Buy 25 mg meclizine overnight delivery
The analgesic properties are independent of the antidepressant effect medicine tramadol generic 25mg meclizine with amex, which requires higher doses, and it has been shown that low doses of amitriptyline (amitriptyline [Elavil] 10 mg) before sleep can have an analgesic effect on chronic pain but have no relationship to the antidepressant actions that require doses up to 20 times greater. These medications often need to be taken for several months and patients must be counseled appropriately; fluoxetine (Prozac) may, in fact, increase bruxism and anxiety and should be carefully monitored. Commonly Used Muscle Relaxants Generic Carisoprodol Chlorzoxazone Meprobamate Methocarbamol Cyclobenzaprine Orphenadrine Diazepam Combination Fixed Dosage Meprobamate Aspirin Orphenadrine Aspirin Caffeine Brand Rela, Soma Paraflex, Parafon Forte D. Miltown, Equanil Robaxin Flexeril Norflex, Disipal Valium Equagesic Norgesic Physical Therapy Many factors contribute to limited range of mandibular motion, including muscular pain or spasm, anterior disk displacement (closed lock), pathologic lesions, traumatic injuries. Initial, mild, or acute symptoms can be managed with soft diet, jaw rest, alternating heat and ice packs, jaw/tongue posture opening exercises, lateral jaw movements, and passive stretching exercises. Once again, the precise sequence of exercise therapy is determined on an individual basis as well as the experience of the clinican or physical therapist and is usually based upon the chronicity of the problem, the degree of pain, and the magnitude of limitation of jaw function. Further reduction of pain and inflammation may require an office-based physical therapy program. Immobilization may cause degenerative cartilagenous and osseous changes to the articulating joint surfaces, significant synovial fluid alterations, and changes to the surrounding tissues. Prolonged reduced jaw motion results in rapid muscle fatigue, muscle weakness, and fibrous tissue contractures. Local Anesthetics Act on nerve cell membrane to prevent generation and conduction of impulses. The patient continues the movement while the clinician applies light pressure in the same direction, and in the last stage of the technique, the mandible is moved to the opposite side with patient assistance. The mandible is then moved downward and forward, while the patient is instructed to protrude and move the jaw laterally, and open the mouth while the clinician manipulates the jaw. After this movement, the mandible is manipulated posteriorly so that the condyle is positioned in a posterosuperior position within the glenoid fossa. Only 18% of the patients received significant benefit from the manipulation, and the more advanced the disk displacement the lower the success of the treatment. Nevertheless, there is no shortage of recommended jaw exercises, and care must be taken to first do no harm (Table 48-14). The use of both cold and heat can alleviate muscle pain and play an equal role during jaw stretching and muscle strengthening exercises. One regimen allows the patient to activate, for example, the suprahyoid muscles (geniohyoid, mylohyoid, digastric, and stylohyoid), thereby inactivating the elevators of the jaw (medial pterygoid, masseter, temporalis). This may allow for relaxation of hyperactive muscles of mastication and may assist in increasing maximal interincisal opening. In the active stretch phase, patients are advised to keep their mouth open for several seconds and then relax the muscles. They are instructed to open their mouth until just before they perceive pain, and then to hold for several seconds, and repeat this exercise several times a day, with a gradual increase in the magnitude of mouth opening. An active lateral stretch exercise, which permits the contralateral lateral pterygoid to be stretched, may be accomplished by visualizing the movements in a mirror. In the active protrusion exercise, also performed in front of the mirror, the mandible is protruded forward while stretching the lateral pterygoid muscles bilaterally. All active movements or excursions are maintained for several seconds, and then slowly released, in order to effect a physiologic "stretch" of the muscles. Isometric exercises have been recommended for patients with severe pain and trismus, and there is no movement during isometrics while the depressor muscles are activated, allowing for relaxation of the opposing elevator musculature (medial pterygoid, masseter, and temporalis). These exercises are typically performed by holding the mandible in a stationary position as the muscles are activated isometrically. The lateral pterygoid muscles may also be exercised in a similar isometric fashion. A physical therapist typically applies refrigerant sprays superficially on the skin surface in a sweeping motion followed by active stretching of the jaw musculature. Cold therapy should be used with caution because of the potential for increased joint stiffness, muscle contracture, and decreased jaw mobility. Cold can also have analgesic effects when applied immediately after a therapeutic exercise regimen. The "stretch and spray technique," initially described by Modell and Simons,42 and later modified by Travell and Simons,41 remains a mainstay of office physiotherapy. The therapist holds the fluoromethane spray approximately 30 to 45 cm from the patient and sprays in a sweeping motion multiple times; this is then followed by active jaw stretching exercises. Possible side effects include superficial skin frostbite and, as mentioned, the potential for increased joint stiffness limiting the jaw exercise regimen. Many physical therapists follow the cryotherapy sprays with moist heat to prevent the jaw muscles from undesirable contracture. Ultrasonograpy and Phonophoresis Deep heat may also be delivered by ultrasonography or phonophoresis. The ultrasound probe is applied to the skin using an acoustic conductive gel, then moved slowly over the affected area in small, circular movements. The operator must be careful not to keep the machine in one place for too long as it may cause overheating of the connective tissue, causing structural damage. The deep heat is intended to increase blood perfusion to the area via vasodilation, clearance of inflammatory mediators from the area, decreasing pain and increasing jaw mobility. The beneficial effects to joints include reduced capsular contracture, breakdown of local calcium deposits, and decreased hyaluronic acid viscosity of the joint synovial fluid with improved mobility. Phonophoresis is an application of ultrasound heat therapy that incorporates a pad filled with a steroid or anesthetic cream that is placed over the affected area. The most common indication for phonophoresis is synovitis associated with painful jaw hypomobility. Contraindications for the use of ultrasonography and phonophoresis include areas that may have a reduced blood circulation, fluid-filled organs, eyes, radiation therapy sites, and malignant tissues, and ultrasound therapy should be used with caution over active bone growth centers. The precise mechanism of action is unknown, although it has been suggested that the gate control theory, counterirritation, neurohumoral substance release, and peripheral blockade mechanisms are all involved. It is used in an attempt to decrease muscle pain and hyperactivity and for neuromuscular reeducation. The patient can control the settings with variable frequency, amplitude, waveform, width, and pulse modes. Treatment may last for several hours and relies on biofeedback from the patient in the control of the specific delivery of the stimulation. The positive polarity produces vasoconstriction, whereas the negative polarity produces vasodilation. The positive polarity reduces nerve irritability, and negative polarity enhances nerve conduction and also softens the affected soft tissues. As mentioned previously, phonophoresis uses ultrasonic waves to transmit molecules of drug through the skin, whereas iontophoresis uses low-level electric current. Iontophoresis transfers ions from a solution through intact skin by passing a direct current between two electrodes. High-volume stimulation (100 V): pumping effects of muscle contraction increase circulation. The deep penetration of the medication also aids in the treatment of severe joint inflammation and pain (Table 48-15). Trigger Point and Muscle Injections A trigger point is an area of hyperirritability in a tissue that, when compressed, is locally tender and hypersensitive and results in referred pain and tenderness. When a needle penetrates this area, it may cause a twitch response and referred pain. A vasodilator effect of the local anesthetic may improve vascular perfusion to the area, thereby allowing harmful metabolites or inflammatory mediators, which may induce pain, to be more readily removed by the increased blood flow to the area. The major limitation of the use of these techniques is the difficulty required to motivate patients with pain to engage in jaw exercise regimens (Table 48-16). Acupuncture uses the relationship between energy flow through meridians, natural elements, and positive and negative life forces. There are several theories regarding the mechanism of action of acupuncture and acupressure.
25 mg meclizine with mastercard
Deltopectoral skin flap as a free skin flap revisited: further refinement in flap design treatment synonym buy meclizine 25 mg free shipping, fabrication and clinical usage. The fasciocutaneous cervicopectoral rotation flap for lower cheek reconstruction: report of three cases. The temporalis muscle flap in reconstruction of intraoral defects: an appraisal of the technique. Reconstruction of intraoral defects after cancer surgery using cervical pedicle flaps. The reconstructive surgeon has many techniques at his or her disposal for realizing these goals; often, this requires complex decision making as to which techniques will yield the best outcome. These decisions should be made by evaluating the patient and the defect on a case-by-case basis. Clearly, the myriad of techniques available to the reconstructive surgeon each have their own merits and demerits and the most ideal technique for one patient may not be adequate for the next. This chapter outlines many of the major options in soft tissue and bony reconstruction. Many smaller defects of the oral cavity may be amenable to simpler techniques for reconstruction such as primary closure, skin grafting, secondary intention, or random pattern local flaps. The Classification of Muscle Flaps Type 1 Type 2 One vascular pedicle One dominant vascular pedicle plus minor pedicles (most common pattern) Two dominant pedicles Segmental vascular pedicles One dominant vascular pedicle and secondary segmental vascular pedicles Gastrocnemius, rectus femoris, tensor fascia lata Abductor digiti minimi, abductor hallucis, biceps femoris, flexor digitorum brevis, gracilis, peroneus longus, peroneus brevis, platysma, semitendinosis, soleus, sternocleidomastoid, temporalis, trapezius, vastus lateralis Gluteus maximus, rectus abdominis, serratus anterior, semimembranosus Extensor digitorum longus, extensor hallucis longus, flexor digitorum longus, flexor hallucis longus, sartorius, tibialis anterior Pectoralis major, latissimus dorsi described in numerous articles throughout our literature and are not covered in this chapter. Instead, the authors focus on the use of regional or distant soft tissue and bone for reconstruction of more complex defects in the head and neck. The authors have attempted to detail the procedures, advantages, and disadvantages in a concise and objective manner. Most regional and distant flaps are based on a vascular pedicle that provides the nutrient inflow and outflow of blood to the transferred tissue. Understanding the variations of the different classifications of muscle-containing flaps is extremely important for the reconstructive surgeon; the studies of the blood supply to muscles reported by Mathes and Nahai1 are primary to this understanding (Table 41-1). The angiosome theory proposes that the human body is composed of approximately 40 blocks of composite tissue, each with its own cutaneous territory supplied by a discrete source vessel. Simply stated, all arteries to the skin travel either directly to their destination (direct perforators) or first travel through other tissues, usually muscle (indirect perforators). Reconstruction of the craniomaxillofacial complex has been a cornerstone of the specialty of oral and maxillofacial surgery, and the reconstructive options for bony defects continue to expand. The use of nonvascularized bone has always been within the everyday realm of maxillofacial surgeons. Recently, the use of microvascular free tissue transfer has become an established and routine reconstructive option in head and neck surgery. Furthermore, it has been embraced by oral and maxillofacial units worldwide wherein free flap reconstruction of such defects is now considered the gold standard of care. As such, this chapter also reviews the commonly used nonvascularized grafts and highlights the advantages as well as disadvantages of their use. Equally, the chapter highlights commonly used microvascular bone flaps and their associated advantages and disadvantages. Their popularity is undeniable owing to proximity, ease of harvest, general reliability, and elimination of the need for specialized instruments and skills for microvascular anastomosis. The main drawbacks of these flaps are the relative limited area of application due to the arc of rotation as well as a limited volume of soft tissue available for reconstruction. Some flaps such as the pectoralis major, temporalis, and latissimus flaps require removal of a relatively large volume of tissue with only a small portion of it used for the actual reconstruction. The combination of these drawbacks has led to an increase in utilization of free tissue reconstruction techniques for head and neck defects. Submental Island Flap the submental island flap was introduced by Martin and coworkers in 19934 and has rapidly increased in popularity in head and neck reconstruction owing to its ease of harvest, accessibility, quality of available tissue, and overall versatility. It can be raised as a cutaneous, musculocutaneous, fasciocutaneous, or osteocutaneous flap and can be utilized as a rotational flap for oral or facial defects as distant as the upper third of the face. This is a consistent branch of the facial artery and arises behind the submandibular gland and crosses anteriorly along the mylohyoid muscle. Here, the artery may pass superficially across the anterior belly of the digastric muscle but passes deep to this muscle 70% of the time. The artery gives off one tow four cutaneous perforators throughout its course,7 which travels through the platysma muscle to the subdermal plexus where it anastomoses with the contralateral artery. This pattern of perfusion allows for reliable skin paddle design that can extend from one mandibular angle to the other. However, split- or full-thickness skin grafting may be utilized in cases in which primary closure cannot be obtained. The facial artery may be ligated distal to the take-off of the submental artery, providing a modest increase in pedicle length. Finally, one or both of the submental artery or vein may be divided and anastomosed to a suitable recipient vessel nearer to the defect. The quality of this donor site is analogous to the skin of the radial forearm flap. Therefore, this flap is well suited for moderate-sized defects of the tongue, floor of mouth, and buccal mucosa. In facial reconstruction, the hair-bearing nature of the submental skin in males and some females must be considered before its use. If a neck dissection is included in the treatment of an oral cavity malignancy, the vascular pedicle must be dissected through the primary lymphatic drainage basin of many of these, tumors which may compromise the oncologic safety of the resection. Some authors have advocated close dissection of the pedicle of this flap in these circumstances to avoid leaving a significant amount of fibroadipose tissue surrounding the vessels. The neck skin can be pinched to determine the maximum dimension of the flap that will facilitate 895 primary closure; otherwise, skin grafting will be required. The dissection is in the subplatysmal plane on the contralateral side of the skin paddle, and because this dissection proceeds toward the pedicle, it is carried over the contralateral anterior belly of the digastric muscle and the mylohyoid muscle in the midline of the neck. The ipsilateral anterior belly of the digastric muscle is detached at the inferior border of the mandible and at the common tendon and included in the flap. The facial artery is usually easily identified behind the submandibular gland as it passes behind the posterior belly of the digastric muscle. It can then be traced distally either through or posterior to the submandibular gland where numerous glandular branches will be encountered and ligated. The submental artery is then dissected off its deep attachments and the distal facial artery can be ligated. The nature of the submental skin makes it particularly useful for tongue, floor of mouth, and buccal mucosa defects. Facial skin can be reconstructed ranging from lips and cheeks as well as the temporal region. Submental flap elevated in the subplatysmal plane until the ipsilateral anterior belly of the digastric. This muscle is incorporated in to the flap by detaching from the mandible and at the common digastric tendon. Anterior and posterior deep temporal arteries and the middle temporal artery (branch off the superficial temporal). First introduced in 1898 by Golovine,12 it is known as one of the oldest muscular flaps in use today. The main disadvantages include a relative lack of soft tissue available for reconstruction, minimal application due to arc of rotation limitations, as well as a contour deformity of the donor site and over the zygoma. Of course, these last two concerns have been addressed by alloplastic implants or autogenous tissue to minimize the donor site defect and by osteotomy of the zygomatic arch to pass the temporalis muscle and prevent a contour deformity. Based on the deep temporal arteries, the temporalis muscle is classified by Mathes and Nahai1 as a type 2 muscle with one dominant pedicle plus minor pedicles. The second blood supply is from the middle temporal artery, which is a branch of the superficial temporal artery. The muscle originates from the superior temporal line and coalesces to a dense tendon at its insertion to the coronoid process. Caudally, the fascia splits in to superficial and deep layers approximately 2 cm above the zygomatic arch; a layer of fat exists between the two layers. The deep and superficial layers continue caudally to fuse with the periosteum of the zygomatic arch.
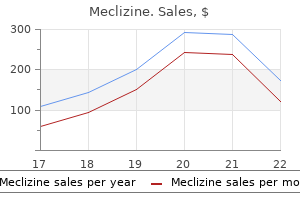
Generic meclizine 25mg otc
All functional dental contacts result from a combination of condylar guidance of movement along with neuromuscular influences medicine mart discount meclizine online amex. This complex, harmonious masticatory system is capable of broad adaptation over time, but the sudden alterations produced by condylar fractures can create certain expected typical clinical findings of functional alterations. Ipsilateral Laterognathia For unilateral fractures, there may be no obvious open bite malocclusion, whereas there may be a laterognathia toward the side of the condylar injury. Ipsilateral Deviation on Opening the opening path of the mandible often becomes an arcshaped deviation toward the side of the condylar injury. Often, this is a first contact followed by a rocking motion of the mandible in to a position of maximum intercuspation. Thus, although the final occlusion may appear normal, careful observation of the path of closure will reveal this functional derangement. Occlusion in a bilateral condylar fracture: a wedge shape open bite with bilateral posterior contacts. Perhaps the most straightforward classification system from a clinical perspective is discussed in the following sections. Balancing Side Occlusal Interferences during Contralateral Mandibular Translation Patients with unilateral condylar fractures may manifest occlusal interferences on the balancing side during attempted contralateral translation of the mandible (during movement to the side opposite the injury). When performing contralateral jaw movement, the functionally shortened ramus on the injured side will cause balancing side interferences, often not allowing unimpeded working side contacts. In addition, limitations in the amount of contralateral lateral excursion may be present. Limitation of Mouth Opening Trismus in the condylar fracture patient may be due to functional interferences of the fracture segments, coronoid impingement, concomitant joint hemarthrosis or to pain from splinting. Anatomic Types of Condylar Fractures Various classifications of condylar fractures have been proposed based upon location, displacement, or resultant functional alterations. There are numerous condylar fracture classifications including those of Brophy,2 Thoma,3 Rowe and Killey,4 and Dingman and Natvig. A classification system based upon functional aspects has not been developed, although Zide and Kent6 attempted to outline those fracture types that would benefit from open versus closed reduction techniques. The patient exhibits bilateral posterior cross-bites and open bite with wide face. An understanding of the preinjury state is important in assessing the results of treatment of subcondylar fractures. Such an evaluation performed in population research studies indicates that pain, deviation, other jaw excursion problems, and joint noise are very frequently present. Although Pullinger and coworkers7 reported on the orofacial and temporomandibular assessment of dental students without condylar fractures and found that 29% had joint noise and 14% had pain, the reader of outcome studies of fractures of the mandibular condyle must consider how a treated population might differ from one that has no injuries. A review of the pertinent studies of condylar fracture treatment will offer an interpretation of the evidence. Each of the clinical studies of condylar fractures suffer from the same biases of addressing too many variables in an inconsistent manner and the problems of developing a comparative study with so many critical success factors that may influence outcome. The surgeon benefits by developing a detailed understanding of the complicated mixture of factors affecting the outcome of condylar fracture treatment. In other words, the studies of functional derangements in closed reduction patients should be compared with studies in normal subjects. One of the first, largest, and most historically important evaluations of closed treatment was performed by MacLennan in 1952. He identified a clinically apparent deformity or malfunction in only 6% of the cases in his series. These were not subjective complaints of the patient, but only those signs on physical examination observed by the clinician. This is not surprising, considering that the occlusal disturbances resulting from closed treatment are usually subtle. Small deviations of the chin, laterognathia, or modestly decreased range of motion are rarely detected by the patient. Park and colleagues10 demonstrated that adverse outcome of closed treatment was dependent upon the location of the fracture and that intracapsular condylar head fractures have the highest incidence of malfunction. Neizen and associates11 recently evaluated closed treatment of condylar fractures in 114 patients assessed before treatment and 1 year posttreatment. The results of closed treatment included 9% of patients still complaining of pain, and 24% describing their occlusion as "fair" or "poor. Because the mandible is not in function during opening and appears only to be limited functionally by the amount of opening, the value of studying deviation remains unclear. McKlennan was the first investigator to systematically demonstrate the efficacy of closed treatment. Subsequently, further objective evaluation of closed treatment has included studies of facial symmetry using radiographic clinical analysis. Ellis and Throckmorton12 performed this evaluation after closed and open reduction of condylar fractures. In the 2 years of the study, the mean shortening of ramus height in the closed reduction group was only 2 to 5 mm. This study does not indicate a functional shortening of the ramus in that the articulation of the condyle simply moved further down the articular eminence and in general permitted maintenance of function and occlusion through a new articular position of the condylar head. Closed Treatment of Condylar Fractures the goals of closed treatment, a more appropriate designation than closed reduction because in most cases no "reduction" of the fracture is performed, include rehabilitation of mandibular function along with restoration of the preinjury occlusion. Closed treatment consists of reestablishing the preinjury occlusion with arch bars or other appropriate appliances. Whereas some clinicians use a brief 1- to 3-week period of maxillomandibular fixation, as described by Walker,8 many contemporary surgeons no longer use continuous maxillomandibular fixation. In the alternative, immediate guiding elastics are used to guide a functional path of movement and correct occlusion. Early functional rehabilitation with range of motion exercises and promoting excursion of the mandible away from the fracture site are additional hallmarks of closed treatment. Active physiotherapy can also include passive movement with or without task-specific devices and other manual manipulation of the jaw. As mentioned, closed treatment of a condylar fracture is not the same as closed reduction. Although improvements in radiographic appearance and displacement do occur, mandibular function is generally restored owing to functional neuromuscular adaptation and also to the condyle functioning further down the articular eminence. Muscle and joint proprioception will guide mandibular movement against a physiologic range of osseous and dental relationships. Thus, small changes in bone contact and tooth occlusion can be accommodated by this response. Does closed treatment of a condylar fracture carry with it a risk of complication and treatment failure that is decreased with open reduction If closed reduction results in an unacceptable incidence of complications with real clinical significance, then overcoming the obstacles to open reduction is an important goal of treatment. To understand the sequelae of condylar fractures, a clinician should include evidence from a nonconcurrent control group, namely, patients who have not sustained condylar fractures. Understanding the baseline of temporomandibular joint function in noninjured adults offers help in assessing how the macrotrauma of a fracture is adapted to over the course of time after closed treatment. The patients available for long-term follow-up offered patient-centered views of the results of their conservative therapy. These patients reported a self-perception of normal mouth opening, but when measured clinically, the maximum interincisal opening was only 34 mm. Whereas a report of restriction of jaw movement by a patient is variable, many clinicians use 35 mm as a guide to maximum interincisal opening that will not be a concern to patients and as a guide to successful functional recovery. In a careful study of closed treatment condylar fracture patients and controls, Murakami and colleagues16 identified only subtle, and seemingly insignificant, differences at 6 months postinjury, and these differences included a greater bite force on the side of injury and diminished lateral excursion away from the side of injury. These findings had continued to diminish in the 6 months after injury and indicated that closed treatment is a viable contemporary option for condylar fracture rehabilitation. There are also many attempts to define those cases of condylar fracture at risk for problems after closed treatment. This information could guide surgeons in to determining who would benefit from open reduction. Lyons Club used patient self-assessment as an essential feature of their review of 120 patients. Silvennoinen and associates18 noted malocclusion in 13% of patients; other complications of treatment were also noted. They contended that "problematic condylar fractures can often be identified preoperatively. A patient with a condylar fracture who cannot obtain a full occlusion will most likely have a shortened ramus on the affected side.
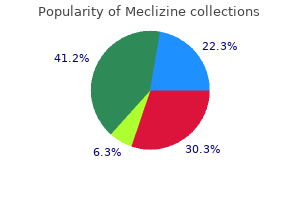
Meclizine 25mg with amex
The orthokeratinized odontogenic cyst should symptoms schizophrenia generic meclizine 25mg with amex, therefore, be placed in a different category. These cysts usually appear as unilocular radiolucencies, but occasional examples have been multilocular. A majority of these cysts are encountered in a lesion that appears clinically and radiographically to represent a dentigerous cyst, most often involving an unerupted mandibular third molar tooth. Histologically, the epithelium is thin and orthokeratinized, and a prominent palisaded basal layer, characteristic of the odontogenic keratocyst, is not present. The reported rate of recurrence of 2% is far lower than the previously quoted statistics for recurrence of the odontogenic keratocyst. This 12-year-old shows some of the clinical features of the nevoid basal cell carcinoma syndrome including mandibular prognathism. The discovery of multiple odontogenic keratocysts is usually the first manifestation of the syndrome that leads to the diagnosis. For this reason, any patient with an odontogenic keratocyst should be evaluated for this condition. The clinical, radiographic, and histologic information permitted a diagnosis of nevoid basal cell carcinoma syndrome. The father had previously undergone the removal of one odontogenic keratocyst of the anterior maxilla. The treatment of the odontogenic keratocyst in patients with nevoid basal cell carcinoma syndrome can be difficult owing to the large number of "recurrences" in these patients. As a matter of point, the author chooses to refer to these "recurrences" as new primary cysts owing to the autosomal dominant penetrance of the syndrome and cyst development. It is certainly possible that many of these cysts are persistent, particularly when considering how common it can be to retain rests of the dental lamina when enucleating an odontogenic keratocyst. Whatever the mechanism, a resection hardly seems to be warranted when managing a syndromic cyst. Glandular Odontogenic Cyst the glandular odontogenic cyst (sialo-odontogenic cyst) is a rare and recently described cyst of the jaws that is capable of aggressive behavior and recurrence. Although it is generally accepted as being of odontogenic origin, it shows glandular or salivary features that seem to point to the pluripotentiality of odontogenic epithelium because cuboidal/columnar cells, mucin production, and cilia are noted in these cysts. Glandular odontogenic cysts occur most commonly in middle-aged adults, with a mean age of 49 years at the time of diagnosis. Plantar pitting can be observed by immersing the foot in povidone-iodine solution followed by a conservative wash of the foot with saline. A red rubber catheter was fashioned (A) and placed in the cyst cavity after suturing the lining of the cyst to the oral mucosa (B). C and D, the marsupialization procedure permitted effective decrease in the size of the cyst so as to permit retention of the teeth and removal of the residual cyst after 9 months. There is a histologic similarity between the glandular odontogenic cyst and the predominantly cystic intraosseous mucoepidermoid carcinoma. Waldron and Koh30 reviewed the similarities between the two lesions and concluded that it is entirely possible that some cases previously diagnosed as central mucoepidermoid tumors may be reclassified as examples of glandular odontogenic cysts. Some authors, however, point to a recurrence rate of approximately 30% and, therefore, recommend resection. Although designated as a cyst, some investigators provide evidence for subclassification as a neoplasm as well. Ghost cell keratinization, the characteristic microscopic feature of this cyst, is also a defining feature of the cutaneous lesion known as the calcifying epithelioma of Malherbe or pilomatrixoma. A and B, this glandular odontogenic cyst presented as a unilocular radiolucency of the anterior mandible crossing the midline. Patients range in age from infant to elderly, with a mean age of occurrence of approximately 30 years. The radiopaque structures within the lesions have been described as either irregular calcifications or toothlike densities. This calcifying odontogenic cyst appears as a mixed radiolucent/radiopaque lesion on the occlusal radiograph. Compound type Complex type Calcifiying cystic odontogenic tumor Dentinogenic ghost cell tumor Tumors with Mesenchyme and/or Odontogenic Ectomesenchyme with or without Odontogenic Epithelium Odontogenic fibroma Odontogenic myxoma/myxofibroma Cementoblastoma *As noted in the section of odontogenic cysts, the odontogenic keratocyst has been considered recently to represent a benign cystic odontogenic tumor. Owing to the lack of universal acceptance of this theory, the odontogenic keratocyst is included in the classification of odontogenic cysts as well as in this table of benign odontogenic tumors. Like normal odontogenesis, odontogenic tumors demonstrate varying inductive interactions between odontogenic epithelium and odontogenic ectomesenchyme. This ectomesenchyme was formerly referred to as mesenchyme because it was thought to be derived from the mesodermal layer of the embryo. It is now accepted that this tissue differentiates from the ectodermal layer in the cephalic portion of the embryo; hence, the designation ectomesenchyme. Odontogenic tumors are typically subclassified by their tissues of origin (see Table 29-3). Tumors of odontogenic epithelium are composed only of odontogenic epithelium without any participation of the odontogenic ectomesenchyme. A, A 65-year-old woman with a large mass of the anterior mandible that showed a neoplastic (solid) calcifying odontogenic cyst on incisional biopsy. A third group, tumors of odontogenic ectomesenchyme, includes those tumors composed principally of ectomesenchymal elements. Although some odontogenic epithelium may be included within these lesions, it does not appear to play an essential role in their pathogenesis. The frequency of odontogenic tumors seems to be geographically determined (Table 29-4). Studies from North America seem to indicate that odontogenic tumors represent approximately 1% of all accessions in oral pathology laboratories,36,37 whereas African studies have a much higher incidence of odontogenic tumors. A 17-year-old girl with obvious facial expansion (A) related to a multilocular radiolucency of the left mandible associated with impacted tooth no. A Ameloblastoma the ameloblastoma is the most common clinically significant and potentially lethal odontogenic tumor. Excluding odontomas, its incidence equals or exceeds the combined total of all other odontogenic tumors. These tumors may arise from rests of the dental lamina, a developing enamel organ, the epithelial lining of an odontogenic cyst, or the basal cells of the oral mucosa. In an analysis of the international literature, 3677 cases of ameloblastoma were reviewed, of which 92% were solid or multicystic, 6% were unicystic, and 2% were peripheral. About 85% of this variant of the ameloblastoma occur in the mandible, most commonly in the molar/ramus region. Buccal and lingual cortical expansion is common, frequently to the point of perforation. Twenty years of undisturbed growth of a solid/multicystic ameloblastoma led to significant facial disfigurement (A), with an impressive radiographic appearance (B). Unfortunately, although most agree that aggressive treatment is essential for cure of this tumor, the fact remains that a consensus has not been reached on the biologic behavior of this neoplasm and how best to treat it. Conflicting opinion, extending backward in time, has served both to educate and to confuse, and it has been left to generations of surgeons to sift and interpret what they consider to be clinically valid. Therefore, the actual margin of the tumor often extends beyond its apparent radiographic or clinical margin. These must be realized as persistent disease because the tumor was never controlled from the outset. When a small burden of tumor is left behind, it may be decades before this persistent disease becomes clinically and radiographically evident, and long after a surgeon falsely proclaimed the patient to be cured. Owing to the highly infiltrative and aggressive nature of the solid or multicystic ameloblastoma, the author recommends resection of the tumor with 1. In this latter tumor, stellate reticulum is not present in the central portions of the nests. One additional exception surrounds the desmoplastic variant, which is generally not a radiolucent tumor radiographically owing to its high content of collagenized stroma. B, the effectiveness of the bony linear margin should always be evaluated by intraoperative specimen radiographs. Unfortunately, any less aggressive treatment modality may be fraught with inevitable persistence discovered at variable times postoperatively.
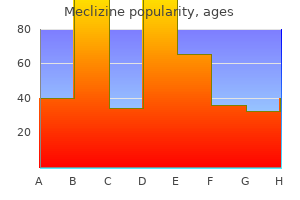
Purchase meclizine paypal
Benign metastasizing pleomorphic adenoma of the parotid gland: a clinicopathologic puzzle symptoms lupus buy 25 mg meclizine amex. Phenotypes in canalicular adenoma of human minor salivary glands reflect the interplay of altered secretory product, absent neuro-effector relationships and the diversity of the microenvironment. Primary high-grade mucoepidermoid carcinoma of the minor salivary glands with cutaneous metastases at diagnosis. Polymorphous low-grade adenocarcinoma versus pleomorphic adenoma of minor salivary glands: resolution of a diagnostic dilemma by immunohistochemical analysis with glial fibrillary acidic protein. Adenoid cystic carcinoma and polymorphous low-grade adenocarcinoma of minor salivary glands: a comparative immunohistochemical study using the epithelial membrane and carcinoembryonic antibodies. Polymorphous low-grade adenocarcinoma of the major salivary glands: report of three cases in an unusual location. Polymorphous lowgrade adenocarcinoma of minor salivary glands: a study of 17 cases with emphasis on cell differentiation. Polymorphous low-grade adenocarcinoma of the salivary glands with transformation to high-grade carcinoma. The role of radiotherapy for patients with adenoid cystic carcinoma of the salivary gland. Results of fast neutron therapy of adenoid cystic carcinoma of the salivary glands. Factors influencing survival rate in adenoid cystic carcinoma of the salivary glands. Adenoid cystic carcinoma of the minor salivary glands: long-term survival with planned combined therapy. Radiotherapy for advanced adenoid cystic carcinoma: neutrons, photons or mixed beam Face-lift approach combined with a superficial musculoaponeurotic system advancement flap in parotidectomy. In general, these can be divided in to those caused by pathogenic microorganisms (infectious stomatitis) and those not infectious in etiology (noninfectious stomatitis). In addition, this chapter addresses pigmented lesions, a common clinical manifestation of a variety of conditions. Patients initially develop primary syphilis through intimate physical contact with an infected person. Most chancres occur genitally, but the oral cavity is the most common extragenital site affected. Chancres tend to be asymptomatic, and most lesions heal without treatment within a couple months. Many patients then progress to secondary syphilis, which is disseminated and characterized by constitutional symptoms and a generalized maculopapular rash of the skin, commonly affecting the palms and soles. Occasionally, verrucous or papillary lesions develop in secondary syphilis and are known as condyloma lata. Some patients develop large areas of necrotizing granulomatous inflammation known as gummatous necrosis or a gumma. Most frequently, oral lesions present as enlarging ulcers or periodontal involvement. Historically, the body reacts to the organism with granulomatous inflammation and the granulomas are typically necrotizing. Type-1 causes predominantly oral disease, and type-2 predominantly genital disease. With the increasing frequency of orogenital sex, crossover is common, but the clinical manifestations of infection are not significantly altered by the type. A small percentage, generally fewer than 10%, of initially exposed patients become clinically ill. Because these patients have no prior immunity, the primary infection is severe and the primary target is the oral cavity. The primary infection is acute and explosive in its onset and characterized by a generalized and somewhat symmetrical stomatitis. Technically, the infection is vesiculobullous in nature but intact vesicles are rarely seen because the roof of the vesicles is very thin and invariably ruptures once formed. Lesions can affect any mucosal surface and are very painful, and patients are invariably febrile with symptomatic adenopathy. The infection resolves spontaneously in 7 to 10 days, but the pain, particularly in children, makes eating and drinking a problem; dehydration can be a significant medical complicating factor. The virus has the ability to be reactivated and travel down the nerve to produce recurrent bouts of infection. Because the patient has been previously exposed to the virus and has some immunity, the recurrent or secondary infection tends to be milder and much more localized. In most instances, it affects the lips, most commonly at the junction of the vermilion and skin. Most patients have a prodrome tongue may undergo atrophy with keratosis known as syphilitic glossitis. The incidence of syphilis has markedly declined because the infection is amenable to antibiotic regimens, particularly benzathine penicillin G. In the United States, incidence has decreased dramatically, due in part to a national gonorrhea control program, but approximately 600,000 new cases occur annually. The diagnosis can be made from smears or culture, and uncomplicated infection responds well to a single dose of ceftriaxone 125 mg intramuscularly. Most viral infections induce neutralizing antibodies and the immune system destroys the virus. The herpesviruses are somewhat unique in that once they enter the body, they are not destroyed but are characterized by latency in which they remain dormant but have the ability to be reactivated, producing recurrent patterns of infection. B A and B, Multiple sharply marginated ulcers of primary herpetic gingivostomatitis. In healthy patients, involvement is site-specific and tends to affect only masticatory mucosa or mucoperiosteum; hard palate, or attached gingiva. Recurrent intraoral herpetic infection is often confused with aphthous ulcers, but aphthous ulcers occur almost exclusively on the lining mucosa, not the mucoperiosteum, and tend to be larger and fewer in number. If doubt exists, however, culture is reliable but inefficient and the diagnosis can be confirmed by cytologic smear. The vesicles/ulcers should be scraped with a blunt instrument like a tongue blade and spread on a glass slide. Alternatively, a few drops of alcohol can be placed on the slide and allowed to air dry. Herpetic infections are self-limiting and often require no treatment, but effective antiviral therapy is available. The literature is mixed on the efficacy for topical antiviral therapy, but for therapy to be effective, it must start at prodrome when viral replication is beginning. When treating topically, it is imperative for patients to be instructed to apply the medication with a covered finger in order to prevent herpetic whitlow. Valacyclovir is metabolized in to a more bioavailable form of acyclovir and is effective at 500 mg twice daily for 5 to 7 days. The diagnosis is usually confirmed by the Paul-Bunnell test, which detects heterophil antibodies. In immunocompetent patients, infection tends to be asymptomatic or produce mild flulike symptoms. Coxsackievirus Coxsackieviruses are enteroviruses that tend to produce epidemic outbreaks in children. The group A viruses produce herpangina, hand, foot, and mouth disease, and lymphonodular pharyngitis. There is significant clinical overlap among these infections, and they are not always caused by distinct strains of the virus. Herpangina is febrile and tends to produce flulike symptoms with sore throat and pharyngitis characterized by erythema with vesicles and shallow ulcers. Similar outbreaks with involvement of the hands and feet are known as hand, foot, and mouth disease. Other outbreaks produce hyperplasia of the small lymphoid aggregates in the palatal mucosa known as lymphonodular pharyngitis. Chickenpox is self-limiting, but once a person is infected, the virus is neurotrophic and travels up sensory nerves to remain latent in sensory ganglia. The eruption is painful and most often affects the trunk, but trigeminal distribution is the second most frequent. Herpes zoster of the external auditory canal with auditory symptoms and facial paralysis is known as Ramsay Hunt syndrome. Infection in young children tends to be asymptomatic, Fungal Infections Most fungi are of relatively low virulence and tend to produce opportunistic infection when alterations of host or environment provide a favorable setting for fungal growth.
Persely (Parsley). Meclizine.
- Dosing considerations for Parsley.
- Are there any interactions with medications?
- Are there safety concerns?
- How does Parsley work?
- What is Parsley?
- Kidney stones, urinary tract infections (UTIs), cracked or chapped skin, bruises, tumors, insect bites, digestive problems, menstrual problems, liver disorders, asthma, cough, fluid retention and swelling (edema), and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96771
Purchase meclizine 25 mg fast delivery
Nevi are subclassified histologically according to the location of the proliferating nevus cells relative to the overlying epithelium medicine 5277 order 25mg meclizine with mastercard. Intradermal nevi have nevus cells located separate from the epithelium in the upper dermis and produce elevated, dome-shaped nodular masses that may be sessile or polypoid. Compound nevi, which show nevus cell nests in both the epithelium and the upper dermis, are slightly elevated nodules. Blue nevi are characterized by spindled to oval nevus cells found in the deeper dermal tissues; they tend to produce elevated, flat-topped nodules with a distinctive blue color. Dysplastic nevi may be a precursor to melanoma, particularly when the lesions are multiple and occur in a familial, autosomal dominant pattern. Clinically, the lesions simulate melanoma, being somewhat larger than typical nevi and show irregular and indistinct borders and variation in color. Chronic irritation may predispose a nevus to malignant transformation and those nevi are normally excised. Clinical changes in a preexisting nevus may herald development of melanoma and also prompt removal. Intraoral lesions tend to be less deeply pigmented than skin lesions, with more than 20% lacking melanin pigmentation entirely, presenting instead as normal-colored nodular masses. Clinically, they may resemble nevi and, thus, should be included in the differential diagnosis with nevi. They commonly do not begin to appear until age 30, a helpful contrasting feature to nevi, and they become more prevalent rather than less prevalent with increasing age. The etiology is likely multifactorial, with race and genetic factors having a strong influence. The incidence of most types of melanoma corresponds best with excessive sunburning early in life, and the lifetime risk of developing melanoma is not believed to increase significantly after the third decade of life. This group includes individuals with fair complexion and blue eyes, often with red hair. These individuals burn easily and tan poorly and often show mottled skin pigmentation with excessive freckling. During the radial growth phase, melanoma cells grow along the epithelial/connective tissue interface but do not invade in to the deeper dermis where access to blood vessels and the potential for distant metastasis are greater. Once a lesion enters the vertical growth phase, however, vascular invasion and perineural spread is commonly seen and metastasis to distant sites is common. Thus, diagnosis of melanoma during the radial growth phase carries a far more favorable prognosis, and the thickness of a lesion becomes the most important prognostic factor. Cutaneous melanomas less than 1 mm in thickness and not ulcerated have a 5-year survival rate of 95% if metastasis is not already present. Patients with documented metastatic disease at a time of diagnosis have a 5-year survival under 20%. They are often described as having a "greasy" surface and "stuck-on" appearance, also helping to separate them clinically from nevi. Chronic sun exposure may be a factor and heredity may play a role as an autosomal dominant familial pattern is seen in many affected individuals. Morbidity and mortality are increasing with this disease owing to its increasing incidence. It is estimated that more than 35% of nodular and superficial spreading melanomas arise within the background of a melanocytic nevus. These lesions have been shown to remain in the radial growth phase for as long as 15 years before demonstrating nodular change and progressing to invasive melanoma. Superficial spreading melanoma is the most common form, representing approximately 70% of the cutaneous lesions. Clinically, the lesions are irregular in outline and show a variation in pigmentation. The surface may also be irregular with nodular foci and/or ulceration developing within an otherwise macular lesion. As the name would indicate, superficial spreading melanoma shows radial growth primarily but progresses to the vertical growth phase more quickly than lentigo maligna and carries a poorer prognosis. Nodular melanoma shows prominent vertical growth early in its development without a significant radial growth phase and is not as strongly associated with sun exposure. It typically presents as a rapidly growing, ulcerated, darkly pigmented mass that is deeply invasive at the time of initial diagnosis. Acral-lentiginous melanoma is the rarest subtype of melanoma but the most commonly seen in black individuals. The palms of the hands, soles of the feet, and underneath the nails are common locations. Intraoral melanomas often present as this subtype and are sometimes referred to as mucosal lentiginous melanoma. Previously, 815 Vascular Lesions Vascular lesions normally present as red to reddish-purple areas and are, therefore, usually easily recognizable as vascular in origin. As the quantity of blood increases, the lesions will darken in color and may be confused with lesions produced by melanin. The normal blood vessels in an area may be markedly dilated, there may be an increased number of blood vessels present in an area, or blood may be spilled from the vessels in to the connective tissue compartment. Lesions produced by dilation of existing blood vessels or proliferation of new blood vessels may blanch with applied pressure over their surface, clearly identifying the intravascular nature of the blood. Lesions produced by blood spillage are often mildly painful on palpation but do not blanch. It usually presents as multiple, small, bright red lesions and can involve any soft tissue site. It can be found at any age but is seen with increased frequency in older individuals. No treatment is necessary, although thrombosed varices are often biopsied because of their firm nature on palpation and the clinical concern to rule out melanoma. Treatment of melanoma consists of assured surgical excision with a wide margin of surrounding normal tissue. Sentinel lymph node dissection now is often performed to assess metastatic status. Radiation therapy is unusual because it is found to be generally ineffective against melanoma. Chemotherapy, immune system modulation therapy, and genetically directed treatment modalities are also being used with greater frequency. Clinically, intraoral lesions often begin as irregular macules that represent the radial growth phase of the lesion, the so-called mucosal lentiginous type of melanoma. Some debate remains as to whether they represent developmental anomalies or true neoplasms. The quantity of blood vessels and their location within the tissue determine the clinical presentation. Intraorally, hemangiomas are red to blue in color, soft to palpation, and usually blanch with applied surface pressure. The color of the lesion is determined by the size of the blood vessels in the lesion. Capillary hemangiomas are normally red; cavernous hemangiomas tend to be blue to purple. Thrombosis within the lesional blood vessels is not uncommon and will produce lesions with a firm, sometimes multinodular character. Whereas any area of the oral mucosa may be involved, the lips, buccal mucosa, and tongue account for a large number of cases. Treatment may not be necessary unless the lesion may be subject to trauma or it becomes a functional or cosmetic problem for the patient. Lesions may begin as macular reddish lesions that subsequently enlarge and become nodular, often ulcerating. Pigmentation increases with increasing size and can produce dark brown to black lesions. Petechiae are defined as pinpoint areas of hemorrhage and are typically associated with breakage of capillary blood vessels. Purpuras are slightly larger, measuring up to 1 cm in diameter, and are often associated with small veins. Ecchymoses are larger than 1 cm and are typically associated with larger blood vessels.
Syndromes
- Call your local emergency number (such as 911) or local hospital for further advice.
- Throat swelling
- Surgery to remove cancerous tissue -- a lumpectomy removes the breast lump; mastectomy removes all or part of the breast and possible nearby structures
- Dress
- DO NOT move the person unless he or she is in danger or near something hazardous.
- Sneeze
- Cancer
- Breathing tube
- Severe change in blood acid levels -- leads to organ damage
Discount meclizine 25mg online
The effects of active infant orthopedics on occlusal relationships in unilateral complete cleft lip and palate symptoms questionnaire cheap meclizine 25mg fast delivery. Language skills of young children with unilateral cleft lip and palate following infant orthopedics: a randomized clinical trial. The comparison of treatment results in complete cleft lip/palate using conservative approach vs. Maxillary arch alignment in the bilateral cleft lip and palate infant, using the pinned coaxial screw appliance. Effect of lip adhesion on labial height in two-stage repair of unilateral complete cleft lip. Nasal symmetry after primary cleft lip repair: comparison between Delaire cheilorhinoplasty and modified rotation-advancement. Nasal symmetry after primary cleft lip repair: comparison between Delaire cheilorhinoplasty and modified rotation-advancement [discussion]. Bilateral complete cleft lip and nasal deformity: an anthropometric analysis of staged to synchronous repair [discussion]. Early correction of the nose in unilateral cleft lip patients using an open method: a 10-year review. Primary repair of the bilateral cleft lip nose: a 15-year review and a new treatment plan. Bilateral complete cleft lip and nasal deformity: an anthropometric analysis of staged to synchronous repair. A preliminary report on one-stage open tip rhinoplasty at the time of lip repair in bilateral cleft lip and palate. The prolabial unwinding flap method for one-stage repair of bilateral cleft lip, nose and alveolus. Craniofacial growth in bilateral cleft lip and palate: ages six years to adulthood. Cephalometric evaluation of facial growth in operated and unoperated individuals with isolated clefts of the palate. A sixcenter international study of treatment outcome in patients with clefts of the lip and palate. Operation der angeborenen totalen spaltung des harten gaumens nach einer neuen methode. The kaleidoscopic world of rare craniofacial clefts: order out of chaos (Tessier Classification). Bilateral buccal flaps with double opposing Z-plasty for wider palatal clefts [discussion]. The doublereversing z-plasty in primary palatoplasty: operative experience and early results. Cleft palate fistulas: a multivariate statistical analysis of prevalence, etiology, and surgical management. If so, at what age is it most appropriate, what material is most ideal, and should adjunctive procedures such as orthodontic expansion be used before or after grafting This chapter reviews what is known, discusses these controversies, and provides a rationale for the approach to the residual alveolar cleft defect. Many cleft patients present with chronic upper respiratory and sinus disease, which may be related to reflux in to the nasal cavity and sinus. There is some evidence that the residual fistula, whether labial or palatal, can have an effect on speech articulation and nasality. There is evidence that closure of the fistula and grafting the cleft defect can improve nasal emission and nasality. Grafting achieves stability of the arch and prevents collapse of the alveolar segments. Grafting provides room for the canine and lateral incisors to erupt in to the arch in to stable alveolar bone and maintains bony support of teeth adjacent to the cleft. Grafting restores continuity not only of the alveolus but also of the maxilla at the piriform rim. This may have a direct aesthetic benefit and may also prove to be of long-term benefit when formal rhinoplasty procedures are performed. To evaluate bone graft success, Bergland and colleagues6 described a semiquantitative approach that divided grafts in to four types based on alveolar crest height. Although this is effective, it has been suggested that occlusal alveolar bone height does not adequately measure success. A modification of the Bergland scale that measures both occlusal and basal bone height may be a better tool for evaluating graft success. Advocates of this approach have not experienced problems with altered facial growth and malocclusion, most likely the result of the limited dissection used in these cases. They have reported improved occlusion and graft success in these patients compared with patients grafted at other ages. This technique may not be possible in all patients, such as those with isolated alveolar clefts without palatal clefting or those in whom segments cannot be orthopedically aligned. In one center, because of these limitations, nearly one half of patients could not be treated with primary grafting. In one study, there was an increased incidence of malformation of permanent lateral incisors in the primary graft group and decreased success of the graft, with only 41% of primary grafts (54% if pregrafting orthopedics was included) resulting in adequate bone height when measured with a Bergland scale. Therefore, it appears at this time that three-dimensional imaging certainly has its place in research but two-dimensional imaging continues to be sufficient for routine monitoring of clinical outcomes. An exception to this might include evaluation of the grafted site for the treatment planning of dental implants after skeletal maturity has been achieved. Outcome measures for various approaches are also defined inconsistently, which makes comparison difficult. Here, alveolar grafting is grouped according to timing as defined later (Table 44-1). Primary Grafting Some define primary alveolar bone grafting as that which is performed simultaneously with lip repair. Still others have defined primary grafting as grafting performed before the palate is repaired. Long-term studies show abnormal maxillary development with maxillary retrognathia, concave profile, and increased frequency of crossbite compared with patients without grafts. Secondary Grafting during the Mixed Dentition (After Eruption of the Maxillary Central Incisors and before Eruption of the Canines) Alveolar reconstruction with grafting during the eruption of the permanent dentition may be best for various reasons. Rationale for grafting and for timing of grafting during this time period include 1. There is minimal maxillary growth after age 6 to 7 years, and the effect of grafting at this time will result in minimal to no alteration of facial growth. General anesthesia is not required for routine orthodontic procedures such as expansion. The donor site for graft harvest is of acceptable volume for predictable grafting with autogenous bone. Factors Contributing to Timing of Grafting during the Mixed Dentition Dental age vs. In some patients, this may be much earlier than the traditionally recommended age for evaluation. Presence of the Lateral Incisor Many proponents of earlier mixed-dentition grafting advocate this timing because of the opportunity to salvage the lateral incisor. The incidence of congenitally missing permanent lateral incisors within the alveolar cleft is between 35% and 60%. Even if the tooth is not perfectly formed, it may still be beneficial to attempt to preserve it. The grafted alveolus will often thin to the point that alveolar width is not adequate for definitive reconstruction with an endosseous implant without additional grafting. Position of the Lateral Incisor If the lateral incisor is mesial to the cleft, it often has adequate space for eruption. However, if the lateral incisor is located in the posterior segment, earlier grafting may be necessary to preserve the lateral incisor.
Meclizine 25mg cheap
Desmoplastic fibroma of the jaws: surgical management and review of the literature symptoms to diagnosis cheap 25 mg meclizine free shipping. Giant-cell reparative granuloma, traumatic bone cyst, and fibrous (fibro-oseous) dysplasia of the jawbones. Central giant cell lesion of the jaw: nonsurgical treatment with calcitonin nasal spray. Central giant cell granuloma of the jaw: a review of the literature with emphasis on therapy options. Limited regression of central giant cell granuloma by interferon alpha after failed calcitonin therapy: a report of 2 cases. Complications of alpha-interferon therapy for aggressive central giant cell lesion of the maxilla. Cysts of developmental origin in the premaxillary region, with special reference to their diagnosis. Radioactive isotope and other investigations in a case of haemorrhagic cyst of the mandible. Disappearing bones: a rare form of massive osteolysis; report of two cases, one with autopsy findings. Treatment of a high-flow arteriovenous malformation by direct puncture and coil embolization. Intraosseous hemangioma of the mandible: a case report and review of the literature. Histiocytosis X: integration of eosinophilic granuloma of bone, Letterer-Siwe disease, and SchullerChristian disease as related manifestations of a single nosologic entity. Multifocal eosinophilic granuloma of the jaw: long-term follow-up of a novel intraosseous corticoid treatment for recalcitrant lesions. However, multiple other malignant lesions can be found in the oral cavity including sarcoma, minor and major salivary gland tumors, mucosal melanoma, lymphoma, or metastatic disease. According to the National Cancer Institute, it is estimated that more than 35,000 new oral and oropharyngeal cancers would be diagnosed and more than 7600 people would die from this disease in 2008. The most recent data on oropharyngeal cancer in the United States demonstrate a 2. In parts of the world, such as Southeast Asia, oral and oropharyngeal cancers account for 8% to 10% of all cancer cases reported. This finding, despite advances in surgical and adjuvant therapies, suggests that earlier diagnosis and prevention are paramount in reduction in oral cancer prevalence and mortality. In the United States, there are also apparent disparities in those afflicted with and dying from oral cancer. Overall, in the United States, there has been a decreasing incidence of oropharyngeal cancer over the last 30 years. Currently, there are data to suggest that specific geographic areas within the United States are showing an increasing oropharyngeal cancer rate, especially in older white males. Even more alarming, when compared with equal stages at the time of diagnosis, African American men have a poorer 5-year relative survival rate compared with other races. A review of trends in 5-year relative survival rates from 2000 to 2005 shows an overall higher incidence and relative mortality rate in African Americans compared with whites1 (Tables 31-1 and 31-2). However, there is an overall reduction in incidence and mortality rates in all races and sexes in this same period compared with earlier data. The curing and heating processes used in manufacturing of the final tobacco product increase these to a much higher level. Polycyclic aromatic hydrocarbons, in particular benzo(a)pyrene, are known to be potent carcinogens. There is an increased risk of developing oral cancer with these products and it should not be viewed as a substitute for tobacco smoking. Alcohol has long been implicated in the development of oral cancer, mainly due to its synergism when used with tobacco. However, a recent pooled analysis demonstrated that heavy alcohol use (>3 drinks/day) in nonsmokers was associated with an increased risk of developing oropharyngeal, hypopharyngeal, and laryngeal cancer when compared with nondrinkers and nonsmokers. No single causative agent has been identified, and many variables likely contribute along the spectrum of normal mucosa to carcinoma. The risk of oral cancer associated with tobacco use is noted to be 2 to 12 times higher than in the nonsmoking population, and up to 95% of individuals with oral cancer will have a tobacco use history. A combination of various carcinogens within tobacco, combined with the heat, may lead to a variable number of genetic mutations in the epithelium of the upper aerodigestive tract. Journal of Clinical Pathology 2006;59:445-453 this cell line continues to undergo clonal expansion. This clonal expansion continues with the cumulative genetic alterations and changes until frank malignancy occurs. The majority of these alterations occur in early mutagenesis, within the change from normal mucosa to premalignant mucosa. There are relatively few changes from a premalignant to a malignant state, thus demonstrating a cumulative effect. Loss of chromosome region 9p21 is found in 70% to 80% of all oral carcinoma and has been demonstrated to be an early event. These have been found to be responsible for p53 degradation and interfere with G1 cell cycle regulation. E7 is believed to be involved with the degradation of Rb, which also disrupts cell cycle regulation. Cancer cells may be described as diploid, tetraploid, or aneuploid based on the number of chromosomes in the cell nucleus. Tumor cells that exhibit diploid chromosomal changes have been noted to have better survival rates. Those with tetraploid and aneuploid features tend to have a worse prognosis and be more resistant to therapy. More significant histologic changes have also been associated with ploidy changes. A precancerous lesion is defined as morphologically altered tissue in which the development of malignancy is more likely than with normal mucosa. A precancerous condition is a condition or generalized disease that does not necessarily alter the appearance of the mucosa but may be associated with a greater risk for the development of cancer. Leukoplakia is defined as a white patch or plaque that cannot be characterized clinically or ascribed to any other pathologic disease. Lesions caused by lichen planus, white sponge nevus, nicotine stomatitis, or other plaque-causing diseases do not qualify as leukoplakia. Leukoplakia is strictly a clinical diagnosis and does not imply any specific histologic diagnosis. Individuals with chronic unprotected exposure to sunlight are at highest risk for development. Ill-fitting dentures, sharp edges on oral prostheses or teeth, or parafunctional oral habits with objects such as toothpicks can be associated with leukoplakia. Obvious traumatic lesions to the buccal mucosa such as the development of a linea alba are not considered leukoplakia. Waldron and Shafer27 in their study of 3,256 lesions submitted to their respective oral pathology departments as "leukoplakia" found that 43% of floor-of-mouth lesions and 24% of both tongue and lip lesions contained some degree of dysplasia or carcinoma. Several studies have also looked at malignant transformation over time and found it to vary from 0. The malignant transformation of these lesions has been studied extensively by Silverman and colleagues. The second year of follow-up in their series exhibited the greatest rate of malignant transformation at 5%. If those lesions initially noted to be dysplastic on biopsy were followed, they had an even higher rate of malignant transformation, at 36. Earlier studies by Silverman and coworkers28,29 found malignant transformation rates of 0.
Order meclizine pills in toronto
Massaging hypertrophic scars has demonstrated marginal effects on the vascularity medicine images order cheap meclizine line, pliability, and height of the scars. Fractures of the facial skeleton in children are less common than in the adult, and only about 1% of facial fractures occur in patients younger than 5 years. This is due to the elastic nature of youthful bone and the smaller facial unit in children that may be exposed to injurious forces. Self-adhering silicone pressure sheets are useful to decrease hypertrophic scar formation in children, particularly over areas of convexity, as in the malar or cheek area as demonstrated in this young child. Mechanism of injury is very important because this may indicate what kind and type of force has been imparted to the craniofacial unit. There will be typically an extensive component of soft tissue injury, both open wounds and edema, that may mask underlying fractures. After several days, the swelling resolves and the typical greenstick fractures return to their anatomic positions much quicker than in the older adult patient. The contemporary high-resolution scanners with less radiation exposure afford the kind of thorough imagery necessary for pediatric facial fracture management. Conversely, there may be traumatically widened sutures, particularly in the skull of young children, that represent true injury and result in hematoma formation or underlying dural tear and must be scrutinized in the early phase of acute management. At birth, the cranium occupies roughly half of the craniofacial unit and, thus, the skull (frontal region) is more frequently injured or fractured than other facial bones. This tendency continues until approximately 6 to 7 years when a reversal in fracture ratios is seen between the skull and the facial bones. This reversal corresponds to the development of paranasal sinuses, elongation and forward projection of the face beyond the frontal area, and the eruption of adult teeth in the anterior jaws. Several studies have evaluated facial fracture incidences and patterns in childhood. The mandible, being a relatively more exposed area during most of childhood, appears to be a target of injury during most of the pediatric developmental period. Small paranasal sinuses and multiple unerupted teeth in children contribute to midfacial skeletal stability and increased resistance to fracture forces and displacement. Extensive swelling over the nasofrontal region often appears to be fractured with laterally displaced nasalorbital bones. Frontal sinus preservation with repair and drainage catheter placed via the nasal cavity in to the nasofrontal duct. The frontal bone thickens with established cortices and a diploe space that absorbs impact forces quite well before a fracture results. The frontal sinus represents an area more susceptible to fracture and fragmentation as the bone thins around the sinus cavity. The frontal sinus generally becomes radiologically evident at approximately age 7 years in most children, though pneumatization is under way via the ethmoids by 12 to 14 months. Frontal sinus fragmentation with displacement of bone fragments in to the sinus or extending intracranially are nearly always seen in older children or adolescents because their frontal sinus has been developed to some extent. Neurosurgical consultation should be obtained if there is intracranial extent of injury. Studies have shown that significant frontal sinus fractures in children are often accompanied by intracranial injury or ocular trauma and are also associated with a higher pediatric injury severity scale and poorer outcomes in recovery than what is observed in adults. Antibiotics are not necessary unless there is a history of chronic sinusitis or surgery is undertaken. Again, current trends maintain sinus cavity integrity with anatomic restoration through fracture reduction and fixation. This catheter can be accessed for periodic lavage of the sinus to maintain the physiologic dynamic of nasosinus health. Frontal sinus comminution occurs less frequently in the pediatric patient than in the adult. In small frontal sinuses, usually stripping the mucosa and obliterating the ductal openings will result in cavity bony fill. This will allow the cranial contents to "herniate" forward and obliterate any retrofrontal space; this will take place over several days. In frontal sinuses larger in volume (typically adolescent males), fat or autogenous bone may be utilized to obliterate the cavity space after the ducts and mucosa have been eliminated. D, Nasofrontal ducts (X) as they interface with the ethmoidal air cells and upper nasal cavity. This may necessitate obtaining dedicated coronal views at 1-mm slices at the orbital apex to determine whether the optic canal contents are involved. Subsequent swelling, pressure, and ischemia of the optic nerve or contents may result, which can be confirmed through serial examinations, if possible, by an ophthalmologist. Often, pediatric patients with entrapment may have none of the typical stigmata of an orbital fracture but will experience associated nausea and vomiting. This is consistent with a "white-eyed" orbital fracture, mostly seen in pediatric patients. For this reason, most orbital wall fractures will improve over several days of observation as the pieces self-reduce to their anatomic positions. Again, bone fragments displaced superiorly and intracranially may result in dural tears and these require neurosurgical repair. The diploe space develops by age 3 or 4 years in most children and may be split to use for orbital wall reconstruction. Rib can also be split, shaped, and placed in the orbit for extensive wall defects. Such fractures become more prevalent with the development of the paranasal sinuses, as is the case with frontal sinus fractures and maxillary fractures. Physical examination demonstrates telecanthus and instability of the medial canthal ligament and central bony fragment. Clinical examination includes the bowstring and Furness tests as well as direct intercanthal measurements. Intercanthal distances are more variable in children, but on average, measurements are approximately 22 mm in infants and increase gradually until adulthood, when approximately 35 mm is the norm. Initial emphasis is placed on restoration of orbital volumes, re-creation of nasal contours, overcorrection of the intercanthal distance, and restoration of midface projection. Transnasal fixation with nonabsorbable sutures is a critical step in surgical reconstruction if the medial canthal tendon insertion is disrupted. Overcorrection is suggested and external bolsters are helpful to support the tissues and prevent pseudotelecanthus. Nasal Complex Nasal fractures are the most common facial fracture in both adults and children owing to its prominent exposure. Patients will often present with considerable nasal bleeding that should be addressed immediately. Clinical examination is usually diagnostic but may be unreliable and difficult in uncooperative children with extensive swelling. Surgical intervention is required for drainage of a septal hematoma, cosmetic deformity, and functional impairment. Closed reduction is typically attempted first with open reduction reserved for complex fractures with loss of projection and stability. After surgical correction, extranasal splinting is ideally accomplished with a molded thermoplastic splint and antibiotic-impregnated intranasal packs, absorbable cellulose, or septal splints. Systemic prophylactic antibiotics for prevention against toxic shock syndrome and endocarditis should be utilized during the packing period. E, Reconstructed fronto-orbital fractures with resorbable fixation and autogenous bone grafts. Such a finding requires prompt surgical intervention to relieve the entrapment, allowing for free range of motion of the eye and prevention of long-term functional sequelae. Alcala-Galiano and coworkers65 reported up to 24% associated ocular injuries with orbital fractures in children; therefore, ophthalmologic consultation should be part of the treatment algorithm. Unless there is vision loss or compromise, permitting edema to dissipate will allow for a more thorough and precise examination. Surgical intervention is best performed within 7 to 10 days in pediatric patients. Findings include maxillary nerve hypoesthesia, malocclusion, trismus, subconjunctival hemorrhage, increased transverse facial dimension, and loss of malar projection. Significant displacement results in increased orbital volume and enophthalmos that may initially be camouflaged by edema especially true in children.