Purchase plendil 5 mg with mastercard
Because this therapy is potentially toxic to the kidneys blood pressure chart time of day order discount plendil on-line, ascorbic acid should not be administered to patients with compromised renal function. Frequent use of nonpreserved topical lubricants helps facilitate epithelial healing in the acute and chronic stages of chemical injury. Necrotic corneal epithelium should be debrided to minimize the release of inflammatory mediators from damaged epithelial cells and to promote reepithelialization. A bandage contact lens may be beneficial for protecting ocular surface epithelium once migration onto the peripheral cornea has begun; however, acute conjunctival swelling and inflammation or late symblepharon formation may prevent retention of the contact lens. A temporary or permanent tarsorrhaphy facilitates reepithelialization due to increased corneal coverage, but as with contact lens use, the drawback is the increased risk of infection in eyes with compromised defense 384 External Disease and Cornea mechanisms. If scleral melting occurs, a rotational graft of tarsoconjunctival tissue from the adjacent eyelid can be performed to promote revascularization. Limbal stem cell transplantation may be performed as soon as 2 weeks after chemical injury if no signs of corneal epithelialization have appeared. However, the prognosis of limbal grafts is better when the eye is not very inflamed; therefore, it is preferable to wait until the acute inflammation has subsided. If there is damage to the conjunctiva of both eyes, then either amniotic membrane alone or oral mucosal grafts may be necessary. The long-term prognosis for a corneal transplant is improved if the ocular surface inflammation has resolved either over time (months to years) or after limbal stem cell grafting (ocular surface reconstruction), if necessary. Even when there is no active ocular surface inflammation, stromal vascularization in the host bed is associated with a much higher risk of rejection in these keratoplasty cases. Keratoprosthesis is another surgical option for these patients, but again, the prognosis is best when the inflammation has been brought under control. The modified Cincinnati procedure: combined conjunctival limbal autografts and keratolimbal allografts for severe unilateral ocular surface failure. Injuries Caused by Temperature and Radiation Thermal Burns Heat Heat is a primary cause of inflammation and stromal protease expression and can lead to collagen melting if severe. Rapid-reflex eyelid closure, Bell phenomenon, and reflex movement away from the source of intense heat usually limit damage to the globe from flames. Burns from molten metal that stays in contact with the eye are more likely to cause corneal injuries that result in permanent scarring. These burns are usually limited to the epithelium and generally require only a brief period of antibiotic and cycloplegic therapy. Prophylactic antibiotics (topical and/or systemic) can help prevent infection of burned eyelids and/or reduce the chances of infectious corneal ulceration. Limited debridement of devitalized tissues and granulation tissue, used with full-thickness skin grafts and tarsorrhaphy, helps minimize eyelid scarring and ectropion. Burned ocular tissue can be protected temporarily by covering the eye with a lubricant and a piece of sterile plastic wrap. Topical corticosteroids help suppress any associated iridocyclitis, but they can also inhibit corneal wound healing and must be used with caution and, in general, for short periods. Freezing Transient corneal stromal edema induced by cold has been reported in a variety of settings, including prolonged exposure to cold when skiing or mountain climbing. Individuals with Raynaud disease and those with cranial nerve V (trigeminal) dysfunction may be especially susceptible. Research suggests that sensory denervation of the eye increases the susceptibility of the endothelium to cold temperatures. Treatment consists of patching to minimize discomfort from eyelid movement, use of a topical antibiotic ointment, and cycloplegia. Ionizing radiation can damage the conjunctiva, cornea, and occasionally the lacrimal glands. Conjunctival edema occurs acutely, often followed by scarring, shrinkage, loss of tear production, and alterations in conjunctival blood vessels with telangiectasia. Necrosis of the conjunctiva and underlying sclera can occur if radioactive material (or a radiomimetic agent such as mitomycin C) is embedded in the conjunctiva. Explosions involving ionizing radiation may lead to perforation of ocular tissues with immediate radiation necrosis. The first step in management of acute radiation injury is removal of all foreign bodies. Late complications are related to decreased tear production, loss of corneal sensation, sloughing of corneal epithelial cells, and failure of the cornea to heal. Secondary microbial keratitis, vascularization, and ocular surface disease can result from dry eyes and compromised epithelial cells. The use of artificial tears or a bandage contact lens may help stabilize the ocular surface in mild cases. If there is recurrent epithelial breakdown despite these measures, significant conjunctival scarring typically precludes the use of a conjunctival flap from that eye. If the fellow eye has not been injured, a contralateral autologous conjunctival flap may be helpful. Alternatively, an amniotic membrane transplant, limbal stem cell transplant, or mucous membrane graft may be employed. The visual prognosis associated with penetrating keratoplasty or limbal stem cell transplantation in these situations is guarded because of the severely compromised ocular surface. Injuries Caused by Animal and Plant Substances Insect and Arachnid Injuries Bee and wasp stings to the cornea and/or conjunctiva cause conjunctival hyperemia and chemosis acutely, sometimes associated with severe pain, corneal edema, and infiltration, with subsequent decreased vision. The significant variability in the acute response is thought to reflect differences in the quantity of the venom injected and whether the reaction to the venom is primarily toxic or immunologic. Initial therapy with cycloplegics and topical (and occasionally systemic) corticosteroids is beneficial. After the acute episode, retained stingers may remain inert in the cornea for years. Caterpillar and tarantula hairs (urticating hairs) may also become embedded in the cornea and conjunctiva. Because of their structure, these urticating hairs tend to migrate more deeply into ocular tissues and elicit a localized granulomatous inflammatory response (ophthalmia nodosum). In these cases, the patient will have an extreme foreign-body sensation until the hairs migrate below the corneal surface. Vegetative Injuries Ocular contact with the milky sap (latex) from a variety of trees can cause toxic reactions manifested by acute keratoconjunctivitis, epithelial defects, and stromal infiltration. The pencil tree and the manchineel tree, widely distributed in tropical regions, are known offenders. Houseplants in the genus Dieffenbachia are known to cause keratoconjunctivitis from calcium oxalate crystals in the cornea; crunching the leaves can cause these crystals to shoot into the cornea. Corneal foreign bodies from coconut shell, sunflower stalk, and ornamental cactus have also been documented. Initial management of injuries caused by all such plant materials should include irrigation and removal of foreign bodies when possible and administration of topical cycloplegics with prophylactic antibiotic coverage, as indicated by the clinical situation. Corticosteroids are best avoided, as they suppress immunity to microbes in general and may promote fungal infection specifically, which is of concern in all cases involving vegetable matter because plant sources are common causes of fungal keratitis. Surgical removal of vegetative foreign bodies should be attempted in order to mitigate the inflammatory response or associated secondary microbial infections. If a patient with a severe injury from plant sources fails to improve after supportive therapy, the possibility of bacterial or fungal infection should be considered and appropriate workup (including culturing and/ or biopsy) performed. Patients with subconjunctival hemorrhage typically have no history of antecedent trauma. Subconjunctival hemorrhage is usually not associated with an underlying systemic disease and rarely has an identifiable cause. Occasionally, a history of vomiting, coughing, or other forms of the Valsalva maneuver can be elicited.
5 mg plendil with mastercard
It eliminates a full-thickness corneal incision into the anterior chamber arteria zygomatica purchase 2.5 mg plendil otc, thereby avoiding the risks of glaucoma, cataract, retinal detachment, cystoid macular edema, expulsive hemorrhage, and endophthalmitis. Because the endothelium is not transplanted, it also eliminates the risk of endothelial rejection and, consequently, decreases the need for topical steroids. Disadvantages Anterior lamellar keratoplasty does not replace damaged endothelium. There are many techniques for dissecting stromal tissue to expose the Descemet membrane, including the Anwar big-bubble technique (see Videos 15-5 and 15-6 for animations of the big-bubble technique), the Melles technique, and, more recently, the use of the femtosecond laser. As discussion of these techniques is beyond the purview of this chapter, the reader is encouraged to consult the references that follow. Even in experienced hands, it may not always be possible to expose the Descemet membrane using these techniques. In these cases, manual dissection is possible, but it poses a risk of reduced best-corrected visual acuity due to incomplete removal of the host stromal tissue and secondary interface haze. Quality of vision and graft thickness in deep anterior lamellar and penetrating corneal allografts. Deep anterior lamellar keratoplasty versus penetrating keratoplasty: a meta-analysis of randomized controlled trials. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty: a report by the American Academy of Ophthalmology. Irrigation and cleaning of the lamellar bed at the time of surgery reduces the likelihood of postoperative opacification. Retained interface debris, secondary vascularization, microbial infections, or wrinkling of the Descemet membrane can reduce vision or prolong vision rehabilitation. Neovascularization can increase the risk of lipid keratopathy, leading to further corneal opacification. Allograft rejection Because the corneal endothelium is not transplanted, endothelial rejection cannot take place. Epithelial rejection, subepithelial infiltrates, and stromal rejection can still occur, but they usually respond to corticosteroid therapy. Complications unique to deep anterior lamellar keratoplasty Rupture of the Descemet membrane If there is a small rupture, the procedure may still be completed but may result in a Descemet detachment (see the following discussion). Double anterior chamber or Descemet detachment Descemet detachment or double (pseudo) anterior chambers can occur because of fluid in the interface, which results from a host perforation or retained viscoelastic material. Injection of air into the anterior chamber can help with reattachment; however, it may also reduce the endothelial cell count and lead to the development of an anterior subcapsular cataract. Reduced postoperative visual acuity is another potential drawback and is discussed separately in the following subsection. This alteration is due to the unevenness and thickness of the donor tissue and the irregularity of the interface between the donor stromal tissue and the host Descemet membrane. Corneal haze determined by confocal microscopy 2 years after Descemet stripping with endothelial keratoplasty for Fuchs corneal dystrophy. The first 100 eyes of standardized Descemet stripping automated endothelial keratoplasty versus standardized Descemet membrane endothelial keratoplasty. Descemet membrane endothelial keratoplasty versus Descemet stripping automated endothelial keratoplasty. Effect of graft thickness on visual acuity after Descemet stripping endothelial keratoplasty: a systematic review and meta-analysis. A soft eye due to a preexisting tube shunt or uncontrolled release of the air increases the likelihood of a decentered or dislocated graft. Retained viscoelastic or the presence of vitreous in the interface may prevent proper adherence of the graft. If the graft remains attached on postoperative day 1, subsequent dislocation is unlikely, although inadvertent trauma or eye rubbing during the first week may displace the donor tissue. Wearing glasses or a shield to protect the eye is recommended, along with exercising caution during instillation of eyedrops. Peripheral detachments not involving the visual axis can be observed over several weeks to ensure there is no progression. If the graft detachment extends into the visual axis or is greater than one-third of the graft area, the surgeon may consider additional injection of air (rebubbling) to tamponade the graft against the host. Initially, rebubbling was not advised because of reports of extensive, visually significant detachments resolving spontaneously. Repeat Descemet membrane endothelial keratoplasty after complicated primary Descemet membrane endothelial keratoplasty. Prevention and management of graft detachment in Descemet membrane endothelial keratoplasty. Pupillary block may also lead to iridocorneal adhesion, damaging the graft and increasing the risk of rejection. Pupil dilation and supine positioning may relieve the pupil block; if this fails, some air should be removed. An inferior iridectomy performed prior to or at the time of the surgery reduces the likelihood of this scenario. It typically remains stable and is asymptomatic unless it occurs in the visual axis. Host epithelium can be pushed into the eye through the main wound, side ports, or venting incisions used to drain interface fluid. Loose donor epithelium may enter the eye if adherent to the donor corneal button because of eccentric trephination beyond the microkeratome excision. In rare cases, epithelial ingrowth leads to graft failure that is missed on clinical examination but recognized on histologic examination of the tissue after removal. In a large series of cases, the majority of patients with epithelial ingrowth were simply observed and continued to see well without further intervention. Epithelial ingrowth after Descemet stripping automated endothelial keratoplasty: description of cases and assessment with anterior segment optical coherence tomography. Interface opacification may occur because of retention of fibers, incomplete removal of the Descemet membrane, and persistence of interface fluid. Textural interface opacity describes a recently reported finding that results from retained viscoelastic or from the shearing of stromal fibrils during an irregular microkeratome donor preparation. Textural interface opacity may be associated with reduced vision, but it typically improves or disappears completely over many months. Textural interface opacity after Descemet stripping automated endothelial keratoplasty: a report of 30 cases and possible etiology. Phakic Descemet stripping automated endothelial keratoplasty: prevalence and prognostic impact of postoperative cataracts. The lower rates probably reflect better surgical technique, which results in less tissue manipulation and a lower rate of graft dislocations and thus less endothelial trauma. In contrast, in a study by Ratanasit and Gorovoy, where all patients were maintained on topical steroids indefinitely, the rejection rate was 2% after 5 years in 51 eyes. If the patient is a steroid responder, loteprednol etabonate or fluorometholone may be substituted. The authors of that study report that the incidence of graft rejection was 0% for patients who continued using topical steroids through the second year but increased to 6% in the second year in patients who stopped the steroids after 1 year. The graft rejections experienced were mild and asymptomatic, and all but one reversed with resumption of steroid therapy. Incidence of early allograft rejection after Descemet membrane endothelial keratoplasty. Graft rejection following Descemet stripping automated endothelial keratoplasty: features, risk factors, and outcomes. Long-term viability of the endothelial cells is influenced by ocular comorbidity such as previous filtering surgery and, in particular, tube shunts. Outcomes after Descemet stripping automated endothelial keratoplasty in patients with glaucoma drainage devices. Descemet stripping endothelial keratoplasty: ten-year endothelial cell loss compared with penetrating keratoplasty.
Syndromes
- Back pain
- Use a sunscreen on your lips when outside in sunny weather
- Withdrawal from family or friends
- Cystic fibrosis
- Chromosomal abnormalities (such as Down syndrome)
- Reduce stress -- try to avoid things that cause you stress. You can also try meditation or yoga.
- Eat a balanced diet with plenty of vitamins and minerals
- Swelling in the parathyroid glands, called primary hyperparathyroidism
- Certain cancers, such as multiple myeloma, a cancer of the breast, lung, neck, and kidney, especially during cancer treatment
Cheap plendil 2.5 mg overnight delivery
Brachial Plexopathy 85 Physical Modalities Physical and occupational therapy to maintain function and palliate pain is a crucial part of the treatment plan for patients suffering from brachial plexopathy blood pressure natural remedies generic plendil 10 mg with visa. Shoulder abnormalities, including subluxation and adhesive capsulitis, must be treated aggressively. Occupational therapy to assist in activities of daily living is important to avoid further deterioration of function. It responds poorly to opioid analgesics and may respond poorly to the medications discussed. The uncontrolled pain of brachial plexopathy can lead to suicide, and strong consideration should be given to hospitalizing such patients. Correct diagnosis of the underlying cause is crucial to the successful treatment of the pain and dysfunction associated with brachial plexopathy, because stretch injuries and contusions of the plexus may respond with time, but plexopathy secondary to tumor or avulsion of the cervical roots requires aggressive treatment. Baclofen Baclofen may be of value in some patients who fail to obtain relief from gabapentin or carbamazepine. Baseline laboratory tests should be obtained before starting baclofen, and the patient should be cautioned about potential adverse effects, which are the same as those associated with carbamazepine and gabapentin. Baclofen is started with a 10-mg dose at bedtime for 2 nights; the dosage is then increased in 10-mg increments given in equally divided doses over 7 days, as side effects allow, until pain relief is obtained or a total dose of 80 mg/day is reached. Invasive Therapy Brachial Plexus Block Brachial plexus block with local anesthetic and steroid is an excellent adjunct to drug treatment. This technique rapidly relieves pain while medications are being titrated to effective levels. The initial block is carried out with preservative-free bupivacaine combined with methylprednisolone. Subsequent daily nerve blocks are carried out in a similar manner, substituting a lower dose of methylprednisolone. This procedure is reserved for patients who have failed to respond to all aforementioned treatments and whose pain is secondary to tumor or avulsion of the brachial plexus. Dorsal Root Entry Zone Lesioning Dorsal root entry zone lesioning is the neurosurgical procedure of choice for intractable brachial plexopathy in patients who have failed to respond to all aforementioned treatments and whose pain is secondary to tumor or avulsion of the brachial plexus. Diagnosis is usually delayed, and patients are often erroneously treated for cervical radiculopathy or primary shoulder disease until the diagnosis becomes clear. Lateral herniated cervical disk, metastatic tumor, or cervical spondylosis that results in significant nerve root compression may also manifest as brachial plexopathy. Initially, the lower portion of the brachial plexus is involved because the tumor growth is from below, causing pain in the upper thoracic and lower cervical dermatomes. The pain is neuritic and may take on a deep, boring quality as the tumor invades the brachial plexus. Movement of the neck and shoulder exacerbates the pain, so patients often try to avoid such movement. Based on the cell type and extent of involvement, chemotherapy and radiation therapy may be indicated. Primary surgical treatment of tumors involving the brachial plexus is difficult, and the results are often disappointing. Although neuropathic pain generally responds poorly to opioid analgesics, given the severity of the pain and the lack of other options, a trial of opioid analgesics is warranted. Administration of a short-acting, potent opioid such as oxycodone is a reasonable starting point. A, Most posterior image with the horizontal course of the T1 nerve root (long arrow), very close to the lung apex. C, T2-weighted short tau inversion recovery image at the same level as B shows the slightly increased signal intensity of the normal C8 nerve roots (arrows). A, this 58-yearold man presented with chronic left arm and shoulder pain along with progressive weakness of his lower arm and hand. A 65-year-old man complained of severe pain in the shoulder radiating to the elbow, the medial side of the forearm, and the fourth and fifth fingers in an ulnar nerve distribution. Screening coronal T1-weighted magnetic resonance imaging shows the brachial plexus from the region of the roots (long arrows) to the region of the trunks and divisions, where tumor invasion (short arrow) and loss of fat planes on the left are seen. The drug is sometimes discontinued owing to laboratory abnormalities erroneously attributed to it. Carbamazepine should be initiated slowly if the pain is not out of control at a starting dose of 100 to 200 mg at bedtime for 2 nights. The patient should be cautioned about side effects, including dizziness, sedation, confusion, and rash. Careful monitoring of laboratory parameters is mandatory to avoid the rare possibility of a life-threatening blood dyscrasia; at the first sign of blood count abnormality or rash, the drug should be discontinued. When pain relief is obtained, the patient should be kept at that dosage of carbamazepine for at least 6 months before tapering of the medication is considered. These drugs can be used in combination with nonsteroidal antiinflammatory drugs and the adjuvant analgesics described here. Carbamazepine Carbamazepine is useful in patients who do not obtain pain relief with gabapentin. Despite the safety and efficacy of Baclofen Baclofen may be of value in some patients who fail to obtain relief from the previously mentioned medications. Baclofen is started with a 10-mg dose at bedtime for 2 nights; the drug is then increased in 10-mg increments given in equally divided doses over 7 days, as side effects allow, until pain relief is obtained or a total dose of 80 mg/day is reached. Subsequent daily nerve blocks are performed in a similar manner, by substituting a lower dose of methylprednisolone. Radiofrequency Destruction of the Brachial Plexus the brachial plexus can be destroyed by creating a radiofrequency lesion under biplanar fluoroscopic guidance. This procedure is reserved for patients for whom all aforementioned treatments have failed. With intravenous gadolinium, the nonenhancing nerve roots can be discerned from the enhancing tumor, and tumor is visible up to the C5 nerve root. Other Neurosurgical Options Cordotomy, deep brain stimulation, and thalamotomy have all been tried, with varying degrees of success. A, Computed tomography of the tumor (T) with region of interest (green line) around the tumor, ipsilateral side of spine, and the chest wall (red arrow). B, Three-dimensional (3D) rendering of extracted topology showing tumor (T), spine, and chest wall. D, Thoracoscopic image of the resection of the chest wall and laminectomy with tumor (T) invading the third rib. Management of tumors involving the chest wall including pancoast tumors and tumors invading the spine. Correct diagnosis is paramount to allow the clinician to design a logical treatment plan. Cervicothoracic tumors and aneurysms must also be considered when evaluating a patient with thoracic outlet syndrome. One or all the structures may be compressed, thus giving the syndrome a varied clinical expression. Thoracic outlet syndrome is seen most commonly in women between 25 and 50 years of age. It has been the subject of significant debate, and the diagnosis and treatment of thoracic outlet syndrome remain controversial. Paresthesias of the upper extremity radiating into the distribution of the ulnar nerve may be misdiagnosed as tardy ulnar palsy. If the pain persists, abnormal position of the shoulder girdle to relieve compression or entrapment of the neurovascular structures may be observed. If vascular compression exists, edema or discoloration of the arm may be noted; in rare instances, venous or arterial thrombosis may occur. Rarely, the symptoms of thoracic outlet syndrome are caused by arterial aneurysm, and auscultation of the supraclavicular region reveals a bruit. The symptoms of thoracic outlet syndrome may be elicited by various maneuvers, including the Adson test, the Brachial plexus Subclavian a.
Purchase plendil 10mg overnight delivery
Stromal keratitis is caused by agents of the genus Nosema blood pressure instruments discount 10 mg plendil fast delivery, whereas the genera Encephalitozoon and Septata have been associated with keratoconjunctivitis. In the keratoconjunctivitis variant, corneal findings include superficial nonstaining opacities described as "mucoid" in appearance, along with dense areas of fine punctate fluorescein staining. Although there is no definitive treatment, topical fumagillin has been used to successfully treat microsporidial keratoconjunctivitis, with little toxic effect. In general, medical regimens require long-term use, and recurrence is common after treatment discontinuation. More recent cases have been reported to be self-limited or responsive to a wide array of commercially available topical ophthalmic antibiotics. Clinical and microbiological profile of microsporidial keratoconjunctivitis in southern India. Emerging prevalence of microsporidial keratitis in Singapore: epidemiology, clinical features, and management. After the bite of an infected vector, such parasites can burrow subcutaneously to reach the eye area. The microfilarial stage is transmitted from human to human by the bite of an infected female deer fly (genus Chrysops) indigenous to West and Central Africa. Extraction of the filarial worm cures the conjunctivitis; antiparasitic treatment for disseminated infestation follows. Diethylcarbamazine is generally given 2 mg/kg 3 times a day for 3 weeks and repeated as necessary. Ivermectin 150 mg/kg may also be effective, but significant adverse effects have been reported in patients with prominent intravascular loiasis. Concurrent administration of corticosteroids and/or antihistamines may be necessary to minimize allergic reactions. Most cases result from the extension of microbial keratitis involving the peripheral cornea. Trauma and contaminated foreign bodies (including scleral buckles) are possible risk factors. Bacteria and fungi can also invade tissue of the eye wall surrounding a scleral surgical wound, but endophthalmitis is more likely in this setting. Scleral inflammation can also be a feature of syphilis, tuberculosis, or leprosy, or infection with Acanthamoeba species, Nocardia species, or atypical mycobacteria. Diffuse or nodular scleritis is an occasional complication of varicella-zoster virus eye disease. If the overlying epithelium is intact, a scleral or episcleral biopsy should be performed to obtain specimens for culture, histologic examination, and molecular diagnostic testing. The workup of nonsuppurative scleritis is guided by the history and findings from the physical examination, as described in Chapter 11. Because of the difficulty in controlling microbial scleritis, subconjunctival injections and intravenous antibiotics may also be used. Hypersensitivity reactions are divided into 4 types in the Gell and Coombs classification. Type I (immediate hypersensitivity) reactions typically occur within minutes after exposure to an allergen. Patients are often sensitized by previous exposure to the offending drug or preservative. Sequelae of chronic contact blepharoconjunctivitis include hyperpigmentation, dermal scarring, and lower eyelid ectropion. Usually, the history provides the necessary clues, but sometimes a "challenge test" is necessary to confirm a suspicion. Such tests should never be done in patients with a known systemic allergy to a drug. Initial management of type I hypersensitivity reactions includes allergen avoidance or discontinuation of the causative agent. Topical vasoconstrictors, either alone or in combination with antihistamines, may provide acute symptomatic relief but should not be used long term. In severe cases, a brief (several-day) course of mild topical corticosteroids or tacrolimus ointment (0. Other ocular findings include periorbital darkening, exaggerated eyelid folds, meibomianitis, ectropion, and chronic papillary conjunctivitis. Infants typically have an erythematous rash, children tend to have eczematous dermatitis with secondary lichenification from scratching, and adults have scaly patches with thickened and wrinkled dry skin. Acute lesions can be controlled with a topical corticosteroid cream or ointment (clobetasone butyrate 0. Oral antipruritic agents such as antihistamines and mast-cell stabilizers can alleviate itching but may exacerbate dry eye with their anticholinergic activity. The allergen, which is typically airborne, enters the tear film and comes into contact with conjunctival mast cells that bear allergenspecific IgE antibodies. Degranulation of mast cells releases histamine and a variety of other inflammatory mediators that promote vasodilation, edema, and recruitment of other inflammatory cells, such as eosinophils. In a presensitized individual, the activation and degranulation of mast cells can be triggered within minutes of allergen exposure. Patients with hay fever conjunctivitis often have other atopic conditions, such as allergic rhinitis or asthma. Symptoms develop rapidly after allergen exposure and consist of itching, eyelid swelling, conjunctival hyperemia, chemosis, and mucoid discharge. Conjunctival scrapings reveal the characteristic eosinophils, which are not normally present on the ocular surface. Thorough cleaning (or changing) of unclean or old carpets, linens, and bedding can be effective in removing accumulated allergens such as animal dander and house dust mites. Contributing factors, including contact lenses and dry eye, should be identified, as they can play an important role in facilitating allergen contact with the ocular surface. Topical vasoconstrictors, alone or in combination with antihistamines, may provide acute symptom relief. Treatment effects usually require continued use over 7 or more days; hence, these drugs are generally ineffective in the acute phase of hay fever conjunctivitis. Topical cyclosporine and oral antihistamines may provide symptom relief in some patients. Hyposensitization injections (immunotherapy) can be beneficial if the offending allergen has been identified. Topical corticosteroids are very effective in managing ocular allergy; however, they should be reserved for cases unresponsive to other treatments and must be used with caution. If corticosteroids are prescribed, patients must be clearly informed of the risks and closely monitored for adverse effects. Recent patents and emerging therapeutics in the treatment of allergic conjunctivitis. It occurs predominantly in patients of African or Asian descent and is more prevalent in hot climates. The limbus has a thickened, gelatinous appearance, with scattered opalescent mounds and vascular injection. A randomized, placebocontrolled clinical trial of tacrolimus ophthalmic suspension 0. Punctate epithelial erosions in the superior and central cornea are frequently noted. Climatotherapy, such as the use of home air-conditioning or relocation to a cooler environment, can be helpful. Patients with mild to moderate disease may respond to topical mast-cell stabilizers. In patients with seasonal exacerbations, these drops are typically started at least 2 weeks before symptoms usually begin. Because of the likely development of corticosteroid-related complications from long-term administration, however, these drugs should be reserved for exacerbations that result in moderate to severe discomfort and/or decreased vision. Because of the propensity of particles of suspended corticosteroid (eg, prednisolone acetate) to lodge between papillae, the use of less potent but soluble corticosteroids such as dexamethasone phosphate is generally preferred. Whenever steroids are prescribed, the potential dangers of long-term topical corticosteroid use are critical to review to emphasize the importance of close follow-up and monitoring for adverse effects.
Purchase plendil 2.5 mg on line
The simplest model for these data is a straight line mean of all the responses (random noise level) shown by the dotted line: P y: (12 heart attack 720p kickass plendil 5mg generic. A more complex model for these data is a fourparameter logistic function of the form: 10 % Max. The sigmoidal curve indicates the best fit four-parameter logistic function to the data points. This shows that the fit to the complex model is statistically preferred (the fit to the sigmoidal curve is indicated). To be significant at the 95% level of confidence (5% chance that this F actually is not significant), the value of F for df 5 6, 10 needs to be. In this case, since F is greater than this value, there is statistical validation for usage of the most complex model. For the complex model, there are four values for max, n, and K; therefore, dfc 5 24 2 12 5 12. This complete procedure then is repeated for a model where the maxima and slopes of the curves are the average of the individual maxima and slopes. To be significant at the 95% level of confidence (5% chance that this F actually is not significant), the value of F for df 5 12, 18, needs to be. Therefore, since F is less than this value, there is no statistical validation for usage of the most complex model. The same conclusion can be drawn from another statistical test for model comparison, namely, through the 12. It can be seen that the lowest value corresponds to the fit with common maxima and slope; therefore, this fit is preferred. Detection of Differences in Curves There are instances where it is important to know the concentration of a drug, such as a receptor antagonist, which first produces a change in the response to an agonist. Calculation of F then can be used to resolve whether the data fit better to a single curve (indicating noise around the control curve and no antagonism) or two separate curves (antagonist produces a low level of receptor blockade). This value is not significant at the 95% level; therefore, there is no statistical support for the hypothesis that the more complex model of individual maxima and slopes is required to fit the data. In this case, a set of curves with common maximum and slope can be used to fit these data. This is often preferred, especially for automated data fitting, since it is simpler than F-tests and can be used with a wider variety of models. Calculation of F indicates that a statistically significant improvement in the fit was obtained by using the complex model (two curves; F 5 4. Therefore, the data indicate that the antagonist had an effect at this concentration. One feature of all these models (with the exception of some instances of the operational model) is that they predict symmetrical curves. Attempting to fit such data to symmetrical functions leads to a lack of fit on either end of the data set. There are a number of options, in terms of empirical models, for fitting asymmetrical data sets. The zero ordinate of this curve indicates the point at which the slope is zero (inflection point of the curve). Before the widespread availability of computer programs allowing nonlinear fitting techniques, linearizing data was a common practice because it yielded simple algebraic functions and calculations. However, as noted in discussions of Scatchard analysis (Chapter 4: Pharmacological Assay Formats: Binding) and double reciprocal analysis (Chapter 5: Agonists: the Measurement of Affinity and Efficacy in Functional Assays), such procedures produce compression of data points, abnormal emphasis on certain data points, and other unwanted aberrations of data. In general, these models are able to fit asymmetrical data sets but require the use of added parameters (thereby reducing degrees of freedom). There are instances where it is important to know whether a given regression line is linear. For example, simple competitive antagonism should yield a linear Schild regression (see Chapter 6: Orthosteric Drug Antagonism). A statistical method used to assess whether or not a regression is linear utilizes analysis of covariance. A prerequisite for this approach is that there must be multiple ordinates for each value of the abscissae. Specifically, it is easier for the eye to detect deviations from straight lines than from curves. Specifically, a bimolecular interaction between a ligand and a receptor predicts a sigmoidal binding curve (according to the Langmuir adsorption isotherm) with a slope of unity if there is no cooperativity in the binding. This means that the binding of one ligand to the receptor population does not affect the binding of another ligand to the population. While there are differences between the curves, they must be compared to each other to detect them. This is because the eye is accustomed to identifying linear plots (no cooperativity, n 5 1) and therefore can identify nonlinear regressions with no required comparison. Analysis of Covariance There are methods available to test whether or not two or more regression lines statistically differ from each other in the two major properties of lines in Euclidean space, namely, position (or elevation) and slope. Schild regressions for phentolamine antagonism of norepinephrine responses in rat anococcygeus muscle. A Schild regression for an antagonist in a given receptor preparation is equivalent to a fingerprint for that receptor and antagonist combination. Under these circumstances, all Schild regressions for a given antagonist in a given uniform preparation should be equivalent for blockade of all agonists for that receptor. However, if there is receptor heterogeneity and the antagonist does not have equal affinity for the receptor types, then unless the agonists used to elicit response have identical efficacy for the receptor types, there will be differences in the Schild regressions for the antagonist when different agonists are used. Before the advent of recombinant systems, natural cells and/or tissues were the only test systems available, and often these contained mixtures of receptor subtypes. Therefore, a test of possible receptor heterogeneity is to use a number of agonists to elicit response and block these with a single antagonist; this is a common practice for identifying mixtures of receptor populations. Conformity of Schild regressions suggests no receptor heterogeneity; a useful way to compare Schild regressions is by analysis of covariance of regression lines. If a mixture of two receptors mediates responses in this tissue, then responses to the selective agonists should be differentially sensitive to the 1-adrenoceptor-selective antagonist. The procedure for determining possible differences in slope of the regressions is given in Table 12. The resulting F value indicates that there is no statistical difference in the slopes of the Schild regressions obtained with each agonist. The procedure for determining possible differences in position of regression lines is given in Table 12.
Buy plendil 2.5 mg line
In general arrhythmia on ecg buy discount plendil 2.5 mg on line, the kinetics of most allosteric modulators has been shown to be faster than the kinetics of binding of the tracer ligand. El-Fakahany, Positive and negative allosteric interactions on muscarinic receptors, Eur. Allosteric modulators (antagonists) will generally decrease the rate of association and/or increase the rate of dissociation of the tracer ligand. The conclusions drawn from a system where the binding of the ligand changes the receptor are different. One such process is agonist binding, in which, due to the molecular property of efficacy, the agonist produces a change in the receptor upon binding to elicit a response. Under these circumstances, the simple schemes for binding discussed for antagonists may not apply. For the purposes of binding, this process can lead to an aberration in the binding reaction as perceived in experimental binding studies. Specifically, the activation of the receptor with subsequent binding of that receptor to another protein (to form a ternary complex of receptor, ligand, and G-protein) can lead to the apparent observation of a "high-affinity" site-a ghost site that has no physical counterpart but appears to be a separate binding site on the receptor. If a ligand predisposes the receptor to bind to G-protein, then the presence of G-protein will drive the binding reaction to the right. Therefore, the property of the ligand that causes the formation of the ternary ligand/receptor/G-protein complex (in this case, efficacy) will cause the ligand to have a higher affinity than it would have if the receptor were present in isolation (no G-protein present). As shown in this figure, the muscarinic agonist oxotremorine has a receptor equilibrium dissociation constant of 6 M in a reconstituted phospholipid vesicle devoid of G-proteins. Displacement in reconstituted phospholipid vesicles (devoid of Gprotein subunits) shown in open circles. Sternweis, Mechanism of muscarinic receptor action on Go in reconstituted phospholipid vesicles, J. However, upon addition of G0 protein, the affinity increases by a factor of 600 (10 nM). The previous discussion assumes that there is no limitation on the stoichiometry relating receptors and Gproteins. In recombinant systems, where receptors are expressed in surrogate cells (often in large quantities), it is possible that there may be limited quantities of Gprotein available for complexation with receptors. Under these circumstances, complex saturation and/or displacement curves can be observed in binding studies. Dotted line indicates a single phase displacement binding curve with a slope of unity. Data shown for (1) 2-phenylaminoadenosine, (2) 2-chloroadenosine, (3) 50 -N-8ethylcarboxamidoadenosine, (4) N6-cyclohexyladenosine, (5) (2)-(R)-N6-phenylisopropyladenosine, and (6) N6-cyclopentyladenosine. It can be seen that the displacement curve has two distinct phases: a high-affinity (presumably due to coupling to G-protein) binding process followed by a lower affinity binding (no benefit of Gprotein coupling). While high-affinity binding due to ternary complex formation (ligand binding to the receptor followed by binding to a G-protein) can be observed in isolated systems where the ternary complex can accumulate and be quantified, this effect is canceled in systems where the ternary complex is not allowed to accumulate. Under these conditions, the G-protein complex does not accumulate, and the coupling reaction promoted by agonists is essentially nullified (with respect to the observable radioactive species in the binding reaction). When this occurs, the high-affinity state is not observed in the binding experiment. Under these circumstances, the high-affinity binding of agonists is not observed, only the so-called low-affinity state of agonist binding to the receptor. It can be seen from this figure that a phase shift for the affinity of the agonists under these two binding experiment conditions is observed. The broken-cell preparation reveals the effects of the ability of the agonists to promote G-protein coupling of the receptor. Thus, ligands that have a high observed affinity in broken-cell systems often have a high efficacy. A measure of this efficacy can be obtained by observing the magnitude of the phase shift of the affinities measured in broken-cell and whole-cell systems. The previous discussions indicate how binding experiments can be useful in characterizing and quantifying the activity of drugs (provided the effects are detectable as changes in ligand affinity). As for any experimental procedure, there are certain prerequisite conditions that must be attained for the correct application of this technique to the study of drugs and receptors. A short list of required and optimal experimental conditions for successful binding experiments is given in Table 4. Some special experimental procedures for determining equilibrium conditions involve the adjustment of biological material. On the one hand, increasing receptor (Bmax) also increases the signal strength and usually the signal-tonoise ratio. On the other hand, a very important prerequisite to the use of the Langmuirian type kinetics for binding curves is that the binding reaction does not change the concentration of tracer ligand being bound. Ideally, the T amount of receptor (magnitude of Bmax) should not limit the amount of [A*R] complex formed and there should be a linear relationship between [A*R] and Bmax. A graph of [A*R] for a concentration of [A*] 5 3 3 Kd as a function of Bmax is shown in 180 160 140 120 100 80 60 40 20 0 0. The binding is saturable the binding is reversible and able to be displaced by other ligands There is a ligand available to determine nonspecific binding There is sufficient biological binding material to yield a good signal-to-noise ratio but not too much so as to cause depletion of the tracer ligand For optimum binding experiments, the following conditions should be met: There is a high degree of specific binding and a concomitantly low degree of nonspecific binding Agonist and antagonist tracer ligands are available the kinetics of binding are rapid the ligand used for determination of nonspecific binding has a different molecular structure from the tracer ligand 4. It can be seen that as Bmax increases, the relationship changes from linear to curvilinear as the receptor begins to deplete the tracer ligand. Lower concentrations are affected at lower Bmax values than are higher concentrations. When Bmax levels are exceeded (beyond the linear range), saturation curves shift to the right and do not come to an observable maximal asymptotic value. For displacement curves, a similar error occurs with excess protein concentrations. The concentration of [A*R] in the presence of a nontracer-displacing ligand [B] as a function of Bmax is given by (see Section 4. Values of Bmax greater than the vertical solid line indicate region where the relationship between Bmax and [A*R] begins to be nonlinear and where aberrations in the binding curves will be expected to occur. The binding of the range of concentrations of radioligands are taken at two values of Bmax (shown by the dotted lines, namely, 130 pM and 60 nM) and plotted as saturation curves for both Bmax values on the top panels (note the difference in the ordinate scales). These comparable scales allow comparison of the saturation curves and show the dextral displacement of the curves with increasing protein concentration. However, in displacement experiments, there are two ligands (tracer and nontraceable ligand) present and they must compete for the receptor. This competition can take considerably longer than the time required for just a single ligand. This is because the free ligands can bind only to free unbound receptors (except in the case of allosteric mechanisms, vide infra). Therefore, the likelihood of a receptor being free to accept a ligand depends on the reversibility of the other ligand, and vice versa. As the Bmax increases (2log Bmax values shown next to curves), the displacement curves shift to the right. It can be seen that a tenfold error in the potency of the displacing ligand [B] is introduced into the experiment by inadequate equilibration time. Radioligand binding experiments are usually initiated by addition of the membrane to a premade mixture of radioactive and nonradioactive ligand. This figure shows that a biphasic binding curve is seen for the slowly dissociating antagonist Ki20227 and not for the rapidly dissociating antagonist sunitinib [20]. Therefore, in the case of displacement experiments utilizing more than one ligand, temporal experiments should be carried out to ensure that adequate times are allowed for complete equilibrium to be achieved for two ligands. While pharmacological function is the main activity monitored in drug discovery, it can sometimes also be useful to know the receptor species binding allosteric and orthosteric ligands. A practical problem with extended models to account for all protein species and activation states is that they become heuristic, i. The factors, denote the influence of the various ligands on the receptor (R) and signaling protein species.
Citrus Seed Extract (Grapefruit). Plendil.
- Dosing considerations for Grapefruit.
- Asthma, lowering cholesterol, hardening of the arteries (atherosclerosis), preventing cancer, weight loss, psoriasis, muscle fatigue, promoting hair growth, toning the skin, reducing acne and oily skin, treating headaches, stress, depression, infections, digestive complaints in people with eczema, yeast infections (as a vaginal douche), and other conditions.
- Are there safety concerns?
- How does Grapefruit work?
- Are there any interactions with medications?
- What is Grapefruit?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96909
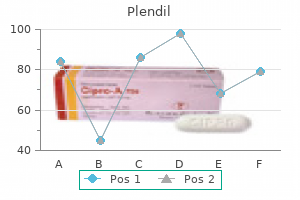
Buy plendil 10 mg overnight delivery
Pregnancy testing to rule out ectopic pregnancy and to guide antibiotic selection is mandatory heart attack kid lyrics buy plendil 5 mg amex. Analysis of fluid obtained from the cul-de-sac via culdocentesis may help differentiate infectious processes as characterized by purulent fluid from the strawcolored fluid of inflammatory disease or the blood of ectopic pregnancy. Endometritis and oophoritis may also be identified as may abscesses involving adjacent organs. Monitoring for compliance and microbial resistance is important to improve the therapeutic outcome. Intrauterine devices should be removed and alternative forms of birth control provided. There is spread of inflammation along the surface of the right hepatic lobe (arrows). If infection spreads to the abdomen, perihepatic infection with subsequent painful adhesions and scarring may occur. Identification of current and recent sexual partners to allow prompt evaluation and treatment is an important public health concern. Asymptomatic 25-year-old woman diagnosed of right adnexal mass with transvaginal ultrasound. Tubaric content is liquid with a signal lower than water on T2 and greater on T1 with saturated fat, compatible with pyosalpinx. Laparoscopic view of fibrous adhesion in all pelvic organs, especially the ovaries and the fallopian tubes. Pelvic inflammatory disease in virginal adolescent females without tubo-ovarian abscess. Comparative study of the clinical features of patients with a tubo-ovarian abscess and patients with severe pelvic inflammatory disease. In men, complaints of concomitant groin, perineal, penile, and scrotal pain are common. Patients suffering from interstitial cystitis often also suffer from irritable bowel syndrome, fibromyalgia, and focal vulvitis. Sleep disturbance is common as the symptoms of interstitial cystitis are often worse at night. Careful bimanual pelvic examination, palpation of the full bladder, rectal examination, and neurologic examination are mandatory to identify other causes of lower urinary tract dysfunction. Examination of females suffering from interstitial cystitis may reveal increased pain on palpation of the urethra and the base of the bladder. In male patients, careful digital examination of the prostate is mandatory to rule out prostatitis and prostadynia, which may confuse the diagnosis. The Hunner ulcer occurs in approximately 5% of patients with interstitial cystitis. AlsoknownastheHunnerlesion,theHunnerulcer appears as a friable patch or ulcer of the bladder mucosa. Biopsy of the Hunner ulcer is mandatory to rule out occult malignancy including carcinoma in situ. These glomerulations are invariably present in at least three quadrants of the bladder with sparing of the trigone. For this reason, a careful targeted history and physical examination, with a systematic search for other causes of irritative lower urinary tract symptoms, must be carried out in every patient suspected of suffering from interstitial cystitis. Neurologic disorders, including Parkinson disease, spinal tumor, spinal stenosis, and multiple sclerosis, must also be ruled out (Table 94. The clinician must also identify coexisting psychological and behavioral abnormalities that may exacerbate the symptoms associated with interstitial cystitis. Many patients with interstitial cystitis have a dysfunctional bladder uroepithelium that allows increased urothelial permeability to the intravesticular instillation of potassium chloride. Intravesticular instillation of potassium chloride in a concentration of 40 mEq/100 mL of water will cause minimal symptoms in patients with normal bladders, but elicit immediate severe irritative bladder symptoms in patients suffering from interstitial cystitis. Agoodstarting point in the treatment of interstitial cystitis is to help patients identify foods and beverages that may exacerbate the symptoms and remove them from their diet. Frequent offenders include caffeinated beverages, alcohol, carbonated beverages, acidic foods including citrus and tomatoes, vinegar, spicy foods, chocolate, and cranberry juice. Therefore, in patients suspected of suffering from interstitial cystitis, a careful evaluation to identify underlying disease processes is mandatory. The disease commonly coexists with various somatic and psychological disorders which must be treated concurrently. The addition of oral polysulfated xylan, pentosan polysulfate may provide symptomatic relief in some patients suffering from interstitial cystitis. The mechanism of action of this drug is thought to be owing to its protective action on the bladder wall in a manner analogous to the naturally occurring glycosaminoglycan coating of the inner bladder in healthy humans. Improvement in the irritative bladder symptoms following intravesticular instillation of potassium chloride supports this theory. The addition of anticholinergic agents, such as oxybutynin and tolterodine, may also be considered in patients with significantirritativesymptoms. Amitriptylinegivenatnightmay help sleep disturbance and treat underlying depression. Immune modulation with cyclosporine, a calcineurin, may reduce irritative symptoms, especially in those patients in whom Hunner ulcer is observed on cystoscopy. The extent of torsion is variable, ranging from 90 to 720 degrees, with complete torsion occurring with twisting of 360 degrees or greater. Although testicular torsion is primarily a disease of neonates and adolescents, it is occasionally seen in 40- to 50-year-olds as well as in patients who suffer testicular trauma. In adolescents and adults, the tunica vaginalis is attached to the posterolateral aspect of the testes, effectively tethering the testes in place. In neonates, because the tunica vaginalis is not yet attached to the gubernaculum, both the spermatic cord and tunica vaginalis twist as a unit. This type of testicular torsion is called extravaginal torsion and can occur pre- or postnatally. Testicular torsion is a true urologic emergency and must be treated within 6 hours of symptom onset if the testicle is to remain viable. Sequelae of testicular torsion include testicular infarction, infection, infertility, pathologic alterations of the retained injured testis, and postsurgical cosmetic deformity. Note the transverse testicular lie of the testicle relative to the spermatic cord. This patient underwent bilateral orchidopexy with complete resolution of his previously intermittent bilateral testicular pain. The pain is severe and is associated with nausea and vomiting in a third of patients. Physical examination will reveal a tender, high riding testis with an abnormal transverse position and loss of the cremasteric reflex. Lifting the affected torsed testis will not relieve the pain as is seen with acute epididymitis. The specificity of this scoring system is such that high-risk patients with a score of five or greater can proceed directly to surgery without color Doppler sonography, with intermediate risk patients with a score of three or four undergoing urgent color Doppler sonography to determine if surgery is required. Findings consistent with the diagnosis include absent or significantly decreased blood flow to the affected testis, decreased flow velocity within the intratesticular arteries, increased resistive indices within the intratesticular arteries, and low resistance hypervascularity after partial de-torsion of the affected testis. Radionuclide studies are also highly accurate in identifying alterations in testicular blood blow. In some patients, manual detorsion may help improve blood flow to the ischemic testis, but definitive surgical treatment with orchiopexy is ultimately required to prevent recurrence. If testicular necrosis has occurred and orchiectomy is required, a testicular prosthesis may be placed after complete healing of the orchiectomy. Antiemetic and anxiolytics may also be used for symptomatic relief, with care being taken not to potentiate the respiratory side effects of administered opioids. Given the incidence of malignancy that is associated with testicular torsion, a high index of suspicion is indicated. Patients who score in the high-risk category should be taken directly to surgery as time is of the essence. Note that the affected left testis is hypointense, and no contrast enhancement is observed that is diagnostic for testicular torsion (arrows).
Discount plendil 2.5mg on-line
Corneal opacification secondary to lipid keratopathy typically develops superiorly and may progress circumferentially blood pressure medication names starting with t generic plendil 2.5mg with visa, but it rarely causes vision loss due to opacification of the visual axis. Although progressive peripheral corneal thinning may occur (leading to increased risk of traumatic rupture), spontaneous corneal perforation is rare. Acute corneal hydrops develops when a rupture (typically spontaneous) of the Descemet membrane occurs and aqueous rapidly saturates the stromal collagen, producing profound edema. Fragmentation of the Bowman layer, iron deposition in the basal epithelium, and focal corneal thinning are also features of keratoconus but not specific to corneal hydrops. Hurler syndrome is a type of systemic mucopolysaccharidosis, a condition in which glycosaminoglycans cannot be completely metabolized because of defects in lysosomal enzymes. Mutations in the genes that synthesize the lysosomal enzymes are responsible for more than 30 different human genetic diseases. The incompletely degraded by-products accumulate in cells, causing alterations in cellular function and properties. Nephropathy is most common in the infantile form of cystinosis (and least common in the adult-onset form). Renal damage is the major medical morbidity and may lead to kidney failure by 10 years of age. Oral administration of cysteamine may be beneficial for posterior segment manifestations (retinopathy, optic neuropathy). The clinical scenario is suggestive of ocular surface disease due to chronic vitamin A deficiency. More common in developing countries, vitamin A deficiency is uncommon in the United States in the absence of a specific risk factor. Possible risk factors that should be solicited during the history include unusually restrictive diets, alcoholism, or any chronic cause of lipid malabsorption (including bowel resection, as well as diseases such as cystic fibrosis). A history of renal transplantation is relevant for patients presenting with band keratopathy. Because of their proximity to the optic chiasm, pituitary tumors are most relevant to visual field defects. Viral envelopes are composed primarily of lipids and proteins, which render them more susceptible to heat, acids, and drying. Adenoviruses, however, are surrounded only by a capsid of primarily glycoproteins, which are intrinsically more resistant to these same environmental stressors. For this reason, alcohol swabbing of a reusable tonometer tip is insufficient to prevent inoculation of subsequent patients in the setting of adenoviral exposure. Acanthamoeba, not adenovirus, is capable of prolonging survival by encysting itself in a dormant form. This condition is believed to be primarily inflammatory rather than actively infectious in origin. Neovascularization and lipid keratopathy are controlled primarily by limiting inflammation through the use of topical corticosteroids. A study of more than 38,000 adults aged 60 years or older showed a 50% reduction in new cases of zoster and a 66% reduction in postherpetic neuralgia. Of note, the immunity may last only about 5 years, and younger adults may benefit more than older adults. Chronic follicular conjunctivitis with an umbilicated eyelid nodule should raise suspicion for molluscum contagiosum. The classic histologic appearance of a molluscum lesion is a cup-shaped nodule with central necrosis, surrounded by epidermal cells with large eosinophilic intracytoplasmic inclusions (Henderson-Patterson bodies). Hyperkeratosis and acanthosis with a papillary growth pattern are typical of verruca vulgaris, caused by human papillomavirus. Hyperacute conjunctivitis with gram-negative intracellular (or extracellular) diplococci is diagnostic of gonococcal conjunctivitis caused by Neisseria gonorrhoeae. If corneal ulceration is present, the patient should be admitted to the hospital to receive intravenous ceftriaxone. In the absence of corneal involvement, outpatient therapy with intramuscular ceftriaxone 1 g and close observation is appropriate. Topical gentamicin ointment may be used as an adjunctive treatment for gonococcal conjunctivitis, but the mainstay of treatment is systemic ceftriaxone. Although major efforts have been undertaken to decrease the incidence of trachoma, it remains endemic in the Middle East, Africa, and parts of Asia. The distinctive features are conjunctival and corneal scarring (predominantly superiorly, although severe cases may be diffuse), bandlike or stellate tarsal scarring (also typically superiorly), trichiasis, and aqueous tear deficiency. Toxic injuries (eg, from alkaline substances) tend to affect the inferior ocular surface in excess of the superior surface. Natamycin is generally considered first-line therapy for most cases of fungal keratitis due to infection with filamentous fungi (eg, Fusarium species). Voriconazole is efficacious against a variety of fungal infections, but it was shown to be inferior to natamycin in a prospective, randomized clinical trial. Fluconazole has largely been replaced by newer azoles (voriconazole, posaconazole) because of their improved ocular penetration with systemic administration. Of note, ocular penetration through intact corneal epithelium is poor for many antifungal agents, including natamycin; for deep lesions, serial epithelial debridement may be indicated to enhance tissue penetration. A chronic corneal ulcer in the setting of contact lens wear may be caused by a variety of pathogens. In this case, the presence of radial perineuritis should raise suspicion for keratitis caused by Acanthamoeba (a protozoa) species. Fungal infections in contact lens wearers may present insidiously or acutely, but radial perineuritis is not typical. Topical medications, such as dorzolamide, are most likely to cause contact dermatoblepharitis. Type I (immediate hypersensitivity) reactions, which are immunoglobulin E mediated, typically occur within minutes after exposure to an allergen. Environmental allergens such as pollen and mold are associated with various ophthalmic manifestations (vernal conjunctivitis, seasonal allergic conjunctivitis) but do not typically cause a contact dermatoblepharitis. Staphylococcus hypersensitivity can also have a variety of ocular manifestations, such as marginal keratitis, but its presentation is not typically similar to that of dermatoblepharitis. Demodex has been implicated in cases of chronic blepharitis but has not been associated with contact dermatoblepharitis. Atopic dermatitis is a chronic condition in genetically susceptible individuals that usually begins in infancy or childhood and may or may not involve the external eye. Treatment includes identifying and minimizing allergens in the environment and in foods. Acute lesions can be controlled with a topical corticosteroid cream or ointment (eg, clobetasone butyrate 0. Both topical and oral T-cell inhibitors (eg, tacrolimus) have been found effective and have fewer adverse effects than corticosteroids, so they are preferred in patients with chronic and severe disease. Oral doxycycline and hydroxychloroquine are not used in the treatment of atopic dermatitis or atopic keratoconjunctivitis. Several additional months of treatment may be beneficial; recent evidence indicates that residual tumor may be present for up to 476 Answers 3 months following clinical resolution. Topical 5-fluorouracil 1% may be given 4 times daily for 1 month, with at least several months off if repeated; alternatively, it may be given 4 times daily for 1 week, followed by a 3-week structured treatment interruption, until resolution, for a maximum of 3 cycles. Nevocellular nevi of the conjunctiva consist of nests or more diffuse infiltrations of benign melanocytes. Nevi near the limbus are usually almost flat, whereas nevi appearing elsewhere on the bulbar conjunctiva tend to be elevated. Small epithelial inclusion cysts occur within about half of all conjunctival nevi, particularly the compound or subepithelial varieties. Several studies have demonstrated that the risk of recurrence after pterygium excision is lower if a conjunctival autograft, rather than an amniotic membrane transplant, is used. Covering the entire defect decreases postoperative inflammation and speeds reepithelialization of the ocular surface. The use of bevacizumab in primary pterygium excision apparently has no effect on the recurrence rate of this condition.
Order plendil 2.5mg with visa
It often arises in the inferior fornix but can also present on the tarsal or bulbar conjunctiva or along the plica semilunaris arrhythmia blood pressure generic 2.5mg plendil fast delivery. Multiple lesions sometimes occur, and the lesion may be extensive in patients with compromised immunity. With its glistening surface and numerous red dots, this form of papilloma resembles a strawberry. Signs of dysplasia include leukoplakia (indicative of keratinization), symblepharon formation, inflammation, and invasion. Surgical excision with cryotherapy or cautery to the base of the lesion is curative in approximately 90% of cases. An incomplete excision, however, can stimulate growth and lead to a worse cosmetic outcome. Surgical manipulation should be minimized to reduce the risk of dissemination of the virus to uninvolved healthy conjunctiva. Adjunctive treatment with topical interferon-a2b or oral cimetidine may be of benefit for extensive or recalcitrant lesions. If the lesion enlarges or shows clinical features suggesting dysplastic or carcinomatous growth, excisional biopsy with adjunctive cryotherapy is indicated. Conjunctival papilloma: features and outcomes based on age at initial examination. A case-control study of immunosuppression resulting from human immunodeficiency virus versus immunocompetency. Conjunctival squamous cell carcinoma arising in immunosuppressed patients (organ transplant, human immunodeficiency virus infection). Related terms include squamous dysplasia, which is used when atypical cells invade only part of the epithelium, and squamous carcinoma in situ, used when cellular atypia involves the entire thickness of the epithelial layer. Although histologic invasion beneath the epithelial basement membrane is present, growth usually remains superficial, with neoplastic cells infrequently penetrating the sclera or Bowman layer. In addition to neoplastic epithelial cells, malignant goblet cells can be shown with mucin stains. Treatment is wide surgical excision; adjuvant therapy may include cryotherapy and radiotherapy. Glandular Tumors of the Conjunctiva Oncocytoma A slow-growing cystadenoma, an oncocytoma is a benign tumor arising from ductal and acinar cells of main and accessory lacrimal glands. Oncocytoma most commonly occurs in older persons and may present as a reddish-brown nodule on the surface of the caruncle. Sebaceous Gland Carcinoma Sebaceous gland carcinoma accounts for approximately 1% of all eyelid tumors and 5% of eyelid malignancies. It usually occurs in older individuals but may be seen in younger persons after radiation therapy. A, Presents as a unilateral blepharoconjunctivitis with injection, pannus, thickened eyelid margin, and eyelash loss. B, White nodules composed of neoplastic sebaceous cells may be present near the limbus. Tumors of Neuroectodermal Origin Table 12-2 lists the ocular surface tumors that arise from melanocytes, nevus cells, and other neuroectodermal cells. For example, a pigment spot of the sclera is a collection of melanocytes associated with an intrascleral nerve loop or perforating anterior ciliary vessel. The term melanosis refers to excessive pigmentation without an elevated mass that may be congenital (whether epithelial or subepithelial) or acquired (whether primary or secondary). Benign Pigmented Lesions Ocular melanocytosis Congenital melanosis of the episclera occurs in approximately 1 in every 2500 individuals and is more common in black, Hispanic, and Asian populations. Affected patients may have a diffuse nevus of the uvea, evident as increased pigmentation of the iris and choroid. The combined ocular and cutaneous pigmentations are referred to as oculodermal melanocytosis (nevus of Ota). In 10% of patients with ocular melanocytosis, secondary glaucoma occurs in the affected eye. The lifetime risk of uveal melanoma in a patient with ocular melanocytosis is about 1 in 400-significantly greater than the approximate 6-per-million risk of the general population. Nevus Nevocellular nevi of the conjunctiva consist of nests or more diffuse infiltrations of benign melanocytes. On histologic examination, nevi can occasionally be very difficult to differentiate from melanoma. Junctional nevi may be difficult to distinguish from primary acquired melanosis (see the section "Primary acquired melanosis" later in the chapter). Nevi appearing elsewhere on the bulbar conjunctiva, plica semilunaris, caruncle, or eyelid margin tend to be elevated. Small epithelial inclusion cysts occur within approximately half of all conjunctival nevi, particularly the compound or subepithelial varieties. Secretion of mucin by goblet cells in the inclusion cysts can cause a nevus to enlarge, giving a false impression of malignant change. Rapid enlargement can occur at puberty, giving rise to a clinical impression of conjunctival melanoma. An amelanotic, vascularized nevus, when inflamed, may resemble an angioma, or it may be misdiagnosed as chronic conjunctivitis. Bilateral conjunctival melanocytic nevi of simultaneous onset simulating conjunctivitis in a child. Conjunctival nevi: clinical features and natural course in 410 consecutive patients. Excisional biopsy should be performed on lesions that show suspicious change or growth. A biopsy should also be performed for pigmented lesions on the palpebral conjunctiva or cornea or in the fornix, as nevi are rare in these locations. The pigmentation can also involve the caruncle and palpebral conjunctiva as well as extend into the cornea with streaks or whorls (striate melanokeratosis). Histologic findings consist of hyperpigmentation of the conjunctival basal epithelial cells without atypia or hyperplasia. Secondary acquired melanosis has a similar appearance but is associated with systemic disease (eg, Addison disease), previous radiation, or pregnancy or is secondary to another conjunctival lesion (eg, squamous papilloma or carcinoma). Complete examination of the ocular surface (including double eversion of the upper eyelid) is essential in any patient with conjunctival pigmentation; see the following section for management of these lesions. It is difficult to predict which lesions may progress, but clinical findings such as larger size (3 clock-hours or more) and caruncular, forniceal, or palpebral location portend a worse prognosis. Two clock-hours or less of conjunctival involvement is associated with a lower risk of malignant transformation; involvement of more than 2 clock-hours is an indication to remove the lesion for histologic diagnosis. Other worrisome signs include progressive enlargement, a nodular component, feeder vessels, and thickening. The most important finding in predicting progression is the presence of cellular atypia, which can be determined only by excisional biopsy. As such, suspicious lesions should be removed and sent for histologic examination and immunohistochemistry. If the pigmentation is diffuse and not amenable to complete excision, adjuvant topical chemotherapy with mitomycin C may be useful to treat the entire ocular surface. The surgeon should exercise care in performing intraocular surgery in a patient with untreated ocular surface neoplasia, as violation of the Bowman layer may lead to tumor seeding within the corneal stroma and internal structures of the eye. Recurrent primary acquired melanosis with atypia involving a clear corneal phacoemulsification wound. Low-risk and high-risk histologic features in conjunctival primary acquired melanosis with atypia: clinicopathologic analysis of 29 cases. Malignant Pigmented Lesions Melanoma With a prevalence of approximately 1 per 2 million in the population with European ancestry, conjunctival melanomas make up less than 1% of ocular malignancies in this group. Although malignant melanoma of the conjunctiva has a better prognosis than cutaneous melanoma, the overall mortality rate is 25%. In rare cases, an underlying ciliary body melanoma can extend through the sclera and mimic a conjunctival melanoma. The degree of pigmentation is variable; approximately 25% of conjunctival melanomas are amelanotic.
Purchase plendil cheap
However can blood pressure medication kill you buy cheapest plendil and plendil, abnormal tissue, like corneal scars or calcium deposits (as in band keratopathy), may ablate at a different rate than normal tissue, so an uneven surface results even if the original surface was smooth. Manual techniques are more likely to respect the Bowman layer and maintain a smooth ocular surface, as the laser does not respect anatomical planes. Frequent application of viscous liquid to the corneal surface during laser ablation can fill in gaps in the surface and help achieve a smooth surface after ablation. Phototherapeutic keratectomy: who are the best candidates and how do you treat them Use of mitomycin-C for phototherapeutic keratectomy and photorefractive keratectomy surgery. A partial tarsorrhaphy can sometimes be very effective and restore some vision to the eye. Persistent epithelial defects and recurrent erosions of the cornea result from defects in the surface epithelium that fail to heal in a timely fashion (see Chapter 4). Trauma from the eyelids during blinking can retard reepithelialization, and if delayed, reepithelialization is further slowed by chronic changes in the basement membrane and anterior stroma. However, it compromises corneal oxygenation and impairs vision; also, some patients cannot tolerate closure of the eye while it is patched. Bandage contact lenses Application of a thin, oxygen-permeable, continuous-wear soft contact lens as a therapeutic bandage can protect loosely adherent remaining or regenerating epithelium from the "windshield-wiper" action of the blinking eyelids. Use of bandage contact lenses has significantly improved and simplified the management of recurrent erosions and persistent epithelial defects. Careful consideration should be given to the choice of a soft contact lens for patients with severe dry eye. In general, patients with dry eye run a high risk of infection with soft contact lenses; punctal occlusion should be performed in these patients to facilitate lens retention and comfort. Frequent lubrication, prophylaxis with antibiotics, and close follow-up are crucial, especially in patients with decreased corneal sensitivity or dry eye. If a conventional soft lens is not tolerated, the use of an acrylic scleral lens may circumvent the problems encountered with a smaller-diameter hydrogel lens. Continuous wear of a soft lens can relieve the symptoms of painful bullous or filamentary keratopathy. Tarsorrhaphy should be considered for patients who have contact lens complications or a high risk of infection. Treatment of corneal thinning/descemetocele Corneal thinning may occur secondary to dellen where the tear film is uneven or may result from stromal inflammation and necrosis. In patients with dellen, the epithelium is intact, but there is an area of thinning next to an area of elevated or edematous tissue. The goals of therapy are to treat the inflammation or infectious component and to facilitate reepithelialization, which prevents progression of stromal collagenolysis. The first order of therapy is to use appropriate antibiotics and anti-inflammatory medications. Topical steroids may reduce inflammation but should be used with caution with aggressive corneal melts. In patients with autoimmune conditions, conjunctival resection in the quadrant of a peripheral melt can be useful. In some cases, cyanoacrylate glue (also called cyanoacrylate adhesive) is helpful. Once the inflammation or infection has been controlled, a bandage lens or tarsorrhaphy may facilitate reepithelialization. An alternative to using cyanoacrylate for a descemetocele is to use amniotic membrane that has been cut to the shape of the defect and then place a patch into the defect where the near-perforation is located. The patch and smaller amniotic membrane may be held in place with a larger amniotic membrane patch, nylon sutures, and a bandage contact lens, or by means of fibrin glue. With time, scar tissue will reinforce the deficient area and may circumvent the need for a corneal transplant. Treatment of perforation Some corneal perforations are small and seal spontaneously before ophthalmic examination, with no intraocular damage, prolapse, or adherence. These cases may require only treatment with systemic and/or topical antibiotic therapy, along with close observation. If a corneal wound is leaking but the anterior chamber remains formed, the leakage may be sealed with pharmacologic suppression of aqueous production (topical ocular hypotensive agent or systemic carbonic anhydrase inhibitor), patching, or a bandage contact lens. Cyanoacrylate glue applied to thinned or ulcerated corneal tissue may prevent further thinning and can prevent leakage through the period of vascularization and repair. The adhesive plug is also thought to retard the entry of inflammatory cells and epithelium into the area, thus decreasing the rate of corneal melting. After the lesion is sealed, new stromal tissue may be laid down, and accompanying corneal vascularization may help ensure the integrity of the area by providing nutrients and antiproteases. Cyanoacrylate glue can usually be applied on an outpatient basis using topical anesthetics. However, if adherent or prolapsed uvea in the leakage site or a flat chamber is encountered, the procedure may be best performed in the operating room using balanced salt solution and/or viscoelastic to re-form the anterior chamber. Before the adhesive is applied, necrotic tissue and corneal epithelium should be removed from the involved area out to a 2-mm zone. A small drop of the fluid adhesive is applied to the corneal wound with the tip of a 30-gauge needle or anterior chamber cannula. The glue does not polymerize on plastic, so an alternative way to apply the adhesive is to spread a small amount on the inside of the sterile plastic wrapping of any medical product that has been cut to a size slightly larger than the perforation. The glue can then be applied to the surface of the cornea in as thin a layer as possible using the plastic handle of a cellulose sponge or the wooden stick of a cotton-tipped applicator. The adhesive plug has a rough surface and can be irritating, so a bandage contact lens is necessary to protect the upper tarsal conjunctiva and to prevent the plug from being dislodged by blinking. Tattoo for Corneal Scars Corneal tattooing has been used for centuries to improve the cosmetic appearance of a blind eye with an unsightly leukoma. For small iris defects, applying a marking pen to the cornea over the affected area can simulate the effect of tattooing. When this solution reacts with a second agent, a black precipitate is formed in the cornea, producing a dark deposit that can simulate a pupil. Another technique involves utilizing the standard methods used in skin tattooing: applying to the cornea a paste of colored pigment, either India ink or a metal oxide, and then using a hypodermic needle or angled blade to drive the pigment into the corneal stroma in the area that needs coverage. Multiple superficial punctures are made until enough pigment has been applied; multiple pigment colors can be used to give a more natural appearance. However, the method is time-consuming and often needs to be repeated if the pigment uptake is inadequate or the pigment migrates. Tarsorrhaphy Tarsorrhaphy, the surgical fusion of the upper and lower eyelid margins, is performed to reduce the exposed surface area of the cornea. It is among the safest, most effective, and most underutilized procedures for healing difficult-to-treat corneal lesions. It can also be used to aid in the healing of indolent corneal ulceration, as is sometimes seen with tear film deficiency, herpes simplex or herpes zoster infection, or stem cell dysfunction. Because the cosmetic effect of a lateral tarsorrhaphy is significant, patients may be reluctant to undergo this procedure and should be counseled on its therapeutic benefits. If closure of more than 3 weeks is desired or if the length of time is uncertain, then permanent but reversible adhesion is induced by denuding the eyelid margin. B, One or two mattress sutures (double-armed 4-0 polypropylene with cutting needles) are passed through the upper and lower eyelids to secure the tarsorrhaphy. Each suture end should be placed through the skin of the upper eyelid approximately 5 mm above the lash line, traverse the upper tarsal plate, exit through the denuded wound surface of the upper eyelid margin, enter through the denuded wound surface of the lower eyelid margin, traverse the lower tarsal plate, and exit through the skin of the lower eyelid approximately 5 mm from the lash line. After infiltration of local anesthetic, a muscle hook is placed under the tissue, and a hemostat is placed (for 5 seconds) across the adhesion to be released. A blade or scissors are used to incise the tarsorrhaphy adhesion parallel to the upper and lower eyelid margins.