Generic 0.1 mg clonidine otc
Mechanical kinking of the catheter tubing is usually accompanied by two-way obstruction prehypertension pregnant buy discount clonidine 0.1 mg line. A flatplate radiograph of the abdomen is often helpful in identifying a kink in the catheter tubing. Heparin should be added to the dialysate whenever fibrin strands or plugs are visible in the effluent. Heparin is more useful prophylactically than therapeutically, preventing the formation of fibrin clots and extension of existing clots. Once outflow obstruction has occurred, irrigation of the catheter with heparin is usually unsuccessful in recovering function. If treatment of constipation and fibrinolytic therapy are not successful in restoring drainage function, and if urinary retention and tubing kinks have been excluded, the catheter is presumed to be obstructed by omentum or other adherent intraperitoneal structures. Interventions to resolve catheter obstruction are now most commonly performed using radiologic and laparoscopic techniques. Fluoroscopic guidewire manipulation has been used to redirect displaced and obstructed catheters. Chapter 23 / Peritoneal Dialysis Catheters, Placement, and Care 443 Forceful straightening of the subcutaneous tunnel can produce tunnel track trauma and infection. Transluminal manipulation is not practical for extended catheters because of the long tubing length. A preprocedure dose of prophylactic antibiotics to provide antistaphylococcal coverage is advisable. Particular attention must be given to antiseptic preparation of the catheter tubing in addition to creating a sterile surgical field for the procedure. After catheter manipulation is performed, restoration of flow function is checked by syringe irrigation. Failure rates for fluoroscopic manipulation as high as 90% were observed when patients had an antecedent history of abdominopelvic surgery or peritonitis, suggesting that adhesions play a major factor in technical failures. Laparoscopy has become an invaluable method of evaluating and resolving catheter flow obstruction. Because laparoscopy can reliably identify the source of flow dysfunction and provide a means for definitive treatment, it is often considered as the next step in the management sequence after other causes for obstruction have been excluded. The dialysis catheter frequently can be used to perform the initial gas insufflation of the abdomen since most catheter obstructions represent outflow problems. Alternatively, a Veress needle is used for insufflation, or the initial laparoscopic port is placed by direct cutdown on the peritoneum. Additional laparoscopic ports for introduction of operating instruments may be required depending on the findings. Omental attachment to the catheter coil with displacement of the tubing out of the pelvis is a common cause of outflow dysfunction. Omental entrapment is relieved by using laparoscopic grasping forceps to strip the omentum from the catheter. The catheter tip is temporarily exteriorized through one of the port sites to facilitate removal of residual intraluminal tissue debris. The omentum is laparoscopically sutured to the upper abdominal region (omentopexy) to keep it away from the catheter. Redundant epiploic appendices of the sigmoid colon and uterine fimbria may siphon up to the catheter coil and produce obstruction. Laparoscopic resection of the involved epiploic appendices and uterine tube prevents recurrent obstruction. Adhesiolysis for poor drainage function, especially after peritonitis, is associated with a 30% failure rate secondary to reforming of adhesions. Catheter tip migration to a position of poor drainage function is frequently caused by shape-memory resiliency forces of a straight catheter bent into a configuration that imposes excessive stress on the tubing. Simply repositioning the catheter will be followed by recurrence of the migration in a high percentage of cases. Laparoscopic suturing of the catheter tip to a pelvic structure has an unacceptable rate of failure due to erosion of the suture. A more reliable approach is to laparoscopically place a suture sling in the suprapubic region through the abdominal wall and around the catheter. A sling will maintain the catheter toward the pelvis and not hinder catheter removal if required at a later date. Erosion of the superficial cuff through the exit site can result from positioning the cuff too close (<2 cm) to the exit wound during catheter placement. In addition, excessive bending of the catheter with a straight intercuff segment to produce a downward exit direction can induce mechanical stresses on the tubing. In combination with close proximity of the cuff to the exit site, the shape-memory forces of a catheter bent into this configuration can lead to tube straightening over time with migration of the superficial cuff toward and through the exit site. Another cause for superficial cuff erosion that can eventually result in extrusion of the entire catheter is outer displacement of the tubing due to poor location and fixation of the deep cuff. Lastly, exitsite infection extending to the superficial cuff may cause it to separate from the surrounding tissues and extrude through the exit site. An extruded cuff becomes a reservoir of bacteria within the vicinity of the exit wound. Exacerbated by daily wetting of the cuff during routine exit-site care, the presence of this infected sponge interferes with maintaining acceptable exit-site hygiene. Using a scalpel blade applied parallel to the cuff surface, the cuff can be shaved in repetitive slices until all of the cuff material is removed. The blade should be changed often to assure ease in performing the shave without applying undue pressure on the tubing. Alternatively, catheters with extruded cuffs can Chapter 23 / Peritoneal Dialysis Catheters, Placement, and Care 445 be managed by replacing the cuffed tubing segment by a splicing procedure, as described in the following section. Details of antibiotic treatment for catheter infections are discussed in Chapter 27. The eventual outcome of a chronic exit-site infection with superficial cuff involvement is a tunnel abscess or progression of the tunnel infection to the peritoneal cavity, producing concurrent peritonitis. Early recognition of chronic exit-site and tunnel infection is essential to provide the best opportunity for catheter salvage. Exit-site infection presents as redness, swelling, and tenderness at the exit site. With tunnel involvement, the signs of infection extend along the subcutaneous course of the catheter. In most cases, exit-site and tunnel infections are accompanied by purulent discharge from the exit site. In chronic smoldering cases, the exit-site skin is loose around the catheter, granulation tissue is present at the skin exit sinus, and purulent material can be expressed through the exit orifice with pressure over the subcutaneous cuff or stroking the skin over the tunnel toward the exit site while gently tugging on the catheter. As long as the infection has not extended to the deep cuff, it is possible to resolve the problem without losing the catheter or interrupting therapy. Ultrasonography of the catheter tunnel is a useful preoperative tool to evaluate for deep cuff involvement, particularly in obese patients where physical signs are often unreliable. Patients found to have infection involving the deep cuff on ultrasonography should undergo catheter removal. Moreover, patients with concurrent peritonitis are not candidates for catheter salvage procedures, as peritonitis suggests that transmural spread of the infection has already occurred. Unroofing the skin and subcutaneous tissue overlying the infected catheter tunnel permits drainage of pus, debridement of granulation tissue, and shaving of the superficial cuff. The catheter, including the shaved tubing segment, is directed out of the medial aspect of the incision and stabilized in this position by securing it to the adjacent skin with sterile adhesive strips. The wound is left open with performance of wet-to-dry dressing changes (once or twice daily) with saline-soaked gauze, and allowed to heal by secondary intention. Depending on the magnitude of the infection, the procedure can be performed in the treatment room or operating room under local or general anesthesia. This may be the preferred salvage procedure for a badly chosen exit-site location that was placed in an infection-prone area, such as within a skin crease, on the apex of a flabby skin fold, or under the belt line. The spliced catheter segment can be routed to a more stable exit-site location including the upper abdomen or chest region.
Cheap 0.1mg clonidine with amex
Other B-cell lymphomas Any subtype of B-cell lymphoma can arise in a colorectal site pulmonary hypertension 60 mmhg buy clonidine with a mastercard, including those thought to arise from peripheral lymph node equivalents. Prognosis the relevant prognostic factors in colorectal lymphomas are similar to those for the small intestine, and have been described in detail in that section. Sobin Definition A variety of benign and malignant mesenchymal tumours that arise in the large intestine as a primary site. Aetiology Aetiological factors are poorly understood for most colorectal mesenchymal tumours. An angiosarcoma has been reported in the colon, related to a persistent foreign body 149. Pathological features Lipomas are composed of mature adipose tissue and are surrounded by a fibrotic capsule. Lipomas should be distinguished from lipohyperplasia of the ileocaecal valve 1726. Most patients with the former have neurofibromatosis, and in these cases plexiform neurofibromas are common. Vascular tumours are classified into benign (such as haemangiomas, lymphangiomas and angiomatosis) and malignant (such as haemangioendotheliomas and angiosarcomas). Histologically typical are sheets of spindle cells interspersed by clusters of extravasated erythrocytes. Leiomyomas usually are detected in the rectum and colon as small polyps arising from the muscularis mucosae, and consist of well-differentiated smooth muscle cells with a similar immunohistochemical profile as observed in oesophageal leiomyomas 1227. Leiomyomatosis has been described in the colon with a circumferential semiconstrictive growth in a 35 cm long segment 529. It is not known whether colorectal leiomyomas and leiomyomatosis have the same colla- A 142 Tumours of the colon and rectum B. Many tumours grow beyond the rectal wall making radical surgery difficult and recurrences common. The survival from large bowel stromal/ smooth muscle sarcomas appears to be slightly higher than that of the small bowel and lower than that of the stomach and oesophagus 461. Despite its short length, the anal canal produces a variety of tumour types reflecting its complex anatomic and histological structure. Squamous, glandular, transitional, and melanocytic components occur at this site, either alone, or in combination. Parc Definition Tumours that arise from or are predominantly located in the anal canal. Topographic definition of anal canal and anal margin the anal canal is defined as the terminal part of the large intestine, beginning at the upper surface of the anorectal ring and passing through the pelvic floor to end at the anus 68. The most important macroscopic landmark in the mucosa is the dentate (pectinate) line composed of the anal valves and the bases of the anal columns. The lower part extends from the dentate line and downwards to the anal verge and has formerly been called the pecten. It is covered by squamous epithelium, which may be partly keratinized, particularly in case of mucosal prolapse. The perianal skin (the anal margin) is defined by the appearance of skin appendages. There are few published, histologically verified incidence rates of anal cancer 540, 600, 1213. For both men and women, urban populations are at higher risk than rural populations 540, 600, 1213, and there are considerable racial differences in incidence. In the United States, blacks tend to have higher incidence rates than whites 1213, while Asians and Pacific Islanders appear to be at very low risk 70. Homosexual men appear to constitute a group at particular risk 368, 538, 140, 96, 369, 540, 1213, 1690, 730. A strong association with tobacco smoking has been established in women, but the role of smoking in men is less clear 367, 539, 730, 733. Haemorrhoids and fissures, fistulae and abscesses in the anal region were long considered predisposing factors 192, 198, 1618. However, three case-control studies 368, 537, 733 and two cohort studies 541, 1074 failed to support the association. Oestrogen and androgen receptors have been found in the anal mucosa and its supportive tissue 1396, suggesting a physiological role of sex hormones in their maintenance. Clinical features Symptoms and signs Anal intraepithelial neoplasia is often an unexpected finding in minor surgical specimens. Clinical manifestations of anal cancer are often late and non-spe- cific and are mainly related to tumour size and extent of infiltration. They include anal pruritus, discomfort in sitting position, sensation of a pelvic mass, pain, change in bowel habit, incontinence due to sphincter infiltration, discharge, bleeding, fissure, or fistula. The initial nonspecificity of clinical features explains why diagnosis can be delayed 855, 1621, 1719, 1835. The clinical diagnosis of an anal tumour should always be confirmed by histological examination. The biopsy should be accompanied by an exact description of location and appearance of the biopsy site. An excisional biopsy is inadvisable, because wound healing delay would postpone optimal chemo-radiotherapy treatment. Enlarged lymph nodes may be excised or biopsied with needle aspiration under radiological control. Macroscopy the tumour may present as a small ulceration or fissure with slightly exophytic and indurated margins, and irregular thickening of the anoderm and anal margin with chronic dermatitis. If ulceration and infiltration develop, the lesion becomes fixed to the underlying structures and may bleed. In advanced stages, the sphincteric muscles are deeply infiltrated although there may be little mucosal ulceration. The examination should include resection lines in all directions and a careful search for lymph nodes. Clinical results of the combined treatment regimes are comparable or even better than those for surgery alone, but detection of residual disease can be more difficult by imaging techniques due to local fibrosis. In such cases a transanal full thickness tru-cut needle biopsy may be helpful 785. In 15-20% of cases, the lesion may infiltrate the lower rectum and the neighbouring organs including the rectovaginal septum, bladder, prostate and posterior urethra, sometimes with suppuration and fistulas. Tumours proximal to the pectinate line drain into the pelvis along the middle rectal vessels to the pelvic side walls and internal iliac chains and superiorly via the superior rectal vessels to the periaortic nodes. Tumours distal to the dentate line drain along cutaneous pathways to the inguinal and the femoral nodal chains. Inguinal lymph nodes can be involved bilaterally in a small number of cases at time of presentation. Retrograde lymphatic drainage occurs in advanced cases when the lymphatics are obstructed by malignant spread 1621, 1719. One pattern is that of large, pale eosinophilic cells and keratinization of either lamellar or single cell type. Another is that of small cells with palisading of the nuclei in the periphery of tumour cell islands. The invasive margin can vary from well circumscribed to irreg- ular, and a lymphocytic infiltrate may be pronounced or absent. This is probably the reason that the proportion of basaloid carcinoma in larger series has varied from 10 to almost 70 %, and that no significant correlation between histological subtype and prognosis has been established. In addition, the histological diagnosis is nowadays nearly always performed on small biopsies, that may not be representative for the whole tumour 492. Apart from the verrucous carcinoma mentioned below, only two rare histological subtypes seem to have a different biological course, both having a less favourable prognosis 1734. The other is characterized by a rather uniform pattern of small tumour cells with nuclear moulding, high mitotic rate, extensive apoptosis and diffuse infiltration in the surrounding stroma. This has been called small cell (anaplastic) carcinoma, but should not be confused with small cell carcinoma (poorly differentiated neuroendocrine carcinoma).
0.1mg clonidine otc
Patients with juvenile polyposis usually present with gastrointestinal bleeding blood pressure cuff name cheap 0.1mg clonidine, manifesting as haematochezia. Melaena, prolapsed rectal polyps, passage of tissue per rectum, intussusception, abdominal pain, and anaemia are also common. Air contrast barium enema and upper gastrointestinal series may demonstrate filling defects, but are non-diagnostic for juvenile polyps. Biopsy or excision of polyps by colonoscopy can be both diagnostic and therapeutic. Small juvenile polyps may resemble hyperplastic polyps, while larger polyps generally have a welldefined stalk with a bright red, rounded head, which may be eroded. Macroscopy Most subjects with juvenile polyposis have between 50-200 polyps throughout the colorectum. The rare and often lethal form occurring in infancy may be associated with a diffuse gastrointestinal polyposis 1643. In cases presenting in later childhood to adulthood, completely unaffected mucosa separates the lesions. This is unlike the dense mucosal carpeting that is characteristic of familial adenomatous polyposis. The individual lobes are relatively smooth and separated by deep, well-defined clefts. The multilobated polyp therefore appears like a cluster of smaller juvenile polyps attached to a common stalk. Such multilobated or atypical juvenile polyps account for about 20% of the total number of polyps 847. A B Age and sex distribution Two-thirds of patients with juvenile polyposis present within the first 2 decades of life, with a mean age at diagnosis of 18. Though extensive epidemiological data do not exist, incomplete penetrance and approximately equal distribution between the sexes can be presumed. Localization Polyps occur with equal frequency throughout the colon and may range in number from one to more than a hundred. Some patients develop upper gastrointestinal tract polyps, most often in the stomach, but also in the small intestine. The contour of polyps is highly irregular, fronded, in contrast to solitary sporadic juvenile polyps. The bizarre architecture differs from the round, uniform structure of sporadic juvenile polyps. A B Histopathology Smaller polyps are indistinguishable from their sporadic counterparts. In the multilobated or atypical variety the lobes may be either rounded or finger-like. Glands show more budding and branching but less cystic change than the classical solitary polyp 847. Cancer in juvenile polyposis There are two histogenetic explanations for the well documented association between colorectal cancer and juvenile polyposis. Alternatively, they may develop through dysplastic change within a juvenile polyp. While both mechanisms may apply, pure adenomas are uncommon in juvenile polyposis. By contrast, foci of low-grade dysplasia may be demonstrated in 50% of atypical or multilobated juvenile polyps. The dysplastic areas may increase in size, generating a mixed juvenile polyp/adenoma. These anomalies most commonly involve the heart, central nervous system, soft tissues, gastrointestinal tract and genitourinary system 316, 1202. Several patients have been reported with ganglioneuromatous proliferation within juvenile polyps 428, 1218, 1513, 2081, and others with pulmonary arteriovenous malformations and hypertrophic osteoarthropathy 348, 1760, 101, 333. The complexes translocate into the nucleus, where they regulate transcription of target genes. It is expressed ubiquitously in different human organ systems, as well as during murine embryogenesis. Haplotype analyses indicate that this is due to a mutation hotspot, rather than an ancient founder mutation 531, 751. The families segregating this particular mutation tend to be large, perhaps indicating high penetrance. Prognostic factors the most severe form of juvenile polyposis presents in infancy, with diarrhoea, anemia, and hypoalbuminemia; these patients rarely survive past 2 years of age. Although polyps in juvenile polyposis patients have classically been described as hamartomas, they do have malignant potential. The risk of colorectal carcinoma is approximately 30-40% and that of upper gastrointestinal carcinoma is 10-15% 749. Typical age of colon carcinoma diagnosis is between 34 and 43 years (range 15-68 years), and upper gastrointestinal carcinoma 58 years (range 21-73 years) 749, 847, 834. Most cases occur in patients who have not been screened radiologically or endoscopically, suggesting that cancers may be preventable through close surveillance. Affected family members have a high risk of developing breast and non-medullary thyroid carcinomas. Clinical manifestaions further include mucocutaneous lesions, thyroid abnormalities, fibrocystic disease of the breast, gastrointestinal hamartomas, early-onset uterine leiomyomas, macrocephaly, mental retardation and dysplastic gangliocytoma of the cerebellum (Lhermitte-Duclos). It has variable expression and an age-related penetrance although the exact penetrance is unknown. By the third decade, 99% of affected individuals have developed the mucocutaneous stigmata although any of the other features could be present already (see Table 6. Despite this, the most com- monly reported manifestations are mucocutaneous lesions, thyroid abnormalities, fibrocystic disease and carcinoma of the breast, gastrointestinal hamartomas, multiple, early-onset uterine leiomyoma, macrocephaly (specifically, megencephaly) and mental retardation 1819, 665, 1152, 1096. Epidemiology the single most comprehensive clinical epidemiological study estimated the prevalence to be 1 per million population 1819, 1334. Once the gene was identified 1071, a molecular-based estimate of prevalence in the same population was 1:200 000 1333. Because of the difficulty in recognizing this syndrome, prevalence figures are likely underestimates. Several varieties of hamartomatous polyps are seen in this syndrome, including lipomatous and ganglioneuromatous lesions 2075. Those in the colon and rectum usually measure from 3 to 10 millimetres but can reach 2 centimetres in diameter. Some of the polyps are no more than tags of mucosa but others have a more definite structure. Most are composed of a mixture of connective tissues normally present in the mucosa, principally smooth muscle in continuity with the muscularis mucosae 242. The mucosal glands within the lesion are normal or elongated and irregularly formed but the epithelium is normal and includes goblet cells and columnar cells 242. Lesions in which autonomic nerves are predominant, giving a ganglioneuroma-like appearance, have been described but seem to be exceptional 1017. In the general population, lifetime risks for breast and thyroid cancers are approximately 11% (in women), and 1%, respectively. The mean age at diagnosis is likely 10 years earlier than breast cancer occurring in the general population 1819, 1096. Because of small numbers, it is unclear if the age of onset is truly earlier than that of the general population. Histologically, the thyroid cancer is predominantly follicular carcinoma although papillary histology has also been rarely observed 1819, 665, 1152 (Eng, unpublished observations). The most important benign tumours are trichilemmomas and papillomatous papules of the skin. Apart from those of the skin, benign tumours or disorders of breast and thyroid are the most frequently noted and probably represent true component features of this syndrome (Table 6. Exons 1 through 6 encode amino acid sequence that is homologous to tensin and auxilin 1065, 1820, 1068. Detailed expression studies in Cowden syndrome 133 development have not been performed.
Clonidine 0.1 mg on line
Some of them can also perform plasmapheresis arterivirus buy 0.1mg clonidine, which is beyond the scope of this chapter. One cannot review them all, and the selection of devices described below should not be considered to be an endorsement of these devices over their competitors. The addition of the preblood pump allows for infusion of fluid in predilution mode or for continuous infusion of anticoagulant into the circuit. Simultaneous pre- and postfilter dilution can be performed by two integral pinch valves that control delivery of replacement fluid to the circuit. Control of ultrafiltration and net patient fluid removal is achieved using an integrated control panel with touch screen, which regulates the dialysate, effluent, preblood pump, and substitution fluid pump speeds. Other features include preconnected cartridge sets that include the filter, a programmable anticoagulant syringe, and optional blood warmer. Furthermore, urea kinetic modeling does not consider middle- or large-molecular-weight solute clearance, and the impact of the latter remains unclear. If desired, subtract this from the total urea clearance to obtain the extracorporeal urea clearance that will be required. Set this equal to the required extracorporeal urea clearance, assuming 100% saturation. This is simply equal to the required drainage volume minus the expected removal (L per day) of excess fluid. A 24-hr urine collection from day 1 to day 2 contains 5 g (178 mmol) of urea nitrogen. Initial total-body water: Initial weight is 60 kg with 8 kg estimated edema fluid. Final total-body water: Final weight is 64 kg, or 4 kg higher, all of which is water, so final total-body water is 36. If time 1 and time 2 are 24 hr apart, then the change in body urea nitrogen content is ~11. Urinary urea nitrogen loss during the 24-hr observation period was measured to be 5 g per day (178 mmol per day). This patient actually had a urea clearance of about 10 L per day (about 7 mL/min), so we can subtract this from the required total clearance. This should be 32 L per day (assuming 100% saturation) minus the volume of excess fluid removal. For example, if we need to remove 3 L of fluid per day to offset hyperalimentation and fluid given with medications, subtract 3 L from 32 L in the example to obtain a required dialysate inflow rate of 29 L per day. We usually ignore residual renal function, because this may be ephemeral, and so we would add back the 10 L per day and use a dialysis solution inflow rate of 39 L per day. Further advancements have been introduced dialysis equipment, but some standard dialysis machines need to be altered to permit delivery of a dialysis solution flow rate of 100 mL/min. Ultrafiltration or variable sodium profiles are not available, and there is no ultrafiltrate time or target goal to set. Clearance, on the bottom, is read from the intersection of the urea nitrogen generation level (g) and the steady-state goal serum urea nitrogen. The dropin, single-use cartridge design, with or without a preattached filter, allows for a range of therapies and minimizes cycler maintenance and disinfection requirements. The cartridge has volume chambers for volumetric balancing, thus eliminating the need for scales, and discharges effluent directly to drain. It operates on a three-pump system (blood, dialysis/infusion solution, ultrafiltration) and an electronic single weighing cell. This machine also features a simplified user interface, an integrated fluid plate warmer, and choice of dialyzer capabilities. In most patients at low risk of bleeding, sys- temic heparin is routinely used as it is inexpensive and easy to implement. The filter will clot periodically and will need to be changed at more frequent intervals. When heparin is not given, several steps may be taken to reduce the likelihood of clotting. The higher dialysate flow rate will compensate for the anticipated loss of clearance as the unheparinized dialyzer slowly clots. Keeping the blood flows at 200 mL/min or higher may also prevent early or excessive clotting. When heparin is not used in patients without coagulation disturbances, the dialyzers will usually clot within 8 hours. Calcium citrate complexes are removed in the effluent and those that return to the circulation are metabolized by the liver and skeletal muscles. Citrate anticoagulation, by reducing local ionized calcium concentration, may also reduce neutrophil and complement activation in the extracorporeal circuit (Schilder, 2014). On average, 3 mmol of citrate per liter of blood circulated is required to suppress the postfilter plasma ionized calcium to 0. Calcium and magnesium losses are replaced by systemic infusions according to strict protocols. This in turn can lead to high anion gap metabolic acidosis (citrate) and a high (>2. These have an advantage of avoiding the return of a lowionized calcium infusate close to the heart in the event that the calcium replacement solution pump fails. A negative pressure valve is inserted into this line so that the infusion will occur in the direction of the blood pump and not directly into the patient should the blood pump stop. A calcium chloride infusion (20 mg/mL in normal saline) is infused via a three-way stopcock valve placed at the venous port of the dialysis catheter. Calcium gluconate infusion may also be given via a peripheral vein catheter, but this will result in higher fluid volumes. The ionized calcium samples should be drawn from two sites and labeled carefully, one being "postfilter" from the postfilter venous sample port and the other from the patient via a systemic arterial or a venous line. The dialysis solution with this method is calcium free and contains sodium 135 mM, magnesium (in the form of magnesium sulfate) 1. A number of these have been described, including that by Fiaccadori (2013), as well as an automated system by Szamosfalvi (2010); the latter group is also working on sensors to measure citrate and ionized calcium levels (Yang, 2011). Low-molecular-weight heparins: Sagedal and Hartmann (2004) argatroban are direct thrombin inhibitors. The dose has to be adjusted according to residual renal clearance and dialysis clearance. These antibodies enhance the anticoagulation effects of lepirudin, and a reduction of the infusion dose may be needed to minimize bleeding risk. Argatroban is eliminated predominantly by liver metabolism and biliary secretion, and for this reason may be a preferred agent in renal failure patients. The administration of fresh frozen plasma is required to reverse bleeding due to overdosage of lepirudin or argatroban. Hemofiltration with high-flux dialyzers can reduce the plasma concentration of hirudin. Nafamostat mesylate is a synthetic serine protease inhibitor and prostacyclin analog with minimal hypotensive activity.
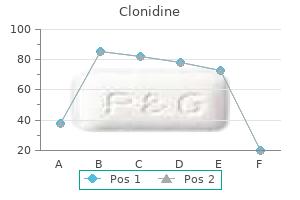
Discount clonidine 0.1mg without prescription
The many reports of phenytoin clearance are conflicting; thus heart attack 40 year old male purchase clonidine 0.1 mg mastercard, it is necessary to carefully monitor unbound drug levels. We generally recommend that all scheduled medications be given immediately after the procedure. Category I includes disorders for which apheresis is accepted as first line of therapy. In these cases, apheresis should be initiated as soon as possible for achieving optimal outcomes. Early use of plasmapheresis is strongly indicated, since the response rate is highest when the serum creatinine is relatively low (<500 mcmol/L or 5. In the largest long-term study using plasmapheresis together with immunosuppressive drugs, almost all patients with creatinine <500 mcmol/L (5. In oliguric dialysisdependent patients, particularly with a high percentage of crescents on renal biopsy, plasmapheresis should probably be reserved for those with pulmonary hemorrhage, because renal function is unlikely to recover. In the large series described earlier, patients received exchange of 50 mL/kg (approximately 1. Other authors would advise exchange of two plasma volumes daily for 7 days, followed by alternate day plasmapheresis for another week. If still indicated clinically, renal biopsy could be performed after the first two or three exchanges, deferring plasmapheresis for 24 hours after biopsy. Citrate anticoagulation may be preferred, where available, in the presence of lung hemorrhage or after renal biopsy. If the patient is severely fluid overloaded, the amount of albumin solution can be reduced to 85% (but not less) of the removed plasma volume. Since relapse may recur promptly on stopping treatment, vascular access should be maintained until platelet count is stable. In patients in whom platelet count decreases to <100,000/mm3, plasmapheresis may be recommenced on an alternate day schedule until platelet count stabilizes. Plasmapheresis has been used for the treatment of cryoglobulinemia for over 20 years because of effective removal of the large immune complexes responsible for clinical features. Although there are no controlled trials, there are multiple reports demonstrating the efficacy of plasma exchange in patients with acute vasculitis and renal involvement. In severe cases, immunosuppressive drugs are also used, together with antiviral therapy in those with hepatitis C. Replacement fluid should be 5% albumin, which must be warmed to avoid precipitation of circulating cryoglobulins. In occasional patients, long-term treatment once a week is required to control symptoms. Use of a centrifugation device is often preferred because of the possibility of the cryoglobulins blocking the plasma filter as they cool and precipitate. Alternative techniques such as double cascade filtration and cryofiltration are expensive and technically difficult, and are not widely used. These patients have a small vessel vasculitis often affecting the kidney, with pauci-immune rapidly progressive glomerulonephritis. Although early trials did not produce clearcut results, Pusey (1991) demonstrated the benefit of plasma exchange, together with immunosuppressive drugs in patients already requiring dialysis. Another recent smaller study reported the benefit of plasmapheresis in patients with a creatinine >250 mcmol/L (2. A recent meta-analysis confirmed the benefit of adjunctive plasmapheresis compared with standard therapy in preventing development of end-stage renal disease. Some patients may require longer periods of treatment, depending on their clinical response. Multiple myeloma can lead to renal impairment through a wide variety of mechanisms, the commonest of which is light-chain cast nephropathy. Although plasmapheresis effectively removes the paraprotein responsible, early trials produced conflicting results. A retrospective study from the Mayo Clinic suggested the benefit of plasmapheresis in patients with proven cast nephropathy who had high light-chain levels and severe renal impairment. In general, we would suggest a regimen of five consecutive exchanges for 5% albumin in patients presenting with acute kidney injury due to light-chain nephropathy. Depending on the clinical response and paraprotein levels, longer treatment may be needed in some patients. An alternative approach to plasmapheresis that has gained favor in the past 5 years is based on effective removal of light chains by hemodialysis using a special high-cutoff dialyzer. In addition to standard chemotherapy, with or without bortezomib, very intensive dialysis is done. In the initial study, in patients with acute renal failure secondary to multiple myeloma, two high-cutoff filters (Theralite, Gambro Renal Products) were connected in series, and 8-hour dialysis sessions were given daily for the first 5 days, followed by 8-hour sessions on alternate days for the next 12 days, followed by 6-hour treatments three times per week. Four grams of salt-poor albumin were given at the end of each extended dialysis session, and intravenous magnesium and oral calcium were given if predialysis levels were low (Hutchison, 2009). Response was encouraging, in terms of sizeable reduction in serum-free light chains and a high percentage of patients recovering renal function. Plasmapheresis has been widely used in lupus nephritis to remove circulating autoantibodies and immune complexes. Despite positive anecdotal reports, one randomized controlled trial showed no benefit of the addition of plasmapheresis to immunosuppressive drugs in patients with lupus nephritis followed up for 3 years. However, patients with crescentic nephritis and those requiring dialysis were excluded, and it could be argued that short-term intervention such as plasmapheresis would have a better effect in these patients. An international trial using high-dose cyclophosphamide synchronized with plasmapheresis was suspended because of a high incidence of adverse effects, so this approach cannot be recommended. There are also reports of the use of immunoadsorption using protein A columns in patients with severe disease unresponsive to other treatment. In the absence of adequate information, we would suggest the use of exchange of 1 plasma volume for 5% albumin for at least 5 consecutive days, and perhaps for longer, depending on clinical response, in patients with rapid recurrence of proteinuria following renal transplantation. The successful use of plasmapheresis, usually with immunosuppressive drugs, has been reported in several small series of patients. We have observed improvement in renal function in some patients treated with this approach. Although there are no controlled trials, there are several reports of the benefit of plasmapheresis in controlling clinical features pending the effects of treatment for the underlying disorder. The use of plasmapheresis in desensitization protocols for high-risk patients should only be carried out in specialized centers. However, there are case reports of plasmapheresis being used in Amanita phalloides mushroom poisoning, to help clear digoxin-Fab complexes in patients with renal failure, to treat snakebite or cisplatin overdose, and to remove infused monoclonal antibodies when this is required (Schutt, 2012). While conventional plasmapheresis can remove tar- get plasma elements such as immunoglobulins, cryoproteins, and lipids, it does so without specificity and requires replacement solutions such as albumin and donor plasma, which can be expensive and lead to adverse reactions. Selective apheresis procedures have been developed to target and remove a specific element from the plasma, and return all other plasma proteins, thus eliminating the need for replacement solutions and the loss of beneficial plasma constituents. The precipitate is then removed from the plasma by a polycarbonate membrane, and the heparin removed by a heparin adsorber, and, finally, the plasma is restored to a physiologic pH via bicarbonate dialysis. Owing to high costs, these columns are typically regenerated and stored, which can be a cumbersome process. There is also an immunoadsorptive device (Lipopak, Pocard, Moscow, Russia) that is marketed to target lipoprotein(a), which is an independent risk factor for coronary heart disease. There are a variety of columns available worldwide that have been designed to selectively bind a target molecule and remove it from the circulating plasma. Finally, many immunoadsorption columns have been developed that contain either an immobilized antigen or peptide designed to bind a specific circulating antibody or molecule.
Purchase clonidine without prescription
In some cases blood pressure side effects trusted clonidine 0.1 mg, there are variable degrees of cellular atypia and multilayering of nuclei. Von Meyenburg complex (biliary microhamartoma) the lesions are small, up to several mm in diameter. Within a fibrous or hyalinized stroma, they present as irregular or round ductal structures that appear somewhat dilated and have a flattened or cuboidal epithelium. Their fibrous stroma shows varying degrees of chronic inflammation and collagenization. Biliary adenofibroma is characterized by a complex tubulocystic biliary epithelium without mucin production, together with abundant fibroblastic stromal components 1972. Its expansive growth, and foci of epithelial tufting, cellular atypia and mitoses favor a neoplastic process. Intrahepatic peribiliary cysts In chronic advanced liver disease and Diffuse and multifocal hyperplasia of peribiliary glands Diffuse, severe, macroscopically recognizable dilatation and hyperplasia of the peribiliary glands of intrahepatic and extrahepatic bile ducts is a rare condition 1319, 437. Small, normal appearing proliferating bile ducts associated with a small connective tissue component and lymphocytic infiltration. The mutations are random with no specific hot spot, being mostly missense mutations and less frequently nonsense mutations 887. Overexpression of c-erbB-2 occurs in one fourth to about two thirds of carcinoma of the biliary tract, and may be used as a phenotypic marker for neoplastic transformation 1912. It also correlates with the markedly increased proliferation indices seen in precancerous glands and cholangiocarcinoma. Biliary epithelial cells are continuously exposed to genotoxic insults such as chronic inflammation and hydrophobic bile acids, predisposing to oncogenic mutations. Progression to malignancy may be due, in part, to failure in activating apoptosis and deleting cells with genetic damages 263. Lymph node spread, vascular invasion, positive margins and bilobar distribution are associated with a high recurrence rate and a poor prognosis. One study found the 5-year survival rate was 39% in patients with mass-forming tumours and 69% for intraductal tumours while no patients with mass-forming plus periductal-infiltrating tumours survived > 5 years 2161. Histologically, squamous cell or sarcomatous elements and mucinous variants confer a poor prognosis 1312, 1313. The 5-year survival rate in patients with lymph node metastases is significantly lower than that in patients without lymph node metastasis (51%). Concomitant hepatolithiasis prevents precise diagnosis preoperatively, and precipitates biliary sepsis. Ponchon Definition A rare tumour containing unequivocal elements of both hepatocellular and cholangiocarcinoma that are intimately admixed. This tumour should be distinguished from separate hepatocellular carcinoma and cholangiocarcinoma arising in the same liver 605. There are similar geographical distribution differences as for hepatocellular carcinoma and a similar age and sex distribution. Macroscopy Gross inspection does not show significantly different morphology compared to hepatocellular carcinoma. In tumours with a major cholangiocarcinomatous component with fibrous stroma, the cut surface is firm. Histopathology Combined hepatocellular and cholangiocarcinoma is the term preferred for a tumour containing both hepatocellular and distinct or separate cholangiocarcinoma. This category should not be used for tumours in which either form of growth is insufficiently differentiated for positive identification. Hepatocytes preferentially express cytokeratins 8 and 18 and, like duct epithelial cells, cytokeratins 7 and 19. However, the different patterns of expression are not as clear-cut in these tumours. Combined hepatocellular and cholangiocarcinoma 181 Bile duct cystadenoma and cystadenocarcinoma C. Ponchon Definition A cystic tumour either benign (cystadenoma) or malignant (cystadenocarcinoma), lined by epithelium with papillary infoldings that may be mucus-secreting or, less frequently, serous. They differ from tumours that arise in cystic congenital malformation and in parasitic infections and hepatolithiasis. Cystadenoma is seen almost exclusively in females, with cystadenocarcinoma appearing equally in males and females. Imaging techniques show multilocular cystic tumour(s), occasionally with tiny papillary folds in the cystic wall. Macroscopy the cysts are usually multilocular and typically range from 5 to 15 cm diameter 809. In cystadenocarcinoma, a large papillary mass may occur as well as solid areas of grey-white tumour in a thickened wall. Tumour spread and staging Cystadenocarcinomas show intrahepatic spread and metastasis to regional lymph nodes in the hepatoduodenal ligament. Distant metastases occur most frequent in the lungs, the pleura and the peritoneum. Histopathology Cystadenomas are usually multilocular and are well defined by a fibrous capsule, which may contain smooth muscle fibres. The contents of the locules are either thin, opalescent or glairy fluid, or mucinous semisolid material. The mucinous type is more common and is lined by columnar, cuboidal, or flattened mucus-secreting epithelial cells resting on a basement membrane; polypoid or papillary projections may be present. About 5% of the tumours reveal neuroendocrine differentiation, as identified by expression of chromogranin and synaptophysin. Subjacent to the basement membrane is a cellular, compacted mesenchymal stroma, which in turn is surrounded by looser fibrous tissue. This mesenchymal component is seen only in females and has been likened to ovarian stroma. The stromal cells express vimentin, and there are many cells that express smooth muscle actin. The lining epithelium is cuboidal and lies on ovarian-like stroma, beneath which is a band of dense tissue. A Large peribiliary cysts in the connective tissue of the hilus; the background liver shows advanced cirrhosis. The serous type consists of multiple, small locules lined by a single layer of cuboidal cells with clear cytoplasm containing glycogen. The cells rest on a basement membrane but are not surrounded by the mesenchymal stroma typical of the mucinous variety. Malignant change may not involve all of the epithelium lining the cyst; it is usually multifocal. The tumours are so well defined that complete removal can usually be achieved with good prognosis. Differentiation from intrahepatic bile duct cystadenoma depends on the demonstration of cytological (particularly nuclear) atypia, mitosis, and invasion of the underlying stroma. Some bile duct cystadenocarcinomas may be misdiagnosed as bile duct cystadenomas because insufficient sampling results in tumour morphology showing no cytological features of malignancy or invasion of the underlying stroma 351, 809, 1268, 2096. Prognostic factors the prognosis of patients with biliary duct cystadenocarcinomas is good if a curative resection is possible. Schmidt Definition A malignant embryonal tumour with divergent patterns of differentiation, ranging from cells resembling fetal epithelial hepatocytes, to embryonal cells, and differentiated tissues including osteoid-like material, fibrous connective tissue and striated muscle fibers. Four percent of hepatoblastomas are present at birth, 68% in the first two years of life and 90% by five years of age. A recent increase in the incidence of tumours in infants with birth weights below 1500 grams has been reported 776, 777, 1899. Localization Hepatoblastomas occur as a single mass in 80% of cases, involving the right lobe in 57%, the left lobe in 15% and both lobes in 27% of patients 1838. Multiple masses, seen in the other 20% of cases, may occur in either or both lobes. Clinical features Hepatoblastomas are often noted by a parent or physician as an enlarging abdomen in the infant that may be accompanied by weight loss or anorexia. Rarely, tumour cells may produce human chorionic gonadotrophin, leading to precocious puberty with pubic hair, genital enlargement and deepening voice, noted most prominently in young boys. Hepatoblastoma is accompanied by anemia in 70% of cases and by thrombocytosis in 50%, with platelet counts exceeding 800 x 109/L in nearly 30% of cases 1717. Other laboratory abnormalities can include elevated levels of serum cholesterol, bilirubin, alkaline phosphatase, and aspartate aminotransferase 10.
Order 0.1 mg clonidine mastercard
Ishikawa O blood pressure 200 over 120 generic clonidine 0.1 mg visa, Ishiguro S, Ohhigashi H, Sasaki Y, Yasuda T, Imaoka S, Iwanaga T, Nakaizumi A, Fujita M, Wada A (1990). Adenosquamous carcinoma of the pancreas: a clinicopathologic study and report of three cases. Ishikawa O, Ohigashi H, Imaoka S, Furukawa H, Sasaki Y, Fujita M, Kuroda C, Iwanaga T (1992). Preoperative indications for extended pancreatectomy for locally advanced pancreas cancer involving the portal vein. Immunohistochemical and molecular biological studies of serous cystadenoma of the pancreas. Primary undifferentiated small cell carcinoma of the esophagus: clinicopathological and flow cytometric evaluation of eight cases. Ito N, Kawata S, Tamura S, Takaishi K, Shirai Y, Kiso S, Yabuuchi I, Matsuda Y, Nishioka M, Tarui S (1991). Itoh T, Kishi K, Tojo M, Kitajima N, Kinoshita Y, Inatome T, Fukuzaki H, Nishiyama N, Tachibana H, Takahashi H, et a (1992). Acinar cell carcinoma of the pancreas with elevated serum alpha-fetoprotein levels: a case report and a review of 28 cases reported in Japan. Immunohistochemical and ultrastructural studies of twelve argentaffin and six argyrophil carcinoids of the appendix vermiformis. Iwafuchi M, Watanabe H, Ishihara N, Enjoji M, Iwashita A, Yanaihara N, Ito S (1987). Neoplastic endocrine cells in carcinomas of the small intestine: histochemical and immunohistochemical studies of 24 tumors. Prognostic value of immunohistochemically identifiable tumor cells in lymph nodes of patients with completely resected esophageal cancer. Primary hepatocellular carcinoma in hereditary haemorrhagic telangiectasia: a case report and literature review. Epidemiology of familial adenomatous polyposis in Finland: impact of family screening on the colorectal cancer rate and survival. Mucin histochemistry of the columnar epithelium of the oesophagus: a retrospective study. Characterisation of a subtype of colorectal cancer combining features of suppressor and mild mutator pathways. Abnormal immunoreactivity of the E-cadherin-catenin complex in gastric carcinoma: relationship with patient survival. Generalized intestinal polyposis and melanin spots of the oral mucosa, lips and digits. Does an erroneous diagnosis of squamous-cell carcinoma of the anal canal and anal margin at first physician visit influence prognosis Altered expression of the cyclin D1 and retinoblastoma genes in human esophageal cancer. Granular cell tumors of the gastrointestinal tract and perianal region: a study of 74 cases. Joslyn G, Carlson M, Thliveris A, Albertsen H, Gelbert L, Samowitz W, Groden J, Stevens J, Spirio L, Robertson M, et al (1991). Identification of deletion mutations and three new genes at the familial polyposis locus. Immunocytological detection of micrometastatic cells: comparative evaluation of findings in the peritoneal cavity and the bone marrow of gastric, colorectal and pancreatic cancer patients. A study of the ratio of hepatocellular carcinoma over cholangiocarcinoma and their risk factors. A newly recognized entity: intraductal "oncocytic" papillary neoplasm of the pancreas. Detection of K-ras and p53 gene mutations in pancreatic juice for the diagnosis of intraductal papillary mucinous tumors. Kaino M, Kondoh S, Okita S, Ryozawa S, Hatano S, Shiraishi K, Kaino S, Akiyama T, Okita K, Kawano T (1996). Multifocal pancreatic serous cystadenoma with atypical cells and focal perineural invasion. In vivo microscopy of hepatic metastases: dynamic observation of tumor cell invasion and interaction with Kupffer cells. The E-cadherin gene is silenced by CpG methylation in human hepatocellular carcinomas. Kato H, Tachimori Y, Watanabe H, Itabashi M, Hirota T, Yamaguchi H, Ishikawa T (1992). Kawanishi K, Shiozaki H, Doki Y, Sakita I, Inoue M, Yano M, Tsujinaka T, Shamma A, Monden M (1999). Prognostic significance of heat shock proteins 27 and 70 in patients with squamous cell carcinoma of the esophagus. Fine structure of three major grades of malignancy of human pancreatic adenocarcinoma. Primary pancreatic lymphoma associated with short bowel syndrome: review of carcinogenesis of gastrointestinal malignancies. Pancreatic metastasis of cardiac rhabdomyosarcoma diagnosed by fine needle aspiration. Mutations of the p53 tumor suppressor gene and the ras gene family in intrahepatic cholangiocellular carcinomas in Japan and Thailand. Frequency of resection, metastasis, and five-year survival rate of early gastric carcinoma in a surgical clinic. Histogenesis of gallbladder carcinoma from investigation of early carcinoma and microcarcinoma. Genetic changes of both p53 alleles associated with the conversion from colorectal adenoma to early carcinoma in familial adenomatous polyposis and non-familial adenomatous polyposis patients. Highly aggressive behavior and poor prognosis of small-cell carcinoma in the alimentary tract: flow-cytometric analysis and immunohistochemical staining for the p53 protein and proliferating cell nuclear antigen. Kimura H, Nakajima T, Kagawa K, Deguchi T, Kakusui M, Katagishi T, Okanoue T, Kashima K, Ashihara T (1998). Further evidence for prognostic significance of epidermal growth factor receptor gene amplification in patients with esophageal squamous cell carcinoma. Molecular pathology of c-kit proto-oncogene and development of gastrointestinal stromal tumors. Intraductal proliferation in the pancreas and its relationship to human and experimental carcinogenesis. Histological and fine structural features of pancreatic ductal adenocarcinomas in relation to growth and prognosis: studies in xenografted tumours and clinico-histopathological correlation in a series of 75 cases. Solid-cystic (papillary-cystic) tumours within and outside the pancreas in men: report of two patients. Kodama I, Kofuji K, Yano S, Shinozaki K, Murakami N, Hori H, Takeda J, Shirouzu K (1998). Lymph node metastasis and lymphadenectomy for carcinoma in the gastric cardia: clinical experience. Hepatocellular carcinoma in a patient with hereditary hemochromatosis and noncirrhotic liver. Hepatocellular carcinoma with sarcomatous change: a special reference to the relationship with anticancer therapy. No evidence of known types of human papillomavirus in squamous cell cancer of the oesophagus in a low-risk area. Kondo F, Wada K, Nagato Y, Nakajima T, Kondo Y, Hirooka N, Ebara M, Ohto M, Okuda K (1989). Biopsy diagnosis of welldifferentiated hepatocellular carcinoma based on new morphologic criteria. Kondo H, Sugano K, Fukayama N, Kyogoku A, Nose H, Shimada K, Ohkura H, Ohtsu A, Yoshida S, Shimosato Y (1994). Detection of point mutations in the K-ras oncogene at codon 12 in pure pancreatic juice for diagnosis of pancreatic carcinoma. Kozuka S, Sassa R, Taki T, Masamoto K, Nagasawa S, Saga S, Hasegawa K, Takeuchi M (1979). Clinical and pathologic study of 105 cases involving oral cavity, larynx and genitalia. Endoscopic mucosal resection of flat and depressed types of early colorectal cancer. Functioning pancreatic acinar cell carcinoma: immunohistochemical and ultrastructural analyses.
Purchase clonidine 0.1 mg
There is no specific method to either reduce lymphatic absorption or to correct impaired aquaporin function venice arrhythmia 2013 order 0.1 mg clonidine with visa. This approach may include shortening dwell times and using icodextrin for long dwells. Icodextrin may be particularly useful in aquaporin deficiency as the ultrafiltration it induces occurs almost exclusively via nonaquaporin channels (La Milia, 2006). Essentially, this involves the use of less hypertonic glucose (Johnson, 2012; Li, 2013). At first, such an approach might be expected to lead to less ultrafiltration and to a greater risk of fluid overload. It is possible, however, to find a balance between glucose sparing and volume control. Effective glucose-sparing strategies include salt and water restriction, the use of loop diuretics to maintain volume, and the use of renin angiotensin system inhibitors to preserve residual renal function. Icodextrin allows the reduction of daily glucose exposure, and there are studies suggesting more stable long-term membrane function with this solution (Davies, 2005). Antihypertensives, other than cardioprotective agents, should only be introduced if this approach has been unsuccessful. Preference should be given to agents that have a beneficial effect on urine volume or residual renal function, such as loop diuretics, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers. The choice of agent in many patients may be driven by coexisting medical conditions such as ischemic heart disease. The cause of hypotension is sometimes unclear, but approximately 20% of cases are secondary to heart failure. An additional 40% may be due to hypovolemia, and it is important to recognize this as hypotension in these patients typically responds to volume repletion and residual renal function may improve as well. Patients with hypotension due to cardiac causes and cases in which no cause can be identified have a poor prognosis, with a high early mortality rate. Agents such as midodrine and fludrocortisone have been used but with no proven long-term benefit. New onset hypotension may, of course, represent developing sepsis or acute cardiac injury. Chapter 26 / Volume Status and Fluid Overload in Peritoneal Dialysis 489 References and Suggested Readings Ates K, et al. Blood pressure, volume, and sodium control in an automated peritoneal dialysis population. Peritoneal glucose exposure and changes in membrane solute transport with time on peritoneal dialysis. Relation between malnutrition inflammation atherosclerosis and volume status: the usefulness of bioimpedance in peritoneal dialysis patients. Brain natriuretic peptide and impedance cardiography to assess volume status in peritoneal dialysis patients. Analysis of ultrafiltration failure in peritoneal dialysis patients by means of standard peritoneal permeability analysis. Association between serum n-terminal pro-brain natriuretic peptide concentration and left ventricular dysfunction and extracellular water in continuous ambulatory peritoneal dialysis patients. Effects of an angiotensin-converting enzyme inhibitor on residual renal function in patients receiving peritoneal dialysis: a randomized, controlled study. Randomized controlled trial of glucose-sparing peritoneal dialysis in diabetic patients. Hypotension in patients on chronic peritoneal dialysis: etiology, management, and outcome. Aquaporin-1 plays an essential role in water permeability and ultrafiltration during peritoneal dialysis. Hypertension in peritoneal dialysis patients: epidemiology, pathogenesis and treatment. Icodextrin increases technique survival rate in peritoneal dialysis patients with diabetic nephropathy by improving body fluid management: a randomized controlled trial. N-terminal pro-brain natriuretic peptide: an independent risk predictor of cardiovascular congestion, mortality, and adverse cardiovascular outcomes in chronic peritoneal dialysis patients. Furthermore, it is the most common cause of treatment failure, accounting for nearly 30% of the cases. The introduction of Y-set and double-bag disconnect systems has substantially reduced the incidence of peritonitis, particularly episodes caused by gram-positive organisms (Monteon, 1998; Li, 2002). This allows bacteria to gain access to the peritoneal cavity via the catheter lumen. Typically, the organisms involved are coagulase-negative staphylococci or diphtheroids. Bacteria present on the skin surface can enter the peritoneal cavity via the peritoneal catheter tract. Bacteria of intestinal origin can enter the peritoneal cavity by migrating across the bowel wall. This is the usual mechanism of peritonitis episodes associated with diarrheal states and/or instrumentation of the colon, and may also be seen with strangulated hernia. Less commonly, peritonitis is due to bacteria that have seeded the peritoneum from a distant site by way of the bloodstream. This is uncommon, but ascending infection may occur from the vagina via the uterine tubes into the peritoneum. The peritoneal leukocytes are critical in combating bacteria that have entered the peritoneal space by any of the routes already mentioned. A number of factors are now known to alter their efficacy in phagocytizing and killing invading bacteria. These unphysiologic conditions may inhibit the ability of peritoneal leukocytes to phagocytize and kill bacteria. High osmolality, low pH, and the presence of the lactate anion combine to cause inhibition of superoxide. There is now some evidence that newer normal pH, "biocompatible" solutions may reduce the peritonitis rate, but this has not been a consistent finding among published studies (Cho, 2014). The antimicrobial actions of peritoneal macrophages are enhanced by both calcium and cholecalciferol. Use of active vitamin D has been reported to reduce the rate of peritonitis (Kerschbaum, 2013). An increased risk of Staphylococcus epidermidis peritonitis has been reported with the use of low-calcium dialysis solutions (Piraino, 1992), but no subsequent confirmatory reports have been published. Using appropriate culture techniques, an organism can be isolated from the peritoneal fluid in over 90% of cases in which symptoms and signs of peritonitis and an elevated peritoneal fluid neutrophil count are present. The responsible pathogen is usually a bacterium, but fungal peritonitis occurs occasionally (Table 27. At least two of the following three findings should be present: (a) symptoms and signs of peritoneal inflammation, (b) cloudy peritoneal fluid with an elevated peritoneal fluid cell count (>100/mcL) due predominantly (>50%) to neutrophils, and (c) demonstration of bacteria in the peritoneal effluent by Gram stain or culture. Sometimes, especially in the elderly, the only symptoms are a relatively sudden loss of residual renal function and postural hypotension. On the other hand, abdominal pain can be present in dialysis patients owing to nonperitonitis-related abdominal causes; in those starting dialysis after a failed transplant in whom steroid treatment has been stopped, abdominal pain due to adrenal insufficiency should be considered. In most patients, sudden onset of cloudy fluid with appropriate abdominal symptoms is sufficient evidence of peritonitis to warrant initiation of antimicrobial therapy. Conversely, a relatively translucent peritoneal fluid does not completely exclude peritonitis. Cloudy fluid has been reported with the use of calcium channel blockers, presumably because they Chapter 27 / Peritonitis and Exit-Site Infection 493 27. Peritonitis is usually associated with an increase increase triglyceride concentration in the peritoneal fluid (Ram, 2012). After disconnecting the drain bag full of in the absolute number and percentage of neutrophils in the peritoneal fluid.