Buy tamoxifen on line amex
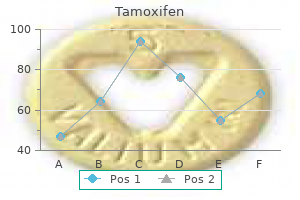
Note that an increase in extracellular K+ women's health clinic liverpool 20 mg tamoxifen amex, that is, hyperkalemia, will depolarize cells, whereas hypokalemia will hyperpolarize cells. This results in an inward current of Na+, which causes further depolarization, which then opens additional Na+ channels. This regenerative (positive feedback) cycle quickly produces an overshooting action potential. Axonal action potentials last only a few milliseconds because two mechanisms rapidly repolarize the membrane. One is the activation of voltagegated K+ channels that open with a slight delay compared with the Na+ channels, resulting in the delayed rectifier outward current carried by K+ ions. Thus, depolarization initially opens Na+ channels (activation) but then closes Na+ channels (inactivation), and the channels remain closed until the membrane repolarizes to a level close to the normal resting potential. This means that prolonged depolarization produced for example, by hyperkalemia, can make excitable cells inexcitable. Inactivation of Na+ channels completely prevents action potential initiation, causing the absolute refractory period. After Na+ inactivation is removed by repolarization, the membrane remains less excitable than normal during the relative refractory period, during which the delayed rectifier K+ channels are transiently open. The action potential propagates because the depolarization and overshoot in an active region (where voltage-gated Na+ channels are open) spread passively by electrotonic conduction to adjacent regions, depolarizing those regions and triggering the same regenerative sequence when the neighboring Na+ channels are opened by the electrotonically conducted depolarization. Electrotonic conduction occurs because the positive Na+ ions entering the cell in the active region are attracted to the net negative charge inside neighboring membrane that is hyperpolarized, and neighboring anions are attracted to the These intracellular and extracellular currents combine in a local circuit that quickly depolarizes membrane adjacent to an active region. Current density underlying electrotonic propagation of depolarization (or hyperpolarization) declines exponentially with distance. The effectiveness of electrotonic propagation often is compared by using the space or length constant, which varies with the square root of the diameter of the axon. This means that electrotonic propagation of current in front of an active region projects farther in axons with larger diameters and therefore that conduction of action potentials is faster in larger axons. The velocity of action potential conduction also depends on how much time it takes for a region of membrane to depolarize. This is characterized by the time constant, which varies directly with membrane resistance Rm and membrane capacitance Cm. If Rm or Cm is large, the rate with which a region of membrane can depolarize (or hyperpolarize) is slow, and this reduces the velocity of action potential conduction. Mammals have increased action potential velocity by myelinating many axons, which in effect reduces Cm. The most rapidly conducting axons are both myelinated and have large diameters (ie, have small and large). Demyelinating diseases such as multiple sclerosis profoundly decrease conduction velocity and cause serious neurologic problems. Instantaneous elimination of which of the following would most rapidly bring Vm close to 0 mV Which of the following best describes the effect of increased extracellular potassium [K+]o If the conduction velocity were found to be augmented, which of the following characteristics would most likely be decreased Action potential amplitude Effective membrane capacitance the concentration gradient for Na+ the rate at which Na+ channels open in response to depolarization Na+ channel density uniformly along a fiber Answers [3. The immediate cause of the resting potential is the high membrane permeability to K+ compared with other ions; if this permeability were to be eliminated, Vm would instantly depolarize to within several mV of 0 mV. The diffusion of K+ down its concentration gradient in the absence of diffusion of anions out of the cell or diffusion of other cations into the cell causes a slight separation of charge across the membrane that generates most of the resting potential. The active transport of K+ into the cell (not, as in answer A, out of the cell) is necessary for setting up the concentration gradient that results in the diffusion of K+ out of the cell. This gradient (and therefore Vm) would take a long time to dissipate if active transport were stopped. Because the membrane is effectively impermeable to Na+ at rest, the transport and concentration gradient for Na+ has very little effect on the resting potential (answers B, C, and E). Sustained depolarization, as occurs with hyperkalemia, inactivates voltage-gated Na+ channels, which remain inactivated until the membrane repolarizes, thus blocking action potential generation. If action potentials are generated, their amplitude will be reduced (answer A), but this is a consequence rather than a cause of reduced excitability. Hyperpolarization also can reduce excitability by increasing the depolarization needed to reach action potential threshold (answers C and D), but this would be produced by hypokalemia, not by hyperkalemia. There is no evidence that prolonged hyperkalemia decreases the number of Na+ channels in the membrane (answer E). Effective membrane capacitance is decreased in many mammalian axons by myelination-the tight wrapping of many glial membranes around the axon, which is functionally equivalent to increasing the thickness of the membrane. Decreasing action potential amplitude (answer A) will decrease rather than increase action potential velocity (see Case 8), as will decreasing the concentration gradient for Na+ (because this will reduce action potential amplitude). In addition, decreases in the opening rate or density of Na+ channels will decrease conduction velocity. The resting potential and action potential in simple excitable systems, such as axons, that are permeable only to K+ and Na+, can be described by the Goldman-Hodgkin-Katz equation, which states that Vm is determined by opposing currents carried by K+ and Na+, which are determined entirely by (1) the ratio of permeabilities to K+ and Na+ and (2) their concentration gradients across the cell membrane. Inactivation of Na+ channels during an action potential prevents subsequent action potential initiation during the brief absolute refractory period, whereas the relative refractory period continues shortly thereafter because the delayed rectifier K+ channels remain open for a somewhat longer period. The spread of depolarization in front of an active region of membrane during an action potential occurs by electrotonic propagation, which is characterized by an exponential decay of the depolarization with distance along the fiber. The velocity of action potential conduction is increased by myelinating axons, which decreases their effective membrane capacitance, and by increasing the fiber diameter, which decreases the intracellular resistance. She states that when she eats certain foods that require a significant amount of chewing (meat), her jaw muscles become weak and "tired. How would a large reduction in extracellular [Ca2+] affect synaptic transmission at the neuromuscular junction The net effect is depolarization that reaches action potential threshold in the muscle cell. Myasthenia gravis is seen more commonly in females, with peak incidence at 20 to 30 years of age. This reduces twitch summation, causing weakness and fatigue, and explains the classic symptoms of myasthenia gravis: muscle weakness that increases with repetitive muscle use (eg, chewing) and partially recovers with rest. Ionotropic receptor: A receptor that is also an ion channel and therefore produces a change in membrane potential when binding of a neurotransmitter opens (or, in some cases, closes) the channel. Metabotropic receptor: A receptor that is linked by signal transduction pathways to potentially diverse cellular responses, including effects on ion channels (not directly linked to the receptor), neurotransmitter release, and gene transcription. Synaptic transmission begins when an action potential propagates from the main axon into the endplate. The channels are equally permeable to Na+, which flows into the cell, and to K+, which flows out of the cell. The combined Na+ and K+ current depolarizes the muscle cell from its resting potential (-80 mV) to the threshold for the action potential (-50 mV), with the resulting action potential propagating across the entire muscle cell. Chemical transmission at other synapses also involves Ca2+-dependent exocytosis of neurotransmitters but can differ in the neurotransmitter released, the receptors bound by the neurotransmitter, the ions involved in mediating the postsynaptic response, and whether metabolic responses are involved. Inhibitory ligand-gated channels often are selectively permeable to Cl-, which usually has an equilibrium potential slightly negative to the resting potential of the neuron. Opening channels permeable to Cl- Opening channels permeable to Ca2+ Opening channels permeable to Na+ and K+ Closing channels permeable to Na+ Closing channels permeable to Cl- and K+ [4. Temporal summation and spatial summation onto the postsynaptic cell increase the likelihood that a postsynaptic action potential will be evoked. All the other features listed are shared by the neuromuscular junction and excitatory chemical synapses in the brain. The duration of brief postsynaptic potentials mediated by ionotropic receptors is limited by enzymatic degradation of neurotransmitter, its diffusion away from the active zones and its active transport into the terminal and nearby cells. Temporal and spatial summation is unnecessary and does not occur at the neuromuscular junction. Opening these channels opposes the depolarizing effects of excitatory synapses that are active at the same time. In many modulatory synapses, neurotransmitter binds to metabotropic receptors that are coupled via G proteins to cell-signaling cascades, which can produce neuronal alterations ranging in duration from tens of seconds to weeks or longer. On examination she is found to have dyspnea with audible wheezes and is diagnosed with asthma. The patient is given an inhaled medication (albuterol), which provides immediate relief of the bronchial constrictive symptoms. The sympathetic 2 receptor agonist albuterol selectively produces bronchial dilation and thus provides relief from bronchial constrictive disorders such as asthma. However, with some receptors it is not possible to achieve selective targeting because the same receptor is found in diverse organs, and many commonly used drugs act on more than one receptor. For example, propranolol, which is used to treat various cardiac and cardiovascular problems, blocks both 1 and 2 receptors. Definitions Parasympathetic nervous system: Division of the autonomic nervous system associated with resting visceral functions.
Purchase tamoxifen 20 mg online
The pneumatic tonometer menopause and pregnancy order tamoxifen 20mg overnight delivery, or pneumatonometer, is an applanation tonometer that shares some characteristics with the Mackay-Marg-type devices. It has a cylindrical air-filled chamber and a probe tip covered with a flexible, inert silicone elastomer (Silastic membrane) diaphragm. Because of the constant flow of air through the chamber, there is a small gap between the diaphragm and the probe edge. Because this instrument covers only a small area of the cornea, it is especially useful in eyes with corneal scars or edema. Noncontact tonometers are often used in large-scale glaucoma-screening programs or by nonmedical health care providers. In addition, indicators of ocular biomechanical properties are calculated, including corneal hysteresis and corneal resistance factor. Rebound tonometers are portable, and topical anesthesia is not required, making them particularly suitable for pediatric populations. The amount of indentation is read on a linear scale on the instrument and converted to mm Hg by a calibration table. This test may be useful in uncooperative patients; however, the results may be inaccurate even when the test is performed by very experienced clinicians. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. Infection control in clinical tonometry Many infectious agents-including the viruses responsible for acquired immunodeficiency syndrome, hepatitis, and epidemic keratoconjunctivitis-can be recovered from tears. Tonometers must be cleaned after each use so that the transfer of such agents can be prevented. For Goldmann-type tonometers and the Perkins tonometer, the tonometer tips (prisms) should be cleaned immediately after use. The prisms should be soaked in a 1:10 sodium hypochlorite solution (household bleach), in 3% hydrogen peroxide, or in 70% isopropyl alcohol for 5 minutes and rinsed and dried before reuse. If alcohol is employed, it should be allowed to evaporate or the prism head should be dried before reuse to prevent damage to the corneal epithelium. Clinical evaluation of the glaucoma patient should include a history of the current complaint, including symptoms, onset, duration, and severity. The clinician should inquire about symptoms often associated with glaucoma, such as pain, redness, colored halos around lights, alteration of vision, and loss of vision. Such conditions include diabetes mellitus, cardiac and pulmonary disease, hypertension, hemodynamic shock, systemic hypotension, sleep apnea, Raynaud phenomenon, migraine and other neurologic diseases, renal stones, and pregnancy. The clinician should take note of a history of corticosteroid use, either topical or systemic. The hyperopic eye is at increased risk of angle-closure and generally has a smaller optic nerve head (also called optic disc). Myopia is associated with optic nerve head morphologies that can be clinically confused with glaucoma, and myopic eyes are at increased risk of pigment dispersion. External Adnexae Examination and assessment of the external ocular adnexae is useful for determining the presence of a variety of conditions associated with secondary glaucomas as well as external ocular manifestations of glaucoma therapy. An example of an association between adnexal changes and systemic disease is tuberous sclerosis (Bourneville syndrome), in which glaucoma may occur secondary to vitreous hemorrhage, anterior segment neovascularization, or retinal detachment. Typical external and cutaneous signs of tuberous sclerosis include a hypopigmented lesion termed the "ash-leaf sign" and a red-brown papular rash (adenoma sebaceum) that is often found on the face and chin. Other changes in the ocular adnexa associated with secondary glaucoma include the subcutaneous plexiform neuromas that are a hallmark of the type 1 variant of neurofibromatosis, the yellow and/or orange papules in juvenile xanthogranuloma, and the skin pigmentation seen in oculodermal melanocytosis (nevus of Ota). Several entities are associated with signs of elevated episcleral venous pressure (see the section Elevated Episcleral Venous Pressure in Chapter 4). The presence of a facial cutaneous angioma (nevus flammeus, or port-wine stain) can indicate encephalofacial angiomatosis (Sturge-Weber syndrome). Orbital varices, arteriovenous fistulas, and superior vena cava syndrome may also be associated with elevated episcleral venous pressure and secondary glaucoma. Intermittent unilateral proptosis and dilated eyelid veins are key external signs of orbital varices. Carotid-cavernous, dural-cavernous, and other arteriovenous fistulas can produce orbital bruits, restricted ocular motility, proptosis, and pulsating exophthalmos. Superior vena cava syndrome can cause proptosis and facial and eyelid edema, as well as conjunctival chemosis. Thyroid eye disease may also be associated with glaucoma; ophthalmic features of this disease include exophthalmos, eyelid retraction, and motility disorders. Use of prostaglandin analogues may result in cosmetic changes to the ocular adnexa; these are described in Chapter 7. Pupils Pupil size may be affected by glaucoma therapy, and pupillary responses are one measure of adherence in patients who are on miotic therapy. Testing for a relative afferent pupillary defect may detect asymmetric optic nerve damage. Corectopia, ectropion uveae, and pupillary abnormalities may also be observed in some forms of secondary open-angle glaucoma and angle-closure glaucoma. In some clinical situations, it is not possible to assess the pupils objectively for the presence of a relative afferent defect, and a subjective comparison between the eyes of the perceived brightness of a test light may be helpful. Testing for color vision, extraocular motility, and cranial nerve abnormality can also be helpful in the differential diagnosis of nonglaucomatous versus glaucomatous optic neuropathy. Biomicroscopy Biomicroscopy of the anterior segment is performed for signs of underlying ocular conditions that may be associated with glaucoma. Long-term use of sympathomimetics and prostaglandin analogues may also cause conjunctival hyperemia, and long-term use of epinephrine derivatives may result in black adrenochrome deposits in the conjunctiva. Allergic reaction to ocular hypotensive medications (especially 2-adrenergic agonists) may be accompanied by a follicular reaction. The use of topical ocular hypotensive medication can also cause decreased tear production, allergic and hypersensitivity reactions (papillary and follicular conjunctivitis), foreshortening of the conjunctival fornices, and scarring. Prior to filtering surgery, the presence or absence of subconjunctival scarring or other conjunctival abnormalities should be assessed. If a bleb is present, its size, height, degree of vascularization, and integrity should be noted, and in the situation of postoperative hypotony, a Seidel test performed. Episclera and sclera Dilation of the episcleral vessels may indicate elevated episcleral venous pressure, as seen in the secondary glaucomas associated with Sturge-Weber syndrome, arteriovenous fistulae, or thyroid eye disease. Oculodermal melanocytosis may affect the sclera, and affected patients are at increased risk for glaucoma and ocular melanoma. Cornea Enlargement of the cornea associated with breaks in the Descemet membrane (Haab striae) is commonly found in developmental glaucoma patients. Glaucomas associated with other anterior segment anomalies are described in the following discussions. Punctate epithelial defects, especially in the inferonasal interpalpebral region, are often indicative of medication toxicity. The following corneal endothelial abnormalities can be important clues to underlying associated secondary glaucoma: Krukenberg spindle in pigmentary glaucoma deposition of exfoliative material in pseudoexfoliation syndrome keratic precipitates in uveitic glaucoma irregular and vesicular lesions in posterior polymorphous dystrophy a "beaten bronze" appearance in the iridocorneal endothelial syndrome large posterior embryotoxon in Axenfeld-Rieger syndrome the clinician should note the presence of traumatic or surgical corneal scars. In the Van Herick method of estimating angle width, the examiner projects a narrow slit beam onto the cornea, just anterior to the limbus. This method may miss narrow angles or angle closure and is not a substitute for gonioscopy, which is discussed in detail later in this chapter. Iris masses, choroidal effusions, or trauma can produce an irregular iris surface contour and nonuniformity or asymmetry in anterior chamber depth. In many circumstances, especially in the assessment of narrow-angle glaucoma, comparing the chamber depth of the 2 eyes is of substantial value. The presence of inflammatory cells, red blood cells, floating pigment, or inflammatory debris (such as fibrin) should be noted. The degree of inflammation (flare and cell) and presence of pigment should be determined before instillation of eyedrops. The clinician should note heterochromia, iris atrophy, transillumination defects, ectropion uveae, corectopia, nevi, nodules, and exfoliative material. Early stages of neovascularization of the anterior segment may appear as either fine tufts around the pupillary margin or a fine network of vessels on the surface of the iris adjacent to the iris root. The clinician should also examine the iris for evidence of trauma, such as sphincter tears or iridodonesis.
Diseases
- Abasia
- Desmoplastic small round cell tumor
- Teebi Naguib Alawadi syndrome
- Goldberg Bull syndrome
- Delta-1-pyrroline-5-carboxylate dehydrogenase deficiency
- Motor neuropathy
- Chromosome 5, uniparental disomy
- Short stature talipes natal teeth
- Symphalangism with multiple anomalies of hands and feet
Purchase cheapest tamoxifen and tamoxifen
Concussive Trauma Subconjunctival Hemorrhage Blood under the conjunctiva creates a dramatic appearance that can alarm the patient menstrual weight buy 20 mg tamoxifen free shipping. Most frequently, patients present with subconjunctival hemorrhage without a history of antecedent trauma. When trauma has occurred, damage to deeper structures of the eye must be ruled out. Subconjunctival hemorrhage is usually not associated with an underlying systemic disease and rarely has an identifiable cause. Occasionally, a history of vomiting, coughing, or other forms of the Valsalva maneuver can be elicited (Table 13-3). However, if a patient suffers from repeated episodes of spontaneous subconjunctival hemorrhage or indicates the presence of a possible bleeding diathesis (easy bruising, frequent bloody noses), a careful medical evaluation may be warranted. Recurrent subconjunctival hemorrhages can be seen in association with systemic illness such as uncontrolled hypertension, diabetes mellitus, or a bleeding diathesis. This condition should be treated with intensive topical lubrication and, occasionally, patching until resolved. Patients should be warned that the hemorrhage might spread around the circumference of the globe before it resolves and that it may change in color from red to yellow during its dissolution. Corneal Changes Blunt trauma to the cornea can result in abrasions, edema, tears in Descemet membrane, and corneoscleral lacerations, usually located at the limbus. Traumatic posterior annular keratopathy or traumatic corneal endothelial rings have also been described. The rings, composed of disrupted and swollen endothelial cells, are whitish gray in appearance and occur directly posterior to the traumatic impact. The endothelial rings appear within several hours of a contusive injury and usually disappear within a few days. Traumatic Mydriasis and Miosis Blunt injury to the globe may result in traumatic mydriasis or, less commonly, miosis. Traumatic mydriasis is often associated with iris sphincter tears that can permanently alter the shape of the pupil. Miosis tends to be associated with anterior chamber inflammation (traumatic iritis; see the following section). Traumatic Iritis Photophobia, tearing, and ocular pain may occur within 24 hours after injury. The inflammation of traumatic iritis is often associated with diminished vision and perilimbal conjunctival injection. The anterior chamber reaction can be surprisingly minimal but is usually present if carefully sought. Treatment should consist of, at the very least, a topical cycloplegic agent to relieve patient discomfort. Once the iritis has diminished, cycloplegia may be discontinued, and topical corticosteroids should be tapered slowly to prevent rebound iritis. Frequently, anterior segment hemorrhage ensues, and the iridodialysis may not be recognized until the hyphema has cleared. A large dialysis may cause polycoria and monocular diplopia, requiring surgical repair. Cyclodialysis Traumatic cyclodialysis is characterized by a separation of the ciliary body from its attachment to the scleral spur, resulting in a cleft. Gonioscopically, this cleft appears at the junction of the scleral spur and the ciliary body band. A cyclodialysis cleft can cause increased uveoscleral outflow and aqueous hyposecretion, leading to chronic hypotony and macular edema. If treatment with topical cycloplegics does not suffice, closure may be attempted by using argon laser, diathermy, cryotherapy, or direct suturing. It results from injury to the vessels of the peripheral iris or anterior ciliary body. At other times, the bleeding is so subtle that it can be detected only as a few circulating red blood cells on slit-lamp examination (microscopic hyphema). The prognosis is good in patients who do not develop complications, but it is not dependent on the size of the hyphema itself. Hyphema is frequently associated with corneal abrasion, iritis, and mydriasis, as well as with significant injuries to the angle structures, lens, posterior segment, and orbit. Juvenile xanthogranuloma, retinoblastoma, and leukemia are associated with spontaneous hyphema in children. Rebleeding the major concern after a traumatic hyphema is rebleeding, for which most studies report an incidence of less than 5%. Rebleeding may complicate any hyphema, regardless of size, and occurs most frequently between 3 and 7 days after injury. The timing of the rebleeding may be related to the lysis and clot retraction that occur during this period. Red blood cells within the anterior chamber release hemoglobin that penetrates the posterior corneal stroma, where it is absorbed by keratocytes. Hemoglobin is converted to hemosiderin within the keratocytes, which in turn causes keratocyte death. On slit-lamp examination, early blood staining is detected by yellow granular changes and reduced fibrillar definition in the posterior corneal stroma. Blood staining leads to a reduction in corneal transparency that may be permanent. Histologically, red blood cells and their breakdown products can be seen within the corneal stroma. Corneal blood staining often slowly clears in a centripetal pattern starting in the periphery. Blunt force applied to the eye displaces the aqueous volume peripherally, causing an increase in hydraulic pressure at the lens, iris root, and trabecular meshwork. If this "wedge of pressure" exceeds the tensile strength of ocular structures, the vessels in the peripheral iris and face of the ciliary body may rupture, leading to hyphema. The force may cause scleral ruptures, typically at the limbus and posterior to the muscle insertions, where the sclera is thinner and unsupported by the orbital bones. Severe trauma leads to subluxation of the lens, retinal dialysis, optic nerve avulsion, and/or vitreous hemorrhage. Medical management the overall treatment plan for traumatic hyphema should be directed at minimizing the possibility of secondary hemorrhage. Specifics of medical management remain controversial; however, most patients are treated with the following: protective shield over the injured eye, restriction of physical activity, elevation of the head of the bed, and daily observation. To reduce the risk of rebleeding, nonaspirin analgesics should be used for pain relief; however, even nonsteroidal anti-inflammatory medications can increase the risk of rebleeding. But if satisfactory home care and outpatient observation cannot be ensured, hospitalization may be required. Most ophthalmologists administer long-acting topical cycloplegic agents initially for comfort, to facilitate posterior segment evaluation, and to eliminate iris movement. Topical corticosteroids are beneficial in controlling anterior chamber inflammation and preventing synechiae formation, and they may play a role in preventing rebleeding. Oral corticosteroids may be used to facilitate the resolution of severe inflammation and/or to prevent rebleeding. Topical antihypertensives (-blockers and -agonists) are the mainstay of therapy, although occasionally intravenous or oral hyperosmotic agents may be required. Surgery is generally recommended at the earliest definitive detection of blood staining. Patients with preexisting optic nerve damage or sickle hemoglobinopathies may require earlier intervention. Table 13-4 the simplest surgical technique is anterior chamber irrigation with balanced salt solution through a paracentesis. The goal is to remove circulating red blood cells that may obstruct the trabecular meshwork; removal of the entire clot is neither necessary nor wise. If irrigation is not successful, the I/A handpiece, which integrates irrigation and aspiration in cataract surgery, may be effective in many cases. The use of a cutting instrument or intraocular diathermy may be necessary in severe cases.
Cheap tamoxifen 20mg with amex
The diagnosis is presumed when there is increased cortisol production and failure to suppress cortisol secretion with dexamethasone menstrual problems discount tamoxifen 20 mg with mastercard. Medical management of adrenal hyperplasia may include the use of ketoconazole or other medications that inhibit steroidogenesis. Glucocorticoids: Steroid hormones, primarily cortisol, secreted by the adrenal cortex that promote the synthesis of enzymes involved in energy balance and fuel utilization. Mineralocorticoids: Steroid hormones, primarily aldosterone, that are secreted by the adrenal cortex and are essential for the maintenance of salt and water balance by the kidney. The adrenals form a complex structure consisting of functionally and morphologically distinct regions: an outer region, the adrenal cortex, and the inner medulla. The adrenal cortex is the site of synthesis and secretion of steroid hormones known as the mineralocorticoids, the glucocorticoids, and the androgens. The bulk of the adrenal gland is the cortex, which is composed of morphologically and functionally distinct segments. Descending into the gland just below the capsule is the zona glomerulosa, clusters of cells that secrete the mineralocorticoid aldosterone. The zona fasciculata penetrates deeply into the cortex and overlays the zona reticularis. The adrenal medulla is heavily innervated and is a source of the circulating sympathetic hormones epinephrine and norepinephrine. Regulation of Adrenal Cortical Hormone Secretion the rate of secretion of the adrenal cortical hormones is dependent on their rate of production. Unlike the peptide hormones, for example, the steroid hormones are permeable to the plasma membranes of cells, and their concentration in the cell is the determinant of the rate at which they leave the cell and enter the plasma. In the plasma, they bind to and are transported by globular proteins such as corticosteroid-binding protein and albumin. The adrenal cortical hormones act on target tissues by diffusing into the cell and forming a complex with a specific intracellular receptor. The mechanism of cortisol inhibition involves cortisol binding to corticosteroid receptors in these tissues and inhibition of specific gene transcription. The failure to lower cortisol production indicates a nonpituitary source of the problem. Physiology of Glucocorticoids Cortisol has a permissive effect on a number of enzymes that mediate the breakdown of fats and protein and hepatic glucose production and is essential for the maintenance of energy balance and fuel utilization in the body. Cortisol also has potent anti-inflammatory and immunosuppressant activities that make it an extremely important therapeutic agent. The glucocorticoids, primarily cortisol and to a lesser extent corticosterone, play a central role in the physiologic response to stress, and their secretion is increased during stress. The physiology of the glucocorticoids is complex and can influence and alter the function of every system in the body. The dominant and most crucial functions involve energy metabolism through the control of the expression of proteins that are essential for the maintenance of energy balance during periods of food deprivation. During periods of fasting, the body rapidly exhausts its carbohydrate supplies and depends on other sources of fuel for metabolic energy. In the liver, cortisol increases the synthesis of enzymes in the gluconeogenic pathway, as well as enzymes in muscle tissue for the breakdown of proteins to provide glucogenic precursors for glucose synthesis. Glucocorticoiddependent enzymes catalyze the breakdown of fats through lipolysis to generate free fatty acids and keto acids for energy production. The combined effect of these actions is to decrease glucose utilization by providing alternate fuels and to maintain plasma glucose levels for tissues that have an absolute requirement for glucose as oxidizable substrate. Tissue injury or other stimuli lead to an increased production of the arachidonic acid derivatives, prostaglandins and leukotrienes. The newly formed arachidonic acid then is converted to the prostaglandin structure by a cyclooxygenase. Physiologically, prostaglandins have localized effects of dilating the vessels in the area of the injury and sensitizing the nerve endings and increasing the sensation of pain. These cytokines are produced primarily in macrophages after stimulation by immune complexes and arachidonic acid metabolites and after injury. In addition to inhibiting their production, the steps outlined above identify loci where glucocorticoids interfere with the signaling pathways and the actions of their products. The glucocorticoids are effective immunosuppressive agents and are an important therapeutic tool. Glucocorticoids inhibit macrophage and T-cell cytokine production, which reduces B-cell proliferation. By these mechanisms, glucocorticoids are able to suppress both humeral and cellular immune responses. The Physiology of Mineralocorticoids the mineralocorticoids, primarily aldosterone, are essential for the maintenance of salt and water balance by the kidney by regulating sodium reabsorption and potassium secretion. Aldosterone is produced in the zona glomerulosa from the common pregnenolone precursor. Atrial natriuretic factor has a negative modulatory effect on aldosterone secretion. The physiologic role of aldosterone is the maintenance of fluid and electrolyte balance, and its secretion is tightly coupled to the vascular volume. A decrease in vascular volume initiates a cascade response with an increase in renal renin secretion from smooth muscle cells of the afferent glomerular arteriole. Therapeutically, it can be used to block the effects of conditions with excessive cortisol secretion. Excretion of excess bicarbonate Generation of metabolic alkalosis Hyperkalemia caused by renal K+ resorption Increased H+ resorption by renal tubular cells Movement of K+ out of cells in exchange for H+ [35. Cortisol has a permissive effect on enzymes involved in the mobilization of various fuels. The hypokalemia leads to a loss of potassium from cells largely in exchange for H+. There are increased reabsorption of bicarbonate and maintenance of the metabolic alkalosis. Cortisol is essential for the expression of numerous enzymes involved in the maintenance of fuel supplies in preparation for and during a fast. At each stage of metabolism, enzymes have been identified as cortisol-dependent, beginning with the generation of glucogenic precursors. Cortisol increases proteolysis and induces the transaminases necessary to convert pyruvate into alanine for transport to the liver for gluconeogenesis. Key enzymes in the gluconeogenic pathway ranging from pyruvate to glycogen, and those involved in the release of glucose from the liver are all known to be inducible by cortisol. Thus, one of its main functions is the continued production of glucose for metabolism by glucose-dependent tissues during a fast. Glucose utilization by tissues that can utilize alternative fuels is reduced by cortisol, which antagonizes insulin-dependent processes. To provide the energy necessary for gluconeogenesis, cortisol enhances triglyceride breakdown and free fatty acid mobilization from fat stores. In addition, cortisol acts synergistically with glucagon to enhance hepatic gluconeogenesis. The inner, medullary region of the adrenal gland is highly innervated and produces the circulating sympathetic hormones epinephrine and norepinephrine. The steroid hormones are permeable to the cell membrane; thus, their rate of secretion is dependent on their rate of production. The patient has no medical problems but there are many family members with diabetes and hypertension. On examination, the patient is a thin ill-appearing male in no acute distress with normal vital signs. A urinalysis reveals glucosuria and a markedly elevated serum fasting blood sugar. The patient is diagnosed with type I diabetes mellitus (insulin-dependent), and is advised by the physician to start insulin therapy. The destruction of the pancreatic islet cells may have multifactorial causes, such as genetic predisposition, viral, or autoimmune. Patients usually present in childhood or early adulthood and account for about 10% of all cases of diabetes. Severe derangements may induce diabetic ketoacidosis, characterized by markedly elevated blood sugar levels, elevated serum ketone levels, metabolic anion gap acidosis, and a variety of metabolic derangements such as hypokalemia. Because the primary deficit is lack of insulin, patients will need insulin replacement to improve their symptoms.
Buy genuine tamoxifen online
It is particularly common among patients who have undergone orthotopic liver transplantation women's health big book of exercises free pdf purchase tamoxifen overnight. In rare instances, Aspergillus endophthalmitis may occur in immunocompetent patients with no apparent predisposing factors. Disseminated infection most commonly involves the lung, with the eye as the second most common site of infection. Aspergillus fumigatus and A flavus are the species most frequently isolated from patients with intraocular infection. The spores of these ubiquitous saprophytic molds become airborne and seed the lungs and paranasal sinuses of humans. Human exposure is very common, but infection is rare and depends on the virulence of the fungal pathogen and immunocompetence of the host. Ocular disease occurs via hematogenous dissemination of Aspergillus organisms to the choroid. Endogenous Aspergillus endophthalmitis results in rapid onset of pain and loss of vision. A confluent yellowish infiltrate is often present in the macula, beginning in the choroid and subretinal space. Retinal hemorrhages, retinal vascular occlusions, and full-thickness retinal necrosis may occur. The infection can spread to produce a dense vitritis and variable degrees of cells, flare, and hypopyon in the anterior chamber. In contrast to the lesions associated with Candida chorioretinitis and endophthalmitis, lesions produced by Aspergillus species are larger and more likely to be hemorrhagic, and they commonly invade the retinal and choroidal vessels, which may result in broad areas of ischemic infarction. The diagnosis of endogenous Aspergillus endophthalmitis is based on clinical findings combined with positive results from pars plana vitreous biopsy and cultures as well as results from Gram and Giemsa stains. Coexisting systemic aspergillosis can be a strong clue, especially among high-risk patients. The diagnosis requires a high degree of suspicion within the correct clinical context and is confirmed by the demonstration of septate, dichotomously branching hyphae on analysis of vitreous fluid specimens. The differential diagnosis of endogenous Aspergillus endophthalmitis includes Candida endophthalmitis, cytomegalovirus retinitis, Toxoplasma retinochoroiditis, coccidioidomycotic choroiditis or endophthalmitis, and bacterial endophthalmitis. Mixed acute (polymorphonuclear leukocytes) and chronic (lymphocytes and plasma cells) inflammatory cells infiltrate the infected areas of the choroid and retina. Branching fungal hyphae may be apparent spreading on the surface of the Bruch membrane without penetrating it. In Candida endophthalmitis, the vitreous is the prominent focus of infection, but in Aspergillus endophthalmitis, the principal foci are retinal and choroidal vessels and the subretinal or subretinal pigment epithelial space. Endogenous Aspergillus endophthalmitis usually requires aggressive treatment with diagnostic and therapeutic pars plana vitrectomy combined with intravitreal injection of amphotericin B or voriconazole; intravitreal corticosteroids may be used in conjunction with these drugs. Other proven, culture-positive choroidal aspergilloma caused by endogenous Aspergillus flavus systemic antifungal drugs, such as itraconazole, endophthalmitis in an immunocompetent miconazole, fluconazole, and ketoconazole, may also be patient with disseminated pulmonary used. B, Light micrograph shows branching hyphae of Aspergillus fumigatus infectious diseases specialist. Endogenous mycotic endophthalmitis: variations in clinical and histopathologic changes in candidiasis compared with aspergillosis. Cryptococcosis Cryptococcus neoformans is a yeast found in high concentrations worldwide in contaminated soil and pigeon feces. It has a predilection for the central nervous system and may produce severe disseminated disease among immunocompromised or debilitated patients. The fungus probably reaches the eye hematogenously; however, the frequent association of ocular cryptococcosis with meningitis suggests that ocular infection may result from direct extension from the optic nerve. Ocular infections may occur months after the onset of meningitis or, in rare instances, before the onset of clinically apparent central nervous system disease. The most frequent presentation of ocular cryptococcosis is multifocal chorioretinitis, which appears as solitary or multiple discrete yellow-white lesions varying markedly in size in the postequatorial fundus. Associated findings include variable degrees of vitritis, vascular sheathing, exudative retinal detachment, papilledema, and granulomatous anterior cellular inflammation. It has been hypothesized that the infection begins as a focus in the choroid, with subsequent extension and secondary involvement of overlying tissues. Severe intraocular infection progressing to endophthalmitis may be observed in the absence of meningitis or clinically apparent systemic disease. The clinical diagnosis requires a high degree of suspicion and is supported by demonstration of the organism with India ink stains or by culture of the fungus from cerebrospinal fluid. Intravenous amphotericin B and oral flucytosine are required to halt disease progression. With optic nerve or macular involvement, the prognosis is poor for recovery of vision. Coccidioidomycosis Coccidioidomycosis is a disease produced by the dimorphic soil fungus Coccidioides immitis, which is endemic to the San Joaquin Valley of central California, certain parts of the southwestern United States, and parts of Central and South America. Infection follows inhalation of dust-borne arthrospores, most commonly resulting in pulmonary infection and secondary dissemination to the central nervous system, skin, skeleton, and eyes. Approximately 40% of infected patients are symptomatic; the vast majority present with a mild upper respiratory tract infection or pneumonitis approximately 3 weeks after exposure to the organism. Erythema nodosum or multiforme may appear from 3 days to 3 weeks after the onset of symptoms; disseminated infection is rare, occurring in less than 1% of patients with pulmonary coccidioidomycosis. Disseminated disease usually causes blepharitis, keratoconjunctivitis, phlyctenular and granulomatous conjunctivitis, episcleritis and scleritis, and extraocular nerve palsies and orbital infection. Uveal involvement is still rarer: fewer than 20 pathologically verified cases have been reported. Vitreous cellular infiltration, vascular sheathing, retinal hemorrhage, serous retinal detachment, and involvement of the optic nerve have also been reported. Positive results of serologic testing for anticoccidioidal antibodies in the serum, cerebrospinal fluid, vitreous, and aqueous, as well as of skin testing for exposure to coccidioidin establishes the diagnosis in the correct clinical context. One-half of patients with ocular involvement have systemic disease, and complement-fixation titers are often elevated (>1:32). With isolated anterior segment involvement, an anterior chamber tap may be useful. The material from the anterior chamber tap may also be directly examined for coccidioidal organisms using the Papanicolaou stain. Intraocular lesions from the anterior segment usually demonstrate zonal granulomatous inflammation that involves the uvea and angle structure, and Coccidioides organisms are usually visible. The differential diagnosis of coccidioidal uveitis includes Candida, Aspergillus, and Histoplasma species endophthalmitis and tuberculous uveitis. Coccidioidal uveitis should be considered in the differential diagnosis of any patient with apparent idiopathic granulomatous iritis who has lived in or tr avel ed through the southwestern United States, southern California and the San Joaquin Valley, northern Mexico, or Argentina, where the organism is endemic. This granuloma was biopsied and a Amphotericin B treatment is usually reserved for peripheral iridectomy just performed because it was causing pupillary block and angle-closure patients with lesions that are worsening rapidly or that glaucoma. Surgical debulking of anterior chamber granulomas, pars plana vitrectomy, and intraocular injections of amphotericin and voriconazole may be required. With systemic disease, much higher doses and a longer duration of intravenous amphotericin therapy or oral voriconazole therapy may be needed. An infectious diseases specialist is essential in the management of coccidioidomycosis. Despite aggressive treatment, ocular coccidioidomycosis carries a poor visual prognosis, and most eyes require enucleation because of pain and blindness. Chronic coccidioidomycosis endophthalmitis without concomitant systemic involvement: a clinicopathological case report. At one tertiary referral center, masquerade syndromes accounted for nearly 5% of all patients who presented for evaluation of uveitis. Treatment with anti-inflammatory medication can improve the vitreous cellular infiltration, but the effect is not longlasting. Other neurologic signs include hemiparesis, cerebellar signs, epileptic seizures, and cranial nerve palsies. Diagnostic testing Ultrasonography may indicate vitreous debris, elevated chorioretinal lesions, and serous retinal detachment. An unusual leopard-spot pattern of alternating hyperfluorescence and hypofluorescence may also be noted. The presence of vitreous cells in cases of uveitis that do not respond to therapy necessitates a vitreous biopsy. Prior to surgery, communication with an experienced pathologist for instructions on the proper and prompt handling of the specimens is necessary to avoid degeneration of the typically friable cells that may occur with delay.
Syndromes
- Abdominal pain
- The amount swallowed
- Difficulty feeling in any area of the body
- Pain
- Persistent or severe pain
- Muscle twitching
- Thin skin with easy bruising
- Not interested in normal activities
Buy generic tamoxifen 20 mg on-line
In the case of phlyctenulosis menopause jaw pain discount tamoxifen generic, corticosteroids are usually necessary early in the course of treatment. Eyelid hygiene and antibiotic therapy alone may be sufficient in cases of marginal infiltrates, but corticosteroids may be introduced earlier if the diagnosis is certain. If epithelial defects are noted over the infiltrates, diagnostic cultures should be considered before corticosteroid treatment is begun. Those occurring on the anterior eyelid in the glands of Zeis or lash follicles are called external hordeola, or styes. Hordeola occurring on the posterior eyelid from meibomian gland inspissation are termed internal hordeola. Both types are associated with a localized purulent abscess, usually caused by S aureus. Occasionally, patients with a chalazion experience blurred vision secondary to astigmatism induced by its pressure on the globe. It should be noted that basal cell, squamous cell, and sebaceous cell carcinoma can masquerade as chalazia or chronic blepharitis. The histologic examination of persistent, recurrent, or atypical chalazia is therefore important. Topically applied antibiotics are generally not effective and, therefore, are not indicated unless an accompanying infectious blepharoconjunctivitis is present. Systemic antibiotics are generally indicated only in rare cases of secondary eyelid cellulitis; however, if the patient has a prominent and chronic accompanying meibomitis, oral doxycycline may be necessary. If the hordeolum evolves into a chalazion that fails to respond to warm compresses and eyelid hygiene, then intralesional injection of a corticosteroid (eg, 0. In general, intralesional corticosteroid injection works best with small chalazia, chalazia on the eyelid margin, and multiple chalazia. Intralesional corticosteroid injection in patients with dark skin may lead to depigmentation of the overlying eyelid skin and thus should be used with caution. Internal chalazia require vertical incisions through the tarsal conjunctiva along the meibomian gland to facilitate drainage and avoid horizontal scarring of the tarsal plates. Structural and Exogenous Disorders Associated With Ocular Surface Disorders Exposure Keratopathy Exposure keratopathy can result from any disease process that limits eyelid closure. Exposure keratopathy is characterized by a punctate epithelial keratopathy that usually involves the inferior one-third of the cornea; however, the entire corneal surface can be involved in severe cases. Large, coalescent epithelial defects may result, which may lead to ulceration, melting, and perforation. Symptoms are similar to those associated with dry eye, including foreign-body sensation, photophobia, and tearing, unless an associated neurotrophic component results in corneal anesthesia. In the earliest stages, nonpreserved artificial tears during the day and ointment at bedtime may suffice. Taping the eyelid shut at bedtime can help if the problem is primarily one of nocturnal exposure. The use of bandage contact lenses can be hazardous in patients with exposure keratopathy because of a high incidence of desiccation and infection. For cases in which the problem is likely to be temporary or self-limited, temporary tarsorrhaphy using tissue adhesive or sutures should be performed. However, if the problem is likely to be long-standing, definitive surgical therapy to correct the eyelid position is mandatory. Correction of any associated eyelid abnormalities, such as ectropion and/or trichiasis, is also indicated. Most commonly, surgical management consists of permanent lateral and/or medial tarsorrhaphy. Insertion of gold or platinum weights into the upper eyelid is also an effective, more cosmetic approach to promote eyelid closure. Reported complications of gold weight implants include infection, shifting, extrusion, induced astigmatism, unacceptable ptosis, and noninfectious inflammatory response to the gold. In cases of paralytic ectropion of the lower eyelid, a horizontal tightening procedure may also be beneficial in correcting the flaccid lower eyelid. Patients have a flimsy, lax upper tarsus that everts with minimal upward force applied to the upper eyelid. The problem may result from spontaneous eversion of the upper eyelid when it comes into contact with the pillow or other bed linens during sleep. Direct contact of the upper eyelid with bed linens may traumatize the upper tarsal conjunctiva, inducing inflammation and chronic irritation. The condition may be unilateral if the patient always sleeps in the same position. Treatment consists of covering the affected eyes with a metal shield, taping the eyelids closed at night, or performing surgical eyelid-tightening procedures. Differential diagnosis includes vernal conjunctivitis, giant papillary conjunctivitis, atopic keratoconjunctivitis, bacterial conjunctivitis, and toxic keratopathy. It is often bilateral; however, 1 eye may be more severely affected than the other. Treatments include topical anti-inflammatory agents, large-diameter bandage contact lenses, superior punctal occlusion, thermocauterization of the superior bulbar conjunctiva, resection of the bulbar conjunctiva superior to the limbus, topical cyclosporine, autologous serum eyedrops, amniotic membrane transplant, and conjunctival fixation sutures. Topical cyclosporine A in the treatment of superior limbic keratoconjunctivitis: a long-term followup. Treatment of superior limbic keratoconjunctivitis by thermocauterization of the superior bulbar conjunctiva. Conjunctival fixation sutures for refractory superior limbic keratoconjunctivitis. Recurrent Corneal Erosion Recurrent erosions typically occur either in eyes that have suffered a sudden, sharp, abrading injury (eg, fingernail, paper cut, tree branch) or in patients with preexisting epithelial basement membrane dystrophy. The superficial injury produces an epithelial abrasion that heals rapidly, frequently leaving no clinical evidence of damage. After an interval ranging from days to years, symptoms suddenly recur without any obvious precipitating event. In contrast to shearing injuries, small, superficial lacerating injuries involving the cornea rarely result in recurrent erosions. Poor adhesion of the epithelium is thought to be caused by underlying abnormalities in the epithelial basement membrane and its associated filament network. Minor episodes usually last from 30 minutes to several hours; typically the cornea has an intact epithelial surface at the time of examination. More severe episodes may last for several days and are often associated with greater pain, eyelid edema, decreased vision, and extreme photophobia. Many patients seem to suffer from ocular discomfort that is out of proportion to the degree of observable pathology. However, slit-lamp examination using retroillumination can frequently reveal subtle corneal abnormalities (eg, epithelial cysts). The corneal epithelium is loosely attached to the underlying basement membrane and Bowman layer, both at the time of a recurrent attack and between attacks, when the cornea appears to be entirely healed. During an acute attack, the epithelium in the involved area frequently appears heaped up and edematous. Although no frank epithelial defect may be present, significant pooling of fluorescein over the affected area is often visible. Occasionally, subtle areas of loosely adherent epithelium can be identified by applying gentle pressure with a surgical sponge following instillation of topical anesthetics. The presence of basement membrane changes in the unaffected eye implicates a primary basement membrane defect in the pathogenesis, whereas the absence of such findings suggests a posttraumatic etiology. Other clinical conditions with associated abnormalities of the epithelial basement membrane include diabetes mellitus and dystrophies of the stroma and Bowman layer (see also the discussion on corneal dystrophies in Chapter 10).
Effective tamoxifen 20mg
A small specimen can be placed on a filter or thin card to maintain the tissue orientation before fixation or cryosection menstrual migraine headaches tamoxifen 20 mg online. For microbiology workup, the biopsied specimens can be minced or homogenized before inoculation of the culture media or tissue smearing for histochemical stainings. Surgical techniques If the corneal lesion is superficial, it may be possible to scrape or peel it away without sharp dissection. When deeper dissection is required, the surgeon can mark the area freehand with an adjustable-depth blade or use a trephine. Care must be taken to maintain the surgical plane and to avoid inadvertent perforation; keeping the dissection plane dry can be very helpful. A lamellar keratectomy can also be performed using a microkeratome, a diamond burr on a surgical drill, or an excimer or femtosecond laser. The excimer laser can remove tissue with much greater precision than is possible with mechanical techniques. Also, if the corneal surface is irregular to begin with and ablates homogeneously, the irregularity will persist. Frequent application of viscous liquid to the corneal surface during ablation fills in the gaps and helps achieve a smooth surface. Phototherapeutic keratectomy: who are the best candidates and how do you treat them Use of mitomycin-C for phototherapeutic keratectomy and photorefractive keratectomy surgery. Management of Descemetocele, Corneal Perforation, and Corneal Edema Bandage contact lens Applying a thin, continuous-wear soft contact lens as a therapeutic bandage can protect loosely adherent remaining or regenerating epithelium from the "windshield wiper" action of the blinking eyelids. Use of bandage contact lenses has significantly improved and simplified the management of recurrent erosions and persistent epithelial defects. The choice of a soft contact lens for patients with severe dry eye can be difficult. In general, patients with dry eye run a high risk of infection with soft contact lenses; punctal occlusion can facilitate lens retention and comfort. High-water-content lenses usually are not appropriate because rapid water evaporation further compounds the hypertonicity-induced surface damage in dry eyes. Frequent lubrication, prophylaxis with antibiotics, and close follow-up are crucial, especially in patients with decreased corneal sensitivity or dry eye. The use of an acrylic scleral lens may circumvent the problems encountered with a hydrogel lens. Even though a hydrogel lens can actually cause corneal hypoxia and increase corneal edema, continuous wear of this type of lens can provide symptomatic relief of painful bullous or filamentary keratopathy. Mild corneal edema can often be managed with hypertonic saline solution and judicious use of topical corticosteroids, if indicated. Tarsorrhaphy should be considered for patients who have contact lens complications or a high risk of infection. Cyanoacrylate adhesive Tissue adhesives, particularly n-butyl cyanoacrylate, have been used widely as an adjunct in the management of corneal ulceration and perforation. Early application of tissue adhesives in the management of stromal melting has greatly reduced the need for urgent surgical interventions such as therapeutic keratoplasty or conjunctival flap. Some perforations are small and seal spontaneously before any ophthalmic examination, with no intraocular damage, prolapse, or adherence. These cases may require only treatment with systemic and/or topical antibiotic therapy, along with close observation. If a corneal wound is leaking but the chamber remains formed, leakage can be reduced or stopped with pharmacologic suppression of aqueous production (topical ocular hypotensive agent or systemic carbonic anhydrase inhibitors), patching, and/or a bandage contact lens. Generally, if these measures fail to seal the wound in 3 days, closure with cyanoacrylate glue or sutures is recommended. Cyanoacrylate tissue adhesive applied to thinned or ulcerated corneal tissue may prevent further thinning and support the stroma through the period of vascularization and repair. The adhesive plug is also thought to retard the entry of inflammatory cells and epithelium into the area, thus decreasing the rate of corneal melting. After the lesion has been sealed, new stromal tissue may be laid down, and accompanying corneal vascularization may help ensure the integrity of the area by providing nutrients and antiproteases. Tissue adhesive can usually be applied on an outpatient basis using topical anesthetics. However, if adherent or prolapsed uvea in the leakage site or a flat chamber is encountered, the procedure should be performed in the operating room using air and/or viscoelastic substances to re-form the anterior chamber. The adhesive is applied under slit-lamp or microscopic observation with a topical anesthetic (eg, proparacaine hydrochloride 0. Before the adhesive is applied, any necrotic tissue and corneal epithelium should be removed from the involved area and a 2-mm surrounding zone. The area is then dried with a cellulose sponge, and a small drop of the fluid adhesive is applied with a 30-gauge needle or a 27-gauge anterior chamber cannula. A drop of viscoelastic solution speeds polymerization of the glue and makes its surface smoother. The glue does not polymerize on plastic, so a simple way to handle it is to spread a small amount on a surface such as the inside of the sterile plastic wrapping of any medical product cut to a size slightly larger than the perforation. It should then be applied to the surface of the cornea in as thin a layer as possible using the plastic handle of a cellulose sponge or the wooden stick of a cotton-tipped applicator. The adhesive plug has a rough surface and can be irritating, so a bandage contact lens is used to protect the upper tarsal conjunctiva and to prevent the plug from being dislodged by eyelid blinking. The use of fibrin sealant, also called fibrin glue, in corneal diseases is currently under investigation. An alternative to applying cyanoacrylate for a near perforation, not actual perforation, is to use multiple layers of amniotic membrane that has been cut to the shape of the defect, placing a patch into the defect where the near perforation is located. This patch may be held in place with a larger amniotic membrane patch, nylon sutures, and a bandage contact lens, or by means of fibrin sealant. With time, scar tissue will reinforce the deficient area and may mitigate against the need for a corneal transplant. Corneal Tattoo Indications and options Corneal tattooing has been used for centuries to improve the cosmetic appearance of a blind eye with an unsightly leukoma. It has also been used occasionally in seeing eyes to reduce the glare from scars and to eliminate monocular diplopia in patients with large iridectomies, traumatic loss of iris, and congenital iris colobomas. When this solution is reacted with a second agent, a dark black precipitate is formed in the cornea, producing a dark deposit that can simulate a pupil. A second technique involves utilizing the standard methods used in skin tattooing: applying to the cornea a paste of colored pigment, either india ink or a metal oxide, and then using a hypodermic needle or angled blade to drive the pigment into the corneal stroma in the area that needs coverage. Multiple superficial punctures are made until enough pigment has been applied; multiple pigment colors can be used to give a more natural appearance. However, the method is time-consuming and often needs to be repeated if the pigment uptake is inadequate or the pigment migrates. Femtosecond-assisted anterior lamellar corneal staining-tattooing in the cosmetic treatment of leukocoria is under investigation. Tarsorrhaphy Tarsorrhaphy is the surgical fusion of the upper and lower eyelid margins. It is one of the safest and most effective procedures for healing difficult-to-treat corneal lesions. It can also be used to aid in the healing of indolent corneal ulceration sometimes seen with tear-film deficiency, herpes simplex or zoster, stem cell dysfunction, or trigeminal nerve (cranial nerve V) dysfunction (neurotrophic lesions). They may be total or partial, depending on whether all or only a portion of the palpebral fissure is occluded. Tarsorrhaphies are also classified as lateral, medial, or central, according to the position in the palpebral fissure. Note that the cosmetic effect of a lateral tarsorrhaphy is significant, and patients are often unhappy with the appearance afterward. Postoperative care Antibiotic ointment is usually applied to the wound twice a day for the first 5 days after the procedure. If anterior lamellar sutures are used over a pledget, ointment is applied until the sutures are removed 2 weeks later. Ointment containing corticosteroids should be avoided, because corticosteroids may interfere with rapid healing.
Order tamoxifen american express
This elastic recoil of the chest wall at any lung volume depends on the compliance of the chest wall womens health center xenia ohio purchase tamoxifen once a day. Chest wall compliance can be altered in states such as scoliosis and ankylosing spondylitis, in which the spine, ribs, and vertebral joints are altered so that compliance is decreased. This can result in a reduction in all lung volumes, including functional residual capacity. Although they do not affect chest wall compliance, neuromuscular diseases can affect respiration; functional residual capacity often will be normal, but residual volume will be increased, and other volumes, capacities, and forced volumes will be reduced. In addition to gas exchange, the pulmonary system is involved in a number of other functions, many of which are related to defense. The air people breathe is far from pure, and there are both mechanical and chemical defenses to protect the lungs and prevent invasion of the body through the Before its arrival in the alveoli, the bulk of inspired air, especially particles larger than 1 mm, come into contact with the walls of the conducting airways. Those walls are lined with cells that secrete mucus and possess cilia that beat with a motion that moves particles toward the oropharynx, where they can be swallowed. Smaller particles that can reach terminal airways and alveoli are removed by macrophages. There also is an abundant immune system composed of lymphocytes and dendritic cells. Many of the phagocytic and immune cells produce reactive oxygen molecules, which can be detrimental to lung tissue, especially in the face of the relatively high oxygen levels existing within the alveoli. To deal with these molecules, lung surfactant contains high levels of the antioxidant glutathione. Many biogenic amines are inactivated in the lung, including serotonin, bradykinin, and several arachidonic acid metabolites. Which of the following lung volumes or lung capacities most likely would be normal Bacteria are cleared more readily from the airways Cilia on the epithelial cells beat more easily Inhaled particles are not trapped Mucus is propelled orally more slowly [17. Decreased lung compliance Decreased strength of the chest wall muscles Increased airway resistance Increased chest wall compliance Functional residual capacity is the volume of air in the lungs when no muscular effort is being expended. All the other volumes and capacities in the lungs depend at least in part on muscular effort. However, the thick mucus impairs ciliary function, thus impeding oral transport of the mucus-trapped particles. The finding of an increase in total lung capacity and functional residual capacity indicates that compliance of the lung is increased. This allows for an increase in dynamic compression of the airways upon a forced expiration. Dynamic compression increases airway resistance and decreases airflow, which is typical of an obstructive pulmonary process. During a forced expiration, airflow is limited by dynamic compression of the airways, which is greater in lungs with increased compliance. Neuromuscular diseases affecting muscles of respiration do not alter functional residual capacity and may not affect tidal volume, but residual volume is increased and all other volumes and capacities are decreased. Particles larger than 1 mm that are inhaled with the air are trapped by the mucus that coats the airways. The ciliary action of airway epithelial cells transports the particles to the pharynx, where they are swallowed. The patient is short of breath on examination with a slightly low pulse oximetry reading, consistent with mild hypoxemia. She has multiple skin lesions, and a biopsy reveals noncaseating granulomas consistent with sarcoidosis. Chest x-ray findings revealing hilar adenopathy are also suggestive of sarcoidosis. The physician explains to the patient that he likely has a restrictive disease process, and recommends formal pulmonary function testing. What changes in pulmonary function would be consistent with a restrictive disease Parameters measured in a pulmonary function test: Changes in the volume of inspired air versus time. Conditions that restrict lung expansion are neuromuscular conditions, problems with the chest wall, pleural disease, and decreased lung compliance. Depending on the nature of the restrictive disease, there may be little or no change in rates of airflow. How restrictive lung processes cause hypoxemia: Thickening of alveolar membrane, which increases the diffusion distance. Examples of restrictive diseases are sarcoidosis, connective-tissue disorders, interstitial pneumonia, environmental exposure, and pulmonary vascular disease. Restrictive diseases result in poor gas exchange because of a thickening of the alveolar membrane that results in restriction of oxygen diffusion with increased diffusion distance. Obstructive disorders result in poor gas exchange because of decreased surface area for diffusion of gases. These two pulmonary problems can often be distinguished from each other by pulmonary function tests, but the clinical presentation is the most important method of diagnosis. Explain how measurements of lung volumes and gas flow rates can be used to distinguish between obstructive and restrictive lung diseases. Discuss alveolar gas exchange and factors that determine the rate of O2 diffusion. Definitions Obstructive disease: Disorders that cause an increase in the airway resistance to flow such as narrowing of the passages due to inflammation or compression. Restricive disease: Disorders that impair or increase the work necessary for lung expansion. The mechanical factors that contribute to lung function fall into the following categories: 1. An easy way to remember the distinction is to realize that obstructive diseases manifest themselves as increased resistance to airflow and restrictive diseases manifest themselves as restriction of lung expansion. It is characterized by noncaseating granulomas, and although it may occur in any tissue, the inflammation generally starts in the lungs or lymph nodes. In the present case, lung injury has occurred because of granule formation in the bronchioles and alveolar sacs and chronic inflammation resulting in scarring or formation of fibrotic tissue. Fibrosis in the lung tissue has a marked effect on the elasticity, or compliance, of the lung. Physically, the lung volume is dependent on two factors: the elastic recoil of the lung to collapse on itself and the outward recoil of the chest wall. The patient breathes through a mouthpiece that is attached to an instrument which measures the volume of air that the patient is moving as a function of time. During normal quiet breathing, expansion of the chest wall reduces the interpleural pressure, causing an expansion of the lung volume. Relaxation of the inspiratory muscles allows a return of the chest wall and a decrease in lung volume. Compliance is the inverse of the elasticity (compliance = volume/pressure) of the lung tissue; therefore, the volume under these conditions will be dependent on and may be used as an estimate of lung compliance. This can be contrasted to a high-compliance lung, which will undergo a larger volume change for a given pressure. There are other mechanical factors that cause restrictive disease, such as neuromuscular weakness of the respiratory muscles, which can prevent full expansion of the chest. Scoliosis or malformations that interfere with chest movements or pneumothorax (air in the chest cavity) can prevent full expansion of the lungs. Rates of airflows may be affected in restrictive diseases, but usually can be identified on the basis of other factors. Obstructive diseases usually can be distinguished by increased resistance to airflow. Resistance to airflow will occur under conditions in which there is a diminished diameter of the airway. Another cause of airway constriction is dynamic compression of airways during expiration. Dynamic compression of airways is more pronounced in high-compliance tissues and is one of the major factors limiting pulmonary function in chronic obstructive pulmonary disease. The diffusion of a gas through a barrier is described by the Fick law of diffusion, which states that the rate of diffusion of a gas through a barrier is dependent on the surface area of the barrier, the thickness of the barrier, the Pulmonary gas exchange is dependent on the surface area and thickness of the pulmonary capillary, the partial pressure difference of the gas between the alveolar and blood compartments, and the residence time of the blood in the alveolar capillary. Thus, factors that affect the surface area or thickness of the pulmonary capillary can have a profound effect on the rate of diffusion of a gas between the two compartments. Gases with different diffusion coefficients illustrate the limitations of gas transfer across the pulmonary capillary. Nitrous oxide (N2O) diffuses very rapidly and equilibrates across the pulmonary capillary in about 0. In contrast, a gas such as carbon monoxide binds avidly to hemoglobin with a reaction time that is faster than the rate of diffusion across the capillary barrier.
Cheap tamoxifen express
Chapters 6 and 7 discuss noninfectious and infectious posterior uveitis women's health newsletter order genuine tamoxifen on-line, respectively, in greater detail. Table 5-5 Table 5-5 Panuveitis In panuveitis, inflammation is diffuse without a predominant site. Inflammation is observed in the anterior chamber, vitreous, and retina and/or choroid. Many systemic infectious and noninfectious diseases associated with uveitis may produce diffuse intraocular inflammation with concomitant anterior uveitis and posterior uveitis. Chapters 6 and 7 discuss noninfectious and infectious panuveitis, respectively, in greater depth, and Chapter 8 covers endophthalmitis. Retinal Vasculitis Retinal vasculitis is defined by the presence of retinal vascular changes in association with ocular inflammation. The term is used in distinction to vasculopathy, in which there are vessel changes but no visible evidence of inflammation. Blood vessel changes include perivascular sheathing and vascular leakage or occlusion shown on fluorescein angiography studies. Peripheral retinal vasculitis may be observed in intermediate uveitis but is not sufficient for the anatomical classification of posterior/panuveitis, whereas diffuse retinal vasculitis is sufficient. Categorization by Clinical Course Uveitis may be subcategorized as acute, chronic, or recurrent: acute uveitis is used to describe episodes of sudden onset and limited duration that usually resolve within 3 months or less, whereas chronic uveitis is persistent, with relapse occurring in less than 3 months after discontinuing treatment. Recurrent uveitis is characterized by repeated episodes separated by periods of inactivity without treatment that last 3 months or longer. Whether the inflammation is severe or low grade can influence categorization and prognosis. The inflammatory process may occur in 1 or both eyes, or it may alternate between them. The distribution of ocular involvement-focal, multifocal, or diffuse-is also helpful to note when classifying uveitis. Nongranulomatous inflammation typically has a lymphocytic and plasma cell infiltrate, whereas granulomatous reactions also include epithelioid and giant cells. Symptoms of Uveitis Symptoms produced by uveitis depend on which part of the uveal tract is inflamed, the rapidity of onset (sudden or insidious), the duration of the disease (limited or persistent), and the course of the disease (acute, chronic, or recurrent). Acute-onset anterior uveitis causes pain, photophobia, redness, and blurred vision. Pain usually results from the acute onset of inflammation in the region of the iris, or from secondary glaucoma. The pain associated with ciliary spasm in anterior uveitis may be a referred pain that radiates over the larger area served by cranial nerve V (the trigeminal nerve). Floaters result from the shadows cast by vitreous cells and "snowballs" on the retina. Presenting symptoms in patients with posterior uveitis include painless decreased visual acuity, floaters, photopsia, metamorphopsia, scotomata, nyctalopia, or a combination of these symptoms. Blurred vision may also result from refractive error such as a myopic or hyperopic shift associated with macular edema, hypotony, or a change in lens position. Table 5-6 Signs of Uveitis the chemical mediators involved in inflammation (see Chapter 1) result in vascular dilation (ciliary flush), increased vascular permeability (aqueous flare), and chemotaxis of inflammatory cells into the eye (aqueous and vitreous cellular reaction). Perilimbal vascular engorgement (ciliary flush) or diffuse injection of the conjunctiva, episclera, or both is typical with acute anterior uveitis. Large keratic precipitates such as these generally indicate a granulomatous disease process. Note the 3 types of iris nodules: A, Koeppe nodules (pupillary border); B, Busacca nodules (midiris); and C, Berlin nodules (iris angle). The vitreous grading scale shown here was used in the Multicenter Uveitis Steroid Treatment Trial. The consensus is that cells in the vitreous strands are old, and cells in the syneretic areas may be new. With this method, standardized photographs are used for comparison with clinical images to ultimately arrive at the level of vitreous haze. Additional uveitic changes may be observed in the vitreous, namely, snowball opacities, which are common in sarcoidosis or intermediate uveitis exudates over the pars plana (snowbank). As pars planitis becomes inactive, the pars plana appears gliotic or fibrotic and smooth; thus, these changes are not referred to as snowbanks. Posterior Segment Signs in the posterior segment of the eye include retinal or choroidal inflammatory infiltrates inflammatory sheathing of arteries or veins exudative, tractional*, or rhegmatogenous* retinal detachment retinal pigment epithelial hypertrophy or atrophy* atrophy or swelling of the retina, choroid, or optic nerve head* preretinal or subretinal fibrosis* retinal or choroidal neovascularization* An asterisk is used to indicate structural complications. Standardization of vitreal inflammatory activity in intermediate and posterior uveitis. A comprehensive history and review of systems is of paramount importance in helping to elucidate the cause of uveitis. In this regard, a diagnostic survey for uveitis as shown in the appendix can be very helpful. The age, sex, sexual practices, and racial background of the patient are important elements in some uveitic syndromes. Table 5-10 Although ocular inflammation may be an isolated process involving only the eye, it can also be associated with a systemic condition. However, ocular inflammation frequently does not correlate with inflammatory activity elsewhere in the body, so it is important for the clinician to carefully review systems. In some cases, the uveitis may actually precede the development of inflammation at other body sites. Immunocompromise, use of intravenous drugs, hyperalimentation, and certain occupations are just a few risk factors that can direct the investigation. Differential Diagnosis of Uveitic Entities the differential diagnosis of uveitis is broad and includes infectious agents (viruses, bacteria, fungi, protozoa, and helminths), noninfectious entities of presumed immunologic or allergic origin, masquerade syndromes such as endophthalmitis and neoplastic disease, and unknown or idiopathic causes. Intraocular lymphoma, retinoblastoma, leukemia, and malignant melanoma may all be mistaken for uveitis. In addition, juvenile xanthogranuloma, pigment dispersion syndrome, retinal detachment, retinitis pigmentosa, and ocular ischemia syndrome all must be considered in the differential diagnosis of uveitis. Although pattern recognition alone is frequently sufficient to establish a definitive diagnosis, accurate biomicroscopic and funduscopic descriptions of posterior segment inflammatory conditions are extremely helpful in forming the differential diagnosis and in distinguishing individual entities because the distribution and evolution of these findings may be quite characteristic. However, many patients do not present with the classic signs and symptoms of a particular disease. Some patients require ongoing monitoring, as the clinical appearance may be unclear or change with time and treatment. The presentation of a disease can also be modified by previous therapy or by a delay in evaluation by the physician. This naming-meshing system first classifies the type of uveitis based on anatomical criteria and associated factors (eg, acute versus chronic, unilateral versus bilateral) and then matches the pattern of uveitis exhibited by the patient with a list of potential uveitic entities that share similar characteristics. Epidemiology of Uveitis Uveitis is responsible for 10% of all blindness cases in the United States, and the incidence of blindness attributable to uveitis is approximately 15 new cases/100,000 persons per year. Prevalence varies by geographic location, age of study population, academic center, and study date. An epidemiologic study of uveitis in northern California suggests an incidence of 52. In addition, the incidence and prevalence were lowest in the pediatric age groups (prevalence of 30/100,000) and highest in those over age 65 years (prevalence of 151. Table 5-11 summarizes the data from several surveys, providing a comparison of the prevalence of various types of uveitis in university/referral-based and community-based populations from around the world. This distribution is generally similar: anterior involvement is most common, followed by panuveitis, then posterior uveitis, and finally intermediate uveitis. Most university/referral-based studies probably overestimate the prevalence of intermediate and posterior uveitis actually present in the community. Incidence and prevalence of uveitis: results from the Pacific Ocular Inflammation Study. Uveitis-a rare disease often associated with systemic diseases and infections: a systematic review of 2619 patients. Characteristics of uveitis presenting for the first time in the elderly: analysis of 91 patients in a tertiary center. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study.
Purchase 20mg tamoxifen mastercard
Associated similar arteriovenous malformations may appear in the orbit and mandible workout tips women's health buy tamoxifen 20mg without a prescription. C, Although it can occasionally have an arteriovenous communication, a retinal macrovessel is distinct from racemose hemangioma. D, Fluorescein angiography highlights the macrovessel, which crosses the macular area and the horizontal midline. The frequency of retinoblastoma ranges from 1 in 14,000 to 1 in 20,000 live births. The mean age at diagnosis depends on family history and the laterality of the disease: patients with a known family history of retinoblastoma: 8 months patients with bilateral disease: 12 months patients with unilateral disease: 24 months Globally, incidence data for retinoblastoma show an approximately 50-fold variation. Registries with the highest incidence of retinoblastoma include countries in Africa. If a patient has bilateral retinoblastoma, there is an approximately 98% chance that it represents a germline mutation. The children of a patient who has the hereditary form of retinoblastoma have a 45% chance of being affected (50% chance of inheriting and 90% chance of penetrance). The remaining patients have new germline mutations and multiple tumors will develop. Unless there are multiple tumors in the affected eye, these patients cannot be distinguished from those without a germline mutation. Much like their counterparts with bilateral retinoblastoma, children with unilateral retinoblastoma and a germline mutation are more likely to present at an earlier age. With these screening methods, there is a 96% chance of finding a new tumor mutation, if one exists. The success rate can be further increased if blood and freshly harvested tumor are available for analysis. Counseling with a genetic specialist is recommended for all families afflicted with or a risk for developing retinoblastoma. Unaffected parents of a child with bilateral involvement have less than a 5% risk of having another child with retinoblastoma. If 2 or more siblings are affected, the chance that another child will be affected increases to 45%. Other presenting features, such as iris heterochromia, spontaneous hyphema, and orbital cellulitis or inflammation, are uncommon. Reported vision problems are infrequent because most patients are preschool-aged children. Table 19-1 the diagnosis of retinoblastoma can generally be made on the basis of an office examination that includes documented visual acuity. The intraocular pressure and corneal diameter of both eyes should be measured intraoperatively. As the tumor grows, foci of calcification develop, giving the tumor its characteristic chalky white appearance. Exophytic tumors grow beneath the retina and may have an associated serous retinal detachment. Diffuse infiltrating retinoblastoma is a rare variant of retinoblastoma that is detected later in childhood (>5 years); it is typically unilateral. Diffuse infiltrating retinoblastoma presents a diagnostic dilemma, as the retina may be difficult to see through the dense vitreous cells. Ultrasonography can aid the diagnosis of retinoblastoma by demonstrating characteristic calcifications within the tumor. A, Clinical appearance shows leukocoria and strabismus associated with advanced intraocular tumor. Note the large retrolental tumor and secondary total exudative retinal detachment. Recent studies have suggested that systemic metastatic evaluation, typically via bone marrow and lumbar puncture, is not indicated in children without neurologic abnormalities or evidence of extraocular extension. Parents and siblings should be examined for evidence of untreated retinoblastoma or retinocytoma, which would represent evidence of a hereditary predisposition to the disease. Children with retinoblastoma should have a complete history and physical examination done by a pediatric oncologist. In the United States, patients rarely present with metastases or intracranial extension at the time of diagnosis. The most frequently identified sites of metastatic involvement in children with retinoblastoma include abdominal viscera, brain, distal bones, lymph nodes, skull bones, and spinal cord. Retinoblastoma cells may escape the eye by invading the optic nerve and extending into the subarachnoid space. In addition, tumor cells may massively invade the choroid before traversing emissary canals or eroding through the sclera to enter the orbit. In the anterior chamber, tumor cells may invade the trabecular meshwork, gaining access to the conjunctival lymphatics. Most of these conditions can be differentiated from retinoblastoma on the basis of a comprehensive history, clinical examination, and results from appropriate ancillary diagnostic testing. Note the dilated retinal blood vessels, foci of calcification (arrow), and cuff of subretinal fluid (asterisk). The condition is unilateral in two-thirds of cases and is associated with microphthalmos, a shallow or flat anterior chamber, a hypoplastic iris with prominent vessels, and a retrolenticular fibrovascular mass that draws the ciliary body processes inward. On indirect ophthalmoscopy, a vascular stalk may be seen arising from the optic nerve head and attaching to the posterior lens capsule. Ultrasonography confirms the diagnosis by showing persistent hyaloid remnants arising from the optic nerve head, usually in association with a closed funnel retinal detachment. Coats disease Coats disease is clinically evident within the first decade of life and is more common in boys. Ultrasonography documents the absence of retinal tumors and shows the collection of cholesterol in the subretinal fluid. Note normal-appearing retinal vessels, as opposed to those found in Coats disease. Toxocariasis presents with posterior and peripheral granulomas, with associated uveitis. Exudative retinal detachment, organized vitreoretinal traction, and cataracts may be present. Ultrasonography shows vitritis, retinal detachment, granulomas, retinal traction, and the absence of calcium. Astrocytomas occasionally arise from the optic nerve head; such tumors are often referred to as giant drusen. Retinal astrocytomas commonly occur in patients with tuberous sclerosis and may also be found in patients with neurofibromatosis; most are not associated with a phakomatosis. The tumor may erode through the iris root or grow along the lens zonular fibers, entering the anterior chamber. Proptosis caused by successfully treated with plaque brachytherapy, but most retinoblastoma with orbital invasion. For most of these tumors, surgical resection is specifically avoided because of late complications and documented metastases associated with this treatment. Fortunately, metastasis is rare with appropriate management, even if the tumor appears frankly malignant on histologic examination. Classification the Reese-Ellsworth Classification for Intraocular Tumors is the historic method of grouping intraocular retinoblastomas. The system takes into account the number, size, and location of tumors and the presence or absence of vitreous seeding. The Reese-Ellsworth classification does not stage extraocular disease, nor does it provide prognostic information about patient survival or vision. The use of external-beam radiotherapy for the treatment of retinoblastoma has been supplanted by the use of primary local and/or systemic chemotherapy. As a result, the International Classification System for Intraocular Retinoblastoma is now the most commonly used system worldwide.