Buy acarbose no prescription
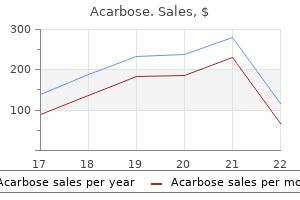
Prognosis and natural history Inflammatory polyps can be lethal in infants and adults alike blood glucose greater than 400 50mg acarbose mastercard, when they cause significant airway obstruction or secondary infectious pneumonias. Individuals with documented lesions have been followed for up to 30 years before requiring their removal. Those associated with infection may be treated with antimicrobials, while aerosolized or systemic corticosteroids may be efficacious in patients with inhalation-injury-induced lesions or asthma. Special clinical features Solitary squamous papillomas commonly afflict men in their sixth or seventh decades of life. Patients usually present with obstructive symptoms, including dyspnea, hoarseness, wheezing and chest pain, as well as fever and productive cough, indicating pneumonia. The younger the child is at his/her first presentation, the more severe the disease. The disease usually recurs many times over many years, becomes widespread and extends into the bronchial tree in up to 5% of patients. Confusion regarding classification appears to be a thing of the past, as one can categorize endobronchial and even endobronchiolar papillomas according to number, location and histology. Squamous cell papillomas Classification, cell of origin, pathogenesis and etiology Squamous cell papillomas can be solitary or multiple, exophytic or inverted. Animal studies conducted in 1933 suggested an infectious, probably viral, etiology. Normal lung is reduced to a bronchiectatic cavity filled with white-tan friable papillary fronds. This computed tomogram shows not only a narrowed trachea, but significant pulmonary centrilobular nodules. Air-fluid levels are not uncommon in the cysts and represent either post-obstructive pneumatoceles or cavitating papillomas. This modality reduces the risk of downward spread of virus, noted in bronchoscopy patients. Bronchiectasis develops proximal and distal to the papilloma on account of the tumor and consequent post-obstructive atelectasis/pneumonia. Large lesions may fill bronchiectatic airways and surrounding lung may form a rim of firm white fibrous tissue. This endobronchial papilloma demonstrates classic architectural features: arborizing fibrovascular cores covered by a proliferative squamous epithelium. Cavitation and surrounding lung fibrosis are also not uncommon; the latter may even suggest tumor invasion. The mass lesions can grow to large sizes and essentially replace entire pulmonary segments. Each fragment is remarkably similar in size and with regard to amount of epithelial proliferation. Exophytic lesions have orderly epithelial maturation extending from the basal layer to the superficial flattened and usually keratinized surface cells. Acanthosis and nonkeratinized surfaces are often seen, along with intraepithelial neutrophils. Not unlike urinary bladder inverted papillomas, endobronchial lesions are exophytic with invaginated nests of bland squamous mucosa. In rare instances atypia reaching the level of carcinoma in situ may be present and in such instances a diagnosis of carcinoma arising in a squamous papilloma should be rendered. The amounts of stroma and stromal lymphoplasmacytic infiltrates vary from very scant to prominent, while the adjacent respiratory mucosa may be normal, inflamed, hyperplastic or metaplastic. These rare lesions are non-keratinizing and show orderly maturation from the basal layer upward. Well-circumscribed, solid, intra-alveolar nests of cytologically bland, non-keratinizing squamous cells may fill alveolar spaces. Distinguishing this process from invasive squamous cell carcinoma can be very difficult. The surrounding lung may be inflamed and/or fibrotic but infiltrative tumor tongues indicative of invasive carcinoma are not appreciated. Bronchial and alveolar parenchymal involvement with laryngotracheal papillomatosis is morphologically similar to the isolated lesions; however, virtually all lesions feature viral cytopathic effect. Multinucleation may be seen and nuclei vary from small and pyknotic to large with evenly distributed coarse chromatin. Smaller basal cells with scant basophilic cytoplasm and round regular nuclei are also noted along with background neutrophils. Scattered single cells are also 854 Chapter 22: Benign epithelial neoplasms and tumor-like proliferations of the lung described. However, positivity appears to correlate with the morphological presence of koilocytosis. Recognizing even focal carcinoma within an otherwise benign squamous papilloma warrants a diagnosis of carcinoma. Prognosis and natural history Surgically resected solitary squamous cell papillomas do not recur, but up to 20% of patients treated with endoscopic removal experience local recurrences. The disease can undergo spontaneous remission, persist as stable disease, or progress. Extralaryngeal spread is noted in approximately 30% of children and less than 20% of adults. The most frequent sites of spread in decreasing order of frequency are the oral cavity, trachea, bronchi, and esophagus. As discussed above, inflammatory polyps lack a true papillary architecture, stromal cores and proliferative epithelium. Squamous cell carcinomas can be endobronchial and papillary but cytological features of overt malignancy are usually appreciated, even when stromal invasion is not obvious. Unlike papillomas, well-differentiated squamous cell carcinomas lack orderly epithelial maturation and often feature keratinization. Difficulties arise when one misinterprets entrapped seromucinous glands for invasion into the polyp stalk. Glandular and mixed squamous cell and glandular papillomas As no more than a dozen glandular papillomas are described in the thoracic literature, comments are very limited. Tumors may closely resemble Schneiderian papillomas of the upper respiratory tract. The glandular epithelium may be ciliated, cuboidal or columnar, and interspersed mucin-rich cells are often identified. A basal cell layer is often apparent and can be highlighted with either p63, K903 or cytokeratin17 immunohistochemical stains. Since cytology and biopsy samples cannot discern these rare lesions from very common adenocarcinomas, surgical resections are required. Mucus gland adenomas feature mucusfilled cysts and tubules, while papillary adenomas are true pulmonary parenchymal, rather than endobronchial lesions. All but one reported case was treated surgically and the only recurrence and death was in the patient unable to tolerate anything more than bronchoscopic treatments. Uniform columnar cells with eosinophilic cytoplasm, round regular nuclei and interspersed mucin-rich cells are surrounded with inflammatory cell-rich mucin while stromal cores contain many plasma cells. Inflamed arborizing papillary cores are lined with discrete foci of glandular and squamous epithelium. Glandular atypia is considered reactive, while squamous atypia is believed to be neoplastic. Minute welldemarcated lesions owe their nodularity to thickened alveolar septa and intraalveolar macrophages. Lesional epithelial cells grow along alveolar walls and feature eosinophlic cytoplasm and round nuclei with vesicular chromatin. Rare multinucleated cells are noted but marked atypia, mitoses or necrosis are absent. Alveolar macrophages also contribute to the nodular character of the lesion by filling airspaces lined by the epithelial cells. Macroscopic pathology Most reported lesions lack macroscopic descriptions but several case reports describe 0. Crowded epithelial cells in the 858 Chapter 22: Benign epithelial neoplasms and tumor-like proliferations of the lung proliferations, very difficult. Multifocal micronodular pneumocyte hyperplasia also features more pronounced alveolar septal thickening and intra-alveolar macrophages.
Buy discount acarbose 25mg
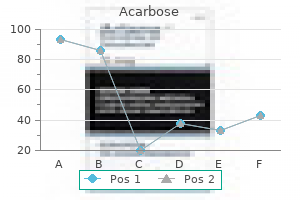
Lung parenchyma surrounding or distal to a carcinoma or other obstructive bronchial lesion may show small inflammatory foci in which a few alveoli feature an alveolar cell proliferation diabetes symptoms early signs order acarbose overnight. These lesions are often in the centriacinar region and demonstrate interstitial inflammation and airspaces filled with macrophages, some "foamy", mononuclear cells and occasional neutrophils. This is a focal, nonspecific inflammatory lesion, probably related to infection or aspiration. This change has also been referred to as "bronchiolization of alveoli" and Lambertosis (see Chapter 17). There may be some chronic inflammation and quite dense fibrous tissue is characteristic. Attention to the cell population lining the lesion airspaces ensures a correct diagnosis. Papillary and alveolar adenomas are benign neoplasms, which occur very rarely in the lung parenchyma (see Chapter 22). These lesions both measure greater than 1 cm and feature either true fibrovascular cores or cystic patterns, respectively. The cells in this lesion are more atypical, columnar and show some nuclear pleomorphism. Increased tumor cell height, greater than the height of columnar cells in associated or adjacent bronchioles 2. Cells growing in a so-called "picket fence" type pattern or the formation of true papillae 3. These are small lesion numbers, considering both lungs were available for examination. Mention has been made of the importance of well-prepared lung tissue, unobscured by other diseases, such as pneumonia, fibrosis, etc. Some data are presented in Table 9, taken from both prospective and retrospective studies. Some figures are not primary source data but reports of data from elsewhere265,266 and others are not prospectively gathered. Atypical adenomatous hyperplasia is common in lungs bearing primary adenocarcinoma. There is ultrastructural and immunohistochemical evidence that possibly a substantial proportion of large cell carcinomas are "dedifferentiated" adenocarcinomas. Some of the Japanese studies report large numbers of adenosquamous carcinomas in their "others" categories (Table 9). It is not clear what criteria were used for this diagnosis and whether, as with large cell carcinoma, an association with adenocarcinoma is being disguised by diagnostic classification. When exposed to asbestos, rats develop pulmonary "adenomatosis" and adenocarcinomas. East Asian populations have a higher incidence of pulmonary adenocarcinoma, in comparison to Western cohorts. Limitations to these studies include the difficulty in identifying lesions of sufficient quality and quantity. These variations probably reflect different definitions of "positive staining", different anti-p53 antibodies used, and variations in the immunohistochemistry process leading to differences in the sensitivity of protein detection. P21 (waf1/cip1) is upregulated by p53 and inhibits cell cycle progression by promoting G1 arrest. The findings are variable and most of these mutations have been deletions in exon 19 or the L858R point mutation in exon 21 (Table 14). In most Japanese studies there seems to be a consistent rise in mutation prevalence as the lesion grade increases. The single P63 protein is a homolog of p53 which probably has regulatory function over P53. The deltaN isotype is found in basal cells, including those of the bronchiolar epithelium, and probably maintains stem-like properties and proliferative capacity. Up to 40% of lung adenocarcinomas show point mutations in codons 12, 13 or 61, with codon 12 being the most frequently altered. G:T transversions are the most frequent change in adenocarcinomas and these are probably related to tobacco exposure. These mutations may be differentially expressed in histologically different areas of the same tumor. This is not the case in Caucasians but whether this is related to smoking, other environmental factors, constitutive genomics or other unknown factors remains to be determined. As such they represent at least a potential risk factor for the development of this increasingly common form of lung cancer. Thus, there are problems in designing longitudinal studies of lesions, to see how, if at all, they progress (see below). Thus the patient is at risk of developing, and dying from a second lung adenocarcinoma. Follow-up studies published to date have mostly used postoperative survival as their endpoint. Lesions were found in the second samples but in two cases (autopsy and completion pneumonectomy) there was a contrast between the large amount of disease in the original and relative lack of disease in the subsequent sample. This is no more than anecdotal comment, but the prospect of a lobectomy not only removing the primary tumor but the larger "at risk" zone which has undergone greater field cancerization than the rest of the lung is intriguing. If this zone is resected with the tumor, then the postoperative risk of second tumors may be less than assumed. One of the most important factors pertaining to preinvasive lesions is the risk of subsequent invasion. More recent work, with advanced scanners, shows promise of better radiological distinction between lesions. All these factors provide evidence that this lesion is a pre-invasive lung lesion; a progenitor of pulmonary adenocarcinogenesis. The histological distinction between these two lesions is difficult and arbitrary. This process may be associated with chronic inflammation and "burnt out" alveolar scars may result. There are similarities between this process and adenocarcinogenesis in association with pulmonary fibrosis, in terms of a proliferative alveolar epithelium undergoing malignant transformation. It is also possible that some adenocarcinomas may arise "de novo" from bronchioloalveolar epithelium. There are at least three well-described pathways of tumor development, which have recognizable morphological changes. Other lesions, such as some proposed patterns of bronchial dysplasia and bronchiolar columnar cell dysplasia, have been suggested as alternative pre-invasive lesions. These deserve consideration but require a greater collective experience and understanding before their true role can be understood. These pathological lesions are well described, the diagnostic challenges arising from their classification are numerous and much is known about the molecular alterations found in this disease complex. Currently there is focus on the possibility of 928 Chapter 23: Pulmonary pre-invasive disease using such molecular markers to facilitate early detection of disease; in practice this would probably be a sputum-based test. There has been a substantial rise in the amount of literature on this subject in the last 10 years, the most recent work concentrating on various aspects of the molecular biology of the process. Among the many fascinating but still largely unanswered questions in this area concern issues around who actually develops pre-invasive lung diseases, what determines which lesions will progress, and which type of invasive tumor develops. Elements of environment and lifestyle expose the lung epithelium to a range of carcinogens. These two major pathways of lung carcinogenesis reflect a common response (malignant transformation) in two separate epithelial compartments. The bronchial epithelium gives rise to several tumor types; it may be that certain molecular events determine which tumor type arises from a common epithelial precursor. Equally, in some cases, the tumor type identified at clinical presentation may be the result of neoplastic progression and/ or dedifferentiation after the lesion becomes malignant. There is evidence that lung adenocarcinomas in particular may have considerable capacity to evolve as the lesion grows. Apart from issues around detection of disease, risk of progression is a key factor in the clinical management of pre-invasive lung disease. Many studies are confounded by various factors, including the understandable ethically driven desire and need to treat disease, rather than to observe its potential evolution into something with metastatic ability. Whether molecular factors can give any insight into the risk of progression remains to be seen. On the other, potential overtreatment of dysplasia or in situ disease risks unnecessary morbidity while depriving clinicians of the opportunity of answering some fundamental questions.
Syndromes
- Feelings that you cannot leave the house.
- Name of the product (ingredients and strengths, if known)
- Breathing tube
- Diving into shallow water
- Lasts for up to several days
- Skin cells
- High blood pressure
- Treatment of other disorders
- To develop ways of coping with the painful body sensations
Purchase acarbose on line amex
Hepatocyte growth factor induces gefitinib resistance of lung adenocarcinoma with epidermal growth factor receptor-activating mutations diabetes mellitus type 2 hereditary buy genuine acarbose online. Comprehensive histologic assessment helps to differentiate multiple lung primary nonsmall cell carcinomas from metastases. Clonal origin of multiple lung cancers: K-ras and p53 mutations determined by nonradioisotopic single-strand conformation polymorphism analysis. Discrimination of double primary lung cancer from intrapulmonary metastasis by p53 gene mutation. Study of the diagnostic difference between the clinical diagnostic criteria and results of immunohistochemical staining of multiple primary lung cancers. Carcinogen exposure, p53 alteration, and K-ras mutation in synchronous multiple primary lung carcinoma. Prognostication of small-sized primary pulmonary adenocarcinomas by histopathological and karyometric analysis. Immunohistochemical expression of estrogen receptor in adenocarcinomas of the lung: the antibody factor. Grade of stromal invasion in small adenocarcinoma of the lung: histopathological minimal invasion and 1088 Chapter 27: Adenocarcinoma of the lung prognosis. Blood vessel and lymphatic vessel invasion in resected nonsmall cell lung carcinoma. Impact of angiolymphatic and pleural invasion on surgical outcomes for stage I non-small cell lung cancer. Molecular predictors of response to epidermal growth factor receptor antagonists in non-small-cell lung cancer. Acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small-cell lung cancers dependent on the epidermal growth factor receptor pathway. Clear cell change in lung adenocarcinoma: a cytologic change rather than a histologic variant. Rising incidence of bronchioloalveolar lung carcinoma and its unique clinicopathologic features. Clinical features of bronchioloalveolar carcinoma with new histologic and staging definitions. The bronchioloalveolar carcinoma and peripheral adenocarcinoma spectrum of diseases. Usefulness of Cdx2 in separating 1089 Chapter 27: Adenocarcinoma of the lung mucinous bronchioloalveolar adenocarcinoma of the lung from metastatic mucinous colorectal adenocarcinoma. A single institution-based retrospective study of surgically treated bronchioloalveolar adenocarcinoma of the lung: clinicopathologic analysis, molecular features, and possible pitfalls in routine practice. Mucin-producing adenocarcinoma of the lung, with special reference to goblet cell type adenocarcinoma: immunohistochemical observation and Ki-ras gene mutation. Mixed mucinous-type and non-mucinous-type adenocarcinoma of the lung: immunohistochemical examination and K- ras gene mutation. Bronchioloalveolar lung carcinomas: K-ras mutations are constant events in the mucinous subtype. Mucinous and nonmucinous bronchioloalveolar adenocarcinomas have distinct staining patterns with thyroid transcription factor and cytokeratin 20 antibodies. Bilateral bronchioloalveolar lung carcinoma: is there a place for palliative pneumonectomy Successful treatment of refractory bronchorrhea by inhaled indomethacin in two patients with bronchioloalveolar carcinoma. Inhaled indomethacin in bronchorrhea in bronchioloalveolar carcinoma: role of cyclooxygenase. Mucinous carcinoma (colloid carcinoma) of the lung diagnosed by fine needle aspiration cytology: a case report. Mucinous colloid adenocarcinoma of the lung with lymph node metastasis showing numerous punctate calcifications. Pulmonary intestinal-type adenocarcinoma does not show enteric differentiation by immunohistochemical study. The spectrum of pulmonary mucinous cystic neoplasia: a clinicopathologic and immunohistochemical study of ten cases and review of literature. Pulmonary mucinous cystadenocarcinoma: report of a case and review of the literature. Recurrence of pulmonary mucinous cystic tumor of 1090 Chapter 27: Adenocarcinoma of the lung borderline malignancy. Pulmonary blastoma with argyrophil cells and lacking sarcomatous features (pulmonary endodermal tumor resembling fetal lung). Pulmonary adenocarcinomas of the fetal lung type: a clinicopathologic study indicating differences in histology, epidemiology, and natural history of low-grade and high-grade forms. Aberrant nuclear localization and gene mutation of beta-catenin in low-grade adenocarcinoma of fetal lung type: upregulation of the Wnt signaling pathway may be a common denominator for the development of tumors that form morules. Pulmonary endodermal tumor resembling fetal lung: report of a case in a 14-year-old girl. Positron emission tomography in well differentiated fetal adenocarcinoma of the lung. Endobronchial adenocarcinoma with endometrioid features and prominent neuroendocrine differentiation. Aberrant intranuclear localization of biotin, biotin-binding enzymes, and beta-catenin in pregnancy-related endometrium and morule-associated neoplastic lesions. Biotin-rich, optically clear nuclei express estrogen receptor-beta: tumors with morules may develop under the influence of estrogen and aberrant betacatenin expression. Fine needle aspiration cytology of pulmonary, well-differentiated fetal adenocarcinoma prepared by the ThinPrep method. Well-differentiated fetal adenocarcinoma of the lung: cytomorphologic features on fineneedle aspiration with emphasis on use of beta-catenin as a useful diagnostic marker. Aberrant nuclear Cdx2 expression in morule-forming tumours in different organs, accompanied by cytoplasmic reactivity. An autopsy case of pulmonary adenocarcinoma of fetal type treated with radiation therapy. Primary pulmonary adenocarcinoma with enteric differentiation resembling metastatic colorectal carcinoma: a report of the second case negative for cytokeratin 7. Pulmonary adenocarcinomas with enteric differentiation: histologic and immunohistochemical characteristics compared with metastatic colorectal cancers and usual pulmonary adenocarcinomas. Primary pulmonary adenocarcinoma with intestinal differentiation mimicking metastatic colorectal carcinoma: case report and review of literature. Table 1 World Health Organization classification of pulmonary squamous cell carcinomas Squamous cell carcinoma Variants Papillary Clear cell Small cell Basaloid Squamous cell carcinoma arises from bronchial epithelium. Basal cells and occasionally columnar goblet cells develop into carcinoma through the metaplasia-dysplasiacarcinoma sequence (see Chapter 23). Recurrent gains on the 3q arm and deletions on the 3p arm are noted in most cases while amplifications cluster in the 3q26:q29 region. Squamous cell carcinoma is a malignant epithelial tumor with keratinization and/or intercellular bridges. Furthermore, deletions of 3p12:14, 4p15:p16, 8p22:p23, 10q and 21q and overrepresentations of 1q21:q25 and 8q11:q25 may be associated with a metastatic phenotype. Cough, wheeze, stridor, dyspnea, pneumonia and hemoptysis lead the list of findings. For example, pulmonary artery invasion or pseudoaneurysm formation can cause hemoptysis,56 compression of the esophagus can lead to dysphagia, invasion of the phrenic nerve causes hemidiaphragmatic paralysis and dyspnea, left recurrent laryngeal nerve involvement causes hoarseness, and apical chest wall involvement may present with Pancoast syndrome (lower brachial plexopathy, Horner syndrome and shoulder pain) (see Chapter 24). A carcinoma involving either the right or left main bronchus but farther than 2 cm from the carina is designated pT2 while a tumor in a main bronchus less than 2 cm from the carina but not involving the carina is designated pT3. A superficial spreading carcinoma of any size with carcinoma limited to the bronchial wall, even if it involves the main bronchus, is classified as T1a. Lobar or complete atelectasis due to airway obstruction may also feature a bulging tumor contour. Direct invasion into regional lymph nodes gives the impression of an extrapulmonary mass (Table 3). Cavitation is more common when there is communication between the central portion of the mass and the bronchial lumen.
Cheap 25mg acarbose fast delivery
Other infections/infestations Rarely bacteria such as Bartonella can cause necrotizing granulomatous inflammation diabetes mellitus etiology buy genuine acarbose on line. Cases of extranodal involvement by cat scratch disease tend to occur in immunocompromised patients; however, several cases of pulmonary involvement have been reported in immunocompetent individuals. Cases of congenital pulmonary syphilis usually show numerous spirochetes and the differential diagnosis may not be a problem. Multiple lesions may fuse to form a large solitary lesion with many plasma cells and only a few multinucleated cells. In the absence of bacilli, a number of differential diagnoses should also be considered. Wegener granulomatosis the hallmarks of Wegener granulomatosis are necrotizing pneumonitis, vasculitis and giant cells (see Chapter 19). Elastic-van Gieson and Martius Scarlet Blue stains are often informative in these cases. Serological studies may also aid in the differential diagnosis, especially when renal disease is absent. Ziehl-Neelsen and fungal stains, such as methenamine silver, are advisable in every case of suspected sarcoid. Histologically, sarcoid granulomas are usually non-necrotizing but might feature necrosis and tend to track along the lymphatics in the pleura, interlobular septa and bronchovascular bundles. They can include multinucleated giant cells and these may contain nonspecific inclusion bodies, such as asteroid or Schaumann bodies (see Chapters 2 and 13). In typical sarcoid granulomas, vasculitis may be present involving the adventitia and media but vascular necrosis is not a common feature. Necrotizing sarcoid granulomatosis, as the name suggests, may contain large areas of necrosis along with nonnecrotizing granulomas. The granulomatous process involves bronchioles, as well as blood vessels, and the vasculitic component may sometimes be prominent. Churg-Strauss syndrome Churg-Strauss syndrome is a rare systemic condition seen in asthmatics and may affect the lung (see Chapter 19). Microscopic features can be variable but include necrotizing, granulomatous inflammation with palisading histiocytes and vasculitis. Differential diagnosis can sometimes be difficult due to overlapping features, which also include the eosinophilic infiltrate. Bronchocentric granulomatosis this disease is usually associated with allergic bronchopulmonary fungal disease in asthmatics (see Chapter 15). Infectious 221 Chapter 6: Pulmonary mycobacterial infections processes of other etiologies, including tuberculosis, may present with bronchocentric granulomas. Rheumatoid nodule Pulmonary rheumatoid nodules are identical to those in the subcutaneous tissue and are composed of palisading histiocytes arranged around central areas of necrosis with or without vasculitis (see Chapters 14 and 21). Foreign-body-type cells from aspiration Organic or non-organic aspirated material triggers an inflammatory reaction, which may vary substantially in intensity but is usually associated with a foreign-body-type multinucleated giant cell reaction. Identification of the foreign-body material is also helpful in the differential diagnosis (see Chapter 17). Granulomatous inflammation in lymph nodes draining cancer Granulomas can sometimes occur in lymph nodes draining a primary tumor, usually a carcinoma. The epithelioid granulomatous reaction may be found even in the absence of neoplastic cells. The actual cause for this granulomatous reaction pattern is unknown but possible factors include direct reaction to tumor cells, therapy-related. Only rarely is lung biopsy required and often this is in those where the diagnosis is not expected. Pleural tuberculosis is usually paucibacilliary and so pleural fluid smears are usually negative. In the non-severely ill the results of pleural fluid culture can be awaited; however, a pleural biopsy, especially in the absence of typical symptoms, may be required to commence therapy. In mediastinal lymph node disease, the inaccessibility of these nodes often means treatment is commenced without pathological confirmation. This is especially the case in those from high-prevalence countries with typical symptoms. Histopathological confirmation may be required more often as the differential diagnoses of sarcoid, lymphoma or metastatic cancer are difficult to exclude. Increasingly, diagnostic evidence is provided by fine-needle aspirate material obtained from relatively non-invasive transbronchial or transesophageal sampling with or without ultrasound guidance. It is in the environmental mycobacterial infections where clinicopathological correlation must be applied most carefully, both to distinguish infection from contamination and to separate these infections from those with M. Correlation of the clinical, radiographic and microbiological findings is critical to correct patient management in such infections. The existence of mycobacteria in different physiological states and the risk of resistance necessitates combination antibiotic therapy. This is based on randomized controlled trials and captured in various international and national guidelines. Drugs used combine bactericidal activity with sterilizing ability and the ability to prevent resistance development. The initial combination usually includes rifampicin, isoniazid, pyrazinamide and either ethambutol or streptomycin. Daily treatment is the norm, but twice and three times weekly regimes are available. In high-income countries this may be reserved for patients at risk of non-compliance. In high-income countries a chest radiograph will always be part of the initial clinical assessment and with typical upper zone cavitary change and typical symptoms, a positive sputum smear will be enough to initiate anti-tuberculous therapy. This may later be modified when sputum cultures and bacterial antibiotic sensitivity become available. In high-risk cases this may be supplemented by early use of gene probes for rifampicin resistance. In sputum smear-negative cases treatment will still be started if radiology and symptoms are typical. It is only in less typical cases that further pathological information is required. This may be possible in high-income countries, but not in the poorer areas of the world. Key aspects of treatment include using drugs from five different classes of anti-tuberculous agents plus at least four drugs to which the organism is likely to be sensitive. Antituberculosis drugs are associated with significant nonpulmonary side effects such as rashes and hepatitis and also include interactions with drugs that the patient may be taking for other purposes. Such effects may occur in one-third of patients and be sufficient to stop or modify therapy in 5:10% of patients. Accurate diagnosis is particularly important for environmental mycobacterial infection. Active disease must first be distinguished from colonization and sample contamination. Ideally before treatment is commenced the patient should be confirmed to have clinical and radiographic features compatible with environmental mycobacterial infection plus the identification of the mycobacterium from multiple respiratory samples. There is a poor correlation between in vitro bacterial sensitivities and clinical response for environmental mycobacteria. Full symptomatic recovery occurs within weeks and always before antituberculous therapy is concluded. Misdiagnosis, delayed diagnosis and patient comorbidities are likely contributing factors. Persisting cavities may lead to later aspergillus colonization or environmental mycobacterial infection. Post-tuberculous bronchiectasis may be a source of chronic bronchopulmonary sepsis. Takeda M, Ito W, Kobayashi N, et al Co-existence of Mycobacterium tuberculosis and Mycobacterium intracellulare in one sputum sample.
Generic acarbose 50 mg line
Horseshoe lung in association with other foregut anomalies: what is the significance Pulmonary sequestration and related congenital bronchopulmonary-vascular malformations: nomenclature and classification based on anatomical and embryological considerations diabetes eating plan purchase 25mg acarbose with visa. Congenital bronchopulmonary vascular malformations: clinical application of a simple anatomical approach in 25 cases. Bronchial atresia is common to extralobar sequestration, intralobar sequestration, congenital cystic adenomatoid malformation and lobar emphysema. Fetal congenital cystic ademomatoid malformations of the lung: a clinical pathologic study of eleven cases. Pulmonary and mediastinal bronchogenic cysts: a clinicopathologic study of 33 cases. Coexistence of bronchial atresia and bronchogenic cyst: diagnostic criteria and embryologic considerations. Subdiaphragmatic bronchogenic cyst with communication to the stomach: a case report. Cutaneous bronchogenic cyst of the back: a case report and review of the literature. Perinatal management of congenital cystic lung lesions in the age of minimally invasive surgery. Congenital cystic adenomatoid malformation: accuracy of prenatal diagnosis, prevalence and outcome in a general population Prenat Diagn 2003;23:997:1002. Cystic adenomatoid malformation of the lung: review of genetics, prenatal diagnosis, and in utero treatment. Outcome of the prenatally diagnosed congenital cystic adenomatoid lung malformation: a Canadian experience. Rhabdomyosarcoma of the lung arising in a congenital adenomatoid malformation Cancer 1977;40:383:8. Bronchioloalveolar carcinoma of the lung and congenital cystic adenomatoid malformation. Bronchioloalveolar carcinoma arising from a congenital cystic adenomatoid malformation in an adolescent: the first case report from the orient. Bronchioloalveolar carcinoma in congenital cystic adenomatoid malformation of lung. Pulmonary congenital cystic adenomatoid malformation as mucinous bronchioloalveolar carcinoma precursors. Congenital pulmonary airway malformation (congenital cystic adenomatoid malformation) with multiple extrapulmonary anomalies: autopsy report of a fetus at 19 weeks of gestation. Prognostic factors associated with congenital cystic adenomatoid malformation of the lung. Successful prenatal management of hydrops, caused by congenital cystic adenomatoid malformation, using serial aspirations. Antenatally suspected congenital cystic adenomatoid malformation of the lung: postnatal investigation and timing of surgery. Congenital cystic adenomatoid malformations may not require surgical intervention. Lower accessory pulmonary artery with intralobular sequestration of lung: a report of seven cases. Congenital bronchopulmonary foregut malformation: pulmonary sequestration communicating with the gastrointestinal tract. Extralobar sequestration with frequently associated congenital cystic adenomatoid malformation, type 2: report of 50 cases. Lobar emphysema, cystic adenomatoid malformation, pulmonary sequestration, and bronchogenic cyst in infancy and childhood: a clinical group. Cystic lung lesions with systemic arterial blod supply: a hybrid of congential cystic adenomatoid malformation and bronchopulmonary sequestration. Congenital lung lesions: classification and concordance of radiological appearance and surgical pathology. Therapeutic embolization of a systemic arterialization of lung without sequestration. Prenatal thoracoabdominal tumor mimicking pulmonary sequestration: a diagnosis dilemma. Systemic arterial supply to the normal basal segments of the left lower lobe treated by coil embolization, with long term follow up. Communicating bronchopulmonary foregut malformations: classification and embryogenesis. Arrest of foregut development in a congenital bronchopulmonary foregut malformation Pediatr Surg Int 1994;9:401:2. Congenital lobar emphysema: the disappearing chest mass: antenatal ultrasound appearance. Congenital lobar emphysema: a case with bronchial atresia and abnormal bronchial cartilage Br J Dis Chest 1982;76:177:84. Congenital lobar emphysema resulting from bronchial sling around a normal right main pulmonary artery. Asynchronous pulmonary hyperplasia associated with tracheal atresia: pathologic and prenatal sonographic findings. Laryngeal atresia or stenosis presenting as second trimester fetal ascites: diagnosis and pathology in three independent cases. Fraser syndrome and cryptopthalmos: review of the diagnostic criteria and evidence for phenotypic mdules in complex malformation syndromes. A case of congenital high airway obstruction syndrome managed by ex utero intrapartum treatment: case report and review of the literature. Congenital pulmonary lymphangiectasis: report of 11 examples with special reference to cardiovascular findings. Autosomal recessive intestinal lymphangiectasis and lymphedema, with facial anomallies and mental retardation. Congenital pulmonary lymphangiectasia presenting as non-immune fetal hydrops and severe respiratory distress at birth: not uniformly fatal. Thoracoscopic stapled resection of multiple esophageal duplication cysts with different pathological findings. Incidence of alveolar capillary dysplasia in severe idiopathic persistent pulmonary hypertension of the newborn. Congenital alveolar dysplasia: an unusual cause of respiratory distress in the newborn. Congenital alveolar capillary dysplasia: a developmental vascular anomaly causing persistent pulmonary hypertension of the newborn. Misalignment of lung vessels: a syndrome causing persistent neonatal pulmonary hypertension. Alveolar capillary dysplasia presenting a pneumothorax: a case report and review of the literature. A rare case of aortic coarctation and ventricular septal defect combined with alveolar capillary dysplasia. Congenital alveolar capillary dysplasia and associated gastrointestinal anomalies. A neonate with coexisting congenital cystic adenomatoid malformation of the lung and alveolar capillary dysplasia: a case report with review of literature. Intralobar sequestration with congenital cystic adenomatous malformation and rhabdomyomatous dysplasia. Rhabdomyomatous dysplasia of the lung: a case report with review of the literature. Rhabdomyomatous dysplasia of the newborn lung associated with multiple congenital malformations of the heart and great vessels. Heterotopic pancreatic tissue presenting as a solid and cystic lung lesion: a very unusual bronchopulmonary foregut malformation. Central nervous system heterotopia in the lung of a fetus with cranial malformation. Embolism of brain tissue in intrapartum and early neonatal deaths: report of 9 cases. The radial alveolar count method of Emery and Mithal: a reappraisal 1: postnatal lung growth. Hypoplasia of medullary arcuate nucleus in unexpected late fetal death (stillborn infants): a pathologic study. Association between pulmonary hypoplasia and hypoplasia of arcuate nucleus in stillbirth. Low amniotic pressure in oligohydramnios: is this the cause of pulmonary hypoplasia A mechanism leading to reduced lung 134 Chapter 3: Congenital abnormalities and pediatric lung diseases, including neoplasms expansion and lung hypoplasia in fetal sheep during oligohydramnios.
Order genuine acarbose line
Apart from interstitial distortion caused by diabetes type 2 diet to lose weight buy cheap acarbose on-line, for example, fibrosis, the only light microscopic findings indicative of alveolar-capillary membrane pathology are indirect and nonspecific. Capillary congestion provides a diagnostic clue to the diagnoses of congestive vasculopathy and pulmonary venoocclusive disease (see below). Vascular architecture at low magnification, in a case of congestive vasculopathy, due to mitral valve insufficiency. The axial muscular artery runs together with the bronchiole in the bronchovascular bundle. The interlobular septum is easily identified in subpleural lung tissue by its connection to the pleura (EvG stain). Pulmonary veins Pulmonary veins have an ill-defined media of smooth muscle cells with interspersed collagen and some elastin fibrils. Interlobular septa are most distinctive in subpleural lung tissue, where they are connected to the pleura. Pulmonary venules are located in the alveolar parenchyma, and are devoid of a muscular media. They have a single elastic lamina, so they are indistinguishable from normal pulmonary arterioles. The only reliable way to identify these venules in tissue sections is to trace their connection to a recognizable vein. Bronchial arteries are usually much smaller in diameter than the pulmonary arteries and are therefore normally inconspicuous. Bronchial arterial enlargement may result from blood shunting between bronchial and pulmonary vascular anastomoses. Underlying causes include bronchiectasis, intralobular sequestration, tetralogy of Fallot and (segmental) atresia of a pulmonary artery. This establishes a bypass, feeding the capillary network (postobstructive vasculopathy). These channels are normally collapsed and inconspicuous but are more prominent if there is pulmonary edema or they contain tumor. They can be highlighted with monoclonal antibody D2:40, which recognizes podoplanin, an O-linked sialoglycoprotein expressed by lymphatic endothelium. Bronchial circulation Bronchial arteries are small systemic muscular arteries arising from the aorta. Bronchial arteries provide oxygen to hilar structures, large airways and the largest pulmonary arteries, the latter via "vasa vasorum". The bronchial arteries travel together with the pulmonary arteries and airways in the bronchovascular bundles but can also be found in the pleura. Occasionally, longitudinal smooth muscle Vascular remodeling during development and aging At birth, the first breaths expand the thoracic volume and expose the lung to high oxygen levels. The resultant abrupt and marked drop in pulmonary arterial resistance causes a significant rise in pulmonary blood flow, while shunting via the foramen ovale and the ductus arteriosus is abolished. The elastic artery features discontinuously layered elastic lamellae and a prominent adventitia (EvG stain). Before birth these arteries are constricted, so the media is thick in comparison to the vascular diameter. After birth, muscular pulmonary arteries rapidly relax, and a more gradual medial thinning follows during the first 3 weeks of life. The adult medial thickness of up to 5:7% of the external vascular diameter is reached at the end of the first year. The number of axial and especially supernumerary arteries increases substantially during the first 2 years of life. These vessels expand the total pulmonary vascular bed and thus contribute to a further decrease in the pulmonary vascular resistance. Experimental evidence also indicates the adventitia is actively involved in vascular remodeling in hypoxia. In pulmonary hypertension, pulmonary arteries show a rapid decrease in caliber from the center to the lung periphery. Evaluation of these features is not very reproducible and correlates poorly with the severity of pulmonary hypertension. There is an abrupt decrease in caliber downstream of the occlusion (so-called Westermark sign). Note the larger caliber of the pulmonary arteries in the areas of increased perfusion, compared to areas with low perfusion. An estimate of a highly elevated pulmonary artery pressure can safely be assumed to be genuinely above the normal range. However, a mildly/moderately elevated pulmonary artery pressure, as estimated by ultrasound, warrants verification by right-heart catheterization. Many of these pathways are closely interconnected, and the relative contribution of specific pathways in pulmonary hypertension of different etiologies is still largely obscure. Our understanding as to how these mechanisms translate to the histopathological features of vasculopathy in pulmonary hypertension in humans is far from complete. We have limited our discussion to the main players in the pathogenesis of pulmonary hypertension, and refer to the various histopathological alterations seen in pulmonary hypertension where possible. Once established, however, arterial hypertension itself comes to act as a stress factor on the vasculature, causing shear stress. In addition the hypoxia that results from a low diffusion capacity and/or low mixed venous oxygen pressure possibly contributes to vascular changes. Thus, in addition to pathogenetic pathways related to its cause, pulmonary hypertension shares pathogenic features; a notion supported by the partly overlapping, partly distinctive patterns of vasculopathy in human pulmonary hypertension. The pathogenesis of pulmonary hypertension has been studied in a variety of animal models such as rats, calves, pigs and mice (including transgenic mice), and by means of different stress factors. These include pulmonary hypoxia (alone, or in combination with other manipulations. Diagram depicting potential mechanisms involved in the development of pulmonary arterial hypertension. Some evidence has emerged that antidepressants may increase the risk of pulmonary hypertension in genetically predisposed individuals. Circulating B cells in pulmonary hypertension patients are activated,67 and are found in vascular lesions. Several appetite suppressants have been identified as risk factors for pulmonary hypertension. It increases pulmonary vascular resistance, and may be involved in hypoxia-induced remodeling. Shear stress occurs in the areas of most intense turbulence, downstream of bifurcations and probably also near the origins of supernumerary arteries. Besides endothelial activation caused by pulmonary hypertension, the endothelium may be directly targeted by other insults, such as a thromboemboli, foreign-body material, schistosoma eggs and auto-antibodies. The effects of endothelial dysfunction are wide-ranging and include vasoconstriction, vascular leakage, inflammation, thrombosis and, ultimately, vascular remodeling. Damage or activation of endothelial cells is implicated in local activation of the clotting cascade and intimal fibrosis. In pulmonary hypertension associated with connective tissue diseases, various auto-antibodies, including antiendothelial antibodies, can be detected. It is currently unknown whether this is a cause or a consequence of pulmonary hypertension and/or vascular remodeling. Taken together, the endothelial proinflammatory, prothrombotic and profibrotic state may be caused by various direct insults, as well as by shear stress resulting from the pulmonary hypertension. Hypoxia Hypoxia and pulmonary vascular tone Pulmonary vascular recruitment and vascular tone are the main regulators of pulmonary arterial pressure. Local oxygen tension is considered the key factor in the regulation of pulmonary vascular tone (reviewed in Marshall et al. In contrast to its effect in the systemic circulation, low oxygen tension elicits a vasoconstrictive response of pulmonary blood vessels, especially pulmonary arteries. This is probably beneficial in the case of uneven ventilation of the lungs, as it redistributes blood flow away from underventilated areas. However, generalized pulmonary hypoxia results in increased pulmonary vascular tone and pulmonary hypertension. Hypoxic pulmonary hypertension has been extensively studied in laboratory animals. It is unknown whether there is pathogenic overlap between hypoxic pulmonary hypertension and these other forms of pulmonary hypertensive disease.
Speckled Jewels (Jewelweed). Acarbose.
- How does Jewelweed work?
- Are there safety concerns?
- Mild digestive disorders, rash from poison ivy, and other conditions.
- What is Jewelweed?
- Are there any interactions with medications?
- Dosing considerations for Jewelweed.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96535
Buy 25mg acarbose free shipping
In such cases the proliferation is modest and often apparent only after immunolabelling blood glucose goes down after eating 25mg acarbose. In this situation it is usually attributable to the consolidation or other pulmonary damage associated with growth of the tumor, especially with airway obstruction. Tumour suppressor gene products, proliferation and differentiation markers in lung neuroendocrine neoplasms. Distinction of pulmonary large cell neuroendocrine carcinoma from small References 1. Adrenocortical hyperfunction in association with anaplastic carcinoma of the respiratory tract. Oat cell carcinoma of the lung: its origin and relationship to bronchial carcinoid. Lung tumors with neuroendocrine morphology: essential radiologic and pathologic features. Neuroendocrine components of the bronchopulmonary tract: hyperplasias, dysplasias and neoplasms. A classification of the spectrum of carcinoid to small cell carcinoma and intervening variants. Neuroendocrine neoplasms of 1178 Chapter 31: Neuroendocrine tumors and other neuroendocrine proliferations of the lung cell lung carcinoma: a morphological, immunohistochemical and molecular analysis. Unbalanced chromosomal aberrations in neuroendocrine lung tumors as detected by comparative genomic hybridization. Differential expression of telomerase activity in neuroendocrine lung tumours: correlation with gene product immunophenotyping. Diffuse idiopathic neuroendocrine cell proliferation presenting as interstitial lung disease. Pathology reporting of neuroendocrine tumors: application of the Delphic Consensus Process to the Minimum Pathology Data Set. Small cell carcinoma of the lung and large cell neuroendocrine carcinoma interobserver variability. Low grade neuroendocrine tumors of the lung (bronchial carcinoids): 25 years experience. Carcinoid tumor of the lung and type-1 multiple endocrine neoplasia associated with persistent hypercalcaemia: a case report. Ectopic growth hormone-releasing hormone secretion by a bronchial carcinoid tumor: clinical experience following tumor resection and longacting octreotide therapy. Re-evaluation of pulmonary neoplasms resected as small cell 1179 Chapter 31: Neuroendocrine tumors and other neuroendocrine proliferations of the lung carcinomas. Significance of distinguishing between welldifferentiated and small cell neuroendocrine carcinomas. Large cell neuroendocrine carcinoma of the lung: a clinicopathologic study of eight-seven cases. Clinical-pathologic analysis of 40 patients with large cell neuroendocrine carcinoma of the lung. Large cell neuroendocrine carcinoma of the lung: a histologic and immunohistochemical study of 22 cases. Large cell neuroendocrine carcinoma of the lung: a 10-year clinicopathologic retrospective study. Large cell neuroendocrine carcinoma and large cell carcinomas with neuroendocrine morphology of the lung: prognosis after complete resection and systematic nodal dissection. Myasthenic (Eaton-Lambert) syndrome associated with pulmonary large cell neuroendocrine carcinoma. Cigarette smoking and bronchial carcinoma: dose and time relationships among regular smokers and lifelong non-smokers. Frequency of different histologic types of bronchogenic carcinoma as related to radiation exposure. Hyponatraemia and bronchogenic carcinoma associated with renal excretion of large amounts of antidiuretic material. Cancer and the Nervous System: the Neurological Manifestations of Systemic Malignant Disease. Carcinoids, atypical carcinoids and small-cell carcinomas of the lung: differential diagnosis of fine-needle aspiration biopsy specimens. Pulmonary carcinoid tumours and well-differentiated neuroendocrine carcinomas: is there room for an atypical carcinoid Comparison of the usefulness of histochemistry and ultrastructural cytochemistry in the identification of neuroendocrine neoplasms. The argyrophil reaction in islet cells of adult human pancreas studied with a new silver nitrate procedure. Neuroendocrine pancreatic tumors: clinical presentation, biochemical and histopathological findings in 84 patients. Synaptophysin: a novel marker for neurons, certain neuroendocrine cells and their neoplasms. Identification and localization of synaptophysin, an integral membrane glycoprotein of Mr 38,000 characteristic of presynaptic vesicles. Neuron specific enolase is a molecular marker for peripheral and central neuroendocrine cells. Antibodies to neuron-specific enolase for the delineation of the entire diffuse neuroendocrine system in health and disease. Immunohistochemical localization of gamma-enolase in normal human tissues other than nervous and neuroendocrine tissues. Immunohistochemical markers of small cell carcinoma and related neuroendocrine tumours of the lung. An achaete-scute homologue essential for neuroendocrine differentiation in the lung. Prognostic significance of neuroendocrine differentiation in adenocarcinoma of the lung. Diagnostic uses of antibodies to keratins: a review and immunohistochemical comparison of seven monoclonal and three polyclonal antibodies. The use of antikeratin antibodies in the immunohistochemical distinction between neuroendocrine (Merkel cell) carcinoma of the skin, lymphoma and oat cell carcinoma. Thyroid transcription factor-1 is the superior immunohistochemical marker for pulmonary adenocarcinomas and large cell carcinomas compared to surfactant proteins A and B. Immunohistochemical and ultrastructural analysis of bronchopulmonary neuroendocrine neoplasms. Detailed deletion mapping of the short arm of chromosome 3 in small cell and non-small cell carcinoma of the lung. Tumor suppressor genes on chromosome 3p involved in the pathogenesis of lung and other cancers. Array-based comparative genomic hybridization analysis of high-grade neuroendocrine tumors of the lung. Immunohistochemical expression of estrogen and progesterone recptors in primary pulmonary neuroendocrine tumors. Immunohistochemical differential diagnosis between large cell neuroendocrine carcinoma and small cell carcinoma by tissue mircroarray analysis with a large antibody panel. Nuclear pleomorphism in typical carcinoid tumours of the lung: problems in frozen section interpretation. Ki-67 immunoreactivity in the differential diagnosis of pulmonary neuroendocrine neoplasms in specimens with extensive crush artifact. Bronchopulmonary carcinoids: an analysis of 1875 reported cases with special reference to a comparison between typical carcinoids and atypical varieties. Diagnostic and therapeutic management of neuroendocrine lung tumors: a clinical study of 44 cases. Typical and atypical pulmonary carcinoids: outcome in patients presenting with regional lymph node involvement. Pulmonary neuroendocrine carcinomas: a review of 234 cases and a statistical analysis of 50 cases treated at one institution using a simple clinicopathologic classification. Surgical treatment for limited small-cell lung cancer: the University of Toronto Lung Oncology Group experience. The use of neuroendocrine immunoperoxidase markers to predict chemotherapy response in patients with non-small cell lung cancer. Neuroendocrine differentiation is an independent prognostic factor in chemotherapy treated non-small cell lung carcinoma.
Purchase discount acarbose on line
These include the interaction between asbestos and cigarette smoking in increasing lung cancer risk blood sugar normal level buy cheap acarbose 25 mg on line, differences in fiber types with respect to potency in the production of lung cancer, and the role of asbestos dose versus asbestosis as the underlying etiological factor. Finally, one must consider the role of fiber analysis of lung tissue in determining the cause of lung cancer in an individual case. Cigarette smoking inhibits clearance mechanisms in the lower respiratory tract and thus can increase the effective dose of asbestos. Furthermore, carcinogens from cigarette smoke, adherent to the surface of asbestos fibers, may be more readily delivered to the respiratory epithelium. Berman and Crump reached a similar conclusion in their extensive literature review. The result must be correlated with the range of values observed in bona fide cases of asbestosis. In everyday practice, fiber burden analysis cannot substitute for or overrule the histological diagnosis of asbestosis. The immunosuppressive therapy which constitutes the mainstay of medical intervention for other forms of pulmonary interstitial fibrosis is ineffective. Historically, deaths result from intractable respiratory failure, with the expected association of decreased life expectancy in proportion to disease severity. Other causes of death include cor pulmonale, carcinoma of the lung and mesothelioma. Studies from the United Kingdom and Finland document considerable and excessive mortality from carcinoma of the lung in workers with asbestosis. Risk differential for lung cancer for chrysotile alone versus amphibole fibers appears to be between 1:10 and 1:50 Modified from reference 111. One of the most controversial areas with respect to asbestos and lung cancer is whether asbestosis is an obligatory precursor of asbestos-related lung cancer (fibrosis/cancer hypothesis), or whether asbestosis and lung cancer are two independent endpoints, each related to the dose of asbestos (fiber burden hypothesis). Proponents of the fibrosis/cancer hypothesis note the oncogenic potential for severe interstitial lung fibrosis, and the tendency for carcinomas to develop in animal models only in cases of asbestosis. Proponents of the fiber burden hypothesis consider asbestos both an initiator and promoter of carcinogenesis, and regard fibrogenesis and carcinogenesis as distinct effects of asbestos exposure. The pro and con arguments in this regard have been presented in detail elsewhere, and have included the fundamental disagreements between experts on the criteria for the diagnosis of asbestosis, laboratory-specific variance in fiber burden analyses and criticisms of the imprecision of epidemiological studies. Asbestosis is primarily a disease of the lung periphery with greatest severity typically in the lower lobes, whereas asbestos-related bronchogenic carcinoma is a more central process and commoner in the upper lobes. Some have argued that epidemiological studies favor asbestosis as the precursor to asbestos-induced lung cancer. This is because 85 to 95% of lung cancers are related to cigarette smoking, whereas asbestos is a causative factor in fewer than 5% of lung cancer cases. Although some studies have reported that asbestosrelated lung cancers are commoner in the lower lobes, others have found that they are more frequent in the upper lobes (similar to cigarette-smoking related lung cancers in the absence of asbestos exposure). Analysis of lung tissue fiber content plays an increasing role in determining the causation of lung cancer in an individual case. This observation was supported by the consensus of experts that met in Helsinki, Finland, in 199788 but is disputed by others. Our studies show one asbestos body per cm2 of an iron-stained lung tissue section is equivalent to approximately 400 asbestos bodies per gram of wet lung tissue. In this regard, there is considerable variation in results analyzing the same sample by different laboratories, since different laboratories follow different protocols. This difference is almost entirely due to the detection of chrysotile (Karjalainen, personal communication, academic dissertation, University of Helsinki 1994). Specifically, when comparing groups of patients with asbestosis, parietal plaques but not asbestosis, and groups with neither, the asbestos body count in the asbestosis cohort was more than 35 times greater than the cohort with plaque only, and more than 300 times greater than the group with neither plaques nor asbestosis. The total asbestos fiber count for the asbestosis cohort was nearly 20 times greater than the cohort with pleural plaque, and more than 50 times that of the cohort with neither. These are of course not mutually exclusive, as cigarette smoking is a cofactor in most asbestos-related lung cancers. The finding of asbestos bodies in the absence of asbestosis is not sufficient to determine causation. It may be an indication for fiber analysis to determine whether the fiber burden is within the range of values observed for patients with asbestosis (see above). Despite decades of research and the development of considerable knowledge in the mechanisms of asbestos-related disease and the means for its diagnosis, the topic remains fraught with controversy, even amongst those considered as experts within the field. This is reflected in a so-called Delphi study of an empaneled group of authorities tendered as experts on the basis of asbestos-related disease publications. In this study, consensus on statements regarding asbestos-related disease was not attained in 9/32 examples. This included statements concerning the diagnosis of pleural and parenchymal lung disease, and the role of asbestos exposure in the causation of lung cancer. Quantification requires removal of the organic matrix in which the fibers are embedded, typically accomplished by wet chemical digestion techniques or low-temperature plasma ashing. The residue can be collected on a membrane filter, which is analyzed by various techniques. The brightfield light microscope can be used for counting asbestos bodies, with fairly good interlaboratory agreement. Asbestos bodies account for a fraction of the fiber content and there is a variable relationship between the numbers of asbestos bodies and uncoated fibers from case to case (although asbestos bodies are a fairly good marker for long amphibole fibers). Preparation techniques have the potential for loss or addition of fibers to the sample. Furthermore, there is no standardized methodology for the analysis of human tissue samples. Consequently, examination of the same specimen by different laboratories using similar techniques may result in values that differ widely. Transmission electron microscopy is generally considered to be the most sensitive method for detecting fibers in tissues, especially for the detection of the finest/smallest fibrils. Therefore, a portion of the filter must be selected, which is assumed to be representative of the entire filter. The filter material must be removed, which is generally accomplished by means of cold finger reflux technique. The number of fibers of a given type per grid is extrapolated to the entire filter, which is in turn extrapolated to a given weight of lung tissue. Transmission electron microscopy can visualize the central capillary (core) of chrysotile fibrils, a useful identifying feature. The filter is coated with a conducting material, such as gold or platinum, which reduces charging artifacts that may interfere with fiber detection. The number of fibers of a given type per field is again extrapolated to the entire filter, which is in turn extrapolated to a given weight of lung tissue. These data combined with fiber morphology permit accurate identification of most fibers. With the descriptions of silicosis in ancient Egyptian mummies, this may be the oldest-known pneumoconiosis. Crystalline polymorphs of silica include quartz, tridymite, cristobalite, coesite and stishovite. Silicates are higher oxidized forms of the element silicon (SiO4) combined with various cations, and the pneumoconioses associated with silicate exposure will be discussed below. In addition, common industrial minerals, such as granite, sandstone and shale, contain considerable amounts of quartz. Occupations involving exposure to silica typically include construction, tunneling, blasting, mining and quarry work, as well as trades using silica-containing abrasives. In some countries with lax health and safety regulations, it is possible to see men surrounded by dust sanding the stone of new buildings. Silica also occurs in a biogenic form (phytoliths) in some plants143 and has been identified in urban air samples and tobacco smoke. The biological activity of silica particles is complex and depends on a number of particle and host factors. Crystalline forms of silica are much more toxic than amorphous forms, which have not been implicated in human disease. Impurities such as iron or aluminum in the crystal exert a protective effect and reduce the toxic bioactivity of silica. The toxicity of quartz particles is enhanced when this layer is removed by acid washing or when freshly cleaved crystal surfaces are exposed, as occurs in sandblasting. Tridymite, which is the most fibrogenic form of crystalline silica, lacks a Beilby layer. Free radical generation from freshly fractured silica particles may also play a role in silica-induced cytotoxicity.
Order acarbose 50 mg mastercard
Myasthenia gravis: a clinical and pathological study of a case associated with a primary mediastinal thymoma and a solitary secondary intrapulmonary thymoma diabetes type 1 pancreas transplant order cheapest acarbose and acarbose. Immunohistochemical markers in the differentiation of thymic and pulmonary neoplasms. Primary intrapulmonary thymoma successfully resected with vascular reconstruction. Primary intrapulmonary spindle cell thymoma with marked granulomatous reaction: report of a case with review of literature. Primary pulmonary malignant teratoma with yolk sac element associated with hematologic neoplasia. Thoracic metastasectomy for germ cell tumours: long term survival and prognostic factors. An intrapulmonary teratoma associated with bronchiectasia containing various kinds of primordium: a case report and review of the literature. Resection of residual pulmonary masses after chemotherapy in patients with metastatic nonseminomatous germ cell tumours. Intrapulmonary cystic benign teratoma: a case report and review of the literature. Fibrobronchoscopic evidence of endobronchial hairs in intrapulmonary teratoma with hemoptysis but without trichoptysis. Malignant transformation of mature cystic teratoma to squamous cell carcinoma involves altered expression of p53- and p16/Rb-dependent cell cycle regulator proteins. Immunohistochemical and molecular studies on malignant transformation in mature cystic teratoma of the ovary. Primary pulmonary teratoma: report of a case and the proposition of "bronchotrichosis" as a new term. Isolated melanoma in the lung where there is no known primary site: metastatic disease or primary lung tumour Primary pulmonary melanoma diagnosis: the role of immunohistochemistry and immunocytochemistry. Primary malignant melanoma of the lung: a case report and review of the literature. Molecular cytogenetics of cutaneous melanocytic lesions: diagnostic, prognostic and therapeutic aspects. Primary malignant melanoma at unusual sites: an institutional experience with review of literature. It is increased in a number of conditions, both benign and malignant, sometimes as localized lesions and sometimes as a diffuse process. These form a superficial plexus in the pleura, draining along interlobular septa to hilar nodes, and a deep efferent plexus around bronchovascular bundles, draining to the hilum and tracheobronchial nodes. Both benign and malignant infiltrates may be associated with other recognizable pathology, such as systemic disease or interstitial lung disease. Difficulties in separating and classifying primary lymphoproliferative lesions, coupled with the problem of distinguishing between benign and neoplastic lymphoid infiltrates, has left a legacy of confusing terminology, which has now been largely clarified with the benefits of immunohistochemistry and molecular techniques. Those malignant lymphomas that are primarily node or bone marrow-based and involve the lungs secondarily are discussed separately, together with pulmonary involvement by leukemic processes. Others, such as intravascular lymphoma and lymphomatoid granulomatosis, are not necessarily confined to the lungs at presentation. However, the pulmonary manifestations are an important component of the primary disease process and they are discussed with primary malignant pulmonary lymphomas. Apart from those conditions typically regarded as lymphoid in origin, this chapter also covers the range of plasma cell disorders, both benign and malignant, and includes amyloidosis. Finally, the histiocytic disorders are discussed with emphasis on pulmonary Langerhans cell histiocytosis, a unique and poorly understood condition that sits on the borderland of neoplasia and diffuse parenchymal lung disease. They are most frequent in adult males, particularly in smokers or workers exposed to asbestos or anthracotic dust. Most are therefore peripheral and those deep within the lung are close to the pleura, within fissures. They share the reactive patterns seen in hilar and mediastinal nodes: in particular, they show sinus histiocytosis, anthracosis, fibrosis and calcification. In patients with leukemia or widespread lymphoma, they may be involved together with other intrathoracic nodes. As well as metastatic carcinoma and small primary carcinomas, the broad differential diagnosis includes other benign lesions such as hamartoma, an infectious granuloma, rheumatoid nodule or nodular amyloidosis. These are associated with specialized overlying epithelium, the lymphoepithelium or dome epithelium, where the M-cells, lacking cilia and possessing deep microvillous folds, are specialized for antigen transport. It is suggested that inflammation in the lung provides the stimulus for the interaction between integrins on circulating lymphoid cells and homing-receptors on lung endothelium, to cause accumulation of T-cells and initiate a complex cytokine system. They maintain the compartmentalized structure of lymphoid tissues, thereby ensuring contact between antigens, antigen-processing cells and lymphocytes. This is usually localized around areas of chronic infection, such as organizing pneumonia or chronic lung abscess. Interstitial lymphoid aggregates may also be seen at a distance from the main lesion. Lymphoid proliferation in interstitial lung disease Reactive hyperplasia of lymphoid tissue is seen to a variable extent in all types of interstitial lung disease. It lacks the typical overlying dome epithelium and includes reactive lymphoid follicles with follicular dendritic cells and germinal centers. Occasionally in any type of interstitial lung disease, the lymphoid hyperplasia may be more pronounced and show features of follicular bronchiolitis (see Chapters 10 and 21). An interstitial lymphoid infiltrate is often prominent in chronic hypersensitivity pneumonitis (extrinsic allergic alveolitis). Generally, the infiltrate is most apparent in bronchial walls and peribronchial tissues, becoming less dense in the more peripheral lung parenchyma. A dense lymphangitic interstitial lymphoid infiltrate may be mistaken for a neoplastic process. Follicular bronchiolitis Follicular bronchiolitis is a form of benign lymphoid hyperplasia in which hyperplastic lymphoid follicles are associated with small airways and distributed along bronchovascular bundles. Many patients have some associated or underlying pathology, and the age and sex incidence depends to a large extent on this. There may be a minor interstitial component immediately surrounding the involved airways but the lung parenchyma is characteristically spared and alveolar septa are not expanded. Nonspecific secondary changes, such as accumulation of foamy macrophages in the distal lung, are due to bronchiolar occlusion or narrowing. At one end of the spectrum, there is some overlap with follicular bronchiolitis, and when the lymphoid infiltrate is particularly dense the distinction from malignant lymphoma is the main consideration. Lymphoid interstitial pneumonia represents a nonspecific response of pulmonary lymphoid tissue to a variety of stimuli. A mixed interstitial infiltrate including plasma cells is associated with alveolar septal fibrosis. Respiratory symptoms include cough and increasing dyspnea, and these may be accompanied by systemic symptoms, such as weight loss, low-grade pyrexia and night sweats. Pulmonary function studies show a restrictive pattern, with reduction of carbon monoxide diffusing capacity, and bronchoalveolar lavage features a lymphocytosis. Serum dysproteinemias occur in up to 80% of patients, usually as a polyclonal hypergammaglobulinemia. Plain chest radiography typically shows bilateral, predominantly lower zone, reticular or reticulonodular infiltrates. The results are variable but most patients show some improvement, and some show complete resolution. Prognosis is similarly unpredictable with up to 50% of patients dying within 5 years, often of opportunist infection following immunosuppression. Microscopically, the dominant feature is a diffuse lymphoid infiltrate expanding the pulmonary interstitium.
Effective 25 mg acarbose
It does metabolic bone disease workup cheap 50mg acarbose with visa, however, enhance sensitivity to hypoxia and subsequent pulmonary hypertension. Adventitial cell proliferation, Histopathological patterns of hypertensive pulmonary vascular disease Introduction the role of biopsy pathology in the diagnosis and clinical management of pulmonary hypertension is limited to those cases where clinical presentation and hemodynamic parameters do not provide an unequivocal diagnosis. Only in those cases does the benefit of a histopathological diagnosis for further clinical management outweigh the risk of a surgical biopsy. Importantly, the histopathological identification of an underlying disease may shift therapeutic options from pulmonary hypertension therapy alone to combined treatment of pulmonary hypertension and an underlying disease, potentially improving prognosis. Although histopathological assessment of vascular lesions in explants and at autopsy may not benefit those individuals, such evaluations allow for correlation with the clinical diagnosis, hemodynamics, the effects of therapy, as well as the detection of undiagnosed or misdiagnosed disease. These investigations are also indispensable for furthering knowledge in this field. For example, little is known about development of histopathological patterns over time, or pharmacological effects on disease. The following sections describe the recognized histological patterns of pulmonary hypertensive vascular disease. These are plexogenic arteriopathy, thrombotic arteriopathy, hypoxic arteriopathy, congestive arteriopathy and pulmonary veno-occlusive disease/capillary hemangiomatosis (Table 3A). These five clinical categories correspond only partially to the histopathological classification. An overview of the clinical classification and corresponding histopathological patterns of vasculopathy is given in Table 3B. Since histopathology provides the most direct assessment of the type, distribution and severity of tissue lesions, our discussion of pulmonary vascular hypertensive disease is based on microscopy. Congenital heart disease with a post-tricuspid left-to-right shunt is a major risk factor. This condition requires early surgical correction to prevent irreversible remodeling of the pulmonary vasculature and persistent pulmonary hypertension, eventually progressing to Eisenmenger syndrome (see below). Schistosomiasis-associated plexogenic pulmonary arteriopathy is largely limited to areas where schistosomiasis is endemic, such as northwestern South America (Brazil, Venezuela and Surinam), parts of the Caribbean (lower Antilles, Puerto Rico and the Dominican Republic) and northeast Africa. Hypoxic arteriopathy Hypoxic arteriopathy 673 Chapter 18: Pulmonary vascular pathology Table 3B: (cont. Metabolic disorders: glycogen storage disease, thyroid disorders Gaucher disease 5. Others: tumoral obstruction fibrosing mediastinitis chronic renal failure on dialysis a Histopathological pattern Hypoxic arteriopathy Hypoxic arteriopathy (see also 1. Thrombotic arteriopathy vascular occlusion by leukemic cells Thrombotic hypoxic congestive Thrombotic Table 5 Pulmonary vascular lesions in plexogenic arteriopathy12,13 5. Arterial medial hyperplasia Cellular intimal proliferation Plexiform lesions Focal fibrinoid necrosis Dilatation lesions, including angiomatoid lesions Tortuosity of pulmonary arteries Concentric laminar intimal fibrosis Necrotizing arteritis (occasionally in severe, advanced disease). Apparently, this form of pulmonary hypertension requires at least one additional stress factor to initiate the cascade of events that leads to clinically manifest disease. In addition to true medial hyperplasia, subendothelial intimal cells may show myofibroblastic differentiation,135,138 which probably contributes to vessel wall functional alterations. Such intimal originally described by Chaves in the 1960s,131:133 hence its former classification in group 4 (thrombotic/embolic disease). There is, however, a type of intimal fibrosis, concentric laminar intimal fibrosis, which is at least highly suggestive of plexogenic arteriopathy. For unknown reasons, concentric laminar intimal fibrosis is especially prominent in systemic sclerosis-associated pulmonary hypertension (see Chapter 21). Concentric laminar intimal fibrosis should not be confused with the development of a new muscular media around a residual lumen in a case with marked nonspecific intimal fibrotic thickening. Such a newly formed muscular media consists of smooth muscle cells hugging the residual lumen, sometimes with newly formed elastin on either side, thus mimicking the media of a muscular pulmonary artery. Arrows indicate the inner (lower arrow) and outer (upper arrow) elastic laminae (EvG stain). There may be associated newly formed elastin mimicking the inner and/or outer elastic laminae of a muscular pulmonary artery. Fibrosis is not concentrically layered, so the new muscle layer stands out from this deeper intimal fibrosis. A computer-aided reconstruction shows plexiform lesions (white) occur in small side branches (supernumerary arteries) arising from larger parent arteries. Distribution of arterial lesions and collateral pathways in the pulmonary hypertension of congenital heart disease: a computer aided reconstruction study. Interestingly, these "dilatation lesions" may be solitary or may cluster together as angiomatoid lesions. The parent axial artery commonly exhibits focal intimal fibrosis near the origin of the supernumerary artery. Focal arteritis is rare, and manifests as a transmural roundcell inflammatory infiltrate, most commonly affecting an axial muscular pulmonary artery. In this prototype, the endothelial lining of the plexus consists of a proliferating apoptosis-resistant population. It has been suggested that the dilatation represents a decompensation of the vascular wall caused by increased intraluminal pressure. Despite claims to the contrary, the plexiform lesion can and should be distinguished from the commoner organizing thrombus or thromboembolus. A muscular pulmonary artery features transmural mixed lymphocytic and granulocytic infiltrates, fibrinoid changes of the vessel wall and a thrombus in the vessel lumen. Effects of therapy Much of our knowledge of pulmonary vascular histopathology was gathered in a time when, apart from cardiac surgery in cases of cardiac malformations or valvular disease, treatment options were virtually non-existent. At including plexogenic arteriopathy, the finding of an obvious post-thrombotic lesion does not indicate thrombotic arteriopathy. Neither does their presence, in addition to the "tell-tale" lesions of plexogenic pulmonary arteriopathy or any other type of hypertensive vascular disease, point to some vague and allencompassing "spectrum of hypertensive vascular disease". Such reasoning effaces essential distinctions in our understanding of pulmonary hypertension. Continuous intravenous administration of prostanoids is reserved for those whose response to oral treatment is insufficient. The effects of treatment on vascular remodeling and the resultant histological phenotype of end-stage disease have been studied. Treated cases showed more frequent and extensive perivascular and peribronchiolar inflammation and alveolar edema. Treated and non-treated control groups did not differ with respect to medial, intimal or adventitial thickness, or number of plexiform lesions. Injury to endothelium, alterations in normal blood flow and alterations in the blood (hypercoagulability) predispose to thrombosis. Some may be due to local thrombosis, or deficient clearing of small thromboemboli that may normally occur over time, rather than due to acute and massive thromboembolism. Pulmonary hypertension develops in up to 40% of patients,187:189 with a mortality rate of almost 50%. However, increased susceptibility to infection is certainly due to repeated episodes of splenic infarction, leading to autospenectomy. Acute chest syndrome or acute vasculopathy is a potentially fatal sickle crisis with a clinicoradiological definition. This precipitates HbS polymerization and vaso-occlusion, causing further hypoxia and inflammation. Vaso-occlusion and bone marrow infarction can cause fat embolism, further damaging the pulmonary circulation. Secretory phospholipase A2 concentrations, which increase in response to inflammation and are known to be very high in acute chest syndrome, further increase expression of adhesion molecules in the pulmonary vasculature, causing more vasoocclusion. It is probable that pulmonary infarction and endothelial injury contribute to the hypertension. Accurate descriptions of pulmonary vasculopathy in well-characterized patients are lacking. Thus, the pathogenesis of pulmonary hypertension in sickle cell disease is multifactorial, rather than purely thrombotic. The clinical features may not be discriminatory either, as the risk factors, signs and symptoms overlap.