100 mg kamagra polo free shipping
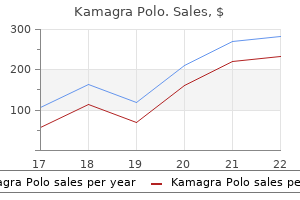
After multiple modes of atrial pacing protocols erectile dysfunction diagnosis code purchase 100 mg kamagra polo with amex, successful conversion to sinus was finally accomplished with eight beats of a 280-ms drive cycle length, followed by three extrastimuli (190-ms intervals each). A bipolar system has the advantages of more reproducible and reliable atrial electrograms. The baseline wanders less, and the atrial electrograms are more distinct and the ventricular electrograms less prominent, which makes the recordings more distinguishable. Note that the prominent ventricular electrogram and the wandering baseline in the unipolar recording are eliminated in the bipolar recording. The stimulator system requires capability for a long pulse width (10 ms) and high current (10 to 25 mA) (40,42,43). Several investigators have shown that pulse widths greater than the standard 2 ms for intracardiac pacing are necessary to overcome high impedance and to penetrate the esophagus to reach the atrial (paraseptal) myocardium, particularly in noninfants. Although reports of pulse width duration for successful transesophageal atrial pacing have included low values of 2 ms, atrial pacing is most consistent and reproducible at 6 to 10 ms and current of 10 to 15 mA. Delivery of stimulus current >15 mA (at a constant pulse width of 10 ms) is associated with patient discomfort (40,42,43). Therefore, for patients with high thresholds, discomfort can be minimized by increasing the pulse width, limiting the current threshold with a goal of <15 mA. Transesophageal atrial pacing is most successful and best tolerated when performed at stimulator outputs 20% above threshold. Some investigators use a constant pulse width of 10 ms and vary the stimulus current to obtain a threshold. With either technique, transesophageal atrial pacing can be accomplished successfully in >90% of pediatric patients using presently available transesophageal electrode catheters without discomfort at relatively low stimulator outputs (less than twice threshold) of <10-ms pulse width and 15-mA stimulus current. Ventricular transesophageal pacing has been accomplished in adults by stimulating at high outputs currents ranging from 20 to 30 mA with a pulse width of 40 ms and by using a specially designed flexible lead passed into the stomach (44,45). The pacing protocols for transesophageal pacing are limited, on a practical basis, to atrial pacing. Premature atrial extrastimulation technique (during sinus and/or eight-beat drive of a-paced rhythm) 4. One or more of the following: Short bursts of a-pacing, continuous atrial decremental a-pacing, premature atrial extrastimulation technique (using one or more drive cycle lengths and one to three extrastimuli) b. Premature atrial extrastimulus technique to determine the antegrade effective refractory of the accessory pathway b. The major differences relate to the esophageal technique being applied primarily for supraventricular arrhythmias, whereas intracardiac studies are applicable to both supraventricular and ventricular arrhythmias. Complications Complications of transesophageal studies are infrequent and predominantly inconsequential (40,49,50). Mechanical or anatomic problems such as undetected obstructions or mucosal trauma, or placement in a bronchus can arise during passage of the catheter through the nares and pharynx. However, with excessively high outputs, or prolonged pacing times in small infants, esophageal damage can occur. Ventricular arrhythmias may be induced from inadvertent ventricular pacing or from rapidly conducting atrial-paced beats (49,51,52). Objectives of Diagnostic Electrophysiologic Studies and Comparison of Intracardiac and Transesophageal Techniques One or more of the objectives listed in Table 21. The potential for intracardiac and transesophageal techniques to achieve the objectives listed in Table 21. In this manner, when presented with an individual patient with a specific diagnostic or therapeutic problem, either the intracardiac or transesophageal technique (or both) can be chosen. Although the intracardiac technique may be superior in accomplishing virtually all of the clinical objectives, limitations in terms of cost, higher risk, and application in small infants may dominate in specific situations, making the transesophageal technique the best choice for the individual patient. The inability to effectively routinely pace the ventricle is the major limitation to the transesophageal technique. Therefore, when the objectives that optimally involve ventricular pacing are analyzed, P. Determine efficacy/safety and optimal mode of antitachycardia pacemaker therapy 12. When catheter access is a problem, the transesophageal catheter can provide additional and/or optional atrial recording/pacing site. Finally, a transesophageal catheter makes an excellent reference electrode for spatial or electrical purposes when doing 3-D mapping with an impedance-based system, because it is both close to the heart and can be fixed in place with tape at the nares. However, despite these changes, several questions regarding the early and late implications of catheter therapy in small children whose myocardial development is still underway remain unanswered (58,59). The Decision to Ablate: Safety Versus Efficacy One overriding theme in the management of arrhythmias in children compared to adults is an emphasis on safety over efficacy. Myocardial (65) and potentially severe coronary injury (66,67,68,69) are more likely with ablation in this age group than in older patients. In children over the age of 4 years with symptomatic arrhythmias, the balance between risks and benefits clearly shifts toward ablation therapy, but generally only if the ablation can be performed safely (73). This leads to the recommendation that such patients undergo risk stratification and those who are at high risk be offered catheter ablation as a therapeutic option (76). Other age-dependent differences in management decisions will be addressed when discussing individual arrhythmias below. Energy Sources Various energy sources have been used for ablation of myocardial tissue. Although many of the techniques rely on the generation of heat to destroy tissue, alternate mechanisms include chemically induced cell death, application of high-current densities to disrupt intracellular membranes, and cooling to first reversibly silence cells followed by freezing to burst them. Cell death appears to occur almost immediately, suggesting that cell death is the result of both protein denaturation and dehydration. Haines and Watson (56) demonstrated that the lesion size grows exponentially with time, with a half-time of about 18 seconds. As noted above, chronic lesions in adult dogs appear to be well demarcated histologically and are approximately the same size as the acute lesions (87). However, in 1994 we reported that chronic atrial and ventricular lesions produced in immature (approximately 1 month old) sheep may increase in size during the subsequent 6 to 8 months of normal development (65). First, lesions can be too large, creating unintentional damage to structures, such as coronary arteries; second, cooling will reduce lesion size when maximum power is already being delivered with a noncooled ablation tip. The time constant (time required to reach 63% of the ultimate asymptotic lesion size of 79 mm3) was 22 seconds. Lesion volume appeared to grow linearly as a function of electrode tip temperature. Previous data in adult animals had shown linear increase in width and depth with tip temperature. Cryotherapy Catheter-based cryotherapy was approved for use in the United States in 2003 for ablation of a variety of cardiac arrhythmias (96,97,98,99,100,101,102,103). Both of these effects appear to be much less likely or absent with cryoablation (113). It should be noted that in the United States due to regulatory issues, the only cryocatheter commercially available for ice mapping has a 4-mm tip. This feature has dramatically enhanced the safety profile in clinical trials to date. One potential advantage might be the simultaneous use of diagnostic ultrasound to monitor lesion production (135). Finally, chemical ablation achieved by delivering a toxic agent such as alcohol into the coronary artery or vein supplying the myocardium responsible for P. Summary: Energy Sources Several energy types are available currently for use in catheter ablation procedures. Procedure: General Preablation Prior to the ablation procedure, standard electrophysiologic techniques should be used to identify the tachycardia mechanism and the location of the arrhythmia substrate.
Diseases
- Gitelman syndrome
- CDG syndrome type 1A
- AIDS dementia complex
- Pulmonary disease, chronic obstructive
- Berger disease
- Chromosome 4 short arm deletion
- Laryngeal abductor paralysis mental retardation
- Gastroesophageal reflux
- Pinta
Discount 100mg kamagra polo with amex
The sheaths are withdrawn off the balloons and the balloons are simultaneously inflated erectile dysfunction girlfriend buy discount kamagra polo 100 mg on line. Again, longer balloons (5 to 6 cm in older children and adolescents) help to stabilize during inflation. As with any interventional catheterization, these patients require anticoagulation with heparin. However, the total experience is limited, and the duration of the relief of the obstruction is unpredictable. Overall 5-year survival was 69% while patients at the later stages of the institutional experience had a 5-year survival of 87%. The tricuspid valve is approached by passing one or two guidewires across the valve, either into the pulmonary artery or to the right ventricular apex. When the balloons are positioned across the stenotic valve, they are inflated simultaneously. Experience with tricuspid valve dilation is limited; but, on the basis of even limited experience and minimal risk, this procedure is offered to the appropriate patients before considering surgery for tricuspid stenosis. Transcatheter Management of Coarctation, Re-Coarctation, and Aortic Arch Obstructions Dilation of peripheral arteries was the first therapeutic catheterization procedure and represents yet another area in which the vascular radiologist introduced the techniques. Dotter and Judkins (1) reported on the dilation of atherosclerotic peripheral arteries at the same time that Rashkind and colleagues were working on the atrial septostomy catheter. The technique for dilation of vessel stenosis uses small, cylindrical, fixed maximal diameter dilating balloons passed over a spring guidewire, positioned across the area of stenosis, and inflated with relatively high pressures. This balloon technique is not only used to treat recurrent or native coarctation of the aorta, but similarly is used for branch pulmonary artery stenoses as well as central and peripheral venous stenoses. In 1979, Sos first experimented with balloon angioplasty of native coarctation in postmortem specimens (90) and this was followed by some fundamental work by Dr. He performed balloon angioplasty on excised human coarctation segments as well as experimentally induced coarctation in lambs (91,92). These intimal injuries appeared to have healed completely on late pathologic examination, leaving the ballooned segment with a normal looking intima. The studies also documented that a balloon diameter of less than twice the size of the coarctation segment was unlikely to achieve a successful dilation, while diameters greater than three times appeared to carry a higher risk of deep and extensive tears. In animal experiments, they implanted Palmaz P308, 188 and 108 stents in the abdominal aorta and documented that stents can be safely redilated P. While one should generally avoid endovascular stent therapy in small infants, in some very rare circumstances the implantation of a low-profile stent in very sick infants may be justifiable, even though one has to accept that these low-profile stents are not expandable to adult size and therefore will eventually require surgical removal. Coarctation with 30 mm Hg peak systolic gradient incidentally found during procedure. A 15-year-old child with a history of coarctation repair (end-to-end) during infancy. One of the major difficulties when comparing the various treatment modalities for native or recurrent coarctation of the aorta, such as surgery, balloon angioplasty, and endovascular stenting, is the fundamental lack of prospective, evidencebased data (98). As such, one has to rely on institutional series (98), the results of which are necessarily influenced by not only the skill of the individual interventional cardiologist and cardiac surgeon in the respective institution, but also by the common institutional policy and experience in treating these lesions. Similar to the comparison of surgical and interventional approaches to coarctation, the decision between balloon angioplasty and primary stenting is often dependent on the individual institutional policy, rather than being guided by evidence-based data. While both balloon angioplasty and endovascular stenting have an important role to play in the primary management of aortic coarctation, there are a number of valid reasons that make primary stenting the more suitable treatment modality, if the size of the patient permits this procedure: Firstly, the results of balloon angioplasty are limited due to elastic recoil of the coarcted segment and the rigidity of an endovascular stent obviously overcomes this problem. Secondly, the degree of trauma to the aortic vessel wall plays an important factor in the potential development of complications such as aneurysm formation. While balloon angioplasty often requires a degree of overexpansion of the coarctation and adjacent vessel wall to achieve a maintainable result, endovascular stenting allows having a successful result while dilating the vessel wall only to the desired diameter-overexpansion is not required. Finally, a subgroup of longer-segment coarctation or arch hypoplasia typically has a poorer outcome after balloon angioplasty alone. Even though primary endovascular stenting offers significant benefits, it is usually avoided in small children and infants, because of the potential for injury to the arterial vessels and access sites as well as the higher likelihood of developing in-stent stenosis when stents are only expanded to fairly small diameters. The goal of the procedure is to achieve reduction in the gradient to less than 10 mm Hg or a 90% or greater relief of the obstruction angiographically. In an observational study, Zabal and colleagues analyzed a cohort of 54 consecutive adult patients who underwent transcatheter treatment for coarctation with the primary endpoint being a composite index of failure, made up of heart-related death, a gradient on follow-up of more than 20 mm Hg, the need for reintervention or complications such as aneurysm formation (99). Upon sheath removal injury to right iliac artery which was treated through implantation of a covered Atrium Cast stent. With the present techniques and equipment, dilation and/or stent implantation for native or recurrent coarctation appears to be successful in achieving immediate relief on the obstruction in more than 90% of cases. However, the cumulative composite procedural success decreased to 86% at intermediate follow-up (3 to 18 months) and 77% at long-term follow-up (>18 months). However, balloon angioplasty alone for native coarctation in smaller children and infants has lower long-term success rates and the results are frequently not well maintained, with up to 66% recoarctation rate. An additional concern when discussing transcatheter interventions for native coarctation is the potentially greater incidence of aortic aneurysm formation in the area of the coarctation dilation. However, the follow-up data is limited, and the long-term outcome is uncertain, at best. Another concern with these aneurysms, particularly following an otherwise successful dilation, is that if subsequent surgery is necessary, it could be more hazardous because of the disappearance of collaterals following a hemodynamically successful dilation. As more follow-up information is gathered regarding dilation of native coarctation, this technique appears more reasonable for discrete lesions in patients over 7 to 12 months of age (102). It has been suggested that gradual conservative expansion of these stents be performed over two or three procedures, especially in tight lesions, to reduce the incidence of dissection or aneurysm formation. A "J" or curved-tip stiff guidewire is positioned retrograde through the coarctation, around the aortic arch, and into the aortic root or occasionally into the right innominate artery. The dilation balloon catheter is passed over the wire and across the area of coarctation. In smaller children and infants, cutting balloon angioplasty frequently adds an additional treatment alternative in patients where endovascular stent placement should be avoided. In the slightly larger patient, when the results of the dilation are not satisfactory and where larger sheaths can be introduced into the arteries, intravascular stents can be used to support the dilated segment of aorta. When stents are used, it is imperative that only stents that eventually can be dilated to the full diameter of the adult descending aorta are used. For example, limiting factors in younger children when considering endovascular stent therapy, are the potential for injury to the arterial vessels and access sites due to the need for larger-sized hemostatic sheaths as well as the higher likelihood of developing in-stent stenosis when stents are only expanded to fairly small diameters. The goal of the interventional procedure in adults is similar to children: To achieve reduction in the gradient to less than 10 mm Hg or a 90% or greater relief of the obstruction angiographically. It has been advocated that the risk of catastrophic aortic injury during or after balloon angioplasty and/or stent placement in the adult (106,107,108) is higher than what would be expected in the younger child, especially when treating primary coarctation. Many adult patients with systemic and exercise-induced hypertension, may present with "just" a 20 to 30 mm Hg upper-to-lower limb blood pressure gradient with an angiographic discrepancy between coarcted segment and the aorta at the diaphragm of not more than 30% to 50%. To achieve an adequate result with balloon angioplasty alone, one would ideally have to expand the area to at least twice the size of the coarctation segment (91,92). However, using this as a guide would lead to significant overdilation of not only the coarcted segment, but also the adjacent "healthy" aorta. Primary stent therapy is therefore the treatment of choice in adults with primary or recurrent coarctation, as it not only avoids the need for overexpansion, but also has a lower risk of recurrence when compared to balloon angioplasty. A 34-year-old pregnant woman hospitalized during her 24th week gestation with severe systemic hypertension. Fluoroscopy time was minimized and appropriate radiation protection measure were taken. This not only identifies areas with medial and intimal disruption as could relate from a previous attempt at balloon angioplasty, but it also allows to clearly define the extension of the abnormal vessel wall, thereby allowing to choose a stent that is of sufficient length to cover the full length of the abnormal vasculature. Some institutions advocate pre-expansion of the coarcted segment as a means of testing aortic wall compliance prior to stent implantation. However, this has the disadvantage of potentially extending a intimal-medial tar into healthy vasculature that subsequently may not be covered during stent placement, therefore potentially acting as a "nidus" for aneurysm formation, especially at the areas immediately adjacent to the placed stent. In adults with very "tight" coarctation, it may be beneficial to expand the aorta not to the full intended diameter in a single procedure, but instead adopting a staged approach where the stent is dilated over two or three sessions up to its desired final diameter, thereby allowing the aorta to heal in between interventional procedures, with a reduced risk of catastrophic aortic wall injury. However, even with a very careful and considerate approach, the risks of treating adult coarctation cannot be fully eliminated and therefore whenever possible, the availability of an approved covered stent variety as a primary or rescue intervention could potentially enhance the safety of these procedures. Covered stents have also been successfully used to exclude aortic aneurysms at the site of (re)coarctation.
100mg kamagra polo fast delivery
In some studies impotence 18 year old order kamagra polo 100mg fast delivery, the posteromedial papillary muscle has been similarly affected (33). There may be diffuse endocardial fibroelastosis of the left ventricle, and the anterior mitral valve leaflet is often thickened. Thinning and scarring of the anterolateral left ventricular wall and apex owing to infarction are noted, and there are often mural thrombi. The heart is usually enlarged, but not as much as in infants, and there is usually no endocardial fibroelastosis. However, there is usually scarring and calcification of the anterolateral papillary muscle and occasionally even of the adjacent left ventricle (18,34). The infant appeared at first to be in obvious distress, as indicated by short expiratory grunts, followed immediately by marked pallor and cold sweat with a general appearance of severe shock. It seems probable that in this infant the curious attacks of paroxysmal discomfort. If this is true, it represents the earliest age at which this condition has been recorded. Older children and adults may be asymptomatic or may have dyspnea, syncope, or angina pectoris on effort. However, typical myocardial infarctions or congestive heart failure is rare in adults. In infants, the heart is usually enlarged, the left ventricle being the predominant ventricle affected. The first heart sound may be soft or absent (if there is mitral regurgitation), and apical gallop rhythms are common. There may be no murmurs, or the murmur of mitral regurgitation, or at times a soft continuous murmur at the upper left sternal border that is similar to the murmur of a small patent ductus arteriosus, which is due to the continuous flow from the anomalous coronary artery into the pulmonary artery. There also may be abnormal R waves or Rwave progression in the left precordial leads. Although this pattern is not pathognomonic for this anomaly (it is seen in myocardial infarcts from other causes or occasionally in cardiomyopathies), if found, the diagnosis of this anomaly should be considered and evaluated by other means. Even in asymptomatic adults, the resting electrocardiogram is abnormal, and abnormal ischemic responses occur with exercise (34). Noninvasive Imaging On the chest film in affected infants there is marked cardiomegaly, predominantly of the left atrium and ventricle, and evidence of pulmonary edema. These features are similar to those of many forms of cardiomyopathy, with which this anomaly is often confused. However, this finding is not specific because it has been seen in cardiomyopathies as well. Echocardiography with Doppler color flow mapping has replaced cardiac catheterization as the standard method of diagnosis (36). The improved resolution of current echocardiographic equipment often allows the abnormal aortic origin of the left coronary artery to be seen. Color Doppler interrogation shows that flow passes from the coronary artery into the pulmonary artery. Therefore, even if the origin of the coronary artery to the aorta is not well defined by two-dimensional imaging, the presence of diastolic flow in the pulmonary artery will be informative. An enlarged right coronary artery should also raise the suspicion of the diagnosis. Echocardiography also will show the size and function of the cardiac chambers, particularly the left ventricle, as well as regional left ventricular wall motion abnormalities and mitral regurgitation. There may be increased echogenicity of the papillary muscle and adjacent endocardium due to fibrosis and fibroelastosis. Computed tomography scans have shown their high resolution in defining coronary artery anatomy and origination in most patients older than infancy. The main advantage of this technique is rapid acquisition times and high resolution. There remains a degree of radiation exposure with this technique, but its ability to define coronary artery abnormalities is excellent. Cardiac Catheterization and Angiography Although previously cardiac catheterization and angiography were commonly used in the diagnosis of congenital coronary abnormalities, currently they are used only if the results of noninvasive imaging are indeterminate. In symptomatic infants, diagnostic cardiac catheterization demonstrates a low cardiac output and high filling pressures, and usually some degree of pulmonary hypertension. In asymptomatic older patients, output and pressures are usually normal except for a slight increase in left ventricular end-diastolic pressure. There may be a left-to-right shunt at the pulmonary arterial level, but because the shunt may be small, its absence does not rule out the diagnosis. Aortic root angiography will show the dilated right coronary artery and, if there are large collaterals, will show filling of the left coronary artery and passage of contrast material from the left coronary to the main pulmonary artery. Attempts at selective left coronary artery angiography will only show filling of the left sinus of Valsalva without opacification of the left coronary artery. Usually selective right coronary artery angiography is diagnostic in showing filing of the left coronary artery via collaterals, with backfilling to its pulmonary ostia (see Video 32. Although pulmonary arterial angiography may show reflux of contrast medium into the origin of the left coronary artery, neither this nor left ventriculography can reliably make the diagnosis. Natural History Of all children born with this rare anomaly, approximately 87% present in infancy (33) and of these, 65% to 85% die before 1 year of age from intractable congestive heart failure (37), usually after 2 months of age. Treatment the first effective surgical treatment was ligation of the left coronary artery at its origin from the pulmonary artery to prevent the steal. Most older children benefit from this procedure, especially if they have extensive coronaryto-pulmonary arterial shunting, but late sudden death can still occur (34,39). Ligation of the origin of the left coronary artery and revascularization via an internal mammary arterial or saphenous venous graft has been successful (40,41), although graft thrombosis and stenosis has occurred, to a much greater degree with vein grafts. Grafts using the internal mammary artery have a longer survival and are preferred when coronary reimplantation cannot be done. Direct reimplantation of the origin of the left coronary artery into the aorta (with a button of pulmonary artery around the origin) has been proven successful and is considered the standard approach in many centers (42,43,44,45). An alternative approach is the Takeuchi procedure, in which an aortopulmonary window is created and then a tunnel fashioned that directs blood from the aorta to the left coronary ostium (46). In the past it was recommended that, because surgical mortality is high in the sickest infants, surgery should be delayed until after 18 to 24 months of age (47). Coronary Artery Fistulae Coronary fistulae are persistent and abnormal connection between the coronary artery and one of the cardiac chambers or pulmonary arteries. In the modern era of high-resolution ultrasound imaging, they are frequently discovered incidentally and if small, pose no significant burden to the patient. However, less commonly they may be large and impose a significant hemodynamic burden or future risk for cardiovascular events (Video 32. Embryologic Development Coronary artery fistulae connecting to the intracardiac chambers are likely the sequelae of incomplete reabsorption of myocardial trabeculations as they connect to the nascent coronary arteries. It has been hypothesized that fistulae connecting to the pulmonary artery may be a consequence of the failure of involution of the aortopulmonary anlage (50). Pathophysiology There are three pathophysiologic consequences of a significant coronary fistula: 1. Distal coronary insufficiency While the presence of any of these findings warrants intervention, it is also clear that coronary fistula may develop significance over time. Some small- to moderate-sized coronary fistulae have demonstrated the capacity to grow over time, while other small ones remain trivial. It is not clear what the risk factors are for development of pathologic significance in such small fistulae. Imaging Most commonly, small coronary fistulae are picked up on echocardiography as a small shunt seen in diastole from the myocardium to a low-pressure right-sided chamber. In these cases, left-sided chambers are of normal dimensions indicating that the degree of shunting is small. It is unusual for there to be an audible murmur associated with small coronary fistulae. Large coronary fistulae may be initially diagnosed following a referral for an abnormal murmur, which may be continuous. The surface echocardiogram may demonstrate dilatation of left-sided chambers, and depending on where the fistula enters the right heart, the right-sided chambers as well. In such large fistulae, the proximal coronary anatomy on the side of the fistula is markedly dilated and may be seen by echocardiography (Video 32. In the older patient, cardiac computed tomography usually provides excellent delineation of the location and anatomy of the large fistula, albeit at a significant radiation dose.
Discount 100 mg kamagra polo visa
Total anomalous pulmonary venous connection: report of 93 autopsied cases with emphasis on diagnostic and surgical considerations impotence ring order generic kamagra polo canada. Total anomalous pulmonary venous connection: morphology and outcome from an international population-based study. Partial and total anomalous pulmonary venous connection in the fetus: two-dimensional and Doppler echocardiographic findings. Cross sectional echocardiographic diagnosis of total anomalous pulmonary venous connection. Infant total anomalous pulmonary venous connection: factors influencing timing of presentation and operative outcome. A proposed pathogenesis of cor triatriatum: impingement of the left superior vena cava on the developing left atrium. Congenital stenosis of individual pulmonary veins: clinical spectrum and unsuccessful treatment by transvenous balloon dilation. The spectrum of systemic venous anomalies varies widely from minor asymptomatic anatomic variations to complex abnormalities that can lead to cyanosis or that might complicate surgical repair of congenital heart disease. Clinically significant abnormalities of the systemic veins are infrequent when visceroatrial situs is lateralized (either situs solitus or situs inversus). In contrast, the incidence of systemic venous anomalies in patients with heterotaxy syndrome exceeds 90% (1,2). Embryology There are three basic venous systems in the human embryo: (a) the cardinal veins and their tributaries, which form the superior and inferior caval systems; (b) the umbilical, vitelline, and omphalomesenteric veins, which carry the blood from the placenta, yolk sac, and intestine; and (c) the pulmonary veins, which return the blood from the lungs. The age of human embryos cannot be estimated reliably on the basis of their length, which may vary greatly (3), or on the number of somites, which are visible for only a limited time. In 1942, therefore, Streeter (4) proposed classifying human embryos into 25 age groups, or horizons, each representing 2 days of embryonic life. Normal Development of the Cardinal and Umbilicovitelline Venous Systems the sinus venosus, that is, the cavity into which all veins eventually drain, develops by enlargement of the confluence of the umbilical veins and joins the atrial segment of the heart through a slit-like opening, the sinoatrial foramen. It will connect with the sinus venosus through the right hepatocardiac channel, which drains into the right horn of the sinus venosus and with the yolk sac via the left omphalomesenteric vein. They drain blood from the fused neural folds that form the central nervous system. They join the anterior cardinals to form the right and left common cardinals (ducts of Cuvier) and drain together with the umbilical and vitelline veins into the right and left horns of the sinus venosus. As the transverse segment of the sinus venosus shifts rightward, it pulls the left horn of the sinus venosus along the posterior atrioventricular groove. The left horn of the sinus venosus and the adjacent part of the common cardinal vein receive the cardiac veins and form the coronary sinus. The mode of formation of the coronary sinus is responsible for the following anatomic P. The ventricular part of the heart is removed at the atrioventricular junction (A-V Jct. The venous blood then flows into the right atrium through the sinoatrial foramen (Sino-Atr. The orifice of a normally formed coronary sinus is always in the anatomically right atrium. The posterior cardinal veins appear first, shortly after the establishment of the anterior cardinal veins. The subcardinal veins are a new venous plexus, which initiates the diversion of the venous P. They are established along the ventromedial borders of the mesonephroi medial and ventral to the posterior cardinals. As the mesonephroi increase in size and bulge toward the midline, the subcardinals are brought closer together. In the mid-mesonephric region, they establish communications with each other by several small vessels, which become confluent to form intersubcardinal anastomoses and eventually a large medial venous space, the subcardinal sinus. When the subcardinal sinus is established, the small vessels that connect the subcardinals with the posterior cardinals drain medially into the subcardinal sinus rather than laterally toward the posterior cardinals. Vessels arising independent of these three systems are indicated by small crosses. As the embryo grows, the blood volume that enters the subcardinal sinus increases and stimulates development of a new unpaired venous channel. At this stage, the posterior cardinals have involuted to the level of the common cardinals proximally and the iliac veins distally. These veins connect the subcardinal sinus with the cephalic remnant of the posterior cardinals via the azygos and hemiazygos veins. By the seventh week of gestation, venous channels have been established to connect the left side with the right side of the paired veins. The development of the connecting channels is followed by partial involution of the left side of the paired veins. Four of these five venous systems begin as bilateral venous channels, a fact that P. A: Based on conditions in pig embryos of 3 to 4 mm, applicable to human embryos of fourth week. C: Based on conditions in pig embryos of 8 to 9 mm, applicable to human embryos of sixth week; (*, inferior vena cava. C: Double cava at lumbar level owing to persistent supracardinal veins on both sides. The umbilical stream tends to pass by way of these vessels into the liver, and the early direct connections of the umbilical veins with the sinus venosus involute. As the embryo grows and the volume of the umbilical venous blood increases, a new large channel is created through the liver substance, the ductus venosus, which connects the left umbilical vein with the right hepatic veins. After birth, the ductus venosus becomes the ligamentum venosum and the left umbilical vein becomes the ligamentum teres (round ligament of liver). It is formed by the suprarenal segment of the right supracardinal vein and the cephalic remnant of the right posterior cardinal vein. It runs up medial to the thoracic vertebrae, to the right of the aorta and the thoracic duct, and receives the lower 10 right intercostal veins. It then turns to the right behind the aorta and the thoracic duct to terminate into the azygos vein. The left upper hemiazygos varies inversely with the size of the left superior intercostal vein. It receives the left intercostal veins that did not drain into the left superior intercostal vein and the lower hemiazygos and terminates in the right azygos or the lower hemiazygos. As the omphalomesenteric veins approach the heart, they lie adjacent to the developing liver. The mesenteric part persists and grows to match the length and complexity of the growing intestine (6). By the sixth week of gestation, the paired mesenteric veins have formed anastomoses with each other. A week later, the left mesenteric vein involutes cephalad to the anastomosis, while the right mesenteric vein involutes caudal to the anastomosis. It descends in front of the aortic arch and the left pulmonary vessels and, after receiving the left superior intercostal vein, it penetrates the pericardium. When this anomaly accompanies other congenital cardiac malformations, it may pose diagnostic and technical difficulties during catheterization and cardiac surgery (16). The coronary sinus can be imaged from the subcostal, apical, and parasternal windows. The left superior intercostal vein is a small systemic vein that can be followed toward the anterior chest wall. Typically, it is associated with severe left atrial outlet obstruction, such as mitral stenosis or atresia with a restrictive patent foramen ovale or an intact atrial septum, and provides an alternative egress for pulmonary venous blood (21). In patients with a normal septum primum and septum secundum, the orifice of the unroofed coronary sinus will function as an interatrial communication. In a study of 58 postmortem cases of visceral heterotaxy with asplenia, the incidence was 67%, and in 46 postmortem cases of polysplenia, the incidence was 13% (1). The reason for the high frequency of an unroofed coronary sinus in asplenia is not P. They are at risk for complications of right-to-left shunting, including paradoxical emboli, brain abscess, strokes, and death. In some patients, the coronary sinus ostium is atretic and there is no significant interatrial communication. The frontal axis of the P wave may be abnormal in patients with heterotaxy syndrome, reflecting a left sinoatrial node or an ectopic atrial rhythm.
Oenanthe aquatica (Water Fennel). Kamagra Polo.
- How does Water Fennel work?
- Are there safety concerns?
- Coughs, intestinal gas, water retention, and other conditions.
- What is Water Fennel?
- Dosing considerations for Water Fennel.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96078
Generic kamagra polo 100 mg online
Histologic patterns described on histology include monocytic infiltrates ved erectile dysfunction treatment purchase 100 mg kamagra polo free shipping, fibrinopurulent exudates, granuloma formation, chronic nodular dermatitis, microabscess formation, and coccobacillary organisms; the presence of granules has been described in disseminated cases. However, in the lymphocutaneous form, the differential diagnosis can be approached more systematically. The sporotrichoid pattern should be differentiated from the more acute ulceroglandular syndrome, as is seen in tularemia and cat-scratch disease (Box 185-2). However, the disease has the potential to disseminate; sternal wound infections may be complicated with osteomyelitis. The importance of direct microscopic examination for the presence of granules cannot be overemphasized. Organisms are detected as Gram-positive, branched filamentous "hyphae," and branching at right angles is diagnostic. Extended treatment for extracutaneous nocardiosis, with parenteral therapy followed by an oral regimen is necessary. Surgery is indicated in cases of abscesses (drainage) or extensive necrosis (debridement). Spontaneous resolution or good clinical response despite inappropriate therapy has been seen in children with Nocardia cellulitis or lymphadenitis. The current standard for sensitivity testing is by the broth microdilution method. In more severe cases or disease involving other organs, a combination of sulfonamide with a second agent is recommended. Immunosuppression is a good indication for a two-drug regimen, including amikacin; 88% cure rate has been reported when this drug is used. The disease has a worldwide distribution but it is more frequent in the tropics, especially in India, Sudan, Somalia, Mexico, and Venezuela. Actinomycetoma affect mainly men, but frequency before 15 years of age is similar in both sexes. These findings suggest that the increase or deficiency of a determined immunoglobulin class, as well as the relationship between different subclasses, play a role in the pathogenesis of actinomycetoma. Walking barefooted or wearing sandals may be considered a risk factor for these infections in rural communities. In women, mycetomas increase in size during pregnancy and spontaneously improve after delivery. Atypical clinical forms include the cryptic mycetoma (without sinus tracts), the so-called mini-mycetoma (single or multiple small lesions observed mainly in children and adolescents), and the occasional inguinal "metastatic" lesions from a primary mycetoma of the foot. Clinical specimens should be sent for direct examination (Gram stain) and culture. The cell block technique of mycetoma aspirates can be use for cytodiagnosis, showing findings similar to histopathologic sections. An enzyme-linked immunosorbent assay has been described for the diagnosis of mycetoma due to N. An additional advantage of this particular assay might be its demonstrated cross-reactivity with N. Botryomycosis is a condition that can mimic actinomycetoma and eumycetoma, both clinically and histologically. The cutaneous form accounts for 75% of the cases; visceral involvement, mainly the lung, is rare. The disease is characterized by localized areas of infiltration, with mass effect and draining sinuses. Botryomycosis is also characterized by the presence of granules, which can be seen macroscopically and microscopically. As in mycetoma, the center of the granule will show agglomeration of the causal agent, most commonly, Gram-positive cocci. Economic considerations may influence the choice of therapy, particularly in developing countries. Molecular identification of the causal agents and development of genetic markers for disease can improve management. Cure may be defined by a lack of clinical activity, absence of grains and negative cultures. Treatment periods are very long, especially with bone and visceral involvement, for which prognosis is poor. Some resistant cases have been treated with amoxicillin, 500 mg, plus clavulanic acid, 125 mg/day for 5 months. Amikacin alone or combined with imipenem are powerful antibiotics used as alternative treatments for severe or multiresistant mycetomas, especially those with bone and visceral involvement. In adults, amikacin is administered 15 mg/kg/day (500 mg intramuscularly twice a day) for 3 weeks; ototoxicity and nephrotoxicity may develop. They have demonstrated good in vitro and in vivo activity against Nocardia asteroides complex, good in vitro sensitivity against A. Linezolid, a new oxazolidinone, has shown in vitro antimicrobial activity against N. The use of clindamycin, ciprofloxacin, and moxifloxacin has been suggested in Nocardia infections. Amputation is not indicated in actinomycetoma because the very low risk of lymphangitic or hematogenous dissemination. Functional impairment is common with osseous, pulmonary, or abdominal visceral involvement. Ameen M et al: Efficacy of imipenem therapy for Nocardia actinomycetomas refractory to sulfonamides. Long-term morbidity: despite curative antibacterial treatment, one-quarter to onethird of patients will have a debilitating and permanent neurological deficit. A clinical challenge: diverse manifestations result from a granulomatous spectrum, and are further increased by superimposed, reactional states. An immunologic opportunity: an exemplary model for the understanding of cellmediated immunity in humans. The bacillary cell wall consists of a peptidoglycan backbone linked to arabinogalactan and mycolic acids. Immunogenic proteins are associated with the cell wall, and also are present in the cytoplasm. Phenolic glycolipid I is a major, species specific and immunogenic constituent of the highly nonpolar outer layer of the bacillus. A twin study has provided compelling evidence that both genetic and environmental factors are important in determining disease susceptibility and expression. Ridley and his associates provided the most detailed description of the granulomatous spectrum of leprosy,28,29 integrating both clinical and histologic changes. The classification is determined primarily by clinical and histologic changes, bacillary numbers being a secondary consideration. Patients along the clinical spectrum of leprosy are presumed to be manifestations of evolving immune responses, which, based on environmental and genetic factors, will eventually gravitate toward one of the two poles. The central red dots are the sequelae or "footprints" of testing for pinprick perception when it is absent. Typically, the lesion is firmly indurated, elevated, erythematous, scaly, dry, hairless, and hypopigmented. In both groups, immunity is sufficient to affect cure, thus, placing an upper limit of 10 cm on lesion size, but antibiotic therapy is recommended.
Generic 100 mg kamagra polo overnight delivery
The cervical lymph nodes are sometimes enlarged impotence young men kamagra polo 100 mg fast delivery, tender, and tethered to the overlying skin; they rarely suppurate. Other systemic sites of involvement include the spleen, intestines, lungs, and liver. Differential diagnosis includes tuberculosis, leishmaniasis, and other deep mycoses. They show numbers of round yeasts with a characteristic form of multiple budding in which a parent cell is surrounded by large numbers of smaller buds. The organism is dimorphic and produces a cottony mycelial-phase growth on primary isolation at room temperature. Serology is very helpful in confirming the diagnosis, the main tests being the immunodiffusion assay and a complement-fixation test. Paracoccidioidomycosis has been reported from most Latin American countries, but the infection is found most commonly in parts of Brazil, Colombia, and Argentina. The infection does not occur in the United States, although it has been reported in Mexico. Exposure rates can be estimated by skin test reactivity and appear to be equal in both males and females, although the prevalence tions are known to occur in bamboo rats of the genus Cannomys, which are large burrowing rodents. The infection affects otherwise healthy individuals as well as those with immune defects and is most common after the rainy season. There are also antigen-detection tests useful in monitoring patients with disseminated disease. The organisms can be seen with special fungal stains such as methenamine silver (Grocott modification). In tissue, the characteristic budding pattern can be seen, although it may be necessary to search several fields to find the most typical structures. In widespread infections, masses of small yeast forms may be mistaken for Histoplasma. There has been no work to demonstrate that there is a subclinical form of Penicillium infection, even though this is likely. Other organs, including the liver, gastrointestinal tract, spleen, and bone marrow, may be affected. Biopsy and, when necessary, culture will distinguish between the different causes. There is no commercial serologic test as yet, although antigen detection systems and polymerase chain reaction have both been used in diagnosis, the latter for identification of cultures. Although the main portal of entry is through inhalation into the lungs, the disease usually presents with signs of extrapulmonary dissemination such as meningitis. Cutaneous lesions can develop as a result of dissemination or, rarely, through inoculation. Relapses can occur, and, where possible, patients should be reviewed periodically after primary therapy. In very extensive infections and in severely ill patients, such as those with the progressive disseminated type of infection, intravenous amphotericin B may be necessary. It is inhaled via the lungs, and it is not known whether there is a primary cutaneous form of the infection. Infections are confined to Southeast Asia, particularly Thailand, South China, and Vietnam. However, there are reports in other Asian countries, including Northeast India, and imported cases are seen in Europe and the United States. Cryptococcosis has a worldwide distribution although exposure rates probably differ markedly in different countries. Clinically the main differences to be seen are those between the neoformans and gattii varieties. However, the most common clinical manifestation of disease is meningoencephalitis. This presents with classic signs of meningismus, changes in consciousness, mental changes, and nerve palsies. Chest signs include the appearance of nodular shadows, cavitation, and pleural effusion. In otherwise healthy patients or those with sarcoidosis, lesions may be solitary, and in such patients, they may be the only clinical manifestation of infection. In primary cutaneous cryptococcosis with direct inoculation of organisms into the skin, the skin lesions are usually solitary nodules that break down and ulcerate. The term primary cutaneous cryptococcosis is also used loosely to describe solitary lesions of cryptococcosis, but in many such cases there is also evidence of dissemination to other internal organs. It is important to investigate all patients who present with cutaneous lesions for evidence of dissemination to other sites. Multiple, discrete, skin-colored papules, and nodules resembling molluscum contagiosum are seen on the face of a male with advanced human immunodeficiency virus disease. It is important to biopsy and culture suspicious lesions in immunocompromised patients. Various biochemical features, such as the production of urease and the ability to pigment on Guizotia seed medium, are characteristic: or molecular probes can be used to confirm the identity Serologic tests are rapid and specific. In tissue sections, the large pleomorphic yeasts stimulate either a granulomatous reaction or very little inflammation. The capsules of the cells can be stained using the mucicarmine or Alcian blue stains. In patients with single skin lesions and no other signs of infection, alternatives such as fluconazole or itraconazole can be used. When they occur, their presence may be very helpful because it is possible to biopsy easily accessible lesions in order to establish the diagnosis. These fungi cause disease in patients with poorly controlled diabetes, neutropenia, or renal disease. Direct invasion through abrasions has been reported following trauma due to a natural disaster. Mucormycosis also has been caused by close apposition of the skin with contaminated dressing materials in the case of R. Infections may respond to intravenous amphotericin, and recent results with lipid-associated amphotericin B formulations have been encouraging. The best known of these organisms are Aspergillus, Scedosporium, Trichosporon, and Fusarium. Skin infection is seen mainly in severely immunocompromised patients such as those with neutropenia. Aspergillus may produce large necrotic lesions such as ecthyma gangrenosum, but smaller papules and cold abscesses also can occur. Skin lesions may occur particularly in two situations: (1) in neutropenic patients, there is often a severe disseminated disease with widespread skin nodules and associated muscle pains,62 and (2) in intravenous drug abusers, candidiasis may present with a follicular, pustular rash in the beard area and scalp. Other lesions include retinal and vitreal deposits and abscesses around the costochondral junctions. Resistance to some azole drugs, such as fluconazole and ketoconazole, is more common with certain non-albicans Candida sp. Laboratory confirmation of the diagnosis is fraught with difficulties chiefly because many of the organisms are also commensals in human sites; because they occur in severely ill patients, the capacity to produce diagnostic antibody titers is compromised. The interpretation of laboratory data is consequently difficult and has to be related to the clinical state of the patient. Ideally, a histologic diagnosis should be made, although biopsy may be impossible because of the risk of bleeding. In many cases, the diagnosis of a systemic mycosis is presumptive, and treatment therefore is given empirically. Draining sinuses communicate from the center of the abscess to the skin or mucosal surface.
Buy genuine kamagra polo on-line
As an alternative to diagnostic cardiac catheterization with its associated risks and higher cost 4 erectile dysfunction drugs buy order kamagra polo uk. The 1H protons can be thought of as tiny bar magnets that, when placed in a strong magnetic field, will align and precess (rotate) around the axis of the magnetic field. The most common approach to compensate for cardiac motion is to synchronize or "gate" image acquisition with the cardiac cycle. Blurring due to respiratory motion can be avoided either by having the patient hold his breath for periods of 5 to 10 seconds during data acquisition, or by synchronizing image data acquisition to the respiratory as well as to the cardiac cycle. Real-time imaging may be particularly useful when a patient has an irregular rhythm and to evaluate respiratory-related variations in blood flow and septal position (9). Accordingly, the need for performing the examination under sedation or anesthesia and an assessment of the risk/benefit ratio for proceeding under these circumstances should be determined well before the examination date. Parents should be provided with a detailed description of the examination and asked to discuss it with their child in an age-appropriate manner in advance to increase the likelihood of a successful study. Although it is possible to wait for young children to fall into a natural sleep using a "feed and swaddle" approach, this method may be time consuming and complicated by early awakening. Its principal drawbacks are an unprotected airway and reliance on spontaneous respiratory effort with the associated risks of aspiration, airway obstruction, and hypoventilation. This motion artifact can be reduced by synchronizing image data acquisition to the respiratory cycle tracked by either a bellows device around the abdomen or by navigator echoes that concurrently image the position of the diaphragm or heart. The principal limitations of both these strategies are prolonged scan times and incomplete elimination of respiratory motion that can lead to reduced image quality. This approach, described in detail elsewhere (2,15), is safe, consistently achieves adequate sedation, protects the airway, and offers control of ventilation. Respiratory motion artifact can be completely eliminated by suspending ventilation in conjunction with neuromuscular blockade. Breath-hold periods of 30 to 60 seconds are typically well tolerated, and allow multiple locations to be scanned efficiently. When utilizing either sedation or anesthesia, it is important that both the nurses and physicians have sufficient experience with these procedures in children with cardiovascular disorders. To maximize patient safety and examination quality, it is recommended that different healthcare providers be responsible for supervising the imaging and sedation/anesthesia aspects of the study, and that both communicate closely with each other. Once inside the scanner, the protons are aligned with the direction of the static xmagnetic field (B0). B: Over several heartbeats, a series of images spanning the cardiac cycle is reconstructed and viewed in cine loop mode. Top: the navigator beam is positioned over the right hemidiaphragm and includes lung and liver tissues. Bottom: the motion of the right hemidiaphragm is continuously displayed along with the acceptance window (horizontal lines). Only data acquired when the position of the right hemidiaphragm is registered within the acceptance window are used for image reconstruction. Following safety screening, physiologic monitoring devices and hearing protection (for both awake and anesthetized patients) are put in place. The signal should be checked both when the patient is outside and then inside the scanner bore. Because young children dissipate body heat faster than adults, the scanner room temperature should be adjusted and prewarmed blankets applied to minimize heat loss. The imaging coil should be chosen to maximize the signal-to-noise ratio over the entire body region to be examined. Adult head or knee coils are often appropriate for infants weighing less than 10 kg, and adult cardiac coil for medium-sized children weighing between 10 and 40 kg. More recently, multichannel coils designed specifically for cardiovascular imaging in infants and young children have become commercially available. Safety Standard clinical imaging scanners present no known hazards to biologic materials. Animal studies evaluating the influence of static magnetic fields have not demonstrated significant biologic effects for fields of up to 2 T (19). Subsequent investigations found that patients with renal failure were at risk for developing this rare but severe complication (26,27). Consequently, most institutions have adopted a policy to avoid using Gd contrast in patients with impaired renal function (28). Fortunately, surgical clips and sternotomy wires implanted in the chest and abdomen are typically only weakly ferromagnetic. These body weights are approximates and other considerations are taken into account when selecting a coil for an individual patient. Reliance on standardized protocols and postexamination review alone in these patients may result in incomplete or even erroneous interpretation. In practice, the anatomy in question is often assessed by more than one imaging sequence, yielding overlapping information that increases diagnostic confidence. In clinical practice, such inhomogeneities are mostly owing to ferromagnetic implants such as sternal wires, prosthetic heart valves, stents, coils, or other implants. As a result, image acquisition can be completed during 10 to 15 seconds of breath holding. The sequence is repeated N2-D times, each with a different phaseencoding value, until all lines of k-space are collected and a 2-D image is reconstructed. The signal from stationary or relatively slow-moving tissues (such as the myocardium) is gray because the spins within the selected slice have reduced signal intensity. An important feature of gradient echo sequences is high imaging speed, which allows reconstruction of multiple images during the cardiac cycle that can be displayed in cine loop format. A: T1-weighted image showing a slightly hyperintense globular tumor (arrow); B: T2-weighted image showing the tumor is markedly hyperintense, consistent with a vascular tumor. The brightness of a given tissue in this case is determined primarily by the ratio of T2-to-T1 relaxation times which results in high contrast between the blood pool (T2/T1 = 360 ms/1,200 ms = 0. The motion of the diaphragm is tracked with a navigator pulse and image data are accepted only when the position of the diaphragm lies within a narrow window defined by the operator. The volume elements (voxels) of the image dataset are typically isotropic, which allows offline reformatting of the image volume in any arbitrary plane. Examples of common clinical applications include imaging of the aorta and its branches, pulmonary arteries, pulmonary veins, systemic veins, aortopulmonary and venous-venous collateral vessels, systemic-to-pulmonary artery shunts, conduits, and vascular grafts (11,46). Although this technique is mostly used for imaging of extracardiac anatomy, we have also found it useful in the evaluation of intraatrial systemic and pulmonary baffles. However, given the trade-offs between spatial and temporal resolutions, the clinical utility of this imaging technique awaits further study. The patient is instructed to hold his/her breath and imaging acquisition is initiated. The time delay between start of contrast injection and data acquisition is determined either by a magnetic resonance fluoroscopic method P. A modest decrease in spatial and temporal resolutions will lower the acquisition time to 4 to 5 seconds while producing diagnostically acceptable images. Patients are instructed to hold their breath at end-expiration to minimize variations in the position of the diaphragm and, consequently, the heart. Two-chamber plane (also known as vertical long-axis plane): A slice is prescribed parallel to the plane of the interventricular septum based on previously obtained scout images in the axial P. This acquisition accounts for the orientation of the ventricles in the transverse plane of the chest. A: Subvolume maximal intensity projection; B: 3-D volume rendering (posterior view). Four-chamber plane (also known as horizontal long-axis plane): A stack of slices (usually four) is prescribed from an end-diastolic image of a slice acquired perpendicular the previous two-chamber cine sequence. In most patients, 12 slices will cover the ventricles from base-to-apex with adjustment of slice thickness between 4 and 8 mm and the interslice spacing from 0 to 2 mm.
Generic kamagra polo 100 mg amex
Factors associated with C after cardiopulmonary bypass in children with congenital heart disease erectile dysfunction what causes it cheap kamagra polo 100 mg on-line. Temporal and anatomic risk profile of brain injury with neonatal repair of congenital heart defects. Vancomycin-Associated Acute Kidney Injury in Pediatric Cardiac Intensive Care Patients. The association of renal dysfunction and the use of aprotinin in patients undergoing congenital cardiac surgery requiring cardiopulmonary bypass. Postoperative prophylactic peritoneal dialysis in neonates and infants after complex congenital cardiac surgery. Effects of ultrafiltration and peritoneal dialysis on proinflammatory cytokines during cardiopulmonary bypass surgery in newborns and infants. Abnormalities of intestinal rotation in patients with congenital heart disease and the heterotaxy syndrome. Outcomes after the Ladd procedure in patients with heterotaxy syndrome, congenital heart disease, and intestinal malrotation. Octreotide treatment of chylothorax in pediatric patients following cardiothoracic surgery. Glycemic profile in infants who have undergone the arterial switch operation: hyperglycemia is not associated with adverse events. Intraoperative hyperglycemia during infant cardiac surgery is not associated with adverse neurodevelopmental outcomes at 1, 4, and 8 years. Comparison of the effectiveness and safety of two insulin infusion protocols in the management of hyperglycemia in critically ill children. Tight glycemic control after pediatric cardiac surgery in high-risk patient populations: a secondary analysis of the safe pediatric euglycemia after cardiac surgery trial. Risk factors for central line-associated bloodstream infection in a pediatric cardiac intensive care unit. Utility of clinical biomarkers to predict central line associated bloodstream infections after congenital heart surgery. Serum cortisol and early postoperative outcome after stage-1 palliation for hypoplastic left heart syndrome. A randomized, double-blind, placebo-controlled pilot trial of triiodothyronine in neonatal heart surgery. Advances in recognition, resuscitation, and stabilization of the critically ill child. Morbidity and mortality after surgery for congenital cardiac disease in the infant born with low weight. Improving the outcome of high-risk neonates with hypoplastic left heart syndrome: hybrid procedure or conventional surgical palliation Prolonged treatment with prostaglandin in an infant born with extremely low weight. Gestational age at birth and outcomes after neonatal cardiac surgery: an analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Despite optimization of standard medical therapy, some children with chronic heart failure will deteriorate clinically to a point that they require hospitalization for inpatient monitoring and treatment with intravenous therapies. Once the condition is recognized, the fundamental therapeutic goals are the same when managing patients with this very challenging clinical syndrome: reverse hemodynamic derangements, correct metabolic abnormalities, and provide symptomatic relief. Achievement of these goals requires individualized care and a familiarity with the risks and benefits of particular therapies. Treatment options for decompensated heart failure are limited and almost all are untested in children. Most of the data relied upon for managing patients with advanced heart failure have been derived from studies in adults, the majority of whom have an ischemic etiology for their myocardial dysfunction. Because data are lacking for the treatment of advanced heart failure in children, we must heed the findings of adult trials, reflect on reliable anecdotal experience, and respect the principle that we should first do no harm when we venture to care for this vulnerable population. Frequently, patients will require a combination of diuretic and intravenous afterload reduction. Patients with decompensated heart failure and reduced blood pressure with normal or low systemic vascular resistance may not benefit from vasodilators and should therefore be considered for inotropic therapy. In these patients, inotropic agents may be necessary to maintain circulatory function, relieve symptoms and improve end-organ function. For example, pediatric patients in systemic ventricular failure have a much higher incidence of concomitant right ventricular failure and pulmonary hypertension. The etiology of right heart failure in children may be similar to that which is seen in the adult experience, secondary to left heart failure, but may also be attributed to intrinsic or anatomic causes. One must consider how the patient can be cannulated, not only in regard to what vessels or chambers to use, but how the cannulae, which at times are on opposite sides than normal. Further consideration of the internal cardiac anatomy with respect to septal defects, hypoplastic chambers, anomalous systemic and venous connections, and extracardiac anatomy. The identification and management of systemic-to-pulmonary shunts, both surgically created. They found that 77% survived to transplant, 5% gained sufficient myocardial recovery to be weaned from support, and 17% died while supported. The strategy is to support the myocardium through the acute process to achieve sufficient recovery to allow for device removal. Acute viral myocarditis, transplant graft rejection, and postcardiotomy shock are examples of potentially recoverable causes of myocardial injury. Unfortunately, late survival for this cohort was poor, with a 1-year mortality rate of 50%. The authors have successfully supported patients with viral myocarditis in their institution, with a survival rate of 80% (15). This therapy was initially described by del Nido and colleagues, and many in our field have championed its use (16,17,18). Novel approaches such as these have resulted in more than 60% of cardiac arrest patients surviving to hospital discharge. Contraindications to Mechanical Circulatory Support Although it is important to consider each patient individually, extreme prematurity, very low birth weight (<1. Other considerations are multisystem organ failure, sepsis, and severe lung disease, although successful support has been demonstrated in all of these scenarios (22,23). That being said, appropriate timing for institution of support is particularly challenging in this group because it is often governed by which devices are available for supporting pediatric patients and institutional experience. Careful consideration must be given to cases on an individual basis prior to committing to long-term support as our surgical and postoperative management experience with these patients and devices is still in its infancy. Our institutional experience has found that among children who are hospitalized with decompensated heart failure, worsening renal function, as defined as a rise in serum creatinine by 0. Patients who are considered acceptable transplant candidates and who have demonstrated inotrope dependency are monitored closely for end-organ injury. Profile 3: Stable but inotrope dependent Patient with stable blood pressure, organ function, nutrition, and symptoms on continuous intravenous inotropic support (or a temporary circulatory support device or both), but demonstrating repeated failure to wean from support due to recurrent symptomatic hypotension or renal dysfunction "Dependent stability. More intensive management and surveillance strategies should be considered, which may in some cases reveal poor compliance that would compromise outcomes with any therapy. Patients are comfortable at rest without congestive symptoms, but may have underlying refractory elevated volume status, often with renal dysfunction. Profile 6: Exertion limited Patient without evidence of fluid overload is comfortable at rest, and with activities of daily living and minor activities outside the home but fatigues after the first few minutes of any meaningful activity. Attribution to cardiac limitation requires careful measurement of peak oxygen consumption, in some cases with hemodynamic monitoring to confirm severity of cardiac impairment. Variable urgency, depends upon maintenance of nutrition, organ function, and activity. Variable, depends upon maintenance of nutrition, organ function, and activity level. Recurrent ventricular tachyarrhythmias that have recently contributed substantially to clinical compromise. This is of increased importance because of longer waiting duration on the transplant list in the recent era. A fundamental question regarding device selection would be therefore if the patient needs pulmonary support. The lack of an oxygenator and the simpler circuit configuration invoke less inflammation which results in a lower level of anticoagulation requirement.
Purchase kamagra polo once a day
Left pulmonary artery slings are rare and thought to develop because the left postbranchial component of the pulmonary artery failed to connect to the left sixth aortic arch erectile dysfunction drugs class purchase kamagra polo paypal, and instead connected to the right sixth aortic arch via the right postbranchial component of the pulmonary artery. Thus, the left pulmonary artery courses from the right pulmonary artery, between the trachea and esophagus to the left side (139). Right pulmonary artery slings are extremely rare, and thought only to occur in the presence of left bronchial isomerism (140). In one study, of 59 patients presenting with symptomatic great arterial anomalies over a 20-year period, 10% had anomalous left pulmonary artery origins (7). Of known cases, a male predominance has been reported, with a male to female ratio of 3:2 (138). Associated Congenital Heart Disease Left pulmonary artery slings have been reported in association with ventricular septal defects, atrial septal defects, persistent left superior vena cava, persistent arterial duct, and tetralogy of Fallot (141,142). There is an increased incidence of imperforate anus in patients with type 2 pulmonary slings, with 14% of patients with a type 2 pulmonary sling affected in one study (135). Esophageal atresia and other gastrointestinal disorders have also been reported (141,143,144,145). Clinical Manifestations the major clinical concern of left pulmonary artery slings is the respiratory symptoms related to the tracheal compression by the pulmonary artery, and abnormal development of the bronchial tree. Type 2 left pulmonary artery slings are especially problematic as they are associated with hypoplasia of the right lung and worse tracheobronchial stenosis (135). Symptoms include stridor, pneumonia, respiratory distress, and respiratory failure. A large review of patients with a pulmonary vascular sling found that 90% presented in infancy (138). Symptoms include dyspnea, wheeze, stridor, cyanosis, apnea, and respiratory failure (138,146). Some patients are asymptomatic initially, with the diagnosis made incidentally (143,146), or they present in adolescence or adulthood, with patients reported to present with wheeze, hemoptysis, dyspnea, cough, or choking sensation (146,147,148). There may also be hyperinflation of the lung secondary to obstructive emphysema, usually affecting the right lung, but it may be bilateral or left sided (138). On barium esophagram, pulmonary slings cause anterior indentation, due to the pulmonary artery coursing between the esophagus and trachea, unlike vascular rings, which are associated with posterior and lateral indentation (138). However, barium esophagram has a low sensitivity, missing more than 20% of cases in one series (138). While bronchoscopy can identify the presence of tracheal rings, it is unable to evaluate the distal bronchi due to the stenosis. Also, bronchoscopy is invasive and not without risk as it can cause edema and worsen any respiratory distress already present (136). However, it often requires sedation, which may not be advisable in a patient experiencing respiratory symptoms (136). Computational fluid dynamics analysis has been proposed to evaluate the effect of the tracheobronchial stenosis on the airway, though the clinical utility remains to be seen (149). Echocardiograms can diagnose the pulmonary sling, but are unable to assess the bronchial anatomy. They are an important part of the workup, however, to assess for any associated intracardiac disease (139). Management and Outcome Pulmonary artery slings carry significant morbidity and mortality. In one review, 7 of 27 patients died, 4 preoperatively and 3 after tracheoplasty (136). Surgical management includes anastomosis of the left pulmonary artery to the pulmonary trunk and tracheoplasty (136). One approach to tracheal stenosis is slide tracheoplasty, where the trachea is transected at the level of the stenosis, a vertical P. In a recent study of 18 patients with tracheal stenosis, 8 due to pulmonary sling, 1 died postoperatively, 2 patients required reoperation for recurrent tracheal stenosis, 2 required tracheostomy for tracheomalacia, and 13 were asymptomatic (150). For patients with long segments of stenosis, tracheoplasty including use of a pericardial patch and costal cartilage has been advocated, with some success but with a high rate of complications including infection and patch dehiscence (151). Postoperative pulmonary stenosis is also a known concern, with 74% of patients developing pulmonary artery stenosis, of whom 45% required at least one reintervention (153). Anomalous Origin of the Left or Right Pulmonary Artery from Aorta Anomalous origin of either the right or left pulmonary artery from the ascending aorta is rare malformation, with the former being more common. These lesions should be differentiated from discontinuous pulmonary arteries, where one of the branches is supplied by an arterial duct (154). The lesion has been called hemitruncus, though this is a misnomer because there are two semilunar valves, rather than the common truncal valve necessary to diagnose common arterial trunk (154). There is frequently associated intracardiac disease, most commonly a ventricular septal defect which may exacerbate the problem (154). The anomalous pulmonary artery acts as a very large aortopulmonary collateral, shunting much of the oxygenated blood back to the lungs and creating a volume load to the left heart. It also exposes the pulmonary vascular bed to systemic arterial pressures, resulting in severe pulmonary vascular obstructive disease if uncorrected (154). Patients may present with tachypnea, failure to gain weight appropriately, respiratory distress, and congestive heart failure (154,155). Surgical treatment includes reimplantation of the pulmonary artery to the pulmonary trunk. Outcome after early intervention is reported to be good, though surgical or percutaneous reintervention to address aortic or pulmonary stenosis is not uncommon (154). Brachiocephalic Artery Compression of the Trachea Rarely, the brachiocephalic artery may arise more posteriorly than normal, and course anterior to the trachea, thereby compressing the trachea. However, some may present in infancy or childhood with symptoms of apnea, chronic cough, respiratory infection, dyspnea, stridor, or wheeze. In addition to tracheal compression due to an anomalous brachiocephalic artery, anatomically normal brachiocephalic arteries are known to cause tracheal compression and secondary respiratory distress in patients with neurologic impairment. Surgical treatment includes aortopexy and tracheal reconstruction as indicated by symptoms (158,159). In one series, infants and children undergoing aortopexy for tracheal compression by the brachiocephalic artery had improved or resolved symptoms at follow-up (159). Interrupted Aortic Arch Anatomy and Embryology the term interrupted aortic arch refers to the presence of discontinuity anywhere along the aortic arch. The lesion is frequently classified according to the system established by Celoria and Patton (160). In type A, the interruption occurs at the aortic isthmus, between the most distal subclavian artery (usually the left subclavian artery) and the descending aorta, proximal to insertion of the arterial duct. In type B, the interruption occurs between the common carotid artery and the subclavian artery (usually the left common carotid artery and left subclavian artery). In type C, the interruption occurs between the brachiocephalic artery and the common carotid artery. The arch is nearly always left sided, with a right aortic arch being reported only rarely (161,162), all of which were type B and associated with DiGeorge syndrome (161,163). In a series of patients reviewed by Van Mierop and Kutsche (164), all patients with type A had an atretic connection between the distal transverse arch and the proximal descending aorta. Also, the distal subclavian artery was proximal to the interruption, indicating that the interruption occurred late in development, after the subclavian artery had migrated from the proximal descending aorta to the distal transverse arch (164,165). In light of this, and of the similar rates of associated cardiac lesions, Van Mierop proposed that interrupted aortic arch type A has a similar etiology as coarctation of the aorta, while other types of interruption have a separate causation. Type B interruption of the aortic arch is thought to occur because of inappropriate regression of the left fourth aortic arch, thereby disconnecting the proximal transverse aorta from the distal transverse aorta between the left common carotid and left subclavian arteries. If the right fourth aortic arch also inappropriately regressed and the right dorsal aorta inappropriately remained, then the right seventh intersegmental artery (future right subclavian artery) will arise anomalously from the proximal descending aorta, a common finding in interrupted aortic arch type B (164). Van Mierop therefore hypothesized that decreased flow to the aortic arch contributes to the interruption. Genetics 22q11 deletion (DiGeorge syndrome) has been reported in 50% to 80% of patients with interrupted aortic arch type B (10,12,166,167,168). It is more common in isolated interrupted aortic arch type B than in cases that are associated with other heart diseases (170). In one series, 43% of patients with 22q11 deletion had interrupted aortic arch (167). It is thought that 22q11 deletion is associated with a disruption of neural crest cell migration required for aortic arch development (167). Though rare, familial cases of interrupted aortic arch type B have been reported in the absence of known associated syndromes (171,172).