Generic female viagra 100mg on line
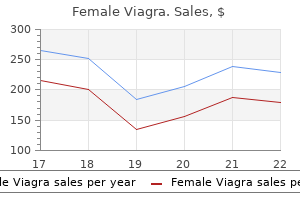
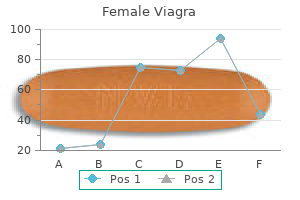
Special multivitamin formulations contain high amounts of fat-soluble vitamins designed to deliver the appropriate doses required menstrual knee pain buy female viagra with a mastercard. Even with these precautions, adequate vitamin D levels may be difficult to maintain due to altered absorption, reduced fat mass, and minimal exposure to sun light. Hypertonic saline (HyperSal): It hydrates the airway mucus secretions and facilitates mucociliary function. Bronchodilator therapy is recommended for patients 6 years or older who demonstrate bronchiole hyperresponsiveness or a bronchodilator response. Chronic use of bronchodilator therapy is recommended to improve lung function by enhancing mucociliary action. Based on the "low-volume model" theory, the use of hypertonic saline would restore airway hydration and enhance mucociliary function. In this study, 24 patients were randomly assigned to receive a daily treatment of 7% hypertonic saline with or without pretreatment of a control. The study also demonstrated that these patients were able to sustain mucus clearance for more than 8 hours. Other studies assessing the use of hypertonic saline have supported this study, showing an improvement in lung function and a 56% reduction in exacerbations. In an attempt to ameliorate these symptoms, providers may use a lower concentration of 3% hypertonic saline. Three randomized controlled trials and a crossover trial involving 520 patients were conducted. It is unclear at this point if the anti-inflammatory effects of macrolides are a combination of antimicrobial and/or immunomodulatory mechanisms of action. A study conducted in Japan first demonstrated the benefit of macrolides against Pseudomonas aeruginosa. Four randomized controlled trials have since demonstrated this effect with azithromycin (250-500 mg) given three times weekly, which has led to increased nutritional status and decreased pulmonary infections. Other treatments are under investigation, but larger studies are needed before they become recommended therapies. Unfortunately, this limits antimicrobial selection, and can contribute to deterioration of pulmonary function (Table 29-5). Early in life, patients will routinely be colonized with Staphylococcus aureus and then later with P. Ultimately, this study showed no significant improvement in health outcomes, therefore, prophylaxis for S. Antibiotics available include extended-spectrum penicillins, select cephalosporins, select carbapenems, aztreonam, quinolones, colistimethate, and aminoglycosides. The only two mechanisms of action represented in this group are cell wall destruction and inhibited cell wall synthesis by ribosomal attachment. Standard practice is to combine these two mechanisms for the best bactericidal results. It is not unusual for patients to have multiple organisms growing in their sputum. The clinician can review the quantitative sputum culture for both the organisms present and the amount or colony forming units grown. By targeting the organisms with the most numerous organisms present and reviewing the susceptibility panels, the clinician can choose the most appropriate regimen. At this point, sputum cultures can be sent to specialized laboratories that will test combinations of antibiotics and report out any synergy results. Aerosolized antibiotics are directly deposited into the lung, providing concentrations that may overcome the standard measures of resistance. A risk factor for acquiring this organism may be broadspectrum antibiotic use (carbapenems and cephalosporins). Caseating granulomas have been found in some patients with clinical disease while other patients with 29 Cystic Fibrosis Anti-inflammatory Therapies Pulmonary inflammation begins early in life, as shown by the predominance of proinflammatory mediators that can be seen on bronchiolar lavage. Anti-inflammatory therapies must address the neutrophil response and inhaled therapies will target the endobronchial location, which is the site of inflammation. High-dose ibuprofen (20-30 mg/kg of body weight twice daily) has proven efficacious in a study where patients showed less decline in pulmonary function when compared with patients given placebo. Patients on high dose ibuprofen were able to maintain weight and had less hospital admissions. The low number of patients using this proven therapy may be related to the requirement to obtain a specific therapeutic level of ibuprofen, which in turn requires frequent blood draws for pharmacokinetic monitoring. Although Aspergillus does not directly inhibit lung function, it may cause allergic bronchopulmonary aspergillosis which is an immunologic-mediated response to the presence of Aspergillus in the lungs. Decline in pulmonary function can be directly related to the number of annual viral infections. Aerosolized antibiotics deliver drug locally to the lung while decreasing the risk of systemic side effects. Routine monitoring of serum aminoglycoside levels is unnecessary in patients with normal renal function using approved doses. This inhaled formulation of aztreonam has demonstrated improvement in respiratory symptoms and lung function in patients older than 6 years. With a larger volume of distribution, patients may require larger antibiotic doses. Critically ill patients may vary from their baseline function and require closer monitoring. Patches may not reliably adhere to the skin as a result of increased sweat on the surface of the skin. At the beginning, both current medications and medications that might be used to treat exacerbations need to be considered. Several of these medications are classified as category C and may pose a potential harm to the fetus. In a woman with severe lung disease, these changes can cause right-sided heart failure. Other pharmacotherapy issues that are seen in this population are altered pharmacokinetics and increased maintenance of nutritional and pulmonary health. In stable outpatients, fasting glucose levels of more than or equal to 126 mg/dL (7. Exercise is encouraged because it can improve peripheral insulin sensitivity and have beneficial effects in overall health, pulmonary function, and well-being. The use of acarbose is also discouraged due to its mechanism of action, which reduces postprandial glucose and insulin excursion by limiting intestinal absorption of glucose. This inhibits the energy absorption in malnourished individuals while causing diarrhea, anorexia, and abdominal discomfort. Sulfonylureas are being considered due to Pediatrics Education of the parents is emphasized in this population, concerning administration of pancreatic enzymes and infant formula. Parents are also counseled to encourage their child to adhere with pulmonary health and nutritional health practices. Transplant Patients Lung transplantation has become an option with a 5-year survival rate of approximately 50%. Kalydeco (ivacaftor) was approved on January 31, 2012, for patients 6 years or older with the G551D mutation. As a result, mucus is thinned by fluid movement into the airways making airway clearance easier for the patient. In a randomized, double-blind, placebo-controlled trial evaluating ivacaftor in patients 12 years or older, ivacaftor met effectiveness endpoints. Researchers saw significant improvements in lung function, risk of pulmonary exacerbations, respiratory symptoms, and weight and sweat chloride concentrations. It is possible that fluctuating estradiol levels are associated with increased pulmonary exacerbations. However, studies in this area are limited and need to be substantiated as hormone therapy is not without risk. Employment is difficult to maintain because some employers may penalize for frequent hospitalizations. The use of new technology now allows support groups via video conferencing and online discussion.
Order female viagra 50mg online
Most of these studies were conducted in prehospital and emergency department settings using 250 mL of 7 women's health clinic brisbane northside order 100mg female viagra. For example, a double-blind, randomized controlled trial involving 229 patients with hypotension and severe brain injury demonstrated no significant differences in neurologic function at 6 months when 250 mL of 7. In order to address ongoing questions of efficacy, the National Heart, Lung, and Blood Institute evaluated hypertonic sodium chloride solutions with or without a colloid (ie, 7. The latter patients, as well as patients undergoing blood loss associated with surgery, frequently need blood components such as packed red blood cells. Additionally, there are immunomodulatory concerns with red blood cell administration. Although there is no optimal hematocrit value for all patients, a minimum hematocrit of 30% (0. Use of a more liberal transfusion strategy has been curtailed in many institutions with the publication of a randomized, multicenter trial involving critically ill patients that found 30-day mortality to be similar whether patients were transfused at a hemoglobin concentration less than 7 or 10 g/dL (70-100 g/L; 4. Although the investigators were cautious about extrapolating the results of this investigation to patients with myocardial ischemia, a subsequent study performed in patients undergoing cardiac surgery found similar results. Citrate that is added to stored blood to prevent coagulation may bind to calcium, resulting in hypocalcemia, although potassium and phosphate concentrations often are elevated in stored blood, particularly when hemolysis has occurred during storage. In patients receiving large amounts of blood, prophylactic calcium administration may be warranted until levels are available. Other issues that must be considered with blood product administration include monitoring for transfusion-related reactions and attention to appropriate warming, particularly when large volumes are given to pediatric patients, because hypothermia is associated with increased fluid requirements and mortality. These more severe forms of blood loss are a function of not only the type of injury but also factors such as medications (eg, aspirin, Coumadin, clopidogrel, enoxaparin, newer oral anticoagulants) and disease states that impair normal coagulation. Concerns with its use in trauma patients are issues related to appropriate dose, timing, and diminished effectiveness in patients with acidosis and severe hypothermia. Evidence of efficacy in a general trauma population that would offset these concerns is lacking. In addition to the use of more restrictive transfusion thresholds, as mentioned previously, these strategies have included hemoglobin-based oxygen carriers and perfluorocarbon compounds to deliver oxygen to tissues. Other strategies have aimed at reducing blood loss through the use of improved procedural and surgical techniques, as well as the administration of hemostatic medications. The only hemostatic medication with a proven mortality benefit is the antifibrinolytic agent, tranexamic acid. A more in-depth review of the results of this trial suggests that the beneficial effects are most likely to occur if tranexamic acid is given within the first 3 hours of injury. While additional data are still needed in specific subpopulations such as patients with traumatic brain injuries, this study is relatively unique in that an intervention apart from surgery and blood product administration was demonstrated to reduce mortality. Guidelines recommend approximately 2 to 4 mL/kg of isotonic fluid (lactated Ringer solution) for each percent burn can be used for calculating the expected fluid requirements for the first 24 hours after the burn. Regardless of the calculated deficit, fluids should be administered until adequate tissue perfusion has been documented (eg, maintenance of urine output of 0. Crystalloids are preferred as initial therapy for burn victims because there is no substantial evidence that colloids mobilize edematous fluid, and there is a theoretical concern that extravascular fluid accumulation might be prolonged by the oncotic actions of albumin and other colloid products that have leaked through vessel walls. Additionally, there is no evidence that colloids reduce mortality in patients with thermal injuries and there is a concern that hydroxyethyl starch and dextran products might even increase mortality through deleterious effects on coagulation and renal function. Some novel therapies for thermal resuscitation have been studied, although larger confirmatory trials are needed prior to use apart from research protocols. Personalized Pharmacotherapy At this time there is little genetic/genomic information that is available to guide personalized pharmacotherapy in patients with hypovolemic shock. Further, as stressed throughout this chapter, fluids are by far the first choice of therapy in conjunction with other definitive interventions such as surgery for traumatic injuries. Nevertheless, there are individual factors that may influence the specific fluid being administered. For example, the lower chloride concentration in lactated Ringer would usually make it preferred over normal saline in patients with a hyperchloremic metabolic acidosis, while the increased osmolarity of normal saline would usually make it preferred over lactated Ringer in a patient with increased intracranial pressure. Some clinicians believe that hypertonic sodium-containing solutions should be the intervention of choice to lower intracranial pressure in patients with head injuries. The appropriate use of invasive hemodynamic monitoring tools, such as right-sided heart catheterization in patients with hypovolemic shock, is controversial. These follow-up investigations suggest it may have been the protocols of care and not the invasive catheter that was responsible for the mortality benefit noted in the original landmark study. Also of note is that patients in all of these studies had severe sepsis and septic shock, so the results might not be applicable to other forms of shock with different pathophysiologic considerations. For example, in hemorrhagic shock due to trauma, the most important intervention is surgical control of bleeding, and anything that delays this control is likely to increase, not decrease, mortality. The most appropriate, cost-effective, and practical parameter(s) for monitoring adequacy of fluid resuscitation in shock is unresolved. Among other things, a complete blood count will enable assessment of possible infection (white blood cell count), oxygen-carrying capacity of the blood (hemoglobin, hematocrit), and ongoing bleeding (hemoglobin, hematocrit, and platelet count). An increasing lactate concentration (arterial, mixed venous, or central venous), an increasing arterial base deficit, or a decreasing bicarbonate concentration are global markers indicative of inadequate perfusion leading to anaerobic metabolism with accumulation of lactic acid. Although the value of these surrogate markers for improving patient outcomes is more controversial, they are considered traditional end points of resuscitation in certain populations such as trauma patients. For example, when blood flow to the liver is interrupted because of sustained hypotension, a condition known as shock liver may occur. In this condition, the levels of transaminases on a liver panel may be markedly elevated in the first couple of days after marked hypotension, although the concentrations should decrease over time. Along with laboratory testing, a more extensive history can be obtained during the subacute monitoring period. The value of pulmonary artery catheters (also known as rightsided heart or Swan-Ganz catheters) has been debated hotly since their introduction. Such catheters are placed to obtain various oxygen-transport variables, some of which cannot be determined reliably from peripheral or other central vessels. The debate was intensified when early studies suggested improved outcomes when cardiac output and other oxygen-transport variables were raised to supranormal levels, the monitoring of which required placement of a pulmonary artery catheter. The controversy led to consensus conferences and workshops, the development of organizational guidelines, and the publication of a meta-analysis (which found a statistically significant reduction in morbidity using pulmonary artery catheters to guide therapy). There were no episodes of pulmonary embolism in the catheter group and eight episodes in the control group (P = 0. This trial is important not only because of the implications for high-risk surgical patients but also because it allows for the conduct of future trials in other patient populations without some of the ethical issues raised about such trials in the past. Part of the concern regarding pulmonary artery catheterization relates to interpretation of its results by inexperienced practitioners. Studies in Europe and the United States found that one of two physicians incorrectly interpreted a tracing from a pulmonary artery catheter. Complications related to pulmonary artery catheter insertion, maintenance, and removal include damage to vessels and organs during insertion, arrhythmias, infections, and thromboembolic damage. To avoid the complications associated with pulmonary artery catheterization, other less invasive tools were developed to obtain similar information. For example, cardiac output determinations have been made by Doppler, bioimpedance, dye, and ionic dilution techniques, although such measurements would not provide other data that are obtained routinely with pulmonary artery catheters (eg, left-sided heart filling pressure). Additionally, advances in pulmonary artery catheter technology that expand the information obtained from such monitoring (eg, mixed venous oxyhemoglobin) are under investigation. Commonly measured and calculated hemodynamic and oxygen-transport indices associated with invasive monitoring are primarily global indicators of tissue perfusion. Attempts have been made to find regional and local indicators of hypoperfusion so that circulatory insufficiency could be treated before overt shock occurs. Although the literature is fairly consistent concerning low gastric intramucosal pH (pHi) values being predictive of death, pHi-guided therapy to decrease mortality has not been demonstrated. Despite these concerns, measures of regional tissue oxygenation continue to be investigated through a variety of novel monitoring techniques. In addition to regional monitoring of tissue perfusion, local methods of monitoring are being studied.
50mg female viagra amex
Therefore women's health center at uic purchase female viagra 100mg on line, antithrombotic therapy with antiplatelet and anticoagulant therapy are necessary to produce a successful outcome. Antiplatelet therapy is also used after the procedure to reduce the risk of stent thrombosis. In patients at high risk of bleeding, a minimum of 2 weeks can be given, as most reendothelialization of the stent surface should have occurred. At the end of the trial, and at the 1 year follow-up, this difference was not significant. Additionally, utilization of arterial grafts was limited to one trial in which only 14% of the patients received one vessel. These trials are also limited by the narrow spectrum of patients selected for enrollment. These trials primarily enrolled patients less than or equal to 65 years of age (>90%), very few women (<5%), and low to moderate risk patients who were clinically stable. These patients included those at high risk of death without surgery (see Table 16-4). A number of relatively poorly conducted trials suggest less than 1 year may be adequate, while the highest quality trial suggest more than a year is optimal. Female and older patients have a higher risk of short-term mortality, but have a similar longterm prognosis compared to the general population. This is related to the progressive atherosclerotic disease in native vessels as well as graft disease over time. The use of arterial grafts has provided promise in reducing occlusion of the coronary artery bypass grafts. Limitations to the use of arterial grafts include vasospasm and long surgical times for harvest. One of the most feared and most common (~ 6%) complications is postoperative neurological impairment, which may be attributed to hypoxia, emboli, hemorrhage, or a metabolic abnormality during or shortly after the surgery. A type 1 deficit is associated with major, focal neurological deficits, stupor, or coma. The incidence of neurologic deficits is equal between the two types, while mortality may be as high as 21% and 10% respectively. While most patients recover without problems, the mortality rate in these patients is 19%, and increases to almost 65% in the 1. Despite the infrequent occurrence of mediastinitis (1%4%), the mortality rate can be as high as 25%. One of these approaches is the off-pump bypass coronary surgery that is performed on a beating heart. By reducing the need for cardiopulmonary bypass and preventing the need for clamping of the aorta, there is a significant reduction in adverse neurologic events, length of hospitalization, and cost. The cardiac motion is reduced by a number of pharmacological and mechanical devices. In addition to the benefits of avoiding cardiopulmonary bypass, the prevention of sternotomy reduces the incidence of wound infections as well as patient recovery time. Aspirin in doses between 100 mg a day to 325 mg three times daily have been shown to be effective in reducing vein graft closure during the first year after the surgery. It is recommended that the first dose of aspirin be given within the first 24 hours of surgery. The efficacy of aspirin is lost if initiation is delayed more than 48 hours postoperatively. Less than 10% of patients enrolled in these trials had an ejection fraction less than 50%. The goal of chronic therapy to provide complete or nearly complete elimination of angina episodes while having the patient take part in normal activities. Both agents are effective for increasing exercise duration and reducing the number of weekly angina episodes. Patients need to be sure to be adequately educated on appropriate use and storage, as well as being sure they have consistent access to the tablets or spray. This may require patients to have multiple vials or canisters that are in areas that they spend time (eg, home, work, car, and garage). The selection of one agent over the other is mainly based on patient preferences and tolerability. Long-acting nitrates do not provide 24-hour angina protection, but this may not be an issue for all patients. Ranolazine provides 24-hour protection, but is a more expensive agent compared to generic nitrates. Ranolazine has a more attractive side effect profile compared to long-acting nitrates, but the severity of these effects will be patient specific. This should be accomplished while the patient is able to do the things in life that they want to do. It is not uncommon for patients to report reduced or no episodes of angina because they have given up on doing things that bring on angina. Once patients have been optimized on medical therapy, symptoms should improve over 2 to 4 weeks and remain stable until their disease progresses. Patients receiving revascularization still require assessment of symptoms of angina at least every 6 to 12 months since a return of angina is not uncommon. While ranolazine has proven to be an effective and well tolerated agent for the management of episodes of angina, it is much more expensive. All other agents used for control of symptoms of angina are available in generic formulations, with many be only $4 a months. Patients who are unable to achieve this goal are defined as having refractory angina. Patients with refractory angina are those who continue to have symptoms, despite maximally tolerated therapy. Due to contraindications or intolerance to higher doses of medications, patients may end up with refractory angina with a smaller medication list than others, and not on full doses of anti-angina agents. While -blockers are typically the agents of first choice in patients with fixed-threshold angina, they are not appropriate agents for patients with vasospasm. The mechanism of worsening angina is most likely due to unopposed 1-adrenergic receptor stimulation during -blockade. While long-acting nitrates can be used in the treatment of vasospasm, the high doses typically needed for adequate symptom control are not well tolerated. Nifedipine, verapamil, and diltiazem are all equally effective as single agents for the initial management of coronary vasospasm. Comparative trials are few in number and do not reveal significant differences among these three drugs for vasospasm. The pathogenesis of coronary heart disease and the acute coronary syndrome (second of two parts). Measurements of coronary blood flow and degree of stenosis: Current clinical implications and continues uncertainties. The coronary collateral circulation: genetic and environmental determinants in experimental models and humans. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: Advantages of a new specific activity scale. Importance of clinical measures of ischemia in the prognosis of patients with documented coronary artery disease. Diabetics with coronary disease have a prevalence of asymptomatic ischemia during exercise treadmill testing and ambulatory ischemia monitoring similar to that of nondiabetic patients. Anatomic versus physiologic assessment of coronary artery disease: Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. Diagnostic and prognostic implications of coronary flow capacity: A comprehensive cross-modality physiological concept in ischemic heart disease. B-type natriuretic peptide and long-term survival in patients with stable coronary artery disease. B-type natriuretic peptide and the risk of cardiovascular events and death in patients with stable angina: Results from the AtheroGene study. Prevalence and prognostic significance of preprocedural cardiac troponin elevation among patients with stable coronary artery disease undergoing percutaneous coronary intervention: Results from the Evaluation of Drug Eluting Stents and Ischemic Events Registry.
Purchase female viagra 100mg online
Drug therapy aims to prevent cell division or cause cell death in the tumour without damaging normal healthy cells women's health clinic yonge street buy female viagra 100mg free shipping. Cancer cells are similar to normal cells, so this is often impossible and explains many of the side effects of chemotherapy. Cytotoxic drugs affect normal dividing cells producing unwanted adverse effects on bone marrow and the cells produced there; reduced healing; loss of hair due to damage to hair producing cells in hair follicles; damage to the gastrointestinal lining; reduced growth in children; sterility; and damage to the foetus. Nausea and vomiting are common with most anti-cancer drugs and are caused by toxic effects on the chemotrigger zone of the central nervous system. A significant symptom is the production of large amounts of uric acid as a result of the breakdown of nucleic acids. High plasma levels of uric acid can precipitate gout, or interfere with treatment for pre-existing gout, or uric acid can deposit in the kidneys and cause kidney damage. Concurrent use of allopurinol can reduce the production of uric acid (see Chapter 7). It seems that this is likely to happen as a result of low-dose single drug chemotherapy. Drugs are therefore generally more effective in combination and may act synergistically. The drugs should be used at the maximum dose that can be tolerated and as frequently as possible to discourage tumour regrowth. An understanding of their pharmacology, drug interactions and pharmacokinetics is essential for safe and effective use, which should be under specialist guidance of an oncologist. The descriptions that follow are not intended to give a comprehensive account of all anti-cancer drugs available, rather to explain the modes of action and to give examples from each group. Toxic effects with all cytotoxic drugs are severe nausea and vomiting, hair loss and bone marrow depression. Although alkylating agents can act on cells at any stage of the cell cycle, they are most effective in the S phase of the cell cycle and are therefore most cytotoxic to rapidly dividing cells. Cyclophosphamide is metabolized to a toxic metabolite called acrolein, which can cause haemorrhagic cystitis, a rare but serious complication. This effect can be counteracted by a high intake of fluid and by using a drug called mesna. Some other examples are busulphan (for leukaemia), carmustine (for brain tumours), treosulphan (for ovarian cancer) and cisplatin (for lung, testicular, bladder, ovarian and cervical cancers). Trimethoprim is selective for bacterial cells because bacterial dihydrofolate reductase is many times more sensitive to trimethoprim than is the human enzyme. Resistance to methotrexate occurs possibly due to reduced uptake into cancer cells or altered enzyme activity. Adverse effects of methotrexate include ulceration of the mouth and lower gastrointestinal tract and bone marrow suppression. With high doses of methotrexate synthetic folinates are used to prevent irreversible bone marrow damage. It should be used with caution in combination with allopurinol because allopurinol inhibits xanthine oxidase. This is similar to the mode of action of the antifungal drug, flucytosine (Chapter 9, page 167). Adverse effects of cytarabine are bone marrow suppression and gastrointestinal disturbances. Apart from nausea and vomiting and bone marrow suppression, adverse effects with doxorubicin are cardiotoxicity and possibility of cardiac failure. Bleomycin is most effective in the G2 phase and during mitosis of the cell cycle, but it is also effective against cells in the G0 phase. Bleomycin is unusual among cytotoxic drugs in that it does not cause bone marrow suppression. However, it is associated with blistering skin rashes and serious progressive pulmonary fibrosis in 10% of patients. Microtubules form the spindle during mitosis, so vinca alkaloids halt mitosis at a certain stage. These drugs are used to treat leukaemia, lymphoma, testicular cancer and lung cancer. Thus migration of white blood cells and axonal transport in neurons are inhibited leading increased susceptibility to infection and neurotoxicity respectively. The mode of action of taxanes is to promote microtubule formation and inhibit their breakdown, so preventing completion of mitosis. The two taxanes currently in use are paclitaxel, which is used in the treatment of ovarian cancer and metastatic breast cancer and docetaxel, which is used to treat metastatic breast cancer, small cell lung cancer and prostate cancer. Adverse effects of paclitaxel and docetaxel are similar, being hypersensitivity reactions, bone marrow suppression, peripheral neuropathy, hair loss and cardiac arrhythmias. A derivative of this chemical, etoposide, is used in small cell lung cancer, lymphoma and testicular cancer. The mode of action of etoposide is not completely known, but it may be due to an inhibitory effect on topoisomerase similar to that of doxorubicin (see above). Adverse effects of etoposide are nausea and vomiting, hair loss and bone marrow suppression. Growth of such tumours can be suppressed by hormones with the opposite action, by hormone antagonists or by inhibition of hormone secretion. Hormonal treatment plays an important role in the management of cancers of the breast, prostate and endometrium. Radioactive iodine, although not a hormone itself, is taken up by the thyroid gland and incorporated into thyroid hormones. During this process, it emits radiation that causes destruction of the thyroid gland. It is a drug that interacts with alcohol and generally increases the effects of central nervous system depressants and can produce hypertension. Normal cells can synthesize asparagine; therefore the drug is selective for certain tumours. They are used only in specific types of cancer, usually if more conventional chemotherapy has failed. Interferons are produced by many cells of the immune system and some (interferon) have anti-tumour effects. Interleukin-2 regulates the proliferation of tumour-killing T lymphocytes and natural killer cells. Monoclonal antibodies (rituximab and alemtuzumab) have been developed recently which cause lysis of B lymphocytes. These drugs are intended to be used in particular types of leukaemia when other forms of treatment have failed to produce a long-lasting remission. The most serious adverse reaction with these drugs is the so-called cytokine release syndrome. This includes fever and chills, nausea and vomiting and allergic reactions such as rashes, itching, angioedema, bronchospasm and difficulty breathing. Cancer cells produce enzymes that can breakdown the extracellular matrix between normal cells and allow cancer cells to invade and spread in normal tissue. Drugs are being developed that inhibit angiogenesis, which is the growth of new blood vessels. A monoclonal antibody (bevacizumab) that inhibits vascular endothelial growth factor already exists for use in metastatic colorectal cancer. Other areas of research include the development of drugs that block the capacity of oncogenes to turn cells malignant; antagonists of growth factors; inhibitors of cell cycle control factors; and gene therapy to restore tumour suppressor gene function. The aim of chemotherapy is to interfere with cell division in tumour cells without damaging normal healthy cells. However, because cancer cells are similar to normal cells, chemotherapy is toxic to rapidly dividing cells in bone marrow, hair follicles and the gastrointestinal tract. Resistance to cancer chemotherapy can occur and for this reason combinations of drugs with different mechanisms of action provide the best chance of a successful cure. Vinca alkaloids inhibit formation of microtubules so that cell division is halted because the spindle cannot form. Taxanes have a similar effect by inhibition of breakdown of microtubules once the spindle has formed. Hormones are used in some hormone-dependent cancers to suppress or antagonize the particular hormone involved.
Order female viagra 50 mg on-line
Second-line agents are less effective or associated with greater side effects; however women's health york pa female viagra 100 mg mastercard, they may be useful in selected clinical situations. Behavioral modification techniques or other forms of psychotherapy also may be helpful in assisting in smoking cessation. Programs that address the many issues associated with smoking (ie, learned behaviors, environmental influences, and chemical dependence) using a team approach are more likely to be successful. Hypnosis may aid in improving abstinence rates when added to a smoking-cessation program but appears to give little benefit when used alone. Advice should be given to smokers even if they have no symptoms of smokingrelated disease or if they are receiving care for reasons unrelated to smoking. Clinicians should be persistent in their efforts because relapse is common among smokers owing to the chronic nature of dependence. However, it must be recognized that the patient must be ready to stop smoking because there are several stages of decision making. There is strong evidence to support the use of pharmacotherapy to assist in smoking cessation. In general, available therapies will double the effectiveness of a cessation effort. Policies to limit airborne exposures in the workplace and outdoors, as well as education efforts of workers and policy makers, are recommended. Instead, it optimizes other body systems so that the impact of poor lung function is minimized. While rehabilitation programs vary based on length of program, and exercise frequency and intensity, those with longer length and more frequent sessions have demonstrated the best clinical benefit. Patients receiving oxygen therapy for at least part of the day have lower rates of mortality than those not receiving oxygen. Long-term oxygen therapy provides even more benefit in terms of survival after at least 5 years of use, and it improves the quality of life of these patients by increasing walking distance and neuropsychological condition and reducing time spent in the hospital. Vaccination against influenza can begin as early as August, with most patients being vaccinated during regular medical visits or at vaccination clinics in October and November. A resting PaO2 of less than 55 mm Hg or SaO2 less than 88% with or without hypercapnia. A resting PaO2 between 55 and 60 mm Hg or SaO2 less than 88% with evidence of right-sided heart failure, polycythemia, or pulmonary hypertension. The most practical means of administering long-term oxygen is with the nasal cannula, at 1 to 2 L/min, which provides 24% to 28% oxygen. Patient education about flow rates and avoidance of flames (ie, smoking) is of the utmost importance. There are three different ways to deliver oxygen, including (a) in liquid reservoirs, (b) compressed into a cylinder, and (c) via an oxygen concentrator. Although conventional liquid oxygen and compressed oxygen are quite bulky, smaller, portable tanks are available to permit greater patient mobility. Oxygen concentrator devices separate nitrogen from room air and concentrate oxygen. Oxygen-conservation devices are available that allow oxygen to flow only during inspiration, making the supply last longer. These may be particularly useful to prolong the oxygen supply for mobile 386 patients using portable cylinders. Bronchodilators relax bronchial smooth muscle, improve lung emptying, reduce thoracic hyperinflation at rest and during exercise, and improve exercise tolerance. There are several classes of bronchodilators to choose from, and classes differ with respect to onset and duration of action, and adverse events. The initial and subsequent choice of medications should be based on the specific clinical situation and patient characteristics. Shortacting medications can be used as needed or on a scheduled basis depending on the clinical situation, and additional therapies should be added in a stepwise manner depending on the response and severity of disease. Considerations should be given to individual patient response, tolerability, adherence, and economic factors. This schema provides clearer guidance on management compared with previous recommendations, and also allows for the individualization of pharmacotherapy based on patient-specific factors of lung function, symptom frequency and severity, and exacerbation risk. According to the guidelines, patients with intermittent symptoms and low risk for exacerbations (Group A) should be treated with short-acting bronchodilators as needed. When symptoms become more persistent (Group B), long-acting bronchodilators should be initiated. Long-acting bronchodilators relieve symptoms, reduce exacerbation frequency, and improve quality of life and health status. There is no clear advantage of one delivery method over another, and it is recommended that patient-specific factors and preferences should be considered in selecting the device. With the exception of short-acting bronchodilators, Adjunctive Therapies In addition to supplemental oxygen, adjunctive therapies to consider as part of a pulmonary rehabilitation program are psychoeducational care and nutritional support. Currently, the primary goal of pharmacotherapy is to control patient symptoms and reduce complications, including the frequency and severity of exacerbations, and improving the overall health status and exercise tolerance of the patient. International guidelines recommend a stepwise approach to the use of pharmacotherapy based on disease severity, which is determined by the results of spirometry, nature of symptoms, and exacerbation rates. The primary goals of pharmacotherapy are to control symptoms (including dyspnea), reduce exacerbations, and improve exercise tolerance and health status. Currently, there is inadequate evidence to support the use of more aggressive pharmacotherapy early in the course of disease because of the lack of a disease-modifying benefit. Patients exhibit variable responses to available therapies and the treatment approach should be individualized. Bronchodilators generally work by reducing the tone of airway smooth muscle (relaxation), thus minimizing airflow limitation. In general, side effects of bronchodilator medications are related to their pharmacologic effects and are dose dependent. There is no clear benefit to one bronchodilator agent or class over others, although inhaled therapy generally is preferred. Clinicians should advise, counsel, and observe patient technique with the devices frequently and consistently. They can cause sinus tachycardia and rhythm disturbances in predisposed patients, but these are rarely reported. Activation of M1 and M3 receptors by acetylcholine results in bronchoconstriction; however, activation of M2 receptors inhibits further acetylcholine release. The lack of systemic absorption of ipratropium greatly diminishes the anticholinergic side effects such as blurred vision, urinary retention, nausea, and tachycardia associated with atropine. The soft-mist inhaler (available as Respimat) is a new type of inhalation device and requires specific patient education to ensure proper use. Compared with standard 2-agonists, ipratropium has a slower onset of action and a more prolonged bronchodilator effect. Because of the slower onset of effect (15-20 minutes compared with 5 minutes for albuterol), it may be less suitable for as-needed use; however, it is often prescribed in that manner. Others report a modest benefit with ipratropium, including a lower incidence of side effects such as tachycardia. The most frequent patient complaints are dry mouth, nausea, and an occasional metallic taste. Both a short-acting 2-agonist and ipratropium represent reasonable choices for initial therapy. When a patient does not achieve adequate control of symptoms with one agent, the combination of a shortacting 2-agonist and ipratropium is a reasonable alternative. Long-acting agents are also recommended for patients at high risk for exacerbation (category C and D). Among these agents, the choices are a short-acting 2-agonist or an anticholinergic. Either class of agents has a relatively rapid onset of action, relieves symptoms, and improves exercise tolerance and lung function. Older agents with less selectivity are no longer available and the choices for short-acting, selective 2-agonists are albuterol and levalbuterol. Racemic epinephrine is available as an over the counter therapy but is not appropriate for chronic treatment.
MENTHA PIPERITA OIL (Peppermint). Female Viagra.
- Are there safety concerns?
- Are there any interactions with medications?
- Relaxing the colon during exams including barium enemas or radiologic procedures.
- Dosing considerations for Peppermint.
- Upset stomach (dyspepsia).
- Nausea following surgery.
- What other names is Peppermint known by?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96691
Buy female viagra with paypal
More if B2 evidence of deficiency Weight menstruation blood generic 100 mg female viagra amex, electrolytes, urine Until intake and outputs A3 output, nystagmus if stabilize and oral dextrose intake is adequate Shaking, tremor, sweating, 3 days or less B2 blood pressure Shaking, tremor, sweating, 1 week or less. Mostdrug-dependenttreatment programs embrace treatment based on the Alcoholics Anonymous approach (ie,a12-stepmodel). Itshouldnotbegiven to patients currently dependent on opiates, as it can precipitate severe withdrawal syndrome. A depot formulation allows monthly administration in a usual dose of 380mgintramuscularly. Screen patients for psychiatric illness or behavior change after starting varenicline. Substance-related Disorders Chapter 71 nervousness, agitation,headache, tremor, and rapidrisein bloodpressure. Treatmentdurationiscommonly 12 weeks in trials, and common side effects include sedation, dry mouth, blurred vision,urinaryretention,andlight-headedness. If prolonged (>6 hours), the kidneys attempt to further compensate by increasing bicarbonateelimination. Readjust the ventilator or treat the underlying disorder causing hyperventilation to treat the respiratory component. One frequently cited normal saline regimen is 1 mL/kg/h for 12 hours pre-andpostprocedure. Intermittent and continuous options have different advantages (and disadvantages) but, after correcting for severity of illness,havesimilaroutcomes. Consequently,hybridapproaches(eg,sustainedlowefficiency dialysis and extended daily dialysis) are being developed to provide the advantagesofboth. Equipotent doses of loop diuretics (furosemide, bumetanide, torsemide, and ethacrynic acid) have similar efficacy. Continuous infusions of loop diureticsappear to overcome diuretic resistance and to have fewer adverse effects than intermittent boluses. Nutritional requirements are altered by stress, inflammation, and injury that lead to hypermetabolic and hypercatabolic states. They include advanced age, reduced kidney mass and low birth weight,racialorethnicminority,familyhistory,lowincomeoreducation,systemic inflammation,anddyslipidemia. Strategy for treatment of hypertension based on urine albumin excretion and target blood pressure. Riskofhypercalcemia may necessitate restriction of calcium-containing binder use and/or reduction in dietaryintake. Symptoms progress from nausea and malaise to headache and lethargy and, eventually, to seizures, coma, and death if hyponatremia is severe or developsrapidly. After hemody- namic stability is restored and intravascular volume is replaced, replace free-water deficitwith5%dextroseor0. Loop diuretics are the mostpotent,followed by thiazide diureticsand then potassium-sparing diuretics. No Administer insulin & glucose Give insulin Follow blood sugar Consider albuterol Consider bicarbonate if acidotic Give exchange resin or consider dialysis Follow potassium level every 2 hours until <5. Intramuscular magnesium is painful and should be reserved for patients with severe hypomagnesemia and limited venous access. Matzke; Chapter 35, Disorders of Calcium and Phosphorus Homeostasis, authored by Amy Barton Pai; and Chapter 36, Disorders of Potassium and Magnesium Homeostasis, authored by Donald F. Mediators of immediate hypersensitivity include histamine, leukotrienes, prostaglandin,tryptase,andkinins. This inflammatory response causes persistent chronic symptoms, including nasal congestion. Peripheral blood eosinophil count may be elevated, but it is nonspecific and has limitedusefulness. Antihistamines should be used with caution in patients predisposed to urinary retention and in those with increasedintraocularpressure,hyperthyroidism,andcardiovasculardisease. If not totally effective, select single-drug treatment based on symptoms: Antihistamines-sneezing, itching, rhinorrhea, and ocular symptoms Decongestants (systemic)-nasal congestion Intranasal steroids-sneezing, itching, rhinorrhea, and nasal congestion Cromolyn-sneezing, itching, and rhinorrhea Intranasal antihistamine-rhinorrhea and itching Intranasal anticholinergic-rhinorrhea If symptoms controlled but adverse effects are bothersome or intolerable, adjust dosage or switch to another agent within the same therapeutic category. If patient is adherent, adjust dosage or if necessary, switch to another agent in a different therapeutic category or add a second agent from a different therapeutic category. For perennial disease, once symptoms are adequately controlled with minimal adverse effects, continue therapy and reassess patient in 6 to12 months. Additional consideration: Assess patient for appropriateness of immunotherapy initially and again if pharmacotherapy options are not sufficiently effective. However, caution patients about potential for drowsiness because systemic availability is approximately 40%. Patients may also experience drying effects, headache, and diminished effectiveness over time. Consumers should read product labels carefully to avoid therapeutic duplication and use combination products only for shortcourses. Children ages 6 months to 5 years may be given one 4-mg chewable tablet or oral granule packetdaily. Poorcandidatesinclude patients with medical conditions that would compromise the ability to tolerate an anaphylactic-type reaction, patients with impaired immune systems, and patients withahistoryofnonadherence. The concentration is increaseduntil the maximum tolerated dose or highest planned dose isachieved. Moreseverereactions(generalizedurticaria,bronchospasm,laryngospasm, vascular collapse, and death from anaphylaxis) occur rarely. Leukotrienes C4, D4, andE4 arereleasedduring inflammatory processes in the lung and produce bronchospasm, mucus secretion, microvascularpermeability,andairwayedema. The nonadrenergic, noncholinergic nervous system in the trachea and bronchi may amplify inflammation by releasing nitricoxide. History of previous asthma exacerbations (eg, hospitalizations, intubations) and complicating illnesses (eg, cardiac disease, diabetes) should be documented. Aerosol administration enhances bronchoselectivityand providesmore rapidresponse and greater protectionagainstprovocations (eg,exercise,allergen challenges) than systemicadministration. Regular treatment (four times daily) does not improve symptom controloveras-neededuse. Intensity of treatment depends on severity of symptoms: up to 3 treatments at 20-minute intervals as needed. Stepwise approach for managing asthma in adults and children age 5 years and older. Median durations with the highest value after a single dose and lowest after chronic administration. Protection refers to the prevention of bronchoconstriction induced by exercise or nonspecific bronchial challenges. The usual regimen is to continue the oral corticosteroid for the duration of hospitalization. If the patient is then started on inhaled corticosteroids, there is no need to taper the systemic corticosteroid dose. Short-acting agents provide complete protection for at least 2 hours; long-acting agents provide significant protection for 8 to 12 hours initially, but duration decreases with chronic regularuse. Toxicities may be decreased by alternate-day therapyorhigh-doseinhaledcorticosteroids.
Buy female viagra 50mg
The area may be painful mensis discount female viagra 100mg without a prescription, firm, soft, warmer, or cooler as compared with adjacent tissue. A stage 2 sore also may be reversible; partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed. May also present as an intact or open/ruptured serum-filled blister or as a shiny or dry shallow ulcer. Depth of the ulcer varies by anatomical location; may range from shallow to extremely deep over areas of significant adiposity. Full thickness tissue loss with exposed bone, tendon, or muscle; can extend into muscle and/or supporting structures (eg, fascia, tendon, or joint capsule) making osteomyelitis possible. Often include undermining and tunneling; depth of the ulcer varies by anatomical location. Full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green, or brown) and/ or eschar (tan, brown, or black) in the wound bed. Suspected deep tissue injury Stage 1 Stage 2 Stage 3a Stage 4a Unstageablea Stage 3, Stage 4, and unstageable lesions are unlikely to resolve on their own and often require surgical intervention. Human bite wounds are notable for potential involvement of Eikenella corrodens in approximately 30% ofinfections. Dirty N/A N/A Obvious preexist- Therapeutic ing infections antibiotics present (abscess, required pus, or necrotic tissue present). Antianaerobic cephalosporins (eg, cefoxitin or cefotetan) are appropriate choices when broad-spectrum anaerobic and gramnegativecoverageisdesired. Educate Develop an educational program that enforces the importance and rationale of timely antimicrobial prophylaxis. Standardize the ordering process Establish a protocol (eg, a preprinted order sheet) that standardizes antibiotic choice according to current published evidence, formulary availability, institutional resistance patterns, and cost. Standardize the delivery and administration process Use a system that ensures that antibiotics are prepared and delivered to the holding area in a timely fashion. Provide visible reminders to prescribe or administer prophylactic antibiotics (eg, checklists). Develop a system to remind surgeons or nurses to readminister antibiotics intraoperatively during long procedures. Provide feedback Follow up with regular reports of compliance and infection rates. Screening for tuberculosis and tuberculosis infection in high-risk populations: Recommendations of the Advisory Council for the Elimination of Tuberculosis. A minimum of two drugs, and generallythree or four drugs,must be usedsimultaneously. Ethambutol can be stopped if susceptibility to isoniazid, rifampin,andpyrazinamideisshown. For patients started on this regimen and found to have a positive culture from the 2-month specimen, treatment should be extended an extra 3 months. Dose may need to be adjusted when there is concomitant use of protease inhibitors or nonnucleoside reverse transcriptase inhibitors. In younger children, ethambutol at the dose of 15 mg/kg per day can be used if there is suspected or proven resistance to isoniazid or rifampin. Data from American Thoracic Society, Centers for Disease Control and Prevention, Infectious Diseases Society of America. Monitoring of serum drug concentrations should be considered to ensure adequate drug absorption, without excessive accumulation, and to assist in avoiding toxicity. Until data become available, begin with doses recommended for patients receiving hemodialysis and verify adequacy of dosing using serum concentration monitoring. Microscopic examination of the urine should be performed by preparation of a Gram stainofunspun or centrifugedurine. Amoxicillin or ampicillin is not recommended because of the high incidence of resistantE. Fluoroquinolones(ciprofloxacinorlevofloxacin)orallyfor7to10days are the first-linechoice in mildto moderate pyelonephritis. Main advantage is the lack of resistance even after long courses of therapy Single-dose therapy for uncomplicated infections, low levels of resistance, use with caution in patients with hepatic dysfunction Urinary Tract Infections the fluoroquinolones have a greater spectrum of activity, including P. They are very useful in renally impaired patients or when an aminoglycoside is to be avoided Second- and third-generation cephalosporins have a broad spectrum of activity against gram-negative bacteria, but are not active against enterococci and have limited activity against P. Aztreonam is a monobactam that is only active against gram-negative bacteria, including some strains of P. Generally useful for nosocomial infections when aminoglycosides are to be avoided and in penicillin-sensitive patients these agents have broad-spectrum activity against both gram-negative and gram-positive bacteria. In patients who relapse after 2 weeks, therapy should be continued for another 2 to 4 weeks. If live vaccines are not administered simultaneously, their administration should be separated by at least4weeks. Forunvaccinated children ages 12 to 14 months, two doses should be given, with an interval of 2 monthsbetweendoses. Inaddition, adolescents should receive a pertussis-containing vaccine with their next doseofTdtoxoids. WhensplenecP tomy is planned, pneumococcal vaccine should be given at least 2 weeks before surgery. More than half of young-onset, dominantly inherited cases are attributed to alterations on chromosomes1,14,or21. May deny memory problems Moderate Patient requires assistance with activities of daily living. Ruleoutmedication use (eg, anticholinergics, sedatives, hypnotics, opioids, antipsychotics, and anticonvulsants)ascontributorsto dementiasymptoms. When switching from one cholinesterase inhibitor to another, 1 week washout is generallysufficient. It is usually well tolerated; side effects include constipation,confusion,dizziness,andheadache. Adverse events (eg, somnolence, extrapyramidal symptoms, abnormal gait, worsening cognition, cerebrovascular events, and increased risk of death [see black-box warning]) offset advantages. Normal membrane conductances and inhibitory synaptic currents then break down, and excitability spreads locally(focalseizure)ormorewidely(generalizedseizure). A tonic-clonic seizurethat isprecededbyan auraislikelya partialseizure thatissecondarilygeneralized. Simple partial onset followed by impairment of consciousness-with or without automatisms 2. Poor prognostic factors include a history of a high frequency of seizures,repeated episodes of status epilepticus, a combination of seizure types, and development of abnormalmentalfunctioning. Expert Panel 2005 Carbamazepine Levetiracetam Lamotrigine Oxcarbazepine Partial seizures (refractory monotherapy) U. Some teratogenic events can be prevented by adequate folate intake; prenatal vitamins with folic acid (~0. Clinical data suggest that oxcarbazepine is as effective as phenytoin, valproic acid,andimmediate-release carbamazepine,withperhapsfewersideeffects. Other side effects include nausea, hepatitis, osteomalacia,cardiacconductiondefects,andlupus-likereactions. It is eliminated exclusively renally, and dosage adjustment is necessary in patients with impairedrenalfunction. Moderate hepatic and renal impairment both increase systemic drug exposurebyupto40%.
Buy female viagra 100mg online
Risk stratification for in-hospital mortality in acutely decompensated heart failure: Classification and regression tree analysis women's health controversial issues order cheap female viagra online. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-convertingenzyme inhibitors. Medical therapy of acute myocardial infarction by application of hemodynamic subsets (first of two parts). Relationship between heart failure treatment and development of worsening renal function among hospitalized patients. Practical applications of intravenous diuretic therapy in decompensated heart failure. Diuretic efficacy of high dose furosemide in severe heart failure: Bolus injection versus continuous infusion. Continuous versus intermittent infusion of furosemide in acute decompensated heart failure. Risk of death associated with nesiritide in patients with acutely decompensated heart failure. Short-term risk of death after treatment with nesiritide for decompensated heart failure: A pooled analysis of randomized controlled trials. Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Effects of tolvaptan, a vasopressin antagonist, in patients hospitalized with worsening heart failure: A randomized controlled trial. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. Dopamine does not enhance furosemide-induced natriuresis in patients with congestive heart failure. Efficacy and safety of high dose versus low dose furosemide with or without dopamine 38. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: A randomized controlled trial. Beta-blocker therapy influences the hemodynamic response to inotropic agents in patients with heart failure: A randomized comparison of dobutamine and enoximone before and after chronic treatment with metoprolol or carvedilol. Advanced heart failure treated with continuous-flow left ventricular assist device. Left ventricular assist device and drug therapy for the reversal of heart failure. The Registry of the International Society for Heart and Lung Transplantation: Thirtysecond Official Adult Heart Transplantation Report-2015; Focus Theme: Early Graft Failure. Clinical pharmacy services in heart failure: An opinion paper from the Heart Failure Society of America and American College of Clinical Pharmacy Cardiology Practice and Research Network. Pharmacist care of patients with heart failure: A systematic review of randomized trials. Transitions of care in heart failure: A scientific statement from the American Heart Association. Assessment of successful treatment of angina includes not only reducing the number of episodes and increasing the amount of exertion needed to precipitate an episode, but also allowing patients to participate in activity that provides a high-level quality of life. Revascularization can provide a survival advantage compared to medical therapy in patients with more extensive atherosclerotic disease. It may also present as chronic stable exertional angina or ischemia without clinical symptoms (silent ischemia). The risk of mortality is greatest for black men, followed by white men, black females, and white females. These patients often have a reduced quality of life due to their inability to conduct activities of daily living without chest pain. The larger the size of the ventricular cavity, the more energy or myocardial work is needed to begin myocardial contraction (systole). Once that occurs, the aortic valve is pushed open and blood is ejected into the systemic circulation. Hurrying is particularly likely to precipitate angina, as are efforts involving motion of the hands over the head. Mental and emotional stress may also precipitate angina, presumably by increasing adrenergic tone, and reduced vagal activity. Sexual activity may also precipitate angina due to the combination of physical exertion and emotional stimulation. Other precipitates of angina include physical exertion after a heavy meal and excessive metabolic demands imposed by chills, fever, thyrotoxicosis, tachycardia from any cause, exposure to cold, and hypoglycemia. Anger can also produce constriction of coronary arteries with preexisting narrowing, without necessarily directly affecting O2 demand. The process of maintaining adequate coronary blood flow to meet the metabolic demands of the myocytes is complex with multiple factors influencing both sides of the supply/demand equation. The process and development of atherosclerosis is covered in detail in Chapter 17. Since their geometry does not typically change acutely, they provide a relatively fixed decrease in myocardial oxygen supply. Determinates of Myocardial Oxygen Supply Coronary Blood Flow Meeting the metabolic demands of the myocardium is centered on the ability to maintain adequate coronary blood flow and coronary arterial pressure. The larger epicardial vessels typically offer little resistance to blood flow and are able to accommodate large increases in coronary flow without producing any significant drops in pressure. Most resistance to flow in normal coronary arteries is provided by the smaller endocardial (R2) vessels. These vessels will contract and dilate to maintain blood flow based on the metabolic demands of the myocardium. Resistance to flow equals R1 + R2 and R2 resistance is normally much greater than R1; hence flow is equal to the driving pressure across the coronary bed divided by the resistance in R2. Dilation in R2 normally occurs in response to exercise or increased myocardial oxygen demand. When an atherosclerotic lesion narrows the conductance vessel, the arterioles dilate under resting conditions to prevent ischemia. Coronary atherosclerotic plaque development typically occurs in the larger epicardial vessels. As these plaques continue to grow and cause luminal narrowing of the vessel, the vessel is transformed from one that originally provides minimal resistance into one that now provides considerable resistance to blood flow. This continues to a point where the epicardial artery resistance becomes dominate. Through autoregulation, this increase in resistance in the R1 or conductance vessels is offset by vasodilation in the R2 or resistance vessels to maintain flow. The most important determinant of stenosis resistance for any given level of flow is the minimum stenosis cross-sectional area. Stenosis length and changes in cross-sectional area distal to the stenosis are relatively minor determinates of resistance for most coronary lesions. Coronary plaques that occupy less than 50% to 70% of the vessel luminal diameter rarely produce ischemia or angina. Therefore, since these smaller plaques do not produce symptoms, the patient and clinician typically have no idea that they are there. Since small plaques have a rich lipid core and thin fibrous cap, they are more prone to rupture and acute thrombus production, making them quite dangerous and lethal (see Chapter 17). Further increments in exercise intensity can no longer be accompanied by further decreased in endocardial (R2) resistance, and no further increments in flow can occur once autoregulation has reached its ceiling. It is inversely related to the minimum stenosis cross-sectional area and varies with the square of the flow rate as stenosis severity increases. The endocardial flow reserve is completely exhausted at rest when the epicardial stenosis severity exceeds 90%, which is also referred to as a critical stenosis. The combination of physical forces of altered coronary pressure, growth factors, and endogenous vasodilators (eg, nitrous oxide and prostacyclin) change native collateral vessels of approximately 200 m in existing epicardial anastomoses into mature vessels that can reach 1 to 2 mm in diameter. The process of angiogenesis is also driven by physical forces and growth factors, but produces smaller, capillary-like vessels from preexisting coronary vessels. These vessels may provide collateral flow when they develop in the border between ischemic and nonischemic regions of the myocardium. Investigation into pharmacologic mechanisms to improve collateral vessel development has been largely disappointing. While chronic nitrates may assist in development of collateral vessels, the use of growth factors and vasodilators have not produced the expected results. Due to the variability in collateral vessel development across different species, the use of animal models for study has significant limitations.