Order generic aciphex pills
An alternative position involves having the leg extended and the foot internally rotated chronic gastritis reversible order aciphex on line. Technique A 3 to 4 cm skin incision is made in the lower lateral thigh above the knee, and dissection is carried down to the tensor fascia. The direction of the glistening white fibers is noted, and the fascia is marked the direction of the fibers on the skin. A line that is parallel to the fibers of the fascia lata is drawn from the incision site just above the knee laterally. These marks indicate the proper direction of undermining for the passage of the fascia stripper to avoid crosscuts in the fascia. The skin overlying and attached to the fascia is then undermined with long, sturdy scissors. Adequate undermining is needed so that there will be no obstruction to the passage of the fascia stripper. When the Crawford stripper or the Masson stripper is used alone, the fascia is initially incised in two areas to create a 6 to 8 mm wide strip of fascia. The fascia stripper is advanced in the dissected plane with the side-cutting edges, which make incisions to create the fascia strip. If the Crawford separator has been used to precut the two longitudinal incisions, the side-cutting edges are not needed, and the stripper is simply advanced. Because the side-cutting mechanisms on the Crawford stripper can become dull, a separate Crawford separator device is used to create the long parallel incisions before using the stripper and its guillotine cutting device. The Crawford separator is inserted through the initial parallel incisions and advanced in the leg to create two long parallel incisions before the tab is cut. The side-cutting edge of the stripper is not needed; only the guillotine cutting device at the end is used to provide a more reliable method of fascia excision. B, A tab is fashioned from the end of the fascial strip and then threaded into the Crawford stripper. The stripper is then advanced along the fascia superiorly up the lateral thigh after the undermining of the soft tissue from the fascia. The Crawford stripper can be used to make side cuts with this passage, but typically the Crawford separator is used to facilitate the side cuts. Alternatively, in younger females who wear shorts, the incision can be made superiorly and the stripper passed inferiorly. B, the skin and the subcutaneous tissue are undermined over the surface of the fascia to facilitate the passage of the stripper. D, the distal end of the strip is separated to create a tab, which is then threaded through the Crawford stripper. Clamps are used to create tension in the fascia while the stripper is passed; we prefer two Kocher clamps. When the desired length of fascia (usually 10 cm or more) is captured in the stripper, the fascia is severed with the guillotine device at the end of the stripper. Fascial strips with fibers that are cut obliquely are to be avoided, because they are prone to shredding. The closure of the leg incision does not usually require the specific closing of the fascia defect; however, the closure of the subcutaneous tissue should be performed with 4-0 Prolene or 4-0 Monocryl. Healing is rarely a problem, and ambulation can occur 12 to 24 hours after surgery. In this form, it is useful as a patch graft for eye socket reconstruction or for canthal reconstruction techniques. A wider area than that used with the stripper is undermined, and incisions are made in the fascia beyond the extent of the skin incision. B, Sheets of fascia as wide as 8 to 10 cm can be obtained through a medium-sized incision. TemporaL Fascia (TemporaLis Fascia) the fascia that overlies the temporalis muscle is an alternative donor site. The temporalis fascia that covers the temporalis muscle originates on the superior aspect of the temporalis fossa and inserts on the zygomatic arch. Temporal fascia may be conveniently harvested in conjunction with certain brow and eyelid procedures, such as reanimation procedures of the eyelids. The temporalis fascia is exposed in the same way that the tensor fascia lata is exposed: by undermining the superficial layer of the temporal fascia or the galea. The graft can then be divided into strips for sling procedures, or it may remain in sheets for other purposes. Temporalis fascia is more fragile than fascia lata, but it can be used satisfactorily for patch-type procedures. However, it is difficult to obtain grafts of sufficient length for frontalis suspension procedures to correct upper lid ptosis. Ear cartilage furnishes rigid support for the lower lid, and it has the ability to become epithelialized over a period of several weeks. Ear cartilage grafts are also useful to stabilize eyelids that have become structurally unsound in the presence of such conditions as tarsus-deficient entropion of the upper or lower eyelid. The larger grafts may produce a temporary irritation to the conjunctiva that can be treated with a cortisone antibiotic ointment. Cartilage grafts with exposed surfaces are not used in the upper lid, because they would impinge directly on the corneal surface. The amount of cartilage available varies from person to person and according to the shape of the ear. Technique Before the graft is obtained, the anterior and posterior skin of the scaphoid portion of the ear is infiltrated with local anesthetic that contains epinephrine and hyaluronidase. This line should be 4 mm from the edge of the helix to avoid causing an ear deformity. The skin incision is made and careful dissection performed down to the level of the ear cartilage to expose the cartilage surface. The full thickness of the cartilage is incised and peeled away from the anterior skin surface with blunt dissection via a cotton applicator stick to preserve the perichondrium. The cartilage, which is normally flat and pliable, can then be shaped and trimmed. B, Excision is performed from the posterior surfaces of the ear; the ear is retracted. D, the cartilage is incised and reflected from the skin and the subcutaneous tissue with blunt dissection to the perichondrium. F, Final closure on the posterior surface is shown with crisscross running vertical mattress sutures in 6-0 nylon. A conchal cartilage graft must be thinned and the surface scored with a scalpel to help flatten and relax the graft. The skin and the subcutaneous tissue are elevated from the conchal portion of the ear. The conchal cartilage is dissected from the anterior skin layer with blunt dissection, which prevents buttonhole formation. A full-thickness slit is made through the marked area, and scissors are used to complete the incision through the full thickness of the cartilage, thus avoiding penetration of the overlying skin. A periosteal elevator or a cotton applicator stick is helpful for reflecting the perichondrium and the subcutaneous tissues off of the surface of the cartilage. C, Blunt dissection is used to separate the cartilage from the skin and the subcutaneous tissue on the anterior surface. E, Alternatively, an anterior incision can be made at the anterior edge of the conchal bowl. When suturing the cartilage into place, the surgeon must avoid the excessive passage of sutures through the grafts; the brittle nature of the cartilage may cause it to crumble with multiple attempts at suturing. Cartilage may be stored in saline solution until it is needed later during the procedure. If good hemostasis is achieved with electrocautery, only ice compresses (without pressure dressings) are used for the ear postoperatively. This material has the advantages of rigidity and a mucous membrane covering, and it can be used as an alternative graft in special situations when other donor material is not available. A, the bilayer graft is harvested as one graft, leaving the mucosa attached to the septum.
Diseases
- Glycogen storage disease type 9
- Ruvalcaba Myhre syndrome
- Amelia cleft lip palate hydrocephalus iris coloboma
- Sensory neuropathy type 1
- Gamma aminobutyric acid transaminase deficiency
- Oculo cerebro osseous syndrome
- Hyperimmunoglobinemia D with recurrent fever
- Exostoses, multiple
- Lead poisoning
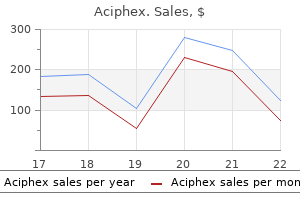
Purchase aciphex with visa
Nakagawa T gastritis symptoms and causes cheap 20mg aciphex free shipping, Kawano H, Kubota T: "Solitary" bone cyst of the cervical spine: case report. Pogoda P, Priemel M, Linhart W, et al: Clinical relevance of calcaneal bone cyst: a study of 50 cyst in 47 patients. Saito Y, Hoshina Y, Nagamine T, et al: "Simple" bone cyst: a clinical and histopathologic study of 15 cases. Sethi A, Agarwal K, Sethi S, et al: Allograft in the treatment of benign cystic lesions of bone. Struhl S, Edelson C, Pritzker H, et al: Solitary (unicameral) bone cyst: the fallen fragment sign revisited. Taneda H, Azuma H: Avascular necrosis of the femoral epiphysis complicating a minimally displaced fracture of "solitary" bone cyst of the neck of the femur in a child: a case report. Violas P, Salmeron F, Chappuis M, et al: Simple bone cyst of the proximal humerus complicated with growth arrest. Yanai Y, Tsuji R, Ohmori S, et al: Malignant change in an intradiploic epidermoid: report of a case and review of the literature. Lipomas involving bone are divided into three types: intramedullary (intraosseous), intracortical/subperiosteal, and parosteal. Incidence and Location Lipomas of bone are extremely rare; fewer than 50 cases are described in the literature. Intramedullary Lipoma Intramedullary lipomas usually occur in the metaphyseal parts of major long bones of the lower extremity-the femur, tibia, and fibula. Central, niduslike calcification is a frequent radiographic feature of intramedullary lipoma 1100 Intracortical and Subperiosteal Lipoma Intracortical and subperiosteal lipomas are extremely rare. Histologically, these lesions consist of mature adipose tissue and, similar to intramedullary lipomas, they do not differ from ordinary lipomas of soft tissue. A and B, Anteroposterior and lateral radiographs show lytic lobulated lesion involving proximal tibial metaphysis in skeletally mature patient. C, Coronal magnetic resonance image of intramedullary lipoma of tibia shows no discernible marrow signal alteration because lipoma is composed of mature adipose tissue. Note bone contour expansion and central niduslike opacities corresponding to areas of fat necrosis. Anterior portion of calcaneus shows lytic lesion with ringlike calcific density in its center. B, Coronal computed tomogram shows lucent lesion in calcaneus that has central cyst; walls of cyst are calcified. C, On curettage, lesion was partly cystic and contained calcified necrotic fat; fragment of cyst wall. A, Anteroposterior radiograph of proximal femur shows lytic intertrochanteric lesion with well demarcated sclerotic margins. Note multifocal coalescent opacities corresponding to calcified areas of fat necrosis. Note the absence of bone trabeculae, a feature helpful in distinguishing this lesion from normal fatty bone marrow. D, Central portion of lesion exhibits features of fat necrosis and dystrophic calcification. Because of their association with the bone surface, parosteal lipomas may have some distinctive radiographic and microscopic features. A characteristic feature of parosteal lipoma (not always seen) is a sclerotic, osseous pedicle that grows from the surface of the bone into the adipose tissue. This bony excrescence can dominate the lesion and can result in radiographic misdiagnosis of the lesion as an osteochondroma. Foci of cartilaginous metaplasia with formation of a cartilaginous cap may be present. Clinical Behavior Approximately 50% of patients who were reported to have primary liposarcoma of bone had metastases after amputation. The lesion typically involves the chest wall and most likely originates within the ribs. The cut surface is marked by the presence of many dilated channels filled with blood. These spaces are separated by a friable, red-brown stroma that contains variable amounts of gritty, shiny, white, cartilaginous tissue. Radiographic Imaging Radiographically vascular-cartilaginous hamartoma presents as an expansile lesion of the rib. The cartilage islands represent well-developed nodules of cartilaginous tissue that are well demarcated from the surrounding vascular component and occasionally form irregular clusters. The vascular component is similar to conventional hemangioma and may contain large, highly cellular areas composed of spindle cells forming narrow vascular channels. The spindle-cell areas may show prominent mitotic activity, but atypical mitoses are absent. Larger-caliber vessels are also present and may form clusters mimicking common (cavernous) hemangioma. Vascular-cartilaginous hamartoma frequently shows features of superimposed secondary aneurysmal bone cyst. Incidence and Location Liposarcoma of bone is one of the rarest of primary bone tumors. Reported cases of intraosseous liposarcoma involved the major long tubular bones, such as the femur, tibia, and humerus. Radiographic Imaging Radiographic features are nonspecific and show a bonedestructive process indicative of a malignant tumor. Microscopic Findings Microscopically, liposarcomas in bone represent highgrade pleomorphic or round-cell (signet-ring) lesions. Differential Diagnosis the high-grade pleomorphic liposarcoma should be differentiated from malignant fibrous histiocytoma. In the evaluation of adipose tissue and differentiation of intraosseous lesions, the presence of residual nonneoplastic tissue of fatty marrow infiltrated by a nonlipomatous tumor should be ruled out before the lesion is classified as a liposarcoma. It is our impression that at least some of the cases previously reported as primary liposarcomas of bone would be currently classified as malignant fibrous histiocytomas. A, Lateral radiograph of femur shows multilobulated, partially lucent parosteal tumor containing areas of mineralization. B, Corresponding magnetic resonance image demonstrates parosteal location of tumor, which for the most part shows same signal intensity as marrow fat. A, Chest radiograph shows large, ill-defined intrathoracic expansile mass arising from the ninth and tenth ribs of a 7-month-old boy. Most of this mass was composed of aneurysmal bone cyst component of cartilaginous hamartoma. C, Radiograph of resection specimen of cartilaginous hamartoma that arose in rib with secondary aneurysmal bone cyst formation. D, Whole-mount section of rib shows intramedullary cartilage lobules and dilated vascular channels (hematoxylin-eosin). A, Islands of mature cartilage within fibrovascular stroma containing numerous capillary-type vessels. B, Higher magnification of A shows islands of cartilage within spindlecell stroma with numerous capillary vessels. Treatment and Behavior these rare lesions are benign and may be cured by en bloc excision of the mass in continuity with the involved rib. Rapid enlargement of the lesion can be clinically observed if vascular-cartilaginous hamartoma is complicated by a superimposed aneurysmal bone cyst. The tumor is composed of nests of cells that have melanin pigment and is also referred to as retinal anlage tumor, melanotic progonoma, or melanotic ameloblastoma. Incidence and Location Melanotic neuroectodermal tumors usually involve the maxilla or mandible but also occur in the soft tissue, the epididymis, and the mediastinum or may present as intracranial (dural or brain) masses. The lesion can be clinically associated with increased levels of catecholamines and urinary excretion of vanillylmandelic acid. Gross Findings the lesion is fibrous and tan, brown, or black, depending on the proportion of the pigmented component. Microscopic Findings Microscopic features are characteristic and consist of two basic cell populations: small neuroblastic cells and larger, melanin-containing epithelial cells arranged in a distinct architectural pattern. The neuroblastic cells occasionally form larger, more diffuse areas in which epithelial alveolar structures are loosely distributed. This may create a more disorganized pattern of neuroblastic cells and solid ephithelial proliferations. Glial fibrillary acidic and S-100 proteins may be focally positive in a small-cell neuroblastic component.
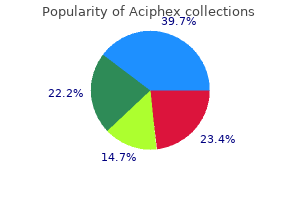
Buy aciphex master card
The lower lid and canthus were revised by loosening and supraplacement of the canthus and insertion of small spacers in the lower lid gastritis diet ��������� order discount aciphex on-line. Fatty tissue can rest directly on the levator aponeurosis, but not dermis due to the formation of scarring. C, the orbital septum can be opened to recruit superior orbital fat for repositioning in the upper sulcus area. An asymmetrical eyebrow position or eyebrow laxity can also cause crease abnormalities. B, Conversely, patients with deep-set eyes and loss of indentation have a deep upper lid sulcus. This usually occurs when cautery is blindly applied to the deep nasal fat pad to control bleeding near the trochlea. The superior ophthalmic vein and medial palpebral artery branch have close proximity to the transitional fat pad and the trochlea. Patients will generally tilt their head toward the side of the injured superior oblique muscle to define the side of injury which is consistent with the Bielschowsky head tilt test. The head tilts toward the side of the injury to compensate for diplopia (the Bielschowsky head tilt test). B, Frontal view showing the position of the nasal fat pad and the relationship to the superior oblique tendon. D, Superior view showing the position of the superior orbital vein and the relationship to the trochlea and fat pad. While the overall results and patient satisfaction are excellent, complications ranging from self-limited problems to lifelong problems can occur. Safe surgical techniques can protect patients, from requiring multiple corrective procedures after surgery. The surgeon must understand the anatomy, function, and limitations of blepharoplasty as well as prevention of problems to avoid complications. Nonetheless, one must be prepared to take care and reassure patients with complications. Complications can be divided into early complications and late complications as well as functional and aesthetic problems. One should evaluate complications, fully understand the underlying problem, and carefully create a treatment plan to restore the patient to normally functioning eyes with an improved aesthetic result. The superficial subciliary cheek lift, a technique for rejuvenating the infraorbital region and nasojugal groove: a clinical series of 71 patients. The evaluation and management of lower eyelid retraction following cosmetic surgery. Surgeons performing revision procedures have a host of techniques from which to choose. Corrective procedures for the lower lids include revision canthoplasty, secondary vertical-vector midface lift to recruit skin, and posterior lamella spacer graft to achieve lid lengthening. For upper lid repair, release and advancement of available skin is performed, and full-thickness skin grafts are used as a last resort. Often a combination with repositioning both lids to correct lagophthalmos that may be causing corneal exposure is required. Upper eyelid closure can be improved with upper lid canthal anchoring and tightening, crisscross canthoplasty, or skin grafts to the upper lid. It is dermis that has been processed and decellularized to eliminate its foreign antigenicity with a host immune system. When placed into a recipient host, it serves as a cellular support scaffold for fibroblastic and hematologic ingrowth. It was first approved for use in Europe in 1997 and is distributed in the United States by Stryker for use in the head and neck. It is used in other surgical markets under different brand names, such as Zimmer Collagen, Pelvicol, and Permacol. Two sheet sizes are commonly used for applications in the eyelid: 4 by 1 cm by 1 mm thick, or 5 by 2 cm by 0. The thicker former size is routinely used in cases of lower lid retraction, and the latter in cases requiring lateral canthal patch reinforcement. All four cases of infection occurred in patients who had a history of multiple prior revision surgeries, and all four resolved with oral antibiotic therapy. While the infection rate was low, precautions now include the use of Hibiclens skin prep. Care must be taken not to get Hibiclens in the eye, because it is indicated for external use only and can cause a chemical burn to the eye. All patients receive intravenous prophylactic antibiotics, such as cefazolin (Ancef), at the time of surgery, and an oral course of a cephalosporin such as cefadroxil (Duricef) for 1 week postoperatively. The advantages of Enduragen include the lack of an autologous donor site, it is sterile, and it has a consistent thickness (1 mm and 0. Enduragen is ready to use immediately without soaking and has lasted longer in our experience. The safe and successful use of AlloDerm has been described by several authors for treatment of lower lid malposition. In brief, scar release, lateral canthal reconstruction, and cheek elevation with a subperiosteal midface lift define this three-part approach to treating lower lid retraction. Many advocates of hard palate grafts transitioned away from the use of hard palatal grafts because of the donor-site morbidity and toward use of AlloDerm for posterior lamellar support. Hard palate grafts trended toward greater improvements in lid position in this same study, although a statistical significance over AlloDerm was not demonstrated. The performance of thick AlloDerm (72/999 inch) has been compared to that of thin AlloDerm by (7 to 14/999 inch) Taban et al for lower eyelid reconstruction. Twenty-four percent of lids actually maintained the same positioning or were lowered by an average of 0. Furthermore, its basement membrane substrate side provides the ideal surface for rapid epithelialization, and it has been shown to reepithelialize in 4 to 6 weeks. Enduragen has performed similarly to AlloDerm in the context of laboratory biomechanical testing, suggesting comparative utility as a static sling in the management of patients with a paralyzed facial nerve. Enduragen was shown to elongate significantly less than AlloDerm when subjected to a constant stress load. However, laboratory testing may not linearly correlate with graft performance after placement in a surgical wound bed. Ultimately, the scaffold should integrate into normal cellular turnover so that the scaffold is no longer recognized as separate from the host recipient. Studies by Vural et al suggest that this phenomenon might account for the stiffness of Enduragen after implantation and its lower potential for resorption compared with AlloDerm. AlloDerm demonstrated extensive cellular infiltration and change in implant shape over time. Medpor Grafts in Oculoplastic Surgery High-density porous polyethylene was introduced as a spacer graft for use in lower eyelid retraction in 2001. In a study by Wong et al, 50 implants were placed in 36 patients and outcomes were reviewed retrospectively. Only one implant in the original series became exposed through the anterior eyelid margin. Despite this low incidence of exposure, the authors indicated that porous polyethylene implants have a role in management of lid retraction after failure of other corrective efforts. Effective correction of lower lid retraction has been described with use of ultrathin porous polyethylene implants in 35 lids of 32 patients. Forty-two percent of patients experienced a complication, with 22% of patients experiencing a major complication such as infection, implant exposure, or implant removal. Minor complications occurred in 25% of patients, and most required surgical removal of the implant. Advantages of ultrathin porous polyethylene implants include its off-the-shelf availability for patients who are incapable of undergoing long periods of anesthesia, and the absence of a donor site for implant harvest. For this reason, we do not recommend routine use of ultrathin porous polyethylene for treatment of lid retraction.
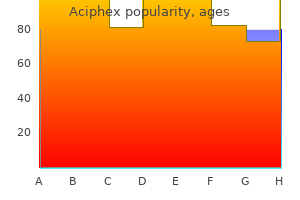
Order aciphex australia
Consequently gastritis workup purchase cheapest aciphex, most cases are located within the soft tissue of proximal parts of the extremities, in the soft tissues of the buttocks, and in the shoulder region. After reviewing the literature, they found only 18 examples in bone, 15 of which occurred in the mandible or maxilla. In view of these data, primary intraosseous malignant peripheral nerve sheath tumor is one of the rarest neoplasms of bone. Microscopically, a typical malignant peripheral nerve sheath tumor is a spindle-cell sarcoma that resembles a fibrosarcoma in regard to its overall cellular structure and architectural organization. In contrast to typical fibrosarcoma, most malignant peripheral nerve sheath tumors are histologically of high grade and show prominent nuclear atypia. Similar to fibrosarcoma, the cells are arranged in fascicles with an occasional herringbone pattern. On rare occasions, foci of skeletal muscle differentiation (malignant Triton tumors) or glandular mucin-secreting structures can be seen. The latter are diagnosed as malignant peripheral nerve sheath tumors because they arise in major nerves or occur in a setting of neurofibromatosis. Immunohistochemically, malignant peripheral nerve sheath tumors are focally positive for neural markers such as S-100 protein, Leu-7, neurofilament protein, and myelin basic protein. Neuron-specific enolase cannot be used alone as evidence of neural differentiation because it is frequently positive in many other lesions. S-100 protein is usually only focally positive, and strong uniform positivity for this marker is rare in malignant peripheral nerve sheath tumors. In cases of strong uniform positivity for S-100 protein, other spindle-cell neoplasms (primarily cellular schwannoma) should be excluded before the diagnosis of malignant peripheral nerve sheath tumor is rendered. Ultrastructural features suggestive of neural differentiation include long, branching, and interdigitating cytoplasmic processes that contain microtubules and neurofilaments. The extracellular matrix contains basal lamina (frequently incomplete), collagen with focal features of long-spaced collagen, and amianthoid fibers. Malignant peripheral nerve sheath tumors are highly aggressive and have a high propensity to metastasize to distant sites, predominantly the lung, liver, and oddly enough, bone. In fact, most malignant peripheral nerve sheath tumors that involve the skeleton either are metastatic or represent secondary involvement of bone by a soft tissue lesion. Regional lymph node metastases are extremely unusual in malignant peripheral nerve sheath tumors. C, Axial computed tomogram showing large sacral malignant peripheral nerve sheath tumor. Scoliosis is a frequent axial anomaly and is present in approximately 50% of patients. Scoliosis in neurofibromatosis typically involves the lower thoracic region and is associated with sharp angulation that can cause paraplegia. Frequently, it is associated with kyphosis predominantly affecting the cervical segment. The most frequent skeletal anomaly is macrocrania, which can be documented in nearly 90% of children with neurofibromatosis. More significant changes in these regions include the congenital absence of a portion of the orbit or sphenoid bone or a defect involving the cranial vault. Another frequent site of this anomaly is the posterior aspect of the sagittal suture. Other anomalies of the appendicular skeleton include pseudarthrosis, focal overgrowth (gigantism), or dwarfism. The anomalies of the long tubular bones may be caused by abnormal appositional growth. In response to trauma and subperiosteal hemorrhage, it is easily detached from the underlying bone, causing large subperiosteal hematomas. Poor callus formation and frequent pseudarthrosis of long tubular bones complicating fractures can also be related to these peculiar features of malfunctioning periosteum in neurofibromatosis. Congenital pseudarthrosis usually occurs in the tibia and in the bones of the forearm. More recent clinical data, however, indicate that patients with Jaffe-Campanacci syndrome may have other stigmata of Text continued on p. A and B, Anteroposterior and lateral radiographs of tibia show erosion caused by malignant peripheral nerve sheath tumor in the overlying soft tissue. A, Lateral radiograph of skull in young adult shows geographic areas of radiolucency in occipital region. B, Anteroposterior radiograph of skull shows large frontoparietal area of sharply defined radiolucency representing absence of calvarial bone. A and B, Anteroposterior and lateral radiographs of leg of child with congenital pseudarthrosis of tibia and lateral bowing deformity of fibula. The typical clinical presentation is the onset of tinnitus or hearing loss during adolescence or early adult life because of the development of bilateral acoustic schwannomas. Patients affected with this syndrome also have an increased risk for other central nervous system tumors. Schwannomas in neurofibromatosis type 2 are similar to the more common solitary sporadic schwannomas. A and B, Severe bowing deformity of radius and remnant of proximal ulna in patient with congenital pseudarthrosis of forearm. C, Clinical photograph showing deformity of left forearm in patient with neurofibromatosis. Neurofibromatosis type 3 criteria are categorized as either definitive or possible, with an additional set of criteria for segmental schwannomatosis Table 14-3). Multiple radiolucent lesions in metaphyses of femora and tibiae bilaterally represent nonossifying fibromas. B, Lateral radiograph of left knee of patient shown in A emphasizes eccentric location of nonossifying fibromas. Additional tumors seen in this image are a middle fossa meningioma and a contralateral optic nerve sheath meningioma. Spinal cord ependymoma is the most common intramedullary spinal cord tumor in neurofibromatosis type 2. The signature lesions of neurofibromatosis type 2, bilateral vestibular schwannomas, often lead to hearing loss that can be treated via cochlear implants. A diagnosis of segmental schwannomatosis is appropriate when a patient meets the criteria for either definitive or possible schwannomatosis, but the schwannomas are confined to a single limb or to five or fewer contiguous spine segmental levels. Clinically the disease affects men and women with equal frequency and presents with multiple, often painful, schwannomas involving skin and soft tissue. Type 2 is subdivided into A, B, and C forms based on the patterns of missense mutations. The individual subtypes have different risk levels for tumor development at various topographic sites. The longer form contains 213 amino acids and the short form consists of amino acid residues 54 to 213 and lacks the acidic repeat domain. A-D, T1-weighted sagittal postcontrast magnetic resonance images showing spinal schwannomas at multiple vertebral levels in schwannomatosis. Von Hippel-Lindau disease is characterized by the frequent development of specific tumors in selected topographic sites. Affected individuals develop hemangioblastomas in the central nervous system, clear cell carcinomas of the kidney, pheochromocytomas of the adrenal gland, extraadrenal paragangliomas, endolymphatic sac tumors, pancreatic microcystic adenomas, and pancreatic neuroendocrine tumors.
Vitacarn (L-Carnitine). Aciphex.
- Improving symptoms and complications of heart disease and heart failure (chest pain, heart attack, and others).
- What is L-carnitine?
- Treating and preventing L-carnitine deficiency.
- Are there safety concerns?
- Improving low birth weight.
- How does L-carnitine work?
- Preventing side effects caused by valproic acid (Depacon, Depakene, Depakote, VPA), a seizure medication.
- Treating male infertility caused by inflammation of some reproductive organs and tissues (prostate, seminal vesicles, and epididymis).
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96985
Discount aciphex 10mg on-line
The depth of penetration is determined by the concentration of croton oil gastritis znacenje purchase generic aciphex from india, so the physician needs to prepare solutions of varying concentrations for each treatment area, such as 0. Another tool that can be used to assess the depth of the peel is epidermal sliding, which occurs when the epidermis separates from the papillary dermis and slides away from the face as a sheet. The number of coats of the peel solution applied has an additive effect, so scarring can result even when low concentrations are used. A Polysporin-Xylocaine jelly mixture is usually applied after the procedure and given to the patient to take home and use on an as-needed basis. Methylprednisolone is given to decrease swelling, and pain is managed with ibuprofen and narcotics as needed. Proper patient selection is key to avoid problems with scarring, hyperpigmentation, and hypopigmentation. Hyperpigmentation is usually transient and responds well to tretinoin and hydroquinone therapy. Scarring can be treated with triamcinolone (10 mg/ml) and 5-fluorouracil injections. Hypopigmentation treatment options are limited, but this result occurs infrequently and usually softens over time. Milia that are seen early during the healing phase can be effectively treated with tretinoin. Although the carbon dioxide laser was developed in 1970, its first use for skin resurfacing was in 1992. As selected layers of skin were "vaporized," new skin elements reformed from adnexal structures with reorganized compact collagen, an extracellular matrix, and new keratinocytes. The treated skin was better hydrated and had renewed elastic properties, which effaced wrinkles and conferred a rejuvenated appearance. It again used water as its target chromophore, but because the laser was more efficiently absorbed, less damage was imparted to surrounding tissues as a result of scatter. From then on, lasers were developed to address various chromophores-such as melanin, hemoglobin, and tattoo ink-with expanding indications and increased efficiency. Treated areas called microthermal treatment zones are separated by zones of normal untreated skin that foster the faster healing of the surrounding laser-injured tissue. Treatment areas can be extended to depths that are unattainable with traditional lasers, because an extensive injury at the deeper level would lead to scarring or pigment changes. The caveat when considering fractionated laser therapy is that up to six sessions spaced 2 to 4 weeks apart are required to achieve results equal to those that can be achieved with one ablative laser session. Fractional laser therapy is indicated for patients who are seeking skin tightening, fine wrinkle reduction, pigment homogenization, and the smoothing of acne scars. It delivers coherent pulses of 1550 nm to its water chromophore over 15% to 25% of the scanned treatment area. Typical microthermal treatment zones are 100 microns in diameter with 300 microns of normal skin between them. Patients of all Fitzpatrick skin types may be treated without a significant risk of pigment changes. Herpetic infection prophylaxis is generally not required except in patients with a history of multiple annual outbreaks. All makeup is removed, and a topical anesthetic is applied for about 1 hour before treatment. Multiple overlapping passes are used at various energy settings, depending on the indication; for example, rhytids may require 20 to 50 mJ, acne scars may need 40 to 70 mJ, and melasma may be treated with 6 to 8 mJ. Patients report a sunburnlike sensation 2 to 12 hours after treatment, depending on the energy level used. The stratum corneum remains intact at the time of treatment, and the epidermis is healed within 24 hours. Because a great deal of surface area goes untreated, there is essentially no crusting or weeping. Erythema and edema can be expected after 2 to 6 days, with some light flaking occurring after 3 to 6 days. Treatments are generally spaced a few weeks apart until the desired aesthetic result is achieved. Electron flow causes polarized molecules to rotate and vibrate, thereby generating heat through friction. Because the resistance to the flow of electrons by epidermal and papillary dermal proteins is low, selective heating occurs in the resistive tissue of the deep dermis and in the fibrous septa within the subcutaneous space. As with laser therapy, skin collagen is denatured by heat, which is then reorganized in a more compact fashion to produce tissue with renewed vasoelastic properties. Thermage, ReFirme, and eMatrix all make use of electric fields to generate heat within tissue. Contraindications include collagen-vascular disease, autoimmune disorders, and immunosuppression; recent (<6 months) isotretinoin treatment; irradiated tissue; and treatment over metal implants or hardware. Pacemakers and defibrillators may be inactivated with radiofrequency therapy, so medical clearance is required. The safety of radiofrequency therapy for pregnant women has not yet been established. Treatment tips that vary the depth of energy concentration, that make use of thermal gradients, and that have varying sizes have been designed to accommodate unique anatomic areas like the eyelids. Patient discomfort during radiofrequency therapy can be mitigated by pretreatment topical analgesics. It differs from radiofrequency methods, however, in that no energy is imparted to tissues superficial to the treatment area, thus making skin cooling unnecessary. Megahertz-frequency ultrasound waves are delivered in short pulses at depths of 1. Another advantage of ultrasound-based therapy is the associated visualization of blood vessels before the delivery of energy, which limits vessel trauma and potential bruising. The procedure can be moderately painful, especially when an extensive area is treated. Pretreatment with topical analgesics and anxiolytics may be required, but many patients are able to tolerate therapy without additional analgesia. Ultherapy provides a nonsurgical face-lift option that has been approved by the U. Patients with extensive skin ptosis or laxity, heavy lipoptosis with jowling, and marked platysmal banding are not candidates for Ultherapy; these patients are better served with surgical interventions. Relative contraindications to Ultherapy include treatment directly over keloids, implants, and fillers, because this may cause further scarring, malfunction, or volume loss, respectively. Judgment should be exercised before treating patients who are at risk for bleeding complications, poor wound healing, infection, or the exacerbation of an autoimmune disorder. B, Elevation of the eyebrows with an increase in the brow-to-lash distance and lifting of the forehead and cheeks after Ultherapy. Various cutoff filters are used to exclude a spectrum of wavelengths to allow only certain treatment wavelengths of 400 to 1200 nm to reach the skin. Because higher fluences are required to achieve desired effects among dark-skinned individuals, risks of epidermal injury and burns increase. In addition to specific wavelengths, unique treatment protocols that involve changes in technique or treatment frequency may be used for the treatment of dyschromia, vascular lesions, or unwanted hair. Practitioners should refer to specific manufacturer recommendations for each indication. Patient response to therapy also varies, with angiomas and telangiectasias clearing after two to three sessions and portwine stains requiring eight or more sessions for successful treatment. Postprocedure care includes the application of ice packs to cool the treatment area, the use of a low-potency corticosteroid cream for 2 to 3 days to speed healing and increase comfort, and direct sun exposure must be avoided for 1 week. Proper wound care and frequent follow-up care are required until symptoms resolve. Hypopigmentation is also rare, but it is difficult to treat when it occurs; the only treatment options are ultraviolet light therapy and time. It was developed as a method for the treatment of acne scars, hypertrophic scars, and traumatic scars. However, new and old scar correction with the use of dermabrasion can be very effective. Superficial demarcated scars can often be completely blended into the surrounding skin. Wider depressions in the skin can also be softened, but they are usually not completely eliminated.
Generic aciphex 10mg visa
We have achieved safe and effective rejuvenation of the lower eyelids while maintaining a natural lower eyelid shape symptoms of upper gastritis 10mg aciphex otc, with minimal risk of scleral show or ectropion. Providing routine lateral canthal support and performing orbicularis suspension to minimize the risk of lower lid malposition are of paramount importance. It corrects lower lid puffiness and dark circles from excess fat and shadowing, as well as loose, wrinkled skin in the lower eyelid while maintaining a natural lower eyelid shape. Therefore skin-muscle flaps have proved scientifically safe and reliable, and, when properly performed, they do not damage the lower eyelid. This demonstrates that very little downward force after a blepharoplasty from swelling and scar contracture can cause an ectropion. The patient shows no evidence of denervation postoperatively in the pretarsal muscle above the incision. B, She underwent a transcutaneous lower blepharoplasty with a spacer graft and is shown postoperatively. In our practice, we have provided lateral canthal support in 100% of the lower blepharoplasty cases for decades. The use of this approach has eliminated frank ectropion after a lower blepharoplasty and has reduced lower lid malposition with scleral show to less than 3%. For a blepharoplasty, a transseptal approach provides direct access to the excess lower eyelid fat for removal and facilitates release of the orbitomalar ligament for fat transposition. Although this is a safe procedure, it requires stretching the lower lid for exposure, which can increase the baseline level of tarsoligamentous laxity; therefore a routine canthopexy should be considered. A skin-pinch excision, chemical peel, or laser treatment can be performed to address the lower eyelid skin; however, no orbicularis is removed or tightened, significantly limiting the degree to which this procedure will smooth the lower eyelid appearance. A word of caution is warranted regarding treatment with chemical peels and lasers to the eyelid skin because this is the thinnest skin in the body, with no subcutaneous layer. Removing eyelid fat with only a transconjunctival blepharoplasty can produce a skeletonized appearance to the lower lid and lid-cheek junction if only fat is removed or if the fat is overresected. B, An incision through the conjunctiva and capsulopalpebral fascia allows fat to herniate. Surgeons should address these subjective concerns by performing a physical examination, which will reveal objective, anatomic, and age-related changes that can be documented. A lower lid snapback test is performed, with assessment of tarsoligamentous laxity. Patients who have more than 18 mm of globe prominence are at increased risk for lower lid malposition after a lower lid blepharoplasty without lateral canthal support. Most patients are concerned about the excess tissue in their lower eyelid causing puffiness and wrinkles. On examination, most patients have lower eyelid fat herniation, fat excess, and skin-muscle excess with decreased skin elasticity. Tarsoligamentous laxity is often directly proportional to age and requires a single suture to maintain the shape of the lower eyelid. For patients whose hyperpigmentation and dark circles cause them to look tired, skin care that includes hydroquinone may be combined with surgery. For patients with more advanced aging changes, an extended lower lid blepharoplasty with fat grafts, fat transfer, or a filler for malar augmentation may be performed to create a smooth lid-cheek junction at the time of surgery under direct visualization. A lower lid blepharoplasty combined with a midface lift is appropriate for these patients and is discussed in Chapter 9. A, Anatomic changes that occur with aging: ptosis of the orbicularis oculi muscle and descent of the malar fat pad. B, External manifestations of aging changes include the formation of midfacial creases and folds. A limited quantity of fatty tissue may be contiguous to these more prominent fat pads. The volume of the fat prominences varies from patient to patient and should be noted preoperatively and recorded photographically. Determining which fat pads are most prominent can be difficult when the patient is on the operating table. Excess lower lid fat is often excised so that it is flush and even with the infraorbital rim. Lower lid fat should not be overresected, because this can cause long-term hollowness in the lower orbit. Fat is also often released from the septum and retrieved over the infraorbital rim to blend the lid-cheek junction. This is performed after the orbitomalar ligament is released to create a space for the repositioned fat. Alternatively, volume can be added to the lower lid using free fat grafts 2 to 3 mm in size taken from the excess fat removed from the upper blepharoplasty or the lateral fat pad of the lower eyelid. Therefore the lower lid should be evaluated for preexisting scleral show and laxity using a snapback test. If a blink is required to reposition the lower lid by tightening the pretarsal muscle, then significant lower tarsoligamentous laxity is present. This is an indication for lateral canthal support during a blepharoplasty procedure. A distraction of more than 6 mm of excess lower lid indicates significant tarsoligamentous laxity and is an indication for a lateral canthoplasty. If laxity is noted preoperatively, when orbicularis oculi muscle tone is present, it will be much more obvious intraoperatively, when the patient is anesthetized. Thus the results of an intraoperative evaluation should supersede those obtained in the office. In some cases, canthopexy or simple tightening can be performed to strengthen the lower lid tone and to provide lid stability. Frequently, however, horizontal tightening procedures with a lateral canthoplasty and lid tightening are necessary to provide stability and to prevent lower lid malposition. The relationship between eye prominence and the eye fissure shape is noted and is helpful for choosing the vertical point of fixation for lateral canthal anchoring. Degree of eye Prominence Standard Eye Position: Hertel Measurement of 15 to 18 mm the position of lower lid fixation in an eye with standard prominence is in line with the center of the pupil. This point of fixation produces a normal eye fissure shape when the canthus is anchored laterally. Deep-Set Eyes: Hertel Measurement of Less Than 15 mm Many patients naturally have a recessed or deep-set position to their eyes in relationship to the lateral orbital rim. This condition is more commonly seen in elderly patients with atrophic enophthalmos. Standard canthal anchoring, or even skin redraping in a vertical vector, can cause upward clotheslining of the lower lid, which produces narrowing of the eye fissure and reduction in the size of the lateral scleral triangle. The position most often used for a lateral canthopexy is deep within the orbit at the level of the inferior pupil. This is a common indicator that a patient has a high risk for lower lid malposition or ectropion if no canthal support is provided during a lower blepharoplasty. These patients have a greater risk of the lower lid pulling downward after a lower lid blepharoplasty, and a standard horizontal tightening procedure may exacerbate the problem by clotheslining the lid margin underneath the prominent eye. With only mild prominence, supraplacement of the lateral canthal tendon at the level of the superior pupil may suffice and allow the lid to ride up on the globe as needed. With increasing eye prominence, however, the success of supraplacement of the canthus is limited. Overelevation of the lower lid in patients with very prominent eyes will impair upper lid closure. Special techniques are needed, such as recession of the inferior retractors or insertion of primary spacer grafts. With age, and in some individuals or families, the tilt is reversed, causing the fissure to have a negative canthal tilt. Patients should be asked to describe how they see their eye shape as it relates to their lateral canthal position. Patients who have developed deep-set eyes from aging should review older photographs of themselves to determine the desired final shape of the eyes. Changing the canthal tilt from negative to positive may be too much of a change for these patients or may be a desired result after a lower lid blepharoplasty.
Generic aciphex 20 mg on-line
The risk of colorectal cancer in patients with ulcerative colitis and sclerosing cholangitis exceeds that associated with ulcerative colitis alone gastritis symptoms bleeding order aciphex with visa. Patients usually present with complications of biliary stricturing, such as obstructive jaundice, cholangitis or abnormal liver-function tests (raised alkaline phosphatase and -glutamyltranspeptidase) at routine screening. Liver transplant is the only hope of long-term survival in those who do not develop cholangiocarcinoma; otherwise, median survival for symptomatic patients is about 15 years. Multiple strictures, particularly in the intrahepatic biliary tree, give a beaded appearance. It is characterized by irregular narrowing of the pancreatic duct and swelling of the gland itself. Pauciarticular disease involves fewer than five joints; characteristically, it affects one large joint, for example the knee, and is most common in women. Attacks usually coincide with relapse of colitis; sometimes there is simultaneous erythema nodosum or iritis (see below). Its pathogenesis may involve deposition of gut-derived immune complexes in the affected joint in genetically predisposed individuals. Although the attacks of arthritis may come and go over many years, the disease is neither progressive nor deforming. Alternatives include 36 paracetamol (acetaminophen) and joint aspiration with steroid instillation. It presents with low backache and morning stiffness, although it can also be asymptomatic. In contrast to mechanical back pain, it is insidious in onset, occurring in younger people. Pyoderma presents initially as a discrete pustule with surrounding erythema; this develops into an indolent painful enlarging ulcer. Lesions are occasionally multiple and may occur at sites of recent trauma, for example operation scars. Histology shows lymphocytic vasculitis with dense secondary neutrophilic infiltration. Pyoderma is often refractory to treatment: options include intralesional, topical and systemic corticosteroids, dapsone, heparin and immunosuppressive drugs such as ciclosporin (cyclosporine), but the most effective is infliximab. Together they occur in fewer than 5% of patients, usually when bowel disease is active. Uveitis is a more serious and often recurrent problem, presenting with headache, red eye and blurred vision; slit-lamp examination shows pus in the anterior chamber (hypopyon). The disease is asymptomatic for many years, presenting eventually with vertebral collapse or long bone fractures. They should avoid becoming either undernourished or obese, stop smoking and take regular exercise. Those with established osteoporosis, or needing long-term therapy with prednisolone, should receive cyclic bisphosphonate therapy. Hormone replacement therapy is associated with an increased risk of breast and gynecologic cancer and thromboembolic disease. The commonest cause is iron deficiency due to intestinal blood loss (often occult), poor iron intake and/or reduced mucosal absorption and cellular utilization of iron as a result of an inflammation-induced increase in serum hepcidin, a peptide hormone produced by the liver which regulates iron transport. Although anemia may seem to be asymptomatic, and indeed is often ignored by doctors, it causes fatigue and impairs quality of life and cognitive function; when severe it can cause shortness of breath and reduce exercise tolerance. Iron should be replaced initially with low-dose oral iron (no more than 100 mg of elemental iron daily) to minimize the risk of intestinal side effects, which are dose-related and include abdominal pain, constipation and diarrhea. Vitamin B12 and folate deficiencies should be replaced with intramuscular vitamin B12 and oral folate, respectively. All patients admitted to hospital, whether as emergencies or for elective surgery, should be kept as mobile as possible and given prophylactic heparin (see Chapter 6). Fatigue is a persistent and overwhelming sense of tiredness, weakness or exhaustion that reduces the capacity for physical and/or mental work and is characteristically unrelieved by sleep or rest. In some patients, one or other of these causes can be identified and treated specifically, but in many their fatigue has no clear explanation. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. Extraintestinal manifestations of inflammatory bowel disease: epidemiology, diagnosis, and management. Consensus statements on the risk, prevention, and treatment of venous thromboembolism in inflammatory bowel disease. Musculoskeletal manifestations in inflammatory bowel disease: a revisit in search of immunopathophysiological mechanisms. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. In younger patients (under 50 years) the main differential diagnoses, depending on presentation, include infection and irritable bowel syndrome. In older people (over 50 years), neoplasia, diverticular disease and ischemia require special consideration. In patients presenting for the first time with diarrhea, a negative test for endomysial or transglutaminase antibodies usually excludes celiac disease. For patients who have recently traveled to endemic areas, serology (as well as stool samples) should be checked for amebiasis, strongyloidiasis and schistosomiasis. Hot fresh samples are essential in recent travelers to look for amebic trophozoites. The transmigration of neutrophils through the mucosa into the lumen is responsible for crypt abscesses and exudate formation. Fecal levels of calprotectin, a neutrophil-derived cytosolic protein that is resistant to bacterial degradation, provide an accurate index of intestinal inflammatory activity. To minimize the risks of bleeding and perforation, a small superficial biopsy should be taken from the posterior rectal wall less than 10 cm from the anal margin using small-cupped forceps. Rectal biopsy is not routinely necessary for those with established ulcerative colitis. Sometimes, however, rectal induration or ulceration, or the presence of perianal disease, points to the diagnosis. In patients who are not severely ill, colonoscopy with biopsies is the most useful test for confirming the diagnosis of ulcerative colitis and assessing disease extent and activity. In chronic cases, pseudopolyps and loss of the normal haustral pattern with apparent shortening of the colon are common. In patients with acute severe ulcerative colitis, colonoscopy may cause perforation and dilation, and most sick patients can be managed satisfactorily without it. However, colonoscopy plays a major role in cancer surveillance in those with chronic extensive ulcerative colitis (see Chapter 7). Later, larger pleomorphic deep ulcers develop, separated by relatively normal-looking mucosa. The advent of wireless capsule endoscopy enables non-invasive visualization of small bowel that is inaccessible to the conventional endoscope. In patients presenting with active disease, a plain film is useful to assess the extent of disease, since fecal residue on a radiograph usually indicates sites of uninflamed colonic mucosa. A plain film (preferably with the individual both supine and erect) is essential if small-bowel obstruction is suspected. Classically, but exceptionally, complicating radio-opaque urinary stones or gallstones are seen (see Table 3. This test has now been largely superseded by colonoscopy in ulcerative colitis; both tests are potentially dangerous in active disease.
Aciphex 10 mg overnight delivery
Unfortunately gastritis diet ���� generic aciphex 10 mg without prescription, many of these patients may turn out to have squamous cell carcinoma of the conjunctiva or sebaceous cell carcinoma. In any long-standing case of chronic conjunctivitis that is not responding to reasonable medical treatment, a full-thickness eyelid biopsy should be performed to rule out these processes. A biopsy of the conjunctiva of the right upper lid showed squamous cell carcinoma. B, She is seen with eyelid and conjunctival lymphoma that, after biopsy, was found to be squamous cell carcinoma. C, Despite superficial radiotherapy, the lesion progressed and required exenteration that included the eyelids and globe but spared the muscles. D, A small tissue conformer was used to expand the skin to help reconstruct the eyelids. It is very important to submit suspiciousappearing chalazion tissue to a pathologist. A rare situation occurs with metastatic eyelid carcinoma in which approximately two thirds of lesions metastatic to the eyelid present as metastatic nodules. These lesions are generally painless; however, as mentioned previously, in 38% of the cases in the literature, the eyelid lesion was a presenting sign of a carcinoma elsewhere. Other neoplastic processes that may present as chalazions are lymphoid lesions or extranodal lymphomas and the rare trichoepithelioma. She presented with restricted orbital movement and infiltration of the right orbit. Treatment for allergies and for a variety of skin problems such as eczema and psoriasis may be undertaken before a neoplastic process is considered. The pagetoid (intraepithelial) component of sebaceous cell carcinoma can also produce a dermatitis-like condition. Morpheaform basal cell carcinomas produce stiffness, thickening, and scaliness of the skin, thus mimicking scleroderma. Although most of these patients truly have only actinic shrinkage, morpheaform basal cell carcinoma can also produce skin contracture. Many patients have been treated for simple cicatricial ectropion when they in fact have invasive morpheaform basal cell carcinoma, which may cause the skin to become indurated and thickened. When repairing any cicatricial ectropion that involves sun-damaged skin, tissue should be submitted for histologic examination. B, Another patient was initially diagnosed with ectropion but was later found to have morpheaform basal cell carcinoma. More extensive distortion of the lashes across the lid margin may appear as upper lid entropion. Most patients who have upper lid entropion acquire it as a result of a scarring inflammatory process such as trachoma or a mucocutaneous disease such as ocular pemphigoid. Patients who have refractory progressive disease, particularly with thickening of the eyelid, should undergo a full-thickness biopsy of the most suspicious area. Purely dermatologic conditions such as rosacea can yield similar results, but neoplastic disease may need to be ruled out in some patients whose conditions demonstrate a refractory clinical course. The most insidious neoplasm that presents in this manner is sebaceous cell carcinoma, which also often involves pagetoid changes. Another neoplastic process that occurs in the periocular area, that has neurotropic tendencies, and that may extend to the eyelids is carcinoma of the lacrimal gland. In our clinical experience, we have seen 14 patients in whom neurotropic invasion was the presenting sign of a neoplastic process or the first sign of recurrence. The biopsy showed infiltrative squamous cell carcinoma with perineural invasion of the infraorbital nerve. B, the biopsy of the right supraorbital nerve (arrows) showed perineural invasion. The patient died of cardiac arrest, and no postmortem permission for autopsy could be obtained. The risk of missing an underlying neoplasm is always possible if a superficial biopsy is taken of a suspicious eyelid lesion. If the tumor is relatively small, excisional biopsy of the entire lesion may be performed. In many cases, a wedge of a larger tumor may be excised as a biopsy specimen as a preliminary step for Mohs surgery. The specimen should be representative of the clinically abnormal lesion; ideally, it should incorporate adjacent normal tissue, it should be sufficiently large for histologic processing, and it should not be crushed or excessively traumatized. B, A full-thickness biopsy of the eyelid margin must be obtained to detect any intralid processes. Special staining techniques can help to differentiate intraepithelial lesions, such as sebaceous cell carcinomas, squamous cell carcinomas, and superficial basal cell carcinomas. Epithelial biopsies are often misinterpreted with regard to the exact type of tumor. For example, squamous cell carcinoma may be diagnosed when the lesion is a sebaceous gland carcinoma with pagetoid skin changes. Such microscopic evaluation may be performed by examining frozen sections at the time of surgery, which allows the surgeon to immediately remove additional tissue if the tumor is histologically present at the margin of the incision. In the case of tumors such as basal cell carcinomas, which usually grow from a single focus, a very high cure rate can be achieved if the extent of resection is controlled by frozen section examination of the margins. For patients in whom the histologic margin of the tumor extends into the orbit, orbital exenteration or irradiation may be required. With malignant eyelid tumors that are multicentric in origin, such as sebaceous cell carcinomas, it may not be possible to completely rely on the examination of resection margins, because only one focus of the lesion may be removed. For tumors that cause early distant metastases, such as nodular melanomas, clear margins offer no guarantee against regional or systemic metastatic disease. The two techniques performed in these locations differ with regard to the methods of sectioning and examining the margins, which are described in the following sections. We resect the primary tumor with gross margins free of tumor, depending on the tumor type. We then send additional margins for frozen section analysis, with immediate reexcision occurring if the results are positive. The dermatologic surgeon performs the excision and sectioning with tumor mapping until clearance is obtained. This allows the pathologist to establish the characteristics of the specific lesion. Additional tissue edges are then submitted in a numbered and orderly manner in separate containers. If a positive margin is encountered, additional edges must be taken until the margin is clear. However, if the lesion is very large and irregular, it can be taxing on the surgeon and the pathologist; this may lead to some imprecision of excision and possibly result in the sacrifice of large amounts of uninvolved tissue. B, the pathologist may vary the orientation when taking the free-floating intraoperative specimens. In most cases, this requires the sacrifice of tissue with very wide margins to have the best chance of eradication of the tumor. It is necessary for the physician to collaborate with an experienced dermatologic surgeon when performing this procedure. Mohs excision is a form of surgical resection in which the tumor is excised in small lamellar tissue blocks. If tumor is present, additional lamellar blocks are excised from the adjacent tissue until all of the malignancy has been removed. In the past, this procedure was called chemosurgery if the tissues were fixed in vivo with chemicals. Mohs excision is time consuming, but it is the most precise of all procedures for ensuring complete tumor removal and preserving normal uninvolved tissues. This procedure is particularly useful for the treatment of tumors that are clinically indistinct but that may still be invasive, such as morpheaform basal cell carcinoma, squamous cell carcinoma, any recurrent tumor, and extensive facial-orbital tumors. It is our practice to use Mohs surgical excision for all lesions, except for those that are very small, distinct, and noninvasive in appearance. To identify this sentinel node, a radioactive tracer is injected into the dermis at the primary tumor site; this can provide a road map that reveals the sentinel nodes.
Aciphex 10mg sale
Soft tissue changes of the intraorbital gastritis home remedy 20mg aciphex with mastercard, submuscular, and subcutaneous fat compartments occur with the loss and descent of soft tissue. The skin and orbicularis and the surface contours that create the relationship between the forehead and midface, as well as the development of wrinkles, sun damage, and excess skin, are the most visible signs of periorbital aging. Therefore one should evaluate each anatomic component to develop a plan for correction and improvement. B, the youthful brow in a male is lower on the supraorbital rim without a significant arch. The temporal fat pad and retroorbicularis oculi fat help to support the lateral brow by maintaining volume. Involution of the soft tissue along the temporal and frontal region leads to temporal hollowing and eventually to descent of the lateral brow. Undercorrection of lateral brow ptosis in a patient undergoing upper blepharoplasty can leave the patient unhappy with the results. Furthermore, fat augmentation with fat grafting can improve the contour of the lateral brow highlight. In cases of severe brow ptosis and dermatochalasis that obstruct vision, a patient may overcompensate by contracting the frontal muscle attempting to raise the brow. The nasal fat pad has been found to be stem cell rich and appears more prominent with age, whereas the central preaponeurotic fat is stem cell poor and involutes with age. Overresection of medial skin, muscle, or fat creates an A-frame deformity often seen with aging and also made worse with overzealous fat removal during traditional blepharoplasty. Therefore a contemporary approach to blepharoplasty should restore the fullness seen in the youthful upper eyelid, address underlying soft tissue ptosis, and replace volume loss in the brow and temporal area to avoid a hollow appearance to the upper lid sulcus or an "operated" appearance. As opposed to excisional techniques, volume replacement can lend support to the overlying skin envelope and restore the brow and lateral lid to a natural position. The reintroduction of fat to depleted areas, which is performed with conservative lifting techniques when indicated, can yield youthful and attractive results. In patients with advanced brow or forehead ptosis, a forehead lift may also be needed. Loss of support, the development of tarsoligamentous laxity, septal attenuation, and eyelid skin laxity contribute to the appearance of lower eyelid "bags" from herniation of the orbital fat pads. In severe cases, negative canthal tilt, scleral show, or worsening of dry-eye symptoms may occur. Classic signs of preorbital aging include the loss of a full, smooth lid-cheek junction. Patients complain of "dark circles," which are often related to the underlying convexity caused by the orbitomalar ligament creating the surface appearance of the nasojugal groove/tear tough medially and the orbitomalar groove laterally. A clear separation between the thin eyelid skin and thick cheek skin over the orbital rim causes a double convexity. The addition of fat in the midface to camouflage this volume deficit can be performed alone or during a blepharoplasty, which can also remove and reposition fat to create a more youthful lower eyelid. This volume restoration and redistribution will reduce the risk of a hollow appearance to the lower lids often associated with conventional surgery. The transfer of damaged cells, which may not survive, will also impair the revascularization of the healthy uninjured cells. Therefore a successful technique should minimize trauma to the cells and remove the nonviable cells before fat grafting. Although the success of fat grafting depends on many factors, the method of harvesting undoubtedly contributes to the eventual longevity of a transplanted graft. Sites for fat harvesting include the areas deemed appropriate for liposuction, namely, the abdomen, flanks, and lateral thighs. Studies have analyzed cell viability in aspirates obtained from the abdomen, flank, thigh, and medial knee and found no difference in adipocyte viability. Others contend that the fat cells are smaller and less fibrous along the inner part of the knee, thereby rendering it most suitable for grafting specifically in the periorbita. Fat grafting to the periorbital region can be done under local anesthesia alone as a single procedure or during other procedures, such as blepharoplasty or face lift, which may require general anesthesia. As with any procedure, the risks and benefits and possible complications, including resorption, contour irregularities, infection, and granuloma formation or excess fat associated with the thin eyelid skin, must be discussed with the patient. Both areas are easy to access in the supine position and most commonly have readily available fat excess for harvest. If fat will be removed from the medial thigh, it should be harvested from both thighs for postoperative symmetry. A 1:1 ratio of local anesthetic to anticipated lipoaspirate is used to minimize cellular trauma and lysis during the harvest. High negative pressures generated by a traditional suction apparatus and even larger syringes invariably violate the fragile cell walls and render the aspirate unsuitable for successful replantation. The cannula should be moved in a fanlike motion to avoid overresection in one area and subsequent contour deformity, a recognized complication of the donor site. Typically, the surgeon should harvest at least two to three times the fat that is planned for injection. Fat graFt PreParation Based on the idea that only undamaged adipocytes will survive after reinjection, most surgeons attempt to refine harvested samples so that the robust, intact cells are separated from ruptured cell membranes and lipid byproducts that would not otherwise survive and could potentially threaten intact cell viability in the recipient bed. Sedimentation by gravity is one such means of purification but can require some time. There are various ways to prepare the fat for injection, including centrifugation; however, there are no definitive studies to show that centrifugation improves fat cell viability compared with noncentrifuged fat. The Coleman method supports the notion that intact harvested parcels of fat can withstand brief centrifugation without rupture or cell lysis. Centrifugation of fat above 3000 rpm or longer than 3 minutes will decrease fat cell viability. There are three layers to the centrifuged fat, with the usable fat in the middle layer. The lower tumescent layer is drained before transfer to a 1 cc syringe for injection. B, the Revolve system can be used; the advantage is that the fat is collected by a closed system and that it is also washed before injection. The fat is collected with a sterile tongue depressor and carefully placed into 10 cc syringes through the posterior opening with the plunger out. The fat graft is then transferred with a closed connector to a 1 cc syringe to facilitate grafting in small amounts, which is of paramount importance in the periorbital region. Blunt cannulas are used to minimize bruising and trauma to the fragile tissue around the orbit and to reduce the risk of intraarterial injection. It has been documented that injection into the supraorbital artery can cause retrograde flow into the central retinal artery, and there have been reports of impaired vision and blindness. Therefore fat grafting is performed using a blunt cannula with a serial threading technique, which injects small amounts of fat or approximately 0. This technique maximizes the surface contact of the fat to the native tissue, thereby improving its chance of survival. B, the thin linear fat grafting that should be injected is shown on the right of the Telfa, compared with the undesirable depot injection shown on the left side of the Telfa. It is often easiest to start deep at the preperiosteal level and then sequentially layer the fat aliquots up to the deep surface of the muscle. However, the urge to overcorrect the area and overly distend the plane with layer on layer should be resisted, since graft viability can be jeopardized by physically increasing the distance from the vascularized surfaces necessary to sustain the graft. Grafting in small aliquots will actually improve viability, so that the degree of correction obtained in the operating room is maintained in the postoperative period and over the long-term. Small-volume fat grafting techniques also avoid contour irregularity and allow more precise injection, which is essential around the eyelids compared with fat grafting techniques to other anatomic areas that are considered large-volume fat grafting. If only upper eyelid fat injection is needed, a small incision is made at the mid brow, and small amounts are injected into the retrorbicularis space in the area above the supratarsal crease. The small triangle at the apex of these marks is extended to this mark and defines the area of the tear trough. In this specific region, the volumes infiltrated should be particularly conservative, usually one or two layers, to mask upper lid hollowing that is associated with aging or a previous upper lid blepharoplasty; these small volumes will also minimize the risk of nodule formation and visibility.