Buy generic casodex 50mg line
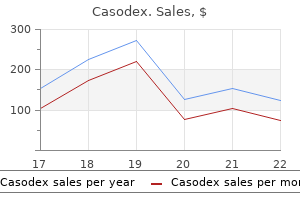
The increase in metabolic rate ranges from about 10 percent in elective surgical operations to 50 percent in multiple trauma and 200 percent in major burns prostate cancer psa scale generic 50mg casodex with visa. The anabolic phase, on the other hand is characterized by protein and fat synthesis and associated with weight gain. Resting energy expenditure is increased after tissue injury, the degree of increase being proportional to the magnitude of trauma. The muscle and liver glycogen, however, cannot continue to supply glucose all the time, as its total store would be exhausted in a day or two. Protein can also be used as an energy source but it cannot be mobilized beyond a certain level. It is important to spare proteins since their excessive breakdown would lead to muscle wasting, ineffective coughing, impaired wound healing and a diminished synthesis of enzymes. Therefore, the calorie distribution of protein to the fuel mixture of the injured is small and the main energy requirement is met from fat. Physiological Basis of Surger y carbohydrate Metabolism After Injury of triglycerides to fatty acids and glycerol. Fatty acids are burnt in the liver Hyperglycemia occurs immediately after injury to supply energy for gluconeogenesis and because glucose is mobilized from stored gly- in the periphery to supply energy directly. In major injuries, the inflammatory cell infiltrate can account for 70 percent of the Protein Metabolism After Injury glucose uptake. In an uninjured person there is equilibrium between a whole body protein synthesis and Fat Metabolism After Injury whole body protein breakdown. After injury Fat is the main energy source in trauma this balance is disturbed with a net protein and starvation. Chapter 8 Endocrine and Metabolic Response to Injur y perfusion from hypotension secondary to hypovolemia or from the administration of nonsteroidal antiinflammatory drugs also worsens oliguria and can lead to acute renal failure. It does not indicate sodium deficiency, as it occurs at a time when total body sodium is elevated. Serum K+ may rise due to cell death, impaired potassium excretion and liberation of potassium by protein catabolism. However, it is more usual to see increased urine potassium excretion which can lead to overall potassium deficit. Acid-base abnormalities: the commonest change is the metabolic alkalosis due to intense reabsorption of sodium in distal tubules of the kidney, accompanied by excretion of K+ and H+ ions. In more severe injuries, a metabolic acidosis supervenes due to poor tissue perfusion and anaerobic metabolism with accumulation of lactic acid. The protein loss occurs primarily from muscle, there being no decrease in the protein content of the liver and the kidneys. Increased cortisol and glucagon and decreased insulin all limit the ability of muscle to take up amino acids. As catabolism of muscle continues, while anabolism is limited by the hormonal changes, there is a net release of amino acids from muscle cells. Alanine is the principal amino acid released from muscle, and is the principal gluconeogenic precursor in the liver. It has been suggested that a cycle similar to the Cori cycle of glucose to lactate to glucose may be achieved through glucose to alanine to glucose. Most of the proteins, which are largely derived from skeletal muscle, are converted to glucose in the liver by the process of gluconeogenesis. The remainder is used by red blood cells and leukocytes, which convert the glucose to lactate and pyruvate. Inflammatory bowel metabolic response which is a stereotyped further hindering excretion of free water disease, Rheumatoid arthritis, Pacreatic can- reaction to any form of injury leading to alterand resulting in lower volumes of high cer (which augments the metabolic response ations in fluid and electrolytes, substrates, and hormones. Infection means invasion of the body by pathogenic organisms, which may be bacte rial, fungal or viral. A pathogenic organism establishes itself in host tissue, multiplies and results in this sue damage, usually due to release of toxic substances. The classification of microor ganisms into pathogenic and nonpatho genic is, however, arbitrary, as pathogenicity depends on an imbalance in the relation ship between the host and the microorgan ism. In a host with reduced body resistance, a less harmful organism may produce severe disease. Conventional pathogens-They cause infec tions in previously healthy individuals and possess high pathogenicity. Conditional pathogens-Cause clinical infec tion only when a predisposing factor is present. Host Defences Surgical infection occurs when the balance between the host resistance and the virulence of the organism is jeopardized. All the local and systemic host defences may be compromised by surgical interven Prevention of Endogenous Infection tion and treatment. Individual boils that are large and painful should be treated by incision and drainage under local or even general anesthetic. Human Sources these include patients with overt clinical infections, those with inapparent or subclini cal infections as well as carriers and excreters of pathogenic organisms. Organisms may be transmitted from one person to another by direct contact, by inhalation, by sexual inter course or transplacentally. Part I General Surgery soUrce of infection Two types of sources are there: (1) Endogenous source of infection, (2) Exogenous source of infection. Peritonitis carbuncle this is a superficial infective gangrene involv ing the subcutaneous tissue by Staphylococcus aureus. Endogenous infections are particularly common after trauma, sur gery and instrumentation and in conditions of lowered local or systemic host defences. The skin and all mucous membranes bear a rich commensal flora and with the excep tion of the skin, this flora is predominantly anaerobic. Bacteroides fragilis (Anaerobes), Site Axilla in female and nape of the neck in male are the commonest sites, others sites are back and the shoulder region. If healing is favorable, the slough separates and the cavity gradually fills up with healthy granulation tissue. Cold abscess - Usually refers to tubercu biotics are given till complete resolution. All sloughs septicemia are removed with gauge swabs or scis It is a condition where organisms not only sors. The apices of the four skin flaps are circulate in the bloodstream, but also prolif cut making, the opening circular and erate therein and produce toxins which cause large. Increased permeability of vessels espe cially capillaries exudation of protein and fibrin formation pyogenic mem brane. Increased vascular permeability out pouring of macrophages and polymorphs release of lysosomal enzymes lique faction of tissue pus formation. Thus, the end result is production of pus which is composed of dead leuckocytes, bac teria and necrotic tissue. The area around the abscess is encircled by fibrin products and is infiltrated with leu kocytes and bacteria. Irritations by deo dorants and excessive sweating have been implicated as precipitating factors. Organisms causing the infection are Staphylococcus aureus, streptococci and a variety of skin commensals. The patient presents with multiple tender swellings under the arm or in the groin, these enlarge and discharge pus. Toxemia is a state in which toxins bacterial the patient feels ill and complains of throb or chemical circulate in the bloodstream and bing pain at the site. Pyemia the signs are those of acute infection Pyemia is a stage of septicemia in which mentioned above, i. Staphylococcus aureus and their toxins are carried in the bloodstream, which initiate Treatment multiple foci of abscesses in various parts of Incision and drainage (I and D), preferably the body.
Purchase casodex with paypal
Underlying lung disease and respiratory muscle wasting from prolonged disuse often complicate weaning mens health 6 pack challenge diet buy 50mg casodex amex. Intact airway reflexes and a cooperative patient are also mandatory prior to completion of the weaning and extubation unless the patient will retain a cuffed tracheostomy tube. Mandatory minute ventilation has also been suggested as an ideal weaning technique, but experience with it is limited. Finally, many institutions use "automated tube compensation" to provide just enough pressure support to compensate for the resistance of breathing through an endotracheal tube. Newer mechanical ventilators have a setting that will automatically adjust gas flows to make this adjustment. The -piece attaches directly to the tracheal tube or tracheostomy tube and has corrugated tubing on the other two limbs. Sufficient gas flow must be given in the proximal limb to prevent the mist from being completely drawn back at the distal limb during inspiration; this ensures that the patient is receiving the desired oxygen concentration. The patient is observed closely during this period; obvious new signs of fatigue, chest retractions, tachypnea, tachycardia, arrhythmias, or hypertension or hypotension should terminate the trial. If the patient can also protect and clear the airway, the tracheal tube can be removed. If the patient has been intubated for a prolonged period or has severe underlying lung disease, sequential -piece trials may be necessary. Improvement in the latter parameter will show as a decrease in venous admixture and an improvement in arterial O2 tension. Constant levels of pressure can be attained only if a highflow (inspiratory) gas source is provided. Progressive reductions in cardiac output are often seen as mean airway pressure and, secondarily, mean intrathoracic pressure rise. Other mechanisms may include leftward displacement of the interventricular septum (interfering with left ventricular filling) because of the increase in pulmonary vascular resistance (increased right ventricular afterload) from overdistention of alveoli, leading to an increase in right ventricular volume. Left ventricular compliance may therefore be reduced; when this occurs, to achieve the same cardiac output may require a higher filling pressure. Circulatory depression is most often associated with end-expiratory pressures greater than 15 cm H2O. E, result of excessive pressure when alveoli are overdistended and pulmonary compliance decreases. By compressing alveolar capillaries, overdistention of normal alveoli can also increase pulmonary vascular resistance and right ventricular afterload. Disruption of alveoli allows air to track interstitially along bronchi into the mediastinum (pneumomediastinum). The latter is best accomplished with an adequate cardiac output and hemoglobin concentration. Ideally, mixed venous oxygen tensions or the arteriovenous oxygen content difference should be followed. Volume infusion or inotropic support may be necessary and should be guided by hemodynamic measurements. Many clinicians favor reducing the inspired oxygen concentration to 50% or less because of the potentially adverse effect of greater oxygen concentrations on the lung. An aerosol mist is a gas or gas mixture containing a suspension of liquid particles. Aerosolized water may be administered to loosen inspissated secretions and facilitate their removal from the tracheobronchial tree. Aerosol mists are also used to administer bronchodilators, mucolytic agents, or vasoconstrictors (metered-dose inhalers are preferred for administration of bronchodilators). A normal cough requires an adequate inspiratory capacity, an intact glottis, and adequate muscle strength (abdominal muscles and diaphragm). Aerosol mists with or without bronchodilators may induce cough as well as loosen secretions. Instillation of hypertonic saline has been used as a mucolytic and to induce cough. Additional effective measures include chest percussion or vibration therapy and postural drainage of the various lung lobes. When thick and copious secretions are associated with obvious atelectasis and hypoxemia, more aggressive measures may be indicated. These include suctioning the spontaneously breathing patient via a nasopharyngeal catheter or flexible bronchoscope, or performing the same two maneuvers through a tracheal tube. Respiratory Failure Respiratory failure may be defined as impairment of normal gas exchange severe enough to require acute therapeutic intervention. Fluid within the interstitial space and alveoli is collectively referred to as extravascular lung water. Albumin is particularly important in this context because water loss to the interstitium will increase when albumin is also lost to the interstitium. A with a value of 1 implies that the endothelium is completely impermeable to albumin, whereas a value of 0 indicates free passage of albumin and other particles/molecules. The pulmonary endothelium normally is partially permeable to albumin, such that interstitial albumin concentration is approximately one half that of plasma; therefore, under normal conditions i must be about 14 mm Hg (one half that of plasma). Pulmonary capillary hydrostatic pressure is dependent on vertical height in the lung (gravity) and normally varies from 0 to 15 mm Hg (average, 7 mm Hg). Few patients with respiratory failure display a pattern as "pure" as these extreme examples. Treatment Regardless of the disorder, the treatment of respiratory failure is primarily supportive while the reversible components of underlying disease are treated. A net movement of water from the interstitium into alveoli occurs only when the normally negative Pi becomes positive (relative to atmospheric pressure). Pulmonary edema is often divided into four stages: Stage I: Only interstitial pulmonary edema is present. The chest radiograph reveals increased interstitial markings and peribronchial cuffing. Blood flow through the capillaries of flooded alveoli results in a large increase in intrapulmonary shunting. Hypoxemia and hypocapnia (the latter due to dyspnea and hyperventilation) are characteristic. Gas exchange is compromised due to both shunting and airway obstruction, leading to progressive hypercapnia and severe hypoxemia. Fluid due to hemodynamic edema has a low protein content, whereas that due to permeability edema has a high protein content. Less common causes of edema include prolonged severe airway obstruction (negative pressure pulmonary edema), sudden reexpansion of a collapsed lung, high altitude, pulmonary lymphatic obstruction, and severe head injury, although the same mechanisms (ie, changes in hemodynamic parameters or capillary permeability) also account for these diagnoses. Pulmonary edema associated with airway obstruction may result from an increase in the transmural pressure across pulmonary capillaries associated with a markedly negative interstitial hydrostatic pressure.
50mg casodex
Calcitonin is a polypeptide hormone that is secreted by parafollicular cells in the thyroid gland androgen hormone inhibitors order casodex paypal. Patients with cancer can present with hypercalcemia whether or not bone metastases are present. Increased gastrointestinal absorption of calcium can lead to hypercalcemia in patients with the milk-alkali syndrome (marked increase in calcium intake), hypervitaminosis D, or granulomatous diseases (enhanced sensitivity to vitamin D). Clinical Manifestations of Hypercalcemia Hypercalcemia often produces anorexia, nausea, vomiting, weakness, and polyuria. Pancreatitis, peptic ulcer disease, and kidney failure may also complicate hypercalcemia. Anesthetic Considerations Significant hypercalcemia is a medical emergency and should be corrected, if possible, before administration of any anesthetic. If surgery must be performed, saline diuresis should be continued intraoperatively with care to avoid hypovolemia; appropriate goal-directed hemodynamic and fluid management therapy (see Chapter 51) should be utilized, especially for patients with cardiac impairment. Serial measurements of [K+] and [Mg2+] are helpful in detecting iatrogenic hypokalemia and hypomagnesemia. Premature diuretic therapy prior to rehydration may aggravate the hypercalcemia by exacerbating volume depletion. Renal loss of potassium and magnesium usually occurs during diuresis, and laboratory monitoring and intravenous replacement as necessary should be performed. Although hydration and diuresis may remove the potential risk of cardiovascular and neurological complications of hypercalcemia, the serum calcium level usually remains elevated above normal. Additional therapy with a bisphosphonate or calcitonin may be required to further lower the serum calcium level. Severe hypercalcemia (>15 mg/dL) usually requires additional therapy after saline hydration and furosemide calciuresis. Intravenous administration of pamidronate (Aredia) or etidronate (Didronel) is often utilized in this setting. Dialysis is very effective in correcting severe hypercalcemia and may be necessary in the presence of kidney or heart failure. It is necessary to look for the underlying etiology and direct appropriate treatment toward the cause of the hypercalcemia once the initial threat of hypercalcemia has been removed. Approximately 90% of all hypercalcemia is due to either malignancy or hyperparathyroidism. When direct measurements of plasma [Ca2+] are not available, the total calcium concentration must be corrected for decreases in plasma albumin concentration (see above). Hypoparathyroidism may be surgical, idiopathic, part of multiple endocrine defects (most often with adrenal insufficiency), or associated with hypomagnesemia. Hyperphosphatemia (see below) is also a relatively common cause of hypocalcemia, particularly in patients with chronic renal failure. Hypocalcemia due to vitamin D deficiency may be the result of a markedly reduced intake (nutritional), vitamin D malabsorption, or abnormal vitamin D metabolism. Chelation of calcium ions with the citrate ions in blood preservatives is an important cause of perioperative hypocalcemia in transfused patients; similar transient decreases in [Ca2+] are also possible following rapid infusions of large volumes of albumin. Hypocalcemia following acute pancreatitis is thought to be due to precipitation of calcium with fats (soaps) following the release of lipolytic enzymes and fat necrosis; hypocalcemia following fat embolism may have a similar basis. Precipitation of calcium (in injured muscle) may also be seen following rhabdomyolysis. Transient hypocalcemia may be seen following heparin, protamine, or glucagon administration. Serial ionized calcium levels should be monitored intraoperatively in patients with a history of hypocalcemia. Intravenous calcium may be necessary following rapid transfusions of citrated blood products or large volumes of albumin solutions. Potentiation of the negative inotropic effects of barbiturates and volatile anesthetics should be expected. Decreased cardiac contractility may result in heart failure, hypotension, Disorders of Phosphorus Balance Phosphorus is an important intracellular constituent. The kidneys are the major route for phosphorus excretion and are responsible for regulating total body phosphorus content. Clinical Manifestations of Hyperphosphatemia Although hyperphosphatemia itself does not appear to be directly responsible for any functional disturbances, its secondary effect on plasma [Ca2+] can be important. Marked hyperphosphatemia is thought to lower plasma [Ca2+] by precipitation and deposition of calcium phosphate in bone and soft tissues. Treatment of Hyperphosphatemia Hyperphosphatemia is generally treated with phosphate-binding antacids such as aluminum hydroxide or aluminum carbonate. Anesthetic Considerations Although specific interactions between hyperphosphatemia and anesthesia are generally not described, renal function should be carefully evaluated. Plasma Phosphorus Concentration Plasma phosphorus exists in both organic and inorganic forms. Of the inorganic phosphorus fraction, 80% is filterable in the kidneys and 20% is protein bound. By convention, plasma phosphorus is measured as milligrams of elemental phosphorus. Plasma phosphorus concentration is usually measured during fasting, because a recent carbohydrate intake transiently decreases the plasma phosphorus concentration. Hypophosphatemia increases vitamin D production, whereas hyperphosphatemia depresses it. The latter plays an important role in the genesis of secondary hyperparathyroidism in patients with chronic kidney failure (see Chapter 30). Intercompartmental shifts of phosphorus can occur during alkalosis and following carbohydrate ingestion or insulin administration. Large doses of aluminum or magnesium-containing antacids, severe burns, inadequate phosphorus supplementation during hyperalimentation, diabetic ketoacidosis, alcohol withdrawal, and prolonged respiratory alkalosis can all produce a negative phosphorus balance and lead to severe hypophosphatemia (<0. In contrast to respiratory alkalosis, metabolic alkalosis rarely leads to severe hypophosphatemia. Treatment of Hypophosphatemia Oral phosphorus replacement is generally preferable to parenteral replacement because of the increased risk of phosphate precipitation with calcium, resulting in hypocalcemia, and also because of the increased risks of hyperphosphatemia, hypomagnesemia, and hypotension. Accordingly, intravenous replacement therapy is usually reserved for instances of symptomatic hypophosphatemia and extremely low phosphate levels (<0. In situations where oral phosphate replacement is utilized, vitamin D is required for intestinal phosphate absorption. Magnesium impairs the calcium-mediated presynaptic release of acetylcholine and may also decrease motor end-plate sensitivity to acetylcholine and alter myocyte membrane potential. In addition to the treatment of magnesium deficiency, administration of magnesium is utilized therapeutically for preeclampsia and eclampsia, torsades de pointes and digoxin-induced cardiac tachyarrhythmias, and status asthmaticus. Factors known to increase renal excretion include hypermagnesemia, acute volume expansion, hyperaldosteronism, hypercalcemia, ketoacidosis, diuretics, phosphate depletion, and alcohol ingestion. Anesthetic Considerations Anesthetic management of patients with hypophosphatemia requires familiarity with its complications (see above). Hyperglycemia and respiratory alkalosis should be avoided to prevent further decreases in plasma phosphorus concentration. Some patients with severe hypophosphatemia may require mechanical ventilation postoperatively because of muscle weakness. Plasma Magnesium Concentration Disorders of Magnesium Balance Magnesium is an important intracellular cation that functions as a cofactor in many enzyme pathways. Suggested mechanisms of action include altering central nervous system neurotransmitter Plasma [Mg2+] is closely regulated between 1. Magnesium sulfate therapy for preeclampsia and eclampsia can cause hypermagnesemia in the mother as well as in the fetus. Treatment of Hypermagnesemia With relatively mild hypermagnesemia, all that is usually necessary is to discontinue source(s) of magnesium intake (most often antacids).

Buy discount casodex on-line
In: McLaurin R prostate cancer genetic testing generic casodex 50 mg otc, Schut L, Venes J, Epstein F (eds) Pediatric neurosurgery: surgery of the developing nervous system. Antidor, Moscow (in Russian) Korshunov A et al (2004) the histologic grade is a main prognostic factor for patients with intracranial ependymomas treated in the micronerosurgical era. According to data of various authors, the incidence of meningioma is from 13 to 20% of all primary brain tumours (Russell 1989; Orrison 2000), occupying first place in the group of the tumours originated from meninges (Sze 1993). Our data included about 5,000 patients with meningioma of a various locations, which, according to the statistics of the Moscow Neurosurgical Institute makes up about 23. Usually meningioma is diagnosed in adults, and the incidence peak is between 40 and 60 years old, and women are affected more frequently; the ratio of men to women is from 1:2 to 1:4 (according to various data) (Buetow et al. Unlike among adults, malignant and giant forms prevail among children (Deen 1982). Any intracranial meningothelial cell regardless of its concrete location, diploic bone layer, the vertebral canal, or an ectopical location, may potentially be the place for meningioma development. In rare cases, the tu- mour may grow from fibroblasts of the dura matter, arachnoid membrane around cranial nerves, and vascular plexus. In many cases, meningioma has no clinical symptoms, and it may be an accidental finding in radiological examination or autopsy (Konovalov 1997). Epileptic seizures, movement, and sensitivity disorders are typical for convex or parasagittal tumours. Visual field changes are the feature of meningioma of sphenoid bone wings, whereas cavernous sinus tumours, as a rule, cause involvement of the third to sixth cranial nerves. Tumours of the second cranial nerve sheath in the orbit or in the optic nerve canal leads to visual loss up to blindness on the lesion side. Neoplasm of the anterior cranial fossa (meningiomas of olfactory fossa) may reach very large sizes due to the mainly asymptomatic clinical course, with the exception of anosmia. Meningioma consistency varies from soft up to cartilaginous density, depending on expressiveness of the fibrous tissue and the presence of calcifications. Tumour stroma may contain small haemorrhagic and necrotic components, cystic, and xanthomatous changes (Burger 1991). As a rule, a reactive thickening of the dura matter is observed around the meningioma. Morphological examination were mainly carried for creation of a more simplified classification, with the use of markers for detection of proliferative activity, signs of aggressive growth, and features of malignancy (Kleihues et al. According to the Moscow Neurosurgical Institute statistical data, the inci- 720 Chapter 8. Sagittal T1-weighted imaging (a) and axial T2-weighted imaging (b) reveals a mass lesion that envelops the optic nerve. The borders of tumour are clearly visible on a background of hyperintensive signal from fat in the orbit. The tumour is mainly supplied from the branches of hypertrophied ophthalmic artery. Histologically, the arrangement of cells with moderate nuclei polymorphism and absence of mitosis and necrosis foci is typical for benign forms. These meningiomas are included in this group: fibroblastic, meningotheliomatous, secretory, transitional, and psammomatous. Atypical meningiomas (more often mixed meningotheliomatous structure) are characterised by marked polymorphism of cells and nuclei, the presence of necrosis foci, and mitotic figures. The histological characteristic of malignant meningiomas includes the following features: dense cell arrangement, multiple mitotic figures, and necrosis foci. According to the Institute data, based on location men- ingiomas are divided into supra- and subtentorial. Rarely are tumours of intraventricular location, pineal area, sheaths of the optic nerves (3%), and craniospinal areas observed. Extracranial meningiomas (paranasal sinuses of nose and cranial vault bones) made up 1%. Benign forms may have a more developed vascular net, whereas ones more malignant have less developed nets. In the literature, the angiographic semiotics of meningioma are described comprehensively and in detail. The meningeal arteries such as the middle meningeal artery belong to the first and the most frequent type. Below is a general table of the most frequently supplying meningeal arteries, depending on the primary location of meningioma (Table 8. It is necessary to note that large, long-growing meningiomas with infiltrative growth, or anaplastic meningiomas may be additionally supplied from pial branches of intracranial arteries. Peri- focal oedema around even the small meningiomas is often combined with this factor (Ildan 1999). On angiograms, such tumours are characterised by marked early contrast accumulation that remains even during a venous angiography phase, i. In a quarter of cases, meningiomas poorly accumulate contrast substance, or do not accumulate it at all, and in these cases, they are isodensive. The vascular net of tumour remains in late capillary phase (f) Tumours of the Meninges 731. Up to 25% of all meningiomas contain calcifications in their structure, which may be solitary and multiple, point-like, and large, and in exceptional situations, the entire tumour may be calcified. Although the presence of large haemorrhages, necrotic parts, and cyst formation (Konovalov 1997; Osborn 2004) are not typical for meningioma, nevertheless, on the periphery the unevenly dilated subarachnoid spaces with signs of degenerative changes of the surrounding parenchyma may be observed, and adjoining cysts (8%) may sometimes reach large sizes. In a third of all cases, there is a hypodensive perifocal zone due to brain tissue oedema. The latter is often combined with anaplastic changes in the neoplasm structure and the pial type of tumour blood supply. The latter changes are the most frequently diagnosed in cases of basal location of meningioma. It is believed that a meningioma may originate from ectopic arachnoid cells in a diploic layer of the cranial vault and the bones of skull base, and the whole tumour has epidural location; it infiltrates and destroys bone. These are so called hyperostotic meningiomas, which are characterised by the combination of widespread infiltration of skull bones and sharp thickening of these bones with the presence of the flat tumour component, the volume of which may be sometimes minimal. Invasive growth of meningioma in the bone tissue sometimes is accompanied by bone destruction or spicule-like changes. There are spicule-like changes in the bone structures method of choice for radiological diagnostics of such tumours. Hyperpneumatisation of the sphenoid sinus is also one of the typical attributes of the meningioma in an area of a tuber of the sella turcica and the anterior clinoid process. In this case, the hyperostosis in an area of meningioma matrix as well as hyperpneumatisation of the neighbouring departments of the sinus may be observed.

Buy genuine casodex online
They commonly infect the nails leading to especially postoperatively prostate cancer hifu purchase casodex uk, the onset of fever thickening and distortion (onychogrypho or an elevated white blood cell count may sis) which itself can lead to mechanical signal an infectious process. The most common type of nosocomial infection is Madura foot caused by Nocardia madurae, a filamentous organism, similar to infections are as follows. Altemeier demonstrated that the risk of wound infection varies according to the formula: Dose of bacterial contamination X Virulence divided by resistance of host Part I General Surgery Treatment Consists of rest, elevation and antibiotics for secondary infection and protracted treatment with dapsone or similar agents. Ultimately if the infections persists and heads to disability then amputation can be considered. Other types of major infections include tuberculosis, and infestation such as guinea worm. Surgical Infection and Burn Urinary tract infection Clinical features Include pain, rigidity and absence of bowel sounds. Clinical Features Fever usually begins or persists after the 4th postoperative day. Part I General Surgery Treatment the basic treatment of wound infection is to open the wound and allowed to drain. Antibiotics are stopped as soon as local inflammation and systemic signs of infec tion have resolved. Intraabdominal abscess-Intraabdominal abscess can arise in the following groups of Treatment patients. Asymptomatic bacteriuria: Treatment with these patients have a 6 to 10 percent appropriate antibiotic for one day after cath risk of developing intraabdominal eter removal. Postoperative intraabdominal infection may Treatment present in one of the two ways viz. This is a line of treatment in these patients, with Appropriate antibiotics and supportive care. Include localized tenderness, intermittent fever and absent bowel sounds, 5 to 10 days after operation. In some instances, abscess is palpable abdominally or rectally (pelvic collection). A 3rd generation cephalosporin above or in combination with tazobactam and metro nidazole 500 mg 12 hourly have been useful. In immunocompromised patients, 750 mg cip rofloxacin 12 hourly, or third generation All intravenous access devices like cannulas, cephalosporn is indicated. Once the infected device is removed, the A variety of agents can infect liver including infection generally resolves, often without bacteria, viruses, protozoa and helminths. Prevention of these infections can only Liver Abscess be achieved by scrupulous attention to anti See also Liver (36) in section 9. Prophylactic antibiotics are no substitute the most common aerobic organisms are E. It is seen are more likely to rupture intraperitoneally in postoperative patients who have received whereas left lobe lesions rupture into the antibiotics (cephalosporins, ampicillin, etc. The primary symptoms are fever, chills, the infection develops because the antibiot anorexia, weight loss, abdominal pain and ics alter the normal gut flora, allowing the nausea. Because of the anaerobic nature of the disease 500 mg metronidazole 12 hourly is the treatment of choice. Part I General Surgery Peritonitis Infective peritonitis may be primary or much more common secondary to some intra abdominal process. Primary Peritonitis Treatment Consists of withdrawing current antibiotics and giving oral vancomycin or metronidazole to which C. Infections include acute cholecystitis, cholan gitis, empyema and chronic cholecystitis. Uncomplicated gallstones are associated with a 30 to 50 percent incidence of positive bile cultures. Pancreatic abscess develops within necrotic into the peritoneal cavity cannot usually pancreatic tissue and requires drainage. Therapy-Antibiotics include a 3rd genera tion cephalosporin alone or in combination Secondary Peritonitis with tazobactam. May occur following a variety of pathological conditions such as peptic ulcer perforation, acute appendicitis pancreatitis, bowel ischemia due to strangu Acute appendicitis requires appendectomy. Therapeutic antibiotics are infection must be closed or exteriorised and indicated if the disease has progressed to the abdominal cavity must be cleaned of 71 Section 2 Surgical Infection and Burn nosocomial pneumonias as well as in severe soft tissue and intraabdominal infections. Clinical Features Similar to those of chronic pneumonia like fever, cough, leukocytosis, pleuritic pain and sputum production. Betalactams(likepeni facultative an aerobic streptococci: cillin, ampicillin, cephalosporins), vanco virulence is determined by the ability to mycin, aminoglycosides, etc. Part I General Surgery carbapenems They are semisynthetic lactams and include imipenem and meropenem. Cefotaxime in com bination with metronidazole will cover most pathogenic bacteria. Most Gram Negative Bacilli mediastinitis cephalosporins They are chemically related to penicillins. The various cephalosporins with their activity and use are given below in Table 9. Surgical Infections Quinolones Ciprofloxacin, norfloxacin, ofloxacin and levofloxacin are oral broad spectrum anti biotics related structurally to nalidixic acid. Major use is in anaerobic bacterial infections, Prophylactic Use of antibiotics also used prophylactically in colonic surgery. It Ever since antibiotics become available they is the treatment of choice for amebiasis, giardia have been used to prevent infection in surgi sis and infection with Trichomonas vaginalis. Part I General Surgery 74 Chapter 10 Burns Systemic effects of burn Treatment Other types of burn injury Complications of burn injury Post burn contracture Definition Classification of Burns Pathophysiology Definition Estimation of the extent of burn - It is calculated by the rule of 9, also called the Rule of Wallace. A burn injury is a coagulative type of necro Patientsownhandrepresents1percentof sis of varying depth of skin and deeper according to severity tissues. ClassifiCation of burns percent, each superior extremity 9 perFull thickness or deep burn <2 percent. Deep or Full thickness burn 3rd degree-It involves the epidermis as well as full thickness of dermis. Sepsis - Eschar of burn wound acts as a By Detecting Physical Changes like good culture media for bacterial growth.

Thyme Essential Oil (Thyme). Casodex.
- Dosing considerations for Thyme.
- What is Thyme?
- Are there safety concerns?
- Are there any interactions with medications?
- Bronchitis, in combination with cowslip; treating hair loss (alopecia areata) when combined with other herbs; improving movement disorders in children when used with other medicines; colic; ear infections; swelling (inflammation) of the tonsils; preventing bedwetting; sore throat; bad breath; bronchitis; and swelling (inflammation) of the lungs and mouth.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96799
Order casodex paypal
Repetitive coughing ("bucking") and straining can have adverse hemodynamic effects prostate cancer ke gharelu upchar in hindi purchase casodex toronto, can interfere with gas exchange, and may predispose to pulmonary barotrauma and self-inflicted injury. Commonly used sedatives include opioids (morphine or fentanyl), benzodiazepines (usually midazolam), propofol, and dexmedetomidine. These agents may be used alone or in combination and are often administered by continuous infusion. Nondepolarizing paralytic agents are used in combination with sedation when sedation alone and all other means to ventilate the patient have failed. Initial Ventilator Settings Depending on the type of pulmonary failure, mechanical ventilation is used to provide either partial or full ventilatory support. High airway pressures that overdistend alveoli (transalveolar pressure >35 cm H2O) have been shown experimentally to promote lung injury. Direct intraarterial pressure monitoring also allows frequent sampling of arterial blood for respiratory gas analysis (both a convenience and a disadvantage, given the large number of unnecessary laboratory tests that are often performed on patients with critical illness). An indwelling urinary catheter will lead to an increased risk of urinary tract infections and should be avoided when possible, but it is helpful for monitoring urinary output. Central venous (and rarely pulmonary artery) pressure monitoring are used in hemodynamically unstable patients. Frequent chest radiographs are commonly obtained to confirm tracheal tube and central venous catheter positions, evaluate for evidence of pulmonary barotrauma or pulmonary disease, and determine whether there are signs of pulmonary edema. Monitoring these parameters not only allows optimal adjustment of ventilator settings but helps detect problems with the tracheal tube, breathing circuit, and ventilator. An abrupt increase in peak inflation pressure together with sudden hypotension strongly suggests a pneumothorax. Discontinuing Mechanical Ventilation There are two phases to discontinuing mechanical ventilation. In the first, "readiness testing," so-called weaning parameters and other subjective and objective assessments are used to determine whether the patient can sustain progressive withdrawal of mechanical ventilator support. The second phase, "weaning" or "liberation," describes the way in which mechanical support is removed. Readiness testing should include determining whether the process that necessitated mechanical ventilation has been reversed or controlled. Neurogenic pulmonary edema appears to be related to a marked increase in sympathetic tone, which causes severe pulmonary hypertension. Increased Transmural Pressure Pulmonary Edema ("Cardiogenic" Pulmonary Edema) Significantly increased Pc can increase extravascular lung water and result in pulmonary edema. As can be seen from the Starling equation, a decrease in c may accentuate the effects of any increase in Pc. Two major mechanisms increase Pc; namely, pulmonary venous hypertension and a markedly increased pulmonary blood flow. Any elevation of pulmonary venous pressure is transmitted passively backward to the pulmonary capillaries and secondarily increases Pc. Pulmonary venous hypertension usually results from left ventricular failure, mitral stenosis, or left atrial obstruction. Increases in pulmonary blood flow that exceed the capacity of the pulmonary vasculature will also raise Pc. Marked increases in pulmonary blood flow can be the result of large left-to-right cardiac or peripheral shunts, hypervolemia (fluid overload), or extremes of anemia or exercise. Generally, this includes measures to improve left ventricular function, correct fluid overload with diuretics, or reduce pulmonary blood flow. By reducing preload, pulmonary congestion is relieved; by reducing afterload, cardiac output may be improved. Positive airway pressure therapy is also a useful adjunct for improving oxygenation. When pulmonary edema is a consequence of acute coronary ischemia and left ventricular failure, intraaortic balloon counterpulsation or other assist devices may be used. Regardless of the type of injury, the lung responds to the ensuing inflammatory response in a similar fashion. The released secondary mediators increase pulmonary capillary permeability, induce pulmonary vasoconstriction, and alter vascular reactivity such that hypoxic pulmonary vasoconstriction is abolished. The lung is often affected in a nonhomogeneous pattern, although dependent areas tend to be most affected. Pulmonary hypertension and low or normal left ventricular filling pressures are characteristic hemodynamic findings. The protective effect of plasma oncotic pressure is lost as increased amounts of albumin "leak" into the pulmonary interstitium; normal-or even low-capillary hydrostatic pressures are unopposed and result in transudation of fluid into the lungs. Treatment In addition to intensive respiratory care, treatment should be directed at reversible processes such as sepsis or hypotension. These three techniques improve oxygenation in many patients with acute lung injury, but they are not risk free and they have not been associated with an improvement in survival. Among the most common serious complications are sepsis, renal failure, and gastrointestinal hemorrhage. Nosocomial pneumonia is particularly common in patients with a protracted course and is often difficult to diagnose; antibiotics are generally indicated when there is a high index of suspicion (fever, purulent secretions, leukocytosis, and change in chest radiograph). Protected specimen brushings and bronchoalveolar lavage sampling via a flexible bronchoscope may be useful. Breach of mucocutaneous barriers by various catheters, malnutrition, and altered host immunity contribute to a frequent incidence of infection. Kidney failure may result from various combinations of volume depletion, sepsis, or nephrotoxins. Prophylaxis for gastrointestinal hemorrhage with sucralfate, antacids, H2 blockers, or proton pump inhibitors is recommended. Near-drowning, with or without aspiration, is suffocation while submerged with (at least temporary) survival. Survival depends on the intensity and duration of the hypoxia and on the water temperature. Pathophysiology Both drowning and near-drowning can occur whether or not inhalation (aspiration) of water occurs. If water does not enter the airways, the patient primarily suffers from asphyxia; however, if the patient inhales water, marked intrapulmonary shunting also takes place. Ninety percent of drowning patients aspirate fluid: fresh water, seawater, brackish water, or other fluids. Although the amount of liquid aspirated is generally small, marked ventilation/perfusion mismatching can result from fluids in the airways and alveoli, reflex bronchospasm, and loss of pulmonary surfactant. Aspiration of gastric contents can also complicate drowning before or after loss of consciousness or during resuscitation. The hypotonic water aspirated following fresh water drowning is rapidly absorbed by the pulmonary circulation; water cannot usually be recovered from the airways. If a significant amount is absorbed (>800 mL in a 70-kg adult), transient hemodilution, hyponatremia, and even hemolysis may occur. In contrast, aspiration of salt water, which is hypertonic, draws out water from the pulmonary circulation into the alveoli, flooding them. Thus, hemoconcentration and hypernatremia may occasionally occur following saltwater drowning. Hypermagnesemia and hypercalcemia have also been reported following near-drowning in salt water.
Purchase 50 mg casodex fast delivery
Techniques for application of deep heat include ultrasound as well as shortwave and microwave diathermy prostate knotweed control buy casodex 50 mg with visa. Application may take the form of cold packs, ice massage, or vapocoolant sprays (ethyl chloride or fluoromethane). McKenzie exercises are particularly helpful for patients with lumbar disc displacement. The efficacy of previous physical therapy techniques should be assessed, and the appropriateness of current physical therapy sessions and of the home exercise program should also be evaluated. By facilitating increased range of motion and providing constant resistance, aquatherapy may be particularly helpful for patients who may not be able to tolerate other forms of therapy. Guastella V, Mick G, Soriano C, et al: A prospective study of neuropathic pain induced by thoracotomy: Incidence, clinical description and diagnosis. Acupuncture patients with chronic pain, particularly that associated with chronic musculoskeletal disorders and headaches. The technique involves insertion of needles into discrete anatomically defined points, called meridians. Stimulation of the needle after insertion takes the form of twirling or of application of a mild electrical current. Insertion points appear to be unrelated to the conventional anatomy of the nervous system. Although the scientific literature concerning the mechanism of action and role of acupuncture in pain management is controversial, some studies suggest that acupuncture stimulates the release of endogenous opioids, as its effects can be antagonized by naloxone. Chou R, Qaseem A, Snow V, et al: Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Pluijms W, Huygen F, Cheng J, et al: Evidence-based interventional pain medicine according to clinical diagnoses. In major open abdominal and thoracic procedures, thoracic epidural blockade with local anesthetic provides excellent analgesia, facilitates mobilization and physical therapy, and decreases the incidence and severity of ileus. The magnitude of the surgical stress response is related to the intensity of the surgical stimulus, can be amplified by other factors, including hypothermia and psychological stress, and can be moderated by perioperative interventions, including deeper planes of general anesthesia, neural blockade, and reduction in the degree of surgical invasiveness. Neuraxial blockade of nociceptive stimuli by epidural and spinal local anesthetics has been shown to blunt the metabolic and neuroendocrine stress response to 2 By sparing opioid use and minimizing the incidence of systemic opioid-related side effects, epidural analgesia facilitates earlier mobilization and earlier resumption of oral nutrition, expediting exercise activity and attenuating loss of body mass. Continuous peripheral nerve blocks with local anesthetics block afferent nociceptive pathways and are an excellent way to reduce the incidence of opioid-related side effects and facilitate recovery. Multimodal analgesia combines different classes of medications, having different (multimodal) pharmacological mechanisms of action and additive or synergistic effects, to control multiple perioperative pathophysiological factors that lead to postoperative pain and its sequelae. Nasogastric tubes should be discouraged whenever possible or used for only a very short period of time, even in gastric and hepatic surgery. Multimodal analgesia and nonopioid analgesia techniques shorten the duration of postoperative ileus. Evolution of Enhanced Recovery Programs Despite increasing numbers of surgical patients who present with complex surgical problems and numerous medical comorbidities, major advances in surgical and anesthetic management have progressively decreased perioperative mortality and morbidity. Further improvement in perioperative outcomes, highlighted by accelerated postoperative convalescence and decreasing occurrence of perioperative complications, will depend on continued evolution of an integrated, multidisciplinary team approach to perioperative care that requires adjustments in multiple aspects of care, including surgical and anesthetic techniques, nursing care, physiotherapy, and nutrition support. The goal is to combine individual evidence-based elements of perioperative care, each of which may have modest benefits when used in isolation, into a tightly coordinated effort that has a synergistic, beneficial effect on surgical outcomes. Although many publications in the surgical literature have highlighted the positive impact of such programs on surgical outcomes, reports documenting the role of anesthesia and analgesia in these programs are few. Little research has been undertaken to define the process of postoperative recovery, and few outcome measures are currently available to confirm that postoperative recovery has been accomplished for a given surgical disease. It is logical to assume that more effective anesthetic interventions will reduce pain, facilitate earlier postoperative mobilization, and allow earlier resumption of oral feeding. In this context, the role of the anesthesia provider must evolve from merely providing satisfactory anesthetic conditions throughout the operation to a focus on enhancing overall perioperative care through techniques that shorten postoperative convalescence and reduce the likelihood of perioperative complications. In endeavoring to do so, the anesthesiologist must become a perioperative physician and an active participant in the surgical team. The incidence of persistent postsurgical pain may exceed 30% after some operations, especially amputations, thoracotomy, mastectomy, and inguinal herniorrhaphy. Well-designed printed materials, such as procedure-specific booklets can be given to patients and families with the advice to keep them at the bedside and utilize them during the hospitalization. Preoperative Risk Assessment & Optimization of Functional Status Identification of patients at risk for intraoperative and postoperative complications, along with preoperative efforts focusing on any comorbidities, can improve surgical recovery. Although international guidelines evaluating the risk for developing cardiovascular, respiratory, or metabolic complications have been extensively reviewed and published, little attention has been given to assessment and optimization of preoperative functional and physiological status. Perioperative statins appear to decrease postoperative cardiovascular complications and should not be abruptly discontinued perioperatively. Several procedure-specific scoring systems based on patient comorbidity, type of surgery, and biochemical data are being used to predict postoperative mortality and morbidity. Smoking, drug abuse, and excessive alcohol use are risk factors for the development of postoperative complications, and preoperative and postoperative interventions aimed at modifying these habits can improve surgical recovery. Many psychological and pharmacological strategies are available to help patients stop excessive alcohol consumption and reduce the risk of alcohol withdrawal. Further studies of preoperative oral fluid and carbohydrate administration are needed to elaborate their role in improving shortand long-term perioperative outcomes. Both pneumatic compression devices and anticoagulant medications are now commonly used. Because neuraxial anesthesia techniques are commonly employed for many patients during major abdominal, vascular, thoracic and orthopedic surgery, appropriate timing and administration of antithrombotic agents in these cases is of critical importance in order to avoid the risk of epidural hematoma. International recommendations on the management of anticoagulated patients receiving regional anesthesia have been recently revised and published and are discussed in other chapters. Guidelines for Food & Fluid Intake Preoperative fasting and surgical stress induce insulin resistance. Furthermore, patients who are not allowed to drink fluids after an overnight fast and patients who receive a bowel preparation experience dehydration, which may increase discomfort and cause drowsiness and orthostatic lightheadedness. Although fasting has been advocated as a preoperative strategy to minimize the risk of pulmonary aspiration during induction of anesthesia, this benefit must be weighed against the detrimental aspects of this practice. For instance, research suggests that avoiding preoperative fasting and ensuring adequate hydration and energy supply may moderate postoperative insulin resistance. All international fasting guidelines allow clear fluids up to 2 h prior to induction of anesthesia in patients at low risk for pulmonary aspiration (see Chapter 18). Moreover, postoperative nitrogen loss and the loss of skeletal muscle mass are attenuated. Magnetic resonance imaging studies in healthy volunteers have shown that the residual gastric volume 2 h after 400 mL of oral carbohydrate (12. The safety of this practice has been tested in patients with uncomplicated type 2 diabetes mellitus, none of whom showed evidence of worsened Antibiotic Prophylaxis Appropriate selection and timing of preoperative antibiotic prophylaxis reduces the risk of surgical site infections. Antibiotics should be administered within 1 h before skin incision and, based on their plasma half-life, should be repeated during prolonged surgeries to ensure adequate tissue concentrations. Antibiotic prophylaxis of surgical site infections should be discontinued within 24 h after surgery (current guidelines permit cardiothoracic patients to receive antibiotics for 48 h following surgery). Strategies to Minimize the Surgical Stress Response the surgical stress response is characterized by neuroendocrine, metabolic, and inflammatory changes initiated by the surgical incision and subsequent procedures that can adversely affect organ function and perioperative outcomes, especially in elderly and physiologically compromised patients. The magnitude of the surgical stress response is related to the intensity of the surgical stimulus; can be amplified by other factors, including hypothermia and psychological stress; and can be moderated by perioperative interventions, including deeper planes of general anesthesia, neural blockade, and reduction in the degree of surgical invasiveness. Much recent effort has focused on developing surgical and anesthetic techniques that reduce the surgical stress response, with the goal of lowering the risk of stressrelated organ dysfunction and perioperative complications. A laparoscopic approach is also associated with less morbidity in elderly surgical patients. Minimally Invasive Surgery Laparoscopic procedures are associated with a reduced incidence of surgical complications, especially surgical site infections, compared with the same procedures performed in "open" fashion. Published data highlight the safety of minimally invasive procedures in the hands of adequately trained and experienced surgeons. Laparoscopic cholecystectomy results in shorter length of hospital stay and fewer complications compared with open cholecystectomy, and similar results have been reported for colorectal surgery. Neuraxial blockade of nociceptive stimuli by epidural and spinal local anesthetics has been shown to blunt the metabolic and neuroendocrine stress response to surgery. To be effective, the blockade must be established before incision and continued postoperatively. However, the advantages of neuraxial blockade are not as evident when minimally invasive surgical techniques are used.
Generic 50mg casodex overnight delivery
The tumour has paraventricular location and partly passes to the surface of cortex of the left occipital lobe 424 Chapter 4 prostate zonal anatomy diagram cheap 50mg casodex free shipping. The prognosis after surgical resection is favourable; cases of malignant transformation are not described in the literature. It makes up less than 1% of all primary tumours and about half of all intraventricular mass lesions of a brain in adults (Bigner et al. Now, about 300 observations of these tumours are described in the literature (Ashkan et al. In tumour structure alongside glial cells, they found cellular structures with neuronal differentiation and the presence of axons, microtubules, neurosecretory granules and synaptic vesicles (Hassoun et al. Usually, these tumours are intraventricular, calcified neoplasms in young patients. They are characterised by a certain clinical, radiological and morphological similarity. Clinically, the tumour manifests by an increase of intracranial pressure, visual and mental impairments, and sometimes by endocrine and pyramidal symptoms. Sometimes they reach gigantic sizes; they almost completely fill the ventricular system, obdurating both lateral ventricles and penetrating into the third and even fourth ventricles through the aqueduct of cerebrum and infiltrating the surrounding structures. In cases of vascular net presence, blood supply is mainly conducted from anterior choroid artery, lateral, and medial lenticulostriatal arteries, and rarely from the branches of pericallosal artery or recurrent artery. The dislocation of cerebral arteries and deep-seated brain veins is observed in cases of vascular net absence. In the majority of observations, the tumours are diagnosed when they reach relatively large size. According to our data based on investigations of 76 patients with neurocytoma, in 50% of cases (38 patients) tumour has mixed structure, in 39% tumour is mainly hyperdense, in 4% is hypodense, and in 7% of cases, it is isodense. The dilatation of lateral ventricles due to hydrocephaly is always observed in cases of neurocytoma. In our series of observations, 95% of patients had hydrocephalus of various degrees. The contrast accumulation can be minimal (14%) or altogether absent (Nishio et al. Our study demonstrated that tumour can infiltrate the wall of lateral ventricles in several sites. The hypertrophied lenticulostriatal arteries (b,c) participating in tumour blood supply are demonstrated (double arrows). Cerebral angiography: the abundant vascular net of tumour (d,e) in the projection of lateral ventricles. The blood supply is performed from multiple coiled branches of the pericallosal artery territory and from the thalamoperforating and the posterior choroid arteries (arrows). The drainage (f) from tumour is performed through hypertrophied vein to the internal vein, and then, into the great vein of Galen and straight sinus. The small calcifications (a), the large ones (b) and calcifications of uneven structure (c) Supratentorial Tumours 427. T2-weighted image (a) and T1-weighted images (b,c) without contrast enhancement reveal a tumour of heterogeneous structure with multiple relatively large cysts. T2-weighted image (c) and T1-weighted images before (d) and after (e) contrast enhancement. Arrows indicate a wide area of infiltration of a wall of the left lateral ventricle. The tumour can only metastasize on brain membranes, with formation of supratentorial nodes. The other neoplasms, such as medulloepithelioma, hemispheric neuroblastoma and ganglioneuroblastoma, and ependymoblastoma are observed extremely rarely. As a rule, it is observed in supratentorial paraventricular areas of the lateral ventricles. However, it is believed that their incidence can reach up to 20% of all brain neoplasm in newborns. Ependymoblastoma has features of ependymal differentiation; it is observed rarely, more often in children of up to 5 years. On scans without contrast enhancement, the tumour is usually hyperdense (a solid component) in comparison with brain tissue. Non-homogeneous and moderate contrast accumulation is observed in the majority of cases. Usually, there is a large neoplasm (5 cm) located in white matter close to ventricular system. The tumour is placed in the projection of the fourth ventricle, and multiple metastases in subependymal area and left frontal area are seen 430 Chapter 4. T2-weighted imaging (a,b) and T1-weighted imaging (c) detect a neoplasm of heterogeneous structure with cysts in right posterior frontal area. The tumour spreading is better evaluated on T2-weighted imaging observed in the pineal area, subcortical nodes and in the suprasellar region. Absent or minimal perifocal oedema despite the relatively large size of neoplasm is a distinctive feature of these tumours. Differential diagnosis should be performed for astrocytoma, ependymoma, oligodendroglioma, teratoidrhabdoid tumour and choroid plexus carcinoma. Cysts and haemorrhages are often found in tumour stroma, whereas calcifications are rare. Metastases in brain tissue are detected in a form of linear or nodal sites of contrast accumulation (Lee 2004). In half of cases, they have infratentorial location away from the middle line, usually in the projection of the cerebellopontine corner. In cases of supratentorial location, they are in a brain hemisphere or suprasellar area. Neuroblastoma (metastatic) is a malignant tumour of the sympathetic nervous system. Its primary location is the paravertebral area of inferior thoracic and lumbar departments of the vertebral column. The most typical clinical symptom is the "raccoon-eyes" sign, bilateral periorbital brightening and ecchymosis. In cases of visceral cranium involvement, typical spicule formation (periostitis) in the projections of bone walls of the orbit and wings of sphenoid bone is seen-a "hair-on-end" appear- Supratentorial Tumours 431. T2-weighted image (b) and T1-weighted image (c) reveal a solid neoplasm with multiple small vessels in its stroma in convexity of left frontoparietal area. T2-weighted imaging (a,b) and T1-weighted imaging (c) detect a neoplasm of heterogeneous structure with signs of subacute intratumoral haemorrhage in deep departments of right temporal area ance. Contrast enhancement helps in detection of soft tissue components, with typical intraorbital spreading (Matthay et al. The sequence with suppression of signal from fat should be used to estimate the intraorbital component. The presence of additional metastases in bones of calvarium is not an exception, and they can be diagnosed together with the lesions of the orbital bones. However, during the past two decades, the number of patients with this disease has dramatically increased, according to some data more than threefold, from 0. The quantity of patients under types of drug immunosuppression has grown, and figures include, for example, patients with organ transplants.


