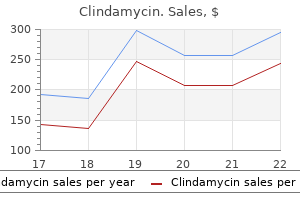
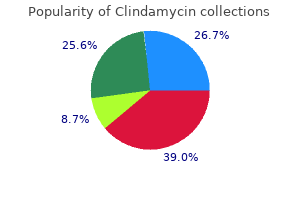
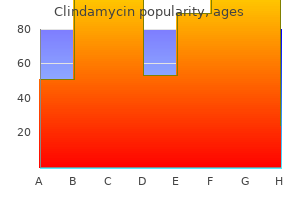
Buy discount clindamycin 300 mg line
Undifferentiated carcinomas containing a distinct population of malignant glands resulting in a biphasic appearance are sometimes designated "carcinosarcomas antibiotic drops for swimmer's ear trusted 150mg clindamycin," especially when the spindle cell components display heterologous stromal differentiation. The epithelial nature of the pleomorphic or spindle cells is confirmed by positive immunostaining for cytokeratin. Undifferentiated Carcinoma with Osteoclast-like Giant Cells Undifferentiated carcinoma with osteoclast-like giant cells of the pancreas (synonyms: giant cell tumor of the osteoclastic type, osteoclastic giant cell carcinoma) is characterized by a dual population of noncohesive mononuclear epithelioid cells and osteoclast-like giant cells. The mononuclear cell component includes both mononuclear histiocytes and the neoplastic cell component, which consists of more atypical, sometimes pleomorphic cells with irregular nuclei and high mitotic activity. Some cases also exhibit separate components of ductal adenocarcinoma or other patterns of undifferentiated carcinoma. Positive immunostaining of the mononuclear neoplastic cells for keratin, although often not present, also indicates epithelial origin. In the latter situation, the neuroendocrine cells remain clustered, although the insular architecture may be disrupted, and an intimate relationship exists between these cells and the neoplastic glands, falsely suggesting that the neuroendocrine elements are part of the neoplastic population. On the other hand, carcinomas composed of significant components of ductal and neuroendocrine cells are rare. By definition, these mixed ductal-neuroendocrine carcinomas contain at least 30% of both elements. It is important to distinguish well-differentiated pancreatic neuroendocrine tumors with glandular differentiation from mixed ductal-neuroendocrine carcinomas; the former entity may show very well-developed lumen formation, but the cells lining the lumina are identical to the welldifferentiated neuroendocrine cells comprising the rest of the neoplasm. The differential diagnosis includes metastases from diffuse-type gastric adenocarcinoma or lobular carcinoma of the breast. The prognosis of signet ring cell carcinoma is at least as poor as that of conventional ductal adenocarcinoma. Medullary Carcinoma Medullary carcinoma is a rare variant of ductal adenocarcinoma that, like its counterpart in the colorectum, shows morphologic features that include a highly cellular, syncytial growth pattern, peripheral circumscription, high mitotic rates, and occasionally tumor-infiltrating lymphocytes. Unlike medullary colorectal carcinoma, medullary carcinoma of the pancreas is only occasionally associated with mutations of the mismatch repair genes50 and is not associated with a significantly better prognosis than ductal adenocarcinoma. So far, only one case has been reported to be a manifestation of the hereditary nonpolyposis colorectal cancer syndrome. As yet, no convincing evidence has been presented to support the existence of benign pancreatic oncocytomas. In addition to such purely oncocytic malignant tumors, focal oncocytic changes may be encountered in otherwise conventional well-differentiated neuroendocrine tumors and has also been observed in solid pseudopapillary neoplasms. Hepatoid Carcinoma this extremely rare variant consists of nests of large epithelioid cells with abundant eosinophilic cytoplasm and central round nuclei containing prominent nucleoli, resembling a primary hepatocellular carcinoma. Clear cell carcinoma of the pancreas must be distinguished from metastatic renal cell carcinoma or adrenal cortical carcinoma. The first three types usually originate from the main duct, whereas the gastric type typically occurs in the secondary, or branch, ducts. It usually occurs in the pancreatic head but may also involve the entire main duct, including the ampulla of Vater. The tumor frequently secretes copious quantities of mucin that lead to massive dilatation of the ducts, resulting in a cystic appearance radiographically and grossly. The resection specimen shows a markedly dilated main pancreatic duct, filled with sticky mucin. Some regions reveal more significant cystic change, with red, soft tumor nodules filling the duct. The invasive carcinoma is composed of stromal mucin pools containing floating neoplastic epithelium. It shows the same complex papillae as the pancreatobiliary type, but the lining cells have deeply eosinophilic cytoplasm and may form cribriform structures. Histologically, it exhibits small papillary projections lined by epithelial cells resembling gastric foveolar cells. Similar, if not identical, changes have been described in pancreata from otherwise healthy subjects and in those removed from patients with a strong family history of pancreatic cancer (see earlier discussion). About 50% have their origin in the head of the pancreas, and 30% involve the entire gland. The invasive tubular carcinoma is usually limited in extent and can be difficult to distinguish from the intraductal components. More than a third of the patients survive beyond 5 years, and a protracted clinical course may be seen even in those patients with recurrence and metastasis to lymph nodes or to the liver. They occur almost exclusively (>95%) in women, usually in the fourth to fifth decades, and are found, in more than 90%, in the tail or body of the pancreas (see Table 11-8). Rare cases have been recorded of mucinous cystic tumors associated with gastrin secretion and Zollinger-Ellison syndrome, presumably because of their content of gastrin-producing neuroendocrine cells. The individual cyst locules are relatively large (in comparison with serous microcystic adenomas; see later discussion), each measuring 1 to 10 cm in most cases. The inner surfaces are smooth or show papillary projections or mural nodules, particularly in those with high-grade dysplasia or invasive carcinoma. Intermediategrade dysplasia is characterized by papillary infolding, cellular pseudostratification, nuclear irregularity, and crowding. Rarely the cyst wall contains pseudosarcomatous or frankly sarcomatous areas,87,88 the latter likely representing a sarcomatoid undifferentiated carcinoma that has lost epithelial differentiation. They are usually benign and commonly present with the symptoms and signs of an expansile abdominal mass, or they are detected incidentally on imaging studies. The patients (in whom women slightly predominate) present at a mean age of 70 years (range 26-91 years) (see Table 11-8). Luteinized cells are present, arranged as large nests of eosinophilic, epithelioid cells (A). The cysts are lined by one cell layer and only occasionally form small micropapillae. Occasionally subtotal macrocystic degeneration is seen, which can simulate the appearance of a pseudocyst. In advanced stages of the disease, these cystic tumors may merge and involve the entire pancreas. They occur predominantly in the head of the pancreas, where they occasionally compress the common bile duct. The place of the solid serous adenoma, a noncystic variant of serous cystic neoplasm,3,93 and serous cystadenocarcinoma91 in the spectrum of serous cystic neoplasms is not yet clear, mainly because of the small number of cases that have been reported so far. In the solid variant, these well-circumscribed tumors are usually smaller than serous cystic neoplasms, measuring between 2 and 4 cm. Serous cystadenocarcinoma is an extremely rare malignant tumor; it resembles serous cystadenoma grossly and microscopically but shows invasion into adjacent structures and vessels and/or metastases. The macrocysticoligocystic variant is more difficult to differentiate from other cystic lesions because of its variegated gross appearance. It occurs mostly in adults in the sixth to eighth decades and predominantly in men, although rare cases have been described in children and adolescents. Patients with acinar cell carcinoma generally are seen initially with nonspecific symptoms due to the effects of the mass; jaundice is unusual. An association with multifocal fat necrosis in the subcutis, bone marrow, and abdomen and polyarthralgia due to massive secretion of lipase has been described in individual patients, usually in the presence of significant hepatic metastases. The best differentiated cells are round and monomorphic and medium to large in size. The less well-differentiated cells are smaller, have less characteristic nuclei, and lack the eosinophilic granularity of the cytoplasm. Polarization of the cells in the solid areas may be found at the interface with the stroma, resulting in basal nuclear palisading in these regions. Acinar cell carcinoma shows positive immunostaining for trypsin, chymotrypsin, and lipase. Scattered neuroendocrine cells positive for chromogranin and synaptophysin may be found in 30% to 40% of cases. In most cases, these mixed carcinomas consist largely of the acinar component, and the available clinical data suggest that they behave similarly to pure acinar cell carcinomas. Acinar cell cystadenocarcinoma represents the rare cystic variant of acinar cell carcinoma. Acinar cell cystadenocarcinomas are just as aggressive as solid acinar cell carcinomas. The differential diagnosis of acinar cell carcinoma is primarily versus pancreatic neuroendocrine tumors, which they can mimic histologically. Acinar cell adenoma has not been recorded convincingly, but acinar cell nodules ("focal acinar cell dysplasia") are commonly identified in surgical specimens and autopsies.
Buy clindamycin 300 mg
The distinction of primary sarcoma from sarcomatoid carcinoma lies in the absence of epithelial components (after extensive sampling) and usually the absence of a history of adenocarcinoma bacteria questions and answers purchase clindamycin 300mg free shipping. Postoperative spindle cell nodule, phyllodes tumor, and pseudosarcomatous fibromyxoid tumor should also be considered in the differential diagnosis. A biphasic tumor with carcinomatous and spindle sarcomatoid components; the latter is usually of a malignant fibrous histiocytoma-like pattern, but is often of an unclassified myxoid pattern, as seen in this example. B, Immunostaining for keratin is positive in both the carcinomatous and sarcomatoid components. It is conceivable that core biopsies targeted at or near the transition zone will have a chance to sample lesions of benign small acinar proliferations of the transition zone. They suggested that stromal changes may be associated with an aggressive behavior of these tumors. The authors evaluated reactive stromal changes in prostate carcinomas in needle biopsy samples and graded them as grade 0 to grade 3; grade 0, with 0% to 5% reactive stroma; grade 1, 6% to 15%; grade 2, 16% to 50%; grade 3, 51% to 100% (at least a 1: 1 ratio between glands and stroma). Of 224 cases of prostate cancer, reactive stromal grading distribution was as follows: reactive stromal grading 0, 1 case (0. Reactive stromal grading in biopsies was correlated with adverse clinicopathologic parameters in the prostatectomy. Patients with reactive stromal grading 1 and 2 had better survival than those with 0 and 3 (P = 0. Reactive stromal grading was an independent predictor of recurrence (hazard ratio = 1. Reactive stromal grading is independent of Gleason 4 + 3 and 3 + 4 in patients with a Gleason score of 7. Therefore the authors concluded that quantitation of reactive stroma and recognition of the stromogenic carcinoma in H&Estained biopsies is useful to predict biochemical recurrence in patients with prostate carcinoma. Although McNeal and collegues24 referred to this lesion as a possibly premalignant lesion, to date convincing evidence for this association is lacking. Solid proliferation of basal cells with peripheral palisading that superficially resembles basal cell carcinoma of the skin is seen. It is characterized by multiple foci of small, nonlobular, crowded, but relatively bland acini on needle biopsy or in prostatectomy specimens at the peripheral zone. Their results suggested that it is a mimicker of adenocarcinoma and should be considered a risk factor for adenocarcinoma and that patients with this finding should be followed closely with repeat biopsy. Left, A well-demarcated nodule contains small glands with minimal intervening stroma; this pattern superficially resembles Gleason 1 or 2 patterns of prostate cancer, but the glands of adenosis retain the basal cell layer (right, 34E12). The basal cells have scanty cytoplasm and oval to short-spindled hyperchromatic nuclei. The margin of the nodule is not encapsulated but is relatively well demarcated in most cases. It has been reported to be associated with sclerosing adenosis397 and clear cell cribriform hyperplasia,398 which are two other benign hyperplastic lesions of the prostate. The cells of squamous metaplasia have abundant eosinophilic cytoplasm and distinct cell borders. In a prostate biopsy, the most helpful features for its diagnosis include solid nests, pseudocribriform glands, multilayering of cells, calcifications, and cellular stroma. The chromatin is finely dispersed, and the nucleus contains occasional small nucleoli. The nests of adenoid basal cell tumor reveal areas of luminal differentiation with an occasional cribriform arrangement. Adenoid basal cell tumor is considered a locally aggressive lesion, but some lesions merge, in histology, with adenoid cystic and basaloid carcinoma. Transitional cell metaplasia is usually seen in the periurethral areas of the prostate. The cells of transitional cell metaplasia are larger and have more cytoplasm than those of basal cell hyperplasia. Solid nests and nests with single or multiple lumina are present in a cellular stroma. The second group of cases (adenoid cystic carcinoma and basaloid carcinoma) show a widespread, haphazard infiltrative growth pattern. Adenoid cystic carcinomas are biologically indolent after prostatectomy but have a low risk of distant metastasis. A lesion that may share similar features of basal cell proliferative lesion, called cylindroma of the prostate, has been reported and is characterized by a jigsaw-puzzle arrangement and heavy accumulation of basement membrane material around and within individual tumor islands,420 which is very uncommon in basaloid proliferations of the prostate. A cribriform pattern of adenoid cystic carcinoma with perineural invasion is seen. However, one study of 19 patients found extraprostatic extension (26%), perineural invasion (26%). Ali and Epstein418 reported 29 cases of basal cell carcinoma of the prostate, including what others call adenoid cell carcinoma of the prostate. Based on these findings, they concluded that basal cell carcinomas are rare tumors that predominantly have an indolent course; however, a small subset behaves aggressively, with local recurrences and distant metastases. The most common morphology among those with an aggressive behavior are tumors with large solid nests, central necrosis, high Ki-67 index, and weak and less staining with basal cell markers. Most florid basaloid proliferations of the prostate fall into one of two categories. The clear cells range in shape from cuboidal to tall and columnar, and nucleoli are absent or inconspicuous. The proliferating cells are round, cuboidal to tall columnar, with a varying but usually abundant amount of cytoplasm that is most often clear. They have uniform, small, round to oval nuclei, which are usually the same size as the nuclei of epithelial cells in adjacent hyperplastic acini. The nuclei at the periphery are slightly larger than those at the center of the proliferation, suggesting cellular maturation toward the center. Cribriform adenocarcinoma, on the other hand, is characterized by a diffuse growth pattern, nucleomegaly, prominent nucleoli, and occasional necrosis. Hulman425 reported a similar lesion of the prostate and compared it with typical adenomatoid tumors using histochemical and immunohistochemical methods; he concluded that the lesion was of prostatic origin and proposed the term pseudoadenomatoid tumor. The term sclerosing adenosis was coined by Young and Clement427 on the basis of the histologic resemblance to that of the breast. Sclerosing adenosis is a rare lesion characterized by proliferation of variably sized, but usually small glands in a cellular stroma. It is of both practical and academic importance to recognize sclerosing adenosis, because of its remarkable resemblance to adenocarcinoma on histologic examination and its myoepithelial differentiation96,97,415,427 Normal prostatic basal cells show no myoepithelial differentiation, as has been demonstrated by Srigley. On microscopic examination, sclerosing adenosis is characterized by an ill-defined nodule containing irregular, small acini and nests or clusters of cells embedded in a cellular stroma. The basal cells are for the most part obscured or compressed, but are present in all cases, at least in some glands. The luminal cells are larger and have clear to eosinophilic cytoplasm and basally located nuclei. The basally located cells tend to be flat to cuboidal, and their nuclei are oriented parallel to the basement membrane. In addition, a distinct population of cells reactive for muscle-specific actin and S-100 protein is identified within the glandular element and the stroma, suggesting myoepithelial differentiation. Unlike acinar adenocarcinoma, sclerosing adenosis is characterized by a proliferation of both glandular and stromal elements. The small, closely packed acini with an infiltrative pattern in sclerosing adenosis may be confused with neoplastic glands, and the proliferating stroma may be misinterpreted as a desmoplastic reaction. Sclerosing adenosis is a lobular proliferation at low power in which the acini typically show variation in size and shape, and at least some of the glands have a clearly visible double cell layer. In contrast to sclerosing adenosis, small acinar adenocarcinoma more often tends to infiltrate into the surrounding prostatic stroma. The stroma in sclerosing adenosis is hypercellular and composed of plump spindle cells, whereas infiltrating adenocarcinoma often does not elicit a response or induces a hyalinized, hypocellular desmoplastic response.
Order clindamycin 150 mg without prescription
A antimicrobial fibers 300mg clindamycin with amex, this thinly encapsulated cellular tumor shows a morphologically different, expansile nodule in the left field. B, the right field shows the preexisting adenoma, with the follicles lined by cells with uniform dark round nuclei. The left field shows the sharply delimited supervening papillary carcinoma, with larger, paler, crowded, and grooved nuclei. Sometimes, areas of an encapsulated neoplasm appear to be diagnostic of papillary carcinoma (follicular variant), whereas other areas exhibit dark round nuclei. Two explanations are possible for this observation: (1) the entire tumor being a papillary carcinoma, just that the nuclear features are not well developed in some foci; (2) papillary carcinoma arising in a follicular adenoma; this has to be considered especially if the typical papillary carcinoma component forms an expansile mass within the tumor or shows an abrupt transition with the follicles that constitute the main tumor. The Diagnostic Approach for Encapsulated Follicular Variant of Papillary Carcinoma versus Follicular Carcinoma Some follicular-patterned tumors are obviously malignant as evidenced by capsular and/or vascular invasion. The main differential diagnoses are follicular carcinoma and encapsulated follicular variant of papillary carcinoma. The problem is less acute than the previous scenario, because at the minimum the diagnosis is a carcinoma. Like the previous scenario, a diagnosis of encapsulated follicular variant of papillary carcinoma should be made only when nuclear features of papillary carcinoma are well developed (see Table 18A-13). The presence of scattered large hyperchromatic nuclei is a feature more commonly observed in follicular carcinoma than in papillary carcinoma. Alternative Terminology An important impetus for overdiagnosis of encapsulated follicular variant of papillary carcinoma is the litigation climate, whereby the pathologist renders this diagnosis using lax criteria to avoid being sued for missing a malignancy. To address the issue of follicular-patterned tumors exhibiting borderline nuclear features, the Chernobyl Pathologists Group has proposed nomenclature to avoid overdiagnosis of papillary carcinoma. Gradual transition into normal-looking nuclei in the surrounding follicles strongly favors a benign process over papillary carcinoma. On the other hand, abrupt change in nuclear morphology of the abnormal focus (usually with absolute nuclear enlargement) compared with the surrounding benign thyroid follicles favors a diagnosis of papillary carcinoma, of course provided that the pale nuclei should at least be crowded and some nuclear grooves should be seen. If the nuclear features are convincing, a diagnosis of papillary carcinoma can be made even if the lesion consists of one single follicle; that is, no minimum size requirement exists for rendering this diagnosis. This is an encapsulated follicular-patterned tumor with no evidence of capsular or vascular invasion. The nuclei exhibit some nuclear features of papillary carcinoma, such as pallor and mild loss of polarity. Such tumors with equivocal nuclear features of papillary carcinoma are designated as "well-differentiated tumor of uncertain malignant potential" according to the Chernobyl Pathologists Group proposal. Multiple Cellular Follicular-Patterned Nodules: Widely Invasive Carcinoma or Multinodular Goiter Multinodular goiter Widely invasive follicular carcinoma Dyshormonogenetic goiter Nodular Hashimoto thyroiditis Papillary carcinoma, follicular variant Collections of Follicles with Pale or Clear Nuclei: Minimum Diagnostic Criteria for Papillary Carcinoma the Problem Clear nuclei are not uncommonly encountered focally, or sometimes extensively, as a nonspecific feature in a wide variety of benign and malignant thyroid lesions, and therefore rendering a diagnosis of papillary carcinoma based merely on pale or clear nuclei is not justified. In addition, for unknown reasons, the nuclei of any type of thyroid lesion can appear pale and "bubbly," characterized by multiple, empty-looking intranuclear "holes" that are devoid of chromatin granules in the rim. The diagnosis should be follicular variant of papillary carcinoma if the typical nuclear features are present. Otherwise, the main distinction is between widely invasive follicular carcinoma and multiple cellular adenomatoid nodules. A, There is a focus comprising follicles with clear nuclei, raising the suspicion of papillary carcinoma. B, the gradual transition of the abnormal follicles (left field) into the normal follicles (right field) favors a benign process. A, Two nodules are evident in this field: the one on the right is predominated by colloid-distended large follicles, whereas the one on the left shows small follicles. B, the nodules in nodular goiter can show high cellularity because of predominance of small follicles (hyperplastic nodules). Nodular Goiter Nodular goiter is the most common thyroid lesion encountered in surgical pathology practice. Although the nodule may appear solitary clinically, other nodules are often present in the background on ultrasound or pathologic examination. Nodular goiter most commonly is composed of variable-sized large follicles distended with colloid (colloid nodule). Some broad protuberances or macropapillae with daughter follicles in the cores commonly are seen. The cells that line the macropapillae are cuboidal to columnar and possess regular dark round nuclei aligned at the base of the cells. Secondary changes such as fibrosis, hemorrhage, and cystic degeneration are common. Some nodules can be highly cellular (adenomatoid nodule), being formed by small follicles or trabeculae lined by nondescript cells or oncocytic cells, mimicking follicular neoplasm or follicular variant of papillary carcinoma. The thyroid is asymmetrically enlarged and multinodular and can weigh up to 600 g. The background thyroid shows small follicles often devoid of colloid, lined by cells with scattered large hyperchromatic nuclei. The nodules often exhibit high cellularity, with mixed microfollicular, trabecular, and solid growth patterns, and variable nuclear atypia (but usually lacking the pleomorphic nuclei seen in the background). The former can be distinguished from the latter by the architectural features: (1) wavy rather than straight trabeculae; (2) prominent hyalinization associated with the trabeculae, often with formation of lumpy eosinophilic deposits; and (3) yellow bodies in the cytoplasm. B, the internodular follicles are often small and not uncommonly devoid of colloid material. Medullary carcinoma can be recognized by the prominent fibrovascular septa, frequent presence of amyloid, and granular chromatin. Poorly differentiated thyroid carcinoma is distinguishable from follicular carcinoma by the presence of necrosis, mitotic activity, or convoluted nuclei. Features favoring a diagnosis of parathyroid carcinoma are discussed under intrathyroidal parathyroid tumor. Invasion of the thyroid follicular epithelium and plugging of follicle lumens by tumor cells is a feature frequently seen in malignant lymphoma, whereas obliteration of the walls and lumens of blood vessels is a feature highly characteristic of undifferentiated thyroid carcinoma. Traversing fibrovascular septa, cellular dehiscence, and amyloid (if present) are features that should point to the diagnosis of medullary carcinoma. Thyroid Tumors and Tumor-like Lesions with Spindle Cells Main Differential Diagnoses Medullary carcinoma Adenomatoid nodule with spindle cell metaplasia Follicular neoplasm with spindle cell metaplasia Papillary carcinoma a. Various benign and malignant mesenchymal tumors Approach to Diagnosis A number of epithelial tumors and tumor-like lesions of the thyroid can have a significant spindle cell component. The diagnosis can usually be reached because some other areas of the lesion often exhibit typical histologic features of the entity. Approach to Diagnosis In a solid-growing invasive tumor of the thyroid, it is most important not to mistake the indolent tumors. Poorly differentiated thyroid carcinoma is distinguishable from follicular or papillary carcinoma on one hand by the presence of 18 Tumors of the Thyroid and Parathyroid Glands 1249 cribriform-morular variant of papillary carcinoma, are relatively minor and are found among the characteristic cribriform structures lacking luminal colloid material. The spindle cells are frankly pleomorphic in undifferentiated carcinoma and sarcoma, and thus the diagnosis should be obvious. When prominent delicate fibrovascular septa are seen, medullary carcinoma should be a serious consideration. A mesenchymal proliferation with features of nodular fasciitis or fibromatosis should prompt a careful search for an underlying papillary carcinoma. Spindle cell metaplasia in papillary carcinoma, follicular adenoma or carcinoma, or adenomatoid nodule can pose difficulties in diagnosis. The spindle cells, which are in fascicles, are bland-looking and intermingled with neoplastic follicles or papillae in at least some foci.
Discount clindamycin online
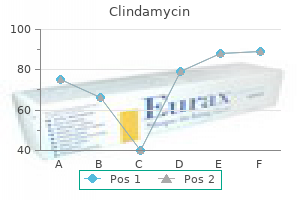
Molecular diagnosis is particularly important in these diseases antibiotics for uti safe for breastfeeding buy cheapest clindamycin, because specific therapies targeting these tyrosine kinases exist or are being developed. Once a diagnosis is established, bone marrow examination is most frequently performed to evaluate efficacy of treatment, to screen for the presence of blast transformation and marrow fibrosis, or to obtain material to monitor minimal residual disease. The disease is today discovered incidentally on peripheral blood examination in an asymptomatic patient in approximately 20% to 40% of cases. In addition, blast crisis may present at extramedullary sites, including lymph nodes, spleen, skin, and elsewhere. The constitutive kinase activity of this fusion gene is now believed to be the principal cause of the chronic phase of clinical disease. Although it is clear that the neoplastic clone is a progenitor for cells of the granulocytic, monocytic, erythroid, megakaryocytic, and lymphoid lineages, the disease is characterized initially by a proliferation of maturing granulocytes and platelets. Unless treated, this chronic disease phase is inevitably followed (usually in 3-5 years) by evolution to more aggressive disease stages, termed the accelerated and blast phases (transformation to acute myeloid or lymphoid leukemia). Thrombocytosis is seen in the majority of cases, and anemia is typically present, with 45% to 60% of patients having hemoglobin levels less than 12. The cellularity is dominated by mature granulocytic forms (neutrophils, eosinophils, and basophils) and megakaryocytes, but a corresponding increase in granulocytic precursors (myelocytes, metamyelocytes, and promyelocytes) is also present. These early forms tend to accumulate in concentric layers 3 to 5 cells thick near the bony trabeculae in a manner analogous to normal granulocytic differentiation. Blast forms are not increased, and patches of blasts or marked thickening of the immature, paratrabecular cell layers should raise the suspicion of progressive disease. Basophils are not readily discernible in core biopsy specimens, because of loss of granules during processing, and are best appreciated in aspirate smear preparations. Erythroid numbers are decreased, with the myeloid to erythroid ratio typically greater than 10: 1. Both myeloid and erythroid differentiation are orderly and without prominent dysplasia. Immunophenotypic analysis of this case revealed a mixed lymphoid and myeloid phenotype. Clusters of tightly apposed megakaryocytes are frequent, a finding that is not commonly seen in the marrows of patients with reactive secondary megakaryocytic hyperplasias. Sea-blue histiocytes (pseudo-Gaucher cells) are present in most cases, secondary to phagocytosis of the excess membrane lipids that result from increased cellular turnover. The spleen shows expansion of the red pulp cords by granulocytic precursors, of which neutrophilic myelocytes are usually the most numerous. The white pulp is correspondingly depleted, and extramedullary hematopoiesis is also noted within the sinuses. Reticulin fibrosis of the splenic cords is also seen, and the combination of a burgeoning hematopoietic mass and compromised blood flow often produces infarcts. Imatinib mesylate (Gleevec) treatment results in bone marrow changes that include reductions in cellularity, myeloid to erythroid ratio (commonly with relative erythroid hyperplasia), and reticulin fibrosis. Chronic Myelogenous Leukemia: Accelerated Phase In addition to the peripheral blood features mentioned earlier, disease progression to accelerated phase will often include increased numbers of blast forms or promyelocytes (particularly in the paratrabecular or parasinusoidal regions). Large sheets of megakaryocytes, accompanied by reticulin or collagen fibrosis or granulocytic dysplasia, are also frequently associated with progression to the accelerated phase. The capacity to evolve to either myeloid or lymphoid leukemia is strong support for the presence of a Philadelphia (Ph)-positive transformed pluripotent stem cell. Blast transformation often occurs in a patchy fashion in the marrow or even at extramedullary sites. The abnormal chromosome 22, which contains the functional fusion gene and has lost a significant part of its long arm to chromosome 9, is designated the Ph chromosome. The features are nearly indistinguishable from chronic-phase chronic myelogenous leukemia. Other forms of chronic myeloid proliferations must also be excluded based on the absence of their clinical, pathologic, and molecular genetic features. Note the sheets of both mature and immature eosinophilic forms containing prominent eosinophilic granules and the absence of neutrophilic forms. The most common presenting signs and symptoms (in decreasing order of frequency) are weakness and fatigue, cough, dyspnea, myalgias, angioedema, fever or rash, and rhinitis. Several eosinophilic myelocytes with large, orange cytoplasmic granules and typical myeloblasts (center) are present. In many cases, the chronic course of the disease and organ infiltration by eosinophils leads to long-term exposure of tissues to the contents of eosinophilic granules, which eventuates in multisystem tissue damage. In addition, one must exclude known causes of secondary eosinophilia, such as reactive causes, and neoplastic disorders with associated eosinophilia, including other clonal myeloid disorders. It is the increase in red cell mass that is the clinical hallmark of this disease-an expansion that is independent of the normal pathways that regulate erythropoiesis and not related to other identifiable causes of secondary erythrocytosis. Following the prodromal or prepolycythemic phase, which is characterized by borderline to mild erythrocytosis, patients enter an overtly polycythemic phase that often culminates in a postpolycythemic myelofibrotic phase that is difficult to distinguish from other causes of myelofibrosis. In addition, neutrophilia, including early neutrophilic precursors, mild basophilia, and mild anemia with nucleated red blood cells, can be seen. Morphologic changes in mature eosinophils include increased size, cytoplasmic vacuolization or clearing, and alterations in nuclear lobation. Erythropoiesis and megakaryopoiesis are usually normal, but sometimes decreased numbers of megakaryocytes are seen. Dysplastic features can be noted in cells of other lineages, and myelofibrosis is also observed in some cases. Clinical and Laboratory Findings the incidence of polycythemia vera has been reported to range from 0. Many of these entities have specific effective treatment options that can be administered only if the diseases are properly recognized by the diagnosing pathologist. As mentioned earlier, this includes some forms of myeloid neoplasia that are stem cell disorders that involve all myeloid lineages but show prominent increases in the eosinophilic lineage. Bone marrow biopsy sample showing hypercelluarlity for age and panmyelosis with prominent erythroid, granulocytic, and megakaryocytic proliferation 2. Endogenous erythroid colony formation in vitro Diagnosis requires the presence of both major criteria and one minor criteria, or the presence of the first major criteria together with two minor criteria. Peripheral Blood, Bone Marrow, and Aspirate Smear Findings Initial evaluation of the peripheral blood during the so-called polycythemic or early phase of polycythemia vera reveals an increased red cell mass and corresponding increases in red blood cell count, hemoglobin, and hematocrit. Histologic examination of the bone marrow reveals hypercellularity resulting from increases in all lineages (granulocytic, erythroid, and megakaryocytic). Associated marrow findings include a variably cellular, often hypocellular, marrow with marked reticulin or even collagen fibrosis, decreased erythropoiesis and granulopoiesis, persistence of megakaryocytes that often show dysplastic nuclear features, and, occasionally, osteosclerotic bone. Early in the disease, the spleen shows marked congestion of the red pulp with inconspicuous white pulp. Extramedullary hematopoiesis (myeloid metaplasia) is prominent only in late disease associated with myelofibrosis. Bone marrow biopsy specimen showing proliferation mainly of the megakaryocytic lineage with increased numbers of enlarged, mature megakaryocytes. No significant increase or left shift of neutrophil granulopoiesis or erthropoiesis. Requires the absence of reticulin or collagen fibrosis, peripheral leukoerythroblastosis, or markedly hypercellular marrow accompanied by megakaryocyte morphology typical of primary myelofibrosis 3. Like polycythemia vera, its clinical course is significantly complicated by a thrombohemorrhagic diathesis. Given the large number of secondary causes of thrombocytosis and the presence of thrombocytosis in other chronic myeloprofilerative disorders, accurate diagnosis of this entity is often very difficult. The median age at 1652 22 Tumors of the Hematopoietic System diagnosis ranges between 60 and 70 years old, but essential thrombocythemia can occur in children. Life-threatening complications include cerebral infarction or hepatic vein thrombosis, as in the BuddChiari syndrome. When bleeding occurs, most commonly from mucosal sites such as the gastrointestinal tract, it can result in profound iron-deficiency anemia. Severe bleeding is rare and usually occurs in patients with the highest platelet counts or those taking antiplatelet drugs.
Cheap clindamycin online master card
The benign features of the epithelium in endometriosis and endocervicosis are also helpful in the distinction from adenocarcinoma antimicrobial kitchen towels buy cheap clindamycin 150mg online. Endocervicosis may cause particular difficulty because it often forms a mass and lacks endometrial stroma and the epithelium is mucinous. As the glands of endocervicosis often are distributed haphazardly in the muscularis propria of the bladder, lack of familiarity with this entity may suggest the possibility of a deeply invasive, well-differentiated mucinous adenocarcinoma. Primary adenocarcinoma must be distinguished from spread of another adenocarcinoma to the bladder. The most common problem of this type is posed by invasion of the bladder by prostatic adenocarcinoma. In most cases, examination of routinely stained sections shows the characteristic small acinar or cribriform appearance of prostatic adenocarcinoma, which differs from that of most adenocarcinomas of the bladder. Even when a prostatic carcinoma has unusual histologic features, it typically stains positively for at least one of these antigens. In this benign lesion glands are often haphazardly disposed in the muscularis propria, raising the concern of carcinoma. An example of a locally advanced case of ductal adenocarcinoma of the prostate directly invading the bladder trigone. In cases of secondary spread from intestinal adenocarcinomas, distinction is often difficult when based on morphologic grounds alone, because many primary adenocarcinomas of the bladder closely resemble intestinal carcinomas. In advanced cases of secondary adenocarcinoma, tumor may, however, involve the bladder mucosa, and cases are well documented in which bladder involvement by colonic or appendiceal carcinoma has been the presenting symptom of disease. Accordingly, the diagnosis of a primary adenocarcinoma of intestinal type is established with certainty only after secondary involvement from the intestinal tract is clinically excluded. Immunohistochemistry cannot reliably distinguish primary from secondary enteric-type adenocarcinoma. The distinction is not possible on morphologic grounds and ultimately rests on the exclusion of a tumor elsewhere by clinical evaluation. Distinction between a signet ring cell carcinoma and a benign process is usually not difficult, although occasional nephrogenic adenomas have tiny tubules that simulate signet ring cells, rarely leading to confusion with signet ring cell carcinoma. The lesion that creates the greatest problem in differential diagnosis with clear cell adenocarcinoma is nephrogenic adenoma. The clinical features associated with nephrogenic adenomas typically differ from those of clear cell adenocarcinomas. Many patients with the former lesion are under 30 years of age (including children), whereas the youngest patient with clear cell adenocarcinoma of the bladder was 43 years old. Nephrogenic 12 Tumors of the Urinary Tract 635 adenoma is usually associated with a history of a genitourinary operation, trauma, or calculi, whereas these associations are usually absent in cases of clear cell adenocarcinoma. Large size also favors a diagnosis of clear cell adenocarcinoma over a nephrogenic adenoma; none of them has been an incidental finding on microscopic examination. Nephrogenic adenomas are typically of microscopic size, although lesions up to 7 cm have been described. Histologic distinction is difficult in occasional cases because both lesions have tubular, cystic, and papillary patterns, and some cases of nephrogenic adenoma show cytologic atypia. Several features, however, favor a diagnosis of carcinoma: these include a conspicuously diffuse arrangement of cells with abundant clear cytoplasm, abundant intracytoplasmic glycogen, prominent nucleoli, nuclear pleomorphism, and mitotic activity. Rare clear cell adenocarcinomas, however, may be cytologically bland and be difficult to distinguish from a nephrogenic adenoma. In such cases, consideration of the clinical history and the size of the lesion, as well as repeated biopsy, may be helpful. It should be remembered that nephrogenic adenomas may recur, so recurrence should not lead to a diagnosis of carcinoma in the absence of convincing microscopic evidence of malignancy. Furthermore, if nephrogenic adenoma were a precursor of clear cell adenocarcinoma, one might expect the latter to be more common in men than women and more common in the bladder than in the urethra, whereas the reverse is true. The distinctive microscopic features of clear cell adenocarcinoma should allow its differentiation from other primary adenocarcinomas of the bladder. Distinction from a metastatic clear cell carcinoma from the female genital tract or kidney may be more difficult. A young age and a history of perinatal exposure to diethylstilbestrol should bring into consideration a metastasis from the female genital tract, which can be excluded only by clinical evaluation. Tumors located in the posterior wall or trigone may represent direct extension of a clear cell adenocarcinoma arising in a urethral diverticulum. Additionally, hobnail cells and intracytoplasmic mucin are typically absent in the renal tumors, in contrast to the bladder tumors. It is also helpful that renal cell carcinoma rarely spreads to the bladder, even in late stages of disease. They are typically elderly, with a mean age of 69 years,211 and their symptoms are similar to those of other patients with bladder cancer; gross hematuria is the most common complaint. Hypercalcemia has been present in at least one case217 and ectopic adrenocorticotropic hormone production in another. The prognosis is generally poor,214 but occasionally radical cystectomy and aggressive adjuvant chemotherapy have resulted in long-term survival. Histologically, they are composed of sheets of small, oat-shaped cells with scant cytoplasm and hyperchromatic nuclei, as well as slightly larger cells with more variation in nuclear chromatin, comparable with the intermediate cell type of pulmonary small cell carcinoma, or mixtures of the two cell types are seen. The tumors may contain small rosette-like structures or, less commonly, malignant giant cells. Cases having features similar to those of large cell neuroendocrine carcinoma of the lung are also seen (see later discussion). Other forms of carcinoma, usually either in situ or invasive urothelial carcinoma, but occasionally squamous cell carcinoma or adenocarcinoma, are present in approximately half of the cases. Immunohistochemical stains for lymphoid and epithelial markers may be helpful in these cases. Primary small cell carcinoma of the bladder should be distinguished from a metastasis. Direct extension from prostatic small cell carcinoma also needs to be considered; this most often occurs in the setting of known prostatic adenocarcinoma and often has an adenocarcinoma component. Prostatic small cell carcinoma is much less common than such urinary bladder tumors. Large Cell Neuroendocrine Carcinoma A few examples of primary large cell neuroendocrine carcinoma have been reported. Mixed histology is often present with urothelial carcinoma, squamous cell carcinoma, or adenocarcinoma. Distinction from a high-grade urothelial carcinoma requires demonstration of neuroendocrine differentiation. Most are cured by transurethral resection, but local recurrence and metastases have occurred. The great rarity of carcinoid of the bladder means that the diagnosis should be made only after other tumors that may simulate carcinoid have been excluded. Small cell carcinoma can have carcinoid-like areas but should be reported as small cell carcinoma. Some urothelial carcinomas grow in the form of nests that superficially resemble those of a carcinoid. Differences in the cytologic features of urothelial carcinoma and carcinoid and the performance of silver stains, immunohistochemistry, or electron microscopy should establish the diagnosis. Their gross appearance varies according to whether they are located predominantly in the lamina propria (most common), in which case they may form a large protuberant mass in the bladder lumen; intramural location or serosal attachment can also be seen. Given the limited experience with these tumors, most authors favor making a diagnosis of leiomyosarcoma in tumors with moderate nuclear atypia, even a few mitotic figures, or an infiltrative growth pattern. MalignantMesenchymalTumors Primary sarcomas of the urinary bladder are also uncommon. A distinct age distribution is seen with rhabdomyosarcoma occurring in children and leiomyosarcoma being most common in adults. In addition, virtually all other types of sarcoma including fibrosarcoma,263 unclassified pleomorphic sarcoma (socalled malignant fibrous histiocytoma),264 osteosarcoma,265 chondrosarcoma,266 angiosarcoma,239 so-called hemangiopericytoma,267 liposarcoma,268 and perivascular epithelioid cell tumor269 occur rarely in the bladder. All of these should be diagnosed only after sarcomatoid carcinoma has been excluded carefully.
Discount clindamycin 150mg with mastercard
It has been recommended that squamous and adenosquamous carcinoma not be assigned a Gleason grade infection occurs when buy clindamycin online pills. B, Under highpower magnification, the tumor cells are revealed between basal lamina and prostatic epithelial cells. Furthermore, the tumor cells often exhibit much greater nuclear pleomorphism and more frequent mitotic activity than prostate adenocarcinoma49,346. Clinical history, careful microscopic evaluation, and immunohistochemical stains are all helpful for this differential diagnosis. Sarcomatoid Carcinoma Sarcomatoid carcinoma of the prostate is another uncommon variant of adenocarcinoma with a biphasic appearance, containing carcinoma and a spindle or pleomorphic sarcomatoid component. It can be difficult to differentiate from true sarcomas in situations in which either the conventional microacinar carcinoma histology is minimal or the tissue sample is limited. The terms carcinosarcoma, malignant mixed mesodermal tumor, spindle cell carcinoma, and carcinoma with pseudosarcomatous stroma have been used in the literature to describe this lesion. Strictly speaking, carcinosarcoma has been traditionally defined as a biphasic tumor with heterologous sarcomatous components. We and others use the term sarcomatoid carcinoma to describe all tumors showing biphasic growth with carcinoma and sarcomatous components regardless of the presence or absence of heterologous elements. In our experience, these tumors are always associated with a high-grade prostatic adenocarcinoma that occurred either previously to , or simultaneously with, the sarcomatoid component. The majority of patients have metastatic disease at the time of diagnosis, and 50% have a history of prostate cancer treated with radiation or hormonal therapy. The pattern is that of high-grade sarcoma and in most cases similar to that of undifferentiated pleomorphic sarcoma of soft tissues. A heterologous sarcomatoid component (osteosarcomatous, chondrosarcomatous, rhabdomyosarcomatous) can be observed in up to one third of cases. This is a small-gland proliferation with small and larger glands lined by hyperchromatic nuclei. Hyperplasia of Mesonephric Remnants Hyperplasia of mesonephric remnants is a rare yet important small glandular proliferation within the prostate gland, the severity of the diagnostic pitfall being exemplified by a case misdiagnosed as cancer that resulted in a radical prostatectomy that did not show evidence of cancer. The acini are lobular, but can be infiltrative and may be architecturally mistaken for adenocarcinoma. This cytologically innocuous finding is probably underreported and interpreted as benign prostatic acini, but this is of no apparent clinical consequence. Microscopically, it is characterized by a lobular proliferation of small tubular structures lined by a single layer of epithelium or by infiltrating glands between muscle bundles and prostatic acini without a stromal desmoplastic response. Confusion with cancer is compounded by the potential of mesonephric remnants to be associated with ganglia and nerves, simulating perineural invasion. Distinction from cancer is usually not a problem when attention is paid to the cytologic features at higher power. The glands show a basal cell layer and contain corpora amylacea or orange-brown secretions, and the nuclei lack nucleomegaly or prominent nucleoli. The lesion consists of tubular structures that are slightly larger than normal ducts and lined by stratified proliferation of elongated fusiform epithelial cells. On high power, the nuclei of the glands are characteristically hyperchromatic, obscuring any nuclear detail, and the cells are situated perpendicular to the basal membrane. This is a proliferation of small to medium-size glands with inconspicuous basal cells. Chapter 12); it was first described in 1949 by Davis,438 who designated it a hamartoma of the urinary bladder, but Friedman and Kuhlenbeck439 shortly thereafter assigned its present name on the basis of its striking resemblance to the developing renal tubules and its possible neoplastic potential. Although nephrogenic adenoma occurs primarily in the bladder, the urethra is involved in 10% to 15% of cases and, less frequently, the ureter440 and renal pelvis. The most common associated conditions include previous surgery or trauma, infection, calculi, or a history of renal transplant. The signs and symptoms in the remainder of the patients are nonspecific and include hematuria, dysuria, frequency, urgency, and suprapubic and flank pain. When nephrogenic adenoma is present in the prostatic urethra and involves suburethral tissue and seemingly infiltrates the prostatic parenchyma proper, it may potentially be confused with a prostatic adenocarcinoma because the common histologic manifestation is a proliferation of closely packed small glands. The tubules of nephrogenic adenoma show considerable variation in size and shape, sometimes being cystically dilated. They are usually small and round to oval but may be convoluted, resembling collecting ducts or convoluted tubules of the kidney. Papillary projections may be seen, either on the surface (exophytic component) or within the dilated tubules. The cytoplasm is usually scant, but occasionally a moderate to large amount of eosinophilic or clear cytoplasm may be seen. The nuclei are round and small or pyknotic and usually lack nucleoli, although they may sometimes be conspicuous. The tubules are lined predominantly by cuboidal cells with eosinophilic cytoplasm. Despite the fact that nephrogenic adenoma may be seen between prostatic ducts, it must be remembered that it is not an invasive lesion. In the prostatic urethra there are submucosal glands, but also prostatic ducts emptying their products into the urethral lumen. Thus nephrogenic adenoma may be in contact with prostatic ducts, giving a false impression of prostatic invasion. Mazal and colleagues451 reported nephrogenic adenoma cases in patients who had renal transplants. Some investigators have suggested that nephrogenic adenoma is a precursor or a benign counterpart of clear cell carcinoma of the genitourinary tract. Although a few cases of nephrogenic adenoma coexisting with a clear cell adenocarcinoma have been reported, a direct relationship between the two has not been proved. Nephrogenic adenoma can recur after conservative therapy, but in no case is it associated with unequivocal malignant change. This lowmagnification photograph shows a cellular tumor with tubular and papillary configuration. They are covered by columnar prostatic epithelium or by a mixture of prostatic and transitional epithelium. They are morphologically identical to prostatic glands and typically are lined by two cell layers, composed of tall columnar epithelial cells with basally located nuclei and a surrounding layer of flattened basal cells. No cellular pleomorphism, necrosis, increased mitoses, or prominent nucleoli are seen. They have been termed adenomatous polyp of prostatic urethra,304 prostatic urethral polyp,305 papillary adenoma of prostatic urethra,306,461 and prostatic caruncle. The lining cells are uniform without nuclear pleomorphism, increased mitoses, or prominent nucleoli. The main characteristics of seminal vesicles include scattered pleomorphic nuclei (monster cells) and golden-brown lipofuscin pigment in the cytoplasm. B, Higher magnification reveals monster cells and golden-brown lipofuscin pigment. Both have tubuloalveolar glands as well as closely packed small acini, which are lined by pseudostratified, tall columnar secretory cells and a layer of small basal cells. Epithelium of the ejaculatory duct and seminal vesicle characteristically contains coarsely granular, yellow-brown lipofuscin pigment. The pigment, however, tends to be finer and less refractile than seminal vesicle pigment. These structures often show small glandular structures arranged in a back-to-back pattern, an therefore they may be confused with a small acinar carcinoma of the prostate. Seminal vesicle secretions are fairly common and are composed of acid mucopolysaccharides. Inspissation of secretions appears to be associated with loss of acidity, presumably resulting in dense plate-like secretions and crystallization. Awareness of both the crystalloid morphology in seminal vesicle tissue and the distinguishing features from prostatic crystalloids may be important when interpreting prostate needle biopsy samples in which seminal vesicle epithelium may be confused for prostate carcinoma because of a small acinar morphology with accompanying cytologic atypia and crystalloid morphology. They are associated with an excretory duct and are frequently surrounded by skeletal muscle. The lesion, however, is located randomly within the prostate; it may be focally present within an acinus or involve groups of acini, but is usually small.
Buy clindamycin 150 mg overnight delivery
The prognosis is favorable and similar to that of a borderline serous tumor infection leg clindamycin 150 mg amex, with a benign evolution even when noninvasive extraovarian tumor implants are present. Branching papillae grow from the cyst linings into the lumina, reminiscent of a borderline serous tumor. Microscopically, the cysts and papillae are lined predominantly by columnar mucinous endocervical-like cells, with variable numbers of indifferent cells with eosinophilic cytoplasm. The papillae are covered by columnar cells with basal nuclei and abundant mucin-filled cytoplasm. Mitotic figures are infrequent in most tumors, and usually minimal nuclear atypia is present. Endometriosis is present in the ovary adjacent to the tumor in 30% to 70% of cases, and in some instances the tumor appears to originate in the endometriosis. This most often takes the form of clusters of eosinophilic or pale cells, usually with little surrounding reaction, within the stroma. The implants are generally of the noninvasive epithelial type and frequently are surrounded by desmoplastic stroma. Neither intraepithelial carcinoma nor stromal microinvasion has been associated with an unfavorable outcome. Endocervical-like mucinous carcinomas appear to be somewhat smaller than intestinal mucinous carcinomas, with an average diameter of about 12 cm. A prominent component of columnar cells with mucinous cytoplasm that resemble endocervical cells is present, although other patterns of differentiation, especially endometrioid, are also commonly present. The pattern of invasion can be expansile or infiltrative, or both patterns can be present. Carcinomas that contain both endocervical-like mucinous and endometrioid components can be viewed as endocervical-like mucinous carcinomas if the mucinous components greatly predominate; otherwise, they are best classified as mixed endometrioid and mucinous carcinomas. Endocervical-like borderline mucinous tumors have a different immunophenotype than intestinaltype mucinous tumors. Mucinous epithelium can be prominent in some Brenner tumors, known as metaplastic Brenner tumors, and expansion of this mucinous component may give rise to some mucinous tumors. The mucinous epithelium is generally a focal finding, but it can be sufficiently prominent to suggest a mucinous cystadenoma, and in a few cases is proliferative and atypical enough to be compatible with a borderline mucinous tumor or even a carcinoma. Ovarian mucinous tumors are occasionally associated with teratomas, and some mucinous tumors appear to be derived from teratomas. Two large series found 41 mucinous cystadenomas; 44 borderline mucinous tumors, including 4 with intraepithelial carcinoma; and 11 mucinous carcinomas. The others may arise from nonintestinal mucinous epithelium in the teratoma, but they also may be collision tumors in which the mucinous tumor is of surface epithelial, rather than germ cell, origin. Pseudomyxoma ovarii is often prominent, especially in women with borderline tumors or carcinomas, and some women have pseudomyxoma peritonei, presumably of ovarian origin in this unusual setting. If there is no evidence of a potential extraovarian primary and sections of the ovary reveal evidence of a teratoma as well as a mucinous neoplasm, it is reasonable to conclude that the mucinous tumor is of primary ovarian origin, presumably arising in the teratoma, despite an unusual immunophenotype or clinical setting. Endometrioid Tumors Endometrioid tumors of the ovary have an epithelial component that resembles proliferative, hyperplastic, or malignant endometrium. Borderline endometrioid tumors occur at an average age of 50 to 51 years, are generally unilateral and confined to the ovary, and have a favorable outcome with no recorded deaths from tumor even when microinvasion is present. Endometrioid carcinoma has a favorable prognosis, relative to other types of adenocarcinoma of the ovary, at least partly because it tends to be low grade and to be detected in an early stage. In a study of 63 members of families with Lynch 676 Ovary, Fallopian Tube, and Broad and Round Ligaments syndrome, cancers developed at a mean age of 48 years. The cut surfaces are tan or white and contain small cysts ranging from a few millimeters to several centimeters in diameter. Microscopically, tubular or cystic glands are surrounded and separated by fibrous stroma. These are columnar, with basophilic or amphophilic cytoplasm and uniform round or oval nuclei. The nuclei may be pseudostratified, as in proliferative endometrium, but mitotic figures are usually rare or absent. Squamous metaplasia may be present and, in rare tumors, the glands are lined by ciliated cells. Russell and colleagues247 and Roth and Merkur249 used the name "proliferating" endometrioid tumors. Kao and Norris250 designated the tumors they reported "adenofibromas with epithelial atypia. Borderline endometrioid tumors are usually unilateral (only 8% were bilateral in one large series) and many are adenofibromas or cystadenofibromas. Microscopically, low-grade borderline endometrioid tumors are adenofibromas with glands of increased density relative to benign endometrioid tumors, showing varied architecture and focal crowding. The epithelial cell nuclei are pseudostratified or stratified, and mild to moderate nuclear atypia and occasional mitotic figures are present (<3 per 10 hpf). The proliferative endometrioid glands resemble those seen in simple or complex endometrial hyperplasia. More proliferative borderline endometrioid tumors exhibit two main patterns of growth. The papillae often have a villoglandular appearance with broad fibrovascular cores. The cells covering the papillae show variable degrees of stratification and atypia. Mitotic activity is usually low (<3 per 10 hpf) but, in some tumors, mitotic figures are more frequent. Proliferative activity can be conspicuous in borderline endometrioid tumors, but the degree of glandular crowding is usually less than in endometrioid carcinoma and the proliferative nests have a smooth contour and are surrounded by stroma. Glands lined by a single layer of benign endometrial-type cells grow in dense fibrous stroma. The glandular pattern is similar to that seen in complex hyperplasia of the endometrium. Squamous and mucinous metaplasia is common, particularly in adenofibromatous tumors, and rare neoplasms contain numerous ciliated cells. Endometriosis is often present in the involved ovary and elsewhere in the pelvis, and origin from endometriosis can be demonstrated in occasional cases. Stromal microinvasion is seen in 5% to 15% of borderline endometrioid tumors, in which small, irregular glands infiltrate the stroma or in which foci of confluent glandular growth appear in an area less than 3 mm. Endometrioid carcinoma is a cystic and solid or completely solid tumor, typically measuring 10 to 20 cm in diameter. Endometrioid carcinoma is a glandular or papillary tumor that resembles adenocarcinoma of the endometrium. The growth pattern is glandular, papillary, or a mixture of the two, and invasion can take the form of haphazard infiltration of the stroma or confluent growth. The papillae often have a villoglandular appearance, with prominent fibrovascular supporting cores. The glands and papillae are lined by columnar cells with amphophilic to basophilic cytoplasm. The degree of atypia, the amount of nuclear stratification, and the extent to which the glands coalesce into foci of solid growth increase as the grade increases. Endometrioid carcinoma can be graded using the same criteria as endometrial adenocarcinoma. Grade 1 tumors grow in a glandular or papillary pattern with less than 5% solid tumor growth. The cells lining the glands in this moderately differentiated adenocarcinoma have an increased nucleus to cytoplasm ratio. The back-to-back glands are lined by columnar cells with stratified hyperchromatic nuclei. Areas of squamous or spindle cell differentiation are not counted in the determination of percentage of solid growth. If the nuclei are grade 3 and the growth pattern is grade 1 or 2, the final grade is increased by one level. Endometrioid carcinoma can also be graded using the previously discussed universal grading system for ovarian cancer (see Table 13A-5). Keratin granulomas, which the surgeon may mistake for tumor implants, are found occasionally on the peritoneum in such patients. Endocervical-like columnar cells with basophilic mucinous cytoplasm or cells with intermediate features between endocervical and endometrioid type cells, but with mucinous cytoplasm, may be present.
Discount clindamycin 300mg with mastercard
In large pedunculated polyps antimicrobial yahoo purchase on line clindamycin, the mucosa may prolapse into the stalk or deeper into the bowel wall and mimic adenocarcinoma ("pseudoinva sion"). Lipohyperplasia of the Ileocecal Valve Variably termed lipomatous hypertrophy, lipomatosis, and lipohyperplasia, an excess of submucosal adipose tissue causing some degree of protrusion into the lumen of the cecum is a relatively common finding and may occasion ally be prominent. The most common of these lesions in the appendix is the sessile serrated polyp,124 which was previously often referred to as diffuse hyper plasia. Villous adenomas are more common than tubular Juvenile Polyposis and Polyps See section on large intestine. Serrated adenomas (often referred to as "tra ditional" serrated adenomas) are rare at this site. Clinical Features Most small adenomas and serrated polyps of the appendix are discovered incidentally by the pathologist on exami nation of an appendectomy specimen. Macroscopic Appearances the appendix is grossly normal in many cases with adenomas and serrated polyps. Some cases with mucin secretion show sausagelike appendiceal dilatation, an appearance often described as a "mucocele. Histologic Appearances Adenomas and serrated polyps of the appendix are similar to their counterparts in the large intestine. Sessile serrated polyps may show areas of progression to cytologic dysplasia, either conven tional dysplasia with hyperchromatic, elongated nuclei and slightly basophilic cytoplasm, or socalled serrated dysplasia with eosinophilic cytoplasm and more vesicular chromatin. In the latter situation, the cystic appendix may be lined by a thin layer of lowgrade dysplastic epithelium (which can be deceptively bland), or entirely devoid of epithelium because of compression by mucin. If no lining is found on initial sampling, more extensive sampling is advisable to identify areas of residual adenoma. The underlying submucosa often undergoes extensive fibrosis and may show dystrophic calcification. Low-Grade Appendiceal Mucinous Neoplasm Terminology applied to lowgrade mucinproducing neo plasms of the appendix associated with pseudomyxoma peritonei has been varied and confusing. Of note, although the ovary may be secondarily involved, it is almost never the primary site. The natural history of lowgrade pseudomyxoma peri tonei is distinctive: the tumor is usually confined to the abdominal cavity throughout the disease course, without metastases to lymph nodes or liver or invasion of adjacent viscera. Radical cytoreductive surgery appears to improve survival130; heated intraperitoneal chemotherapy in this setting may be beneficial in selected patients. Of note, patients with local ized periappendiceal disease at presentation appear to have a lower risk of development of pseudomyxoma peri tonei, particularly when no epithelium is detected. Metastases to the ovary are common at presenta tion and may easily be mistaken for an ovarian primary. The prognosis is worse for nonmucinous adenocarcino mas and signet ring cell carcinomas. Histologic Appearances Appendiceal adenocarcinomas resemble colorectal ade nocarcinomas. They are nearly always asymptomatic, being found inci dentally in appendectomy specimens. Tumors less than 1 cm have very low metastatic potential, those between 1 and 2 cm have a low risk, and tumors greater than 2 cm (which account for at most 5% of appendiceal carcinoid tumors) have a signifi cant risk of lymph node metastases. Patients with appendiceal carcinoid tumors almost never develop carcinoid syndrome, which occurs in only a subset of those rare patients who have liver metastases. Macroscopic Appearances Appendiceal carcinoid tumors are usually localized to the tip of the appendix. Larger tumors are often relatively well circumscribed and appear yellow after formalin fixation. Histologic Appearances Most carcinoid tumors of the appendix resemble ileal (enterochromaffin cell) carcinoid tumors and are com posed of small nests of cells with round nuclei, granular chromatin, inconspicuous nucleoli, and eosinophilic cyto plasm. Tubular car cinoid tumors, composed of small tubules and trabecu lae,144 may be mistaken for metastatic adenocarcinoma. Uniform cytomorphology with bland nuclei and expres sion of chromogranin are helpful distinguishing features. Immunohistochemistry Appendiceal carcinoid tumors are usually strongly and diffusely positive for broadspectrum keratins, chromo granin. Goblet cell carcinoid tumors are more aggressive than conventional carcinoid tumors of the appendix and may present with peritoneal dissemina tion, with a predilection for the ovaries. Patients with metastatic disease at presentation have a guarded prognosis, although their clinical course may be relatively indolent. Mixed adeno neuroendocrine carcinomas (adenocarcinomas arising in goblet cell carcinoid tumors; see histologic appearances) progress rapidly, and affected patients usually succumb to metastatic disease within 5 years. Histologic Appearances Goblet cell carcinoid tumors typically infiltrate through the wall of the appendix in a concentric fashion. The tumor is composed of small nests of cells with abundant intracytoplasmic mucin and eccentric, compressed hyper chromatic nuclei, resembling goblet cells or signet ring cells. Occasional Paneth cells and neuroendo crine cells are often (though not invariably) seen. The entire appendix may be involved, although the mucosa is often relatively spared. Goblet cell carcinoid tumors may progress to con ventional adenocarcinoma, in which case the term mixed adenoneuroendocrine carcinoma (or adenocarcinoma exgoblet cell carcinoid tumor) may be applied. The signet ring cell carcinoma subtype may be mistaken for meta static gastric carcinoma; the concentric pattern of growth would favor an appendiceal primary, and identification of the goblet cell carcinoid component can help confirm the diagnosis. The clinical term mucocele describes a sausagelike, dilated gross appearance of the appendix, caused by the accumu lation of mucin in the lumen. Nerve Sheath Proliferations Appendiceal "neuroma" (also known as neurogenic appendicopathy or neurogenous hyperplasia) is a common incidental histologic finding at the time of appendec tomy. Adenomas are more common in men, and the incidence increases with age, as does the number of adenomas. Patients with Lynch syndrome have adenomas at a younger age, but they are usually few in number. Adenomas occur throughout the colon and rectum with a fairly even anatomic distribution. They are usually asymptomatic, being detected at colonoscopic screening for colorectal cancer. Macroscopic Appearances Adenomas are usually less than 1 cm and appear as sessile polyps. Larger adenomas may be pedunculated and protrude into the lumen with a submucosal stalk. A small subset of adenomas is flat or slightly depressed; such lesions are difficult to recognize endoscopically. The adenoma shows architectural complexity, and the lesional cells contain rounded nuclei with vesicular chromatin. Tubular adenomas contain tubular structures and have a relatively flat surface, whereas villous areas consist of fingerlike projections containing small amounts of lamina propria. Most adenomas show lowgrade (mild to moderate) dysplasia, with relatively uniform, elongated hyperchromatic nuclei showing pseudostrat ification but maintaining polarity with apical, often slightly basophilic cytoplasm, lining crypts or villi with relatively even architectural distribution. In highgrade (severe) dysplasia, nuclei show loss of polarity, often with a more rounded con figuration, vesicular chromatin, prominent nucleoli, and variability, and architectural complexity is seen, with crib riforming and a backtoback crypt configuration. Highgrade dysplasia encompasses lesions for merly designated "carcinoma in situ"; the latter term should not be used to avoid confusion. Intramucosal ad enocarcinoma can be applied to lesions showing mark edly complex architecture with severe nuclear atypia, singlecell infiltration of the lamina propria, or a des moplastic stromal response, although the latter finding is rare in the absence of submucosal invasion. Because essentially no metastatic potential exists without sub mucosal invasion, some pathologists prefer not to use the designation intramucosal adenocarcinoma and in stead retain the term high-grade dysplasia for all such lesions. In such lesions, there is a risk of overinterpreting the findings as invasive adenocarcinoma. The presence of lamina propria, hemosiderin, rounded crypt contours, acellular mucin pools or pools of mucin partially surrounded by a strip of dysplastic epithelium, and lowgrade dysplasia favors a benign diagnosis, whereas a desmoplastic stromal response, irregularly infiltrative mucin pools, single neo plastic cells floating within the mucin, and highgrade dysplasia (particularly when the overlying adenoma shows lowgrade dysplasia) argue for invasive adenocarcinoma. The term malignant polyp has been used to refer to small polypoid adenocarcinomas (without an adenoma tous component) and adenomas that contain foci of ade nocarcinoma invading the submucosa. The former lesion, and sessile adenomas associated with adenocarcinoma invasive into the submucosa, should both be treated with segmental colectomy, when medically appropriate, owing to the significant risk of lymph node metastasis. In con trast, pedunculated polyps with invasive adenocarcinoma into the submucosa can be managed conservatively,157 provided none of the following ("unfavorable") features are identified: lymphovascular invasion, poor differentia tion, a positive submucosal margin, or tumor 1 to 2 mm from the margin.