Generic floxin 400 mg online
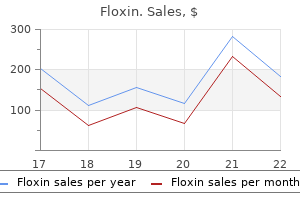
Protein intakes greater than the minimum requirement are usually inconsequential virus 1980 order floxin in united states online, as surfeit amino acids are normally easily catabolized. The average protein consumption in wealthy societies is approximately twice the average minimum requirement. Many diseases (or their treatment) increase the dietary protein requirement, by (1) increasing amino acid loss from the body (as in malabsorption and protein loss via wound exudates, fistulas or inflammatory diarrhea), removing amino acids from the circulation (renal replacement therapy), or (2) increasing muscle protein catabolism (as with high-dose glucocorticoid therapy). Protein-catabolic critically ill patients often excrete 15 g N/day or more in their urine in the absence of dietary protein provision. Sufficiently generous protein provision can minimize this kind of muscle atrophy, and there is widespread agreement that protein-catabolic patients require much more dietary protein requirement than healthy people. The exact magnitude of the increase has not yet been determined, but the most frequent recommendation for patients with protein-catabolic diseases is 1. Protein-Energy Interaction Energy deficiency-whether deliberate, as in weight reduction therapy, or inadvertent, as frequently occurs in hospitalized patients-increases amino acid loss from muscle and increases the dietary protein requirement. Micronutrients Minimum amounts of nine water-soluble vitamins (the B vitamins and vitamin C) and four fat-soluble vitamins (A, D, E, and K), eight minerals (calcium, phosphate, potassium, sodium, chloride, magnesium, zinc, and iron), essential fatty acids, and several essential trace elements (notably including selenium, copper, and iodine) are required throughout life to avoid deficiency diseases and death. Patients who have been hospitalized for more than a few days commonly consume inadequate amounts of food and the micronutrients it provides. Overt deficiencies of potassium, sodium, magnesium, phosphate, and iron occur so often in hospitalized patients that it is standard practice to monitor for and correct them. Many drugs used in acutecare medicine induce renal potassium, magnesium, or zinc wasting that necessitate appropriate increases in their provision. Gastrointestinal losses from nasogastric drainage tubes or intestinal losses from fistulas or diarrhea incur losses of potassium, sodium, calcium, magnesium, and zinc which add to their normal daily requirement. Less studied, but nonetheless common, are subclinical or unrecognized deficiencies of calcium, zinc, vitamin D, vitamin C, and possibly other micronutrients. Physicians often assume that consumption of the regular hospital diet will protect patients from these deficiencies. These patients are at risk of a variety of micronutrient deficiency diseases in addition to the symptoms and disability created by continuing in-hospital starvation. They include inadvertent or physician-ordered food deprivation, psychologic depression or distress, poorly controlled pain or nausea, badly presented unappealing food, communication barriers, anorexia nervosa, physical or sensory disability (including dysgeusia), thrush, dysphagia and other mechanical difficulties ingesting food, partial obstruction of the esophagus, stomach or intestinal tract, intestinal angina, and very commonly, combinations of these causes. The body normally adapts to starvation by reducing energy expenditure and curtailing protein catabolism, partly by hormone- and nervous system-regulated alterations in cellular metabolism, and partly by reducing its muscle mass. These adaptations enable prolonged survival during sub-lethal starvation, but survival comes at a cost that includes lethargy, a tendency to hypothermia, muscle atrophy (including of the cardiac and respiratory muscles), skin thinning, and functional disability. Until this terminology is better standardized, we suggest that health care workers explicitly distinguish among (1) situations that create a risk of inadequate nutrient intake, (2) situations in which inadequate intake of specific nutrients actually occurs and creates a discernable risk of developing a specific nutritional disease, and (3) the specific diseases themselves, as enumerated below. Old age is irreversible, but adequate protein and energy provision combined with physical rehabilitation can be lifesaving. As well, their reduced muscle protein mass is unable to release amino acids into the circulation at a rate sufficient to meet the need for protein synthesis at sites of injury and healing, and within the central protein pool to regulate the immuno-inflammatory process. The modern obesity epidemic has created a population of obese patients with chronic inflammation and starvation whose muscle atrophy outpaces their fat loss. Intravascular albumin pool redistributes into this large volume, decreasing the serum albumin concentration. Muscle atrophy and dietary protein deficiency perpetuate inflammation-induced hypoalbuminemia, because muscle protein and the diet provide the amino acids required for hepatic albumin synthesis. Hypoalbuminemia will not improve as long as systemic inflammation persists, even with prolonged optimal nutritional therapy. After systemic inflammation has subsided, several weeks of optimal nutrition may be required for serum albumin concentrations to renormalize. Conditions that increase body protein loss can be identified by measuring the rate of body N loss. Most N leaves the body in the urine (almost all of it in urea, ammonium, and creatinine), the feces, skin, and by other minor routes. Total N is not usually measured in hospital laboratories, but urinary urea concentrations are routinely available. Formulas are available that estimate that total N loss solely from 24-h urinary urea excretion. A recent, validated formula estimates daily total N loss (g) = g N in urinary urea/0. Net muscle protein catabolism follows approximately first-order ("decay") kinetics, such that the rate of N loss from muscle is proportional to the existing total amount of N available to be lost. Muscle atrophic, protein-catabolic patients lose less body N/day in absolute terms than an equivalently catabolic patients with normal muscle mass, but they are at nevertheless at greater risk of succumbing to their critical illness. Survival during prolonged, severe starvation depends both on fat and protein stores. Since protein and energy targets are based on normal body weight, this calculation is useful in situations in which actual body weight is unreliable or difficult to measure. These tools are often hindered by ambiguity about the intended meaning of "malnutrition" and failure to distinguish between screening and diagnosis. Diagnosis also involves an estimation of the probability that the diagnosis is correct and a judgment about its severity. By contrast, screening is the application of a test that identifies people at sufficiently high risk of a certain disease to warrant carrying out definitive procedures to establish the diagnosis or rule it out, or which identifies people at sufficient risk of developing the disease to warrant specific preventive interventions. A judgment is also reached as to how urgently nutritional intervention is required. Its disadvantage is that it is time-consuming and labor-intensive, and demands interest in and attention to the specific needs of individual patients. The details and evidence related to these products go beyond the scope of this chapter. It is relatively simple, safe, inexpensive, and maintains the digestive, absorptive, and immunologic barrier functions of the gastrointestinal tract. Pliable, small-bore feeding tubes make placement relatively easy and acceptable to most patients. They are available in a wide variety of formats that generally meet the nutritional requirements of a normal, healthy person. The proteins (from casein, whey, or soy) are intact and require normal pancreatic enzyme function for digestion and absorption. Fermentable (soluble) fibers such as pectin and guar are metabolized by colonic bacteria, yielding short-chain fatty acids that fuel colonocytes. Nonfermentable (insoluble) fibers increase fecal bulk, improve peristalsis, and may improve diarrhea. Although convenient and cost-effective, these products have fixed nutrient composition and thus are dosed according to the volume required to meet calorie requirements. For example, 1 L of a standard ready-to-use admixture of 5% amino acids and 25% dextrose provides 50 g of amino acids (equivalent to 41. A sterile compounder can accurately generate an appropriate recipe for such a patient. For example, 1 L of an admixture of 600 mL of 15% amino acids, 300 mL of 70% dextrose, and 100 mL of electrolyte/micronutrient mix contains 90 g amino acids (equivalent to 75 g of protein substrate) and 1020 kcal. The specific contribution of each non-essential amino acid to a nutritional admixture is less important than the total amount of non-essential N it provides. For example, 100 g of free mixed amino acids provide 83 g protein substrate and 340 kcal. They are primarily designed for patients with known maldigestion and malabsorption, but they are sometimes used empirically for patients who have had prolonged bowel rest or are critically ill without strong evidence of their superiority, or when a patient is intolerant of a standard polymeric formula. Traditional lipid emulsions are based solely on soy bean oil, but they are giving way to mixed emulsions that include medium-chain triglycerides, n-9 monounsaturated fatty acids, and n-3 fatty acids. Emulsions of pure soybean oil, a mixture of 80% olive oil and 20% soybean oil, and a mixture of 30% soybean oil, 30% medium chain triglycerides, 25% olive oil and 15% fish oil are available. The more complex lipid emulsions are more highly enriched in n-3 fatty acids and fewer n-6 polyunsaturated fatty acids than soybean 2328 lipid, which is more prone to lipid peroxidation and could promote the formation of the pro-inflammatory n-6 derivatives. As a general rule, lipid infusion rates should not exceed 8 g/h (for a 70 kg patient) or 175 g (1925 kcal)/day. Parenteral water-soluble vitamin requirements are greater than standard oral requirements because hospitalized patients often have vitamin deficiencies or increased requirements, and because intravenous administration of vitamins increases urinary losses.
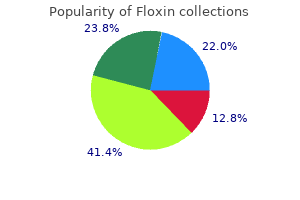
Buy 200mg floxin fast delivery
From observational epidemiologic studies and limited clinical (human and animal) studies antibiotics for mastitis buy cheap floxin 400mg on line, flavonoids have been postulated to play a role in the prevention of several chronic diseases, including neurodegenerative disease, diabetes, and osteoporosis. The ultimate importance and usefulness of these compounds against human disease have not been consistently demonstrated. However, the oxidized metabolites retinaldehyde and retinoic acid are also biologically active compounds. The term retinoids includes all molecules (including synthetic molecules) that are chemically related to retinol. Retinaldehyde (11-cis) is the form of vitamin A that is required for normal vision, whereas retinoic acid is necessary for normal morphogenesis, growth, and cell differentiation. Retinoic acid does not function directly in vision and, in contrast to retinol, is not involved in reproduction. Vitamin A is found in the human food supply in two forms: preformed as esters and provitamin A in carotenoids. There are >600 carotenoids in nature, ~50 of which can be metabolized to vitamin A. In humans, significant fractions of carotenoids are absorbed intact and are stored in liver and fat. Once binding has occurred, the retinol-binding protein complex interacts with a second protein, transthyretin. This trimolecular complex functions to prevent vitamin A from being filtered by the kidney glomerulus, thus protecting the body against the toxicity of retinol and allowing retinol to be taken up by specific cell-surface receptors that recognize retinol-binding protein. A certain amount of vitamin A enters peripheral cells even if it is not bound to retinol-binding protein. After retinol is internalized by the cell, it becomes bound to a series of cellular retinol-binding proteins, which function as sequestering and transporting agents as well as co-ligands for enzymatic reactions. Retinoic acid is a ligand for certain nuclear receptors that act as transcription factors. The receptors can either stimulate or repress gene expression in response to their ligands. The retinoid receptors play an important role in controlling cell proliferation and differentiation. These regimens are efficacious, and they are far less expensive and more widely available than injectable water-miscible vitamin A. For reasons that are not clear, while early neonatal vitamin A may reduce infant mortality, vitamin A given between 1 and 5 months of age has not proven effective in improving survival in high-risk settings. Children hospitalized with measles should receive two 60-mg doses of vitamin A on two consecutive days. Vitamin A deficiency most often occurs in patients with malabsorptive diseases. Typically, such patients are diagnosed in advanced care settings where they are treated for 1 month with 15 mg/d of a water-miscible preparation of vitamin A. This treatment is followed by a lower maintenance dose, with the exact amount determined by monitoring serum retinol. Finding application elsewhere in medicine, retinoic acid is useful in the treatment of promyelocytic leukemia (Chap. It was postulated that -carotene would be an effective chemopreventive agent for cancer because numerous epidemiologic studies had shown that diets high in -carotene were associated with lower incidences of cancers of the respiratory and digestive systems. However, intervention studies in smokers found that treatment with high doses of -carotene actually resulted in more lung cancers than did treatment with placebo. Again, however, the effectiveness of these agents has not been proved by intervention studies, and the mechanisms underlying these purported biologic actions are unknown. Selective plant-breeding techniques that lead to a higher provitamin A carotenoid content in staple foods may decrease vitamin A malnutrition in low-income countries. Liver, fish, and eggs are excellent food sources for preformed vitamin A; vegetable sources of provitamin A carotenoids include dark green and deeply colored fruits and vegetables. Exclusive breastfeeding can cover the vitamin A needs of infants if the mother has an adequate vitamin A status and a large enough volume of milk. If the nursing mother has inadequate vitamin A intake, concomitant diseases, or her infant was a preterm delivery, breast milk probably will not supply enough vitamin A to prevent deficiency. In developing countries, chronic dietary deficiency is the main cause of vitamin A deficiency and is exacerbated by infection. In early childhood, low vitamin A status results from inadequate intakes of animal food sources and edible oils, both of which are expensive, coupled with seasonal unavailability of vegetables and fruits and lack of marketed fortified food products. Factors that interfere with vitamin A metabolism may also affect status or function. For example, concurrent zinc deficiency can interfere with the mobilization of vitamin A from liver stores. Alcohol interferes with the conversion of retinol to retinaldehyde in the eye by competing for alcohol (retinol) dehydrogenase. Drugs that interfere with the absorption of vitamin A include mineral oil, neomycin, and cholestyramine. Stable isotopic or invasive liver biopsy methods are available to estimate total body stores of vitamin A. However, vitamin A deficiency severe enough to cause any clinical stage poses an increased risk of death from diarrhea, dysentery, measles, malaria, or respiratory disease. This is because vitamin A deficiency can compromise barrier, innate, and acquired immune defenses to infection. About 10% of pregnant women in undernourished settings also develop night blindness (assessed by history) during the latter half of pregnancy; this level of moderate to severe vitamin A deficiency is associated with an increased risk of maternal infection and death. Maternal vitamin A deficiency may also exacerbate already low vitamin A nutrition and associated risks for the newborn. Toxicity the acute toxicity of vitamin A was first noted in Arctic explorers who ate polar bear liver and has also been seen after administration of 150 mg to adults or 100 mg to children. Acute toxicity is manifested by increased intracranial pressure, vertigo, diplopia, bulging fontanels (in children), seizures, and exfoliative dermatitis; it 2316 may result in death. Among children being treated for vitamin A defi- ciency according to the protocols outlined above, transient bulging of fontanels occurs in 2% of infants, and transient nausea, vomiting, and headache occur in 5% of preschoolers. Chronic vitamin A intoxication is largely a concern in industrialized countries and has been seen in otherwise healthy adults who ingest 15 mg/d and children who ingest 6 mg/d over a period of several months. Manifestations include dry skin, cheilosis, glossitis, vomiting, alopecia, bone demineralization and pain, hypercalcemia, lymph node enlargement, hyperlipidemia, amenorrhea, and features of pseudotumor cerebri with increased intracranial pressure and papilledema. Liver fibrosis with portal hypertension may also result from chronic vitamin A intoxication. Provision of vitamin A in excess to pregnant women has resulted in spontaneous abortion and in congenital malformations, including craniofacial abnormalities and valvular heart disease. Commercially available retinoid derivatives are also toxic, including 13-cis-retinoic acid, which has been associated with birth defects. Thus contraception should be continued for at least 1 year and possibly longer in women who have taken 13-cis-retinoic acid. However, for unclear reasons, in one African setting there has been a negative effect on mortality rates in incompletely vaccinated girls. High doses of carotenoids do not result in toxic symptoms but should be avoided in smokers due to an increased risk of lung cancer.
Syndromes
- Thyroid hormone replacement pills, if the goiter is due to an underactive thyroid
- Transient ischemic attack (TIA)
- Throat spasm
- Increased sensations of sight, hearing, and taste
- Shortness of breath
- Swelling of the face, eyes, or tongue
- Benzodiazepines (such as diazepam or lorazepam)
- Encephalitis (brain infection)
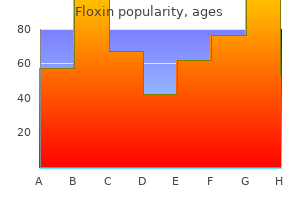
Best order for floxin
Many drugs used in the coronary care unit antibiotic breakpoint buy genuine floxin line, such as atropine, H2 blockers, and narcotics, can produce delirium, particularly in the elderly. The primary goal of treatment with antiplatelet and anticoagulant agents is to maintain patency of the infarct-related artery, in conjunction with reperfusion strategies. Bivalirudin was associated with a lower rate of bleeding, largely driven by reductions in vascular access site hematomas 5 cm or the administration of blood transfusions. Acute intravenous beta blockade improves the myocardial O2 supply-demand relationship, decreases pain, reduces infarct size, and decreases the incidence of serious ventricular arrhythmias. In patients who undergo fibrinolysis soon after the onset of chest pain, no incremental reduction in mortality rate is seen with beta blockers, but recurrent ischemia and reinfarction are reduced. Serum magnesium should be measured in all patients on admission, and any demonstrated deficits should be corrected to minimize the risk of arrhythmias. With advances in management, the mortality rate in each class has fallen, perhaps by as much as one-third to one-half. Infarction of 40% of the left ventricle usually results in cardiogenic shock (Chap. With the addition of intraarterial pressure monitoring, systemic vascular resistance can be calculated as a guide to adjusting vasopressor and vasodilator therapy. The former patients usually benefit from diuresis, while the latter may respond to volume expansion. The overall chamber enlargement that occurs is related to the size and location of the infarct, with greater dilation following infarction of the anterior wall and apex of the left ventricle and causing more marked hemodynamic impairment, more frequent heart failure, and a poorer prognosis. The extent of infarction correlates well with the degree of pump failure and with mortality, both early (within 10 days of infarction) and later. It may be secondary to previous diuretic use, to reduced fluid intake during the early stages of the illness, and/or to vomiting associated with pain or medications. By contrast, diuretic agents are extremely effective, as they diminish pulmonary congestion in the presence of systolic and/or diastolic heart failure. These drugs should be used with caution, however, as they can result in a massive diuresis with associated decreases in plasma volume, cardiac output, systemic blood pressure, and, hence, coronary perfusion. Nitrates in various forms may be used to decrease preload and congestive symptoms. Oral isosorbide dinitrate, topical nitroglycerin ointment, and intravenous nitroglycerin all have the advantage over a diuretic of lowering preload through venodilation without decreasing the total plasma volume. Only 10% of patients with this condition present with it on admission, while 90% develop it during hospitalization. Typically, patients who develop cardiogenic shock have severe multivessel coronary artery disease with evidence of "piecemeal" necrosis extending outward from the original infarct zone. The mechanisms responsible for infarction-related arrhythmias include autonomic nervous system imbalance, electrolyte disturbances, ischemia, and slowed conduction in zones of ischemic myocardium. An arrhythmia can usually be managed successfully if trained personnel and appropriate equipment are available when it develops. Since most deaths from arrhythmia occur during the first few hours after infarction, the effectiveness of treatment relates directly to the speed with which patients come under medical observation. Whereas in the past, frequent, multifocal, or early diastolic ventricular extrasystoles (so-called warning arrhythmias) were routinely treated with antiarrhythmic drugs to reduce the risk of development of ventricular tachycardia and ventricular fibrillation, pharmacologic therapy is now reserved for patients with sustained ventricular arrhythmias. Prophylactic antiarrhythmic therapy (either intravenous lidocaine early or oral agents later) is contraindicated for ventricular premature beats in the absence of clinically important ventricular tachyarrhythmias, because such therapy may actually increase the mortality rate. As described earlier (see "Beta-Adrenoceptor Blockers"), they should be used routinely in patients without contraindications. The occurrence of ventricular fibrillation can be reduced by prophylactic administration of intravenous lidocaine. In fact, in addition to causing possible noncardiac complications, lidocaine may predispose to an excess risk of bradycardia and asystole. For these reasons, and with earlier treatment of active ischemia, more frequent use of beta-blocking agents, and the nearly universal success of electrical cardioversion or defibrillation, routine prophylactic antiarrhythmic drug therapy is no longer recommended. Sustained ventricular tachycardia that is well tolerated hemodynamically should be treated with an intravenous regimen of amiodarone (bolus of 150 mg over 10 min, followed by infusion of 1. If ventricular tachycardia does not stop promptly, electroversion should be used (Chap. Ventricular arrhythmias, including the unusual form of ventricular tachycardia known as torsades des pointes (Chaps. Although the in-hospital mortality rate is increased, the long-term survival is excellent in patients who survive to hospital discharge after primary ventricular fibrillation; i. This result is in sharp contrast to the poor prognosis for patients who develop ventricular fibrillation secondary to severe pump failure. For patients who develop ventricular tachycardia or ventricular fibrillation late in their hospital course. Ventricular Tachycardia and Fibrillation Within the first Supraventricular Arrhythmias Sinus tachycardia is the most common supraventricular arrhythmia. If it occurs secondary to another cause (such as anemia, fever, heart failure, or a metabolic derangement), the primary problem should be treated first. Digoxin is usually the treatment of choice for supraventricular arrhythmias if heart failure is present. If heart failure is absent, beta blockers, verapamil, or diltiazem are suitable alternatives for controlling the ventricular rate, as they may also help to control ischemia. A randomized study of the prevention of sudden death in patients with coronary artery disease. The appropriate management is selected based on measurement of left ventricular ejection fraction, the timing following infarction, and whether revascularization has been performed. Accelerated junctional rhythms have diverse causes but may occur in patients with inferoposterior infarction. Sinus Bradycardia Treatment of sinus bradycardia is indicated if hemodynamic compromise results from the slow heart rate. Atropine is the most useful drug for increasing heart rate and should be given intravenously in doses of 0. Persistent bradycardia (<40 beats/min) despite atropine may be treated with electrical pacing. This difference is related to the fact that heart block in inferior infarction is commonly a result of increased vagal tone and/ or the release of adenosine and therefore is transient. In anterior wall infarction, however, heart block is usually related to ischemic malfunction of the conduction system, which is commonly associated with extensive myocardial necrosis. However, acceleration of the heart rate may have only a limited impact on prognosis in patients with anterior wall infarction and complete heart block in whom the large size of the infarct is the major factor determining outcome. Administration of a fibrinolytic agent is an alternative to early mechanical revascularization. It is important to diagnose the chest pain of pericarditis accurately, because failure to recognize it may lead to the erroneous diagnosis of recurrent ischemic pain and/ or infarct extension, with resulting inappropriate use of anticoagulants, 1884 nitrates, beta blockers, or coronary arteriography. When it occurs, com- plaints of pain radiating to either trapezius muscle is helpful, because such a pattern of discomfort is typical of pericarditis but rarely occurs with ischemic discomfort. Anticoagulants potentially could cause tamponade in the presence of acute pericarditis (as manifested by either pain or persistent rub) and therefore should not be used unless there is a compelling indication. The incidence of arterial embolism from a clot originating in the ventricle at the site of an infarction is small but real. Arterial embolism often presents as a major complication, such as hemiparesis when the cerebral circulation is involved or hypertension if the renal circulation is compromised. When a thrombus has been clearly demonstrated by echocardiographic or other techniques or when a large area of regional wall motion abnormality is seen even in the absence of a detectable mural thrombus, systemic anticoagulation should be undertaken (in the absence of contraindications), as the incidence of embolic complications appears to be markedly lowered by such therapy. Left Ventricular Aneurysm the term ventricular aneurysm is usually used to describe dyskinesis or local expansile paradoxical wall motion. Normally functioning myocardial fibers must shorten more if stroke volume and cardiac output are to be maintained in patients with ventricular aneurysm; if they cannot, overall ventricular function is impaired.
Discount floxin online visa
If the clinical examination does not clearly identify the diagnosis virus updates floxin 200mg online, hemodynamic assessments. In patients with elevated serum lactate levels, resuscitation should be guided towards normalizing these levels when possible. In patients with septic shock requiring vasopressors, the recommended target mean arterial pressure is 65 mmHg. Dobutamine use is suggested when patients show persistent evidence of hypoperfusion despite adequate fluid loading and use of vasopressors. Red blood cell transfusion is recommended only when the hemoglobin concentration decreases to <7. Infection Control So long as no substantial delay is incurred, appropriate samples for microbiologic cultures should be obtained before antimicrobial therapy is started. Antibiotic therapy should be narrowed once pathogens are identified and their sensitivities determined and/or once clinical improvement is evident. If needed, source control should be undertaken as soon as is medically and logistically possible. Spontaneous breathing trials should be used in mechanically ventilated patients who are ready for weaning. General Supportive Care Patients requiring a vasopressor should have an arterial catheter placed as soon as is practical. Hydrocortisone is not suggested in septic shock if adequate fluids and vasopressor therapy can restore hemodynamic stability. Continuous or intermittent sedation should be minimized in mechanically ventilated sepsis patients, with titration targets used whenever possible. Continuous or intermittent renal replacement therapy should be used in patients with sepsis and acute kidney injury. Pharmacologic prophylaxis (unfractionated heparin or low-molecular-weight heparin) against venous thromboembolism should be used in the absence of contraindications. Stress ulcer prophylaxis should be given to patients with risk factors for gastrointestinal bleeding. The goals of care and prognosis should be discussed with patients and their families. Support Of Organ Function the primary goal of organ support is to improve delivery of oxygen to the tissues as quickly as possible. Because crystalloid solutions vary in tonicity and inorganic/organic anions, few of these preparations closely resemble plasma. Many think that a greater intravascular volume is gained by use of colloids in shock, but the effects of colloids are modified by molecular weight and concentration as well as by vascular endothelial changes during inflammation. If the patient is allergic to -lactam antibiotics, use (1) aztreonam (2 g q8h) or (2) ciprofloxacin (400 mg q12h) or levofloxacin (750 mg q24h). Regimens include (1) cefepime (2 g q8h), (2) meropenem (1 g q8h) or imipenem-cilastatin (0. If the local prevalence of cephalosporinresistant pneumococci is high, add vancomycin (as above). If the patient is allergic to -lactam antibiotics, use levofloxacin (750 mg q24h) or moxifloxacin (400 mg q24h) plus vancomycin (as above). Endotracheal intubation protects the airway, and positivepressure breathing allows oxygen delivery to metabolically active organs in favor of inspiratory muscles of breathing and the diaphragm. An experiment in dogs showed that the relative proportion of cardiac output delivered to respiratory muscles in endotoxic shock decreased by fourfold with spontaneous ventilation over that with mechanical ventilation. During intubation, patients in shock should be closely monitored for vasodilatory effects of sedating medications or compromised cardiac output due to increased intrathoracic pressure, both of which may cause hemodynamic collapse. With hemodynamic instability, noninvasive mask ventilation may be less suitable in patients experiencing sepsis-associated acute respiratory failure. Adjuncts One of the great disappointments in sepsis management over the past 30 years has been the failure to convert advances in our understanding of the underlying biology into new therapies. Researchers have tested both highly specific agents and those with more pleotropic effects. The specific agents can be divided into those designed to interrupt the initial cytokine cascade. However, subsequent phase 3 trials failed to confirm this effect, and the drug was withdrawn from the market. Many adjunctive treatments in sepsis and septic shock target changes in the innate immune response and coagulation cascade. Specific adjuncts like glucocorticoids in septic shock have continued to be widely used. A large negative clinical trial and a conflicting systematic review in 2009 extended the debate about whether glucocorticoids lower 28-day mortality or improve shock reversal. Most meta-analyses report no change in mortality but an increase in shock reversal with glucocorticoid treatment. Despite a large number of observational studies suggesting that statin use mitigates the incidence or outcome of sepsis and severe infection, there are no confirmatory randomized controlled trials, and statins are not an element in routine sepsis care. De-Escalation of Care Once patients with sepsis and septic shock are stabilized, it is important to consider which therapies are no longer required and how care can be minimized. The de-escalation of initial broad-spectrum therapy, which observational evidence indicates is safe, may reduce the emergence of resistant organisms as well as potential drug toxicity and costs. The added value of combination antimicrobial therapy over that of adequate single-agent antibiotic therapy in severe sepsis has not been established. Current guidelines recommend combination antimicrobial therapy only for neutropenic sepsis and sepsis caused by Pseudomonas. Only weak evidence supports the use of balanced crystalloids, and guidelines recommend against using hydroxyethyl starches for intravascular volume replacement. When circulating fluid volume is adequate, vasopressors are recommended to maintain perfusion of vital organs. Vasopressors such as norepinephrine, epinephrine, dopamine, and phenylephrine differ in terms of half-life, - and -adrenergic stimulation, and dosing regimens. Although no difference was observed in 28-day mortality or in predefined septic-shock subgroup, arrhythmias were significantly greater with dopamine. As a result, expert opinion and consensus guidelines recommend norepinephrine as the first-choice vasopressor in septic shock. Levels of the endogenous hormone vasopressin may be low in septic shock, and the administration of vasopressin can reduce the norepinephrine dose. Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Even with intensive care, nosocomial mortality rates for septic shock often exceeded 80% as recently as 30 years ago. Burden of Disease Collaborators report that the primary risk factor for sepsis and septic shock-i. However, with advances in training, surveillance, monitoring, and prompt initiation of supportive care for organ dysfunction, the mortality rate from sepsis and septic shock is now closer to 20% in many series. Although some data suggest that mortality trends are even lower, attention has been focused on the trajectory of recovery among survivors. Patients who survive to hospital discharge after sepsis remain at increased risk of death in the following months and years. Those who survive often suffer from impaired physical or neurocognitive dysfunction, mood disorders, and low quality of life. However, an analysis of the Health and Retirement Study-a large longitudinal cohort study of aging Americans-suggested that severe sepsis significantly accelerated physical and neurocognitive decline. Among survivors, the rate of hospital readmission within 90 days after sepsis exceeds 40%.
Buy floxin 400mg without prescription
Thus virus ntl cheapest generic floxin uk, the process of stone formation may begin years before a clinically detectable stone is identified. Data suggest an increasing prevalence, likely due to Westernization of lifestyle habits. In addition to the medical costs associated with nephrolithiasis, this condition also has a substantial economic impact, as those affected are often of working age. Some reports have relied on symptomatic events, while others have been based on imaging. Most experts agree that radiographic evidence of a second stone should be considered to represent a recurrence, even if the stone has not yet caused symptoms. Some studies have examined the relation between diet and changes in the lithogenic composition of the urine, often using calculated supersaturation. However, the composition of the urine does not perfectly predict risk, and not all components that modify risk are included in the calculation of supersaturation. Thus, dietary associations are best investigated by prospective studies that examine actual stone formation as the outcome. Dietary factors that are associated with an increased risk of nephrolithiasis include animal protein, oxalate, sodium, sucrose, and fructose. Dietary factors associated with a lower risk include calcium, potassium, and phytate. Several conditions predispose to stone formation, including gastrointestinal malabsorption. A number of other medical conditions are more likely to be present in individuals with a history of nephrolithiasis, including hypertension, gout, cardiovascular disease, cholelithiasis, reduced bone mineral density, and chronic kidney disease. Although in the distant past dietary calcium had been suspected of increasing the risk of stone disease, several prospective observational studies and a randomized controlled trial have demonstrated that higher dietary calcium intake is related to a lower risk of stone formation. The reduction in risk associated with higher calcium intake may be due to a reduction in intestinal absorption of dietary oxalate that results in lower urine oxalate. Low calcium intake is contraindicated as it increases the risk of stone formation and may contribute to lower bone density in stone formers. Despite similar bioavailability, supplemental calcium may increase the risk of stone formation. The discrepancy between the risks from dietary calcium and calcium supplements may be due to the timing of supplemental calcium intake or to higher total calcium consumption leading to higher urinary calcium excretion. Owing to its low and often variable bioavailability, much of the oxalate in food may not be readily absorbed. Although observational studies demonstrate that dietary oxalate is only a weak risk factor for stone formation, urinary oxalate is a strong risk factor for calcium oxalate stone formation, and efforts to avoid high oxalate intake should thus be beneficial. Higher intake of animal protein may lead to increased excretion of calcium and uric acid as well as to decreased urinary excretion of citrate, all of which increase the risk of stone formation. Higher sodium and sucrose intake increases calcium excretion independent of calcium intake. Higher potassium intake decreases calcium excretion, and many potassium-rich foods increase urinary citrate excretion due to their alkali content. Other dietary factors that have been inconsistently associated with lower stone risk include magnesium and phytate. Vitamin C supplements are associated with an increased risk of calcium oxalate stone formation in men, possibly because of raised levels of oxalate in urine. Thus, male calcium oxalate stone formers should be advised to avoid vitamin C supplements. Although high doses of supplemental vitamin B6 may be beneficial in selected patients with type 1 primary hyperoxaluria, the risk is not reduced in other patients. Fluid intake is the main determinant of urine volume, and the importance of fluid intake in preventing stone formation has been demonstrated in observational studies and in a randomized controlled trial. Observational studies have found that coffee, tea, beer, wine, and orange juice are associated with a reduced risk of stone formation. Citrate reabsorption is influenced by the intracellular pH of proximal tubular cells. Metabolic acidosis, including that due to higher animal flesh intake, will lead to a reduction in citrate excretion by increasing reabsorption of filtered citrate. However, a notable proportion of patients have lower urine citrate for reasons that remain unclear. This characteristic does not appear to be associated with the risk of calcium oxalate stone formation. Nondietary Risk Factors Age, race, body size, and environment are important risk factors for nephrolithiasis. The incidence of stone disease is highest in middle-aged white men, but stones can form in infants as well as in the elderly. There is geographic variability, with the highest prevalence in the southeastern United States. Weight gain increases the risk of stone formation, and the increasing prevalence of nephrolithiasis in the United States may be due in part to the increasing prevalence of obesity. Environmental and occupational influences that may lead to lower urine volume, such as working in a hot environment or lack of ready access to water or a bathroom, are important considerations. Urinary Risk Factors As mentioned above, lower urine volume results in higher concentrations of lithogenic factors and is a common and readily modifiable risk factor. A randomized trial has demonstrated the effectiveness of higher fluid intake in increasing urine volume and reducing the risk of stone recurrence. This association is likely due to a combination of genetic predisposition and similar environmental exposures. While a number of rare monogenic disorders cause nephrolithiasis, the genetic contributors to common forms of stone disease remain to be determined. The two most common and well-characterized rare monogenic disorders that lead to stone formation are primary hyperoxaluria and cystinuria. Primary hyperoxaluria is an autosomal recessive disorder that causes excessive endogenous oxalate generation by the liver, with consequent calcium oxalate stone formation and crystal deposition in organs. Intraparenchymal calcium oxalate deposition in the kidney can eventually lead to renal failure. Cystinuria is an autosomal recessive disorder that causes abnormal reabsorption of filtered basic amino acids. The excessive urinary excretion of cystine, which is poorly soluble, leads to cystine stone formation. Cystine stones are visible on plain radiographs and often manifest as staghorn calculi or multiple bilateral stones. Although there is limited evidence for several aspects, there are standard approaches to patients with acute and chronic presentations that can reasonably guide the clinical evaluation. It typically requires weeks to months (and often much longer) for a kidney stone to grow to a clinically detectable size. Although the passage of a stone is a dramatic event, stone formation and growth are characteristically clinically silent. A stone can remain asymptomatic in the kidney for years or even decades before signs. Thus, it is important to remember that the onset of symptoms, typically attributable to a stone moving into the ureter, does not provide insight into when the stone actually formed. Renal colic is a misnomer because pain typically does not subside completely; rather, it varies in intensity. When a stone moves into the ureter, the discomfort often begins with a sudden onset of unilateral flank pain. The intensity of the pain can increase rapidly, and there are no alleviating factors. This pain, which is accompanied often by nausea and occasionally by vomiting, may radiate, depending on the location of the stone. If the stone lodges in the upper part of the ureter, pain may radiate anteriorly; if the stone is in the lower part of the Higher urine calcium excretion increases the likelihood of formation of calcium oxalate and calcium phosphate stones. While the term hypercalciuria is often used, there is no widely accepted cutoff that distinguishes between normal and abnormal urine calcium excretion. In fact, the relation between urine calcium and stone risk appears to be continuous; thus, the use of an arbitrary threshold should be avoided.
Purchase 400 mg floxin
Although frequently attempted bacteria require nitrogen for the synthesis of proven floxin 200 mg, most of these latter patients will not respond to plasmapheresis and steroids. Patients with advanced renal failure who present with hemoptysis should still be treated for their lung hemorrhage, as it responds to plasmapheresis and can be lifesaving. Kidney transplantation is possible, but because there is risk of recurrence, experience suggests that patients should wait for 6 months and until serum antibodies are undetectable. Disease in the younger age group is usually explosive, with hemoptysis, a sudden fall in hemoglobin, fever, dyspnea, and hematuria. Hemoptysis is largely confined to smokers, and those who present with lung hemorrhage as a group do better than older populations who have prolonged, asymptomatic renal injury; presentation with oliguria is often associated with a particularly bad outcome. As these lesions progress, there is concomitant interstitial nephritis with fibrosis and tubular atrophy. It is classically characterized by episodic hematuria associated with the deposition of IgA in the mesangium. There is a male preponderance, a peak incidence in the second and third decades of life, and rare familial clustering. There are geographic differences in the prevalence of IgA nephropathy, with 30% prevalence along the Asian and Pacific Rim and 20% in southern Europe, compared to a much lower prevalence in northern Europe and North America. It was initially hypothesized that variation in detection, in part, accounted for regional differences. With clinical care in nephrology becoming more uniform, this variation in prevalence more likely reflects true differences among racial and ethnic groups. IgA nephropathy is predominantly a sporadic disease but susceptibility to it has been shown uncommonly to have a genetic component depending on geography and the existence of "founder effects. IgA deposition in these entities is not usually associated with clinically significant glomerular inflammation or renal dysfunction and thus is not called IgA nephropathy. IgA deposited in the mesangium is typically polymeric and of the IgA1 subclass, the pathogenic significance of which is not clear. Abnormalities have been described in IgA production by plasma cells; in IgA clearance, by the liver and in mesangial IgA clearance and receptors for IgA. Currently, however, abnormalities in the O glycosylation of the hinge region of primarily polymeric IgA1 seem to best account for the pathogenesis of sporadic IgA nephropathy. Synthesis of poorly galactosylated IgA1 results in exposure of N-acetyl-galactosomine in truncated IgA1 hinge regions which is recognized by IgG or IgA1 antibodies leading to formation of immune complexes in the circulation or in situ after glomerular deposition of galactose-deficient IgA1. The galactose-deficient IgA1 may evade liver catabolism and preferentially deposit in the mesangium. A second hit, such as a viral or other antigen exposure, may be necessary for disease manifestation. Although each of these diseases has some unique clinical features, most features do not predict relapse or progression, and as a group, they are generally treated in the same way. Since mortality is high without treatment, virtually all patients receive urgent treatment. Induction therapy usually includes glucocorticoids and either cyclophosphamide or rituximab. Plasmapheresis is recommended in rapidly progressive renal failure or pulmonary hemorrhage. Steroids are tapered soon after acute inflammation subsides, and patients are maintained on cyclophosphamide or less toxic agents such as azathioprine, methotrexate, or rituximab for up to a year to minimize the risk of relapse. Presentation without renal involvement is termed limited granulomatosis with polyangiitis, although some of these patients will show signs of renal injury later. Chest x-ray often reveals nodules and persistent infiltrates, sometimes with cavities. Biopsy of involved tissue will show a small-vessel vasculitis and adjacent noncaseating granulomas. Although associated with an unacceptable high mortality rate without treatment, the greatest threat to patients, especially elderly patients in the first year of therapy, is from adverse events, which are often secondary to treatment, rather than active vasculitis. Patients should also be monitored long term for malignancy after immunosuppressive therapy. The two most common presentations of IgA nephropathy are recurrent episodes of macroscopic hematuria during or immediately following an upper respiratory infection often accompanied by proteinuria or persistent asymptomatic microscopic hematuria. Rarely patients present with acute renal failure and a rapidly progressive clinical picture. Cumulatively, risk factors for the loss of renal function identified thus far account for <50% of the variation in observed outcome but include the presence of hypertension or proteinuria, the absence of episodes of macroscopic hematuria, male sex, older age of onset, and extensive glomerulosclerosis or interstitial fibrosis on renal biopsy. Several analyses in large populations of patients found persistent proteinuria for 6 months or longer to have the greatest predictive power for adverse renal outcomes. Tonsillectomy and fish oil have also been suggested in small studies to benefit select patients. Granulomatosis with Polyangiitis Patients with this disease Disorders of the Kidney and Urinary Tract Microscopic Polyangiitis Clinically, these patients look somewhat similar to those with granulomatosis with polyangiitis, except they rarely have significant lung disease or destructive sinusitis. The distinction is made on biopsy, where the vasculitis in microscopic polyangiitis is without granulomas. Churg-Strauss Syndrome When small-vessel vasculitis is associated with peripheral eosinophilia, cutaneous purpura, mononeuritis, asthma, and allergic rhinitis, a diagnosis of Churg-Strauss syndrome is considered. Hypergammaglobulinemia, elevated levels of serum IgE, or the presence of rheumatoid factor sometimes accompanies the allergic state. Lung inflammation, including fleeting cough and pulmonary infiltrates, often precedes the systemic manifestations of disease by years; lung manifestations are rarely absent. A third of patients may have exudative pleural effusions associated with eosinophils. Small-vessel vasculitis and focal segmental necrotizing glomerulonephritis can be seen on renal biopsy, usually absent eosinophils or granulomas. The cause of Churg-Strauss syndrome is autoimmune, but the inciting factors are unknown. By definition kidneys with C3 glomerulopathy show sole or dominant staining for C3 but can have variable light microscopy with mesangial proliferative or membranoproliferative patterns seen most commonly. The optimal therapies remain undefined but include inhibition of the renin-angiotensin system, anticoagulants, steroids and other immunosuppressants. Increasing evidence suggests a benefit of therapy with eculizumab, a monoclonal antibody directed at C5 which is activated by C3. Classically, the glomerular tuft has a lobular appearance; intramesangial deposits are rarely present and subendothelial deposits are generally absent. Nephrotic syndrome, hypertension, and renal insufficiency all predict poor outcome. In the presence of proteinuria, treatment with inhibitors of the renin-angiotensin system is prudent. Evidence for treatment with dipyridamole, Coumadin (warfarin), or cyclophosphamide is not strongly established. If defects in the complement pathway are found, treatment with eculizumab is of hypothetical but unproven benefit. In particular, pegylated interferon and ribavirin are useful in reducing viral load.
Juglans cinerea (Butternut). Floxin.
- Gallbladder disorders, hemorrhoids, skin diseases, constipation, cancer, infections, restoring body function, and other uses.
- Are there any interactions with medications?
- Dosing considerations for Butternut.
- Are there safety concerns?
- How does Butternut work?
- What is Butternut?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96722
Discount floxin 200mg otc
Recurrent infections can result in injury to superficial mucosal vessels oral antibiotics for acne pregnancy effective floxin 200mg, with bleeding and, in severe cases, life-threatening hemoptysis. Management of massive hemoptysis usually requires intubation to stabilize the patient, identification of the source of bleeding, and protection of the nonbleeding lung. Control of bleeding often necessitates bronchial artery embolization and, in severe cases, surgery. Increasing attention is being given to defining clinical phenotypes of bronchiectasis in light of clinical, radiographic, and microbial features and to developing screening tools for the assessment of quality of life and disease severity. Possible suppressive treatments include (1) administration of an oral antibiotic. Furthermore, patients with different patterns of microbial colonization may not all experience similar benefits with macrolide therapy. In addition, ongoing consistent attention to bronchial hygiene can promote secretion clearance and decrease the microbial load in the airways. Pancreatic Findings the complete name of the disease, cystic fibrosis of the pancreas, refers to profound tissue destruction of the exocrine pancreas, with fibrotic scarring and/or fatty replacement, cyst proliferation, loss of acinar tissue, and ablation of normal pancreatic architecture. As in the lung, tenacious exocrine secretions (sometimes termed concretions) obstruct pancreatic ducts and impair production and flow of digestive enzymes to the duodenum. The sequelae of exocrine pancreatic insufficiency include chronic malabsorption, poor growth, fat-soluble vitamin insufficiency, high levels of serum immunoreactive trypsinogen (a diagnostic test used in newborn screening), and loss of pancreatic islet cell mass. The etiology of this dramatic anatomic defect in the male genitourinary system is not understood but may represent a developmental abnormality secondary to improper secretion by the vas or associated structures. Abnormalities of female reproductive tract secretions are likely contributors to an increased incidence of infertility among women with the disease. Robust pulmonary inflammation in the setting of inspissated mucus and chronic bacterial infection leads to collateral tissue injury and further aggravates respiratory decline. The ~1480-amino-acid molecule encodes a passive conduit for chloride and bicarbonate transport across plasma membranes of epithelial tissues, with direction of ion flow dependent on the electrochemical driving force. In numerous epithelia, chloride and bicarbonate release is followed passively by the flow of water, allowing for mobilization and clearance of exocrine products. Intense pulmonary inflammation is largely driven by chronic respiratory infection. Distinguishing the single nucleotide transversions or other polymorphisms with causal relevance can sometimes present a significant challenge. Schematic of the surface epithelium and supporting glandular structure of the human airway. A higher magnification view of a mucus plug tightly adhering to the airway surface, with arrows indicating the interface between infected and inflamed secretions and the underlying epithelium to which the secretions adhere. Failure of this mechanism disrupts normal hydration and transport of glandular secretion and is widely viewed as a proximate cause of obstruction, with concomitant tissue injury. Notably, hyperviscosity of eccrine sweat is not a clinical feature of the disease. Sweat ducts function to reabsorb chloride from a primary sweat secretion produced by the glandular coil. Chest physiotherapy several times each day is a standard means to promote clearance of airway mucus. The time, complexity, and expense of home care are considerable and take a significant toll on patients and their families. Improved treatments directed toward nutritional deficits, pulmonary inflammation, mucostasis, and other sequelae therefore remain a high priority in the field. Aggressive intervention in this setting can restore a large component of lung function, but ongoing and cumulative loss of pulmonary reserve reflects the natural history of the disease. Poor prognostic indicators such as sputum culture containing Burkholderia cepacia complex, mucoid P. Typical inpatient antibiotic coverage includes combination drug therapy with an aminoglycoside and -lactam for at least 14 days. Many families elect parenteral antibiotic treatment at home, and additional studies are needed to evaluate specific drug combinations, duration of therapy, and home versus inpatient management. Hypersensitivity to Aspergillus (allergic bronchopulmonary aspergillosis) occurs in ~5% of individuals with the disease and should be suspected in the absence of a response to conventional treatment. The disease is most common among whites (~1 in 3300 live births) and much less frequent among African-American (~1 in 10,000) or Asian populations (~1 in 33,000). These few genotype-phenotype correlations notwithstanding, genotype is, in general, a poor predictor of overall respiratory prognosis. Determining the optimal timing for surgery presents a substantial challenge, particularly because overall prognosis for individuals with severe lung disease is sometimes difficult to predict, and mortality associated with transplantation can be significant. Chronic administration studies of the drug are ongoing, and indicate significant benefit in terms of respiratory function and other clinical parameters. A dual formulation with ivacaftor confers improvement in pulmonary function among F508del homozygous individuals (~45% of the U. As a consequence, patient access to potentially efficacious agents (and off-label prescribing) is largely precluded. Moreover, clinical trials intended to expand drug label are difficult based on the small numbers of patients carrying ultra-rare alleles. Similar challenges to drug access have been noted in numerous other settings for which precision medicine has become a therapeutic priority. It has also become increasingly clear that carefully specified approaches to patient management can have an impact on overall prognosis. Well-defined measures for outpatient care are now established, including thresholds for hospital admission, antibiotic regimens, nutritional guidelines, periodicity of diagnostic tests, and other clinical parameters. The initiative has improved endpoints such as weight gain, body mass index, and pulmonary function. Based on data indicating that early nutritional and other therapies can be beneficial, newborn diagnosis is expected to significantly promote health among those with the disease. Implementation of quality improvement measures and novel therapeutics worldwide has become an increasing imperative. It is clear that future interventions will be tailored to specific genotypic abnormalities. Patients with a history of cigarette smoking without chronic airflow obstruction may have chronic bronchitis, emphysema, and dyspnea. Upon long-term exposure to cigarette smoke in genetically susceptible individuals, lung epithelial cells and T and B lymphocytes recruit inflammatory cells to the lung. Biological pathways of protease-antiprotease imbalance, oxidant/antioxidant imbalance, apoptosis, and lung repair lead to extracellular matrix destruction, cell death, chronic inflammation, and ineffective repair. Although most of these biological pathways influence multiple pathobiological results, only a single relationship between pathways and results is shown. Pulmonary vascular destruction occurs in concert with small airway disease and emphysema. The dominant current paradigm for the pathogenesis of emphysema comprises a series of four interrelated events: (1) Chronic exposure to cigarette smoke in genetically susceptible individuals triggers inflammatory and immune cell recruitment within large and small airways and in the terminal air spaces of the lung. Uptake of apoptotic cells by macrophages normally results in production of growth factors and dampens inflammation, promoting lung repair. It is unlikely that the intricate and dynamic process of septation that is responsible for alveologenesis during lung development can be reinitiated in the adult human lung. The elastase:antielastase hypothesis, proposed in the mid-1960s, postulated that the balance of elastin-degrading enzymes and their inhibitors determines the susceptibility of the lung to destruction resulting in air space enlargement. The elastase:antielastase hypothesis remains a prevailing mechanism for the development of emphysema. However, a complex network of immune and inflammatory cells and additional proteinases that contribute to emphysema has subsequently been identified. Upon exposure to oxidants from cigarette smoke, lung macrophages and epithelial cells become activated, producing proteinases and chemokines that attract other inflammatory and immune cells. Matrix metalloproteinases and serine proteinases, most notably neutrophil elastase, work together by degrading the inhibitor of the other, leading to lung destruction.
Safe floxin 200 mg
Reduced fetal urine production may contribute to oligohydroaminos and pulmonary hypoplasia antibiotics for pcos acne generic 200 mg floxin with visa. About 30% of affected neonates die shortly after birth due to respiratory insufficiency. These cysts may rarely become large and hemorrhagic, occasionally requiring nephrectomy when nephron-sparing surgery is not possible. Increasingly, nephron-sparing surgical approaches are being used for removal of cancerous lesions in order to preserve kidney function. Inherited diseases affecting the tubulointerstitial compartment of the kidney can lead to secondary glomerular stress and glomerulosclerosis with some degree of concomitant proteinuria. Similarly, disorders of glomerular function will typically lead to secondary interstitial fibrosis and tubule atrophy. From a clinical perspective, therefore, distinguishing between a genetic disease of the renal tubules and a disease of the glomerulus may not be easy, particularly in the absence of a gross phenotype such as large kidney cysts. Thus, mutations in other yet-to-be identified genes are able to produce similar interstitial kidney disease, both with and without hyperuricemia. These histologic features are not diagnostic of any particular genetic entity, and the specific diagnosis must be made by other means. Genetic tests for alterations in specific genes are increasingly available in the clinical setting. Each of the individual forms of nephronophthisis is quite rare, but together this category constitutes the most common inherited childhood form of kidney failure requiring kidney replacement therapy. Some of these gene defects cause limited kidney disease, while many cause ciliopathies characterized by multiple organ involvement. Joubert syndrome is defined by multiple neurologic findings, including hypoplasia of the cerebellar vermis. However, it is a major contributor to kidney failure in children, accounting for more than one-third of end-stage kidney disease in this group. It is not uncommon for such genetic lesions that affect both kidney and neurocognitive function. For example, renal tubular dysgenesis, defined by altered tubule development, can be caused by prenatal exposure of angiotensin converting enzyme inhibitors or angiotensin receptor blockers. Kidney biopsy shows chronic tubulointerstitial nephritis, as well as interstitial fibrosis. Kidney histology shows karyomegaly in addition to the non-specific findings of interstitial fibrosis and tubular atrophy. Thirteen of the genes involved in encoding components of the mitochondrial respiratory chain are located on the mitochondrial genome that is inherited maternally. These defects of oxidative phosphorylation may affect multiple organs and tissues. Tubulointerstitial disease may be seen on kidney biopsy, and progression to kidney failure may occur. Glomerular involvement, manifest as proteinuria and glomerulosclerosis, can also develop. Patients may have several defects in proximal tubule transport, including the Fanconi syndrome. Some patients may also have acidosis, hypophosphatemic rickets, hypercalciuria, glycosuria, and tubular proteinuria. Altered flow characteristics in the kidney tubules may lead to the development of formation of a nidus for stone formation. In addition, a previously unrecognized epidemic of kidney disease is leading to very high rates of kidney failure in and near the western coast of Central America. This mesoamerican nephropathy is particularly common in Nicaragua and El Salvador. Mesoamerican nephropathy patients do not have significant proteinuria, suggesting that this is a disease of the kidney tubules and interstitium. The cause is unknown, but some have suggested that a combination of toxic environmental factors and heat stress underlie the development of this kidney disease, which has a striking male predominance. However, the fact that in many families, a large fraction of the men are affected with kidney disease has suggested that a strong genetic component is involved, as well. Vivante A, Hildebrandt F: Exploring the genetic basis of early-onset chronic kidney disease. Salant Inflammation or fibrosis of the renal interstitium and atrophy of the tubular compartment are common consequences of diseases that target the glomeruli or vasculature. Distinct from these secondary phenomena, however, are a group of disorders that primarily affect the tubules and interstitium, with relative sparing of the glomeruli and renal vessels. The acute nature of this group of disorders may be caused by aggressive inflammatory infiltrates that lead to tissue edema, tubular cell injury, and compromised tubular flow, or by frank obstruction of the tubules with casts, cellular debris, or crystals. Urinary sediment is often active with leukocytes and cellular casts, but depends on the exact nature of the disorder in question. Renal ultrasonography may reveal changes of "medical renal disease," such as increased echogenicity of the renal parenchyma with loss of corticomedullary differentiation, prominence of the renal pyramids, and cortical scarring in some conditions. Because of the nonspecific nature of the histopathology, biopsy specimens rarely provide a specific diagnosis. Thus, diagnosis relies on careful analysis of history, drug or toxin exposure, associated symptoms, and imaging studies. Later, he described the lesion as "an acute inflammation of the kidney characterized by cellular and fluid exudation in the interstitial tissue, accompanied by, but not dependant on, degeneration of the epithelium; the exudation is not purulent in character, and the lesions may be both diffuse and focal. Peripheral blood eosinophilia adds supporting evidence but is present in only a minority of patients. Renal biopsy is generally not required for diagnosis but reveals extensive interstitial and tubular infiltration of leukocytes, including eosinophils. However, depending on the duration of exposure and degree of tubular atrophy and interstitial fibrosis that has occurred, the renal damage may not be completely reversible. Glucocorticoid therapy may accelerate renal recovery, but does not appear to impact long-term renal survival. More often, patients are found incidentally to have a rising serum creatinine or present with symptoms attributable to acute renal failure (Chap. More insidious reactions to the agents listed in Table 310-1 may lead to progressive tubulointerstitial damage. Examples include proton pump inhibitors and, rarely, sulfonamide and 5-aminosalicylate (mesalazine and sulfasalazine) derivatives and antiretrovirals. It is not clear if the recent association of proton pump inhibitors with incident chronic kidney disease involves an intermediate step of prolonged, subclinical interstitial nephritis. Diagnosis is often confounded by the fact that the ocular symptoms precede or accompany the renal disease in only one-third of cases. Additional extrarenal features include fever, anorexia, weight loss, abdominal pain, and arthralgia. Most patients experience some improvement in renal function if treated early with glucocorticoids before the development of significant interstitial fibrosis and tubular atrophy (Table 310-2). Other immunosuppressive agents may be required for those who relapse frequently upon steroid withdrawal. Tuberculosis should be ruled out before starting treatment because this too is a rare cause of granulomatous interstitial nephritis. Fibrotic lesions that form pseudotumors in the affected organs soon replace the initial inflammatory infiltrates and often lead to biopsy or excision for fear of true malignancy. Although the involvement of IgG4 in the pathogenesis is not understood, glucocorticoids have been successfully used as first-line treatment in this group of disorders, once they are correctly diagnosed. Renal biopsy in such patients reveals a more chronic inflammatory infiltrate with granulomas and multinucleated giant cells. The presence in some cases of autoantibodies to a tubular antigen, similar to that identified in rats with an induced form of interstitial nephritis, suggests that an autoimmune response may be involved. Recently, cases have been identified in which autoantibodies that may be important in disease pathogenesis were seen to target antigens expressed by collecting duct or proximal tubular brush border. Acute bacterial pyelonephritis does not generally cause acute renal failure unless it affects both kidneys or causes septic shock. Acute renal failure may occur when crystals of various types are deposited in tubular cells and interstitium or when they obstruct tubules.
Order 400 mg floxin otc
Ureteric obstruction may be treated by percutaneous nephrostomy tube placement or ureteral stent placement ukash virus buy floxin 400 mg cheap. Relief of obstruction is usually followed by an appropriate diuresis for several days. In rare cases, severe polyuria persists due to tubular dysfunction and may require continued administration of intravenous fluids and electrolytes for a period of time. Fluid and sodium should be restricted, and diuretics may be used to increase the urinary flow rate. In decompensated heart failure, stepped diuretic therapy was found to be superior to ultrafiltration in preserving renal function. Electrolyte and Acid-Base Abnormalities the treatment of dysnatremias and hyperkalemia is described in Chap. Ionized calcium should be monitored rather than total calcium when hypoalbuminemia is present. Excessive nutrition may increase the generation of nitrogenous waste and lead to worsening azotemia. Total parenteral nutrition requires large volumes of fluid administration and may complicate efforts at volume control. Uremic bleeding may respond to desmopressin or estrogens, but may require dialysis for treatment in the case of long-standing or severe uremia. Gastrointestinal prophylaxis with proton pump inhibitors or histamine (H2) receptor blockers is required. Venous thromboembolism Dialysis is indicated when medical management fails to control volume overload, hyperkalemia, or acidosis; in some toxic ingestions; and when there are severe complications of uremia (asterixis, pericardial rub or effusion, encephalopathy, uremic bleeding). On the other hand, initiating dialysis too early may unnecessarily expose individuals to intravenous lines and invasive procedures, with the attendant risks of infection, bleeding, procedural complications, and hypotension. The initiation of dialysis should not await the development of a life-threatening complication of renal failure. Small solutes are removed across a semipermeable membrane down their concentration gradient ("diffusive" clearance) and/or along with the movement of plasma water ("convective" clearance). The choice of modality is often dictated by the immediate availability of technology and the expertise of medical staff. Hemodialysis can be used intermittently or continuously and can be done through convective clearance, diffusive clearance, or a combination of the two. Hemodialysis is an intermittent procedure that removes solutes through diffusive and convective clearance. Continuous intravascular procedures were developed in the early 1980s to treat hemodynamically unstable patients without inducing the rapid shifts of volume, osmolarity, and electrolytes characteristic of intermittent hemodialysis. Studies have failed to show that continuous therapies are superior to intermittent therapies. Peritoneal dialysis has enjoyed widespread use internationally, particularly when hemodialysis technology is not as readily available. Because of its continuous nature, it is often better tolerated than intermittent procedures like hemodialysis in hypotensive patients. Peritoneal dialysis may not be sufficient for hypercatabolic patients due to inherent limitations in dialysis efficacy. Postdischarge care under the supervision of a nephrologist for aggressive secondary prevention of kidney disease is prudent. Gaudry S et al: Initiation strategies for renal-replacement therapy in the intensive care unit. The responses to reduction in nephron number are mediated by vasoactive hormones, cytokines, and growth factors. Risk factors include small for gestation birth weight, childhood obesity, hypertension, diabetes mellitus, autoimmune disease, advanced age, African ancestry, a family history of kidney disease, a previous episode of acute kidney injury, and the presence of proteinuria, abnormal urinary sediment, or structural abnormalities of the urinary tract. In addition, recent research in the genetics of predisposition to common complex diseases (Chap. The prevalence in West African populations seems to have arisen as an evolutionary adaptation conferring protection from tropical pathogens. As in other common diseases with a heritable component, environmental triggers (such as a viral pathogen) transform genetic risk into disease. These equations are valid only if the patient is in steady state, that is, the serum creatinine is neither rising nor falling over days. The presence of albuminuria in general serves as a well-studied screening marker for the presence of systemic microvas-cular disease and endothelial dysfunction. It has been validated in several cohorts around the world, although the risk for progression appears to be greater in North America, accounting for the regional adjustment in the equation. Moreover, in the absence of the risk factors noted above, population-wide screening is not recommended. However, the majority of these patients will show no further deterioration of renal function. Right: Secondary glomerular changes associated with a reduction in nephron number, including enlargement of capillary lumens and focal adhesions, which are thought to occur consequent to compensatory hyperfiltration and hypertrophy in the remaining nephrons. However, it is now appreciated that such individuals can be considered in two categories. The first includes patients with a subclinical primary glomerulopathy, such as focal segmental or global glomerulosclerosis (Chap. The second includes patients in whom progressive nephrosclerosis and hypertension is the renal correlate of a systemic vascular disease, often also involving large- and small-vessel cardiac and cerebral pathology. The relative contribution of each category varies among different geographic regions. Although serum urea and creatinine concentrations are used to measure the excretory capacity of the kidneys, accumulation of these two molecules themselves does not account for the many symptoms and signs that characterize the uremic syndrome in advanced renal failure. These include watersoluble, hydrophobic, protein-bound, charged, and uncharged nitrogencontaining non-volatile products of metabolism. It is thus evident that the serum concentrations of urea and creatinine should be viewed as being readily measured, but very incomplete surrogate markers for retained toxins, and monitoring the levels of urea and creatinine in the patient with impaired kidney function represents a vast oversimplification of the uremic state. A host of metabolic and endocrine functions normally performed by the kidneys is also impaired, and this results in anemia, malnutrition, and abnormal metabolism of carbohydrates, fats, and proteins. Elevated levels of C-reactive protein are detected along with other acute-phase reactants, whereas levels of so-called negative acute-phase reactants, such as albumin and fetuin, decline. In summary, the pathophysiology of the uremic syndrome can be divided into manifestations in three spheres of dysfunction: (1) those consequent to the accumulation of toxins that normally undergo renal excretion; (2) those consequent to the loss of other kidney functions, such as fluid and electrolyte homeostasis and hormone regulation; and (3) progressive systemic inflammation and its vascular and nutritional consequences. Chronic dialysis can reduce the incidence and severity of many of these disturbances, so that the florid manifestations of uremia have largely disappeared in the modern health setting. However, even optimal dialysis therapy is not completely effective as renal replacement therapy, because some disturbances resulting from impaired kidney function fail to respond to dialysis. This expansion may contribute to hypertension, which itself can accelerate nephron injury. Notwithstanding these two homeostatic responses, hyperkalemia may be precipitated in certain settings. These include increased dietary potassium intake, hemolysis, hemorrhage, transfusion of stored red blood cells, and metabolic acidosis. Importantly, a host of medications can inhibit renal potassium excretion and lead to hyperkalemia. These include conditions associated with hyporeninemic hypoaldosteronism, such as diabetes, and renal diseases that preferentially affect the distal nephron, such as obstructive uropathy and sickle cell nephropathy. The majority of patients can still acidify the urine, but they produce less ammonia and, therefore cannot excrete the normal quantity of protons. Animal and human studies have suggested that even modest degrees of metabolic acidosis may be associated with the development of protein catabolism. The concomitant sodium load mandates careful attention to volume status and the need for diuretic agents. Hyperparathyroidism stimulates bone turnover and leads to osteitis fibrosa cystica.
200mg floxin fast delivery
The patient should be asked about fever; change in character of sputum; and associated symptoms such as wheezing papillomavirus buy on line floxin, nausea, vomiting, diarrhea, myalgias, and chills. Inquiring about the frequency and severity of prior exacerbations can provide important information; the single greatest risk factor for hospitalization with an exacerbation is a history of previous hospitalization. The physical examination should incorporate an assessment of the degree of distress of the patient. The chest examination should establish the presence or absence of focal findings, degree of air movement, presence or absence of wheezing, asymmetry in the chest examination (suggesting large airway obstruction or pneumothorax mimicking an exacerbation), and the presence or absence of paradoxical motion of the abdominal wall. Approximately 25% of x-rays in this clinical situation will be abnormal, with the most frequent findings being pneumonia and congestive heart failure. The presence of hypercarbia, defined as a Pco2 >45 mmHg, has important implications for treatment (discussed below). The need for inpatient treatment of exacerbations is suggested by the presence of respiratory acidosis and hypercarbia, new or worsening hypoxemia, severe underlying disease and those whose living situation is not conducive to careful observation and the delivery of prescribed treatment. These may be administered separately or together, and the frequency of administration depends on the severity of the exacerbation. Patients are often treated initially with nebulized therapy, as such treatment is often easier to administer in those in respiratory distress. It has been shown, however, that conversion to metered-dose inhalers is effective when accompanied by education and training of patients and staff. This approach has significant economic benefits and also allows an easier transition to outpatient care. The addition of methylxanthines (theophylline) to this regimen can be considered, although convincing proof of its efficacy is lacking. Patients with moderate or severe exacerbations are usually treated with antibiotics, even in the absence of data implicating a specific pathogen. In patients admitted to the hospital, the use of systemic glucocorticoids reduces the length of stay, hastens recovery, and reduces the chance of subsequent exacerbation or relapse. One study demonstrated that 2 weeks of glucocorticoid therapy produced benefit indistinguishable from 8 weeks of therapy. Hyperglycemia, particularly in patients with preexisting diagnosis of diabetes, is the most frequently reported acute complication of glucocorticoid treatment. Studies have demonstrated that in patients with both acute and chronic hypercarbia, the administration of supplemental O2 does not reduce minute ventilation. It does, in some patients, result in modest increases in arterial Pco2, chiefly by altering ventilation-perfusion relationships within the lung. This should not deter practitioners from providing the oxygen needed to correct hypoxemia. Invasive (conventional) mechanical ventilation via an endotracheal tube is indicated for patients with severe respiratory distress despite initial therapy, life-threatening hypoxemia, severe hypercarbia and/or acidosis, markedly impaired mental status, respiratory arrest, hemodynamic instability, or other complications. For patients aged >65 admitted to the intensive care unit for treatment, the mortality rate doubles over the next year to 60%, regardless of whether mechanical ventilation was required. Hobbs B et al: Genetic loci associated with chronic obstructive pulmonary disease overlap with loci for lung function and pulmonary fibrosis. Lange P et al: Lung-function trajectories leading to chronic obstructive pulmonary disease. Rosas Diffuse parenchymal lung diseases include a large number (>200) of heterogeneous conditions that affect the lung parenchyma with varying degrees of inflammation and fibrosis. Physical examination findings Frequent rales at lung bases, digital clubbing is common. Fatigue, tightening of skin, exaggerated cold response, reflux, and difficulty swallowing. Bilateral subpleural reticular changes most prominent in lower, posterior lung zones. Mostly unknown, some Mostly unknown, debate about solvent and although silicate dusts silicate exposures. This algorithm represents a common approach to sub-classifying the interstitial lung diseases. It is typical to divide the interstitial lung diseases into those of known and unknown causes (although it is important to note that genetic studies demonstrate that a significant portion of familial and idiopathic pulmonary fibrosis [classically described as diseases of unknown cause] may be explained, in part, by genetic factors). Equally important to knowledge of disease classification is knowledge of disease prevalence. Cough with hemoptysis could also suggest a secondary pulmonary infection that can be seen in patients with traction bronchiectasis and in those receiving immunosuppressive therapy. The percentage of pulmonary fibrosis that is familial, as opposed to idiopathic, varies by study, with estimates ranging from <5% to as high as 20%. Occupational and environmental exposure histories are also important to obtain as they might identify exposures known to cause pulmonary fibrosis. However, the cost-effectiveness and the extent of laboratory testing that should be ordered in various clinical contexts have yet to be determined (as there is a relatively long list of auto-antibody tests that could be ordered). Although pulmonary function testing is rarely diagnostic, reductions in lung function help to characterize the extent of disease, and evidence for decline in repeated measures of pulmonary function. For example, enlarged hilar lymph nodes and a pattern of central nodular opacities in the mid to upper lung zones can suggest sarcoidosis. Trans-bronchial lung biopsies and lymph node biopsies (in sarcoidosis in particular) can lead to a confident diagnosis in patients with likely granulomatous lung disease. The diagnostic yield of biopsies tends to be higher if obtained prior to treatment. The desire to obtain a surgical lung biopsy should be weighed against the risks which can include a short-term mortality rate of as high as 5%. Although this remains a useful approach to classifying this diverse group of disorders it is important to recognize that genetic studies are challenging this classic categorization. It is important to remember that prognosis and treatment vary widely by disorder (and disease extent). Further meta-analyses have suggested that anti-fibrotic therapy may also improve survival. Additional unique findings include more diffuse imaging abnormalities with a predominance not limited to the lung bases, imaging abnormalities that spare the subpleural regions, and thickening of the bronchovascular bundles (as is apparent in the right mid lung zone on this image). Peribronchiolar, or perilobar opacities can be present and sometimes a rim of subpleural sparing (often referred to as a reversed halo or atoll sign) can be seen which can help to aid in the diagnosis. Sarcoidosis: Sarcoidosis can present with varied imaging abnormalities but a pattern of mediastinal and hilar lymphadenopathy with a pattern of reticular-nodular opacities involving the bronchovascular bundles (apparent in this image) are common features. Additional findings can include diffuse small nodules in a miliary pattern, larger nodular opacities, extensive ground glass infiltrates and, mosaic attenuation suggestive of small airways involvement, and in more advanced cases, signs of pulmonary fibrosis. Additional important diagnostic findings include fibroblast foci, which are subepithelial collections of myofibroblasts and collagen (as is apparent in the higher powered inset of this image). Sarcoidosis: the hallmark histopathologic feature of sarcoidosis is presence of granulomas (as are apparent numerously in the low powered image and more closely visualized in the higher powered inset image). Typically these are referred to as non-caseating which suggests the absence of necrosis. Caseating granulomas are rare in sarcoid and should prompt additional evaluation for an underlying infection. Because malignancy can result in a granulomatous reaction it is important to closely survey biopsy specimens with granulomatous involvement for additional signs of malignancy. Physical therapy and supplemental oxygen, when indicated, can improve exercise tolerance and reduce likelihood of developing pulmonary hypertension. Oxygen therapy, pulmonary rehabilitation, and lung transplantation may be required in patients with progressive disease. Volume loss and traction bronchiectasis involving the lower lung zones can also be found.