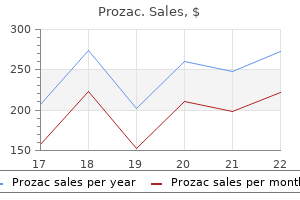
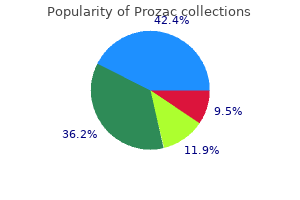
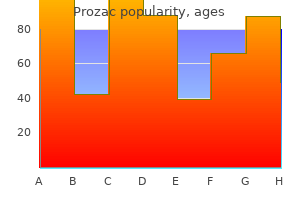
Generic prozac 60 mg with mastercard
Thirdly anxiety pregnancy discount prozac 10mg without a prescription, there have been recent advances in the manipulation of the mouse genome, such that it is the most appropriate vertebrate in which to perform Chapter 66 Molecular otology, development of the auditory system and recent advances in genetic manipulation Table 66. Finally, the mouse is useful in embryological and developmental studies, and invasive physiological tests can also be performed in anaesthetized mice, which provide important clues to the basis of the dysfunction and could not be carried out in humans. At the same time as the development of the arches and clefts, a number of outpocketings known as the branchial pouches appear on the lateral wall of the pharynx. These pouches gradually penetrate the surrounding mesenchyme, but do not establish an open communication with the exterior. The mesodermal core of the branchial arches is pleuripotential in that it can give rise to any number of structures, for example cartilage, muscles or arteries. The development of the branchial apparatus is covered in Chapter 65, Head and neck embryology. The development of the outer ear is hence controlled, in part, by genes that determine the identity of the first and second arches. This regulation is mediated through the segmentation of the developing hindbrain into rhombomeres. The hindbrain is the source of the neural crest cells that populate the branchial arches. Mutations in the genes that control the development of the fourth segment of the hindbrain, rhombomere 4, can cause abnormalities of the outer ear. Middle-ear morphogenesis can be altered under various conditions that cause congenital abnormalities in head development. Genes that are expressed in the first and second branchial arches and in the hindbrain segments that give rise to these arches, appear to have a significant role in patterning the middle ear. These include Gsc,14, 15 Dlx2,20 retinoic acid receptors (Rars),21 Prx1,22 Otx2,23 Hoxa1,12 Hoxb113 and endothelin-related molecules. A central role of this process is played by the tympanic ring, which is a C-shaped membranous bone that develops from midbrain and rhombomere 1 neural crest and provides physical support to the tympanic membrane. The malleus, originating from the midbrain and rhombomeres 1 and 2 crest cells, and the incus, originating from rhombomeres 1 and 2 crest cells, both derive from the first branchial arch. The second branchial arch element of the middle ear, the stapes, derives from rhombomere 4. Proper development of the branchial arches, and thus the ossicles, depends on information provided by the neural crest, the mesoderm, and the overlying epithelia. The vertebrate ear develops from a complex convergence of tissues from all three germ layers (endoderm, mesoderm and ectoderm), as well as the neural crest. A major contribution to the outer ear is made from the first and second branchial arches, which include the arch ectoderm and mesoderm. The middle ear is formed from cells arising from the neural crest and paraxial mesodermal cells that initially migrated to the branchial arches and then coalesced to form the middle ear components. It also contains contributions from the endoderm, as it is lined by mucosal tissue that expands into the middle ear from the oral cavity. The epithelial tissues and neurons of the inner ear are formed of placodal ectoderm, which invaginates to form the otocyst, a cartilaginous capsule that eventually ossifies and surrounds the epithelial core of the inner ear. On the medial side of the ossicular chain, the formations of the stapes and the oval window appear to be controlled by the Hoxa2 gene;27 the insertion of the stapes into the oval window seems to be regulated by the Pou3f4 gene. Initially, they form a single structure, the cochleovestibular ganglion, which divides into the cochlear and vestibular ganglia as development proceeds. The inner ear then enlarges, while undergoing complex changes, in order to assume its final morphology. Hindbrain segmentation occurs at the same time that the otic placode arises and the hindbrain could be crucial for otic placode specification. By the time the otocyst that is adjacent to rhombomere 5 has formed, hindbrain segmentation is complete. At this time, neural crest cells migrate out of the hindbrain and stream around the adjacent otocyst as they descend ventrally to form the branchial arches, together with their surrounding mesodermal cells, providing information transfer from neural ectoderm to the otic field. Basic processes in the development of the otic vesicle have been shown to include the initiation and completion of each of the following overlapping steps. Specification of the otic field then enables the placodally competent ectoderm to be restricted to the prospective ear region. Determination occurs when the otic field progressively acquires its identity and becomes committed to its otic fate. Regional and cell-fate specification of the otic vesicle may be related to the earliest stage of regional gene expression and to the first events of cell differentiation, respectively. The first neural crest cells to migrate are those contributing to the head of the malleus, followed by those forming the head of incus. The next to migrate are rhombomere 4 crest cells contributing to the stapedial footplate. The crest cells that make the tympanic ring and the handle of malleus start their migrations shortly after. This is then followed by the migration of crest cells that form the stapedial arch and those contributing to the neck of the malleus. These have to be connected in a normal and orderly fashion, so that the middle ear can function properly. By embryonic day 17 (E17), it attains its mature shape of one and three-quarters turns. The organ of Corti develops from the thickened epithelial cells of the cochlear duct. This thickened area is formed of tall columnar cell mounds: the lesser and the greater epithelial ridges. The main events of semicircular canal formation in a developing mouse occur between 11. From the medial aspect of the otocyst, an uncoiled tube grows out and projects dorsally. The first two semicircular canals to form, the superior and the posterior, develop from a shared pocketshaped rudiment. The canals are formed by fusion of the lateral and medial epithelial surfaces of the out-pocketing and the subsequent disappearance of the fused region of epithelia. The superior canal forms first, followed closely by the posterior; the horizontal canal forms last from a separate rudiment. By E13, all the major changes that the inner ear undergoes are complete and the inner ear labyrinth resembles a miniature replica of its adult form. Origin of the sensory organs the inner ear houses the receptor cells for two distinct sensory pathways: the auditory and vestibular systems. Patterning of the inner ear into prospective auditory and vestibular sensory areas is associated with restricted gene expression domains during the stages of development from otic placode to otocyst. In the absence of this gene, the hair cell phenotype aborts at an early stage, eventually leading to the death of hair cells and the supporting cells. Chapter 66 Molecular otology, development of the auditory system and recent advances in genetic manipulation] 817 Modifier genes affecting the development of the auditory system More often than not, a given genetic disorder may manifest in a variety of ways. Modifier genes affect the phenotypic outcome of a given genotype by interacting in the same or parallel biological pathway as a disease gene. The effect can be enhancing, leading to a more severe mutant phenotype, or suppressive, reducing the mutant phenotype even to the extent of completely restoring the normal condition. Modifier genes can also alter the clinical presentations of a given disease, resulting in different combinations of traits. Moreover, multiple modifier genes may act in combination to create a cumulative effect on the expression of a phenotype. It may one day be possible to reverse certain types of defect that affect the early development of the auditory and vestibular systems. A prerequisite for treatment will almost certainly be early and accurate diagnosis. Groups with strong family histories of vestibular disorders and/or deafness with any related syndromes and premature newborns should be targeted for screening in the first instance.
Purchase prozac 20 mg line
If intracranial complications are found depression test for social security discount prozac line, hourly neurological monitoring is likely to be appropriate. The aim of these investigations is to: confirm the diagnosis of the complication; define the extent and site of the complication; help planning of any treatment; confirm that there is no other covert complication present. Animal experiments have demonstrated that visual loss may be irreversible if retinal ischaemic time exceeds 100 minutes. In most reported case series, adolescent and young adult males are more commonly affected,12, 13 possibly due to the vascularity of the diploeic system in this age group. A study of 74 patients admitted with orbital complications secondary to rhinosinusitis identified an incidence of 24 percent for concomitant intracranial complications in patients aged seven or older (mean age 15 years 11 months) who required surgical intervention for their orbital complications. Whenever there is a history suggestive of intracranial pathology, specific enquiries should be made to elicit symptoms and signs of rhinosinusitis as a primary cause of the presenting problem. In the case of orbital cellulitis, the main aim of radiological investigation will be to define the extent and site of the disease. If there is full ocular movement and normal vision (including colour vision), no immediate radiological investigation is indicated, unless there are concerns about an intracranial problem also being present. Appropriate investigations should be undertaken to confirm the presence, and site of, a suspected surgically treatable abscess prior to drainage. Plain x-rays have no role here, as they are unable to define anything but the grossest orbital abnormalities. This approach will give the greatest chance of picking up small abnormalities, which might be missed with scans carried out in only one plane. Similarly, although ultrasound imaging may pick up orbital abnormalities, it will not demonstrate the important surgical anatomy. Similarly, the culture of any purulent material found in the nose on clinical examination at the time of surgery in the sinuses or from an abscess is important. In patients with a diagnosed complication of rhinosinusitis, urinalysis should be undertaken to detect diabetes mellitus, which might have led to immunocompromise. The exception to this would be when vision was affected by pressure on the optic nerve resulting from surrounding inflammation without abscess formation. The aim of medical management is two-fold: (1) to control and eliminate the disease process directly relating to the complication; and (2) to control and eliminate the primary rhinosinusitis. Although antimicrobials will form the mainstay of medical treatment, many clinicians would advocate specific treatment for nasal decongestion with the aim of facilitating resolution of the underlying rhinosinusitis. A typical decongestant regime would be the intranasal administration of ephedrine 0. The selection of antibiotics will usually be made before any information regarding the infecting organism or its sensitivity to antimicrobials is available. The choice of antibiotics, therefore, needs to be of a broad enough spectrum to cover the likely infecting organisms, but at the same time be reasonably selective in order to minimize the development of microbe resistance. The likely infecting organisms are Streptococcus pneumoniae and other Streptococcus spp. To these ends, on suspicion of a complication of rhinosinusitis, a full blood count should be performed. Other investigations As in any infective condition, it is important, if possible, to establish the nature of the infecting organism and its antimicrobial sensitivities. In patients with antibiotic sensitivities, other appropriate antibiotics should be selected in accordance with local microbiology policies. It should be noted that the incidence of bacterial species isolated is not wholly consistent across series reports and it is possible that the major pathogens vary geographically. This may be due to differences in the use of antibiotics and subsequent selective pressures on pathogenic bacteria (although equally it may represent sensitivities of culture techniques and the influence of the relatively small numbers of cases). It is possible that the current trend away from routine prescription of antibiotics for upper respiratory tract infections will lead to a relative increase in the incidence of complicated rhinosinusitis. It could be argued that if there were such an urgent need to reduce pressure effects that surgical intervention would be more appropriate. If there is not a significant clinical improvement in the first 24 hours of medical treatment, surgical intervention should be considered. Additionally, if there is clinical deterioration, then emergency surgical intervention is likely to be appropriate. For orbital complications, intravenous antibiotic administration should continue until clinical improvement is well established and only then should oral treatment be substituted. A good indication of established improvement is the absence of pyrexia for a period of 24 hours combined with a general clinical improvement. In all instances, the importance of working with and consulting other clinical colleagues should not be overlooked. Surgical the surgical treatment of patients with complications of rhinosinusitis can be conveniently divided into that necessary for the treatment of the rhinosinusitis and that necessary for the treatment of the complication. These are likely to be carried out at the same time, but may involve more than one team of surgeons. The principles of draining any pus and establishing ventilation of the sinuses remain exactly the same and are described elsewhere. Where the complication has arisen from acute rhinosinusitis, it is likely that the operative field will be very haemorrhagic, making endoscopic surgery much more difficult than in the presence of chronic rhinosinusitis alone. Contraindications for an endoscopic approach include any intracranial complication, osteomyelitis of the frontal bone or orbital complications with an acute visual problem. Some surgeons suggest that endoscopic ethmoidectomy together with removal of the lamina papyracea and perinasal drainage of the orbital abscess is sufficient treatment. However, unless the surgeon is extremely familiar with endoscopic nasal surgery, it is probably easier and wiser to use an external approach. This has the advantage of allowing an assistant to help keep the operative field clear. The former, endonasal, siting is likely to result in less cosmetic deformity than leaving an external drain. As far as the otorhinolaryngologist is concerned, discussion needs to take place as to whether the neurosurgical approach is going to be done at the same time as any sinus surgery. There is little evidence to help decide whether these should be done as separate procedures, but as with orbital cellulitis, it is probably better to undertake the surgery for the complication at the same time as undertaking surgical treatment for the underlying rhinosinusitis. However, intracranial complications are most likely to arise from frontal rhinosinusitis rather than disease of the other paranasal sinuses, and definitive surgery on the frontal sinus is difficult at the best of times. In these circumstances, it is probably better to undertake a temporary drainage procedure at the time of surgery for the intracranial complication, rather than attempt a formal sinus reventilation procedure or obliteration. A frontal sinus trephine procedure with placement of an external drain is likely to give the best immediate result, leaving the decision about any definitive surgical procedure until the patient has fully recovered from treatment of the complication. Other concurrent complications of rhinosinusitis should be excluded prior to theatre. Following surgery, a prolonged course (six weeks) of culture-directed antibiotic therapy should be given. Occasionally the orbital abscess will lie away from the lamina papyracea, especially if there is a frontal rhinosinusitis. The major complications of rhinosinusitis are orbital and intracranial infection, of which orbital complications are the more common. A more recent study of 219 patients showed an overall mortality rate of 16 percent. Chapter 120 Complications of rhinosinusitis] 1547 [Surgical treatment is normally required for resolution in patients with abscess formation. This makes it very difficult to design studies in any particular area that would result in level 1 or 2 evidence. The evidence presented here is, therefore, mostly based on the results of retrospective case series reviews.
Cheap prozac master card
The Foley catheter is inflated with up to 15 mL of water teenage depression symptoms uk prozac 10 mg, pulled forward to engage in the posterior choana and anterior packing is then inserted. The Foley catheter needs to be secured anteriorly, taking care not to cause pressure over the columella. Posterior packing causes considerable pain and may cause hypoxia secondary to soft palate oedema. Knowledge of the blood supply of the nasal cavity and the likely sources of epistaxis will inform the choice of ligation technique. Ligation should be performed as close as possible to the likely bleeding point; thus, the hierarchy of ligation is: sphenopalatine artery; internal maxillary artery; external carotid artery; anterior/posterior ethmoidal artery. The operation can be performed with an operating microscope or more commonly using a rod lens endoscopic technique. The incision is carried down to the bone and a mucosal flap is elevated posteriorly until the fibroneurovascular sleeve arising from the sphenopalatine foramen is identified. The foramen can be difficult to identify, but its location is signalled by the crista ethmoidalis. The artery is exposed transantrally via anterior (sublabial) or combined anterior and medial (endoscopic) techniques. In the traditional sublabial approach, an antrostomy is formed taking care to preserve the infraorbital nerve. The mucosa of the posterior wall of the antrum is then elevated and a window is made through into the pterygopalatine fossa. The branches of the internal maxillary artery are identified pulsating within the fat of the fossa and are carefully dissected out prior to clipping with haemostatic Endonasal sphenopalatine artery ligation Endonasal sphenopalatine artery ligation conforms to the ideal of controlling the bleed as close as possible to its nasal source. The proximal internal maxillary artery, descending palatine and sphenopalatine branches are all clipped and ideally divided. An endoscopic variation on this technique uses a middle meatus antrostomy, as an instrument port with a 4-mm endoscope is inserted through a small canine fossa antrostomy. Nevertheless, the relative technical ease of this procedure justifies its use in extreme cases. This procedure can be carried out under local or general anaesthetic using either a skin crease incision or a longitudinal incision parallel with the anterior border of the sternomastoid. The carotid bifurcation is identified and the external carotid confirmed, double-checked for arterial branches and then ligated in continuity. Some authors advocate anterior and posterior ethmoidal artery ligation as an adjuvant to this procedure. In one study, external carotid artery ligation secured haemostasis in 14 out of 15 patients. The arteries are approached by a medial canthal incision which is carried down to the bone of the anterior lacrimal crest. Periosteal elevators are then used to elevate and laterally retract the bulbar fascia. The anterior ethmoidal artery is seen as a fibroneurovascular mesentry running from the bulbar fascia into the anterior ethmoidal foramen. The vessel is clipped and divided and dissection is continued to identify the posterior artery which is located approximately 12 mm behind. Endoscopic transethmoidal ligation of the anterior ethmoidal artery has been described, but is unlikely to be technically possible in most cases. Some authors have advocated septal surgery as a primary treatment for failed packing. It is essential to exclude arteriovenous malformations, aneursyms and fistulae prior to embolization. Once the bleeding vessel is identified, a fine catheter is passed into the internal maxillary circulation and particles (polyvinyl alcohol, tungsten or steel microcoils) are used to embolize the vessels. The ipsilateral facial artery is also embolized in order to prevent recirculation. Complications include skin necrosis, paraesthesia, cerebrovascular accident and groin haematomas. The choice between embolization and ligation is likely to depend on local expertise, availability and experience. Bleeding is usually minor and troublesome, rather than life threatening, and it is uncommon to see bleeding by the time the patient presents. A full and detailed history and examination should identify factors such as aspirin use, liver disease or bleeding from the margins of a septal perforation. Rarely, nasal tumours present with recurrent blood-stained discharge which should be distinguished from epistaxis per se. Patients using topical nasal medications (particularly steroid sprays) frequently report minor recurrent bleeds. If a bleeding point can be identified, cautery is used but often no single vessel can be identified and an area of vestibulitis is found. Evidence for the efficacy of topical antiseptic creams is available from paediatric studies and it is likely (but unproven in adults) that chlorhexidine and neomycin creams may reduce the frequency of bleeding. If there is a history of cardiovascular disease or vascular graft surgery then aspirin should not be discontinued, otherwise temporary cessation of aspirin may be required to allow the recurrent bleeding to settle. In such cases, treatment of the epistaxis demands close liaison with haematologists and physicians. Trauma Post-traumatic nasal haemorrhage does not conform to the normal pattern of epistaxis and its origin and severity is almost infinitely variable. Persistent bleeding can occur from the ethmoidal arteries following frontoethmoidal fracture. In this case, the vessels may be lacerated, incompletely divided or even held open by fractures through their bony mesentries. Severe haemorrhage refractory to packing should be managed by open approach ligation. Catastrophic bleeding has been reported after head injuries due to delayed rupture of an internal carotid artery pseudoaneurysm. Thus persistent or unexpectedly severe bleeding even some time after a head injury should be seen as an indication for angiography. Bleeding is often from multiple sites and attempts at instrumentation lead to further mucosal damage and bleeding. After resuscitation, anterior packs should be inserted and the haematology team consulted. With large areas of bleeding or oozing, fibrin glue can be used as a haemostatic dressing. Penetrance is variable, but reaches 97 percent by age 50 years and occasional atavistic cases are observed. An exception is the severe haemorrhage which ocurrs following between 3 and 9 percent of inferior turbinectomies. Anterior subtotal turbinectomy may carry a reduced risk of post-operative bleeding. Retraction of the vessel into the orbit can give rise to a tension haematoma of the orbit and is a surgical emergency (see Chapter 117, Surgical management of rhinosinusitis). Massive and usually fatal epistaxis can result from damage to the internal carotid artery during posterior ethmoid or sphenoid sinus surgery. The bleeding is usually uncontrollable but packing, angiography and embolization may be tried. Large multicentre comparisons of these treatments have not been conducted and, due to the relative rarity of the condition, this situation is likely to persist. The risk, albeit small, of missing a tumour is another good reason for nasal endoscopy in epistaxis cases. Publications consistently fail to classify epistaxis or define the study population. Thus studies involve heterogeneous groups of patients and different types of epistaxis making comparisons difficult, as result level 1 and 2 evidence is scarce. An anatomical investigation of blood vessels of the lateral nasal wall and their relation to turbinates and sinuses. Continued bleeding after indirect therapy should be seen as an indication to move to the next level of management.
Best buy for prozac
Two patients continue to have oedema after one attempt and one patient was lost to follow up what us bipolar depression buy generic prozac 20 mg. The decision should be left to the patient as to whether they want a more conservative procedure such as this, which has a relatively higher frequency of recurrence and need for reoperation. Care is taken to ensure that the frontal sinus opening is bordered by bone on all sides and that mucosa is preserved at least on one part of the circumference. At the end, a rubber finger stall can be introduced into the frontal sinus for about five days. Some authors85, 86, 87, 88 advocated the use of soft, flexible silicone stents in cases of a frontal sinus neoostium of less than 5 mm in diameter, since more rigid silicone tubes have not given good results. This is followed by resection of the frontal sinus septum or septa, if there is more than one. Starting on one side of the patient, the midline is crossed until the contralateral lamina papyracea is reached. To achieve the maximum possible opening of the frontal sinus, it is helpful to identify the first olfactory fibres on both sides: the middle turbinate is exposed and cut from anterior to posterior along its origin at the skull base. After about 5 mm, the first olfactory fibre is observed coming out of a small bony hole. This provides excellent landmarks for the anterior border of the olfactory fossa on both sides which allows completion of the frontal sinus floor resection until close to the first olfactory fibre. Alternatively, this procedure can be done with the endoscope alone, although it is more time consuming. Finally, a rubber finger stall is placed into each frontal sinus and two more are put in the ethmoid cavity on each side. The rubber finger stalls do not stick to the surrounding tissue and are therefore easily and painlessly removed. In the interim, a major part of the surgical cavity has re-epithelized, making postoperative treatment simple. The primary lateral approach is recommended if the previous ethmoidal work was incomplete and the middle turbinate is still present as a landmark. One should adopt the primary medial approach if the ethmoid has been cleared and/or if the middle turbinate is absent. The medial approach begins with the partial resection of the perpendicular plate of the nasal septum, followed by identification of the first olfactory fibre on each side as already described. The principle difference between the endonasal median frontal sinus drainage and the classic external Jansen, Lothrop, Ritter, Lynch and Howarth operation is that the bony borders around the frontal sinus drainage are preserved. This makes it more stable in the long term and reduces the likelihood of reclosure by scarring, which may lead to recurrent frontal sinusitis or a mucocoele, as well as the avoidance of external scarring. Its use in patients with severe polyposis without these risk factors has not been determined and should be evaluated. Results of endonasal frontal sinus surgery Judging the results of endonasal frontal sinus surgery requires a postoperative follow up of ten or more years. Applying subjective and objective criteria to evaluate the success of endonasal frontal sinus drainage (grade 1, endoscopically normal mucosa, independent of the subjective complaints; grade 2, subjectively free of symptoms, but with endoscopically visible inflammatory mucosal changes; grade 3, no subjective improvement and pathologic mucosa, therefore failure), it was possible to achieve a success rate of 83. Results After a mean follow up of 62 months, 40 of 41 patients (98 percent) had a widely patent epithelized nasofrontal communication. Ninety-one percent of the patients with chronic frontal sinusitis or mucocoeles noted complete relief of their frontal discomfort within one week. This first series of re-evaluation of long-term results demonstrates the value of endonasal frontal sinus surgery. Only 8 percent of patients needed revision at follow up of between three and ten years. This approach permits an optimal view encompassing the entire frontal sinus and allows complete micro-endoscopic removal of mucosa and obliteration of the sinus with abdominal fat as described by Tato and Bergaglio, as far back as 1949. This operation is somewhere between the endonasal median drainage and the osteoplastic flap obliteration with regard to the extent of surgery. From this image, the contours of the frontal sinus are cut out as a template which is preserved in a disinfectant solution. For aesthetic purposes, shaving of the hair should be avoided, as generally the coronal incision is used. The evening before the operation, the hair should be washed with disinfectant solution to avoid infection. This ends in a fracture of the frontal sinus floor just posteriorly of the supraorbital ridge (continued over). Surgery requires general anaesthesia, with orotracheal intubation and the insertion of a pharyngeal pack to avoid aspiration. The preferred incision for uni- and bilateral osteoplastic frontal sinus operation in individuals with a full head of hair is the bitemporal coronal incision. In patients with male pattern baldness, the incision is located in the hair-bearing corona. Injection with local anaesthetic and suprarenin 1:200,000 or better 1:120,000, 15 minutes before making Chapter 118 the frontal sinus] 1517 the incision reduces bleeding. Using partly blunt, partly sharp dissection extending to the supraorbital ridge and over the root of the nose, the scalp flap is pulled caudally on both sides, leaving behind the periosteum and the bone, thus preserving the supraorbital and supratrochlear vascular nerve bundles. Next, the template of the frontal sinus that was excised from the occipito-frontal x-ray is carefully positioned on the root of the nose so that the borders of the frontal sinus can be marked on the periosteum. Then, the osteotomy is made in the bone, from which the periosteum has been elevated, a few millimetres inside the marked line. The oscillating saw is angled at 301 towards the frontal sinus, allowing a surface that is as wide as possible to be created for the later replacement of the bony lid. When opening the frontal sinus bilaterally, the intersinus septum must be separated from the anterior frontal sinus wall with an angled chisel. The supraorbital ridge slightly anterior to the controlled fracture in the region of the frontal sinus floor is preserved and the bony lid hinges on the periosteal flap. The diseased tissue is then removed according to the pathological-anatomical findings. Fractures must be exposed to their full extent, repositioned and, if necessary, a dural lesion should be treated with duraplasty. In cases secondary to trauma or osteoma, where there is healthy frontal sinus mucosa, it must be decided whether the mucosa around the infundibulum is sufficiently healthy to preserve the frontal sinus or whether obliteration should be carried out. If obliteration is indicated, the frontal sinus mucosa can be removed using a microscope and/or endoscope. The inner layer of the bony walls must be drilled away with a burr using a microscope and/or endoscope, as only by doing so can the mucosa be completely removed. In a high percentage of cases, simply macroscopically stripping off the mucosa leads to inflammatory recurrences and mucocoeles. It allows total removal of the mucosa leaving the bony vascular channels open, which facilitates the revascularization of fat, used for obliteration. In dangerous areas such as exposed dura and the central roof of the orbit, the frontal sinus mucosa is safely removed with a diamond drill under microscopic control, which in experienced hands is not a contraindication for the obliterative frontal sinus operation. The mucosa in the region of the frontonasal ostium is inverted nasally and the drainage opening is blocked with bone or cartilage splints fixed with fibrin glue. The bone can be taken from the calvarium, or more easily pinna conchal cartilage can be used. Through this three-layered closure, the frontal sinus is securely isolated from the nasal cavity, and growth of mucosa into the sinus with the associated risk of mucocoele formation prevented. Next, abdominal fat is harvested either via a pre-existing scar or an incision around the navel. The abdominal fat is temporarily placed in isotonic saline solution and is then placed into the frontal sinus with pieces held together by fibrin glue, until the sinus cavity is completely filled. The periosteal bone lid is replaced and wedged closed with a tap of the mallet and then the periosteum is sutured. If the bone lid fractures during elevation, these bony fragments should be fixed together either with absorbable threads, wire sutures or miniplates. Finally, the scalp flap is flipped back into place, two suction drainages are inserted and the coronal incision closed with single stitch sutures. The tube drains are removed no later than two days after surgery, otherwise removal is difficult and more painful. Persistent changes of the frontal contour (embossment, depression) occurred in 10. The amount of adipose tissue detectable in the last scan was less than 20 percent in the majority of cases (53 percent) and more than 60 percent in only 18 percent of cases and decreased significantly with time.
Purchase prozac toronto
If this tube leaks at less than 20 cm of water pressure through the subglottis mood disorder test cheap prozac 10mg with amex, the next larger size is placed. The nasal passages, nasopharynx, oropharynx, supraglottic and glottic airway should be assessed, and pathology such as choanal atresia, adenoid hypertrophy, tonsillar hypertrophy, laryngomalacia and vocal cord paralysis should be excluded. To avoid the risk of inducing laryngospasm, the nasopharyngoscope should not be advanced below the level of the glottis. Although the precise mechanism is unclear, laryngospasm may happen even in children with bilateral true vocal cord paralysis. The surgical and anaesthetic team must work together closely and must have specific knowledge of the paediatric airway and of appropriate instrumentation. In a child with a compromised airway, who does not have a tracheotomy tube, preoperative administration of dexamethasone, 0. Possible options include spontaneous ventilation, assisted ventilation, jet ventilation and apnoea with intermittent bag and mask ventilation. Spontaneous ventilation offers the best dynamic assessment of the airway and is thus recommended. Endoscopy may be performed with the laryngoscope introduced into the airway and suspended in position. Some surgeons prefer to expose the larynx with an Chapter 89 Laryngeal stenosis Table 89. Endoscopy may also be performed with a ventilating bronchoscope or a Hopkins rod telescope, keeping in mind that the technique itself is not as important as the information gained. We prefer to use the Hopkins rod telescope, exposing the larynx with a straight anaesthetic laryngoscope blade. The child spontaneously ventilates a mixture of sevoflurane and oxygen through an endotracheal tube placed in the oropharynx, and with additional intravenous anesthesia provided by propofol bolus. Rigid bronchoscopy provides a superior assessment of the larynx, especially the posterior glottic area. Flexible bronchoscopy is often extremely valuable in assessing a larynx that is difficult to access with rigid instrumentation and may provide valuable information about airway dynamics, such as the degree of pharyngeal collapse, glossoptosis and the presence of laryngomalacia, tracheomalacia or bronchomalacia. Flexible bronchoscopy also permits evaluation beyond the eighth generation of bronchi in older children and allows specific lavage of bronchial subsegments, which may provide information about silent aspiration if lipid-laden macrophages are found. Oesophagogastroduodenoscopy can provide information about oesophagitis, gastritis and the status of the lower oesophageal sphincter, especially in regard to whether a previous fundoplication is still functional. Preoperative evaluation of gastro-oesophageal reflux with dual probe pH monitoring and/or oesophageal biopsy is advisable, and should be mandatory in a child with an active larynx or recalcitrant airway stenosis following previous reconstruction. Placement of a pH probe may be done at the time of oesophagogastroduodenoscopy, at the time of bronchoscopic evaluation or may be performed as an elective procedure unrelated to endoscopic evaluation. Patients should be off antireflux medication for at least one week prior to pH probe placement. While normal paediatric values for the upper port do not exist, positive readings should be viewed with suspicion. The recently developed impedance probe not only measures acid, but can also provide an indication of the volume of a reflux bolus and the height in the oesophagus to which it progresses. This is more difficult to evaluate in a child who is entirely gastrostomy (G-tube) fed. Alternatively, a radio nucleotide spit study may be performed; a drop of radioactive material is placed on the tongue and its passage is monitored to either the stomach or lung fields. In a child suspected of aspirating, a bronchoalveolar lavage, which can identify lipid-laden macrophages, may be useful. This does not, however, provide useful information in a child who is wholly G-tube fed. In these children, preoperative evaluation to assess the relative risk of aspiration is strongly advocated. A barium swallow or video swallow study may provide information not only on the presence of aspiration, but also on what substances are most likely to be aspirated. A functional endoscopic evaluation of swallowing, whereby the larynx is visualized with a nasopharyngoscope while a child swallows food or drink, can provide valuable information about the relevant risk of aspiration and the mechanism of aspiration as well as the presence or absence of normal laryngeal sensation. Having knowledge of the possibility of postoperative aspiration allows for appropriate preoperative counselling and management to minimize this risk. Innately, there are three things that may be aspirated, namely food and drink presented by mouth, saliva and gastric reflux. Most children and families presented with the choice of a gastrostomy tube or a tracheotomy tube will chose the former. The primary aim of laryngotracheal reconstruction is decannulation, and this operative procedure is rarely warranted if decannulation cannot be achieved. In children with tracheotomy dependency, it is important to evaluate whether surgical correction of laryngeal stenosis will permit decannulation. Similarly, children with progressive neuromuscular disorders, diaphragmatic weakness or central hyperventilation syndrome, may not Evaluation of aspiration Paediatric airway reconstruction runs the inherent risk of turning a child with laryngeal stenosis into a chronic aspirator. While this risk cannot always be accurately evaluated preoperatively, in most cases a thorough evaluation provides ample warning signs. In a child who is tracheotomy dependent, copious tracheotomy secretions or secretions stained by food material indicate chronic Chapter 89 Laryngeal stenosis] 1155 be candidates for decannulation. If results of a sleep evaluation indicate pulmonary compromise that precludes decannulation, laryngeal reconstruction may be futile. Voice evaluation Voice evaluation in children with laryngeal stenosis, tracheotomy dependency or following laryngotracheal reconstruction is in its infancy and is poorly understood. It is clear, however, that laryngeal reconstruction can have a negative impact on the voice, particularly in children requiring supraglottic or glottic surgery and in those in whom a laryngofissure is required to reconstruct the airway. What is unclear is which underlying pathologies and reconstructive procedures place the voice at greatest risk, and also the extent to which a voice anomaly relates to the initial aetiology of the laryngotracheal stenosis. Children have a tremendous drive to communicate, which often compensates for severe anatomic dysfunction. In these children, laryngotracheal reconstruction may be extremely beneficial in terms of regaining voice, even if decannulation is not achieved. In some children, a period of observation prior to considering surgical intervention is the best course of action. This strategy is most appropriate in a child with an active or inflamed larynx that is not amenable to medical intervention. An active larynx is generally related to gastro-oesophageal reflux disease or eosinophilic oesophagitis and is, therefore, potentially amenable to such intervention. In children in whom the aetiology of an active larynx is unknown, laryngeal reconstruction is unwise until the laryngeal inflammation has improved. A waiting period is also advisable in a child who has recalcitrant stenosis after a recent airway reconstruction, or in a child whose larynx is healing from laryngeal trauma. While laryngotracheal reconstruction can be effectively performed in children less than 3 kg if other criteria permit, a 10 kg guideline is most commonly used. Nevertheless, airway reconstruction of a larger child is technically much easier to perform. In a child with a high risk for aspiration or with certain craniofacial anomalies, surgical reconstruction may be inappropriate in that the laryngeal stenosis may actually protect the lungs from aspiration. In some children, ongoing aspiration may lead to a consideration of laryngotracheal separation rather than laryngeal reconstruction. While not universally accepted or rigorously proven, most experts in paediatric laryngotracheal reconstruction believe that gastrooesophageal reflux disease is both a cofactor for the development of subglottic stenosis and a negative influence on the outcome of operative reconstruction. Although a child with a progressive neuromuscular disorder may be considered for laryngotracheal reconstruction to improve vocal function, this seldom enables long-term decannulation. The child with complex medical problems Historically, children presenting for airway reconstruction were otherwise healthy children with a stenosed larynx. In such children, an interdisciplinary team approach is advisable for adequate assessment both before and after planned reconstruction. The most important decision to be made is whether it is advisable to even attempt reconstruction. If so, consideration must be given to other interventions indicated prior to proceeding with laryngeal reconstruction.
Isatis Tinctoria (Isatis). Prozac.
- Dosing considerations for Isatis.
- What is Isatis?
- Prostate cancer, upper respiratory infections, inflammation in the brain, hepatitis, lung abscess, psoriasis, diarrhea, and HIV.
- How does Isatis work?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96877
Buy prozac 40 mg with visa
Active anterior rhinomanometry mood disorder activities 60 mg prozac for sale, using surgical tape to seal a pressure-sensing tube into the nasal passage, is one of the most commonly used methods for clinical determination of nasal resistance. Nasal airway resistance can also be measured by use of a head-out body plethysmograph (displacement type) and, with this method, the flow head is located on the side of the body-box and the pressure-sensing tube is passed along the floor of the nasal cavity. This is to control for air leaks around the mask which are a common source of error. A single measurement of nasal airway resistance is unreliable and a standard operating procedure should be implemented to prevent investigator bias when gathering data. This equation is a compromise that has been generally accepted by rhinologists and it does not take into consideration the separate components of laminar and turbulent airflow. Nasal airflow increases with increase of transnasal pressure, but at higher pressures there is a limitation of flow due to the increased frictional effects of turbulent airflow. The flow-limiting effect of nasal alar collapse is only apparent during rapid or close to maximum inspiratory manoeuvres. The curvilinear relationship between transnasal pressure and flow means that one cannot simply determine nasal resistance from the slope of the graph, as would be the case with a straight-line relationship. It is, however, possible to define the resistance at any given sample point along the curve and this has been the solution recommended for a standardized measurement of nasal resistance. The right and left nasal airflows are normally asymmetrical due to the nasal cycle and therefore a single pressure value may relate to two different airflows. It is, therefore, sensible to standardize nasal resistance by measuring both nasal airflows at the same sample pressure point rather than by measuring transnasal pressures at the same sample flow point. Unilateral nasal airflow measured at a sample pressure point of 150 Pa and bilateral nasal airflow measured at 75 Pa are recommended as universal standards. When quoting values for total nasal resistance it should be stated whether the value was obtained by measurement of total nasal airflow using posterior rhinomanometry, or whether the airflows of the nasal passages have been measured separately. It is possible to sample the curve at numerous points and obtain an average resistance value with the aid of a microprocessor, and this technique has particular advantages when comparing the resistance values of different segments of the respiratory tract. Normal nasal airflow In adult subjects free from signs of nasal disease, mean total resistance has been reported to be around 0. Studies by Broms9 have provided a table of predictive values for height and nasal resistance in the decongested nose that are useful in assessing the extent of any deviation from normality in patients with nasal skeletal stenosis. Total nasal resistance gives an overall measure of nasal function, however, it is a very crude measurement as it provides no information about the separate nasal passages. Rhinologists have a dilemma when assessing nasal function as the nose consists of two separate dynamic airways. The ophthalmologist or audiologist would never consider using a bilateral measure of vision or hearing when assessing function as this measure could fail to detect blindness in one eye or deafness in one ear. Similarly, the measurement of total resistance may fail to detect unilateral nasal obstruction. However, it is not very informative to quote the mean of unilateral resistance when measured over several hours because this mean value will have a large standard deviation due to the instability of unilateral resistance. The range of unilateral nasal airway resistance in a group of healthy volunteers when recorded over a six to eight hour period has been shown to vary from 0. One way to overcome the dilemma of spontaneous changes in unilateral nasal resistance is to decongest the nose prior to assessment. This solution is of use to the Chapter 107 Measurement of the nasal airway] 1375 surgeon whose main interest may be in assessing the extent of any nasal anatomical problem. One solution is to quantify the extremes of unilateral resistance or the amplitude of the unilateral changes in resistance that occur over a period of several hours. This approach has been used to determine the unilateral changes in resistance and to assess the efficacy of nasal surgery. The advantage of unilateral measurements are that they provide a comprehensive assessment of the dynamic nose rather than the crude snapshot that is provided by a single measure of total resistance. The accuracy of acoustic rhinometry like rhinomanometry is dependent on the interface between the equipment and the nose. For example, the cross-sectional area of the nasal vestibule is susceptible to distortion if a tube is inserted into the nose. Mispositioning of the nasal tube and air leaks are just as likely to give spurious measurements with acoustic rhinometry as face mask leaks with rhinomanometry, but with care the technique of acoustic rhinometry provides reproducible data. The resolution of acoustic rhinometry is also limited by the speed of sound and this means that the maximum linear resolution of this device can only be around 7 mm. The method consists of generating an acoustic pulse from a spark source or speaker and the sound pulse is transmitted along a tube into the nose. The sound pulse is reflected back from inside the nose according to changes in the local acoustic impedance which are related to the cross-sectional area of the nasal cavity. The reflected sound is detected by a microphone, which transmits the sound signal to an amplifier and computer system for processing into an area distance graph. The cross-sectional area measurements obtained with acoustic rhinometry correlate extremely well with area measurements made by computed tomography scans, and nasal airway resistance measured by rhinomanometry, but the accuracy of acoustic rhinometry is unreliable in the posterior part of the nose, especially when the nasal passage is congested. The plot of crosssectional area against distance can also be expressed as nasal volume for given distances along the nasal passage. Technical specifications for standard operating procedures for acoustic rhinometry have been standardized as regards the accuracy and repeatability of measurements and the acquisition of data. The measurement is effort dependent and is less sensitive than rhinomanometry or acoustic rhinometry in determining small changes in conductance. Simple peak flow instruments such as the Wright, miniWright and Youlten flow meters are often used to measure nasal peak flow with the use of a face mask. However, the use of more sensitive spirometers can improve the accuracy and reproducibility of nasal measurements. It is based on a comparison of the acoustic output from the nose and the mouth for a given spoken word or phrase. Subjects with Normal values for acoustic rhinometry the normal value for minimum cross-sectional area for a nasal passage is quoted as 0. Nasalance is the measure of the ratio of sound output from the nose compared with the sound output from the mouth, expressed as a percentage. There is an inverse relationship between nasalance and nasal airway resistance, and subjects with nasal obstruction will have a low measure of nasalance, whereas a subject with a patent nose, especially after decongestion, will have a high nasalance. The measurement of nasalance is used to assess the quality of speech by speech therapists, and can also be used to study speech in patients with disorders of palatal function, such as cleft palate or following surgery of the palate. The changes in position of the turbinate can be plotted by directly observing the turbinate through a binocular microscope. The technique of measuring the position of the inferior turbinate by means of microscopy is termed rhinostereometry. The subjects head is fixed rigidly by the subject biting onto a tailor made tooth-splint fixed to the frame of the microscope stand. The changes in position of the turbinate can be measured in millimetres by means of a scale on the eye-piece of the microscope. Studies on the nasal cycle have demonstrated that the mucosal swelling causes the turbinate to change position by up to 3. However, measurements of resistance do not provide a direct measure of how the airflow is partitioned between the two nasal passages. With each breath the tidal volume is divided at the nose into two airstreams according to the relative resistance to airflow of each nasal passage. Deviation of the nasal septum is likely to cause an anatomical asymmetry of the nasal passages and influence the partitioning of nasal airflow. Measurement of the partitioning of nasal airflow can be made by measuring the volume of air expired from each side of the nose with a spirometer during a slow vital capacity manoeuvre. The introduction of small portable spirometers means that spirometry is not limited to the research laboratory and measurements can be easily made in the clinic. Measurements of partitioning of nasal airflow have been used to monitor the physiological changes in airflow associated with the nasal cycle and after nasal decongestion they may be useful to assess the anatomical changes in airflow associated with nasal septal deviation, pre- and postoperatively. However, in the assessment and treatment of nasal disease the clinician is mainly concerned with restoring normal nasal function to the nasal airway by reducing nasal obstruction by medical or surgical means. Congestion in the ethmoid region may cause contact of ethmoid surfaces and a sensation of pressure and obstruction that would have little or no effect on nasal airway resistance. Similarly, pressure changes in the middle ear and paranasal sinuses may cause a sensation of nasal obstruction without any effect on nasal airway resistance. Another factor that may explain the lack of correlation between objective and subjective measures of nasal obstruction is that the nasal airway consists of two parallel airways and the total nasal conductance may be near normal even if one nasal passage is obstructed.
Best prozac 20 mg
This was supplemented by a hand search of current journals and by reference to the published results of the National Prospective Tonsillectomy Audit available on the Royal College of Surgeons of England website ( Children are offered surgery primarily to reduce the frequency and severity of recurrent sore throats depression group activities order prozac cheap. This chapter focuses on the role of tonsil surgery in recurrent sore throats in children. Participation was dependent on children having a history of seven episodes of sore throat in the year prior to the study, five or more in the preceding two years or three or more in each of the preceding three years. Children randomized to the nonsurgical group proceeded to surgery at the subsequent request of the parents. Children having adenoidectomy, as well as tonsillectomy, were included, making it impossible to exclude this intervention as relevant to the outcome of treatment. Children in the control limb of the study had active therapy, which may have minimized the morbidity. A number of randomized controlled studies of varying but generally poor quality have subsequently contributed little. Two parallel randomized controlled trials compared surgery with nonsurgical management for children with a history of recurrent episodes of throat infection, but with less stringent entry criteria than for the original studies. Benefits were marginal, such that the authors concluded that the benefits were outweighed in this group of children by the morbidity and risks of the operation. The authors concluded that adenotonsillectomy had no major clinical benefits over watchful waiting in children with mild upper respiratory symptoms. Perhaps inadequate knowledge of the natural history and expected outcome of recurrent sore throats in children has bedevilled the quest for a sound evidential base for current practice. In a randomized controlled trial in adults, 36 participants underwent immediate tonsillectomy. Follow-up was short but at 90 days, streptococcal pharyngitis had recurred in 24 percent of the control group and in 3 percent of the tonsillectomy group. The authors concluded that adults with a history of recurrent streptococcal pharyngitis were less likely to have further streptococcal or other throat infections or days with throat pain if they had their tonsils removed. The overwhelming view of clinicians is that in judiciously chosen patients tonsillectomy brings about significant benefit. The results of the Scottish Tonsillectomy Audit found a high level of satisfaction among those undergoing surgery (97 percent satisfaction rate at one year). Despite the availability of guidelines and protocols in practice, a decision to undertake tonsillectomy is made by negotiation between the parent/carer and the otolaryngologist. Some units have introduced nurse-led clinics where strict protocols are used to determine eligibility for surgery. It will be illuminating to see if these protocols have a material effect on surgery rates. Sociocultural factors There is no published evidence that the pattern of disease varies by racial, ethnic, climatic or cultural factors across the globe, but there are wide variations in the rate of tonsillectomy by geographical region. In the Scottish Tonsillectomy Audit, sizeable variations in tonsillectomy rate were found between different regions in the same country, from four per 10,000 in Forth Valley to ten per 10,000 in Dumfries and Galloway. In the developing world, the incidence of surgery is much lower, related perhaps to access to health care and parental expectations and preferences. Tonsillectomy is more common in large conurbations suffering higher levels of deprivation. Data from the Department of Health Statistics show that around 30,000 of these were in children with an approximately equal gender ratio ( The majority are for recurrent sore throats with most of the remainder for airway obstruction. Patients should meet all the following criteria: sore throats due to tonsillitis; five or more episodes of sore throat per year; symptoms for at least a year; episodes of disabling sore throat which prevent normal functioning. The results of evaluation of quality of life before and after the operation suggest that tonsil disease has a marked adverse effect on quality of life and that there is significant benefit from surgery. Given the frequency with which tonsil surgery is performed, it should be easy to teach, but above all it must be safe. In recent years, perceived advantages in terms of reduced blood loss, less pain, more rapid healing and easier surgical technique have led to the introduction of several new methods. As with any surgical procedure, the risks of surgery must be balanced against the potential benefit. Cognizance should be taken of whether the frequency of episodes is increasing or decreasing. The difficulties associated with implementing guidelines and the paucity of effect of guidelines on clinical practice are well known. Moreover, when guidelines are broken, they tend to be broken more often in favour of offering rather than withholding surgery. A relatively low cost but high volume procedure to alleviate a troublesome but nonlife-threatening condition, the operation has attracted the attention of those with an interest in the economics of health care. In uncomplicated cases, this usually involves at least two weeks absence from school with attendant implications for the parent or carer. Healthrelated quality of life indices and the economic aspects of sore throats in children have now been considered. Blood vessels traversing the plane of dissection are dealt with either by ligature or diathermy as required. Blood loss during tonsillectomy can be considerable and may constitute over 10 percent of total circulating blood volume. Diathermy tonsillectomy In recent years, the technique has evolved of using diathermy not only as an aid to haemostasis when the tonsil has been delivered, but to dissect the tonsil from its bed. This has the obvious advantage from the point of view of both operator and patient, particularly if a child, of reducing intraoperative blood loss to a minimum. Various claims and counterclaims have been made regarding the advantages and disadvantages of this technique, the most common alternative to traditional cold steel tonsillectomy. These demonstrated reduced intraoperative bleeding but increased pain in the diathermy group, with no difference in secondary haemorrhage rate. When a patient is counselled for surgery, the risk of tonsillectomy complications, and in particular postoperative haemorrhage, should be carefully explained to the patients/parents. Surgeons using monopolar diathermy should consider using an alternative technique. All trainee surgeons should become competent in cold steel dissection and haemostasis using ties, before learning other techniques in tonsillectomy. Inexperienced trainees must be supervised by a more senior surgeon until competency has been achieved. Irrespective of seniority and experience, surgeons who wish to start using new techniques, such as coblation, should undergo appropriate training. For tonsillectomy, data should be presented by the surgeon, indicating the technique used for dissection and haemostasis and power settings if applicable, type of instrument used, and any difficulties encountered. It is the responsibility of the surgeon, and if appropriate his trainer, to follow up any identified problems appropriately. Use of single-use instruments should also be recorded, especially for cold steel dissection. There is an urgent need for new standards for diathermy machines so that the amount of power used is obvious to the user. Manufacturers of diathermy machines should be encouraged to produce machines with information on the total amount of energy delivered to patients. Hospitals should encourage the use of machines that provide clear information on power settings. Manufacturers of single-use instruments should be encouraged to improve the quality of the instruments. Reprinted from the National Prospective Tonsillectomy Audit, available on the Royal College of Surgeons of England website ( Chapter 96 Tonsillectomy] 1235 Coblations tonsillectomy this relies on the use of a specially designed bipolar electrical probe, which both coagulates and cuts the tissues as it develops the dissection plane between tonsil and capsule.
Buy 10 mg prozac visa
Laryngeal papillomas: histomorphometric evaluation of multiple and solitary lesions vascular depression definition discount 40 mg prozac mastercard. Recurrent respiratory papillomatosis in children: a retrospective study of management and complications. Voice quality of prepubescent children with quiescent recurrent respiratory papillomatosis. A review of current thinking and an outline of a proposed study to further unravel the aetiology and pathogenesis of this complex disease. They are inclined to place toys, foodstuff and household articles in the ear, nose or the oral cavity. Foreign bodies lodged within the ear, nose, larynx, trachea, pharynx or oesophagus may present as a minor irritation or a life-threatening problem. Foreign bodies within the external auditory canal can be classified as inanimate or animate. Inanimate objects can be inert or corrosive/irritant, organic or nonorganic and hydrophobic or hydrophilic. Presentation Although it is usually children that present with aural foreign bodies, self-instrumentation of the ear canal not infrequently brings the embarrassed adult to the otolaryngologist. Inert foreign bodies may be completely asymptomatic and go unnoticed for many weeks, months or even years. Gradual wax impaction medial to a small foreign body may lead to a later presentation due to the disruption of the physiological keratinocyte migration. Although the pinna is a part of the external ear, diseases of the pinna are covered in Chapter 236, Conditions of the pinna and external auditory canal; Chapter 236g, Acquired atresia of the external ear; Chapter Chapter 92 Foreign bodies in the ear and the aerodigestive tract in children] 1185 the isthmus is the narrowest part of the external auditory canal and objects frequently impact at this point. Button batteries are arguably the most dangerous foreign body in the ear, producing tissue necrosis as the alkaline fluid seeps out of them. General anaesthesia may be required for removal of up to 30 percent of objects, especially in the paediatric population. The use of the otomicroscope has been shown to produce a higher success rate for foreign body removal. Although some individuals will require surgical removal via an end-aural incision,13 there are now case reports of the use of acetone14 and warm 3 percent hydrogen peroxide15 which suggest these conservative techniques may be worth trying before subjecting a child to general anaesthesia. Repeated unsuccessful attempts at foreign body removal by an inexperienced practitioner will distress an anxious child and may compromise the options open to an otolaryngologist. If there is any doubt whatsoever about the potential success of an attempted extraction, then referral to a specialist is indicated. The otolaryngologist should have a low threshold for arranging a semi-urgent admission for general anaesthetic removal if conservative methods fail. Urgent removal can only be justified for battery removal, or where severe oedema and symptoms exist. Oils performed poorly (51 seconds) and water and saline were particularly slow (180 seconds). If a nasal foreign body slips back into the nasopharynx it will usually be swallowed or expectorated. No complication of barotrauma to either the ears or lower airway has been reported in the literature search employed for this chapter. Soft objects such as sponge fragments or tissue paper are the commonest to be found in the nose, in contrast to the hard objects inserted into the ears. Rigid endoscopes provide excellent visualization and can potentially minimize mucosal trauma. Although it has been claimed that a 4 mm rigid nasendoscope can be passed with ease in children as young as two years of age without decongestion,19 with the increased availability of smaller 2. The use of nebulized adrenaline provides excellent nasal decongestion and can greatly facilitate removal of foreign bodies, either by nose blowing or using instrumentation. Magnets may be of use21 and nasal washing has been proposed as a method of removing foreign bodies, but is not widely practised. Rhinolith A rhinolith is a partially or totally calcified mass of tissue in the nasal cavity which may form around a foreign body nidus or can develop de novo. Each mucin layer subsequently becomes calcified, perhaps aided by the presence of turbulent air currents. They are classified as endogenous when they form around normal body material, such as blood clots, misplaced tooth remnants or bony sequestra. Ingested foreign bodies in children represent a major global public health problem. Chapter 92 Foreign bodies in the ear and the aerodigestive tract in children] 1187 and nuts for tracheobronchial aspiration. Bear in mind that an object in the upper oesophagus can cause airway obstruction by pressing on the adjacent trachea. Once the presumptive diagnosis of a pharyngo-oesophageal foreign body has been made, arrangements should be made for early removal as oedema and mucosal swelling will make retrieval more difficult. The use of rigid angled nasendoscopes and curved forceps designed for fish bone removal has greatly facilitated fish bone removal from the oropharynx under local anaesthetic in adults,39 but general anaesthesia is more likely to be needed in a child. Other original techniques, such as using nasal suction catheters in conjunction with nasendoscopy, have also been described. The vast majority of swallowed objects pass through the digestive tract and are excreted, often undetected. There is a clear history of ingestion in 96 percent and the median age was three years in a retrospective ten-year review of 327 patients. Complications, including respiratory symptoms and abscess formation, occured in 7. For the investigation and management of suspected perforation of the oesophagus the reader is referred to Chapter 156, Oesophageal diseases. Emergency practitioners use this fact to argue for the widespread teaching of airway-clearing manoeuvres to new parents. Tracheo-bronchial tree the peak incidence of inhaled foreign bodies is between the ages of one and three years, with a male:female ratio of 2:1. This can be followed by a relatively symptom-free period as the object lodges in the lower airway. Partial obstruction of one of the main stem bronchi causes the characteristic wheeze over one side of the chest on auscultation and the hyperinflation of one lung evident on chest x-ray, although these classical findings are by no means universal. Upon expiration, the positive pulmonary pressure compresses the main bronchi, occluding the airway around the offending object, preventing expulsion of the air. Although most patients present with a history of wheeze or cough, up to 20 percent may present after several days due to secondary respiratory complications. Residents may only Larynx Glottic impaction of a foreign body often leads to laryngospasm and sudden complete airway obstruction and death with peak incidence at one to three years. In recent years, audit has shown that 85 percent of airways are cleared before emergency teams arrive, with 38 percent being cleared by the children themselves. If the foreign body goes untreated, mediastinal shift, pneumothorax or pneumonia are common sequelae. Smaller foreign bodies may induce granuloma formation and an aggressive search for the foreign body must be made in new cases of bronchial granuloma. Once a foreign body is removed, a meticulous examination of the tracheobronchial tree must be undertaken to exclude further foreign bodies/fragments or other abnormalities. In a series of 250 patients with tracheobronchial foreign bodies, there was a clear history of ingestion in only 38 percent of cases and over 99 percent of cases were successfully treated endoscopically. When bronchoscopy was performed, foreign bodies were identified and removed in 80 percent of cases. The sensitivity of a chest radiograph was 66 percent with a specificity of 51 percent. The combination of history, signs and radiological abnormalities is more useful than any one separately and a high index of suspicion is essential. Otolaryngologists traditionally believe rigid endoscopes to be the optimal instrument for tracheo-bronchial foreign bodies.