Cheap verapamil 240mg fast delivery
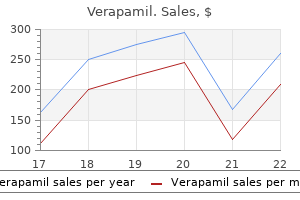
Tissue-preserving operations were defined as a segmentectomy based on Couinaud anatomy or based on the segmental anatomy of the portal vein; classic hepatectomies included formal or extended right or left hemihepatectomies blood pressure units cheap verapamil express. They specifically noted a higher rate of biochemical liver insufficiency, as defined by hyperbilirubinemia, elevated serum ammonia, and prothrombin time prolongation (26% vs. The physiologic advantage of lesser hepatic resection persisted when analysis was confined to noncirrhotic patients (n = 141). Interestingly, more contemporary series failed to demonstrate the same degree of physiologic benefit from parenchymal preservation. In one series that reported perioperative outcomes after 100 posterior sectionectomies and 480 right hepatectomies performed between 2000 and 2012 at multiple institutions, (Fisher and colleagues (2013) found that blood loss, percentage of patients transfused, hospital length of stay, and morbidity and mortality were equivalent between the groups. The relatively high morbidity (42% for all complications) experienced by both groups may speak to the high physiologic impact associated with even a posterior sectionectomy and may explain why few differences were observed between the groups, in contrast to other series where parenchymal preservation included single segmentectomies and smaller wedge resections. However, patients in the parenchymal preservation group experienced a statistically and clinically significant decrease in liver dysfunction (1% vs. Wedge resections should in theory offer even more benefit from parenchymal preservation than segment-based resections. However, there were early concerns that nonanatomic or wedge resections as opposed to strictly anatomic operations based on one or more portal pedicles might be associated with higher blood loss and greater risk of bile leak. For example, Zorzi and colleagues (2006) retrospectively reviewed 300 hepatic resections in 253 consecutive patients who underwent either wedge or anatomic hepatic resection for colorectal liver metastases over a 13-year period. Anatomic resections included segmentectomies, multisegmentectomies, sectionectomies, or segmentectomy plus sectionectomy (see Chapter 2) and were performed for large, deeply situated, or multiple clustered metastases; wedge resection was performed for small, peripheral, and isolated metastases. Median length of stay for both groups was 7 days; there was only one postoperative death after wedge resection (1. By reducing liver failure and decreasing the physiologic impact of surgery, parenchymal-preserving techniques maximize the patient population eligible for surgery. Unfortunately, many patients with malignant hepatic tumors are not candidates for resection because of underlying liver disease or the extent of tumor burden. This includes patients whose liver function will not permit a formal hepatic resection and those with bilobar disease or anatomically challenging lesions such as those deep, centrally located, or involving or threatening major vasculature. These situations can be common in the population referred for surgical evaluation. Zorzi and colleagues (2006), in their review of 300 hepatic resections for colorectal cancer metastases, noted that 43% of patients had multiple metastases and 12% underwent more than one wedge or anatomic resection at surgery. Although they did not comment on the number of patients who would have been ineligible for surgery if parenchymal-sparing techniques had not been employed, this report and other data suggest that a large number of patients stand to benefit from techniques that preserve liver parenchyma and/or allow multiple synchronous resections or staged operations. Biochemical definition of liver dysfunction based on hyperbilirubinemia, elevated serum ammonia, and prothrombin time prolongation. Treatment: Resection Chapter 108A Parenchymal preservation in hepatic resectional surgery: rationale and indications 1635 likely have been ineligible for surgery. While demonstrating the safety of parenchymal-preserving techniques for resection of primary and secondary hepatic malignancy, it is imperative that surgeons demonstrate that these techniques preserve oncologic principles of removing tumor and tumor-bearing tissue with a sufficient margin and in a manner minimizing the risk of local recurrence (see Chapters 103A and 103B). Colorectal liver metastases are histologically wellcircumscribed (Yamamoto et al, 1995). Micrometastases in the surrounding liver parenchyma are rare and primarily found at the immediate tumor border, and satellitosis and Glisson sheath extension are uncommon (Kokudo et al, 2002; Scheele et al, 1995). The series included patients who underwent an extended hepatectomy (18%) and hemihepatectomy (39%), as well as lesser resections. Patients were classified into four subgroups according to the width of the resection margin: positive (tumor <1 mm from surgical margin) or negative (by 1-4, 4-9, or at least 10 mm). With a median follow-up of 29 months, 225 of the 557 patients developed a recurrence (40%). A positive resection margin affected disease-free survival, but sites and incidence of recurrence were similar among patients with a negative margin of resection, regardless of the width of the margin. Median survival also did not differ based on whether the patient underwent an extended hepatectomy, a hemihepatectomy, or less than a hemihepatectomy. In a separate study, oncologic outcomes were examined in a subset of these patients (n = 253) undergoing less than a 1. Survival after hepatic resection of colorectal liver metastases, stratified by margin status. No significant difference in survival was seen in patients with a negative surgical margin, regardless of the width of the margin (all P >. Operative goals were to resect all disease with a margin of microscopically normal tissue. The incidence of isolated intrahepatic recurrence after a wedge resection was only 14% compared to 9% after an anatomic resection (P =. Recurrence at the surgical margin was more common in patients who had a positive resection margin regardless of the type of resection, but margin positivity was equivalent between the groups. The goal of either surgical approach was to removal all intrahepatic tumors with sufficient margins. In a subset analysis of patients with unilobar disease, the authors noted an ipsilateral intrahepatic recurrence rate of 19. Moreover, 90% of patients who had tumor recurrence in the hepatic lobe ipsilateral to their original surgery were resectable in a second operation, with a 5-year survival rate of 58. Recurrences were much less likely to be resectable (20%) among those undergoing more extensive, anatomically based resections (of whom half required hemihepatectomy to clear their initial disease). In this series, operative morbidity and mortality were slightly higher in the anatomic resection group, a finding that was not borne out by the multiinstitutional study (Pawlik et al, 2005; Zorzi et al, 2006). They reported similar overall survival between the two groups and repeat hepatectomy more often after parenchymal-sparing hepatectomy. In the subset of patients who had recurrence in the liver only, anatomic resection was an independent factor of noncandidacy for repeat hepatectomy, and the survival was significantly better in the parenchymal-sparing hepatectomy group. The same appears true for other secondary malignancies of the liver (Billingsley et al, 1998). Although no study has specifically evaluated the prognostic value of margin width, we and other investigators have found that surgical resection versus resection and ablation versus ablation alone does not significantly influence outcomes (Mayo et al, 2010; Saxena et al, 2011). In contrast, anatomic resections that remove the hepatic segment defined by tumor-bearing (Agrawal & Belghiti, 2011; Liau et al, 2004). Five-year disease-free and overall survival were 67% and 28%, respectively, in the segmentectomy and subsegmentectomy group and 35% and 16% in the group undergoing limited resection. The authors attempted to control for this imbalance using multivariable Cox proportional hazards model accounting for other prognostic factors and still found that anatomic versus nonanatomic resection carried a favorable survival benefit. In 2008, Eguchi and colleagues reported long-term results from the Liver Cancer Study Group of Japan, which has been conducting nationwide surveys of patients with primary liver cancer since 1969. With a median follow-up of over 2 years, overall survival appeared to favor anatomic resection (34% survival at 10 years vs. However, diseasefree survival was highest among patients who underwent anatomic resection (40% vs. In these two other studies, choice of operative strategy rested with the surgeon, and minor/nonanatomic hepatectomy was performed more frequently in patients with impaired liver function. Therefore, the definitive nature of survival outcomes in this and other inherently biased retrospective studies (Fuster et al, 1996; Imamura et al, 1999) has been questioned by authors who believe that an uncompromising anatomic resection is not strictly necessary to achieve oncologic goals (Ahn et al, 2013; Torzilli et al, 2005). However, the rationale behind performing anatomically based but parenchymal-sparing operations over more extensive resections must include demonstration that parenchymal-sparing techniques do not put the patient at an oncologic disadvantage by failing to remove "at risk" tissue that can be the source of tumor recurrence. Others have demonstrated similar disease-free and overall survival rates after parenchymal-preserving versus hemihepatectomy and more extensive resections (Kosuge et al, 1993; Imamura et al, 1999; Okada et al, 1994), suggesting that when a margin-negative resection can be achieved by a parenchymal-sparing segmental resection, more extensive operations do not proffer a survival advantage. Surgical approach was based entirely on preoperative evaluation of tumor extent: local E. Extended right or left hepatectomies (n = 66) were performed for lesions invading beyond the confluence of the bile ducts. The vast majority (93%) of segmental resections could be performed with a microscopically clear margin, and 71% of extended resections were margin negative. However, local excision in this series carried a dismal 62% rate of margin positivity and was associated with a poor, 8% 5-year overall survival. Of note, extended hepatectomy was associated with significantly higher morbidity (48% vs. Parenchymal-preserving techniques allow for second, "salvage" operations and for planned two-stage strategies.
Syndromes
- Metabolic alkalosis
- Children: 9 to 23
- Infant may pull into and keep a standing position while holding onto furniture
- Time it was swallowed
- Severe low blood sugar (from insulinomas)
- Liver function tests (especially alkaline phosphatase or bilirubin levels)
- Chronic glomerulonephritis
- Immunoelectrophoresis - urine
- Impetigo
- Have any other people in your family or social group had similar problems?
Buy verapamil 80mg line
Gastrointestinal bleeding in connection with biliary symptoms should arouse the suspicion of biliary tract hemorrhage hypertensive crisis verapamil 80 mg cheap. Biliary colic symptoms are seen in 70% of pateints; and jaundice is identified in up to 60%. All three findings are seen in approximately one quarter of patients with hemobilia (Green et al, 2001). In addition to retained blood clots within the biliary tree producing the signs and symptoms of obstructive jaundice, patients may initially present with ascending cholangitis with accompanying high fever and rigors (Kurisu et al, 2005). The fate of blood in the biliary tree depends on a variety of factors, including the rate of bleeding, the source (arterial or venous), the timing (continuous or intermittent), and the frequency (solitary or recurrent). A sudden onset of massive bleeding, as in a ruptured hepatic artery aneurysm, may produce such a rapid amount of blood that the initial clinical presentation is hematemesis or melena. The formation of clots depends on the quality and the quantity of the bleeding, and their fate depends on whether clots are dissolved, expelled into the intestine, or retained in the biliary tract (Sandblom & Mirkovitch, 1979). When retained, clots act like calculi and can cause symptoms of biliary colic when passing (Clancy & Warren, 1997), jaundice when retained (Baig et al, 2012), cholecystitis if they lodge in the gallbladder (Parekh & Corvera, 2010), and pancreatitis if they obstruct a common channel above the sphincter (Alis et al, 2010). Only rarely do clots remain in the biliary tree long enough to be encrusted and form stones (Luzuy et al, 1987; Olsen, 1982). The actual workup of a patient with suspected hemobilia ultimately depends on the presentation and suspected etiology. It is important to remember that hemobilia may have a delayed presentation and may recur repeatedly over months and years (Ahmad et al, 2010). In some cases the artery also opens into the portal system (Gurakuqi et al, 2008). The arteriographic catheter should not be withdrawn until it has been decided whether embolization of the feeding artery should be considered as treatment. Arteriography is of special value in discovering central liver lesions, which may be difficult or impossible to localize during exploratory laparotomy. Although selective angiography is considered the gold standard for diagnosis in hemobilia, care must be taken in interpreting arteriograms because they may appear normal if the study is performed when there is no active bleeding. Surgical Intervention In 1903, Kehr first demonstrated that ligation of the proper hepatic artery could be successfully used in hemobilia in a case of communication between a hepatic artery aneurysm to the cystic duct. A, Sonogram indicating dense material in the gallbladder, interpreted as microcalculi or inspissated bile. Filling defect in the common duct is caused by a gelatinous bile plug, probably a blood clot that disappeared through the sucker. Chapter 125 Hemobilia and bilhemia 1925 nonoperative approaches (Green et al, 2001; Sandblom, 1972; Yoshida et al, 1987) (see Chapters 21, 27, and 124). However, surgical intervention still has a role in cases where transarterial embolization has failed or where the etiology demands an operative approach. Cholecystectomy done for gallstones and surgical resection for intrahepatic or extrahepatic neoplasms is a suitable approach in patients who are hemodynamically stable with signs and symptoms of hemobilia. The surgical approach involves ligation of the bleeding vessel and/or excising the (pseudo) aneurysm. Intraoperatively, if the bleeding vessel is not appropriately identified, ligation of the right or left hepatic artery can be done with little concern for perioperative necrosis, provided free flow of the respective portal vein is demonstrated to ensure adequate oxygenation of liver parenchyma. The biological response caused by the interaction of the small molecule and its target protein can be described mathematically when the drug dose or concentration is plotted against its biological effect. The term drug target is a general term that refers to any binding site (or sites) that interacts with a drug. This category includes cell surface proteins that initiate physiological signaling cascades in response to neurotransmitters, hormones, cytokines, growth factors, autacoids, or other circulating signals. The first two types of drug targets include molecules involved in neurotransmitter or hormone-initiated cell signaling and/or the regulation of the internal milieu of cells. These targets include molecules that detect chemical signals and initiate a cellular response via activation of signal transduction pathways. The third type of target is generalized and includes biological molecules with any function, often widely expressed in human cells; these targets provide more of a challenge in achieving drug specificity. Drug specificity is a very important pharmacodynamic issue, with the most useful drugs affecting an intended specific cellular function without eliciting untoward effects. A drug may achieve organ or tissue selectivity as a consequence of selective tissue expression of the drug target. Targets represented in the first two groups above regulate specific functions of particular cells and are expressed selectively in various organs, an advantage in achieving a selective response to drugs. These types of molecules represent the primary targets of many drugs in clinical use because the targets themselves have evolved for selective physiological functions. As an example, a limited number of cells in the body express the -adrenergic receptor; thus, -adrenergic receptor antagonists such as propranolol have relatively selective effects. The proton pump inhibitors, such as esomeprazole, inhibit this enzyme by covalent modification of the protein and cause a large decrement in H+ ion secretion. While a small number of drugs, such as osmotic diuretics (Chapter 38), do not work by interacting with macromolecules, the concept of receptors and intracellular enzymes as specific sites of drug action is essential to understanding pharmacology. The specificity of such interactions introduces the concept of molecular recognition. Drug targets must have molecular domains that are spatially and energetically favorable for binding drug molecules with high affinity. It is not surprising that most drug targets are proteins because proteins fold to form three-dimensional structures that could easily be envisioned to complement the structures of drug molecules. The resulting dose- or concentration-response curve is an important pharmacodynamic relationship that dictates how to administer the proper dosage of drug to achieve a therapeutic effect without untoward responses. Covalent bonds require considerable energy to break and are often irreversible when formed in drug-receptor complexes. Ionic bonds are also strong but may be reversed by a change in the intracellular milieu or pH. Most drug-receptor interactions involve multiple weak bonds extended over the surface of a protein that lead to an affinity high enough to be clinically useful. He proposed the idea of specific "side chains" on cells that would interact with a drug, based on mutually complementary structures. Each cell would have specific characteristics used to recognize particular molecules. While simplistic, this lock-and-key analogy still helps explain drug specificity because it emphasizes the idea that the drug and its target must be structurally complementary to recognize each other and allow the small molecule to bind to the macromolecule with high affinity. Understanding the general properties of cellular receptors provides a foundation for an understanding of all drug-target interactions. The sequencing of the human genome has led to the identification of the amino acid sequences and the diversity of the many classes of cellular receptors, both those residing in the plasma membrane and in the cell cytoplasm. These advances have also revealed many new receptors that are potential targets for further pharmaceutical development. Parallel advances in understanding the many signaling systems activated by cell surface receptors have provided a more complete understanding of how a molecule acting at the surface of a cell can regulate cellular function. As many clinically useful drugs activate or inhibit these receptors and signaling systems, the large families of cellular receptors provide a foundation for understanding how drugs can act with biological precision. One concept is that there can be a quantitative relationship between the drug concentration in the fluid bathing the receptor and the subsequent physiological response. The affinity of a drug for its receptor is a measure of the binding constant of the drug for the receptor protein, and the efficacy of the response is a measure of the ability of the drug to activate the receptor and its signaling system. A high affinity means that low concentrations of drug are needed to occupy receptor sites, whereas a low affinity means that much higher concentrations of drug are needed. The concentration-response curve is also influenced by the number of receptors available for binding; in general, activating more receptors can produce a greater response (see Quantitative Relationships). The size, shape, and charge of a drug binding site on a receptor determines its affinity for any of the vast array of chemically different hormones, neurotransmitters, or drug molecules it may encounter. Drug binding to receptors often exhibits stereoselectivity, in which stereoisomers of a drug that are chemically identical, but have different orientations around a single bond, can have very different affinities. A second key concept is that receptors and their distribution in the tissues of the body are a major determinant of the specificity of drug action. A corollary to this concept is that for a receptor to be physiologically relevant, it must receive a signal and be coupled to a downstream signaling system that regulates a key function of the tissue. As an example, histamine H2 receptors can be found on many cells in the periphery, but only in the parietal cells in the stomach do they receive histamine as a signal to stimulate gastric acid secretion.
Discount verapamil 240mg amex
Histamine release from mast cells prehypertension eyes verapamil 240 mg for sale, which can lead to bronchospasm, excessive bronchial and salivary secretions, and hypotension, is a major problem with tubocurarine, but a lesser problem with succinylcholine and mivacurium, and an even smaller problem with the aminosteroids. Approximately 30% of patients receiving atracurium experience significant histamine release, while pancuronium, doxacurium, rocuronium, and vecuronium are devoid of this action and free of cardiovascular effects. Histamine release may also occur with cisatracurium and mivacurium, but no cardiovascular effects are observed at clinical doses. Pancuronium can cause moderate increases in heart rate, blood pressure, and cardiac output as a consequence of sympathomimetic and anticholinergic effects. Dysrhythmias can be induced with the older agents, but the newer agents have greater cardiac safety margins, reducing their cardiac effects. Although nondepolarizing neuromuscular blocking drugs are generally selective for nicotinic cholinergic receptors in skeletal muscle, parasympathetic and sympathetic ganglia can be affected if drug concentrations are sufficiently high. At normal doses, most agents do not exhibit these effects except for tubocurarine, which produces a significant degree of ganglionic blockade. Succinylcholine may stimulate ganglia, resulting in alterations in heart rate and hypertension. Muscarinic effects can be evoked with pancuronium at doses used to produce neuromuscular blockade and with tubocurarine and atracurium at higher doses. Further, the electrolyte content of body fluids can have a major influence on the degree of blockade and consequent adverse effects of succinylcholine, which can release K+ rapidly from many cells. This may pose an unacceptable risk in patients with extensive soft tissue injury because the prolonged depolarization can lead to severe hyperkalemia and result in prolonged apnea or cardiac arrhythmias and arrest if plasma K+ concentrations 13 mM. Drug interactions are known to occur between neuromuscular blockers, anesthetics, Ca++ channel blockers, and some antibiotics. Many volatile anesthetic agents enhance the action of the nondepolarizing neuromuscular blockers by decreasing the open time of the nicotinic receptor. The local anesthetic bupivacaine potentiates blockade by nondepolarizing and depolarizing agents, and lidocaine and procaine prolong the duration of action of succinylcholine by inhibiting butyrylcholinesterase. The administration of succinylcholine with halogenated inhalational anesthetics can precipitate malignant hyperthermia in genetically susceptible patients. This reaction, which is manifest by sustained muscle contraction, an increased O2 consumption, and an increased body temperature, is a pharmacogenetic disorder and results from the failure of the sarcoplasmic reticulum to resequester Ca++. Malignant hyperthermia is rare, with the highest incidence following the combined use of halothane and succinylcholine (Chapter 26). However, it is a potentially life-threatening situation and, if untreated, may prove fatal. Treatment involves cessation of drug administration, rapid cooling, and administration of dantrolene. Ca++ channel blockers, many antibiotics, and, to a lesser extent, -adrenergic receptor blockers potentiate neuromuscular blocking drugs. The duration of action of vecuronium, pancuronium, doxacurium, and pipecuronium is reduced in patients taking the anticonvulsants phenytoin or carbamazepine because these agents decrease the affinity of nicotinic receptors for neuromuscular blockers and increase the number of receptors on muscle fibers. In addition, the duration of action of vecuronium is prolonged in patients treated with cimetidine. Naturally, neuromuscular blocking agents must be used with caution in patients with neuromuscular disorders, such as myasthenia gravis or Lambert-Eaton myasthenic syndrome. Genetic variations in butyrylcholinesterase activity, resulting in either lower concentrations of normal enzyme or an abnormal enzyme, may also lead to prolonged actions of succinylcholine. A clinically effective dose of succinylcholine in healthy patients produces neuromuscular blockade lasting <15 minutes; in a patient with a variant of this enzyme with decreased effectiveness, the same dose may last much longer. Ganglionic Blocking Drugs the adverse effects of the ganglionic blocking agents represent an extension of their pharmacological actions and include dry mouth, tachycardia, constipation, and urinary retention, as well as excessive hypotension and impotence. The major adverse effects associated with the use of the neuromuscular and ganglionic blocking agents are summarized in the Clinical Problems Box. In recent years, the search for new neuromuscular relaxants has concentrated on developing drugs with a rapid onset and shorter and more predictable duration of action with minimal side effects. These drugs can produce effects that may impact nursing care or physical or occupational therapy in certain settings. Understanding the actions of these agents will help provide awareness of the potential impact of these agents on the care provided. The general anesthetic halothane was administered with succinylcholine to a surgical patient, and shortly thereafter the patient exhibited sustained muscle contractions, an elevated temperature, and tachycardia. The patient has a butyrylcholinesterase mutation leading to decreased enzyme activity. What would you expect to see in an individual given the ganglionic blocker mecamylamine At low doses, tubocurarine blocks only nicotinic receptors at the neuromuscular junction, whereas mecamylamine blocks only nicotinic receptors at autonomic ganglia because: A. Ganglionic nicotinic receptors are different from skeletal muscle nicotinic receptors. Neuromuscular blockade in the 21st century management of the critically ill patient. The consequences of activation of the sympathetic nervous system are best characterized by the phrase "flightor-fight" response, which helps predict the types of physiological responses caused by both stimulation of this system and the use of sympathomimetic (mimicking sympathetic responses) pharmacological interventions. The physiological consequences of sympathetic activation include increasing heart rate and cardiac contractility to elevate cardiac output, shifting blood flow from internal organs not critical for fight or flight. Additional relevant physiological changes include bronchodilation to increase airflow and consequently enhanced gas exchange. Epi itself is considered the fight-or-flight hormone and activates all adrenergic receptor subtypes-that is, 1, 2, 1, 2, and 3. Sympathomimetics may exert their effects by binding directly to adrenergic receptors (direct-acting agonists), by elevating endogenous catecholamines (indirect-acting agents), or via both mechanisms (mixedaction agents). In general, these drugs are used clinically for disorders in which mimicking the fight-or-flight response helps improve or provide relief from the underlying disease. Most adrenergic receptor agonists, with the exception of 2 agonists, function as sympathomimetics. The therapeutic use of these agents is dictated primarily by the specific receptor subtype(s) with which they interact. Clinically important sympathomimetic effects in a specific organ or tissue can be achieved without a major disruption in the function of other organs or tissues because the distribution of adrenergic receptor subtypes varies by organ and tissue. For example, 1-adrenergic receptor agonists, such as phenylephrine, are useful for promoting vasoconstriction to decrease nasal congestion without direct effects on the heart. In contrast, -selective agonists, such as isoproterenol, are preferred when increased cardiac contractility is desired and vasoconstriction would be detrimental, such as ionotropic support in heart failure. Similarly, due to the distribution of 2-adrenergic receptors, drugs that selectively activate these receptors, such as albuterol, promote bronchodilation without having significant cardiovascular effects. The consequences of activation of the sympathetic nervous system are best characterized by the phrase "flight-or-fight" response, which facilitates predicting the types of physiological effects caused by stimulation of this system and by pharmacological interventions that are sympathomimetic. The physiological effects are geared toward satisfying increased tissue O2 and energy requirements and concomitant cardiovascular demand. Both heart rate and cardiac contractility are increased to elevate cardiac output, blood flow is shifted from internal organs not critical for fight-or-flight to skeletal muscle, and energy is made available via increased metabolism. Moreover, there are other physiological changes pertinent to fight or flight, such as bronchodilation and activation of sudomotor pathways. Drugs that facilitate or mimic the actions of the sympathetic nervous system are called sympathomimetics, adrenomimetics, or adrenergic agonists. Sympathomimetics may exert their effects by binding directly to adrenergic receptors (direct acting;. These drugs are generally used clinically for disorders in which mimicking the fight-or-flight response helps to improve the condition or provide relief for the underlying disease. The therapeutic use of these sympathomimetics is primarily dictated by the specific receptor subtype(s) with which they interact. Adrenergic agonists are useful in a variety of clinical settings, ranging from treatment of cardiogenic shock to palliative treatment in asthma. This article will discuss the physiological effects of activating different adrenergic receptor types, the drugs that act on these receptors, and the therapeutic uses of these drugs. Of these, only four receptors (1, 2, 1, and 2) are important in current clinical pharmacology. In contrast, propranolol, a competitive antagonist at both 1 and 2 receptors, causes a parallel shift to the right of responses mediated by both cardiac 1 receptors and bronchial 2 receptors without affecting the 1 receptor response.
Buy generic verapamil 240mg on-line
Shibata T blood pressure for athletes generic 120mg verapamil otc, et al: Small hepatocellular carcinoma: is radiofrequency ablation combined with transcatheter arterial chemoembolization more effective than radiofrequency ablation alone for treatment Takayasu K, et al: Superselective transarterial chemoembolization for hepatocellular carcinoma. Woo S, et al: Chemoembolization of extrahepatic collateral arteries for treatment of hepatocellular carcinoma in the caudate lobe of the liver, Cardiovasc Intervent Radiol 2014. The techniques used in this field are targeted to the tumors to allow delivery of toxic chemotherapeutic, radiotherapeutic, and thermal doses with minimal toxicity to normal structures; this minimizes the systemic toxicity associated with these therapeutic options and allows delivery of doses to the tumor that would not be possible by using systemic delivery methods. In this article, the general concepts associated with radioembolization and its specific use in different primary and secondary malignancies of the liver will be discussed (Table 96B. Hepatic Artery the proper hepatic artery that supplies the liver is a continuation of the common hepatic artery, a branch of the celiac trunk. The proper hepatic artery branches into the right and left hepatic arteries, which supply the corresponding lobes of the liver. The cystic artery supplying the gallbladder usually arises from the right hepatic artery, and the right and left hepatic arteries give rise to the segmental branches; these eventually branch into the small vessels found in the portal triads. Unlike the normal hepatic parenchyma, liver tumors are supplied primarily by hepatic arterial blood and are hypervascular structures compared with the surrounding uninvolved parenchyma (see Chapters 18 and 19). Hepatic tumors may parasitize arterial blood flow from the arteries that supply segments adjacent to the segment the tumor is in and those of surrounding organs, such as the stomach. This relative arterial hypervascularity of the tumors with respect to the normal parenchyma has been the basic principle behind transarterial therapies for targeting liver tumors. Conformal-beam therapy, which uses a threedimensional approach rather than broad axial plane techniques, has been shown to minimize the toxicity to normal hepatic parenchyma (Dawson et al, 1999). However, even with the use of conformal-beam therapy, the radiation delivered to normal hepatic parenchyma limits the maximum dose that can be delivered to the tumor without compromising safety. External-beam radiation has limitations in treatment of liver tumors in specific locations; this includes tumors near the dome of the liver, which carry the risk of exposing the lungs to radiation and increasing the risk of radiation pneumonitis, and tumors in the caudate lobe in close proximity to the porta hepatis, where risk of damage to the major biliary and vascular structures is a consideration. Dose fractionation, dose delivery to the tumor in fractions, is beneficial in targeting radiosensitive and radioresistant malignant cells at different sessions, but multiple treatments are required. Respiratory movement must be considered to minimize the incidence of normal tissue complications, although recent advances in the technology of external-beam radiation have been shown to increase safety and efficacy of this technique, such as stereotactic body radiotherapy, proton radiotherapy, and carbon ion radiotherapy; these are establishing the role of external-beam radiotherapy in the management of liver tumors (Dawson & Guha, 2008; Fukumitsu et al, 2009; Nomiya et al, 2008). Radioembolization Given the distinct vasculature of hepatic tumors described earlier, radioembolization provides a mode of delivering localized radiotherapy to the tumor. A radiation dose of as much as 150 Gy can be administered, minimizing the complications of external radiation. Radioembolization has been shown to have promising outcomes in primary and secondary hepatic malignancies by numerous investigators. Their study consisted of a small number of patients but showed a favorable response, observed by the reduction in size of palpable masses. A dose-escalation study on animals was performed, which formed the basis of the Phase I dose-escalation evaluations in humans (Wollner et al, 1987). Shepherd and colleagues (1992) conducted a Phase I dose-escalation study using 90Y microspheres in 10 patients. In contrast to earlier studies, none of the patients in this study experienced hematologic toxicity, a fact that emphasizes the value of assessing angiographic findings and extrahepatic shunting before treatment (Shepherd et al, 1992). The technical aspects of dosimetry, radioassays, safety, and efficacy were discussed by many studies that followed (Andrews et al, 1994; Yan et al, 1993). Lau and colleagues (1994) showed that tumor response was proportional to the dose delivered, with improved survival in patients receiving more than 120 Gy. The patency of the portal vein and the presence of arterioportal shunting are assessed. The inadvertent spread of the microspheres is prevented by a meticulous study of the vascular anatomy of the liver and collateral nontarget flow (Covey et al, 2002). Coil embolization of nontarget vessels may be necessary to decrease the unintended deposition of microspheres. Some examples of vessels that may need to be embolized are inferior esophageal, left inferior phrenic, accessory left gastric, supraduodenal, and retroduodenal arteries. The minimal incidence of complications following coil embolization and the grave clinical consequences associated with the inadvertent deposition of microspheres in the stomach, duodenum, or pancreas favor prophylactic coil embolization before radioembolization in select cases. This pretreatment nuclear scan is important to prevent certain complications associated with the treatment. All hepatic vessels are assessed during the angiogram, and the arteries feeding the tumor are studied in detail. As the tumor may parasitize blood flow from surrounding vessels, it is necessary to study its vascular supply in detail. Failure to recognize a vessel supplying the tumor may lead to the incomplete targeting of the lesion and treatment failure. Laboratory Workup the laboratory workup is important to assess the pretreatment functional status of the liver. Pretreatment Angiography and Coil Embolization Radioembolization requires pretreatment diagnostic mesenteric angiography (see Chapter 21). B, Schematic representation of radiation segmentectomy with highly radioactive particles preferentially accumulating in the tumor because of its arterial hypervascularity and microspheres accumulating in the surrounding parenchyma of the injected segments. Vials of six different activities are available; the only difference in the vials is the number of spheres; 1. The activity of the vial varies inversely with the time elapsed after calibration. The calculation of the dose requires the use of three-dimensional reconstruction of the target site to calculate the volume of the liver to be infused. The volume in cubic centimeters is then used to calculate the mass in grams by multiplying it by a factor of 1. As suggested by the small particle size, the embolic effect of the available microscopic spheres is minimal. They are known to lodge in the precapillary arterioles, but their small size also allows deep penetration into the tumor with minimal changes in the vascular supply to the tumor. The partition method is seldom used, because it is applicable only in special circumstances. The procedure is performed on an outpatient basis, and the patient is discharged on the same day (Salem et al, 2002). New Concepts Radiation Segmentectomy Recently, the concept of radiation segmentectomy has been discussed.
Buy discount verapamil 120 mg
It has been termed hemobilia (Sandblom blood pressure under stress order verapamil cheap, 1948) from the Greek haima ("blood") and the Latin bilis ("bile"). Causes of hemobilia include iatrogenic and accidental trauma, gallstones, inflammation, vascular disorders, and neoplasms. With the increasing use of invasive diagnostic and therapeutic procedures involving the biliary tract, iatrogenic trauma has become the predominant etiology of hemobilia (see Chapters 21, 27, 30, 52, 122, and 124). Major, profuse hemobilia is a rare but sometimes lifethreatening complication of liver or biliary tract disease or trauma. Minor hemobilia occurs more frequently but rarely is of long-lasting clinical significance. With the advent of interventional radiologic approaches, treatment of symptomatic hemobilia has shifted from surgical therapy to selective transcatheter hepatic arterial embolization (see Chapters 21, 27, and 124). Surgical therapy through partial hepatectomy, hepatic artery ligation, or a combination of both procedures is rarely necessary and reserved for patients in whom the hepatic arterial branches cannot be safely or adequately embolized because of anatomic or technical reasons, or for patients who have large intrahepatic hematomas and/or sepsis. In 1777, Antoine Portal presented a case in which he made the diagnosis before the death of the patient and confirmed it at autopsy. In this early treatise, Portal (1813) drew attention to the difficulty of finding the source of hemorrhage in the biliary tract, "when they are slight in quantity and occur but seldom," and to the risk of mistakenly tracing them to a healthy organ, a mistake that has been made repeatedly in the history of hemobilia. The first published case in North America was by a Boston surgeon, Jackson (1834), who reported on the clinical and pathologic consequences of an "aneurysm of the hepatic artery bursting into the hepatic duct," the first direct observation of an abnormal communication between the blood vessels and biliary ducts (see Chapter 124). Other, less common causes include nematodes, blood coagulation defects, choledochal cysts, pancreatitis, and portal hypertension. In one of the first publications devoted solely to hemobilia, Sandblom (1972) reported on 355 cases of hemobila reported before 1972, with the largest number secondary to accidental trauma. Over the next 30 years, iatrogenic trauma surpassed all other causes of hemobilia and currently is responsible for the majority of cases (Green et al, 2001; Yoshida et al, 1987). The increase in hemobilia caused by iatrogenic trauma parallels the advent and increasing use of both diagnostic and therapeutic instrumentation of the biliary tract. From there it is either impelled upwards through reverse peristalsis or downwards the normal way" (Glisson, 1654). Over a century elapsed before the subject of hemorrhage into the biliary tract was addressed again. The incidence of clinically significant hemobilia after percutaneous liver biopsy is between 0. Francis Glisson (1957-1677) gave the first account (1654) of hemorrhage into the biliary tract in his treatise Anatomica Hepatis. Previous studies demonstrated the risk of hemobilia after percutaneous liver biopsy may be greater in patients with chronic liver disease because of the presence of ascites, coagulopathy, or platelet dysfunction and following liver transplant (Jabbour et al, 1995; Piccinino et al, 1986). However, a recent study of 2740 percutaneous liver biopsies in patients with advanced chronic liver disease (cirrhosis) determined that only an elevated international normalized ratio above 1. Percutaneous transhepatic stent placement produced a large, subcapsular hepatic hematoma and hemobilia. Correction of coagulopathy should also reduce the development of clinically significant hemobilia (Hines et al, 1972). Other potential risk factors, including absence of biliary dilation, cirrhosis, ascites, and extensive hepatic tumor burden, do not appear to be predictive of hemobilia. The development of a hepatic artery pseudoaneurysm may precede the clinical manifestations of hemobilia by several weeks because of a delayed presentation. Therefore, a high degree of clinical suspicion and accurate history taking often are needed to diagnose hemobilia accurately (see Chapter 21). The advent of laparoscopic cholecystectomy for treatment of choleliathiasis and cholecystitis was originally feared to produce an increased incidence of hemobilia secondary to vascular injury, specifically to the right hepatic artery, within the porta hepatitis (see Chapter 35). Stewart and colleagues (1995) reported five cases of hemobilia following the advent of laparoscopic cholecystectomy, four of which were the result of traumatic aneurysm of the right hepatic artery. A large registry of 77,604 cases of patients undergoing laparoscopic cholecystectomy demonstrated that significant vascular injury was seen in only 0. It appears that the potential fear of increased incidence of hemobilia after laparoscopic cholecystectomy was overstated and most likely secondary to the learning curve of laparoscopic surgery. Surgical procedures and instrumental exploration of the intrahepatic ducts may damage the walls, with great risk of hemorrhage. Minor bleeding constantly accompanies such procedures, but the hemorrhage generally ceases spontaneously, and the resulting clots promptly dissolve. As in other types of traumatic hemobilia, there may be a considerable interval between the trauma and the bleeding episode. However, minor intraductal bleeding can result in confusing temporary postoperative jaundice. It ruptured into the biliary tract and caused exsanguinating hemobilia, diagnosed through duodenal endoscopy and treated successfully with embolization. Typically, hemobilia following liver transplant is secondary to a percutaneous liver biopsy. If hemobilia does occur in this setting, only selective embolization, as described later, should be used out of concern for periprocedural hepatic necrosis, ischemic biliary stricture, or sepsis. Nonsurgical management of blunt liver trauma in hemodynamically stable patients has become the standard treatment and is successful in 50% to 80% of patients (Carrillo et al, 1998; Forlee et al, 2004). The incidence of hemobilia after major liver injury has been reported to be as high as 3% (Merrell & Schneider, 1991), but in other reports the overall incidence is less than 0. The clinical manifestations of blunt trauma to the liver depend on the anatomic site of damage. Tearing or injury to the liver capsule without deep parenchymal injury typically results in intraperitoneal hemorrhage and is managed with emergent operative exploration. Deep parenchymal injury or a central rupture may leave a large cavity into which damaged bile ducts and blood vessels drain. The resulting biloma or hematoma may continue to expand while liver healing is impaired. If operation for blunt liver trauma is necessary, careful exploration of central injuries should be performed to ensure adequate hemostasis and ligation of biliary radicles before use of packs to control bleeding. The conservative management of liver injuries has not resulted in an increase in the incidence of hemobilia after accidental trauma (Carrillo et al, 1998). In a series of 135 patients with severe liver injuries managed nonoperatively, only two developed hemobilia (Carrillo et al, 1999). Other causes of accidental trauma resulting in hemobilia include injury to the gallbladder, occurring in up to 2% of patients with blunt abdominal trauma (Erb et al, 1994). Neoplasms Neoplasms account for only about 5% of all cases of major hemobilia (Green et al, 2001; Sandblom, 1972; Yoshida et al, 1987). Primary and secondary malignant neoplasms of the liver, bile ducts, gallbladder, and pancreas can all present with hemobilia when the tumors invade the biliary system (see Chapters 49-51 and 91-94). The rate of blood loss is rarely rapid and in most cases produces a slow onset of microcytic anemia. Malignant tumors are three times more likely to cause hemobilia than benign tumors. Liver metastases rarely cause hemobilia; similarly, hemobilia is infrequently a sequela of primary cancers in the liver (Kitagawa et al, 1999). Hemobilia has been described from metastases in such rare locations as the gallbladder wall (Sadamori et al, 2012) and from melanoma in the ductal mucosa (Qu et al, 2003). In cases of hemobilia caused by malignant tumors in the gallbladder (HernandezCastillo et al, 2002), the bleeding is most marked if the tumor grows in a polypoid fashion (Strauss, 1929). In the bile ducts, benign adenoma (Teter, 1954), polyps, or polyposis has a protracted course of hemobilia.
Yucca angustifolia (Yucca). Verapamil.
- Dosing considerations for Yucca.
- Are there safety concerns?
- Arthritis, migraines, digestive disorders, diabetes, high blood pressure, high cholesterol, high triglycerides, poor blood circulation, skin problems, and other conditions.
- How does Yucca work?
- What is Yucca?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96718
Generic verapamil 240mg online
Advances in perioperative care of the donor and recipient blood pressure for men purchase verapamil 240mg on-line, organ preservation methods, and surgical techniques have resulted in a 5 year overall survival of 78% for all recipients (Kim et al, 2015). Although gains during the last 40 years in the field of hepatic transplantation are notable, many limitations remain, not the least of which is the relatively fixed pool of cadaveric organ donors. Specialized transplant techniques include living-related-donor liver transplantation and split-liver transplant (see Chapters 117 and 119, respectively). The improvement in patient outcome has led to an expansion in the indications for transplantation and a concomitant increase in the number of patients referred to transplant centers and listed for transplantation (see Chapter 112). Historically, the donor-to-recipient disparity leads to longer waiting times and worsening medical status, with a peak waiting list attrition rate of 187 per 1000 patient-years at risk in 1999. This rate declined by 15% and has remained steady at approximately 160 per 1000 patient-years at risk (Kim et al, 2015; Thuluvath et al, 2010). Because of the limited supply of donor organs, appropriate recipient and donor selection is paramount to improve resource use and long-term outcome. More than 80% of liver transplantations are for noncholestatic liver disease, of which the most common etiologies are viral hepatitis (25%) and alcoholic cirrhosis (20%) (Kim et al, 2015). Persistent disparity between patients on the waiting list and recipients of deceased-donor and living-donor allografts. Biliary atresia is the most common indication for liver transplantation in patients younger than 18 years (Busuttil et al, 2005; Goss et al, 1998). Further, severe morbid obesity is associated with an increased risk of infectious complications and posttransplantation malignancy (Dick et al, 2009). Patients with renal insufficiency or renal failure secondary to hepatorenal syndrome or patients with chronic kidney disease may benefit from simultaneous liver-kidney transplantation; 8. The recipient selection process has undergone extensive revisions to ensure objective and equitable allocation of a scarce resource (cadaveric donor livers) while attempting to avoid futile transplantation. Waiting lists grew under this system, and it became evident that these parameters were inadequate measures of disease severity. In 1999, the Institute of Medicine proposed that instituting a continuous disease severity score based on medical urgency over waiting time could improve the allocation of cadaveric livers for transplantation (Freeman et al, 2002). Special considerations for certain subsets of patients with liver disease are ongoing. Since 2002, the number of patients on the waiting list with exception points for any condition has more than doubled, with close to 900 on the list in 2008 (Thuluvath et al, 2010). The theoretic ideal donor is an otherwise healthy, hemodynamically stable young person who suffers an irreversible cerebral insult that results in brain death; restriction to the use of ideal donors fails to meet the demands of an ever-expanding waiting list (Feng et al, 2006). Special consideration must be given to recipient selection because a sicker recipient might not tolerate a period of slow graft function or ischemia reperfusion injury to the same extent as a healthier recipient. Carefully selected older donor grafts (including septuagenarians and octogenarians) have been used with good success (Chapman, 2015; Feng & Lai, 2014). Although liver allografts with 30% to 60% steatosis are used in select groups of recipients, greater than 60% steatosis significantly increases the risk of primary nonfunction (Urena et al, 1999). The disadvantages include morbidity and rare mortality in the donor population (Brown et al, 2003). Graft survival rate improves when donor warm-ischemia time is less than 30 minutes and cold-ischemia time is less than 10 hours (Mateo et al, 2006). Based largely on the initial body of work by Starzl and colleagues, this section describes the surgical procedures commonly used at Washington University in St. Donor Hepatectomy Management of a cadaveric organ donor begins preoperatively, immediately after identification of a candidate and after evaluation by trained transplant coordinators. After brain death, severe physiologic derangements can occur, and physiologic instability increases in proportion to the length of time between declaration of death and organ procurement (Nygaard et al, 1990). The progression from brain death to somatic death results in the loss of 10% to 20% of potential donors (Wood et al, 2004). Intravascular volume repletion to normovolemia is the cornerstone of management; however, vasopressors or inotropic agents often are necessary to achieve an adequate perfusion pressure. The use of low-dose arginine vasopressin allows a reduction in the dosing of -adrenergic agents, which may impair end-organ perfusion (Pennefather et al, 1995). A thorough review of the medical management of potential organ donors can be found elsewhere (Wood et al, 2004). Surgical techniques for procuring abdominal organs from brain-dead, heart-beating donors have been described previously (Farmer et al, 2001; Merkel et al, 1972; Starzl et al, 1984, Chapter 116 Orthotopic liver transplantation 1805 1987). A midline incision from the suprasternal notch to the pubis is performed, followed by sternotomy and entry into the peritoneum. The abdomen is inspected for any evidence of malignancy or gross gastrointestinal ischemia, which would preclude transplantation. Procurement proceeds in several phases: warm dissection and cannulation, exsanguination with cold perfusion and organ removal, and back-table dissection and organ preparation. In the warm-dissection phase, the liver is mobilized by dividing the umbilical, falciform, and left triangular ligaments. Hepatic arterial anatomy is delineated by inspection of the gastrohepatic ligament and porta hepatis to identify aberrant arterial anatomy. A right medial visceral rotation, or CattelBrasch maneuver, is performed, by which the right colon and mesentery of the small intestine are mobilized and reflected toward the donor left upper quadrant. The infrarenal aorta is exposed at the bifurcation, and proximal and distal control is obtained. The inferior mesenteric vein is identified, controlled, and cannulated for subsequent portal perfusion. Next, the intestinal contents are returned to the lower abdomen with attention turned again to the porta hepatis. The distal common bile duct is circumferentially dissected, distally ligated, and transected. The gallbladder is flushed out through a choledochotomy to clear bile from the gallbladder and biliary tree to potentially limit injury to the bile duct epithelium. After reflection of the left liver medially, control of the supraceliac aorta is obtained, facilitated by dividing the diaphragmatic crura. When the thoracic and abdominal teams are ready, the donor is exsanguinated through the suprahepatic vena cava. The donor abdomen is packed with ice slush for topical cooling during the flushing phase. After satisfactory cooling and flushing with preservation solution, the portal dissection is initiated. The general goals of this dissection are to delineate the arterial anatomy and dissect the arterial inflow back to the aorta. The diaphragm and all tissues between the right kidney and liver are divided, and the hepatic graft is removed from the donor and packed in ice. The final preparation of the donor graft usually occurs at the recipient hospital and is a cold, back-table preparation of the arterial and venous cuffs. In the controlled setting, the donor is brought to the operating room, and support is withdrawn. Heparin is administered to reduce risk of thrombus formation in the graft (Bernat et al, 2006). Apnea and cessation of circulation ensue after a variable amount of time, at which point of death is declared. Circulation is unlikely to resume after 2 minutes of complete cessation; a minimum waiting period of 2 minutes is required, and a 5-minute interval between asystole; pronouncement of death before further intervention is strongly encouraged (Bernat et al, 2006). The goal now becomes rapid reperfusion of the organs for procurement with cold preservation solution; this usually is accomplished by a quick midline laparotomy and cannulation of the aorta. Alternatively, some centers use cannulae placed before death in the femoral artery and vein. Less than 30 minutes of donor warm-ischemia time is generally considered acceptable (Bernat et al, 2006). Hepatectomy is performed as in a standard brain-dead donor, usually followed by a back-table flush.
Generic verapamil 240 mg on line
Blood cell counts are required for individuals prescribed clozapine because this agent can lead to: A prehypertension triples heart attack risk buy 240 mg verapamil amex. Dopamine, the antipsychotic molecule: a perspective on mechanisms underlying antipsychotic response variability. Towards a unified understanding of lithium action in basic biology and its significance for applied biology. It is characterized by feelings of sadness, anxiety, guilt, and worthlessness; disturbances in sleep and appetite; fatigue and loss of interest in daily activities; and difficulties in concentration. Symptoms of depression can last for weeks, months, or years, and depression is a major cause of morbidity and mortality. In any given year, nearly 10% of the population (almost 20 million adults in the United States) suffers from a depressive illness, and depression is a factor in more than 40,000 suicides per year in the United States, making it one of the most widespread of all life-threatening disorders. Although depression can affect any age, the current mean age of onset is 25 to 35 years. Of particular concern is the rate of depression and suicide among children, adolescents, and the aged, which is increasing at an alarming pace and often goes unrecognized. Depression is a symptom of many different illnesses and may arise as a result of substance abuse (alcohol, steroids, cocaine, etc. Three of the most important psychiatric illnesses that present with depressive symptoms are major depressive disorder (also referred to as unipolar depression), persistent depressive disorder (formerly termed dysthymia), and bipolar disorder (Chapter 16). Major depressive disorder may be totally disabling (interfering with work, sleeping, and eating), and episodes may occur several times during a lifetime. Persistent depressive disorder is less severe and involves long-term chronic symptoms that do not disable totally but keep a person from functioning at his or her highest level. Although the molecular and cellular etiology of depression remains unknown, it is generally accepted that depression involves impaired monoaminergic neurotransmission, leading to alterations in the expression of specific genes. In addition, postmortem and imaging studies have demonstrated neuronal loss and shrinkage in the prefrontal cortex and hippocampus in depressed patients, alterations that could be tempered by antidepressants. Within the past several years, as evidence of adult neurogenesis has become increasingly clear, the idea has emerged that depression may be caused by impaired neurogenesis in the adult hippocampus. Studies have demonstrated that new neurons can proliferate from progenitor cells in the hippocampus, a process impaired by stress and stress hormones such as the glucocorticoids and enhanced by antidepressants. Furthermore, it has been shown that neurogenesis is required for antidepressants to exert their behavioral effects in laboratory animals. Thus impaired monoaminergic transmission in specific brain regions may lead to a decreased expression of transcription or growth factors required for sustaining neurogenesis, dendritic branching, and synaptic connections, resulting in depression. Major depressive disorder, persistent depressive disorder, and the depression associated with anxiety disorders are treated with compounds classified as antidepressants. These compounds include the tricyclic antidepressants, the serotonin selective reuptake inhibitors, norepinephrine reuptake inhibitors, serotonin/norepinephrine reuptake inhibitors, multiaction agents, and monoamine oxidase inhibitors. Although the specific sites of action and neurotransmitter selectivity differ for these agents, they all increase monoaminergic neurotransmission in the brain. Anxiety is a pervasive feeling of apprehension, characterized by diffuse symptoms such as feelings of helplessness, difficulties concentrating, irritability, and insomnia and is manifest by somatic symptoms including gastrointestinal disturbances, muscle tension, excessive perspiration, tachypnea, tachycardia, nausea, palpitations, and dry mouth. Both the benzodiazepines and nonbenzodiazepine drugs are used to treat anxiety disorders. The term anxiety refers to a pervasive feeling of apprehension, characterized by diffuse symptoms such as feelings of helplessness, difficulties concentrating, irritability, and insomnia. Anxiety is also manifest by somatic symptoms including gastrointestinal disturbances, muscle tension, excessive perspiration, tachypnea, tachycardia, nausea, palpitations, and dry mouth. Anxiety disorders are chronic and relentless, can progress if not treated, and include panic disorder, obsessive-compulsive disorder, social phobia, social anxiety disorder, generalized anxiety disorder, and specific phobias. Although posttraumatic stress disorder was classified as an anxiety disorder for many years, it has been reclassified as a "trauma and stressor-related disorder. Depression often accompanies anxiety disorders, and when it does, it should be treated. However, at other times, symptoms may be severe enough to cause considerable distress. When patients exhibit anxiety so debilitating that lifestyle, work, and interpersonal relationships are severely impaired, they may require drug treatment. Although these compounds may be of great benefit, concurrent psychological support and counseling are absolute necessities for the treatment of anxiety and cannot be overemphasized. Both benzodiazepine and nonbenzodiazepine drugs are used to treat anxiety disorders, with the benzodiazepines the most commonly prescribed anxiolytics in the United States. Before the introduction of these compounds in the 1960s, the major drugs used to treat anxiety were primarily sedatives and hypnotics, including barbiturates, compounds with potent respiratory depressant effects that led to a high incidence of overdose and death. Although the benzodiazepines are not devoid of side effects, they have a wide margin of safety, with anxiolytic activity achieved at doses that do not induce clinically significant respiratory depression. The nonbenzodiazepine anxiolytics include buspirone and -adrenergic receptor antagonists; many antidepressants are also approved for the treatment of anxiety. The characteristics and treatment of depression and anxiety are summarized in the Therapeutic Overview Box. This group of agents includes the primary amines amitriptyline, clomipramine, doxepin, and imipramine, and the secondary amines desipramine and nortriptyline. Multiaction Agents the multiaction compounds, often referred to as atypical antidepressants, represent a very heterogeneous group and include bupropion, mirtazapine, nefazodone, trazodone, and vortioxetine. In addition, stimulation of 1-adrenergic receptors on serotonergic cell bodies and dendrites increases their firing rate. Interestingly, chronic antagonism of these receptors leads to their paradoxical down regulation, although the role of this mechanism in mediating the antidepressant actions of these compounds remains to be elucidated. The contribution of these actions to the antidepressant efficacy of this compound is not yet understood. Although ketamine and esketamine (the S-enantiomer of ketamine) are not approved for depression at the time of preparation of this chapter, it is expected that esketamine will obtain approval for the treatment of depression with suicidal ideation in 2018. Anxiolytics Anxiety may be treated with the benzodiazepines, buspirone, -adrenergic antagonists such as propranolol, and several antidepressants. Benzodiazepines bind to one of these modulatory sites, often referred to as the benzodiazepine binding site or benzodiazepine receptor. Barbiturates bind to another allosteric site, while compounds such as the poison picrotoxin bind to other sites on the receptor. The -carbolines, such as harmine and harmaline, which occur widely throughout the plant and animal kingdoms, also interact with the benzodiazepine binding site. The inverse agonists block the effects of the benzodiazepines but have no therapeutic use. Rather, they are thought to be responsible for the psychedelic properties of some plant species. Rather, flumazenil competitively antagonizes the actions of the benzodiazepines and is used therapeutically to treat benzodiazepine overdose. Flumazenil also competitively antagonizes the effects of the inverse agonists and the benzodiazepine receptor agonists because they also bind at the same allosteric site. It is as effective as the benzodiazepines as an anxiolytic but does not have anticonvulsant, muscle relaxant, or sedative effects. The -adrenergic receptor antagonists, such as propranolol (Chapter 12), are useful for the short-term relief of anxiety, such as for the treatment of performance anxiety. These agents are competitive antagonists at all -adrenergic receptors and suppress the sympathetically mediated somatic and autonomic symptoms of anxiety. The mood-elevating properties of antidepressants are associated with a blunting or amelioration of the depressive state, such that there is an improvement in all signs and symptoms of depression, although rates of improvement of individual symptoms may differ. A major problem, however, is that it takes several weeks for the maximal therapeutic benefit of these compounds to become apparent. This limitation is particularly disturbing given the potential for depressed patients to commit suicide, underscoring the clinical importance of esketamine for immediate treatment. Esketamine was granted a "breakthrough therapy designation" by the United States Food and Drug Administration in 2013 for treatment-resistant depression and in 2016 for depression with an imminent risk for suicide. Although the antidepressants facilitate monoaminergic transmission immediately, their therapeutic efficacy may not be evident for several weeks.
Purchase cheap verapamil online
The technical goals in biliary reconstruction are to achieve a tension-free anastomosis between viable ducts or intestine pulse pressure of 10 cheap verapamil 80 mg line. The method used depends on many factors, including the size match of the donor and recipient common bile duct and the presence of preexisting biliary pathology. Choledochojejunostomy is used when the previously mentioned technical goals cannot be realized. Most pediatric recipients require choledochojejunostomy because of small duct size and a history of biliary atresia. Before anastomosis, both the donor and the recipient bile ducts should be trimmed sharply to remove devitalized tissues, and brisk bleeding should be evident from the cut ends. Accommodation for size mismatch with ductoplasty of the larger duct or spatulation of both ducts has been described (Buczkowski et al, 2007; Nissen & Klein, 2009). The choledochocholedochostomy and choledochojejunostomy anastomoses are accomplished with the use of fine absorbable monofilament suture in a single-layer closure. Proponents believe that decompression of the biliary tree reduces the rate of clinically significant leaks, whereas others point to data that suggest a higher rate of biliary stricture from internal stents. At our institution, biliary stenting is performed selectively based on individual case circumstances and surgeon preference. Retransplantation is the treatment of choice and typically is required within 72 hours. Some authors also report the distinctly separate category of initial poor function, in which allografts might have a chance for functional recovery; however, no consensus for a clear definition exists. Factors reported as associated with nonfunction include prolonged cold- and warm-ischemic times, donation after cardiac death, intraoperative systemic hypotension (mean arterial pressure <40 mm Hg), significant donor steatosis, and recipient factors such as portal vein thrombosis, renal failure, dependence on life support, and status 1 listing (de Vera et al, 2009; Fernandez-Merino et al, 2003; Johnson et al, 2007; Marsman et al, 1996; Nair et al, 2002; Ploeg et al, 1993; Reich et al, 2003; Sharma et al, 2010; Strasberg et al, 1994). Although it has been proved that severe macrosteatosis (>60%) increases risk of graft failure, the influence of moderate steatosis (30%60%) remains unclear (Yoo et al, 2003a), and such allografts can be used with careful selection (Doyle et al, 2010). As would be expected, the likelihood of primary nonfunction is increased in the presence of multiple risk factors. The risk of surgeon-dependent technical complications increases when more complex surgical techniques, such as split-liver donation, are used. Examples of factors generally attributed to technical error include early thrombosis of the hepatic artery or portal vein and biliary complications such as leak or stricture. Invasive infection and certain metabolic complications are side effects of the immunosuppressive regimens currently in use. Also, primary nonfunction, subacute and chronic graft rejection, and recurrence of certain causes of initial liver failure eventually result in graft loss. If diagnosis is prompt, emergency exploration with attempted thrombectomy and revascularization may salvage the graft, although this is usually not possible. Some reports suggest that endovascular procedures- intraarterial thrombolysis, percutaneous transluminal angioplasty, and endoluminal stenting-can be successful in hepatic arterial revascularization (Singhal et al, 2010). However, a majority of patients eventually require retransplantation (Bekker et al, 2009; Duffy et al, 2009). Clinical presentation may be asymptomatic or may result in perihepatic abscess, biliary leak, biliary strictures, or cholangitis (Gunsar et al, 2003). Treatment may be attempted with endoscopic or percutaneous biliary decompression, stenting, or even systemic anticoagulation. Systemic anticoagulation may be sufficient in patients with preserved graft function (Duffy et al, 2009). Symptoms of portal hypertension but preserved graft function often can be managed medically with standard therapies for ascites in combination with variceal banding or sclerotherapy; however, the graft salvage rate with these alternative strategies is typically much less than 50% (Duffy et al, 2009) (see Chapter 120). The most common area of stenosis is the extrahepatic portal venous anastomotic site. Many stenoses can be managed endovascularly with percutaneous transhepatic balloon angioplasty and stenting (Woo et al, 2007) (see Chapter 120). Biliary strictures occur twice as frequently as anastomotic biliary leaks and can be classified as anastomotic or nonanastomotic (ischemic cholangiopathy) (Balsells et al, 1995; Qian et al, 2004). Most anastomotic strictures are managed endoscopically with balloon dilation and stenting. Ischemic cholangiopathy more often results from bile duct ischemia or an immune response, appears later and affects multiple sites, tends to be more difficult to manage, and is rarely amenable to endoscopic treatment. Nonanastomotic strictures are associated with a higher rate of graft failure requiring retransplantation (Axelrod et al, 2014; Chan et al, 2008; de Vera et al, 2009; Pine et al, 2009). A multidisciplinary approach to diagnosis and management of biliary complications is necessary and can result in higher patient and graft survival rates (Verran et al, 1997). In an asymptomatic patient with stable liver function, biliary complications can often be managed nonoperatively. Major leaks or total disruption usually requires operative conversion to a choledochojejunostomy or hepaticojejunostomy, an option that can result in long-term biliary patency (Langer et al, 2009). Initial presentation typically includes a mild increase in transaminase levels with or without associated graft dysfunction or biliary complications. Restenosis can occur in as many as one-third of patients within 1 year after stenting (Ueno et al, 2006) (see Chapter 120). Depending on the timeliness of diagnosis and the acuity of the patient, several treatment options exist. In patients with Chapter 116 Orthotopic liver transplantation 1809 Numerous studies have evaluated the use of T tubes and internal stents for prophylactic biliary decompression. Several have identified T-tube use as an independent risk factor for increased postoperative biliary complications. The effectiveness of internal stenting in reducing biliary complications also remains inconclusive (Welling et al, 2008) (see Chapter 120). Intraabdominal infections occur in 40% of recipients, with a higher incidence in patients with other noninfectious surgical complications (Reid et al, 2009). Liver transplant recipients are significantly immunocompromised and are at highest risk for infectious complications from the following risk factors: immunosuppressant medications, malnourishment, chronic illness, multiple blood-product transfusions, and lengthy and complex surgical procedures. The risk is further increased by the comorbidities of diabetes and morbid obesity, which are consistently increasing in the recipient population (Wong et al, 2014, Dick et al, 2009). Diagnosis of infection can be complicated by a relative absence of symptoms, because infection frequently manifests only as a leukocytosis (Reid et al, 2009). As part of the pretransplantation evaluation, recipients should undergo an infectious disease workup and should receive appropriate vaccines. Appropriate antimicrobial prophylaxis can reduce the postoperative infection rate by more than half, depending on the pathogen. Bacterial pathogens are the most common infectious agent in the early postoperative period, and the proportion of posttransplantation infections caused by bacteremia has increased significantly (Singh et al, 2004). Vascular catheters account for one-quarter of bacteremia for all pathogens combined. The emergence of drugresistant organisms resulting from overuse of common antibiotics has made the treatment of infected liver transplant recipients increasingly difficult. Without appropriate prophylaxis, the overall incidence in this population is 50% to 60%, with clinically apparent infections usually occurring 3 to 12 weeks after transplant (Farmer et al, 2001). The standard regimen includes an induction with intravenous ganciclovir followed by prophylaxis with oral ganciclovir for 3 to 6 months. Prolonged prophylaxis (100 days) can be costly and might be unnecessary in low-risk patients. Historically, fluconazole was almost universally included in antimicrobial prophylaxis, but this resulted in an increase in Aspergillus infections because Aspergillus is not susceptible to fluconazole. Although prophylaxis against Aspergillus is not supported by the literature (Braun et al, 1998; Singh 2000), voriconazole, amphotericin B, and caspofungin may be used alone or in combination for treatment of invasive aspergillosis (Singh et al, 2008), which is associated with a 40% 1-year mortality rate after infection (Pappas et al, 2010). Infection with the protozoan Pneumocystis carinii occurs in 3% to 11% of liver transplant patients in the absence of prophylaxis (Singh, 2000). Because T-cell immunity is the primary defense against P carinii, prolonged use of corticoste. Trimethoprimsulfamethoxazole (single strength, once daily) offers highly effective prophylaxis at a low cost and with minimal side effects. The University of Pittsburgh experience shows that immunosuppression can be withdrawn successfully in almost one-third of patients, although it is unknown exactly what traits allow such weaning. Hyperacute rejection is mediated by preformed antibodies in the recipient and is directed against the graft endothelium. These antibodies produce activation of the innate immune system through the complement cascade, ultimately leading to rapid graft destruction.
Purchase verapamil 120mg overnight delivery
In this analysis heart attack 23 years old purchase cheap verapamil on line, multivariate factors that identified a better prognosis included age younger than 50 years, primary location in lung or bowel, and pretransplant somatostatin therapy. Multivariate analysis showed that age older than 50 years and upper abdominal exenteration or Whipple procedure at transplantation were associated with a poor outcome. Additional indications include growth retardation and the development of metabolic bone disease. The most common indication for transplantation in children remains disorders of the biliary system, most often biliary atresia (see Chapter 40). The procedure of portoenterostomy may be effective in some children if performed early, but if performed after 2 months, the chance of a successful outcome is limited. Thus if bile drainage is not established soon Chapter 112 Liver transplantation: indications and general considerations 1749 suggestion of malignancy. In patients with sclerosing cholangitis, as indicated earlier, investigation of the biliary tree may be indicated. This may reveal undiagnosed cholangiocarcinoma but also may result in an episode of cholangitis. In particular, those with a long history of pancolitis require full investigation by colonoscopy. In the presence of dysplasia, it may be sensible to consider early colectomy because the additional effect of immunosuppression may further increase the risk of colon cancer. Routine psychiatric evaluation is not indicated unless there is a history of psychiatric disease that may preclude successful rehabilitation. A dental examination is required, and any carious teeth are usually removed before transplantation. Consent the assessment is a good time to ensure the candidate understands not only the benefits of transplants but also the risks and the implications. Because of the increasing shortage of organ donors, surgeons are using increasingly marginal organs. Vitamin deficiency should be corrected, and the patient should adopt a high-protein, high-calorie diet. The presence of encephalopathy should not exclude a highprotein diet, and other methods should be used to control hepatic encephalopathy, such as use of lactulose and, if necessary, metronidazole, rifaxamin, or neomycin. Candidates should have their immunization history reviewed and immunization offered as indicated. In particular, live or attenuated vaccines, which are contraindicatd in the immunosuppressed patient after transplantation, should be considered at this time. It is reasonable to offer nonimmune patients immunization with hepatitis A and B vaccines. The presence of ascites itself may be an indication for treatment, because not only do these patients remain catabolic, but they also are at risk of spontaneous bacterial peritonitis. Patients with ascites should be treated with prophylactic antibiotics, such as ciprofloxacin or amoxicillin/clavulanate, which are not only effective and cost-effective, but also without major risk of developing bacterial resistance. The role of such shunts before transplantation remains uncertain; although effective in reducing portal hypertension, and thus improving ascites and risk of variceal hemorrhage, insertion carries the risk not only of sepsis but also of perforation and portal vein thrombosis. In particular, nonsteroidal antiinflammatory drugs should be avoided because of the risks of inducing gastric hemorrhage, renal failure, and fluid retention. Drugs such as opiates that result in constipation and sedative drugs should also be avoided because of the risk of precipitating encephalopathy. Diuretics must be used with care and renal function carefully monitored; renal failure is associated with a poor outcome after transplantation and hyponatremia with the development of central pontine myelinolysis. The transplant clinicians need to remain in close contact with the patient so that problems can be detected and treated early. While the waiting time for transplantation increases, patients will deteriorate and may experience complications precluding a successful outcome, or the probability of survival may become too small for transplantation to proceed. With the increasing shortage of donor organs, transplant clinicians need to consider those criteria that suggest a patient should be removed from the transplant list. Bruix J, Sherman M: Practice Guidelines Committee, American Association for the Study of Liver Diseases. Burdelski M, et al: the role of dynamic liver function tests in liver transplantation. Day E, et al: Predictors of psychological morbidity in liver transplant assessment candidates: is alcohol abuse or dependence a factor

Discount 80mg verapamil with visa
Some centers will withhold listing from those who continue to smoke cigarettes or do not comply with nicotine withdrawal programs heart attack kit purchase verapamil 120 mg with amex. Malnutrition in these patients has many causes: the disease itself; poor intake; dietary restrictions (often inappropriate in those with encephalopathy), and malabsorption, which itself has many causes. Malnutrition is associated with increased susceptibility to infection and poor healing. Although in liver disease the degree of malnutrition may be difficult to quantify, malnourished patients fare poorly, with reported mortality of 15% (Campillo et al, 2003). Illicit Drug Use As with tobacco users, some centers will exclude from transplantation those with active illicit drug use and those who fail to engage in withdrawal treatment. Those who are well stablilized on methadone as opioid replacement therapy should not be excluded and generally should continue on a stable dose. Age There is no agreed upper age limit, but increasing age is associated independently with mortality after transplant (Burroughs et al, 2006). The concept of biologic age has superseded that of chronologic age, although the former cannot readily be Chapter 112 Liver transplantation: indications and general considerations 1739 defined or quantified. Previous Abdominal Surgery the presence of adhesions, especially in the patient with portal hypertension, adds considerably to the difficulties of surgery and may affect outcome, especially when this involves surgery to the biliary tree (Neuberger et al, 1999). Infection Active bacterial, fungal, or protozoal sepsis is an absolute contraindication to transplantation. Once appropriate therapy has been instituted, however, the patient is a suitable candidate for the procedure. Medium-term outcomes are encouraging (Stock & Terrault, 2015), but the procedure remains limited to a few centers. Pulmonary angiography and right-sided heart catheterization may be indicated, as suggested by the clinical and simple investigations. Arterial hypoxemia (oxygen saturation <92% or arterial oxygen pressure <70 mm Hg) may be found in up to 70% of patients with liver disease. Causes of this hypoxemia include ventilation/perfusion mismatch, diffusion limitation, alveolar hypoventilation, shunt, and a diffusion/ perfusion abnormality (Krowka & Cortese, 1990). Furthermore, pulmonary dysfunction is present in up to 2% of patients with advanced liver disease. The presence of significant pulmonary disease is usually apparent on history and examination, but sometimes significant pulmonary disease may be cryptic. The diagnosis is suggested by showing orthodeoxia (a fall in arterial blood oxygen when standing) and the presence of intrapulmonary shunting (demonstrated by bubble echocardiography or nuclear medicine scanning with 99mTc macroaggregated albumin). Cardiovascular Disease As with other diseases, the prognosis of patients with cardiovascular diseases will dictate whether liver replacement is an appropriate therapy. Preoperative assessment of cardiovascular status is, at best, imprecise; no clear guidelines are available to define limits below which grafting is unsafe. All candidates should undergo at least echocardiography not only to detect abnormalities of the heart muscle and valves, but also to seek evidence of pulmonary hypertension. When evidence of possible ischemic heart disease is found, patients should have a stress test, such as dobutamine- or adenosine-stimulated echocardiography and myoscintigraphy. Functional testing of cardiac reserve may be helpful, but there is no clear indication of when transplant is contraindicated. Stenting, usually with antiplatelet therapy, is associated with a better outcome than coronary artery bypass graft. This results from pulmonary vasoconstriction and leads to vascular remodeling, resulting in pulmonary hypertension (Hoeper et al, 2004). Respiratory Function Routine screening of patients with chest radiograph, electrocardiogram, lung function tests, and measurement of peripheral oxygen saturation will usually identify those with pulmonary problems. A preoperative partial pressure of oxygen of less than 50 mm Hg and a lung scan with brain uptake of more than 20% (Arguedas et al, 2003) strongly predict high mortality. These patients, however, may be candidates for a triple transplant (heart, lung and liver). Similar considerations apply to those with cystic fibrosis, cystic lung disease, and liver disease. This may result from the insulin intolerance associated with advanced liver disease and thus will resolve after successful transplantation. Those with insulin-dependent diabetes have a worse outcome after transplant (Hoehn et al, 2015). Evidence of proliferative retinopathy, diabetic nephropathy, or autonomic neuropathy, as evidenced by simple tests such as abnormal beat-to-beat variation on Valsalva maneuver or postural hypotension, may be relative contraindications for transplantation. The presence of advanced microvascular disease puts the patient at risk of major autonomic disruption during the procedure, and survival of such patients is relatively poor (Haydon & Neuberger, 2001). Hyponatremia is a common finding in patients with advanced chronic liver disease and occurs usually as a consequence of injudicious diuretic therapy or because of the reduced free water clearance. Grafting patients with severe hyponatremia (serum sodium <120 mmol/L) has shown that there is an increased risk of central pontine myelinolysis (Yun et al, 2009). Significant hyponatremia should be corrected before transplantation by simple water restriction and, if appropriate, stopping diuretic therapy, or if more rapid correction is required, use of renal support. These may occur because of the cirrhosis itself or as part of an associated underlying thrombotic tendency. In early series, portal vein thrombosis was considered a contraindication to transplantation, but it is now appreciated that this is no longer the case, and portal venous inflow to the graft can be provided by the superior mesenteric vein or even a splenic vein. It is only in rare patients with extensive venous thrombosis, and when it is impossible to provide a suitable portal supply to the graft, that transplantation may be currently contraindicated. In hepatorenal syndrome, there is no structural damage to the kidney, and once satisfactory liver function is reestablished, the kidney will function normally. Therefore although the prognosis may be reduced in the presence of advanced renal insufficiency (Rimola et al, 1987), the hepatorenal syndrome is not an absolute contraindication to transplantation. However, in the patient with coexisting advanced renal disease, it may be advisable to consider combined liver and kidney transplantation. Renal function remains a major predictive factor for survival after transplantation (Nair et al, 2002), as well as the risk for renal impairment. The Israel Penn Tumour Registry has identified tumors that carry a high risk of recurrence after transplantation (Box 112. Caution must be used when following these recommendations, however, because the registry relies on voluntary reports rather than a systematic review. Most centers will offer transplantation when the risk of recurrence is less than 10% at 5 years. Only in exceptional cases should patients with these extrahepatic malignancies be considered suitable candidates for transplantation. Chapter 112 Liver transplantation: indications and general considerations 1741 Bone Disease Many patients with chronic liver disease will have bone disease. The occurrence of osteomalacia, caused by vitamin D malabsorption, is low and can readily be corrected by parenteral administration of vitamin D. Osteoporosis, however, is a much greater problem and is particularly seen in female patients with chronic cholestatic disease. In many cases, successful transplantation will halt or retard the progression and may even improve bone mineralization (Guichelaar et al, 2007). The presence of severe osteoporosis may result in additional complications if there is significant thoracic or lumbar vertebral collapse or the presence of fractures. The development of severe osteoporosis may well be an indication for transplantation in itself. The common causes of death are cerebral edema, multiorgan failure, sepsis (bacterial or fungal), cardiac arrhythmia or arrest, and respiratory failure (Ostapowicz et al, 2002). Several groups have now published prognostic factors, and based on those, criteria are available for superurgent transplant (Table 112. The inclusion of serum lactate in the King prognostic criteria may provide greater accuracy (Riordan & Williams, 2002). The patient remains at risk for complications of increased intracerebral pressure for as long as 48 hours after successful transplantation (Dabos et al, 2004; Keays et al, 1991). Once the decision for transplantation has been made, clotting should be normalized as much as possible given the constraints of volume replacement and avoidance of the complications of intracerebral edema. However, such a procedure may be indicated in a patient who is rapidly deteriorating and a graft has been found, but logistic conditions may enforce some delay before the graft can be successfully performed.