Purchase indocin now
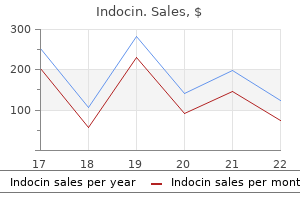
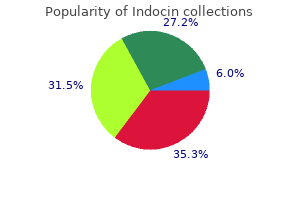
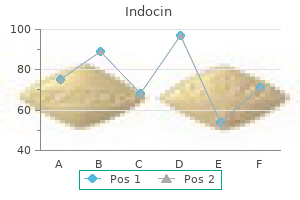
Patients may also qualify for Medicare if they do not meet these criteria but have uremic symptoms (nausea arthritis in back mattress buy indocin visa, vomiting, pericardial pain, acidosis, or hyperkalemia) or pulmonary edema refractory to diuretics. Renal failure itself is a catabolic state, and it is commonly difficult for patients on dialysis to regain lost weight. Given the chronic nature of renal disease, patients frequently remain unaware of the severity of their illness. Protein intake may fall spontaneously with the result that symptoms of uremia do not develop, but this is at the expense of a loss of lean body mass. It is only when dialysis is started that many patients appreciate how ill they have become. Lack of awareness can be avoided by carefully questioning the patient for insidious symptoms of uremia. For example, patients should be asked to compare their current eating habits and lifestyle with those 6 to 12 months previously. Kaplan-Meier curves showing no difference in time to death after early or late dialysis start. Because dialysis treatment has a finite life, either from loss of peritoneal function or failure of vascular access, starting treatment earlier will bring forward the time when further procedures or a change of modality is necessary. Moreover, there is likely to be resistance from many patients to the suggestion that they should start dialysis when they have no symptoms of uremia. The nephrologist would need complete confidence in the laboratory values as well as in the evidence supporting early commencement of dialysis to persuade a reluctant, asymptomatic patient. Starting dialysis is the first step in a lifelong commitment to renal replacement therapy. Patients will be asked to comply with a wide variety of inconvenient and sometimes unpleasant treatments. A high level of compliance is required for a successful outcome, and, particularly in the United States, there is concern about the level of noncompliance that is associated with increased mortality. A prospective study in the Netherlands provides useful data to help the patient and nephrologist agree when to commence treatment. However, this difference was no longer present by the end of the first 12 months of treatment. Retrospective and prospective nonrandomized comparative studies have failed to indicate a consistent survival advantage for either modality. Prevalent Distribution of Dialysis Patients by Modality 2010 Bangladesh Japan Argentina Germany Bosnia/Herzegovina Chile Portugal Israel Greece Czech Republic United States Croatia Russia Austria Malaysia Brazil Belgium Dutch sp. Small patients may be intolerant of the volume of dialysate needed to achieve adequate dialysis, particularly if they have negligible residual renal function. It may also be difficult to achieve adequate clearances in patients with a body mass index exceeding 35 kg/m2. Discomfort resulting from increased intra-abdominal volume can be significant in patients with chronic respiratory disease, low-back pain, or large polycystic kidneys. The presence of ischemic bowel disease, inflammatory bowel disease, or diverticulitis is likely to increase the incidence of peritonitis as a result of organisms passing through the bowel wall into the peritoneum. Abdominal wall infection may lead to peritonitis via the exit site and catheter tunnel. Severe malnutrition may lead to poor wound healing and to leakage from the catheter tunnel. In addition, peritoneal protein losses during dialysis may exacerbate hypoalbuminemia. At the other end of the spectrum, it may prove difficult to satisfactorily place a peritoneal catheter through the abdominal wall in patients with morbid obesity. Thereafter, absorption of glucose from the dialysate, which may average as much as 800 kcal/day, may contribute to further weight gain. As discussed in Chapter 91, access to the circulation can usually be obtained, even in patients with extensive vascular disease or previous surgery. Severe coagulopathy may make management of anticoagulation for the extracorporeal circuit difficult. The interpretation and reporting of these data are the responsibility of the author and in no way should be seen as an official policy or interpretation of the U. Because an increasing proportion of new dialysis patients are elderly, there may be no one available who is able or willing to take on this responsibility. It removes the inconvenience of traveling to and from the dialysis facility and gives patients the freedom to dialyze at a time that suits them. More frequent dialysis significantly reduces the time taken to recover after each treatment, reduces dietary restrictions and antihypertensive medications, and leads to an improved quality of life. The detrimental effects of central venous catheters persist even after the catheter has been removed. Patients presenting late for dialysis should still benefit from an education program about their options for long-term treatment. Possible factors affecting these decisions are discussed in the following sections. In countries such as the United Kingdom and Canada, where facilities are publicly funded from taxation, the use of more expensive types of dialysis-for example, high-volume hemodiafiltration-is limited. In the developed world, the practice of starting dialysis in patients who are very elderly or dependent on others for their care or who have multiple comorbid conditions varies significantly among countries and among nephrologists within those countries. Severe cognitive impairment in a patient would much more strongly influence a nephrologist in the United Kingdom not to start dialysis than in the United States. It has also provided a systematic approach to conflict resolution if there is disagreement regarding the benefits of dialysis. Withdrawing dialysis seems more like actively causing death than withholding dialysis, whereby death is allowed to occur naturally. Furthermore, it does not take into account the value of even a short extension of life that allows the patient and his or her family to prepare for death. Against this ethical background, are there any objective criteria that can be applied to identify patients who are unsuitable for dialysis Although advanced age was used as a simple exclusion criterion in the early days of dialysis, the elderly are now the most rapidly growing section of the dialysis population. Consultation with an ethics committee or ethics consultants may be required to clarify issues of disagreement, and negotiate a resolution. Physicians and institutions that refuse to accept the patient and their reasons should also be documented in the medical record. A Canadian study of patients starting dialysis43 used a comorbidity scoring system to quantify factors likely to predict early death. Indeed, it was impossible even to identify the small proportion of patients with a very poor prognosis. Clinicians were more accurate than the scoring system in identifying patients with less than a 50% risk of death by 6 months, but they tended to overestimate the risk of death in the worst prognostic groups. For example, 30% of patients whose predicted probability of death was considered to be 80% or higher survived for more than 6 months. Although these patients had a 1-year survival of only 19%, some survived at least 2 years. Quality of life is also strongly predictive of mortality, even after statistical correction for these comorbid factors. This may give the patient and his or her family a better understanding of what life on dialysis entails and may allow time for further discussion among all parties. The duration of the trial should be judged for each individual, and clinical and biochemical parameters such as serum albumin should be reviewed regularly. The quality of life is better without dialysis, and patients are more likely to die at home. Conservative therapy is best delivered by the specialist predialysis multidisciplinary team and should include a dietician, a social worker, and psychological support. The team should have close links with palliative care specialists so that there is a smooth transition from active medical therapy to end-oflife care. It may be appropriate to involve a psychologist, social worker, or religious counselor. It may be necessary to refer the case to a formal ethics committee, if one exists locally, to clarify the issues of disagreement and enable a resolution. A physician cannot be compelled to offer treatment against his or her professional judgment, but the physician is ethically and legally obliged to attempt to transfer the care of the patient to another physician. Only as a last resort, if no alternative dialysis unit can be found and after adequate advance notice has been given, should dialysis be withdrawn.
Generic 50mg indocin
Endovascular Intervention Endovascular intervention is the first option for central venous obstruction treatment rheumatoid arthritis treatment guidelines 2015 purchase 75mg indocin mastercard. Primary or additional stent implantation gives a much better outcome, with 1-year patency rates up to 56% or higher. Stent placement should avoid overlapping the ostium of the internal jugular vein because this vein is essential for future placement of central venous catheters. Similarly, a stent placed in the innominate vein should not overlap the ostium of the contralateral vein; otherwise, contralateral stenosis may occur and preclude future use of the contralateral limb for access creation. Surgical bypass to the ipsilateral jugular vein or contralateral subclavian or jugular vein is the first option in these patients. Alternative surgical approaches for upper limb vascular accesses with compromised venous outflow are axillary vein to femoral, saphenous, or popliteal vein and right atrial bypasses. Ultimately, ligation of the upper limb access can be considered, which will relieve local symptoms but loses a valuable dialysis access. Surgical Intervention For grades 1 and 2, conservative treatment of ischemia is advocated. Physical examination, including observation and palpation of peripheral vessels, may be inadequate and misleading for the diagnosis of symptomatic ischemia. A grade 1 to 4 classification for accessinduced ischemia can be used to outline the severity of the disease; this ranges from minor symptoms to finger necrosis. In most patients, it is necessary to add a saphenous vein or prosthetic graft bypass to the forearm arteries to augment distal hand perfusion (distal revascularization and interval ligation;. The results of these procedures are usually good, with relief of symptoms and preservation of the access site (Table 91-4). Two types of catheters are used in practice: nontunneled catheters for short-term dialysis, with a limited use and high morbidity; and tunneled cuffed catheters, which can be used up to several months with lower morbidity. The femoral route requires catheters of 30 to 35 cm in length for the distal tip to be located in the inferior vena cava. The subclavian vein should not be used because of the very high risk of subsequent venous stenosis. For sufficient blood flow rates to be achieved, the diameter of these catheters must be ideally 12 to 14 French. Tunneled central venous catheters have two lumens, each having a length of 40 cm, 10 cm of which is tunneled under the skin; the cannulae are made of synthetic polymer with a large internal lumen and a Dacron cuff to ensure subcutaneous anchoring. The catheter characteristics rely on the type of polymer, design, and geometry (double-lumen catheters, dual catheters, split catheters). The internal jugular vein and femoral vein routes are preferred because of ease of implantation and low risk of complications, such as central vein stenosis. Various societies have issued recommendations for the management of catheter infections. Infections Involving Temporary Catheters Tunneled Cuffed Double-Lumen Central Venous Catheter Inserted in the Right Internal Jugular Vein When a temporary dialysis catheter becomes infected, it should always be removed. The majority of these infections respond well to systemic antibiotics and meticulous exit site care, and the removal of the catheter is generally not required. Patients with a tunnel track infection sometimes but not always have an associated exit site infection; untreated, they can rapidly develop bacteremia. Patients with a tunnel track infection present with fever as well as local signs of pain, swelling, fluctuance, and erythema along the track of the catheter. Because tunnel track infections involve a potential space, in an area with limited vascular supply, and an implanted synthetic material, they respond poorly to antibiotics alone and require catheter removal. When a patient with a dialysis catheter has a fever, catheter infection must always be considered. The conventional approach is to remove the catheter with interval replacement at a different site after the infection has resolved. Although this is effective, it leads to an additional temporary catheter if dialysis is needed before the catheter can be replaced. Attempts to "salvage" an infected catheter with systemic antibiotic therapy lead to resolution of infection in only about 30% of patients. Another treatment option is to combine systemic antibiotics with antibiotic "lock" solutions. Many different cocktails of antibiotics mixed with either heparin or citrate have been tested; a popular regimen is vancomycin 2. Several studies have reported that exchange of the catheter over a guidewire 48 hours after initial antibiotic treatment is more effective than treatment with antibiotics alone and is as effective as removal of the catheter and delayed replacement, with the advantages of only one invasive procedure and preservation of the venous access site. The most important measure to prevent catheter infection is meticulous handling of the catheter at all times. The dialysis nurses need procedures for accessing the catheters under strict sterile conditions, and it is of the utmost importance that these catheters never be accessed by untrained personnel. Data from randomized trials indicate that antibiotic lock solutions significantly reduce the incidence of infection. Causative Organisms in Dialysis Catheter Infections Polymicrobial Gram positive Staphylococcus aureus Staphylococcus epidermidis Enterococcus Corynebacterium Gram negative Enterobacter Pseudomonas Acinetobacter Citrobacter Serratia Klebsiella Other gram-negative organisms Mycobacteria 16% 89% 30% 37% 17% 5% 33% 11% 7% 4% 4% 2% 3% 3% 2% Prevention of Infection Table 91-5 Causative organisms in dialysis catheter infections. An aminoglycoside or a cephalosporin is a good choice for gram-negative coverage; however, local microbiologic epidemiology must be taken into consideration, especially with regard to antibiotic resistance. Catheter Removal the decision to remove a tunneled cuffed dialysis catheter because of an episode of catheter-associated bacteremia is not straightforward. The clinical condition of the patient and response to initial therapy, the presence of metastatic complications, the infecting organism, and the availability of other vascular access sites must all Catheter obstruction may be caused by endoluminal fibrin deposits, restricting the catheter lumen or obstructing catheter side holes at the tip, or external fibrin sleeves surrounding the catheter, resulting in inadequate flow and excessive extracorporeal blood pressure alarms during the dialysis session. Depending on the location of the fibrin clot (arterial or venous line), there may be high negative arterial pressure (obstruction at the arterial catheter line) or high positive venous pressure (obstruction at the venous catheter line). Prevention of clot formation in the catheter tip during the interdialytic period is crucial. This is achieved by installing an antithrombotic lock solution (trisodium citrate 30% is superior to standard heparin or low-molecular-weight heparin). Regular use of low-dose warfarin or antiplatelet agents has failed to improve catheter function in dialysis patients in randomized trials. To correct catheter dysfunction, it is recommended that the catheter lumen be cleaned periodically by application of a fibrinolytic agent (urokinase) as a lock solution or by continuous infusion on both arterial and venous lines. Occluded catheters are reopened either by a mechanical method (brush) or pharmacologically (urokinase). Removal of the fibrin sleeve may be achieved by lasso wire stripping or by infusion of a fibrinolytic solution (urokinase) for 3 to 6 hours. Effect of preoperative sonographic mapping on vascular access outcomes in hemodialysis patients. Vascular access surgery managed by renal physicians: the choice of native arteriovenous fistulas for hemodialysis. Obesity is not an obstacle for successful autogenous arteriovenous fistula creation in haemodialysis. Lipectomy as a new approach to secondary procedure superficialization of direct autogenous forearm radial-cephalic arteriovenous accesses for hemodialysis. Brachiobasilic versus brachiocephalic arteriovenous fistula: A prospective randomized study. Evaluation of the efficacy of the transposed upper arm arteriovenous fistula: A single institutional review of 190 basilic and cephalic vein transposition procedures. Brachiobasilic arteriovenous fistula: Different surgical techniques and their effects on fistula patency and dialysis-related complications. Arteriovenous fistula formation using transposed basilic vein: Extensive single centre experience. A randomized multicenter study of the outcome of brachial-basilic arteriovenous fistula and prosthetic brachial-antecubital forearm loop as vascular access for hemodialysis. Transposed brachialbasilic arteriovenous fistulas versus prosthetic upper limb grafts: A metaanalysis. Multicenter evaluation of a polyurethane vascular access graft as compared with the expanded polytetrafluoroethylene vascular access graft in hemodialysis applications. A prospective comparison of two expanded polytetrafluoroethylene grafts for linear forearm hemodialysis access: Does the manufacturer matter Evaluation of 4-mm to 7-mm versus 6-mm prosthetic brachial-antecubital forearm loop access for hemo- 27.
| Comparative prices of Indocin | ||
| # | Retailer | Average price |
| 1 | Verizon Wireless | 227 |
| 2 | Ahold USA / Royal Ahold | 643 |
| 3 | Safeway | 435 |
| 4 | Ace Hardware | 926 |
| 5 | Williams-Sonoma | 678 |
| 6 | Sherwin-Williams | 649 |
| 7 | BJ'S Wholesale Club | 555 |
| 8 | Trader Joe's | 150 |
| 9 | ShopRite | 570 |
| 10 | Target | 565 |
Purchase indocin 75 mg fast delivery
There is death of superficial osteocytes and increased osteoclastic activity causing rarefaction arthritis in knee and fluid indocin 50mg with visa, microcyst formation and occasionally microfractures of the subjacent bone. These changes result in remodelling of bone and changes in the shape of joint surface leading to flattening and mushroomlike appearance of the articular end of the bone. This is followed by pain and swelling of joints usually in symmetrical fashion, especially involving joints of hands, wrists and feet. Extraarticular manifestations infrequently produce symptoms, but when present complicate the diagnosis. Rheumatoid nodules are particularly found in the subcutaneous tissue over pressure points such as the elbows, occiput and sacrum. Ankylosing spondylitis or rheumatoid spondylitis is rheumatoid involvement of the spine, particularly sacroiliac joints, in young male patients. Immunocompromised and debilitated patients are increasingly susceptible to suppurative arthritis. There may be formation of inflammatory granulation tissue and onset of fibrous adhesions between the opposing articular surfaces resulting in permanent ankylosis. Uncommon in the West, the disease is seen not infrequently in developing countries more commonly in children and also in adults. The joint space may contain tiny greywhite loose bodies and excessive amount of fluid. Aggregated deposits of monosodium urate monohydrate (tophi) in and around the joints of the extremities. A family history of gout is present in a fairly large proportion of cases indicating role of inheritance in hyperuricaemia. Hyperuricaemia and gout may be classified into 2 types: metabolic and renal, each of which may be primary or secondary. Primary refers to cases in which the underlying biochemical defect causing hyperuricaemia is not known, while secondary denotes cases with known causes of hyperuricaemia. Hyperuricaemia of metabolic origin this group comp rises about 10% cases of gout which are characterised by overproduction of uric acid. The secondary metabolic gout is due to either increased purine biosynthesis or a deficiency of glucose6phosphatase. Hyperuricaemia of renal origin About 90% cases of gout are the result of reduced renal excretion of uric acid. Renal disease per se rarely causes secondary hyperuricaemia such as in polycystic kidney disease and leads to urate nephropathy. Acute gouty arthritis this stage is characterised by acute synovitis triggered by precipitation of sufficient amount of needleshaped crystals of monosodium urate from serum or synovial fluid. There is joint effusion containing numerous polymorphs, macrophages and microcrystals of urates. Tophi are surrounded by inflammatory reaction consisting of macrophages, lymphocytes, fibroblasts and foreign body giant cells. Three types of renal lesions are described in the kidneys: acute urate nephropathy, chronic urate nephropathy and uric acid nephrolithiasis. They were initially regarded as inflammatory in origin and hence the name synovitis. Giant cell tumour of tendon sheath (Nodular tenosynovitis) the localised nodular tenosynovitis is seen most commonly in the tendons of fingers. The tumour shows infiltrate of small oval to spindled histiocytes with numerous interspersed multinucleate giant cells lying in a background of fibrous tissue. Grossly, the synovium has characteristic spongelike reddishbrown or tan appearance with intermingled elongated villous projections and solid nodules. The enlarged villi are covered by hyperplastic synovium and abundant subsynovial infiltrate of lymphocytes, plasma cells and macrophages, many of which are lipidladen and haemosiderinladen. The most common location is dorsum of wrist but may be found on the dorsal surface of foot near the ankle. It may or may not communicate with the joint cavity or tendon where it is located. Gout is a disorder of purine metabolism manifested by hyperuricaemia, recurrent attacks of characteristic acute arthritis, deposits of tophi in and around the joints, and in some cases uric acid nephrolithiasis. Pigmented villonodular synovitis and nodular teno synovitis are diffuse and localised form respectively of the same underlying process. A ganglion is a small, round or ovoid, movable, subcuta neous cystic swelling due to degeneration of synovium. The major functions of striated skeletal muscle are to convert chemical energy into mechanical energy, to act as a store of energy and proteins, and to play a role in the metabolism of the body. The muscle, however, cannot function as a contractile organ without a nerve supply. For this purpose, there are motor units, each of which consists of the following: 1. Motor neuron cell body located in the spinal cord anterior horn, or a cranial nerve nucleus. Here, two important groups of specific diseases-neurogenic and myopathic diseases, are discussed here. A classification of neuromuscular disorders based on the part of the motor unit involved is presented in Table 26. By light microscopy, a few clumps of lymphocytes may be found around small blood vessels. By immunocytochemistry combined with electron microscopy, it is possible to demonstrate the complex of IgG and complement at the neuromuscular junctions. In demyelination, on the other hand, there is conduction block in the nerve impulse but no denervation and hence muscle atrophy does not occur. These include amyotrophic lateral sclerosis as an example of anterior horn cell disease, and peripheral neuropathy causing injury to myelinated axon. In amyotrophic lateral sclerosis, there are characteristic fasciculations of muscles of the shoulder and tongue. Cardiac conduction defects; mental impairment; cataracts; frontal baldness; gonadal atrophy Hypertension Benign 4. Facioscapulohumeral type Limb-girdle type Oculo-pharyngeal type Autosomal dominant Autosomal recessive Autosomal dominant 2nd4th decade Early child hood to adult 5th6th decade Benign 5. Each type of muscular dystrophy is a distinct entity having differences in inheritance pattern, age at onset, clinical features, other organ system involvements and clinical course. However, in general, muscular dystrophies manifest in childhood or in early adulthood. Myopathies are primary skeletal muscle diseases resulting in chronic muscle weakness. These include hereditary or muscular dystrophies, inflammatory, endocrine, metabolic and toxic myopathies. An Xray of the right knee shows an expanded and osteolytic mass in the right lower femur in the region of metaphysis. Instead, sarcomas originate from the primitive mesenchymal cells having the capacity to differentiate along different cell pathways. As discussed in Chapter 7, soft tissue sarcomas metastasise most frequently by the haematogenous route and disseminate commonly to the lungs, liver, bone and brain. Lymph node metastases are often late and are associated with widespread dissemination of the tumour. Superficially-located tumours tend to be benign while deep-seated lesions are more likely to be malignant. Malignant tumours have frequently increased vascularity while benign tumours are selectively avascular. Approximately 15% of soft tissue tumours occur in children and include some specific examples of soft tissue sarcomas. The lesions of these tissues are embryologically derived Soft Tissue Tumours Table 27. Intermediate, locally aggressive these tumours are locally destructive, infiltrative and often recur but do not metastasise. Intermediate, rarely metastasising this category of tumours is also locally destructive, infiltrative and recurrent but in addition about 2% cases may have clinical metastasis which may not be predicted by morphology. Malignant Tumours in this category are clearly malignant- they are locally destructive, infiltrative and they metastasise in a high percent of cases.
Cheap indocin 75mg with mastercard
Resorptive phase is characterised by follicles lined by columnar epithelium and containing lightly stained vacuolated and scalloped colloid arthritis in back and stomach pain cheap indocin online american express. Iodine trapping by thyroidal cells involves absorbing of iodine from the blood and concentrating it more than twentyfold. The thyroid hormones so formed are released by endocytosis of colloid and proteolysis of thyroglobulin within the follicular cells resulting in discharge of T3 and T4 into circulation where they are bound to thyroxine-binding globulin. The relative frequency of some of these diseases varies in different geographic regions according to the iodine content of the diet consumed. Cardiac manifestations in the form of tachycardia, palpitations and cardiomegaly are invariably present in hyperthyroidism. These patients develop high grade fever, tachycardia, cardiac arrhythmias and coma and may die of congestive heart failure or hyperpyrexia. Cretinism or congenital hypothyroidism is the development of severe hypothyroidism during infancy and childhood. Neurological features such as deafmutism, spasticity and mental deficiency are more evident in sporadic cretinism due to developmental anomalies and dyshormonogenetic defects. In the process, B cells are also activated to form autoantibodies, which bring about immune destruction of thyroid parenchyma. Grossly, the classic form is characterised by diffuse, symmetric, firm and rubbery enlargement of the thyroid which may weigh 100-300 gm. There is extensive infiltration of the gland by lymphocytes, plasma cells, immunoblasts and macrophages, with formation of lymphoid follicles having germinal centres. These cells have abundant oxyphilic or eosinophilic and granular cytoplasm due to large number of mitochondria and contain large bizarre nuclei. The disease is more common in young and middle-aged women and may present clinically with painful moderate thyroid enlargement with fever, features of hyperthyroidism in the early phase of the disease, and hypothyroidism if the damage to the thyroid gland is extensive. Microscopically, the features vary according to the stage of the disease: Initially, there is acute inflammatory destruction of the thyroid parenchyma and formation of microabscesses. These granulomas consist of central colloid material surrounded by histiocytes and scattered multinucleate giant cells. Morphologically similar appearance may be produced in cases where vigorous thyroid palpation may initiate mechanical trauma to follicles, so-called palpation thyroiditis. Microscopically, there is extensive fibrocollagenous replacement, marked atrophy of the thyroid parenchyma, focally scattered lymphocytic infiltration and invasion of the adjacent muscle tissue by the process. The evidence in support is the intense lymphocytic infiltrate around the ocular muscles and detection of circulating autoantibodies against muscle antigen that cross-react with thyroid microsomes. The colloid is markedly diminished and is lightly staining, watery and finely vacuolated. In extreme cases, the lids can no longer close and may produce corneal injuries and ulcerations. Simple goitre often appears at puberty or in adolescence, following which it may either regress or may progress to nodular goitre. Sporadic (non-endemic) goitre Non-endemic or sporadic simple goitre is less common than the endemic variety. Hyperplastic stage is the early stage and is characterised by tall columnar follicular epithelium showing papillary infoldings and formation of small new follicles. Involution stage generally follows hyperplastic stage after variable period of time. Such endemic areas are several high mountainous regions far from the sea where iodine content of drinking water and food is low such as in the regions of the Himalayas, the Alps and the Ande. Cut section shows lobules of translucent gelatinous light brown parenchyma and areas of haemorrhage. Since nodular goitre is derived from simple goitre, it has the same female preponderance but affects older individuals because it is a late complication of simple goitre. Possibly, epithelial hyperplasia, generation of new follicles, and irregular accumulation of colloid in the follicles-all contribute to produce increased tension and stress in the thyroid gland causing rupture of follicles and vessels. This is followed by haemorrhages, cystic change, scarring and sometimes calcification, resulting in development of nodular pattern. Cut surface shows multiple nodules separated from each other by incomplete fibrous septa. The predominant histologic features are: nodularity, extensive scarring with foci of calcification, areas of haemorrhages and variable-sized follicles lined by flat to high epithelium and containing abundant colloid. The contrasting features of diffuse and nodular goitre are summarised in Table 25. Besides the follicular adenoma, other conditions which may produce clinically apparent solitary nodule in the thyroid are a dominant nodule of nodular goitre and thyroid carcinoma. The tumour cells are benign follicular epithelial cells lining follicles of various sizes. These cells may also form trabecular, solid and cord patterns with little follicle formation. Accordingly, the following 6 types of growth patterns are distinguished, though more than one pattern may be present in a single tumour: 1. Microfollicular (foetal) adenoma consists of small follicles containing little or no colloid and separated by abundant loose stroma. These tumours, however, do not show capsular and vascular invasion-features which distinguish it from follicular carcinoma. Primary lymphomas of the thyroid comprise less than 5% of thyroid cancers and majority of them possibly evolve from autoimmune (lymphocytic) thyroiditis (page 795). Carcinoma of the thyroid gland has 4 major morphologic types with distinctly different clinical behaviour and variable prevalence. Pathogenesis of thyroid cancer is explained on combination of these environmental etiologic factors and distinct genetic alterations in different microscopic types. External radiation the single most important environmental factor associated with increased risk of developing thyroid carcinoma after many years of exposure to external radiation of high dose. Evidences in support include: high incidence of thyroid cancer in individuals irradiated in early age for enlarged thymus and for skin disorders, in Japanese atomic bomb survivors, and in individuals living in the vicinity of nuclear accident sites. The tumour is well-encapsulated with compression of surrounding thyroid parenchyma. Cell of origin Gross Pathognomonic microscopy Regional metastases Distant metastases 10-year survival Parafollicular Moderate size Solid nests, amyloid stroma Common Rare 60-70% 2. It can occur at all ages including children and young adults but the incidence is higher with advancing age. Some cases first come to attention by spread to regional lymph nodes and cause cervical lymphadenopathy. Tumour cells the tumour cells have characteristic nuclear features due to dispersed nuclear chromatin imparting it ground glass or optically clear appearance and clear or oxyphilic cytoplasm. Invasion the tumour cells invade the capsule and intrathyroid lymphatics but invasion of blood vessels is rare. Psammoma bodies Half of papillary carcinomas show typical small, concentric, calcified spherules called psammoma bodies in the stroma. Follicular carcinoma presents clinically either as a solitary nodule or as an irregular, firm and nodular thyroid enlargement. In contrast to papillary carcinoma, regional lymph node metastases are rare but distant metastases by haematogenous route are common, especially to the lungs and bones, and sometimes this may be the presenting feature. Microscopy shows branching papillae having flbrovascular stalk covered by a single layer of cuboidal cells having ground-glass nuclei (inbox). The prognosis of follicular carcinoma is between that of papillary and undifferentiated carcinoma: 10-year survival rate is 50-70%. Medullary Thyroid Carcinoma Medullary carcinoma is a less frequent type derived from parafollicular or C-cells present in the thyroid and comprises about 5% of thyroid carcinomas. Secretion of calcitonin and other peptides Like normal C-cells, tumour cells of medullary carcinoma secrete calcitonin, the hypocalcaemic hormone. The amyloid deposits are believed to represent stored calcitonin derived from neoplastic C-cells in the form of prohormone. Sometimes, the tumour cells may be arranged in sheets, ribbons pseudopapillae or small follicles.
Indocin 50 mg mastercard
Irrespective of the source of vitamin D arthritis in the back with bone spurs discount indocin 25mg with mastercard, it must be converted to its active metabolites (25-hydroxy vitamin D and 1,25-dihydroxy vitamin D or calcitriol) after its metabolism in the liver and kidney for being functionally active. The main storage site of vitamin D is the adipose tissue rather than the liver which is the case with vitamin A. Maintenance of normal plasma levels of calcium and phosphorus the major essential function of vitamin D is to promote mineralisation of bone. This is achieved by the following actions of vitamin D: i) Intestinal absorption of calcium and phosphorus is stimulated by vitamin D. However, in hypocalcaemia, vitamin D collaborates with parathyroid hormone and causes osteoclastic resorption of calcium and phosphorus from bone so as to maintain the normal blood levels of calcium and phosphorus. Proliferation of cartilage cells at the epiphyses followed by inadequate provisional mineralisation ii. Biochemical changes these are as follows: i) Lowered levels of active metabolites of vitamin D (25-hydroxy vitamin D and 1, 25-dihydroxy vitamin D). Biochemical changes these are: i) normal or low serum calcium levels; ii) plasma phosphate levels lowered; and iii) raised serum alkaline phosphatase due to increased osteoblastic activity. It may be worthwhile to note here that another chronic disorder of skeleton seen in elderly, osteoporosis, is clinically similar but biochemically different disease (Chapter 26). Vitamin E is found in most of the ordinary foods such as vegetables, grains, nuts and oils. Anti-oxidant activity Active form of vitamin E acts as an antioxidant and prevents the oxidative degradation of cell membranes containing phospholipids. Scavenger of free radicals Vitamin E scavenges free radicals formed by redox reaction in the body (page 15) and thus maintains the integrity of the cell. Estimation of plasma prothrombin, thus, affords a simple in vitro test for determining whether there is deficiency of vitamin K. Because most of the green vegetables contain vitamin K and that it can be synthesised endogenously, vitamin K deficiency is frequently a conditioned deficiency. Due to malabsorption syndrome Patients suffering from malabsorption of fat develop vitamin K deficiency. Administration of vitamin K to such patients is of no avail since liver, where prothrombin synthesis utilising vitamin K takes place, is diseased. The major sources of vitamin C are citrus fruits such as orange, lemon, grape fruit and some fresh vegetables like tomatoes and potatoes. The physiologic functions of vitamin C are due to its ability to carry out oxidation-reduction reactions: L-Ascorbic Acid Dehydro L-Ascorbic acid + 2H+ + 2e 1. Vitamin C has been found to have antioxidant properties and can scavenge free radicals. Besides collagen, it is necessary for the ground substance of other mesenchymal structures such as osteoid, chondroitin sulfate, dentin and cement substance of vascular endothelium. Vitamin C being a reducing substance has other functions such as: hydroxylation of dopamine to norepinephrine; maintenance of folic acid levels by preventing oxidation of tetrahydrofolate; and role in iron metabolism in its absorption, storage and keeping it in reduced state. This may be due to deficiency of intercellular cement which holds together the cells of capillary endothelium. The epiphyseal ends of growing long bones have cartilage cells in rows which normally undergo provisional mineralisation. It may be the result of haemorrhage, interference with formation of folic acid or deranged iron metabolism. Now, vitamin B complex is commonly used for a group of essential compounds which are biochemically unrelated but occur together in certain foods such as green leafy vegetables, cereals, yeast, liver and milk. Most of the vitamins in this group are involved in metabolism of proteins, carbohydrates and fats. Thiamine hydrochloride is available in a variety of items of diet such as peas, beans, pulses, yeast, green vegetable roots, fruits, meat, pork, rice and wheat bran. The vitamin is lost in refined foods such as polished rice, white flour and white sugar. Thiamine after absorption is phosphorylated to form thiamine pyrophosphate which is functionally active compound. In addition, thiamin plays a role in peripheral nerve conduction by an unknown mechanism. Flabby, thin-walled, enlarged and globular appearance of the heart due to four-chamber dilatation. Dry beriberi (peripheral neuritis) this is marked by neuromuscular symptoms such as weakness, paraesthesia and sensory loss. Wet beriberi (cardiac manifestations) this is characterised by cardiovascular involvement, generalised oedema, serous effusions and chronic passive congestion of viscera. The heart in beriberi is flabby (due to thin and weak myocardium), enlarged and globular in appearance due to 4-chamber dilatation. Microscopic examination of the heart shows hydropic degeneration of myocardial fibres, loss of striations, interstitial oedema and lymphocytic infiltration. It is characterised by degeneration of ganglia cells, focal demyelination and haemorrhage in the nuclei surrounding the region of ventricles and aqueduct. Cheilosis and angular stomatitis are characterised by occurrence of fissures and cracks at the angles of mouth. All of these can be converted into biologically active coenzyme, pyridoxal 5-phosphate. The major physiologic functions of pyridoxine are related to: i) fat metabolism; ii) protein metabolism; iii) amino acid metabolism such as decarboxylation of amino acids, transmethylation of methionine, conversion of tryptophan to niacin; iv) steroid metabolism; v) neurotransmitter synthesis; and vi) haem synthesis. Folate (Folic Acid) and Cyanocobalamin (Vitamin B12) Both these vitamins included in the B complex group are required for red cell formation. It is available in food sources such as organ meat, soya beans, egg yolk; however eggwhite has a protein avidin which binds to biotin and blocks its bioavailability. Hence, the clinical practice is to administer combination of these members of vitamin B complex. Watersoluble vitamins consist of vitamin C and members of B complex group; in addition choline, biotin and flavonoids are newer members of this group. Its deficiency may produce rickets in growing children and osteomalacia in adults. Vitamin K deficiency causes hypoprothrombinaemia and may produce haemorrhagic disease of newborn. Vitamin C deficiency results in scurvy having lesions and clinical manifestations in early childhood and in the very aged. Besides, deficiency of choline may cause fatty liver and flavonoids act as antioxidants. Endogenous Synthesis of Carcinogens or Promoters i) In the context of etiology of gastric carcinoma, nitrites, nitrates and amines from the digested food are transformed in the body to carcinogens-nitrosamines and nitrosamides. Inadequate Protective Factors As already mentioned, some components of diet such as vitamin C, A, E, selenium, and b-carotenes have protective role against cancer. Mechanisms of components of diet acting in carcinogenesis are due to certain exogenous carcinogenic agents in diet, endogenous synthesis of carcinogens or their promoters, and dietary content poor in protective factors against cancer, mainly antioxidants. Hypoplasia is incomplete development of an organ not reaching the normal adult size. Developmental dysplasia is defective development of cells and tissues resulting in abnormal or primitive histogenetic structures. While anencephaly results from failure of neural tube closure, spina bifida occurs from incomplete closure of the spinal cord and vertebral column, often in the lumbar region. Foetal hydantoin syndrome Babies born to mothers on antiepileptic treatment with hydantoin have characteristic facial features and congenital heart defects. Consumption of alcohol by pregnant mother in first trimester increases the risk of miscarriages, stillbirths, growth retardation and mental retardation in the newborn. In the western countries, develop mental and genetic birth defects constitute about 50% of total mortality in infancy and childhood, while in the developing and underdeveloped countries 95% of infant mortality is attributed to environmental factors such as poor sanitation and undernutrition. Certain chemicals, drugs, physical and biologic agents are known to induce such birth defects and are called teratogens. The effects of teratogens are intrauterine death and growth retardation, defects in functions or malformations. The branch of science dealing with the study of human chromosomal abnormalities is called cytogenetics. Nuclear sexing can be done for genetic female testing by preparing and staining the smears of squamous cells scraped from oral cavity, or by identifying the Barr body in the circulating neutrophils as drumstick appendage attached to one of the nuclear lobes.
Syndromes
- Procedures that place a tube into the urethra (such as a catheter or cystoscope)
- Shock
- Leavening agents that release acids when they are heated react with baking soda to help biscuits, cakes, and other baked goods rise.
- Time it was swallowed
- Delays in growth
- Headaches
- When drowsy, stop driving until fully alert. Sleepiness may cause more accidents than alcohol.
- What medications does the person take?
Order 75mg indocin mastercard
Higher levels of physical activity are associated with a lower risk of abnormal glucose intolerance in renal transplant recipients how to relief arthritis cheap indocin 50 mg without a prescription. Hospitalized atrial fibrillation after renal transplantation in the United States. Obesity and cardiac risk after kidney transplantation: Experience at one center and comprehensive literature review. Cardiac troponin T before and after kidney transplantation: Determinants and implications for posttransplant survival. Serum stem cell factor level in renal transplant recipients with posttransplant erythrocytosis. Tubular function in patients with hypokalemia induced by sirolimus after renal transplantation. Renal allograft failure in a hyperparathyroid patient following initiation of a calcimimetic. Tertiary hyperparathyroidism in kidney transplant recipients: characteristics of patients selected for different strategies. Benefits associated with antiviral treatment in kidney allograft recipients with chronic hepatitis B infection. Impact of sirolimus, tacrolimus and mycophenolate mofetil on osteoclastogenesis-implications for posttransplantation bone disease. Outcome at 3 years with prednisonefree maintenance regimen: A single center experience with 349 kidney transplant recipients. A 1-year randomized, double-blind, placebo-controlled study of intravenous ibandronate on bone loss following renal transplantation. New-onset gout after kidney transplantation: Incidence, risk factors and implications. Only a decade ago, it was believed that nonimmunologic causes were the main factors leading to chronic allograft injury and graft loss. Whereas immunologic causes are now believed to be mainly responsible for late allograft injury and graft failure, nonimmunologic causes still represent significant risk factors for (late) graft injury and graft loss. The donor graft itself may present with significant preexisting disease, limiting long-term graft survival. Although some allografts are lost as a result of one specific cause, others accumulate the burden from several different causes with gradual loss of functioning nephrons. Main contributors to late graft injury and late graft loss are summarized in Box 107-2. Female donor gender negatively affects kidney graft survival, with reduced survival when female grafts are transplanted into male recipients (risk ratio 1. This is not only a result of reduced nephron mass ("nephron underdosing"), because a comparable effect is found for cardiac allografts. Other mechanisms may include possible differences in the immunogenicity of male and female grafts. Although it is asymptomatic in the immunocompetent host, it becomes activated in the immunocompromised patient. Graft survival has steadily improved over the last 25 years because of a reduction in both early and late graft loss. Changes thought not due to rejection-either acute or chronic Box 107-1 Banff classification of renal allograft pathology (2007 update of original 1997 classification). It is likely that the associated arteriolopathy and narrowing of the lumen contribute to development of fibrosis and atrophy after watershed infarcts within areas of ischemia. Local hypoxia leads to formation of free oxygen radicals, which promote cellular death by apoptosis. Diagnosis and management of recurrent disease are discussed further in Chapter 108. Calcineurin inhibitor nephrotoxicity affects all histologic compartments of the transplanted kidney. Confirmation of the diagnosis is made by exclusion of other causes, such as donor hyalinosis (which can be detected on the implantation biopsy specimen), diabetes, and hypertensive nephrosclerosis. Striped fibrosis is subjectively defined by a dense stripe of cortical fibrosis and atrophic tubules adjacent to Calcineurin Inhibitor Toxicity the vasculopathy in chronic allograft injury resembles systemic vascular disease, raising the possibility that conventional risk factors for cardiovascular disease may be implicated. In a multicenter, retrospective study of 29,751 kidney transplant recipients, elevated systolic blood pressure above 180 mm Hg (compared with <140 mm Hg) at 1 year was associated with a doubled risk of graft failure at 7 years. Dyslipidemias, including raised levels of total cholesterol, lowdensity lipoprotein cholesterol, and triglycerides, and cigarette smoking have also been associated with late graft failure. Some studies also suggest that hyperuricemia, which is common in patients with metabolic syndrome, may have a role in chronic allograft injury. The management of hypertension, dyslipidemia, and other cardiovascular risk factors in the transplant recipient is discussed further in Chapter 106. Early acute cellular rejection (within 3 months of transplantation) that is adequately diagnosed and treated and in which the serum creatinine returns to baseline values after treatment usually has no impact on long-term graft survival. Staining of glomerular capillaries (A) and circumferential staining of peritubular capillaries (B) are typical. Multiple and severe late acute cellular rejection episodes are predictive of chronic graft dysfunction more than early cellular rejection and acute vascular rejection, which have stronger associations with acute graft loss. Especially in chronic antibody-mediated rejection, however, C4d in peritubular capillaries may be negative (C4d-negative antibody-mediated rejection). Exact criteria for the definition of C4d-negative antibody-mediated rejection are currently lacking; however, it is believed that more than 50% of all chronic antibody-mediated rejection episodes are C4d negative. Other risk factors are previous nonadherence, psychiatric disorders, substance abuse, and insufficient socioeconomic support, and also adverse effects from immunosuppressive medication. In a recent study, 14 out of 61 patients (23%) who were converted from cyclosporine to everolimus at 3 to 4. However, substantial nephron loss may occur before a rise in serum creatinine becomes evident. Persistent or worsening proteinuria is also a late sign of chronic allograft injury. Proteinuria may be assessed by dipstick urine analysis, by spot urine protein-creatinine ratio, or by measurement of the 24-hour urine protein excretion. The Doppler resistive index gives an estimate of intrarenal (but also systemic) compliance and is most useful in longitudinal studies in the same patient to assess progressive graft vascular injury. The role of protocol biopsies in the early detection of chronic allograft injury remains controversial. Chronic allograft dysfunction is common and can have many causes; however, if it is left untreated, it can ultimately result in progressive renal injury, which in turn will heal by scarring and interstitial fibrosis. An overview of the differential diagnosis of chronic allograft dysfunction is given in Box 107-2. Transplant glomerulopathy is characterized by duplication of glomerular capillary basement membranes and mesangial matrix expansion, in the absence of immune deposits. In addition, there may be (but not necessarily) a deposition of C4d in glomerular capillaries, and also in peritubular capillaries. Clinicopathologic studies suggest that transplant glomerulopathy is a manifestation of capillary injury occurring in conjunction with interstitial, peritubular capillary, and glomerular inflammation, although it may also occur independently of interstitial fibrosis and tubular atrophy, or transplant arteriopathy. Induction therapy, with an interleukin-2 receptor antagonist or antithymocyte globulin, should be used to prevent early acute cellular rejection. Although it is currently a matter of debate whether alloantibodies should be monitored routinely in all patients who have undergone transplantation, it seems to be justified in immunologically high-risk patients, desensitized patients, and patients with suspected rejection and during therapy for antibody-mediated rejection, with the goal of recognizing allograft injury in its early stages and preventing its progression to chronic rejection. Protocol biopsies may further help in guiding post-transplant therapy at least in high-risk recipients, although definitive proof of the usefulness of protocol biopsies is currently lacking. Strategies for the prevention of chronic allograft injury are summarized in Box 107-3. The management of hypertension, dyslipidemia, and other cardiovascular risk factors in the transplant recipient is discussed in Chapter 106. After a specific diagnosis has been established, targeted treatments can be initiated. References Treatment of Chronic Allograft Injury In all patients with chronic allograft injury, there must be a focus on the effective management of nonimmunologic risk factors for progressive graft failure. Although reduction of blood pressure to a target below 130/80 is believed to be beneficial, the preferred agent for blood pressure 1. Kidney grafts from brain dead donors: Inferior quality or opportunity for improvement Accepting kidneys from older living donors: Impact on transplant recipient outcomes. Gene-expression profiles and age of donor kidney biopsies obtained before transplantation distinguish medium term graft function.
Buy cheap indocin 50 mg line
Hyaluronate capsule of group A Streptococcus is identical to human hyaluronate present in joint tissues and thus these tissues are the target of attack arthritis knee water exercise buy indocin 75mg low price. These autoantibodies cause damage to human tissues due to cross-reactivity between epitopes in the components of bacteria and the host. Streptococcal epitopes present on the bacterial cell wall, cell membrane and the streptococcal M protein, are immunologically identical to human molecules on myosin, keratin, actin, laminin, vimentin and N-acetylglucosamine. Evolution of fully-developed Aschoff bodies occurs through 3 stages all of which may be found in the same heart at different stages of development. Intermediate (proliferative or granulomatous) stage It is this stage of the Aschoff body which is pathognomonic of rheumatic conditions. These are large mononuclear cells having central round nuclei and contain moderate amount of amphophilic cytoplasm. With passage of months and years, the Aschoff body becomes less cellular and the collagenous tissue is increased. The occurrence of vegetations on the atrial surfaces of the atrioventricular valves (mitral and tricuspid) and on the ventricular surface of the semilunar valves (aortic and pulmonary) further lends support to the role of mechanical pressure on the valves in the pathogenesis of vegetations. Microscopically, the inflammatory changes begin in the region of the valve rings (where the leaflets are attached to the fibrous annulus) and then extend throughout the entire leaflet, whereas vegetations are usually located on the free margin of the leaflets and cusps. B, Opened up chambers and valves of the left heart show irregularly scarred mitral valve leaving a fish-mouth or buttonhole opening between its two cusps (black arrow). A, Microscopic structure of the rheumatic valvulitis and a vegetation on the cusp of mitral valve in sagittal section. B, Section of the myocardium shows a healed Aschoff nodule in the interstitium having collagen, sparse cellularity, a multinucleate giant cell and Anitschkow cells. Vegetations present at the free margins of cusps appear as eosinophilic, tiny structures mainly consisting of fibrin with superimposed plateletthrombi and do not contain bacteria. The valves show diffuse thickening as a result of fibrous tissue with hyalinisation, and often calcification. The affected area shows oedema, fibrinoid change in the collagen, and cellular infiltrate of lymphocytes, plasma cells and macrophages with many Anitschkow cells. The lesions in the coronaries are seen mainly in the small intramyocardial branches. Histologically, the lesions may be like those of hypersensitivity angiitis (page 385), or sometimes may resemble polyarteritis nodosa. There may be endarteritis obliterans and thrombosis of cortical and meningeal vessels. Pleuritis is often accompanied with serofibrinous pleural effusion but definite Aschoff bodies are not present. However, once the heart is involved, it is often associated with reactivation and recurrences of the disease. Bacterial endocarditis of both acute and subacute type may supervene due to inadequate use of antibiotics. Endocarditis can be broadly grouped into non-infective and infective types (Table 14. Frequently, fibrinous or serofibrinous pericarditis with pericardial effusion is associated. Microscopically, the verrucae of Libman-Sacks endocarditis are composed of fibrinoid material with superimposed fibrin and platelet thrombi. Similar inflammatory changes may be found in the interstitial connective tissue of the myocardium. Following diseases and conditions are frequently associated with their presence: 1. Although classification of bacterial endocarditis into acute and subacute forms has been largely discarded because the clinical course is altered by antibiotic treatment, still a few important distinguishing features are worth noting (Table 14. Other less common etiologic agents include other strains of streptococci and staphylococci. Bacteraemia, septicaemia and pyaemia: Bacteria gain entry to the blood stream causing transient and clinically silent bacteraemia in a variety of day-to-day procedures as well as from other sources of infection. Following are some of the examples of such conditions: i) Impaired specific immunity in lymphomas. Another alternative hypothesis is the occurrence of nonbacterial thrombotic endocarditis from prolonged stress which is followed by bacterial contamination. A summary of the distinguishing features of the principal types of vegetations is presented in Table 14. Small, multiple, warty, grey brown, translucent, firmly attached, generally produce permanent valvular deformity 4. Microscopy Composed of fibrin with superimposed platelet thrombi and no bacteria, Adjacent and underlying endocardium shows oedema, proliferation of capillaries, mononuclear inflammatory infiltrate and occasional Aschoff bodies. Medium-sized, multiple, generally do not produce significant valvular deformity Composed of fibrinoid material with superimposed fibrin and platelet thrombi and no bacteria. The underlying endocardium shows fibrinoid necrosis, proliferation of capillaries and acute and chronic inflammatory infiltrate including the haematoxylin bodies of Gross. Small but larger than Often large, grey-tawny to those of rheumatic, single greenish, irregular, single or or multiple, brownish, multiple, typically friable firm, but more friable than those of rheumatic Composed of degenerated valvular tissue, fibrinplatelets thrombi and no bacteria. The underlying valve shows swelling of collagen, fibrinoid change, proliferation of capillaries but no significant inflammatory cell infiltrate. Grossly, the lesions are found commonly on the valves of the left heart, most frequently on the mitral, followed in descending frequency, by the aortic, simultaneous involvement of both mitral and aortic valves, and quite rarely on the valves of the right heart. They begin from the contact areas of the valve and may extend along the surface of the valves and on to the adjacent endocardium. In the early stage, the lesions are confined to the heart, while subsequent progression of the disease leads to involvement of extra-cardiac organs. Both these have their pathogenesis in circulating immune complexes (hypersensitivity phenomenon) (page 654). The causes of death are cardiac failure, persistent infection, embolism to vital organs, renal failure and rupture of mycotic aneurysm of cerebral arteries. Tuberculous endocarditis Though tubercle bacilli are bacteria, tuberculous endocarditis is described separate from the bacterial endocarditis due to specific granulomatous inflammation found in tuberculosis. The severest manifestation of cardiovascular syphilis is aortic valvular incompetence. Fungal endocarditis Rarely, endocardium may be infected with fungi such as from Candida albicans, Histoplasma capsulatum, Aspergillus, Mucor, coccidioidomycosis, cryptococcosis, blastomycosis and actinomycosis. Viral endocarditis There is only experimental evidence of existence of this entity. Generally, the valve leaflets are diffusely thickened by fibrous tissue and/or calcific deposits, especially towards the closing margin. Elevated left atrial pressure, in turn, raises pressure in the pulmonary veins and capillaries, reducing the pulmonary function and causing exertional dyspnoea which is the chief symptom of mitral stenosis. Valves of the left side of the heart are involved much more frequently than those of the right side of the heart. Normal mitral valve (A) contrasted with mitral stenosis (B) and mitral insufficiency (C). A few other conditions cause mitral insufficiency by dilatation of the mitral ring such as in myocardial infarction, myocarditis and left ventricular failure in hypertension. As a consequence of left atrial hypertension, pulmonary hypertension occurs resulting in pulmonary oedema and right heart failure. It is of 2 main types: non-calcific and calcific type, the latter being more common. In rheumatic aortic stenosis, the commissures are fused and calcified, while in nonrheumatic aortic stenosis there is no commissural fusion. Later, when cardiac failure supervenes, there is dilatation as well as hypertrophy of the left ventricle (eccentric hypertrophy). The three cardinal symptoms of aortic stenosis are: exertional dyspnoea, angina pectoris and syncope. Angina pectoris usually results from elevation of pulmonary capillary pressure and usually develops due to increased demand of hypertrophied myocardial mass. Normal aortic valve (A) contrasted with aortic stenosis (B) and aortic insufficiency (C). The lesions are characteristically located in the valves and endocardium of the right side of the heart.
Effective 25 mg indocin
Ischaemic colitis passes through 3 stages: infarct arthritis in neck and back pain order on line indocin, transient ischaemia and ischaemic stricture. However, the surgical submitted specimens generally are of the ischaemic stricture. Thus, the gross appearance can be confused with either of the two types of inflammatory bowel disease. The muscularis may also show inflammatory changes and patchy replacement by fibrosis. The blood vessels may show atheromatous emboli, organising thrombi and endarteritis obliterans. A pseudomembrane composed of necrotic epithelium, fibrin and inflammatory cells may develop. In healed cases, stricture formation, malabsorption and short bowel syndrome are the usual complications. Necrotising enterocolitis is an acute inflammation of the terminal ileum and ascending colon, occurring primarily in premature and low-birth-weight infants. Exogenous factors In addition to role of genetic factors and deranged T-cell mediated immunity, a role for several exogenous and environmental factors has been assigned: i) Microbial factors: At different times, role of a variety of microbes in initiation of inflammatory response by the body has been suspected. Luminal surface of longitudinal cut section shows segment of thickened wall with narrow lumen which is better appreciated in cross-section (arrow) while intervening areas of the bowel are uninvolved or skipped. The histological features present are: transmural chronic inflammatory cell infiltration, deep fissures into the bowel wall, submucosal widening due to oedema, some prominent lymphoid follicles and a few non-caseating epithelioid cell granulomas in the bowel wall. In more chronic cases, fibrosis becomes increasingly prominent in all the layers disrupting muscular layer. The appearance of colon may vary depending upon the stage and intensity of the disease because of remissions and exacerbations. Mucosa shows linear and superficial ulcers, usually not penetrating the muscular layer. Crypt distortion, cryptitis and focal accumulations of neutrophils forming crypt abscesses. These may be internal fistulae between the loops of the intestine, or external fistulae such as enterocutaneous, rectal and anal fistulae. Toxic megacolon (Fulminant colitis) is the acute fulminating colitis in which the affected colon is thin-walled and dilated and is prone to perforation and faecal peritonitis. There is deep penetration of the inflammatory cell infiltrate into muscle layer which is disrupted. Pathogenetically speaking, these microorganisms can cause enterocolitis by 2 mechanisms-by enteroinvasive bacteria producing ulcerative lesions, and by enterotoxin-producing bacteria resulting in non-ulcerative lesions. Subsequently, the mesenteric lymph nodes are affected which show typical tuberculous granulomatous inflammatory reaction with caseation necrosis. In advanced cases, transverse fibrous strictures and intestinal obstruction are seen. Mucosa and submucosa show ulceration and the muscularis may be replaced by variable degree of fibrosis. Grossly, the terminal ileum, caecum and/or ascending colon are thick-walled with mucosal ulceration. But now-a-days due to control of tuberculosis in cattle and pasteurisation of milk, virtually all cases of intestinal tuberculosis are caused by M. Enteric Fever the term enteric fever is used to describe acute infection caused by Salmonella typhi (typhoid fever) or Salmonella paratyphi (paratyphoid fever). The margins of the ulcers are slightly raised due to inflammatory oedema and cellular proliferation. There is never significant fibrosis and hence fibrous stenosis seldom occurs in healed typhoid lesions. The main complications of the intestinal lesions of typhoid are perforation of the ulcers and haemorrhage. The illness results from either bacterial invasion or bacterial toxigenic effect on the bowel. Staphylococcal food poisoning Staphylococcus aureus infection acquired from contaminated food produces either mild food poisoning by enterotoxins, or may cause more severe form of the illness called pseudomembranous enterocolitis described below. Staphylococcal food poisoning occurs due to liberation of enterotoxins by the bacteria. Clostridial food poisoning Infection with anaerobic organisms Clostridium welchii, following consumption of contaminated meat results in acute food poisoning (page 172). Botulism this is a severe form of paralysing illness caused by ingestion of organism, Clostridium botulinum, which produces neurotoxin. Salmonella food poisoning (Salmonellosis) this is an infection (and not caused by toxins) occurring due to food contaminated by S. Infection occurs by faeco-oral route and is seen with poor personal hygiene, in densely populated areas, and with contaminated food and water. It is more prevalent in the tropical countries and primarily affects the large intestine. Here, they invade the epithelium of the mucosa, reach the submucosa and produce the characteristic flask-shaped ulcers (page 178). In advanced cases, typical flask-shaped ulcers having narrow neck and broad base are seen. Complications of intestinal amoebic ulcers are: amoebic liver abscess or amoebic hepatitis, perforation, haemorrhage and formation of amoeboma which is a tumour-like mass. Intestinal tuberculosis can occur as primary, secondary or hyperplastic ileocaecal type. In a classic case, there are multiple tranverse ulcers and strictures causing intestinal obstruction. There are oval ulcers along the long axis of the small intestine and may be complicated by perforation. Bacterial food poisoning may be caused by staphylococci, Clostridia, and Salmonella. Partial villous atrophy is the mild form of the lesion in which villi fuse with each other and thus become short and broad, commonly called as convolutions and irregular ridges. The surface epithelium is cuboidal and there is increased plasma cell infiltrate in the lamina propria. Subtotal and total villous atrophy is exhibited by a number of conditions such as nontropical sprue, tropical sprue, intestinal lymphomas, carcinoma, protein-calorie malnutrition etc. The condition is characterised by significant loss of villi in the small intestine and therefore Mucosal damage. However, following hypotheses have been proposed in causing mucosal cell damage: 1. There may be partial villous atrophy which is replacement of normal villous pattern by convolutions, or subtotal villous atrophy characterised by flat mucosal surface. The major sequela of long-term coeliac sprue is increased incidence of intestinal carcinoma in these cases. Collagenous Sprue this entity is regarded as the end-result of coeliac sprue in which the villi are totally absent (total villous atrophy) and there are unique and diagnostic broad bands of collagen under the basal lamina of surface epithelium. Some workers consider collagenous sprue as a variant of coeliac sprue without classifying it separately. Tropical Sprue this disease, as the name suggests, occurs in individuals living in or visiting tropical areas such as Caribbean countries, South India, Sri Lanka and Hong Kong. Protein-Losing Enteropathies A number of disorders of the gastrointestinal tract are accompanied by excessive protein loss without concomitant increase in protein synthesis, thus resulting in hypoproteinaemia. Amongst the malignant tumours, the most frequently encountered, in descending frequency, are: carcinoid tumours, lymphomas and adenocarcinoma. Carcinoid tumour, a peculiar neoplasm most common in the midgut, and lymphoma are described below. Foregut carcinoids, located in the stomach, duodenum and oesophagus are also argyrophil type and are encountered as frequently as in the hindgut (10-20%). Ileal and gastric carcinoids are commonly multiple, whereas appendiceal carcinoids commonly involve the tip of the organ and are solitary. Right-sided heart failure due to involvement of tricuspid and pulmonary valves and endocardium (page 431). Obstructive: Faecolith Calculi Foreign body Tumour Worms (especially Enterobius vermicularis) Diffuse lymphoid hyperplasia, especially in children. Microscopically, the tumour cells are monomorphic and have typical endocrine pattern. In further advanced cases called acute gangrenous appendicitis, there is necrosis and ulcerations of mucosa which extend through the wall so that the appendix becomes soft and friable and the surface is coated with greenish-black gangrenous necrosis.
Purchase 25mg indocin mastercard
The disadvantage is that the tidal volume varies depending on compliance and any increase in airway resistance can decrease the tidal volume to dangerously low levels arthritis in back mattress purchase indocin 25 mg with mastercard. This mode is used in patients with poor lung compliance which requires a higher pressure. For patients in whom conventional mechanical ventilation fails to achieve adequate oxygenation, open lung ventilation may be considered. It minimizes shearing forces due to alveolar collapse by stenting alveoli open at end expiration. It is managed with four variables, a time at a high pressure (Thigh) and lower pressure (Tlow) and the pressure high (Phigh) and low (Plow). It is set to have a higher Thigh to recruit alveoli with ventilation occurring with spontaneous breaths over the Phigh and during the pressure release to Plow. FiO2 should be adjusted to ensure adequate oxygenation with the lowest possible FiO2 to prevent pulmonary oxygen toxicity. It has been shown that a lung-protective strategy, during an abdominal operation, with lower volume ventilation may improve clinical outcomes (N Engl J Med. As a result, the tidal volume should be decreased to maintain plateau pressures <30 cm H2O and to minimize barotrauma but >20 cm H2O to minimize atelectasis. Longer expiratory times allow patients with obstructive lung disease to exhale fully and prevent breath stacking. Longer inspiratory times, which decrease peak airway pressures, are useful in patients with low pulmonary compliance. Inverse-ratio ventilation takes advantage of breath stacking, using I:E ratios from 1:1 to 4:1. This improves gas exchange by progressive alveolar recruitment with a higher mean airway pressure. Sedation and neuromuscular paralysis is often necessary in mechanically ventilated patients to control anxiety, allow for rest, and synchronize breathing. The need for paralysis is rare, except in patients with severe respiratory failure and decreased pulmonary compliance. The extent of paralysis should routinely be assessed with neuromuscular monitoring, and adequacy of anesthesia should be ensured with a processed electroencephalogram. The patient who has required prolonged ventilatory support may require several days to weeks to wean because of marginal respiratory muscle strength and the time required for lung recovery. In general, hemodynamic instability or high work of breathing are contraindications to weaning. The first priority is to switch to bag ventilation using 100% oxygen to ensure adequate ventilation and oxygenation. Listen closely for any change in breath sounds consistent with a pneumothorax, new lung consolidation, or pleural fluid collection. Barotrauma from high peak airway pressures can lead to subcutaneous emphysema, pneumomediastinum, and pneumothorax. Oxygen toxicity refers to levels of intra-alveolar oxygen high enough to cause lung damage. The precise mechanism is unknown, but likely involves oxidation of cell membranes due to oxygen radicals. Tracheoinnominate fistula is caused by erosion of a tracheostomy tube into the innominate artery. Emergent treatment consists of insertion of a finger into the tracheostomy and applying ventral pressure to compress the artery. Orotracheal intubation should be performed and a thoracic surgical consult obtained. This method of support, with its necessary anticoagulation, is fraught with complications. In the critical care setting, it may be necessary as temporary support for a patient with reversible myocardial damage after surgery (Chapter 30). Shock is defined by global tissue hypoxia and occurs when the supply of oxygen is insufficient to meet metabolic demands. Hypovolemic shock results from loss of circulating blood volume caused by acute hemorrhage, fluid depletion, or dehydration. Patients are peripherally vasoconstricted, tachycardic, and have low jugular venous pressure. The most common causes include sepsis, neurogenic shock, adrenal insufficiency, and liver failure. Neurogenic shock results from interruption of the spinal cord at or above the thoracolumbar sympathetic nerve roots, which produces loss of sympathetic tone, causing vasodilation. Jugular venous pressure is elevated while the peripheral tissues demonstrate vasoconstriction. These patients typically are peripherally vasoconstricted and tachycardic with an elevated jugular venous pressure. Supplemental oxygen should be administered or an airway placed to achieve a SaO2 >92%. For most critically ill patients, a transfusion trigger of 7 g/dL is appropriate, except with an ongoing myocardial infarction or severe ischemic cardiomyopathy (N Engl J Med. A continuous cardiac monitor provides the heart rate and indirect clues about stroke volume. With the exception of the patient in pulmonary edema, patients in circulatory shock should initially receive 10 to 20 mL/kg bolus of a crystalloid solution. A metabolic acidosis can reflect the depth of circulatory compromise and the adequacy of resuscitation. Therapy focuses on control of ongoing loss and restoration of intravascular volume. Patients with blood losses of up to 20% can be resuscitated using crystalloid solutions. However, because salt solutions equilibrate with the interstitial space, volume replacement requires three times the estimated volume deficit. Patients in whom diaphoresis, ashen facies, and hypotension develop have lost 30% or more of their blood volume and require transfusion. To achieve rapid infusion rates, short, large-bore intravenous catheters in a peripheral vein are best. In addition, if intravenous attempts are unsuccessful, intraosseous access can be quickly obtained. A multilumen central line is not effective for rapid volume resuscitation since resistance to flow is proportional to catheter length and inversely proportional to catheter lumen radius raised to the fourth power. Hypothermia is aggravated by rapid infusion of room temperature crystalloid and refrigerated blood, impairing oxygen unloading and compromising coagulation; therefore fluids and blood products should be warmed. The diagnosis and treatment of adrenal insufficiency in septic shock are evolving. The use of corticosteroids is not without risk as it does increase the risk of infection (N Engl J Med. These guidelines state that patients with primary adrenal insufficiency or those with septic shock refractory to fluid resuscitation and vasopressors, without performing a cosyntropin stimulation test, should be treated with moderate-dose hydrocortisone due to a faster resolution of shock seen in multiple studies and a survival advantage (Crit Care Med. A recent meta-analysis evaluating the use of steroids for septic shock did not show a survival advantage, though again, there was faster resolution of shock (Anesth Analg. Future studies will need to clarify the utility of corticosteroids and any subgroups where they are beneficial. A peripheral vasoconstrictor, phenylephrine or norepinephrine, is administered to increase vascular tone if hypotension is refractory to volume infusion. Because patients with spinal shock tend to equilibrate body temperature with their environment, fluids and room temperature must be kept warm. Tension pneumothorax is treated by needle decompression followed by tube thoracostomy. Pericardial tamponade is treated by needle decompression, often with catheter placement for drainage. Options include systemic anticoagulation, thrombolysis, and surgical clot removal. Intra-aortic balloon counterpulsation may be necessary before and during recovery from definitive surgical treatment. If perfusion remains inadequate, the only remaining option is mechanical circulatory support.
Order indocin canada
This is an area of ongoing debate in liver and arthritis in neck heat or cold discount 75mg indocin, to a lesser extent, cardiac transplantation and is discussed in detail later. The general advantages and disadvantages of simultaneous dual-organ transplantation are shown in Table 111-1. Although kidney biopsy might be useful in determining the degree of reversibility, in practice it is not commonly performed. This reflects the perceived technical difficulties of performing the procedure in critically ill-often coagulopathic-patients, in whom a biopsy-related bleed could have catastrophic consequences. Indeed, these complications might be more severe in nonrenal transplant recipients because of other risk factors. For example, antiproliferative immunosuppressants exacerbate anemia and corticosteroids exacerbate metabolic bone disease. The initial evaluation should include thorough review of renal function in the peritransplantation period and exposure to nephrotoxins. Finally, some have advocated switching of cyclosporine to low-dose tacrolimus, although the supporting data are less compelling. Thus, hypertension, anemia, and hyperparathyroidism should be managed according to standard guidelines. In practice, lifestyle modification and several antihypertensive drugs are usually required for achievement of target blood pressure. With either modality, mortality is much higher compared with matched nontransplant controls. There seems little doubt that in those fit for the procedure, sequential kidney transplantation is the best form of renal replacement therapy. Because patients have already undergone transplantation, the addition of the renal allograft does not imply a huge increase in immunosuppression (typically, this is increased only in the perioperative period). When it is feasible, a preemptive living donor transplant is probably the best option. Initial mortality is higher in nonrenal transplant recipients receiving a kidney transplant as opposed to staying on the waiting list (reflecting the complications of surgery and more immunosuppression), but mortality in the medium and long term is much lower. Severe rhabdomyolysis has been reported, usually when statins are prescribed with cyclosporine and an inhibitor of the cytochrome P-450 system, such as diltiazem or ketoconazole and other azole-based antifungal agents. The number and percentage of simultaneous liver-kidney transplants have increased greatly in the United States in recent years. The main issue, of course, is deciding which patients are likely to have meaningful renal recovery after liver transplant alone. Singlecenter studies suggest that use of a combination of clinical and histologic criteria allows effective prediction of which patients will benefit most from simultaneous liver-kidney transplantation. Renal biopsy was performed by the percutaneous or transjugular method and had a moderate rate of complications21,22; some believe that it adds little discriminating value. In the largest reported study, 1% of heart transplant recipients required renal replacement therapy before transplantation. Ventricular assist devices are sometimes used as a bridge to cardiac transplantation and can improve renal function in this setting. In some patients there may also be a component of chronic kidney injury caused by renovascular disease or hypertension or atheroembolism. In addition to the causes shown in Table 111-2, factors that may be important after cardiac transplant surgery are prolonged aortic cross-clamping, large fluid volume shifts, and prolonged allograft ventricular dysfunction. As in liver transplantation, the question of whether the patient is best served by heart-alone or simultaneous heart and kidney transplantation sometimes arises. The absolute number of such dual transplants remains low but is steadily increasing in the United States (71 in 2012, equivalent to about 3. At this time, it seems reasonable to limit the combined transplants to patients with at least a severity of kidney disease similar to that shown in Box 111-1. First, aggressive diuresis is often prescribed to minimize any pulmonary edema in the allograft. Although it is probably rare, this "new disease" emphasizes the importance of maintaining a broad differential diagnosis for any kidney disease occurring after solid organ transplantation and the usefulness of performing a renal biopsy when the clinical presentation is unusual. The most encouraging therapy to date is defibrotide, an oligonucleotide with antithrombotic and fibrinolytic effects on microvascular endothelium, but with apparently few systemic adverse effects. These include prerenal syndromes caused by hepatorenal syndrome (see later) and hypovolemia (induced by vomiting and diarrhea or bleeding). Obstructive uropathy is much rarer but can be caused by severe hemorrhagic cystitis or fungal infection of the collecting system. The pathophysiology is thought to involve radiotherapy- and chemotherapy-induced damage to the endothelium of hepatic venules with subsequent venular thrombosis and sinusoidal and portal hypertension. The initial symptoms and signs are weight gain, edema, and ascites, then right upper quadrant abdominal pain and tenderness, jaundice, and abnormal liver function test results. In the setting of hepatorenal syndrome, there is some evidence that they are associated with less of an increase in intracranial pressure. In addition, the daily obligate fluid intake in these patients is frequently massive, and fluid balance is most easily controlled by a continuous technique. Vascular access can be problematic because of thrombocytopenia and neutropenia predisposing to bleeding and infection, respectively. Characteristic clinical features are slowly rising serum creatinine, hypertension, and disproportionate anemia (see also Chapter 29). The glomerulus shows thickened capillary walls with "double contours" and segmental occlusion and collapse of capillaries (orange arrows). A summary of diagnostic criteria (and their limitations) is provided in reference 45. Kidney biopsy is rarely required unless the presentation is atypical, because the biopsy findings are unlikely to significantly alter management and the biopsy carries increased risks in patients with thrombocytopenia and other morbidities. Histopathology typically shows microthrombi in arterioles and glomerular capillaries, mesangiolysis, glomerular basement membrane duplication, and tubular injury with interstitial fibrosis. Prevention involves renal shielding (from irradiation damage) and avoidance of other nephrotoxic agents at the time of conditioning. Renal ultrasound is often used to exclude post-renal causes, but other imaging studies are usually unnecessary. On occasion, the allogeneic stem cell donor can donate a kidney; a great benefit of this approach is that a state of tolerance to the allograft should exist, and hence minimal or no immunosuppression is required. Good outcomes after renal transplantation have been reported in carefully selected patients. The growing problem of chronic renal failure after transplantation of a nonrenal organ. Biopsy-diagnosed renal disease in patients after transplantation of other organs and tissues. Calcineurin inhibitor-sparing regimens in solid organ transplantation: Focus on improving renal function and nephrotoxicity. Implications of acute kidney injury after heart transplantation: What a surgeon should know. Acute renal failure after lung transplantation: Incidence, predictors and impact on perioperative morbidity and mortality. Chronic kidney disease after nonrenal solid organ transplantation: A histological assessment and utility of chronic allograft damage index scoring. Calcineurin inhibitor minimisation versus continuation of calcineurin inhibitor treatment for liver transplant recipients. An emerging population: Kidney transplant candidates who are placed on the waiting list after liver, heart, and lung transplantation. Home dialysis is a successful strategy in nonrenal solid organ transplant recipients with end-stage renal disease. Mycophenolate mofetil monotherapy in liver transplantation: 5-Year follow-up of a prospective randomized trial. Use of mechanical ventilation and renal replacement therapy in critically ill hematopoietic stem cell transplant recipients. Defibrotide for the treatment of severe hepatic veno-occlusive disease and multiorgan failure after stem cell transplantation: A multicenter, randomized, dose-finding trial. Defibrotide for prophylaxis of hepatic veno-occlusive disease in paediatric haemopoietic stem-cell transplantation: An open-label, phase 3, randomised controlled trial.