Order cefaclor from india
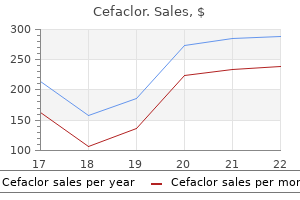
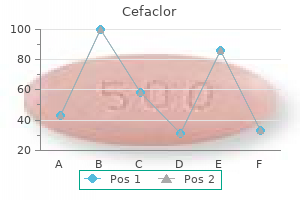
Renal Exploration Renal exploration for persistent or delayed bleeding during initial nonoperative management of a renal injury occurs in a small percentage of cases (LeeVan et al medications qid discount cefaclor 250 mg on-line. The goals of exploration at this time are similar to the goals of renal exploration for unstable patients at the time of initial presentation, but patients are typically more stable. The goals include isolation and control of renal vasculature, complete exposure of the area of injury, debridement of any devitalized tissue, closure of collecting system defects, closure of renal parenchyma over a bolster, and adequate drainage of the area. Renal Arterial Occlusion Another type of renal artery injury is complete or partial occlusion of renal arterial flow after blunt trauma caused by renal artery embolism or an intimal flap. This type of injury has been observed successfully, but a postinfarction syndrome with fever and flank pain may be expected, and these patients should be followed for the development of hypertension (Jawas and Abu-Zidan, 2008; Xu et al. Exploration with nephrectomy may be considered for uncontrolled pain or infection in a patent who is being observed. In more than 50 reported cases, percutaneous renal artery revascularization by interventional radiologists with angioplasty and/or endovascular stenting has been reported to successfully salvage some kidneys with completely occluded or partially occluded renal arteries after blunt trauma (Jahangiri et al. Control of Renal Vasculature When renal exploration for trauma was more common, the method and timing of control of the renal vessels was a topic of interest. Some advocated for early control of vessels through an incision in the mesentery medial to the inferior mesenteric vein to identify the aorta and renal vessels as a way to decrease nephrectomy risk (Carroll et al. In addition, retrospective series with early vascular control seemed to have lower nephrectomy rates than series without early vascular control (Atala et al. One randomized trial between early vascular control and no early vascular control did not show a difference in nephrectomy rates, and the early vascular control group had longer operative times (Gonzalez et al. For early control of vessels, an incision in the posterior mesentery medial to the inferior mesenteric vein over the aorta is made, and vessel loops are applied around the renal vessels and tightened if needed. Ureteropelvic Junction Disruption Ureteropelvic junction disruption is a rare renal injury but is important not to miss (Murphy et al. This injury is associated with high-velocity acceleration/deceleration injuries and hyperextension of torso (Palmer and Drago, 1981; Pesenti et al. A rapid change in position of the more mobile kidney away from the more fixed proximal ureter is thought to be the pathophysiology. The urine analysis usually shows some degree of hematuria, but a significant minority of cases do not demonstrate hematuria (Al-Qudah and Santucci, 2006; Brandes et al. This surgery is difficult as the renal pelvis is typically not dilated, and good exposure is essential. Debridement of any nonviable ureter and renal pelvis should be performed followed by a spatulated, tension-free anastomosis of the ureter to the renal pelvis. We recommend doing the repair over a double-J ureteral stent left in place for 4 to 6 weeks and over a retroperitoneal Reconstruction Versus Nephrectomy In addition to stopping life-threatening hemorrhage, one goal of renal exploration should be to save and reconstruct the kidney whenever feasible and safe for the patient (Kitrey et al. After opening up Gerota fascia, vascular control of the main renal arteries and veins should be obtained if this has not been done. The kidney should be freed up so the entire area of injury is exposed, which may require exposure of the entire kidney. Any bleeding parenchymal vessels should be oversewn with absorbable suture and any holes in the collecting system closed with absorbable suture. Small renal defects can be closed by placing large absorbable sutures through the renal capsule. Larger renal defects are typically closed after packing the defect with hemostatic bolsters or omentum. For closure of larger defects, we like to use bolsters of hemostatic agents and to close the defect over the bolster using the sliding clip technique; however, many different techniques for renorrhaphy are available (Benway et al. If the renal injury is too severe to repair or would leave a very small portion of remaining kidney, nephrectomy should be performed. In addition, if the patient is unstable and it is safest to expedite surgery with nephrectomy to save the life of the patient because of hypothermia, coagulopathy, or ongoing blood loss, nephrectomy should be performed. In a penetrating injury, especially high-velocity gunshot wounds, it is important to inspect the ipsilateral ureter for any injury and repair if found. Renal Arterial Laceration Because the kidney does not have good collateral arterial flow, whatever renal segments that are devitalized by an arterial injury typically are not salvageable. If the main renal artery is avulsed or injured and bleeding significantly, the surviving patient will be hemodynamically unstable and should be explored with an anticipated nephrectomy. In fact, attempts to repair these types of injuries are associated with poorer outcomes (Knudson et al. In a patient with a solitary kidney or bilateral renal arterial injuries, consideration should be given to an attempt at renal artery injury repair (Kitrey et al. Vascular surgery consultation should be obtained if available for these rare situations. Bilateral ureteropelvic junction disruption injury after a high-velocity motor vehicle collision. A nephrostomy tube could also be considered based on surgeon preference or if repair was tenuous. Although there is little guidance from literature, we would recommend delayed repair about 2 to 3 months after drain placement. The delayed surgery follows the same principles as the immediate surgery, but scar tissue in the area of the renal pelvis and proximal ureter may make the surgery more difficult. Nephrectomy should always be mentioned to families as a possibility if a repair is not possible. Cases have been managed successfully with an indwelling ureteral stent, and others have undergone operative repair (Ashebu et al. Renal Pelvis Rupture Renal pelvis rupture is a rare finding after renal trauma (Ashebu et al. Large fluid collection around dilated renal pelvis led to ureteral stent placement and percutaneous drain into urinoma (A). Percutaneous drain fluid consistent with urine and removed after drainage was minimal. Retrograde pyelogram at time of ureteral stent removal showing no extravasation (B). After the patient recovers from the injury, options include removal of the ureteral stent followed by pyeloplasty several weeks later or pyeloplasty with an indwelling ureteral stent. In our experience, removal of the ureteral stent followed by delayed robotic-assisted laparoscopic pyeloplasty 8 to 12 weeks later has worked well with minimal periureteral inflammation and scarring. However, given concern for infection in a poorly draining kidney after ureteral stent removal, a pyeloplasty with an indwelling ureteral stent in place can be performed. Duplex Kidney Duplication anomalies can make management of urine leaks more complicated, and urologists need to keep in mind that approximately 1% to 2% of the population have complete duplications of the renal collecting system, and partial duplications such as bifid pelvis are more common (Privett et al. For example, if a ureteral stent is placed for a urine leak into the upper pole ureter when the urine leak is coming from the lower pole of the kidney, this obviously would not help the urine leak. Fusion Anomalies and Ectopic Kidney In general, renal injuries to kidneys with fusion anomalies or ectopic kidneys are managed similarly to kidneys without fusion or position anomalies. Follow-Up and Long-Term Issues Once a patient has recovered from his or her traumatic injuries, several issues should be addressed with the patient and family. These issues include follow-up imaging, need for assessment of remaining renal function in the injured kidney, long-term risks of hypertension and chronic kidney disease, and physical activity limitations. Grade 4 injury to left-sided moiety with chronic ureteropelvic junction obstruction of a horseshoe kidney. Immediate contrast phases showing chronic-appearing hydronephrosis with hematoma in collecting system and perirenal hematoma (A and B). Delayed phases showing urine leak (red arrow) (C) and isthmus (D) of horseshoe kidney. Late Repeat Imaging and Assessment of Renal Function One issue that comes up at time of discharge is what follow-up imaging pediatric renal trauma patients should have. The risk for renal scarring is approximately 60% for grade 3 injures and closer to 100% for grade 4 to 5 injuries, with some decline in differential function (Dunfee et al. Typically renal scans are obtained if there is concern about significant loss of function and/or if hypertension is present in follow-up. In adults after a grade 3 or higher injury, the risk for developing hypertension is likely 5% to 15% (Osterberg et al.
Cheap 250mg cefaclor amex
No cases of testicular atrophy occurred medications for rheumatoid arthritis buy cefaclor 500mg with visa, and high testes requiring surgery occurred in 4%, which was inversely related to body weight. After division of the sac distal to the ring, the peritoneum was closed using a purse-string suture of a nonabsorbable material. The median operating time was 22 minutes (unilateral, 7 to 30; bilateral, 12 to 42) with one recurrence. Multiple reports have been published regarding a laparoscopic approach to the incarcerated hernia whereby the bowel is brought back into the abdomen, inspected, and the hernia closed by variable techniques (Zhou et al. They purport three main advantages of the laparoscopic approach: aversion of edematous tissue by bypassing the cord structures; bowel reduction performed under direct visual control; and inspection of the incarcerated organ at case end. Viral Sterile or traumatic Scrotal edema or erythema Diaper dermatitis, insect bite, or other skin lesions Idiopathic scrotal edema Orchitis Associated with epididymitis with or without abscess Vasculitis. These noncommunicating scrotal masses are tense and extend into the abdomen, where they may be palpable. Abdominoscrotal hydroceles usually manifest in infancy as such or as scrotal hydroceles that enlarge over time (Celayir et al. Associated diagnoses include cryptorchidism, contralateral hernia, hydrocele, or vanishing testis. The most likely cause is enlargement and extension of a scrotal hydrocele into the retroperitoneal or properitoneal space after closure of the processus. Massive enlargement could extend into the upper abdomen and be associated with hydroureteronephrosis, lower extremity edema, or appendicitis (reviewed by Cuervo et al. The traditional surgical approach is an inguinal incision with proximal dissection of the sac from its abdominal attachments and distal complete or partial mobilization, with or without orchidopexy. Some authors advocate orchidopexy to avoid iatrogenic cryptorchidism (Bayne et al. Aspiration of the scrotal component may facilitate the proximal dissection (Cuervo et al. Alternative approaches include a midline abdominal approach for large bilateral cases (Serels and Kogan, 1996) or laparoscopic decompression of the abdominal component followed by inguinal excision (Abel et al. To avert injury to the spermatic cord or vas, a strip of the lining of the sac may be left along the cord (Cuervo et al, 2009; Ferro et al. Tightening of a patulous internal ring is described but may be unnecessary because the processus vaginalis is invariably closed. Belman (2001) described a primary scrotal approach with drainage, excision, and extensive plication with limited dissection. Persistent scrotal swelling, hematoma, and undescended and/or hypoplastic testis was reported in 11 inguinal cases and infection in 2 scrotal cases. Although all of these diseases can occur at any time during childhood, appendage torsion is typically most common after infancy and before puberty, whereas epididymitis and spermatic cord torsion are most common in the perinatal and pubertal periods. Torsion of an appendage and epididymitis are managed conservatively with limited consequence; prompt surgical exploration for testicular torsion is imperative because the gonad is at considerable risk of ischemic damage or loss, particularly when there is a delay in presentation, evaluation, or management. Delay in presentation for medical attention may stem from patient embarrassment or denial but also from lack of public awareness regarding torsion and the possible consequences. In response, these authors presented an electronic module aimed at educating health care providers on the evaluation and differential diagnosis of acute scrotal pain that was learned within 30 minutes, increased confidence in assessment (Friedman et al. Spermatic Cord Torsion Acute Intravaginal Spermatic Cord Torsion Predisposing Factors. Intravaginal torsion is commonly attributed to excess mobility of the testis within a "bell-clapper deformity," wherein the tunica vaginalis abnormally fixes proximally on the cord. Although found in 12% of males at autopsy (Caesar and Kaplan, 1994a), the prevalence of torsion is much lower: 8. There is evidence for a familial predisposition (Collins and Broecker, 1989; Cubillos et al. Ultrasound offered a rapid, available, and safe modality to assess testicular architecture, intraparenchymal blood flow, and other anatomic details (hydrocele, scrotal thickening). However, in other studies the sensitivity in confirming decreased or absent blood flow in proven cases of spermatic cord torsion was only 63% to 90%, possibly because of enhanced detection of flow with newer equipment and/or user-dependent characteristics (Bentley et al. Increased epididymal size and/or echogenicity and altered epididymal vascularity, usually absent or reduced but occasionally increased, may provide additional support for the diagnosis of torsion (Nussbaum et al. Infrared thermography showed significant reduction in scrotal temperature by 1 hour after 720-degree torsion and prompt normalization with detorsion in a sheep model (Capraro et al. Transscrotal near infrared spectroscopy was able to reliably discriminate torsion from nontorsion in a select group of children with acute testis pain (Schlomer et al. The inciting event for torsion is unknown but may include cold temperature (Chiu et al. Cryptorchid testes are at increased risk of torsion and difficult to assess because of the high position. The prevalence of testicular torsion is 1 in 4000 (Williamson, 1976) with left-sided predominance and rare bilaterality. Classically, boys complain of acute, severe scrotal pain that occurs at rest (even sleep) or with physical activity or after trauma. Alternatively, patients may have milder, less acute, or even absent scrotal pain or may have inguinal or abdominal pain. Scrotal edema and erythema may be present, depending on the duration or degree of torsion. The most common physical findings are generalized testicular tenderness, abnormal orientation of the testis, and absent cremasteric reflex. Inspection may identify the high-riding testis from a foreshortened cord and horizontally oriented testis. The genitofemoral reflex arc, normally present after age 2 years (Caesar and Kaplan, 1994b), is elicited by scratching the inner thigh with resultant testis elevation. Some studies report reduced or absent reflex in all cases of testicular torsion (Caldamone et al. The presence of a cremasteric reflex correlates with intact testicular blood flow but does not unequivocally indicate normal testicular perfusion, especially if the clinical presentation is otherwise suggestive of torsion. Although anterior epididymal position, thickening of the cord, testicular induration, loss of boundaries between the testis and epididymis, scrotal edema, and/or erythema may be present, landmarks become obliterated and the examination less reliable as the duration of torsion increases. Several efforts have been made to offer a better clinical assessment of testicular torsion in patients with the acute scrotum. According to use of a decision tool, patients with acute (<72 hours) scrotal pain and all of the following had no risk of testicular torsion (100% sensitivity and negative predictive value): normal testicular lie, lack of nausea and vomiting, and age 0 to 10 years (Shah et al. Urinalysis is of limited usefulness in cases of testicular torsion but is used to identify pyuria and/or bacteriuria associated with epididymitis or hematuria, implicating a urinary tract calculus. Before the advent of reliable and rapid scrotal imaging, immediate scrotal exploration was routine. Radionuclide imaging carried about 90% sensitivity and specificity but was lengthy, was Management and Surgical Treatment Testicular torsion is a true surgical emergency because testis viability is inversely related to duration of torsion. B-Mode (left) and color Doppler ultrasonography (right) images showing hyperechoic central body of the snail and coiling of blood within the distal spermatic cord around the central echogenic "body. The affected testis is re-examined for potential viability, and the largely subjective decision for orchidopexy or orchiectomy is made. A Doppler flow probe or incision of the tunica albuginea (Arda and Ozyaylali, 2001) with assessment of bleeding may document intratesticular flow after detorsion; however, the reliability of these assessments lacks validation. If the testis is to be retained, it is fixed either via dartos pouch or directly to the dartos with nonabsorbable suture. Risk factors for orchiectomy include young age, African-American race, and being on Medicaid or lacking insurance (Cost et al. This may reflect the transfer of patients, which delayed treatment by 75 minutes in the study by Bayne et al. Orchiectomy is performed by dividing the cord into segments, each of which is ligated with nonabsorbable suture. In cases of orchiectomy, prosthesis placement is usually offered after complete healing or later in puberty; however, Bush and Bagrodia (2012) demonstrated the feasibility of performing concurrent prosthetic placement and orchiectomy. The degree of torsion may provide incomplete vascular occlusion, helping to explain the variability of these data or have a multiplicative effect on the time course to testis loss (Dias et al.
Cefaclor 500mg with mastercard
Herzog B treatment xanthelasma purchase cefaclor 250mg overnight delivery, Steigert M, Hadziselimovic F: Is a testis located at the superficial inguinal pouch (Denis Browne pouch) comparable to a true cryptorchid testis Khairi A, Shehata S, El-Kholi N: Is it necessary to close the peritoneum over the deep inguinal ring during laparoscopic orchidopexy Kvist K, Clasen-Linde E, Langballe O, et al: the expression of markers for intratubular germ cell neoplasia in normal infantile testes, Front Endocrinol (Lausanne) 9:286, 2018. Minehan T, Touloukian R: Letter: cryptorchidism in siblings, Pediatrics 53(5):770, 1974.
Order generic cefaclor on line
Lane C treatment urinary retention order cheap cefaclor line, Boxall J, MacLellan D, et al: A population-based study of prevalence trends and geospatial analysis of hypospadias and cryptorchidism compared with non-endocrine mediated congenital anomalies, J Pediatr Urol 13(3):284. Single institution outcome analysis of three surgical techniques over a 10-year period, J Pediatr Urol 12(1):28. Manzoni G, Bracka A, Palminteri E, et al: Hypospadias surgery: when, what and by whom Schlomer B, Breyer B, Copp H, et al: Do adult men with untreated hypospadias have adverse outcomes Snodgrass W, Bush N: Staged tubularized autograft repair for primary proximal hypospadias with 30-degree or greater ventral curvature, J Urol 2017a. Snodgrass W, Villanueva C, Bush N: Primary and reoperative hypospadias repair in adults-are results different than in children Springer A, van den Heijkant M, Baumann S: Worldwide prevalence of hypospadias, J Pediatr Urol 2015. Thiersch C: Uber die Entsehungweise und operative Behandlung des Epispadie, Arch Heilkd 10:1869. Testicular descent is a complex and prolonged event that is completed in the third trimester of gestation or soon after birth. The fetal structure that orchestrates descent of the testis, the gubernaculum, is anatomically well-characterized, but gaps in knowledge remain regarding its mechanical function during testicular descent. Genetic and/or environmental factors likely contribute to failure of testicular descent, but also these remain largely unknown. Cryptorchidism was traditionally considered a congenital anomaly identifiable at birth, but strong evidence now exists that an initial diagnosis well beyond the neonatal period is not uncommon. Clinically significant differences that affect long-term outcome, if any, between the acquired and congenital presentations of cryptorchidism remain obscure. Retractile testes may represent a milder form of the disease in some cases, conferring a higher risk for acquired cryptorchidism that is diagnosed later in childhood. Ultrasonography and other forms of imaging are rarely if ever needed for diagnosis, and hormonal therapy is no longer advocated as a first-line treatment for cryptorchidism. Present evidence supports surgery as the preferred treatment, with the specific approach depending on testicular palpability and position, size, patient age, and overall health status. Suboptimal semen quality is common in bilateral cases, but can also occur in unilateral cryptorchidism, although paternity may be preserved. Long-term outcome depends on laterality, age at treatment, and potentially, on the underlying etiology. Most absent testes are vanishing or vanished, present initially in development but lost as a result of vascular accident or torsion unilaterally (monorchia) or, very rarely, bilaterally (anorchia) (Abeyaratne et al. Acquired cryptorchidism is defined as a cryptorchid testis that was documented as scrotal at a previous examination. Recurrent cryptorchidism is defined as a cryptorchid testes that was undescended at birth, descended spontaneously, and is subsequently extrascrotal. Secondary cryptorchidism and testicular retraction have been used to describe a testis that is suprascrotal after inguinal hernia repair or as a complication of orchidopexy, respectively. Testicular malposition after hernia repair could be caused by either primary maldescent or postoperative scarring. Retractile testes are scrotal testes that retract easily out of the scrotum but can be manually replaced in a stable scrotal position and remain there at least temporarily until there is recurrent stimulation. Testes that are significantly retractile, that is, those that rarely remain in a stable scrotal position (spontaneously or with manipulation) and/or are located at rest in the high scrotum may or may not be diagnosed as cases of acquired cryptorchidism on longitudinal examination. Downstream effects and interactions, if any, between hormonal and neural pathways, are poorly defined.
Purchase cefaclor with a visa
In another study from England medications 7 rights purchase cefaclor 250 mg free shipping, investigators showed a statistically significant difference in the incidence of anemia between 410 bacteriuric pregnant women and 409 control pregnant women (Williams et al. This separation increased during the third trimester (32 weeks), when 25% of women treated with placebo alone had anemia, but only 16. Furthermore, in the 31 untreated (placebo-treated) bacteriuric women who subsequently developed pyelonephritis, the incidence of anemia was 45. These investigators concluded that "untreated bacteriuria increases the likelihood of developing anemia during pregnancy and that this risk is enhanced by the development of acute pyelonephritis, even if it is treated promptly" (Williams et al. If nitrofurantoin is used, however, this is discontinued at 35 weeks of gestation because of an increased risk of hemolytic anemia in the neonate. If a pregnant woman has a single episode of pyelonephritis or two episodes of cystitis, daily suppression with either nitrofurantoin or cephalexin should be considered until delivery. It is prudent to prescribe a full 3- to 7-day course of therapy in pregnant women. However, there was not adequate evidence at that time to suggest that a single-dose treatment was as effective as standard conventional treatment (Widmer et al. A more recent Cochrane review published in 2015 looked at the duration of treatment for asymptomatic bacteriuria (Widmer et al. The authors looked at 13 studies that included 1622 women and compared single-dose treatment with 4- to 7-day course (short) treatment. The review found that a 7-day regimen was more effective than a 1-day course, especially for preventing a low-birth-weight outcome, but this was based on only one study. There were no differences for other review outcomes such as pyelonephritis and preterm birth. The authors concluded by saying although more trials were needed, women with asymptomatic bacteriuria in pregnancy should be treated with a standard time regimen of antibiotics. If the culture is positive, the cause of bacteriuria must be determined to be lack of resolution, bacterial persistence, or reinfection. If the infection is unresolved, proper selection and administration of another drug will likely solve the problem. If the problem is bacterial persistence or rapid reinfection, antimicrobial suppression of infection or prophylaxis (Pfau and Sacks, 1992) throughout the remainder of the pregnancy should be considered. Pregnant women with acute pyelonephritis should be hospitalized and initially treated with parenteral antimicrobial agents until clinical improvement is noted. There is no strong evidence to recommend a specific treatment regimen in pregnant women. Carbapenems are generally used in select severe cases including those caused by multidrug-resistant bacteria (Matuszkiewicz-Rowinska et al. However, older series reported that more than 95% of these patients respond within 24 hours using ampicillin and an aminoglycoside (Cunningham et al. Parenteral treatment should be tailored on the basis of culture sensitivities before transitioning to oral antibiotics. If improvement is not seen within 72 hours of the commencement of antibiotics, a renal ultrasound should be performed to assess for stone, obstruction, or abscess. They also found there was a significant reduction in asymptomatic bacteriuria in women who had a high clinic attendance rate and had received nitrofurantoin and close surveillance (Schneeberger et al. Fluoroquinolones are contraindicated because of their effects on immature cartilage. The "gray baby" syndrome is a toxic effect of chloramphenicol on neonates resulting from the inability of the infant to metabolize or excrete the drug. Sulfonamides may cause kernicterus and neonatal hyperbilirubinemia and should be avoided in the third trimester. Information about pregnancy in women with renal insufficiency is available online at ExpertConsult. Although little is known about the outcome of pregnancies with differing degrees of renal insufficiency, it is known that normal pregnancy is rare if the preconception serum creatinine level exceeds 3 mg/ dL (about 30 mL/min clearance). The degree of renal function impairment is the major determinant for pregnancy outcome. However, the perinatal mortality is approximately four times higher with severe disease. The rate of perinatal morbidity associated with low birth weight or prematurity doubles with mild to moderate maternal renal disease; in moderate to severe disease it doubles once again (Vidaeff et al. Bacteriologic characteristics of infection in the elderly differ from those in younger patients (Baldassarre and Kaye, 1991). However, there is a significant increase in the incidence of Proteus, Klebsiella, Enterobacter, Serratia, and Pseudomonas spp. One study found that in community-dwelling older women, organisms responsible for asymptomatic bacteriuria include E. Enterococci in the elderly tend to resolve without treatment; this is felt to represent colonization (Das et al. Bacteriuria caused by gram-positive bacteria is much more common in elderly men than in elderly women (Jackson et al. Polymicrobial bacteriuria is also more common among the geriatric population (Nicolle etal. Cumulatively, the shift in the pattern of uropathogens, the high frequency of polymicrobial infections, and antimicrobial resistance in the elderly are due in large part to an increase in institutionalization and hospitalization, catheterization, and overall antimicrobial usage (Routh et al. By the year 2050, however, the population aged 65 and over in the United States is projected to be 83. Even severe upper tract infections may not be associated with fever or leukocytosis (Baldassarre and Kaye, 1991). Therefore it is not recommended to send urine cultures on patients for nonspecific symptoms or chronic urinary symptoms such as incontinence and frequency, nor for asymptomatic patients(ModyandJuthani-Mehta,2014;Nicolle,2002). Sending urine studies in patients with dementia or other impaired mental status (when defining dysuria is difficult) may be of clinical benefit when not responsive to other interventions. If elderly patients experience mental status changes yet no urinary complaints, they should be hydrated then reassessed. Finally, obtaining a culture to document clearance of bacteria is never recommended (Mody and Juthani-Mehta, 2014). A high index of suspicion is warranted when evaluating geriatric patients; therefore diagnosis should rely on the results of a carefully obtained urinalysis and culture. However, counts of 102 or more bacteria are clinically significant in catheterized specimens (Kunin,1987;Nicolleetal. Urinary dipstick testing for leukocyte esterase, nitrites, or both has a different specificity and sensitivity depending on the clinical population. In contrast to young adults, in whom bacteriuria is 30 times more prevalent in women than in men, this ratio in the elderly progressively decreases to 2:1. The prevalence of bacteriuria in the elderly increases with age (Brocklehurst et al. Bacteriuria is present in greater than 20% of healthy community-dwelling women older than 80 years of age and in 6% to 15% of community-dwelling men who are older than 75 years of age (Nicolle,2003). Inastudyof373 women and 150 men older than 68 years of age, 24% of functionally impaired nursing home residents had bacteriuria compared with 12% of healthy domiciliary subjects (Boscia et al. Screening for Bacteriuria Screening for asymptomatic bacteriuria in elderly residents in the community or long-term care facilities is not recommended (Abrutynetal. The treatment of asymptomatic bacteriuria to improve incontinence has not been justified (Baldassarre and Kaye, 1991; Ouslander et al. Although studies have demonstrated decreased survival in bacteriuric patients compared with non-bacteriuric control subjects, it is unclear whether increased mortality rates and bacteriuria are causally related (Abrutyn et al. Age-related changes include a decline in cell-mediated immunity, incomplete bladder emptying, neurogenic bladder dysfunction, increased perineal soiling as a result of fecal and urinary incontinence, increased incidence of urethral catheter placement, and, in women, changes in the vaginal Chapter 55 (Deville et al. These data are linked to the fact that, unlike in younger adults, pyuria and in turn the presence of leukocyte esterase, has been shown to be an inaccurate predictor of bacteriuria in the elderly. Pyuria is common in elderly patients, and pyuria alone is not a good predictor of bacteriuria nor an indication for antimicrobial treatment in the elderly population (Nicolle etal. However, the absence of pyuria was a good predictor of the absence of bacteriuria, and this accounts for the high specificity associated with dipstick testing. Finally, declining functional and mental status in elderly adults, as well as a potentially difficult body habitus, often makes obtaining a true midstream clean-catch urine specimen extremely challenging. In institutionalized elderly patients and those with limited dexterity, a catheterized specimen may be the only way to obtain an uncontaminatedurinespecimen(Nicolle,2002;Nicolleetal. Because urinary tract abnormalities can predispose to and complicate the management and sequela of bacteriuria in the elderly, a thorough urologic evaluation is warranted.
Elder berry (Elderberry). Cefaclor.
- "The flu," also called influenza.
- Cancer, constipation, nerve pain, chronic fatigue syndrome (CFS), hayfever, HIV/AIDS, and other conditions.
- Dosing considerations for Elderberry.
- What is Elderberry?
- What other names is Elderberry known by?
- Are there safety concerns?
- How does Elderberry work?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96444
250mg cefaclor
Overall medications identification buy cefaclor no prescription, the incidence of renal malignancy in dialysis patients is 5 to 50 times greater than in the general population (Ishikawa, 1993; Levine et al. The risk factors for tumor development include male gender, duration of dialysis, and kidney weight, but not type of dialysis. Most tumors (86%) are asymptomatic, and the symptomatic ones are related mostly to bleeding from tumor. Many manifest exclusively as persistent hematuria and are not seen by any available imaging techniques. Nephrectomy is recommended for tumors larger than 3 cm or for smaller ones that are associated with persistent hematuria or rapid growth (Ishikawa, 2000; Truong et al. This disease entity was first described in 1977 in patients receiving hemodialysis; however, it soon became apparent that the disorder is almost as common in patients receiving peritoneal dialysis (Dunhill et al. The prevalence and severity of this disease increase with the duration of azotemia and the subsequent need for dialysis. The incidence increases to 44% within 3 years after initiation of dialysis, to 60% at 5 years after initiation of dialysis, and to greater than 90% if the patient is on dialysis for 10 or more years. A successful renal transplant was previously thought to delay or even reverse the cystic changes, but this is not supported by more recent data (Doublet et al. Histopathology Both kidneys are usually smaller than normal, and the cysts are multiple and bilateral. Bilateral multiple renal cysts and diffuse calcification in enlarged kidneys in a patient undergoing chronic hemodialysis. However, cystic disease was not the cause of the uremia, and the diagnosis of acquired renal cystic disease was made. Infection should be suspected if ultrasonographic examination shows internal echoes or a thickened wall. Cyst puncture can be used to confirm the diagnosis and to identify the infecting microorganism. The cysts are unilocular and contain clear, straw-colored, or gelatinous fluid, with frequent bleeding and/or neoplastic transformation. Most cysts are lined by a single layer of epithelium composed of flat nondescript cells, cells with abundant cytoplasm and hyaline droplets, or small cuboidal cells resembling those from distal tubules or collecting ducts. Cysts usually show secondary changes, including luminal deposition of degenerated blood, hemosiderin, or calcium oxalates (Hughson et al. The nuclei of the epithelial cells in these cases are round and regular, without prominent nucleoli (Hughson et al. However, some cysts (atypical or hyperplastic) are lined by epithelial cells with larger, irregular nuclei that contain prominent nucleoli and may show mitotic activity. Moreover, some hyperplastic cysts have papillary projections, and to some observers the distinction between cyst and neoplasm becomes blurred when papillary hyperplasia predominates. Most renal nodules that are smaller than 1 cm in diameter are adenomas, and most that are larger than 3 cm in diameter are carcinomas. It is believed that atypical hyperplastic epithelium occurs even without cyst formation and that these cells are the precursors of atypical cysts and adenomas (Hughson et al. Therefore the clinician must not ignore the native kidney left in situ during a renal transplantation. Treatment Bleeding episodes are often treated conservatively with bed rest and symptom control. Persistent bleeding and pain, however, may require nephrectomy or renal embolization. If heparinization is associated with hematuria during hemodialysis, peritoneal dialysis may be substituted. Although small renal tumors may metastasize, it is known that those smaller than 3. Although metastases are statistically less likely to occur from small than from large tumors, small tumor size is not a guarantee against metastasis. The benefit of screening in this population continues to be the subject of much debate. It has been proposed that screening be restricted to patients younger than 55 years who have been on dialysis for at least 3 years and are in good general health (Sarasin et al. Ultrasonography usually shows small, hyperechoic kidneys with cysts of various sizes. In contrast, renal cancer in the transplant population behaves aggressively and warrants aggressive evaluation before and after renal transplantation. Passage of a stone through the narrow channel into the calyx may cause pain and hematuria. It is a transitional epithelial-lined, smoothwalled, spheric cavity that communicates with the pelvicalyceal system by a thin channel or neck, typically in the upper or lower pole. It is sometimes known as a pyelogenic cyst, especially if it arises from the renal pelvis. Although some peripelvic cysts are simple cysts that arise from the renal parenchyma and impinge on the renal pelvis, true cysts derived from the renal sinus have no parenchymal cause. Thus the terms parapelvic and peripelvic are terms better used to describe the location of parenchymal cysts, and the term renal sinus cyst more accurately describes all other cysts in the hilum that are not derived from the renal parenchyma but rather from the other structures of the renal sinus, such as arteries, lymphatics, and fat. The predominant type of renal sinus cyst appears to be a result of dilation of lymphatics; however, the mechanism responsible for these changes is not known. Other renal sinus cysts are caused by fluid replacing adipose tissue in the renal sinus as the kidney becomes affected by local vascular disease and atrophy. Patients are usually in their fifth or sixth decades and are almost always asymptomatic. These cysts are usually discovered incidentally in the course of evaluation for other conditions, such as urinary tract infections, nephrolithiasis, hypertension, and prostatism. Ultrasonography will show multiple echo-free areas in the region of the renal sinus. A diagnosis of hydronephrosis is established without question when dilated calyces are seen to communicate with a dilated renal pelvis. On nonenhanced scans, multiple renal sinus cysts resemble a dilated renal pelvis and thus mimic hydronephrosis. Differential diagnosis should include renal sinus lipomatosis (fat density), lymphoma, hemorrhage, and urinoma. Atiyeh B, Husmann D, Baum M: Contralateral renal abnormalities in multicystic-dysplastic kidney disease, J Pediatr 121:65, 1992. Avni E, Thova Y, Lalmand B, et al: Multicystic dysplastic kidney: natural history from in utero diagnosis and postnatal followup, J Urol 138:1420, 1987. Bernstein J: Developmental abnormalities of the renal parenchyma: renal hypoplasia and dysplasia, Pathol Annu 3:213, 1968. Bernstein J: Glomerulocystic kidney disease: nosological considerations, Pediatr Nephrol 7:464, 1993. Cantani A, Bamonte G, Ceccoli D, et al: Familial nephronophthisis: a review and differential diagnosis, Clin Pediatr (Phila) 25:90, 1986. Proceedings of the Tenth Annual Conference of the National Computer Graphics Association. Griffel B, Pewzner S, Berandt M: Unilateral "oligomeganephronia" with agenesis of the contralateral kidney, studied by microdissection, Virchows Arch A Pathol Anat Histopathol 357:179, 1972.
Syndromes
- Increased activity
- Absent or decreased deep tendon reflexes
- Hemoglobin
- Increased pressure in the brain continues or gets worse
- Echocardiogram
- A serious build-up of fluid in people with congestive heart failure, cirrhosis, or kidney disease
- Drug, alcohol, and tobacco abuse
Buy discount cefaclor 500mg line
Vaginal atresia occurs when the urogenital sinus fails to contribute to formation of the lower (distal) portion of the vagina symptoms 10 dpo cheap cefaclor master card. A very shallow dimple caudal to the urethral opening may be appreciated on physical examination. Palpation of a distended vagina on rectal examination may help distinguish this condition from testicular feminization or vaginal agenesis. Surgical correction consists of a transverse incision at the level of the hymenal ring. Dissection is carried out through the fibrous area of the absent lower vagina until the upper vagina is reached. As in treatment of a transverse vaginal septum, distention of the vagina with retained menstrual blood products can prove extremely beneficial in that it acts as a tissue expander. After the obstruction is drained and the vaginal mucosa is identified, a pull-through procedure can be performed to bring the distended vagina down to the introitus. Ramenofsky and Raffensperger (1971) described a combined abdominoperineal approach that can help in exposing and anastomosing the distal vagina to the perineal skin. Vaginal agenesis, which occurs at an incidence of approximately 1 in 5000 live female births, is congenital absence of the proximal portion of the vagina in an otherwise phenotypically. Although Renaldus Columbus is credited by some authors as the first to describe a case of vaginal agenesis, Mayer (1829) was one of the first to report vaginal agenesis in stillborn children (Lesavoy, 1985). In 1838 Rokitansky reported 19 adult autopsy cases of uterovaginal agenesis, including 3 with associated unilateral renal agenesis. This may be caused by improper induction of the sinovaginal bulbs from the neighboring uterovaginal primordium. Chronologically, the uterovaginal canal develops at a point in embryogenesis during which other critical mesodermally derived organ systems are also forming, which in part explains the many associated findings. In contrast to vaginal atresia, the hymenal fringe is usually present, along with a small vaginal pouch, because they are both derived embryologically from the urogenital sinus. This syndrome is in fact second only to gonadal dysgenesis as a cause of primary amenorrhea. A minority of patients have cyclic abdominal pain caused by retention of menstrual fluid in the uterus. Inguinal hernia is less common in this disorder than in complete androgen insensitivity syndrome (Schmid-Tannwald and Hauser, 1973). In approximately 10% of patients, a normal but obstructed uterus or rudimentary uterus with functional endometrium is present (Bates and Wiser, 1985; Murray and Gambrell, 1979; Singh and Devi, 1983). In one of the largest single series, Salvatore and Lodovicci (1978) reported that of 91 patients with vaginal agenesis, almost 25% lacked a uterus, 55% had a solid rudimentary uterus, and the remaining 30% had other abnormalities of this organ. In addition they demonstrated that, although the fallopian tubes were normal in 32% of cases, they were rudimentary in almost 50% and completely absent in 10%. Although occasionally cystic, the ovaries were always present and functional (Salvatori and Ludovicci, 1978). The atypical form (type B) is characterized by asymmetrical uterine buds and/or abnormally developed fallopian tubes. This distinction is important because the overwhelming majority of associated findings and other organ systems have been reported to be present with the atypical form, whereas in the typical form these findings are usually absent (Strubbe et al. The association between vaginal agenesis and developmental abnormalities of the kidney was first recognized by Rokitansky (1838). Approximately one-third of patients were found to have abnormal renal findings on intravenous pyelography or ultrasound examination (Strubbe et al. Renal anomalies are present almost exclusively in patients with the atypical subtype of vaginal agenesis (type B). The authors concluded that progressive perineal dilation should be offered as first-line therapy in adolescents with congenitally absent vagina. Modifications of the Frank technique of perineal pressure have been developed that incorporate the surgical placement of tension sutures to aid in directing pressure from a Plexiglas dilator against the vaginal dimple (Vecchietti, 1979). The mold, often referred to as an "olive," has sutures attached to it that are guided in a cranial direction through the vesicorectal space into the peritoneal cavity and brought out through the abdominal wall (Vecchietti technique). Tension is progressively increased via the abdominal wall sutures until sufficient vaginal length has been achieved. To avoid a formal laparotomy, laparoscopic techniques have been described to assist in dissection of the tissue plane for the Vecchietti technique (Borruto, 1992; Brucker et al. The first landmark advance in vaginal reconstruction is attributed to Abbe in 1898. He described dissecting a canal between the rectum and urethra and lining this area with split-thickness skin grafts. This procedure was later popularized by McIndoe, and the procedure that now bears his name has gained wide acceptance in the United States (McIndoe and Banister, 1938). Preoperative preparation consists of full mechanical and antibiotic bowel preparation. A transverse incision is made at the level of the perineal dimple, and the potential space between the urethra and the rectum is carefully dissected up to the level of the peritoneal reflection. The graft and mold are then inserted into the potential space, and the labia minora are sutured around the stent to prevent extrusion during the initial healing phase (McIndoe, 1950). Many types of vaginal stents have been used for this purpose, including packed gauze, wood covered with a condom, silicone foam, acrylic, various metals, and inflatable vaginal stents (Barutcu and Akguner, 1998; Chen, 1994; Concannon et al. The Foley catheter is replaced by a suprapubic catheter and postoperatively the patient is kept at strict bed rest for 1 full week. A high incidence of postoperative vaginal stenosis necessitates postoperative vaginal dilation (Ingram, 1981). Excellent patient satisfaction has been reported in most large series (Alessandrescu et al. Other options for creation of a neovagina with local tissues include the use of full-thickness skin graft from the buttocks or full-thickness skin flaps based on the labia majora. Those who champion the use of full-thickness skin grafts report a lower incidence of graft contracture than when split-thickness graft techniques are used (Sadove and Horton, 1988). The Williams (1964) vaginoplasty involves a creation of a vaginal pouch from the labia majora. The combination of this procedure and Frank-type dilation along the vaginal access can provide a satisfactory result. The close proximity of the mesonephric and paramesonephric structures during the early phase of fetal development is thought to be the reason for this frequent association of renal anomalies. Not surprisingly, the converse is also true: the incidence of associated genital anomalies in female patients with renal anomalies ranges between 25% and 89% (Thompson and Lynn, 1966). Associated congenital abnormalities of the skeletal system have been described in 10% to 20% of cases (Strubbe et al. Congenital fusion (failure of segmentation) of the cervical vertebrae, known as the Klippel-Feil syndrome, occurs approximately once in 30,000 to 40,000 live births (Gunderson et al. The association between this abnormality of cervical somite development and vaginal agenesis was first recognized by Duncan (1977). Additional, albeit less common, skeletal abnormalities include scoliosis and abnormalities of the hands and face (Fisher et al. Although this does not appear to occur as frequently as in other conditions that affect the female genitalia. Regardless of the method used, it can be very helpful to have the patient speak with someone who has previously undergone treatment before a specific management strategy is initiated (Ingram, 1981). The nonoperative approach, initially popularized by Frank (1938), involves gentle pressure of graduated hard dilators against the perineal surface to create a progressive invagination of the vaginal dimple.
250 mg cefaclor fast delivery
Inset treatment 7th march purchase cefaclor cheap online, Cutaway side view demonstrating close association of the two polar ureters with a common vascular supply. This incision is then continued around the bladder mucosal edge of the ureterocele including the orifice of the lower pole ureter. The bladder mucosal surface is also incised around the edge of the ureterocele to permit complete removal of the ureterocele. Inset, the fully mobilized distal ureterocele is retracted caudally, revealing its narrowing attachment at the bladder neck. Both are brought into the bladder through a newly formed muscular hiatus to provide adequate tunnel length for the ureteral reimplantation. The thinned-out posterior bladder wall is repaired with multiple interrupted sutures to provide adequate muscular backing for the ureters. The bladder mucosa surrounding the ureterocele defect is mobilized to permit covering of the ureters. Right, Final appearance of the ureteral tunnel after completion of the reimplantation. Although this eliminates the need to dissect out the ureterocele and avoids injury to the underlying vagina, it is our impression that this approach has inherent risks that can be avoided by a controlled and predictable surgical approach of trigonal reconstruction. A major problem with marsupialization may be uncommon, but it seems preferable to definitively correct the anatomic and functional defect as certainly as possible on the first open operation when needed. Reported results of ureterocele excision and common sheath reimplantation are very good, although persisting reflux can be an issue in 5% to 10% of patients. Although the clinical significance of this has been called into question, persisting reflux in this context must be viewed with caution. Both proximal and distal approaches may be used, and these have been described with open and laparoscopic techniques. This management technique has become increasingly used, even in nonfunctioning upper poles, as concerns for long-term problems with hypertension have not been substantiated, and the procedure can be completed through a fairly small incision, often no larger than a herniorrhaphy-type incision (Prieto et al. Operative view of robotic ureteroureterostomy for ectopic ureter presenting with incontinence. This can be done at the distal ureter via an inguinal, open approach (Huisman et al. It is critically important in this type of procedure to correctly identify the recipient lower pole ureter, and it is strongly recommended to cystoscopically place a stent into the lower pole ureter at the start of the procedure. Other options to achieve this goal are the proximal anastomotic technique of ureteroureterostomy or pyeloureterostomy (El Ghoneimi et al. Such high anastomoses may be preferable to a distal ureteroureterostomy with a dilated upper pole, because the latter may result in more urinary stasis with a distal anastomosis. Whether the "yo-yo" phenomenon is clinically significant remains uncertain, but we prefer a proximal anastomosis when there is a significant mismatch in ureteral size. A generous longitudinal pyelotomy or ureterotomy is made in the lower recipient pole to overcome such disproportion, and the anastomosis is performed in an end-to-side fashion. The distal portion of the upper pole ureter should be aspirated with a feeding tube to decompress it. If there is no reflux, the resection is taken as distally as possible and the remnant lower portion of ureter may be left open. If reflux is present in an ectopic ureter, it should be taken as close to the bladder neck as possible. If associated with a ureterocele, it may be possible to avoid resection of the ureterocele as long as it is well decompressed. Laparoscopy has also been utilized to aid with performing open ureteroureterostomy to improve ease of procedure and minimize size of incision needed for ureteroureterostomy. A babcock was then used through the small incision through which ureteroureterostomy was to be performed to grasp the ureters from the retroperitoneum and deliver them for the surgery (Grimsby et al. This technique did not increase operative time, and the success of the operation and complication rate was comparable to the traditionally performed procedures. Our preferred method of incising the ureterocele is similar to the one described by Rich et al. Making the incision as distally on the ureterocele and as close Laparoscopic Procedure Both ureteroureterostomy and pyeloureterostomy can be readily performed laparoscopically (Gonzalez, 2007; Steyaert, 2009), which is aided with robotic control (Kutikov et al. Operative times and complication rates were comparable, with slightly shorter length of hospitalization in robotic cases. In the robotic cases, cystoscopy with lower pole stenting was consistently performed, however the type of stent varied because of surgeon preference (Lee et al. This series similarly showed efficacy of the procedure, with 100% resolution of hydronephrosis postoperatively (Biles et al. Extravesical ureteroceles, however, are more likely to have persisting or new reflux and may require secondary surgery based on the presence of reflux in 70% by some series (Chowdhary et al. In the meta-analysis by Byun and Merguerian, the presence of lower pole reflux and the location of the ureterocele are similar in their impact on outcomes (Byun and Merguerian, 2006). These factors did not seem to be additive, to the bladder floor as possible lessens the chance of postoperative reflux into the ureterocele. We favor the latter instrument because it has a finer tip and allows for more precision, and the angle allows for easier manipulation. In older children, the resectoscope with the Collins hot knife may be used to make the incision. Laser incision has been reported with equivalent results (Marr and Skoog, 2002; Jankowski and Palmer, 2006; Ilic et al. The ureterocele should be incised deeply because ureteroceles may be thick walled. For the ectopic ureterocele that extends into the urethra, adequate drainage may be achieved by either a longitudinal incision that extends down from the intravesical portion into the urethral portion or by two separate punctures, one in the intravesical portion of the ureterocele and one in the urethral portion of the ureterocele. In the uninfected well child, no bladder catheter is left in place, and most children are treated as outpatients. Some authors favor puncture instead of incision, but no data are available that demonstrate a clear difference. The incision should be made inferiorly and medially to limit the risk for reflux, but the key goal is decompression. The ureterocele should be incised with the bladder partially filled, but not so much as to efface the ureterocele. Statistical differences are indicated between selected groups based on two-tailed Fisher exact testing. In some series an observational approach has been taken, and resolution has been reported in a few series with variable followup (Jesus et al. The usefulness of observing these patients is dependent on occurrence of infection and parental preferences. Ureterostomy for Ectopic Ureter the ectopic ureter in a neonate with sepsis or with massive dilation may be best managed with a temporary end ureterostomy, although drainage with either endoscopic ureteral incision and stenting or nephrostomy tube is also an option (El Ghoneimi et al. This has the advantage of permitting acute decompression to manage sepsis and permit later assessment of any function in the affected renal unit before definitive management. By performing an end ureterostomy, the ureter can decompress, and it is in position to be reimplanted if the renal unit is felt to be salvageable. No resection of redundant ureter is performed because this will shorten in time, and some length will be needed to perform the reimplantation. The stoma should be positioned at what would be the lateral end of a Pfannenstiel incision. Assessment of functional status is performed shortly before definitive surgery, usually in 4 months or after 6 months of age. If there is no function appreciable, partial or total nephrectomy is performed with removal of the entire ureter to the stoma. Voiding cystourethrogram demonstrating reflux into the upper pole of a duplex system after ureterocele incision. In comparison with an open approach of any modality, however, the simplicity of ureterocele incision coupled with the potential for definitive cure, even if not in a large fraction, is appealing. Summary of Clinical Decision Making For ectopic ureters, clinical decision making is much more straightforward than for ureteroceles and rests on whether to maintain the upper pole of a duplex system.
Buy cefaclor 500mg visa
Osman Y medicine used for adhd order cefaclor without a prescription, El-Tabey N, Mohsen T, et al: Nonoperative treatment of isolated posttraumatic intraperitoneal bladder rupture in children-is it justified It is present in 40% of patients with advanced stage disease but in only 5% to 10% of children with low-stage disease (Brodeur et al. These findings have been so striking that neuroblastoma was the first tumor in which the intensity of chemotherapy for a patient was determined not only by the stage and histology of the tumor but also by its "biologic markers," which were primarily chromosomal (Matthay et al. Deletion of the short arm of chromosome 1 (1p) is found in 25% to 35% of neuroblastomas and is an adverse prognostic marker (Brodeur et al. The deletions are of various lengths, but, in a series of eight cases, a consensus deletion included the segment 1p36. This deletion is present in 70% of advanced stage neuroblastoma, and it has been demonstrated to be an independent prognostic factor (Attiyeh et al. There have been reports of constitutional abnormalities involving the short arm of chromosome 1 (Laureys et al. An additional genetic abnormality, gain of one to three copies of 17q, often the result of translocation with chromosomes 1 or 11, has been demonstrated to correlate with more aggressive tumors (Bown et al. The break points vary, but the addition of a region from 17q22-qter is common, suggesting that genes replicated in this region provide an advantage (Schleiermacher et al. Unfortunately, more than half of the children are seen initially with metastatic disease. Neuroblastoma is known to arise from cells of the neural crest that form the adrenal medulla and sympathetic ganglia. Tumors may occur anywhere along the sympathetic chain within the neck, thorax, retroperitoneum, or pelvis or in the adrenal gland: 75% arise in the retroperitoneum, 50% in the adrenal, and 25% in the paravertebral ganglia. The variety of locations where these tumors arise and the spectrum of their differentiation result in a wide range of clinical presentations and behaviors (Brodeur, 1991). These tumors can undergo spontaneous regression (Brodeur, 1991), differentiate to benign neoplasms, or exhibit extremely malignant behavior. Biologic factors have been defined that predict and explain much of the variance in behavior between tumors. Epidemiology and Genetics Incidence Neuroblastoma accounts for 8% to 10% of all childhood cancers. Genetics There have been a number of familial cases reported that are postulated to represent an autosomal dominant pattern of inheritance (Knudson and Strong, 1972; Robertson et al. Although the median age at diagnosis of neuroblastoma is 19 months, in familial cases it is 9 months (Kushner et al. At least 20% of patients with familial neuroblastoma have bilateral adrenal or multifocal primary tumors, which are unusual in spontaneous cases. The risk for development of neuroblastoma in a sibling or offspring of a patient with neuroblastoma is less than 6% (Kushner et al. Linkage analysis in seven families with two or more first-degree relatives affected with neuroblastoma identified a single interval at chromosome 16p12-13 with consistent linkage (Maris et al. This suggested that a hereditary neuroblastoma predisposition gene may be located at this site and may explain the familial cases. Constitutional Chromosome Abnormalities Numerous karyotypic abnormalities have been found in neuroblastoma, and these are recognized to have prognostic significance. These Embryology and Spontaneous Regression In 1963 Beckwith and Perrin coined the term in situ neuroblastoma for small nodules of neuroblasts found incidentally within the adrenal gland that are histologically indistinguishable from neuroblastoma. This revised system has been demonstrated to add independent prognostic information beyond the contribution of age that is one of the factors contained in the system (Sano et al. Ganglioneuroma is a histologically benign, fully differentiated counterpart of neuroblastoma. It is unclear whether ganglioneuroma arises de novo or by maturation of a preexisting neuroblastoma or ganglioneuroblastoma. Metastatic lesions from neuroblastoma have been observed to develop the histology of mature ganglioneuroma, supporting the latter theory (Hayes et al. One of its important aspects is determining whether the tumor is stroma poor or stroma rich. Patients with stroma-poor tumors with unfavorable histopathologic features have a very poor prognosis (less than 10% survival) (Shimada et al. Stroma-rich tumors can be separated into three subgroups: nodular, intermixed, and well differentiated. Tumors in the latter two categories more closely resemble ganglioneuroblastoma or immature ganglioneuroma and carry a higher rate of survival. When compared with other clinical features, these histologic patterns were independently predictive of outcome (Shimada et al. In contrast to neuroblastomas, ganglioneuromas are most often diagnosed in older children and are usually located in the posterior mediastinum and retroperitoneum, with only a small number arising in the adrenal glands (Enzinger and Weiss, 1988). Ganglioneuromas often grow to a very large size before they cause symptoms as a result of compression of adjacent structures or extension into the spinal canal (Benjamin et al. Because survival is not influenced by extent of resection, it should be used only in those patients in whom significant symptoms are present, and aggressive attempts at resection should be avoided (DeBernardi et al. In situ neuroblastoma was found during postmortem examination in 1 of 224 infants younger than 3 months. This represents an incidence of approximately 40 to 45 times greater than that of clinical tumors, suggesting that these small tumors regress spontaneously in most cases. Subsequent studies have shown that these nodules of neuroblasts are found in all fetuses studied and generally regress (Ikeda et al. The concept of in situ neuroblastoma has been used to support the argument that many neuroblastomas arise and regress spontaneously. This concept has been further supported by population-based studies in Quebec province and in Japan, where prospective screening of infants for neuroblastoma has been performed based on urinary catecholamine excretion. An increased number of children were identified with low-stage neuroblastoma, a higher frequency than present clinically, but resection of those tumors did not result in a decrease in the incidence of advanced-stage tumors seen at an older age (Hayashi et al. A subsequent German Neuroblastoma Screening Study postponed screening until 10 to 19 months of age. Fewer early stage cases were identified, and a greater frequency of patients with unfavorable clinical and biologic features were identified, but there was no decrease in the mortality of these patients (Schilling et al. Evaluation of adrenal tumors resected in the neonatal period, whether cystic or solid, showed that in most, the "biologic markers" were favorable (Kozakewich et al. The highly favorable outcome of infants diagnosed with neuroblastoma in the population screening studies led to attempts at expectant observation.