Cheap 50mg revia overnight delivery
Eruptive lingual papillitis is thought to result from a viral infection medications prescribed for anxiety purchase genuine revia on-line, and the 50% transmission among family members further supports this theory. Median rhomboid glossitis may result from abnormal fusion of the posterior portion of the tongue, but it is almost always chronically infected with Candida. Histologically, the changes are those of a simple, chronic inflammation with fibrosis, and usually with fungal hyphae in the parakeratin layer. Treatment with clotrimazole troches or oral antifungals, such as itraconazole, may lead to improvement. They are attributed to elastic tissue deterioration with aging and may be associated with Fordyce angiokeratomas of the scrotum. Eosinophilic ulcer occurs most frequently on the tongue but may occur anywhere in the oral mucosa. It is characterized by an ulcer with indurated and elevated borders that is usually covered by a pseudomembrane. It develops rapidly, most often on the posterior aspect of the tongue, and spontaneously resolves in a few weeks. The histopathologic findings show a predominantly eosinophilic infiltrate with some histiocytes and neutrophils. However, 5 of the 16 patients reported had no evidence of infection and simply showed eosinophilic infiltrates below the ulcer. Most are discussed elsewhere in this book, and several are uncommon entities that affect specialized oral structures, such as the many subtypes of benign and malignant proliferations that occur in the major and minor salivary glands. These are not covered further here, and only a few select neoplasms are presented. Gupta, et al: A clinical predicament-diagnosis and differential diagnosis of cutaneous facial sinus tracts of dental origin. Treatment requires the removal of the offending tooth or root canal therapy of the periapical abscess. The surface is generally glistening and opalescent, often reticulated, and may even be somewhat pigmented. The white pellicle is adherent to the underlying mucosa, and attempts to remove it forcibly cause bleeding. The lips, gums, cheeks, and edges of the tongue are the most common sites, but the lesion may arise on the anus and genitalia. Biopsy of these white lesions may reveal orthokeratosis or parakeratosis with minimal inflammation, or there may be evidence of varying degrees of dysplasia. A benign form is usually a response to chronic irritation and has very little chance of conversion into the precancerous dysplastic form. Unfortunately, it is not possible to predict clinically which lesions will be worrisome histologically, except that if ulceration, red areas, or erosions are scattered throughout, the lesion is most likely precancerous. When the lesion occurs on the lip, leukoplakia is closely related to chronic actinic cheilitis, which consists of a circumscribed or diffuse keratosis, almost invariably on the lower lip. It is preceded by an abnormal dryness of the lip and may be caused by smoking (especially pipe smoking) or chronic sun exposure. In old lesions, the epithelium may be desquamated, and there may be fissures or ulcerations. Such changes are associated with more or less hyperemia and tenderness, and with a tendency to bleed after slight trauma. Oral hairy leukoplakia is a term used to describe white, corrugated plaques that occur primarily on the sides of the tongue. It may be seen in patients with local or systemic immunosuppression such as those on steroid inhalers, on immunosuppressant or chemotherapy, therapy, or with leukemia. This is a virally induced lesion, discussed in Chapter 19, which has a characteristic histology. Leukoplakia of the vulva usually occurs in obese women after menopause as grayish white, thickened, pruritic patches that may become fissured and edematous from constant rubbing and scratching. Secondary infection with edema, tenderness, and pain may occur It is differentiated from lichen planus by the absence of discrete, rectangular, or annular flat papules of violaceous hue in the mucosa outside the thickened patches, about the anus, on the buccal mucosa, or on the skin. On the penis, although leukoplakia may occur, a similar precancerous process called erythroplasia (of Queyrat) is usually seen instead. Histologically, it shows only hyperkeratosis, without parakeratosis or cellular atypia. A shallow shave excision suffices to cure it and to rule out precancerous leukoplakia; no fulguration is required. Medical therapies that have been the subject of randomized clinical trials may lead to temporary resolution of the lesions, but relapses and adverse effects are common, and there is no evidence that they prevent the transformation to malignancy. On the other hand, small, inflamed patches may be the site of a rapidly growing tumor, which, with relatively insignificant local infiltration, may involve the cervical lymphatics. Carcinoma in leukoplakia usually begins as a localized induration, often around a fissure, or as a warty excrescence or a small ulcer. The degree of epithelial atypia may be considered in staging the risk of developing malignancy. The distinctive picture is that of a white mass resembling a cauliflower covering the tongue and extending on to the other portions of the mucous membranes, including the oropharynx, larynx, and trachea. The histologic features are those of papillomatosis, acanthosis, and varying degrees of dysplasia of the epithelium, without disruption of the basement membrane. It is reasonable to expect the eventual development of epidermoid carcinoma in most patients. In the differential diagnosis, leukoplakia, proliferative verrucous leukoplakia, candidiasis, acanthosis nigricans, and condyloma acuminatum should be considered. The recommended treatment is surgical excision; however, it is often followed by recurrence and spread. Histologically, there is cellular atypia, pleomorphism, hyperchromatism, and increased mitotic figures. Initially flat, usually white patches are present, but the lesions relentlessly become warty, exophytic masses. The most frequent sites are the lower lip, tongue, soft palate, and floor of the mouth. Intraoral lesions frequently develop from leukoplakia or erythroplakia, at sites of frequent irritation, or from long-standing mucosal inflammatory disease such as ulcerative lichen planus. About 20% of oral squamous cell cancers have an associated focus of leukoplakia; these tend to be diagnosed at a less advanced stage than those where no associated leukoplakia exists. The risk factors may also include xeroderma pigmentosa (tip of tongue), dyskeratosis congenita, dystrophic epidermolysis bullosa erosive lichen planus, and oral submucous fibrosis. Unfortunately, the survival rate has remained at 50% for many years because disease is often discovered late, after it has metastasized to the cervical lymph nodes. Surgical excision is the treatment of choice; the roles of sentinel lymph node dissection and adjuvant chemotherapy and/or radiation are all controversial issues undergoing active study. Akrish S, et al: Oral squamous cell carcinoma associated with proliferative verrucous leukoplakia compared with conventional squamous cell carcinoma. Progression of the disorder generally stops at puberty the disease is inherited as an autosomal dominant disorder. A mutation in the mucosal keratin pair K4 and K13 has been identified as the inherited defect. Cai W, et al: Current approaches to the diagnosis and treatment of white sponge nevus. Kimura M, et al: Mutation of keratin 4 gene causing white sponge nevus in a Japanese family. Among the melanocytic nevi of the cellular type, the intramucosal type occurs most frequently, with the compound nevus next and the junction nevus occurring only rarely. Feller L, et al: A review of the aetiopathogenesis and clinical and histopathological features of oral mucosal melanoma. Histologically, there was a unique finding of clusters of dyskeratotic cells in the prickle cell layer in all affected sites. Use of etretinate afforded some improvement, but the condition continued unabated more than 20 years. The blue nevus has dendritic cells in the submucosa Lentigines show acanthosis of rete ridges on biopsy.
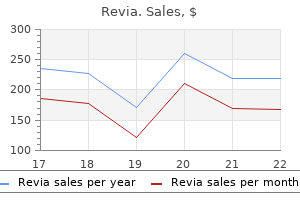
Revia 50 mg
Dermatologists are frequently presented with the dilemma of whether to discontinue blood thinners in the setting of surgery treatment depression generic revia 50mg amex. Data and multiple reviews have shown that continuous treatment with blood thinners perioperatively in patients undergoing Mohs and cutaneous surgery is not associated with an increase in surgical complications leading to significant morbidity. In contrast, discontinuation of these medications may increase he risk of catastrophic cerebral and cardiovascular complications. Multiple authors believe that the potential adverse effects of discontinuing essential medical blood thinners far outweigh the potential side effects of surgical bleeding. As such, it is recommended that patients be maintained on all medically necessary blood thinners during cutaneous surgery. In contrast, patients taking aspirin for primary prevention may discontinue use 2 weeks before any surgical procedure. There is an extensive literature documenting the safety and overall low infection rate of skin procedures (ranging from surgical excisions, to laser, to liposuction). In some cases, making a proper diagnosis of infection can be challenging, with other conditions being mimickers. The Centers for Disease Control and Prevention defines a surgical site infection as occurring within 30 days of the procedure and involving only skin and subcutaneous tissue of the incision. A detailed medical history must be obtained, including information on drug allergies, current medications (including herbal or natural supplements), smoking/ tobacco status, presence of a pacemaker or implantable cardioverter/ defibrillator, recently implanted prosthetic devices, history of prior wound infection or perioperative bleeding, and history of endocarditis or cardiac valvular or congenital malformation. Although procedures such as curettage, biopsy, destruction, and excision have been key components of the field, the practice has evolved to include a greater number and extent of surgical procedures. Dermatologists have a greater understanding of cutaneous pathology, which places them in a unique role to manage complex surgical procedures that arise in the skin. In addition, outpatient dermatologic surgery has been shown to be cost-effective, safe, and efficacious, delivering a greater degree of patient convenience, particularly compared with other fields. The American Board of Dermatology therefore mandates surgical exposure and experience for all residents in dermatology residency programs. This article and Chapters 38 and 39 provide a survey of procedures, indications, and appropriate management within the spectrum of the dermatologic surgery field. Palamaras I, Semkova K: Perioperative management of and recommendations for antithrombotic medications in dermatological surgery. Plovanich M, Mostaghimi A: Novel oral anticoagulants: what dermatologists need to know. The main issues surrounding antibiotic prophylaxis are prevention of surgical site infections and reduction of the risk of endocarditis or contamination of prosthetic devices in high-risk patients. As a general rule, wound infections associated with skin surgery procedures occur at an extremely low rate. Although reducing infection is one objective in the use of antibiotics, dermatologists must consider the risks of such treatment, including adverse drug reactions, serious drug reactions, drug interactions, development of resistant strains of bacteria, and increased cost. Determining the indications for antibiotic prophylaxis for surgical site infections requires an understanding of the various types of wound that the dermatologist may encounter. In cases where infection leads to dehiscence, the wound can be packed or allowed to heal by second intention. A culture should be performed before initiating empiric antibiotics to determine sensitivities Staphylococcus aureus is the most common pathogen, and cephalexin or dicloxacillin is an appropriate first-line treatment. Al hough this antibiotic has been associated with colitis, the short courses of clindamycin typically used with surgical site infection generally do not present a problem. Ciprofloxacin can be used for infections with a higher likelihood of gram-negative or Pseudomonas organisms. The use of topical antibiotics after routine skin surgery has not been shown to reduce the incidence of surgical site infection. Several studies have demonstrated that petrolatum was as effective as topical antibiotics in terms of incidence of infection. In addition, many patients on topical antibiotics had a higher incidence of allergic contact dermatitis. Finally, studies have shown the overall cost saving of switching from postoperative bacitracin to petrolatum. As such, routine use of topical antibiotics ought to be avoided in the postoperative period. Antibiotics given at the conclusion of the procedure are not as effective in preventing infection, because they are not incorporated into the coagulum of the wound. Most dermatologic procedures are of short duration, so a single preoperative dose of antibiotics 1 hour before the start of the case is sufficient. In rare cases with an extended dermatologic procedure, a second dose of antibiotics can be administered 6 hours postoperatively. The choice of antibiotic is based on the most likely causative organism at the surgical site (Table 37. Other pathogens to consider in some situations include Streptococcus viridans (oral mucosa) and Escherichia coli (perineal and genital location). First-genera ion cephalosporins are an ideal initial choice for the treatment of wound infection because of their coverage of ks fr Antibiotic Selection and Timing. Clean (class I) wounds, which constitute the vast majority of dermatologic surgery procedures, do not require antibiotic prophylaxis. Some exceptions to this that have been advocated include surgical cases that violate mucosal membranes (oral, nasal, anogenital) and patients with heavily colonized skin (atopic dermatitis, infected skin), as well as those in whom a wound infection would result in significant morbidity. However, dermatologic surgeons do not universally agree on these exceptions, and the role for antibiotic prophylaxis is still debated. Clean wounds (class I) are created on normal skin using clean or sterile technique. Examples include excision of neoplasms, noninflamed cysts, biopsies, and most cases of Mohs surgery. Of note, this incidence is based on general surgery cases, which are often of longer duration and a greater extent than most dermatologic procedures. An ibiotic prophylaxis has been limited to patients with the conditions listed in Box 37. All other cardiac conditions, including mitral valve prolapse and other forms of congenital heart disease, no longer require prophylaxis for any procedure. Antibiotic prophylaxis is reasonable when procedures involve manipulation of gingival tissue, perforation of oral mucosa, or incision or biopsy of the respiratory mucosa, or when performed on infected skin, but only in patients with underlying cardiac conditions associated with the highest risk of adverse outcome, as outlined in Box 37. Antibiotic prophylactic regimens for those select high-risk patients should be a single dose of antibiotic administered 1 hour before the procedure (Table 37. However, guidelines for dental procedures in patients with joint replacement can be extrapolated to certain procedures. Patients with joint replacement probably do not need prophylactic antibiotics for clean wounds. If mucosa is invaded, prophylaxis may be appropriate and reasonable in the small number of patients who might be at high risk of joint infection. Consultation with orthopedic surgery is appropriate in determining whether antibiotic prophylaxis is necessary. Cephalosporins are rapidly absorbed when taken orally and have good tissue penetration. Aminopenicillins, such as ampicillin and amoxicillin, have better gram-negative, enterococcal, and group A streptococcal coverage. However, because it has only weak antimicrobial activity, alcohol is not recommended for more extensive procedures. Chlorhexidine has a broad spectrum against gram-positive and gram-negative organisms, a rapid onset of activity, and sustained residual activity even after being wiped off, and it is nonstaining. Chlorhexidine has been reported to cause both ototoxicity and keratitis from direct tympanic or ocular contact However, this is mainly in patients under general anesthesia who cannot respond to immediate irritation associated with ocular contact, a problem that is avoided in most dermatologic procedures performed under local anesthesia.
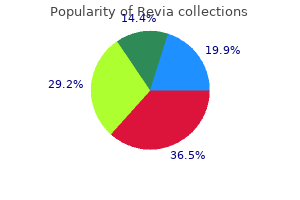
Generic 50mg revia amex
Carotenemia may cause a yellow tint in the skin that is especially prominent on the palms and soles symptoms 4 days before period buy genuine revia on-line. Tumors causing such elevations in serum androgens often cause more dramatic masculinization with clinical findings such as a deepening voice, increased muscle mass, enlargement of the clitoris, decreased breast size, galactorrhea, and absent periods. In congenital adrenal hyperplasia, testing should include levels of cortisol, aldosterone, and precursor hormones, and in some patients, cosyntropin (Cortrosyn) stimulation tests. The question remains whether treatment with corticosteroid replacement results in better outcomes than empiric antiandrogen therapy. Treatment of the cutaneous signs of androgen excess is successful with an oral contraceptive and often also an androgen-blocking agent such as cyproterone acetate, flutamide, or finasteride. Spironolactone, which competes for the androgen cytosol receptors, has proved useful as a systemic antiandrogen in the treatment of hirsutism and acne. Adrenal-androgenic female pattern alopecia may improve with topical minoxidil or spironolactone. Chorionic villous biopsy may identify homozygous adrenogenital female fetuses and allow for dexamethasone therapy to prevent intrauterine virilization of the external genitalia. Depending on the degree of thyroid deficiency, a wide variety of signs and symptoms may be evident. The main consequence of extreme thyroid deficiency is cretinism and its attendant mental retardation, but much more prevalent are lesser degrees of intellectual and neurologic deficits seen in areas of the world where iodized salt is still not routinely available. Disturbances in the amount, texture, and distribution of the hair with patchy alopecia are common. Wide-set eyes, a broad, flat nose, and periorbital puffiness characterize the face. A protuberant abdomen with umbilical hernia; acral swelling; coarse, dry, brittle nails; a clavicular fat pad; and hypothermia with cutis marmorata are also seen. Mandatory screening programs for congenital hypothyroidism (as in the United States) has led to dramatically improved cognitive outcomes. Middle-aged women are the adults most often affected Patients with Turner and Down syndrome are predisposed to hypothyroidism and the production of thyroid autoantibodies. Other associations with hypothyroidism include lichen planopilaris and cutaneous sarcoidosis. Funakoshi T, et al: Risk of hypothyroidism in patients with cancer treated with sunitinib. Ryder M, et al: Endocrine-related adverse events following ipilimumab in patients with advanced melanoma. In Hashimoto thyroiditis, the most common cause of hypothyroidism in the United States, thyroid peroxidase antibodies are present in 95% of patients and antithyroglobulin antibodies in 65%. In those with positive antibodies but normal thyroid function, hypothyroidism will develop at a rate of 5% per year. The hair is thin and has a downy texture, and nonscarring diffuse alopecia may be observed. The skin may darken to produce a bronzed appearance or melanoderma; melasma of the cheeks is seen is some cases. Nail changes are present in approximately 5% of patients with Plummer nails, a concave contour of the plate with characteristic distal onycholysis. It usually occurs after treatment of hyperthyroidism and is frequently associated with exophthalmos and pretibial myxedema. It may, however, occasionally precede the thyrotoxicosis and has been recognized in euthyroid and hypothyroid patients. It can be confused clinically with acromegaly, pachydermoperiostosis, pulmonary osteoarthropathy, or osteoperiostitis, but the radiologic findings are pathognomonic. Pretibial myxedema, consisting of bilateral, localized, cutaneous accumulations of glycosaminoglycans, occurs in 4% of patients who have or have had Graves disease. Most pronounced is faulty dentition when hypoparathyroidism is present during development of the permanent teeth. A diffuse scantiness of the hair and complete absence of axillary and pubic hair may be found. Of patients with idiopathic hypoparathyroidism, 15% develop mucocutaneous candidiasis. Hypoparathyroidism may also occur in DiGeorge syndrome, or with parathyroid infiltration or their inadvertent surgical removal during thyroid surgery. Hypoparathyroidism with resultant hypocalcemia may trigger bouts of impetigo herpetiformis or pustular psoriasis. This results in short, stubby fingers and toes, with dimpling over the metacarpophalangeal joints (Albright sign). Shirai K, et al: Dramatic effect of low-dose oral steroid on elephantiasic pretibial myxedema. Yu H, et al: Elephantiasic pretibial myxedema in a patient with Graves disease that resolved after 131I treatment. Vitiligo is present in 7% of patients with Graves disease and occurs with an increased frequency in Hashimo o thyroiditis. Urticaria may be seen in patients with thyroid autoantibodies and may clear with the administration of thyroid hormone, even in euthyroid patients. A wide range of other autoimmune disorders may be seen in patients with Graves disease or Hashimoto autoimmune thyroiditis. Treatment is with radioactive iodine or antithyroid drugs such as methimazole or propylthiouracil. It may also occur infrequently during the course of Hashimoto thyroiditis and primary hypothyroidism. Patients with pretibial myxedema regularly have associated ophthalmopathy and occasionally thyroid acropachy. Although usually not clinically apparent, approximately half of patients with Graves disease have mucopolysaccharide deposition in the preradial area of the extensor aspects of the forearms. Improvement in the plaques of pretibial myxedema has resulted from intralesional injections of triamcinolone acetonide and with high-potency topical corticosteroids under occlusion. Compression stockings or complete decongestive physiotherapy, and a combination of manual lymphatic drainage, bandaging, and exercise, are useful and safe. Pentoxifylline, octreotide, plasmapheresis, and cytotoxic drugs have all been reported to help in small numbers of patients, but negative reports also exist. This can occur when the serum calcium/phosphorus product is greater than 65 mg/dL. This may manifest as large, subcutaneous nodules or white, often linearly arranged papules centered around joints. Additionally, calciphylaxis, although most common in the patient with secondary hyperparathyroidism and renal failure, may be seen occasionally in primary hyperparathyroidism. The most frequently observed abnormality is hypercalcemia from hypersecreting tumors of the parathyroid glands. This autosomal dominant inherited disease usually presents in the fourth decade of life with clinical symptoms related to hypersecretion of hormones specific for the type of tumor present. The angiofibromas are smaller and less numerous than those present in tuberous sclerosis. Vidal A, et al: Cutaneous lesions associated to multiple endocrine neoplasia syndrome type 1. With extensive involvement, lesions can be found on the areolae, conjunctivae, lips, and buccal mucosa, and around the umbilicus. The palms or soles may show thickening of the palmar or plantar skin with exaggeration of the dermatoglyphs. Small, papillomatous, nonpigmented lesions and pigmented macules may occasionally be found in the mucous membranes of the mouth, pharynx, and vagina. Acanthosis nigricans can best be understood by grouping the associations in the following manner. Most cases are associated with adenocarcinoma, especially of the gastrointestinal tract (60% stomach), lung, and breast, or less often the gallbladder, pancreas, esophagus, liver, prostate, kidney, colon, rectum, uterus, and ovaries. A few cases have been observed in childhood, but most begin after puberty or in adulthood. In 40% of these patients, tripe palms are the presenting sign of an undiagnosed malignancy. It presents as a grayish, velvety thickening of the skin of the sides of the neck, axillae, and groins.
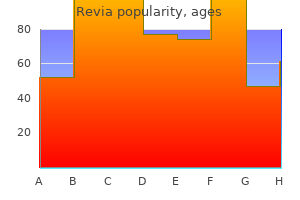
Cheap revia online mastercard
Grafts can be categorized as full symptoms 3 days after embryo transfer 50 mg revia for sale, split, or composite; when to use each depends on the depth of the defect, vascular supply, and concern about skin cancer recurrence. Full-thickness skin grafts have a full dermis and are the most common grafts used in dermatologic surgery. The graft is defatted, trimmed to fit the defect, anchored in place with peripheral and basting sutures, and secured with a tie-over dressing. Common donor sites include the preauricular cheek, postauricular crease, conchal bowl, upper eyelid, upper inner arm, and clavicle. However, the increased skin thickness results in an increased metabolic demand and a higher rate of necrosis and failure. The graft is sustained by passive diffusion of nutrients from the wound bed during this stage. The graft becomes edematous, and the fibrin network attaches the graft to the bed. Inosculation is the next stage of wound healing, with revascularization resulting from linkage of dermal vessels in the graft to the wound bed. Neovascularization occurs from capillary ingrowth to the graft from the recipient base and side walls. Full circulation can be restored in 7 days and depends on graft thickness and vascularity of the wound bed. Split-thickness skin grafts have only a partial dermis and are useful for covering large areas or improving surveillance in tumors with a high risk of recurrence (see Video 37. Grafts can be meshed, which results in an expanded size to provide coverage for larger defects. Compared with full-thickness skin grafts, split-thickness grafts have a higher rate of survival and shorter healing time, do not require repair of the donor site, and are a good choice for areas that are poorly vascularized because oo ks Skin Grafts. Hairs remaining in the graft are above the level of the bulb and will not persist once the graft takes. However, split-thickness grafts have a higher degree of contraction, lack skin appendages, and provide a poorer cosmetic match than full-thickness grafts. The original technique used zinc chloride paste to fix tissue in vivo, followed by surgical excision. Ted Tromovitch and Sam Stegman in San Francisco modified Mohs technique in the 1970s to a fresh frozen tissue variant that con inues to be used today. The basic surgical principles in Mohs micrographic surgery are similar to those used in standard excision, although unique challenges are encountered with Mohs surgery. A complete understanding of pathology, anatomy, cutaneous oncology, advanced surgical reconstruction, and management of surgical complications is critical to a successful patient outcome. Any dermatologist performing Mohs micrographic surgery should be well trained in this technique and all the accompanying challenges of surgical and postoperative care. Mohs micrographic surgical excision is a tissue-sparing technique that employs frozen-section control of 100% of the surgical margin (see Video 37. Immunohistochemical stains can be used in specific cases to help identify residual tumor. In an effort to help identify which patients and tumors are appropriate for treatment with Mohs surgery, a joint task force has established guidelines for appropriate-use criteria. These guidelines should be followed to prevent overuse of Mohs surgery for inappropriate clinical situations. A smartphone "app" is available for easy reference when evaluating patients in the clinic. Other tumors that can be successfully treated by Mohs surgery include dermatofibrosarcoma protuberans, atypical fibroxanthoma, and microcystic adnexal carcinoma. Several studies have demonstrated comparable local recurrence, metastasis, and disease-specific survival rates in head and neck melanomas treated with Mohs micrographic surgery compared with standard excision. Dermatol Surg 2011; 37: 1069 Chin-Lenn L, et al: Comparison of outcomes for malignant melanoma of the face treated using Mohs micrographic surgery and wide local excision. Foroozan M, et al: Efficacy of Mohs micrographic surgery for the treatment of dermatofibrosarcoma protuberans. Leibovitch I, et al: Cutaneous squamous cell carcinoma treated with Mohs micrographic surgery in Australia. Dermatol Surg 2017; 43: 98 Nosrati A, et al: Outcomes of melanoma in situ treated with Mohs micrographic surgery compared with wide local excision. Pugliano-Mauro M, Goldman G: Mohs surgery is effective for high-risk cutaneous squamous cell carcinoma. Topical agents offer the advantage of limiting photosensitivity to the application site and have become widely used in dermatology. It is applied and left on the skin for a sufficient period to allow for accumulation within the target cells. Gentle scraping or curettage before application is performed to increase penetration. Blue light targets the 417-nm peak and has a more superficial penetration, making it an appropriate choice for the treatment of epidermal lesions such as actinic keratoses. Following absorption of light, the photosensitizer is con verted from a stable ground state to an excited triplet state the excited-triplet-state electrons interact with tissue oxygen, creating singlet oxygen. Systemic photosensitizing molecules are large, lipophilic molecules that require intravenous administration to reach the target site. One of the major disadvantages of these systemic drugs is the prolonged period of phototoxicity. However, individual patient factors must be considered when choosing a treatment option. Basset-Seguin N, et al: Consensus recommendations for the treatment of basal cell carcinomas in Gorlin syndrome with topical methylaminolaevulinate-photodynamic therapy. Christensen E, et al: High and sustained efficacy after two sessions of topical 5-aminolaevulinic acid photodynamic therapy for basal cell carcinoma. The use of ionizing radiation in dermatologic therapy of benign conditions has all but disappeared, because of highly effective medical therapies and the potential genetic and somatic hazards of radiation. Radiation is an appropriate primary treatment for skin cancer in patients who refuse surgery or who are not optimal surgical candidates. Red light should be used instead of blue light because it penetrates more deeply and thus more effectively treats adnexal extensions. Squamous Cell Carcinoma in situ Hadley J, et al: Results of an investigator-initiated single-blind split-face comparison of photodynamic therapy and 5% imiquimod cream for the treatment of actinic keratoses. Scola N, et al: A randomized, half-side comparative study of aminolaevulinate photodynamic therapy vs. Serra-Guillen C, et al: A randomized comparative study of tolerance and satisfaction in the treatment of actinic keratosis of the face and scalp between 5% imiquimod cream and photodynamic therapy with methyl aminolaevulinate. Zaiac M, Clement A: Treatment of actinic cheilitis by photodynamic therapy with 5-aminolevulinic acid and blue light activation. Electronic surface brachytherapy delivers radiation without using an isotope using a miniaturized x-ray tube. This form of treatment contains no actively radioactive isotope components, so it is subject to much less regulation and offers the advantage of less shielding requirements for patients and staff. Long-term outcomes for electronic brachytherapy are not yet available, but many centers have reported initial cohorts with good short-term cosmesis. At present, additional comparative research is needed for these modalities to determine their proper role in the treatment and management of cutaneous malignancies relative to surgery. Radiation therapy may also be considered if surgical margins show microscopic evidence of residual tumor after excision. Caccialanza M, et al: Radiotherapy of recurrent basal and squamous cell skin carcinomas. Han A, Ratner D: What is the role of adjuvant radiotherapy in the treatment of cutaneous squamous cell carcinoma with perineural invasion Jambusaria-Pahlajani A, et al: Surgical monotherapy versus surgery plus adjuvant radiotherapy in high-risk cutaneous squamous ce l carcinoma.
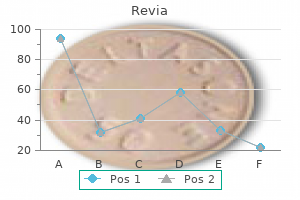
Revia 50 mg with mastercard
Histologically symptoms 6 months pregnant order revia 50mg otc, there are intracorneal or subcorneal aggregates, predominantly of neutrophils, although eosinophils may also be found. Similar lesions may appear on the buccal mucosa, tongue, gingiva, and the perianal mucosa; macules may also occur around the mouth, on the central face, perianally, and on the backs of the hands, especially the fingers, toes, and tops of the feet. More than two thirds of patients have lesions on the hands and feet, and 95% have perioral lesions. Skin lesions grow in size and number until puberty, after which they begin to regress Buccal pigmented macules tend to persist. The associated polyps, which are histologically characteristic, are most common in the small intestine, but may also occur in the stomach, colon, and least commonly the rectum. The polyposis of the small intestine may cause repeated bouts of abdominal pain and vomiting. These cancers occur in the colon (39% of patients), stomach (29%), and small intestine (13%). The prevalence of cancers by anatomic site is pancreas (26%), breast (54%, can be bilateral), ks oo oo ks ok s ok s oo Banno K, et al: Hereditary gynecological tumors associated with Peutz-Jeghers syndrome (review). Patients with truncation of the gene rather than a missense mutation are more severely affected, suggesting a phenotype/genotype correlation. Laugier-Hunziker syndrome presents with mucosal pigmentation and pigmented nail streaks. A proteinlosing enteropathy may develop and is associated with the degree of intestinal polyposis. Onset is typically after age 30 in this sporadically occurring, generally benign condition. Hypogeusia (reduced taste) is the dominant initial symptom in Cronkhite-Canada, followed by diarrhea and ectodermal changes. Hepatic dysfunction occurs simultaneously with the appearance of an eruption of discrete red-brown, erythematous papules in the intertriginous areas (areas of friction) of the lower abdomen, buttocks, and lateral upper chest. Periungual pigmentation occurs in up to half of acutely poisoned patients at 3 months. Arsenic is an elemental metal that is ubiquitous, existing in nature as metalloids, alloys, and a variety of chemical compounds. These various forms of arsenic may be deposited into water, soil, and vegetation, producing serious health risks. Certain regions of Pakistan, India (West Bengal and Eastern India), Mongolia, China, Cambodia, and Vietnam have high levels of arsenic in their drinking water, exposing millions of people to levels of arsenic that result in health consequences. Evidence indicates that polymorphisms in arsenic-metabolizing (methylation) pathways, specifically converting monomethylarsonic acid to dimethylarsinic acid, may portend higher risk. Arsenic exposure is also associated with a significant reduction in circulating helper T cells, perhaps contributing to increased cancer risk. Patchy hyperpigmentation may be accentuated in the inguinal folds, on the areolae, and on palmar creases. Areas of hypopigmentation may be scattered in the hyperpigmented areas, giving a "raindrop" appearance. Blackfoot disease-arsenic-induced peripheral vascular disease that can lead to vasospasm and peripheral gangrene-and a severe peripheral neuropathy can also occur with chronic arsenic ingestion. Histologically, the arsenical keratosis on the palms and soles shows hyperkeratosis, parakeratosis, acanthosis, and papillomatosis. Bowen disease represents the majority of arsenic-induced skin cancers and may appear on sun-exposed or sun-protected skin. Basal cell carcinomas are frequent, are usually multiple, are most common on the trunk, and can be in sun-protected sites. Two autosomal recessive forms of juvenile hereditary hemochromatosis are described, caused by mutations in the Hemojuvelin and the Hepcidin gene. Mutations in the transferrin receptor 2 gene lead to a form of autosomal recessive adult-onset hemochromatosis. Ferroportin mutation leads to an adult-onset form of autosomal dominant hemochromatosis. Only a minority of persons with the most common genetic defects causing hemochromatosis will develop disease. With widespread genetic testing, the age of diagnosis has been decreased, and the number of asymptomatic affected females has dramatically increased. The characteristic cutaneous manifestation is gray to brown generalized mucocutaneous hyperpigmentation. Discolorations from medications containing silver and gold are discussed n Chapter 6. If Monsel solution is used, to minimize tattooing, it is best applied with a cotton-tipped applicator barely moistened with the solution, then rolled across a wound that has just been blotted dry. The percentage of affected males with pigmentation is about 30%, and in women, fewer than 10% of diagnosed patients have skin changes. Biopsy of affected hyperpigmented skin shows dermal iron deposition, but the visible pigmentation is actually increased epidermal melanin in the basal cell layer. Porphyria cutanea tarda occurs more commonly in patients with hemochromatosis due to inhibition of uroporphyrinogen decarboxylase in the liver by iron overload. In patients with chronic venous insufficiency, the risk of lower leg ulceration is increased sixfold in those also carrying the C282Y mutation, leading some to suggest that this test should be ordered in at-risk patients at the initial stages of venous insufficiency. Consuming alcohol and smoking, as well as coexistent hepatitis C virus infection, make it more likely that persons with genetic predisposition will develop clinical disease. A score of 45 or less is normal, except in premenopausal women, in whom greater than 35 may be considered abnormal. All forms of hemochromatosis are reated with phlebotomy until satisfactory iron levels are attained. Once cirrhosis is present, phlebotomy does not prevent development of hepatocellular carcinoma, which occurs in 30% of patients. Xia Y, et al: Well water arsenic exposure, arsenic-induced skin lesions and self-reported morbidity in Inner Mongolia. Zamboni P, et al: Hemochromatosis C282Y gene mutation increases the risk of venous leg ulceration. Titanium screws used for orthopedic procedures, if close to the skin, can cause cutaneous blue-black hyperpigmentation. In cases of degeneration of artificial knee joints, periprosthetic black pigment can be seen, resulting from titanium deposition. Rarely, this pigment may migrate to the skin, resulting in dermal blue-gray patches over the shin Titanium pigment was recently reported due to intralesional and topical application of triamcinolone in a patient with alopecia areata. Melanin stains are positive, but polarizing foreign material can be seen, and x-ray spectro photometry reveals titanium in the tissue. Fa mi Z, et al: Burden of skin lesions of arsenicosis at higher exposure through groundwater of Taluka Gambat district Khairpur, Pakistan. It usually occurs after age 40, and its prevalence increases with age, exceeding 90% in Koreans over age 60. Arbache S, et al: Activation of melanocytes in idiopathic guttate hypomelanosis after 5-fluorouracil infusion using a tattoo machine. Rerknimitr P, et al: Topical tacrolimus significantly promotes repigmentation in idiopathic guttate hypomelanosis. Shilpashree P, et al: Therapeutic wounding: 88% phenol in idiopathic guttate hypomelanosis. Shin J, et al: the effect of fractional carbon dioxide lasers on idiopathic guttate hypomelanosis. The lesions are irregularly shaped and sharply defined, similar to depigmented ephelides. Histologically, there is epidermal atrophy and reduced numbers of hypoactive melanocytes. Topical calcineurin inhibitors, by their stimulation of melanocyte migration and activity, can be therapeutic.
Revia 50mg otc
Other sites of involvement include the axillae symptoms syphilis buy generic revia online, abdomen, forehead, penis, and vulva. Genital syringomas may cause genital pruritus and may be mistaken for genital warts. Some have suggested that eruptive syringomas represent a proliferative process of inflamed normal eccrine glands, analogous to traumatic neuroma being a proliferation of normal peripheral nerve. The fact that numerous lesions appear after "waxing" in the pubic areas supports this hypothesis. Other features include hypodontia, hypotrichosis, nail dystrophy, and palmoplantar keratoderma. Turan E, et al: A rare association in Down syndrome: milialike idiopathic calcinosis cutis and palpebral syringoma. Gandhi V, et al: Eccrine hidrocystoma successfully treated with topical synthetic botulinum peptide. Woolery-Lloyd H, et al: Treatment for multiple periorbital eccrine hidrocystomas: botulinum toxin A. The rare "plaque-type" syringoma may be mistaken for a microcystic adnexal carcinoma. In general, except in eruptive cases, syringomas develop slowly and persist indefinitely without symptoms. This is approximately 30 times the frequency seen in patients with other syndromes. Histologically, syringomas are characterized by dilated cystic spaces lined by two layers of cuboidal cells and epithelial strands of similar cells. Some of the cysts have small, comma-like tails, which produce a distinctive picture, resembling tadpoles or the pattern of a paisley tie. At times, the cells of the syringoma have abundant clear cytoplasm, which represents accumulated glycogen. Treatment is difficult, but many lesions respond to very light electrodessication or shave removal. Lesions with papillary proliferations of the lining are classified as cystadenomas. The lesion will bleed on slight trauma A distinctive finding is the cup-shaped shallow depression from which the tumor grows and protrudes. A rare variant is called eccrine poromatosis, in which more than 100 lesions may involve the palms and soles and may be associated with hidrotic ectodermal dysplasia, immunosuppression, or chemotherapy. Nodular and clear cell hidradenomas are larger nodules that often involve the head or neck but may occur anywhere. Histologically, poromas demonstrate solid masses of uniform, cuboidal epithelial cells with ample cytoplasm and focal duct differentiation. The cells are smaller than those in the contiguous epidermis and tend to arrange themselves in cords and broad columns extending downward from the normal epidermis. Areas of clear cell and cystic degeneration may be present, and an underlying dermal duct tumor or hidradenoma may be present. Melanocytes may be dispersed throughout the tumor and may be clinically hyperpigmented. These lesions resemble clonal seborrheic keratoses, except for the presence of focal duct differentiation. Dermal duct tumors are composed of the same small acrosyringeal cells as other acrospiromas. When the cells form a large nodule, the tumor is referred to as a nodular hidradenoma. When clear cells and cystic degeneration are prominent, the tumor is referred to as a clear cell hidradenoma. A distinctive feature of the latter two tumors is the presence of areas of eosinophilic hyalized stroma. This is the staining pattern of the sweat duct ridge and acrosyringium (intraepidermal portions of sweat duct). Malignant degeneration may occur, and atypia is sometimes minimal within tumors that have metastasized. The most frequent sites of involvement are the legs (30%), feet (20%), face (12%), thighs (8%), and arms (7%). Of interest is the rare involvement of the palms and soles, despite these having the greatest concentration of sweat glands. These tumors are of intermediate aggressiveness, with metastases usually occurring to regional lymph nodes and, less often, hematogenously. Atypia may be marked or minimal, with pleomorphic or monomorphous nuclei and abundant or scant eosinophilic cytoplasm. Most frequently, the cells are smaller and more basophilic than those in benign acrospiromas with a high mitotic rate. The degree of ductal differentiation is variable the tumors can be deeply infiltrative. Perineural and lymphovascular involvement by the tumor can be present and should be noted on the dermatopathology report. As with other cutaneous neoplasms, margins should be free of tumor islands and tumor stroma to be considered negative. Local recurrence approaches 20%, and lymph node metastases occur in about 20% of patients. Occasionally, multiple lesions may be present and may occur in a linear or segmental pattern. Spiradenoma has a generally benign clinical course and occurs most frequently between ages 15 and 35, although it has also been reported in infancy and childhood. Rarely, malignant transformation occurs, and the subsequent tumor may also have features of a cylindroma (spiradenocylindrocarcinoma). Microscopically, spiradenoma demonstrates either a single nodule or multiple basophilic nodules within the dermis. Three cell ypes are present: cells with large, pale-gray nuclei; those with smaller, darker-gray nuclei; and jet-black lymphocytes peppered throughout the nodule. Ductlike structures are often present, as are large, pink hyaline globules that resemble the bright-red hyaline basement membrane material that outlines the islands of cylindromas. In fact, spiradenomas and cylindromas often occur together in the same patient, and hybrid collision tumors are quite common. These have historically been thought to be of eccrine lineage, but both tumors may instead originate from the hair follicle bulge. When painful, eccrine spiradenoma may be mistaken for leiomyoma, glomus tumor, neuroma, and angiolipoma Treatment is simple excision. Spiradenocylindrocarcinoma presents as a solitary nodule that may have experienced an abrupt change in size. The tumor is firm but rubberlike and pink-blue; it ranges in size from a few millimeters to several centimeters. The solitary cylindroma is considered to be nonhereditary and at times may be found in areas other than the head and neck. Histologically, these are cylindrical masses of epithelial cells surrounded and segmented by thick bands of a hyaline material. Cylindroma may be mistaken for pilar cyst, but the distinctive appearance and consistency make diagnosis easy, especially in the multiple type. Treatment is surgical; success using ablative laser therapy has also been reported. Englander L, et al: A rare case of multiple segmental eccrine spiradenomas J Clin Aesthet Dermatol 2011; 4: 38 Gordon S, et al: Pediatric segmental eccrine spiradenomas. Brooke-Spiegler syndrome including the phenotypic variant of multiple familial trichoepitheliomas and correlation with the histopathologic findings in 379 biopsy specimens. Ulceration and crusting may occur, and continued growth may obstruct the meatus, resulting in hearing loss.

Order revia 50 mg without prescription
Aggressive and cautious management with dressings and diabetic foot care is required treatment 1st degree burns buy discount revia 50 mg line. Lesions appear after periods of relative hypoglycemia, perhaps explaining the clinical resemblance of diabetic bullae to pressure bullae. Treatment is diabetic control, aspiration of the bulla to prevent expansion by hydrostatic pressure, and aggressive wound management to optimize healing and prevent infection. Although shin spots occur individually in people who do not have diabetes, if four or more are present the specificity is high for diabetes. Patients with diabetic dermopathy have a higher risk of nephropathy and retinopathy. Lesions begin on the lower extremities as crops of four or five dull-red macules 0. Joint symptoms begin with limitation of joint mobility in the fifth finger at the metacarpophalangeal and proximal joints and progress radially to the other fingers. Chatterjee N, et al: An observational study of cutaneous manifestations in diabetes mellitus in a tertiary care hospital of eastern India. Hammer E, et al Risk factors for necrobiosis lipoidica in type 1 diabetes mellitus. Kato M, et al: Necrobiosis lipoidica with infiltration of Th17 cells into vascular lesions. South Med J 2009; 102: 643 Mahmood T, et al: Cutaneous manifestations of diabetes mellitus. Mirhoseini M, et al: A study on the association of diabetic dermopathy with nephropathy and retinopathy in patients with type 2 diabetes mellitus. Kumar P, et al: Infantile erythrodermic psoriasis Indian J Paediatr Dermatol 2017; 18: 248. It is associated with evidence of diabetic neuropathy and probably represents a form of neuropathic pruritus. The characteristic findings are a pellagra-like dermatitis following exposure o sunlight, intermittent cerebellar ataxia, psychosis, and constant aminoaciduria. The dermatitis occurs on exposed parts of the skin, chiefly the face, neck, hands, and legs. The erythematous scaly patches flare up into a hot, red, exudative state after exposure to sunlight, followed by hyperpigmentation. Involvement of the feet also occurs and is thought to contribute to the development of chronic ulcerations. Such open sores on the neuropathic, microvascularly compromised, infectionprone diabetic foot pose a constant threat to life and limb. This enzyme converts citrulline and aspartic acid to argininosuccinic acid, as a part of the urea cycle. Low plasma arginine levels result, and the hypothesis is that, because keratin is 16% arginine, dermatitis may occur. Neonates who present with severe deficiencies and hyperammonemic crises may develop erosive, erythematous, scaling patches and plaques prominent in the perioral, lower abdominal, diaper, and buttock regions or erythroderma similar to psoriasis. In carbamoyl phosphate synthetase deficiency, low plasma arginine levels may also occur, and similar cutaneous findings have been reported in this second metabolic defect of the urea cycle. Murao K: Photodynamic therapy for necrobiosis lipoidica is an unpredictable option. Endocrinol Metab Clin North Am 2013; 42: 869 Quondamatteo F: Skin and diabetes mellitus Cell Tissue Res 2014; 355: 1. Shenavandeh S, et al: Diabetic muscle infarction and diabetic dermopathy two manifestations of uncontrolled prolong diabetes mellitus presen ing with severe leg pain and leg skin lesions. They are usually extremely sensitive to light, and about 50% have an eczematous dermatitis. It is clinically similar to atopic dermatitis, with a predilection for the flexures. The dermatitis is worst in the youngest patients, may improve with dietary treatment, and has been exacerbated by phenylalanine challenge in a carrier of the recessive gene. Indurations of the thighs and buttocks are present early in infancy and increase with time. For many years, the dark urine may be the only indication of the presence of alkaptonuria. Later, the cartilage of the nose and tendons, especially those on the hands, becomes discolored. The bluish macules have a predilection for the fingers, ears, nose, genital regions, apices of the axillae, and buccal and vaginal mucosae. Palmoplantar pigmentation may occur and may be accentuated along the thenar and hypothenar eminences as pigmented pitted areas some with hyperkeratosis. When this enzyme is deficient, the normal recycling of proline residues obtained from collagen degradation is impaired. A buildup of iminodipeptides results, with disturbances in connective tissue metabolism and excretion of large amounts of iminodipeptides in the urine. The most important cutaneous signs, which almost always appear before the affected person is 12 years old, are skin fragility; ulceration and scarring of the lower extremities; photosensitivity and telangiectasia; poliosis; scaly, erythematous, maculopapular, and purpuric lesions; and thickening of the skin with lymphedema of the legs Systemic signs and symptoms include mental deficiency, splenomegaly, recurrent infections and facial dysmorphism with low hairline, frontal bossing, and saddle nose. Because C1q has a high proline content, a relative deficiency of functional C1q may explain the high frequency of lupus erythematosus in these patients. Ciecierega T, et al: Severe persistent unremitting dermatitis, chronic diarrhea and hypoalbuminemia in a child; Hartnup disease in set ing of celiac disease. Large amounts of neutral amino acids, including tryptophan, are present in the urine, establishing the diagnosis. The skin lesions respond to niacinamide, but the neurologic disease may not improve. Longo N, et al: Single-dose, subcutaneous recombinant phenylalanine ammonia lyase conjugated with polyethylene glycol in adult patients with phenylketonuria. The presence of phenylpyruvic acid in the urine is demonstrated by a characteristic deep-green color when a few drops of ferric chloride solution are added. If compliance is poor, the manifestations, including eczema, may develop at any age, followed by improvement of the skin with reinstitution of the diet m et t. The apocrine sweat glands are rich in ochronotic pigment granules, and the intradermal injection of epinephrine into the skin of the axillary vault will yield brown-black sweat droplets in the follicular orifices. Histologically, there are large, irregular ochre bodies within the reticular dermis. These represent degenerated elastic fibers with deposition of ochronotic pigment and stain black with crystal violet or methylene blue. Ochronotic arthropathy first involves the axial spine joints, followed by the knees, shoulders, and hips. Radiographs show a characteristic appearance of early calcification of the intervertebral disk and later narrowing of the intervertebral spaces with eventual disk collapse. Dietary restriction of tyrosine and phenylalanine is recommended but may not prevent progression of disease. This results in accumulation of the blue discoloration on the collagen fibers where hydroquinone is applied. All skin types can be affected, but ethnic groups with he highest prevalence of melasma and hydroquinone use are primarily reported: African Americans, Africans, and Asians. Because most patients use the hydroquinone to treat melasma, findings of melasma may overlay the skin findings of exogenous ochronosis. Hyperchromic pinpoint papules may occur, that on dermoscopy can be seen associated with follicular openings. Confetti-like depigmentation (from the hydroquinone) may be admixed with the hyperpigmentation. Treatment is challenging but stopping the application of hydroquinone may lead to improvement. Schaefer M, et al: Increased prevalence of subcutaneous lipomas in patients with Wilson disease. Affected persons develop hepatomegaly, splenomegaly, and neuropsychiatric changes. Slurred speech, a squeaky voice, salivation, dysphagia, tremors, incoordination, and spasticity may all occur.
Buy 50mg revia overnight delivery
Women have a thicker subcutaneous fatty layer than men symptoms torn rotator cuff revia 50mg with amex, which helps to insulate them from colder temperatures. Saturated fat is defined as containing carbon atoms that are bound to as many hydrogen atoms as possible becoming saturated with them. The degree of saturation determines how solid the molecule is at various temperatures. These straight fatty acid chains have saturated fat molecules packed closely together at room temperature making them solid. Fatty acid molecules with many double-bonded carbon atoms are called polyunsaturated. Many types of margarines and baked products contain trans fats, which are oils solidified by adding hydrogen atoms at the sites of carbon double bonds. Trans fats are now known to increase risks for heart disease even more significantly than solid animal fats. Oppositely, the omega-3 fatty acids from coldwater fish are known to decrease the risk of heart disease and certain inflammatory diseases. Fatty acid molecules with one double bond between carbon atoms are called unsaturated. Double bonds cause fatty acid chains to form "kinks," meaning they cannot be packed closely enough to solidify. Therefore, triglycerides with either short fatty acid chains or unsaturated fatty acids are oils. Examples include oils from corn, olives, Phospholipids Similar to a fat molecule, a phospholipid consists of a glycerol portion with fatty acid chains. They are structurally related to glycolipids and are actually modified triglycerides. A phospholipid includes a phosphate group that is soluble in water and two molecules of fatty acids. The distinctive chemical properties of phospholipids come from the phosphorus-containing group. The heads of these molecules (the phosphorus-containing part) are polar, attracting other polar or charged particles (including ions or water). The unique phospholipids can be used as the primary material for the building of cell membranes. Steroids Steroid molecules are large, basically flat lipid molecules that share a distinctive carbon framework in comparison with fats or oils. All steroid molecules have the same basic structure: three six-carbon rings joined to one five-carbon ring. Cholesterol is the most important steroid and is ingested in animal foods such as cheese, eggs, and meat. Although essential for human life, excessive cholesterol participates in atherosclerosis and related disease. In the cell membranes, cholesterol is the raw material that helps to synthesize vitamin D, bile salts, and steroid hormones. Eicosanoids Eicosanoids are lipids that are mostly derived from arachidonic acid, a 20-carbon fatty acid existing in all cell membranes, the most important of which are the prostaglandins and related acids. Prostaglandins are important for blood clotting, inflammation, labor contractions, regulation of blood pressure, and many other body processes. Prostaglandin synthesis and inflammatory effects are blocked by medications such as the cyclooxygenase inhibitors and nonsteroidal anti-inflammatory drugs. Explain the most common type of lipids and list the components their molecules contain. It may also be a low level of high-density lipoproteins, which contributes to the development of atherosclerosis. They make up between 10% and 30% of cell mass and are the basic structural materials of the body. On cell surfaces, some proteins combine with carbohydrates to become glycoproteins. Proteins include biologic catalysts (enzymes), contractile proteins of muscles, and the hemoglobin of the blood. Biochemistry 43 There are more than 200,000 types of proteins in the human body, the full set known as the proteome. All proteins contain carbon, hydrogen, oxygen, and nitrogen atoms, with small quantities of sulfur also present. Protein molecules consisting of amino acids held together by peptide bonds are called peptides, which are joined together via dehydration synthesis. Each type of peptide is named for the amount of amino acids that are united: dipeptide (2), tripeptide (3), polypeptide (10 or more), and so on. Although most proteins are macromolecules, polypeptides that contain more than 50 amino acids are called proteins. Macromolecules are large and complex, with as few as 100 to over 10,000 amino acids. The way they bind determines how the proteins they produce are structured and how they function. A change in one amino acid that is linked to others produces an entirely unique function. Types of Proteins Proteins are generally classified as either fibrous or globular. Fibrous proteins are longer and resemble "strands" and are highly stable and insoluble in water. Collagen, the most abundant protein in the body, is a fibrous protein as are elastin, keratin, and some contractile proteins found in muscles. Globular proteins are important in almost all biologic processes and are therefore also referred to as functional proteins. Examples of globular proteins are antibodies, protein-based hormones, and enzymes. Enzymes are catalysts for nearly every chemical reaction taking place in the body. These complex units consist of a nitrogencontaining base, a pentose sugar, and a phosphate group. Severity ranges from subclinical deficiencies to obvious wasting (edema, hair loss, skin atrophy) to starvation. Nucleic acids store and process information at the molecular level inside the cells. Otherwise, biochemical reactions would occur extremely slowly, almost to no effect. Enzyme Characteristics Enzymes Enzymes are globular proteins that promote chemical reactions by lowering the activation energy requirements. Activation energy is the energy that must be overcome for a chemical reaction to occur. Therefore, they make chemical reactions possible and catalyze the reactions that sustain life. In the body, enzymes assist in the digestion of food, drug metabolism, protein formation, and many other types of reactions. Enzymes make metabolic reactions possible inside cells by controlling temperature conditions that otherwise would be too mild for them to occur. They increase the speed of enzymatic reactions greatly, enzyme Enzymes differ in their makeup. Some are only made of proteins, whereas others have a two-part structure, consisting of a protein portion (the apoenzyme) and a cofactor. Enzyme cofactors may be either a metal element ion (such as iron or copper) or an organic molecule that assists the reaction. Most organic cofactors are derived from B (or other) vitamins, in which case they are referred to as coenzymes. Some control one chemical reaction, whereas others regulate a small group of similar reactions by binding to molecules that are only slightly different.


