Discount nizagara 50mg fast delivery
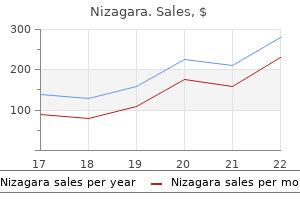
More recently erectile dysfunction 70 year olds purchase cheap nizagara on-line, the "midurethral theory" or "integral theory" has been described by Petros and Ulmsten [10]. This concept is based on earlier studies suggesting that the distal and midurethra play an important role in the continence mechanism [11] and that the maximal urethral closure pressure is at the mid-urethral point [12]. This theory proposes that damage to the pubourethral ligaments supporting the urethra, impaired support of the anterior vaginal wall to the mid-urethra, and weakened function of part of the pubococcygeal muscles, that insert adjacent to the urethra, are responsible for causing stress incontinence. This association of urethral hypermobility and stress urinary incontinence was also noted by Watson in 1924 [14] although it was not until 1949 that the first retropubic procedure for stress incontinence was described by Marshall et al. This early example of cooperation between two urologists and a gynecologist described "the correction of stress incontinence by simple vesicourethral suspension" in a series of 50 patients including 12 men with postprostatectomy stress incontinence. They reported an initial 82% success and 7% improvement rate, and the procedure became popular in the management of women with stress urinary incontinence. Rather than placing the sutures in the periosteum of the pubic symphysis, he described the attachment of the anterolateral vagina to the pectineal ligament using three sutures on each side [16]. He initially reported a series of 53 patients with 100% success rate and subsequently published a 9-year series of results in 1968 with a 93% success rate and an 8% incidence of enterocele [17]. Over the last 50 years, the Burch colposuspension has remained an efficacious and durable procedure in the surgical management of stress urinary incontinence and has undergone several modifications. This observation led to the widely adopted technique of providing support to the bladder neck without overelevation. Although many authors have reported excellent short-term subjective results from laparoscopic colposuspension [21], early studies showed inferior results to the open procedure [22,23]. More recently, the description of the "integral theory" has revolutionized the concept behind the traditional approach to retropubic surgery and has led to the introduction of the mid-urethral tapes using a retropubic [24,25] and transobturator approach [26]. While these procedures have largely replaced retropubic urethropexies in clinical practice, the colposuspension still has an important role in the management of women with stress urinary incontinence. Each suture should include the paraurethral tissue, lateral wall of the urethra, and the vaginal wall. The sutures are then fixed to the periosteum of the superior pubic ramus or the perichondrium of the symphysis pubis. At the end of the procedure, a Redivac drain should be placed in the retropubic space and a suprapubic catheter used for postoperative urinary drainage. Results Overall, there have been 58 published papers between 1951 and 1998 that have included 3238 patients, although many of these studies were retrospective case series. Overall cure rates were approximately 88% with results of 92% and 84% in primary surgery and redo surgery, respectively [27]. Two of these longterm studies have shown the efficacy rates to reduce over time with reported success rates being 90% and 77% at 1 year, 86% and 57% at 5 years, and 72% and 28% at 10 years [34,36]. Patients present with a history of severe suprapubic pain 1115 radiating into the groins and perineum, and a bone scan shows increased uptake in the suprapubic region. Long-term antibiotic treatment over several months is generally required, and occasionally, a retropubic abscess may require drainage. The abdomen and vagina are then prepared as a sterile operating field in order to allow the manipulation of the vaginal fornices and bladder neck by the surgeon. An indwelling Foley catheter is then inserted and the balloon inflated with 6 mL of water to allow the identification of the bladder neck. A low transverse suprapubic incision approximately 1 cm above the pubic symphysis is made and the rectus fascia incised taking care not to open the peritoneal cavity unless a concomitant intra-abdominal procedure is being performed. Vaginal manipulation is also used to further assist in the elevation of the lateral vaginal fornices while the bladder is swept medially. Two to four delayed absorbable sutures are inserted into the paravaginal fascia on each side and each tied down onto the vaginal tissue ensuring hemostasis. The suture is then passed vertically through the ipsilateral iliopectineal ligament, taking care not to pull the bladder neck open, and left untied. The bladder is left on free drainage using a suprapubic catheter for 48 hours prior to starting a clamping regimen. When considering all studies of colposuspension, objective cure rates varied between 59% and 100% (median 80%) and subjective cure rates between 71% and 100% (median 88%). Based on these results, colposuspension would appear to have comparable objective and subjective outcomes to traditional sling procedures and to both retropubic and transobturator mid-urethral tapes. Outcome: Colposuspension Historically, there have been many prospective case series and cohort studies assessing the efficacy of colposuspension with some studies providing long-term follow-up data up to 20 years (Table 71. The first of these was reported by Jarvis in 1994 [41] who reviewed 1726 women with a follow-up of at least 1 year and a mean objective success rate of 84. More recently, the Cochrane group has published a meta-analysis of 39 randomized controlled trials involving 2403 women with a mean follow-up of 1 year. While success rates tend to be slightly lower following failed previous continence surgery, continence rates between 65% and 86% are generally reported indicating the efficacy of colposuspension as a secondary procedure. Outcome: Colposuspension versus Anterior Colporrhaphy There have been seven trials comparing colposuspension with anterior colporrhaphy (Table 71. In general, success rates tend to be lower in the group of patients having anterior colporrhaphy as compared to colposuspension. While some studies indicate comparable success rates in the short term, the longer-term studies would suggest that efficacy is less good when compared to colposuspension. Outcome: Colposuspension versus Paravaginal Repair There has been only one randomized controlled trial comparing colposuspension with paravaginal repair in 72 women with a follow-up at 24 months [65]. There was a significantly higher success rate in the colposuspension arm compared to the paravaginal repair arm (100% vs. Outcome: Colposuspension versus Traditional Sling Procedures Seven trials have compared colposuspension with traditional sling procedures (Table 71. The evidence suggests that traditional sling procedures have similar efficacy to colposuspension although it may be associated with a higher incidence of voiding difficulties [27]. While there is considerable evidence to support the use of autologous fascial slings, adverse events may be more common following the use of synthetic sling materials. Conversely, significantly, more patients were found to have voiding difficulties following colposuspension [76] and subsequently were taught self-catheterization. In addition, significantly more women required surgery for urogenital prolapse following colposuspension [78]. Outcome: Colposuspension versus Laparoscopic Colposuspension There have been seven reported studies comparing open and laparoscopic colposuspension (Table 71. In addition to the published studies, the Cochrane group has also reported a meta-analysis of 22 studies including laparoscopic colposuspension [86]. In comparison to open colposuspension, they found subjective cure rates from 58% to 96% in the open group compared to 62% to 100% in the laparoscopic group at 18-month follow-up. Bladder and urethral trauma may occur during dissection in the retropubic space, and the reported incidence of bladder injury is 1. In addition, the ureters may be injured or kinked at the level of the most cephalad suture with one series of 60 cases reporting an incidence of 6. Postoperative Complications Overactive Bladder "De novo" urgency and urge incontinence may be reported, although whether this really represents new pathology or simply symptoms that were not adequately diagnosed preoperatively remains open to debate. While the exact cause may be multifactorial and partially explained by increased outflow resistance, postoperatively, there is some evidence to suggest that damage to the autonomic innervation may occur following dissection and mobilization of the bladder neck [99]. These findings support the findings of earlier studies that reported an incidence of detrusor overactivity between 12% and 18. Voiding Difficulties Voiding difficulty may occur early or late in the postoperative period.
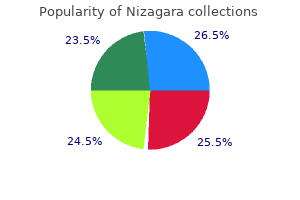
Generic 100mg nizagara fast delivery
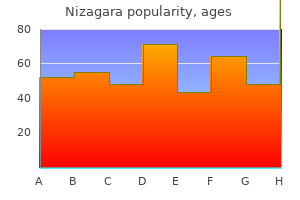
The results from uroflowmetry should be reported in the standard format: Qmax/Vvoid/Vres erectile dysfunction medications generic order nizagara online. The adoption of these standards will aid the interpretation of uroflowmetry results. This process will usually be aided by the a priori completion of a frequency volume chart and free uroflowmetry. There are certain key recommendations that will lead to the performance of a successful urodynamic study: First, a good urodynamic investigation should be performed interactively with the patient. Second, there should be continuous and careful observation of the signals as they are collected, and the continuous assessment of the qualitative and quantitative plausibility of all signals. Third, artifacts should be avoided, and any artifacts that occur should be corrected immediately. It is always difficult and is often impossible to correct artifacts during a retrospective analysis. Furthermore, it is more time-consuming than if the signals are continuously observed and tested at regular intervals and artifacts recognized during the urodynamic study and corrected. At present, ambulatory urodynamic monitoring has to rely on retrospective quality control and artifact corrections. However, in principle, the same quality criteria apply for ambulatory urodynamic monitoring as for standard urodynamics [2]. This makes a consensus on quality even more important, because only when such criteria are precisely defined can they be implemented in an "automated intelligent" ambulatory system. Quality control relies on pattern recognition and a knowledge of normal values as well as prior identification of useful information obtained from noninvasive urodynamics and all other sources relevant for the urodynamic question. Useful information obtained from noninvasive testing includes typical voided volumes and postvoid residual volumes as well as the expected values for Qmax. Only by good preparation can it be ensured that (1) the proper answers to the urodynamic questions will be obtained before the study is terminated and (2) essential modifications, additions, or repetitions of measurements will have been performed in order to derive the necessary information. The effective practice of urodynamics requires (1) a theoretical understanding of the underlying physics of the measurement, (2) practical experience with urodynamic equipment and procedures, (3) an understanding of how to ensure quality control of urodynamic signals, and (4) the ability to analyze critically the results of the measurements. Because urodynamics deals largely with mechanical measurements such as pressure and volume and their related changes in time, and because many 1836 analytical models use mechanical concepts such as resistance to flow or contraction power, it is essential that the nature of these measurements and concepts, in particular for pressure and flow rate, are understood. Therefore, in addition to a comprehensive understanding of anatomy and physiology, some basic knowledge of biomechanics and physics is required. The quality control of urodynamic measurements must be approached on a holistic basis. Different types and levels of data quality and plausibility control should be used (1) on a physical and technical level, (2) on a biomechanical level, and (3) on a pathophysiological clinical level. A common problem in urodynamics is that clinicians often proceed immediately to a clinical interpretation, that is, to level 3, without a critical analysis of the potential pathophysiologic information content, without considering the plausibility of the signals (level 1), without considering the biomechanical context of the measurements (level 2), and without taking into account the physical properties of the parameters, technical limitations, and accuracy of the signals. Therefore, it is recommended that invasive urodynamics should not be performed without precise indications and well-defined "urodynamic questions" that are to be answered by the results of the urodynamic study. However, a significant delay is to be expected for the typical urodynamic flow rate recorded extracorporeally. This delay will vary with anatomy, pathology, flow rate, and the setup for measurement. Our understanding of the actual dynamics of flow rate changes is limited, and the relatively slow response of most flowmeters may not be sufficient to match the dynamics of the much faster pressure signal. Therefore, we recommend the use of more descriptive terminology for synchronizing pressure and flow values, such as pdet. This indicates more complex causes, possibly psychogenic, but also physiologic, for example, that a difference in detrusor contraction strength may be involved, and that the fast filling rate used in clinical studies may lead to reduced contractility. This could also explain the difference in results between conventional and ambulatory studies. Zero pressure and reference height are concepts that are often confused in urodynamics, for example, by use of the misleading term "zero reference height. Zero pressure is the value recorded when a transducer is open to the environment when disconnected from any tubes or catheters, or when the open end of a connected, fluid-filled tube is at the same vertical level as the transducer. The reference height is the level at which the transducers must be placed so that all urodynamic pressures have the same hydrostatic component. It is often argued that it does not make a difference for the most relevant parameter, pdet, if the same error is introduced to pves and pabd, as they tend to cancel each other out. The hydrostatic pressure is real and important, and 1837 inevitably plays a role in any intracorporeal pressure recording. Also, it is only meaningful to subtract one pressure from the other- for example, (pves pabd = pdet)-when both are recorded to the same reference level. Pressure Transducers Urodynamic techniques are developed using external pressure transducers connected to the patient with fluid-filled lines, allowing easier compliance with the standards of correct zero and reference height. Catheter-mounted pressure transducers, so-called microtip transducer catheters, have become popular due to their apparent higher accuracy, better dynamic resolution, and their apparent independence from hydrostatic pressure. A catheter-mounted pressure transducer is an advantage for dynamic recordings of urethral pressures during coughing (stress profiles) as well as for ambulatory urodynamics in mobile patients. Here, only the application of catheter-mounted pressure transducers for intravesical and pabd recordings will be discussed as urethral pressures are dealt with in a separate report [4]. All aspects of urodynamic pressure recording outlined in the preceding section are valid and independent of transducer type. It is impossible to define the precise position of an intravesical and a rectal catheter-mounted pressure transducer as to place them at any common level, and impossible to position them at the standard level of the upper border of the symphysis pubis. It has become popular to circumvent this problem by setting the catheter-mounted pressure transducer to zero pressure when inside the body at the start of pressure recording. This, however, means that both the standard zero pressure as well the reference level are ignored, so that such recorded pressure cannot be compared between patients or centers. Thus, there are significant potential errors: By ignoring the correct atmospheric zero pressure, an error of up to 50 cmH2O can occur, and as the reference height of catheter-mounted pressure transducers is usually undetermined, another potential error of 10 cmH2O is possible for a full bladder. In addition, when a study starts with zero pabd, then the commonly observed pabd decrease at pelvic floor relaxation during voiding will result in negative pabd values, and thus in pdet being higher than pves. The same problem of apparent independence from the existing hydrostatic pressure also applies to air-filled catheters and/or connection tubings. Due to the absence of a water column between the balloon-covered opening on the catheter and the external transducer, the reference height in an air-filled system will refer to the position of the sensing balloon on the catheter and not to the external transducer. It is recommended that external transducers connected to fluid-filled tubings and catheters be used for intravesical and pabd recording. If microtip or air-filled catheters are used, any deviation from standard zero and reference level should be minimized and taken into account at the time of data analysis. Urodynamic Catheters Comparison between patients and urodynamic studies performed in different centers would be facilitated by the use of standard catheters. It is recommended that for the measurement of intravesical pressure and for bladder filling, the standard catheter for routine urodynamics is a transurethral doublelumen catheter. Only in small children and patients with severe constrictive obstruction (stricture) does suprapubic pressure recording have clear advantages. Intraurethral catheters should be as thin as possible, limited only by the practicality of insertion and by internal lumen sizes, which should be sufficiently large to avoid excessive damping of pressure transmission and to achieve the desired filling rate with standard pumps. The major advantage of a double-lumen catheter is that the fill/void sequence can be repeated without the need for recatheterization. This can result in an incorrect filling volume being indicated by the machine when the filling volume is calculated from the pump setting. For example, with a filling rate set at 60 mL/min and an actual filling rate of 30 mL/min, the machine will show double the filling 1838 volume. With some equipment, higher filling rates are possible; it is essential that any system should be critically tested to (1) measure the maximum filling rate that can be achieved by a particular catheter attached to an individual pump and (2) correct or calibrate the indicated infused volume.
Generic nizagara 25mg online
The rate of perioperative complications was identical to that of the outside-in route [33] erectile dysfunction at the age of 28 generic nizagara 100mg fast delivery. The Debodinance study [34] is a nonrandomized prospective study of a series of 100 women. At 1year follow-up, he does not report any significant difference in terms of perioperative or late-onset complications, postoperative dysuria, or de novo urge incontinence. For the majority of authors, the comparative study of the complications for the inside-out and outside-in routes does not show any significant difference between the two [40] (cf. Unfortunately, 285 of them were not comparative studies, did not have a control group, or were not explicit enough to be used. The metaanalysis was only able to use 18 articles, 6 randomized studies (representing 492 women), and 12 cohort studies (representing 2009 women). It was not possible to clearly evaluate the objective cure rate due to evaluation criteria that were unclear and varied from one study to the other. The relative risk of perioperative complications with the transobturator route compared to the retropubic route is 0. The relative risk of de novo urge incontinence at 1-year follow-up with the transobturator route compared to the retropubic route is 0. The results are determined based on several variables (route first of all, but also type of tape). The risk of nerve injuries to the pudendal nerve and the posterior terminal branch of the obturator nerve is controversial from the anatomical point of view for the inside-out transobturator approach [7,65]. Pudendal nerve damage has been proven in some studies on the inside-out approach [66]; however, the rarity of this complication does not lead to a conclusion that there is a greater neurological risk with inside-out than with outside-in approach. The risk of injury to the posterior terminal branch of the obturator nerve has been demonstrated anatomically [32]. When using the inside-out technique, passing as close as possible to the external side of the ischiopubic ramus limits the risk of injury to the posterior terminal branch of the obturator nerve. Poorly discriminated pain in the groin and root of the thigh region, usually transient, is more common in inside-out procedures [44]. Passing through the pelvic insertion of the adductor longus muscle may be responsible for postoperative pain [32]. Pain can have several other etiologies: infection of the implant requiring its removal and also idiopathic retraction of the implant. Chronic inflammatory reactions have also been described and perhaps painful scar neuromas during prosthetic ingrowth [69]. Some studies show that placing a tape by the retropubic route is more effective in the short and medium term than the transobturator route, when there is sphincter deficiency (86. There is a greater risk of vaginal erosion, in particular laterally, but this is due to poor insertion technique. Fixation of Gore-Tex slings to the pubococcygeal tendons: A simple technique of treating stress urinary incontinence using only the vaginal approach. Anatomical risks of transobturator suburethral tape in the treatment of female stress urinary incontinence. Transobturator surgery for female urinary continence: From outside to inside or from inside to outside: A comparative anatomic study. Recommendations for the treatment of non-neurological urinary incontinence in women, February 2010. Guidelines for the surgical treatment of female urinary stress incontinence in women using the suburethral sling. Synthesis of the guidelines for the treatment of non-neurological urinary incontinence in women. A comparison of two versions of the transobturator tension-free vaginal tape procedure. Influence of different sling materials on connective tissue metabolism in stress urinary incontinent women. Suburethral sling inserted by the transobturator route in the treatment of female stress urinary incontinence: Preliminary results in 117 cases. Prospective study on 185 females with urinary incontinence treated by an outside-in transobturator suburethral sling. Transobturator tape in treatment of stress urinary incontinence: It is time for a new gold standard. Surgical treatment of female stress urinary incontinence with a transobturator tape (Monarc): Short-term results of a prospective multicenter study. A new minimally invasive method in the treatment of urinary incontinence in women. Surgical treatment of female stress urinary incontinence with a trans-obturator-tape (T. Novel surgical technique for the treatment of female stress urinary incontinence: Transobturator vaginal tape inside-out. Transobturator surgery for female stress incontinence: A comparative anatomical study of outside-in vs inside-out techniques. A prospective trial comparing tension-free vaginal tape and transobturator vaginal tape inside-out for the surgical treatment of female stress urinary incontinence: 1-year followup. A comparative study of outside-in and inside-out transobturator tape procedures for stress urinary incontinence. Inside-out versus outside-in transobturator tension-free vaginal tape: A 5-year prospective comparative study. Complications following outside-in and inside-out transobturator-tape procedures with concomitant gynecologic operations. Prospective comparison of the "inside-out" and "outside-in" transobturator-tape procedures for the treatment of female stress urinary incontinence. Comparison of retropubic vs transobturator approach to midurethral slings: A systematic review and meta-analysis. Review of transobturator and retropubic tape procedures for stress urinary incontinence. Two-year comparison of tension-free vaginal tape and transobturator tape for female urinary stress incontinence. De novo urgency after tension-free vaginal tape versus transobturator tape procedure for stress urinary incontinence. A prospective randomized trial comparing tension-free vaginal tape versus transobturator tape in patients with stress or mixed urinary incontinence: Subjective cure rate and satisfaction in median follow-up of 46 months. Tension-free vaginal tape versus tension-free vaginal tape obturator in women with stress urinary incontinence. Retropubic compared with transobturator tape placement in treatment of urinary incontinence: A randomized controlled trial. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: Results of a multicentre randomised trial. Effectiveness and complication rates of tension-free vaginal tape, transobturator tape, and tension-free vaginal tape-obturator in the treatment of female stress urinary incontinence in a medium- to long-term follow up. Inside out transobturator vaginal tape versus tension-free vaginal tape for primary female stress urinary incontinence: Meta-analysis of randomized controlled trials. Transobturator vaginal tape inside out procedure for stress urinary incontinence: Results of 102 patients. Transobturator vaginal tape inside out for the surgical treatment of female stress urinary incontinence: Anatomical considerations. A prospective randomized trial of comparing the clinical outcome of tension-free vaginal tape and transobturator tape for stress urinary incontinence. Impact of the transobturator tape procedure on sexual function in women with stress urinary incontinence. Pathology of traditional surgical nets for hernia repair after long-term implantation in humans. Tension-free vaginal tape for surgical relief of intrinsic sphincter deficiency: Results of 5-year follow-up. Usefulness of retropubic tape for recurrent stress incontinence after transobturator tape failure. Three-year follow-up of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency. Tension-free vaginal tape for the treatment of urodynamic stress incontinence with intrinsic sphincteric deficiency.
Discount nizagara 100 mg
Simpler methods include merely vaginal mobilization of the urethra and bladder neck off from the pubic ramus and plication of the lower bladder impotence at 17 cheap nizagara american express, bladder neck, and urethra in an attempt to elongate the urethra. Most patients who do return with ongoing incontinence problems have a short urethra of only 1. A sling of levator muscle or scar tissue is used if there is no muscle complex remaining. This gives a 70% complete cure rate with no ongoing incontinence and 15% improved in their continence and 15% have no change [69]. This improvement is maintained in a 6-month follow-up but longer-term follow-up is not available. Those not improved or improved slightly but not satisfactorily can use the urethral plug as the urethra is now longer and narrower. Urinary Retention After removal of the catheter on day 10 or 14 after fistula repair, up to 8% of patients will have urinary retention with overflow. All patients should have a residual urine volume checked after their catheter is removed. It is usually treated with recatheterization with "bladder training," that is, clamping the catheter and releasing every 2 hours. After 48 hours, 70% of patients are voiding normally and the remaining will need a time of self-catheterization. Frequency and Voiding Disorders It has been noticed that on removing the catheter patients often complain of frequency of micturition and some voiding problems. It was often thought that this may resolve with time and could have been secondary from a prolonged catheterization; however, recent evidence from Ethiopia shows this problem is ongoing in at least some women. Of the 35 women studied with persistent incontinence despite fistula closure, 77% had more than eight episodes of voiding in 24 hours and 51% voiding more than 15 times. A further 13 persistently incontinence women were studied and this revealed a significant number of voiding dysfunctions with low flow rates, prolonged voiding times, and the average voided volume of only 72 mL [71]. Sexual and Reproductive Complications Other ongoing problems include dyspareunia in 11% of those sexually active (only 35% were sexually active at 6 months follow-up), 30% of women will have ongoing amenorrhea at 6 months, and nearly half of whom do not have an obvious cause, such as being postmenopausal, had a cesarean hysterectomy at the time of delivery, being pregnant, or on a long-acting progesterone contraception [39]. Social and Mental Health Most patients return to their normal living arrangements once they are cured and start to attend social functions and return to work. Several recent studies have shown improvements in social, physical, and mental health once they are cured [33,34,36]. Some, however, do not and still suffer ongoing mental health problems and difficulties with reintegrating back into their communities. All of the 71 cases had a fistula described as complicated, meaning that they had one or more of the following: excessive scarring, total destruction of the urethra, ureteric orifices outside the bladder or at the edge of the fistula, a small bladder, both recto- and vesicovaginal fistulae in conjunction, or the presence of bladder stones. Patients were more likely to have a failed repair if they (1) had a ruptured uterus at the time of labor, (2) had a previous failed repair, (3) presented with limb contractures, (4) presented malnourished or in poor health, (5) had a fistula described as complicated, and (6) had blood transfusion [72]. It is usually recommended that you should wait for 3 months before attempting another repair. Provisions need to be made for the patient to return to the hospital or if the patient is suffering severely, they can stay within the hospital and wait for their second repair. The only option for these women to have any quality of life is either to have a bladder augmentation or a urinary diversion operation. Patients who have such severe injuries often have their urethra affected, so even with a good reservoir, they are still unable to hold their urine. If the urethra is intact, then self-catheterization may be needed to effect full drainage of the bladder as the augmented bladder cannot contract, or mucous secreted from the bowel lining may block the urethra. This may be unmanageable for a woman living in the developing world, far from a supply of catheters and clean equipment. The former two options require an intact anal sphincter and the woman to agree to pass urine through the anus. The ileal conduit restricts a patient to living near a service that can supply the conduit bags, which are often rare in the developing world. The patient also needs to be close to a health center that knows how to deal with any complications. The ureters and kidneys in these women are often dilated and compromised and ascending infections can be common. There are anecdotal cases of ileal conduits being performed on patients, and then the patient has been unable to access bags, leaving her in a worse state than she was to start with. This should be an attainable dream in the twenty-first century and this suffering is placed in medical texts of yesteryear. The task, however, is immense with up to many thousands of new obstetric units being required for Africa alone to supply adequate maternity care [76]. In tandem with this, roads need to be built, transport systems put in place, and, most importantly, men and women educated. Until all this is achieved, the obstetric fistula patient will still need our caring attention. The obstetric vesicovaginal fistula: Characteristics of 899 patients from Jos, Nigeria. Obstetric fistula: A study of women managed at the Monze Mission Hospital, Zambia. Childbearing, health and social priorities: A survey of 22,774 consecutive hospital births in Zaria, Northern Nigeria. Dead mothers and injured wives: the social context of maternal morbidity and mortality among the Hausa of Northern Nigeria. Estimating the prevalence of obstetric fistula: A systematic review and meta-analysis. Obstructed labour injury complex: Obstetric fistula formation and the multifaceted morbidity of maternal birth trauma in the developing world. Risk factors for developing residual incontinence after vesicovaginal fistula repair. Reduction in the incidence of stress urinary incontinence complicating a fistula repair. Five years experience of ureterovaginal fistula following obstetric or gynaecological intervention. Urinary and faecal incontinence following delayed primary repair of obstetric genital fistula. The obstetric fistula and peroneal nerve injury: An analysis of 974 consecutive patients. Bilateral common peroneal nerve palsy secondary to prolonged squatting in natural childbirth. The impact of surgical treatment on the mental health of women with obstetric fistula. Urinary changes in obstetric vesico-vaginal fistulae: A report of 216 cases studied by intravenous urography. Pituitary and ovarian function in women with vesicovaginal fistula after obstructed and prolonged labour. Predicting the risk of failure of closure of obstetric fistula and residual urinary incontinence using a classification system. Factors influencing urinary fistula repair outcomes in developing countries: A systematic review. Classification of female genitourinary fistula: Inter- and intra-observer correlations. The immediate management of fresh obstetric fistulas with catheter and/or early closure. Spontaneous closure of vesicovaginal fistulas after bladder drainage alone: Review of the evidence. Factors influencing choice of surgical route of repair of genito-urinary fistula, and the influence of route of repair on surgical outcomes: Findings from a prospective cohort study. Transvaginal mobilization and utilization of the anterior bladder wall to repair the vesicovaginal fistulas involving the urethra. Prevention of residual urinary stress incontinence following successful repair of obstetric vesico-vaginal fistula using a fibro-muscular sling. Outcome of obstetric fistula repair after 10-day versus 14-day Foley catheterisation. Sling procedures after repair of obstetric vesicovaginal fistula in Niamey, Niger. A new method to manage residual incontinence after successful obstetric vesicovaginal fistula repair.
Purchase nizagara paypal
Abdominal sacral colpopexy with mersilene mesh in the retroperitoneal position in the management of posthysterectomy vaginal vault prolapse and enterocele impotence order nizagara in india. Vaginal versus abdominal reconstructive surgery for the treatment of pelvic 1497 19. The structure of the bladder neck, urethra and pelvic floor in relation to female urinary incontinence. Laparoscopic sacrocolpopexy with two separate meshes along the anterior and posterior vaginal walls for multicompartment pelvic organ prolapse. Laparoscopic sacrocolpopexy, hysterectomy, and Burch colposuspension: Feasibility and short-term complications of 77 procedures. Laparoscopic promontory sacral colpopexy: Is the posterior, recto-vaginal, mesh mandatory Porcine dermis compared with propylene mesh for laparoscopic sacral colpopexy: A randomized controlled trial. Long-term results of robotic assisted laparoscopy: Sacrocolpopexy for the treatment of high grade vaginal vault prolapse. Basic science and clinical studies coincide: Active treatment approach is needed after a sports injury. Tension-free vaginal tape and laparoscopic mesh colposuspension in the treatment of stress urinary incontinence: Immediate outcome and complications-A randomised clinical trial. Randomized prospective comparison of needle colposuspension versus endopelvic fascia plication for potential stress incontinence prophylaxis in women undergoing vaginal reconstruction for stage 3 or 4 pelvic organ prolapse. Laparoscopic sacrocolpopexy with Gynemesh as graft material-Experience and results. A comparison of laparoscopic and abdominal sacral colpopexy: Objective outcome and perioperative differences. Vaginal sacrospinous colpopexy and laparoscopic sacral colpopexy for vaginal vault prolapse. The absolute indication is fertility preservation in women who have not yet completed childbearing. However, this is a small group of patients; most women presenting requiring surgery for prolapse have no desire for further children, indeed the majority are postmenopausal. The latter is a contentious statement; clinical data is still sparse and will be discussed in this chapter. However, when there is loss of apical support, traditional vaginal hysterectomy will not correct defects. This is most readily apparent when women present with procidentia; it is self-evident that hysterectomy will not treat vaginal eversion. If hysterectomy is performed, additional vaginal suspension needs to be provided, usually either by sacrospinous fixation or sacrocolpopexy. Hysteropexy, in our view, offers a more logical approach, and furthermore avoids vaginal mesh, with the attendant extrusion risk it carries. While it has served the gynecologist well for many years, its continued use raises some significant questions. Vaginal hysterectomy fails to address the underlying deficiency in connective tissue pelvic floor support [1] that causes prolapse; indeed, the uterosacral ligaments are cut during the operation-it is hardly surprising that recurrent prolapse rates are so high, with rates of up to 40% described in the literature [2,3]. Recurrence can manifest with vaginal vault eversion, or more commonly recurrent enterocoele/cystocele. We know that cystocele commonly arises because of loss of apical type 1 vaginal support [4], and until apical support is established, it will recur. Up to one in four women may develop a vault hematoma following vaginal hysterectomy. This may be due to the wish to preserve fertility, or due to the belief that female identity is bound up in the female genital organs. It frequently arises after they have researched literature and the internet themselves and become aware that there are alternatives to hysterectomy. The overall rate of hysterectomy as treatment for menstrual dysfunction is also declining significantly. In 1888, Archibald Donald first described the Manchester repair as an alternative to vaginal hysterectomy for patients with uterine prolapse, although this may have been a more useful technique for patients with an elongated cervix rather than a true uterine descent. In 1934, Victor Bonney highlighted the passive role of the uterus in uterovaginal prolapse, telling us it was merely the symptom of underlying poor pelvic floor support [6]. Subsequent surgeons have developed techniques for uterine preservation via a vaginal, abdominal, or laparoscopic approach. His method involved a posterior colpotomy with division of the uterosacral ligaments from the cervix, plication across the midline, and reinsertion into the cervix. The cervix or uterosacral ligament is transfixed to the sacrospinous ligament using either permanent or delayed absorbable sutures. In 2001, Maher [9] reported a small comparison study between sacrospinous hysteropexy and vaginal hysterectomy with sacrospinous vault fixation, with no differences in objective or subjective outcomes at follow-up. Other studies have suggested that sacrospinous hysteropexy has a shorter operative time and reduced blood loss as compared to vaginal hysterectomy [10]. One study also reported less postoperative incidence of overactive bladder symptoms in the sacrospinous hysteropexy group [11]. Sacrospinous hysteropexy is the most studied vaginal technique for uterine preservation prolapse surgery; however, in general, the studies assessing it are of poor quality, with small numbers, of short follow-up periods, of lack of controls, and with limited functional outcome data. The technique of posterior vaginal slingplasty [13] was first described in 2001, using a mesh kit to create "neo-uterosacral ligaments. Abdominal Approach A number of methods for abdominal hysteropexy have been described, including transfixing the uterus to the anterior abdominal wall and ventral fixation to the pectineal ligaments. Most techniques use the sacral promontory as the fixation point, giving rise to the term abdominal sacrohysteropexy. Abdominal suture sacrohysteropexy [16] was described as early as 1957, with the uterine fundus being fixed to the sacral promontory with silk sutures. More recent techniques have utilized a variety of synthetic meshes to aid fixation. Leron and Stanton [18] followed up 13 women undergoing abdominal sacrohysteropexy and found it to be a safe and effective surgery for the management of uterine prolapse. Sacrohysteropexy was associated with a shorter operative time and hospital stay, with a reduction seen in intraoperative blood loss. It is difficult to interpret data reporting comparisons between abdominal sacrohysteropexy and hysterectomy due to variations used in surgical technique and differences in mesh type, size, shape, and attachment points. Laparoscopic Approach Laparoscopic abdominal surgery has, with very few exceptions, replaced laparotomy in many centers. The laparoscope confers better vision than laparotomy, allowing a magnified, high definition view. Furthermore, the long instruments allow better pelvic access, particularly behind the uterus, than laparotomy confers. A number of laparoscopic uterine suspension procedures have been described using different methods. Laparoscopic ventrosuspension proposes suturing the round ligaments to the rectus sheath. The round ligament is not however particularly robust, and perhaps as expected, it has been shown to have poor outcomes, with one case series of nine women reporting recurrent prolapse in all but one patient within 6 months [21]. While they reported good outcomes, all patients experienced significant pain or dragging 1501 sensations over the mesh attachment site. Recently, techniques have focused on using the sacral promontory as a point of fixation. The peritoneum is opened over the sacral promontory and the rectum is reflected laterally. A tunnel is created by blunt dissection underneath the peritoneum from the sacral promontory to the insertion of the uterosacral ligament complex into the cervix on either side. Mersilene tape on a needle is placed through the cervix, through the uterosacral ligaments, and through the peritoneal tunnels on each side before being tacked to the sacral promontory bilaterally to suspend the uterus. This technique aims for the sling to resemble newly created uterosacral ligaments.
PINK GRAPEFRUIT (Grapefruit). Nizagara.
- Asthma, lowering cholesterol, hardening of the arteries (atherosclerosis), preventing cancer, weight loss, psoriasis, muscle fatigue, promoting hair growth, toning the skin, reducing acne and oily skin, treating headaches, stress, depression, infections, digestive complaints in people with eczema, yeast infections (as a vaginal douche), and other conditions.
- Are there any interactions with medications?
- What is Grapefruit?
- Are there safety concerns?
- Dosing considerations for Grapefruit.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96909
Purchase cheap nizagara line
Nordenstam J impotence journal buy nizagara 50mg online, Mellgren A, Altman D, Lopez A, Johansson C, Anzen B, Zhong-ze Li, Zetterstrom J. Immediate or delayed repair of obstetric anal sphincter tears-A randomised controlled trial. Increasing incidence of anal sphincter tears among primiparas in Sweden: A population-based register study. Anal incontinence in women with third or fourth degree perineal tears and subsequent vaginal deliveries. Detecting anal sphincter injury: Acceptability and feasibility of endoanal ultrasound immediately postpartum. Differences in outcomes after third- versus fourth-degree perineal laceration repair: A prospective study. Anal endosonographic findings in the follow-up of primarily sutured sphincteric ruptures. Anatomic and functional results of surgical repair after total perineal rupture at delivery. Anal sphincter damage after vaginal delivery: Functional outcome and risk factors for fecal incontinence. Third-degree obstetric perineal tear: Long-term clinical and functional results after primary repair. Anal sphincter tears at vaginal delivery: Risk factors and clinical outcome of primary repair. Effect of new guideline on outcome following third degree perineal tears: Results of a three-year audit. Anal incontinence after obstetric sphincter tears: Incidence in a Norwegian county. Primary repair of obstetric anal sphincter laceration: A randomized trial of two surgical techniques. A prospective cohort study of women after primary repair of obstetric anal sphincter laceration. Long-term ailments due to anal sphincter rupture caused by delivery-A hidden problem. Anal sphincter function and integrity after primary repair of thirddegree tear: Uncontrolled prospective analysis. Risks of anal incontinence from subsequent vaginal delivery after a complete obstetric anal sphincter tear. Symptoms and anal sphincter morphology following primary repair of third degree tears. A randomized clinical trial comparing primary overlap with approximation repair of third degree obstetric tears. Early evaluation of bowel symptoms after primary repair of obstetric perineal rupture. Endosonography in the evaluation of anal function after primary repair of a third-degree obstetric tear. Objective methods cannot predict anal incontinence after primary repair of extensive anal tears. Anal incontinence after anal sphincter disruption: A 30-year retrospective cohort study. Management of obstetric anal sphincter injury: A systematic review and national practice survey. Anterior anal sphincter repair for fecal incontinence: Good long term results are possible. Long term results of overlapping anterior anal-sphincter repair for obstetric trauma. How to repair an anal sphincter injury after vaginal delivery: Results of a randomised controlled trial. The overlap technique versus end-to-end approximation technique for primary repair of obstetric anal sphincter rupture: A randomized controlled study. Overlapping compared with end-to-end repair of third- and fourth-degree obstetric anal sphincter tears: A randomized controlled trial. Overlapping compared with end-to-end repair of third-and fourth-degree obstetric anal sphincter tears: A randomized controlled trial. Overlapping compared with end-to-end repair of complete third-degree or fourth-degree obstetric tears: Three-year follow-up of a randomized controlled trial. Immediate repair of obstetric anal sphincter rupture: Mediumterm outcome of the overlap technique. Primary repair of advanced obstetric anal sphincter tears: Should it be performed by the overlapping sphincteroplasty technique Internal anal sphincter defect influences continence outcome following obstetric anal sphincter injury. Anal incontinence after obstetric sphincter tears: Outcome of anatomic primary repairs. Postoperative anal canal length predicts outcome in patients having sphincter repair for fecal incontinence. Antibiotic prophylaxis for prevention of postpartum perineal wound complications: A randomized controlled trial. Randomised clinical trial of a laxative alone versus a laxative and a bulking agent after primary repair of obstetric anal sphincter injury. Risk factors of recurrent anal sphincter ruptures: A population-based cohort study. National survey of perineal trauma and its subsequent management in the United Kingdom. Preserving the pelvic floor and perineum during childbirth-elective caesarean section Anal incontinence may range from mild leakage of gas causing social embarrassment to complete daily loss of control of feces and avoidance of all social activities. In general, therapy may be categorized into nonsurgical treatment, sphincter repair, sphincter augmentation, sphincter replacement, nerve stimulation, and fecal diversion (Table 94. Each of these treatments has different risks, success rates, and degrees of invasiveness. A recent task force of the American Society of Colon and Rectal Surgeons reviewed newer treatment alternatives to offer guidance [15]. The impact of dietary fiber must not be underestimated; in the treatment of 1431 incontinence, it provides stool bulk with little morbidity and has been shown to be very effective. The most studied medication is loperamide, which improves stool consistency and may also improve anal resting tone [18,19]. The best patients to undergo biofeedback are those with mild or moderate incontinence who have failed or are not good candidates for medical treatment [20]. Though there are very few large studies of the efficacy of biofeedback, it has been shown to be beneficial to many patients without imposing morbidity [21,22]. However, one study found that less than half of all patients referred for biofeedback actually completed the treatment, largely due to the lack of convenient access to a treatment center [23]. It has been shown that the willingness to complete all recommended biofeedback sessions is the strongest independent predictor of success [26]. One to several sessions per week are conducted for a number of weeks, though there is no single treatment regimen that is routinely followed. Other adjunctive treatments may be utilized, including digital feedback, manometric testing, ultrasound guidance, electrical stimulation, or anal balloons. Anal manometry may also be used to 1432 monitor the treatment effect, which has been shown to be durable at 1 year after finishing therapy [30,31]. The type of biofeedback offered is dependent on the individual physical therapist and the patient level of comfort with various treatment modalities. Eligible candidates have a thin anovaginal septum or a palpable sphincter defect, confirmed with an anal ultrasound. Nonetheless, the majority of overlapping sphincteroplasties are performed in women with a history of prior vaginal deliveries [33].
Syndromes
- Use of certain medications (including glucocorticoids/steroids, and opioid painkillers such as morphine)
- Chest x-ray
- Al-Anon/Alateen - www.al-anon.org
- Brittle nails
- Heart damage, including: Heart attack, angina (chest pain due to narrowed blood vessels or weakened heart muscle), heart rhythm disturbances
- Yeast infection
- Breathing blood or food into the lungs
Purchase nizagara once a day
Chronic failure may be due to atrophy of the periurethral tissues decreasing the compressive bulk within the cuff erectile dysfunction 18-25 generic 50 mg nizagara mastercard, not allowing for pressure to be dispersed evenly around the urethra, resulting in recurrent incontinence. Newly designed cuff backing has addressed this issue; however, it must be considered in cases of failure [14]. Surgical judgment should be used when replacing the malfunctioning portion of the device rather than the whole device. Indications for complete replacement of the device include fluid leakage, which may allow foreign material into the system, or chronic emplacement of the device (more than 3 years) [15]. Device erosion has decreased since the introduction of modified cuff architecture; however, it remains a concern with any foreign body implantation. Significant risk factors for erosions include perioperative injury, incorrect implantation technique, history of prior procedures, and infection [12]. Erosion of the sphincter cuff into the urethra is commonly associated with recurrent incontinence, although urinary tract infection and/or wound surgical site infection may be the first and only symptom. Erosion of the cuff through the vaginal wall is associated with vaginal bleeding and discharge. Erosion of the pressure-regulating reservoir into the bladder is rare, and may present as a urinary tract infection or infection of the device. Infection or erosion should be treated with explantation of the entire device in the majority of cases. In cases of cuff erosion into the urethra, the placement of an omental flap between the cuff and urethra is recommended at reoperation. When replacement of the pump is necessary, it should be moved to the opposite labium. The device with cuff erosion into the vaginal wall may be salvaged utilizing a Martius flap and vaginal wall closure. Before all salvage attempts, the patient should be counselled as to the high risk of eventual necessity for removal of the complete device. The average success rate ranges from 68% in a series of 31 women studied by Donovan et al. Reoperation for cuff malfunction or tubing problems has been as high as 21% in earlier series [18]; however, there is a clear trend toward reduced numbers of device failures due to technological advancements made over the years. Similar continence rate were found in another series of 55 patients at an average followup of 9. The transvaginal approach affords direct visualization of the difficult dissection of the urethrovaginal plane and the option of a suprameatal incision to allow in the anterior dissection of the urethra. Advantages of the transabdominal approach include lack of a vaginal incision and improved exposure to the endopelvic fascia and anterior bladder neck dissection. Additionally, transabdominal exposure allows the opportunity to perform a deliberate cystotomy to assist in a particularly difficult dissection. Regardless of operative approach, emphasis should be placed on meticulous surgical approach as intraoperative complication places the patient at risk for postoperative problems such as infection and erosion with eventual device explantation. The fatae of the "modern" artificial urinary sphincter with a follow-up of more than 10 years. The management of injuries to the urethra, bladder or vagina encountered during difficult placement of the artificial urinary sphincter in the female patient. Use of the artificial urinary sphincter in the management of severe incontinence in females. Stress urinary incontinence due primarily to intrinsic sphincteric deficiency: Experience with artificial urinary sphincter and sling cystourethropexy. Comparison of the long-term outcomes between incontinent men and women treated with artificial urinary sphincter. The use of the artificial urinary sphincter in the treatment of urinary incontinence in the female patient. Role of the artificial urinary sphincter in the treatment of stress incontinence in women. Long-term functional outcomes after the implantation of artificial urinary sphincter in women suffering from stress urinary incontinence. Laparoscopic artificial urinary sphincter implantation for female genuine stress urinary incontinence: Technique and 4-year experience in 25 patients. Laparoscopic approach for artificial urinary sphincter implantation in women with intrinsic sphincter deficiency incontinence: A single-centre preliminary experience. Laparoscopic approach for artificial urinary sphincter implantation for women with severe stress urinary incontinence. Robot-assisted laparoscopic artificial urinary sphincter insertion in men with neurogenic stress urinary incontinence. This, in combination with an increase in public awareness, has more and more women actively seeking treatment. This in turn has led to an increase in the number of patients having postoperative voiding issues. In a retropubic urethropexy, sutures elevating the bladder neck may be too tight and can cause overcorrection of the urethrovesical angle or "hypersuspension. Excessive periurethral scarring can occur anteriorly between the urethra and the pubis and lead to urethral compression. Sutures placed too distally can cause kinking with obstruction and an inadequately supported bladder neck/proximal urethra with potentially continued stress incontinence. With suburethral sling procedures, excessive tension on the sling around or under the urethra is usually responsible for obstruction. Sling tensioning, be it fascial or polypropylene, is highly arbitrary with considerable variability between surgeons as to what constitutes an appropriate amount of tension. This approximately corresponds to a two fingerbreadth width between the rectus fascia and the sutures once tied down. As a result, small nuances in tension may explain the difference in outcomes and complications reported by different groups [1]. Less commonly, displacement of the sling from its intended position may result in obstruction. This shorter distance may indicate a more proximal sling or may indicate a tighter sling (one that elevates the urethra more toward the symphysis), 1211 either of which may be responsible for the subsequent obstruction [6]. Also, in theory, patients with an altered wound healing cascade, as in the case for keloid formers or those suffering from scleroderma, can result in excessive scarring and lead to obstruction, even in cases where the sling appears to be loosely tied. When the problem persists, botulinum A toxin injection into the urethral sphincter has been reported to be successful [8]. Finally, impaired detrusor contractility may be responsible for a "relative obstruction" after incontinence surgery. The pathophysiology of obstructive symptoms is fairly easy to explain, but that of de novo storage symptoms is more complex. However, it is important to remember that a portion of patients who preoperatively have mixed symptoms will have their urge symptoms assume a more prominent and bothersome role once the stress incontinence has been cured postoperatively [9]. Several authors have demonstrated detrusor instability in association with obstruction [10,11]. They postulated that it was suggestive of the deleterious effects of chronic insidious obstruction as the sling tightens due to the increasing shrinkage over time [12]. It is believed by some that increased detrusor overactivity secondary to obstruction develops due to the acquired parasympathetic denervation sensitivity, while others believe that damage inflicted on the autonomic innervation of the bladder by surgical dissection leads to this without obstruction [13,14]. Others have suggested alterations in cholinergic and purinergic afferent pathways due to obstruction playing an integral role in the development of storage symptoms [15]. Although the exact pathophysiological mechanisms may not be agreed upon, it is clear that de novo storage symptoms do develop in a large number of patients with urethral obstruction. Patient may elect to remain obstructed rather than undergo further surgery or risk recurrence of incontinence. While evidence exists that women who void with no/minimal detrusor pressure or who void primarily with Valsalva maneuvers were more likely to require prolonged catheterization [22,23]; there are conflicting reports [24,25]. However, these results are confounded by the fact that surgical modification was allowed based on preoperative results, with nearly all modifications making surgery less obstructive, likely undertaken due to the theoretically higher risk of retention in those with detrusor underactivity or acontractility. Thereafter, there is a very low probability that any persistent retention will resolve without intervention.
Order nizagara uk
There are many examples of acquired defects erectile dysfunction treatment melbourne buy cheap nizagara online, the increasing use of indwelling devices provides niches for bacterial colonization and infection. Staphylococcus epidermidis) grow on these foreign bodies in a biofilm, protect them from host defense. Cellular factors in innate immunity: Natural defense against the invasion of the blood and tissue is mediated by phagocytic cells. Phagocytosis is the process by which the invading organisms are ingested by phagocytic cells, ingestion being followed by intracellular killing. Macrophages consist of histiocytes (wandering ameboid cells found in the tissue), the fixed reticulo -endothelial cells and blood monocytes. The innate immune system provides a rapid, initial means of defense against infection using genetically programmed receptors that recognize these structural features of microbes that are not found in the host. Pattern recognition receptors engagement can lead to activation of the host cell and its secretion of antimicrobial substances. Scavenger receptors that are involved in internalization of bacteria and phagocytosis of host cells that are undergoing apoptosis. Opsonins, the molecules (C3a, IgM), which bind to microbes to facilitate their phagocytosis. Inflammation: Tissue injury, initiated by the entry of pathogens leads to inflammation, which is an important non-specific mechanism of defense. The increased vascular permeability will allow easier access for neutrophils and monocytes. Acquired Immunity the resistance an individual acquires during life is called acquired immunity. Active Immunity (Adaptive Immunity) Active immunity or adaptive immunity is capable of recognizing and selectively eliminating specific foreign microorganisms and molecules, i. Active immunity sets in only after a latent period, which the immunological machinery needs for its functioning. When the individual is facing the same antigen subsequently, there is no latent or lag phase and the immune response is prompt, powerful and prolonged (Table 3. The antigenic specificity of the immune system permits it to distinguish minor difference among antigens. The antibodies can distinguish between two protein molecules that differ in only a single amino acid. The immune system is capable of generating tremendous diversity in its recognition molecules, permitting to recognize vast arrays of unique structures on foreign antigens. Once the immune system recognized and responded to an antigen, it exhibits immunological memory to recognize the same antigen, subsequently and react in a heightened manner (Refer Table 3. Finally, the immune system, normally responds to foreign antigens, indicating that it is capable of distinguishing self from non-self. The phagocytic cells crucial to nonspecific immune responses are intimately involved in igniting the specific immune response. Conversely various soluble factors produced during specific immune response have been shown to augment the activity of these phagocytic cells. Naturally acquired active immunity: this type of immunity is obtained when a person is exposed to antigens in the course of daily life. Once acquired, the immunity lasts for rest of its life such as in measles and chickenpox. For other diseases, especially in intestinal diseases, the immunity is short lasting. In syphilis, malaria and few other diseases, a special type of immunity is observed known as infection immunity (premunition). Comparison of active and passive immunity Active Passive Obtained passively, no participation Conferred by ready-made antibody Produced actively by the host immune system Induced by infection (clinical and subclinical) Induced by immunogens, vaccines Durability Lag phase Immunological memory Negative phase Application to immune deficient subjects Protection is durable and effective Present Present, subsequent challenge is more effective May occur Not applicable Protection is transient and less effective No lag phase No immunological memory, hence no secondary response No negative phase Effective in immune deficient hosts 32 Textbook of Immunology Artificially acquired active immunity: this type of immunity results from vaccination or immunization. Vaccinations may be inactivated bacterial toxins (toxoids), killed microorganisms, live but attenuated microorganisms or parts of microorganisms such as capsules. Killed vaccines are generally less immunogenic than the live vaccines and the immunity lasts only for a short period. Killed (inactivated) Passive Immunity Passive immunity is resistance exhibited by the host, when ready-made antibodies or defensive cells are introduced into the body. This form of protection is passive, because the individuals own immune system does not make antibodies or defensive cells against the disease producing agents or toxins. Naturally acquired passive immunity: this type of immunity involves natural transfer of antibodies from mother to her infant and also from mother to fetus. Certain antibodies (IgA) are passed from the mother to her nursing infants in breast milk, especially in the first secretion called colostrum. During pregnancy, some of the maternal antibodies are also transferred through placenta to the fetus. If the mother is immune to diphtheria, rubella or polio, the newborn Bacterial products Bacterial products and killed bacteria 2. Artificially acquired passive immunity: this type of immunity involves the introduction of antibodies into the body. These antibodies come from animal or person, who is already immune to the disease. Convalescent sera from patients very recently recovered from measles, rubella, etc. At times, instead of whole lymphocytes, an extract of lymphocytes (transfer factor of Lawrence) may be introduced as a therapeutic procedure in certain disease, such as lepromatous leprosy, immunodeficiency diseases such as Wiskott-Aldrich syndrome, disseminated malignancy, etc. Local Immunity the mucosal immune system is composed of the lymphoid tissues that are associated with the mucosal surface of the gastrointestinal, respiratory and the urogenital tracts. The system involves production of mucosal-related Ig that is IgA (secretory immunoglobulin). The primary function of the mucosal immune system is to provide defense to the host at mucosal surface, locally. Optimal host defense at the mucosal surface depends on both intact mucosal immue responses and non-immunologic protective functions such as residential bacterial flora, mucosal motor activity (peristalsis; ciliary function), mucus secretion that create barrier between potential pathogens and epithelial surfaces and innate immunity factors (lactoferin, lactoperoxidase and lysozyme). The concept local immunity has gained importance in the treatment of infections, which are either localized or where it is operative in combating infection at the site of primary entry of pathogens. The Sabin vaccine (for poliomyelitis) is administered orally to promote local IgA Indication of Passive Immunization 1. Passive immunization may also be employed to suppress active immunity, when the latter may be injurious. The commonest example is the use of Rh immunoglobulin during delivery to prevent immune response to rhesus factor in Rhnegative women with Rh-positive babies. Ideally, it is employed to provide immediate protection to non-immune individual with a tetanus-prone wound. Herd Immunity Herd immunity refers to an overall immunity exhibited by a community, which is relevant in the control of epidemic diseases. However, if a significant number of unprotected individuals become infected, the infection could spread rapidly through the unprotected members of population. In the course of that rapid replication, new mutant forms might arise that could evade the immune response and produce diseases in vaccinated individuals as well. The response may involve exclusively the humoral or cellular limb of the immune system, but most commonly involves both. Different lymphocytes, each with different set of receptors, recognize different epitopes on the same antigen. Based upon the nature of immune responses they generate, the antigens/epitopes are divided into three broad functional categories: 1. Immunogens (Complete Antigens) Immunogens are antigens/epitopes that induce immune response either by producing antibody or sensitized lymphocytes, which in turn react specifically with immunogens, which produced them. Although all molecules that have the property of immunogenicity also have the property of antigenicity, 36 Textbook of Immunology the reverse is not true. Some small molecules called haptens are antigenic, but incapable by themselves of inducing specific immune response. Haptens (partial Antigens) Haptens are small molecular weight substances, which are antigenic, but incapable by themselves of inducing specific immune response. The drug is not immunogenic by itself, but some people develop hypersensitivity reaction to it. In these people, when penicillin combines with serum protein, the resulting combined molecules initiate an immune reaction.
Order nizagara 100 mg mastercard
Robotic-assisted laparoscopic surgery for hysterectomy and pelvic organ prolapse repair erectile dysfunction age factor buy nizagara in united states online. Utilization and perioperative outcomes of robotic vaginal vault suspension compared to abdominal or vaginal approaches for pelvic organ prolapse. Robotic-assisted and laparoscopic sacrocolpopexy: Comparing operative times, costs and outcomes. Cost-minimization analysis of robotic-assisted, laparoscopic, and abdominal sacrocolpopexy. Analysis of the learning process for laparoscopic sacrocolpopexy: Identification of challenging steps. Long-term outcomes after totally robotic sacrocolpopexy for treatment of pelvic organ prolapse. They can occur in a number of anatomical locations along the urinary tract and the female reproductive system (Table 106. Over 90% of these are obstetrical in nature, caused by obstructed labor and poor access to medical care [2]. There are an estimated 500,000 women with untreated urogenital fistulas worldwide [6]. Many women in developing countries never present for treatment due to poor access to care and lack of financial resources. In one study, women who sought treatment presented an average of 5 years after the development of symptoms. However, these data are limited by the inability to differentiate between primary repairs, reoperations, and erroneous medical coding. Furthermore, this figure does not account for fistulas that were managed on an outpatient basis or managed conservatively without surgical intervention. The medicolegal implications and financial impact on the healthcare system are also important considerations [10]. In order to minimize the negative impact of urogenital fistula, accurate and timely diagnosis is critical. Effective management requires accurate diagnosis and avoidance of unnecessary tests and therapies. Finally, the clinician must be certain that any concomitant injuries to the urogenital tract have been ruled out or adequately addressed. This chapter will focus on the epidemiology, etiology, presentation, and diagnosis of female urogenital fistula. Poor nutrition, diabetes, atherosclerosis, steroid use, tobacco use [38], and ischemic states further increase the risk of fistula development in these patients [6]. Obstetrical injury due to obstructed labor is the leading cause of urogenital fistula in the developing world. The exact cause of foot drop is unknown, but it is thought to occur as a result of sacral nerve injury during fetal descent or peroneal nerve injury from prolonged squatting during obstructed labor [1]. The level of injury to the pelvic viscera is determined by the level at which fetal descent stops [12]. Therefore, any combination of urogenital fistulas, including vesicovaginal, urethrovaginal, ureterovaginal, vesicouterine, ureterouterine, and vesicocervical fistula, can develop as a result [9]. Rectovaginal fistulas can also 1559 occur after obstructed labor; however, they will not be discussed as they are beyond the scope of this chapter. Iatrogenic injury during pelvic surgery is the most common of cause of urogenital fistula in the developed world. Symmonds reviewed 800 cases in the United States and found that 75% of these injuries occurred during hysterectomy, while only 5% were caused by obstetrical injury [23]. Approximately 600,000 women undergo hysterectomy annually in the United States, and approximately 60% of these are performed for benign disease, including uterine leiomyoma and endometriosis [24]. Studies indicate that the rate of bladder injury during hysterectomy ranges from 1% to 5%, while the rate of ureteral injury ranges from 0. However, a majority of postoperative fistulas are thought to occur as a result of an unrecognized injury [29]. They found that the risk of fistula development was the greatest among women who had an abdominal hysterectomy performed for cervical cancer (1. Women undergoing total abdominal hysterectomy for benign diseases had a urogenital fistula rate of 0. Previously irradiated tissue undergoes progressive changes secondary to obliterative endarteritis, which can cause fibrosis, necrosis, and subsequent fistula formation [5,35]. The cumulative dose and proportion of external beam or brachytherapy delivered to the genitourinary organ have been shown to be associated with higher rates of fistula formation in some studies [36,37]. Smoking has also been implicated as an added risk factor in patients undergoing pelvic radiation therapy. Spontaneous fistulas can develop in patients with a history of malignancy or pelvic irradiation weeks to decades after treatment with a median of 8. Thus, secondary malignancies and oncological recurrences should be ruled out in patients with a history of pelvic malignancy [39]. Examination under anesthesia should be strongly considered in these patients in order to obtain biopsies and evaluate for concomitant pelvic masses prior to planned surgical repair. This occurs secondary to inadequate emergency obstetrical care during obstructed labor. The consequent prolonged contact between the fetus and a large area of pelvic soft tissue and visceral organs causes an ischemic pressure necrosis [11,15]. The level of injury to the lower urinary tract is determined by the level at which fetal descent is halted during labor [11,12]. However, these fistulas typically occur in the setting of operative deliveries requiring forceps or vacuum assistance. A urinoma can form and subsequently drain urine through the vaginal cuff forming an epithelialized tract with subsequent fistula formation. Another potential cause of posthysterectomy urogenital fistula is inadvertent suture incorporation of the posterior bladder wall during the vaginal cuff closure. The ensuing posterior bladder wall ischemia can lead to tissue necrosis and subsequent fistula formation. These injuries are typically supratrigonal and medial to the ureteral orifices [6,19]. In one series, over 60% of vaginal vault fistulas occurred after total abdominal hysterectomy [3]. It is estimated that only about half (51%) of all bladder injuries 1561 are identified and repaired intraoperatively [28]. Unfortunately, the true incidence of urogenital fistula after peerreviewed data is sparse, largely comprised of case reports. Ureterovaginal Fistulas Ureterovaginal fistulas are rare complications that are often caused by unrecognized injury to the ureter during pelvic surgery. Considered one of the most serious complications in pelvic surgery, consequences include paralytic ileus, sepsis, renal failure, and renal loss [13,16]. Although the ureter can be injured during any pelvic surgery, injury occurs most commonly during gynecological operative procedures. In the literature, the incidence of ureteral injury during hysterectomy ranges from 0.