Cheap meloxicam generic
Effects of intensive diabetes therapy on neuropsychological function in adults in the Diabetes Control and Complications Trial psoriatic arthritis in the knee order 15 mg meloxicam free shipping. The association of atherosclerosis, vascular risk factors, and retinopathy in adults with diabetes: the atherosclerosis risk in communities study. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss: Early Treatment Diabetic Retinopathy Study Report #18. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Serum lipoproteins in the diabetes control and complications trial/epidemiology of diabetes intervention and complications cohort: associations with gender and glycemia. Impact of pregnancy on the progression of diabetic retinopathy in Type 1 diabetes. Pre-eclampsia is a potent risk factor for deterioration of retinopathy during pregnancy in Type 1 diabetic patients. National Institute of Child Health and Human Development Diabetes in Early Pregnancy Study. Diabetic cataract removal: postoperative progression of maculopathy-growth factor and clinical analysis. Cataract surgery in patients with diabetic retinopathy: visual outcome, progression of diabetic retinopathy, and incidence of diabetic macular oedema. A prospective, case controlled study of the natural history of diabetic retinopathy and maculopathy after uncomplicated phacoemulsification cataract surgery in patients with type 2 diabetes. Quantifying alterations of macular thickness before and after panretinal photocoagulation in patients with severe diabetic retinopathy and good vision. Treatment with intravitreal steroid reduces blood-retinal barrier breakdown due to retinal photocoagulation. Panretinal photocoagulation and intravitreal triamcinolone acetonide for the management of proliferative diabetic retinopathy with macular edema. Cellular and molecular abnormalities in the vascular endothelium of diabetes mellitus. Vascular damage in a mouse model of diabetic retinopathy: relation to neuronal and glial changes. Role of vascular endothelial growth factor in regulation of physiological angiogenesis. Inhibition of vascular endothelial growth factor prevents retinal ischemia-associated iris neovascularization in a nonhuman primate. Vascular endothelial growth factor induces rapid phosphorylation of tight junction proteins occludin and zonula occluden 1. Vitreous and aqueous concentrations of proangiogenic, antiangiogenic factors and other cytokines in diabetic retinopathy patients with macular edema: Implications for structural differences in macular profiles. Vascular endothelial growth factor-induced retinal permeability is mediated by protein kinase C in vivo and suppressed by an orally effective beta-isoform-selective inhibitor. Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Intravitreal injection of triamcinolone: an emerging treatment for diabetic macular edema. Glucocorticoid regulation of endothelial cell tight junction gene expression: novel treatments for diabetic retinopathy. An ocular clinicopathologic correlative study of six patients from the Diabetic Retinopathy Study. Characterization of macular edema from various etiologies by optical coherence tomography. The exudative lesions in diabetic retinopathy with special regard to the hard exudate. Tractional cystoid macular edema: a subtle variant of the vitreomacular traction syndrome. Optical coherence tomography assessment of the vitreoretinal relationship in diabetic macular edema. Impaired color vision associated with diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report No. Temporal variation in diabetic macular edema measured by optical coherence tomography. Diurnal variation in retinal thickening measurement by optical coherence tomography in center-involved diabetic macular edema. Ophthalmoscopy versus photography- Early Treatment Diabetic Retinopathy Study Report Number 5. Reproducibility of macular thickness and volume using Zeiss optical coherence tomography in patients with diabetic macular edema. Repeatability and reproducibility of fast macular thickness mapping with stratus optical coherence tomography. Errors in retinal thickness measurements obtained by optical coherence tomography. Detection of diabetic foveal edema: contact lens biomicroscopy compared with optical coherence tomography. Comparison of the clinical diagnosis of diabetic macular edema with diagnosis by optical coherence tomography. Diabetic macular edema assessed with optical coherence tomography and stereo fundus photography. Comparison of the modified Early Treatment Diabetic Retinopathy and mild macuilar grid laser strategies for diabetic macular edema. The correlation between fluorescein angiographic and optical coherence tomographic features in clinically significant diabetic macular edema. Intravitreal triamcinolone acetonide for diabetic diffuse macular edema: preliminary results of a prospective controlled trial. Oscillatory potentials, macular recovery time, and diabetic retinopathy through 3 years of intensified insulin treatment. Multifocal electroretinogram and shortwavelength automated perimetry measures in diabetic eyes with little or no retinopathy. Retinal function in normal and diabetic eyes mapped with the slow flash multifocal electroretinogram. Visual fields correlate better than visual acuity to severity of diabetic retinopathy. Visual acuity and perimetry as measures of visual function in diabetic macular oedema. The use of scanning laser ophthalmoscope microperimetry to detect visual impairment caused by macular photocoagulation. Vitrectomy for diabetic macular traction and edema associated with posterior hyaloidal traction. Modified grid laser photocoagulation versus pars plana vitrectomy with internal limiting membrane removal in diabetic macular edema. Vitrectomy results in diabetic macular oedema without evident vitreomacular traction. Prospective evaluation of intravitreal triamcinolone acetonide injection in macular edema associated with retinal vascular disorders. Time course of changes in retinal thickness and visual acuity after intravitreal triamcinolone acetonide for diffuse diabetic macular edema with and without previous macular laser treatment. Treatment of intraocular proliferation with intravitreal injection of triamcinolone acetonide. Intravitreal triamcinolone injection for diabetic macular edema: a clinical and fluorescein angiographic case series. Intraocular pressure elevation after intravitreal triamcinolone acetonide injection. Exudative macular degeneration and intravitreal triamcinolone: 18 month follow up. Cataract formation and other complications of intravitreal triamcinolone for macular edema.
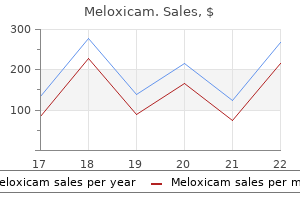
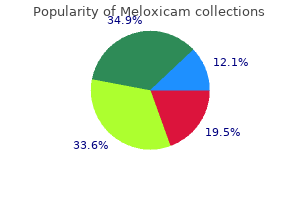
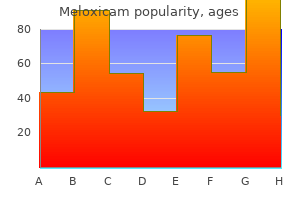
Buy genuine meloxicam on-line
This is particularly evident for individuals with a red-green color vision defect who have a reduced number of cone types from three to two and they have a reduced number of fundamental color sensations neck brace for arthritis in neck purchase meloxicam without a prescription. Because blue and yellow are processed in an opponent fashion, for a dichromat, there are no intermediate hues that represent the simultaneous sensation of both blue and yellow. Here the hue components have been resampled with the same reduced resolution as in panel (c). The spatial resolution of the hue components (b) and (f) are very different but on casual inspection they appear nearly identical. If you look closely you can see that the yellow color is blurred outside the black lines. This is largely ignored by the visual system that uses the black and white edges to define detailed boundaries in the image. The hue information is used to define qualities of the objects other than spatial detail. However, the term dichromat is also appropriate because dichromats see only two hues. In contrast, people with normal color vision see more than 100 different hues in addition to black, white, and gray. Dichromats confuse red with green, and they confuse, with red and green, all colors in the spectrum that fall between them, including yellow, orange, and brown. They see blue and violet as the same color, and bluegreen is indistinguishable from white or gray. During evolution, the midget ganglion cell system is believed to have arisen in an ancestor to modern primates prior to the emergence of trichromatic color vision. The neighbors of an L/M cone would have been predominately of the identical spectral type because S cones are many times fewer in number (~5% of the total in humans). Assuming a balanced center versus surrounds, this system signals the presence of light/dark boundaries in a visual scene. These are exactly the stimulus conditions we associate with the percepts of black and white. In addition to serving the percepts of black and white, this system presumably evolved to serve high acuity spatial vision, signaling the presence of dark/light edges with great detail and precision. Representing more than 90% of the ganglion cells that serve the central retina, the midget ganglion cells are the only output neurons that have sufficient numbers to transmit information about fine detail in the image. Accordingly, the midget ganglion cells appear to simultaneously serve two purposes in vision for a dichromat. In turn, the percepts of black and white in the dichromatic image are responsible for coding information about fine detail in the image. We know that it is evening because of the red of the sunset or that a colleague is embarrassed because of the redness in his face. However, we do not need to know details of the spatial distribution of the colored areas. The S cones are used in color vision but they do not participate in providing high acuity. They can participate in providing hue information at a much lower sampling density than the L and M cones that provide information about spatial detail. These low resolution hue components provide almost no information that allows us to recognize the objects in the scene. Small bistratified ganglion cells make up less than 10% of the total output of the retina and they have opponent blue-yellow responses. However, they all respond to blue and inhibit to yellow, leaving us without an explanation of the physiological basis for the yellow half of the blue-yellow opponent system. It is possible that a subpopulation of midget ganglion cells is also involved in blue-yellow color vision and they could be important for providing the required two opponent parts of the system. If this were true, details of the specialized functions of each of three major ganglion cell populations carrying information to the brain would be easily understood. The midget ganglion cells provide the biological substrate for percepts of black and white and are responsible for carrying information about high acuity spatial detail. The second major ganglion cell population, the parasol cells, are responsible for the perception of motion. These make up only ~5% of ganglion cells in the fovea but are a much larger proportion of ganglion cells in the peripheral retina where our motion perception is most acute. Although details are left to be worked out, the third major ganglion cell population, the small bistratified ganglion cells must participate in blue-yellow color vision. However, the introduction of red-green color vision complicates the story because adding a randomly distributed third cone type makes almost every midget ganglion cell respond to either diffuse red or diffuse green light in addition to dark and light edges. How this is accomplished is one of the fascinating remaining mysteries of our visual system. VanMeeteren A: Calculations on the optical modulation transfer function of the human eye for white light. Hyvarinen L, Rovamo J, Laurinen P, Peltomaa A: Contrast sensitivity function in evaluation of visual impairment due to retinitis pigmentosa. Hyvarinen L, Rovamo J, Laurinen P, et al: Contrast sensitivity in monocular glaucoma. Hyvarinen L, Laurinen P, Rovamo J: Contrast sensitivity in evaluation of visual impairment due to macular degeneration and optic nerve lesions. Hyvarinen L, Laurinen P, Rovamo J: Contrast sensitivity in evaluation of visual impairment due to diabetes. Assessment of vision using vertical and horizontal gratings and optotypes at different contrast levels. Bodis-Wollner I: Visual acuity and contrast sensitivity in patients with cerebral lesions. Brown B: Reading performance in low vision patients: relation to contrast and contrast sensitivity. Shlaer S, Smith E, Chase A: Visual acuity and illumination in different spectral regions. Bollinger K, Sjoberg S, Neitz M, Neitz J: Topographical cone photopigment gene expression in deutan-type red-green color vision defects. Neitz M, Neitz J: A new mass screening test for color-vision deficiencies in children. Neitz M, Carroll J, Renner A, et al: Variety of genotypes in males diagnosed as dichromatic on a conventional clinical anomaloscope. Carroll J, Neitz M, Neitz J: Testing hypotheses about visual pigments underlying deutan color vision. Winderickx J, Battisti L, Hibibya Y, et al: Haplotype diversity in the human red and green opsin genes: evidence for frequent sequence exchange in exon 3. Neitz M, Neitz J, Grishok A: Polymorphism in the number of genes encoding longwavelength sensitive cone pigments among males with normal color vision. Carroll J, McMahon C, Neitz M, Neitz J: Flicker-photometric electroretinogram estimates of L: M cone photoreceptor ratio in men with photopigment spectra derived from genetics. Carroll J, Neitz M, Hofer H, et al: Functional photoreceptor loss revealed with adaptive optics: an alternate cause of color blindness. Hofer H, Carroll J, Neitz J, et al: Organization of the human trichromatic cone mosaic. Second, in most cases it permits a quantitative assessment of the degree of malfunction that can be followed up over time for the purpose of projecting long-term prognosis or evaluating a prospective treatment. Third, outcomes from these measures may be shown to the patient as variations in fundus reflectance or as waveforms on photographs or paper so that the patient can appreciate the type and magnitude of his or her visual malfunction and thereby actively participate with the ophthalmologist in the initial and follow-up examinations. The first three methods, though not measures of function per se, are always presented in the context of measures of function in interpreting hereditary retinal disease. Guidelines are presented for obtaining reliable and reproducible results and, in some cases, for interpreting variations within a single session and between visits in a given patient as well as differences that may exist among normal subjects. The difference in the reflected light before and after the bleaching episode provides a measure of the amount of visual pigment. Density differences are then quantified by comparing unbleached with bleached areas captured in a single image11,12 or between successive images. For assessing rhodopsin density, the mid-peripheral fundus, in which cone photoreceptors are scarce, is generally chosen. For assessing cone pigment density, the fovea, in which rods are fewest, is chosen.
Buy meloxicam 7.5 mg overnight delivery
The program is accredited by the National Commission for Certifying Agencies and has certified over 800 individuals to date rheumatoid arthritis signs 7.5 mg meloxicam visa. The responsibility for injecting the dye sometimes falls to the angiographer or a technician. There are however, some legal issues associated with unlicensed personnel performing fluorescein injections. A thorough understanding of the circulation phases and appearance of the dye in a normal eye is essential for interpretation of abnormalities. The tight junctions of the endothelial cells in normal retinal capillaries make them impermeable to fluorescein leakage. Additional anatomical features contribute to the interpretation of the fluorescein angiogram. The choriocapillaris is the capillaryrich layer of the choroid characterized by fenestrated capillary walls that leak fluorescein dye freely into the extravascular space within the choroid. In the posterior fundus, the choriocapillaris is arranged in a mosaic of lobules that contributes to the patchy choroidal fluorescence often seen in the early phases of the angiogram. Choroidal flush In a normal patient, the dye appears first in the choroid ~10 s following injection. The major choroidal vessels are impermeable to fluorescein, but the choriocapillaris leaks fluorescein dye freely into the extravascular space. A delay in the arm-to-retina time may reflect a problem with the fluorescein dye injection or circulatory problems with the patient including heart and peripheral vascular disease. Arteriovenous phase Complete filling of the retinal capillary bed follows the arterial phase and the retinal veins begin to fill. This finding, along with the presence of xanthophyll pigment and taller, more pigmented retinal pigment epithelial cells, contributes to the relative hypofluorescence of the macula. Complete filling of the veins occurs over the next 10 s with maximum vessel fluorescence occurring ~30 s after injection. The perifoveal capillary network is best visualized in the peak venous phase of the angiogram. When present, cilioretinal arteries fill along with the choroidal flush since both are supplied by the short posterior ciliary arteries. The arteriovenous phase of the angiogram comprises the time when the retinal arteries, capillaries, and veins contain fluorescein. In the early arteriovenous phase, thin columns of fluorescein are visualized along the walls of the larger veins (laminar flow). As the fluorescein dye begins to exit from the retinal arteries and capillaries, the concentration of fluorescein within the veins increases, resulting in a decrease in fluorescence of the arteries and an increase of fluorescence of the veins. The intensity of fluorescence diminishes slowly during this phase as fluorescein is removed from the bloodstream by the kidneys. The late phase of the angiogram demonstrates the gradual elimination of dye from the retinal and choroidal vasculature. Any other areas of late hyperfluorescence suggest the presence of an abnormality, usually the result of fluorescein leakage. Hypofluorescence is caused by either blockage of the normal fluorescence pattern or abnormalities in choroidal or retinal vascular perfusion. Blocked fluorescence Blocked fluorescence is most commonly caused by blood but can result from the deposition of abnormal materials such as lipid exudate, lipofuscin, xanthophyll pigment, or melanin pigment. Fluorescein angiography is very helpful in determining the anatomic location of the blocking material, which in turn, is important in identifying the etiology of the abnormality. Abnormal vascular perfusion Abnormal vascular perfusion results in hypofluorescence of the retinal and/or choroidal circulation depending on the location of the abnormality. Common causes of retinal hypoperfusion include retinal arterial and venous occlusions and ischemic disease due to diabetes and other causes. Choroidal hypoperfusion may be produced by ophthalmic artery occlusion, giant cell arteritis, and hypertensive choroidopathy. It is important to understand the relationship between hypofluorescence due to filling defects and the specific phase of the angiogram. These are descriptive terms that refer to the time specific, relative brightness of fluorescence in comparison with a normal study (Table 128. Hypofluorescence Key Features Hypofluorescence is usually caused by the blockage of normal fluorescence or abnormal vascular perfusion. Autofluorescence and pseudofluorescence are terms to describe the appearance of apparent hyperfluorescence in the absence of fluorescein. Autofluorescence Autofluorescence refers to recordable hyperfluorescence that is believed to occur naturally in certain pathologic entities such as optic nerve drusen and astrocytic hamartomas. The ability to visualize the retinal circulation overlying the blocking defect confirms the subretinal location of the hemorrhage. Note that there are scattered patches of more prominent hypofluorescence from intraretinal hemorrhages. Pseudofluorescence Pseudofluorescence occurs as a result of crossover in the spectral transmission curves of the exciter and barrier filters. If too much crossover is present, reflectance from bright fundus structures will not be fully blocked by the barrier filter. Modern interference filters rarely exhibit significant crossover unless they have deteriorated. Control photographs are routinely taken before injection of fluorescein to detect the possible presence of pseudofluorescence. Transmission defect Depending on the density of retinal pigmentation, background fluorescence from the choroid can be visible as hyperfluorescence in the angiogram. It is important to differentiate hyperfluorescence due to transmission defects from leakage. The hyperfluorescence usually appears early in the angiogram and is not associated with leakage in the late phase. Leakage 1698 Leakage refers to hyperfluorescence in the angiogram due to extravasation of fluorescein dye. The phenomenon of hyperfluorescence related to fluorescein leakage is demonstrated in this patient with diabetic retinopathy. This pair of images demonstrates fluorescein leakage from exudative age-related macular degeneration. For example, fluorescein leakage is seen in eyes with choroidal neovascularization related to age-related macular degeneration. Staining Staining refers to late hyperfluorescence resulting from the accumulation of fluorescein dye into certain tissues. Normal staining can occur in the optic nerve and sclera as a result of normal choroidal leakage. Retinal neovascularization is characterized by profuse leakage on fluorescein angiography. The areas of retinal neovascularization usually are located at the junction of the perfused and nonperfused retina. A number of additional diagnostic imaging procedures serve as an adjunct to angiography. Monochromatic fundus photography with other colors of light has been used for decades, but is probably underutilized given its inherent value. In the early to mid 1990s, enthusiasm for this procedure exceeded its practical applications. In 1925, Vogt described the use of green light to enhance the visual contrast of anatomical details of the fundus.
Purchase 15 mg meloxicam with amex
However arthritis in dogs symptoms uk best buy meloxicam, visual field defect and night blindness that may appear out of proportion to fundus changes may be noted. Histologically, there is chronic nongranulomatous chorioretinitis with eosinophilic infiltration and necrosis of the retina and pigment epithelium. Centers for Disease Control and Prevention: Outbreak of leptospirosis among white water rafters: Costa Rica, 1996. Rabinowitz: Bilateral multifocal choroiditis with serous retinal detachment in a patient with Brucella infection: case report and review of the literature. Ishibashi Y, Watanabe R, Hommura S, et al: Endogenous Nocardia asteroides endophthalmitis in a patient with systemic lupus erythematosus. Barquet N, Gasser I, Domingo P, et al: Primary meningococcal conjunctivitis: report of 21 patients and review. Brownstein S, Mahoney-Kinsner J, Harris R: Ocular Candida with pale-centered hemorrhages. Macular Photocoagulation Study Group: Argon laser photocoagulation for ocular histoplasmosis: results of a randomized clinical trial. Macular Photocoagulation Study Group: Krypton laser photocoagulation for neovascular lesions of ocular histoplasmosis: results of a randomized clinical trial. Colin J, Prisant O, Cochener B, et al: Comparison of the efficacy and safety of valaciclovir and acyclovir for the treatment of herpes zoster ophthalmicus. Hertzberg R: Twenty-five-year follow-up of ocular defects in congenital rubella syndrome. Silveira C, Belfont R, Burnier M, et al: Acquired toxoplasmic infection as a cause of toxoplasmic retinochoroiditis in families. Silveira C, Belfont R, Nussenblatt R, et al: Unilateral pigmentary retinopathy associated with ocular toxoplasmosis. Thorne Birdshot chorioretinopathy is an uncommon chronic posterior uveitis characterized by vitritis and multiple ovoid, hypopigmented spots concentrated in the posterior pole and midperiphery of the retina. Although birdshot retinochoroidopathy has been a common nomenclature used to label this disease, birdshot chorioretinopathy is more consistent with what is thought to be the primary location of the inflammatory lesions, the choroid. Enumeration of autoreactive helper T-cells in patients with birdshot reveals a frequency of between four and seven S-Ag-specific T-cells/106 peripheral blood lymphocytes. These data support a role for an autoimmune mechanism in birdshot chorioretinopathy. In one report, an enucleated, phthisical eye from a patient diagnosed with birdshot chorioretinopathy in the other eye revealed a mild lymphocytic infiltration of the iris and ciliary body. The underlying choroid had a milder granulomatous infiltration that was thought to be a secondary response. However, this patient had a history of trauma and lens subluxation in the eye that was not enucleated and this, combined with the granulomatous inflammation largely confined to the retina has made many experts question the diagnosis. In fact, the clinical findings of this case appear to be more consistent with sympathetic ophthalmia. A second case of birdshot chorioretinopathy examined at autopsy has been reported by Gaudio and colleagues. Focal lymphocytic inflammation was observed in the choroid and adjacent to choroidal vessels accompanied by milder inflammation in the retina along the retinal blood vessels and around the optic disk. The pooled mean age of patients with birdshot chorioretinopathy obtained from 512 patients reported in 39 articles published in the English literature through 2002 was 53 years + 9. The larger lesions may become confluent and result in geographic depigmentation or even produce a blonde appearance to the fundus. A rare patient may develop fine pigmentary changes in the sensory retina or around retinal vessels. These lesions typically are located in the postequatorial fundus and often assume a radial orientation. Blurred vision (present in up to 88% of patients) and floaters (present in up to 66% of patients) appear to be the most common symptoms experienced by patients with birdshot chorioretinopathy, even in those patients who present to the ophthalmologist with 20/20 visual acuity. Subretinal neovascular membrane formation in a patient with birdshot chorioretinopathy. The most prominent finding observed on fluorescein angiography is leakage of fluorescein dye from the retinal vessels and capillaries. Birdshot lesions, which may be distinctive on fundoscopic examination, do not typically block the underlying choroidal phases of the fluorescein angiogram and show minimal hyperfluorescence and staining in the latter phases of the study. The sensitivity, specificity, and positive predictive value of these criteria for the diagnosis of birdshot chorioretinopathy was 97. They are smaller and whiter than birdshot lesions and, as indicated in the name, are evanescent. Multifocal choroiditis and panuveitis syndrome is a white-dot syndrome of the retina that can present with multifocal fundus lesions and vitritis. Intraocular lymphoma may present with fundus lesions which typically are subretinal yellow infiltrates primarily located in the posterior pole. Approximately 50% of patients will have central nervous system involvement at the time of diagnosis of intraocular lymphoma. Infectious forms of uveitis, such as tuberculosis and syphilis, can present with vitritis and light-colored lesions of the fundus. Skin rashes, malaise, night sweats, and pulmonary symptoms may suggest the presence of a systemic infection. Patients with sarcoidosis also may present with a diffuse uveitis with white dots of the fundus. The presence of hilar lymphadenopathy on chest radiograph supports the diagnosis of sarcoidosis. Fundus white dots are not typical in pars planitis, though retinal vasculitis may occur. Other white dot syndromes should be distinguished from birdshot chorioretinopathy. Fluorescein angiography shows a distinctive pattern of early blocking and late hyperfluorescence in these lesions. However, a growing number of reports suggest that patients with birdshot chorioretinopathy have progressive loss of visual function in the absence of clinically active inflammation and central visual acuity loss. A growing body of evidence suggests that birdshot chorioretinopathy is a chronic, progressive disease;22,33,54 however, it is unknown when aggressive treatment must be instituted in order to prevent loss of visual function. Note the resolution of vitreous cells in the color photographs and the improvement in retinal edema and retinal vasculitis after this therapy. The best method of monitoring patients with birdshot chorioretinopathy has not been established, although it appears that monitoring for central visual acuity loss and clinical signs of intraocular inflammation alone is insufficient. Data from a prospective cohort study of patients with birdshot chorioretinopathy24 may help to establish superior treatment and monitoring algorithms for these patients. Patients may complain of ocular symptoms such as blurred vision, floaters, and difficulties with night vision, despite objectively normal visual acuity on examination. When to institute immunosuppressive drug therapy and how to effectively monitor this disease over long-term follow-up has yet to be established. LeHoang P, Girard B, Deray G, et al: Cyclosporine in the treatment of birdshot retinochoroidopathy. It is characterized by bilateral granulomatous uveitis associated with exudative retinal detachment and with extraocular manifestations including pleocytosis of the cerebrospinal fluid, and in some cases, dysacusis, poliosis, alopecia, and vitiligo. No history of penetrating ocular trauma or surgery preceding the initial onset of uveitis 2. Bilateral ocular involvement (a or b must be met, depending on the stage of disease when the patient is examined) a. Early manifestations of disease (i) evidence of diffuse choroiditis (with or without anterior uveitis, vitreous inflammatory reaction, or optic disk hyperemia) which may manifest as (a) focal areas of subretinal fluid, or (b) bullous serous retinal detachments b. Meningismus (malaise, fever, headache, nausea, abdominal pain, stiffness of the neck and back, or a combination of these factors); note that headache alone is not sufficient to meet the definition of meningismus b. Integumentary finding (not preceding onset of central nervous system or ocular disease) a.
Generic meloxicam 7.5 mg line
An optimized model can then be used prospectively to design and evaluate patientspecific treatment algorithms (2) rheumatoid arthritis in 20s buy meloxicam 15 mg fast delivery. Extensiometry experiments illustrating elastic and viscoelastic behavior in a 7-mm, full-thickness horizontal corneal strip from a 63-year-old donor. In the experiment on the right, the same sample is maintained at a constant displacement and load is measured over time to generate a stress relaxation curve. Hydrophilic stromal glycosaminoglycans generate a negative intrastromal fluid pressure under which the entire stroma is compressed. The swelling pressure is further resisted by tear film evaporation, the epithelial and endothelial barriers and active endothelial transport. In a simple elastic shell model, this elastic weakening results in a forward herniation that, if considered alone, would result in corneal steepening. In practice, this hyperopic response dominates when ablation is limited to the anterior stroma; deeper circumferential insults may ultimately cause net corneal steepening. It should also be clear from the above discussion that a nonlinear function does not allow definition of a single modulus value, but instead requires its definition as a function of load or as a mean value over a specified loading interval. Despite its limitations, extensiometry has revealed important deficits in elastic tensile strength in keratoconus28 and remains the standard for ex vivo elastic modulus determination. Second International Conference on the Ultrasonic Measurement and Imaging of Tissue Elasticity. In clinical practice, biomechanical flattening augments the effects of a myopic procedure and impedes efforts to correct hyperopia. This is supported by the observation that large overcorrections must be attempted to treat high levels of primary hyperopia. This difference in efficacy can be attributed to the considerable differences between the loadbearing characteristics of virgin corneas and corneas that have been altered by previous surgery. The flap and stromal bed responses to flap creation may depend on the flapcreation technology used. The meniscus-shaped flaps produced by most mechanical microkeratomes have less consistent dimensions and may exacerbate the hyperopic stromal bed response by disrupting an unpredictable number of additional lamellae in the mid-periphery. Femtosecond lasers, which allow more precise specification of flap morphology, could potentially reduce the astigmatic effects of flap creation and improve nomogram quality by reducing patient-to-patient variability. Staged procedures incorporating a re-measurement delay after flap creation44,45 have been investigated as a means of accounting for the separate effects of flap creation and photoablation. This approach is advocated most often in the setting of postkeratoplasty ametropia and astigmatism, where the biomechanical and wound healing responses to flap creation can be quite unpredictable. Complex structures like the cornea can be divided into a mesh of representative geometries (finite elements) with their own material properties. Creating an appropriate mesh with representative material properties is critical to accurate simulation. All models are exquisitely sensitive to errors in specified material properties, particularly the elastic modulus,22,50 and will benefit from improved techniques for measuring properties in individual patients. Instead, central steepening of the posterior corneal surface may reflect a relative posterior movement of the peripheral stroma in response to the differential swelling described previously. Lower keratocyte density, less collagen interweaving and more hydrophilic proteoglycans may all contribute to a propensity to viscoelastic failure and abnormal repair. Another is to model the risk of ectasia based on measurable geometric and material properties in individual refractive surgery candidates. Biological diversity in this response is the norm, even in contralateral eyes of the same patient. As such, it is a major variable contributing to refractive overcorrection, undercorrection and regression as well as induced astigmatism and haze formation. Though presented in the form of a linear cascade for simplicity, the interactions are complex, often occur simultaneously and are influenced by other factors not discussed here. The corneal nerves, lacrimal glands and tear film are also important participants. This injury, which may result from microkeratome or femtosecond lasermediated tissue disruption, alcohol exposure or a mechanical scrape, is followed by release of cytokines from the injured epithelium and epithelial basement membrane. Disruption of the epithelial barrier potentiates the effects of epithelial and lacrimal cytokines by providing enhanced access to the stroma. Increasing numbers of keratocytes undergo the more proinflammatory process of necrosis following the initial wave of apoptosis. These cells, which arrive through the limbal blood supply and the tear film,70 participate in phagocytosis of apoptotic and necrotic debris and may serve other functions within the stroma. Though described as a cascade, many of the components noted here occur simultaneously or overlap temporally. In most cases, epithelial injury by scrape, incision, laser exposure or other mechanism is the inciting event of corneal wound healing, although direct injury can be induced using modalities such as intrastromal femtosecond laser ablation. The earliest stromal change observable after epithelial injury is the nearly instantantaneous programmed cell death (apoptosis) of underlying keratocytes. Within hours, residual stromal keratocytes begin to undergo proliferation and migration to repopulate areas of reduced stromal cellularity. The earliest mitosis in a cornea with a scrape injury is seen in the peripheral and posterior cornea. Thousands of bone marrow-derived cells also migrate into the cornea in the first hours after injury. The primary role of these cells appears to be phagocytosis of dead cells and other debris, but these cells may have additional functions that have yet to be characterized. Depending on the type and extent of injury, myofibroblast cells may be generated in the cornea. According to current dogma, these cells are derived from keratocytes that proliferate to form stromal fibroblasts which then, under the influence of transforming growth factor beta and other cytokines, differentiate into myofibroblasts. However, recent studies have demonstrated that myofibroblasts in skin110 and lung111 are actually derived from bone-marrow derived cells. Further work is needed to determine the origin or origins of myofibroblasts in the cornea. When they do develop, myofibroblasts typically arise in stroma near the surface epithelium or near ectopic epithelium within stromal incisions where the requisite cytokines for development are produced. Recent studies have demonstrated that surface irregularity71 as well as associated abnormalities of the regenerated basement membrane71,74 are important factors in myofibroblast generation. Important species-related differences in the tendency to generate myofibroblasts also exist. Rabbits are much more prone to development of myofibroblasts and corneal haze than humans and mice. These cells, known as myofibroblasts, appear in quantities that depend on the level of correction, surface irregularity and other factors. Myofibroblasts are, therefore, key effectors of corneal haze formation and regression due to stromal collagen and extracellular matrix remodeling. The delicate balance between stromal regeneration and fibrosis depends in large part upon the activity of these cells. Restoration of the epithelial basement membrane promotes the nonfibrotic myofibroblast phenotype74,75 and is, therefore, an important event in suppressing haze formation. Myofibroblasts, when present, typically reach maximum density within the first few months of the surgical insult and then slowly disappear over the ensuing weeks. The contributions of the stroma and the epithelium to regression depend on postoperative time, type of refractive surgery, whether treatment was directed at hyperopia or myopia and other factors. For example, undiagnosed epithelial hyperplasia that persists to the 3 or 6 month postoperative visits could mimic residual refractive error; if an enhancement surgery is performed, resolution of the hyperplasia will ultimately lead to an overcorrection. Many cases of clinically significant haze improve without intervention, even after one postoperative year. Failure on the part of the posterior keratocytes to generate sufficient resistance to stress relaxation and viscoelastic creep could be a factor in ectasia.
Buy meloxicam 7.5mg with visa
Therapy with penicillin arthritis diet express buy on line meloxicam, tetracycline, or doxycycline is effective for systemic disease. It includes a low-grade fever, arthralgia, lymphadenopathy, and hepatosplenomegaly. Infections of the lung, bone, kidney, central nervous system, and heart are rare but serious complications. The ocular manifestations that have been reported include acute or chronic granulomatous and nongranulomatous uveitis, nummular keratitis, and optic neuritis. The uveitic component of brucellosis is thought to be a noninfectious immune response. If there are severe neurologic abnormalities or ocular inflammation, intravenous penicillin G or ceftriaxone is used. Topical corticosteroids may be used for uveitis, although the beneficial role of systemic or periocular steroid therapy is still controversial. Between 20% and 50% of the cases of nocardiosis are seen in otherwise healthy patients, but the disease is usually more prevalent in patients who are immunocompromised or on antimicrobial therapy. The clinical manifestations can range from a mild iridocyclitis to severe panophthalmitis. In such cases, keratoconjunctivitis, corneal ulcer, scleritis, and dacryocystitis may also be noted. Although human infection is rare, there have been multiple epidemic outbreaks around the world. Uveitis is also common (up to 45%) and typically occurs several weeks to months after the febrile phase of the disease. If immune compromise is present, combination therapy of a sulfonamide with a third-generation cephalosporin or imipenem is advised. Although primary infection usually occurs in the lung, the eye can also be the initial port of entry. Primary infection in the eye typically presents as corneal, conjunctival, and scleral disease. The most common ocular manifestation is a chronic granulomatous iridocyclitis that is usually bilateral. In addition to multifocal choroiditis, serpinginous-like choroiditis has been reported with increasing frequency. Tuberculosis cannot be ruled out even if all above tests are negative, and a high clinical suspicion can be useful in assisting the diagnosis. Patients who have been inadequately treated with isoniazid and rifampin can develop antibiotic-resistant tuberculous uveitis. The organism spreads from the lungs to the rest of the body through the blood stream. The result is a sudden onset of fever, lethargy, cutaneous purpura, meningitis, and ocular infection. Intraocular infection can result in acute fulminant endophthalmitis, which may be bilateral or unilateral. Among patients with severe intraocular infection or with evidence of systemic infection, intravenous amphotericin B may be used in conjunction with local therapy. However, the drug has fairly low ocular penetration when administered systemically even in the presence of ocular inflammation. Oral fluconazole has been shown to have excellent ocular penetration with few systemic side effects. Systemic administration of voriconazole (oral or intravenous) has also been shown to be effective in treatment of ocular candidiasis. Vitrectomy may be useful in some patients with severe vitritis or endophthalmitis. It is usually seen in intravenous drug abusers in large cities and in hospitalized patients who are receiving widespread antibiotic therapy or hyperalimentation, have had abdominal surgery, or have had an indwelling intravenous catheter for a prolonged period of time. Hematogenous dissemination of the fungus can affect heart valves, the central nervous system, eyes, and other organs. Since in two studies, 37% of patients who died of systemic infection had eye involvement and 78% of patients with candida endophthalmitis were found to have systemic infection on autopsy, ocular infection is a useful diagnostic sign in distinguishing candidemia from systemic candidiasis. The earliest lesions are in the retina or inner choroid; they are similar in appearance to lesions resulting from Aspergillus infection. Photomicrograph of the retina in a patient with chorioretinitis secondary to Candida albicans. A necrotizing lesion adjacent to the macula in an intravenous drug abuser with Candida chorioretinitis. Retinal hemorrhages, multifocal choroiditis, choroidal granuloma, retinitis, vitritis, and endophthalmitis have all been reported. Patients may present with visual loss and an enlarged blind spot from acute disk swelling. The histoplasmin skin test is not recommended because it is not diagnostic and can aggravate the macular lesion. Patients who develop extrafoveal or juxtafoveal subretinal neovascularization are candidates for argon or krypton photocoagulation. The infection is more common in people who are immunocompromised or have chronic debilitating disease. Approximately 6% of the patients with cryptococcal meningitis have ocular complications. Intraocular infection can also occur either hematogenously or by direct spread from intracranial sites. There is one report of a solitary vitreoretinal abscess in a patient with cryptococcosis. Aspergillus fumigatus endophthalmitis (proven at autopsy) in a patient who had recovered from miliary tuberculosis. Histologically, there is usually acute and granulomatous inflammation, but the inflammation may be minimal in immunosuppressed patients. A positive cryptococcal titer on examining the cerebrospinal fluid may be used to initiate antifungal therapy. The primary infection, pulmonary coccidioidomycosis, is asymptomatic or associated with a mild respiratory infection. Although there is an association between disseminated disease and immunosuppression, most of the patients are previously healthy individuals. Treatment is reserved for patients with severe disseminated disease, especially if there is ocular involvement. It begins in the retina and spreads to involve the choroid, vitreous, and ciliary body. Multifocal yellow-white lesions of the choroid with retinal necrosis and vitritis are seen. The organism grows rapidly in culture, and diagnosis can be made by isolating the organism from ocular fluid or tissue. The treatment of choice is pars plana vitrectomy and intravitreal amphotericin B injection. Systemic combination therapy of the newer antifungal agents voriconazole and capsofungin has been shown to be effective in treating infections that are resistant to amphotericin B. The infection may spread to skin, lung, and bone via the blood stream and result in disseminated abscesses. Up to 30% of the patients have central nervous system involvement, and these patients uniformly have poor survival. It can result from either hematogenous dissemination or direct extension from the eyelid or face. The most common finding is an anterior uveitis sometimes associated with iris nodules or ciliary body abscesses. Font and co-workers reported a case of endogenous panophthalmitis from blastomycosis.
Buy meloxicam without prescription
Hirvela H early onset arthritis in neck purchase 7.5 mg meloxicam amex, Luukinen H, Laatikainen L: Prevalence and risk factors of lens opacities in the elderly in Finland: a population-based study. Sasaki K, Shibata T, Obazawa H, et al: Classification system for cataracts: application by the Japanese Cooperative Cataract Epidemiology Study Group. Sasaki K, Sakamoto Y, Shibata T, et al: the multi-purpose camera: a new anterior eye segment analysis system. Hockwin O, Dragomirescu V, Laser H: Measurements of lens transparency or its disturbances by densitometric image analysis of Scheimpflug photographs. Lerman S, Hockwin O: Automated biometry and densitography of anterior segment of the eye. Hockwin O, Lerman S, Ohrloff C: Investigations on lens transparency and its disturbances by microdensitometric analyses of Scheimpflug photographs. Khu P, Kashiwagi T: Quantitating nuclear opacification in color Scheimpflug photographs. Hockwin O, Laser H, Kapper K: Image analysis of Scheimpflug negatives: comparative quantitative assessment of the film blackening by area planimetry and height measurements of linear densitograms. Douvas N, Allen L: Anterior segment photography with the Nordenson retinal camera. Kawara T, Obazawa H: A new method for retroillumination photography of cataractous lens opacities. Miyauchi A, Mukai S, Sakamoto Y: A new analysis method for cataractous images taken by retroillumination photography. Sakamoto Y, Rankov G, Sasaki K: Comparison of retroillumination images of crystalline lenses taken with different camera types. Kuroda T, Fujikado T, Maeda N, et al: Wavefront analysis of higher-order aberrations in patients with cataracts. Kuroda T, Takashi F, Maeda N, et al: Wavefront analysis in eyes with nuclear or cortical cataract. The first written description of couching came from Susruta (also spelled Sushruta), an ancient Indian surgeon (c. If the patient then recognizes forms, the lancet is slowly withdrawn and molten butter is put on the eye. The patient sat with her or his face illuminated by the midday sun streaming in from a window. A pointed needle was plunged either through the sclera ~4 mm temporal to the limbus or through clear cornea. The relative safety of this retro-iris position probably was the major reason why the couching operation remained in vogue up through the nineteenth century. The ultimate intraoperational test of success was when the patient reported that she or he could begin to see forms again. Couching apparently was not the only method for removing the coagulated suffusion from behind the iris. Although the father of modern cataract surgery, Jacques Daviel, introduced the incisional extraction of the cataract in 1753, surgeons still extolled the virtues of couching for another 150 years. Samuel Sharp, the first surgeon to make the corneal incision in cataract extraction with a single knife: A biographical and historical sketch. Daviel faced his seated patient and made his incision at the lower limbus with a keratome. The incision was extended with scissors right and left above the level of the pupil. Between 1753 and 1862, three milestones took place that profoundly affected the direction of cataract surgery: 1. He had the patient lie on his or her back and operated from the head of the table. Samuel Sharp (1753) described surgery that introduced the subject of taking the entire lens out of the eye with the capsule intact. Albrecht von Graefe (1867) devised his long, thin, sword-like corneal knife to facilitate the corneal incision. Terson (1871) removed the cataract in toto with a spoon introduced behind the lens. This significant advancement was further endorsed by Suarez de Mendosa (1891), Eugene Kalt (1894), and Frederick Verhoeff (1916). He utilized external pressure with a muscle hook on the peripheral inferior cornea to loosen zonules. With sufficient mechanical zonulolysis, he then expressed the lens using pressure from the muscle hook creeping superiorly over the cornea. Later, Smith would describe a modification of his mechanical zonulolysis that would allow for an actual linear sliding of the whole lens without tumbling. Gentle traction coupled with side-to-side movements enabled E Kalt, G Stanculeann, and Arnold Knapp (1910) to lyse inferior zonules. Verhoeff at the Massachusetts Eye and Ear Infirmary was not satisfied with the tumbling maneuver. The forceps was designed in such a way that its tips were gentle on the capsule, thus reducing risk of capsular rupture. Because the lens was actually pulled out of the eye without tumbling and with less external pressure, vitreous loss was less of a threat. The next breakthrough came to intracapsular surgery with the development of chemical zonulolysis. Mechanical zonular destruction was first used by Christiaen (1845) and Luca (1866). Jose Barraquer (1958) demonstrated the dramatic efficacy of chemical zonulolysis using an enzyme a-chymotrypsin. The final significant improvement arrived when T Krawawicz in Poland (1961) introduced the cryoextractor. A miniature erysiphake with a small rubber suction bulb attached to the probe end. Despite the encouraging results, there remained a substantial rate of potentially blinding complications, including aphakic retinal detachment and cystoid macular edema, which could be reduced by keeping the posterior capsule intact. But the major concern was the optical rehabilitation of the aphakic patient with glasses. Few surgeons actually stuck to the technique because it was technically difficult and dangerous (high risk of corneal damage, capsular rupture, vitreous loss, and nucleus dislocation into the vitreous). The procedure also failed to catch on because a primary capsulotomy was taught, thus negating the advantage of compartmentalizing the anterior and posterior segments. While Kelman was developing his emulsification, John Shock (1972) introduced the alternative phacofragmentation and irrigation system. William Simcoe (1977) introduced his Simcoe curved 23-gauge cannula connected to a small irrigating bulb. Harold Scheie described a procedure for aspirating a soft congenital cataract from the eye through small incisions. He devised the technique of removing a window of anterior capsule with toothed forceps, by aspirating a soft nucleus or by expressing a hard nucleus, and by irrigating and aspirating a portion of the remaining cortex through a bent olive-tip cannula. The miotic pupil held the pedestal central until the loops stuck or scarred down to the posterior capsule. By 1977, Worst and colleagues reported on a large series of 2000 cases using this new lens. Kelman was the invited guest of national medical meetings and showed films of his revolutionary work. He conducted courses at his local New York hospital and published an instruc- History of Cataract Surgery James Gills was also leading the way in Florida by performing high-volume surgery and perfecting the Gills method (with help from Robert Welch). The Gills method was a simple manual technique of nucleus expression followed by cortical cleanup with an end-opening Gills 25-gauge cannula attached to a 3-mm syringe. His cortical cleanup in a semiclosed chamber utilized the concept of engaging the cortex in the cannula port and then wiggling and teasing the cortex free from its capsular adherence.
Cheap meloxicam 7.5 mg free shipping
Only among humans is there widespread variability in the number of visual pigment genes on the X-chromosome with a high frequency of arrays containing more than two opsin genes arthritis care diet and exercise buy meloxicam online now. Instead it is a group of disorders that can be dichotomized at the first level according to what is missing to cause the perceptual loss, and at a second level according to the degree of color vision that remains (Box 123. The degree to which color vision is impaired is determined by the spectral properties of the pigments encoded by the genes that remain. For example, in a recent study 53 of 55 protanopes lacked genes for L opsin, and 51 of 73 deuteranopes lacked genes for M opsin. In summary, the most severe red-green color vision defects, the dichromacies, are commonly explained by the straightforward deletion of cone opsin genes. Another relatively common cause is a point mutation that disrupts the function of the encoded opsin. Recent evidence indicates that there is a fundamental difference in the effects on the cone mosaic that results from these two mechanisms for color vision deficiency, specifically with regard to what happens to the subpopulation of cones that do not contribute to color vision. In the case of the singlegene dichromat, it appears that all of the cones that would have become L or M cones express the available X-chromosome opsin gene and so no cone photoreceptors are lost. In contrast, evidence indicates that in dichromats with two or more opsin genes in which the first or second gene encodes an opsin with an inactivating amino acid substitution(s), a subpopulation of photoreceptors express the mutant gene, which ultimately results in the death of the photoreceptor, giving rise to a lower than normal cone density and leaving gaps in the cone mosaic. As a result, there is tremendous variation in the amino acid sequences of the L and M cone photopigments found in humans with normal color vision. When the gaps in his mosaic were modeled as M cones and cone density recalculated taking into account the modeled cones, the density estimate was normal. Taken together, these observations support the hypothesis that in some forms of color vision deficiency, the cause is a loss of photoreceptor cells that is due to a malfunction in the production or function of the photopigment. Males who have opsin gene arrays in which the first two genes encode photopigments of the same functional class but with a difference in peak sensitivity of less than 2. As the term for their condition implies, affected individuals have trichromatic color vision, but it is not based on L, M, and S pigments like normal color vision. Referring to the photopigments underlying anomalous trichromacy according to their spectral sensitivities promotes a clearer understanding of the cause of the differences between normal versus anomalous trichromacy. The genes can be categorized as encoding an L-class or an Mclass pigment by the sequence of exon 5. Individuals with deuteranomaly lack M cones but they have two distinct classes of L-cone that are different enough in spectrum to provide the basis for limited color vision in the red-green region of the spectrum. An anomalous trichromat with a large spectral difference between the L or M cone subtypes has the basis for much better color vision than a person with two cone subtypes that are nearly identical. When color vision in the red-green region of the spectrum is mediated by cones that differ in peak sensitivity by fewer than 2. Spectral tuning of the L and M cone photopigments is achieved through amino acid substitutions at a limited number of positions. Substitutions at these positions distinguish the L-class from the M-class pigments. The yellow balls indicate amino acid positions at which substitutions produce spectral shifts, and that are responsible for variability in the absorption spectrum among the L-class, among the M-class, and between the L- and M-classes. Substitutions at the yellow positions have a relatively small effect on the absorption spectrum in comparison to the red positions. The blue balls indicate amino acid positions that are variable among L- and M-class pigments but that do not influence the absorption spectrum. In addition, tritan defects show incomplete penetrance, meaning that there is variability in the degree to which color vision is impaired among individuals with the same underlying gene defect, even within a family. That is, even among members of the same family, some individuals might exhibit a complete loss of S-cone function, whereas other members may exhibit a milder, incomplete loss. Tritan deficiencies have been associated with mutations of the S-opsin gene resulting in four different amino acid substitutions. In addition, the spectral shifts produced by the polymorphisms in the M-class pigments are relatively small compared to shifts made by the same amino acid substitutions at the corresponding positions of the L pigments. From the deduced amino acid sequences of the pigments encoded by the genes in the first two positions of the X-chromosome opsin gene array, the spectral separation of the pigments underlying color vision can be predicted. It is the large difference in spectral absorption between L and M cones that underlies the excellent color discrimination in the Visual Acuity, Adaptation, and Color Vision in the S opsin do not cause retinal degeneration. However, the absence of retinal degeneration does not imply that the S cones do not degenerate. If so, the tritan phenotype would be a function of age, reflecting a progressive loss of S cones over time. The low penetrance aspect of the disorder may simply reflect that younger observers have not yet lost enough S cones to manifest symptoms. The prevalence of inherited tritan defects have been reported to be quite low, but they may be grossly underestimated for a variety of reasons including the fact that standard color vision tests do not test for tritan defects, they are extremely difficult to test for, and the phenotype may be agedependent. The true incidence of inherited tritan defects and the ultimate fate of the S cones in affected individuals must await further experimentation. A particularly exciting prospect is the application of cutting edge imaging technologies using adaptive optics to the study of the retinal architecture in tritan subjects. Mutations in the gene encoding the alpha subunit have also been found in families with rod monochromacy, and in patients with incomplete achromatopsia. For example, most people agree that all color experience can be described using eleven basic color terms which in English are white, black, red, green, yellow, blue, brown, gray, orange, purple, and pink. Seven of the basic colorsred, green, blue, yellow, black, white, and gray-seem to be truly fundamental in that each of these sensations seem to be unique and not describable as a combination of the others. Thus, color experience can be reasonably explained as the combination of six unique sensations. The same is true of black and white if one accepts that gray is not the simultaneous sensation of black and white but rather the absence of either. The facts of our vision are that three types of cone photoreceptor are responsible for three pairs of sensations. The question is: how are the signals from the three types of receptors combined in the nervous system to yield the three opponent pathways A great deal is known about the anatomy and physiology of the visual system that can be brought to bear on that question, but many aspects of the neural circuits for coding color remain puzzling. In the task of understanding the neural operations responsible for transforming the cone signals into perception, a simplification is that of considering reduced color vision systems with fewer cone types and fewer fundamental sensations. These disorders are associated with reduced or absent cone function, denoted as incomplete and complete achromotopsia, respectively. Blue cone monochromacy is a form of incomplete achromatopsia in which affected individuals base their vision on S cones and rods, and thus have diminished capacity for all aspects of vision mediated by cones including color vision and acuity. Rod monochromacy is a form of complete achromatopsia in which vision is mediated only by rods. Blue cone monochromats who in psychophysical tests appear to have more than one class of functional cone have been reported. One example is autosomal recessive incomplete achromatopsia which has a prevalence of 5% among the Pingelapese islanders in Micronesia. The fan represents the signal that various colored lights evoke in the S, M, and L cones. In the central retina, each midget bipolar cell receives input from a single middle- (M) or long-wavelength sensitive (L) cone, and contacts a single midget ganglion cell. This one-to-one organization allows the signal from each M or L cone to be transmitted to higher brain regions. This comparison is achieved via horizontal cells that provide lateral reciprocally inhibitory interconnections between all cones. Neither will respond to stimuli, such as diffuse uniform white light, that produce activity in a cone that is equal to the average activity of its neighbors. At the ganglion cell stage, the responses of receptors has already been combined by postreceptoral circuitry to produce neurons with specialized response properties. As introduced in Chapter 111, this processing begins at the output terminal of the cone itself, the cone pedicle. Thus, at its synaptic terminal (pedicle), every cone compares the number of quanta it absorbs as opposed to the average number of quanta absorbed by its neighbors. Assuming that the potential change at the pedicle produced by a cone absorbing light is evenly balanced with the opposing input from the average of its neighbors, then, if the number of quanta absorbed by a cone is greater than the average absorbed by its neighbors, it hyperpolarizes.