Buy minomycin 50 mg with amex
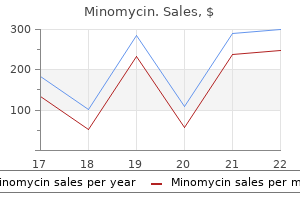
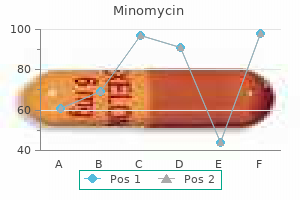
In (b) antibiotic 93 2264 order minomycin amex, a posterior view of all vascular structures, and in (c), a posterior view only on the pulmonary arteries is provided. In contrast, the right pulmonary artery appears larger than normal and almost like a direct extension of the main pulmonary artery. The small calibre of the left pulmonary artery may explain the high incidence of anastomotic problems that have been observed in the past with attempts to reimplant the vessel at the main pulmonary artery. This lesion is often associated with hypoplasia and other abnormalities of the tracheal and bronchial cartilages. Respiratory symptoms predominate, as the most severe compression is on the trachea. More than 50% of infants also have severe tracheobronchial anomalies such as absence of the posterior membranous component, tracheomalacia, stenosis, webs, or complete tracheal rings. Although the presence of complete rings does not imply that high-graded stenosis will be observed, the trachea is often narrower than normal. The complete rings may be localized at the region where the sling passes around the trachea, although in some cases, the entire trachea consists of complete ringed cartilages. Severe stenosis can involve the carina and extend for a considerable distance into one or both mainstem bronchi. Clinical findings 417 Vascular rings associated with left aortic arch Two extremely rare complete rings occur in the presence of a left aortic arch, and both are associated with a right-sided descending thoracic aorta. If a right ligamentum arteriosum were present instead of one on the left, its course would proceed from the base of this anomalous right subclavian artery to the right pulmonary artery, and a complete ring would exist. Most patients are symptomatic, but the occasional patient may present with dysphagia. The right subclavian artery arises more distally as a branch of the proximal right-sided descending aorta. The ligamentum arteriosum arises from the base of the right subclavian artery or a nearby diverticulum and travels to the right pulmonary artery. This is because in as many as 90% of cases in which symptomatic tracheal compression is produced by the innominate artery, the vessel is noted angiographically to have a normal origin from the aorta. When an anatomic abnormality is noted in these cases, the innominate artery appears to originate from a more distal and leftward position on the arch than normal. As it takes its course from left to right, it crosses the trachea anteriorly and in doing so may produce compression of the trachea. Cervical aorta this a rare anomaly in which the aorta ascends into the neck on the right or left side, forming a pulsatile mass in the supraclavicular region. Several morphological types have been described according to the side of the aortic arch (contralateral or ipsilateral) and the origin of the head and neck vessels. In addition, noisy breathing may be heard during both inspiration and expiration (biphasic stridor), while in asthma, the noise is mainly at the end of expiration. A common finding in all forms of vascular rings is fact that recurrent respiratory infections occur. In children with double aortic arches, if both arches are widely patent, the rings are tight, and patients present with biphasic stridor in the first weeks of life. Children with double aortic arches are often small and poorly developed, and hold their head in hyperextension. Children with a pulmonary artery sling and/or complete tracheal rings often have severe respiratory distress requiring emergent intubation and ventilation. Children with the innominate artery compression syndrome often present with apnea as an initial symptom. Feeding difficulties occur when solid feeding is attempted to be introduced to the infant. Physical exam may be within normal limits, but one may see coughing, dyspnea, drooling, or dysphagia. Infants will feed poorly due to respiratory distress and may have lifethreatening episodes of apnea and cyanosis. Double aortic arch has also been reported in association with other chromosomal anomalies, such as trisomy 21 and other syndromes. One of the more important noncardiac features that sometimes are found in association with double aortic arch is esophageal atresia, insofar as an undiagnosed arch anomaly may complicate repair of the esophageal atresia, which is usually recognized earlier than the double aortic arch. Another noncardiac anomaly that may be associated with vascular rings is a congenital laryngeal web, which may present with the same symptoms and signs as a vascular ring. Accordingly, patients with persistent stridor or upper airway obstruction after repair of a vascular ring, particularly those with a chromosome 22q11 deletion, should be evaluated for the presence of a congenital laryngeal web. Chest radiography Children usually present with symptoms of respiratory difficulty; therefore, chest radiography is always the first and most commonly performed test. Look for the position of the aortic arch, which is usually identifiable on the plain chest radiograph. The identification of a right aortic arch on chest radiograph in a child with airway difficulties, respiratory distress, or dysphagia should alert the clinician to a higher likelihood of a vascular ring. An ill-defined arch location is often observed in patients with double aortic arch. Such a finding should raise the suspicion of an arch anomaly in a symptomatic child. Other radiographic findings that may be noted with vascular rings include compression of the trachea and hyperinflation and or atelectasis of some of the lobes of either lung. A specific finding associated with anomalous left pulmonary artery is hyperinflation of the right lung. In general, chest radiography is not very sensitive in the diagnosis of vascular rings. In patients with double aortic arch, the frequency of phenotypes satisfying the clinical criteria for these various syndromes is not known. Rather, the important point is that double aortic arch may be associated with band 22q11 deletion, which has various other possible manifestations. These include, but are not limited to , palatal abnormalities, laryngotracheal anomalies, speech and learning delay, characteristic facial features, hypocalcemia, abnormalities of T-cell-mediated immune function, and neurologic defects. Occasionally, patients with double aortic arch may have anomalies consistent with either vertebral, anal, cardiac, Barium esophagram Most authorities consider barium esophagram to be the most important study in patients with a suspected vascular ring, and it is diagnostic in the vast majority of cases. Structures without a lumen, such as a ligamentum arteriosum or an atretic arch, have no blood flow and are difficult to identify with color-flow echocardiography. Also, identification of compressed midline structures and their relationship to encircling vascular anomalies may be difficult to detect, especially for the less experienced echocardiographer. These modalities provide excellent delineation of all of the associated structures. Aortic angiography and cardiac catheterization In the past, diagnostic aortography was performed in selected cases to delineate the anomalous arch vasculature. However, reported cases exist of rare arch anomalies in which aortography was the only study from which the correct anatomic configuration was identified. Cardiac catheterization is useful in cases in which associated cardiac abnormalities are known or suspected and echocardiography does not provide adequate diagnostic information. Patients having anomalies in which the right subclavian artery takes a retroesophageal course have a posterior defect slanting upward from left to right. The posterior defect in these cases is usually not as broad as that found in double aortic arch. In opposition, in patients with left aortic arch and aberrant subclavian artery, the oblique filling defect is mirror-imaged. An experienced radiologist can usually distinguish a double aortic arch from the retroesophageal subclavian artery based on the esophageal impression. Cases of abnormally located innominate artery causing tracheal compression have normal findings on esophagram. Bronchoscopy this diagnostic study has been used in the evaluation of children with symptoms of airway obstruction or compression. It is rarely required in the diagnosis of the various types of complete vascular ring. In case a simple vascular ring was diagnosed by other tests, a bronchoscopy should not be performed, due to the added risks and costs. In the presence of a vascular ring, pulsatile external tracheal compression is easily observed.
Generic minomycin 50 mg line
There is no consensus regarding optimal timing of decompression; however antibiotics shelf life generic minomycin 50 mg amex, it appears that early surgical intervention is associated with a better prognosis compared with delayed surgical treatment. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial. Quality of life and radiological outcome after cervical cage fusion and cervical disc arthroplasty. Experience in the surgical management of 82 symptomatic herniated thoracic discs and review of the literature. Spinous process marking: a reliable method for preoperative surface localization of intradural lesions of the high thoracic spine. Percutaneous placement of radiopaque markers at the pedicle of interest for preoperative localization of thoracic spine level. Intraoperative localization of thoracic spine level with preoperative percutaneous placement of intravertebral polymethylmethacrylate. Minimally invasive thoracic microendoscopic diskectomy: surgical technique and case series. Structural changes in the lumbar intervertebral discs; their relationship to low back pain and sciatica. Structural and ultrastructural analysis of the cervical discs of young and elderly humans. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Comparison of Nurick grading system and modified Japanese Orthopaedic Association scoring system in evaluation of patients with cervical spondylotic myelopathy. Diffusion tensor imaging of lumbar spinal nerve in subjects with degenerative lumbar disorders. Acute spontaneous cervical disc herniation causing rapidly progressive myelopathy in a patient with comorbid ossified posterior longitudinal ligament: case report and literature review. Non-traumatic acute paraplegia caused by cervical disc herniation in a patient with sleep apnoea. Nontraumatic acute complete paraplegia resulting from cervical disc herniation: a case report. Non-traumatic acute paraplegia associated with cervical disc herniation: a case report. Cervical intradural disc herniation after spinal manipulation therapy in a patient with ossification of posterior longitudinal ligament: a case report and review of the literature. A quantitative analysis of posterolateral approaches to the ventral thoracic spinal canal. Spinal cord compression caused by a protruded thoracic disc; report of a case treated with antero-lateral fenestration of the disc. Thoracoscopic approaches to the thoracic spine: experience with 241 surgical procedures. Thoracic disc herniation and acute myelopathy: clinical presentation, neuroimaging findings, surgical considerations, and outcome. Prognosis for recovery of bladder function following lumbar central disc prolapse. Costs and cost-effectiveness of epidural steroids for acute lumbosacral radicular syndrome in general practice: an economic evaluation alongside a pragmatic randomized control trial. Treatment of radiculopathies: a study of efficacy and tollerability of paravertebral oxygen-ozone injections compared with pharmacological anti-inflammatory treatment. Does early surgical decompression in cauda equina syndrome improve bladder outcome Minimally invasive approach to extraforaminal disc herniations at the lumbosacral junction using an operating microscope: case series and review of the literature. Fehlings Abstract Cervical spinal canal stenosis may lead to chronic progressive myelopathy from static and/or dynamic cord compression. However, in certain patients, cervical stenosis can result in rapid deterioration or may predispose healthy individuals to acute spinal cord injury following relatively mild trauma. The evaluation of patients with suspected cervical stenosis includes the radiographic determination of osseous and soft-tissue canal encroachment, with multiple grading systems with poor predictive value for the likelihood of future neurologic deterioration. Although the overall likelihood of catastrophic injury in patients with preexisting cervical stenosis appears minimal, in this chapter three clinical scenarios in which acute surgical intervention should be considered more carefully are reviewed. In patients with rapidly progressive degenerative cervical myelopathy, although the precise timing of surgical decompression has not yet been studied explicitly, postoperative functional outcomes are highly dependent on baseline status; hence, surgical decompression within days of clinical presentation may be appropriate. In cases of acute traumatic central cord syndrome, patients should be monitored closely and early surgical decompression considered within 1 to 3 days for patients with persistent deficits and ongoing radiographic compression. In patients with cervical cord neurapraxia, a condition most commonly seen in athletes, neurologic status should be carefully monitored for improvement over the first 1 to 3 days following injury, to distinguish this diagnosis from other injuries that require urgent surgical intervention. Keywords: central cord syndrome, cervical neurapraxia, cervical stenosis, myelopathy, surgical decompression, surgical timing of the intervertebral ligaments, bony remodeling (spondylosis) and osteophyte formation, and joint hypermobility and listhesis. The clinical examination may also guide the choice of subsequent radiographic studies. Patients with rapidly progressive myelopathy or persistent neurologic deficits following an acute traumatic incident, with radiographic evidence of ongoing cord compression, warrant consideration for emergent surgical decompression. In contrast, neurologically intact patients or those with improving deficits and without frank spinal instability, even in the presence of radiographic cord compression, are not necessarily appropriate for urgent surgery. Multiple ischemic, inflammatory, and immune pathways have been implicated in the subsequent responses to chronic cord compression. Natural History the vast majority of patients with cervical stenosis do not develop clinical myelopathy. In one of the largest studies to date of a predominantly elderly population, 24% showed radiographic cervical cord compression, with no association between cord compression and the development of myelopathic signs. Much less common, constituting the remaining 5%, are scenarios involving the acute development of myelopathy or rapidly progressive myelopathy, which merit consideration for urgent surgery within days of presentation. Among patients with symptomatic myelopathy, 5 to 18% may be classified as group I. Three distinct groups of patients have been described: younger patients (< 50 years of age) with severe traumatic fracture/dislocation and cord compression, older patients (> 50 years of age) with hyperextension injury without fracture in the context of a stenotic cervical spine, and younger patients sustaining a low-velocity injury resulting in acute central disk herniation without bony injury. Microvascular ischemia results in selective damage to the most medial white matter tracts located within the lateral funiculi, consistent with the anatomical location of the lateral corticospinal and rubrospinal tracts. These tracts have been shown evolutionarily to be progressively important for upper extremity and hand function, supporting the clinical findings of predominantly upper extremity weakness. Cervical stenosis with intramedullary T2 signal change (arrow) is demonstrated, secondary to ossification of the posterior longitudinal ligament and mild cervical spondylosis. Patients undergoing surgical decompression in delayed fashion, after 2 weeks, retain the potential for long-term neurologic improvement; however, this may occur more slowly and incompletely than if surgery is performed early. Particularly in younger patients with cervical stenosis and neurologic deficits following a traumatic hyperextension insult, without bony or ligamentous injury, it may be wise to delay surgical treatment until at least 24 hours have passed, in order to allow time for the spontaneous resolution of symptoms, except in cases where the neurologic injury is severe or imaging reveals a dramatic degree of spinal cord compression. Prophylactic surgical decompression in asymptomatic patients with canal stenosis is not recommended. Most symptomatic presentations occur with insidious onset, typically with myelopathy or radiculopathy, and elective surgery is an appropriate treatment option. Patients with rapidly progressive myelopathy should be considered for urgent surgical decompression within days of presentation. Acute traumatic central cord syndrome should be monitored closely, and early surgical decompression should be considered within 1 to 3 days for patients with persistent nonimproving neurologic deficits and ongoing radiographic compression. Cases of suspected cervical cord neurapraxia, most commonly seen in athletes with axial loading or hyperextension injuries, should be carefully assessed over the first 1 to 3 days following injury to distinguish this diagnosis from other injuries that could merit urgent surgical intervention. Cervical cord neurapraxia: classification, pathomechanics, morbidity, and management guidelines. Cervical spondylotic myelopathy: the clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder.
Purchase discount minomycin on line
It can happen that if a section through a nerve repaired by the epineural technique is placed under a microscope virus images generic 100 mg minomycin with visa, the fascicles are seen to be disrupted, buckled, and poorly aligned. The gaps we leave behind often fill with connective tissue and block neural regeneration. The "mushroom" has to be removed prior to the repair by trimming it back to the epineurium. This is easily done by laying each dissected end on a sterile tongue blade and excising the "mushroomed" portion with a fresh unused scalpel blade. Sometimes additional proximal and distal dissection is required to further relax the nerve. After the wound is closed, the limb is splinted for 3 to 4 weeks to prevent undo tension on the nerve anastomosis. This is the time required for a healing nerve to obtain an adequate tensile strength to sustain movement without disruption. Physical therapy and rehabilitation are required after any peripheral nerve repair. First introduced in 1953 by Sunderland,6, 16 it has become technically feasible only with the introduction of the operating microscope in the mid-1960s by Smith. It is the best form of repair in those cases in which only a few large fascicles are identifiable. The technique is also particularly useful for repairing the distal portion of a nerve in instances in which severed components typically can be mobilized and juxtaposed with minimal tension. In the urban environment, where a knife or glass is often involved in a nerve injury, a not uncommon situation is one in which the nerve is only partially severed, with some fascicles left intact. In some cases-in particular those in which a delayed repair is elected-one finds a nerve with disrupted fibrotic ends that require resection, with resultant foreshortening of the fascicles. In such instances, placement of an interfascicular graft (discussed below) rather than a fascicle repair is more appropriate. The anatomical dissection is carried out in such a fashion as to assure that both ends are sufficiently mobile to be approximated without tension. The superficial epineurium is then excised 3 to 4 mm on each end to expose the fascicles. Electromyography done post injury showed no return of function or axonal conduction. Occasionally the fascicles will "mushroom" out and need to be trimmed back to the perineurium before closure. In some cases, the fascicles cannot be identified, and here an epineural repair is more easily performed. This technique is similar to that described for the fascicle repair, except that groups of fascicles are selected for repair. In such cases, interposing fascicular epineurium is typically present, and it is in its plane that the dissection is carried out. Penetrating Injuries of Peripheral Nerves described for fascicle repair is then performed using whatever epineurium can be located. To overcome this problem, the use of nerve grafts harvested from other regions has been introduced. Historically, nerve grafts have waxed and waned in popularity but are now considered essential in some repairs, particularly those involving significant gaps between the nerve ends. There is no question that with better techniques and a clearer understanding of when to use them, grafts have proved effective in enhancing the recovery of appropriately selected injured nerves. The excellent clinical studies of Millesi and Samii5 and others18,19,20,21 have reintroduced the use of nerve grafts. It is beyond the scope of this chapter to review studies of graft physiology; the interested reader is referred to the work of Millesi, Samii, and others. About 1 cm of the epineurium is removed to provide an adequate exposure of the internal anatomy. As has been mentioned above, special care must be taken not to traumatize the nerve during suture placement. In our experience four to six grafts will typically be needed to repair a medium-sized nerve such as the medial or ulnar nerve. Occasionally, after dissecting the injured nerve, the surgeon will find a poor demarcation of the fascicle groupings. In these cases, it is often easier to arbitrarily divide the groupings with the grafts placed in an approximate manner. After a graft is placed, the extremity is splinted or otherwise immobilized for 3 to 4 weeks to allow healing without undue tension. To repeat a critically important point and the ultimate reason for performing a nerve graft: while providing an anatomical track, it assures that the tension along the suture line is not excessive. It is now well established that a regenerating axon will not cross a line of tension; furthermore, tension increases connective tissue proliferation, which becomes a barrier to a regenerating nerve. The use of a nerve graft will provide additional length, prevent tension, and with appropriate attention to the anatomical repair serve as an excellent medium for repair and growth. It can usually be located just behind and below the lateral malleolus and then followed up the calf. By "gently" tugging on the nerve during the dissection, it can be seen in outline and followed up the leg. Its removal can cause some sensory loss to the base of the foot, but most patients do not find this a problem; this outcome should, of course, be described to the patient prior to surgery. This nerve was once frequently used, but the risk of partial sensory loss to the hand has made it acceptable only as a last resort. In any procedure that requires a graft of significant length or multiple grafts, the sural nerve remains the best source. Nerves are inherently elastic and when cut will immediately retract up to 1 to 2 cm. In the acute period, such retraction is readily overcome with further anatomical dissection and additional relaxation of the nerve. As the interval of time since the injury increases, the natural response of the nerve is to form an intraneural fibrosis, permanently foreshortening the nerve endings. Intraoperative recordings showed a partial injury with some fascicles intact and some disrupted. There are natural limitations to this technique, as it can be applied only in a few of anatomical locations. The ulnar nerve can be transposed at the elbow over the epicondyle, providing an additional 3 to 5 cm of length. The median nerve can be transposed just anterior to the pronator teres, allowing up to 2 cm of additional length. When the radial nerve has been transected in a humerus injury, it can be transposed anteriorly and placed between the biceps and the brachialis. In appropriate circumstances, transposition can avoid the necessity of placing a graft. Mobilization is useful in the instance of nerves without multiple proximal motor branches, which tether the nerve. A nerve is typically supplied along its length by an incoming palisade of vessels, which can be easily identified. A generous dissection will usually allow mobilization of an additional 2 to 4 cm of nerve. The main disadvantage to this technique is that the nerve may be required to survive on the basis of its internal vascular supply, its external supply often being disrupted by the mobilization. Also, as a result of the anatomical dissection, the surgical bed becomes scarred, sometimes impeding a regenerating nerve.
Buy minomycin 100mg mastercard
In the absence of termination antimicrobial benzalkonium chloride buy minomycin 100 mg on line, the natural fetal demise of antenatally diagnosed cystic lung disease is 28%. Spontaneous involution of cystic lung lesions can occur, but complete postnatal resolution is rare, and apparent spontaneous "disappearance" of antenatally diagnosed lesions should be interpreted with care, as nearly half of these cases subsequently require surgery. The cystic adenomatous malformation volume ratio predicts an 80% increased risk of hydrops fetalis if more than 1. The spectrum of intervention include simple centesis of amniotic fluid, thoracoamniotic shunt placement, percutaneous laser ablation, and open fetal surgical resection. A large cystic mass and hydrops in isolated cystic lung lesions are the only real indication for fetal intervention. Normal vaginal delivery in recommended unless maternal condition indicates otherwise. Large lesions are predicted to become symptomatic shortly after birth (as high as 45% in some series); thus, delivery at a specialized center would be appropriate. However, smaller lesions are less likely to be symptomatic at birth, and delivery could be done at the referring institution with follow-up in a pediatric surgery clinic. Plain radiography should not be relied upon since it will miss and underestimate many lesions. Surgical excision of postnatal asymptomatic lesions remains controversial, with some centers opting for conservative management. Small lesions, less than 1 cm, may be managed expectantly, bearing in mind that the true resolution of these lesions is exceptional. Successful outcome of greater than 95% has been reported for these surgically managed asymptomatic lung lesions. In some, the absence of tracheal flow in color Doppler can be visualized during fetal breathing movements. Abdominal wall defects Abdominal wall defects in fetuses include gastroschisis, exomphalos, bladder exstrophy complex, cloacal exstrophy, and body stalk syndrome. The defects that occur more commonly are gastroschisis and exomphalos, but these are distinct abdominal wall defects with an unclear etiology and a controversial prognosis. Thus karyotyping, in addition to detailed sonographic review and fetal echocardiogram, is essential for complete prenatal screening. If termination is not considered, normal vaginal delivery at a center with neonatal surgical expertise is recommended and delivery by caesarean section only reserved for large exomphalos with exteriorized liver to prevent damage. Occasionally, in vulnerable infants with severe pulmonary hypoplasia or complex cardiac abnormalities, the exomphalos may be left intact and allowed to slowly granulate and epithelialize by application of antiseptic solution. Malrotation and adhesive bowel obstruction does contribute to mortality in isolated exomphalos; however, the majority of these children survive to live normal lives. On prenatal scan with a detection rate of 100%, the bowel appears to be free-floating, and the loops may appear to be thickened due to damage by amniotic fluid exposure causing a "peel" formation. However, a recent systematic review looking at the outcome of antenatal bowel dilatation showed no difference in mortality, length of bowel resection, time to feeding, or length of hospital stay. A recent study5 has challenged elective preterm delivery with a randomized control trial. Despite efforts to plan elective delivery, 50% of cases will require emergency caesarean section due to development of fetal distress. Various methods of postnatal surgical repair include the traditional primary closure, reduction of bowel without Dilated bowel exomphalos anesthesia, reduction by preformed silo, or reduction by means of a traditional silo. Coexisting intestinal atresia could be repaired by primary anastomosis or staged with stoma formation. Variation in achieving full enteral feeding due to prolonged gut dysmotility is expected in all cases. The long-term outcome in gastroschisis is dependent on the condition of the bowel. The mortality of liveborn infants is 5%, with a further 5% suffering short bowel syndrome and 10% requiring surgery for adhesive bowel obstruction. Late third-trimester fetal loss should always be mentioned during fetal counseling. Prenatally, the condition may be suspected from maternal polyhydramnios and absence of a fetal stomach bubble at the 20th-week anomaly scan. Specific surgical conditions 69 sensitive, with a positive predictive value of 56%. These associated anomalies are present in more than 50% of cases and worsen the prognosis; thus, prenatal karyotyping is essential. Postnatal surgical management is dependent on the size and condition of the baby, length of esophageal gap, and associated anomalies. Primary repair of the esophagus is the treatment of choice; however, if not achieved, staged repair with upper esophageal pouch care and gastrostomy or organ replacement with stomach or large bowel are other options. Long-term outcomes are indicated by improved perinatal management and inherent structural and functional defects in the trachea and esophagus. Quality of life is better in the isolated group with successful primary repair as compared to those with associated anomalies and delayed repair. Since the large bowel is mostly a reservoir, with no physiologic function in utero, defects in this region such as anorectal malformations or Hirschsprung disease are very difficult to detect. Bowel dilatation and echogenic bowel may be associated with cystic fibrosis; therefore, all such fetuses should undergo postnatal evaluation for this disease. A cystic mass identified in this way may represent a normal structural variant or a pathological entity requiring surgical intervention postnatally. Excluding cysts of renal origin, the differential diagnosis includes ovarian cysts, enteric duplication cysts, meconium pseudocysts, mesenteric cysts and choledochal cysts. Less common diagnoses include extralobar pulmonary sequestration and pancreatic, splenic, urachal, and adrenal cysts. Almost all cysts are benign, and many are selflimiting; however, these cysts create a high level of anxiety for the prospective parents, especially suspected adrenal cysts. Regular antenatal consultation and fetal counseling by the appropriate team may reduce parental anxiety levels. Resolution of these cysts was reported in 30% of cases, and of all the antenatally diagnosed cysts, 40% will come to surgical intervention. Duodenal atresia has a characteristic "double-bubble" appearance on prenatal scan, resulting from the simultaneous dilatation of the stomach and proximal duodenum. Detection rate on second-trimester anomaly scan is almost 100% in the presence of polyhydramnios and the doublebubble sign. However, a late trimester event may only be detected due to polyhydramnios or not detected at all. The postnatal survival rate is >95%, with associated anomalies, low birth weight, and prematurity contributing to the <5% mortality. Temporary delay in enteral feeding occurs due to the dysmotility in the dilated stomach and duodenum. There are many bowel abnormalities that may be noted on prenatal scanning (dilated bowel, ascites, cystic masses, hyperperistalsis, poyhydramnios, and echogenic bowel); however, none is absolutely predictive of postnatal outcome. Four types have been defined: l l Type 1-external tumor with a small presacral component Type 2-external tumor with a large presacral component 70 Fetal counseling for surgical malformations Abd. Two major issues are the indications for intervention in bladder outlet obstruction and early pyeloplasty in infancy in cases with hydronephrosis. Ultrasonography provides measurements of the renal pelvis, assessment of the renal parenchyma, as well as detection of cysts in the cortex. Oligohydramnios is indicative of poor renal function and poor prognosis owing to the associated pulmonary hypoplasia. Urogenital anomalies coexist with many other congenital abnormalities, and amniocentesis should be offered in appropriate cases. It is estimated that 3% of infants will have an abnormality of the urogenital system, and half of these will require some form of surgical intervention. Fetal treatment of tumor resection or ablation of feeding vessel has been attempted in hydropic patients. Caesarean section may be offered to patients with large tumors to avoid the risk of bleeding during delivery.
Proven 50 mg minomycin
A new intravenous fat emulsion containing soybean oil antibiotics for sinus infection during pregnancy purchase minomycin discount, medium-chain triglycerides, olive oil, and fish oil: A single-center, double-blind randomized study on efficacy and safety in pediatric patients receiving home parenteral nutrition. Gall-bladder contractility in neonates-Effects of parenteral and enteral feeding. Small volumes of enteral feedings normalise immune function in infants receiving parenteral nutrition. Enteral nutrition can be delivered via an enteral feeding tube (nasogastric/ nasoduodenal/nasojejunal, orogastric/oroenteric), a gastrostomy, or a jejunostomy. Gastrostomy is one of the oldest abdominal operations in continuous use1 and has played an important role in the management of various surgical conditions of the neonate. In the past decades, there has been remarkable improvement in surgical techniques for gastrostomy placement. New techniques such as fluoroscopic guidance or electromagnets permit tube placement in the small bowel without radiographic confirmation. Gastrostomies are these days used not only in patients with major congenital anomalies of the gastrointestinal tract and abdominal wall but in an increased number of infants and children without surgical pathology. In most of these, the indication is an inability to swallow, usually secondary 160 to central nervous system impairment. Ironically, often these are patients who have survived because of aggressive neonatal resuscitation and technological advances. Additional indications include gastric access for esophageal bougienage and administration of medications. Nasogastric feeding tube versus gastrostomy Because the newer 5F and 8F infant feeding tubes are highly biocompatible and remain smooth and soft for prolonged periods of time, they are usually well tolerated, even by the smallest premature infants. Beyond this arbitrary time frame, complications such as naso-otopharyngeal infections and gastroesophageal reflux tend to increase. Gastrostomies should be considered when direct gastric access for feeding or the administration of medication is expected to last more than several months. Nasogastric decompression tube versus gastrostomy With careful attention to appropriate intragastric position and regular flushing, nasogastric or orogastric tubes generally decompress more effectively than do gastrostomy tubes. It should be remembered that most commercially available 8F tubes are designed for feeding and have only two Gastrostomy in select neonatal surgical pathology 161 holes. However, care must be taken not to make the holes too big in order to avoid kinking. These 8F tubes should be attached directly or via a short connecting tube to a spillresistant open container and irrigated regularly. Double-lumen (vented) catheters, such as the 10F Replogle tube, originally designed for the aspiration of saliva in patients with esophageal atresia, tend to be much stiffer and are therefore more likely to cause problems. Additionally, if the venting lumen is obstructed and suction is applied, mucosa is sucked into the holes, leading to trauma and rendering the tube ineffective. If additionally, a stomach bypass is required, a gastrostomy with a jejunal extension tube should be placed or a jejunostomy created. Major abdominal wall defects Prolonged ileus typically follows the repair of gastroschisis and, occasionally, other major wall defects. Although decompressive gastrostomies are not routinely employed, they can be helpful in patients with gastroschisis and associated atresia, particularly those requiring long-term continuous feeding. The analysis of large series demonstrates that esophago-esophagostomy without the use of a gastrostomy is safe9 and may in fact be beneficial for decreasing the incidence of gastroesophageal reflux. The stoma, employed for the decompression or feeding, can also be used to provide access for the management of anastomotic complications such as leakage or strictures. Short-gut syndrome Infants who have lost over 50% of their small bowel have profound alteration of gastrointestinal physiology. As the remaining intestine undergoes adaptive changes, continuous enteral feedings become necessary. As this latter process can be fairly lengthy, direct gastric access via gastrostomy is desirable. Other surgical pathology In any neonatal or infant condition in which a prolonged ileus or partial luminal occlusion. Duodenal obstruction Congenital duodenal obstruction is usually associated with proximal duodenal dilatation and atony as well as gastric dilatation. Total parenteral nutrition and nasogastric decompression are generally effective in postoperative management. As stated, nasogastric tubes tend to drain better than gastrostomies in the immediate postoperative period. However, a gastrostomy can eliminate the need for long-term nasogastric or orogastric intubation and the complications associated with placement and maintenance of these tubes. Gastrostomies interfere less with oral feedings than do nasogastric tubes, although the newer, smaller catheters are better tolerated. Gastrostomies are preferred over jejunostomies because the latter are less physiological and more prone to mechanical complications. Gastrostomies, as well as any other enteral tubes placed in infants, are associated with a long list of potential early and late complications. Gastrojejunal tubes may eliminate the need for antireflux surgery in patients with gastroesophageal reflux. Jejunostomies have been found to provide more complications, such as internal hernia and volvulus (the latter particularly in the Roux-en-Y jejunostomies or the "dissociation" technique bypassing the stomach as described by Bianchi). A notable morbidity after gastrojejunal tube placement has been described ranging from persistent reflux to dislodgement and intestinal perforation. Normal feeding gradually returned, and a few weeks after this picture was taken, the gastrostomy could be removed. The main indications in infants are swallowing difficulty secondary to central nervous system lesions as well as other abnormalities of deglutition, feeding supplementation, large-volume medications, and chronic malabsorption syndromes. Because the neurologically impaired children frequently have foregut dysmotility and gastroesophageal reflux in addition to swallowing difficulties, antireflux procedures are at times added to gastrostomies. There are conflicting results about an increased risk of pathologic gastroesophageal reflux after gastrostomy tube placement in neurologically impaired children, resulting in divergent recommendations of simultaneous antireflux surgery. These techniques and their many variations are based on three fundamental principles: Stamm gastrostomy 163 1. Formation of a serosa-lined channel from the anterior gastric wall around a catheter. This catheter is placed in the stomach and exits either parallel to the serosa, as in the Witzel technique, or vertically, as in the Stamm or Kader approaches. Construction of a tube or conduit from a full-thickness gastric wall flap, leading to the skin surface. A standard gastrostomy tube or a skin-level device can be placed under local anesthesia, although general anesthesia is preferred because abdominal wall relaxation is required. After the tract is well healed, this stoma is suitable for the passage of dilators or guide wires. The procedure is very short, and there is no postoperative ileus, no potential for bleeding or wound disruption, and only minimal interference with subsequent interventions on the stomach, such as a fundoplication. The main disadvantage of this and other pure endoscopic techniques is that the virtual space between the stomach and the abdominal wall cannot be visualized. One of these is the percutaneous endoscopic "push" technique, which is performed with the aid of needledeployed gastric anchors or T-fasteners, and the Seldinger method of guide-wire introduction followed by progressive tract dilatations. These are essentially expansions of the aforementioned methods, significantly increasing the choices of gastric access techniques available to surgeons managing infants. When possible, a nasogastric tube is inserted for decompression and to help identify the stomach, if necessary. This incision should be neither too high, because it would bring the catheter too close to the costal margin, nor too low, avoiding the colon and the small bowel. However, this approach is less desirable because the linea alba is the thinnest area of the abdominal wall. Fascial layers are incised transversely and the rectus muscle retracted or transected. When identification of the stomach is not immediate, downward traction of the flimsy greater omentum readily allows visualization of the transverse colon and stomach. The site should be neither too high, because this would interfere with a fundoplication should one be needed in the future, nor too low, because stomas at the level of the antrum are prone to leakage and pyloric obstruction by the catheter. The surgeon must not place the catheter too close to the greater curvature, to avoid the so-called gastric pacemaker and to minimize the potential for gastrocolic fistula. The gastrotomy, at the center of the purse string, is made sharply through the serosa and muscular wall of the stomach.
Purchase minomycin with a visa
If hypotension is prevented best antibiotic for sinus infection while pregnant minomycin 50mg lowest price, normal humans can tolerate an extremely low arterial oxygen tension (PaO2) without major neurologic manifestations or sequelae. Gray and Horner34 reported that among 22 patients with a PaO2 of 20 mm Hg or less, 8 remained alert, 7 somnolent, and 7 comatose. Severe hypoxia usually causes clinical signs of a metabolic encephalopathy, with deterioration in level of consciousness to eventual coma, along with changes in respiratory pattern, tremor, asterixis, myoclonus, and flexor or extensor posturing. Such problems as hypothermia, severe hyper- or hypoglycemia, hyponatremia, and drug intoxications may alter level of consciousness35 and should be considered when first evaluating any patient in coma with or without evidence of brainstem dysfunction, especially when the clinical history is unclear. Prolonged or persistent herniation will lead to irreversible ischemic damage to the deep midline structures of the cerebral hemispheres and the brainstem, resulting in permanent morbidity or death. It is critical that systemic hypotension be prevented or rapidly corrected to maintain brain perfusion. If the blood pressure is initially normal, hydration should be moderated to avoid overhydration, which may aggravate cerebral edema or lead to pulmonary edema. In the head-injured patient, the most common cause of systemic hypotension is hemorrhagic shock. These alternatives should be considered if the blood pressure does not respond to initial volume resuscitation, or if the clinical picture does not fit with that of hemorrhagic shock. Common sites of hemorrhage include the chest and abdomen, pelvis, and long bone fractures. Except in the setting of hemorrhagic shock, Andrews recommends the immediate bolus infusion of mannitol, 1. It remains predominantly in the intravascular space and causes a direct vasoconstriction because of its effects on blood viscosity. Because of the cardiovascular effects of mannitol infusion, its use is generally contraindicated in the setting of cardiovascular instability or hemorrhagic shock. Recently, Cruz et al,3 in a prospective randomized class I study, compared initial use of mannitol, using "conventional dosage" and "high" dosage in patients with documented subdural hematomas. The low-dosage group had significantly worse cerebral oxygen extraction and cerebral swelling than the high-dosage group. Preoperative improvement in anisocoria was also significantly better in the high-dosage group. After 6 months, the Glasgow Outcome Scale scores were significantly better in the high-dosage group than in those receiving the conventional dosage. The Recognition and Management of Cerebral Herniation Syndromes cell volume, which also improves circulation, decreasing hyperemia and hypoperfusion. Decompressive craniectomy has also become a recognized treatment for herniation caused by hemispheric infarction, particularly in the nondominant hemisphere. This may include evacuation for lobar or nondominant hemispheric spontaneous hemorrhage15 and immediate percutaneous ventricular drainage for hydrocephalus. Of patients who are hemodynamically unstable because of traumatic injuries to the chest or abdomen, some must go directly to the operating room for treatment of these life-threatening lesions. If the patient has not been resuscitated from initial cardiac arrest, or has not had profound hypotension, in which case the clinical findings of herniation are often false localizing,31 it may be reasonable to consider performing exploratory burr holes on the side of the dilated pupil. In the case of nonlateralizing signs of herniation, the burr holes should be placed bilaterally. Intraoperative ultrasonic imaging of the brain parenchyma can further enhance the diagnostic yield of exploratory burr holes, allowing identification of parenchymal hematomas or other mass lesions. The prognosis for functional recovery may be quite good, particularly among younger patients who exhibit reversal of the clinical signs of herniation with use of mannitol and hyperventilation, and who have an intracranial mass lesion that can be surgically removed. They noted that when one or both pupils were nonreactive, all 96 patients older than 50 years of age, and all but one of 121 patients older than 40 years of age, were finally dead or vegetative. For patients with nontraumatic causes of herniation, the prognosis may be much better for functional recovery, as the brain itself may have intact function except for the cause of the herniation syndrome. For patients with acute hydrocephalus,7 tumor-related cerebral edema,9 temporal lobar hemorrhage,15 hemispheric infarction,55 or cerebellotonsillar herniation from lumbar drainage,4 appropriate resuscitation and corrective reversal of mass effect can result in a satisfactory outcome. Upper brain-stem compression and foraminal impaction with intracranial space-occupying lesions and brain swelling. The oval pupil: clinical significance and relationship to intracranial hypertension. Unilateral fixed dilation of the pupil as a false-localizing sign with intracranial hemorrhage: case report and literature review. Brain stem compression secondary to adipose graft prolapse after translabyrinthine craniotomy: case report. Reevaluation of lumbar puncture; a study of 129 patients with papilledema or intracranial hypertension. Implications of systemic hypotension for the neurological examination in patients with severe head injury. The effect of axial traction during orotracheal intubation of the trauma victim with an unstable cervical spine. Long-term outcome after medical reversal of transtentorial herniation in patients with supratentorial mass lesions. Mannitol causes compensatory cerebral vasoconstriction and vasodilation in response to blood viscosity changes. Magnetic resonance imaging measurements and clinical changes accompanying transtentorial and foramen magnum brain herniation. Acute foramen magnum syndrome caused by an acquired Chiari malformation after lumbar drainage of cerebrospinal fluid: report of three cases. Results of immediate surgical exploration without computed tomography in 100 patients. Posterior fossa decompression for life-threatening tonsillar herniation in patients with gliomatosis cerebri: report of three cases. The tentorial notch and complications produced by herniations of the brain through that aperture. The tentorial notch: anatomical variation, morphometric analysis, and classification in 100 human autopsy cases. Brain shift, level of consciousness, and restoration of consciousness in patients with acute intracranial hematoma. Intracranial volume-pressure relationships during experimental brain compression in primates. Role of hypertonic saline for the management of intracranial hypertension after stroke and traumatic brain injury. Intraoperative ultrasound imaging of the entire brain through unilateral exploratory burr holes after severe head injury: technical note. One-year outcome after decompressive surgery for massive nondominant hemispheric infarction. Variations in weaponry and projectile ballistic properties lead to a broad spectrum of both intracranial and extracranial damage. Current management is based on cumulative military experiences accumulated since World War I and has been modified to address the civilian population. Despite significant advancements in critical care medicine and microsurgical techniques, these injuries continue to present a formidable challenge for neurosurgeons. Treatment strategies focus on initial resuscitation, assessment of damage through imaging studies, providing appropriate supportive care, and surgical intervention when indicated. Keywords: gunshot wound, penetrating brain injury, skull fracture, traumatic brain injury Penetrating wounds from explosive devices, whose fragments are not aerodynamic and are thus slowed by air friction, usually resemble those from low-velocity bullets in their irregular shape and trajectory. These pressure waves pass through brain, which is 75% aqueous, like ripples from a stone dropped in a puddle: proximally the waves have short wavelength and high amplitude, but as they travel through tissue, their wavelength increases and their amplitude decreases. Nearby tissue thus sustains greater disruption, but with high-velocity objects, the volume of injury can extend far beyond the initial trajectory. For example, a very-high-velocity bullet may create a cavity 15 times larger than its diameter. The projectile leaves a permanent tract of necrotic and ischemic tissues and damaged blood vessels. Peripheral to this tract lies an annulus of brain parenchyma that, although relatively less grossly disrupted, shows necrosis with axonal, neuronal, and astrocytic destruction and neutrophil infiltration. Surrounding this annulus, widespread axonal damage and injured, hyperchromatic, and vacuolated neurons are seen.
Buy 50mg minomycin with visa
In addition antibiotic treatment for mrsa buy minomycin in united states online, if one twin dies, the other twin is at risk for neurologic injury due to a sump phenomenon in the placenta and demised fetus and from embolism. The International Amnioreduction Registry showed that amnioreduction resulted in survival of 58%. The trial was stopped early after interim analysis showed a clear survival advantage to laser therapy: 76% versus 51% for single survivor and 36% versus 26% for dual survivor. Complications include neurologic deficits with motor and somatosensory abnormalities. In addition, bowel and bladder function is often deranged due to injury to the autonomic nervous system. Despite postnatal repair of the defect, the attendant morbidity from neurologic abnormalities is severe, and up to 30% of patients die before reaching adulthood. The second hit is postulated to be due to direct trauma to the exposed neural elements while the fetus is in utero. As the acardiac, acephalic twin grows, the normal pump twin goes into high-output cardiac failure and hydrops. Ability to select the fetus that will benefit from prenatal treatment Stem cells and gene therapy Gene therapy for prenatally identifiable diseases is currently experimental and is being actively pursued for specific disorders. In utero treatment with stem cells and/or virally directed genes may halt the progression of disease during gestation. The fetal immune system develops gradually, and prior to 15 weeks gestation, the fetus is in a preimmune state. Specific issues for in utero treatment of genetic diseases include timing of diagnosis, timing of therapy, delivery of stem cells or genes, sources for stem cells, and durability of treatment. With the advent of chorionic villus sampling, genetic diseases can be identified in the first trimester. Timing of potential treatments is crucial in order to take advantage of the possible preimmune status of the fetus, making fetuses potentially more receptive to exogenous genes or cells. Others have investigated the use of retroviral vectors in order to insert genetic material into fetal animals. This approach reduces the problem of obtaining the large numbers of stem cells needed to create even a modest amount of chimerism. Other approaches include use of maternal stem cells or genetic material as studies have demonstrated early cross-trafficking of maternal cells in the fetus. Candidate diseases include hematologic, immunologic, metabolic, and neurologic abnormalities. Currently, in utero gene therapy and stem cell therapy are in their infancy but remain active topics of research and investigation. The progress seen in the field of fetal surgery is a testament to the power of a rigorous investigational process, i. Through these efforts, diseases with historically high perinatal mortality rates have shown improved survival with fetal surgery. New areas of research include tissue engineering, stem cell therapy, and gene therapy. As always, maternal safety must remain paramount, and risk to the mother should be minimized at all times. Many people have contributed to the development and success of fetal treatment and diagnosis. Collaborative, multidisciplinary teams are critical for the success of any fetal treatment program. It is also important to acknowledge the significant contributions of patients and their families to this enterprise. The brave families who chose to undergo early fetal therapies are the true pioneers on whose shoulders the success of fetal treatment rests. Procedure-related risk of miscarriage following amniocentesis and chorionic villus sampling: A systematic review and meta-analysis. Fetal cell-free nucleic acids in the maternal circulation: New clinical applications. Efficacy of radiofrequency ablation for twin-reversed arterial perfusion sequence. Fetal aortic valvuloplasty for evolving hypoplastic left heart syndrome: Postnatal outcomes of the first 100 patients. Congenital diaphragmatic hernia: A systematic review and summary of best-evidence practice strategies. An early gestational fetal lamb model for pulmonary vascular morphometric analysis. Experimental fetal tracheal ligation reverses the structural and physiological effects of pulmonary hypoplasia in congenital diaphragmatic hernia. Evidence and patterns in lung response after fetal tracheal occlusion: Clinical controlled study. Fetal intervention for mass lesions and hydrops improves outcome: A 15-year experience. Congenital cystic adenomatoid malformation in the fetus: Natural history and predictors of outcome. Resolution of hydrops fetalis in congenital cystic adenomatoid malformation after prenatal steroid therapy. Tumor metrics and morphology predict poor prognosis in prenatally diagnosed sacrococcygeal teratoma: A 25-year experience at a single institution. Minimally invasive therapy for fetal sacrococcygeal teratoma: Case series and systematic review of the literature. Endoscopic laser surgery versus serial amnioreduction for severe twin-to-twin transfusion syndrome. Efficacy of radiofrequency ablation for twin reversed arterial perfusion sequence. The paralysis associated with myelomeningocele: Clinical and experimental data implicating a preventable spinal cord injury. Creation of myelomeningocele in utero: A model of functional damage from spinal cord exposure in fetal sheep. In utero repair of experimental myelomeningocele saves neurological function at birth. In utero hematopoietic cell transplantation for the treatment of congenital anomalies. In those complex conditions, prosthetic materials are used because of the lack of biocompatible tissues able to replace or regenerate damaged organs. Besides the risk of infection, the major drawback of using a prosthetic patch closure is the risk of dislodgment and subsequent recurrence of the initial problem. Moreover, foreign body reactions and implant rejection occur when synthetic polymers are used. Regeneration of natural tissue from living cells to restore damaged tissues and organs is the main purpose of regenerative medicine. This relatively new field has emerged by the combination of tissue engineering and cell transplantation as a possible strategy for the replacement of damaged organs or tissues. In order to give rise to a new functional organ-like structure, several variables, such as local environment, nutrients, and metabolites, are pivotal. These variables, in the context of tissue engineering, are mainly dependent on the provision of a three-dimensional growth structure termed "scaffold. Synthetic scaffolds lack bioactivity, are mechanically strong and can be engineered with bespoke macrostructure and microstructure, which has the potential to enhance cellular growth and organogenesis. So far, their potency, together with the difficulties related to their allogenic origin, have limited their possible clinical application. This procedure specifically entails the removal of an oocyte nucleus in culture, followed by its replacement with a nucleus derived from a somatic cell obtained from a patient. Besides, this cells could be stored and used subsequently for the treatment of future medical conditions. As a consequence, this could be relevant to the creation of autologous tissues for use in children who are born with complex malformations, in which tissue viability represents a problem and where patient-specific cells could be created in vitro. It creates genetically matched tissues, but genetic manipulation of the cells during reprogramming can be teratogenic. The latter is particularly important in the context of congenital malformation, as surgical treatment is often complicated by insufficient available tissue at time of repair.
Discount minomycin 50 mg fast delivery
Body surface cultures and gastric aspirates are of limited value in the evaluation of sepsis bacteria 1 minomycin 50 mg low price. Tracheal aspirates may be of value in intubated neonates shortly after birth and immediately after endotracheal tube placement. The first signs of infection in a preterm infant are often apnea, bradycardia, and cyanosis followed by lethargy and increased respiratory effort. Tachycardia is a nonspecific finding, and bradycardia is often a sign of more advanced sepsis. Meningitis may present with a high pitched cry, abnormal movements, arching of the back, and tense fontanels. The incidence of meningitis in healthy-appearing infants is low, but the incidence is up to 23% in bacteremic patients. Neonatal Infection: antibiotics for prevention and treatment 2012 [cited February 20, 2016]. Additionally, if analysis is delayed greater than 2 hours, values may change significantly. Abdominal x-ray can be used to evaluate intra-abdominal causes of sepsis, such as pneumatosis intestinalis in infants suspected of having necrotizing enterocolitis. Acute phase reactants and biomarkers Acute phase reactants and biomarkers can be measured in the evaluation of neonatal sepsis. There is no single biomarker that can be used to reliably diagnose neonatal sepsis. One study evaluated 13 clinical and laboratory signs of sepsis and found that the maximum positive predictive value of any sign studied was 31. Significant advances have been made in the prevention of sepsis in both the perinatal and peripartum period as well as in the early postpartum management of neonates. Alternatives for penicillin allergic mothers have not been measured in controlled trials for efficacy but include cefazolin, clindamycin, erythromycin, and vancomycin. Although aggressive skin care, including 3% hexachlorophene bathing, can significantly reduce S. Indeed, a recent randomized controlled trial investigating umbilical cord care demonstrated superiority and safety of chlorhexidine powder to dry care. Recommendations of space range from 36 to 100 square feet and nurse to patient ratio of 1:4 to1:1, depending on acuity. Although good outcome studies of individual interventions are not possible due to power restrictions, quality assurance and intervention bundle studies indicate that combined implementation of infection control techniques reduces the risk of nosocomial infections. This includes frequent hand hygiene, gowns and gloves, care of invasive devices, sterilization of equipment, and epidemic control techniques. The Surviving Sepsis Campaign guidelines now include pediatric considerations in the management of severe sepsis but do not distinguish between neonates and children. Resuscitation should include (1) maintaining the airway and attaining adequate oxygenation and ventilation, (2) maintaining circulation defined as normal perfusion and blood pressure, and (3) maintaining threshold heart rates. Therapeutic endpoints include capillary refill of less than 2 seconds, normal pulses with no difference in central and peripheral pulses, warm extremities, urine output of greater than 1 mL/kg/h, normal mental status, normal blood pressure for age, preductal and postductal oxygen saturation difference of less than 5%, and oxygen saturation of >95%. Significantly decreased tissue perfusion has several measurable laboratory and biochemical effects in the neonate. In particular, metabolic acidosis, base deficit, and serum lactate can be utilized as markers of poor perfusion. Fluid boluses of 10 mL/kg should be given up to 60 mL/kg in the first hour to attain normal perfusion and blood pressure. Vasoactive support may be required, but pulmonary vascular resistance should be considered when selecting a vasopressor and support for persistent pulmonary hypertension of the newborn should be initiated if needed. Due to the differing proportions of alpha- and beta-adrenergic receptors in the neonate, there has been significant skepticism regarding the utility of alpha-specific medications such as phenylephrine or norepinephrine, although they are used routinely in older patients. Nevertheless, a prospective trial evaluating norepinephrine demonstrated improved tissue perfusion and relative safety in the neonate with shock refractory to fluid and classic vasopressors. Nonetheless, current neonatal guidelines generally favor dopamine over dobutamine as an initial choice of vasopressor, and epinephrine as a rescue medication for dopamine-refractory shock, despite ongoing debate about the optimal pressor for different types of shock. Calcium chloride infusions, along with various other forms of calcium replacement, have been strongly advocated in the pediatric and anesthesia communities,75 but safety and intravenous access issues have not been studied in the setting of calcium infusion for septic shock. Nevertheless, most units prefer to add calcium to intravenous fluid and parenteral nutrition, as well as intravenous calcium boluses to maintain calcium in the normal range. Evidence supports endocrine replacement therapy in the setting of neonatal shock refractory to vasopressor treatment. Early nongenomic effects, on the other hand, are responsible for the efficacy of endocrine Management 227 Table 20. In particular, corticosteroids lead, in a nongenomic, rapid fashion, to the prevention of endocytosis of adrenergic receptors and downregulation of secondary messenger systems that lead to tachyphylaxis to both autologous and extrinsically infused adrenergic vasopressors. There are currently no evidence-based guidelines on weaning hydrocortisone in neonates. In the case of refractory shock, pericardial effusion, pneumothorax, blood loss, hypoadrenalism, hypothyroidism, inborn errors of metabolism, or heart disease should be evaluated and treated as discussed above. Patients should also be evaluated for other causes of infection, and aggressive source control should be initiated for infected or necrotic tissue. Blood cultures should be obtained, and empiric antibiotics should be administered within 1 hour of the identification of sepsis. Furthermore, decreasing Gram-negative and Gram-positive sepsis has led to a commensurate rise in anaerobic, fungal, and viral sepsis. The treatment duration varies from 10 to 14 days depending on the pathogen, while treatment for meningitis is usually longer. Duration should be adjusted based on response to therapy or complications including abscesses, osteomyelitis, or endocarditis. Trends in inflammatory biomarkers have been evaluated to determine response to antibiotic therapy and may allow for the early discontinuation of antibiotics in healthy appearing neonates. New therapies and preventive strategies Several new therapies have been proposed for the management of neonatal sepsis. Furthermore, neonates with birth weight between 401 and 750 g and the use of a third-generation cephalosporin were found to increase the risk of developing candidiasis, while enteral feeding appeared protective. These include cerebral palsy, visual impairment, delayed psychomotor development, low Bayley Scales of Infant Development scores, overall poor neurodevelopment, and impaired growth. Sepsis-induced endocarditis and thrombosis can cause rare complications such as pulmonary embolism, valvular damage, and infectious thromboembolism. As the prevention, identification, and therapy of sepsis advance, the epidemiology and bacteriology of the disease shift making optimal treatment of sepsis an evolving process. The World Health Organization Global Health Observatory Data Repository: World Health Organization; 2015 [cited 2015 February 24]. Neurodevelopmental and growth impairment among extremely low-birthweight infants with neonatal infection. Early goal-directed therapy in severe sepsis and septic shock revisited: Concepts, controversies, and contemporary findings. The influence of early hemodynamic optimization on biomarker patterns of severe sepsis and septic shock. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock, 2012. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). Identification of infants unlikely to have serious bacterial infection although hospitalized for suspected sepsis. Febrile infants at low risk for serious bacterial infection-An appraisal of the Rochester criteria and implications for management. Predictive model for serious bacterial infections among infants younger than 3 months of age. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Comparison of procalcitonin with C-reactive protein and serum amyloid for the early diagnosis of bacterial sepsis in critically ill neonates and children. Optimizing care and outcome for late-preterm (nearterm) infants: A summary of the workshop sponsored by the National Institute of Child Health and Human Development.