Cheap propecia uk
This distinction is important because the rules for primary reflux resolution do not apply to cases of reflux secondary to obstructing lesions hair loss cure etf propecia 1mg cheap, such as posterior urethral valves or the neurogenic bladder seen with spina bifida. Grading reflux allows physicians to communicate findings quickly and to understand what the chances are for the natural resolution of primary reflux. This 3-month-old infant had a high fever and a positive urine culture that failed to respond to parenteral antibiotic therapy. A and B, the ultrasound examination showed signs of right hydronephrosis and hydroureter. Most cases are identified by fetal sonography; however, in this instance, the young parents did not seek prenatal care. After cutaneous diversion of this ectopic ureter, the infant became afebrile, and ureteral reimplantation was performed successfully 6 months later. The International Reflux Study used this grading scale, which is based on findings of a conventional fluoroscopic voiding cystourethrogram. By evaluating the findings in detail, a better understanding of the severity, potential treatment modalities, and outcome can be achieved and used for the benefit of the patient. Growing clinical evidence (Sillen et al, 1992, 1996a, 1996b) suggests that voiding pressures are dramatically increased in infants with reflux, especially in boys. These studies have shown that, even in normal males, voiding pressures are elevated in the neonatal period and decline dramatically during the first 2 years of life. The data demonstrate that voiding pressures in boys with high-grade reflux are often threefold to fourfold higher than those seen in older children. In these boys, reflux often resolves in a surprisingly short period of time, implying that the pressures drop with maturation of bladder function. Of interest, female newborns do not fare as well with resolution of neonatal reflux on a grade-for-grade basis, nor are their voiding pressures as elevated. These clinical observations are supported by experimental findings suggesting that there are gender-related differences in bladder neck function. The key concept is that voiding pressures are elevated, especially in male neonates with reflux, and that these pressures diminish over time. These observations have great bearing on how reflux resolution rates should be interpreted in newborns. Evidence from a multicenter study suggests that reflux detected in the first months of life as part of a workup for prenatal hydronephrosis has a better chance for spontaneous resolution, grade for grade, than that diagnosed in the child at 2 to 4 years of age (Herndon et al, 1999). This radiographic finding was also confirmed at cystoscopy, where the ectopic ureter (+) clearly enters the proximal urethra below the bladder neck (*). However, this course of action demands that parents comply with antibiotic prophylaxis and understand that a breakthrough infection rate as high as 20% is possible (Herndon et al, 1999). This series also indicated the benefit of circumcision in males with known reflux (Herndon et al, 1999). It is absolutely crucial for any parent and referring physician to understand that successful reimplantation surgery diminishes but does not eradicate the likelihood of pyelonephritis. A child with innate susceptibility will still experience bladder infections despite the absence of reflux. Several studies have shown that siblings of patients with reflux also have a higher likelihood of having reflux, with an incidence that declines in older siblings. Several studies have shown an increased incidence of renal scarring in siblings whose reflux was discovered by screening (Sweeney et al, 2001; Wan et al, 1996). However, Parekh et al (2002) suggest that sibling reflux follows a more benign course, and they noted no renal scarring after antibiotic prophylaxis. On the other hand, would the cohort of patients in this study have done as well without a diagnosis and antibiotic prophylaxis In one metaanalysis of the world literature on screening studies for reflux in asymptomatic siblings, Hollowell and Greenfield (2002) concluded that there was no evidence to support this practice. The extent to which screening averts renal complications or hospital admissions for pyelonephritis will be best answered by prospective trials. The traditional view was that identifying the pediatric patient with reflux was crucial to allow for antibiotic prophylaxis to be administered to prevent recurrent pyelonephritis and renal scarring. The embryologic studies of Mackie and Stephens (1975) suggested that much of the focal hypoplasia seen in kidneys with reflux is present at birth and have been borne out in clinical practice by a 20-year experience of neonatal evaluations for antenatally diagnosed hydronephrosis. Further support has come from newer molecular studies of ureteral bud development in knockout and transgenic mice, showing that aberrant ureteric bud development is associated with abnormal renal morphology. It is becoming clear that most of the renal insufficiency in patients with reflux reflects aberrant embryogenesis and not damage secondary to infection. In this setting, the high-grade reflux was associated with renal dysplasia at the onset, and renal failure was progressive. What is currently being debated is the role of long-term antibiotic prophylaxis in the management of these patients. This case demonstrates the association of bilateral grade V reflux with renal dysplasia. The voiding cystourethrogram (A) and ultrasound scan (B) shown here were performed within the first 2 weeks of life, and the child had never had a diagnosed urinary tract infection during this interval. Despite sterile urine, the serum creatinine level was elevated, and the renal sonogram showed increased echogenicity and poor corticomedullary differentiation. This case indicates that renal insufficiency associated with reflux often is present at the outset and is not always secondary to infection. The National Institutes of Health has currently funded the multicenter Randomized Intervention Vesicoureteral Reflux trial (Mathews et al, 2009) with the goal of obtaining the best data to help settle this debate. However, these studies do not enroll patients younger than 2 months, and they exclude patients with comorbidities. Sillen U, Bachelard M, Hansson S, et al: Video cystometric recording of dilating reflux in infancy, J Urol 155:1711-1715, 1996a. Batisky There is a significant risk of neonates developing complications related to thromboembolic phenomena, and the issues related to vessels supplying and draining renal vasculature will be discussed in this chapter. Clearly there are a number of conditions that can result in an imbalance of the delicate homeostasis between bleeding and thrombosis. Some may be genetic, some may relate to underlying stresses during pathologic processes, and some may relate to treatments for the pathologic processes. A major risk factor for renal arterial obstruction is umbilical artery catheterization. Before the advent of umbilical artery catheterization, only a few cases of renal artery thrombosis were seen. Other significant risk factors are shock, coagulopathy, and congestive heart failure. Trauma at the time of insertion of umbilical artery catheter by endothelial injury is postulated to be the cause of aortic thrombus formation which then leads to thrombosis of one or both renal arteries (Box 88-1). High umbilical artery catheters, placed at the T6 to T10 vertebral level, have been associated with a decreased incidence of clinical vascular complications without a statistically significant increase in any adverse effects (Barrington, 2000b). The chances of umbilical artery catheter occlusion can be decreased by adding heparin to the infusing fluid at a concentration as low as 0. The symptoms can be classified based on clinical severity; minor thrombosis with mildly decreased limb perfusion, hypertension, and hematuria; moderate thrombosis with decreased limb perfusion, hypertension, oliguria, and congestive heart failure; and major thrombosis with hypertension and multiorgan failure (Box 88-2). Laboratory findings associated with renal arterial thrombosis are thrombocytopenia, hypofibrinogenemia, elevated fibrin split products, variable prothrombin and thromboplastin times, conjugated hyperbilirubinemia, elevated blood urea nitrogen and creatinine, hyperreninemia, and hematuria. Angiography is the standard diagnostic modality and should be performed through the umbilical artery line if surgical intervention or intrathrombotic fibrinolytic therapy is being considered. In newborns with mild signs of organ dysfunction and stable aortic and renal arterial thrombosis, management of hypertension, transient renal insufficiency, and mild congestive heart failure is recommended.
Syndromes
- Using poor judgment and losing the ability to recognize danger
- Not standing for a long time (if you have NMH)
- A family history of the disorder
- Muffled voice
- A saline implant may be placed through a cut near your belly button. An endoscope is used to move the implant up to the breast area. Once in place, the implant is filled with saline.
- Shortness of breath with activity or when lying down
- The space between crib bars should be no more than 2.5 inches.
- Seizure medicines such as valproic acid, gabapentin, and topiramate
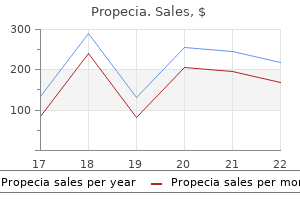
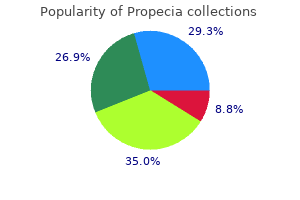
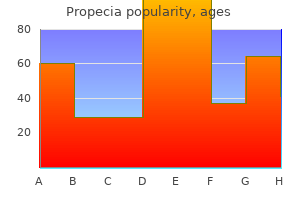
Cost of propecia
When exercise testing is terminated hair loss cure october 2012 propecia 1mg with mastercard, the ventricular arrhythmias rapidly recede in most patients. Holter monitoring, during which a patient should be encouraged to perform exercise, can be used as an alternative test in selected cases, although its sensitivity is thought to be low. In patients with exercise-induced ventricular arrhythmias, initially concealed structural heart disease, such as arrhythmogenic or hypertrophic cardiomyopathy, mitral valve prolapse, and myocardial ischemia may be alternate diagnoses. Cardiac imaging techniques and genetic testing may help the clinician in making a specific diagnosis. However in some cases, the underlying condition may be revealed only after close follow-up. Predictive genetic testing of relatives with a 50% risk of carriership (cascade screening) is fairly straightforward. When both parents of a mutation-carrying proband have a negative genetic test, the possibility of mosaicism should be considered. It is hoped that larger patient populations and longer follow-up durations will reveal these risk markers in the near future. Key aspects of disease management and familial evaluation in patients with catecholaminergic polymorphic ventricular tachycardia. However, these patient series included mainly probands, so cardiac event rates may be much lower in relatives. In addition, a significant proportion of events may be due not to -blocker inefficacy but rather to noncompliance. The presence of couplets or ventricular tachycardia during exercise testing has been shown to be significantly associated with future cardiac events, with moderate sensitivity and specificity of 0. In an international study that included 33 severely affected patients, flecainide (1. It is important to note that proarrhythmia caused by flecainide was not observed in this relatively young patient population. With this procedure, the lower half of the left stellate ganglion and thoracic ganglia T2 to T4 are removed, thereby inhibiting and largely preventing norepinephrine release in the heart. Leenhardt A, Lucet V, Denjoy I, et al: Catecholaminergic polymorphic ventricular tachycardia in children: A 7-year follow-up of 21 patients. Coumel P, Fidelle J, Lucet V, et al: Catecholamineinduced severe ventricular arrhythmias with AdamStokes in children: Report of four cases. Marjamaa A, Hiippala A, Arrhenius B, et al: Intravenous epinephrine infusion test in diagnosis of catecholaminergic polymorphic ventricular tachycardia. Nof E, Belhassen B, Arad M, et al: Postpacing abnormal repolarization in catecholaminergic polymorphic ventricular tachycardia associated with a mutation in the cardiac ryanodine receptor gene. Sumitomo N, Sakurada H, Taniguchi K, et al: Association of atrial arrhythmia and sinus node dysfunction in patients with catecholaminergic polymorphic ventricular tachycardia. Bai R, Napolitano C, Bloise R, et al: Yield of genetic screening in inherited cardiac channelopathies: How to prioritize access to genetic testing. Roux-Buisson N, Cacheux M, Fourest-Lieuvin A, et al: Absence of triadin, a protein of the calcium release complex, is responsible for cardiac arrhythmia with sudden death in human. Roux-Buisson N, Egea G, Denjoy I, et al: Germline and somatic mosaicism for a mutation of the ryanodine receptor type 2 gene: Implication for genetic counselling and patient caring. Hayashi M, Denjoy I, Hayashi M, et al: the role of stress test for predicting genetic mutations and future cardiac events in asymptomatic relatives of catecholaminergic polymorphic ventricular tachycardia probands. Swan H, Laitinen P, Kontula K, et al: Calcium channel antagonism reduces exercise-induced ventricular arrhythmias in catecholaminergic polymorphic ventricular tachycardia patients with RyR2 mutations. Katz G, Khoury A, Kurtzwald E, et al: Optimizing catecholaminergic polymorphic ventricular tachycardia therapy in calsequestrin-mutant mice. Atallah J, Fynn-Thompson F, Cecchin F, et al: Video-assisted thoracoscopic cardiac denervation: A potential novel therapeutic option for children with intractable ventricular arrhythmias. In patients with low ejection fraction and extensive wall motion abnormalities, nuclear imaging may not be sensitive enough to exclude diffuse coronary artery disease. Hence, cardiac catheterization with coronary angiography should be performed to exclude or define coronary artery disease in patients for whom revascularization would be considered. Less than half of patients with evidence of cardiac sarcoid at autopsy will have had clinically apparent cardiac involvement. Patchy noncaseating granulomas tend to involve the basal ventricular septum with disruption of cardiac conduction. Sudden cardiac death accounts for two-thirds of terminal events in patients with overt cardiac sarcoidosis. In a review of unexplained heart block in patients younger than 55 years of age, cardiac sarcoid or giant cell myocarditis accounted for 25% of cases, and these patients had a high incidence of sudden death or ventricular tachycardia or the need for cardiac transplantation. Some causes of heart failure such as sarcoidosis and inherited mutations of lamin nuclear proteins can trigger ventricular arrhythmias directly, even in the absence of clinical systolic dysfunction. More commonly, ventricular arrhythmias arise within a substrate of myocyte hypertrophy and chronic myocardial remodeling with diffuse or focal fibrosis, in common response to various causes of cardiac injury. Ventricular arrhythmias may present simultaneously with the diagnosis of systolic dysfunction or heart failure. Therapeutic options and prognosis for ventricular arrhythmias in the setting of heart failure are constrained by the cause and the clinical severity of the heart failure. Those with the worst heart disease gain the least in terms of survival after an aborted arrhythmic event caused by death from pump failure and other related comorbidities. In the short term, addressing congestion and hypoperfusion will maximize the chance of a successful procedural outcome. Note possibility of prior embolic infarction from atrial fibrillation or dilated ventricle. Although generally considered as distinct entities on the basis of biopsy and presentation, sarcoidosis and giant cell myocarditis may represent different levels along a spectrum of inflammation with giant cells. Hearts showing sarcoidosis on endomyocardial biopsy have occasionally been found to have areas consistent with giant cell myocarditis after removal at the time of transplantation. Cases of patients in whom giant cell myocarditis has been stabilized for a year or longer by high-dose immunosuppressive therapy have been reported. Most cases are related to an allergic reaction to long-term administration of a drug, but eosinophilic syndromes from other causes may also cause eosinophilic myocarditis. Arrhythmias and systolic dysfunction generally respond well to steroid treatment and withdrawal of the offending drug, although patients may be left with restrictive physiology. It should be noted that Lyme disease has been reported rarely to cause clinical myocarditis with or without clinical conduction system disease. Most cases are transmitted in an autosomal dominant pattern, but autosomal recessive, X-linked, and mitochondrial inheritance patterns are also well recognized. Sudden death and ventricular arrhythmias are often the initial presentation frequently provoked by exercise. Peripartum cardiomyopathy is rarely associated with clinical arrhythmias, except in the setting of severe hypoxia or acidosis. When evidence shows some clinical improvement by this time, longer deferral would be desirable in patients in whom the only identifiable cause is one that may be reversible, such as peripartum cardiomyopathy or heart failure with a recent history of heavy alcohol intake. In heart failure with known coronary artery disease, ischemia and infarction that contribute to hemodynamic deterioration and arrhythmias may occur without recognized angina. Baseline abnormalities of cardiomyopathy may mask typical diagnostic features; therefore perfusion stress imaging or coronary angiography is often required. Identifying the type of ventricular arrhythmia is helpful in determining the cause. Hypoperfusion should be suspected in patients with a narrow pulse pressure, even if the systolic blood pressure is preserved, and in patients with vague mental status and cool calves and forearms. Because functional capacity is not well correlated with the ejection fraction, careful questioning about daily activities and limiting symptoms is crucial for assessment of disease trajectory. Once attributed solely to decreased cardiac output, renal dysfunction with progressive heart failure is now recognized to be influenced more by elevated right-sided filling pressures. The rate of heart failure progression is accelerated by even modest degrees of renal impairment. The dynamic nature of renal function in advanced heart failure is crucial to recognize in relation to clearance of antiarrhythmic agents and risk of life-threatening hyperkalemia in the setting of aldosterone antagonists. When hemodynamic stabilization cannot be achieved, or when the hemodynamic profile remains uncertain, right-heart catheterization can be useful for clarifying right- and left-sided filling pressures, perfusion, and systemic and pulmonary vascular resistance to guide further therapy.
Cheap 1mg propecia visa
In addition hair loss medicines buy 1 mg propecia mastercard, careful and prompt attention to reinstitution of parenteral nutrition during episodes of intolerance of enteral feeds cannot be overemphasized. Changes in both morphogenesis and cellular differentiation drive structural formation of the gastrointestinal tract in the developing embryo. Advances in molecular biology have revealed that specific aspects of gastrointestinal tract development involve genetically controlled interaction between trophic compounds and cellular receptors, as described later for the different organs of the gastrointestinal tract. From a global perspective, the gastrointestinal tract results from embryonic invagination and folding during week 4 of gestation. Eventually, the buccopharyngeal and cloacal membranes rupture, permitting a direct communication between the fetal gastrointestinal tract and the in utero environment. A series of folding, lengthening, and luminal dilation events result in the formation of the foregut (esophagus, stomach, duodenum, liver, and pancreas); the midgut (jejunum, ileum, ascending colon, and transverse colon); and hindgut (descending colon, sigmoid colon, and rectum). With additional elongation and growth during the first trimester, the developing gut migrates into the umbilical cord. Thus, by the second trimester, basic morphogenesis of the fetal gastrointestinal tract is complete. Although dysmotility is a normal developmental "milestone" in the fetal environment, uncoordinated peristalsis in the extremely low-birthweight infant is associated with significant postnatal problems. Knowledge of the cellular and molecular processes of early morphogenesis is rapidly expanding and involves crosstalk between maternal and fetal factors during development. We first discuss the embryology of the gastrointestinal tract in advance of discussing functional development including digestion. In the second stage, the lung bud develops from the caudal lung field proximal to the liver. Next, in the third stage, longitudinal ridges appear inside the lumen of the developing foregut, which results in a distinct and separate dorsal esophageal area. The fourth stage involves proliferation of the longitudinal ridges, resulting in a tracheoesophageal septum. Subsequently, apoptosis in the central section of the septum begins the initial separation of the dorsal and ventral compartments. In the fifth stage, there is the formation of definitive respiratory and esophageal structures between weeks 6 and 7 of gestation. Researchers utilizing Drosophila and murine models have identified a myriad of key signaling pathways in foregut development. Hedgehog binds to a cell membrane receptor Patched (Ptc) resulting in downstream signaling and transcription factor mediated cell differentiation. The muscular layers (the inner circular and outer longitudinal) become visible by 9 weeks. By week 12 of gestation, the gastric mucosa has differentiated into the various types of epithelium: the zymogen, endocrine, mucous, and parietal cells. Several trophic factors have been shown to be involved in gastric epithelial differentiation. The foregut, midgut, and hindgut are shown with their individual blood supply supported by the common dorsal mesentery in the sagittal plane. Note the narrow duodenocolic isthmus from which the midgut loop depends and the right-sided position of the small intestine and left-sided position of the colon. Maintenance of this position within the abdomen after birth is termed nonrotation. C, About the 10th week of intrauterine life, during the second stage of rotation (anteroposterior view). The bowel in the temporary umbilical hernia is in the process of reduction; the most proximal part of the prearterial segment entering the abdomen to the right of the superior mesenteric artery is held forward close to the cecum and ascending colon, permitting the bowel to pass under it. As the coils of small intestine collect within the abdomen, the hindgut is displaced to the left and upward. From its original sagittal position, the midgut has rotated 270 degrees in a counterclockwise direction about the origin of the superior mesenteric artery. Fibroblast growth factors 10 and 2, proteins in the hedgehog pathway, are strong determinants of gastric epithelial differentiation, in particular with parietal cell differentiation (Spencer-Dene et al, 2006). Fate-mapping experiments demonstrate that the liver arises from precursor cells in the developing ventral foregut as well as from a small group of endodermal cells tracking down the ventral midline. The pancreas is also induced in lateral endoderm domains, adjacent and caudal to the lateral liver domains, and in cells near the dorsal midline of the foregut (Zaret and Grompe, 2008). After the initial differentiation, several transcription factors shape the developing liver precursor cells into hepatocytes and bile duct cells. By 14 weeks, immunoreactive insulin can be detected and pancreatic zymogen granules are present in the acinar cells. Trypsin, lipase, and amylase are secreted into the duodenum by 31 weeks (Zoppi et al, 1972). The cranial portion of the bud differentiates into hepatic parenchyma, and the caudal portion into the gallbladder. In the absence of Hh (A), the receptor Patched (Ptc) exerts an inhibitory effect on Smoothened (Smo), a transmembrane protein with homology to G-protein-coupled receptors. In the presence of Hh ligand-binding (B), the inhibitory action of Ptc on Smo is released. Therefore, it is important to understand the development of the cellular differentiation as well as overall intestinal length. As previously mentioned, the hedgehog signaling pathway is also important in endodermal and mesodermal differentiation in small intestinal development. Glucagon-like peptide 1 and 2 are secreted by intestinal neurons and L cells, respectively, and are associated with increased intestinal length (Sigalet et al, 2004). Clinical trials in adults are underway administering glucagon-like peptide 2 in patients with short bowel syndrome and may eventually show promise in pediatric patients with intestinal failure. The small intestine is well developed after its extracorporeal migration into the umbilical cord. By 12 weeks, this primitive structure takes on the gross anatomic features of the colon. At this same time, the midgut rotation is completed, resulting in the cecum being located in the right lower abdominal space. The hallmark of colonic function is coordinated motility, especially in the development of the rectum. The rectum forms by 8 weeks, and formation of complete muscle layers and neural migration of neural crest cells are accomplished by 24 weeks. By 22 weeks, the premature colon maintains some aspects of the small intestine, including villi and disaccharidase function. With developmental maturation, the colonic crypt structures dominate the mucosal surface, and the intestinal characteristics diminish (Raul et al, 1986). From a cellular developmental aspect, several trophic factors have been linked to colonic differentiation. The developing enteric nervous system is derived in a large part from the vagal neural crest cells with additional contribution from migration of the precursor cells from the sacral region. As with other aspects of gastrointestinal tract development, the mucosal immune system undergoes both fetal and postnatal changes. The dramatic changes following exposure to food and bacterially derived molecules after birth have been shown to be a major determinant in ongoing mucosal immune modification. Although primarily considered to be involved in digestion, gastric acid, bile salts, and pancreatic secretions function to inhibit potential pathogenic bacterial growth. Previously, it was believed that mucus functions in a nonspecific manner to prevent bacterial adhesion and expel potential pathogens. It is now clear that certain components of the mucus layer are involved in mucosal healing. Specifically, the trefoil factor family has proangiogenic and antiapoptotic qualities, as well as modulating cell-to-cell contacts and potentiating epidermal growth factor (Hoffmann, 2005). The epithelial barrier function is accomplished by intracellular proteins that anchor the cells to each other, preventing large molecules from penetrating. Recently, it has been shown that these proteins are not just "spot welds" but are dynamic in nature and respond to physiologic and pathologic stimuli (Graham et al, 2009).
Cheap propecia 1 mg with mastercard
Furosemide hair loss in men 501 cheap 5mg propecia otc, digoxin, and afterload reduction are often needed to control heart failure, and some cardiologists will start these medications in the immediate postnatal period because of the high likelihood of infants developing congestive heart failure. It is very rare that palliative banding of the pulmonary artery is needed to control heart failure symptoms. The degree of pulmonic stenosis determines the pathophysiology of the disease process. As the stenosis of the valve worsens, right ventricular pressure increases along with the degree of right ventricular wall stress. In severe, or critical, pulmonic stenosis (discussed later), heart failure can develop in the neonate accompanied by cyanosis due to right-to-left shunting at the atrial level. The degree of stenosis is generally classified based on the pressure drop across the pulmonic valve, with mild stenosis defined as a gradient <30 mm Hg, moderate stenosis as a gradient of 30 to 60 mm Hg, and severe stenosis as >60 mm Hg. In many instances, mild narrowing of the branch pulmonary arteries occurs in the neonate and produces a murmur that is heard widely throughout the chest. This lesion likely reflects mild hypoplasia of the branch pulmonary arteries due to decreased in utero pulmonary blood flow and the postnatal transition where these vessels must accommodate the entire cardiac output. B, Using color Doppler imaging, turbulence in the main pulmonary artery is seen above the pulmonic valve. Consideration of the valve gradient is critical because of the prognostic significance of the value. In infants, however, follow-up of patients with echo gradients <40 mm Hg found that 29% developed progressive valve stenosis, with half of those showing an increase in the first 6 months of life (Rowland, 1997). Neonates with moderate valve stenosis may face an even greater likelihood of developing progressive stenosis, although limited data exist. A systolic ejection murmur of pulmonic stenosis can be heard in the neonatal period at the upper left sternal border. Typically, although the fast heart rate in the neonate may make it difficult to appreciate, a systolic ejection click just after the first heart sound (S1) can be heard in most of these infants and is an important feature to distinguish pulmonic stenosis from other lesions. As the gradient across the valve worsens, a thrill may be palpable at the upper left sternal border. As the degree of stenosis progresses further and becomes severe, the murmur and click will diminish and may even be absent as right ventricular dysfunction worsens. Of note is that while progressive pulmonic stenosis may be able to be estimated on the basis of the murmur, the clinical condition of the infant may not change appreciably until the degree of stenosis becomes severe. The findings on laboratory studies in infants with pulmonic stenosis will vary depending on the degree of stenosis. Electrocardiogram will demonstrate right ventricular hypertrophy in most patients with moderate stenosis, although the study may be normal when mild stenosis is present. Chest radiography is often normal unless poststenotic dilation of the main pulmonary artery has developed. The valve will have varying degrees of dysplasia that is characterized by thickened, poorly mobile leaflets that dome during systole. As discussed earlier, Doppler echo generally gives a value of stenosis that is 20% to 30% higher than the peak-to-peak pressure gradient measured as cardiac catheterization. Treatment of isolated pulmonic stenosis, even in the neonate, can readily be performed by balloon valvotomy in the cardiac catheterization laboratory. Mild or moderate pulmonary insufficiency, should it develop after balloon valvotomy, is usually well tolerated. Recurrent stenosis and more significant pulmonic insufficiency are found more often when valvotomy is needed in the neonatal period (Garty et al, 2005). Levels of obstruction of the left ventricular outflow tract can also occur at the subvalvar and supravalvar levels. Subvalvar stenosis is rarely diagnosed in the neonatal period, but often progresses later in life as a fibromuscular ridge beneath the aortic valve. Supravalvular stenosis can present in the newborn period and is often associated with Williams syndrome. As with pulmonic stenosis, the pathophysiology and physical findings associated with aortic valve stenosis depend on the degree of obstruction. Certainly the most common aortic valve abnormality addressed in the neonatal period is critical aortic stenosis associated with decreased left ventricular function. Mild (aortic valve gradient <30 mm Hg) and moderate (valve gradient of 30 to 60 mm Hg) aortic valve stenosis is not commonly encountered in the neonatal period. When it is, these milder forms of stenosis are generally associated with a bicuspid aortic valve and tend to progress with age. The rate of change of progression throughout infancy and childhood is quite variable and necessitates frequent follow-up of these patients. The murmur in the newborn with aortic stenosis may be difficult to localize to the upper right sternal border as in older children. A thrill is usually palpable at the suprasternal notch with even mild aortic valve stenosis with a precordial thrill felt as the degree of stenosis increases. Usually a click from the stenotic aortic valve is heard at the apex or lower left sternal border. Chest radiograph is of limited benefit in following these patients, with the focus of the diagnostic assessment being the echocardiogram. Pulsed Doppler is used to determine the gradient across the valve; color Doppler imaging can define the presence of aortic insufficiency. Initial management of moderate aortic valve stenosis is balloon valvotomy in the cardiac catheterization laboratory. The balloon is sized in an effort to limit aortic insufficiency, which is much less well tolerated than insufficiency of the pulmonic valve. If significant aortic valve insufficiency is present or develops, surgical repair or valve replacement is needed. In neonates and infants, the Ross procedure is usually the procedure of choice (Elkins et al, 1994). In this procedure, the pulmonary valve is removed intact from the patient and sewn into the aortic position, and a homograft is placed in the pulmonic position. Interestingly, the pulmonary autograft generally demonstrates good growth and excellent function in the aortic position. Although the child will outgrow the pulmonary homograft, replacing it and managing progressive pulmonic stenosis is much easier than addressing the aortic valve. The shunt results in mixing of the systemic and pulmonary venous returns that can occur between the atria and ventricles or great vessels. Defects manifesting predominantly with cyanosis can be further subclassified by the amount of associated pulmonary blood. If there is no restriction to pulmonary blood flow, cardiac output to the lungs will increase as the normal postnatal drop in pulmonary vascular resistance occurs. Clinically, this results in tachypnea, poor feeding, hepatomegaly, and pulmonary edema. Much of the neonatal management is aimed at balancing the ratio of systemic to pulmonary blood flow. Defects with restriction to pulmonary blood flow typically present with cyanosis without associated symptoms of congestive heart failure. If the restriction is severe, pulmonary blood flow may be dependent on a left-to-right shunt through the ductus arteriosus. Lesions presenting primarily with cyanosis in the newborn period are discussed below. Desaturated blood returns to the right ventricle and is recirculated to the body via the aorta, while oxygenated blood returns to the left ventricle and is recirculated to the lungs. With absent or small communications between the circulations, severe systemic acidosis and hypoxia develop after birth, resulting in death. Cyanosis is apparent within the first few hours of life and is not responsive to oxygen. Because of the arrangement of the great vessels, the louder closure of the anterior aortic valve obscures closure of the more posterior pulmonary valve. Chest radiograph may be normal or reveal a narrow mediastinum with slight predominance of the right ventricle resulting in an "egg on a string" appearance. Prostaglandin E1 is started to maintain patency of the ductus arteriosus (dose of 0. In the setting of adequate mixing, pulmonary overcirculation may develop as pulmonary vascular resistance drops. A, the dashed lines depict the planned location of transection of the great vessels.
Discount generic propecia uk
Approximately 80% of total plasma magnesium is filtered through the glomerulus and is reabsorbed mainly in cortical segments of the thick ascending limb of the loop of Henle new hair loss cure close to market generic propecia 1mg amex. Once the maximal tubular reabsorption is exceeded, filtered magnesium is excreted into the urine. Hormones regulate magnesium reabsorption by changing the transepithelial voltage and paracellular permeability of tubular cells. Approximately 10% of plasma Pi is noncovalently bound to protein, whereas 90% circulates as ions or as complexes with sodium, calcium, or magnesium. About 80% to 85% of total body phosphorus contributes to mechanical support as part of the hydroxyapatite lattice of bone. Although phosphorus and calcium can be absorbed along the entire length of the small intestine, most phosphate transport takes place in the jejunum and ileum, whereas most calcium absorption occurs in the duodenum. The renal proximal tubule is the principal regulatory site for phosphorus homeostasis (Silver and NavehManey, 2009). At lower serum phosphorus levels, most filtered phosphorus is reabsorbed; at higher levels, most filtered phosphorus is excreted. This adaptation permits avid tubular phosphate conservation despite high ambient serum phosphate levels. For this reason, neonatal disorders of chronic hypophosphatemia and/or phosphorus depletion usually result from inadequate dietary supply (as in preterm infants) or intrinsic. Deficiency or excess of either hormone causes hypocalcemia or hypercalcemia, respectively. This versatile receptor mediates actions of its two physiologic ligands in multiple tissues and signals through several second messenger pathways. Previtamin D in the skin undergoes isomerization to the biologically inert vitamin D. Maternal total serum calcium declines slightly during pregnancy, reaches a nadir in the mid-third trimester, and then increases slightly toward term. The maternal serum phosphorus and magnesium profiles are similar to that of calcium. The interplay of calcitropic and progestational hormones in pregnancy protects the maternal skeleton from demineralization. In the third trimester, fetal plasma total and ionized calcium and phosphorus levels are higher than maternal levels, producing a state of "physiologic fetal hypercalcemia" (Rubin et al, 1991). Human calcitonin is a 32-aminoacid chain with a 1,7-disulfide bridge and a C-terminal prolinamide. Alternative splicing of several transcripts from the calcitonin gene produces several polypeptide products, some of which have uncertain calcitropic importance. The primary stimulus for calcitonin secretion is a rise in circulating calcium concentration. Calcitonin lowers serum calcium and phosphorus chiefly by inhibiting bone resorption. Currently, there is no compelling evidence that the calcitonin-like calcium-lowering hormones are critical regulators of calcium homeostasis in nonpregnant adult humans, perhaps because the low prevailing rate of bone turnover blunts the impact of the antiresorptive actions. However, calcitonin may have important calcitropic functions in pregnant and lactating women and in the fetus and neonate, and in other mammals, particularly rodents, whose bones are constantly growing. In human newborns, the C cell population and serum calcitonin concentrations are much greater than in adults. In humans, a doubling of maternal intestinal calcium absorption and a net increase of calcium accretion into bone compensate for the formidable demand on maternal calcium (Prentice, 2000). In healthy term newborns, total calcium concentration and Ca2+ decline from nearly 11 mg/dL and 6 mg/dL, respectively, in umbilical cord blood to serum levels of 8 to 9 mg/dL and 5 mg/dL by 24 to 48 hours. Serum calcitonin levels increase sharply during the 1st day and remain elevated compared with those in adults. By 2 weeks of life, serum calcium rises to the mean values observed in older children and adults. During the 1st week of life, urinary phosphate excretion is significantly higher in preterm than in term infants but then approximates that of term infants, possibly owing to accelerated postnatal renal maturation. After the first several days, calcium excretion increases with a magnitude inversely proportional to gestation. These changes may reflect the relative phosphate deficiency in many preterm infants, which results in an adaptively low urinary phosphate excretion, decreased bone mineralization, and, consequently, relatively high urinary calcium excretion. Under conditions of normal acid-base status and normal serum albumin, serum total calcium and Ca2+ levels are linearly correlated, so total serum calcium measurements remain useful as a screening test. However, because Ca2+ is the physiologically relevant fraction, in sick infants it may be preferable to assay [Ca2+] directly in freshly obtained blood samples. A precise definition of hypocalcemia, like hypoglycemia, in preterm infants is particularly difficult to formulate. A useful approach to the classification of neonatal hypocalcemia is by time of onset. Clinical Findings Because Ca2+ couples excitation and contraction in skeletal and cardiac muscle, increased neuromuscular excitability (tetany) is a cardinal feature of hypocalcemia. However, hypocalcemic signs in neonates are variable and may not correlate with the magnitude of the decline in Ca2+. Although some infants are severely affected, others having equally depressed serum calcium levels may be asymptomatic. Tetanic infants are jittery and hyperactive, frequently exhibit muscle jerks and twitches, and may have generalized or focal clonic seizures. Occasionally, respiratory or gastrointestinal rather than neurologic signs predominate. Laryngospasm with inspiratory stridor, sometimes severe enough to cause cyanosis or anoxia, or wheezing due to bronchospasm may be a presenting manifestation. Vomiting, possibly related to pylorospasm, sometimes causes hematemesis or melena. At times, the gastrointestinal signs are severe enough to mimic those of intestinal obstruction. Other signs of neonatal tetany include extensor hypertonia, apnea, tachycardia, tachypnea, and edema. Early Neonatal Hypocalcemia Hypocalcemia occurring during the first 3 days of life, usually between 24 and 48 hours postpartum, is termed early neonatal hypocalcemia. In preterm infants, there is a steeper and more rapid postnatal decline in serum calcium; the magnitude of depression is inversely proportional to gestational age. However, the fall in Ca2+ is not proportional to the fall in total calcium concentration, and the ratio of ionized to total calcium in these newborns is higher than at term. This "sparing" of Ca2+ may be related to the lower serum protein concentration and pH in prematurity. The sparing effect on Ca2+ also, in part, explains the frequent absence of hypocalcemic signs in preterm infants. High renal sodium excretion in preterm infants also probably aggravates calciuric losses. Currently, there is no convincing evidence that abnormalities in vitamin D metabolism are involved in the etiopathogenesis of hypocalcemia in preterm infants. Early neonatal hypocalcemia with hyperphosphatemia is frequently observed in severely stressed or asphyxiated infants. The causes are probably multifactorial and include, to varying degrees, renal insufficiency, tissue catabolism, and acidosis. Low serum Ca2+ and elevated serum magnesium levels have been correlated with severity of hypoxic-ischemic encephalopathy and poor outcome (Ilves et al, 2000). The course usually is similar to that of early neonatal hypocalcemia in preterm infants, although hypocalcemia sometimes persists for several additional days. Hypercalcitonemia, hypoparathyroidism, abnormalities in vitamin D metabolism, and hyperphosphatemia all have been implicated, but none has been consistently found. Late Neonatal Hypocalcemia Late neonatal hypocalcemia, or hypocalcemia developing after 3 to 5 days of life, occurs more frequently in term than in preterm newborns and is not usually associated with maternal diabetes, birth trauma, or asphyxia. Serum calcium levels frequently increase when these infants are placed on a low-phosphate formula and supplemental calcium. The pathogenesis of this "transient hypoparathyroidism" in late neonatal hypocalcemia is not readily apparent. In other infants, maternal vitamin D deficiency can cause late (or occasionally "early") neonatal hypocalcemia.
New Zealand Green Lipped Sea Mussel (New Zealand Green-Lipped Mussel). Propecia.
- How does New Zealand Green-lipped Mussel work?
- Are there safety concerns?
- Osteoarthritis, rheumatoid arthritis, and asthma.
- Dosing considerations for New Zealand Green-lipped Mussel.
- What is New Zealand Green-lipped Mussel?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96806
Order 5mg propecia otc
Vasoactive medications can be used to alter systemic vascular resistance and improve ventricular function hair loss nizoral cheap propecia 1 mg without prescription. Use of these medications is determined by clinical presentation and echocardiographic findings. Milrinone can be used to provide some afterload reduction, if tolerated by blood pressure. The inotropic effects of milrinone are also an advantage if ventricular function is poor. In addition to decreasing pulmonary blood flow, afterload reduction has the added benefit of decreasing tricuspid valve regurgitation if it is present. Milrinone also dilates the pulmonary vascular bed, so care should be taken when it is used. Although counterintuitive, when faced with an unoperated patient with high oxygen saturations and low peripheral blood pressure, the gentle addition of milrinone may improve blood pressure simply by increasing systemic blood flow. The immediate goal of surgical palliation is to provide stable unrestricted systemic and coronary blood flow and reliably restricted pulmonary blood flow. The Sano modification has the presumed benefit of providing pulsatile flow to the pulmonary arteries without aortopulmonary diastolic run off and coronary steel. A hybrid procedure that combines stent placement in the ductus arteriosus by the cardiologist and pulmonary artery banding by the surgeon is an approach being taken by a number of institutions that provides a relatively noninvasive stage I palliation for hypoplastic left heart syndrome (Caldarone et al, 2007). Each of these procedures has its pros and cons and its advocates and detractors (Caldarone et al, 2007; Ghanayem et al, 2006; Malec et al, 2003). Longer-term prospective studies are needed to determine the optimal approach to stage I palliation. The superior cavopulmonary anastomosis (bidirectional Glenn) is usually performed between 4 and 6 months of age. During this procedure, the conduit providing pulmonary flow is removed and the superior vena cava is anastomosed to the pulmonary artery. An inferior cavopulmonary anastomosis (Fontan completion) is performed by one of several techniques. Physiologically, obstruction to pulmonary venous flow results in pulmonary venous hypertension that is transmitted to the pulmonary capillary bed, resulting in pulmonary edema. The ductus arteriosus is ligated, and an incision is made from the proximal ascending aorta around the aortic arch to the level of the ductus. B, A pulmonary homograft is utilized to create a patch to reconstruct the neoaorta. C and D, this homograft patch is used to connect the proximal main pulmonary artery and pulmonary (neoaortic) valve to the ascending aorta and transverse arch. E, A modified BlalockTaussig shunt is placed from the base of the innominate artery to the right pulmonary artery. F, An alternative technique utilizing a circumferential tube graft from the proximal main pulmonary artery to the distal transverse aortic arch. Not shown: Atrial septectomy is performed to provide unobstructed egress from the pulmonary veins to the right ventricle. Newborns thus present with profound cyanosis and respiratory distress that is not responsive to medical management. Prostaglandins may help minimize the obstruction by maintaining patency of the ductus venosus, but patency of the ductus arteriosus does not improve the clinical picture, because the limitation to pulmonary blood flow is not due to insufficient antegrade flow, but rather obstructed outflow. The pulmonary veins can be small because of limited flow, making them difficult to detect by two-dimensional and color Doppler imaging. The Blalock-Taussig shunt is replaced with a Gore-Tex tube inserted from the right ventricle to the main pulmonary artery. During normal development, the common pulmonary vein becomes incorporated into the left atrium, resulting in the usual pattern of two right and two left pulmonary veins entering the left atrium. Abnormal incorporation of the common pulmonary vein can result in cor triatriatum, a condition in which the common pulmonary vein joins the left atrium through a single opening. Surgical resection of the membrane that separates the left atrium and common pulmonary vein is an effective treatment. Significant preoperative pulmonary venous obstruction increases surgical mortality. The stenosis can occur in the supravalvular region, at the valve annulus, or within the mitral valve support apparatus. Typical congenital mitral stenosis is characterized by thickened leaflets, short or absent chordae tendineae, obliteration of interchordal spaces, and two separate papillary muscles. Supravalvar mitral ring occurs when there is connective tissue outgrowth on the atrial surface of the mitral valve leaflets, leading to a decreased mitral valve orifice. The mitral valve orifice can also be stenotic secondary to a parachute mitral valve, when most or all chordae tendineae insert onto only one papillary muscle. Another form of obstruction occurs with a double orifice mitral valve, where a tongue of tissue connects the anterior and posterior mitral valve leaflets. A mitral arcade or hammock occurs when the leaflets are connected directly or by short chordae to the papillary muscles. Congenital mitral stenosis frequently occurs in conjunction with other left-sided obstructive lesions. Symptoms from mitral stenosis usually occur in the first 2 years of life and may consist of shortness of breath, respiratory distress or wheezing, cyanosis, and pallor. Cardiac exam reveals a rumbling apical diastolic murmur, loud first heart sound, and loud split second heart sound. Echocardiogram is used to define mitral valve anatomy and localize the area of obstruction. Doppler can be used to determine valve gradient and estimate right ventricular pressure. Treatment options for congenital mitral valve stenosis include balloon mitral valvuloplasty, surgical mitral valvuloplasty, and mitral valve replacement. Despite recent improvements in outcomes, intervention and mitral valve replacement have relatively poor short-term outcomes (McElhinney et al, 2005). Patients with additional leftsided obstructive lesions or associated defects frequently require single-ventricle palliation. Frontal view through opened aorta demonstrates stenotic and dysmorphic aortic valve with commissural fusion. Severe aortic valve stenosis is defined as a Dopplerderived pressure gradient greater than 60 mm Hg. Moderate stenosis is defined as gradient of 30 to 60 mm Hg, whereas mild stenosis is a peak gradient less than 30 mm Hg. In the setting of depressed left ventricular function, the Doppler echo-derived gradient may be significantly lower and underestimate the severity of the stenosis. The longstanding pressure overload on the left ventricle causes left hypertrophy and left ventricular scarring (endocardial fibroelastosis). In some cases, as discussed earlier, the disease progresses to hypoplastic left heart syndrome. Attempts have been made to identify fetuses at high risk for progressing to hypoplastic left heart syndrome and then perform an in utero valvuloplasty with the hope of alleviating the obstruction and altering the course of the disease (Makikallio et al, 2006). Although initial results with this procedure are promising, more work is needed in this area. Clinically, critical aortic stenosis manifests in the newborn period with signs of decreased systemic perfusion: pallor, decreased pulses, and prolonged capillary refill. The volume and quality of the murmur correlate with the severity of stenosis in the setting of normal left ventricular function. If left ventricular function is depressed, the murmur may be soft despite severe stenosis. Electrocardiogram reveals left ventricular hypertrophy with possible T-wave abnormalities. Heart size is typically normal on chest film, although the aortic knob may be prominent and pulmonary congestion may be present. Echocardiogram is used to define the location and severity of the left ventricular outflow tract obstruction. Aortic stenosis is commonly found with other left-sided obstructive lesions, with possible underdevelopment of left heart structures. These findings may alter the treatment plan and lead to single-ventricle palliation. Published models have attempted to identify echocardiographic findings that predict the suitability of a two-ventricle repair in neonates with critical aortic stenosis (Colan et al, 2006; Lofland et al, 2001; Rhodes et al, 1991).
Order propecia 1mg without a prescription
During the early neonatal period hair loss cure at home propecia 5 mg online, however, the increased oxygen-carrying capacity of blood (see Physiologic Anemia of Infancy and Prematurity, later) may blunt any compensatory erythropoietic activity in cases of mild hemolysis. Consequently, hyperbilirubinemia in excess of normal neonatal levels may be the only apparent manifestation of hemolysis. In most cases of significant hemolysis, however, some degree of reticulocytosis is usually present. The spectrum of clinical problems ranges from minimal anemia and hyperbilirubinemia to severe anemia with hydrops fetalis. At one time, before effective prevention of Rh sensitization was available, hemolytic disease of the newborn was responsible for more than 10,000 deaths annually in the United States (Freda et al, 1975). Rh Hemolytic Disease: Erythroblastosis Fetalis the role of Rh antibody in classic erythroblastosis fetalis was first elucidated by Levine and Katzen in 1941 (Levine et al, 1941). Several Rh antigens are recognized, each of which is detected by specific antibodies. It is known that Rh blood group antigens are determined by at least two homologous but distinct membrane-associated proteins. Two of these membrane proteins have separate isoforms (C and c; E and e), which are detected by specific antibodies (anti-C and anti-c; anti-E and anti-e). A lowercase d is used to denote the absence of D, or Rh-negative status; it is not related to a specific antigen-no "anti-d" serum has been identified. It is high in whites (15%), lower in blacks (5%), and virtually nonexistent in Asians. Current understanding of the natural history of Rh sensitization is derived largely from clinical experience gained before the immunologic prevention of neonatal hemolysis was readily available. Historically, Rh hemolytic disease was rare (occurring in 1% of cases) during the first pregnancy involving an Rh-positive fetus but increased significantly with each subsequent pregnancy. The major factor responsible for the reduced death rate is the development of Rh immune globulin to prevent maternal sensitization. The practice of administering a single intramuscular dose of Rh immune globulin (300 g) to unsensitized Rh-negative mothers within 72 hours of delivering an Rh-positive infant led to the virtual elimination of Rh(D) sensitization as a major cause of hemolytic disease in newborns (Freda et al, 1975). The few treatment failures seen were attributed to fetomaternal bleeding of greater than 30 mL at delivery or bleeding that occurred antenatally. Moreover, the dose of Rh immune globulin should be increased proportionately when there is evidence of larger-than-normal fetomaternal bleeding at delivery. All women should be screened at the time of delivery using the rosette test to screen for fetal red cells (Brecher, 2002). Positive results should be followed by a quantitative test such as the Kleihauer-Betke test (Judd, 2001). Rh immune globulin also should be administered to unsensitized Rh-negative women after any event known to be associated with increased risk of fetomaternal hemorrhage. Despite the use of antenatal and postnatal prophylaxis with Rh immune globulin, 0. A recent case-control study (Koelewijn et al, 2009) demonstrated several independent risk factors for sensitization, including nonspontaneous delivery. However, in almost half of the failures, none of these risk factors could be identified. Depending on the amount of anti-D absorbed, a variable degree of fetal hemolysis occurs, thereby leading to anemia, hepatosplenomegaly, and increased bilirubin formation. In utero, bilirubin is removed by transfer across the placenta into the maternal circulation; therefore, hyperbilirubinemia is not a problem until after delivery, when levels may increase because of immaturity of hepatic conjugating enzymes. The major threat to the fetus is severe anemia leading to hydrops fetalis and intrauterine death. Aside from early phototherapy, these newborns generally require no therapy unless the postnatal rate of rise in bilirubin is greater than expected. Infants who do not become sufficiently jaundiced to require exchange transfusion are at risk of development of severe late anemia associated with a low reticulocyte count, usually at 3 to 6 weeks of age; thus, it is important to closely monitor hemoglobin levels after hospital discharge. This form is characterized by hemolysis, moderate anemia (cord blood hemoglobin less than 14 g/ dL), and increased cord blood bilirubin levels (greater than 4 mg/dL). The risk of development of bilirubin encephalopathy is high if these neonates do not receive treatment. This approach has been responsible for the favorable outcome for most infants with moderate alloimmune hemolysis. It is common for newborns who receive exchange transfusion to demonstrate a lower-than-normal hemoglobin concentration at the nadir of their "physiologic" anemia. Severe hemolytic disease is seen in approximately 25% of affected infants, who are either stillborn or hydropic at birth. Understanding of hydrops fetalis, originally attributed to high-output cardiac failure secondary to severe anemia, is incomplete. One of these is low colloid osmotic pressure resulting from hypoalbuminemia, a consequence of hepatic dysfunction. Management of seriously affected fetuses is directed at the prevention of severe anemia and death. An increase in the maternal anti-D titer in a previously sensitized Rh-negative woman is a good serologic measure of a fetus in potential jeopardy. Moreover, a previous history of neonatal hemolytic disease resulting from anti-D antibodies suggests that the current fetus also may be at risk. In this regard it may be useful to know the fetal Rh blood type because this identifies those Rhnegative infants who are not at risk. When the fetus is found to be Rh-negative, no further maternal monitoring or fetal blood studies are necessary. An increase in the maternal titer of immunoglobulin G (IgG) anti-D indicates maternal sensitization but does not accurately predict the potential severity of fetal hemolysis. More recently, efforts have been made to use noninvasive detection of fetal anemia. Ultrasonography signs of hydrops fetalis represent a relatively late sign of fetal anemia, often not developing until Hgb values are more than 7 gm/dL below gestational age norm. In this study, 45% of infants had severe anemia at cordocentesis, defined as a hemoglobin level at least 5 standard deviations below the mean for gestational age. It was suggested by the authors that more than 50% of invasive procedures might be avoided using this technique. The rate of fetal trauma and morbidity associated with cordocentesis is less than 2% (Parer, 1988; van Kamp et al, 2005). Cordocentesis should be performed with blood available for intravascular intrauterine transfusion if necessary. Such blood should be type O, RhD negative, cytomegalovirus negative, and less than 72 hours from collection; extended crossmatch is often performed with maternal blood type. The transfusion is generally administered at approximately 20 mL per kg estimated fetal weight with a target of 40 to 50% hematocrit. For a full discussion and algorithm for management of pregnant patients with RhD alloimmunization, see Moise, 2008b. This hyperbilirubinemia reflects the severity of hemolysis and its effects on the fetal liver. Neonatal exchange transfusion, amniocentesis, selective early induction of delivery, and intrauterine fetal blood transfusions all have contributed to the declining neonatal death rate from Rh incompatibility. In persons with type A and type B blood, naturally occurring anti-B and anti-A isoantibodies largely are IgM molecules that do not cross the placenta. In contrast, the alloantibodies present in persons with type O blood also include IgG antibodies that can traverse the placenta (Abelson and Rawson, 1961). Laboratory features include evidence of minimal to moderate hyperbilirubinemia and, occasionally, some degree of anemia. The peripheral blood smear is characterized by marked spherocytosis that is indistinguishable from that seen in hereditary spherocytosis (see Hereditary Spherocytosis, later). Additional follow-up at 2 to 3 weeks of age to check for anemia in these infants is essential. Minor Blood Group Incompatibility With the sharp decline of hemolytic disease caused by Rh incompatibility, the proportion of cases caused by Rh c, Rh E, Kell, Duffy, and Kidd incompatibility has increased from the previous estimates of 1% to 3%, to as high as 20% (for Kell sensitization) (Geifman-Holtzman et al, 1997; Moise, 2008a).

Generic 5 mg propecia with mastercard
Clefts can affect the primary palate (lip hair loss in men zip up boots order genuine propecia online, alveolus, or anterior portion of the hard palate that extends to the incisive foramen) and secondary palate (posterior hard palate and soft palate). Clefts of the primary and secondary palate can be unilateral or bilateral and complete or incomplete. Children with cleft palate are at increased risk for eustachian tube dysfunction, recurrent otitis media, and acquired hearing loss, as well as speech issues later in childhood. Feeding difficulties, nasal regurgitation of feeds, and difficulty gaining weight may occur in infants with a cleft palate (submucous and overt clefts of the palate). Lateral facial clefting or macrostomia is associated with syndromes, including craniofacial microsomia and Treacher Collins syndrome. Midline clefting can be associated with other congenital defects as can be seen in orofaciodigital syndrome and frontonasal dysplasia. Orofacial clefting is rarely associated with clefting of the airway structures, such as cleft larynx or extension of clefting into the trachea. Clefting of the larynx may result in stridor, a hoarse cry, respiratory distress, swallowing dysfunction, feeding difficulties, regurgitation, and aspiration. Endocrine abnormalities can arise because the midline malformation affects the development of the hypothalamus and the pituitary gland. Clinical manifestations can include growth hormone deficiency, adrenal hypoplasia, hypogonadism, diabetes insipidus, and thyroid deficiency. Neurologic manifestations that warrant close attention include seizures, hypotonia, spasticity, autonomic dysfunction and developmental delays. An infant boy with hypertelorism, hypospadias, orofacial clefting, and symptoms of airway obstruction or aspiration should be evaluated for Opitz syndrome. Because of the potential impact of the orofacial cleft on breathing, eating, hearing, speech, facial growth, and dental health, it is recommended that infants and children with clefts be referred to a multidisciplinary care team for long-term management. In remote areas, the nearest cleft team may be found through the Cleft Palate Foundation website. Box 95-1 outlines one example of the multidisciplinary team of providers that might contribute to the care of a child born with a craniofacial malformation. On the initial assessment, the provider should assess the cleft and examine the infant for dysmorphic features and other anomalies. Hearing should be evaluated by evoked otoacoustic emissions, or by brainstem auditory evoked response if the newborn does not pass the initial hearing screen. A neonate with a complete cleft lip should be evaluated by a craniofacial or cleft team in the first 2 weeks of life, and some centers offer taping or presurgical molding (nasoalveolar molding) that can be initiated in this time period. Many mothers will be able to breastfeed an infant born with an isolated cleft lip. Breastfeeding a baby with cleft palate (with or without cleft lip) will prove extremely challenging because the open palate will not generate the negative pressure needed for sucking. There are a variety of cleft nipples/bottles that have been devised to allow for oral feeding including the cleft palate nurser (squeeze bottle), Haberman feeder, and Pigeon bottle ( Make sure the child is feeding in an upright position, as gravity will help prevent nasal regurgitation. Adequate weight gain is important, because these children will undergo multiple surgeries in the 1st year of life. Newborns with clefts are considered nutritionally high risk, and a dietitian should be consulted to help determine caloric needs and to closely monitor growth. In general, surgical closure of the lip and nasal deformity is done within the first 3 to 6 months of life. Palatoplasty typically occurs between 9 and 12 months of age to optimize speech and language development. If there are concerns about airway clefting or anomalies of the larynx or trachea, a chest x-ray should be obtained and the airway evaluated, in addition to appropriate evaluation of associated anomalies. Microlaryngoscopy under general anesthesia remains the gold standard in the diagnosis of a laryngeal cleft (Rahbar et al, 2006). Early diagnosis and proper repair of the laryngeal cleft are essential to prevent injury to the lungs. In approaching diagnosis of a syndrome, it is important to categorize the type of cleft (lip with or without palate, U-shaped or V-shaped cleft palate, or more atypical orofacial cleft) and to look for any other malformations. A referral to a clinical geneticist is recommended when an underlying diagnosis is suspected but not established. Testing may occur as part of the evaluation for fetuses with congenital heart disease, or due to parental history of 22q11. The clinical indications for genetic testing for this condition in neonates frequently include congenital heart malformations (particularly conotruncal anomalies), seizures secondary to hypocalcemia, dysphagia, cleft palate, and/or respiratory distress secondary to upper airway obstruction. In this section, we focus on the evaluation of infants with craniofacial characteristics suggestive of 22q11. Common features identified on the newborn physical exam include cleft palate, small, overfolded helices, and tapered fingers. Other clues to the diagnosis include dysphagia and/or nasal regurgitation (even in the absence of an overt cleft palate), congenital heart disease (most commonly conotruncal anomalies), and hypocalcemia (with or without seizures). For this reason, recommendations vary regarding routine testing of infants with isolated cleft palate. Most agree, however, that molecular testing is indicated for children with a cleft palate in combination with any of the other features that can be observed in 22q11. Before the availability of genetic testing for this condition, individuals with clinical features of 22q11. Subsequently, a subset of children with overlapping features in these conditions (such as congenital heart disease and cleft palate) was also noted to share a deletion on chromosome 22q. It has been estimated that more than 90% of individuals with "classic" features of the 22q11. In addition, many of the clinical comparative genome hybridization platforms are designed to detect deletions in this region. Evaluation and Management Infants for whom there is a high clinical suspicion and those testing positive for this deletion should receive genetic counseling in addition to studies to identify associated health concerns. Left to right: normal head shape, sagittal synostosis, coronal synostosis, and metopic synostosis. Additional studies include echocardiogram to evaluate for congenital heart malformations and renal ultrasound. Newborns should have a palatal exam to evaluate for overt or submucous clefting, as well as a diagnostic audiogram. Infants with evidence of dysphagia (even in the absence of a palatal cleft) would likely benefit from an evaluation by a feeding specialist to determine if a cleft bottle would be helpful. Additional recommendations for screening evaluations and management can be found at the GeneTests website (McDonald-McGinn et al, 2005). Advances in molecular genetics are permitting the identification of defective genes and their pathways in describing these congenital anomalies. The genetic etiology of syndromic craniosynostosis in humans is only partially understood. Known risk factors include male gender, intrauterine head constraint, twin gestation, and maternal smoking. Although uncommon, the most frequently encountered associated anomalies include congenital heart defects and genitourinary tract malformations. Premature fusion of the suture before birth leads to abnormal head shape in the newborn period. A breech-positioned neonate can have scaphocephaly or dolichocephaly that may be concerning for sagittal synostosis. However, in sagittal synostosis, frontal bossing progresses, whereas the head shape in a breech infant will normalize over time. Coronal synostosis is the second most common single suture synostosis (20% to 30%) with a prevalence of one in 10,000 births (Cohen, 2000a). Birth prevalence of all craniosynostoses is estimated to be 300 to 400 of every 1 million live births (Cohen, 2000a). In normal infants, open sutures allow the cranium to expand as the brain grows, producing the normal head shape. If one or more sutures fuse prematurely, there is restricted growth perpendicular to the fused sutures and compensatory growth in the patent sutures, producing abnormal head shape.
Order propecia 5 mg free shipping
The late-preterm and premature newborn are even more susceptible to these influences hair loss curezone body odor discount propecia 1mg amex. Any pathologic process that increases the production or impairs the elimination of bilirubin can exacerbate the normally occurring physiologic jaundice in newborns. Certain demographic, environmental, and genetic risk factors, among a myriad of icterogenic contributors, merit special clinical attention. Data derived from risk instruments that incorporate several factors support the potential multifactorial etiopathogenesis of marked hyperbilirubinemia; albeit genetic contributors may go undetected and individual factors confer different degrees of risk (Newman et al, 2000, 2005). These instruments further highlight the clinical importance of two specific risk factors in particular, namely (1) late preterm gestational age and (2) exclusive breastfeeding (Keren et al, 2008; Newman et al, 2000, 2005). This exaggerated hepatic immaturity contributes to the greater prevalence, severity, and duration of neonatal jaundice in late preterm infants. Pilot Kernicterus registry, a database of voluntarily reported cases of kernicterus (Bhutani et al, 2004, 2006). Moreover, the registry demonstrates that late preterm neonates show signs of bilirubin neurotoxicity at an earlier postnatal age than term newborns, indirectly suggesting a greater vulnerability to bilirubin-induced brain injury (Bhutani et al, 2006). Of the other clinical factors observed in conjunction with late preterm gestation hyperbilirubinemia risk, breast milk feeding has been identified most consistently, indeed almost uniformly, and therefore appears to be of paramount importance (Bhutani et al, 2004, 2006). Late preterm neonates, because of their immaturity, often demonstrate less effective sucking and swallowing and may have difficulties achieving consistent nutritive breastfeeding (Wang et al, 2004), phenomena that may predispose to varying degrees of lactation failure. Suboptimal feeding was the leading reason for discharge delay during birth hospitalization in late preterm neonates in one recent study (Wang et al, 2004). Pediatricians, therefore, need to be alert to the potential of suboptimal breast-milk feeding in late preterm neonates and not be misled by the seemingly satisfactory breastfeeding efforts of late preterm newborns during the birth hospitalization when limited colostrum volumes make it a challenge to adequately assess the effectiveness of breast-milk transfer (Neifert, 2001). Late preterm infants who are breastfed merit timely post birth-hospitalization discharge follow-up and lactation support (Bhutani et al, 2006; Watchko, 2006b). Lactation support coupled with regular neonatal weight checks is helpful in averting lactation difficulties and in the early identification of those mother-infant pairs prone to lactation failure. What does the association between exclusive breast milk feeding and kernicterus imply with respect to the etiopathogenesis of marked neonatal jaundice Numerous studies have reported an association between breastfeeding and an increased incidence and severity of hyperbilirubinemia, both during the first few days of life and in the genesis of prolonged neonatal jaundice (Hansen, 2001; Kivlahan et al, 1984; Linn et al, 1985; Maisels et al, 1986; Schneider, 1986). The latter studies suggest that many breastfed infants who develop marked neonatal jaundice do so in the context of a delay in lactation or varying degrees of lactation failure. Indeed, an appreciable percentage of the breastfed infants who develop kernicterus have been noted to have inadequate intake, and variable but substantial degrees of dehydration and weight loss (Bhutani et al, 2004; Johnson et al, 2002; Maisels et al, 1995). Inadequate breast milk intake, in addition to contributing to dehydration, can further enhance hyperbilirubinemia by increasing the enterohepatic circulation of bilirubin and resultant hepatic bilirubin load. The enterohepatic circulation of bilirubin is already exaggerated in the neonatal period, in part because the newborn intestinal tract is not yet colonized with bacteria that convert conjugated bilirubin to urobilinogen, and because intestinal -glucuronidase activity is high. Earlier studies in newborn humans and primates suggest that the enterohepatic circulation of bilirubin may account for up to 50% of the hepatic bilirubin load in neonates (Gartner et al, 1977; Poland et al, 1971). Moreover, fasting hyperbilirubinemia is largely due to intestinal reabsorption of unconjugated bilirubin, an additional mechanism by which inadequate lactation and/or poor enteral intake may contribute to marked hyperbilirubinemia in some newborns. In the context of limited hepatic conjugation capacity in the immediate postnatal period, any further increase in hepatic bilirubin load will likely result in more hyperbilirubinemia. Recent studies confirm that early breastfeeding jaundice is associated with a state of relative caloric deprivation (Bertini et al, 2001) and resultant enhanced enterohepatic circulation of bilirubin (Bertini et al, 2001; Maisels, 2000a). Breastfeedingassociated jaundice, however, is not associated with increased bilirubin production (Stevenson et al, 1980). Lactation failure is not uniformly present in affected infants, suggesting that other mechanism(s) may be operative in breastfeeding-associated jaundice, a finding that merits further clinical study. Breast-milk feeding may act as an environmental modifier for selected genotypes and thereby potentially predispose to the development of marked neonatal jaundice (Watchko, 2005, 2004). Although the relationship between breast-milk feeding and jaundice must be recognized, the benefits of breastmilk feeds far outweigh the related risk of hyperbilirubinemia. Cases of severe neonatal hyperbilirubinemia with suboptimal breast-milk feedings underscore the need for effective lactation support and timely follow-up exams. It is a noteworthy contributor to endemic rates of bilirubin encephalopathy in several developing countries. Sixty percent of this subgroup demonstrate bilirubin levels >95% (high risk zone) on the bilirubin nomogram of Bhutani et al (odds ratio 10. African Americans as a group have a lower incidence of neonatal hyperbilirubinemia: odds ratio 0. Consistent with this assertion, Kaplan and Hammerman, (2004a) have reported that 48. Although this association exists in approximately 15% of pregnancies, only a small fraction of such infants will develop significant hyperbilirubinemia. As contrasted with nonjaundiced newborns on the first postnatal day, newborns with overt jaundice in the first 24 postnatal hours are more likely to receive phototherapy (18. Hemolytic disease, immune mediated and otherwise, should be a diagnostic consideration in any infant with early clinical jaundice. Innate ethnic variation in hepatic bilirubin clearance (Ho, 1992) also contributes to the biologic basis of hyperbilirubinemia risk in Asian newborns as revealed by genetic analysis of enzymatic variants that modulate bilirubin metabolism. The high incidence of neonatal hyperbilirubinemia in East Asian populations appears to be at least partly attributable to the prevalence of these hepatic gene polymorphisms. Extravascular red cells have a markedly shortened life span, and their heme fraction is quickly catabolized to bilirubin by tissue macrophages that contain heme oxygenase and biliverdin reductase (Odell, 1980). Thus, cephalhematoma, subdural hemorrhage, massive adrenal hemorrhage, and marked bruising can be associated with increased serum bilirubin levels, typically manifest 48 to 72 hours after the extravasation of blood (Odell, 1980). This temporal pattern is consistent with the evolution of ecchymoses and bilirubin formation in situ and also accounts for why extravascular blood can cause prolonged indirect hyperbilirubinemia (Odell, 1980). An unusual but dramatic example of how extravascular blood can contribute to the genesis of hyperbilirubinemia is found in reports of marked jaundice associated with the delayed absorption of intraperitoneal blood in infants who received fetal intraperitoneal red cell transfusions (Rajagopalan et al, 1984; Wright et al, 1982). In one such case, 13 exchange transfusions were necessary to control the hyperbilirubinemia that resolved only when approximately 87 mL of packed red cells were evacuated from the intraperitoneal cavity (Wright et al, 1982). Although other causes of extravasation generally are not associated with such large amounts of sequestered blood and resultant bilirubin load, they can nevertheless contribute to the development of jaundice. However, an excess risk in siblings independent of other hyperbilirubinemia risk factors expected to recur in sibships (including breastfeeding, lower gestational age, and hemolytic disease) suggests that genetic rather than environmental effects are responsible (Gale et al, 1990; Khoury et al, 1988). Jaundice in neonates becomes evident first on the face and progresses in a cephalocaudal fashion with increasing hyperbilirubinemia as classically characterized by Kramer (1969). Acute bilirubin encephalopathy may develop during hazardous hyperbilirubinemia and evolve into the chronic adverse neurodevelopmental sequelae of kernicterus. Kernicterus is a devastating, disabling neurologic disorder classically characterized by the clinical tetrad of (1) choreoathetoid cerebral palsy, (2) high-frequency central neural hearing loss, (3) palsy of vertical gaze, and (4) dental enamel hypoplasia, the result of bilirubin-induced cell toxicity (Perlstein, 1960). Originally described in the context of severe hyperbilirubinemia secondary to Rh hemolytic disease (Evans and Polani, 1950; Vaughan et al, 1950), kernicterus has also been 80 70 60 Percent 50 40 30 20 10 0 reported in other hemolytic conditions. These factors have combined to unmask a previously underappreciated potential to develop extreme hyperbilirubinemia among a select number of neonates, the biological basis of which appears to be in part genetically determined. Recent population-based kernicterus incidence estimates for term neonates in developed countries range from approximately 1 per 30,000 (Sgro et al, 2006) to 1 per 100,000 (Manning et al, 2006); higher rates have been reported for (1) preterm newborns (Watchko, 1994) and (2) infants born in developing countries where kernicterus is a serious endemic problem. Stage 1 occurs during the first few days, with the infant having decreased activity, poor sucking, hypotonia, and a slightly high-pitched cry. Sometimes these changes are accompanied with seizure activity, backward arching of the neck (retrocollis) and trunk (opisthotonos), and fever. Stage 3 is evidenced by hypertonia with marked retrocollis and opisthotonos, stupor, coma, and a shrill cry. The preponderance of evidence in the medical literature suggests that once an infant demonstrates signs of opisthotonos, some damage to the central nervous system has occurred. Van Praagh (1961) reported that all infants with definite opisthotonos (20 of 20 infants in his review) proved to have kernicteric sequelae on follow-up, although he did not comment on the extent of the adverse neurodevelopmental findings. Jones et al (1954) reported that the presence of definite abnormal signs, such as opisthotonos, in the neonatal period was associated with the development of handicap(s) but was not necessarily predictive of the severity of that handicap(s) (although most infants experienced moderate to severe neurodevelopmental sequelae). In contrast to these earlier reports, Harris et al (2001) follow-up experience in six neonates with marked hyperbilirubinemia showed that transient neurologic abnormalities may not correlate with long-term prognosis. In their study, however, only two infants demonstrated opisthotonos; one recovered without sequelae (peak serum bilirubin 30. These findings illustrate the selective vulnerability and regional nature of kernicterus and concordancy of neuroimaging and neuropathology in this disorder. The concentration of this unbound bilirubin fraction is believed to dictate the biologic effects of bilirubin in jaundiced newborns, including its potential neurotoxicity. The full-term newborn infant has a significantly lower plasma albumin level than the adult and, correspondingly, fewer bilirubin binding sites.

Propecia 1mg cheap
Given that approximately 75% of families affected with hereditary spherocytosis manifest an autosomal-dominant phenotype hair loss cure dht purchase genuine propecia on line, a positive family history can often be elicited and provide further support for this diagnosis. The diagnosis of hereditary spherocytosis can be confirmed using the incubated osmotic fragility test, which is a reliable diagnostic tool in neonates after the first weeks of life when coupled with fetal red cell controls. Of these, the alpha-thalassemia syndromes are the most likely to be clinically apparent in newborns. Each human diploid cell contains four copies of the alphaglobin gene, and thus, four alpha-thalassemia syndromes have been described reflecting the presence of defects in 1, 2, 3, or 4 alpha-globin genes. Alphathalassemia trait is associated with two alpha-thalassemia mutations and in neonates is not associated with hemolysis. Alpha-thalassemia trait, however, is common in African American populations and can be detected by a low mean corpuscular volume of <95 m3 (normal infants 100 to 120 m3) (Schmaier et al, 1973). Hemoglobin H disease results from the presence of three thalassemia mutations and can cause hemolysis and anemia in neonates (Pearson, 1982). Homozygous alpha-thalassemia (total absence of alpha chain synthesis) results in profound hemolysis, anemia, hydrops fetalis, and almost always stillbirth or death in the immediate neonatal period. The pure beta thalassemias do not manifest themselves in the newborn period and the gamma thalassemias are (1) incompatible with life (homozygous form), (2) associated with transient mild to moderate neonatal anemia (if one or two genes are involved) that resolves when beta chain synthesis begins, or (3) in combination with impaired beta chain synthesis, associated with severe hemolytic anemia and marked hyperbilirubinemia (Oort et al, 1981). Such jaundice may be severe; in one historical series, a full third of affected infants required exchange transfusion to control their hyperbilirubinemia (Matthay et al, 1981), and kernicterus in the context of pyruvate kinase deficiency has been described (Oski et al, 1964). The diagnosis of pyruvate kinase deficiency is often difficult because the enzymatic abnormality is frequently not simply a quantitative defect, but in many cases involves abnormal enzyme kinetics or an unstable enzyme that decreases in activity as the red cell ages. Historically Rh incompatibility has been viewed as the most clinically important immune-mediated hemolytic disorder. The incidence of isoimmunization to the Rh D antigen, however, has declined since the introduction of Rho(D) immune globulin in 1968 and is now estimated at approximately 1 case per 1000 live births (Bowman, 2000; Chavez et al, 1991). Most instances of Rh isoimmunization are due to the Rh D antigen (Bowman, 2000; Gottvall et al, 1994). The severity of hemolysis varies in the context of Rh isoimmunization, but almost half of Rh-positive infants born to Rhsensitized mothers will have moderate or severe disease. Isoimmunization secondary to minor blood group antigens, such as Kell, Duffy, and Kidd, can also lead to significant hemolysis in utero and postnatal hyperbilirubinemia, although these antigens are far less potent in inducing antibodies than Rh D. The incidence of clinically significant sensitization to the minor blood group antigens as determined by metaanalysis approximates 1 in 330 pregnancies (Solola et al, 1983). Although this association exists in approximately 15% of pregnancies, only a fraction of infants born in this context will develop significant hyperbilirubinemia (Naiman, 1982; Ozolek et al, 1994). Defining which infants will become so affected is difficult to predict using laboratory screening tests. The latter may reflect a paucity of A and B antigens on newborn red cells and/or the absorption of serum antibody by A and B antigen epitopes throughout the body tissues and fluids (Naiman, 1982). Only a few affected infants develop hyperbilirubinemia to levels requiring exchange transfusion (Mollison, 1983). More current literature (Leistikow et al, 1995; Quinn et al, 1988; Ozolek et al, 1994), however, suggests that such routine screening is not warranted given the low yield and cost, consistent with the tenor of recommendations of the American Association of Blood Banks (Judd et al, 1990). At birth, blood supply to the newborn right liver lobe changes from the high oxygen content of the umbilical vein to the low oxygen content of the portal vein. Blood flow through the hepatic arteries develops only in the 1st week of extrauterine life, and the ductus venosus may remain partially patent for several days, allowing blood to bypass the liver. Crigler and Najjar first described a clinical syndrome of severe chronic nonhemolytic unconjugated hyperbilirubinemia in 1952 (Crigler et al, 1952). Although inherited in an autosomal recessive pattern, the type I syndrome has marked genetic heterogeneity (Clarke et al, 1997). Phototherapy is the mainstay of treatment for infants and children with Crigler-Najjar type 1 syndrome, although neonates may develop hazardous levels of hyperbilirubinemia necessitating exchange transfusion. Liver transplantation is the only current definitive therapeutic intervention for this disorder (Shevell et al, 1987). These rare but important clinical syndromes must be included in the differential diagnosis of prolonged marked indirect hyperbilirubinemia. Gilbert syndrome, originally described at the turn of the previous century (Gilbert et al, 1901), is far more common and characterized by mild, chronic, or recurrent unconjugated hyperbilirubinemia in the absence of liver disease or overt hemolysis (Gourley, 1994). Typically, the indirect hyperbilirubinemia associated with Gilbert syndrome is seen during fasting associated with an intercurrent illness. Interestingly, in about half of patients there is also an unexplained, shortened red cell life span and increased bilirubin production (Powell et al, 1967). Gilbert syndrome affects ~9% of the population and a genetic basis for this disorder has been defined (Bosma et al, 1995). Although Gilbert syndrome is most commonly diagnosed in young adulthood, investigators have long speculated that this disorder might contribute to indirect hyperbilirubinemia in the newborn period (Odell, 1980; Oski, 1984; Valaes, 1976). Taken together, these studies demonstrate that Gilbert syndrome is a significant contributing factor to neonatal jaundice. The role of Gilbert syndrome in the genesis of extreme hyperbilirubinemia remains unclear, although (1) the low direct bilirubin fractions and (2) evidence of poor feeding and prominent weight loss. The albumin level is inversely correlated with gestational age, so this lack of binding sites is more pronounced in preterm infants. Bilirubin-albumin binding may also be modified by clinical conditions and the presence of competing compounds. As a result, the framing of guidelines for the use of phototherapy and exchange transfusion in these infants is a capricious exercise at best and one for which no claim of an evidence base can be made (Maisels et al, 2003). These guidelines are provided by various experts, none of whom would likely make any claim for the greater validity of one approach versus another. The postnatal maturation of hepatic bilirubin uptake and bilirubin conjugation may also be slower in premature infants (Cashore, 2000). In addition, the delay in the initiation of enteral feedings that is so common in the clinical management of sick premature newborns may limit intestinal flow and bacterial colonization, resulting in a further enhancement of bilirubin enterohepatic circulation (Cashore, 2000). These developmental and clinical phenomena contribute to the greater degree and duration of neonatal jaundice in premature infants. Despite the near-universal finding of clinical jaundice in the very low-birthweight infant, kernicterus has virtually disappeared in postmortem series of premature neonates (Jardine, 1989; Perlman, 1978; Watchko, 1994), and postkernicteric bilirubin encephalopathy and central neural hearing loss related to neonatal hyperbilirubinemia have not emerged as important clinical sequelae in neurodevelopmental follow-up of premature infants (Cashore, 2000). Direct reacting or conjugated bilirubin levels should not be subtracted from the total. Used at these levels and in therapeutic doses, phototherapy should, with few exceptions, eliminate the need for exchange transfusions. Table 79-6 outlines the aggressive and conservative phototherapy treatment guidelines and exchange transfusion thresholds used in the Network study. Their data suggest that aggressive phototherapy may be preferred for infants of 751 to 1000 g birthweight because of significant neurodevelopmental benefit including a reduction in athetosis and severe hearing loss (Morris et al, 2008). However, their findings also raised concerns for aggressive phototherapy use in infants with birthweight of 501 to 750 g because of a higher mortality rate in that subgroup-that is, increased mortality may offset any potential neurologic benefits of aggressive treatment in these smallest of infants (Morris et al, 2008). Although it is unclear why phototherapy might increase mortality in this birthweight cohort, speculation focuses on greater light penetration deep into subcutaneous tissues via thin gelatinous skin and possible oxidative injury to cell membranes (Maisels, 2009; Vreman et al, 2004). Few neonates required exchange transfusion, confirming again the broad efficacy of phototherapy in preterm neonates. However, additional clinical study is needed to further clarify the hyperbilirubinemia risk of premature neonates and frame guidelines for phototherapy and exchange transfusion in preterm infants that are evidence based (Maisels et al, 2003). Support of successful breastfeeding is also an important part of hyperbilirubinemia control. Coupling the gestational age with knowledge of hyperbilirubinemia risk factors will determine which portion of the algorithm is operative for a given neonate. Phototherapy was first introduced at the Rochford (Essex) General Hospital by Cremer et al (1958) and has proven to be exceedingly successful. Certainly phototherapy, if used appropriately (Maisels, 1996), is capable of controlling the bilirubin levels in almost all low-birthweight infants, with the possible exception of the occasional infant with severe erythroblastosis fetalis or marked bruising. In a similar fashion, phototherapy has proven effective in controlling bilirubin levels and preventing the need for exchange transfusion in most term and late-preterm neonates as well- exceptions on occasion being infants with severe hemolysis. If discharging 72 hr, time follow-up according to age at discharge or concerns other than jaundice. Infants are designated as "higher risk" because of the potential negative effects of the conditions listed on albumin binding of bilirubin, the blood-brain barrier, and the susceptibility of the brain cells to damage by bilirubin.