Discount yasmin online
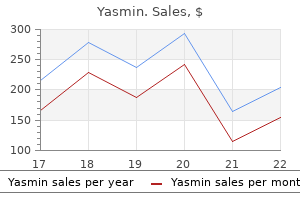
Dosing is in increments of four units which may prevent fine tuning of the meal dose birth control pills 60s cheap yasmin 3.03 mg line. It is too early to know how well this product will be accepted by patients and healthcare providers. When initiating therapy with glargine or detemir as the basal insulin, traditionally 50% of the total daily dose is given as basal insulin and the rest as prandial insulin divided equally before meals. Meal dose of insulin can be fixed, but it is better to determine the dose based on carbohydrate content of the meal. This requires learning carbohydrate counting and knowing the dose of insulin required to cover counted carbohydrates. Patients are also provided with a sliding scale (correction insulin) to use as a third component of therapy at times when blood glucose is higher than desired. Key to good control is blood glucose self-monitoring by the patient and frequent adjustment of the regimen until control is achieved. American Association of Clinical Endocrinologists and the American College of Endocrinology. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: update regarding thiazolidinediones. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Quality of life and treatment satisfaction in adults with Type 1 diabetes: a comparison between continuous subcutaneous insulin infusion and multiple daily injections. Comparative accuracy of 3 blood glucose monitoring systems that communicate with an insulin pump. Recently, continuous glucose monitors have been developed that measure interstitial glucose levels every few minutes and are used in conjunction with insulin pumps. Type 2 Diabetes About 85% patients with type 2 diabetes will require insulin at one time. Adding basal coverage is the first step and prandial coverage is added later (either at all meals or at the largest meal first). Premixed insulin combination can be used twice a day (before breakfast and dinner) with success in some patients, especially if lunch is skipped. Gestational Diabetes In patients with gestational diabetes, insulin therapy is indicated when exercise and nutritional therapy are ineffective in controlling prandial and fasting blood glucose levels. Basal therapy alone may be sufficient, but often multiple daily injections are required. Relation of glycemic control to diabetic microvascular complications in diabetes mellitus. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Although the metabolic derangement has direct effects on the neurons and support cells of the retina, the retinal vascular changes dominate the clinical manifestations of disease and are directly implicated in the macular edema and neovascularization that represent the principal causes of vision loss. Diabetic retinopathy is classified into nonproliferative and proliferative stages. Over time they sometimes become acellular, just as damaged retinal capillaries can evolve into "ghost" vessels devoid of endothelial cells and pericytes. Possible contributing factors may include alterations in the retinal microenvironment from metabolic effects on neurons, glial cells, and endothelial cells; endothelial cell injury secondary to leukostasis from altered interaction between endothelial cells and leukocytes; response of endothelial cells to altered balance between proliferative and antiproliferative factors; structural changes in the capillary wall (such as from loss of pericytes); or increase in intraluminal pressure. Microaneurysms visualized by ophthalmoscopy or angiography commonly appear and disappear over time, though some retain a stable appearance for years. The presence of microaneurysms alone, in the absence of other features of diabetic retinopathy, remains compatible with normal vision. However, as the number of microaneurysms increases, there is a greater risk of retinopathy progression. Chapter 48 (Diabetic retinopathy: Genetics and etiologic mechanisms) reviews what we know about the early biochemical and cellular alterations leading to diabetic retinopathy, while Chapter 47 (The epidemiology of diabetic retinopathy) discusses the incidence and prevalence of retinopathy. Visualized clinically by angiography, leakage may arise from microaneurysms, retinal capillaries, or other microvascular abnormalities, and can be highly variable in magnitude and extent. Retinal vascular incompetence may or may not result in localized areas of thickening of the retina. Hard exudates, extravascular deposits of lipid-rich material that result from spillage and incomplete resorption of plasma lipoproteins, may accumulate. Intraretinal hemorrhages appear in the posterior pole and in the retinal periphery. It can occur in areas of demonstrable retinal vascular incompetence, as visualized by angiography, and also in regions of retinal ischemia. In areas of capillary nonperfusion on angiography, retinal thickening may result from ischemia in the absence of prominent vascular leakage, though hyperpermeable microvascular abnormalities at the borders of such regions may contribute to swelling. In some cases, usually in the setting of severe thickening involving the fovea, subretinal fluid may also be present. In some eyes, it can persist for years, while in others it may spontaneously resolve. For example, there is evidence that the vitreous may function as an important regulator of intraocular oxygen tension, a finding that could have important implications for diabetic retinopathy and other diseases involving retinal hypoxia. Such factors are presented briefly here and discussed in greater detail in Chapter 47 (The epidemiology of diabetic retinopathy). Pertinent medical history is sought from the patient, and supplemented by records from his or her primary care physician or endocrinologist as warranted. CapillaryClosure,MicrovascularRemodeling, andRetinalIschemia One of the most serious consequences of diabetic retinopathy is progressive loss of functional retinal capillaries. Regions of acellular capillaries in histologic sections have been shown to correspond to areas of capillary nonperfusion visualized by fluorescein angiography. It has been difficult to determine whether such vessels represent altered preexisting capillaries or neovascularization within the retina. Occasionally, in cases of extensive capillary nonperfusion, the retina acquires a featureless appearance with a relative dearth of visible vessels, hemorrhages, or microvascular abnormalities. Cross-sectional and longitudinal analyses from population-based epidemiologic studies have established the association between prevalence of retinopathy and duration of disease. Epiretinal membrane formation, arising from liquefaction of the vitreous gel and consequent effects at the vitreoretinal interface, can occur with advancing age in otherwise healthy eyes but is more common in diabetic eyes. The observational studies have demonstrated that greater hyperglycemia is associated with increased prevalence and severity of diabetic retinopathy. In patients without retinopathy at enrollment, the 3-year risk of developing retinopathy was reduced by 75% in the intensive insulin treatment group compared with the conventional treatment group. The benefit of better glycemic control was also evident in patients with existing retinopathy at baseline, as shown by a 50% reduction in the rate of progression of retinopathy compared with controls. At the 6- and 12-month visits, more intensive insulin treatment exerted a small adverse effect on retinopathy progression, similar to that described in other trials of glycemic control. However, among eyes with little or no retinopathy at the time of initiating better control of hyperglycemia, it was found that such "early worsening" of retinopathy was unlikely to threaten vision. This represented a fivefold increase in risk of progression for patients with HbA1C around 10% compared with those with HbA1C around 7%. After 12 years, the rate of retinopathy progression was reduced by 21% and the use of laser photocoagulation was reduced by 29% in those getting intensive glycemic control compared with those getting conventional treatment. A subset including 2856 participants was evaluated for progression of retinopathy by comparison of fundus photographs taken at baseline and at 4 years. The glycemia trial, performed alongside other studies evaluating control of blood pressure and plasma lipids, was halted early at a median of 3. A subset of 1263 participants in the blood pressure trial was evaluated for progression of retinopathy just as in the glycemia arm of the study, with comparison of fundus photographs at baseline and 4 years. The severity of retinal hard exudates was also a significant risk factor for moderate visual loss during the course of the study.
Discount 3.03mg yasmin amex
Four-year incidence and progression of diabetic retinopathy and macular edema: the Los Angeles Latino Eye Study birth control xojane buy yasmin 3.03mg amex. Unchanged incidence of severe retinopathy in a population of type 1 diabetic patients with marked reduction of nephropathy. The 30-year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Changes in visual impairment prevalence by period of diagnosis of diabetes: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. The 25-year incidence of visual impairment in type 1 diabetes mellitus: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. The association of atherosclerosis, vascular risk factors, and retinopathy in adults with diabetes: the Atherosclerosis Risk in Communities Study. The relation of atherosclerotic cardiovascular disease to retinopathy in people with diabetes in the Cardiovascular Health Study. Prevalence of diabetic retinopathy in adult Latinos: the Los Angeles Latino Eye Study. Native American ancestry is associated with severe diabetic retinopathy in Latinos. Incidence of end-stage renal disease in type 2 (non-insulin-dependent) diabetes mellitus in Pima Indians. Retinopathy in Pima Indians: relationships to glucose level, duration of diabetes, age at diagnosis of diabetes, and age at examination in a population with a high prevalence of diabetes mellitus. Longitudinal studies of incidence and progression of diabetic retinopathy assessed by retinal photography in Pima Indians. Prevalence and risk factors for diabetic retinopathy in the multiethnic population of Mauritius. Clustering of long-term complications in families with diabetes in the Diabetes Control and Complications Trial. Familial clustering of diabetic retinopathy in South Indian Type 2 diabetic patients. Evaluating the role of epigenetic histone modifications in the metabolic memory of type 1 diabetes. The association of previously reported polymorphisms for microvascular complications in a meta-analysis of diabetic retinopathy. HbA1c variability as an independent risk factor for diabetic retinopathy in type 1 diabetes: a German/Austrian multicenter analysis on 35,891 patients. Residual insulin production, glycaemic control and prevalence of microvascular lesions and polyneuropathy in longterm type 1 (insulin-dependent) diabetes mellitus. Significance of residual insulin production in long-term type I diabetes mellitus. The effect of residual beta-cell function on the development of diabetic retinopathy. The relationship of C-peptide to the incidence and progression of diabetic retinopathy. Insulin and risk of diabetic retinopathy in patients with type 2 diabetes mellitus: 84. Estimating the delay between onset and diagnosis of type 2 diabetes from the time course of retinopathy prevalence. The absence of a glycemic threshold for the development of longterm complications: the perspective of the Diabetes Control and Complications Trial. Glycosylated hemoglobin and the risk of retinopathy in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy. Effect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. Prevalence of diabetic retinopathy: a population study from the Swedish island of Gotland. Kidney and eye diseases: common risk factors, etiological mechanisms, and pathways. Uric acid, type 2 diabetes, and cardiovascular diseases: fueling the common soil hypothesis Serum lipids and proliferative diabetic retinopathy and macular edema in persons with long-term type 1 diabetes mellitus: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. The epsilon4 allele of apolipoprotein E gene is a potential risk factor for the severity of macular edema in type 2 diabetic Mexican patients. Association between plasma triglycerides and high-density lipoprotein cholesterol and microvascular kidney disease and retinopathy in type 2 diabetes mellitus: a global case-control study in 13 countries. Interaction of ethanol, prostacyclin, and aspirin in determining human platelet reactivity in vitro. Moderate alcohol consumption, estrogen replacement therapy, and physical activity are associated with increased insulin sensitivity: is abdominal adiposity the mediator An epidemiologic approach to the study of retinopathy: the Pittsburgh diabetic morbidity and retinopathy studies. Effect of pregnancy on microvascular complications in the Diabetes Control and Complications Trial. Progression of diabetic retinopathy during pregnancy in women with type 2 diabetes. Progression of diabetic retinopathy in pregnancy: association with hypertension in pregnancy. Impact of pregnancy on the progression of diabetic retinopathy in type 1 diabetes. Pregnancy-induced sight-threatening diabetic retinopathy in women with type 1 diabetes. Prognosis for life in patients with diabetes: relation to severity of retinopathy. The association of alcohol consumption with the incidence and progression of diabetic retinopathy. Alcohol intake and the risk of coronary heart disease mortality in persons with older-onset diabetes mellitus. Prevalence of small vessel and large vessel disease in diabetic patients from 14 centres. The World Health Organisation Multinational Study of Vascular Disease in Diabetics. Pittsburgh InsulinDependent Diabetes Mellitus Morbidity and Mortality Study: physical activity and diabetic complications. Risk factors for incident retinopathy in a diabetic and nondiabetic population: the Hoorn study. Association between body mass index and diabetic retinopathy in Chinese patients with type 2 diabetes. Leisure time physical activity is associated with poor glycemic control in type 1 diabetic women: the FinnDiane study. Physical activity and proliferative retinopathy in people diagnosed with diabetes before age 30 yr. Physical activity and the risk of progression of retinopathy or the development of proliferative retinopathy. The relation of socioeconomic factors to the incidence of proliferative diabetic retinopathy and loss of vision. Variation in office-based quality: a claims-based profile of care provided to Medicare patients with diabetes.
Cheap 3.03mg yasmin otc
Fourth cranial nerve palsy and bilateral acute retinal necrosis following human herpesvirus 6 infection of the central nervous system birth control pills for heavy periods cheap yasmin 3.03 mg line. Human T-cell lymphotropic virus type-1 associated T-cell leukemia/lymphoma masquerading as necrotizing retinal vasculitis. Rapidly progressive outer retinal necrosis in the acquired immunodeficiency syndrome. Progressive outer retinal necrosis and acute retinal necrosis in fellow eyes of a patient with acquired immunodeficiency syndrome. A polymerase chain reaction-based assay for diagnosing varicella-zoster virus retinitis in patients with acquired immunodeficiency syndrome. Validation of a diagnostic multiplex polymerase chain reaction assay for infectious posterior uveitis. Real-time quantitative polymerase chain reaction diagnosis of infectious posterior uveitis. Acute retinal necrosis: the effects of intravitreal foscarnet and virus type on outcome. The potential impact of the varicella vaccine and new antivirals on ocular disease related to varicella-zoster virus. Visual results and complications after retinal reattachment in the acute retinal necrosis syndrome: the influence of operative technique. Surgical management of retinal detachment associated with the acute retinal necrosis syndrome. Long-term outcomes in patients undergoing vitrectomy for retinal detachment due to viral retinitis. Timing of prophylactic and early vitrectomy for firstpresenting or recurrent acute retinal necrosis syndrome. Efficacy and necessity of prophylactic vitrectomy for acute retinal necrosis syndrome. High dosage of oral valaciclovir as an alternative treatment of varicella zoster acute retinal necrosis syndrome. Systemic side effects of antiviral therapy in a patient with acute retinal necrosis. Successful treatment with combination of systemic antiviral drugs and intravitreal ganciclovir injections in the management of severe necrotizing herpetic retinitis. Intravitreal antiviral injections as adjunctive therapy in the management of immunocompetent patients with necrotizing herpetic retinopathy. Intravitreal antivirals in the management of patients with acquired immunodeficiency syndrome with progressive outer retinal necrosis. Progressive outer retinal necrosis syndrome: successful treatment with a new combination of antiviral drugs. Combination systemic and intravitreal antiviral therapy in the management of acute retinal necrosis syndrome. Combination systemic and intravitreal antiviral therapy in the management of acute retinal necrosis syndrome (an American Ophthalmological Society thesis). Fortunately, in the majority of cases the loss of visual function is minimal or even at times reversible, following discontinuation of the inciting drug. We present those medications known to produce a well-described anomaly and have omitted others that have not been definitively proven to cause retinal abnormalities. The medications are grouped according to the type of retinal toxicity they produce, and they are summarized in Box 92. After the cessation of chloroquine treatment, early subtle macular changes may possibly revert back to normal. Although far advanced cases may progress despite discontinuation of the drug, most patients remain stable with long-term follow-up. Currently it is prescribed for treatment of amebiasis, rheumatoid arthritis, systemic lupus erythematosus, and in countries primarily outside the United States, for prophylaxis against malaria. Photograph (A) and fluorescein angiogram (B) show early perifoveal pigmentary changes. Photograph shows bone-spicule pigmentary changes that can develop in advanced cases. It has been detected in the plasma, red blood cells, and urine of patients 5 years after their last known ingestion. Screening for toxicity has been more fully evaluated recently for hydroxychloroquine (see below), and similar testing is likely appropriate for chloroquine as well. Although it can produce a retinopathy identical to chloroquine, its occurrence is much less common. These patients should be given a dose based on their ideal body weight, otherwise overdosage may occur. Adjunctive testing now allows for earlier detection of hydroxychloroquine toxicity. If ocular toxicity occurs,35,37,38,61 and is recognized at an early stage, efforts should be made to communicate this directly to the prescribing physician so that alternative treatment options can be discussed with the patient. In early 2016, the American Academy of Ophthalmology task force on screening recommendations for hydroxychloroquine retinopathy published new updated guidelines in the journal Ophthalmology. Color photograph (A) showing mild macular pigment mottling in a patient on hydroxychloroquine. Fluorescein angiogram (B) demonstrates hyperfluorescence in the area of the perifoveal pigmentary changes. Fundus autofluorescence (C) shows a perifoveal hypoautofluorescence with a border of hyperautofluorescence. Spectral domain optical coherence tomography (D) shows atrophy of the outer nuclear layer and disruption of the ellipsoid segment. Fundus photograph (A) and fluorescein angiogram (B) show central and peripheral nummular pigmentary changes with corresponding atrophy of the choriocapillaris. Additionally, it is important to recognize that patients of Asian descent tend to have perifoveal retinopathy, rather than central macular involvement. Finally, one needs to be aware that coexisting renal disease and/or concurrent usage of tamoxifen may increase or hasten development of hydroxychloroquine retinopathy. A Phenothiazines Thioridazine Blurred vision, dyschromatopsia (reddish or brownish discoloration of vision), and nyctalopia characterize acute toxicity with thioridazine. Retinal toxicity from thioridazine is dependent more on the total daily dose than on the cumulative amount of drug received. Photograph (A) and fluorescein angiogram (B) show diffuse pigmentary and choriocapillaris atrophy, optic atrophy, and vascular attenuation. In the initial stages of toxicity, visual field testing can reveal mild constriction, paracentral scotomas, or ring scotomas. Experimental studies demonstrate that phenothiazines both alter enzyme kinetics and inhibit oxidative phosphorylation with subsequent abnormalities in rhodopsin synthesis. A review of the daily and cumulative drug dosage is essential in patients taking thioridazine. Chlorpromazine Chlorpromazine is a piperazine similar to thioridazine but lacks the piperidyl side chain as mentioned above. Other ocular effects include oculogyric crisis, miosis, and blurred vision caused by paralysis of accommodation. Usual doses range from 40 to 75 mg/day, but dosages up to 800 mg/day are not uncommon. Similar to thioridazine, the development and extent of toxicity are more closely related to daily dosage than total amount of drug taken. Photograph (A) and fluorescein angiogram (B) show granular pigmentary changes, though less severe than those generally seen with thioridazine. Pigment epithelial detachment, optic neuropathy, retinal vein occlusion, retinal hemorrhage, cystoid macular edema, and anterior chamber inflammation have also been reported. A large proportion of patients with objective signs of retinal toxicity remain asymptomatic.
Purchase genuine yasmin line
They have been seen to produce chronic or recurrent serous retinal detachment following schisis of the inner retina in around 45% of cases with variable intraretinal cystoid edema birth control 72 hour pill buy yasmin online. In this case, however, patients frequently experience pain on ocular movement and ultrasound B-scans demonstrate thickening of the suprachoroidal space with the characteristic T-sign. As the disease progresses to become persistent or chronic, with the resolution of subretinal fluid, there is increasing hyperautofluorescence due to the accumulation of non-shed fluorophores. Most of the time, large tumors are detected clinically, but sometimes small tumors, especially choroidal hemangiomas, are difficult to discern in the presence of subretinal fluid. Ultrasonography is useful in detecting and differentiating the nature of the tumor. In smokestack appearance, the leakage again starts as a pinpoint in the early phase, but gradually the hyperfluorescence ascends and expands to form a mushroom cloud or umbrella-like appearance. Poor visual acuity on presentation and long-standing macular detachment suggest worse prognosis. It has been shown to improve; however, the condition never reverts to normal after resolution of subretinal fluid with or without treatment. Correction of corticosteroid level, when possible, can lead to resolution of detachment in 90% of cases. In a series of 30 patients, the diode group had faster visual recovery and better final contrast sensitivity than the argon laser group without any persistent scotoma. A 30-mL infusion of verteporfin is administered for 10 minutes, followed by delivery of laser at 689 nm 15 minutes after the commencement of infusion. Visual acuity improved significantly in 92% of cases compared with 33% of the control group. Ketoconazole interferes with endogenous glucocorticoid production in part by inhibiting the conversion of 11-b-deoxycortisol to cortisol. Indocyanine green video angiography of older patients with central serous chorioretinopathy. Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Indocyanine green angiography and pathophysiology of multifocal posterior pigment epitheliopathy. Risk factors for recurrence of serous macular detachment in untreated patients with central serous chorioretinopathy. Central serous chorioretinopathy after local application of glucocorticoids for skin disorders. Risk of central serous chorioretinopathy in adults prescribed oral corticosteroids: a population-based study in Taiwan. Central serous chorioretinopathy associated with inhaled or intranasal corticosteroids. Bilateral central serous chorioretinopathy caused by intranasal corticosteroids: a case report and review of the literature. Bilateral serous retinal detachment resembling central serous chorioretinopathy following epidural steroid injection. Loss of visual acuity due to central serous retinopathy after steroid injection into the shoulder bursa. Acute bilateral central serous chorioretinopathy following intra-articular injection of corticosteroid. Central serous chorioretinopathy associated with topical corticosteroids in a patient with psoriasis. Central serous chorioretinopathy following vitrectomy with intravitreal triamcinolone acetonide for diabetic macular oedema. Advances in imaging techniques have not only resulted in more accurate diagnosis and management but have also broadened the horizons for the development of new treatments. Combination therapies involving the above treatment modalities may have a role in preventing permanent visual loss in this so-called benign disease and thus warrant additional studies in the form of large-scale randomized trials. Comparison of autofluorescence and optical coherence tomography findings in acute and chronic central serous chorioretinopathy. Risk factors for posterior cystoid retinal degenerationin central serous chorioretinopathy. Study of choroidal vascular lesions in central serous chorioretinopathy using indocyanine green angiography. Exacerbation of central serous chorioretinopathy following intravitreal triamcinolone injection. Changes in choroidal thickness after systemic administration of high-dose corticosteroids: a pilot study. Graft-vs-host-diseaseassociated conjunctival chemosis and central serous chorioretinopathy after bone marrow transplant. Retinal complications in patients with solid organ or bone marrow transplantations. Concentration of cytokines in the aqueous humor of patients with central serous chorioretinopathy. An association between central serous chorioretinopathy and gastroesophageal reflux disease. Should central serous chorioretinopathy be added to the list of ocular side effects of phosphodiesterase 5 inhibitors A case of idiopathic central serous chorioretinopathy in a 12-year-old male treated with bevacizumab. Angiographic characteristics of acute central serous chorioretinopathy in an Asian population. Chronic central serous chorioretinopathy associated with serous retinal detachment in a series of Asian patients. Subretinal dot like precipitates and yellow material in central serous chorioretinopathy. Peripheral retinal detachments and retinal pigment epithelial atrophic tracts secondary to central serous pigment epitheliopathy. Bullous retinal detachment: an unusual manifestation of idiopathic central serous choroidopathy. Optical density ratio in the subretinal fluid: differentiating chronic central serous chorioretinopathy and polypoidal choroidal vasculopathy. Morphologic characterization of dome-shaped macula in myopic eyes with serous macular detachment. Choroidal findings in domeshaped macula in highly myopic eyes: a longitudinal study. Resolution of foveal detachment in dome-shaped macula after treatment by spironolactone: report of two cases and mini-review of the literature. The optical tomography ophthalmoscope for examination of central serous chorioretinopathy with precipitates. Correlation of spectral domain optical coherence tomography findings and visual acuity in central serous chorioretinopathy. Comparative study of patients with central serous chorioretinopathy undergoing focal laser photocoagulation or photodynamic therapy. Direct, indirect, and sham laser photocoagulation in the management of central serous chorioretinopathy. Subthreshold diode micropulse photocoagulation for the treatment of chronic central serous chorioretinopathy with juxtafoveal leakage. Nonvisible subthreshold micropulse diode laser (810 nm) treatment of central serous chorioretinopathy: a pilot study.
Buy 3.03 mg yasmin with mastercard
Kawasaki disease predominantly affects young children and is the most common cause of acquired heart disease in the United States and Japan birth control for women of faith buy discount yasmin 3.03mg on-line. Kawasaki disease is usually defined as a persistent fever for a minimum of 5 days with a minimum of four out of the following: (1) polymorphous rash; (2) bilateral conjunctival injection without exudates; (3) oropharyngeal involvement, including red fissured lips, strawberry tongue, and red pharynx without exudates; (4) peripheral changes including edema of extremities, sole erythema, and periungual desquamation; and (5) cervical lymphadenopathy. Axial arthropathy and effusions can also occur, but the articular symptoms will usually resolve after the acute phase. Other RheumaticDisease 1617 orbital inflammation may lead to orbital socket contraction with enophthalmos, restrictive ophthalmopathy, and chronic pain. Anterior, posterior and panuveitis have all been described in this context and may be isolated or associated with scleritis. Neuro-ophthalmic consequences most commonly occur secondary to orbital involvement, but may also arise due to vasculitis causing ischemic optic neuropathy. Like other vasculitides, the suggested treatment to induce remission is pulsed intravenous cyclophosphamide with oral steroids. If disease is limited, then methotrexate in combination with oral corticosteroid can be used rather than cyclophosphamide. Systemic symptoms include fever, weight loss, arthralgias, and, rarely, arthritis. Other pulmonary manifestations include pulmonary infiltrates, pulmonary hemorrhage, and pleural effusions. Cardiac involvement includes eosinophilic endomyocarditis, coronary vasculitis, valvular heart disease, congestive heart failure, hypertension, and pericarditis. Skin lesions are common and typically include nonthrombocytopenic palpable purpura, with erythematous, maculopapular, or pustular lesions being reported. Ophthalmic disease may arise from two processes: vasculitis and granuloma formation. Clinical presentations include conjunctival nodules,250 peripheral ulcerative keratitis, episcleritis, scleritis, uveitis (rare), retinal vasculitis,251 retinal artery occlusion, ischemic optic neuropathy, cranial neuropathies,252 and orbital disease (presenting with an orbital inflammatory syndrome). Rapidly progressive glomerulonephritis may occur, resulting in acute renal failure necessitating renal dialysis. Varying degrees of pulmonary involvement can occur; these can range from mild dyspnea to life-threatening pulmonary hemorrhage. Involvement of both the central and peripheral nervous system is described and includes peripheral neuropathy, mononeuritis multiplex, cerebral hemorrhage/infarction, seizures, or headache. Other systemic manifestations include cardiac, gastrointestinal, otorhinolaryngeal, and venous thromboembolism. Corticosteroids Most treatment-related visual morbidity is associated with corticosteroid treatment. Overall and cancer related mortality among patients with ocular inflammation treated with immunosuppressive drugs: retrospective cohort study. The prevalence of rheumatoid arthritis in the United Kingdom: new estimates for a new century. Impact of smoking as a risk factor for developing rheumatoid arthritis: a metaanalysis of observational studies. The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Mortality rate in rheumatoid arthritis patients developing necrotizing scleritis or peripheral ulcerative keratitis: effects of systemic immunosuppression. Management and therapy of dry eye disease: report of the Management and Therapy Subcommittee of the International Dry Eye WorkShop (2007). The Assessment of Spondyloarthritis International Society classification subcapsular cataract and exogenous corticosteroids is well established. Prognosis will be worse if there is visually significant posterior segment disease. Increased intraocular pressure due to exogenous corticosteroids may occur in up to 30% of the normal population, with 5% experiencing an increase of more than 15 mmHg (reviewed by Clark255). Corticosteroid-induced ocular hypertension must be monitored and treated where there is a risk of progression to secondary glaucoma. These drugs can cause a reversible, visually insignificant keratopathy (cornea verticillata) and, more importantly, an irreversible sight-threatening maculopathy. Endstage disease includes generalized atrophy, peripheral pigmentation, arteriolar attenuation, and optic atrophy. In both cases, risk increases with increasing dose, increasing duration, and reduced renal function. Additionally, they recommend that one or more of the following should be performed where available: spectral domain optical coherence tomography, multifocal electroretinography, or fundus autofluorescence. Although fundus examinations are advised for documentation, the aim is to detect changes before visible maculopathy. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Adalimumab effectively reduces the rate of anterior uveitis flares in patients with active ankylosing spondylitis: results of a prospective open-label study. Decreased incidence of anterior uveitis in patients with ankylosing spondylitis treated with the anti-tumor necrosis factor agents infliximab and etanercept. Uveitis associated with inflammatory bowel disease compared with uveitis associated with spondyloarthropathy. Ocular manifestations in a communitybased cohort of patients with inflammatory bowel disease. Family history of inflammatory bowel disease in patients with idiopathic ocular inflammation. Treatment strategies for scleritis and uveitis associated with inflammatory bowel disease. A cross-sectional comparative study of patients with "psoriatic arthritis" and seronegative and seropositive polyarthritis: clinical aspects. Epidemiology of juvenile idiopathic arthritis in a multiethnic cohort: ethnicity as a risk factor. Prevalence, risk factors, and outcome of uveitis in juvenile idiopathic arthritis: a long-term followup study. Derivation and validation of systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. The classification of glomerulonephritis in systemic lupus erythematosus revisited. Oral and ocular sicca symptoms and findings are prevalent in systemic lupus erythematosus. Acute ocular ischaemia and orbital inflammation associated with systemic lupus erythematosus. Antiphospholipid antibodies: a risk factor for occlusive ocular vascular disease in systemic lupus erythematosus and the "primary" antiphospholipid syndrome. Tuberculous choroidal granulomas in a patient with systemic lupus erythematosus: a case report. Endogenous Nocardia asteroides endophthalmitis in a patient with systemic lupus erythematosus. Prospective observational single-centre cohort study to assess the effectiveness of treating lupus nephritis with rituximab and mycophenolate mofetil but no oral steroids. Risk factors for development of uveitis differ between girls and boys with juvenile idiopathic arthritis. Biomarkers of chronic uveitis in juvenile idiopathic arthritis: predictive value of antihistone antibodies and antinuclear antibodies. Male gender and poor visual outcome in uveitis associated with juvenile idiopathic arthritis. Male gender as a risk factor for complications in uveitis associated with juvenile idiopathic arthritis.
Order yasmin 3.03mg without a prescription
A serologically diagnosed human case of cutaneous larva migrans caused by Ancylostoma caninum birth control 4 inactive pills buy cheap yasmin 3.03mg line. Clinical treatment of diffuse unilateral subacute neuroretinitis with albendazole. Report from the 2009 Inter-American Conference on Onchocerciasis: Progress towards eliminating river blindness in the Region of the Americas. Profile of eye lesions and vision loss: a cross-sectional study in Lusambo, a forest-savanna area hyperendemic for onchocerciasis in the Democratic Republic of Congo. Morphology of posterior segment lesions of the eye in patients with onchocerciasis. The use of systemic and intravitreous steroid in inflammation secondary to intraocular cysticercosis: case report. Orbital cysticercosis: clinical manifestations, diagnosis, management, and outcome. Intraocular cysticercosis: clinical characteristics and visual outcome after vitreoretinal surgery. Epidemiology and Risk Factors Clinical Assessment of the Patient Medical Evaluation of the Patient Endogenous Bacterial Endophthalmitis Endogenous Fungal Endophthalmitis Treatment Strategies Systemic Pharmacotherapies Intravitreal Pharmacotherapies Surgical Treatments Suggested Management injection, trauma, or keratitis. Patients with endogenous endophthalmitis may present with varying degrees of pain, inflammation, and visual loss. In the anterior chamber, cell and flare, fibrin, posterior synechiae, and hypopyon may occur. In the posterior segment, findings may include vitreous opacification and chorioretinitis, including hemorrhage, cotton-wool spots, retinal opacification, and vasculitis. An insidious onset, focal vitreous opacities, and chorioretinal infiltrates suggest fungal etiology. Relatively more rapid progression and more severe intraocular inflammation suggest bacterial etiology. Endogenous endophthalmitis may present as a relatively mild and nonspecific anterior uveitis. The rate of initial misdiagnosis has been reported as high as 63% in one large series. An increasing number of immunocompromised patients are receiving antineoplastic agents, immunomodulating agents, and newer broad-spectrum antimicrobial agents, all of which may reduce normal flora. Chronic (delayed-onset) postoperative endophthalmitis Propionibacterium acnes Candida parapsilosis Coagulase-negative staphylococci Filtering bleb-associated endophthalmitis Streptococcus spp. Staphylococcus aureus Gram-negative organisms Endophthalmitis associated with microbial keratitis Gram-negative organisms Staphylococcus aureus Fusarium spp. Endophthalmitis associated with intravitreal injection Coagulase-negative staphylococci Streptococcus spp. One published classification scheme for endogenous bacterial endophthalmitis used zones of anatomic involvement (Box 90. Generally, the medical evaluation is performed in consultation with an infectious disease specialist or other medical specialist. A high index of suspicion should be maintained because both the ophthalmic and systemic symptoms are quite variable. In one series, 43% of patients with endogenous endophthalmitis had no nonocular symptoms. Intraocular cultures are also important in patients who progress despite treatment with empiric antimicrobial therapy. Obtaining cultures from multiple sites may be necessary to make a specific diagnosis. In one series of patients with endogenous bacterial endophthalmitis, the rate of diagnostic cultures was 74% for vitreous, 72% for blood, and 96% overall. Fungi may be differentiated using several criteria, but are commonly divided between unicellular yeasts and multicellular molds. Some fungi may grow with both yeast-like and mold-like morphology in tissues or culture. Fungi may also be classified by pigmentation (moniliaceous versus dematiaceous), virulence (pathogenic versus opportunistic), or clinical presentation (cutaneous, subcutaneous, or systemic). Note creamy white chorioretinal lesion, with associated retinal hemorrhage and evidence of vasculitis. Candida albicans is the most common yeast isolate and the most common overall fungal isolate in patients with endogenous fungal endophthalmitis. Among patients with diagnosed candidemia, reported rates of endogenous endophthalmitis range from less than 3%58 to 44%. Yellow or fluffy-white vitreous opacities, sometimes connected by strands of inflammatory material ("string of pearls" configuration), may be noted. The choroid and retina are highly vascular structures, which suggests that systemic pharmacotherapy may be sufficient to treat infections confined to these structures, while severe intravitreal involvement may require intravitreal agents. This patient was an intravenous drug abuser and improved with empiric oral fluconazole. The selection of systemic pharmacotherapies is frequently made in consultation with an infectious disease or other medical specialist. The management is typically individualized based on the severity of the ocular and systemic infections. For example, in a prospective study, intravenous teicoplanin was reported to have poor intravitreal penetration. Systemic gatifloxacin is no longer commercially available, due to an associated dysglycemia in some patients. Amphotericin B has been widely used in the treatment of various fungal infections. An alternative liposomal formulation is also available,97 but experience with this formulation in the treatment of endogenous fungal endophthalmitis is limited at this time. The use of amphotericin B is limited by multiple toxic effects, including renal failure, chills, fever, vomiting, nausea, diarrhea, dyspnea, malaise, anemia, characteristic central macular chorioretinal inflammatory lesion. Additionally, Aspergillus endophthalmitis may be associated with retinal vascular occlusion, choroidal vascular occlusion, exudative retinal detachment, and/or diffuse hemorrhagic retinal necrosis. The Infectious Disease Society of America recommends ophthalmic evaluation for all patients with fungemia. These recommendations are mainly based on older studies, which found rates of ocular involvement in fungemic patients as high as 37%. Although a very small number of verbal patients with fungal endophthalmitis were asymptomatic, the screening results may not change the patient management and may not be cost-effective. The imidazoles (miconazole and ketoconazole) were used historically, but largely have been replaced by the newer triazoles (fluconazole, itraconazole, voriconazole, and posaconazole), although a case report documented a good outcome in endogenous Aspergillus terreus endophthalmitis using intravitreal amphotericin B, oral ketoconazole, and topical natamycin. Itraconazole may also be prescribed orally but is used infrequently in the treatment of endogenous endophthalmitis. Voriconazole is generally effective against most Candida species (including those resistant to fluconazole, such as C. Successful treatment of refractory Fusarium deep keratitis or endophthalmitis has been reported with oral (or oral plus topical) posaconazole. These are newer agents and, compared with amphotericin B and the azoles, relatively little has been reported about their use in endogenous endophthalmitis. In a patient with bacteremia due to a known organism, targeted pharmacotherapy may be considered in patients with suspected ocular involvement. To reduce the risk of aminoglycoside toxicity, ceftazidime or ceftriaxone may be considered as an alternative to amikacin. Ceftazidime may precipitate when mixed with vancomycin, but this does not appear to affect its clinical efficacy. Intravitreal daptomycin has been reported to be safe and effective in treating one case of bilateral endogenous endophthalmitis secondary to vancomycin resistant S.
Discount 3.03 mg yasmin with amex
Nineteen of these patients "showed a peculiar and consistent pattern of ocular lesions" that included both discrete atrophic birth control vasectomy order 3.03 mg yasmin otc, sparsely pigmented or unpigmented, peripheral lesions (frequently referred to as "histo spots") and later cystic lesions in the macula. Woods and Wahlen concluded that previous benign systemic histoplasmosis was responsible for the ocular findings in these 19 patients. Characterized by multiple chorioretinal scars with similar findings to ocular histoplasmosis. One study examined distinguishing features of multifocal choroiditis compared to ocular histoplasmosis. Scarring and permanent chorioretinal lesions are not usually observed (see Chapter 79, White spot syndromes and related diseases). Peripapillary atrophy and associated peripheral chorioretinal atrophy is not present (see Chapter 94, Traumatic chorioretinopathies). Areas of focal atrophy may be present in the macula, but the atrophy is not usually seen in the periphery. Peripapillary atrophy is often not present (see Chapter 69, Neovascular (exudative or "wet") agerelated macular degeneration). Visual acuity returned to 20/20 3 months after enrollment and remained at 20/20 throughout the 5-year follow-up period. The usual histoplasmosis infection is a relatively mild illness with flu-like respiratory symptoms. Studies in Tennessee have demonstrated that almost 90% of children of 13 years of age had positive reactions to histoplasmin skin tests. Occasionally, epidemics of systemic disease outbreak may occur that are often associated with high levels of environmental exposure. The development of initial neovascular disciform lesions has been reported at around 2 per 100, 000 population per year. The most widely accepted theory involves focal infection of the choroid at the time of systemic infection. The most promising animal models are primates, in which systemic infection and ocular lesions have been produced. It is likely that these lesions develop earlier in life and are only coincidentally discovered during ophthalmic examinations for causes of visual symptoms that may or may not be related to ocular histoplasmosis. The vast majority of disciform lesions occur in Caucasians with only around a dozen cases reported among African Americans. It is unclear whether this genetic predisposition specifically reflects the susceptibility to ocular histoplasmosis or to infection by H. The vision loss in this disease often occurs in middle-aged individuals who are in the most active and productive stage of their life. Either in the absence of further inflammation or under the influence of recurrent episodes of inflammation, the choroidal blood vessels surrounding an atrophic chorioretinal scar (D) may decompensate and cause serous exudation, choroidal neovascularization, and transient serous detachment of the retina (E). This process in turn may result in a hemorrhagic detachment of the retina (F) that resolves as a disciform scar (G). No treatment is known to prevent inactive lesions from giving rise to exudative or hemorrhagic neovascular complexes that typically end in disciform macular scars. Whether there is a role to manage active histo spots is unclear since many or perhaps most spontaneously involute. Visual acuity improved or stabilized in 69% of eyes, with 44% of eyes improving at least 2 lines. Eighty percent of eyes showed vision stabilization or improvement in the juxtafoveal group. Sixty percent of eyes with juxtafoveal lesions achieved a final visual acuity of 20/40 or better. Eyes with subfoveal lesions had similar results, with 83% of eyes having stabilization or improvement in vision. The mean pretreatment acuity in these eyes was 20/50, and the mean final visual acuity was 20/50. Examination of 22 eyes 2 years following initial treatment revealed that 45% of eyes had gained 1. Fluorescein angiograms were taken at time of study entry, 6 and 12 months after enrollment, and annually thereafter. A total of 289 eyes were randomized between krypton laser treatment and no treatment. A loss of 6 or more lines was seen in 11% of the treated eyes compared to about 30% of the controls. After a single intravitreal injection of bevacizumab, the visual acuity improved to 20/30 by 6 months follow-up. After 3 months, visual acuity improved from a mean baseline visual acuity of 20/114 to 20/55. Fifty-eight percent of eyes had 20/40 or better vision at final follow-up compared to 21% at baseline. Nine patients had 12 month follow-up and improved from a mean baseline visual acuity of 20/150 to 20/45. Overall, the mean initial visual acuity was 20/88 and the mean final visual acuity was 20/54. Both of the studies examining bevacizumab were retrospective, with significant methodologic shortcomings, and the results should be interpreted with caution. Mean baseline visual acuity was 20/53, and the final mean visual acuity was 20/26 (p<. Visual acuity improvement was noted in 81% of eyes, stability of visual acuity was recorded in 13% of eyes, and vision loss was reported in 6 % of eyes. This study randomized eyes to monthly ranibizumab or 3-monthly injections followed by an as needed (prn) dosing schedule at monthly visits. Nine eyes (of 30) with ocular histoplasmosis were included in this trial, four in the monthly arm and five in the prn arm. There were no statistically significant differences between the groups at any time point. No serious ocular or systemic adverse events were observed, but larger sample sizes are needed to detect infrequent severe adverse events. Early research suggests that it may have an important role in the management of this condition. Subgroup analysis of these five patients revealed that all five eyes experienced stabilization or improvement in visual acuity with a mean gain of 2. A total of 151 eyes were included in the study, and 104 eyes had at least a 12-month follow-up period. There was no difference in visual acuity at 12 months or 24 months between the bevacizumab monotherapy and combination groups. Visual acuity improved or stabilized in 80% of eyes, including 30% that gained 1 line or more. Cataract progression and increased intraocular pressure were concerning ocular side-effects. In fact, the recurrence rate after submacular surgery is higher than recurrence following laser photocoagulation. At 2 years, vision had improved or remained stable in 20% more patients treated with surgery than with observation. Subgroup analyses revealed that nearly all of the benefit seen with surgery was in those eyes with 20/100 or worse baseline visual acuity. In this subset of 92 eyes, 76% of surgery eyes remained stable or improved compared to 50% of eyes that were observed. Color photograph (C) and early frame of fluorescein angiogram (D) taken 6 months after submacular surgery show a well-demarcated postoperative disturbed area of the retinal pigment epithelium. Systemic histoplasmosis diagnosed before death and produced experimentally in guinea pigs. The probable role of benign histoplasmosis in the etiology of granulomatous uveitis.