Buy genuine biaxin on line
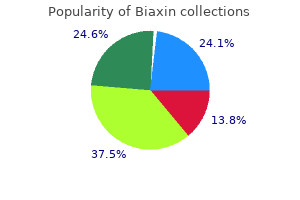
This section briefly focuses on the cell-to-cell communication mechanisms that have been observed between neoplastic cells and the major cell types that form the tumorassociated vasculature and on the strategies that could disrupt these interactions with the vascular microenvironment gastritis diet treatment medications cheap biaxin online. Glioma cells also interact directly with mural cells (pericytes and smooth muscle cells) of the tumor-associated vasculature. Although glioma cells that migrate along blood vessels disrupt the coupling between astroglia and mural cells that is necessary to regulate vascular tone, the tumor cells appear to take control of this function: glioma cells replace astrocytes in releasing potassium (through calciumdependent potassium channels), which regulates smooth muscle cell contraction and therefore local blood pressure. However, differentiation between these populations has been difficult because there is no robust consensus to identify a "microglia-specific" marker. M2 macrophages are "alternatively" activated cells with immunosuppressive and tumor-promoting functions. These categories are not rigidly Therapeutic Relevance of the Glioma-Associated Vasculature Glioblastomas, the most aggressive type of gliomas, are some of the most highly vascularized types of solid tumors. Accordingly, antiangiogenic therapies have become a predominant chemotherapeutic strategy used in combination with standard or other experimental treatments for high-grade gliomas. Both cilengitide and bevacizumab have shown positive results in the treatment of recurrent glioblastoma, such as extension of progression-free survival and improvement in quality-of-life indicators. M1/M2 states can be identified by the expression of characteristic genes and antigens that have been extensively reviewed. Representative, false-color images of an experimental syngeneic glioblastoma model developed in immunocompetent mice. Notice the high density of microglia and macrophages in and around the tumor border. The tumor introduces heterogeneity in this population by inducing the conversion of microglia to the M2 phenotype, which is restricted to the tumor core and margin. E, Magnified image from the area indicated in C and D (dashed rectangle), with arrows showing the boundary between the periphery of the tumor, infiltrated by highly ramified microglia, and the tumor core with less ramified M2 microglia. A recent transcriptomic study has suggested that the genes expressed by glioma-associated microglia do not clearly match the M1 and M2 gene sets observed in peripheral macrophages from other solid tumors and may be therefore a unique phenotype that responds to unique signals from glioma cells. These cells retain certain innate immune functions, such as phagocytosis and direct cytotoxicity when co-cultured with tumor cells, although to a lesser extent than normal microglia. As a result of the paracrine influence of glioma cells, gliomaassociated microglia are deeply "re-educated" not only to lack antitumor responses but also to contribute to tumor progression. Li168 and Rolle169 have summarized a large number of studies showing that glioma-associated microglia release multiple cytokines that promote glioma cell proliferation and invasion. Therapeutic Relevance of Glioma-Associated Microglia the paracrine influence of glioma, which re-educates M1 microglia that was attracted to the tumor into the M2 tumor-promoting phenotype, is a clear example of tumor cells introducing heterogeneity to control their microenvironment. Normal functions of microglia, such as immune surveillance, scavenging of cell debris, and termination of immune responses, are aberrantly used to favor glioma escape from its local microenvironment as the tumor grows. Numerous examples from experimental models have shown that depletion of glioma-associated microglia is sufficient to reduce tumor growth and invasion. As an alternative strategy, the fact that a proportion of gliomaassociated microglia arises from recruited peripheral macrophages has spurred significant interest in the use of these cells as potential Trojan horses to disrupt glioma growth. Li and collaborators have proposed that autologous monocytes could be harvested from the patient, genetically manipulated, and re-introduced to deliver a toxic payload once they are recruited into the tumor. As described previously, some of those strategies attempt to deplete or inhibit Tregs in the local glioma microenvironment to reduce local tolerance. As a complement, other strategies have focused on activating cytotoxic T-cell responses by inhibiting immune checkpoint effectors. Immune checkpoints are a host of signaling mechanisms that inhibit T-cell cytotoxicity and regulate the extent of immune responses. As with other solid tumors, gliomas induce a tolerant state that reduces inflammatory and immune responses against neoplastic cells. Studies in large patient cohorts have established a negative correlation between patients with a history of asthma and glioma incidence. Preliminary results were encouraging but have not yet been replicated or extended. These cells have been expanded and shown to be toxic against autologous tumor cells. The primary end point of this study was to demonstrate the safety of the procedure, which was well tolerated and reported only minor adverse events. Understanding this heterogeneity is critical to identifying mechanisms of tumor growth and therapy resistance that may not be located in the tumor cells themselves but instead in the tumor-associated cells. Because there are no known genomic aberrations in tumorassociated cells, targeting these cells is likely to meet less resistance than targeting the neoplastic clones. Better understanding of the genetic and molecular landscape of the tumor microenvironment will help define novel glioma biomarkers and identify key mechanisms of tumor support that can be disrupted to advance glioma therapy. Microregional extracellular matrix heterogeneity in brain modulates glioma cell invasion. Gliomas that appear histologically similar and used to be grouped as tumors of the same type or grade can instead be classified in a variety of molecular subgroups defined by specific mutations, epigenetic alterations, and metabolic features. Glioma heterogeneity is therefore one of the most challenging aspects for the successful treatment of these tumors because therapies must face a diverse, ever-evolving population of malignant cells. Molecular and genetic profiling of gliomas has also revealed extensive heterogeneity of the tumor microenvironment, although systematic classification of the microenvironmental heterogeneity is far from complete. A clear example is illustrated by the regional changes in tumor cell metabolism due to local hypoxia and nutrient depletion: although tumor-associated cells lack the extensive metabolic reprogramming of glioma cells, they show changes in glucose and acetate metabolism that parallel those observed in tumor cells. Moreover, the nature and extent of those changes are likely to depend on the genetic alterations of the tumor cells directing the reprogramming. Autocrine factors that sustain glioma invasion and paracrine biology in the brain microenvironment. Glioma cells on the run: the migratory transcriptome of 10 human glioma cell lines. Gene expression profile of glioblastoma multiforme invasive phenotype points to new therapeutic targets. Glioblastoma recurrence patterns after radiation therapy with regard to the subventricular zone. Transformation of quiescent adult oligodendrocyte precursor cells into malignant glioma through a multistep reactivation process. Delayed leptomeningeal and subependymal seeding after multiple surgeries for supratentorial diffuse low-grade gliomas in adults. The paradox of neoplastic glial cell invasion of the brain and apparent metastatic failure. Extracellular space volume measured by two-color pulsed dye infusion with microfiberoptic fluorescence photodetection. Extracellular matrix glycoproteins and diffusion barriers in human astrocytic tumours. Adhesion of human glioma cell lines to fibronectin, laminin, vitronectin and collagen I is modulated by gangliosides in vitro. Mimicking white matter tract topography using core-shell electrospun nanofibers to examine migration of malignant brain tumors. Chondroitin sulfate proteoglycans potently inhibit invasion and serve as a central organizer of the brain tumor microenvironment. Extracellular matrix determinants of proteolytic and non-proteolytic cell migration. Bradykinin enhances invasion of malignant glioma into the brain parenchyma by inducing cells to undergo amoeboid migration. Expression and function of water channels (aquaporins) in migrating malignant astrocytes. Altered production and proteolytic processing of brevican by transforming growth factor beta in cultured astrocytes. Compensation mechanism in tumor cell migration: mesenchymal-amoeboid transition after blocking of pericellular proteolysis. The role of versican isoforms V0/V1 in glioma migration mediated by transforming growth factor-beta2. The proteoglycan brevican binds to fibronectin after proteolytic cleavage and promotes glioma cell motility.
Order cheapest biaxin
Gamma motoneuron activity prevents this problem by shortening the intrafusal fibers gastritis in pregnancy biaxin 500 mg low cost, which assists movement by increasing activation of alpha motoneurons through type Ia feedback. Gamma motoneuron activity also increases reciprocal inhibition of the antagonist muscle. When a muscle is stretched, it contracts in an attempt to regain its original length. It inhibits the motoneuron pools of antagonistic muscles through a disynaptic pathway. Researchers studying spasticity tend to stress definitions that emphasize abnormal reflex responses, whereas clinicians tend to stress more global definitions, primarily related to impairment of movement. To further complicate the issue, many clinical syndromes associated with spasticity are caused by injuries at multiple sites in the neuraxis, and the pathologic mechanisms producing motor dysfunction are equally varied. The narrow physiologic definition of spasticity is "a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes. In addition to hyperactive reflexes, spasticity can be associated with various signs and symptoms designated "positive" or "negative"6: positive signs are produced by overactivity. In spasticity, an increase in deep tendon reflexes and resistance to passive stretch of the limb are positive signs. It is the negative signs that usually create the clinically significant problems that are disabling for the patient. Increased muscle tone, clonus, and hyperactive reflexes occasionally interfere with initiation and smooth completion of a movement. A broader and more insightful definition of spasticity emphasizes the movement disorder associated with the velocitydependent resistance and reflex hyperexcitability, not simply its clinical signs. Decreasing tone and exaggerated reflexes produced by medications or surgery do not necessarily mean Mechanisms Underlying Reflex Function To understand how changes in these mechanisms lead to spasticity, the events that occur when a muscle is stretched must be traced. In a closed-loop system, it is impossible to identify the beginning and end of a sequence of events. Structures involved in the control of movement at the spinal and peripheral levels. The text describes the sequence of events (1 through 3) that occurs in the stretch reflex arc. In addition to monosynaptic Ia excitatory pathways, polysynaptic pathways also converge on the alpha motoneuron. Interneurons (shaded circles) interposed in these pathways are controlled by descending pathways. Excitatory synapses are represented as angle signs and inhibitory synapses as a dot. Pierrot-Deseilligny,10,11 Pierrot-Deseilligny and Mazieres,12 and Sehgal and McGuire13 discussed these mechanisms in detail. Sehgal and McGuire also provided a detailed explanation of the different electrophysiologic testing procedures that are used to deduce which mechanisms are underlying the spasticity. It has been suggested that Ia discharge is normally reduced by presynaptic inhibition and that reduced levels of presynaptic inhibition could lead to an increase in the stretch reflex. This reduction in presynaptic inhibition could give rise to an increased reflex response. There is also evidence of a decrease in presynaptic inhibition in paraplegic patients but not in hemiplegic patients. Lack of reciprocal inhibition can lead to unwanted activation of the antagonist muscle and impede movement. The Ia inhibitory interneuron receives excitatory synaptic input from numerous descending pathways, including the corticospinal tract. DecreasedRecurrentInhibition Motor axons give off recurrent collaterals that activate Renshaw cells, which in turn inhibit alpha motoneurons,10 thereby creating a recurrent inhibitory circuit. In patients with hemiplegia (most often from stroke) and in patients with spinal cord injury (most often from trauma), recurrent inhibition increases at rest. In contrast, patients with progressive paraparesis caused by hereditary spastic paraparesis or amyotrophic lateral sclerosis exhibit reduced recurrent inhibition. During active movements in spastic patients, an increased reflex response may be caused by lack of inhibition of Renshaw cells. In healthy subjects, Renshaw cells are inhibited, which in turn inhibits the Ia inhibitory interneuron directed to the antagonist motoneuron. This allows reciprocal inhibition to function to suppress a stretch reflex in the antagonist muscles. ReciprocalIaInhibition When a muscle is stretched, the reflex evoked in that muscle is normally accompanied by inhibition of the opposing muscle. This finding of reciprocal inhibition has had a pervasive influence on the understanding of movement control. Selective blockade of the fusimotor system has been used clinically in spastic patients. Injection of dilute procaine into the motor points of spastic and rigid muscles decreases muscle tone. However, at a different site, intrathecal and epidural injections of local anesthetic did not reveal a link between increased fusimotor activity and spasticity. Although the gamma motoneuron hyperactivity hypothesis has been influential, the evidence to support it is indirect, inconclusive, and circumstantial. On muscle stretch, impulses from group Ib fibers are transmitted to homonymous motoneuron pools and heteronymous pools acting synergistically to inhibit stretch. This was demonstrated by Delwaide and Oliver,31 who showed that Ib inhibition was markedly reduced in spastic patients. Excitatory interneurons are represented by open circles; inhibitory interneurons, by filled circles. Notice that alpha and gamma motoneurons are controlled by descending pathways. The column "Mechanism" lists the putative mechanism by which hyperreflexia could occur. The evidence indicates strongly that decreased presynaptic inhibition, decreased inhibition from supraspinal centers, and decreased Golgi tendon organ inhibition can each play a role in hyperreflexia. However, the importance of each mechanism may vary with the type of injury that causes hyperreflexia. It is strikingly clear that different causes of spasticity can have opposing effects on the patterns of inhibition and excitation observed in various spinal pathways. Lack of descending control of Renshaw cells leads to impairment of voluntary movements and prevents modulation of control of the antagonist muscle, as has been shown by Katz and Pierrot-Deseilligny. Lesions at numerous levels of the central nervous system may upset the delicate balance between excitatory and inhibitory input that influences the alpha motoneuron. There may also be a change in the intrinsic properties of motoneurons in spasticity. There are two reasons why the spinal circuits can malfunction: abnormal descending control and local changes at the spinal level. AbnormalDescendingControl One way to consider the diminished motor control in patients with spasticity is from a developmental perspective. Before a baby can stand, the flexor reflexes in the lower limbs must be inhibited and the extensor reflexes enhanced to brace the limbs against gravity; this is a function of the vestibulospinal and facilitatory reticulospinal tracts. For the child to walk, the extensor pattern of reflex standing in the lower limbs must be inhibited, and the flexor synergy of the lower limbs must be integrated into a walking pattern. This requires involvement of the motor cortex to inhibit extensor activity and facilitate flexor activity. Incorrect threshold settings for the afferent neurons could lead to a hyperactive response. If the motor cortex or its projections are damaged, the brainstem exerts primary control. If the brainstem assumes complete control, a decorticate posture-flexion of the upper limbs and extension of the lower limbs-develops. In cerebral spasticity, the stretch reflexes in the upper limb flexors and lower limb extensors are enhanced. If the spinal cord is damaged, even brainstem control is disrupted, so that flexor reflexes and stretch reflexes are released from inhibition.

Biaxin 250 mg lowest price
Thus far gastritis disease definition buy biaxin 500 mg on-line, the results have been mixed; some studies revealed no cognitive changes and others indicated neuropsychological changes that affect return to work or thinking. The variation in results can be attributed partly to methodologic differences in procedures and study logistics, but this approach remains a potential tool for teasing out the role of the basal ganglia in behavior rather than sensorimotor skills. By detailed studies and computational modeling, Frank and associates were able to determine that deep brain stimulation interfered only with the normal ability to slow down when faced with decision conflict. Careful cognitive neuroscience investigation of a simple behavior, impulsivity, in collaboration with neurosurgeons thus resulted in the discovery of two independent mechanisms that caused people to become impulsive. Traumatic brain injury, both penetrating and closed, has long been an area of collaboration between neurosurgeons and neuropsychologists that has resulted in scientific advances in the understanding of episodic memory, executive functions such as planning, and social behavior. Of course, only one case cannot prove efficacy, but it does raise the possibility that deep brain stimulation can help at least a subset of patients in minimally conscious states by increasing their arousal. To objectify more subtle changes, the techniques of cognitive neuroscience would be helpful. This effort not only may be clinically useful in helping the patient communicate better but also, as in the other examples presented earlier, it may also lead to a basic scientific advance by clarifying the concepts of arousal and consciousness. Deep brain stimulation and recording will continue to elucidate the role that local neural assemblies play in a larger functional network in the foreseeable future. Although some brain cancers can be treated effectively with surgery and medical treatment, others are extremely difficult to treat, and the prognosis is dire. In the case of a slow-growing tumor, changes in cognition or social function may be among the first symptoms identified, inasmuch as formal neuropsychological evaluation is quite sensitive to subtle decrements in performance and behavior. In all these cases, careful clinical observation, family reports, and self-reports are essential for gathering information about the effects of interventions; however, they do not provide objective and sensitive assessments of the cognitive and social functions that may be affected by the cancer and its treatments. A neuropsychologist can provide these assessments, while also gauging the need for psychological interventions that can be helpful in coping with the mood state changes. In addition, neuropsychologists can play an important role in planning rehabilitation and management of patients whose cancer is successfully treated. Therefore, special scenarios for clinical trials have to be considered, and some guidelines have been established. Clinical neuropsychologists can determine with varying degrees of precision the premorbid and postsurgical neurobehavioral status of patients and can help distinguish psychiatric problems (even those that preceded the onset of the condition that necessitated neurosurgical intervention) from problems caused by the central nervous system condition or surgery. Research-oriented clinical neuropsychologists (or cognitive neuroscientists) can provide useful collaboration if a neurosurgeon is interested in exploring specific aspects of the neural representation of functions in the brain. Furthermore, areas of the right frontal lobe or other brain regions are not safer to operate on just because they do not contain eloquent. Regions such as the right prefrontal cortex have unique functions that assist in social behavior, planning, and inference among other functional processes. Disruption of cortical functioning involving this kind of activity can affect outcome as much as or more than a selective language disorder. Much of what is summarized in this chapter can be found in previous editions of this textbook and in much more detail in current neuropsychology or cognitive neuroscience handbooks26,27: that is, a summary of the past and current uses of neuropsychology that are available to neurosurgeons. Four relatively new research areas stand out: plasticity, brain-machine interfaces, regenerative medicine, and optogenetics. The variability of the brain in terms of both functional localization and recovery of function is well known. What is the spatial extent of functionally unique cognitive maps in the cortex, and what are the principles by which cortical maps expand or contract How does injury affect maps adjacent to the injured brain sectors or in homologous areas in the uninjured hemisphere What happens when artificially introduced stem cells integrate within a neural network An electrode array is implanted, and signals are sent to a computer interface, which then interprets the signals and instructs a device on the basis of machine-learning algorithms. The keys to the success of these experiments are reliable interpretation of the neural codes that the computer is receiving and recording of a sufficient number of neurons to enable reliable instructional codes to be transmitted to the computer. This motor control application was obvious as a first attempt at a brain-machine interface, and although much work needs to be done, some promising findings have already emerged, such as those indicating that people can learn to think appropriately so that the computer can encode the output and allow a device to move. Could scientists develop memory storage devices that supplement current modes of thinking Ideally, this could all be done with a genetic or epigenetic set of instructions, but this method might be so complicated that it precludes all but the most general types of instructions, which would be insufficient to promote specific functions or abilities. The neuropsychologist and neurosurgeon have important roles to play in these future efforts. Applications of regenerative medicine in clinical neuroscience are still new; the most interesting research still occurs in animal models. Optogenetics (see Chapter 45) is a technique that is revolutionizing basic systems level neuroscience and may one day be available for human research. Simply navigating through it for the purposes of surgical precision and efficacy has proved a challenge. Identifying the function of its various regions has proved as much of a challenge. For clinical neuropsychologists and cognitive neuroscientists, research since 1990 has enabled dramatic improvements in the ability to precisely evaluate patients, identify the functions of various brain regions, measure their change over time, and predict outcome. Clinical neuropsychologists and cognitive neuroscientists provide an essential service to the neurosurgeon and can be intellectual partners in the effort to resolve the remaining mysteries of the human brain. Cognitive rehabilitation interventions for executive function: moving from bench to bedside in patients with traumatic brain injury. Overestimation and unreliability in "feeling of doing" judgments about temporal ordering performance: impaired self-awareness following frontal lobe damage. Symptom management, rehabilitation strategies, and improved quality of life for patients with brain tumors. Residual impairments and work status 15 years after penetrating head injury: report from the Vietnam Head Injury Study. Pharmacological interventions for the treatment of radiation-induced brain injury. Restoring sensorimotor function through intracortical interfaces: progress and looming challenges. Facilitation of memory encoding in primate hippocampus by a neuroprosthesis that promotes task-specific neural firing. Young blood reverses age-related impairments in cognitive function and synaptic plasticity in mice. Adult neurogenesis and its role in neuropsychiatric disease, brain repair and normal brain function. Haines likelihood ratios are reviewed, and we demonstrate how to calculate and interpret each property. Neurosurgeons are becoming increasingly aware of the need to offer concrete scientific support for their medical practices. Tradition and reasoning from pathophysiologic principles, while important in generating hypotheses, are not a substitute for scientific method. Determining how and what outcomes should be measured is necessary to develop improved outcome assessments. We examine techniques of outcome measurement and many of the available measurement instruments used in neurosurgery. Clinical researchers and clinicians using clinical research must be familiar with the various research designs available and commonly used in the medical literature. To better understand the features of study design, it is helpful to consider factors that limit the ability of a study to answer a question. We list specific study designs with descriptions of the usefulness and pitfalls of each study method. Because randomized clinical trials provide the best evidence for clinical practice, we offer a brief summary of the design of these trials. The chapter ends with a review of the welldefined process of evaluation and introduction of new drugs, as well as the application of this process to the introduction of new surgical techniques. As the evidence base for neurosurgery evolves, its influence on the practice of neurosurgery will increase.
Purchase cheap biaxin on-line
A clinical comparison of subdural screw pressure measurements with ventricular pressure gastritis symptoms upper right quadrant pain generic biaxin 500mg on-line. Regional brain tissue pressure gradients created by expanding extradural temporal mass lesion. External ventricular drains versus intraparenchymal intracranial pressure monitors in traumatic brain injury: a prospective observational study. Intracranial pressure telemetry: first experience of an experimental in vivo study using a new device. Diagnostic accuracy of intraocular pressure measurement for the detection of raised intracranial pressure: meta-analysis: a systematic review. Usefulness of transcranial Doppler-derived cerebral hemodynamic parameters in the noninvasive assessment of intracranial pressure. A noninvasive estimation of cerebral perfusion pressure using critical closing pressure. Measuring elevated intracranial pressure through noninvasive methods: a review of the literature. Management of hydrocephalus in infancy: use of acetazolamide and furosemide to avoid cerebrospinal fluid shunts. Regional cerebral blood flow and intraventricular pressure in acute head injuries. The relation between intracranial pressure, mean arterial pressure and cerebral blood flow in patients with severe head injury. Cerebral venous oxygen content as a measure of brain energy metabolism with increased intracranial pressure and hyperventilation. Comparison of 85krypton and 133xenon cerebral blood flow measurements before, during, and following focal, incomplete ischemia in the squirrel monkey. Abnormal cerebral blood volume in regions of contused and normal appearing brain following traumatic brain injury using perfusion magnetic resonance imaging. The effects of dihydroergotamine in patients with head injury and raised intracranial pressure [see comments]. Regional cerebral blood flow in apoplexy due to occlusion of the middle cerebral artery. A practical method of serial bedside measurement of cerebral blood flow and metabolism during neurointensive care. Analysis of the response to therapeutic measures to reduce intracranial pressure in head injured patients. Effect of head elevation on intracranial pressure, cerebral perfusion pressure, and cerebral blood flow in head-injured patients [see comments]. Aspects on the cerebral perfusion pressure during therapy of a traumatic head injury. Effect of cerebral perfusion pressure on contusion volume following impact injury. Hypertonic saline resuscitation of patients with head injury: a prospective, randomized clinical trial. Safe Study Investigators, Australian and New Zealand Intensive Care Society Clinical Trials Group, Australian Red Cross Blood Service, et al. High-dose barbiturate control of elevated intracranial pressure in patients with severe head injury. Failure of high-dose steroid therapy to influence intracranial pressure in patients with severe head injury. Control of vasogenic edema in a brain tumor model: comparison between dexamethasone and superoxide dismutase. Electroencephalography in brain edema (127 cases of brain tumor investigated by cranial computerized tomography). Corticosteroid therapy in patients with cerebral tumors: benefits, mechanisms, problems, practicalities. Lipid hydrolysis and peroxidation in injured spinal cord: partial protection with methylprednisolone or vitamin E and selenium. Preliminary report: effects of high dose methylprednisolone on delayed cerebral ischemia in patients at high risk for vasospasm after aneurysmal subarachnoid hemorrhage. Penetration of 14C-labelled mannitol from serum into cerebral spinal fluid and brain. Investigation of intravascular haemolysis during treatment of acute stroke with intravenous glycerol. Effect of mannitol and furosemide on blood-brain osmotic gradient and intracranial pressure. Furosemide and mannitol in the treatment of acute experimental intracranial hypertension. Effect of mild hypothermia on uncontrollable intracranial hypertension after severe head injury [see comments]. The use of moderate therapeutic hypothermia for patients with severe head injuries: a preliminary report [see comments]. Hypothermia and rapid rewarming is associated with worse outcome following traumatic brain injury. Hemicraniectomy for malignant middle cerebral artery territory infarction: an updated review. Management of intracranial hypertension in head injury: matching treatment with cause. Effects of cerebrovascular pressure reactivity-guided optimization of cerebral perfusion pressure on brain tissue oxygenation after traumatic brain injury. Optimal Cerebral Perfusion Pressure Management at Bedside: A Single-Center Pilot Study. Detection of cerebral compromise with multimodality monitoring in patients with subarachnoid hemorrhage. A comparison of certain acid-base characteristics of arterial blood, jugular venous blood and cerebrospinal fluid in man, and the effect on them of some acute and chronic acid-base disturbances. Reviews that outline the history of research and recent advances in this area and that provide detailed summaries beyond the scope of this chapter are cited in the references. It may be difficult to separate edema into these distinct classes in every patient because more than one of these types exist simultaneously as a result of the nature and timing of the underlying disorder. Because interstitial edema and osmotic edema have fewer causes or are uncommon in neurosurgical patients, our principal focus in this chapter is on vasogenic and cytotoxic edema. Continued redistribution of water, ions, peptides, and other neuroactive substances within and between the cells of the central nervous system (neurons, glia, microglia, and endothelial cells) may exacerbate the severity of the edema. The tight junctions between adjacent endothelial cells in the brain, which are nonpermissive in comparison to those in the systemic circulation, prevent the paracellular transport of most molecules. It can result from a variety of physiologic and pathologic processes and is frequently responsible for much of the morbidity and mortality associated with brain tumors and a variety of other disorders, including trauma, infarction, hemorrhage, and infection. Paul Ehrlich was the first to identify a potential barrier between the vasculature and the brain after he observed that intravenous albumin-bound dyes stained all tissues except the brain. This limits the effect of fluxes of systemic metabolism, such as occur with exercise, a meal, or starvation. It may be difficult to separate edema into these distinct classes in every patient because more than one of these types exist simultaneously as a result of the nature and timing of the underlying disorder (see Table 53-2). It has the potential to result in profound shifts in the relative volumes occupied by the cellular and interstitial elements. Tight junctions restrict the entry of hydrophilic materials and high-molecular-weight molecules. A thin basement membrane surrounds the endothelial cells and provides both structural support and a dense physical barrier between the circulation and the microenvironment of the brain. B, In vasogenic edema, increased permeability of the capillaries, through dehiscent or incompetent tight junctions, leads to exudation of a plasma ultrafiltrate and water into the extracellular space. Arrows demonstrate flow through the tight junctions and into the extracellular space. In addition, in an in vivo biologic assay of vascular permeability by intradermal injection, the Miles assay, the enhanced vascular permeability produced by the protein was blocked by antibodies to the partially isolated protein.
Buy generic biaxin 250 mg online
From the clinical perspective of evaluating a patient with visual symptoms at seizure onset gastritis diet 101 generic biaxin 500mg fast delivery, the experience of Bien and colleagues looking at 20 patients with epileptic visual auras may be helpful: elementary visual hallucinations, illusions, and visual field deficits were noted in seizures arising not only in the occipital lobe but also in the occipitotemporal region and the anteromedial temporal lobe. Patients often experience complex partial epilepsy, which if lacking visual symptoms may be indistinguishable from that of temporal lobe origin. Spread along the inferior longitudinal fasciculus presumably underlies this expression, just as that along more superior pathways may manifest itself with accompanying motoric semiology, similar to that seen in some frontal lobe epilepsies. Evaluation of the medically intractable patient will be influenced by these, because small, discrete lesions. As one would expect, visual field deficits are not uncommon in this patient population, and documentation of formal visual fields is essential. Patients with physiologic and structural findings well localized to an occipital lobe who already have a homonymous hemianopia can often proceed directly to occipital resection. Those with more extensive or less discrete pathology, discordant data, or preserved visual function in the relevant visual field may warrant an intracranial investigation. The strategic questions driving an intracranial study should determine the location and extent of electrode array. In such an instance, subdural grids over the region of concern may be very useful. A frequent concern in the patient with longstanding complex partial epilepsy with accompanying imaging findings suggesting medial temporal lobe involvement is whether or not a resection should also include the hippocampus. Coverage in such a situation, usually using depth electrodes placed either down the long axis of the hippocampus or from a lateral approach, must be able to address this. In the patient without a homonymous hemianopia in whom vision sparing is a goal, coverage of the calcarine cortex can be of value. An interhemispheric subdural grid can provide important information about both seizure onset and, with mapping, visual function localization. Given the significant potential of visual function morbidity from any resective approach in this region, understanding the spatial relationship between epileptogenesis and function is critical. With respect to seizure outcome, at least one series demonstrated a correlation between extent of intracranial array coverage of the occipital lobe and seizure outcome. Many patients may be very accepting of a superior quadrantanopia in return for seizure freedom; an inferior quadrantanopia is less well tolerated. Production of a hemianopia is obviously of still greater concern, and although some incapacitating, refractory seizure disorders may motivate some patients to accept this, it is a deficit many if not most patients and neurosurgeons would prefer to avoid; its prospect in some instances may rule out a resective strategy. All of these considerations must explicitly recognize that in a substantial subset of patients, resection may not ensure a seizure-free outcome. Variation in a given case will depend on whether or not visual preservation is a goal and on the extent of resection. Welllocalized lateral seizure onset associated with well-imaged, small, and discrete pathology may enable resection with preservation of primary visual cortex. In both instances, awareness of subcortical visual projections and their preservation is essential. Particular series in which electrocorticography has helped determine extent of resection include those of Binder and colleagues, Chang and colleagues, and Dorward and colleagues. Such resection can follow initial occipital resection, although the greater distance to the more anterior hippocampus renders this more technically difficult. Both for integration of the multimodality information common to the intractable epilepsy patient and for accuracy in incorporating that information into the surgical procedure, image guidance in these procedures has been useful. Outcomes There has not been an extensive neurosurgical experience with resection in occipital lobe epilepsy. The incidence of such an outcome ranges from 26% to 81%, with the majority of more recent series having ranges of 50% to 81% (Table 74-2). Eighteen of their 26 patients had normal visual fields before surgery; in only one patient was this preserved. Of the eight patients with preoperative visual deficits, six patients experienced an increased deficit. New quadrantanopias were seen in 12 patients; new hemianopias developed in four patients. Of 21 patients with intact preoperative fields, new deficits were seen in 11 patients (52. This 24-year-old woman had had complex partial seizures, characterized by staring, headache, chewing, and bilateral automatisms since the age of 9 years. D, Ictal recordings demonstrate seizure onset along the inferior aspect of the left occipital lobe. E, At the time of returning to the operating room for removal of the electrode array and occipitotemporal section, the image-guidance contour corresponding to the planned occipital resection volume is superimposed on the surgical field. Involvement of the primary somatosensory cortex of the postcentral gyrus is most common, but the second somatosensory area located at the parietal operculum and a third sensory area in the posterior parietal region-these second and third areas subserving less spatially discrete, sometimes bilateral, and presumably more integrative function-may alternatively be involved. Descriptive accounts of subjective sensations, the most common being elementary in the form of perceived tingling, numbness, or pins and needles, are well documented in the older literature. Somatosensory sensations reported either as an aura or at seizure onset were noted in 4 of 11 patients by Williamson and colleagues,36 in 5 of 8 patients (63%) by Boesebeck and colleagues,39 and in 13 of 28 patients (46%) by Kasowksi and colleagues. Boesebeck and colleagues found that the absence of auras inconsistent with structural pathology on imaging studies was more often associated with seizure-free outcome after surgery,39 but more recent experiences have not found such clinical phenomena consistent, reliable, or as helpful as other information. Simple partial seizures were found in 5 of 28 patients (18%) in the series of Kasowski and colleagues42 but in 31 of 40 patients (78%) in that of Binder and colleagues. A similar number of patients (7 of 11, or 64%) displayed asymmetrical tonic seizures with or without clonic activity in the study by Williamson and colleagues. In the study by Kasowski and colleagues, 10 of 28 patients (36%) had focal clonic activity and 5 patients (18%) tonic posturing. At least one study has shown surprising unreliability in demonstration of the site of seizure origin,36 but its usefulness to map cortical function that must be preserved has often been invaluable. The most common underlying pathologies in the larger surgical series have been low-grade tumor (most commonly ganglioglioma, low-grade astrocytoma, oligodendroglioma, or dysembryoplastic neuroepithelial tumor), cortical dysplasia, vascular malformations, and gliosis. The most common neurological deficits have been a usually incomplete Gerstmann syndrome (agraphia, acalculia, finger agnosia, and right-left disorientation) or hemisensory syndrome, with smaller numbers of patients experiencing deficits in visual fields, language, or strength. Increasingly the usefulness of image guidance to coordinate information from multiple preoperative imaging studies and ensure accurate execution of a preoperative surgical plan is being appreciated. Dorfer and colleagues have described a technique in which a parietal corticotomy extending down to the ventricle and then into the interhemispheric fissure, down to the posterior callosum, which in turn is sectioned, and then across the parietal and temporal operculum and along the temporal horn and including the amygdala is performed. Neuromonitoring and image guidance are employed, and unexpected morbidity has been low. Ten children were operated on in this fashion, nine of them (90%) becoming seizure free. In the past two decades, a growing number of studies have reported seizure onset localization to the insula, as well as positive results after targeted resective surgery. Traditionally, insular epilepsy was considered inoperable primarily because of the hazards of operating deep in the sylvian fissure as well as unclear effectiveness. Modern neuroimaging and improved technical considerations have rapidly contributed to improvements in localization and safer surgery. It has been suggested that it may play a role in secondary sensory processing, language and motor control, or higher autonomic control, and as a component of the limbic system. Nevertheless, some specific characteristics of insular seizures, such as vegetative, viscerosensory, and somatosensory symptoms, occur according to the complex physiology and extensive connections of the insular cortex. On the other hand, some aspects of temporal lobe seizures may be related to involvement of the insular cortex. The close connections with other potentially epileptogenic areas such as temporomesial structures or the frontal or central cortex can be considered as a reason for misleading findings in electrophysiologic and imaging investigations. Thus the implantation of depth electrodes is critical for evaluating insular cortex involvement. For lesions in the insula, the choice of frontal or temporal operculum resection depends on whether there is involvement of the operculum itself (as is often found with low-grade gliomas). The resection focuses on removing the cortex alone, while protecting the underlying white matter including capsule and basal ganglia structures. Inferiorly, along the deep temporal aspect of the insula, care must be taken to protect tiny lenticulostriate vessels that feed the internal capsule and other critical deep structures. Intraoperative monitoring of motor and language is an essential adjunct to insular surgery. As mentioned earlier, insula recordings are increasingly recognized as an important adjunct to nonlesional epilepsy localization.

Generic biaxin 250mg online
Seminal work was described by Vidal gastritis milk discount biaxin amex, who upon observing modulations of signals in the electroencephalogram, had the foresight in 1973 to ask, "Can these observable electrical brain signals be put to work as carriers of information in man-computer communication or for the purpose of controlling such external apparatus as prosthetic devices or spaceships Although computational abilities were initially restrictive, advances in microprocessor design and digital signal analysis now outperform neuroprosthetics requirements such that computational speed is no longer a rate-limiting factor. Similar technologic advances have provided the necessary tools for device development, allowing innovative applications to introduce motor, sensory, visual, auditory, speech, and other modalities to the field. Here we review these applications in neuroprosthetics by presenting the state of the art across a multitude of modalities and emphasize the role of neurosurgeons in its translation from fundamental research to clinical application. In contrast, it may be independent in application, such as the cochlear implant, with which acoustic information recorded from a microphone is translated into corresponding electrical stimulus delivered to the acoustic nerve, thereby providing auditory perception to the otherwise deaf ear. Neuroprosthetics may also be broadly characterized by the modality of operation. To date, the most successful neuroprosthesis that has seen widespread adoption and success in clinical application is the cochlear implant. For neurosurgery, the developing neuroprosthetic research that is poised to affect the field is motor output prosthetics. With these canonical examples in mind, the various modalities of interfacing with the nervous system and their clinical implications will be explored. The electroencephalogram, therefore, represents measurement of summated electrical potentials from the electrochemical interaction of a vast number of cells, both neuronal and glial in origin. By periodically sampling a continuous signal in regular short intervals, discrete values are obtained and stored in series, thereby converting the signal from an analog to a digital domain. The time-varying signal is then analyzed as the sum of multiple sinusoidal signals of varying frequency and amplitudes. This process commonly employs the discrete Fourier transform and is said to convert from the time domain to the frequency domain. In the frequency domain one can observe the change in power at a given frequency over time, which is known as timefrequency analysis. The distribution of signal power across a range of frequencies is the signal spectrum, and its plot over time is the spectrogram. By time-locking the sampled signal to measured subject data, correlations are made between cortical activity and task performance. One such observation in signals measured over the motor homunculus is the reliably reproducible decrease in spectral power in the 8- to 13-Hz range with overt or imagined movement of the hand contralateral to the side of cortical recording. A classical understanding of a neuroprosthetic is a device that records brain signals from the user. The source of signals used as input to the device can range from individual neuronal spiking, to field potential from cortical ensembles, to action potentials conducted by peripheral nerves. Examples include computer cursor movement, robotic arm control, and reanimation of paretic limbs. By reversing the direction of information transfer one can similarly develop an input device. In this scenario the device input is recorded from the external environment and converted into an appropriate stimulus delivered to the nervous system. These are classically defined as the delta band below 4 Hz, theta band from 4 to 8 Hz, mu band from 8 to 13 Hz (also known as alpha), beta band from 13 to 30 Hz, and gamma band beyond 30 Hz. Wolpaw and colleagues demonstrated the transformation of this source signal to effector output by training subjects to control a virtual cursor displayed on a computer screen. In effect, the velocity of cursor movement was derived in real time from changes in the mu spectral power volitionally modulated by the user. Translation to those affected by neuromuscular disorders would be impractical if overt motor function were required for the production of an adequate source control signal. By definition then, those who would benefit from such a prosthesis would be the very population incapable of initiating a control signal, obviating its clinical applicability. Thankfully, preservation of this function has been demonstrated in subjects with long-term deficits in whom volitional modulation of stable electrophysiologic structure was maintained. This distance is occupied by the meninges, bone, and scalp, which results in limited spectral and spatial resolution. For a scalp-based electrode to record a measurable signal from the cortex, electrical potentials must be summated across an area of cortex approximately 6 cm2 in diameter. Additionally, spike-sorting algorithms allow for detection of action potentials to the resolution of individual neurons. Because of the risk associated with placement of intraparenchymal electrodes, the bulk of experimental data has been conducted with animal models. Research in animal models has shown great success and illustrates vast potential for future neuroprosthetic applications. A large contribution to our current understanding of motor system electrophysiology and movement encoding has been garnered from macaque monkey experiments. With sufficient understanding of motor electrophysiology, the neural signals associated with intention of movement can be decoded. This has been advanced by research teams performing real-time control of robotic arms with macaque monkeys through electrode arrays implanted in the motor cortex. When depth electrodes are implanted for a prolonged time, a process of gliosis occurs, resulting in scar formation at the electrode interface. Over time, gliosis functionally insulates the electrode, limiting its recording ability, and ultimately prohibits its ability to adequately interface with the brain. Although invasive in nature, these signals may achieve the best balance of signal quality, durability, and reliability to enable a neuroprosthetic solution for the future. Also, because the electrodes are extraparenchymal, the immunologic response to the implant and its concomitant inflammatory and gliotic response are substantially reduced owing to the lack of tissue disruption. There have been numerous studies examining motor intentions to enable control of external devices. In the clinical scenario of presurgical invasive monitoring, identification of language areas in the cortex is often of primary concern. The user is then able to control the direction of a virtual cursor by saying out loud, or imagining saying covertly, various discriminating words preassigned to the opposing direction (Video 109-3). Reach and grasp by people with tetraplegia using a neurally controlled robotic arm. The importance of greater spectral bandwidth is illustrated in studies demonstrating information content beyond classical motor physiology in gamma rhythms. Furthermore, Gaona and colleagues demonstrated selectivity of sub-bands in the high gamma range for behavior- and location-dependent activation with performance of various cognitive tasks. Similarly, spatial resolution is greatly improved with placement of electrodes directly on the cortical surface. This higher anatomic fidelity translates to improved discrimination of cognitive tasks. Examples of higher anatomic resolution providing better intentional decoding include accurate decoding of individual finger movement (versus just hand movement) and phoneme articulation (versus just general speaking). This plays an important role in filtering noise and ambient signal from the environment to achieve a signal-to-noise ratio adequate for neuroprosthetic application. Over the course of the 4-week implant period, the user was able to quickly progress through a series of experiments sequentially demonstrating two-dimensional cursor, three-dimensional cursor, and ultimately three-dimensional robotic arm control (Video 109-4). These interfaces may be intraneural or extraneural, or they may be indirect interfaces with the nervous system through monitoring of muscle fiber activity. Generally speaking, this nerve-based approach offers numerous clinical advantages for a limb prosthesis in the setting of limb loss in patients who are otherwise neurologically intact. Intraneural design requires the integration of a conducting electrode into the individual axons of the nerve. Intraneural devices provide superior selectivity in motor activation and sensory recording. Examples of popular electrode arrays include those developed by the University of Michigan and University of Utah. Both devices employ penetrating electrodes to interface with axons within the nerve. Current methods of peripheral nerve surgery demonstrate a wide range of successful nerve transplantation and reanimation procedures, particularly in the setting of trauma. Peripheral neuroprosthetics extend the application of nerve transfer to allow for a new interface with external devices for functional restoration.
Diseases
- Bonneman Meinecke Reich syndrome
- Mesomelic dwarfism Reinhardt Pfeiffer type
- Weissenbacher Zweymuller syndrome
- Gay Feinmesser Cohen syndrome
- Caroli disease
- Usher syndrome, type 1C
- Brachydactyly nystagmus cerebellar ataxia
- Anorgasmia
- King Denborough syndrome
- Roy Maroteaux Kremp syndrome
Buy biaxin pills in toronto
Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus 253 gastritis or ibs generic 250mg biaxin otc. Atypical meningioma: randomized trials are required to resolve contradictory retrospective results regarding the role of adjuvant radiotherapy. Adjuvant radiotherapy for atypical and malignant meningiomas: a systematic review. Epidemiologic data on meningiomas in East Germany, 1961-1986: incidence, localization, age and sex distribution. Treatment decision making based on the published natural history and growth rate of small meningiomas. Classification of brain tumors is an evolving process, with obsolete entities being discarded and newly recognized tumors added with each successive revision. In the past, classification has relied heavily on recognition of morphologic patterns and immunohistochemical identification of differentiation antigens, but with the discovery a decade ago of the association between the translocation and subsequent deletion of chromosomal arms 1p and 19q2,3 and the responsiveness of anaplastic oligodendroglioma to treatment, a new era of molecular classification of brain tumors began. Current advances in molecular methodologies, particularly in the fields of genomics, transcriptonomics, and proteomics, have revolutionized brain tumor classification, and although the present classification remains based on morphology, histology is increasingly being complemented by genetic characterization of neoplasms. These malignant tumors may develop as a result of anaplastic progression from a preexisting, low-grade diffuse astrocytoma or may arise de novo. The mean age of patients with anaplastic astrocytoma at initial diagnosis is approximately 41 years, which falls between the age means for patients with low-grade diffuse astrocytoma and glioblastoma. Anaplastic astrocytomas typically show anaplastic progression to glioblastoma after an average of 2 years. In many cases they infiltrate across the corpus callosum or arise directly within it, with bilateral extension (butterfly tumor). Multifocal tumors are observed in about 2% of patients and are often mistaken for metastatic disease on preoperative neuroimaging studies. The necrotic tumor mass may be partially delineated on gross examination, but infiltrating glioma cells can easily be identified microscopically well beyond the apparent gross tumor boundaries. Mitotic figures are typically readily identified, and corresponding proliferation marker indices, such as the Ki-67 antigen, show elevated levels. Vascular proliferation is defined as the presence of blood vessels with multilayered vessel walls (more than two cell layers thick). Complete surgical resection is rarely attained with diffuse astrocytoma because of the inherently infiltrative nature of the neoplastic cells, which extend well beyond the apparent gross margin of the tumor. Mitotic figures are either absent or rare, and there is no vascular proliferation or necrosis. Despite their benign morphologic appearance, diffuse astrocytomas have an intrinsic tendency to recur, spread extensively, and undergo anaplastic progression to a higher grade. The time to recurrence and progression after initial clinical evaluation varies from case to case but ranges from months to several years. The most malignant form of diffuse glioma, glioblastoma is also the most common primary brain tumor. Diagnostic histopathologic features, as shown here, include tumor necrosis with surrounding pseudopalisading tumor cells (referred to as pseudopalisading necrosis) and hyperplasia of adjacent blood vessels (vascular proliferation) in response to the hypoxic conditions. Based on clinical, morphologic, and molecular characteristics, glioblastomas can be further subclassified into a number of subtypes with prognostic significance (see text for details). In contrast to diffuse astrocytomas, pilocytic astrocytomas exhibit very little tendency for anaplastic progression. Pilocytic astrocytomas preferentially affect the cerebellum, brainstem, optic nerves, and third ventricular region. Invasion of the overlying leptomeninges is common, but this feature does not constitute a negative prognostic factor. Microscopically, many pilocytic astrocytomas exhibit a biphasic architectural pattern consisting of compacted areas of elongated, piloid (hair-like) cells alternating with loosely textured and microcystic areas populated by scattered stellate cells. In pilocytic astrocytomas, mitotic activity, vascular proliferation, and necrotic foci do not have the same ominous prognostic significance as when present in diffuse astrocytomas. In favorable anatomic locations, such as the cerebellum, surgical resection of pilocytic astrocytoma has the potential to be curative. Distinctive histologic features include a monomorphic population of neoplastic pilocytes in a prominent myxoid background stroma. The pleomorphic, giant, and often multinucleated cells may display a variable xanthomatous change in their cytoplasm because of intracellular accumulation of lipids. As with pilocytic astrocytoma, invasion of the overlying meninges is characteristic and does not constitute a negative prognostic factor. This tumor is almost invariably associated with tuberous sclerosis, although this condition is often not known at initial evaluation. Both lesions share a superficial cerebral cortical location, large size, circumscribed growth pattern, and development during infancy. Surgical resection is the treatment of choice, and the prognosis is generally more favorable than would otherwise be suggested by the typically very large size of most of these tumors at diagnosis. The preferential location of these tumors is the white matter of the cerebral hemispheres, from which tumor cells typically infiltrate the overlying cortex. As viewed macroscopically and on neuroimaging studies, oligodendrogliomas often appear somewhat more circumscribed than astrocytomas. They are composed of uniform round cells with cleared cytoplasm surrounding a central spherical nucleus (fried egg appearance). The hallmark morphologic features of oligodendroglioma that separate this diffuse glioma from the astrocytic series are the uniformly round nuclei with surrounding cytoplasmic clearing ("perinuclear halos"). As opposed to the diffuse gliomas of astrocytic or oligodendroglial differentiation, ependymoma exhibits a significantly less infiltrative growth pattern that predisposes to surgical resection. The most characteristic architectural feature of ependymoma, as illustrated here, is perivascular pseudorosettes (cuffs of finely fibrillar cytoplasmic processes that the tumor cells extend to blood vessel walls). A branching network of small delicate blood vessels (chicken wire pattern) is a classic histologic feature of many oligodendrogliomas. Subpial tumor infiltration, perineuronal satellitosis, and perivascular satellitosis of tumor cells (secondary structures of Scherer) are characteristically seen in oligodendrogliomas that infiltrate gray matter. No oligodendroglioma-specific immunohistochemical markers are currently available. Oligodendrogliomas generally recur locally and ultimately undergo anaplastic progression. The hallmark genetic signature of oligodendroglioma (low grade and anaplastic) is combined whole-arm deletion of chromosomes 1p and 19q, which arises secondary to an initial translocation event and constitutes an independent prognostic marker, with 1p or 19q loss being associated with improved outcome regardless of the specific therapeutic regimen. There is no consensus on the minimal percentage of each component required for diagnosis of a mixed glioma. In general, anaplastic oligoastrocytoma exhibits high-grade features such as increased mitotic activity and often microvascular proliferation, but otherwise it has the same subjective diagnostic criteria as oligoastrocytoma. Anaplastic oligoastrocytomas that exhibit deletion of both 1p and 19q are considered to have a favorable genetic signature, whereas those with intact 1p/19q status and p53 immunopositivity are considered genetically closer to astrocytomas. An infratentorial location is the most frequent in children, whereas in adults most of these tumors are supratentorial. Ependymomas may occur outside the ventricular system in the brain parenchyma and also in the spinal cord. As seen histologically, classic ependymomas are moderately cellular tumors composed of oval cells with monomorphic nuclei and tapering eosinophilic cytoplasm. Some ependymomas have a more glial appearance, whereas others are more epithelioid. Some ependymoma variants (cellular, tanycytic) mimic other primary tumors, although others (papillary, clear cell) may mimic secondary tumors. Electron microscopy may be required in some cases to identify the ultrastructural features associated with ependymal cell differentiation (intercellular lumina filled with microvilli and sometimes cilia and prominent intercellular junctional complexes). The tumor is usually well circumscribed and covered by an outer layer of investing leptomeninges (capsule). Surgical resection of intact tumors can be curative in some cases; however, the presence of micrometastases, which are not visible to the unaided eye, or frank capsular breaching by the tumor can lead to diffuse dissemination among the nerve roots of the cauda equina and ultimately result in significant morbidity. Asymptomatic lesions are often discovered only as incidental findings at autopsy, but subependymomas occasionally produce ventricular obstruction of the lateral or fourth ventricles. As seen microscopically, the tumor is composed of clusters of small, uniform, benign-appearing tumor cell nuclei separated by extensive cell-free areas of finely fibrillary matrix. Lateral ventricular examples are prone to prominent microcystic change that can obscure the characteristic multinodular architecture. As viewed both macroscopically and microscopically, choroid plexus papilloma closely recapitulates the papillary architecture of normal choroid plexus, but the tumor cells tend to be more crowded and columnar, as opposed to the cuboidal morphology of normal choroid plexus epithelium.

Order biaxin 500mg mastercard
As mutations in critical genes accumulate in a cell gastritis from ibuprofen purchase biaxin 250mg overnight delivery, a cancer develops in a stepwise fashion. In brain cancers, it is not clear how long it takes for mutations to accumulate and in what order all the mutations might occur because the early stages of the tumors are not easily observed during development. This is normally true, except in a situations such as the presence of unstable amplifications that give rise to heterogeneity for this change in the tumor, or the acquisition of a late-occurring mutation in the latter stages of tumor cell clonal expansion. For most mutations, however, the same mutations that drive cancer formation will appear in all parts of the tumor. However, a vast number of preexisting mutations throughout these relatively unstable genomes are present within the tumor at very low frequency. This preexisting heterogeneity becomes very problematic when selection pressure, such as a drug or therapy, causes a resistant mutation in one or more cells to expand, creating a therapy-resistant tumor. Linkage and association studies can locate the approximate region of the chromosome responsible for a disease phenotype based on finding a polymorphic marker that cosegregates in the families affected by the disease. The prototype cancer gene syndrome involves the inheritance of a tumor suppressor mutation when there is one mutated allele in the germline and when a second spontaneous mutation inactivates the second allele. This first hit increases the chances of tumor formation in someone with the germline mutation dramatically, but by itself is not sufficient. Because the first hit is inherited as a germline mutation, it can be transmitted to offspring. Cancers are thought to start with a single mutation in a single cell, and then accumulate the necessary mutations in critical genes to grow in an uncontrolled manner. Each of the cells in the tumor will therefore have the same complement of mutations and will be "clones" with respect to mutation sequences. Tumor growth may not occur appreciably in many tumors until there are numerous mutations. In this diagram, only three steps are shown, although for the highest grade malignancy, many more mutations per cell are observed. Oncogenes are activated with a gain of function, whereas tumor suppressors are inactivated. Point mutations and other small intragenic sequence changes can activate or inactivate a gene. Entire genes can be lost or gained with homozygous deletion and genomic amplifications. Parts of two genes can be fused during a chromosomal amplification to form a new oncogene. Table 114-1 lists some of the more common cancer-associated mendelian disorders that have brain tumors as part of the phenotype. Mendelian disorders are genetic diseases that have a clear pattern of inheritance within families, such as dominant or recessive inheritance. Most of the syndromes that involve brain tumors have an autosomal dominant mendelian inheritance pattern. If the mutation appears only in the tumor, and not in the normal tissue, it is evidence for a somatic mutation acquired during tumor development. The classic scenario for a brain tumor phenotype with mendelian inheritance is the dominant inheritance of a mutation in a tumor suppressor gene, with an average of 50% of offspring inheriting one copy of the mutated gene from the affected parent. In the case of tumor suppressor genes, both copies need to be inactivated to initiate the process of tumor formation. When one mutation is inherited as the first "hit," there is a high probability of the second being inactivated. Although most mendelian disorders that include in the phenotype an increased risk for brain tumors are relatively rare in the general population, there are some exceptions. Neurofibromatosis is the most common of the syndromes with brain tumors as a phenotypic feature. About 10% or less of these patients will develop a malignancy from one of the multiple benign tumors. Therefore, a mutation in any of these genes can lead to an increased risk for brain and other cancers. Not only do inherited patterns help researchers locate the genes that can initiate brain tumors, but also identifying a familial risk for cancer is good clinical practice. A new patient with clustering of brain tumors or other types of tumors in his or her family will often want to know if there is a gene responsible and what the risk is for family members. Identifying the responsible gene gives the patient options for genetic counseling and for family planning and provides the opportunity for early diagnosis and treatment of other family members carrying the disease-causing gene allele. In some cases, identifying a cancer syndrome in a family can be lifesaving for a family member. Gain-of-function mutations are changes that either enhance the normal gene function or add a new function. Gain-of-function mutations are activating and change a proto-oncogene to an oncogene. This activation of an oncogene then contributes functionally to tumor progression, in concert with other gene mutations. Oncogenes are typically activated either by genomic amplification of the region containing the gene or by small mutations that alter the protein sequence. Occasionally, splicingrelated mutations that add or delete gene exons can activate an oncogene. Mutations commonly inactivate a tumor suppressor by producing a new stop codon (truncating mutation), deleting all or part of the gene, disrupting the gene promoter, altering splicing, or changing amino acids, rendering the protein nonfunctional. This elevated mutation rate then leads to critical mutations in oncogenes and tumor suppressors, although many new mutations will occur throughout the entire genome. The resulting accelerated mutation rate then leaves the cell primed to activate oncogenes and to inactivate tumor suppressors at an accelerated rate. In the coding regions of genes, a point mutation that alters the three-letter genetic code in such a way that the amino acid is changed is referred to as a nonsynonymous change. A synonymous (silent) mutation is one that does not alter the amino acid at that position. Normally, these silent changes are thought to be nonfunctional, but there may be hidden regulatory sequences within the coding region that can cause a functional change. A point mutation may also change an amino acid to a stop codon, and along with other mutations that induce early termination, it is often referred to as a truncating mutation. Point mutations and other changes can also alter gene regulatory regions in the gene or at regulator regions distant from the gene. Other common small mutations can alter gene splicing, alter transcript levels, or form new proteins. Insertion and deletions of one or more bases can have the same effect as point mutations. New amino acids can be added or deleted to a protein, either activating a new function or deleting the normal function. Homozygous deletions are sometimes observed in a cancer genome and are frequently a signal to the researcher that a tumor suppressor gene was located in the lost region of the genome. When the number of alleles is increased substantially beyond the normal two copies, it is known as genomic amplification or gene amplification. Increased copy numbers of a gene by genomic amplification are a reliable indication that an oncogene is located in the amplified region. Either the normal gene can be found to be amplified (and simply increases its normal function to pathologic levels), or a mutated oncogene can be found in the amplified region. Mutated genes can also be present in genomically amplified regions, and the mutation might occur either before or after the amplification. The number and combinations of mutations that can be used by the cancer cell to escape the normal control mechanisms are far larger and more complex than originally envisioned by researchers. Although the different genes that can be mutated to form a tumor are numerous for a particular tumor type, these mutations cluster into a smaller number of pathways of basic cancer mechanisms. The common pathways are those that control cell cycle, growth factor signaling, and the p53 checkpoint. This complex pattern of individual mutations suggests that, at a genetic level, there are many ways to alter the pathways leading to this most common brain cancer. Fortunately, these molecular pathways are at least in part characterized and understood, giving rise to the hopes that brain tumors can be better classified by their molecular changes and that critical points in the pathways might serve as useful therapeutic targets. In the following sections, attention is devoted to describing the mutations that give rise to the common types of brain tumors. It is important to note that there are few, if any, mutations specific to a particular cancer.
Trusted 250mg biaxin
A gastritis symptoms livestrong buy 250mg biaxin with amex, Photograph taken during electrode implantation surgery shows a standard clinical grid electrode with an intercontact distance of 1 cm (upper left) and a high-density custom grid electrode with an intercontact distance of 5 mm (lower right). C, Photograph showing a standard clinical depth electrode (top) and a custom depth electrode with multiple high-impedance microcontacts on the electrode shaft (bottom). Positions of subdural contacts are mapped on a three-dimensional surface rendering of a preoperative magnetic resonance image. Verification of Electrode Placement Accurate localization of electrodes on the brain surface is crucial to correctly interpreting research data. Locations of subdural contacts on exposed cortical surface are best documented by photographs taken at the time of both implantation and explantation surgery. By matching the details of gyral and pial vessel anatomy, it is possible to localize surface contact locations with millimeter accuracy. Localizing electrodes on the ventral surface of the brain is a difficult challenge because these electrodes cannot be viewed directly during surgery and consequently cannot be documented with intraoperative photography. Most clinical grid or strip electrodes are constructed with a center-to-center intercontact distance of 1 cm. High-density electrodes with less than 5 mm of interelectrode distance provide better spatial resolution and can be fabricated without altering the clinical risk profile of the grid. Customized electrodes may have more electrode contacts and lead cables attached to them than standard clinical electrodes; however, single-tailed electrode cables can reduce the number of cables by combining multiple lead cables into a single bundle, thereby reducing the number of penetrations through the scalp. As in purely clinical electrode implantations, preoperative planning is essential to optimize electrode coverage while minimizing mass effect caused by the electrodes. Displacement of cortex by grids or cables may occur because of the stiffness of the baseplate of the electrodes and cables. Compression of the cortical surface can be minimized by making careful cuts on the baseplate of the grid electrodes and meticulously looping cables to avoid undue torsion on the grid or strip electrodes. In a series of approximately 200 patients who underwent implantation with chronic intracranial electrodes at the University of Iowa over a 15-year period, there was no significant difference in the infection rates of patients who were research participants and those who were not. Accumulation of blood in the subdural space either beneath or above the grid electrodes may occur. Therefore, it is possible to determine the position of contacts in relation to skull base bony structures. Finally, the position of electrodes can then be mapped onto the surface rendering of the preoperative brain image. Modern signal processing methods also enable investigators to use a wide range of analytic methods to discern what physiologic events are relevant to the cognitive functions being investigated. The practical challenge is to carefully plan and execute experimental protocols so that the results are interpretable and the limitations of the methods used are appropriately recognized. Depending on the specific research question being addressed, research recordings may require a wider frequency bandwidth. In addition, the higher sampling rates (>1000 Hz) used for research recordings enable investigators to study high-frequency brain activity that is not captured with standard clinical sampling rates. Most institutional review boards and hospital biomedical engineers require this level of electrical isolation for the patient. It is imperative to follow local or hospital safety regulations regarding use of research equipment on human subjects. Almost all modern neurophysiologic recording systems have a digital recording design. Recorded data can be stored on digital recording media such as hard disk drives or optical recording media. Stored data can be analyzed offline with various commercially available or custom-made software. Among various sources of noise, power line noise is typically the most disruptive and requires the greatest attention to eliminate. Therefore, every possible effort must be made to reduce noise contamination at its source. A significant amount of medical and nonmedical equipment is necessary for both the medical treatment and the convenience of the subjects, who spend several days and possibly up to 2 weeks in the room. It is useful to unplug as many power cords as possible from alternating current power outlets when research recording is being performed. If any equipment can be run on battery power, it should be turned to battery mode. Hospital-grade power cords must be used for all equipment, if possible, not only to reduce the noise level but also to reduce the chance of injuring the patient by leakage of current. These tasks can range from language functions to complex social behavior, including ethical decision making, as well as economic or financial decision making. Because these cognitive functions are highly developed in humans, most of these functions are difficult to study in a meaningful way in nonhuman animals. Emotion is another complex cognitive function that offers potential advantages for study in humans rather than other species because investigators can directly ask subjects how they are feeling and what kinds of emotions they are experiencing during experimental manipulations. The following points must be considered carefully when a cognitive task is designed: (1) factors of interest and nuisance factors, (2) timing of stimulus delivery and response, (3) generation and recording of the timing signal, (4) order of stimulus presentation or response, and (5) number of trials. After defining them, it should be determined how many levels each factor has and which nuisance, or confounding, factors need to be controlled, in accordance with the principles of cognitive psychology research. A randomized block design is often used to control contamination with nuisance factors. For example, the development of fatigue or fluctuation of attention level can be problematic in many cognitive tasks. When the effect of conditions A and B is to be compared, if experimental sessions are conducted sequentially by delivering condition A in the first session and condition B in the second session, it is likely that levels of fatigue and attention will not be the same between these sessions. Some cognitive functions are altered by antiepileptic drugs; therefore, experiments investigating these functions would be optimally performed when the subject has been weaned off these drugs. The length of the interstimulus or intertrial interval should be based on considerations of what cognitive function is of interest and which region of the brain is being studied. For example, for investigation of lower level sensory cognition in a primary sensory cortex, the interstimulus interval can be shorter than that required for investigation of highly complicated cognitive function in the higher order cortex in the temporal or frontal lobe. When more than two stimuli are presented or more than two different responses are required, the order of their occurrence should be randomized or counterbalanced, and the frequency of occurrence should also ideally be equalized. It is necessary to conduct a sufficient number of trials to obtain robust statistical power. This issue is particularly important and challenging for experiments performed on epilepsy surgery patients. In most instances, these patients can maintain a high level of attention and fully participate in complex behavior tasks for less than 30 minutes per experimental block. Neural structures in the medial temporal lobe play important roles in cognitive functions related to emotion, memory, and learning. For these reasons, the medial temporal lobe is one of the brain regions most extensively investigated with intracranial electrodes in epilepsy patients. The direct measurements of electrical neuronal activities with fine temporal resolution of the intracranial recordings is a valuable complement to the noninvasive research methods. With this experimental approach, neurons in the medial temporal lobe, including the hippocampus, parahippocampal gyrus, and entorhinal cortex, were found to respond to visual stimuli of specific items. Some of these neurons responded not to what subjects were seeing but to what subjects perceived, imagined, or attended. Two different kinds of neurons were found, one representing "place" cells that respond to specific spatial locations and the other representing "view" cells that respond to specific views of task-relevant landmarks. The activities of some place cells were modulated by specific combinations of goals of task and place; for example, certain cells were activated only when a particular house was found in a particular location. To extend this work, a subsequent study replicated previous findings from animals to demonstrate grid-like neuronal activity during spatial navigation in the human hippocampus, entorhinal cortex, and cingulate cortex. This grid-like pattern of neuronal spiking may provide a mechanism through which humans are able to triangulate their position to effectively navigate through space. Additional work has revealed the existence of movement-related theta oscillations in the hippocampus and the neocortex, and these theta oscillations were significantly correlated with various cognitive functions.
Order biaxin 250mg without prescription
The effect is immediate during the operation and remains for a sustained period of time gastritis virus biaxin 500mg visa. A French neurologist, Guillaume-Benjamin-Amand Duchenne,9 in 1861 wrote, "I must confess that I am unable to solve this important problem. Thalamotomy for dystonia became almost forgotten by the 1990s, largely because of the dramatic effect of pallidal operations on generalized dystonias. A literature search uncovered the few case reports mentioned previously, but we eventually determined to attempt the Vo-complex thalamotomy described by Goto and colleagues. The patient returned to the profession and in 2008 was listed in the Guinness Book of World Records as the best-selling cartoon artist in the world. They are often of maximum importance to the sufferer, who possibly sees his livelihood in jeopardy, because his hand has forgotten its cunning. In focal hand dystonia, three components (task specificity, dystonia, and tremor) are present in various degrees. There are no useful laboratory or imaging studies, although there are many reports of functional changes in the cerebral cortex detected with magnetic resonance imaging. The idiosyncrasies of movements are always associated with a specific task, such as writing, drawing, playing musical instruments, or using special tools that require highly repetitive movements or extreme motor precision. Most patients have a history of extensive use of the fingers for very skilled and precise movements. The symptoms only appear when the patient performs a specific task such as writing, using scissors, or playing an instrument. About 70% of such patients experience no symptoms at all when performing other tasks, such as using a knife, using chopsticks, or typing; the remaining 30% may have dystonic symptoms triggered by multiple tasks. The symptoms are always the same and constant, although they may be milder in the morning in the early stage of the disease. In a few patients, the dystonic symptom becomes so severe that task specificity is lost and the symptom persists generally. Differential diagnosis includes primary pure writing tremor,36 essential tremor, and peripheral injury-induced focal dystonia. If a patient has both dystonia and dystonic tremor of the hand, stereotactic ablation of both the Vo and Vim nuclei of the thalamus can control the symptoms (Videos 97-1 and 97-2). The Arm Dystonia Disability Scale (eTable 97-2)46 is designed to quantify disability on a scale of 0% to 100%, with 100% indicating no disability. Even if the symptom seems minimal to the clinician, its persistence may cause the patient tremendous difficulty in pursuing his or her profession. Very minimal involuntary extension of the little finger may become a serious issue for a professional classic solo-guitarist, whereas a similar symptom in a violinist in an amateur orchestra may not be as serious. Our experience suggests that the duration of symptoms before surgery does not affect the surgical outcome. Patients who suffered for 30 to 40 years showed improvements similar to those seen in patients who had suffered just 1 to 2 years of symptoms. Conservative therapies should not be denied, however, if the patient prefers to explore them. Surgical management is appropriate when the patient is convinced of the limitation of conservative therapies and has decided to undergo surgery. Procedures have been performed in adolescents but should generally be avoided in patients older than 60 years because of a higher possibility of surgical complications. This may occur spontaneously and even after treatment with unilateral thalamotomy. Such patients may ask to undergo surgery on the contralateral side of the thalamus as well, but of course, bilateral operations are exceptional and very dangerous. Bilateral thalamotomy is contraindicated because of the high risk for complications such as speech problems and cognitive deterioration. This was seen in the 1960s and 1970s when large lesions were made in the thalamus. It seems possible now, however, that sequential bilateral thalamotomy may be safer if the lesion size is minimum. Leksell SurgiPlan computer software (Elekta) can determine a stereotactic trajectory that does not pass through the ventricle. The operation is performed under local anesthesia (1% lidocaine with norepinephrine) without sedation. It is important that the patient remain awake and alert so that symptoms can be monitored during surgery. It is not necessary to fully shave the head; clipping a small area of hair along the incision line is sufficient. A monopolar radiofrequency probe (1-mm diameter tip with a 2- or 4-mm uninsulated length) is then inserted through the bur hole. Electrical stimulation (130 to 160 Hz, 100-msec pulse width, up to 15 mA) is applied to identify the optimal position for the lesion. At this target, no dramatic changes of symptoms have been observed in our series, even with the strongest stimulation (15 mA, approximately 7 V), nor have any sensory or pyramidal motor symptoms been seen. We have therefore regarded the Vo target as an electrically nonresponsive silent region. This is very interesting because it is generally believed that high-frequency stimulation should improve symptoms, if coagulation works. Patients are not alerted to the exact timing of the macrostimulation and thermocoagulation to avoid placebo effects. Blood pressure is strictly monitored and controlled to minimize operative complications. When inserting the electrode probe, the probe is gently twisted to pass through the brain parenchyma smoothly to avoid vascular tears. The bur hole is covered with a small ceramic cap for cosmetic purposes, and the scalp is closed in two layers. To avoid complications and to obtain the best surgical results, the following are critical: 1. Intraoperative photographs of ventro-oralis thalamotomy for task-specific focal hand dystonia. Patients are asked to perform activities that induce focal hand dystonia during surgery to check improvement with stereotactic ablation of the ventro-oralis nucleus. In our experience, Vo thalamotomy is effective only for the symptoms in the distal part of the limb and does not treat the symptoms nearer the body trunk. The most common transient complications were mild dysarthria and hemiparesis appearing 2 to 3 days after surgery and lasting 2 to 3 weeks. This is probably due to edema formation around the thermocoagulation lesion, and it may be necessary to administer small doses of oral steroids for several days. Three patients complained of a strange, uncomfortable sensation in the tip of the tongue that persisted for approximately 6 months after surgery. This suggests the possible location of a structure related to tongue tip sensation below the Vo nucleus of the thalamus. In contrast to the previous reports on thalamotomy, we had no incidence of severe complications in our series. A period of 30 seconds of coagulation time is sufficient to create a permanent lesion. Longer coagulation times unnecessarily increase the area of the reversible heat penumbra zone. Friendly and gentle communication should be maintained with the patient during surgery. Important, of course, in any operation under local anesthesia, this attitude facilitates the social acceptance of surgical intervention for such seemingly mild physical symptoms. If there is no improvement during surgery, delayed response is not to be expected. There are some recurrences; about 10% of patients experience recurrence of the symptoms within 3 months. During surgery, there is a region of heat penumbra where the neural function stops, the symptoms improve, but the neurons are not completely ablated. We assume that such functional inactivation of neurons and their recovery with time are the reasons for recurrence within 3 months. Most patients with recurrence do seek additional surgical treatment, because of the substantial improvement of symptoms immediately following the initial procedure.


