Generic precose 50mg free shipping
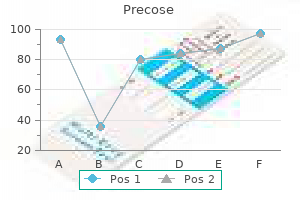
Accurate diagnosis of these conditions is essential to guide treatment options and to allow informed communication of the prognosis and genetic advice diabetes prevention 8 week plan order precose 50mg with amex. In amyotrophic lateral sclerosis, cell death of upper and lower motor neurons results in progressive failure of the neuromuscular system affecting limb, bulbar, and respiratory muscles. Average life expectancy is only 2 to 3 years from the onset of symptoms, with death usually resulting from respiratory failure. Characteristic clinical features are of combined upper and lower motor neuron signs in the bulbar, upper, and lower limb regions. Neuroprotective agents such as riluzole and edaravone have only modest effects on survival, but emerging gene therapy trials hold promise. Features of androgen insensitivity are likely to be present as well as mild distal sensory abnormalities. In approximately 75% of patients, the disease starts distally, focally, and asymmetrically in an upper or lower limb (Video 391-1), followed by progressive spread of injury in an anatomically logical progression to contiguous groups of motor neurons. Affected individuals may notice weakness, wasting or clumsiness of one hand, or unilateral footdrop. Muscle cramps may precede other clinical features, and fasciculations are most noticeable in the large proximal limb muscles. In the upper limbs, the thenar and intrinsic hand muscles tend to be severely affected, whereas the triceps and finger flexors are relatively spared until late in the disease. In the lower limbs, the pattern of weakness is often in a pyramidal distribution (flexors weaker than extensors), with early weakness of hip flexion and ankle dorsiflexion and severe involvement of the distal muscles. The first problem is usually slurring of speech, initially apparent only when the individual is tired. Patients often have a mixed spastic/flaccid dysarthria in which speech develops a tight strangled quality because of the upper motor neuron component, with a superimposed nasal quality as a result of the flaccid lower motor neuron weakness of the palate and nasopharynx. In patients with bulbar disease, examination often reveals weakness of the facial muscles; a spastic, weak, wasted, and fasciculating tongue; and a brisk jaw jerk. Dysphagia, initially more pronounced for liquids than for solids, usually follows the dysarthria within a few weeks or months (Video 391-3). Complications include weight loss and prolonged and arduous meal times with frequent episodes of coughing, drooling of saliva, and aspiration pneumonia. More commonly, respiratory muscle weakness develops insidiously and causes dyspnea and orthopnea. Diaphragmatic weakness may be apparent from the paradoxical movement of the abdominal wall during inspiration and a marked decline in forced vital capacity in the supine position. Symptoms of nocturnal carbon dioxide retention may develop, including interrupted sleep, morning headaches, anorexia, and daytime somnolence. Neck muscle weakness, which is common later in the course of disease, causes difficulty holding the head upright (dropped head syndrome). Eye movements tend to be spared even in advanced disease, thereby permitting limited communication by movements of the eyes. Although severe spastic spinobulbar paresis ultimately develops in these patients, the duration of survival is commonly 10 to 15 years after the onset of symptoms. The progressive bulbar palsy variant usually progresses to involve the limbs, although limb signs may not be present initially. A similar focal manifestation in the lower limbs, flail leg syndrome, is another recognized segmental variant. Non-neuronal cells in the vicinity of motor neurons may contribute importantly to neuronal injury. Associations have been reported with alterations in at least eight other genes in cases that appear sporadic. Thinning of the hypoglossal nerves and ventral spinal roots may be observed, and muscle atrophy is obvious. A cardinal feature in residual motor neurons is the presence of ubiquitinated proteinaceous inclusions, which may be compact or skeinlike. In the motor cortex, there is variable loss of upper motor neurons and astrocytic gliosis. In the descending corticospinal tracts, axonal loss, myelin pallor, and gliosis are seen. The atrophied skeletal muscle shows clusters of angular atrophic fibers and fiber-type grouping that results from serial denervation and reinnervation. The selectivity of the disease process for the motor system is now recognized to be relative, and involvement of extramotor parts of the central nervous system can be found, especially in the sensory and spinocerebellar pathways, substantia nigra neurons, and dentate granule cells in the hippocampus. Some of these inclusions comprise dipeptide proteins generated by aberrant translation of the G4C2 repeats. Lower motor neuron degeneration causes weakness, atrophy, and fasciculation of the limb and bulbar musculature. Features of upper motor neuron dysfunction include the incongruous presence of active or brisk tendon reflexes in a wasted limb, increased muscle tone, and sometimes the presence of Babinski sign. Upper motor neuron bulbar disease causes pseudobulbar palsy, with emotional lability, a brisk jaw jerk, slowing of repetitive tongue movements, and strained effortful speech. The diagnosis also requires the absence of other disease processes as determined by electrophysiologic testing, neuroimaging, and (if performed) biopsy. Neuroimaging of the brain and spinal cord is usually needed to exclude structural pathology. Muscle biopsy is indicated only in atypical cases when diagnostic uncertainty persists. Regions reflect segmental motor neuron pools: bulbar, cervical, thoracic, and lumbosacral. Awaji criteria for the diagnosis of amyotrophic lateral sclerosis: a systematic review. Gynecomastia, distal sensory features, perioral fasciculation, indolent progression. Pure motor disorders can result from compression of the deep palmar branch of the ulnar nerve and posterior interosseous branch of the radial nerve. Characteristic pattern of weakness with early involvement of the long finger flexors and quadriceps. The average 5-year survival rate is 25%, and approximately 5% of patients will survive for more than 10 years. The usual cause of death is respiratory failure, which may be accompanied by bronchopneumonia. Teams typically include a neurologist, nurse specialist, occupational therapist, physical therapist, speech and language therapist, and dietitian. During the course of the disease, patients frequently require referral for placement of a gastrostomy tube9 and to provide respiratory support. A1 It may cause fatigue, nausea, and dizziness, but these effects are frequently transient. Liver function tests should be performed at baseline and monthly for the first 3 months of therapy. New experimental approaches include gene therapy and antisense oligonucleotide technology to reduce the expression of disease-causing genes, small molecules to improve muscle contraction, and cell-based therapy aimed primarily at providing a supportive environment to prolong the survival of endogenous motor neurons. Good clinical care must focus on symptoms and preservation of independence and quality of life. In one randomized trial, mexiletine (300 mg/day) resulted in large dose-dependent reductions in the frequency and severity of muscle cramps. A3 In patients with progressive bulbar problems, optimal positioning, attention to food and fluid consistency, and protective swallowing techniques are helpful. Nuedexta (a combination of 20 mg dextromethorphan and 10 mg quinidine once daily) has been shown to improve symptoms of pseudobulbar affect (inappropriate tearfulness and laughter) and is also currently under study for symptoms of swallowing and speech dysfunction. A4 If weight loss continues, high-calorie nutritional supplements are added between meals. A5 Placement of a gastrostomy tube via endoscopy or under radiologic guidance is recommended in patients in whom dehydration, weight loss of 10 to 15%, frequent distressing choking episodes, prolonged and tiring mealtimes, or aspiration pneumonia develop. Management must emphasize detection and prevention of aspiration pneumonia, assistance in clearing of secretions by agents to reduce saliva production.
Syndromes
- To follow people who have had high cholesterol levels and are being treated
- Complete blood count with differential
- Factitious hyperthyroidism
- Medicines to treat symptoms
- Begins pedaling tricycle
- Complete blood count (CBC)
- Do not darken in the sun so may appear lighter than surrounding healthy skin
- Drooling or frothing at the mouth
Purchase precose without prescription
Both gonococcemia (Chapter 283) and meningococcemia (Chapter 282) can manifest with cutaneous lesions diabetes dogs oregon discount precose 25mg online. When accompanied by disseminated intravascular coagulation, large areas of retiform purpura and severe peripheral ischemia may develop. Cutaneous involvement in chronic meningococcemia is a reflection of lymphocytic or leukocytoclastic vasculitis. Pseudomonas infections of the skin vary from "hot tub" folliculitis (Chapter 410) to soft tissue infections of the external ear. Interdigital toe web infections that begin as simple tinea pedis can be complicated by superimposed Pseudomonas infection and result in erythema, swelling, tenderness, and drainage. Depending on its severity, treatment varies from topical antiseptics to oral or intravenous fluoroquinolones. Fungal Infections A variety of fungal infections involve the skin and nails and are most commonly due to dermatophytes (tinea), Candida spp, and Malassezia spp (pityriasis versicolor, also referred to as tinea versicolor) (Chapter 409; also see Table 412-1). Although both dermatophyte infections and pityriasis versicolor are associated with scaling, cutaneous candidiasis is characterized by erythema, a more erosive appearance, and satellite pustules. Septic emboli caused by Candida or other opportunistic fungi such as Aspergillus (Chapter 319) or Fusarium often have a clinical appearance similar to that of ecthyma gangrenosum secondary to gram-negative bacilli such as Pseudomonas. The responsible organisms can be detected histologically in biopsy specimens or by bedside examination of dermal scrapings; culture confirms the specific organism. While rare, cutaneous plaques secondary to Pneumocystis jiroveci favor the external ear canal. Scabies is characterized by pruritus in association with papules, papulovesicles, and linear burrows as well as signs of scratching, such as excoriations and areas of dermatitis. The number of mites living within the stratum corneum is limited in immunocompetent hosts; when scraped and examined microscopically, linear burrows provide the highest yield of mites and eggs. In elderly and immunosuppressed patients, a form of scabies known as crusted (previously Norwegian) scabies manifests as multiple areas of scaling and crusting that are teeming with mites. Infestations with scalp lice are seen most commonly in children, who may be symptom free or have marked pruritus. In addition to the lice, multiple egg casings ("nits") are attached to the proximal portions of scalp hairs. Pubic lice are sometimes called "crabs" because their bodies are shorter and broader than those of scalp or body lice and thus resemble the shape of a crab. Because of their leg span, these lice reside primarily on pubic hairs and less often on axillary hairs or eyelashes. Treatment of body lice involves discarding egg- and lice-infested clothing; for head lice, potential sources of reinfection, such as hairbrushes, should be discarded. Sexual and household contacts of patients with pubic lice and scabies, respectively, must be treated similarly to the patient who has symptoms. Cutaneous lesions are seen in leishmaniasis (Chapter 327), amebiasis (Chapter 331), schistosomiasis (Chapter 334), onchocerciasis (Chapter 335), strongyloidiasis (Chapter 335), and hookworm infections (Chapter 335). Dog and cat hookworm infections lead to cutaneous larva migrans, with serpiginous erythematous tracks that correspond to the path of migration of the hookworm larvae in sites where there has been direct contact with infected sand, most commonly the feet. In immunocompromised hosts, cutaneous plaques can occasionally develop from free-living amebae such as Acanthamoeba. Complications of oculocutaneous albinism include decreased visual acuity, nystagmus, photophobia, and an increase in cutaneous carcinomas, especially squamous cell carcinoma. These signs and symptoms are most severe in those who produce the least pigment and have the greatest amount of cumulative sun exposure. The differential diagnosis includes total vitiligo (absence of melanocytes histologically) and a few inborn errors of metabolism. Treatment consists of longitudinal ophthalmologic care and minimizing sun exposure. In welldeveloped lesions, the skin is white, not tan, in color due to complete loss of melanin. Disorders of linear hypopigmentation consist primarily of nevoid conditions caused by somatic mosaicism. A minority of patients have associated central nervous system, musculoskeletal, or ocular abnormalities. Idiopathic guttate hypomelanosis with small, well-demarcated hypopigmented macules on the shin. Vitiligo, which is caused by a loss of melanocytes within the skin, is also associated with autoimmune endocrinopathies and alopecia areata. T cells that recognize antigens on the surface of melanocytes (and melanoma cells) are found within the skin and in peripheral blood. A5 Combinations of follicular and epidermal stem cell suspensions are an experimental approach for difficult-to-treat disease. The favored sites for this common age-related disorder, which may be related to chronic sun exposure, are the shins and the extensor surface of the forearms. Linear streaks of hyperpigmentation can be due to nevoid conditions that reflect cutaneous mosaicism, as in linear hypopigmentation (see earlier) and several genodermatoses. The latter corresponds to the cutaneous venous plexus and is seen most commonly in the lumbosacral region where heating pads have been applied or on the anterior thighs from laptop computers. The most common causes of circumscribed hypermelanosis are pityriasis (tinea) versicolor (which can present as both hypopigmentation and hyperpigmentation, hence its name), postinflammatory hyperpigmentation, and melasma. Although postinflammatory hypopigmentation is most often associated with atopic dermatitis, it also can occur with sarcoidosis (Chapter 89), cutaneous lupus erythematosus (Chapter 250), and mycosis fungoides (Chapter 176). The lesions are exacerbated by ultraviolet light and estrogen (oral contraceptives, pregnancy). Melasma is treated with daily broad-spectrum sunscreens plus lightening agents such as hydroquinone (4% cream) and retinoic acid (0. The explanation for the increased incidence is speculative in most instances, with the exception of curled hairs leading to pseudofolliculitis barbae. Tightly curled hairs, when shaved, are usually cut at an oblique angle, which results in a sharp tip at the distal end of the hair shaft that allows penetration of the skin adjacent to the hair follicle and subsequent inflammation. In the former situation, they are thought to represent an exaggerated response to wound healing, with increased formation of collagen not only at the site of the trauma (as in hypertrophic scars) but also in adjacent, previously uninvolved skin. Treatment options include intralesional corticosteroids, intralesional interferon, pulsed dye laser, or excision followed by radiation therapy. These locations can help narrow the differential and guide further diagnostic testing and therapy in many patients. Because of its potential systemic implications, careful medical evaluation is required (Table 412-6). Combination of follicular and epidermal cell suspension as a novel surgical approach in difficult-to-treat vitiligo: a randomized clinical trial. Efficacy of transplantation of combination of noncultured dermal and epidermal cell suspension vs epidermal cell suspension alone in vitiligo: a randomized clinical trial. Antibiotics after incision and drainage for uncomplicated skin abscesses: a clinical practice guideline. Managing keloid scars: from radiation therapy to actual and potential drug deliveries. Of the following entities, which is seen more commonly in African Americans than in Asians or whites Tinea (pityriasis) versicolor Answer: D Entities that are seen more commonly in African Americans are outlined in Table 412-3. A 60-year-old woman presents with an area of reticulated hyperpigmentation overlying the lumbosacral spine. Fixed drug eruption secondary to nonsteroidal anti-inflammatory drugs Answer: C Erythema ab igne is seen at sites of repeated heat exposure, such as from heating pads and computer batteries. Hyperpigmentation due to cupping and moxibustion (traditional Chinese medicine) or a fixed drug eruption is circular in shape, not reticulated. Melasma can affect extrafacial sites, but they are primarily the extensor forearms and upper chest, and the lesions are circumscribed, not reticulated. Patients with the genodermatosis dyskeratosis congenita have reticulated pigmentation and pancytopenia, but lesions would not be limited to the lower back.
Purchase precose cheap
Diplomacy is needed to establish whether the motivation reflects a medicolegal concern rather than a biologic change in the patient diabetes test results chart 25mg precose amex. Sometimes the stimulus for the consultation can best be addressed by providing reassurance and confirmation. Sometimes the stimulus is an unspoken political wish to transfer the care of a burdensome patient from one physician to another. A consultant should develop an understanding of how to interact with other clinicians under such ambiguous circumstances. Requests for consultation often arrive outside conventional working hours, are usually tinged with a sense of urgency, and sometimes cluster to encompass more than one patient. Developing an effective method for prioritizing patients is a crucial clinical skill. One communication strategy is to provide an objective estimated time of arrival for the initial request from the surgical team. Postoperative hypoxemia is common and persistent: a prospective blinded observational study. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. Poverty, social neglect, substandard medical care, unhealthy life habits, and complications of psychiatric treatments are major contributors to the increased morbidity and mortality of patients with chronic psychiatric disorders, who have a 20-year average decline in life expectancy. Integrated care models that coordinate general medical care with psychiatric care can help meet the needs of patients with chronic psychiatric problems. As many as 15% of patients who are admitted for psychiatric care may be transferred to a general hospital for medical conditions that arise or deteriorate during inpatient psychiatric care. Febrile illnesses, acute neurologic changes, and falls account for nearly half of the transfers (Table 406-1). Medical deterioration, which often is unexpected and severe, can have major adverse consequences. Evaluation is difficult in the context of psychotic disorders, developmental abnormalities, or dementia with behavioral disturbance, because these patients are often vague or silent about physical suffering. Obstacles to efficient decisionmaking and therapeutic interventions are common in the setting of standalone psychiatric hospitals, which may lack access to short laboratory turnaround time, advanced imaging, and consulting specialists. Psychiatric patients are also at risk of major adverse effects of psychiatric drugs. Of great concern are those that have life-threatening potential, such as delayed myocardial repolarization leading to torsades de pointes; myocarditis; pulmonary embolism and alveolitis leading to gas-exchange failure; agranulocytosis and bowel perforation followed by septic shock; seizures with post-ictal arousal failure; neuroleptic malignant syndrome with rhabomyolysis-related acute kidney injury; liver failure; severe hyponatremia; and laryngospastic dystonia producing airway obstruction. Patients treated with second generation antipsychotic drugs are prone to weight gain, metabolic syndrome, and prediabetes, which in turn increase the prevalence of type 2 diabetes mellitus and atherogenic dyslipidemia. Frequent monitoring, exercise programs, dietary interventions, and early use of metformin are considered essential for reducing the risk of cardiovascular lethal events. Renal insufficiency, anemia, poor nutritional status, and older age are also independent predictors of medical deterioration. Medical deterioration can have major adverse consequences for psychiatric inpatients. First, it may lead to life-threatening complications if the condition is not rapidly diagnosed and treated. Third, it prolongs the length of stay and can add considerable expense to the episode of psychiatric illness, especially when patients are transferred from locked psychiatric units to a general hospital, where they require constant observation by qualified personnel. Medical consultation for psychiatric patients creates unique challenges in evaluation of the chief complaint. Many patients with outpatient psychiatric disorders have somatic symptoms, such as fatigue, weakness, dizziness, headache, insomnia, widespread pain, and constipation. In most of these patients, the underlying mental illnesses are mood disorders (unipolar depression and dysthymia), anxiety disorders (panic disorder and generalized anxiety disorder), somatoform disorders, substance use disorders (most often alcohol, opiates, cocaine, and benzodiazepine), and borderline personality disorder. As a group, these patients have many physical complaints and resist a psychological explanation for their symptoms even when the medical evaluation fails to identify objective abnormalities. After careful interdisciplinary evaluations, patients whose unexplainable somatic symptoms are diagnosed as hypochondriasis may respond to treatment with fluoxetine (see Table 369-5) and cognitive-behavioral therapy. Includes neuroleptic malignant syndrome and serotonin syndrome (also see Tables 406-4 and 406-5). Patients with mania secondary to bipolar affective disorder may receive lithium, anticonvulsants (most commonly valproate), antipsychotics, and benzodiazepines. Medical consultation in psychiatry should be informed by knowledge about the serious complications of these drugs (Table 406-2). Metabolic syndrome is more prevalent (range, 29 to 63%) in schizophrenic and other psychiatric patients treated with second-generation antipsychotics, especially clozapine but also olanzapine, risperidone, and quetiapine because they induce substantial weight gain. As a result, up to 40% of patients receiving long-term treatment with antipsychotics have impaired glucose tolerance, and about 10% have diabetes. For example, in randomized trials, metformin, 850 mg twice daily, significantly reduced the weight gain and reversed the metabolic abnormalities associated with the initiation of second-generation antipsychotic drugs, A2 and a single daily dose of 750 mg may prevent weight gain if it is initiated at the onset of olanzapine treatment. Another option is to switch from olanzapine, quetiapine, or risperidone to aripiprazole, A3 which is less likely to cause weight gain. The administration of the glucagon-like peptide-1 receptor agonist liraglutide (starting with a dose of 0. In a small number of patients, a competing hypothesis proposes that clozapine induces hypereosinophilic myocarditis, colitis, hepatitis, pancreatitis, alveolitis, and interstitial nephritis. In patients in whom myocarditis develops, the mortality rate is as high as 50%, with almost half the deaths occurring suddenly and unexpectedly. The average duration of exposure to clozapine before diagnosis or death is 21 days, and the dosage range is 50 to 725 mg/day. Common symptoms are fever (48%), dyspnea (35%), influenza-like illness (30%), chest pain (22%), and fatigue (17%). Laboratory features include left ventricular hypokinesia or reduced ejection fraction (48%) or pericardial effusion (17%) on echocardiography, nonspecific repolarization abnormalities on electrocardiography (35%), peripheral eosinophilia (35%), elevated creatine kinase and troponin levels (22%), and radiographic evidence of heart failure (13%). The diagnosis can be confirmed by endomyocardial biopsy showing fraying of myocytes and perivascular infiltrates with degranulated eosinophils. Among survivors, symptoms resolve or substantially improve after discontinuation of clozapine and treatment with high-dose corticosteroids. Clozapine-induced dilated cardiomyopathy may be caused by an evolving myocarditis or by chronic injury mediated by free radicals, similar to the myocarditis produced by doxorubicin (Chapter 54). The demographic features are similar to those of myocarditis, but the mean duration of treatment before diagnosis is much longer (9 months vs. Patients have clinical or echocardiographic evidence of left ventricular dysfunction without eosinophilia or enzymatic evidence of myocardial necrosis. Antipsychotics affect the cardiac potassium channel by blocking the rapidly activating component of the rectifier potassium current (Chapter 55). This effect translates into a dose-dependent increase in the duration of phase 3 of the action potential. Compared with nonusers of antipsychotic drugs, the risk for sudden death is twice as high for current users of conventional (first-generation) antipsychotics and is 2. A baseline electrocardiogram and serum electrolyte values should be obtained before starting of antipsychotic drug therapy, tricyclic antidepressants, and methadone. Half the psychiatric patients with dysphagia have a fast-eating syndrome seen in association with restlessness, poor chewing skills, food pocketing in the cheeks, and attention deficits that characterize psychotic disorders and mental retardation. Bradykinetic dysphagia, which is seen in 25% of psychiatric patients with choking episodes, is due to the antidopaminergic and anticholinergic effects of psychotropic medications. This condition, which features reduced lingual range of motion, increased oral transit time, decreased pharyngeal peristalsis, and delayed initiation of the swallowing reflex, is seen in patients with neurologic features of drug-induced parkinsonism (Chapter 381). Dyskinetic dysphagia (7% of choking cases), which generally occurs in patients maintained with long-term antipsychotic medication, is part of the clinical spectrum of tardive dyskinesia (Chapter 382). The examination reveals involuntary contractions of the tongue and perioral musculature, clumsiness of voluntary movements of the tongue, and discontinuous bolus propulsion in the oral stage. In the remaining patients, the dysphagia is due to cerebrovascular disease (11%) or to pharyngeal or esophageal disease (7%). Laryngeal dystonia, which is a life-threatening complication of antipsychotic drug therapy, primarily with haloperidol and phenothiazines, is produced by acute spasmodic contraction of the adductor laryngeal muscles. Patients typically indicate extreme subjective distress by clutching their anterior cervical area. Most patients also have other dystonias involving the head and neck, including torticollis, retrocollis, trismus, tongue protrusion, and deviation of the eyes (up, down, or sideward).
Cheap 50mg precose with visa
A definite diagnosis of multiple sclerosis can be made in which of the following clinically isolated syndromes in which no better explanation can be found: A diabetes type 2 disability 50mg precose amex. The inflammatory process extends throughout the subarachnoid space around the brain and spinal cord and involves the ventricles. Proper diagnosis is dependent not only on detection of the offending organism, but also on a proper understanding of the risk factors, clinical manifestations, and laboratory findings, including the host immune response and the features on neuroimaging. In a substantial proportion of cases, the organism may be elusive and initial empirical therapy may be required. The incidence of bacterial meningitis has dropped dramatically to about one to two cases per 100,000 adults in developed countries since the introduction of vaccines against bacterial pathogens such as Haemophilus influenzae type b (Chapter 282), Streptococcus pneumoniae (Chapter 273), and Neisseria meningitidis (Chapter 314). Although all human microbes have the potential to cause meningitis, only a few organisms account for most cases of bacterial meningitis. The clinical setting in which meningitis develops may provide a clue to the specific bacterial cause. In developed countries, Listeria monocytogenes (Chapter 277) is emerging as the most common cause of bacterial meningitis, with peak frequencies in the neonatal period and in persons older than 60 years of age. Simultaneous mixed bacterial meningitis is rare but may occur after neurosurgical procedures, penetrating head injury, head trauma with fracture of the cribriform plate, erosion of the skull or vertebrae by adjacent neoplasm, extension of osteomyelitis, or intraventricular rupture of a cerebral abscess. Isolation of anaerobes should strongly suggest the latter two of these situations. In approximately 10% of patients with pyogenic meningitis, the bacterial cause cannot be defined. Over the past several decades, gram-negative bacillary meningitis has doubled in frequency in adults, a change reflecting more frequent and extensive neurosurgical procedures, as well as other nosocomial factors. Listeria infections are most often food-borne via dairy products, processed meats, uncooked vegetables, and precut salads. Although Listeria meningitis may occur in immunocompetent individuals, it occurs most frequently in individuals who are immunocompromised owing to organ transplantation, hemodialysis, corticosteroid therapy, cytotoxic drugs for treatment of cancer or autoimmune diseases, liver disease, alcoholism, uncontrolled diabetes, and pregnancy. Meningitis caused by coagulase-negative staphylococci, which represents approximately 3% of cases in large urban hospitals, occurs as a complication of neurosurgical procedures and is often caused by methicillin-resistant strains. In large tertiary care hospitals, approximately 40% of cases of bacterial meningitis in adults are of nosocomial origin. Meningococcal disease, including meningitis, may occur sporadically and in cyclic outbreaks. High-risk groups include individuals who live in close quarters such as crowded classrooms, college dormitories, military barracks, or jails. With the introduction of the meningococcal vaccine, the incidence meningococcal meningitis has decreased drastically, although vaccinated populations remain vulnerable to the serotypes that are not covered by the vaccine. The incidence of meningococcal meningitis was probably underestimated historically when the diagnosis was based on isolation of the organism. Predisposing factors for the development of pneumococcal meningitis include acute otitis media (Chapters 273 and 398), with or without mastoiditis, in approximately 20% of adult patients. Pneumonia is present in approximately 15% of patients with pneumococcal meningitis, a much higher frequency than in meningitis caused by H. Acute pneumococcal sinusitis (Chapter 398) is occasionally the initial focus from which infection spreads to the meninges. Cochlear implants, particularly those that include a positioner, have been implicated in childhood bacterial meningitis caused by S. Alcoholism (Chapter 30) is an underlying risk factor in 10 to 25% of adults with pneumococcal meningitis in urban hospitals. Meningitis caused by gram-negative bacilli takes one of three forms: neonatal meningitis, meningitis after trauma or neurosurgery, or spontaneous meningitis in adults. Meningitis caused by group A streptococci is uncommon but occasionally occurs after acute otitis media, more often in children than in adults. On gross examination, purulent exudate in the subarachnoid space is most abundant in the cisterns at the base of the brain and over the convexities of the rolandic and sylvian sulci, which are expansions of the subarachnoid space. Although neither the infecting organism nor the inflammatory exudate directly invades cerebral tissue, the subjacent brain becomes congested and edematous. The pial barrier generally prevents bacterial meningitis from causing a cerebral abscess; when these two processes coexist, the sequence is usually that an initial abscess leaks its contents into the ventricular system and produces secondary ventriculitis and meningitis. The inflammatory exudate can extend around the perivascular spaces to adjacent structures, especially the arteries and veins that carry a layer of pia mater and arachnoid membrane as they enter the brain from the cortical surface. Cortical thrombophlebitis results from venous stasis and adjacent meningeal inflammation. Involvement of cortical and pial arteries by peripheral aneurysm formation and vascular occlusion or narrowing (related to spasm, arteritis, or both) of the supraclinoid portion of the internal carotid artery at the base of the brain occurs in approximately 15% of patients with meningitis. The anterior and middle cerebral arteries may have markedly increased intracerebral blood flow velocity (an index of stenosis or arterial spasm) on transcranial Doppler ultrasonography, a finding corresponding to focal cerebral signs. In fulminating cases, particularly meningococcal meningitis, cerebral edema may be marked even though the pleocytosis is only moderate. Rarely, temporal lobe herniation through the tentorium develops in such patients and compresses the midbrain, thereby leading to ipsilateral third nerve palsy and contralateral hemiparesis; or cerebellar herniation through the foramen magnum with compression of the medulla, which results in apnea, hemodynamic instability, and coma. Damage to cranial nerves occurs in areas where dense exudate accumulates around the nerves; the third and sixth cranial nerves are also vulnerable to damage by increased intracranial pressure. Ventriculitis accompanies most cases of bacterial meningitis and may rarely progress to ventricular empyema. Obstruction of the foramina of Magendie and Luschka at the base of the fourth ventricle results in noncommunicating or obstructive hydrocephalus, whereas obstruction at the level of the arachnoid granulations in the venous sinuses results in communicating hydrocephalus. Patients with neutropenia are at higher risk for meningitis with Pseudomonas aeruginosa and members of the Enterobacteriaceae family. Bacteremia is usually initiated by pharyngeal adhesion and colonization by an infecting strain. Meningococci invade the nasopharyngeal mucosal cells by means of endocytosis and are transported to the abluminal side in membrane-bound vacuoles. When these meningeal pathogens gain access to the blood stream, their intravascular survival is aided by the presence of polysaccharide capsules that inhibit phagocytosis and confer resistance to complement-mediated bactericidal activity. Once established in any part of the meninges, infection quickly extends throughout the subarachnoid space. Bacterial meningitis following head trauma occurs because of a dural fistula from the nasal cavity, paranasal sinuses, or middle ear to the subarachnoid space. The most frequent site is at the cribriform plate, where the bone is thin and the dura is tightly adherent to the bone. Cytokines appear to enhance the passage of leukocytes by inducing several families of adhesion molecules that interact with the corresponding receptors on leukocytes. Cytokines also can increase the binding affinity of a leukocyte selectin, leukocyte adhesion molecule, for its endothelial cell receptor and may thereby further contribute to trafficking of neutrophils into the subarachnoid space. In bacterial meningitis, neutrophils move into the subarachnoid space but are not able to control the bacterial infection because their phagocytic properties are inefficient as a result of a lack of opsonic and bactericidal activity. Within the subarachnoid space, neutrophils release prostaglandins, matrix metalloproteinases, and free radicals that disrupt the endothelial intercellular tight junctions and the subendothelial basal lamina. Cerebral blood flow, which depends on mean arterial pressure, is increased in the early stages of meningitis, but it subsequently decreases, substantially in some patients, which may cause ischemic neurologic injury. Localized regions of marked hypoperfusion, attributable to focal vascular inflammation or thrombosis, can occur in patients with normal blood flow. Impairment of cerebral blood flow autoregulation, as measured by transcranial Doppler ultrasonography of the middle cerebral artery, occurs early in acute bacterial meningitis and causes cerebral blood flow to correspond directly to mean arterial blood pressure, with attendant hyperperfusion or hypoperfusion of the brain. On recovery, the ability of the cerebral vasculature to maintain a constant level of perfusion despite variations in mean arterial pressure is restored. Most patients with communityacquired pyogenic meningitis have had an antecedent or accompanying upper respiratory tract infection or nonspecific febrile illness, acute otitis (or mastoiditis), or pneumonia. Myalgia, particularly in patients with meningococcal disease, backache, and generalized weakness are common symptoms. The illness usually progresses rapidly, with the development of confusion, obtundation, and loss of consciousness. Occasionally, the onset may be less acute, with meningeal signs being present for several days to a week. General Physical Findings Evidence of meningeal irritation is usually present, as evidenced by a stiff neck, Kernig sign (inability to straighten the leg when the hip is flexed to 90 degrees), and Brudzinski sign (involuntary flexion of the hip and knee when the neck is passively flexed). Patients with defective humoral immunity and an inadequate antibody response are particularly vulnerable to meningitis with S. For example, deficiencies in the complement system predispose patients to *Data from 696 cases reported in van de Beek D, de Gans J, Spanjaard L, et al. The study included 671 patients who had a total of 696 episodes of community-acquired meningitis.
Order precose with mastercard
Treatment is surgical excision diabetes test levels buy precose 50mg with amex, often with the Mohs micrographic surgical technique. Except in rare circumstances, such as in immunosuppressed patients or patients with xeroderma pigmentosa, the prognosis is excellent. Paradoxically, decreased tearing can result in irritation and secondary increased (reflux) tearing. Most daily tear production is not by the lacrimal gland but by small collections of lacrimal glands, mucus-producing glands, and sebaceous glands located throughout the conjunctiva, eyelid, and anterior orbital soft tissue. Because tear film production is lower during sleep, patients often note symptoms on awakening followed by slow resolution over minutes or hours. Wind and lowhumidity environments, such as in commercial airliners, can exacerbate symptoms. The reduction in aqueous components of tears is often associated with a compensatory increase in mucus production, which tends to blur vision until the patient blinks or uses supplemental tears. Hyphema, which is a sign of serious ocular damage, may lead to secondary glaucoma and blood staining of the cornea. The most common site of rupture of a globe is at the limbus (junction of cornea and sclera), where a pigmented mass may be noted. The mass may be either a blood clot or an anteriorly displaced uveal tract (usually iris). Any manipulation of the globe may force the remaining intraocular tissue through the wound and may make the injury irreparable. Cataract and retinal detachment are not common except in severe accidental trauma. A unilateral cataract or unilateral glaucoma may occur decades after the injury, even when an injury is too minor to be recalled. Severe cases may require surgical debulking of the infection (vitrectomy) to reduce the microbial and inflammatory debris burden and to treat associated vitreoretinal pathology. Inflammation of any part or parts of the uveal tract (iris, ciliary body, and choroid) may be called anterior or posterior uveitis, iritis, iridocyclitis, or choroiditis. The inflammation may be acute or chronic, and an underlying systemic cause is found in approximately 50% of cases. Uveitis accompanies many autoimmune diseases, often without correlation to the activity of the systemic inflammation. Anterior uveitis or conjunctivitis is nearly universal in patients with reactive arthritis (Chapter 249). About 25% of patients with ankylosing spondylitis (Chapter 249) develop acute, recurrent anterior uveitis. Two to 12% of patients with inflammatory bowel disease (Chapter 132) develop anterior uveitis, which is also common with psoriatic arthritis but not with psoriasis alone (Chapters 249 and 409). Most cases of endophthalmitis involve a breach in the eye wall (cornea and sclera), associated with either accidental trauma (incidence of approximately 5%) or surgical procedures (incidence of approximately <0. The initial sign is often evidence of inflammatory cells either within the aqueous (anterior uveitis) or within the vitreous (vitritis). Common microbial organisms include toxin-producing grampositive species and gram-negative species that are often associated with rapidly destructive course. Other organism of relatively low virulence, Propionibacterium acnes and Staphylococcus epidermidis, follow a more indolent course with less potential destruction. Metastatic endophthalmitis infection from a primary source outside of the eye is an unusual cause. Diagnosis is established by sampling anterior chamber fluid or preferably vitreous fluid (vitreous tap) and evaluation of that fluid by Gram stain and culture. Prophylaxis against endophthalmitis includes preoperative topical instillation of povidone-iodine and intracameral antibiotic injection at the end of cataract surgery. The orbital septum divides the soft tissues of the eyelid from the soft tissues of the orbit. Orbital tissue is more susceptible to damage by the inflammation than is the preseptal tissue. The clinical signs of preseptal cellulitis include soft tissue swelling, hyperemia, and conjunctival chemosis (edema). Extension of inflammation posterior to the orbital septum is indicated by proptosis of the globe and ophthalmoplegia (restricted motion). Preseptal cellulitis, commonly resulting from minor penetrating trauma, may evolve into an abscess. Diffuse injection of the conjunctiva with a watery discharge is evident in this case of viral conjunctivitis. Viral conjunctivitis produces watery discharge, foreign body sensation, preauricular lymphadenopathy, and conjunctival follicles seen on slit lamp examination. Herpes simplex corneal epithelial keratitis in diffuse light and in light passed through a cobalt blue filter after fluorescein staining (inset). Treatment of orbital cellulitis, which can lead to septic optic neuritis, intracranial spread, and cavernous sinus thrombosis, may require intravenous antibiotics and surgical drainage of a paraorbital abscess. Initially, the main signs of primary herpes simplex keratitis are a red eye and a corneal epithelial dendritic ulcer. Herpes simplex keratitis can recur and may extend into the corneal stroma and cause a red eye, ocular discomfort, blurred vision, and corneal scarring. The condition is highly contagious through direct contact or inhalation of respiratory particles. After an incubation period of 3 to 7 days, the patient presents with red eyes (Table 395-4), itching, burning, foreign body sensation, and often a discharge, which persist for 5 to 15 days. Preauricular lymphadenopathy may be present, and a history of upper respiratory tract infection is common. Bacterial Conjunctivitis Fewer than 5% of cases of conjunctivitis are caused by bacteria, mostly Staphylococcus, Haemophilus, or Streptococcus species. Bacterial conjunctivitis responds to broadspectrum antibiotic solutions or ointments. Herpes Zoster Ophthalmicus Herpes zoster ophthalmicus (shingles, Chapter 351) has a propensity to involve one or more branches of the trigeminal nerve. The virus also can affect the uveal tract and, in immunosuppressed patients, the retina. When the trigeminal nerve is involved, spread to the inside of the eye (uveitis) is most likely if vesicles are present in the inner corner of the eyelids or on the nose, especially the tip of the nose (Hutchinson sign). If the uvea is not involved, the skin lesions heal with some scarring but no long-term effects. In patients with moderate to severe skin involvement, treatment can be started with oral acyclovir (800 mg orally five times per day for 7 to 10 days) or valacyclovir (1 g three times a day for 10 to 14 days). Like herpes simplex virus, herpes zoster can affect the cornea and patients should be monitored for recurrent disease. Chlamydial Conjunctivitis Adult inclusion conjunctivitis is a chronic conjunctivitis caused by sexual transmission of Chlamydia trachomatis (Chapter 302). Oral erythromycin (500 mg orally, four times daily for 7 days) or azithromycin (1 g orally twice daily for 7 days) is required. It causes an entropion, inversion of the eyelashes (trichiasis), corneal vascularization, and opacification. Topical erythromycin or tetracycline, twice daily for 3 to 4 weeks, can be effective, but surgical epilation or eyelid reconstruction may be required. Pseudomonal and Gonococcal Keratitis Keratitis, which is inflammation of the corneal stroma, can be caused by spread of pathogens internally from a corneal ulcer. Small yellow choroidal lesions may be seen, and retinal periphlebitis may occur secondarily. To avoid intraocular spread, urgent and aggressive antibiotic treatment is necessary. Another gram-negative cause of a virulent keratitis is Neisseria gonorrhoeae (Chapter 282), especially in neonates. Corneal infection is accompanied by copious tearing and a characteristic hyperpurulent discharge. Prompt treatment with topical irrigation (normal saline to remove mucopurulent material) and penicillin G (100,000 units/kg/day given intravenously in four divided doses for 7 days) is essential to prevent corneal perforation. In tertiary syphilis, the miotic Argyll Robertson pupil reacts poorly to light but briskly to accommodation. The presumptive diagnosis is made on the characteristic intense, retinal, wedgeshaped reaction, with considerable exudates and hemorrhages, giving the terms "pizza pie retinitis" and "hemorrhagic cottage cheese retinitis" to the entity. Treatment is with antiviral drugs: ganciclovir (5 mg/kg intravenously twice daily, two to three times per week), foscarnet (90 mg/kg intravenously twice daily, twice per week), or cidofovir (5 mg/kg intravenously, weekly for 3 weeks) with follow-up maintenance.
Poison Flag (Orris). Precose.
- Dosing considerations for Orris.
- Are there safety concerns?
- How does Orris work?
- What is Orris?
- Purifying blood, skin diseases, bronchitis, cancer, improving appetite and digestion, inflammation of the spleen, liver and kidney problems, vomiting, constipation, bad breath, teething pain, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96636
50 mg precose sale
Deep brain stimulation of the internal segment of the globus pallidus diabetic toes purchase 50mg precose with mastercard, thalamus, and the subthalamic nucleus,14 can be considered in medically refractory, disabling dystonia, especially in patients with idiopathic dystonia. Transient tics are extremely common in childhood, and simple tics may begin in childhood and persist throughout adult life. Secondary tics are caused by a defined underlying brain disease or environmental factor. The tics of Tourette syndrome are now classified as a neurodevelopmental disorder. Tics vary in terms of complexity, from abrupt, brief, meaningless movements or sounds (simple motor tics such as eye blinking, nose wrinkling, or head jerking; simple vocal-phonic tics such as sniffing, throat clearing, or grunting) to more sustained, more deliberate, almost meaningful gestures or utterances (complex motor tics such as touching, hand shaking, and jumping; complex vocal tics such as echolalia [repeating others], palilalia [repeating oneself], and coprolalia [uttering profanities]). The frequency of the tics in an individual patient varies markedly over minutes, hours, days, weeks, and years. Tics are often described by patients as being "semivoluntary" in response to an inner, irresistible urge. Premonitory sensory symptoms occasionally precede the tic, usually in the same general anatomic area as the tic itself. Tics can be partially or completely voluntarily suppressed for variable periods, but often at the expense of mounting inner tension and psychological discomfort. Performing the tic or sometimes even substituting another more acceptable behavior for the socially inappropriate tic alleviates the tension. There is a male preponderance of 3: 1 for the classic syndrome, but female patients manifest obsessivecompulsive features more often than tics. Involuntary swearing (coprolalia), a highly publicized feature of the syndrome, is present in fewer than 10% of patients. When tics (isolated or as part of Tourette syndrome) interfere with social and physical function, low-dose clonazepam (0. The most effective treatments for disabling tics are the dopamine receptor blockers such as risperidone (0. An alternative without this complication is the dopamine depleter tetrabenazine (50 to 200 mg/day). Injected botulinum toxin may be effective for simple motor tics of the face and neck and may also reduce the urge to perform the tic. More aggressive use of botulinum toxin in neck muscles should be considered in patients with very forceful neck tics, which have rarely been associated with complications such as noncompressive myelopathy and vertebral artery dissection. Obsessive-compulsive symptoms may respond well to selective serotonin reuptake inhibitors. Behavioral disorders, which remain a major therapeutic challenge, may require a variety of psychotherapeutic or behavioral modification approaches. Even in the absence of behavioral disturbances, comprehensive behavioral intervention therapy, which incorporates habit reversal training, can be very effective as first-line therapy for tic disorders. Promising preliminary reports of deep brain stimulation require confirmation in controlled clinical trials. The distribution of myoclonus may be focal, segmental, multifocal, or generalized. When myoclonus involves more than one body area, the movements may be synchronous or asynchronous. Palatal myoclonus, now referred to as palatal tremor, is a rhythmic movement disorder originating in the brainstem and involving the soft palate as well as the eyes, facial muscles, neck, and limbs; it is commonly the result of a focal lesion. Myoclonus can be classified according to the anatomic site of origin, usually with the assistance of detailed electrophysiologic assessments. Drug treatment includes a variety of anticonvulsant medications, most notably clonazepam (1. Postanoxic action myoclonus (the Lance-Adams syndrome) in some patients who survive severe cerebral anoxia also may respond to 5-hydroxytryptophan (400 to 2800 mg/day) given with carbidopa (75 to 300 mg/day). Acetazolamide (250 to 1000 mg/day) may be useful for patients with action myoclonus. Zonisamide (300 mg/day) improves myoclonus and related disability in patients with myoclonus-dystonia. A5 the natural history of Tourette syndrome is to stabilize and in the majority of cases to improve in adolescence. Myoclonus generally arises in the central nervous system, although rare peripheral causes are described, and it is distinct from abnormal muscle activity associated with peripheral nervous system diseases, such as fasciculations or myokymia. Myoclonus can be classified according to origin (E-Table 382-1), including physiologic, essential, epileptic, and symptomatic forms. Physiologic myoclonus, such as hypnic (sleep) jerks and hiccups, occurs in normal healthy subjects. Patients with essential myoclonus, which may be sporadic or inherited, often have additional postural tremor or dystonia, and this disorder is probably the same as what is now referred to as myoclonus dystonia (see Dystonias, earlier). Epileptic myoclonus arises in the context of seizures (Chapter 375), including many inherited generalized epileptic syndromes and the progressive myoclonic epilepsies. Symptomatic myoclonus occurs in association with a large number of encephalopathic states. Myoclonic jerks are very short, typically persisting for less than 100 msec, although occasional patients have longer muscle bursts. Myoclonus can be spontaneous, action induced, reflex (induced by various sensory stimuli), or a combination. Action myoclonus occurs during purposeful movement and is often very disabling owing to its interference with volitional activity. Some patients demonstrate only generalized body jerking or an exaggerated startle response that habituates poorly after repeated stimuli. By comparison, other patients experience disabling stiffness in response to sudden unexpected stimuli, such as a loud sound. Additional medications that have been tried with mixed results include clobazam, levetiracetam, valproic acid, and phenobarbital. Neuroleptic drugs, which block postsynaptic dopamine receptors, particularly the D2 subtype, can result in a variety of movement disorder syndromes, including acute dystonic reactions, akathisia, drug-induced parkinsonism (including the "rabbit syndrome" with perinasal and perioral rest tremor), the neuroleptic malignant syndrome, and a variety of later-onset, often persistent, movements referred to as tardive dyskinesia. Metronidazole also rarely can cause an encephalopathy that typically manifests as dysarthria and gait instability. Acute dystonic reactions (Chapter 406) are most often seen in young patients who are receiving potent antipsychotic agents. Symptoms range from overt dystonic postures of the face and neck, to involuntary prolonged deviation of the eyes (oculogyric crises), to simple slurring of speech and difficulty coordinating the tongue. Symptoms often vary from moment to moment and can increase with anxiety and improve with relaxation or reassurance. Other drugs that possibly provide benefit include amantadine, propranolol, zolpidem, ginkgo biloba, and clonazepam. Consideration should be given to discontinuing concurrent anticholinergic medications. The physician must regularly reassess the need for ongoing neuroleptic therapy, consider switching to an atypical agent when possible (particularly quetiapine and clozapine; Chapter 369), and routinely evaluate the patient for the presence of early subtle clinical features, such as mild pursing of the lips or rolling movements of the tongue in the mouth. Unfortunately, tardive dyskinesia may persist for many years despite withdrawal of neuroleptic treatment in up to 50% of patients. Several atypical neuroleptics, such as risperidone and olanzapine, nevertheless block dopamine D2 receptors sufficiently to cause drug-induced parkinsonism and tardive dyskinesias. Typically, the patient performs a variety of purposeful or semipurposeful, often complex, movements in response to an uncomfortable subjective restlessness, including pacing when standing, marching in place, rocking, shifting weight, moving legs when sitting, picking at clothing or hair, rubbing body parts with hands, and other similar movements. Akathisia is most often a side effect of medications, especially neuroleptic drugs and selective serotonin reuptake inhibitors (Chapter 369). Akathisia is a common reason for psychiatric patients to comply poorly with their medications; management includes adjustment of the dose or type of antipsychotic agent and trials of -blockers. Rare patients experience a very disabling and persistent form referred to as tardive akathisia. The neuroleptic malignant syndrome (Chapters 404 and 406) is an uncommon but severe, sometimes fatal, complication of neuroleptic therapy. Patients usually manifest a combination of features including fever, marked rigidity, changes in level of arousal, and autonomic instability. Laboratory abnormalities include a marked increase in the serum creatine kinase level and the blood leukocyte count.
Discount precose 50 mg
The written report and verbal communications should be comprehensive and commonly include more basic medical content and specific recommendations than may be typical of a consultation for a medical subspecialist diabetes symptoms at 30 order precose line. Subspecialty consultations requested by primary care physicians may be for advice, a technical procedure, or ongoing comanagement (Table 402-3). Consultations for general practitioners or family physicians generally follow the same guidelines as those for general internists. However, because both the training and ongoing practices of such physicians may or may not include the same spectrum and complexity of disease encountered by typical general internists, the subspecialty consultant must use judgment regarding both the initial consultation and the advisability of ongoing comanagement. It is critical that requesting and consulting physicians agree about the reason for the consultative request. Effective communication at the time of the request will improve the value of the consultation and clarify the question. When there is doubt regarding the reason for the consultation, the consultant should speak directly to the referring physician before completing and documenting the evaluation of the patient. Common reasons for medical consultation include assessment of perioperative risk; interpretation of a laboratory abnormality; help in performing a procedure, in obtaining advice, or in selecting therapy; and aid in providing long-term care. Prophylactic strategies (venous thromboembolism, endocarditis, and surgical site infection) infrequently generate requests for medical consultation because they are commonly standardized to conform to practice guidelines at individual institutions. Adherence by the requesting physician to any of the recommendations made by the consultant is higher for consultations with fewer recommendations. Another strategy to minimize the number of recommendations is to restrict advice to pertinent issues at the time, preferably in order of their importance. Requesting physicians are also more likely to adhere to recommendations when the patient is sicker, when the consultation is performed promptly, when advice is given to institute specific therapy rather than perform more diagnostic testing, when the consultant writes frequent follow-up notes, and when computerized order entry support systems are used to convey recommendations. When giving advice about medications, consultants should indicate specific doses and duration of treatment. When consulting for psychiatrists or in the peripartum period, the consultant requires special expertise to understand the different expressions of signs and symptoms in specific populations, as well as how and when to modify typical medical recommendations because of special circumstances (Chapters 226 and 406). Although these consultations occasionally result in long-term comanagement, more commonly they revolve around the resolution of an isolated problem. Although requesting physicians may perceive reduced medicolegal risk when they obtain and even document a curbside consultation, consultants may fear the risk for malpractice liability themselves when offering such advice. However, courts have consistently found that curbside consultants have no liability because no direct physician-patient relationship exists. Rather, the relationship is only between the requesting and consulting physicians. Increasingly, physicians are using electronic communication, either as part of a shared electronic medical record or by e-mail, to supplement formal consultation requests. An obvious advantage of this approach is that the requesting and consulting physician can communicate on their own schedules. Potential benefits include saving time, reducing costs, and improving continuity and access to specialty care. However, the lack of reimbursement for such activities may be a barrier to e-consultations. For example, mandatory inpatient infectious disease consultations, as part of an antimicrobial stewardship program, can improve the rational use of antimicrobial agents in the hospital and after discharge. Similarly, instituting routine consultation for patients with certain sentinel conditions, such as diabetes, may improve outcomes. A consultation that begins with an initial encounter or a limited number of follow-up visits may evolve into ongoing comanagement. In such an arrangement, the physician initially serving in a consultative role becomes at least coequal to the requesting physician in the provision of ongoing care. This arrangement is obvious in situations in which the consultation was requested specifically for the provision of ongoing care. Other examples include situations in which an oncologist assumes principal care of a patient with a malignancy or a nephrologist assumes principal care of a patient with end-stage renal disease who is being maintained on dialysis. In some of these situations, a general internist who initially requested the consultation may now become the consultant and provide advice on preventive care and occasional help with intercurrent medical problems. Medical consultants may become comanagers of postoperative surgical patients, with a potential for improving outcomes. In an early randomized trial of perioperative patients, formal comanagement, in which a medical physician took responsibility for managing medical problems rather than acting in a consultative role, reduced postoperative complications; in addition, both nurses and surgeons preferred this model. In one study of comanagement on a neurosurgical service, for example, nursing staff perceived substantial improvement in the quality of patient care, and costs were reduced, but there were no differences in mortality, readmission rates, or length of stay. In some institutions, comanagement for orthopedic or other surgical patients has become routine and does not require a specific request for consultation. Internists currently comanage more than one third of surgical inpatients in some hospitals. The consultant is responsible to two parties: the patient and the referring physician. The consultant should not limit communication to the referring physician and must not withhold discussion and recommendations from the patient. However, the consultant should not usurp the role of the referring physician, who remains responsible for assembling information and advice from varied sources, as well as for developing an integrated plan with the patient. For example, in the preoperative setting, the consultant should not express a final opinion regarding the suitability of proceeding to surgery without first discussing all relevant considerations with the referring surgeon. Understand the urgency of the consultation so that the consultation will be performed on a timely basis that meets the needs of the requesting physician and patient. Perform a focused but careful history and physical examination-do not rely on information gathered by others. Do not rehash information in an overly detailed note-emphasize the key issues your evaluation reinforced or discovered. Be sure your recommendations are clearly listed and appropriately detailed-for example, indicate specific drugs, doses, and durations. Indicate how to monitor the effectiveness of your recommendations, as well as how to contact you urgently if problems arise. Remember that personal contact with the requesting physician, even if very brief, may be far more helpful than the best of written notes. Do not disappear-follow the patient as frequently as appropriate, in coordination with the requesting physician. Electronic Consultations Mandatory Consultations Comanagement consultation request were to frame the question, to indicate clearly whom to call with the response, and to establish urgency. Consultants should be careful to restrict their advice to their particular area of expertise. For example, unless a particular antipsychotic medication is contraindicated because of a medical issue (Chapter 406), it is wisest to defer decision making regarding psychiatric management to the psychiatrist. The most important attributes of a consultative role are simple, concise recommendations and a clearly stated rationale for decision making. Detailed differential diagnosis is less important, and literature support is usually unnecessary. For example, primary care physicians note that failure to receive timely reports from consultants limits their ability to provide high-quality care. These recommendations serve as a helpful guide for consultants to improve adherence to their advice and, as a result, improve patient outcomes. Specific interactive training on the principles of consultation can increase the effectiveness of consultative communication. In the current era, ready access to online medical references may potentially reduce curbside requests. Consultants in "cognitive" specialties such as infectious diseases, rheumatology, and endocrinology provide a disproportionate amount of informal (compared with formal) consultations. Both generalists and specialists participate in an average of three to four curbside consultations per week. These consultations commonly involve questions about diagnostic tests, treatment plans, and the potential value of a formal consultation (which follows about one third of curbside consultations) in the future. To be effective, curbside consultations should be brief, involve a single question, and require no direct examination of the patient or medical records. An important limitation of curbside consultations is that the consultant must rely on limited, secondhand information from the requesting physician rather than primary data from direct evaluation of the patient. Consultants report that such indirect information is inaccurate in as many as half of curbside consultations.
Generic 25mg precose mastercard
Oscillopsia diabetic menu buy generic precose, the sensation that the environment is moving when it actually is not, is another symptom of impaired cerebellar coordination of the eyes. Myokymia (wormlike muscle movements) under the skin, especially around the face, however, is fairly common. There is also increased incidence of bipolar disease, which may manifest after treatment of depression or treatment with corticosteroids. Pseudobulbar affect, either pathologic laughing or crying, is seen in patients with more advanced disease. Most patients do not progress to dementia (Chapter 374), but cognitive and behavioral impairments are major causes of losing employment and marital discord. Organ Dysfunction Bladder symptoms are extremely common, but often are not volunteered, so specific questions must be asked concerning urinary frequency, urgency, incontinence, or retention. Careful discrimination of a spastic bladder (detrusor muscle spasm) causing incontinence from an atonic bladder or spasm of the external sphincter (the latter two causing retention) leading to overflow incontinence is critical to designing treatment (Chapter 23). Bowel dysfunction commonly manifests as constipation (Chapter 127), which may be primary (related to spinal cord involvement) or secondary (related to self-induced dehydration to manage urinary frequency or to side effects of anticholinergic drugs). Bowel incontinence secondary to an incompetent anal sphincter is less common and most often occurs as an isolated episode of fecal urgency, sometimes related to dietary change or diarrheal illness, or as a sequela of prolonged compaction. In women and men, loss of libido and inability to achieve orgasm can occur as a result of medication, loss of sensation, heatinduced worsening of symptoms, physical barriers to intercourse (impaired mucosal moisture, spasticity, and pain), depression, or disorders of body image. The lesion causing these symptoms is more commonly in the cervical spinal cord rather than the thoracic spinal cord, even when the first sign is partial footdrop. It is likely that axons that must conduct impulses over the longest distance (entire length of the spinal cord) from a site of inflammatory demyelination will become symptomatic before axons delivering signals to closer synapses (adjacent anterior horn cells in the cervical cord). Clinically, the weakness may be severe and may result in an obvious paralysis or be so subtle as to be undetectable. Heat-induced fatigue and weakness, as manifested by focal symptoms (slapping of a foot or dragging a leg) occurring after 15 to 20 minutes of exercise and resolving with rest, are characteristic of early demyelinating disease. The early absence of associated hyperreflexia and plantar extensor responses (Babinski sign) may make it difficult to document corticospinal tract involvement. Ataxia may occur as a result of impaired delivery of sensory information up the spinal cord or from demyelination of cerebellar pathways in the brain stem or cerebellum. Often, the two are mixed and may be confounded further by visual loss and impaired ability to compensate by fixing on the environment; this combination commonly causes dizziness in crowds, in which fixation may be further obscured. Appendicular dysmetria resulting in tremor on reaching for an object is a common cause of impaired coordination and dexterity. It may be linked to depression but often occurs independently and can be the most disabling symptom of the disease. A sleep history is important to exclude daytime fatigue resulting from disrupted sleep secondary to pain, cramps, bladder frequency, sleep apnea, periodic limb movements, depression, or disrupted sleep-wake cycles. Daytime fatigue even after a good night of sleep may occur in mid-afternoon and may be described as being "unplugged" or completely drained. Even minor elevations of the body temperature can dramatically worsen symptoms (Uhthoff phenomenon). Some patients complain of worsened symptoms in cold weather, likely related to increased dysfunction of already stiff muscles or signal blockade consistent with the known physiology of nerve conduction, which has an inverted U-shaped temperature versus conduction curve. Relapses are more frequent in the first 6 postpartum months, but no evidence indicates that pregnancy changes the natural history of the disease. Patients may have no detectable residual deficit, or they may accumulate significant permanent disability from an attack. Await further clinical attack implicating a different site Dissemination in time, demonstrated by: 1. This stage of the disease, which is characterized by at least 6 months of progressive worsening without evidence of a relapse, can be diagnosed with confidence only retrospectively. It is more common in middleaged men and typically has more involvement of the spinal cord and fewer inflammatory brain lesions. This rare form of the disease may progress to a quadriplegic, obtunded state with death as a result of intercurrent infection, aspiration, or respiratory failure from brain stem involvement. Diagnostic criteria allow for the diagnosis to be made on clinical grounds alone as long as appropriate exclusionary testing is performed (Table 383-3). Further, repeated episodes of neurologic dysfunction that could be explained based on one lesion. Axial fluid attenuation inversion recovery image of the brain from a patient with multiple sclerosis revealing classic multiple periventricular and deep white matter high-signal lesions. Lesions generally range in size from 2 mm to 2 cm; larger plaques occasionally resemble a tumor. Sagittal fluid attenuation inversion recovery image of the brain from a patient with multiple sclerosis revealing classic periventricular lesions radiating outward from the ventricles (arrows). Axial T1-weighted image after gadolinium contrast showing an actively inflamed ring-enhancing lesion (arrow) in a patient with multiple sclerosis. Sagittal T2-weighted image of the brain and cervical spine from a patient with multiple sclerosis. Axial T1-weighted image showing numerous areas of T1 low signal ("black holes"), ventricular enlargement, and diffuse atrophy. Lesions that enhance on a T1-weighted sequence usually have a concomitant lesion in the same location on a T2-weighted image. Gadolinium enhancement may be homogenous, central, or in a ring pattern; it typically persists for 2 to 8 weeks and thus may be missed on intermittent scans. In clinically isolated demyelinating syndromes (see later), the sensitivity is even lower (~50%). Evoked Potential Tests Evoked potentials (Chapter 368) may be useful in some situations to document objective evidence of slowed conduction owing to demyelination in locations different from those recognized clinically. Before considering a symptomatic therapy, the patient should be educated about the purpose of the drug and its side effect profile. On learning that these drugs have no long-term impact on disease activity, patients may elect not to use them for relief of symptoms alone. Symptomatic therapies are best started at low doses and frequently require titration to obtain the optimal balance between efficacy and side effects. Optical coherence tomography is performed with an office-based device that uses the reflection of infrared light (from an exogenous source directed through the pupil) off the back of the eye to quantify the thickness of retinal tissues, including the peripapillary retinal nerve fiber layer and macular layers. Copper deficiency can cause dorsal column pathology, neuropathy, anemia, and optic neuropathy. Vitamin D deficiency (Chapter 231), which is becoming increasingly common, can cause proximal weakness, fatigue, asthenia, bone loss, and impaired immune function. Vitamin A deficiency, although not common in industrialized countries, can cause night blindness and immune dysfunction. Spinocerebellar atrophy and hereditary myelopathy cause slowly progressive disease but do not cause sensory and visual abnormalities. In addition to appropriate supportive care and counseling, antidepressant therapy with one of the "activating" serotonergic or noradrenergic drugs (fluoxetine, sertraline, citalopram, escitalopram, venlafaxine, or bupropion) can be of benefit for depression as well as for anxiety and panic symptoms (see Table 369-5) Most patients do not seem to tolerate paroxetine well long term; fluoxetine and sertraline work for panic and anxiety. Patients with pain or insomnia may benefit more from a sedating antidepressant (amitriptyline, nortriptyline, or trazodone) given at bedtime, which may have the added anticholinergic benefits on urinary bladder urgency. Spasticity can be managed by physical therapy, stretching, and institution of either baclofen (5 to 160 mg in divided doses) or tizanidine (2 to 32 mg in divided doses). Either drug should be started as a single agent at a low dose at bedtime, gradually increasing to three to four times daily, with a larger dose at bedtime to target nocturnal symptoms. Baclofen should never be discontinued abruptly because of the potential for a severe withdrawal reaction. Bladder urgency resulting from detrusor muscle spasm can be managed effectively with anticholinergics (antimuscarinic) such as oxybutynin (5 to 20 mg in divided doses) or tolterodine (1 to 4 mg) or focal intravesicular injections of botulinum toxin, but these agents can cause temporary urinary hesitancy or retention. Bladder ultrasonography permits accurate bedside assessment of postvoid residual volume to determine whether a patient is retaining excessive amounts of urine (>50 mL is abnormal but >300 mL requires intervention). Primary urinary retention is difficult to treat with drugs, but external sphincter spasm can be treated with 1a-adrenergic receptor blockers such as tamsulosin (0. Bethanechol (10 to 150 mg in divided doses) may be tried for an atonic bladder, but intermittent catheterization is often required. Alternative causes of bladder symptoms such as urinary tract infections, prostatic enlargement, or anatomic changes following pregnancy should be considered and managed separately.
Generic 25 mg precose visa
The frequency of Yq microdeletion in azoospermic and oligospermic Iranian infertile men diabetes symptoms 2 year old buy precose 25 mg overnight delivery. An analysis of the frequency of Y-chromosome microdeletions and the determination of a threshold sperm concentration for genetic testing in infertile men. Sperm retrieval rate and reproductive outcome of infertile men with azoospermia factor c deletion. Gr/gr deletions on Y-chromosome correlate with male infertility: an original study, metaanalyses, and trial sequential analyses. Intracytoplasmic sperm injection may lead to vertical transmission, expansion, and de novo occurrence of Ychromosome microdeletions in male fetuses. Independent specialization of the human and mouse X chromosomes for the male germ line. Spinal and bulbar muscular atrophy: a trinucleotide-repeat expansion neurodegenerative disease. Long polyglutamine tracts in the androgen receptor are associated with reduced trans-activation, impaired sperm production, and male infertility. Highly parallel genome-wide expression profiling of individual cells using nanoliter droplets. Environmentally induced epigenetic transgenerational inheritance of phenotype and disease. Water and soil pollution determinant of water and food quality/contamination and its impact on male fertility. Human exposure to endocrine disrupting chemicals: effects on the male and female reproductive systems. Epigenetics in male reproduction: effect of paternal diet on sperm quality and offspring health. Environmental epigenetic transgenerational inheritance and somatic epigenetic mitotic stability. Environmentally induced epigenetic transgenerational inheritance of reproductive disease. Parental occupational exposure to exhausts, solvents, glues and paints, and risk of childhood leukemia. The carboxylterminal domain of the mammalian enzymes is related to bacterial restriction methyltransferases. Assessing loss of imprint methylation in sperm from subfertile men using novel methylation polymerase chain reaction Luminex analysis. Histone modification signatures in human sperm distinguish clinical abnormalities. Temporal trends in sperm count: a systematic review [97] [98] [99] [100] [101] [102] [103] [104] [105] [106] [107] [108] [109] [110] [111] B. Paternal smoking and risk of childhood acute lymphoblastic leukemia: systematic review and meta-analysis. Change in paternal grandmothers early food supply influenced cardiovascular mortality of the female grandchildren. National Center for Health Statistics: Health, United States, 2008, with chartbook. High-fat diet reprograms the epigenome of rat spermatozoa and transgenerationally affects metabolism of the offspring. Differential methylation in inflammation and type 2 diabetes genes in siblings born before and after maternal bariatric surgery. Placental imprinting variation associated with assisted reproductive technologies and subfertility. Abnormal methylation of imprinted genes in human sperm is associated with oligozoospermia. Infertility diagnosis has a significant impact on the transcriptoms of developing blastocysts. Role of oxidative stress in male reproductive dysfunctions with reference to phthalate compounds. Methylation changes in mature sperm deoxyribonucleic acid from oligozoospermic men: assessment of genetic variants and assisted reproductive technology outcome. They are key regulators of several critical cellular processes, such as the buffering of cytosolic calcium, apoptosis via the mitochondrial permeability transition pore, and other signaling pathways [1]. Mitochondria originated from bacteria which were endosymbionts in the eukaryotic cell [5]. The mitochondrial genome consists of different polymorphic variant combinations, which are associated with populations from specific regions or continents. Mitochondrial genetics processes such as spermatogenesis [11], the incidence of meiotic chromosome errors during oogenesis [12], and predisposition to ageassociated disorders [1]. The generation of mitochondrial energy is necessary to support a multitude of cellular processes, including several associated with reproduction and embryogenesis. This article covers different aspects related to mitochondrial genetics during gametogenesis and preimplantation embryo development. Mitochondrial inheritance and replication Mitochondria and their genome have a nonMendelian pattern of inheritance, and they are passed from a mother to her children [13]. The likelihood of clinically significant heteroplasmy being present through generations is reduced by a mechanism known as the genetic bottleneck [14]. It is thought that the genetic bottleneck takes place toward the end of oogenesis, and can be influenced by different mutations [15]. Sperm mitochondria enter the oocyte after fertilization, but are lost during early embryogenesis through a ubiquitination and autophagy process ([16,17]). There have been some recent reports of paternally derived mitochondria persisting in individuals of some families [20], however, such cases are rare. It should be noted that the timing of the mitochondrial genome replication differs from that of the actual organelle. The processes of fusion and fission are critical for correct mitochondrial function. Specifically, mitochondrial replication occurs via fission, which leads to the generation of new organelles during cell division, ensuring in this way that the number of mitochondria in the daughter cells remains the same as in the mother cell [35]. Additionally, fission facilitates the isolation of damaged or dysfunctional mitochondria. Autophagosomes target such organelles, and deliver them to lysosomes to be recycled (mitophagy). It is also thought that fusion can rescue damaged mitochondria from undergoing mitophagy [37]. These findings suggested that mutations are occurring much more frequently in the mitochondrial genome. Wallace and colleagues [44] were the first to identify inherited mitochondrial diseases. Currently over 250 disease-causing mutations have been described, including point mutations and deletions [45]. The disease severity is affected by the type of mutation, and whether it is present in heteroplasmic or homoplasmic form, whereas their incidence is thought to be approximately one in every 200 newborns [46]. Mitochondrial diseases are incurable and can end up being debilitating or even lethal. The Mitochondrial Medicine Society has recently come up with some recommendations on certain therapies that could help individuals affected by mitochondrial disease. Specifically, certain supplements such as the reduced form CoQ10 (ubiquinol), alpha-lipoic acid, and riboflavin can be prescribed to mitochondrial disease patients. Others, such as L-carnitine or folinic acid can also be administered when patients are deficient [47]. Mitochondrial genetics Research has also focused on identifying ways of preventing the transmission of mitochondrial diseases from a carrier woman to her children, and several different approaches have been proposed. The issue with this approach is that the children conceived will be genetically related to the male partner, but not the female partner. Routine prenatal diagnosis is also feasible, but it is not advisable due to the inability to accurately predict the phenotype. Both involve transplanting the nuclear genome between oocytes before or after fertilization [45,54,55]. A summary of the different types of mitochondrial disease inheritance and associated symptoms is shown in Table 9.
Order precose 25 mg with amex
Evidence-based algorithms can assist in estimating the risk of recurrence after the withdrawal of medications diabetes symptoms feeling hot precose 50 mg sale. When febrile seizures occur in the setting of a neurologic abnormality or are prolonged or complicated, the risk for later epilepsy is increased. Prognosis after a Single Unprovoked Seizure Activity Restrictions in Epilepsy Complete prevention of seizures is the goal of treatment. Patients with even infrequent seizures are at risk for harm to themselves or others while driving, operating machinery, working near depths or heights, swimming, or doing activities that entail risk of injuries. Patients with inadequately controlled seizures should be advised to avoid such activities. Some jurisdictions require patients or physicians to notify authorities if they have a condition that alters consciousness. The duration of restriction of activities after seizures are controlled varies among jurisdictions, and physicians must be aware of these requirements. Once seizures are controlled, these restrictions are unnecessary, and it is important to encourage normal activities to avoid stigmatization. Considerations in Women Changes in hormone levels during the menstrual cycle may aggravate seizures perimenstrually in some women. The administration of oral contraceptives (Chapter 225), Depo-Provera, acetazolamide (250 to 500 mg/day), or clobazam (10 to 20 mg/day) may reduce perimenstrual seizures. Enzyme-inducing antiepileptic drugs (see Table 375-8) that reduce estrogen the risk of experiencing recurrent seizures after a first unprovoked seizure ranges from 21 to 69% at 2 years and from 34 to 70% at 5 years. The risk is lower in the general population than in hospital-based studies (36% at 1 year and 45% at 2 years). The probability of a relapse decreases with time; about 50% of recurrences occur within 6 months of the initial seizure, and 76 to 96% occur within 2 years. The risk rises dramatically if more than one seizure has occurred; after a second unprovoked seizure, the risk for a third seizure is 73%, and after a third seizure, the risk for a fourth seizure is 76%. Prognosis of Epilepsy the natural history of untreated epilepsy, mostly in developing countries, shows that 30 to 40% of patients obtain 5- to 10-year remissions without treatment. In developed countries, where treatment is generally started after two unprovoked seizures have occurred, the likelihood of 5-year remission is about 60% when patients are followed for 10 years, and about 70% when patients are followed for 20 years. In the long term, sustained freedom from seizures is achieved in about 60% of patients (early remission in about 35 to 40% of patients and late remission in about 20 to 25%), about 16% of patients fluctuate between relapses and remissions, and about 25% never achieve seizure remission. Epilepsy is considered to be resolved in patients who had an age-dependent epilepsy syndrome and are now past the applicable age, or in patients who have been seizure free for at least 10 years, with no seizure medications for the last 5 years. Conversely, the duration of active epilepsy before achieving control is one of the most powerful predictors of remission. If seizures remain uncontrolled during the first year after diagnosis, the chance of ever achieving control is only 60%. If the period of uncontrolled seizures extends to 4 years, the chance of ever achieving control is only 10%. The presence of multiple seizure types and frequent generalized tonic-clonic seizures is associated with a lower likelihood of remission. Less than 40% of patients with newly diagnosed mesial temporal lobe epilepsy will be controlled with medications, although familial cases are more easily managed medically. Children whose seizures remain uncontrolled are at risk of developing cognitive impairment, especially at a younger age, thereby emphasizing the importance of prompt seizure control. In children with absence epilepsy, the 12-month probability of seizure control and remaining on medication is about 35 to 40% overall, but it is higher for ethosuximide (45%) and valproic acid (44%) than for lamotrigine (21%). In longitudinal population studies of children with newly diagnosed epilepsy, quality of life improves over time in about 50%, remains stable in 30%, and deteriorates in 20%. Patients with epilepsy are at risk for poor psychosocial outcomes, depression, and increased mortality. The major causes of death are underlying conditions such as stroke and pneumonia, although unnatural deaths from unintentional injury and poisoning are also more common. Patients who undergo successful epilepsy surgery, the most effective treatment for drug-resistant focal epilepsy, have a 66% decrease in mortality compared with medically treated patients. Evidence-based guideline: management of an unprovoked first seizure in adults: report of the Guideline Development Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Antiepileptic drug monotherapy for epilepsy: a network metaanalysis of individual participant data. Efficacy and safety of antiepileptic drugs for refractory partial-onset epilepsy: a network meta-analysis. Epilepsy surgery and meaningful improvements in quality of life: results from a randomized controlled trial. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. An overview of psychogenic non-epileptic seizures: etiology, diagnosis and management. Comparative safety of anti-epileptic drugs during pregnancy: a systematic review and network meta-analysis of congenital malformations and prenatal outcomes. Individualised prediction model of seizure recurrence and long-term outcomes after withdrawal of antiepileptic drugs in seizure-free patients: a systematic review and individual participant data meta-analysis. Cause of death and predictors of mortality in a communitybased cohort of people with epilepsy. About two thirds of patients with epilepsy are well controlled with one antiepileptic drug, but those who fail two antiepileptic drugs have a low chance of being controlled with further drug trials and are considered pharmacoresistant. The type of seizure and epilepsy syndrome determine which antiepileptic drug should be used to treat an individual patient. Antiepileptic drugs with a broad spectrum of efficacy against many types of seizures include valproate and levetiracetam, but some drugs like carbamazepine can exacerbate absence seizures. Valproate carries a high risk of major congenital malformations and poor intellectual development in children exposed to this medication in utero, so it should be avoided during pregnancy if possible. Answer: E Although over a dozen new antiepileptic drugs have been developed in recent years, they are no more effective than older drugs such as phenytoin, valproate, or carbamazepine. For example, in children with absence epilepsy, ethosuximide and valproate are more effective than the newer drug lamotrigine. Valproate, levetiracetam, lamotrigine, and topiramate have a broad spectrum of efficacy against focal and generalized seizures. Fortunately, most patients are well controlled with the first antiepileptic medication if it is appropriately chosen. However, because a lack of response to the first two antiepileptic drugs entails a poor prognosis, these patients are considered drug-resistant and should be referred to an epilepsy center. Although several drugs have risks of fetal malformations, valproate has the highest risk and also produces enduring deleterious effects on the intellectual development of children exposed in utero. During pregnancy, valproate should be used at the lowest possible dose or avoided if at all possible because the teratogenic effect is dose dependent. Brain surgery for epilepsy is safe and superior to medical therapy in patients with temporal lobe epilepsy. The benefits of surgery are enduring; over 50% of patients can be expected to remain entirely seizure free at 10 years. Only patients who have failed all first-line drugs and still have frequent seizures are eligible for surgery. Before considering surgery, clinicians should ensure that common causes of poor response to antiepileptic drugs, such as lifestyle issues, are addressed and that the patient is adherent to appropriate antiseizure medications. Various types of electrical stimulation of the nervous system, including deep-brain stimulation, may be beneficial for selected patients with drug-resistant epilepsy. Answer: C Patients who have failed two adequate trials of antiepileptic drugs should be referred for an evaluation of epilepsy surgery. Early surgery, performed within 2 years of developing drug resistance, is vastly superior to medical therapy in patients with temporal lobe epilepsy, with a number needed to treat with surgery, compared with medical therapy, to achieve seizure freedom of 2. About 65% of patients are free of seizures in the long term, compared with only 8% with medical therapy. Pseudoresistance to antiepileptic drugs is common and should be investigated thoroughly. The most common causes are an incorrect diagnosis of epilepsy, using the wrong drug, poor adherence to medication, and lifestyle issues that increase the chance of seizures, such as sleep deprivation and excessive alcohol use.