Purchase sevelamer online now
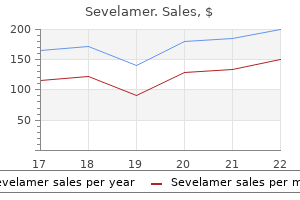
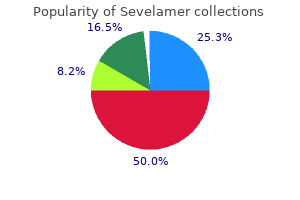
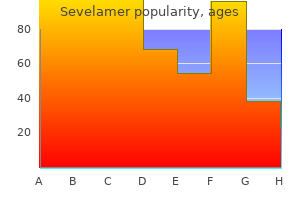
In patients with the murmur of aortic regurgitation gastritis mayo clinic order sevelamer with a visa, a wide pulse pressure (80 mm Hg or more) increases the probability of moderate-to-severe regurgitation. Pulse pressure may be normal, abnormally small (narrow), or abnormally large (wide; see the section on Abnormal Pulse Pressure). The mean arterial pressure can be estimated by (S + 2D)/3, where S is systolic blood pressure and D is diastolic blood pressure. Indirect measurements required cumbersome mechanical devices and were not widely accepted until 1896, when the Italian Riva-Rocci invented the blood pressure cuff. In 1901, after Harvey Cushing first brought the blood pressure cuff to America and encouraged its use in neurosurgical patients, most clinicians resisted using it because they believed palpation of pulse revealed much more information, including its "fullness," "tension," "rate," "rhythm," "size," "force," and "duration". Janeway showed, for example, that the first sign of intestinal perforation or hemorrhage in patients with typhoid fever was progressive hypotension. The oscillometric method, in contrast, has the advantages of convenience, reduced observer bias, and elimination of the auscultatory gap. These recommendations, however, are designed to avoid misdiagnosis of hypertension and may not be as relevant to clinicians using the blood pressure cuff to diagnose other abnormalities, such as hypotension or abnormalities of pulse contour. In some clinical scenarios, described in the section Findings and Their Clinical Significance, additional measurements are necessary, including those of the legs or opposite arm or measurements taken with the patient in different positions. The artery collapses because cuff pressure exceeds diastolic pressure; it opens again with each beat because cuff pressure is less than systolic pressure. The sound represents the sudden deceleration of the rapidly opening arterial walls, which causes a snapping or tapping sound, just like the sail of a boat snaps when it suddenly tenses after tacking in the wind or a handkerchief snaps when its ends are suddenly drawn taut. The genesis of the Korotkoff sounds, therefore, is similar to the genesis of other snapping or tapping sounds produced by the sudden deceleration of other biologic membranes, such as the normal first and second heart sounds or the femoral pistol shot sounds of aortic regurgitation (see Chapters 40 and 45). Even before the discovery of Korotkoff sounds, clinicians used the blood pressure cuff to measure both systolic and diastolic blood pressure. Clinicians still use this technique to measure the blood pressure of hypotensive patients (a D. The initial tapping sound at systolic blood pressure is phase 1; a swishing murmur is phase 2; the reappearance of a softer tapping sound is phase 3; the disappearance of the tapping and appearance of a much softer murmur ("muffling") is phase 4; and the disappearance of all sound is phase 5. In the first method, the clinician applies light pressure to palpate the brachial artery just below the blood pressure cuff. As the cuff is deflated, the first appearance of a pulse indicates systolic blood pressure. The cuff pressure at this lower limit of maximal pulsation indicates the diastolic blood pressure. As the cuff pressure decreases, the indicator needle of an aneroid manometer starts to bob with increasing amplitude, until the bobbing suddenly disappears at the moment cuff pressure falls below diastolic pressure. Measurements of systolic and diastolic blood pressure by palpation differ from readings by auscultation by only 6 to 8 mm Hg or less. These recommendations are based on the following observations: (1) shorter periods of supine rest significantly reduce the sensitivity of postural vital signs for detecting blood loss, and (2) after normal persons stand, the pulse rate stabilizes after 45 to 60 seconds and the blood pressure stabilizes after 1 to 2 minutes. Counting the heart rate first, beginning at 1 minute, allows more time for the blood pressure to stabilize. Much higher cuff pressures are then necessary to cause collapse of the artery, leading the clinician to misdiagnose hypertension when it is not present. The greatest errors, according to these data, occur from using too small of a cuff; the risk of underestimating true pressure with too large a cuff is relatively minor. Because the distal pulse persists during the auscultatory gap, however, clinicians can avoid this mistake by palpating the systolic pressure before using the stethoscope. Clinical studies minimize this and other observer biases by using oscillometric devices or a random zero sphygmomanometer (an instrument that blinds the clinician to the true reading). Detecting essential hypertension is the reason blood pressure should be measured in every person, even when asymptomatic, because the disorder is common and treatable and because treatment reduces cardiovascular morbidity and overall mortality. A single study from 1985 proposed that a simple physical finding, Osler sign, accurately identifies patients with pseudohypertension. It occurs commonly in elderly individuals, whether or not they have hypertension (presenting in 11% of individuals over the age of 75 years and 44% over the age of 85 years). In patients with myocardial infarction, a systolic blood pressure of less than 80 mm Hg predicts a greater incidence of congestive heart failure, ventricular arrhythmias, and complete heart block. The average difference in systolic blood pressure between the two arms is 6 to 10 mm Hg. In this syndrome, stenosis or occlusion of one subclavian artery proximal to the origin of the vertebral artery reduces the pressure distal to the obstruction, which causes the flow in the vertebral artery to reverse directions: instead of traveling normally up the vertebral artery to perfuse the brain, blood flow courses downward to perfuse the arm. Rare patients with aortic dissection present with the physical findings of pulsatile sternoclavicular joints74 or unilateral femoral pistol shot sounds (see Chapter 45). In patients with coarctation, however, the femoral pulse is delayed, due both to delay in arrival at the legs and to more rapid than normal conduction of the wave to the arms. This relationship has been validated in one setting: patients with known left ventricular dysfunction. Normally, the blood pressure remains relatively stable during this shift because of compensatory increases in cardiac output, heart rate, and systemic vascular resistance, and transfer of blood from the pulmonary circulation to the systemic side. For example, in persons younger than 65 years, postural hypotension is found in 8% before moderate blood loss and 9% after blood loss. For those 65 years or older, postural hypotension is detected in 11% to 30% before blood loss and about 25% after blood loss. After moderate blood loss, 1% have tachycardia in the supine position and only 13% have supine hypotension; after large blood loss, only 10% have tachycardia and 31% have hypotension. Sinus bradycardia, in contrast, is a common arrhythmia after blood loss and frequently precedes the drop in blood pressure that causes patients to faint. Patients with structural lesions tend to have higher blood pressures (from reflex responses to increases in intracranial pressure-the Cushing reflex-or from the etiologic association of hypertension and stroke) than do patients with metabolic encephalopathy (whose severe comorbidities often are associated with lower blood pressure). Traditionally, the blood pressure cuff was used to test capillary fragility, although measurements of blood pressure were not part of the test. Capillary fragility tests were designed to detect abnormally weakened capillary walls in the skin that would burst more easily when distended, resulting in the appearance of high numbers of petechiae. A large number of diseases were associated with capillary fragility, ranging from coagulopathies, vitamin deficiencies. The negative pressure technique applied suction to a defined area of the skin, a technique whose undoing H. Rumpel and Leede, consisted of raising the venous pressure by a tourniquet or blood pressure cuff around the arm and counting petechiae that subsequently developed in a defined area distally. This test was eventually standardized,100 but interest fell after the introduction of better diagnostic tests for coagulation and the other associated disorders. More recently, increased capillary fragility was believed to represent a sign of diabetic retinopathy,101 but this was soon disproven. Recommendations for blood pressure measurement in humans and experimental animals. A statement for professionals from the subcommittee of professional and public education of the American Heart Association Council on high blood pressure research. Sphygmomanometer cuff size and the accuracy of indirect measurement of blood pressure. Korotkoff sounds: observations on pressure-pulse changes underlying their formation. A note on the measurement of diastolic and systolic blood pressure by the palpation of arterial vibrations (sounds) over the brachial artery. A review of common errors in the indirect measurment of blood pressure (sphygmomanometry). Review: a century of confusion; which bladder for accurate blood pressure measurement Association of the auscultatory gap with vascular disease in hypertensive patients. Effect of vertical displacement of the arm on indirect blood-pressure measurement. Does the position or contact pressure of the stethoscope make any difference to clinical blood pressure measurement.
Buy generic sevelamer from india
Oligodendrocytes Astrocytes Microglial cells Schwann cells Satellite cells Ependymal cells A gastritis symptoms in child cheap 400mg sevelamer mastercard. Anchor neurons and blood vessels; maintain extracellular environment around neurons; assist in the formation of the blood brain barrier E. Anterior horn Central canal Lateral horn Posterior horn Spinal arachnoid mater Spinal dura mater Posterior 7 Cerebrospinal fluid is produced by the a. The corpus callosum is a large tract of white matter that connects the right and left cerebral hemispheres. Why do you think the anesthetic is injected into the epidural space instead of the subarachnoid space Motor to the muscles of swallowing; taste to the posterior one-third of the tongue F. Motor to the muscles of facial expression; taste to the anterior two-thirds of the tongue J. Motor to four of six extrinsic eye muscles; dilates the pupil; opens the eye; changes the shape of the lens K. Motor to the muscles of swallowing and speaking; motor to the thoracic and abdominal viscera L. Motor one of six extrinsic eye muscles (lateral rectus muscle) 8 13 the receptor that detects the stretch in a stretch reflex is called a(an) a. Sensation may be conscious or subconscious, depending on the destination of the sensory information. This information never makes it to the cerebral cortex, so you are not consciously aware of it. However, information eventually taken to the cerebral cortex for integration and interpretation. The following exercises ask you to examine the anatomy and physiology of the special senses: vision, hearing and equilibrium, taste, and smell. You also will examine the general senses in this unit, which include touch, pain, and temperature. Many of the external structures of the eye protect the delicate eyeball, and others move the eyeball. The palpebrae meet medially and laterally at the medial and lateral canti (or commissures), respectively. There are several structures in and around the palpebrae that contain sebaceous or mucous glands to lubricate the palpebrae and anterior surface of the eyeball. One of the most prominent external structures of the eye is the lacrimal apparatus, which produces and drains tears. The lacrimal apparatus consists of the lacrimal gland, located in the superolateral orbit, and the ducts that drain the tears it produces. From here, tears travel through the nasolacrimal duct and, finally, empty into the nasal cavity just inferior to the inferior nasal concha (which is why your nose runs when you cry). In addition, two muscles that open and close the eye insert into and around the palpebrae: the levator palpebrae superioris muscle and the orbicularis oculi muscle. The eyeball itself is a hollow organ that is divided into two main portions: the anterior cavity and the posterior cavity. The boundary for the cavities is a crystalline structure known as the lens, which is one of the structures in the eye that refracts (bends) light coming into the eye to focus it. The anterior cavity is anterior to the lens and is filled with a watery fluid called aqueous humor. Aqueous humor is produced relatively constantly and drained by a structure called the scleral venous sinus. Unlike aqueous humor, vitreous humor is present at birth and remains relatively unchanged throughout life. The outermost layer of the eyeball is the fibrous tunic, which consists mostly of dense irregular collagenous connective tissue. It is white because of numerous collagen fibers that contribute to its thickness and toughness (in the same way a joint capsule or a ligament is tough and white). It is made chiefly of the ciliary muscle, smooth muscle fibers that control the shape of the lens. The photoreceptors known as rods are scattered throughout the retina and are responsible for vision in dim light and for peripheral vision. Cones, the second type of photoreceptor, are concentrated at the posterior portion of the retina. It is also known as the blind spot because its lack of photoreceptors means that this region can produce no images. When viewing nearer objects, however, additional "fine-tuning" refraction is needed by the lens. This is accomplished with the help of the ciliary muscle-when its smooth muscle fibers contract, the ciliary body moves closer to the lens and removes tension on the suspensory ligaments. This causes the lens to become rounder, an adjustment called accommodation which allows the lens to provide the additional refraction necessary to focus light on the retina. When the eye switches to a distant object again, the ciliary muscle relaxes, which moves the ciliary body farther away from the lens and puts tension on the suspensory ligaments. This flattens the lens and allows the cornea to again become the primary refractive medium. Sclera Iris 2 3 Use scissors to remove the adipose tissue surrounding the eyeball. Hold the eyeball at its anterior and posterior poles, and use a sharp scalpel or scissors to make an incision in the frontal plane. Take care to preserve the fragile retina-the thin, delicate yellow-tinted inner layer. In this procedure, you will see (no pun intended) firsthand the differences in vision produced by the rods and the vision produced by the cones. Have him or her continue to stare forward and attempt to read what you have written. Have your partner stand 20 feet in front of a Snellen eye chart and read down the chart, stopping with the smallest line read accurately. For example, a person with 20/40 vision can see at 20 feet what someone with perfect vision could see at 40 feet. Visual acuity: 9 5 With the lights still dimmed and your partner standing in the same place, hold a piece of dark green or dark blue paper over the Snellen chart. Visual acuity: Paper color: 7 In which scenario were visual acuity and color vision better Have your lab partner measure with a ruler the distance from the page to your eye with a ruler. These irregularities decrease visual acuity because these structures are unable to focus light precisely on the retina. The ossicles transmit vibrations from the tympanic membrane to the inner ear through a structure called the oval window, to which the stapes is attached. The vestibule is an egg-shaped bony cavity that houses structures responsible for static equilibrium, which refers to maintaining balance when the body is not moving. Situated at right angles to one another, the semicircular canals work together with the organs of the vestibule to maintain equilibrium. Their orientation allows them to be responsible for a type of equilibrium called rotational equilibrium. The cochlea has a hole in its lateral wall called the round window, which plays a role in allowing the perilymph in the cochlea to vibrate. The structures of the cochlea transmit sound stimuli via the cochlear portion of the vestibulocochlear nerve. Procedure 1 Model Inventory for the Ear Identify the following structures of the ear on models and diagrams, using this unit and your textbook for reference. As you examine the anatomical models and diagrams, record the name of the model and the structures you were able to identify on the model inventory in Table 9. Conductive hearing loss results from interference of sound conduction through the outer and/or middle ear. Sensorineural hearing loss results from damage to the inner ear or the vestibulocochlear nerve. Two clinical tests can help a healthcare professional determine whether hearing loss is conductive or sensorineural: the Weber test and the Rinne (rinn-ay) test.
Purchase generic sevelamer on line
Glomerular capsule (1) Parietal layer (2) Visceral layer (3) Podocytes (4) Capsular space 2 chronic gastritis reflux esophagitis discount sevelamer 800mg fast delivery. Procedure 4 Kidney Dissection In this procedure, you will now dissect a preserved kidney and locate several of the structures you just identified on models and diagrams. Safety Note 1 2 3 Obtain a fresh or preserved kidney specimen and dissection supplies. If the thick surrounding connective tissue coverings are intact, note their thickness and amount of adipose tissue. Use scissors to cut through the connective tissue coverings, and remove the kidney. Following are some hints to aid you: the renal artery typically has the thickest and most muscular wall, and it branches into several segmental arteries prior to entering the kidney. The renal vein is thinner, flimsier, and often larger in diameter than the renal artery. The ureter has a thick, muscular wall, but it does not branch after it leaves the kidney. Also, its diameter is usually smaller than either the renal artery or the renal vein. Keeping these points in mind, determine the location of the renal artery, the renal vein, and the ureter on your specimen. This pressure pushes fluid and solutes out of the glomerulus and into the capsular space. This pressure tends to oppose filtration and pulls water into the glomerular capillaries by osmosis. Filtrate is similar in composition to blood, but it lacks most of the proteins and cells we find in blood. Notice in the figure that the cells of the visceral layer, known as podocytes, have extensions called foot processes that interlock to form narrow filtration slits. The filtration membrane acts in a similar manner to the filter in your coffeemaker. Just as a coffee filter holds back the coffee grounds while allowing water and other solutes to pass through into your coffee, the filtration membrane prevents large items, such as proteins and cells, from leaving the blood while allowing small substances, such as water, glucose, amino acids, electrolytes, and metabolic wastes, to leave the blood and enter the filtrate. This selectivity is vitally important, as the nephron tubules and collecting system cannot reabsorb large proteins or cells; for this reason, any that entered the filtrate would be lost to the urine. The filtrate contains a number of substances our bodies need to reclaim, including water, glucose, amino acids, and many different ions. About 99 percent of the water in the filtrate and most of the solutes are reabsorbed through the epithelium of the nephron tubules and returned to the blood. If the water were not reabsorbed in the renal tubules and the collecting ducts, we would lose our entire plasma volume in fewer than 30 minutes. Examples Visceral layer membrane of secreted substances include potassium of glomerular ions, hydrogen ions, and uric acid. Distal tubule Filtrate in tubule lumen Cytosol in tubule cell Endothelial cell of capillary Blood in Interstitial peritubular fluid capillary Reabsorption Secretion 15 Interstitial fluid Tubule lumen Peritubular capillary Apical membrane Basolateral membrane Tubular secretion: Substances are moved from the blood, to the interstitial fluid, through the tubule cells, into the filtrate. A kidney is easily modeled with either animal blood or simulated blood and simple dialysis tubing, which has a permeability similar to that of the filtration membrane. Substances to which the "filtration membrane" is permeable will enter the surrounding water (the "filtrate"), whereas those to which the membrane is not permeable will remain in the tubing. Each strip consists of 10 small, colored pads that change color in the presence of certain chemicals, such as glucose or hemoglobin. The strip is interpreted by watching the pads for color changes and comparing the color changes to a color-coded key on the side of the bottle. Please note that for this exercise you will read only four of the 10 boxes: blood, leukocytes, protein, and glucose. Note that the model kidney must sit in water for 25 minutes while you wait for your results. Securely tie off one end of the tubing with string and open the other end of the tubing by wetting the end of the tube and rubbing it between your fingers. Place the tied-off tube in a 200 mL beaker containing about 150 mL of deionized water. Turn the bottle on its side and compare the colors of the pads for glucose, blood, leukocytes, and protein. You will notice that on the side of the bottle, time frames are listed for each substance that is tested. Wait these listed amounts of time to watch for reactions; otherwise, you could obtain false negative results. If you wait too long to read the results, though, the colors will tend to darken and may blend with adjacent colors. Historically, the urine was evaluated for color, translucency, odor, and taste (yes, taste! Today, while these characteristics are still examined (except, thankfully, taste), we also utilize urinalysis test strips, as we did in Exercise 15-2 (p. In the second part of the exercise, you will research potential causes of the abnormalities that you detected. Use a new strip for each sample, and take care to clean your graduated cylinder thoroughly between each sample that you test. Please note that this is simulated urine rather than real urine, although it contains the same chemicals as real urine and should be handled with equal caution. Compare the resulting colors and patterns on the test strip to those on the key on the bottle. Use your textbook, the internet, or both, as a resource to determine which disease state(s) could lead to the abnormality you detected in each sample. You will examine the path taken by (1) an erythrocyte (a red blood cell), (2) a molecule of glucose, and (3) a molecule of urea. Following are some hints to help you: Remember the basic rules of blood flow: You must pass through a capillary bed in order to get from an artery to a vein. Also recall that there are two capillary beds in the microcirculation of the kidney: the glomerulus and the peritubular capillaries. Similarly, if an item is filtered at the glomerulus, but is never reabsorbed, it must go through the whole nephron and collecting system to end up in the urine. Part 1 Erythrocyte 9 Trace an erythrocyte from the renal artery to the renal vein (remember that glucose is filtered at the glomerulus, but is reabsorbed into the blood). Part 2 Glucose Trace a molecule of glucose from the renal artery to the renal vein (remember that glucose is filtered at the glomerulus, but is reabsorbed into the blood). Capsular space Nephron loop- descending limb Medullary collecting duct Nephron loop- ascending limb Papillary duct Distal tubule Cortical collecting duct 6 Urine drains from the urinary bladder via the a. Your lab partner wonders how the cells of the renal tubules and ducts of the collecting system obtain oxygen and nutrients when their capillary bed is located only in the renal corpuscle. Why do you think this is so, considering the anatomy of the female and male urinary tracts The fluid and solutes in the filtrate have been removed from the blood and are located in the renal tubule. The third and finest filter in the filtration membrane is created by the podocytes and their filtration slits. Substances such as glucose, proteins, and erythrocytes are secreted into the filtrate. Now consider a hydrogen ion that is not filtered but is instead secreted from the peritubular capillaries into the filtrate at the distal tubule. Trace the pathway this hydrogen ion would take from the afferent arteriole to the point at which it exits the body of a male in the urine. The other organ systems we have discussed all function in some manner to help maintain homeostasis of the body. The reproductive system, however, plays a lesser role in maintaining homeostasis and a greater role in perpetuating the species. Finally, we examine the process of development, and the unique anatomy and structures of the developing human. The layer of connective tissue deep to the scrotum extends up into the pelvic cavity to form a structure known as the spermatic cord. On the posterior surface of the urinary bladder, the ductus deferens widens to form its terminal portion, the ampulla.
Discount sevelamer amex
Hence eosinophilic gastritis symptoms discount sevelamer 800mg with mastercard, an abscess or malignant lesion within the parotid gland may result in facial paralysis. Clinical anatomy 15 In addition, the retromandibular vein passes through the anterior portion of the gland and is a useful radiological marker for defining the superficial and deep portions of the gland. The submandibular gland is a mixed serous and mucous salivary gland and forms the majority of saliva production at rest. Its superficial portion fills the space between the mandible and mylohyoid muscle, while its deep part lies between the mylohyoid and hyoglossus. The duct may become obstructed by a calculus, which causes painful enlargement of the gland. The sublingual glands lie anterior to hyoglossus in the sublingual fossa of the mandible. These mucus glands drain via multiple openings into the submandibular duct and sublingual fold of the floor of the oral cavity. Herpes zoster reactivation will result in a pattern of vesicular eruption consistent with the distribution of that division. The parapharyngeal space is a potential space in the form of an inverted pyramid running from the skull base to the greater cornu of the hyoid, bounded by the pharynx medially, pterygomandibular raphe anteriorly and mandible laterally. Peritonsillar or dental infections may spread along this space to form parapharyngeal abscesses requiring urgent drainage. The retropharyngeal space is a midline potential space between the alar and prevertebral faciae, extending from the skull base to the mediastinum. It contains lymphatics draining the nasal and oral cavities, oropharynx and nasopharynx. As such it represents a path of least resistance for infection to spread to the intrathoracic compartment leading to mediastinitis. This article provides a systematic and thorough stepwise guide for clinicians assessing patients. Ensure that both you and the patient are seated comfortably and at the same level. Choose the largest speculum that will fit comfortably into the ear and place it onto the otoscope. Gently pull the pinna upwards and backwards to straighten the ear canal (backwards in children). The pinna is pulled up and back and the tragus pushed forward in order to straighten the external auditory canal during otoscopy. Use the light to observe the direction of the ear canal and the tympanic membrane. The eardrum is better visualized by using the left hand for the left ear and the right hand for the right ear. Adjust your position and the otoscope to view all of the tympanic membrane in a systematic manner. The ear cannot be judged to be normal until all areas of the tympanic membrane are viewed: the handle of malleus, pars tensa, pars flaccida (or attic) and anterior recess. If the view of the tympanic membrane is obscured by the presence of wax, this must be removed. If the patient has undergone mastoid surgery where the posterior ear canal wall has been removed, methodically inspect all parts of the cavity and tympanic membrane or drum remnant by adjusting your position. The normal appearance of a mastoid cavity varies; practice and experience will allow you to recognize pathology. Tuning fork tests can be used to confirm audiometric findings, especially if the hearing test does not seem to be congruent with the clinical findings. They are also useful as a quick bedside test for checking that the patient has not suffered a dead ear following surgery. Low-frequency tuning forks provide greater vibrotactile stimulation (which can be misinterpreted as an audible signal by the patient), while high-frequency tuning forks have a higher rate of decay. There is evidence to suggest, however, that a 256 Hz tuning fork is more reliable than a 512 Hz tuning fork (3, 4). They must be performed in conjunction in order to diagnose a conductive or sensorineural hearing loss. It is essential that the examiner checks that they can hear the tuning fork as this also serves as a comparative test of hearing. The tuning fork is presented to the patient with the prongs of the fork held vertically and in line with the ear canal. The tuning fork is held by the ear for a few moments before its base is firmly pressed against the mastoid process behind the ear. The lamp light can be directed onto the head mirror and the beam focused onto the patient. Examine the profile of the nose, looking for external deviation of the nasal dorsum. Gently raise the tip of the nose to allow you to examine the vestibule of the nose and the anteroinferior end of the nasal septum. Hold the metal loop on your index finger with the finger pointing towards you and the prongs away from you. Swing your middle finger to one side of the Thudichum and your ring finger to the other. You can now squeeze the Thudichum and use the prongs to open the nares to examine the nasal cavity. This provides a view of the nasal septum, inferior turbinate and head of the middle turbinate. A flexible nasolaryngoscope or a rigid endoscope is required in order to assess the middle meatus, posterior nasal cavity and postnasal space. In children, especially if a foreign body is suspected, it is often kinder simply to lift the tip of the nose rather than use a Thudichum speculum. Misting or condensation on the metal surface during expiration provides a measure of nasal patency. Position the patient supine (or sitting in a chair) with the head turned to the opposite side. With the microscope illuminating the ear, take this opportunity to study the pinna, canal opening and surrounding skin for scars or sinuses. Hold the speculum between the index finger and thumb, place the middle finger into the conchal bowl and gently pull the pinna posteriorly. Warn the patient that they will hear a loud hissing noise and may patient to open their mouth (this manoeuvre often increases the anteroposterior diameter of the canal as the condyle of the mandible is related to the anterior canal wall). Remember that the hairy outer third of the canal is relatively insensitive but the thin inner skin is extremely sensitive. Using a wide bore sucker, begin by removing debris within the lateral hairy portion of the canal. Try to remove all the debris, especially in cases of otitis externa where debris will result in an ongoing infection if not removed. If the debris or wax is too hard or the procedure too uncomfortable for the patient, a course of sodium bicarbonate ear drops (two drops three times a day for two weeks) will be required before a further attempt at wax removal is made. If the tympanic membrane is obscured, microsuction along the anterior canal wall until the tympanic membrane is visible (the tympanic membrane is continuous with the posterior canal wall and can be damaged if microsuction follows the posterior canal wall). If there is trauma to the ear canal or if bleeding occurs, prescribe a short course of antibiotic ear drops, warning the patient of the risk of ototoxicity. The nasoendoscope may be used with or without a sheath, depending on local decontamination protocols.
Discount sevelamer 800mg on line
Possible diagnoses are third nerve palsy gastritis diet 4 your blood generic 800mg sevelamer, tonic pupil, pharmacologic mydriasis, or abnormal iris. This restless undulation, called hippus or pupillary unrest, is more prominent in younger patients and during exposure to bright light. Clinicians of the 19th century associated hippus with diverse disorders, ranging from myasthenia gravis to brain tumors, but hippus is now known to be a normal phenomenon. As simple anisocoria waxes and wanes over time, it is the usually same eye that displays the larger pupil. Because both pupillary constrictor muscles normally receive identical signals from the midbrain, they constrict the same amount, which may be small or large depending on the summation of light intensity coming into both eyes. For example, both pupils dilate the same amount in darkness, constrict an identical small amount when a dim light is held in front of one eye, and constrict an identical larger amount when a bright light is held in front of one eye. With a light held in front of one eye, ipsilateral pupillary constriction is called direct reaction to light and contralateral constriction is called consensual reaction. The anatomy of the normal light reflex has two important clinical implications: 1. Because the signal in both outgoing third nerves is identical in these disorders, representing the summation of light intensity from both eyes, the pupils are the same size. Unilateral afferent disease is similar to the experiment of holding a bright light in front of one eye. Asymmetric disease of the efferent connections guarantees that the signals arriving at the pupil are different and therefore that the pupil size will be different. The dotted lines show how nerve impulses from the retina and optic nerve on one side (right eye in this example) contribute to the nerve impulses of both third nerves, via the crossing of the nerve impulses from the nasal retina in the optic chiasm and the abundant interconnections between both pretectal nuclei and both Edinger-Westphal nuclei. The reaction has three parts: (1) constriction of the pupils (pupilloconstrictor muscle), (2) convergence of eyes (medial rectus muscles), and (3) accommodation of the lenses (ciliary body). Marcus Gunn in 1904, it is clear from his report that the sign was generally known to clinicians of his time. Kestenbaum named the finding in 1946 after Marcus Gunn,4 and in 1959 Levatin introduced the swinging flashlight test, which is how most clinicians now elicit the finding. This test compares the amount of pupilloconstriction produced by illuminating one eye with that produced by illuminating the other. Both pupils constrict strongly when the light is shining into the normal eye, but, as the light swings over to illuminate the abnormal eye, both pupils dilate (dilation occurs because the pupils respond as if the light were much dimmer, producing less bilateral constriction-or net dilation-compared with when the light is shining in the normal eye). Because clinicians usually focus on the illuminated pupil, the one that dilates is labeled as having a relative afferent pupillary defect, or the Marcus Gunn pupil. There has been some debate whether eyes with afferent defects also display abnormal pupillary release. To overcome this, the clinician should angle the light by holding the light source slightly below the horizontal axis. Correct interpretation of the test ignores hippus, which otherwise can make interpretation difficult. The clinician should avoid the tendency to linger with the flashlight on the eye suspected to have disease. Uneven swinging of the light may temporarily bleach the retina being illuminated more, thus eventually producing a relative pupillary defect and erroneously confirming the initial suspicion. To avoid this and ensure equal illumination of both retinas, the clinician should silently count: "one, two, switch, one two, switch," and so on. If the patient has only one pupil that reacts to light (see the section on Anisocoria), the test is performed the same way, although the clinician focuses only on the normal iris to interpret the results. A relative afferent defect implies ipsilateral optic nerve disease or severe retinal disease. If the disease is asymmetric, the sensitivity of the finding is 92% to 98%, much higher than that for other tests of afferent function, including visual acuity, pupil cycle times, appearance of optic disc during funduscopy, and visual evoked potentials. During the swinging flashlight test, the pupils constrict when the normal eye is illuminated (rows 2 and 4) but dilate when the abnormal eye is illuminated (rows 3 and 5). Although both pupils constrict or dilate simultaneously, the clinician is usually focused on just the illuminated pupil. The pupil that dilates during the swinging flashlight test has the relative afferent pupillary defect and is labeled the Marcus Gunn pupil. In fact, during the time of Galen, the classical Roman physician, clinicians tested the pupillary light reaction of patients with cataracts to determine whether vision could be restored after couching (couching was an ancient treatment for cataracts that used a needle to displace the cataract posteriorly; a preserved light reaction indicated that the retina and optic nerve behind the cataract were intact). Originally described by Douglas Moray Cooper Lamb Argyll Robertson in 1868, this finding had great significance a century ago because it settled a long-standing debate whether general paresis and tabes dorsalis were the same disease. The pupillary abnormality was found in a high proportion of patients with both diseases and was limited to these diseases, arguing for a common syphilitic origin of both. The introduction of the Wasserman serologic test for syphilis in 1906 confirmed that the two diseases had the same cause. Either of these disorders may eliminate the light reaction when light is directed into the abnormal eye, although the pupils still constrict with the near synkinesis. However, in contrast to other causes of light-near dissociation, optic nerve and retinal disease severely impair vision. Dorsal Midbrain Syndrome (Parinaud syndrome, Sylvian Aqueduct Syndrome, Pretectal Syndrome). Common causes of the dorsal midbrain syndrome are pinealoma in younger patients and multiple sclerosis and basilar artery strokes in older patients. After damage to the third nerve (from trauma, aneurysms, or tumors, but not ischemia), regenerating fibers originally destined for the medial rectus muscle may instead reinnervate the pupillary constrictor, thus causing pupillary constriction during convergence but the absence of reaction to light. However, unlike Argyll Robertson pupils, this finding is unilateral, and most patients also have anisocoria, ptosis, and diplopia. Near-light dissociation was historically associated with von Economo encephalitis lethargica, although experts now believe it indicates that the patient is not trying hard enough to focus on the near object. These patients are invariably comatose from cerebral catastrophes causing elevated intracranial pressure. It represents either a problem with the pupillary constrictor muscle (parasympathetic denervation, iris disorder, pharmacologic pupil) or the pupillary dilator muscle (sympathetic denervation, simple anisocoria). Yes No No Yes Simple anisocoria Yes Horner syndrome Cerebral herniation (Hutchinson pupil) Comatose No 1) Light-near dissociation 2) Supersensitive to topical pilocarpine 1) Chest findings No Yes 2nd-order neuron lesion 1) No light-near dissociation 2) No constriction to pilocarpine 1) Vascular headache Two other tests distinguish Horner syndrome from simple anisocoria: the cocaine or apraclonidine eyedrop tests (see the text) and pupillary dilator lag. Patient 1 (top) has more prominent anisocoria in light than darkness, indicating that the pupillary constrictor of the larger pupil is abnormal. Patient 2 has more prominent anisocoria in darkness than light, indicating that the pupillary dilator of the smaller pupil is abnormal. In patient 2, both pupils will react to light, whereas the larger pupil of patient 1 does not react well to light. If there is a poor light reaction in the eye with the larger pupil, the pupillary constrictor of that eye is abnormal. If there is a good light reaction in both eyes, the pupillary dilator of the eye with the smaller pupil is abnormal. If anisocoria is worse in light than darkness, the pupillary constrictor of the eye with the larger pupil is abnormal. The patient in the bottom row lacks ptosis and ophthalmoplegia, indicating the findings are confined to the pupil itself: possible diagnoses are the tonic pupil, pharmacologic mydriasis, or a disorder of the iris. If an abnormal pupillary constrictor muscle is present, the fixed, dilated pupil is due to parasympathetic defect, iris disorder, or pharmacologic blockade. The most important questions in these patients are: (1) Is there a full third nerve palsy or are the findings confined to the pupillary constrictor Importantly, the abnormal pupil is almost always accompanied by at least some degree of ptosis and ophthalmoplegia. In the normal eye the ciliary ganglion sends 30 times the number of nerve fibers to the ciliary body (the muscle that focuses the lens during the near synkinesis) as to the iris. The pupil of these patients thus fails to respond to light, although during near vision, which normally activates the ciliary body, the misdirected fibers to the iris cause the pupil to constrict. At baseline, there is anisocoria with the right pupil larger than the left (first row). After instillation of dilute pilocarpine eyedrops (fourth row), the pupil constricts markedly. However, most cases are idiopathic, a condition dubbed the Adie pupil (named after William John Adie, although the syndrome was more thoroughly and accurately described by others before his 1931 paper).
Cheap sevelamer 800 mg mastercard
Some investigators have hypothesized that fascial planes connecting the broad ligament and the lower abdominal wall are responsible for the Cullen sign in ectopic pregnancy gastritis y embarazo order sevelamer on line,18 although this does not explain why the sign sometimes appears in patients with free rupture into the peritoneal cavity outside of the broad ligament. It usually presents as a hard dermal or subcutaneous nodule and, in approximately 20% of patients with the lesion, it represents the initial sign of malignancy. Nonetheless, many patients with aneurysms lack this finding, especially if their abdominal girth is large or the aneurysm is small. In the days before clinical imaging, palpation of a relaxed abdomen was so essential that patients with tense abdominal muscles were often reexamined after immersion in a hot bath or after anesthesia had been induced with ether or chloroform, to determine whether an abnormality was present or not. Clinicians have been measuring the liver span ever since Piorry introduced topographic percussion in 1828,2 although after introduction of the x-ray it became apparent that the estimated span often differed from the actual span, leading most clinicians to adopt the view that the percussed liver span was just an index of liver size, not a precise measurement. Clinicians place the upper border too low (2 to 5 cm)4,5 and lower border too high (more than 2 cm in approximately half of patients),4,6 except in patients with chronic obstructive lung disease, in whom the error with the top border is less. After the edge is located, the clinician should note its consistency (a cirrhotic liver is firmer than a healthy one)8 and whether the edge has any irregularities or masses. Moreover, approximately * the normal upper limit for the cephalocaudad dimension of the liver on ultrasonography, from its lower border in the midclavicular line to its upper margin with the lung, is 13 cm. In patients with jaundice the findings of a palpable liver and liver tenderness are unhelpful, both appearing equally often in patients with hepatocellular disease. Nonetheless, the lack of consensus on the proper technique of locating the liver will quickly discourage the serious student of auscultatory percussion. Various experts recommend placing the stethoscope on the xiphoid,4,54 near the umbilicus,55 superior to56 or at the costal margin,57 at four separate positions over the liver,58 or above the suspected center. Only one study supports the technique, showing that 78% of estimates of the lower border are within 2 cm of the actual border (by ultrasonography), compared with 44% for conventional percussion and palpation. One study comparing the different positions found all three to be equivalent21; the approach clinicians use probably depends most on personal preference. In patients with jaundice the palpable spleen modestly increases probability of hepatocellular disease. The clinician percusses the lowest left intercostal space in the anterior axillary line (usually the eighth or ninth); if the percussion note in this location, usually resonant, becomes dull with a full inspiration, the test is positive. The patient is positioned in the right lateral decubitus position, and the clinician percusses from the lower level of pulmonary resonance in the posterior axillary line downwards obliquely to the lower midanterior costal margin. The test is positive if the border of dullness on this line lies more than 8 cm from the costal margin. Its upper border is marked by the limits of cardiac dullness (usually the sixth rib), its lower border is the costal margin, and its lateral border is the anterior axillary line. Although Traube suggested that dullness in this space was a sign of pleural effusion,66 Parrino in 1987 suggested that it could be a sign of splenic enlargement. Traube space dullness becomes even less accurate in overweight patients or those who have recently eaten. Many textbooks call the sign Courvoisier law, as if the positive result were pathognomonic of malignancy, although the Swiss surgeon Courvoisier originally presented the finding in 1890 as only an interesting observation. Some apply it to patients without jaundice (clearly not what Courvoisier intended)71; others define the positive sign as any palpable gallbladder, tender or nontender (some patients with cholecystitis have tender enlarged gallbladders)72-74; and still others expand the positive sign to include a dilated gallbladder discovered during surgery, clinical imaging, or even autopsy. In one series of 86 hospitalized patients with distended gallbladders (as detected by computed tomography or at laparotomy, only 46 (53%) were palpable at the bedside: 83% had a malignant cause of the obstruction and 17% a benign one. Courvoisier original hypothesis-that the gallbladder of choledocholithiasis fails to dilate because its walls are fibrotic from chronic cholecystitis-is probably incorrect because experiments with gallbladders of jaundiced patients show that both dilated and nondilated gallbladders have similar wall stiffness. When analysis is restricted to just those patients with extrahepatic obstruction, the sensitivity of the dilated gallbladder in malignant obstruction today (25% to 55%) is lower than it was for Courvoisier. The reduced sensitivity may simply reflect that patients with malignant obstruction today, compared with those from a century ago, are diagnosed more quickly using clinical imaging, before pressures increase enough to enlarge the gallbladder greatly. This distribution of fluid and air causes four characteristic signs of ascites: (1) Bulging flanks; (2) flank dullness. Flank dullness is positive if there is a horizontal border between dullness in the flank area and resonance (or tympany) in the periumbilical area. Shifting dullness describes flank dullness that shifts as the patient changes position, usually by rolling on to one side. The sign is based on the principle that air-filled loops of intestine, floating on peritoneal fluid, move to the uppermost position in the abdomen. In a patient with a positive response, the border between resonance and dullness shifts away from the side that is most dependent. To elicit the fluid wave, the clinician places one hand against the lateral wall of the abdomen and uses the other hand to tap firmly on the opposite lateral wall. In the positive response the tap generates a wave that is transmitted through the abdomen and felt as a sudden shock by the other hand. In addition to these four signs, most patients with ascites also have edema, from hypoalbuminemia and the weight of the peritoneal fluid compressing the veins to the legs. Findings having relatively little diagnostic value are positive flank dullness, positive bulging flanks, and negative fluid wave. The finding of a flat or everted umbilicus was also diagnostically unhelpful in one study. It is a disorder of elderly patients, affecting 1% to 2% of patients over the age of 50. The clinician should place one hand on each side of the aorta and measure its diameter, subtracting the estimated thickness of two layers of skin and subcutaneous tissue. Most studies do not specifically define the positive finding (instead stating simply the positive finding is "aortic aneurysm present by palpation"), although others define it as an estimated diameter greater than 3 cm using the previously described method. Aneurysms between 3 and 5 cm in diameter are difficult to detect, and if aneurysm is instead defined as a focal bulging more than 5 cm in diameter-the diameter usually indicating surgical repair-the sensitivity of bedside examination increases to more than 80% in almost all series. These results indicate that the negative examination significantly decreases probability of an aneurysm of more than 5 cm in diameter, especially if the patient has a girth of less than 100 cm or has a palpable aorta. The most common cause for a false-positive examination is an abnormally tortuous aorta. The clinical estimation of liver size: a comparison of techniques and an analysis of the source of error. Observer variation in the clinical and radiological assessment of hepatosplenomegaly. The disparity of the size of the liver as determined by physical examination and by hepatic gammascanning in 504 patients. Correlation of liver and spleen size: determinations by nuclear medicine studies and physical examination. The relative accuracy of estimation of enlargement of the liver and spleen by radiologic and clinical methods. The significance of a palpable liver: a correlation of clinical and radioisotope studies. Examiner dependence on physical diagnostic tests for the detection of splenomegaly: a prospective study with multiple observers. Manifestations of metastatic tumors of the liver: a study of eightyone patients subjected to needle biopsy. Decision-making model for a non-invasive diagnosis of compensated liver cirrhosis. New doppler ultrasound signs improve the non-invasive diagnosis of cirrhosis or severe liver fibrosis. Differential diagnosis of jaundice: report of a prospective study of 61 proved cases. Application of a prediction rule to select which patients presenting with lymphadenopathy should undergo a lymph node biopsy. Fever after a stay in the tropics: diagnostic predictors of the leading tropical conditions. Clinical and laboratory predictors of imported malaria in an outpatient setting: an aid to medical decision making in returning travelers with fever. Predictive parameters for a diagnostic bone marrow biopsy specimen in the work-up of fever of unknown origin. Auskultatorische Methode zur bestimmung der Lebergroesse-ein einfaches, probates Schnellverfahren. Splenomegaly at a United States County hospital: diagnostic evaluation of 170 patients. Carcinoma of the pancreas: diagnostic and operative criteria based on one hundred consecutive autopsies. Oxford screening programme for abdominal aortic aneurysm in men aged 65 to 74 years.
Buy discount sevelamer 400 mg online
Identifying the presence of clinically significant hepatic involvement in hereditary haemorrhagic telangiectasia using a simple clinical scoring index gastritis garlic cheap sevelamer american express. Simple data from history and physical examination help to exclude bowel obstruction and to avoid radiographic studies in patients with acute abdominal pain. Disease of a single segment causes claudication; disease of multiple segments causes rest pain and limb-threatening ischemia. Only patients with diabetes or thromboangiitis obliterans develop disease in the peroneotibial segment. Disease in this segment usually causes no claudication in patients with diabetes but causes foot pain in those with thromboangiitis obliterans (Buerger disease). A traditional finding of vessel stenosis is the limb bruit, either iliac (above the inguinal crease), femoral (in the thigh), or popliteal. In patients who have undergone femoral artery puncture for cardiac catheterization, the presence of a continuous femoral bruit. The patient then sits up and dangles the foot over the edge of the examining table, the clinician then recording how long it takes for the vein to rise above the level of the skin surface. In the studies of capillary refill of patients with suspected peripheral vascular disease, investigators applied firm pressure for 5 seconds to the plantar skin of the great toe and then timed how long it took for normal skin color to return after releasing the pressure. Abnormal pallor with elevation and a deep rubor in the lowered position are features of vascular disease. The positive response was abnormal pallor with elevation and the appearance of a dusky red flush spreading proximally from the toes in the dependent position. In another study16 the presence of foot coolness was diagnostically unhelpful, although A. Definition of findings: for limb bruit present, femoral artery bruit23,25,27 or iliac, femoral, or popliteal bruit. In these patients, however, the pulses often diminish or disappear during exercise. Writing soon after Buerger introduced the capillary refill time as a test of peripheral vascular disease (his expression test), Lewis9 and Pickering8 showed it was an unreliable sign because prompt refill could occur from the veins of a limb rendered completely ischemic experimentally. In one study of patients with significant groin hematomas or new limb bruits after cardiac catheterization, two findings were diagnostic. The body normally responds to decreased cardiac output by reducing cutaneous blood flow to the skin, which may produce cool limbs, longer capillary refill times, and mottling of the limbs (mottling is a blotchy or lacelike pattern of dusky erythema). In patients with critical illness, each of these signs, alone or in combination, identifies patients with reduced cardiac output, worse prognosis, or both. Measurement and interpretation of the anklebrachial index: a scientific statement from the American Heart Association. Effect of diagnostic criteria on the prevalence of peripheral arterial disease: the San Luis Valley diabetes study. Indirect systolic pressures and pulse waves in arterial occlusive disease of the lower extremities. A critical evaluation of stress testing in the diagnosis of peripheral vascular disease. The Circulatory Disturbances of the Extremities: including Gangrene, Vasomotor and Trophic Changes. A study of the dorsalis pedis and posterior tibial pulses in one thousand individuals without symptoms of circulatory affections of the extremities. A study of the semeiological reliability of dorsalis pedis artery and posterior tibial artery in the diagnosis of lower limb arterial occlusive disease. The incidence of palpable dorsalis pedis and posterior tibial pulsations in soldiers: an analysis of over 1000 infantry soldiers. Diagnostic utility of the history and physical examination for peripheral vascular disease among patients with diabetes mellitus. Diagnostic value of signs and symptoms associated with peripheral arterial occlusive disease seen in general practice: a multivariable approach. Clinical relevance of pedal pulse palpation in patients suspected of peripheral arterial insufficiency. The accuracy of the physical examination for the detection of lower extremity peripheral arterial disease. The sensitivity, specificity, and predictive value of traditional clinical evaluation of peripheral arterial disease: results from noninvasive testing in a defined population. Ankle-brachial index measured by palpation for the diagnosis of peripheral vascular disease. Pulse oximetry as a potential screening tool for lower extremity arterial disease in asymptomatic patients with diabetes mellitus. Diagnosis of peripheral occlusive disease: comparison of clinical evaluation and noninvasive laboratory. Difficulty in assessing the severity of aortoiliac disease by clinical and arteriographic methods. Predictive value of bruits and doppler pressure measurements in detecting lower limb arterial stenosis. Accuracy of clinical examination in the evaluation of femoral false aneurysm and arteriovenous fistula. Association of physical examination with pulmonary artery catheter parameters in acute lung injury. Less often, they develop over the heel, plantar midfoot, or previous amputation sites. The term ulcer area refers to the product of the maximum ulcer width and maximum ulcer length. Nonetheless, conventional examination often fails to detect diabetic polyneuropathy, and approximately half of patients with diabetic ulceration lack complaints of numbness or pain3 and can still detect the touch of a cotton wisp or pinprick. To use the monofilament, the patient should be lying supine with eyes closed, and the monofilament should be applied perpendicular to the skin with enough force to buckle it for approximately 1 second. The patient responds "yes" each time he or she senses the monofilament as the clinician randomly tests each site on the foot multiple times. In clinical studies, anywhere from 1 to 10 different sites on the foot are tested, but each study defines the abnormal result as inability to consistently sense the monofilament at any site. Testing the plantar surface of the first and fifth metatarsal heads may be the most efficient and overall accurate bedside maneuver. However, it is also possible that a better indicator of protective sensation is one of the other seven monofilaments between 6. Although historically the most common causes were syphilis (affecting the larger joints of the lower extremity) and syringomyelia (affecting the larger joints of the upper extremity), the most common cause currently is diabetes. One proposed test is the probe test, in which the clinician gently probes the ulcer base with a sterile, blunt, 14. The test is positive, suggesting osteomyelitis, if the clinician detects a rock-hard, often gritty structure at the ulcer base without any intervening soft tissue. Definition of findings: for positive probe test, ulcer area, and predictors of nonhealing wound, see text. The findings of erythema, swelling, or purulence are unhelpful in diagnosing osteomyelitis. In one study of more than 27,000 diabetic foot ulcers treated with debridement, moist wound dressings, and measures to reduce pressure on the foot. The prevalence and incidence of lower extremity amputation in a diabetic population. The prevalence of foot ulceration and its correlates in type 2 diabetic patients: a population-based study. Comparison of quantitative sensory-threshold measures for their association with foot ulceration in diabetic patients. Clinical examination versus neurophysiological examination in the diagnosis of diabetic polyneuropathy. Possible sources of discrepancies in the use of the Semmes-Weinstein monofilament. Neuro-arthropathy (Charcot joints) in diabetes mellitus (clinical study of 101 cases). Probing to bone in infected pedal ulcers: a clinical sign of underlying osteomyelitis in diabetic patients. Identifying diabetic patients at high risk for lower-extremity amputation in a primary health care setting.
Order cheap sevelamer on line
The advanced training includes tissue-preparation techniques gastritis pain after eating discount sevelamer online mastercard, microscopy, cytochemistry, anatomy and physiology, histology, immunology, and other subjects. Similarities and differences between lysosomes and peroxisomes in structure, contents, and functions 9. How proteins are processed and secreted after their assembly on a ribosome Assess Your Learning Outcomes To test your knowledge, discuss the following topics with a study partner or in writing, ideally from memory. Structural and functional distinctions between microvilli, cilia, flagella, and pseudopods 5. Structural distinctions and respective advantages of three types of cell junctions-tight junctions, desmosomes, and gap junctions 6. What organelles have in common and how they differ, as a class, from other cellular components 4. Structure of the nucleus, particularly of its nuclear envelope, chromatin, and nucleoli 5. Two forms of endoplasmic reticulum, their spatial relationship, their structural similarities and differences, and their functional differences 6. Structure of the Golgi complex and its role in the synthesis, packaging, and secretion of cell products 4. Cells specialized for absorption of matter from the extracellular fluid are likely to show an abundance of a. A serves as a mechanical linkage between adjacent cells but does not obstruct the movement of materials through the space between cells. Cells are somewhat protected from mechanical trauma by a spongy carbohydrate surface coat called the. A cell specialized for absorption would be expected to have a high density of cilia on its surface. A cell can release its secretory products by exocytosis, phagocytosis, or pinocytosis. Cells of the digestive glands store enzymes in their lysosomes and release them into the digestive tract when needed to digest food. White blood cells can move about in the tissues by means of either cilia or pseudopods. Identify which organelles of the mammary gland cells are involved in synthesizing and secreting these components, and describe the structural pathway from synthesis to release from the cell. A person with lactose intolerance cannot digest lactose, so instead of being absorbed by the small intestine, this sugar passes undigested into the large intestine. Which of the membrane transport processes do you think is most directly involved in the diarrhea Consider a cardiac muscle cell, an enzyme-producing pancreatic cell, a phagocytic white blood cell, and a hormone-secreting cell of the ovary. The synchronized beating of such cilia serves to move an egg or embryo toward the uterus. For example, these trillions of cells belong to only 200 types or so, and are organized into tissues that fall into just four broad categories-epithelial, connective, nervous, and muscular. An organ is a structure with discrete boundaries that is composed of two or more of the main tissue types (usually all four). Organs derive their function not from their cells alone but from how the cells are organized into tissues. This article describes the structural and functional characteristics of the major human tissues, and later chapters describe the histological organization of the respective organ systems. With its 50 trillion cells and thousands of organs, the human body may seem to be a structure of forbidding complexity. ThePrimaryTissueClasses Histology1 is the study of tissues and how they are arranged into organs. A tissue is a group of similar cells and cell products that arise from the same region of an embryo and work together to perform a specific structural or physiological role in an organ. The matrix (extracellular material) is nonliving matter secreted by the tissue cells. In summary, a tissue is composed of cells and matrix, and the matrix is composed of fibers and ground substance. These stains lend contrast to such structures as cell nuclei, cytoplasm, and extracellular fibers, but one must remember that these colors are entirely artificial; they do not represent the natural colors of the organs. You must keep this in mind and try to translate the microscopic image into a mental image of the whole structure, like trying to imagine what a whole loaf of bread looks like if you had seen only a few slices. Note that grazing sections (upper left and right) would miss the yolk, just as a tissue section may miss the nucleus of a cell and create an illusion that the cell did not have one. A section far from the bend would give the impression of two separate tubules; a section near the bend would show two interconnected lumina (interior spaces); and a section still farther down could miss the lumen completely. With experience, however, one recognizes that the separated pieces are parts of a single tube winding its way to the organ surface. Apply What You Know How would a cylindrical blood vessel look in two dimensions if cut lengthwise (a longitudinal section); if cut perpendicular to this (a cross section); and if cut on a slant between these two (an oblique section) CellShapes Descriptions of organ and tissue structure often refer to the shapes of the cells by the following terms (fig. Squamous cells line the esophagus and form the surface layer (epidermis) of the skin. Columnar-distinctly taller than wide, such as the inner lining cells of the stomach and intestines. Squamous, cuboidal, and columnar cells often look polygonal when viewed from above rather than from the side. Classify each of the following into one of the four primary tissue classes: the epidermis, fat, the spinal cord, most heart tissue, bones, tendons, blood, and the inner lining of the stomach. What is the term for a thin, stained slice of tissue mounted on a microscope slide Epithelial tissue, or epithelium,5 consists of a flat sheet of closely spaced cells, one or more cells thick, like bricks in a wall. The upper surface is usually exposed to the environment; to an internal space of a body cavity; or to the lumen, or internal space, of a hollow organ. Epithelium covers the body surface, lines body cavities, forms the external and internal linings of many organs, and constitutes most gland tissue. Epithelia contain no blood vessels, but they almost always lie on a layer of loose connective tissue and depend on its blood vessels for nourishment and waste removal. Between an epithelium and the underlying connective tissue is a layer called the basement membrane, composed mainly of protein. The cell surface attached to the basement membrane is called the basal surface; the upper surface, opposite from this, is the apical surface; and the lateral surfaces between these two form the sides of the cell. These surfaces often differ in their functions (such as absorption, secretion, attachment, or intercellular communication) and therefore differ in the components of their plasma membranes. Epithelia are classified into two broad categories-simple and stratified- with four types in each category. In a simple epithelium, every cell touches the basement membrane, whereas in a stratified epithelium, some cells rest on top of other cells (like a multistory apartment building) and do not extend to the basement membrane (fig. Three types of simple epithelia are named for the shapes of their cells: simple squamous (thin scaly cells), simple cuboidal (squarish or rounded cells), and simple columnar (tall narrow cells). In the fourth type, pseudostratified columnar, not all cells reach the free surface; the shorter cells are covered over by the taller ones, but all of them reach the basement membrane-much like trees in a forest that reach different heights but are all anchored in the soil below. Simple columnar and pseudostratified epithelia often produce protective mucous coatings. Pseudostratified columnar epithelium is a special type of simple epithelium that gives a false impression of multiple cell layers. Three of the stratified epithelia are named for the shapes of their surface cells: stratified squamous, stratified cuboidal, and stratified columnar epithelia. The fourth type, transitional epithelium, was named when it was thought to represent a transitional stage between stratified squamous and stratified columnar epithelium. Stratified columnar epithelium is rare (occurring in short transitional zones where one epithelium type grades into another) and we will not consider it any further. The most widespread epithelium in the body is stratified squamous epithelium, which deserves further discussion.