the change in the phenotype may be a consequence of the transformation process. The most recent annual percentage change for each rate is indicated adjacent to the respective regression line. The translocations result in dysregulated or increased expression of an oncogene that is positioned near one or more of the strong Ig enhancers. Rarely, tumors can have translocations involving two of the primary translocation groups, suggesting that there can be some complementation. It is a histone methyltransferase for H3K36me2, and when overexpressed it results in a global increase in H3K36 methylation, and a decrease in H3K27 methylation, which might explain some of the many changes in gene expression associated with t(4;14) tumors. Interestingly, in patients with t(4;14) or t(14;16) or t(14;20) or del17p, the presence of one or more trisomies is associated with a substantially better prognosis than with the absence of trisomies. Oncogenic pathways can be activated through cell intrinsic or extrinsic mechanisms. Much of this knowledge is already being utilized for diagnosis, prognosis, and risk-stratification of patients. A characteristic symptom of cirrhosis is distention of the abdomen caused by the accumulation of fluid in the peritoneal cavity. When the liver fails to produce adequate amounts of albumin, an albumin deficiency, hypoalbuminemia, develops and fluid leaks out of the blood vessels, causing edema. Because the necrotic cells of the cirrhotic patient fail to produce albumin, ascitic fluid develops, as does edema, particularly in the ankles and legs. Bile accumulates in the blood, leading to jaundice and, because bile is not secreted into the duodenum, clay-colored stools. The excess of bile, carried by the blood to the kidneys, imparts a dark color to urine. Other signs are related to the fact that the diseased liver cannot perform its usual biochemical activities. Estrogens then have no effect on the male, but the cirrhotic liver does not inactivate estrogens. The breasts enlarge, a condition known as gynecomastia, and the palms of the hands become red because of the estrogen level. Know Your Viruses the more you know about how a virus is transmitted, the better prepared you can be to prevent infection. Hepatitis B and C are transmitted through contaminated needles and syringes and by sexual intercourse. Hepatitis B and C are rarely transmitted by transfusions because blood is screened for viruses. Which type of hepatitis can be controlled by practicing good handwashing techniques Elevated ammonia causes neurologic disorders, including confusion, disorientation, stupor, and a tremor called asterixis or "liver flap. Although chronic alcoholism is the leading cause of cirrhosis, other diseases can also cause it. Severe chronic hepatitis, chronic inflammation of the bile ducts, and certain drugs and toxins can cause necrosis of the liver cells, which is the first step in the development of cirrhosis. Liver damage cannot be reversed, but further damage can be prevented by treating alcoholism or liver infections that are at the root of cirrhosis. For example, edema is treated with diuretics and portal hypertension is remedied with beta blockers to reduce blood pressure. Cancer of the liver Hepatocarcinoma, or cancer of the liver, is a rare primary malignancy of the liver with a high mortality rate. While liver cancer comprises 1% of all cancers in the United States, it accounts for 6% and 2% of cancer deaths in men and women, respectively. Liver cancer is most prevalent in Chapter Nine Diseases and Disorders of the Gastrointestinal System L 187 men over age 60, and the incidence increases with age. Most cancer found in the liver is secondary, a result of metastasis from cancer in other organs, especially the colon, rectum, stomach, pancreas, esophagus, lung, or breast. Other causes of liver cancer may include aflatoxin, a toxin from a mold that grows on peanuts and rice. If the tumor obstructs the portal vein, ascites develops in the abdominal cavity, as it does in cirrhosis. General symptoms may include loss of weight and an abdominal mass and pain in the upper right quadrant of the abdomen. Diagnosis includes serum levels of enzymes that arise from diseased liver tissue, but correct diagnosis depends on needle biopsy or open biopsy. Prognosis for cancer of the liver is poor because usually the malignancy has developed elsewhere and has spread to the liver. The usual treatment for gallstones is surgical removal of the gallbladder, a cholecystectomy. Occasionally, undetected cholesterol stones are retained in the common bile duct after surgery. Administering a solubilizing agent through a catheter into the bile duct may dissolve the remaining stones, preventing the necessity of repeated surgery. Diseases of the Gallbladder Gallstones (Cholelithiasis) Gallstones are precipitated bile components in the gallbladder and bile ducts. Gallstones and gallbladder disorders (cholecystitis, discussed in the following subsection) are common, affecting about 1 million Americans per year. Risk factors include gender (affects women more often), obesity, age, and family history. The stones arise in the gallbladder when the bile composition changes or when gallbladder muscle activity reduces, as it may during pregnancy, use of oral contraceptives, diabetes mellitus, obesity, cirrhosis, and pancreatitis. The stones consist principally of cholesterol, bilirubin, and calcium when in excess. Gallstones, also called biliary calculi, may be present in the gallbladder and give no symptoms. Small stones, referred to as gravel, can enter the common bile duct and cause an obstruction with excruciating pain. Cholecystitis Cholecystitis is an inflammation of the gallbladder usually associated with gallstones (cholelithiasis). Chills and fever, nausea and vomiting, belching, and indigestion are symptoms; in chronic cholecystitis these symptoms occur especially after eating fatty foods. The presence of fat in the duodenum stimulates the gallbladder to contract, which causes pain. Prolonged inflammation causes the walls of the gallbladder to thicken, making it impossible for the gallbladder to contract properly. Lack of blood flow because of the obstruction brought about by the swelling can cause an infarction. To reduce the risk of pancreatitis, one should stop smoking, stop drinking alcohol, and ensure good hydration. Diseases of the Pancreas Pancreatitis Acute pancreatitis is a serious, painful inflammation of the pancreas. Pancreatitis is more prevalent in women than in men and usually occurs after age 40. The prognosis is good if pancreatitis is associated with gallbladder disease but is very poor if it is related to alcoholism. The intense pain radiates to the back and resembles the sharp pain of a perforated ulcer. If a large area of the pancreas is affected, both endocrine and digestive functions of the gland become impaired.
Generic pepcid 40mg visa
In rare cases, mast cell disease is not identified at initial diagnosis but becomes apparent later in the disease medicine keychain order pepcid 40mg without a prescription. Aggressive systemic mastocytosis includes criteria for systemic mastocytosis and includes one or more of the C findings (Table 80. Finally, mast cell leukemia is a type of systemic mastocytosis with diffuse marrow infiltration with 20% or more mast cells in the bone marrow aspirate smear129. This is an aggressive disease with similar prognosis as found in aggressive systemic mastocytosis. Special stains, including toluidine blue and chloracetate esterase, will mark normal mast cells, but more specific immunophenotypic markers now exist. In the bone marrow, immunohistochemistry can be performed on the core biopsy and will show paratrabecular aggregates of mast cells with associated fibrosis in systemic mastocytosis. Because bone marrow aspirates may yield hemodilute samples due to the fibrosis with fewer mast cells for analysis, flow cytometry immunophenotyping may require a higher number of events for adequate immunophenotypic characterization of mast cells present132. Other mutations include tyrosine or phenylalanine substitutions for aspartate at codon 816 and lysine for glutamic acid at codon 839136. Bone marrow biopsy shows a paratrabecular nodule of spindled mast cells admixed with scattered eosinophils (A). Peripheral blood neutrophils may appear toxic but without dysplasia, and there is no monocytosis, eosinophilia, or basophilia. The platelet count may be normal, but thrombocytopenia develops with progressive splenomegaly. Cytogenetics are abnormal in 20% of patients and have included trisomy 9, deletion of 11q, deletion of 20q, and trisomy 21153. Prognosis is variable and reports of transformation to acute leukemia are documented142,154,155. Patients are young men with eosinophilia and a subset may present with elevated serum tryptase levels139. Morphologic findings are those of a hypercellular marrow with a myeloid hyperplasia and marked eosinophilia; fibrosis is typically present. The bone marrow biopsy is striking for marked fibrosis that accompanies a hypercellular marrow with eosinophilia (A). These disorders may present with cytopenias and dysplastic changes of any cell line, similar to the myelodysplastic syndromes, as well as leukocytosis, hypercellular marrow with fibrosis, and organomegaly, features more commonly associated with myeloproliferative disorders. The presence of fibrosis alone in a case that is otherwise typical of myelodysplasia is not sufficient to use this category. Patients often have both dysplastic changes and elevated white blood cell counts with splenomegaly. Promonocytes, with more immature nuclear chromatin, may be present in the blood, but monoblasts are usually rare to absent. Regardless of the presenting neoplasm, patients usually have eosinophilia in the blood, marrow, or both. The bone marrow biopsy is hypercellular with a granulocytic hyperplasia and marrow eosinophilia (A). Peripheral blood smear with monocytes demonstrating abundant pale cytoplasm containing fine granulation, and folded nuclei with delicate chromatin and small nucleoli. Dysplastic hypogranular neutrophils, a single blast, and a nucleated red cell are also present. A recent consensus guideline defines morphologic criteria to help standardize the differentiation of monoblasts and promonocytes from immature and mature monocytes177. When granulocytic hyperplasia is prominent, it may be difficult to distinguish the abnormal monocyte population from myelocytes. Erythroid precursors and megakaryocytes may demonstrate prominent dysplastic changes, but often these cell types are normal in appearance. When bone marrow blasts and promonocytes are 20%, such cases are now diagnosed as acute myeloid leukemias. Flow cytometry may Who criTeria For chroNic MyeloMoNocyTic leuKeMia Persistent peripheral blood monocytes >1. Chapter 80 Pathology of the Myeloproliferative Neoplasms be helpful in excluding acute myeloid leukemia, but enumeration of blasts (including monoblasts and promonocytes) must be based on morphology rather than flow cytometry. The most frequent recurring cytogenetic abnormalities include trisomy 8, monosomy7/deletion (7q), structural abnormalities of 12p, and i(17q). Granulocytes are left-shifted and dysplastic with hypolobated nuclei and hypogranular cytoplasm. The bone marrow is hypercellular, with an elevated myeloid-to-erythroid ratio, and marrow fibrosis may be prominent. Dyserythropoiesis and megakaryocyte dysplasia are common and megakaryocytes may be reduced in number with associated thrombocytopenia. Patients may develop acute leukemia or bone marrow failure secondary to marked fibrosis. Other ancillary studies, particularly immunophenotyping studies, are usually not helpful unless an elevation in blasts is present. Response to: Differentiating Juvenile Myelomonocytic Leukemia from Infectious Disease. Peripheral blood smear shows left-shifted leukocytosis and dysplastic monocytosis. A small blast is above a sparsely granulated lone platelet adjacent to a monocyte. Many of these cases have typical features of myelodysplasia, as well as an atypical finding more suggestive of a myeloproliferative disorder, such as marked marrow fibrosis and hypercellularity or organomegaly. Such cases may be termed myelodysplastic/myeloproliferative disease, unclassifiable, with a comment describing the atypical findings. These cases have no sex predilection or specific cytogenetic abnormality and must be differentiated from the 5q syndrome. The bone marrow contains >15% ringed sideroblasts with an accompanying atypical megakaryocytic proliferation; megakaryocytes often resemble those seen in essential thrombocythemia. Bone marrow aspirate shows numerous erythroid precursors and left-shifted immature myeloid cells with dysplasia. The bone marrow biopsy shows dysplastic megakaryocytes, small hypolobated forms, and micromegakaryocytes, in a hypercellular marrow, with inset demonstrating numerous ringed sideroblasts. Given the mix of morphology among these diseases, correlation with clinical, hematologic, and cytogenetic/molecular genetic findings is imperative for precise classification. Multicenter independent assessment of outcomes in chronic myeloid leukemia patients treated with imatinib. The correlation of breakpoint cluster region rearrangement and p210 phl/abl expression with morphological analysis of Ph-negative chronic myeloid leukemia and other myeloproliferative diseases. The 2001 World Health Organization and updated European clinical and pathological criteria for the diagnosis, classification, and staging of the Philadelphia chromosome-negative chronic myeloproliferative disorders. Agnogenic myeloid metaplasia: a clonal proliferation of hematopoietic stem cells with secondary myelofibrosis. A large proportion of patients with a diagnosis of essential thrombocythemia do not have a clonal disorder and may be at lower risk of thrombotic complications. World Health Organization-defined eosinophilic disorders: 2011 update on diagnosis, risk stratification, and management. Identification of a point mutation in the catalytic domain of the protooncogene c-kit in peripheral blood mononuclear cells of patients who have mastocytosis with an associated hematologic disorder. Elevated serum tryptase levels identify a subset of patients with a myeloproliferative variant of idiopathic hypereosinophilic syndrome associated with tissue fibrosis, poor prognosis, and imatinib responsiveness. Efficacy of imatinib mesylate in the treatment of idiopathic hypereosinophilic syndrome. Myelodysplastic and myeloproliferative disorders of childhood: a study of 167 patients. Chronic eosinophilic leukemias and the myeloproliferative variant of the hypereosinophilic syndrome. Mutations of the ras protooncogenes in chronic myelogenous leukemia: a high frequency of ras mutations in bcr/abl rearrangement-negative chronic myelogenous leukemia.
Buy 40 mg pepcid visa
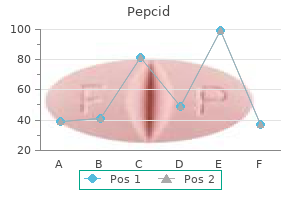
Draw a family of cardiac function curves describing the relationship between filling pressure and cardiac output under various levels of sympathetic tone medicine 6 clinic buy generic pepcid 20 mg. Blood that had previously accumulated in the atrium behind the closed mitral valve empties rapidly into the ventricle and this causes an initial decrease in atrial pressure. Later, the pressures in both chambers slowly increase together as the atrium and ventricle continue passively filling with blood returning to the heart through the veins. Atrial contraction is initiated near the end of ventricular diastole by the depolarization of the atrial muscle cells, which causes the P wave of the electrocardiogram. This important figure summarizes a great deal of information and should be studied carefully. Cardiac cycle phases: A) diastole; B) systole that is divided into three periods; C) isovolumetric contraction; D) ejection, and E) isovolumetric relaxation. At normal heart rates, atrial contraction is not essential for adequate ventricular filling. Atrial contraction plays an increasingly significant role in ventricular filling as heart rate increases because the time interval between beats for passive filling becomes progressively shorter. Note that throughout diastole, atrial and ventricular pressures are almost the same. Pressure in the left ventricle continues to increase sharply as the ventricular contraction intensifies. When the left ventricular pressure exceeds that in the aorta, the aortic valve opens. The period of time between mitral valve closure and aortic valve opening is referred to as the isovolumetric contraction phase because, during this interval, the ventricle is a closed chamber with a fixed volume. Pressure builds simultaneously in both the ventricle and the aorta as the ventricular muscle cells continue to contract in early systole. Aortic pressure begins to decrease because blood is leaving the aorta and large arteries faster than blood is entering from the left ventricle. Throughout ejection, there are very small pressure differences between the left ventricle and the aorta because the aortic valve orifice is so large that it presents very little resistance to flow. Eventually, the strength of the ventricular contraction diminishes to the point where intraventricular pressure decreases below aortic pressure. A dip, called the incisura or dicrotic notch, appears in the aortic pressure trace because a small volume of aortic blood must flow backward to fill the aortic valve leaflets as they close. After aortic valve closure, intraventricular pressure decreases rapidly as the ventricular muscle relaxes. Note that atrial pressure progressively increases during ventricular systole because blood continues to return to the heart and fill the atrium. The ventricle has reached its minimum (end-systolic volume) at the time of aortic valve closure. During the early, most rapid phase of systolic ejection, the aorta distends because more blood is being put into it from the left heart than is leaving it to the systemic organs. The overall result is that the aortic pressure reaches a maximum value (systolic pressure) near the middle of ventricular systole. During diastole, the arterial pressure is maintained by the elastic recoil of walls of the aorta and other large arteries. Nonetheless, aortic pressure gradually decreases during diastole as the aorta supplies blood to the systemic vascular beds. The lowest aortic pressure, reached at the end of diastole, is called diastolic pressure. The difference between diastolic and peak systolic pressure in the aorta is called the arterial pulse pressure. Typical values for systolic and diastolic pressures in the aorta are 120 and 80 mm Hg, respectively, with a pulse pressure of 40 mm Hg. At a normal resting heart rate of about 70 beats/min, the heart spends approximately two thirds of the cardiac cycle in diastole and one third in systole. When increases in heart rate occur, both diastolic and systolic intervals become shorter. This shortening of the systolic interval tends to blunt the potential adverse effects of increases in heart rate on diastolic filling time. Both ventricles have synchronous systolic and diastolic periods and the valves of the right and left heart normally open and close nearly in unison. Because the two sides of the heart are arranged in series in the circulation, they must pump the same amount of blood and therefore must have the same cardiac output. The major difference between the right and left pumps is in the magnitude of the peak systolic pressure. S1 can be heard most clearly by placing the stethoscope over the apex of the heart. Because this discrepancy is enhanced during the inspiratory phase of the respiratory cycle, inspiration causes what is referred to as the physiological splitting of the second heart sound. The discrepancy in valve closure during inspiration may range from 30 to 60 milliseconds. One of the factors that leads to prolonged ejection of the right ventricle during inspiration is that the decreased intrathoracic pressure that accompanies inspiration transiently enhances venous return and diastolic filling of the right heart. For reasons that will be detailed later in this chapter, this extra filling volume will be ejected but a little extra time is required. When they are present, however, they, along with S1 and S2, produce what are called gallop rhythms (resembling the sound of a galloping horse). When present, the third heart sound occurs shortly after S2 during the period of rapid passive ventricular filling and, in combination with heart sounds S1 and S2, produces what is called ventricular gallop rhythm. Although S3 may sometimes be detected in normal children, it is heard more commonly in patients with left ventricular failure. The fourth heart sound, which occasionally is heard shortly before S1, is associated with atrial contraction and rapid active filling of the ventricle. Thus, the combination of S1, S2, and S4 sounds produces what is called an atrial gallop rhythm. Typical pulmonary artery systolic and diastolic pressures are 25 and 8 mm Hg, respectively. The pressure pulsations that occur in the right atrium are transmitted in retrograde fashion to the large veins near the heart. They are collectively referred to as the jugular venous pulse, and can provide clinically useful information about the heart. The c wave, which follows shortly thereafter, coincides with the onset of ventricular systole and is caused by an initial bulging of the tricuspid valve into the right atrium. Right atrial pressure decreases after the c wave because of atrial relaxation and a downward displacement of the tricuspid valve during ventricular emptying. Right atrial pressure then begins to increase toward a third peak, the v wave, as the central veins and right atrium fill behind a closed tricuspid valve with blood returning to the heart from the peripheral organs. With the opening of the tricuspid valve at the conclusion of ventricular systole, right atrial pressure again decreases as blood moves into the relaxed right ventricle. Shortly afterward, right atrial pressure begins to increase once more toward the next a wave as returning blood fills the central veins, the right atrium, and right ventricle together during diastole. Each major phase of the ventricular cardiac cycle has a corresponding phase of cardiac muscle length and tension change. During diastolic ventricular filling, for example, the progressive increase in ventricular pressure stretches the resting cardiac muscle to greater lengths along its resting length-tension curve and causes a corresponding increase in muscle tension. These sounds are normally heard by auscultation with a stethoscope placed on the chest. At the onset of systole, the ventricular muscle cells develop tension isometrically (during the isovolumetric contraction phase) and intraventricular pressure increases accordingly. After the intraventricular pressure increases sufficiently to open the outlet valve, ventricular ejection begins as a consequence of ventricular muscle shortening. Systemic arterial pressure is often referred to as the ventricular afterload because it determines the tension that must be developed by cardiac muscle fibers before they can shorten.
Generic pepcid 40 mg online
It is caused by mutations of the NaV channel of skeletal muscle that make them slowly inactivating; the myotonia results from abnormal reopenings of the NaV channels the treatment 2014 order pepcid in india. Moderate elevation of extracellular potassium favors aberrant gating with persistent and prolonged reopenings. The Na current through these channels may cause skeletal muscle weakness by depolarizing the cells, thereby inactivating normal NaV channels, which are then unable to generate action potentials. Attacks can be stopped by ingesting a high sugar load or by thiazide diuretics, both of which reduce extracellular potassium. They can be prevented by a diet low in potassium and high in carbohydrates, and also with thiazides. Outdoors on a cold and windy day, her face stiffened in a grimace and she could not open her eyes or move them from side to side. These symptoms disappeared within a few minutes after she had entered a warm room. During pregnancy she had daily attacks of weakness; within a few days after delivery she improved. Forty-five minutes later, she was so stiff that she could make no quick movements. At that time, she could not lift her head, arms, or legs, nor could she move her limbs on the examination table. Myotonia (difficulty of relaxing muscles) of her facial and extraocular muscles was intense. This disease also affected her son, sister, mother, maternal aunt, and maternal grandfather. The inheritance was due to a single autosomal, dominant gene with probably complete penetrance. This positive feedback loop produces the all-or-none quality and the propagation of action potentials. K+ leaving the cell repolarizes the membrane potential and terminates action potentials. Voltage clamping, or negative feedback control of the membrane potential, facilitates understanding of the currents underlying the action potential. The amplitude and direction of the sodium current vary with the amplitude of voltage-clamp steps in membrane potential. The gating current is a direct sign of the conformational changes in the sodium channel proteins. Following an action potential, excitable cells have an absolute refractory period when they will not produce a second action potential and then a relative refractory period when a larger stimulus is required to produce a second action potential. Demyelinating diseases slow the conduction velocity and may block the propagation of action potentials. Action potentials appear differently when they are recorded with a pair of wires placed on the outside of a nerve bundle. Compound action potentials, the sum of many externally recorded action potentials, have properties that differ from those of single action potentials recorded with intracellular electrodes. There is an inward current (If) associated with pacemaker activity in cells of the sinoatrial node. Stimulation of sympathetic nerves leading to the heart or application of norepinephrine produces A) a decrease of If, a decrease in heart rate, and an increase in strength of contraction. B) a decrease of If, an increase in heart rate, and an increase in strength of contraction. C) an increase of If, an increase in heart rate, and an increase in strength of contraction. D) an increase of If, a decrease in heart rate, and a decrease in strength of contraction. E) an increase of If, an increase in heart rate, and a decrease in strength of contraction. Propagation of a nerve impulse does not require A) closure of potassium channels that maintain the resting potential. The compound action potential recorded with a pair extracellular electrodes from an intact bundle of nerve fibers A) propagates without change in size or shape. If a threshold is exceeded, further increase in stimulus does not increase the response. Hyperkalemia (high extracellular potassium concentration) can stop the heart because A) potassium ions bind to sodium channels, preventing their activity. C) the membrane potential of heart cells depolarizes and its sodium channels inactivate. Myelination of axons A) reduces conduction velocity to provide more reliable transmission. Consider the following three channels in ventricular muscle cells: sodium channel (NaV), inward rectifier potassium channel (Kir), and calcium channel (CaV). Choose the answer that best describes which of these channels is open during the plateau phase of the ventricular action potential. Describe the biosynthesis and actions of acetylcholine, catecholamines (dopamine, norepinephrine, epinephrine), serotonin, histamine, and excitatory and inhibitory amino acids. Describe the structure of the neuromuscular junction and the functions of the various substructures. Describe the actions and explain the mechanisms for the effects of Ca2+ and Mg2+ on transmitter release. Describe how acetylcholine interacts with receptors on the postsynaptic membrane and the fate of the acetylcholine. Describe the generation of the endplate potential and the effects and mechanisms of action of acetylcholine esterase inhibitors and blockers of acetylcholine receptors. Describe facilitation and posttetanic potentiation of transmitter release and how these processes can be used to explain certain features of myasthenia gravis and recovery from receptor blockade. Describe the structures and explain the functions of the various parts of neurons. Describe transport of materials up and down axons (orthograde and retrograde axonal transport) including mechanisms and materials. Describe the differences and similarities between synaptic transmission at a central synapse and at neuromuscular junctions. Describe the integration of information and repetitive firing in neurons and the concept of presynaptic inhibition. Most synapses are chemical; the presynaptic neuron releases a transmitter substance that diffuses across the synaptic cleft and binds to a receptor on the postsynaptic cell. Thus, they do not readily pass through lipid membranes and can be compartmentalized as needed. Chemical synapses offer the possibility of amplification, signal inversion, and persistent effects; electrical synapses are faster and seem to be used when synchronization is more important than computation (information processing). Chemical synapses may be excitatory or inhibitory, depending on their effect on the postsynaptic cell. They are chemosensitive channels that are opened by nicotine and blocked by curare. The nonpeptide transmitters are concentrated inside vesicles by specific H/transmitter cotransporters. The transmitter concentration inside the vesicle can be quite high, on the order of 20,000 molecules in a 20-nm radius sphere, or about 30 mM. After release, transmitters are degraded or transported back into the presynaptic terminal for reuse. Some transmitters are small polypeptides that are synthesized on rough endoplasmic reticulum near the nucleus, packaged by the Golgi apparatus, and then transported in vesicles the length of the axon by an active process called axoplasmic transport. Recently Botox injections have been used to treat dystonia, a movement disorder characterized by involuntary muscle contractions, and cosmetically to locally block facial muscles that wrinkle the skin. Excessive doses or systemic toxin delivery from contamination during food canning can lead to death. The battlefield countermeasures are to block the postsynaptic receptors on the heart with atropine.
Purchase 20 mg pepcid otc
Eyelid Infections One of the most noticeable lesions found on the eyelid is the common stye or hordeolum medications migraine headaches pepcid 40mg low cost. The precise incidence of the common stye is difficult to determine because many individuals do not seek treatment for these lesions. The etiology of a hordeolum is infection with staphylococcus bacteria, which trigger abscess formation on the upper and lower eyelid. Symptoms generally include redness, pain, and swelling with a foreign-body sensation on the eye. Impaired Color Vision and Color Blindness Color vision is made possible by photoreceptors in the retina called cones. These are sensitive to certain wavelengths of light that are associated with different colors. Inherited deficiencies in these cones cause various degrees of impaired color vision. Most people with impaired color vision cannot distinguish shades of red and green. The prevalence of this type is about 1 in 12 males of northern European ancestry but it is lower in other ethnic groups. Some people with impaired color vision cannot distinguish shades of blue and yellow. Complete absence of color vision is called color blindness and is rare, affecting 1 in 30,000 people worldwide. Color vision impairments and color blindness are carried on the X chromosome, so these occur more often in males, although females can inherit the condition too. Color blindness can be diagnosed with a multicolored, spotted eye chart in which colored numbers are embedded and visible to those with normal color vision. Ocular Tumors Retinoblastoma Retinoblastoma is a rare, recessively inherited childhood tumor of the retina. Approximately 40% of retinoblastomas are inherited, with carriers of the mutant gene having a 10,000-fold increased risk for the development of retinoblastoma. Retinoblastoma generally affects children under 6 years of age and is most commonly diagnosed during the first 2 years of life. Treatment of retinoblastoma is aimed at preserving vision, destroying the tumor, and monitoring for metastasis. Large tumors are treated by removal of the affected eye(s) with as much of the optic nerve as necessary. In contrast, metastatic retinoblastoma tends to spread to the brain and bone marrow and is associated with a poor prognosis. Genetic counseling can help families understand the genetic consequences of retinoblastoma and estimate the risk of disease in family members. The pinna directs sound into the auditory canal, a skin-lined tube that leads to the middle ear. The innermost part of the auditory canal is also lined with glands that secrete cerumen, a waxy substance that keeps the tympanic membrane soft and flexible. The middle ear begins at the tympanic membrane (ear drum), a fibrous tissue that spans the auditory canal. Sound waves trigger vibrations of the tympanic membrane, which transmits the vibrations to three middle-ear bones, the auditory ossicles. The stapes vibrates against an opening in the cochlea, a snail-shaped organ within the inner ear. Vibrations moving through the fluid of the cochlea stimulate specialized structures called hair cells, which transmit information about the vibrations along the auditory nerve to the brain for interpretation. Diagnostic Tests and Procedures: the Ear External exam reveals conditions of the external ear and auditory canal. An otoscope permits visualization of the auditory canal and the condition of the tympanic membrane. Hearing tests utilize head phones or tuning forks to assess hearing and the causes of hearing loss. Diseases and Disorders of the Ear Diseases and Disorders of the External Ear Cerumen Impaction As already noted, cerumen keeps the tympanic membrane soft and flexible. In most people cerumen that is secreted slowly moves to the outer ear and flakes off. Signs and symptoms of impaction are ringing in the ear (tinnitus), earache, or diminished hearing Anatomy and Physiology Review: the Ear the ear is the organ of hearing and balance. The portion of the outer ear that is external to the skull is called the pinna; it is covered by skin and supported by cartilage. Treatment should be done by a doctor because the tympanic membrane is delicate and can be easily injured while removing impacted cerumen. To prevent impaction, the ear should not be cleaned with cotton swabs, which usually push cerumen deeper and against the tympanic membrane. If buildup is excessive, a doctor may recommend occasionally applying baby oil or hydrogen peroxide to soften the cerumen, followed by warm water to flush it out. Otitis externa is treated with antibiotics or antifungal medications and analgesics. Otitis externa can be prevented by drying the external ear opening after bathing or swimming. Difficult to prevent, the risk for otitis media can be reduced by avoiding exposure to smoking and air pollution. Breastfeeding infants until 6 months of age has been shown to reduce the incidence of otitis media. Diseases and Disorders of the Inner Ear Hearing Loss Presbycusis is age-related hearing loss and is the most common cause of hearing loss in adults. The risk factors include increasing age, family history of presbycusis, repeated exposure to loud noises, smoking, and certain medical conditions. Signs and symptoms include difficulty understanding conversations, especially in a noisy room. Those with hearing loss may withdraw from social situations to avoid hearing problems. Treatment may include hearing aids if the auditory nerve and cochlea remain functional. The degree of age-related hearing loss can be prevented by reducing exposure to loud noises or by using ear plugs and ear protection when exposed to loud noises. Other causes of hearing loss include trauma, high fever, toxins, certain antibiotics, and infections. Diseases and Disorders of the Middle Ear Otitis Media Otitis media is a middle ear infection. More than 5 million cases of acute otitis media occur among children in the United States each year. Age is the main risk factor for otitis media, which affects mainly infants and children. Children are more susceptible than adults because their nearly horizontal auditory tubes prevent adequate drainage. Diagnosis is based on the observation of a bulging tympanic membrane and effusion (pus and fluids). Hearing protectors can help reduce dangerous noise in areas where noise cannot be controlled or eliminated. How can you tell if hearing loss is caused by nerve problems or by problems with middle ear ossicles Age-Related Diseases and Disorders Age-related changes in vision include loss of visual acuity and decreased sensitivity to light. With age the curvature of the cornea decreases, impairing refraction and its ability to focus light. With age the lens increases in thickness and decreases in elasticity, making it more difficult to accommodate and focus on objects at a close distance. Alterations in sound receptors, neurons, and blood supply to the inner ear are among the changes associated with age. Changes in vision and hearing can be managed with surgical procedures, eyeglasses, and hearing aids. Older adults may not like using hearing devices or eyeglasses because of cost and embarrassment about these signs of aging. However, vision and hearing impairment, balance problems, and reduced muscle strength and coordination contribute to falls among aging adults.
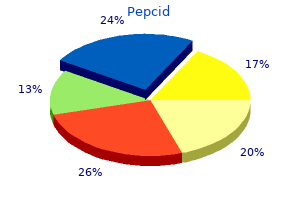
Order 20 mg pepcid overnight delivery
When peripheral venous pressure is increased to 10 mm Hg, considerable venous return occurs with a central venous pressure of 7 mm Hg, and venous return stops only when central venous pressure is increased to 10 mm Hg treatment action group purchase 40 mg pepcid with amex. Thus, increasing peripheral venous pressure shifts the whole venous function curve to the right. By similar logic, decreased peripheral venous pressure caused by blood loss or decreased sympathetic vasoconstriction of peripheral veins shifts the venous function curve to the left. In most contexts, however, "cardiac output" implies the output of the left heart pump. How is it then, as has often been previously implied, that central venous pressure (the filling pressure of the right heart) profoundly affects cardiac output (the output of the left heart) The short answer is that in the steady state, the right and left hearts have equal outputs. The major conclusion here is that left atrial pressure will change in the correct direction to match left ventricular stroke volume to the current right ventricular stroke volume. If central venous pressure were to decrease to 0 mm Hg, cardiac output would decrease (to 2 L/min) and venous return would increase (to 7 L/min). With a venous return of 7 L/min and a cardiac output of 2 L/min, the volume of the central venous compartment would necessarily be increasing and this would produce a progressively increasing central venous pressure. Moreover, if central venous pressure were to increase from 2 to 4 mm Hg, venous return would decrease (to 3 L/min) and cardiac output would increase (to 7 L/min). This would quickly reduce the volume of blood in the central venous pool, and the central venous pressure would soon fall back to the original level. The cardiovascular system automatically adjusts to operate at the point where the cardiac and venous function curves intersect. Central venous pressure is always inherently driven to the value that makes cardiac output and venous return equal. Cardiac output and venous return always stabilize at the level where the cardiac function and venous function curves intersect. Intersection points indicate equilibrium values for cardiac output, venous return, and central venous pressure. At a particular moment, the existing influences on the heart dictate the cardiac function curve on which it is operating, and similarly, the existing influences on peripheral venous pressure dictate the venous function curve that applies. Thus, the influences on the heart and on the peripheral vasculature determine where the cardiac and venous function curves intersect and thus what the central venous pressure and cardiac output (and venous return) are in the steady state. In the intact cardiovascular system, cardiac output can rise only when the point of intersection of the cardiac and venous function curves is raised. All changes in cardiac output are caused by a shift in the cardiac function curve, a shift in the venous function curve, or both. The cardiac function and venous function curves are useful for understanding the complex interactions that occur in the intact cardiovascular system. Assume that before the hemorrhage, sympathetic activity to the heart and peripheral vessels is normal, as is the blood volume. The normal cardiac and venous function curves intersect at point A, so cardiac output is 5 L/min and central venous pressure is 2 mm Hg in the normal state. When blood volume decreases due to hemorrhage, the peripheral venous pressure decreases and the venous function curve is shifted to the left. In the absence of any reflex responses, the cardiovascular system must switch its operation to point B because this is now the point at which the cardiac function curve and the new venous function curve intersect. This automatically occurs because at the moment of blood loss, the venous function curve is shifted to the left and venous return decreases below cardiac output at the central venous pressure of 2 mm Hg. Subnormal cardiac output evokes a number of compensatory mechanisms to bring cardiac output back to more normal levels. One of these is an increase in the activity of cardiac sympathetic nerves that, as discussed in Chapter 24, causes a shift to a cardiac function curve that is higher than normal. The effect of increasing cardiac sympathetic activity is illustrated by a shift in cardiovascular operation from point B to point C. In itself, the increased cardiac sympathetic nerve activity increases cardiac output (from 3 to 4 L/min) but causes a further decrease in central venous pressure. This decrease in central venous pressure occurs because points B and C lie on the same venous function curve. Venous return is higher at point C than at point B, but the venous function curve has not shifted. An additional compensatory mechanism evoked by blood loss is increased activity of the sympathetic nerves leading to veins. Recall that this increases peripheral venous pressure and causes a rightward shift of the venous function curve. Therefore, increased sympathetic activity to veins tends to shift the venous function curve, originally decreased by blood loss, back toward normal. Thus, peripheral venous constriction raises cardiac output by increasing central venous pressure and moving upward along a fixed cardiac function curve. It must be pointed out that separating the response to hemorrhage into distinct, progressive steps. In reality, the reflex venous and cardiac responses occur simultaneously and so quickly that they will keep up with the blood loss as it occurs. Thus, the actual response to hemorrhage would follow nearly a straight line from point A to point D. In summary, point D illustrates that normal cardiac output can be sustained in the face of blood loss by the combined effect of peripheral and cardiac adjustments. Hemorrhage is only one of the numerous potential disturbances to the cardiovascular system. From what has been presented in this chapter, it is possible to conclude that a patient with abnormally high central venous pressure must have a depressed cardiac function curve, a right-shifted venous function curve, or both. Very high central venous pressures are a hallmark of patients with congestive heart failure because they have the combination of dysfunctional heart muscle (depressed cardiac function curve) and excessive fluid volume (right-shifted venous function curve). Abnormally low central venous pressures, on the other hand, could theoretically be caused by either an increased cardiac function curve or a leftshifted venous function curve. Because gravity keeps veins in the head and neck collapsed when a normal individual is upright, there is no distention (or retrograde pulsations from atrial contractions) observed in these neck veins. Conversely, when fully recumbent, neck veins are full and pulsations are detected. If a normal individual is placed in a semi-recumbent position so that external jugular veins are positioned at 7 cm above the right atrium, the point between the collapsed venous segment and the filled segment can often be visualized. Abnormally high central venous pressure is associated with neck vein distention at a higher level (perhaps even when the patient is upright). Because of its diagnostic value in critical care situations, central venous pressure is often monitored continuously via a catheter inserted in a peripheral vein and advanced centrally until its tip is in the central venous compartment. In some situations, it is desirable to assess left atrial pressure, which is the filling pressure for the left side of the heart. This is commonly done with a specialized, flow-directed venous catheter with a small inflatable balloon at its tip to drag it with the blood flow through the right ventricle and pulmonic valve into the pulmonary artery. The balloon is then deflated and the cannula is advanced further until it wedges into a terminal branch of the pulmonary vasculature. The pulmonary wedge pressure recorded at this junction provides a useful estimate of left atrial pressure because there are no valves between the left atrium and the catheter tip. She often has to get up at night to urinate and has noticed that her feet and ankles seem to be swollen. She reports several episodes of waking up at night feeling like she could not catch her breath until she got out of bed and stood at her open window. She has been physically well until this condition developed over the last few months. She does not smoke or drink and takes no medicines except for an occasional aspirin or antacid. Auscultation of the chest with a stethoscope indicates normal heart sounds but abnormal breath sounds with fine crackles heard over both lung bases late in expiration. An echocardiogram revealed dilated cardiac chambers, thickened left ventricular wall, and a left ventricular ejection fraction of 0. She was diagnosed with chronic congestive heart failure secondary to chronic hypertension. Once her condition stabilizes, she will be treated with beta-adrenergic receptor blockers at a low dose to decrease sympathetic stimulation of the heart.
Purchase 20 mg pepcid fast delivery
Both pentostatin and cladribine are excreted by the kidneys and the creatinine should be measured before each treatment and therapy only continued as long as renal function is not impaired medicine 02 discount pepcid uk. Remissions are prolonged, and most relapsing patients respond to a second cycle of therapy. It is difficult to require these added studies for patients being treated from a clinical protocol. Occupational exposures, animal exposure and smoking as risk factors for hairy cell leukaemia evaluated in a case-control study. Diagnostic application of two-color flow cytometry in 161 cases of hairy cell leukemia. Selective influences in the expressed immunoglobulin heavy and light chain gene repertoire in hairy cell leukemia. Lack of allelic exclusion by secondary rearrangements of tumour B-cell receptor light chains in hairy cell leukaemia. Gene expression profiling of hairy cell leukemia reveals a phenotype related to memory B cells with altered expression of chemokine and adhesion receptors. Hairy cell leukaemia: biological and clinical overview from immunogenetic insights. High-resolution genomic profiling in hairy cell leukemia-variant compared with typical hairy cell leukemia. Chromosomal gains and losses are uncommon in hairy cell leukemia: a study based on comparative genomic hybridization and interphase fluorescence in situ hybridization. Constitutively activated Rho guanosine triphosphatases regulate the growth and morphology of hairy cell leukemia cells. Autocrine and paracrine regulation of neoplastic cell growth in hairy cell leukemia. Serum soluble interleukin-2 receptor is associated with clinical and pathologic disease status in hairy cell leukemia. Serum soluble interleukin-2 receptor levels in hairy cell leukemia: correlation with clinical and hematological parameters and with a-interferon treatment. Risk factors for severe infection in patients with hairy cell leukemia: a long-term study of 73 patients. Clonally expanded T cells in hairy cell leukemia patients are not leukemia specific. The bone marrow fibrosis of hairy-cell leukemia is caused by the synthesis and assembly of a fibronectin matrix by the hairy cells. The natural history and clinico-pathological features of the variant form of hairy cell leukemia. Randomized comparison of pentostatin versus interferon alfa-2a in previously untreated patients with hairy cell leukemia: an intergroup study. Recombinant alpha-2b-interferon in therapy of previously untreated hairy cell leukemia: long term results of study by cancer and leukemia group B. Long-term follow-up of interferonalpha induction and low-dose maintenance therapy in hairy cell leukemia. Response to interferonalpha in patients with hairy cell leukemia relapsing after treatment with 2-chlorodeoxyadenosine. On the bioavailability of oral and subcutaneous 2-chloro-2-deoxyadenosine in humans: alternative routes of administration. Subcutaneous injections of 2-chlorodeoxyadenosine for symptomatic hairy cell leukemia. Weekly intermittent 2-CdA is less toxic and equally efficacious when compared to continuous infusion in hairy cell leukaemia. Long-term follow-up of front-line treatment of hairy cell leukemia with 2-chlorodeoxyadenosine. Phase 2 study of rituximab in the treatment of cladribine-failed patients with hairy cell leukemia. Phase 2 study of cladribine followed by rituximab in patients with hairy cell leukemia. Recombinant immunotoxins and other therapies for relapsed/refractory hairy cell leukemia. Rituximab with pentostatin or cladribine: an effective combination treatment for hairy cell leukemia after disease recurrence. Second cancer incidence and cause-specific mortality among 3,104 patients with hairy cell leukemia: a population-based study. The significance of minimal residual disease in hairy cell leukemia patients treated with deoxycoformycin: a long term follow-up study. Long-term results for pentostatin and cladribine treatment of hairy cell leukemia. Long-term outcome following treatment of hairy cell leukemia with pentostatin (Nipent): a national cancer institute of Canada study. An update: 12-year follow-up of patients with hairy cell leukemia following treatment with 2-chlorodeoxyadenosine. Very long-term eradication of minimal residual disease in patients with hairy cell leukemia after a single course of cladribine. Epstein-Barr virus positive large B-cell lymphoma arising in a patient previously treated with cladribine for hairy cell leukemia. Primary cutaneous lymphomas usually present without signs of extracutaneous malignancy at onset of symptoms; they represent an entity distinct from nodal lymphomas with secondary cutaneous involvement. However, initial lesions occasionally appear to improve following topical steroid application, which masks early recognition of the underlying malignancy. Afflicted patients presented only with persistent, generalized pruritus and no clinical eruption. Plaques are sharply demarcated, scaly, elevated lesions that may have annular, arcuate, or serpiginous borders. Plaques with thick scale can mimic psoriasis or nummular eczema, whereas annular lesions with central clearing may be confused with tinea corporis. Prominent involvement of the palms and/or soles may result in hyperkeratosis, fissuring, or frank keratoderma. F thickening, coalescing plaques, and tumors may result in characteristic "leonine facies". The tumor stage is more clinically aggressive than the patch and plaque stages, and may be associated with histologic transformation to a large cell process with a vertical growth phase (see section "Histopathology and Prognosis"). In addition, there are other cutaneous T-cell lymphoproliferative disorders that appear to be specific entities with unique clinical, histologic, and prognostic features. These studies include routine histology, immunophenotyping, and molecular genotyping. Communication between the clinical staff, dermatologists, and pathologists is essential to ensure that the appropriate types of biopsies are done and are properly handled. Punch biopsies can be divided into halves, one half for routine histology and the other half for immunophenotyping and/or molecular diagnostic studies. Sections for routine histology should be fixed in a good nuclear fixative such as B5 to facilitate evaluation of nuclear morphology and recognition of characteristic cerebriform cells. If it is a large biopsy of a cutaneous tumor or a lymph node biopsy, it may provide adequate tissue to prepare cell suspensions for immunophenotyping by flow cytometry and for cytogenetic studies. The tissue for immunophenotyping by flow cytometry should be promptly delivered to the appropriate laboratory in cell culture media. For leukemic infiltrates, cytochemical stains can be performed on air-dried touch imprints from freshly cut surfaces. A small sliver of the biopsy can be shaved off and fixed in glutaraldehyde for electron microscopy if needed.
Cheap pepcid 40 mg visa
Plasmacytoid lymphocytes and plasma cells contain abundant intracellular Ig, which usually is monotypic IgM without IgD and can be detected using paraffin immunoperoxidase reactions symptoms 24 safe pepcid 20mg. These lymphomas are usually widespread at diagnosis with generalized adenopathy and extensive bone marrow involvement. They may involve extranodal sites, such as the Waldeyer ring, or present as lymphomatous polyposis of the lower gastrointestinal tract. Mitotic activity is often brisk, and large lymphocytes are usually few in number except in the pleomorphic form of the blastoid variant, in which they predominate. There is now molecular genetic evidence that at least some blastoid variants of mantle cell lymphoma are morphologic transformations of typical mantle cell lymphoma. Deletion of 13q is the most frequent abnormality and correlates with a stable clinical course in older patients. A: Low magnification shows diffuse architectural effacement, which, on higher magnification in (B), is composed of sheets of small irregular lymphocytes with few large cells. Almost one-third of patients with mantle cell lymphoma have somatic mutation of their Ig heavy chain genes. Clinically, these lymphomas appear more aggressive than other marginal zone lymphomas. Microscopically, the most striking feature is a nodular infiltrate centered on the preexisting white pulp lymphoid follicles. The inner central zone of small lymphocytes resembles normal mantle zone cells with scant cytoplasm and small irregular nuclei, clumped chromatin, and indistinct nucleoli. The lymphocytes occupying the marginal zone appear similar to normal splenic marginal zone lymphocytes. These have welldefined clear cytoplasm and round/oval nuclei with a more open chromatin pattern and indistinct nucleoli. Variable numbers of large lymphocytes with prominent nucleoli are also present in the marginal zone. Occasionally, plasmacytic differentiation within the marginal zone or in the center of the nodules can be observed. Bone marrow involvement is nodular or interstitial and frequently intrasinusoidal. On molecular genetic studies, approximately one-half of cases show somatic mutation, and one-half have unmutated Ig genes. Recently, a primary low-grade B-cell splenic lymphoma showing morphologic features distinct from splenic marginal lymphoma has been described. This entity is often referred to as "splenic diffuse red pulp small B-cell lymphoma. The infectious process not only creates the microenvironment for development of the tumor but also the microenvironment necessary to sustain the tumor progression. For this reason, many of the cases have been mistakenly diagnosed as pseudo-lymphomas before the application of clonality and genetic studies. When they disseminate they tend to go to other mucosal sites, a phenomenon thought to be a result of homing programming. Characteristic are the centrocyte-like cells, small to medium-sized lymphocytes with irregular nuclei. Alternatively, the neoplastic cells may have a monocytoid appearance with abundant pale cytoplasm and distinct cell borders. Variable numbers of plasma cells are frequently present, often adjacent to epithelium. In approximately one-third of cases the plasma cells are part of the neoplastic clone and may show atypical features such as Dutcher bodies. Stomach: extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue. B: Centrocyte-like cells with moderate amounts of clear cytoplasm invade gastric glands, producing lymphoepithelial lesions. Comprising 30% to 40% of all lymphomas, they are the most common lymphoma type in the United States and Europe. The large neoplastic lymphoid cells grow in a purely diffuse pattern and efface the underlying tissue architecture. Tingible body macrophages, apoptotic bodies, mitotic figures, and zones of necrosis and/or fibrosis variably accompany the neoplastic cells. The most common presentation is as a bulky mass of lymph nodes, but up to 40% of cases arise in extranodal sites, including spleen or bone marrow. The pattern of bone marrow involvement may be concordant or discordant-constituted by a lower grade lymphoma. A: On low magnification, a neoplastic large lymphocyte population diffusely effaces lymph node architecture. B: On high magnification, round nuclei, partially clumped chromatin, small nucleoli and modest amounts of pale cytoplasm characterize the tumor cells. They tend to occur in older patients, are more frequent in women than in men, and tend to be disseminated at the time of diagnosis. The fraction of Ki-67+ cells in a tumor is a general indicator of its proliferative rate. Rather, a complex karyotype with genetic imbalances occurs in two-thirds of cases. Small lymphocytes and histiocytes in varying proportions dominate the histologic picture. In contrast, the neoplastic cells are in the minority and are singly distributed without clustering together or forming sheets. Centroblast-like, immunoblast-like, or pleomorphic cytologic features typify the neoplastic cells in most cases. Occasional large neoplastic cells with rounded to lobulated nuclei, delicate chromatin, small nucleoli, and pale cytoplasm are present. The phenotype of both the neoplastic cells and the reacting cell populations usually resolves the differential diagnostic problems. Of patients who present with intraocular involvement, intraparenchymal brain involvement eventually develops in the majority, and about 20% of patients who present with intracerebral disease will develop intraocular involvement. The tumor cells are variably accompanied by a richly vascular fibrous stroma that frequently circumscribes clusters of neoplastic cells. This can be a cause of diagnostic difficulty, because fibrosis itself and/or compression artifact introduced when biopsying a firm mass, can obscure the tumor cells. Some examples are composed of cells resembling centroblasts; others contain a prominent population of immunoblast-like neoplastic cells. A nonneoplastic population of T cells and histiocytes often accompanies, and together with fibrosis can also potentially obscure, the neoplastic cells. The neoplastic cells usually have cytologic features of centroblasts or immunoblasts or a combination of both. Reactive astrocytes, activated microglial cells, and histiocytes complete the histologic picture. Preoperative corticosteroid therapy to reduce intracerebral edema prior to biopsy can cause intralesional necrosis or regression of the neoplasm. Sometimes tumor cell ghosts can be recognized within the necrotic areas suggesting the diagnosis, but in some cases steroid therapy leaves behind only a mixture of small T-lymphocytes and histiocytes or sheets of foamy macrophages. In most cases sufficient sampling, careful microscopic observations, and application of immunohistochemical stains can readily distinguish these two from one another. The most abnormal-appearing neoplastic cells frequently surround the areas of necrosis. Other cases, termed "polymorphous subtype" contain a tumor cell population of large immunoblasts, plasma cells, and cells with transition features between plasma cells and immunoblasts. A: the tumor diffusely effaces tissue architecture and is associated with necrosis (left). The neoplastic cells are medium size and large with hyperchromatic, irregular nuclei. Genetics Insufficient numbers of cases have been studied to comment on recurring genetic abnormalities in these tumors. These lymphomas usually affect children and young adults and often present at extranodal sites.