Cheap 100mg dapsone with visa
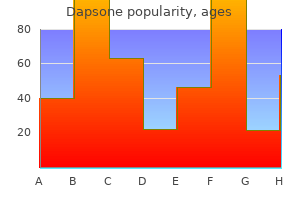
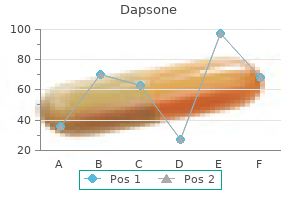
Avoid or use with caution if history of hepatotoxicity with other drugs or in active liver disease acne juvenil buy line dapsone. Monitor liver function if treatment continues for longer than one month, if receiving other hepatotoxic drugs, if history of hepatotoxicity with other drugs, or in hepatic impairment Counselling Patients should be told how to recognise signs of liver disorder and advised to seek prompt medical attention if symptoms such as anorexia, nausea, vomiting, fatigue, abdominal pain or dark urine develop 5 Infections Heart failure Following reports of heart failure, caution is advised when prescribing itraconazole to patients at high risk of heart failure. Itraconazole should be avoided in patients with ventricular dysfunction or a history of heart failure unless the infection is serious. By mouth, oropharyngeal candidiasis, see under Sporanox oral liquid below Vulvovaginal candidiasis (see also Recurrent Vulvovaginal Candidiasis, section 7. By intravenous infusion, systemic aspergillosis, candidiasis and cryptococcosis including cryptococcal meningitis where other antifungal drugs inappropriate or ineffective, histoplasmosis, 200 mg every 12 hours for 2 days, then 200 mg once daily for max. By intravenous infusion, 6 mg/kg every 12 hours for 2 doses, then 4 mg/kg every 12 hours (reduced to 3 mg/kg every 12 hours if not tolerated) for max. Oropharyngeal candidiasis (severe infection or in immunocompromised patients only), 200 mg with food on first day, then 100 mg once daily with food for 13 days. Prophylaxis of invasive fungal infections in patients undergoing bone-marrow transplantation or receiving chemotherapy for acute myeloid leukaemia and myelodysplastic syndrome who are expected to become neutropenic, and who are intolerant of fluconazole or itraconazole, 200 mg 3 times daily with food, starting before transplantation or before chemotherapy and continued until neutrophil count recovers. Monitor liver function before treatment and during treatment 5 Infections Contra-indications acute porphyria (section 9. Doctors should review patients who are being treated with oral ketoconazole for fungal infections, with a view to stopping treatment or choosing an alternative treatment. Patients with a prescription of oral ketoconazole for fungal infections should be referred back to their doctors. Systemic absorption may follow use of miconazole oral gel and may result in significant drug interactions. Nystatin is used for oral, oropharyngeal, and perioral infections by local application in the mouth (section 12. Amphotericin by intravenous infusion is used for the treatment of systemic fungal infections and is active against most fungi and yeasts. Lipid formulations of amphotericin (Abelcet and AmBisome ) are significantly less toxic and are recommended when the conventional formulation of amphotericin is contra-indicated because of toxicity, especially nephrotoxicity or when response to conventional amphotericin is inadequate; lipid formulations are more expensive. For the role of amphotericin in the systemic treatment of fungal infections, see p. For the role of echinocandin antifungals in the prevention and systemic treatment of fungal infections, see p. Resistance to flucytosine can develop during therapy and sensitivity testing is essential before and during treatment. For the role of flucytosine in the treatment of systemic candidiasis and cryptococcal meningitis, see p. Griseofulvin is effective for widespread or intractable dermatophyte infections but has been superseded by newer antifungals, particularly for nail infections. Duration of therapy is dependent on the site of the infection and may extend to a number of months. Terbinafine is the drug of choice for fungal nail infections and is also used for ringworm infections where oral treatment is considered appropriate (see p. Monitor liver function-discontinue if significant and persistent abnormalities in liver function tests develop. Use with caution in hepatic impairment (avoid if severe) or if receiving other hepatotoxic drugs. The choice of an alternative regimen depends on factors such as the response to previous treatment, tolerance and the possibility of crossresistance. The majority of virus infections resolve spontaneously in immunocompetent subjects. A number of specific treatments for viral infections are available, particularly for the immunocompromised. This section includes notes on herpes simplex and varicella-zoster, human immunodeficiency virus, cytomegalovirus, respiratory syncytial virus, viral hepatitis and influenza. However, combination antiretroviral therapy maximises the chance of preventing transmission and represents optimal therapy for the mother. Combination antiretroviral therapy may be associated with a greater risk of preterm delivery. Although antiretrovirals increase life expectancy considerably and decrease the risk of complications associated with premature ageing, mortality and morbidity remain slightly higher than in uninfected individuals. Although it should be started before the immune system is irreversibly damaged, the need for early drug treatment should be balanced against the risk of toxicity. Commitment to treatment and strict adherence over many years are required; the regimen chosen should take into account convenience and patient tolerance. The development of drug resistance is reduced by using a combination of drugs; such combinations should have synergistic or additive activity while ensuring that their toxicity is not additive. It is recommended that viral sensitivity to antiretroviral drugs is established before starting treatment or before switching drugs if the infection is not responding. The timing and choice of treatment should also take account of clinical symptoms, comorbidities, and the possible effect of antiretroviral drugs on factors such as the risk of cardiovascular events. Antiretrovirals for prophylaxis are chosen on the basis of efficacy and potential for toxicity. Other nucleoside reverse transcriptase inhibitors include abacavir, didanosine, emtricitabine, lamivudine, stavudine, and tenofovir. The protease inhibitors include atazanavir, darunavir, fosamprenavir (a pro-drug of amprenavir), indinavir, lopinavir, ritonavir, saquinavir, and tipranavir. Ritonavir in low doses boosts the activity of atazanavir, darunavir, fosamprenavir, indinavir, lopinavir, saquinavir, and tipranavir increasing the persistence of plasma concentrations of these drugs; at such a low dose, ritonavir has no intrinsic antiviral activity. Protease inhibitors are associated with lipodystrophy and metabolic effects (see below). Nevirapine is associated with a high incidence of rash (including Stevens-Johnson syndrome) and occasionally fatal hepatitis. Efavirenz has also been associated with an increased plasma-cholesterol concentration. Cobicistat is a pharmacokinetic enhancer that boosts the concentrations of other antiretrovirals, but it has no antiretroviral activity itself. Stavudine (especially in combination with didanosine), and to a lesser extent zidovudine, are associated with a higher risk of lipoatrophy and should be used only if alternative regimens are not suitable. Dyslipidaemia is associated with antiretroviral treatment, particularly with protease inhibitors. Protease inhibitors and some nucleoside reverse transcriptase inhibitors are associated with insulin resistance and hyperglycaemia. Of the protease inhibitors, atazanavir and darunavir may be less likely to cause dyslipidaemia, while saquinavir and atazanavir may be less likely to impair glucose tolerance. Nucleoside reverse transcriptase inhibitors Cautions Lactic acidosis Life-threatening lactic acidosis associated with hepatomegaly and hepatic steatosis has been reported with nucleoside reverse transcriptase inhibitors. They should be used with caution in patients (particularly obese women) with hepatomegaly, hepatitis (especially hepatitis C treated with interferon alfa and ribavirin), liver-enzyme abnormalities and with other risk factors for liver disease and hepatic steatosis (including alcohol abuse). Treatment with the nucleoside reverse transcriptase inhibitor should be discontinued in case of symptomatic hyperlactataemia, lactic acidosis, progressive hepatomegaly or rapid deterioration of liver function. Stavudine, especially with didanosine, is associated with a higher risk of lactic acidosis and should be used only if alternative regimens are not suitable.
Diseases
- Acromicric dysplasia
- Wrinkly skin syndrome
- Toriello syndrome
- Charcot Marie Tooth disease deafness mental retardation
- Sener syndrome
- Tsukuhara syndrome
- Cutis laxa osteoporosis
- Ectopia pupillae
- Cataract aberrant oral frenula growth retardation
- Femur fibula ulna syndrome

Cheap dapsone 100mg fast delivery
Other reported side-effects include headache acne xia generic 100 mg dapsone visa, dizziness, fatigue, malaise, taste disturbance, paraesthesia, bronchospasm, fever, serositis, vasculitis, myalgia, arthralgia, positive antinuclear antibody, raised erythrocyte sedimentation rate, eosinophilia, leucocytosis, and photosensitivity. Use of these combination products should be reserved for patients whose blood pressure has not responded adequately to a single antihypertensive drug and who have been stabilised on the individual components of the combination in the same proportions. Short-term treatment within 24 hours of onset of myocardial infarction in clinically stable patients, initially 6. Prophylaxis of symptomatic heart failure after myocardial infarction in clinically stable patients with asymptomatic left ventricular dysfunction, initially 6. Hypertension, 1initially 1 mg once daily (reduced to 500 micrograms daily if used in addition to diuretic (see notes above), or in cardiac decompensation, in severe hypertension, in volume depletion, in the elderly, or in renal impairment), then adjusted according to response; usual maintenance dose 2. Hypertension, used alone, initially 5 mg once daily; if used in addition to diuretic (see notes above), or in renal impairment, lower initial doses may be required; usual maintenance dose 20 mg once daily; max. Initially 5 mg daily before food; if used in addition to diuretic (see notes above), in elderly, in patients with heart failure, angina or cerebrovascular disease, or in renal or hepatic impairment, initially 2. Hypertension, initially 10 mg once daily; if used in addition to diuretic (see notes above) or in cardiac decompensation or in volume depletion, initially 2. Hypertension, initially 4 mg once daily in the morning for 1 month, subsequently adjusted according to response; if used in addition to diuretic (see notes above), in elderly, in renal impairment, in cardiac decompensation, or in volume depletion, initially 2 mg once daily; max. Heart failure (adjunct), initially 2 mg once daily in the morning under close medical supervision (see notes above), increased after at least 2 weeks to max. Hypertension, initially 5 mg once daily in the morning for 1 month, subsequently adjusted according to response; if used in addition to diuretic (see notes above), in elderly, in renal impairment, in cardiac decompensation, or in volume depletion, initially 2. Prophylaxis after myocardial infarction (started at least 48 hours after infarction), initially 2. Label: 22 Perindopril arginine with diuretic Note For hypertension not adequately controlled by perindopril alone. Hypertension, initially 10 mg once daily; with a diuretic (see notes above), in elderly, or in renal impairment initially 2. Monitoring of plasma-potassium concentration is advised, particularly in the elderly and in patients with renal impairment; lower initial doses may be appropriate in these patients. They may adversely affect fetal and neonatal blood pressure control and renal function; skull defects and oligohydramnios have also been reported. They are not recommended in breast-feeding and alternative treatment options, with better established safety information during breast-feeding, are available. Symptomatic hypotension including dizziness may occur, particularly in patients with intravascular volume depletion. Prophylaxis after myocardial infarction (starting as early as 3 days after infarction), initially 500 micrograms once daily, gradually increased to max. Hypertension, initially 8 mg (intravascular volume depletion 4 mg) once daily, increased if necessary at intervals of 4 weeks to max. Hypertension, usually 40 mg once daily (but 20 mg may be sufficient), increased if necessary after at least 4 weeks, to max. Hypertension, usually 80 mg once daily (initially 40 mg once daily in intravascular volume depletion); if necessary increased at intervals of 4 weeks up to max. Heart failure, initially 40 mg twice daily increased at intervals of at least 2 weeks up to max. Aliskiren is licensed for the treatment of hypertension, either alone or in 128 2. For details on the management of stable angina and acute coronary syndromes, see section 2. Although they are potent coronary vasodilators, their principal benefit follows from a reduction in venous return which reduces left ventricular work. Unwanted effects such as flushing, headache, and postural hypotension may limit therapy, especially when angina is severe or when patients are unusually sensitive to the effects of nitrates. Sublingual glyceryl trinitrate is one of the most effective drugs for providing rapid symptomatic relief of angina, but its effect lasts only for 20 to 30 minutes; the 300-microgram tablet is often appropriate when glyceryl trinitrate is first used. The aerosol spray provides an alternative method of rapid relief of symptoms for those who find difficulty in dissolving sublingual preparations. Duration of action may be prolonged by transdermal preparations (but tolerance may develop, see below). Isosorbide dinitrate is active sublingually and is a more stable preparation for those who only require nitrates infrequently. It is also effective by mouth for prophylaxis; although the effect is slower in onset, it may persist for several hours. Duration of action of up to 12 hours is claimed for modified-release preparations. The activity of isosorbide dinitrate may depend on the production of active metabolites, the most important of which is isosorbide mononitrate. Isosorbide mononitrate itself is also licensed for angina prophylaxis; modified-release formulations (for once daily administration) are available. Glyceryl trinitrate or isosorbide dinitrate may be tried by intravenous injection when the sublingual form is ineffective in patients with chest pain due to myocardial infarction or severe ischaemia. Intravenous injections are also useful in the treatment of congestive heart failure. Label: 21 2 Cardiovascular system Tolerance Many patients on long-acting or transdermal nitrates rapidly develop tolerance (with reduced therapeutic effects). Reduction of blood-nitrate concentrations to low levels for 4 to 12 hours each day usually maintains effectiveness in such patients. Conventional formulations of isosorbide mononitrate should not usually be given more than twice daily unless small doses are used; modifiedrelease formulations of isosorbide mononitrate should only be given once daily, and used in this way do not produce tolerance. Vasodilators can act in heart failure by arteriolar dilatation which reduces both peripheral vascular resistance and left ventricular pressure during systole resulting in improved cardiac output. By transdermal application, see under preparations Nitronal (Merck Serono) A Injection, glyceryl trinitrate 1 mg/mL. Label: 25 Dose prophylaxis of angina, 1 tablet in the morning (half a tablet if headache occurs), increased to 2 tablets in the morning if required 2.

Buy dapsone 100mg mastercard
Thus skin care products reviews by dermatologists cheap dapsone 100mg line, the identification of the differences in the cell division machineries of different bacteria will provide new and more explicit targets. It is apparent that targeting any of the key proteins of cell division may offer a good solution to arrest bacterial proliferation. The machinery is so huge that it provides many points of intervention, which can be exploited through more rigorous and focused research. With active research in the quest for the inhibitors of bacterial cell partitioning, it is possible that these inhibitors may emerge as effective tools to curb bacterial infections in the future. Bacterial mitosis: partitioning protein ParA oscillates in spiral-shaped structures and positions plasmids at mid-cell. Isolation of inactive 8-oxotetrahydrothalifendine, canadine, beta-hydrastine, and two newquinic acid esters, hycandinic acid esters-1 and -2. Auto-activation mechanism of the Mycobacterium tuberculosis PknB receptor Ser/Thr kinase. Traditionally, the cytoplasmic membrane was not considered a viable antibacterial target because of the potential for membrane-active agents to also disrupt the mammalian membrane, producing cytotoxic effects [2, 3]. Although this perception is quite valid, the clinical development of the membraneactive antibiotic daptomycin [4], and more recently telavancin [5], coupled with our increased understanding of the mode of action of antimicrobial defense peptides [6], has advanced the membrane as a natural and druggable target for antibiotics that can be selective for bacteria. A number of academic and industrial antibiotic discovery and development programs have therefore emerged, focusing on optimizing the antibacterial action of antimicrobial peptides, their nonpeptide mimetics or organic molecules that target the cytoplasmic membrane [1, 7, 8]. Arising from these discovery programs are numerous reports demonstrating that membrane-active antibiotics display exceptional chemotherapeutic properties including rapid bactericidal action, activities against multidrug-resistant pathogens and low prospects for the emergence of resistance [1, 12]. Besides these attributes, an added advantage displayed by several membrane-active antibiotics is their ability to eradicate bacteria residing in physiologically dormant states. This is an admirable property, considering that dormant bacteria are often refractory to killing by established classes of bactericidal antibiotics and the type of agents required to kill dormant bacteria was relatively unknown. Consequently, the finding that several membrane-active antibiotics kill persistent bacteria is an evolving paradigm for treating infections that persist. In this article, we examine this evolving Antibiotics: Targets, Mechanisms and Resistance, First Edition. We also discuss some of the obvious limitations for the discovery and clinical development of such agents. Initially, we briefly describe why dormant bacteria are hard to eradicate, which illustrates why targeting the membrane is a novel and expanding paradigm for treating persistent infections. A comprehensive review of the membrane and associated bioenergetics as drug targets has also been described elsewhere [1]. Clinical examples where antibiotic treatment failure coincides with the occurrence of dormant bacteria, include staphylococcal biofilms found in endocarditis and medical-device-related infections, cystic fibrosis caused by Pseudomonas aeruginosa [23, 24], recurrent streptococcal otitis media and sore throat [17, 25], ischemic osteomyelitis [26], nonhealing chronic wounds [27], and tuberculous granuloma caused by latent Mycobacterium tuberculosis [18]. Unfortunately, for biofilm-mediated infections, antimicrobial treatment failure is common and requires the surgical removal of the infected devices or wound tissues colonized by biofilms [27, 30, 31]. The need for prolonged periods of treatment also increases the risk of patient noncompliance and the selection of genetic mechanisms of resistance [22]. During the development of an infection, bacteria first enter into a period of rapid growth, but this declines as the infection progresses because of nutrient limitations and the response of the immune system. The effect this has on antibiotic efficacy was appropriately described by Eagle in 1952 [32], showing that even high concentrations of penicillin failed to eradicate streptococci in the older stages of infection in mice. The poor efficacy of penicillin was attributed to bacteria occurring in a nonmultiplying state with low metabolic activity. Growth resumes when favorable conditions reoccur, resulting in actively growing cells that are more susceptible to killing by antibiotics [16]. In addition, in an infection, various subtypes of dormant bacteria are likely to coexist. Therefore, the antibiotic susceptibilities of cells within the dormant population are also likely to vary [1, 22], which implies that no single agent may effectively kill all subpopulations of dormant cells. These conditions slow and eventually stop the growth of bacteria, resulting in dormant cells [16, 36]. This has much to do with the manner in which most agents were discovered as molecules that inhibit macromolecular biosynthesis and corrupt processes essential to logarithmically growing bacteria. The drawback of this approach is that dormant cells undergo a genetically regulated downshift in active cellular metabolism, causing a substantial decrease in the activity of several biosynthetic processes, including those that are targeted by many established antibiotics [9, 16, 22, 37, 38]. It is therefore presumed that the targets for most antimicrobial agents are either absent, or only occur in limited amounts, and, even if present, that the corruption of processes required for rapid growth are not deleterious to the survival of metabolically inactive bacteria [1, 15]. For example, -lactam antibiotics kill by activating peptidoglycan hydrolases and this requires active peptidoglycan synthesis in growing cells. Also, tobramycin and ciprofloxacin preferentially kill metabolically active cells within the peripheral regions of P. PhoU, a protein that acts as a global repressor of cellular metabolism, is a leading example of the potential of this approach. Therefore, as an antidormancy target, the inhibition of PhoU may hinder the metabolic shift down for cells to become dormant [45]. This complicates 186 8 the Membrane as a Novel Target Site for Antibiotics to Kill Persisting Bacterial Pathogens target selection for drug discovery processes. For example, the ribosome-associated proteins RelA and SpoT, which are responsible for the production of the global regulator (p)ppGpp, enable cells to respond to nutrient starvation as part of the stringent response [50]. Thus, both RelA and SpoT would need to be inhibited in some bacteria to abolish the role of the stringent response and cause cells to be more susceptible to antibiotics. Interestingly, ofloxacin failed to sterilize the biofilm of SpoT/RelA mutants [51], suggesting that additional mechanisms are also responsible for recalcitrance. A further complication is that dormant cell types may be present in an infection before the administration of therapy [9, 22] and strategies targeting their formation may be ineffective. Indeed, once bacteria attain a persistence state, they may diminish the role of enzymes needed for the initial transition stages. This view is exemplified by the signal transduction DosR/S system that regulates more than 50 genes and is central to M. Accordingly, DosR initially emerged as an attractive antitubercular target [52], but findings of Rustad et al. Another way forward to obtain agents that kill dormant bacteria would be to derail the cellular processes or targets that are essential to bacterial viability in both growing and nongrowing physiological states, as we articulate here for the membrane. It is already evident from numerous research studies that the membrane is essential, selective killing of bacterial pathogens is achievable, and membrane-active agents typically exhibit a multitarget mode of action that results in potent bactericidal properties and low prospects for resistance emergence. From membrane damage numerous cellular functions are affected, including macromolecular synthesis. Other molecules affect the permeability of the membrane bilayer and cause pores to form, from which cytoplasmic contents are leaked from the cell and cells may rapidly die. This binding may be part of the killing mechanism and also could engender specificity for prokaryotes if they lack mammalian counterparts. It should be noted that not all agents would exhibit these actions or even similar actions as this depends on drug structure and interactions made within the membrane. However, the development of membrane-active molecules has been hindered because of reasonable concern over the potential for cross-reactivity with the mammalian cytoplasmic membrane [3]. Nevertheless, the recent successful medical use of the membrane-active antibiotics daptomycin (a cyclic lipopeptide) and lipoglycopeptides (telavancin, oritavancin, and dalbavancin) against gram-positive infections indicate that bacterial specificity is therapeutically achievable. The selectivity of these agents is due to their preferential interaction with the negatively charged phospholipids. In contrast, mammalian membranes are characterized by an abundance of cholesterol (25%) and the presence of zwitterionic phospholipids; negatively charged phospholipids are rare in the outer leaflets of mammalian cells [64]. These differences allow daptomycin to selectively act on bacteria, where it first oligomerizes in the presence of calcium ions (Ca2+) to form micelle-like amphipathic structures that are pseudopositively charged, with the hydrophobic decanoyl side chain facing inwards [65]. The selectivity of oritavancin also appears to be mediated by the positively charged molecule interacting with bacterial phosphatidylglycerol and cardiolipin, as shown by studies with model membranes [66, 67].
Purchase dapsone 100 mg otc
Reduction of nephrotoxicity associated with cisplatin in patients with advanced solid tumours of non-germcell origin skin care equipment discount dapsone online amex, consult product literature. Secondly, prolonged use of these drugs, particularly when combined with extensive irradiation, is associated with a marked increase in the incidence of acute non-lymphocytic leukaemia. Cyclophosphamide is used mainly in combination with other agents for treating a wide range of malignancies, including some leukaemias, lymphomas, and solid tumours. It is given by mouth or intravenously; it is inactive until metabolised by the liver. Ifosfamide is related to cyclophosphamide and is given intravenously; mesna (section 8. Chlorambucil is used either alone or in combination therapy for some lymphomas and chronic leukaemias. However, patients occasionally develop severe widespread rashes which can progress to Stevens-Johnson syndrome or to toxic epidermal necrolysis. If a rash occurs further chlorambucil is contra-indicated and cyclophosphamide is substituted. Melphalan is licensed for the treatment of multiple myeloma, polycythaemia vera, childhood neuroblastoma, advanced ovarian adenocarcinoma, and advanced Urothelial toxicity Haemorrhagic cystitis is a common manifestation of urothelial toxicity which occurs with the oxazaphosphorines, cyclophosphamide and ifosfamide; it is caused by the metabolite acrolein. Mesna reacts specifically with this metabolite in the urinary tract, preventing toxicity. Mesna is used routinely (preferably by mouth) in patients receiving ifosfamide, and in patients receiving cyclophosphamide by the intravenous route at a high dose. However, in practice, melphalan is rarely used for ovarian adenocarcinoma; it is no longer used for advanced breast cancer. Melphalan is also licensed for regional arterial perfusion in localised malignant melanoma of the extremities and localised soft-tissue sarcoma of the extremities. Interstitial pneumonitis and life-threatening pulmonary fibrosis are rarely associated with melphalan. Busulfan given by mouth or intravenously, followed by cyclophosphamide, is also licensed as conditioning treatment before haematopoietic stem-cell transplantation in adults and children. Frequent blood tests are necessary because excessive myelosuppression may result in irreversible bone-marrow aplasia. Bone-marrow toxicity is delayed, and the drug is therefore given at intervals of 4 to 6 weeks. Treosulfan is given by mouth or by intravenous or intraperitoneal administration and is used to treat ovarian cancer. Skin pigmentation is a common sideeffect and allergic alveolitis, pulmonary fibrosis and haemorrhagic cystitis occur rarely. Thiotepa is licensed in combination with other chemotherapy as conditioning treatment in adults and children with haematological disease or solid tumours before haematopoietic stem cell transplantation. Mitobronitol is occasionally used to treat chronic myeloid leukaemia; it is available on a named-patient basis from specialist importing companies, see p. Cumulative renal damage and delayed pulmonary fibrosis may occur with intravenous use. Carmustine implants are licensed for intralesional use in adults for the treatment of recurrent glioblastoma multiforme as an adjunct to surgery. Carmustine implants are also licensed for high-grade malignant glioma as adjunctive treatment to surgery and radiotherapy. It is given by mouth and has both an antimitotic effect (Busulphan) Indications see notes above Cautions see section 8. Chronic myeloid leukaemia, induction of remission, by mouth, 60 micrograms/kg daily (max. Hyperpigmentation of skin, nails, and oral mucosa, and red coloration of the urine, may occur. Idarubicin has general properties similar to those of doxorubicin; it is mostly used in the treatment of haematological malignancies. Diarrhoea, abdominal pain, haemorrhage, cardiac disorders, rash, and red pigmentation of the urine are commonly reported. Many cytotoxic antibiotics act as radiomimetics and simultaneous use of radiotherapy should be avoided because it may markedly increased toxicity. Daunorubicin, doxorubicin, epirubicin and idarubicin are anthracycline antibiotics. It is given by injection into a fast-running infusion, commonly at 21-day intervals. Doxorubicin is largely excreted in the bile and an elevated bilirubin concentration is an indication for reducing the dose. Diarrhoea, dehydration, and red coloration of the urine can commonly occur, and renal damage has been reported. Supraventricular tachycardia related to drug administration is an uncommon complication. Higher cumulative doses are associated with cardiomyopathy and it is usual to limit total cumulative doses to 450 mg/m2 because symptomatic and potentially fatal heart failure is common above this dose. Patients should be assessed before treatment by echocardiography; the elderly, and those with cardiac disease, hypertension, or who have received myocardial irradiation, should be treated cautiously. Caution is necessary with concomitant use of cardiotoxic drugs, or drugs that reduce cardiac contractility. Some evidence suggests that weekly low-dose administration may be less cardiotoxic. Doxorubicin is also given by bladder instillation for the treatment of transitional cell carcinoma, papillary bladder tumours and carcinoma in-situ. They may reduce the incidence of cardiotoxicity and lower the potential for local necrosis, but infusion reactions, sometimes severe, may occur. Hand-foot syndrome (painful, macular reddening skin eruptions) occurs commonly with liposomal doxorubicin and may be dose limiting. Mitoxantrone is structurally related to doxorubicin; it is used for metastatic breast cancer. It is given intravenously and is well tolerated, but myelosuppression and dose-related cardiotoxicity occur; cardiac examinations are recommended after a cumulative dose of 160 mg/m2. Pixantrone is licensed as monotherapy for the treatment of refractory or multiply relapsed aggressive nonHodgkin B-cell lymphomas, although the benefits of using it as a fifth-line or greater chemotherapy in refractory patients has not been established. Baseline investigations should include a full blood count, assessment of cardiac function measured by left ventricular ejection fraction, and measurement of serum concentrations of total bilirubin and total creatinine. Severe myelosuppression is a common side-effect, and cardiotoxicity may occur during or following treatment; full blood count and cardiac function should be monitored throughout treatment. Patients with cardiac risk factors should have the risks and benefits of treatment carefully assessed. Photosensitivity is a theoretical risk and patients should be advised to follow sun protection strategies.
Meadowsweet. Dapsone.
- Dosing considerations for Meadowsweet.
- What is Meadowsweet?
- Are there any interactions with medications?
- How does Meadowsweet work?
- Bronchitis, heartburn, upset stomach, ulcers, gout, joint problems, bladder infections, and other conditions.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96150
Buy generic dapsone 100 mg
Methotrexate inhibits the enzyme dihydrofolate reductase acne 5 purchase 100mg dapsone, essential for the synthesis of purines and pyrimidines. Methotrexate is used as maintenance therapy for childhood acute lymphoblastic leukaemia. It is contra-indicated in significant renal impairment because it is excreted primarily by the kidney. It should also be avoided in the presence of significant pleural effusion or ascites because it can accumulate in these fluids, and its subsequent return to the circulation may cause myelosuppression. Systemic toxicity may follow intrathecal administration and blood counts should be carefully monitored. It is licensed as monotherapy or combination therapy for adjuvant treatment of advanced colon cancer following surgery, for monotherapy or combination therapy of metastatic colorectal cancer, and for first-line treatment of advanced gastric cancer in combination with a platinum-based regimen. Capecitabine is also licensed for second-line treatment of locally advanced or metastatic breast cancer either in combination with docetaxel (where previous therapy included an anthracycline) or alone (after failure of a taxane and anthracycline regimen or where further anthracycline treatment is not indicated). It is also given for chronic lymphocytic leukaemia in patients who have failed to respond to standard regimens containing an alkylating agent. Cladribine produces severe myelosuppression, with neutropenia, anaemia, and thrombocytopenia; haemolytic anaemia has also been reported. High doses of cladribine have been associated with acute renal failure and severe neurotoxicity. Patients treated with cladribine or fludarabine are more prone to serious bacterial, opportunistic fungal, and viral infections, and prophylactic therapy is recommended in those at risk. To prevent potentially fatal transfusion-related graft-versus-host reaction, only irradiated blood products should be administered. Prescribers should consult specialist literature when using highly immunosuppressive drugs. Clofarabine is licensed for the treatment of acute lymphoblastic leukaemia in patients aged 1 to 21 years who have relapsed or are refractory after receiving at least two previous regimens. Nelarabine is licensed for the treatment of T-cell acute lymphoblastic leukaemia and T-cell lymphoblastic lymphoma in patients who have relapsed or who are refractory after receiving at least two previous regimens. Neurotoxicity is common with nelarabine and close monitoring for neurological adverse events is strongly recommended-discontinue if neurotoxicity occurs. Gemcitabine is used intravenously; it is given alone for elderly patients or for palliative treatment, or with cisplatin as first-line treatment for locally advanced or metastatic non-small cell lung cancer. Combined with cisplatin, gemcitabine is also licensed for the treatment of advanced bladder cancer. Combined with carboplatin, gemcitabine is licensed for the treatment of locally advanced or metastatic epithelial ovarian cancer which has relapsed after a recurrencefree interval of at least 6 months following previous platinum-based therapy. Its predominant use is in the induction of remission of acute myeloblastic leukaemia. A liposomal formulation of cytarabine for intrathecal use is licensed for lymphomatous meningitis. Fludarabine is well tolerated but it does cause myelosuppression, which may be cumulative. Immunosuppression is also common (see panel on cladribine and fludarabine below), and co-trimoxazole is used to prevent pneumocystis infection. Immune-mediated haemolytic anaemia, thrombocytopenia, and neutropenia are less common side-effects. Haemolytic uraemic syndrome has been reported rarely and gemcitabine should be discontinued if signs of microangiopathic haemolytic anaemia occur. The Scottish Medicines Consortium has advised (November 2006) that gemcitabine is accepted for restricted use for the treatment of metastatic breast cancer, which has relapsed following previous chemotherapy including an anthracycline (unless contra-indicated). Gemcitabine is not recommended for patients who can have potentially curative surgery. There is insufficient evidence about its use for second-line treatment of pancreatic adenocarcinoma. It may also be used topically for certain malignant and pre-malignant skin lesions. Toxicity is unusual, but may include myelosuppression, mucositis, and rarely a cerebellar syndrome. It is also licensed as monotherapy for maintenance treatment in locally advanced or metastatic non-small cell lung cancer other than predominantly squamous cell histology that has not progressed immediately following platinum-based chemotherapy. Raltitrexed is generally well tolerated, but can cause marked myelosuppression and gastro-intestinal side-effects. Reduce dose by 50% on the next treatment cycle if serum-bicarbonate concentration less than 20 mmol/ litre Pregnancy avoid (toxicity in animal studies); manufacturer advises effective contraception during and for 3 months after treatment in men or women; see also Pregnancy and Reproductive Function, p. Azathioprine, which is metabolised to mercaptopurine, is generally used as an immunosuppressant (section 8. The dose of both drugs should be reduced if the patient is receiving allopurinol since it interferes with their metabolism. Tegafur in combination with gimeracil and oteracil is given by mouth; gimeracil inhibits the degradation of fluorouracil and oteracil decreases the activity of fluorouracil in normal gastrointestinal mucosa. Tegafur in combination with gimeracil and oteracil is licensed for the treatment of advanced gastric cancer when used in combination with cisplatin. Tioguanine is given by mouth for the treatment of acute leukaemias and chronic myeloid leukaemia. Tioguanine has a lower incidence of gastrointestinal side-effects than mercaptopurine. Long-term therapy is no longer recommended because of the high risk of liver toxicity; treatment with tioguanine should be discontinued if liver toxicity develops. It is used in the treatment of intermediate-2 and high-risk myelodysplastic syndromes, chronic myelomonocytic leukaemia, and acute myeloid leukaemia, in adults who are not eligible for haemotopoietic stem cell transplantation. By mouth, leukaemia in children (maintenance), 15 mg/m2 weekly in combination with other drugs 8. By intravenous injection or infusion, or by intra-arterial infusion, or by intramuscular injection, or intrathecal administration, consult product literature Methotrexate (Non-proprietary) A Injection, methotrexate (as sodium salt) 2. Patients with neurotoxicity commonly have peripheral paraesthesia, loss of deep tendon reflexes, abdominal pain, and constipation; ototoxicity has been reported. Motor weakness can also occur, and increasing motor weakness calls for dose reduction or discontinuation of these drugs. Myelosuppression is a dose-limiting side-effect of vinblastine, vindesine, vinorelbine, and vinflunine; vincristine causes negligible myelosuppression. The vinca alkaloids cause severe local irritation and care must be taken to avoid extravasation. Severe bronchospasm has been reported following administration of the vinca alkaloids (more commonly when used in combination with mitomycin-C). Important Vinblastine, vincristine, vindesine, vinflunine, and vinorelbine injections are for intravenous administration only. Inadvertent intrathecal administration can cause severe neurotoxicity, which is usually fatal. The National Patient Safety Agency has advised (August 2008) that adult and teenage patients treated in an adult or adolescent unit should receive their vinca alkaloid dose in a 50 mL minibag. Teenagers and children treated in a child unit may receive their vinca alkaloid dose in a syringe. Etoposide may be given orally or by slow intravenous infusion, the oral dose being double the intravenous dose. A preparation containing etoposide phosphate can be given by intravenous injection or infusion.
Buy dapsone 100mg low price
If a patient with suspected bacterial meningitis without non-blanching rash cannot be transferred to hospital urgently acne 4 year old cheap 100mg dapsone otc, benzylpenicillin (see p. In hospital, consider adjunctive treatment with dexamethasone (particularly if pneumococcal meningitis suspected in adults; section 6. Suggested duration of treatment at least 10 days 5 Infections Meningitis caused by meningococci Benzylpenicillin or cefotaxime1 Suggested duration of treatment 7 days. To eliminate nasopharyngeal carriage in patients treated with benzylpenicillin or cefotaxime see Table 2, section 5. If micro-organism highly penicillin- and cephalosporin-resistant, add vancomycin and if necessary rifampicin. Suggested duration of antibacterial treatment 14 days Meningitis caused by Haemophilus influenzae Cefotaxime1 Consider adjunctive treatment with dexamethasone (section 6. Azithromycin or doxycycline Alternative, erythromycin Suggested duration of treatment azithromycin as a single dose or doxycycline for 7 days Suggested duration of treatment 14 days Gonorrhoea: uncomplicated Contact tracing recommended. Choice of alternative antibacterial regimen depends on locality where infection acquired. Azithromycin + i/m ceftriaxone Suggested duration of treatment single-dose of each antibacterial Alternative when parenteral administration not possible, cefixime + azithromycin Suggested duration of treatment single-dose of each antibacterial Suggested duration of treatment single-dose of each antibacterial Suggested duration of treatment single-dose of each antibacterial Alternative if micro-organism sensitive to a quinolone, ciprofloxacin + azithromycin Pharyngeal infection, azithromycin + i/m ceftriaxone 1. Doxycycline + metronidazole + i/m ceftriaxone or ofloxacin + metronidazole Suggested duration of treatment 14 days (use i/m ceftriaxone as a single dose). Benzathine benzylpenicillin [unlicensed] Suggested duration of treatment single-dose (repeat dose after 7 days for women in the third trimester of pregnancy) Alternatives, doxycycline or erythromycin Suggested duration of treatment 14 days Late latent syphilis (asymptomatic infection of more than 2 years) Contact tracing recommended. Benzathine benzylpenicillin [unlicensed] Suggested duration of treatment once weekly for 2 weeks Alternative, doxycycline Suggested duration of treatment 28 days 5 Infections Asymptomatic contacts of patients with infectious syphilis Doxycycline Suggested duration of treatment 14 days Blood Septicaemia: community-acquired A broad-spectrum antipseudomonal penicillin. If anaerobic infection suspected, add metronidazole to broad-spectrum cephalosporin. If other resistant micro-organisms suspected, use a more broad-spectrum beta-lactam antibacterial. If anaerobic infection suspected, add metronidazole to broad-spectrum cephalosporin Septicaemia related to vascular catheter Vancomycin1 If Gram-negative sepsis suspected, especially in the immunocompromised, add a broad-spectrum antipseudomonal beta-lactam. Consider removing vascular catheter, particularly if infection caused by Staphylococcus aureus, pseudomonas, or Candida species Meningococcal septicaemia If meningococcal disease suspected, a single dose of benzylpenicillin (see p. Benzylpenicillin or cefotaxime2 To eliminate nasopharyngeal carriage in patients treated with benzylpenicillin or cefotaxime see Table 2, section 5. Suggested duration of treatment 6 weeks for acute infection If penicillin-allergic, clindamycin Consider adding fusidic acid or rifampicin for initial 2 weeks. Suggested duration of treatment 6 weeks for acute infection If meticillin-resistant Staphylococcus aureus suspected, vancomycin1 Consider adding fusidic acid or rifampicin for initial 2 weeks. Suggested duration of treatment 6 weeks for acute infection Septic arthritis Seek specialist advice if prostheses present. Metronidazole Suggested duration of treatment 3 days or until symptoms resolve Alternative, amoxicillin Suggested duration of treatment 3 days or until symptoms resolve Gingivitis: acute necrotising ulcerative Antibacterial required only if systemic features of infection. Metronidazole Suggested duration of treatment 3 days or until symptoms resolve Alternative, amoxicillin Suggested duration of treatment 3 days or until symptoms resolve Periapical or periodontal abscess Antibacterial required only in severe disease with cellulitis or if systemic features of infection. Amoxicillin Suggested duration of treatment 5 days Alternative, metronidazole Suggested duration of treatment 5 days 1. Metronidazole Alternative, doxycycline Throat infections Most throat infections are caused by viruses and many do not require antibacterial therapy. Consider antibacterial, if history of valvular heart disease, if marked systemic upset, if peritonsillar cellulitis or abscess, or if at increased risk from acute infection. Phenoxymethylpenicillin In severe infection, initial parenteral therapy with benzylpenicillin, then oral therapy with phenoxymethylpenicillin or amoxicillin1. Suggested duration of treatment 10 days If penicillin-allergic, clarithromycin2 Suggested duration of treatment 10 days 5 Infections Sinusitis Antibacterial should usually be used only for persistent symptoms and purulent discharge lasting at least 7 days or if severe symptoms. Amoxicillin1 or doxycycline or clarithromycin2 Suggested duration of treatment 7 days. In severe infection, initial parenteral therapy with co-amoxiclav or cefuroxime may be required Otitis externa Consider systemic antibacterial if spreading cellulitis or patient systemically unwell. Flucloxacillin If penicillin-allergic, clarithromycin2 If pseudomonas suspected, ciprofloxacin (or an aminoglycoside) Otitis media Many infections caused by viruses. In children without systemic features, antibacterial treatment may be started after 72 hours if no improvement. Consider earlier treatment if deterioration, if systemically unwell, if at high risk of serious complications. Suggested duration of treatment 5 days (longer if severely ill) If penicillin-allergic, clarithromycin2 Suggested duration of treatment 5 days (longer if severely ill) 1. Topical fusidic acid Suggested duration of treatment 7 days is usually adequate (max. Suggested duration of treatment 7 days If penicillin-allergic, oral clarithromycin1 Suggested duration of treatment 7 days Erysipelas Phenoxymethylpenicillin or benzylpenicillin If severe infection, replace phenoxymethylpenicillin or benzylpenicillin with high-dose flucloxacillin; if meticillin-resistant S. Suggested duration of treatment at least 7 days If penicillin-allergic, clindamycin or clarithromycin1 If meticillin-resistant S. Suggested duration of treatment at least 7 days Cellulitis Flucloxacillin (high-dose) If streptococcal infection confirmed, replace flucloxacillin with phenoxymethylpenicillin or benzylpenicillin. If Gram-negative bacteria or anaerobes suspected, use broad-spectrum antibacterials. For tetanus-prone wound, give human tetanus immunoglobulin (with a tetanuscontaining vaccine if necessary, according to immunisation history and risk of infection), see under Tetanus Vaccines, section 14. Also, give antibacterial prophylaxis to the index case if they are in contact with vulnerable household contacts or if they are under 10 years of age. Vulnerable individuals include the immunocompromised, those with asplenia, or children under 10 years of age. If there are 2 or more cases of invasive Haemophilus influenzae type b disease within 120 days in a pre-school or primary school, antibacterial prophylaxis should also be given to all room contacts (including staff). For details of those who should receive chemoprophylaxis contact a consultant in communicable disease control (or a consultant in infectious diseases or the local Health Protection Agency Laboratory) 2. For details of those who should receive chemoprophylaxis contact a consultant in communicable disease control (or a consultant in infectious diseases or the local Health Protection Agency laboratory). For details of those who should receive chemoprophylaxis contact the lead clinician for local tuberculosis services (or a consultant in communicable disease control). For tetanus-prone wound, give human tetanus immunoglobulin (with a tetanus-containing vaccine if necessary, according to immunisation history and risk of infection), see under Tetanus vaccines, section 14. For biliary complications following liver transplantation, add i/v amoxicillin or i/v teicoplanin3 Percutaneous endoscopic gastrostomy or jejunostomy1 Single dose of i/v co-amoxiclav or i/v cefuroxime Use single dose of i/v teicoplanin3 if history of allergy to penicillins or cephalosporins, or if high risk of meticillinresistant Staphylococcus aureus Prevention of infection in orthopaedic surgery Joint replacement including hip and knee1 Single dose2 of i/v cefuroxime alone or i/v flucloxacillin + i/v gentamicin Prevention of early-onset neonatal infection i/v benzylpenicillin (or i/v clindamycin if history of allergy to penicillins) Give intrapartum prophylaxis to women with group B streptococcal colonisation, bacteriuria, or infection in the current pregnancy, or to women who had a previous baby with an invasive group B streptococcal infection. Consider prophylaxis for women in preterm labour if there is prelabour rupture of membranes or if intrapartum rupture of membranes lasting more than 18 hours is suspected. If history of allergy to penicillins or to cephalosporins or if high risk of meticillin-resistant Staphylococcus aureus, use single dose2 of i/v teicoplanin3 + i/v gentamicin Closed fractures1 Single dose2 of i/v cefuroxime or i/v flucloxacillin If history of allergy to penicillins or to cephalosporins or if high risk of meticillin-resistant Staphylococcus aureus, use single dose2 of i/v teicoplanin3 Open fractures i/v co-amoxiclav alone or i/v cefuroxime + i/v metronidazole (or i/v clindamycin alone if history of allergy to penicillins or to cephalosporins) Add i/v teicoplanin3 if high risk of meticillin-resistant Staphylococcus aureus. Start prophylaxis within 3 hours of injury and continue until soft tissue closure (max. At first debridement also use a single dose of i/v cefuroxime + i/v metronidazole + i/v gentamicin or i/v co-amoxiclav + i/v gentamicin (or i/v clindamycin + i/v gentamicin if history of allergy to penicillins or to cephalosporins). At time of skeletal stabilisation and definitive soft tissue closure1 use a single dose of i/v gentamicin + i/v teicoplanin3 5 Infections Prevention of infection in gastro-intestinal procedures Operations on stomach or oesophagus1 Single dose2 of i/v gentamicin or i/v cefuroxime or i/v co-amoxiclav Add i/v teicoplanin3 if high risk of meticillin-resistant Staphylococcus aureus High lower-limb amputation1 i/v co-amoxiclav alone or i/v cefuroxime + i/v metronidazole4 Continue antibacterial prophylaxis for at least 2 doses after procedure (max. If history of allergy to penicillin or to cephalosporins, or if high risk of meticillin-resistant Staphylococcus aureus, use i/v teicoplanin3 + i/v gentamicin + i/v metronidazole4 Open biliary surgery1 Single dose2 of i/v cefuroxime + i/v metronidazole4 or i/v gentamicin + i/v metronidazole4 or i/v co-amoxiclav alone Add i/v teicoplanin3 if high risk of meticillin-resistant Staphylococcus aureus Resections of colon and rectum for carcinoma, and resections in inflammatory bowel disease, and appendicectomy1 Single dose2 of i/v gentamicin + i/v metronidazole4 or i/v cefuroxime + i/v metronidazole4 or i/v co-amoxiclav alone Add i/v teicoplanin3 if high risk of meticillin-resistant Staphylococcus aureus 1. Intravenous antibacterial prophylaxis should be given up to 30 minutes before the procedure 2.

Order dapsone in india
Escherichia coli is the most common cause of urinarytract infection; Staphylococcus saprophyticus is also common in sexually active young women skin care educator jobs purchase dapsone with paypal. Pseudomonas aeruginosa infections usually occur in the hospital setting and may be associated with functional or anatomical abnormalities of the renal tract. Staphylococcus epidermidis and Enterococcus faecalis infection may complicate catheterisation or instrumentation. A specimen of urine should be collected for culture and sensitivity testing before starting antibacterial therapy;. Pregnancy Urinary-tract infection in pregnancy may be asymptomatic and requires prompt treatment to prevent progression to acute pyelonephritis. Penicillins and cephalosporins are suitable for treating urinarytract infection during pregnancy. Sulfonamides and quinolones should be avoided during pregnancy; trimethoprim should also preferably be avoided particularly in the first trimester. Renal impairment In renal failure antibacterials normally excreted by the kidney accumulate with resultant toxicity unless the dose is reduced. This applies especially to the aminoglycosides which should be used with great caution; tetracyclines, methenamine, and nitrofurantoin should be avoided altogether. Children Urinary-tract infections in children require prompt antibacterial treatment to minimise the risk of renal scarring. Amoxicillin should only be used if the organism causing the infection is sensitive to it. If the patient is severely ill, then the infection is best treated initially by injection of a broad-spectrum antibacterial such as cefotaxime or coamoxiclav; gentamicin is an alternative. Children under 3 months of age should be transferred to hospital and treated initially with intravenous antibacterial drugs such as ampicillin with gentamicin, or cefotaxime alone, until the infection responds; full doses of oral antibacterials are then given for a further period. Antibacterial prophylaxis with low doses of trimethoprim or nitrofurantoin may be considered for children with recurrent infection, significant urinarytract anomalies, or significant kidney damage. The antibacterial chosen should reflect current local bacterial sensitivity to antibacterials. Uncomplicated lower urinary-tract infections often respond to trimethoprim, nitrofurantoin, or amoxicillin given for 7 days (3 days may be adequate for infections in women; see also Table 1, section 5. Widespread bacterial resistance to ampicillin, amoxicillin, and trimethoprim has been reported. Alternatives for resistant organisms include co-amoxiclav (amoxicillin with clavulanic acid), an oral cephalosporin, nitrofurantoin, pivmecillinam, or a quinolone. Fosfomycin [unlicensed] can be used, on the advice of a microbiologist, for the treatment of uncomplicated lower urinary-tract infections caused by multiple-antibacterial resistant organisms when other antibacterials cannot be used; in adults, it is given as a single oral dose of 3 g. Long-term low dose therapy may be required in selected patients to prevent recurrence of infection; indications include frequent relapses and significant kidney damage. Trimethoprim, nitrofurantoin and cefalexin have been recommended for long-term therapy. Methenamine (hexamine) should not generally be used because it requires an acidic urine for its antimicrobial activity and it is ineffective for upper urinary-tract infections; it may, however, have a role in the prophylaxis and treatment of chronic or recurrent uncomplicated lower urinary-tract infections. Acute pyelonephritis can lead to septicaemia and is treated initially by injection of a broad-spectrum antibacterial such as cefuroxime or a quinolone if the patient is severely ill; gentamicin can also be used. Prostatitis can be difficult to cure and requires treatment for several weeks with an antibacterial which penetrates prostatic tissue such as trimethoprim, or some quinolones. Severe chronic recurrent infection, 100 mg every 6 hours with food for 7 days (dose reduced or discontinued if severe nausea). Aspergillosis Aspergillosis most commonly affects the respiratory tract but in severely immunocompromised patients, invasive forms can affect the heart, brain, and skin. Itraconazole is also used for the treatment of chronic pulmonary aspergillosis or as an adjunct in the treatment of allergic bronchopulmonary aspergillosis [unlicensed indication]. Label: 9, 14, 21, 25 Dose uncomplicated urinary-tract infection, 1 capsule twice daily with food Genito-urinary surgical prophylaxis, 1 capsule twice daily on day of procedure and for 3 days after Candidiasis Many superficial candidal infections including infections of the skin (section 13. Topical therapy may not be adequate in immunocompromised patients and an oral triazole antifungal is preferred. Following successful treatment, fluconazole can be used for prophylaxis against relapse until immunity recovers. Following successful treatment, itraconazole can be used for prophylaxis against relapse until immunity recovers. Mild localised fungal infections of the skin (including tinea corporis, tinea cruris, and tinea pedis) respond to topical therapy (section 13. Systemic therapy is appropriate if topical therapy fails, if many areas are affected, or if the site of infection is difficult to treat such as in infections of the nails (onychomycosis) and of the scalp (tinea capitis). Oral imidazole or triazole antifungals (particularly itraconazole) and terbinafine are used more frequently than griseofulvin because they have a broader spectrum of activity and require a shorter duration of treatment. Tinea capitis is treated systemically; additional topical application of an antifungal (section 13. If treatment is necessary, a systemic antifungal is more effective than topical therapy. For the role of topical antifungals in the treatment of onychomycosis, see section 13. It also achieves good penetration into the cerebrospinal fluid to treat fungal meningitis. Fluconazole is excreted largely unchanged in the urine and can be used to treat candiduria. Itraconazole capsules require an acid environment in the stomach for optimal absorption. Itraconazole has been associated with liver damage and should be avoided or used with caution in patients with liver disease; fluconazole is less frequently associated with hepatotoxicity. Posaconazole is licensed for the treatment of invasive fungal infections unresponsive to conventional treatment. Voriconazole is a broad-spectrum antifungal drug which is licensed for use in life-threatening infections. Immune reconstitution syndrome Improvement in immune function as a result of antiretroviral treatment may provoke a marked inflammatory reaction against residual opportunistic organisms; these reactions may occur within the first few weeks or months of initiating treatment. Lipodystrophy syndrome Metabolic effects associated with antiretroviral treatment include fat redistribution, insulin resistance, and dyslipidaemia; collectively these have been termed lipodystrophy syndrome. The usual risk factors for cardiovascular disease should be taken into account before starting antiretroviral therapy and patients should be advised about lifestyle changes to reduce their cardiovascular risk. For cautions, contra-indications and side-effects see under individual drugs Trizivir (ViiV) A patients at high risk of cardiovascular disease (especially if 10-year cardiovascular risk greater than 20%); interactions: Appendix 1 (abacavir) Hypersensitivity reactions Life-threatening hypersensitivity reactions reported-characterised by fever or rash and possibly nausea, vomiting, diarrhoea, abdominal pain, dyspnoea, cough, lethargy, malaise, headache, and myalgia; less frequently mouth ulceration, oedema, hypotension, sore throat, acute respiratory distress syndrome, anaphylaxis, paraesthesia, arthralgia, conjunctivitis, lymphadenopathy, lymphocytopenia and renal failure; rarely myolysis; laboratory abnormalities may include raised liver function tests (see Lactic Acidosis p. Whenever possible avoid concomitant treatment with other drugs known to cause pancreatic toxicity. Label: 23, counselling, administration, see below Excipients include aspartame equivalent to phenylalanine 36. Patients temporarily unable to take zidovudine by mouth, by intravenous infusion over 1 hour, 0.
Order 100 mg dapsone overnight delivery
Thus acne meds 100mg dapsone amex, simple kill-the-bug screens in both types of standard libraries will require powerful secondary and counterscreens. Compounds chemically or biologically different from this shorter list of comparators could then be characterized. Phenotypic screens were designed to discover new classes of compounds with known phenotypes or phenotypes projected from observation of conditional mutants of essential genes. An example of the former is the spheroplasting screen for cell-wall-active agents, based on the behavior of penicillin-treated gramnegatives in hypertonic medium [53, 61]. With the advent of tools for relatively easy genetic manipulation and engineering, bacterial strains could be manipulated to give enhanced readouts for interference with a specific intracellular function, gene product, or promoter. These screens can be efficiently run in agar diffusion assays, where a test compound produces a gradient due to diffusion from a well or filter placed on agar inoculated with a test organism. This is useful because in assays such as the reporter-type screen noted earlier, high concentrations will kill or inhibit growth and thus reporter expression can be detected only at subinhibitory concentrations. In a liquid assay, usually run at a single concentration, the critical subinhibitory concentration inducing the reporter, but not killing the cell, might be missed. With a bank of stress regulon screens, each strain will be a control for the others. With a reporter-based single target or pathway, a control strain should be constructed in which the chosen reporter is under the regulation of a different promoter, which should not be affected by the desired inhibitor. It is best to set up such phenotypic screens in a way as to give a positive readout. In order to be robust, a screen must be well controlled and shown to have a very low rate of false positives. For specific novel antibacterial inhibitors of enzymes or pathways, the expected hit rate is very low. Were it not, empirical screening and follow up of most libraries would likely have found them already. Thus, if a screen has a 1% hit rate in a chemical library, it is highly likely that it is finding junk. Two methods should be highlighted: whole-cell antisense screens for specific targets and pathways and synergy screens for compounds that, at subinhibitory levels, enhance the activity of known antibacterials. Where antibacterial inhibitors of specific gene products were known, antisense downregulation of those genes led to specific sensitization to the inhibitors [69]. Thus, it was recognized that such antisense strains or strains with similarly downregulatable targets could be used for screening by comparing the sensitivity of a strain with a downregulated target to that of an isogenic wild type [69, 71]. The concept that downregulation of one step in a pathway (such as GyrB) can lead to sensitization of other steps in the pathway (such as DnaE) was evident in the construction of the antisense array that can be used to identify antibacterial mechanism of action [59]. Run in this way, synergy screens are hypersensitive in that they will perforce select for inhibitors which, in the absence of the -lactam, would not show antibacterial activity on their own at the tested concentration. Before the advent of bacterial genome sequencing, target selection was often made on the basis of microbial genetic demonstration of essentiality of the function, usually through the use of conditional mutants. As noted earlier, phenotypic screens were often based on the behavior of the mutants when grown under nonpermissive conditions. While phenotypic screens have the benefit of finding compounds that can enter cells, they require follow up to determine the actual target of any inhibitor. It must not be assumed that any antibacterial activity of an enzyme inhibitor is due solely to the inhibition of that enzyme; this must be proved. Several of the large pharmaceutical companies, including Roche and SmithKline Beecham, did extensive genomic panning for novel targets. Perhaps it was this accident of timing that turned antibacterial discovery into a search for new targets. The reasoning was that the standard antibacterials in use, the ones to which resistance was rising, had very few molecular targets and, therefore, inhibitors directed toward new genomics-revealed targets 38 2 Antibacterial Discovery: Problems and Possibilities should not be cross-resistant with the older agents. Of course, much of the preexisting resistance to these older agents was not target directed but, instead, directed toward the inhibitors themselves. However, it was indeed to be expected that new chemical classes directed at new targets would not exhibit cross-resistance. This reasoning, however, neglected the probability that, as discussed earlier, targeting of single enzymes is very likely to select for preexisting mutations in the target organism. Instead of taking significant time for resistance from exogenous sources to arise, resistance might be expected to occur overnight, during therapy. Yet genomics-/bioinformatics-based targeted discovery appears to have made up the bulk of antibacterial discovery efforts in the genomic era. The reasons for this lack of output are complex, usually not disclosed and are likely due to a number of factors. That is, even when inhibitors were found, they either had no antibacterial activity or that activity was not related to enzyme inhibition. In my experience, this appears to be a common finding in antibacterial discovery, but there are, of course, exceptions. The Ro5 denotes physicochemical parameters that should favor oral bioavailability. Additional analysis of the differences between antibacterials and other human health drugs have been recently published [2, 47, 49, 50]. Of these, 95% were Triton-reversible aggregators, leaving 70 detergent-insensitive hits (0. But these consisted of -lactams, nonreproducible activities, detergent-resistant aggregators, and promiscuous or other covalent inhibitors. Thus, false positives appeared to overwhelm any true, and especially, weak actives. Any targeted screening hit must be tested for selectivity, to reduce potential for human toxicity, and for specificity, to demonstrate that the antibacterial activity is due solely to the inhibition of the in vitro-inhibited 40 2 Antibacterial Discovery: Problems and Possibilities target. Phenotypic whole-cell assays that are designed to reflect the intracellular mechanism of inhibitors can be used for secondary testing of in vitro screening hits that exhibit antibacterial activity. As most of the present day screening seems to involve high-throughput robotic liquid handling systems, assays that have few steps after initial mixing, single-concentration dosing (generally in duplicate), are favored. They do not seem to involve validating tests for robustness by inclusion of many negative controls. One might ask whether setting up assay systems that accommodate millions of samples is worth it if the samples are mostly junk. Given that standard chemical libraries have been problematic for antibacterial screening, how can the best use be made of them In the study on screening for inhibitors of -lactamase referenced earlier [83], the authors, who had found no progressable hits in their biochemical screen had, in parallel, performed docking calculations on the same library. But in silico screening and fragment-based design (and screening) may be a way out of the bad-library conundrum. Those compounds have been selected for some reason, for some advantage, whether for weapons production or for signaling. But for screening of extracts and even whole broths, the goal is to find ways of selecting for compounds not detected by the old screening methods. Although there is no hard numeric evidence for it, in my experience, it seems that the best and most selective antibacterial antibiotics are produced by Actinomycetes and other bacteria.

Cheap dapsone 100mg otc
The immature airways are more collapsible than adults and such collapse is often localized to anatomic sites (laryngomalacia skin care with ross order 100 mg dapsone, tracheomalacia and bronchomalacia). Pediatric bronchoscopes are arbitrarily defined as those scopes with outside diameter of less than 5. Adult scopes because of their larger diameter (6 mm or greater) are not indicated in children aged 10 years or younger. Later, models of pediatric bronchoscope have had essentially the same physical characteristics (diameter 3. Contraindications There is no absolute contraindication to flexible fiberoptic bronchoscopy in pediatric age group. Indications Indications for flexible bronchoscopy in neonatal infants and pediatric age group includes the following:11-16 Diagnostic 1. Assessment of position, patency or airway damage related to endotracheal or tracheostomy tube. Complications the incidence of serious complication in pediatric bronchoscopy is small. Procedure the procedure should be described to the child and parents using positive reassuring words, to alleviate anxiety of both the child and parents. In almost all children an intravenous access should be established to administer sedatives (midazolam 66 Atlas of Fiberoptic Bronchoscopy 0. Occasionally a child may fail to respond to the above and may be induced with a small dose of ultrashort acting barbiturate. Children are further prepared for flexible bronchoscopy by ensuring that their stomach is empty. Older children are kept fasting for atleast 4 hours, while younger children are allowed to have clear liquids untill 2 hours. Longer fasting period of 4 to 6 hours is required (if general anesthesia is to be used). In children younger than 4 years, it is advisable to pass a suction catheter through, the nose into the stomach before beginning the bronchoscopy. If further topical anesthesia is necessary in the lower airways, 1 percent lignocaine is used. Ventilation may be maintained, either using a venturi technique or by the use of a ventilating side arm on the bronchoscope. List of calculated medications doses based on the weight of the patients should be available. Two suction setups should be simultaneously maintained, one for use through bronchoscope and one for control and care of oral secretions. Careful monitoring is necessary to ensure that the child continues, to ventilate and oxygenate well. Infants, as small as 540 g have been found to ventilate satisfactorily around this instrument. In virtually, every other aspect flexible bronchoscopies in children are conducted in the same way as in adults. One other use is when entry via nasal route is desired and partial obstruction and narrowing of anatomy prevents safe passage of the large bronchoscope. Spelunking on the pediatric airways: explorations with the flexible fiberoptic bronchoscope. Value of bronchoalveolar lavage in the management of severe acute pneumonia and interstitial pneumonitis in the immunocompromised child. Use of Pediatric Bronchoscopes in Adults Because their length is same as that of adult bronchoscopes (550 mm), the smallest pediatric instruments allow entry into additional, 3 to 5 distal bronchial generations with good visualization. They may be also used for the evaluation, of cryptogenic hemoptysis and chronic cough in which the airway examination is negative, with an adult bronchoscope, repeating the examination with a pediatric bronchoscope may increase the diagnostic yield. The development of lasers with different wavelengths and in particular of neodymium-doped crystal lasers, has permitted transmission of the beam through fiberoptic systems. It also has a strong thermal characteristic that can be used to coagulate blood vessels and other viable tissues, when placed at a distance from the target. The use of laser in tracheobronchial tree requires careful consideration of the anatomic location and configuration of the lesion. If the lesion is in close proximity Advances in Fiberoptic Bronchoscopy to the esophagus or pulmonary artery, endobronchial laser therapy poses risk of fistula formation. The main complications of endoscopic laser resection are cardiac arrhythmias, hypoxia, hemorrhage, airway perforation, transient pneumothorax, mediastinal emphysema, cardiac arrest, myocardial infarction, embolism and fire. Electrocautery is an alternative treatment technique for immediate debulking of intraluminal tumor and has a curative potential in patients with radiologically occult cancer. Electrocautery can be applied either using a rigid or a flexible applicator specially designed for this purpose. The choice of technique and instruments, whether rigid or flexible, under general or local anesthesia, depends upon the expertise of the bronchoscopist and the risk assessment. The degree of tissue destruction depends upon the power used, duration of contact, the surface area of contact, the density and moisture of tissue. Complications of electrocautery for endobronchial lesions can be hemorrhage, respiratory failure, pneumonia, fire/explosion and fibrosis. The estimated incidence of clinically significant bleeding in patients treated with electrocautery is 2. The advantages are that the results are immediate, when using electrocautery in combination with mechanical tumor removal, simple, cost-effective for both benign and lowgrade malignant lesions. This may be attractive for the treatment of superficial spreading tumors, for quick hemostasis, for recurrent respiratory papillomatosis and for obstructive bronchogenic carcinomas. Cryotherapy may be superior to lasers for distal lesions, because of lower risk of airway perforation. But, cryotherapy cannot be used to achieve rapid relief of symptomatic airway obstruction and it is not effective in paucicellular lesions that are relatively impervious to freezing, such as fibrotic stenosis, cartilaginous or bony lesions or lipomas. The two cryogens available to the pulmonologist are liquid nitrogen and nitrous oxide. Nitrous oxide is the commonest cooling agent used in tracheobronchial cryotherapy. Cryotherapy is associated with greater difficulties in control and depth of penetration. The only method of monitoring freezing using an endoscope is the bioelectric method. The most common serious complication is hemorrhage, others include edematous reaction, trauma. This technique ensures the delivery of a maximal therapeutic dose of radiation, to the tumor with a minimal effect on normal surrounding tissues. This can be done either by directly introducing the source into the tumor, via the natural route (endoluminal brachytherapy) or by placing the source into the tumor bed during tumor resection. Relief of airway obstruction is the primary goal of endobronchial brachytherapy, although curative treatment may be attempted in conjunction with external beam radiation in selected patients. Complications include hemoptysis, which may be fatal postradiation bronchitis and stenosis of airways. This freezing effect is maintained for about 20, the area is rewarmed, resulting in thawing. The indications for cryotherapy are similar to endobronchial laser or electrocautery. The advantages with cryotherapy is safety not only for the operator, but also for the patient and its cost-effectiveness. Serious complications of brachytherapy include massive hemoptysis and fistula formation. Because of the risk of fatal hemorrhage, every effort should be made to rule out involvement of central vessels before treatment is administered. The mechanism of action involves the activation of a photosensitive molecule with the subsequent creation of a variety of active forms of oxygen, causing peroxidative reactions leading to cell damage and cell death. Indications include, relief of neoplastic endobronchial obstruction, delay of the tumor progression and improvement of symptoms making inoperable patients operable in selected cases. Based on the foundation material several types of stents are available, which include polymer, metallic, covered metallic, hybrid stents. More recently, however, stents made of silicone or special alloys, such as nitinol (a nickel-titanium alloy with shape and size memory capacity that allow self-expansion on deployment), have had good results.