Purchase lotrisone online pills
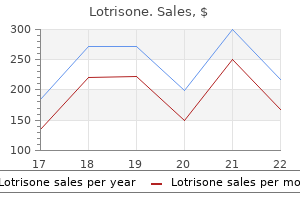
On the other hand antifungal essential oils list 10 mg lotrisone for sale, special populations such as patients with trisomy 21, cyanotic heart disease, and those on antiplatelet therapy may require additional specific testing. An increased hematocrit in a normovolemic child gives an indication of the magnitude and chronicity of hypoxemia. A hematocrit more than 60% may predispose to capillary sludging and secondary end organ damage, including stroke. Echo-Doppler imaging is especially helpful for defining intracardiac abnormalities. The ability to interpret anatomy and physiology accurately requires a skilled echocardiographer, reaffirming the need for a well-integrated interactive team. Although the complexities posed by extreme anatomic variation and changing loading conditions render intraoperative echo-Doppler challenging even for experienced echocardiographers, the pediatric cardiac anesthesiologist should develop some familiarity with its capabilities and limitations so as to participate in critical intraoperative management decisions. It may be an alternative to cardiac catheterization in select patients and may provide noninvasive assessment of coronary anomalies, myocardial perfusion defects, and the detection of conditions associated with myocardial scarring. However, with advances in technology such as respiratory gating and use of free-breathing protocols, images can be acquired with the patient spontaneously breathing. This eliminates the need for general anesthesia with an endotracheal tube and breath-holds, thus allowing for intravenous sedation with spontaneous breathing instead. Although many anatomic questions can now be reliably answered noninvasively, catheterization remains a vital tool for cases that present complex anatomic questions or require knowledge of physiologic data. Acquired or congenital anatomic variants that might have an impact on planned vascular access or surgery Careful review of the cardiac catheterization data and an understanding of their potential impact on the operative and anesthetic plan are essential. Not all medical problems can be evaluated and corrected preoperatively; the surgeon, cardiologist, and anesthesiologist must discuss the potential management problems and need for further evaluation or intervention before arrival in the operating room. Appropriate communication and cooperation will optimize patient care and facilitate perioperative clinical management. The anesthesia machine must have the capacity to provide air, O2, and N2O to help balance pulmonary and systemic blood flow. Intravenous tubing must be free from air bubbles to prevent paradoxical air embolism, and air filters should be added to all infusion lines. Resuscitative drugs, labeled and ready for administration, should include succinylcholine, calcium gluconate or calcium chloride, sodium bicarbonate, atropine, lidocaine, phenylephrine, and epinephrine. An inotropic infusion, usually epinephrine or dopamine, should be premixed and ready for administration in highrisk cases, but additional infusions are prepared if their need is strongly suspected. For all pediatric cases, certain anesthetic drugs should be available (etomidate, propofol, ketamine). No single drug can be recommended; how a particular drug is used is more important. In pediatric cardiac anesthesia, many patients have limited reserve and high endogenous catecholamine levels released in an adaptive response to their underlying cardiac disease. The resuscitative drugs should therefore be prepared and immediately available before anesthetic induction. Surface cooling with a heating and cooling water mattress, ice in watertight bags, and an efficient room and ambient temperature control system are important in the operative management of these patients. Noninvasive monitoring equipment is ideally placed before induction of anesthesia, although the anesthesiologist may elect to defer application of monitoring devices in the crying child until immediately after the induction. Standard monitoring includes electrocardiography, pulse oximetry, capnography, and an appropriate-sized blood pressure cuff (either oscillometric or Doppler). Additional monitoring includes an indwelling arterial catheter and temperature probes. Continuous monitoring of arterial pressure is possible only through an indwelling intraarterial catheter. In young children, cannulation of the radial artery with a 22- or 24-gauge catheter is preferred. Careful inspection, palpation, four-extremity noninvasive blood pressure determinations, and ultrasound use help ensure that previous or currently planned operative procedures. Other sites available for cannulation include the ulnar, femoral, axillary, and umbilical (in neonates) arteries. Cannulation of the posterior tibial or dorsalis pedis arteries is not usually sufficient for complex operative procedures. Rectal and nasopharyngeal temperatures are monitored because they reflect core temperature and brain temperature, respectively. Monitoring of esophageal temperature is a good reflection of cardiac and thoracic temperature. Tympanic probes, although a useful reflection of cerebral temperature, can cause tympanic membrane rupture. Pulse oximetry and capnography provide instantaneous feedback concerning adequacy of ventilation and oxygenation. They are useful guides in ventilatory and hemody namic adjustments to optimize Qp/Qs before and after surgically created shunts and pulmonary artery bands. Peripheral vasoconstriction in patients undergoing deep hypothermia and circulatory arrest renders digital O2 saturation probes less reliable. In the newborn, the use of a tongue sensor has been advocated to provide a more central measure of O2 saturation, with less temperature-related variability. For example, in children undergoing a Fontan procedure for tricuspid atresia or a univentricular heart, catheters in the Fontan pathway and the pulmonary venous atrium are especially useful. As a general guideline, a transvenous pulmonary artery catheter may be placed using the internal jugular approach in children weighing more than 7 kg. For infants weighing less than 7 kg, percutaneous placement of a pulmonary artery catheter can be performed from the femoral vein. Note the insertion of the papillary muscle of the tricuspid valve on the interventricular septum. The use of intraoperative transthoracic monitoring lines and echo-Doppler imaging limits the need for transvenous pulmonary artery catheters in most cases. The use of echoDoppler imaging is now regarded as standard of care for almost all pediatric cardiac surgeries. Postbypass echo-Doppler evaluation is able to immediately assess the quality of the surgical repair and cardiac function by examining ventricular wall motion and systolic thickening. By identifying patients with right or left ventricular contraction abnormalities after bypass, as determined by a change in wall motion or systolic thickening, echo-Doppler provides guidance for immediate pharmacologic interventions. Importantly, postbypass ventricular dysfunction and residual structural defects identified by echo-Doppler imaging are associated with an increased incidence of reoperation and higher morbidity and mortality rates. Thus, this monitoring tool is helpful in assessing surgical repair and identifying operative risk factors, which will hopefully improve outcomes. This finding necessitated immediate reinstitution of cardiopulmonary bypass and repeat repair. Note the absence of turbulent flow with the loss of the mosaic of white particles. The advantage of this technique is its utility as a continuous monitor of cardiac structure and function, without interrupting surgery. Early limitation in views has been virtually eliminated as a result of clinical experience and improved biplane images. A second technique for intraoperative echocardiographic analysis in children is the epicardial approach. This technique best facilitates the probe manipulations necessary for thorough interrogation of the major structures and dynamic function of the heart. The advantage of this approach is that all views can be obtained in patients of any size. Among the disadvantages are the need for sufficient operator skill and experience to perform the manipulations, the need to interrupt surgery to manipulate the probe, and the possible deleterious impact of direct myocardial mechanical manipulation. The primary goal of brain monitoring is to improve our understanding of cerebral function during cardiac surgery so that effective brain protection strategies can be developed. Numerous intraoperative techniques have been used for monitoring the brain to prevent secondary brain injury from hypoxia, ischemia, emboli, and electrophysiologic derangements. Because this residual electrical activity during arrest is associated with ongoing cerebral metabolism, an isoelectric state may prevent ischemic injury to the brain during circulatory arrest.
Ashwaganda (Ashwagandha). Lotrisone.
- What is Ashwagandha?
- Are there any interactions with medications?
- Dosing considerations for Ashwagandha.
- Tumors, tuberculosis, liver problems, swelling (inflammation), ulcerations, stress, inducing vomiting, altering immune function, improving aging effects, fibromyalgia, and other conditions.
- How does Ashwagandha work?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96916
Discount lotrisone online
Anesthesia for Interventional or Diagnostic Cardiac Procedures Advances in interventional and diagnostic cardiac catheterization techniques are significantly changing the operative and nonoperative approach to the patient with a congenital heart defect zeasorb antifungal powder order 10 mg lotrisone otc. Common interventions in the cardiac catheterization laboratory are shown in Table 78. Stenotic aortic and pulmonic valves, recurrent aortic coarctations, and branch pulmonary artery stenoses can be dilated in the catheterization laboratory, avoiding surgical intervention. Innovative interventional procedures improve vascular anatomy, reduce pressure loads on ventricles, and decrease the operative risk for these patients. Complications are more common during interventional catheterization and include arterial thrombosis, arrhythmias (especially heart block), hemodynamic instability, embolization of devices or coils, bleeding, perforation of the major vessels or heart, and lung reperfusion injuries. Constant vigilance, correction of electrolyte imbalance, maintenance of acid-base status, and appropriate heparinization will mitigate some of the morbidity. High-risk patients undergoing diagnostic evaluation of pulmonary artery hypertension in anticipation of heart-lung transplantation also require anesthetic management. Despite the attendant high risks for the procedure in patients with suprasystemic right ventricular pressure, these patients are best managed with general anesthesia and controlled ventilation. Anesthetic management of interventional or diagnostic procedures in the catheterization laboratory must include the same level of preparation that applies in caring for these patients in the operating room. These patients have the same complex cardiac physiology and, in some cases, greater physiologic complexity and less cardiovascular reserve. Interventional catheterization procedures can impose acute pressure load on the heart during balloon inflation. Large catheters placed across mitral or tricuspid valves create acute valvular regurgitation or, in the case of a small valve orifice, transient valvular stenosis. The anesthetic plan must consider the specific cardiology objectives of the procedure and the impact of anesthetic management in facilitating or hindering the interventional procedure. In general, the three distinct periods involved in an interventional catheterization are the data acquisition period, the interventional period, and the postprocedural evaluation period. During the data acquisition period, the cardiologist performs a hemodynamic catheterization to evaluate the need for and extent of the planned intervention. Ideally a patient would be kept spontaneously ventilating, but this is impractical. A secured airway allows the anesthesiologist to concentrate on hemodynamic issues. Positive-pressure ventilation also reduces the risk for air embolism; the cardiologist can measure pressures during expiration to obtain the most accurate data. During spontaneous ventilation, a large reduction in intrathoracic pressure can entrain air into vascular sheaths and result in moderate-to-large pulmonary or systemic air emboli. Precise device placement is also facilitated with muscle relaxants that eliminate patient movements and controlled ventilation, thereby reducing the respiratory shifting of cardiac structures. Substantial blood loss and changes in ventricular function occur commonly during the intervention. In the postprocedural period, the success and physiologic impact of the intervention are evaluated. Blood pressure, mixed venous O2 saturation, ventricular end-diastolic pressure, and cardiac output, when available, are used to assess the impact of the intervention. A brief description of some of the interventional procedures and the associated anesthetic implications follows. The success of these interventions will undoubtedly result in widespread availability and use over the next few years. Each side of the device consists of a Dacron mesh patch suspended in six spring-loaded arms that open like an automatic umbrella. The sheath and device are then pulled back so the distal arms contact the left atrial septum. Once adequately seated, the sheath is pulled farther back to expose the proximal side of the device and the proximal arms, which spring open to engage the right side of the atrial septum. Data continue to support closure of defects of small-to-moderate size (<8-20 mm) in appropriate-size patients with appropriate septal length and device diameter. Left ventriculotomies are associated with a high incidence of left ventricular dysfunction and have been relegated to a position as the least desirable surgical option. However, a significant incidence of complications occurs, including heart block, blood loss, and hemodynamic instability. In the latter case, systemic output is decreased and a period of severe hypotension is unavoidable. This highly specialized application of the clamshell device is confined to only a few pediatric centers in the United States. Peripheral pulmonary artery stenosis is not a surgically amenable lesion and is particularly suited to catheterization and angioplasty. Balloon angioplasty is accomplished by tearing the vascular intima and media, allowing the vessel to remodel and heal with a larger diameter. The balloon is placed across the stenotic lesion so that the middle of the balloon is at the stenosis. In patients without a shunt, acute increase in right ventricular afterload can cause systemic hypotension and right ventricular failure. In an early series, complications included hypotension (40%), pulmonary artery rupture (3%), unilateral reperfusion pulmonary edema (4%), aneurysmal dilation of the dilated pulmonary vessel (8%), death (1. Anesthetic support minimizes hemodynamic compromise by anticipating changes in blood flow patterns, treating transient hypotension, and providing airway support to minimize the risks associated with pulmonary artery disruption and acute unilateral pulmonary edema. Such patients can have multiple areas of severe branch pulmonary artery stenosis, with resultant systemic or suprasystemic right ventricular pressures and right ventricular dysfunction. Patients can also have coronary stenosis and develop subendocardial ischemia from hemodynamic disturbances in the setting of biventricular hypertrophy. The presence of supravalvular aortic stenosis, biventricular outflow tract obstruction, and coronary stenosis is associated with increased perioperative risk. Tachycardia and subendocardial ischemia should be avoided in the presence of ventricular hypertrophy. Catheters placed antegrade via the right side of the heart into the neoaorta can induce hemodynamically significant tricuspid and neoaortic regurgitation, resulting in hemodynamic instability. Careful monitoring and aggressive hemodynamic intervention result in a good outcome. In selected instances, to minimize the risk that coils may escape to threaten vital organ perfusion, cardiologists request the use of general anesthesia with a muscle relaxant. Depending on the lesion, patients might manifest severe cyanosis, low-output or high-output cardiac failure, or coronary ischemia. Extra care should be exercised in patients with coronary fistulas to maintain myocardial O2 supply and reduce demand. Materials used for embolization can include surgical gel (Gelfoam), alcohol, and coils. Some of these substances can induce severe allergic reactions with hemodynamic collapse. Angiography is used to demonstrate successful occlusion of the vascular structure and ascertain appropriate placement. Exceptions include neonates with critical aortic or pulmonary stenosis and patients with significant ventricular dysfunction who exhibit unstable hemodynamics. Balloon valvuloplasty is indicated in valvular pulmonary or aortic stenosis with valvular gradients more than 50 mm Hg. Balloon dilation is effective in most patients, except those with dysplastic valves. Valvular aortic stenosis is associated with poor surgical outcome in the neonatal period. All therapies are palliative, with a high incidence of repeat interventions, and balloon valvuloplasty is often the initial treatment. Residual obstruction or regurgitation is common after balloon dilatation and can require repeat intervention. A real risk exists for damage to the aortic valve and subaortic septum, with the consequence of acute aortic insufficiency and coronary ischemia.
Order lotrisone 10mg visa
Supraventricular tachycardia due to WolffParkinson-White syndrome in children: early disappearance and late recurrence anti fungal pneumonia purchase genuine lotrisone. Management of supraventricular arrhythmias in adults with congenital heart disease. Postoperative nausea and vomiting in children and adolescents undergoing radiofrequency catheter ablation: a randomized comparison of propofol- and isofluranebased anesthetics. Effects of propofol or isoflurane anesthesia on cardiac conduction in children undergoing radiofrequency catheter ablation for tachydysrhythmias. Electrophysiological effects of desflurane in children with Wolff-Parkinson-White syndrome: a randomized crossover study. Outcome of intra-atrial re-entrant tachycardia catheter ablation in adults with congenital heart disease: negative impact of age and complex atrial surgery. Increasing prevalence of atrial fibrillation and permanent atrial arrhythmias in congenital heart disease. Acute hemodynamic benefit of multisite ventricular pacing after congenital heart surgery. Does biventricular pacing improve hemodynamics in children undergoing routine congenital heart surgery Resynchronization therapy after congenital heart surgery to improve left ventricular function. Practice advisory on anesthetic care for magnetic resonance imaging: an updated report by the American Society of Anesthesiologists task force on anesthetic care for magnetic resonance imaging. Free-breathing whole-heart 3D cine magnetic resonance imaging with prospective respiratory motion compensation. Ten-year institutional experience with palliative surgery for hypoplastic left heart syndrome: risk factors related to stage I mortality. The overall goal of therapy in shock is to treat the underlying cause, return adequate oxygen delivery to the tissues, and remove metabolic products that developed during anaerobic metabolism. It appears that the faster the body returns to adequate perfusion, the better the overall outcome. At least 16,000 American children (8-20 per 100,000 children per year) suffer a cardiopulmonary arrest each year. Acute chest syndrome is the leading cause of death and the second most common complication in sickle cell disease. Tumor lysis syndrome is a metabolic crisis precipitated by acute lysis of a large number of tumor cells. Accidents and trauma are the leading causes of death in children 1 to 14 years of age. Relationship Between the Intensive Care Unit and the Operating Room the field of pediatric intensive care may have originated from anesthesia, but these areas have grown apart over time. Due to the extensive training, there are few individuals who cover both disciplines. It is important that this occurs in the preanesthetic as well as the postanesthetic setting. Similarly, understanding the operative and anesthetic course will guide the next several days of management. A complete anesthesia sign-out includes pertinent past medical history, allergies, ease of mask ventilation, induction agents, ease of intubation, decisions regarding extubation, venous and arterial access, blood products, fluid totals, inotropic agents, medications delivered including timing of antibiotics, complications, laboratory values, and most recent blood gas. This information may be available in the anesthetic record; however, a short verbal summary by the anesthesiologist provides a greater amount of practical detail. In pediatric hospitals, families participate in multidisciplinary rounds with their nurses, respiratory therapists, pharmacists, and physician caring for their child. This does not require more time than traditional rounds and it does not compromise teaching. An international multidisciplinary team of experts in neonatal, pediatric and adult critical care recently published Guidelines for Family Centered Care. We see significant family satisfaction with participation in rounds and we believe it likely benefits the team and patient as well. Parents may display behaviors that out of context may seem abnormal, such as excessive clinginess, intellectualizing the process, blaming others (including their spouses), minimizing, and seeking opinions everywhere (the internet, environmental care, etc. We must attempt to understand what drives these behaviors to provide optimal care. This emphasizes that social workers, psychologists, and child and family therapists are all part of the critical care team. Caregiver attitudes toward parental presence will need to be addressed, as the likelihood of this event increases over time. However, we have seen that resistance to family presence among providers is decreasing over time. A means for declining on the part of the clinician as well as the parent must be available. In the same manner, someone other than the person performing the procedure should be looking after the family, even for what we believe to be routine procedures. We also must give younger trainees the opportunity to opt out of family presence during procedures. A final topic that needs to be addressed is the use of palliative care services for our critically ill patients. There is a role for early consultation of palliative care, as we do not believe in restricting its use or support to just those patients who are near to death. There are great benefits to palliative care intervention to provide families ongoing support and opportunities to develop coping mechanisms. However, some clinicians may continue to resist due to concerns regarding litigation. In a survey of 1018 Illinois residents, 27% indicated they would sue, but 38% stated they would recommend the hospital if appropriate disclosure and remediation occurred. The attending remains present until all questions are answered or additional time is scheduled if necessary. Most hospitals will track errors or negative outcomes through a quality assurance program. Medical errors will occur, but they should also be an opportunity to improve practice quality and prevent future events. We also find their services exceedingly helpful for children with chronic medical conditions who are anticipated to die during a future admission. With a team approach, we try to minimize pain and suffering for the child and family at the end of life. However, with this concept there is a significant interplay with financial, societal, ethical, personal, and religious opinions and feelings. It may be difficult to define futility, but when the pain and suffering of continuing life are more severe than the inevitability of death, care may become futile. However, pain relief and caring support for the child and family can never be classified as futile care. Space should be provided for parents to remain with their children during the day and for parents to sleep overnight. Parents should be encouraged to participate as much as possible in the care of their child. Each bed space should be standardized so that it can be used to provide any level of care. Private rooms are ideal, but if shared rooms are necessary, the distance between beds must be adequate to ensure privacy and minimize nosocomial infection. Devices for diversion and entertainment should be available for conscious children. During this time, myocytes engage in rapid protein synthesis and rapid cell growth, which requires a high intracellular concentration of nuclei, mitochondria, and endoplasmic reticulum. The greater number of nonelastic and noncontractile elements makes the neonatal myocardium less compliant, and it contracts less efficiently than the adult myocardium. In the fetus and newborn, the decreased ventricular compliance causes small changes in end-diastolic volume to induce large changes in end-diastolic pressure. In addition, augmentation of stroke volume by the Frank-Starling mechanism is less effective in young children. The medical director oversees the quality of patient care, patient triage, implementation of policy and procedures, in-service education, and coordination of consultants.
Lotrisone 10 mg sale
Inotropic support may be necessary to maintain systemic blood pressure as balloons and crimped valves traverse the valve orifice antifungal home remedies for dogs purchase cheap lotrisone on line. In the catheterization laboratory, growing usage of general anesthesia to support patients during complex procedures ideally positions cardiac anesthesiologists to perform this service in a new context. In addition, cardiac anesthesiologists understand imaging in the context of anesthetic care and are capable of manipulating hemodynamics as observation of cardiac function requires. Functional interpretation of structural defects can be critical as repairs are made. Real-time 3D guidance during catheter placement, ballooning, or device implantation is an important and new component of interventional cardiology. It is relatively new in intracardiac imaging and for cardiac anesthesiologists; it defines an exciting and important role that goes a step beyond the job of maintaining homeostasis during the stress of surgery. To this end, information from fluoroscopic and echocardiographic images can augment each other when unusual anatomy or clinical circumstances are observed. Data from each imaging modality should be discussed if contradictory interpretations arise. It may be important to alternate between 2D and 3D imaging to clarify temporal and spatial details127,128 so that accurate placement of wires and catheters can occur. Closure of paravalvular leaks or stenting of stenotic pulmonary veins, for example, may require both types of imaging. Real-time 3D imaging can clearly depict the proximity of equipment and devices to targeted defects by permitting rotation of acquisitions in all directions, thereby delineating structures in their native orientation. Valve position and function is assessed, gradients are calculated, the absence of coronary ostial occlusion is confirmed, and the need for any remedial activity is discussed. As technology evolves, percutaneous procedures for structural heart disease will become more sophisticated. Patients with congenital, acquired, and surgically created defects will become eligible for treatment by interventional cardiology procedures. As the population ages and medical therapies achieve increased effectiveness, more patients who in the past would not have been candidates for any intervention will be offered procedures that either prolong life or improve its quality. The current expansion of minimally invasive, nonsurgical approaches to disease will continue and, as a result of these changes, demand for anesthesiology services will escalate. Perhaps the most significant lessons include our understanding of the needs of the patients and proceduralists-and the expectation that the same standards of care will be required wherever anesthesia care is provided. Inclusion of procedural areas within our practice requires a new model of service delivery. Over the past 30 years, anesthesiologists revolutionized safety, reliability, and the scope of perioperative practice. It is also required to ensure that each health system can successfully compete and remain financially solvent. We must provide more efficient and, in many cases, more flexible services in nontraditional settings as long as we remain attentive to patient needs and safety considerations. We also need to communicate when an anesthesia provider is required for some procedures, what equipment, supplies, and other needs must be met, and how to do so costeffectively. To do so requires that we document our services and outcomes and evaluate alternative approaches to care in a thoughtful and evidence-based manner. In an era of increasing medical specialization and fragmentation of care delivery, particularly in the context of accountable care organizations and bundled payments, these are the critical indices of success. Proper variable cost accounting demonstrates that the cost of patient care involving an efficiently deployed anesthesiologist is less than the cost imposed on the whole system by those procedures that start without anesthesia personnel and end with an urgent, unanticipated call. The expense of (1) delaying a procedure, (2) stopping a procedure for inadequate or excessive sedation, (3) hospitalizing a patient, and (4) rescheduling or redoing procedures is forbidding. However, the costs are not always obvious because they are spread over multiple cost centers. Strategic Positioning For anesthesiologists, strategic positioning occurs when the needs of customers are satisfied with minimal cost to the anesthesiologists. The customers are not just patients-they are also medical proceduralists and third-party payers. If we can provide a safer and more comfortable, time-efficient, and cost-effective environment for proceduralists, the value of anesthesiologists will be clear. If we develop a bridge between medical and surgical treatment by facilitating hybrid procedures and interdisciplinary approaches, the overall value of our presence will be incontrovertible to proceduralists, patients, insurance companies, regulatory bodies, and government agencies. Financial Silos and Teamwork the increased requirements by third-party payers to provide value-based care requires that anesthesiologists work collaboratively with our colleagues to define new models of care and integrated care requires collaboration and interdisciplinary effort. Team building requires communication and coordination based on common experience and vocabulary. In many cases, this process will be most effective if we align anesthesiologists and other providers by service lines which collaboratively define standard approaches to care for specific patient populations. Sustainable Strategy: Key Points An effective strategy is one that maintains a dynamic and profitable market presence. Anesthesiologists have two related parallel sets of priorities: creating and maintaining a stable but flexible customer base, and achieving financial sustainability. Operational effectiveness will ensure that appropriate resource allocation permits innovation. Team building will ensure that proceduralists understand the rationale for close cooperation and generate a foundation for better integrated finances. Reframing boundaries and elimination of silos will enhance integration, productivity, and the quality of care across the board. The overall strategy must be to make our specialty indispensable to customers and potential customers while enhancing the lives of patients by improving outcomes and stimulating progress. Our expertise will generate consistent reimbursement if we have the data to demonstrate the benefit of that presence. As technology continues to proliferate and diversify, the distinction between medical and surgical approaches to treatment becomes blurred. We must continue this work in new venues and work to build bridges to continue to strengthen our specialty. If this opportunity and its associated intellectual challenges are ignored, the status of anesthesia, a key medical subspecialty, may be threatened. If the challenge is accepted, the practice of anesthesiology will be on the front lines of changing and advancing medical science. Regardless of the venue or the technique, anesthesiologists remain a critical and constant guardian of the integrative medical perspective, patient safety, and efficient procedural processes. Wendy Gross, who was a contributing author to this topic in the prior edition of this work. Handbook of Cardiac Electrophysiology: A Practical Guide to Invasive Ep Studies and Catheter Ablation. American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Growth of nonoperating room anesthesia care in the United States: a contemporary trends analysis. Traditional fee-for service medicare systems and fragmented patient care: the backdrop for non-operating room procedures and anesthesia services in anesthesia outside the operating room. Management of staffing and case scheduling for anesthesia outside of the operating room. Patient safety: anesthesia in remote locations in anesthesia outside the operating room. Preoperative patient evaluation for anesthesia care outside of the operating room. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: a report. Projected national impact of colorectal cancer screening on clinical and economic outcomes and health services demand. An initial investigation of bispectral monitoring as an adjunct to nurse-administered propofol sedation for colonoscopy. Can remifentanil be a better choice than propofol for colonoscopy during monitored anesthesia care Total intravenous vs inhalational anesthesia for colonoscopy: a prospective study of clinical recovery and psychomotor function. Acute reactions to intravascular contrast media: types, risk factors, recognition and specific treatment. Pharmacological prevention of serious anaphylactic reactions due to iodinated contrast media: systematic review. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions.

Purchase 10mg lotrisone mastercard
The United States model antifungal active ingredient buy generic lotrisone canada, in which all anesthesiologists treat trauma patients-but few do so exclusively-has led to a relative dearth of research, publication, and education in this field. In small hospitals and military and humanitarian practice, austere conditions may influence the resources available. Patient information may be limited, and allergies, genetic abnormalities, and previous surgeries may create sudden crises. Patients are frequently intoxicated, with full stomachs and the potential for cervical spine instability. Simple operations may become complicated, and specialty surgical and anesthesia equipment may be required on short notice. Patients often have multiple injuries requiring complex positioning, multiple procedures, and the need to consider priorities in management. Some studies have suggested that mechanism of injury alone is a poor predictor for trauma center referral. Additional studies have justified mechanism of injury as a parameter that helps reduce inappropriate transport of patients with major trauma to nontrauma centers. Verification of an open airway and acceptable respiratory mechanics is of primary importance because hypoxia is the most immediate threat to life. Inability to oxygenate the patient will lead to permanent brain injury and death within 5 to 10 minutes. Trauma patients are at risk for airway obstruction and inadequate respiration for the reasons listed in Box 66. The point of injury in the patient with penetrating trauma may be utterly discernible-even to the inexpert provider-but the extent of tissue damage and depth of shock may be less detectible compared to the patient suffering from a blunt traumatic injury. Conversely, the patient with penetrating trauma will lose blood volume externally together with loss into body cavities, whereas the patient with blunt trauma may present in hemorrhagic shock with no obvious signs of hemorrhage. Resolution of urgent needs is followed by a meticulous secondary survey and further diagnostic studies designed to reduce the incidence of missed injuries. If establishment of a secure airway and adequate ventilation requires a surgical procedure such as a tracheostomy, tube thoracostomy, or open thoracotomy, this procedure must precede all others. Hemorrhage is the next most pressing concern since ongoing blood loss is inevitably fatal. Assessment of the circulation consists of an early phase, during active hemorrhage, and a late phase, which begins when hemostasis is achieved and continues until normal physiology is restored. In the early phase, diagnostic efforts focus on the five sites of bleeding detailed in Table 66. Immediate actions to control hemorrhage can include application of pelvic binders for bleeding associated with pelvic fractures or tourniquet application for extremity injuries. This includes exploration of the neck or pericardium to rule out hemorrhage in sensitive compartments. Patients with unstable spinal canal injuries and incomplete neurologic deficits will also benefit from early surgical decompression and stabilization. The final step in the primary survey is complete exposure of the patient and a head-to-toe search for visible injuries or deformities, including deformities of bones or joints, soft tissue bruising, and any breaks in the skin. The anesthesiologist can assist in this procedure by support of the head and neck, maintenance of the airway, and care in manipulating the spine. After the primary survey, a more deliberate secondary examination is undertaken that includes a thorough history and physical examination, diagnostic studies, and subspecialty consultation. Any remaining injuries are diagnosed at this time and treatment plans established. The presence of a limb-threatening injury due to vascular compromise, compartment syndrome, or a severely comminuted fracture is one such indication. A trauma patient may have injuries requiring emergency surgery coexisting with injuries that can be repaired at any time. The anesthesiologist plays an important role in determining which procedures to perform, in which order, and which procedures should be postponed until the patient is more stable. Emergent surgical procedures were started within 30 minutes of arrival in 77% of patients and within 60 minutes in 92%. Anesthesia in War and Austere Conditions "While it is evident that the general principles of anesthesia are not affected by the circumstances of war, it is equally evident that it is our duty to assiduously seek those means in anesthesia which are especially suited to the exigencies of battle. Recent conflicts and events have allowed anesthesiologists, nurse anesthetists, and other providers to help improve management of traumatically injured patients in the areas of anesthesia, resuscitation, and damage control surgery. Management of battlefield casualties typically follows the same flow as outlined earlier, but with special consideration in the areas of prehospital interventions, resuscitation, technologic and logistic support, patient movement, mass casualty management, and surgical interventions. Paradoxically, the ability to get many of the severely wounded patients to a hospital. Even in the late l960s, wounded soldiers were evacuated out of Vietnam within 3 days of injury. In the most recent conflict, the time from injury in the Middle East until movement to more definitive medical care in Europe or North America is often within 24 to 48 hours. In preparation for such rapid movement, the anesthesiologist must ensure that perioperative interventions such as airway management, pain control, and adequacy of resuscitation are addressed before transfer. Given the limited number of anesthesia providers in most combat-related scenarios, often they are not involved in the triage process. If available, however, anesthesia support can enhance emergency airway management, establishment of venous access, and supervision of resuscitative efforts. Only 10% to 20% of arriving casualties require immediate lifesaving interventions, although a much larger percentage will ultimately require surgical procedures. Logistic support chains may be long and unable to provide sufficient supplies in the early phases of a conflict. With special training in airway management, provision of anesthesia and sedation, resuscitation, and pain management, anesthesiologists may find themselves involved in triage, emergency management, and perioperative and critical care. The anesthesiologist should have a plan for the initial approach to the airway and for coping with any difficulties that might develop. Once the decision to obtain a definitive airway is made, efforts will continue until a cuffed tube is in position in the trachea, whether by conventional intubation or via a surgical approach. Failure to commit to a surgical airway soon enough results in bad outcomes more commonly than do complications of a procedure that might have been unnecessary. Endotracheal intubation is commonly required and is specifically indicated in the following conditions: Cardiac or respiratory arrest Respiratory insufficiency (see Box 66. Endotracheal intubation is best accomplished in almost all cases with a modified rapid sequence approach by an experienced clinician. Anesthesia and neuromuscular blockade allow the best tracheal intubating conditions on the first approach to the airway, which is advantageous in an uncooperative, hypoxic, or aspirating patient. Attempts to secure the airway in an awake or lightly sedated patient increase the risk for airway trauma, pain, aspiration, hypertension, laryngospasm, and combative behavior. Blind intubation (oral or nasal) is discouraged in patients with maxillofacial trauma and laryngeal or tracheal injury. Individual practitioners and trauma hospitals should determine their own algorithm, based on available skills and resources. However, cricoid pressure may worsen the laryngoscopic grade of view in up to 30% of patients58 without providing effective prevention of aspiration of gastric contents. The lack of evidence supporting the use of cricoid pressure and its potential to make intubation more difficult led the American Heart Association to recommend discontinuation of its use during cardiac arrest situations. If preoxygenation is not possible because of facial trauma, decreased respiratory effort, or agitation, rapid desaturation is a possibility. Positive-pressure ventilation during all phases of induction provides the largest possible oxygen reserve during emergency airway management and will help mitigate hypoxia if intubation proves difficult. In this situation, large tidal volumes and high peak inspiratory pressures should be avoided. Application of cricoid pressure during attempts at positive-pressure ventilation should be considered to reduce gastric inflation, but it may prevent effective ventilation in some patients necessitating discontinuation. The front of the cervical collar is removed once in-line manual stabilization of the spine is established, allowing for cricoid pressure and greater excursion of the mandible. Stabilization of the cervical spine will generally occur in the prehospital environment, with the patient already having a rigid cervical collar in place.
Lotrisone 10mg otc
When a standard manual defibrillator is used in resuscitation antifungal infection cream buy generic lotrisone online, the rescuer needs to interpret the rhythm and shock when appropriate. If the rescuer is unfamiliar with the waveform used or the manufacturer recommendations, then the maximal available energy should be used as the default energy. Stacked defibrillation is considered only during cardiac surgery or in the cardiac catheterization laboratory where invasive monitoring and defibrillation pads are in place already. These parameters can be monitored continuously, without interrupting chest compressions. An abrupt increase in any of these parameters is a sensitive Update to Airway Management and Ventilation in Cardiac Arrest When cardiac arrest occurs, adequate oxygen delivery is required to restore the energy state of the heart as well as other vital organs, and consequently ventilation becomes an essential part of the resuscitation. Options include standard bag-mask ventilation versus placement of an advanced airway. There is inadequate evidence to show a difference in survival or favorable neurologic outcome with the use of bag-mask ventilation compared with endotracheal intubation or other advanced airway devices. The choice of bag-mask device versus advanced airway insertion is determined by the skill and experience of the provider. After placement of an advanced airway, it is recommended to provide 1 breath every 6 seconds (10 breaths/min) while continuous chest compressions are being performed. Extreme caution should be taken to avoid excessive airway pressure that will compromise venous return in cardiac arrest patients, as hyperventilation is common during enthusiastic resuscitation. Asystole should be differentiated from agonal bradycardia and fine ventricular fibrillation. In the traumatized patient, hypovolemia, cardiac tamponade, and tension pneumothorax are possible causes of cardiac arrest and must be considered and acutely treated. Unanticipated cardiac arrest occurring in the intraoperative and postoperative periods should include acute massive pulmonary thromboembolism or air emboli as possible causes. Electrolyte and metabolic derangements such as severe hyperkalemia, metabolic acidosis, or drug. Asystole Asystole is the complete and sustained absence of electrical activity and portends extremely poor prognosis. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. The -adrenergic effects of epinephrine are controversial because they may increase myocardial work and reduce subendocardial perfusion. Thus standard-dose epinephrine (1 mg every 3-5 minutes) is recommended for patients in cardiac arrest. The exceptions to this recommendation are special circumstances requiring higher or repeated doses of epinephrine, such as in patients with -blocker overdose, calcium channel blocker overdose, or when epinephrine is titrated to real-time physiologically monitored parameters. Therefore early administration of epinephrine is recommended after the onset of cardiac arrest caused by an initial nonshockable rhythm. Vasopressin is a nonadrenergic peripheral vasoconstrictor that also causes coronary and renal vasoconstriction. Vital signs such as noninvasive blood pressure or oxygen saturation may be difficult to obtain. These factors can easily confuse healthcare providers rendering care to these patients. Clinical findings such as skin color and capillary refill are reasonable predictors of the presence of adequate flow and perfusion. Chest compressions are ineffective because the mechanical ventricles are rigid and cannot be compressed. The only therapeutic option is to try to restore mechanical function of the device. One liter of normal saline solution should be administered intravenously to treat for possible hypovolemia. Assisted ventilation should be performed as needed, and the patient should be transported to the hospital as soon as possible. However, manual conventional chest compressions are frequently affected by fatigue, varying skill levels and training, pauses during defibrillation and the switch of rescuers, and adherence to protocols. These devices are designed to deliver compressions of consistent rate and depth, eliminate fatigue as a factor, and provide an opportunity to reduce the frequency and length of pauses in compression. The possible explanation for this discrepancy between early studies and the large clinical trial is that application of the mechanical device resulted in long pauses of chest compression (median device application time 36. Future emphasis should be placed on streamlining and appropriately timing the deployment of these compression devices. Cardiopulmonary Resuscitation in Adults and Children With Mechanical Circulatory Support: A Scientific Statement From the American Heart Association. Echocardiography has revolutionized our ability to assess the etiology and hence the management of these patients. However, performing and interpreting echocardiography frequently proves much more challenging in the real scene of cardiac arrest. It is less affected by the body habitus, presence of subcutaneous air, and by chest movements. The caveat is that the interpretation of spontaneous cardiac movement is still very operator-dependent. In addition, in cases of significant bradycardia, the image could be potentially interpreted as cardiac standstill between the cardiac contractions. Cardiac or Respiratory Arrest Associated With Opioid Overdose In the United States in 2013, 16,235 people died of prescription opioid toxicity, and an additional 8257 died of heroin overdose. Regardless of the care setting and route of administration, the initial goal of therapy is to restore and maintain patent airway and ventilation, preventing respiratory and cardiac arrest, without provoking severe opioid withdrawal. Identifying clinical signs of possible stroke (sudden weakness or numbness of the face, arm, or leg, especially on one side of the body; sudden confusion, trouble speaking, or understanding; sudden trouble seeing in one or both eyes; sudden trouble walking, dizziness, loss of balance, or coordination; or sudden severe headache with no known cause) is important because fibrinolytic treatment must be provided within a few hours of onset of symptoms. Recognition and Management of Specific Arrythmias this section highlights recommendations for management of patients with acute symptomatic arrhythmias. It needs to be emphasized that electrocardiographic and rhythm information should be interpreted within the context of total patient assessment. For example, when a patient with respiratory failure and severe hypoxemia becomes hypotensive and develops a bradycardia, the bradycardia is not the primary cause of instability. In general, "unstable arrhythmias" refer to a condition in which vital organ function is acutely impaired due to inefficient cardiac contractions and insufficient cardiac output, or cardiac arrest is ongoing or imminent. When an arrhythmia causes a patient to be unstable, immediate intervention is indicated. In such cases, more time is available to decide on the most appropriate intervention. In both unstable and symptomatic cases, the provider must make an assessment as to whether the arrhythmia is causing the patient to be unstable or symptomatic. However, when bradycardia is the cause of symptoms, the rate is generally less than 50 beats/min. A slow heart rate may be physiologically normal for some patients, whereas a heart rate of more than 50 beats/min may be inadequate for others. Because hypoxemia is a common cause of bradycardia, initial evaluation of any patient with bradycardia should focus on signs of increased work of breathing (tachypnea, intercostal retractions, suprasternal retractions, paradoxical abdominal breathing) and oxygen saturation as determined by pulse oximetry. If oxygenation is inadequate or the patient shows signs of increased work of breathing, supplementary oxygen should be provided. The provider must identify signs and symptoms of poor perfusion and determine if those signs are likely to be caused by the bradycardia. Asymptomatic or minimally symptomatic patients do not necessarily require treatment unless there is suspicion that the rhythm is likely to progress to symptoms or more advanced bradyarrhythmias. If the bradycardia is suspected to be the cause of acute altered mental status, ischemic chest discomfort, acute heart failure, hypotension, or other signs of shock, the patient should receive immediate treatment. Atropine will also unlikely be effective in patients who had heart transplantation because the transplanted heart lacks vagal innervation. At lower doses, dopamine has a more selective effect on inotropy and heart rate; at higher doses (>10 g/kg/min), it also has vasoconstrictive effects. Epinephrine, as described previously, is a catecholamine with - and -adrenergic actions. Isoproterenol is a -adrenergic agent with -1 and -2 effects, resulting in an increase in heart rate and vasodilation.
Syndromes
- Amount swallowed
- Vaginal bleeding (heavier than usual or after menopause)
- Sputum culture and throat culture
- Have you eaten anything unusual of late?
- Internal bleeding, such as in the gastrointestinal tract
- The surgeon makes a surgical cut on the side of your thigh.
- You have a fever over 101 degrees Fahrenheit
Discount lotrisone line
As right ventricular function improves fungi vs parasite buy lotrisone 10 mg lowest price, right atrial pressure falls, right-to-left shunting decreases, and systemic arterial saturation rises. Venous and arterial access may be achieved through a large central artery and vein, usually the carotid artery and internal jugular vein, or by direct chest cannulation. Recovery from severe ventricular dysfunction is predicated on the concept that the myocardium has sustained a transient injury. Complications, however, were not associated with age, cause, type of anesthetic, or airway management. The associated hypotension results in coronary ischemia, which worsens this cycle. Perioperative factors thought to precipitate a pulmonary hypertensive crisis include hypoxia, hypercarbia, acidosis, hypothermia, pain, and airway manipulations in patients with pulmonary hypertension. Such patients present for hemodynamic catheterization, drug study, and noncardiac and cardiac surgical procedures. Pulmonary vasodilator therapy and inotropes must be continued in the perioperative period. Investigations include a comprehensive echocardiogram with occasional chest computed tomography angiography to exclude pulmonary thromboembolic disease. After premedication, the patient should be monitored with pulse oximetry to ensure the patient does not hypoventilate or become hypoxic. An intravenous induction with carefully titrated doses of ketamine may be the safest; if no intravenous is present, an inhalational induction with sevoflurane can be performed safely with 100% O2, keeping the end-tidal sevoflurane concentration as low as possible and quickly obtaining intravenous access. Procedures with potential for blood loss, hemodynamic instability, and changes in ventilatory status mandate invasive arterial monitoring. Care should be taken to avoid systemic hypotension while achieving general anesthesia. Hypotension in the presence of euvolemia may need to be treated with inotropes and, if necessary, 1-agonists. In the circumstance of intracardiac shunts, changes in FiO2 have little effect on PaO2. As these lung segments become increasingly hypoxemic, secondary hypoxic vasoconstriction occurs. In practice, this is accomplished with relatively large tidal volumes and low respiratory rates, which produce an exaggerated chest excursion. To maximize these cardiopulmonary interactions, high tidal volume with low respiratory rates should be employed. In immature animals, the myocardium is less responsive to isoproterenol and causes tachycardia and increased myocardial O2 consumption. These latter effects may reduce coronary perfusion and result in relative myocardial ischemia. Both prostaglandin E1 and prostacyclin have a pulmonary vasodilating effect; however, both drugs produce systemic hypotension, which severely limits their use. Infusion of these drugs into the right side of the circulation produces a potent short-lived relaxation of the pulmonary artery smooth muscle. Preliminary reports indicate that bosentan improves symptoms, exercise tolerance, and hemodynamics in patients with pulmonary hypertension. The drug is well tolerated and free of side effects apart from a dose-dependent increase in liver enzymes. Although nonselective, it is rapidly inactivated by hemoglobin and, when inhaled, produces no systemic vasodilation. In pediatric patients, restoration of hemostasis has proved difficult; diagnosis of the problem and treatment are marginally effective. Second, the type of operation performed in neonates and infants usually involves more extensive reconstruction and suture lines, creating more opportunities for surgical bleeding than in adult cardiac patients. Heparin is traditionally administered based on patient weight, at an empiric dose of 400 units/kg. Such a setup allows for individual variability in heparin efficacy and metabolism. In the absence of such a system, empiric dosing is recommended at 1 to 3 units/mL of priming solution. In addition, other heparin cofactors, including 2-macroglobulin, may play an important, though poorly understood, role in anticoagulation in young children. Blood heparin concentration devices may be used to dose protamine according to the amount of circulating heparin in the patient, accounting for metabolism or recent dosing. Delayed hepatic clearance of heparin resulting from organ immaturity and the predominant use of hypothermic circulatory arrest in the young decrease metabolism and excretion of heparin. This should be assessed before administering additional protamine, which in excess may contribute to postoperative bleeding. The surgeon should first attempt to identify any obvious source of surgical bleeding at the sites of repair. Routine administration of blood products to correct laboratory coagulation abnormalities in the absence of bleeding is never clinically indicated. Under most circumstances, meticulous surgical technique, appropriate administration of protamine, adequate patient temperature, and platelet infusion will correct excessive bleeding. Although use of transfusion algorithms demonstrate reduced transfusion and even decreased mortality in adults having cardiac surgery,258,259 no large or multicenter trials have been conducted examining transfusion algorithms in children. Complicating the development of algorithms in children is the heterogeneity in congenital defects, the surgical operation performed, and the complexity across congenital heart centers. Antifibrinolytics exert their effects by reversibly binding to lysine analogue sites on plasminogen, a molecule primarily responsible for the breakdown of fibrin. By inhibiting plasminogen, and therefore plasmin, the procoagulant effects of fibrin remain. Lysine analogues epsilon amino-caproic acid and tranexamic acid are efficacious in reducing bleeding and transfusion requirement in pediatric cardiac surgery. Blood transfusion during the perioperative period must be thoughtful and intentional. Injudicious use of blood products to correct individual coagulation abnormalities separately further exacerbates dilution of existing procoagulants, and carries the risk of multiple donor exposures. Transfusion should be undertaken as specifically indicated by an impairment in tissue oxygenation or documented coagulopathies with clinically significant bleeding. Algorithms may improve hemodynamic stability262; research is needed to confirm improved outcomes. A recent study demonstrated an association between the indication for blood transfusion and postoperative morbidity in a cohort of children having cardiac surgery. Study results indicated that patients who required transfusion to maintain a target postdilutional hematocrit on pump had no increase in morbidity, while those requiring a therapeutic transfusion experienced severe morbidity and mortality. Routine correction of these abnormalities with infusion of blood products is not warranted. Administration of blood products should not occur in the absence of clinical evidence of bleeding and the identification of a specific defect requiring targeted component therapy. Routine use of blood products for volume replacement is also to be avoided; lactated Ringer or saline solution can be satisfactorily administered at a reduced cost without the hazards associated with transfusion. Postoperative Management Immediate postoperative care of the pediatric patient who has undergone cardiothoracic surgery is an important period in the overall sequence of anesthetic and surgical management. Although the primary influence on outcome is determined by the conduct of the operation, postoperative care is an important factor. As a member of the operative team, it is necessary that the anesthesiologist understand and become involved during the immediate postoperative period. Detailed principles of postoperative management of pediatric cardiac surgical patients are beyond the scope of this chapter. However, a few general guiding principles and approaches are given to provide fundamental knowledge for the anesthesiologist. In the immediate postoperative setting, abnormal convalescence and specialized problems must be recognized and managed appropriately. Therefore, the guiding principle in the management of the postoperative patient is an understanding of both normal and abnormal convalescence after anesthesia and cardiac surgery. The immediate postoperative period, even that of normal convalescence, is one of continuous physiologic change because of the pharmacologic effects of residual anesthetic agents and the ongoing physiologic changes secondary to abrupt alteration in hemodynamic loading conditions, surgical trauma, and extracorporeal circulation. Despite these changes, postoperative care should be predictable and standardized for most patients undergoing cardiac procedures. Because physiologic change after cardiac surgery is dramatic but self-limiting during normal convalescence, recognition of abnormal processes can be difficult.

Order lotrisone 10mg fast delivery
It can also cause venous gas embolism fungi queensland cheap 10mg lotrisone with amex, decreased venous return, and cardiac collapse if right heart failure develops. The anesthesiologist must also be ready for potential conversion to open thoracotomy due to bleeding or an inability to obtain adequate surgical exposure. An increase in operative issues must be anticipated for surgeons learning to use the robot. However, robotic surgery does have increased costs in comparison to laparoscopic alternatives. However, there is a real need to investigate the outcomes and costs of a robotic approach versus a more traditional approach. More data are needed to identify the type of cases and patient populations that will improve patient outcomes and reduce costs via robotic surgery. Recognizing the unique physiologic changes and positioning challenges that accompany robotic surgeries will allow anesthesiologists to best care for their patients. Acknowledgment the authors would like to acknowledge Sumeet Goswami, Priya Kumar, and Berend Mets for contributions they made in prior versions of this chapter. The influence of the Trendelenburg position on haemodynamics: comparison of anaesthetized patients with ischaemic heart disease and healthy volunteers. The effects of the exaggerated lithotomy position for radical perineal prostatectomy on respiratory mechanics. Comparison of volumecontrolled and pressure-controlled ventilation in steep Trendelenburg position for robot-assisted laparoscopic radical prostatectomy. Comprehensive review: is it better to use the Trendelenburg position or passive leg raising for the initial treatment of hypovolemia Comparison of the effect of the Trendelenburg and passive leg raising positions on internal jugular vein size in critically ill patients. Comparison of 30-Day postoperative outcomes after laparoscopic vs robotic colectomy. The response to Trendelenburg position is minimally affected by underlying hemodynamic conditions in patients with aortic stenosis. Prolonged steep Trendelenburg positioning increases the risk of postoperative morbidity in patients undergoing robotic surgery for presumed gynecologic malignancy. The effect of the modified Z Trendelenburg position on intraocular pressure during robotic assisted laparoscopic radical prostatectomy: a randomized, controlled study. Effect of prolonged pneumoperitoneum on intraoperative urine output during laparoscopic gastric bypass. Transient but significant visual field defects after robot-assisted laparoscopic radical prostatectomy in deep Trendelenburg position. Impact of intraoperative fluid administration on outcome in patients undergoing robotic-assisted laparoscopic prostatectomy-a retrospective analysis. Early and late perioperative outcomes following radical cystectomy: 90-day readmissions, morbidity and mortality in a contemporary series. Sharpening the focus on causes and timing of readmission after radical cystectomy for bladder cancer. Hospitalization trends after prostate and bladder surgery: implications of potential payment reforms. Prospective randomized controlled trial of robotic versus open radical cystectomy for bladder cancer: perioperative and pathologic results. Comparing open radical cystectomy and robot-assisted laparoscopic radical cystectomy: a randomized clinical trial. Perioperative outcomes and oncologic efficacy from a pilot prospective randomized clinical trial of open versus robotic assisted radical cystectomy. No differences in population-based readmissions after open and robotic-assisted radical cystectomy: implications for post-discharge care. Does steep Trendelenburg positioning effect the ocular hemodynamics and intraocular pressure in patients undergoing robotic cystectomy and robotic prostatectomy Outcomes of laparoscopic and robotic partial nephrectomy for large (>4 cm) kidney tumors: systematic review and meta-analysis. Outcomes of robotic versus laparoscopic partial nephrectomy: an updated meta-analysis of 4,919 patients. Multicenter analysis comparing robotic, open, laparoscopic, and vaginal hysterectomies performed by high-volume surgeons for benign indications. Learning curve in concurrent application of laparoscopic and robotic-assisted hysterectomy with lymphadenectomy in endometrial cancer. Learning curve analysis of the first 100 robotic-assisted laparoscopic hysterectomies performed by a single surgeon. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. Outcomes of roboticassisted laparoscopic hysterectomy stratified by body mass index. A comparison of operative outcomes between standard and robotic laparoscopic surgery for endometrial cancer: a systematic review and meta-analysis. Robotic versus laparoscopic right colectomy: an updated systematic review and meta-analysis. Laparoscopic versus robotic colectomy: a national surgical quality improvement project analysis. Robotic cholecystectomy versus conventional laparoscopic cholecystectomy: a meta-analysis. Robotic single-site versus multiport laparoscopic cholecystectomy: a case-matched analysis of short- and long-term costs. Robotic-assisted versus laparoscopic cholecystectomy: outcome and cost analyses of a case-matched control study. A comparative study of outcomes between single-site robotic and multi-port laparoscopic cholecystectomy: an experience from a tertiary care center. Robotic single-port laparoscopic cholecystectomy is safe but faces technical challenges. Laparoscopic vs open hepatic resection for benign and malignant tumors: an updated meta-analysis. Robotic liver surgery for minor hepatic resections: a comparison with laparoscopic and open standard procedures. Robotics in hepatobiliary surgery-initial experience, first reported case series from India. Laparoscopic versus robotic surgery for hepatocellular carcinoma: the first 46 consecutive cases. The University of Pennsylvania curriculum for training otorhinolaryngology residents in transoral robotic surgery. A flexible, single-arm robotic surgical system for transoral resection of the tonsil and lateral pharyngeal wall: next-generation robotic head and neck surgery. Robotic surgery in oral and maxillofacial, craniofacial and head and neck surgery: a systematic review of the literature. Transoral robotic surgery of the oropharynx: clinical and anatomic considerations. Two-year survival analysis of 50 consecutive head and neck cancer patients treated with transoral robotic surgery in a single European centre. Endoscopic coronary artery bypass grafting with the aid of robotic assisted instruments. Robotically assisted totally endoscopic atrial septal defect repair: insights from operative times, learning curves, and clinical outcome. Robotic techniques improve quality of life in patients undergoing atrial septal defect repair. Totally endoscopic robotic-assisted repair of patent ductus arteriosus and vascular ring in children. Integrated coronary revascularization: percutaneous coronary intervention plus robotic totally endoscopic coronary artery bypass. Results of the prospective multicenter trial of robotically assisted totally endoscopic coronary artery bypass grafting.
Order lotrisone toronto
The composition of the dialysis fluid is similar to that of plasma and consists of approximately 130 mEq/L of sodium fungi bio definition cheap lotrisone amex, 100 mEq/L of chloride, 35 mEq/L of acetate or lactate as a buffer, 3. The glucose concentration of the solution can be either isosmotic or hyperosmotic. Respiratory compromise may occur with peritoneal dialysis because the increased abdominal pressure caused by the dialysate in the abdomen may prevent effective spontaneous ventilation. Severe dehydration, circulatory collapse, and metabolic derangements are other complications of peritoneal dialysis. The principles of hemodialysis are essentially the same as those of peritoneal dialysis, except the blood interfaces with a semipermeable membrane rather than with the peritoneum. Hemodialysis is more appropriate in the acute setting with life-threatening electrolyte disturbances, fluid overload, and toxic ingestions. An ultrafiltrate of plasma is created by hydrostatic pressure exerted across a highly permeable membrane, with simultaneous blood volume replacement with a modified lactated Ringer solution. Furthermore, technical challenges occur in smaller patients due to flow characteristics of smaller dialysis catheters. Hemodialysis can be performed with two separate 5 Fr single lumen catheters, but typically a dual-lumen 7 Fr catheter at a minimum is required. The use of regional anticoagulation with citrate avoids the concerns of systemic anticoagulation and may reduce the risk of systemic bleeding. In general, children do better than adults; in fact, children usually recover completely from a renal insult if the hypoxia or ischemia lasted only a short time and other organ systems are not involved. Children with chronic renal failure require long-term outpatient peritoneal dialysis or hemodialysis until they can undergo renal transplantation. This syndrome is characterized by microangiopathic hemolytic anemia, thrombocytopenia, and acute renal injury. Infections can be spread by person-to-person contact in daycare centers, institutions, and the military. There is also a familial form of the disease that accounts for a small percentage of the total cases. In fact, some investigators consider the two disorders a continuum of the same disease. Toxin-induced damage to renal endothelial cells, the vasculature, and other organs is directly or indirectly associated with the activation of leukocytes. Patients usually have abdominal cramping, bloody diarrhea, tenesmus, and vomiting. Mildly affected patients exhibit anemia, thrombocytopenia, azotemia, and decreased urine output, and have an uncomplicated course. In severely affected patients, anuria is common, hypertension and seizures may occur, and the duration of illness is prolonged. A small number of children exhibit progressive and permanent renal insufficiency, severe and recurrent hemolysis, thrombocytopenia, and neurologic impairment. Hemolysis often causes hyperbilirubinemia and, despite reticulocytosis, severe anemia with hemoglobin concentrations of 4 to 5 g/dL. Thrombocytopenia is the result of platelet destruction and sequestration in the liver and spleen. Acute renal failure with oliguria or anuria usually lasts less than a week but may linger for more than 10 weeks. Meticulous attention should be paid to volume status, electrolyte and acid-base balance, nutrition, antisepsis, and treatment of hypertension and coagulopathies. Accurate fluid intake and output measurements and frequent assessment of weight and volume status are important for management of these patients. If nephrotoxic drugs must be given, the drug dose should be adjusted and serum concentrations monitored closely. Daily fluids should be restricted to the amounts required to replace insensible losses, urine output, and other ongoing losses. Enteral feedings are preferred, but parenteral feeding may be necessary if ileus develops. Dialysis, improved nutrition, and supportive care have decreased the mortality rate from 100% in the original report to less than 10% in the last 30 years. Congenital adrenal hyperplasia, pheochromocytoma, and iatrogenic chronic adrenal insufficiency will be discussed briefly. Congenital Adrenal Hyperplasia Congenital adrenal hyperplasia is an autosomal recessive disorder that is associated with deficiencies in either 21-, 11-, or 17-hydroxylase. This condition is usually manifested in the first few weeks of life as feeding difficulty, vomiting, and failure to thrive. If the deficiency is not diagnosed and treated early in life, affected children may suffer severe cardiovascular collapse. Treatment requires aggressive support of intravascular volume and myocardial function, glucose, and replacement of the deficient hormones. Cortisol can be replaced by oral administration of hydrocortisone at a dose of 25 mg/ m2/day divided into three doses; if the child cannot tolerate oral medication, cortisone acetate can be administered intramuscularly at a dose of 37. For emergency therapy, when the oral route is not possible and perfusion of the muscle is poor, hydrocortisone acetate is used intravenously at a bolus dose of 1. Deficiencies of 11- and 17-hydroxylase do not result in salt wasting; masculinization and hypertension are the common initial signs Pheochromocytoma Less than 5% of pheochromocytomas are diagnosed in childhood. As a rule, these tumors are confined to the adrenal medulla, but they can occur anywhere throughout the sympathetic chain. The clinical signs and symptoms of excessive catecholamines are the same as those in adults. Such use may cause a hypoadrenal state and increase the risk for cardiovascular collapse during a severe illness or stress. Replacement of stress-level steroids (three times the daily replacement dose) is required. Anterior Pituitary Panhypopituitarism is usually secondary to a tumor or to aggressive dissection of a tumor. This syndrome is precipitated by a number of mechanisms, including head trauma, neurosurgery, meningitis, hypoxia, and any major surgical procedure in which there is large-volume fluid shifts and fluid replacement. This syndrome is treated by fluid restriction and, in severe cases, by the infusion of hypertonic or isotonic saline. However, it is uncommon to find a blood glucose level below 40 mg/dL in normal, nourished premature, or term neonates. The usual symptoms of hypoglycemia include tachycardia, diaphoresis, weakness, mental clouding, seizures, and coma. The causes of hypoglycemia can be subdivided into disorders of increased utilization and disorders of decreased production. Transient hypoglycemia of the newborn is caused by decreased or immature hepatic gluconeogenesis and it self-corrects within hours to days. If the hypoglycemia persists, hepatic enzyme deficiencies, endocrine problems, or hyperinsulinism. Other causes of hypoglycemia in the neonatal period include sepsis, hypothermia, hypoxia, and transplacental exposure to maternal hypoglycemic drugs. In older children, hypoglycemia is associated with ketotic hypoglycemia,569 hepatic enzyme abnormalities, hyperinsulinism, hepatic failure, and Reye syndrome, and it is a side effect of certain drugs. Regardless of cause, the initial treatment of hypoglycemia is glucose administration. The second category of patients with hyperglycemia in critically ill children are those who develop elevated glucose during treatment for their underlying disease process, likely due to stress biology. The clinical syndrome includes dehydration and hypovolemic shock from hyperglycemic osmotic diuresis, compensatory hyperventilation (Kussmaul pattern), life-threatening electrolyte depletion, and in cases of severe metabolic imbalance, neurologic obtundation and coma. Adequate intravascular volume is restored with an isotonic glucose-free solution, combined with exogenous insulin administration, commonly referred to as a "two-bag system. Most clinicians continue the insulin infusion until the acidosis is nearly corrected. These children have total-body potassium depletion, but potassium should not be added to any infusion until there is urine output.
10 mg lotrisone fast delivery
Systematic review: the epidemiology and natural history of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis in adults antifungal leaves purchase 10 mg lotrisone otc. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. Prevalence of minor depression in elderly persons with and without mild cognitive impairment: a systematic review. Measures of executive function and depression identify patients at risk for postoperative delirium. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. Optimized antidepressant therapy and pain self-management in primary care patients with depression and musculoskeletal pain: a randomized controlled trial. Perioperative use of selective serotonin reuptake inhibitors and risks for adverse outcomes of surgery. Postoperative cognitive dysfunction: minding the gaps in our knowledge of a common postoperative complication in the elderly. Developed in collaboration with the American College of Surgeons, American Society of Anesthesiologists, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Anesthesiologists, and Society of Vascular Medicine Endorsed by the Society of Hospital Medicine. Preoperative cognitive stratification of older elective surgical patients: a cross-sectional study. Degree of discrepancy between self and other-reported everyday functioning by cognitive status: dementia, mild cognitive impairment, and healthy elders. Frailty for surgeons: review of a National Institute on Aging Conference on Frailty for specialists. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. Association of a frailty screening initiative with postoperative survival at 30, 180, and 365 days. Surgical palliative care consultations over time in relationship to systemwide frailty screening. Discrepancies between surgery and anesthesiology preoperative medication histories. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. Age changes in pain perception: a systematicreview and meta-analysis of age effects on pain and tolerance thresholds. Sustainability and scalability of the hospital elder life program at a community hospital. Effect of a modified hospital elder life program on delirium and length of hospital stay in patients undergoing abdominal surgery: a cluster randomized clinical trial. Screening for cognitive impairment in older adults: a systematic review for the U. Preoperative mild cognitive dysfunction predicts pulmonary complications after coronary artery bypass graft surgery. The prevalence and impact of undiagnosed cognitive impairment in older vascular surgical patients. Pre-operative mild cognitive dysfunction predicts risk for post-operative delirium after elective cardiac surgery. Sensitivity and specificity of the animal fluency test for predicting postoperative delirium. The cognitive disorders examination (Codex) is a reliable 3-minute test for detection of dementia in the elderly (validation study on 323 subjects). Codex (cognitive disorders examination) for the detection of dementia and mild cognitive impairment. Delirium in older people after proximal femoral fracture repair: role of a preoperative screening cognitive test. Monitoring depth of anaesthesia in a randomized trial decreases the rate of postoperative delirium but not postoperative cognitive dysfunction. Recommended best practices for postoperative brain health from the 2016 perioperative neurotoxicity working group summit. Initial results of a large multidisciplinary prospective study examining preoperative variables predictive of poor surgical outcomes. Frailty as a predictor of morbidity and mortality in in patient head and neck surgery. Simplified frailty index to predict adverse outcomes and mortality in vascular surgery patients. Predictors of critical care-related complications in colectomy patients using the National Surgical Quality Improvement Program: exploring frailty and aggressive laparoscopic approaches. Association of a modified frailty index with mortality after femoral neck fracture in patients aged 60 years and older. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. Simple frailty score predicts postoperative complications across surgical specialties. Successful emergency airway management is based on having a clear plan, such as the American Society of Anesthesiologists algorithm for difficult airways adapted for trauma. In general, rapid sequence induction of anesthesia and in-line cervical stabilization, followed by direct laryngoscopy or video laryngoscopy, is the safest and most effective approach. The use of cricoid pressure is controversial and is no longer a class I recommendation. Recognition of hemorrhagic shock is at the center of advanced trauma life support. Hemorrhagic shock indicates the need for rapid operative treatment, with the possibility of a damage control approach. Although establishing an adequate airway remains the initial priority, obvious hemorrhage should be concurrently addressed through immediate application of tourniquets or direct pressure. Resuscitation during acute hemorrhagic shock has undergone a significant change in emphasis. Current recommendations are to allow permissive hypotension during active bleeding by limitation of crystalloid infusion. Recognizing the impact of early coagulopathy in trauma, a "hemostatic" resuscitation should be employed, with an emphasis on maintenance of blood composition by early transfusion of red blood cells, plasma, and platelets, and viscoelastic monitoring when available. Management of patients with severe traumatic brain injury requires monitoring and maintenance of cerebral perfusion and oxygenation for successful operative and intensive care management. Operative timing for the surgical management of traumatic injuries, including orthopedic trauma, must be balanced between early definitive repairs and the potential for worsening overall physiologic stress. Trauma anesthesiology includes a substantial component of critical care practice (see also Chapter 83). For both children and adults younger than age 45, traumatic injuries remain the leading cause of death in the United States. Community-based prevention has included efforts to incorporate airbags in motor vehicles, mandate the use of helmets on motorcycles, encourage citizens to wear seat belts, punish intoxicated drivers, and promote responsible handgun ownership. All these measures have had an impact on the demographics of injury in much the same manner that smoking cessation, dietary modification, and routine mammography have affected the incidence of heart disease and cancer. Trauma center designation is a process outlined and developed at a state or local level. A trauma system is an example of tiered regionalization because the most seriously injured patients in a geographical catchment area are cared for at designated tertiary care trauma centers. The needs of orthopedic and reconstructive surgery patients are outlined and the chapter concludes with a discussion of postoperative issues for the anesthesiologist managing the trauma patient. Estimations of blood loss are imprecise and classically taught shock classifications are commonly confounded by extremes of age and variations in physiological reserve. This collar may be kept in place for several days before the complete gamut of tests to rule out cervical spine instability have been completed (see later discussion).