Buy 2mg hytrin amex
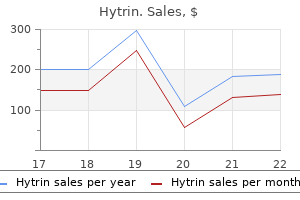
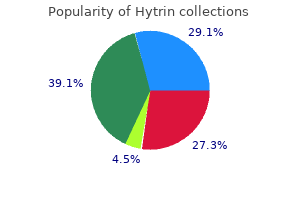
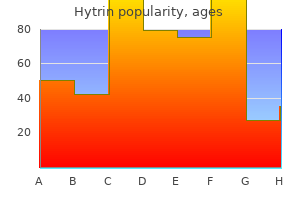
This results in release from the tonic control over prolactin secretion by the pituitary even when the tumour itself may be non-functioning arteria epigastrica cranialis superficialis commissura labiorum dorsalis 1mg hytrin free shipping. Although conceptions have occurred at some time in the future from the few remaining follicles ovulating, such conceptions are very uncommon. There are numerous causes of hyperprolactinaemia, although one of the most important is the presence of a pituitary tumour or prolactinoma, which has been detected in up to 10% of females on postmortem examination; however, the great majority of these are asymptomatic microadenomas. Alternatively, patients may present with symptoms such as galactorrhoea, menstrual disturbance or symptoms associated with large pituitary tumours such as visual disturbance or headache. However, this latter presentation is in fact relatively rare as most pituitary tumours are microadenomas which do not cause mass effects. Hyperprolactinaemia is an important cause of disruption to the menstrual cycle due to negative feedback of high prolactin levels on the hypothalamicpituitary axis. Effects of raised prolactin include a shortening of the luteal phase due to inadequate pre-ovulatory follicular development or, as levels rise causing negative feedback, hypogonadotrophic hypogonadism with resultant anovulation and/or amenorrhoea. Dopamine released from the hypothalamus reaches the pituitary via the hypophyseal-portal system of vessels and tonically inhibits the secretion of prolactin (dopamine is also known as prolactin inhibiting factor). Moderately raised prolactin is also seen occasionally in association with the polycystic ovarian syndrome, possibly due to the effect of increased unopposed oestrogen in the setting of chronic anovulation. Examination ought to note whether galactorrhoea is directly observed and include examination of visual fields. Given that small elevations of prolactin may occur physiologically, those noted with small to moderate degrees of hyperprolactinaemia ought to undergo repeat testing to confirm a persistent elevation in levels. In those without an obvious clinical cause, imaging should be undertaken to exclude a pituitary tumour. Formal assessment of visual fields is necessary for those with demonstrated pituitary tumours and may be performed serially in monitoring response after treatment. Expectant management Those with raised prolactin in the setting of a microadenoma or functional hyperprolactinaemia in the absence of any structural cause, and not desiring immediate fertility, may elect to undergo observation with yearly measurement of serum prolactin levels, especially if menstruation remains regular. Those whose symptoms are drug induced will usually experience resolution with withdrawal or reduction of medication if this is feasible. For those who are oestrogen deficient, replacement therapy ought to be considered in order to prevent loss of bone mineral density. This can be in the form of combined oestrogen-progestogen hormone therapy or the contraceptive pill. Although concern has been raised that high oestrogen levels could in fact increase the secretion of prolactin by direct action on pituitary lactotrophs, studies have shown this not to be the case in practice. Additionally, those with adequate oestrogen levels who are not menstruating regularly should have some cyclical progestogen therapy to prevent endometrial hyperplasia from prolonged exposure to unopposed oestrogen. Medical treatment Patients experiencing anovulation due to raised prolactin who desire fertility, as well as all those with macroadenomas, should undergo first-line treatment with dopamine receptor agonists. Bromocriptine is a shorter acting agent that is usually administered twice daily, but troublesome side effects of orthostatic hypotension leading to dizziness and fainting as well as nasal congestion, constipation, nausea and vomiting can occur, especially early on in treatment. Therefore, bromocriptine is usually started at a low nighttime dose and gradually increased over a period of weeks. Cabergoline is a longer acting agent that allows administration twice per week with at least similar efficacy and fewer reported side effects to bromocriptine. Whichever agent is chosen, withdrawal of therapy for a number of weeks after 12 months of therapy should be considered to assess whether spontaneous remission has occurred, with reinstatement of therapy if raised prolactin is detected off medication. Surgery and radiation therapy Surgical resection of pituitary tumours is usually reserved for situations where symptomatic tumours fail to respond to medical treatment or patients suffer intolerable side effects from such treatment. This is usually performed via a transsphenoidal approach and, where possible, medical treatment should continue until the time of surgery to prevent tumour re-expansion and reduce the volume for resection. Radiation, either external or brachytherapy, has been used in the treatment of macroadenomas but has been associated with higher rates of damage to surrounding normal structures. While the dosing regimen for cabergoline is more favourable, there is more clinical experience with bromocriptine in those desiring fertility, although no deleterious side effects have been noted to date with those who do in fact conceive on cabergoline. Dopamine agonists are successful in achieving ovulation and pregnancy in up to 90% of women where this is the sole cause of infertility. Despite a lack of evidence of teratogenicity, bromocriptine does cross the placenta and it is recommended that dopamine agonist therapy be ceased at diagnosis of pregnancy for most patients. In some cases of macroadenoma, patients may be continued on medication under close specialist supervision. Pregnancy may cause enlargement of the pituitary gland with clinical consequences, and this occurs in approximately 2% of microprolactinomas and 20% of macroprolactinomas. There is no contraindication to breastfeeding in the setting of prolactinomas; however, if treatment with dopamine agonists is needed in the postnatal period, they will cause suppression of lactation. A number of techniques are available to assist ovulation for these women, including medical treatment (in the form of oral medications or injectable gonadotrophins) and surgical techniques (such as laparoscopic ovarian diathermy in the setting of polycystic ovarian syndrome). The aim of all methods of ovulation induction is to restore unifollicular development, leading to the release of a single ovum in order to achieve a singleton pregnancy. However, due to the very nature of medications used to achieve ovarian stimulation, multiple pregnancy can result if the monitoring of response to treatment is inadequate. This is especially so given the fact that different women can have a remarkably different ovarian response to the very same dose of ovulation-inducing medication. It is given for 5 days in the follicular phase of the cycle, similar to clomiphene; however, it is less likely to cause negative effects of oestrogen deficiency on endometrial thickness due to its shorter half-life when compared to clomiphene. Despite this, it still remains a second-line agent due to the comparatively less experience with its use and safety profile compared with clomiphene, although the available data fails to demonstrate any known increased rate of congenital malformations with its use. Tamoxifen Tamoxifen is a selective oestrogen receptor modifier that has differing effects on the oestrogen receptors at different sites in the body. It is an antagonist at the hypothalamus while exerting an agonist effect on the bone and endometrium. Hence, it can induce ovulation when given in the follicular phase in a manner similar to clomiphene. However, it again is not used as widely for this indication due to there being less experience with it than with clomiphene and a lack of regulatory approval for this indication. Given that these medications work by increasing secretion from the anterior pituitary, they are only appropriate in situations of intact hypothalamo-pituitary function and therefore do not work in the setting of hypogonadotrophic hypogonadism. Other oral ovulation-induction agents Metformin Metformin is a biguanide medication used in type 2 diabetes that decreases hepatic gluconeogenesis and acts peripherally as an insulin sensitising agent. However, given the efficacy of drugs that directly act to restore ovulation, such as clomiphene, there is debate about the role of metformin for this indication. Metformin is probably better reserved for those with proven insulin resistance on formal glucose tolerance testing and for those with a body mass index above the normal range. Clomiphene citrate Clomiphene citrate is administered for 5 days in the early part of the menstrual cycle, usually from day 2 to day 6 or from day 5 to day 9. The manufacturers recommend a maximum of 100 mg daily, but many clinicians will increase to 150 mg or even 200 mg before resorting to gonadotophin therapy. Ultrasound can be used to track response to the medication and detect multifollicular development that will increase the risk of multiple pregnancy and lead to advice to avoid unprotected intercourse for that cycle. Testing of the mid-luteal progesterone level will give an indication if the dose of clomiphene utilised in that cycle was sufficient to induce ovulation or needs to be escalated for future cycles. Bromocriptine As discussed earlier in this chapter, dopamine agonists will restore ovulation in the majority of patients with hyperprolactinaemia. Alternatively, Letrozole Letrozole is an aromatase inhibitor which blocks the conversion of androgens to oestrogen. Close monitoring is vitally important in these cycles to detect those who over-respond to medication, with a higher risk of multiple pregnancy compared with other medical treatments for anovulation. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. A number of diathermy punctures are made to the ovary that result in cautery to the ovarian tissue at a number of points. The exact mechanism of action is unknown but it is assumed that some destruction of ovarian stroma occurs that results in a reduction of androgen production. Comparison of tamoxifen and clomiphene citrate for ovulation induction: a meta-analysis. Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Occasionally, very high levels of androgens can lead to voice change or virilisation. Less commonly, non-classical congenital adrenal hyperplasia and occasionally androgen-secreting tumours are responsible for hyperandrogenism.
Order hytrin 1 mg fast delivery
This 27-year-old woman complained of severe dysmenorrhoea heart attack jaw pain right side buy genuine hytrin, dyspareunia and cyclical right-upper quadrant pain. A A 19-year-old woman with histologically proven endometriosis, demonstrating clear vesicles and peritoneal window*. Pain is likely due to direct stimulation of sensory nerves plus formation of adhesions. Bimanual examination may reveal tenderness, fixation and nodularity in the pouch of Douglas. Tenderness when palpating the uterosacral ligaments and tightening (bow-like) may be noted. In the majority of patients, there will be no obvious clinical signs except tenderness to palpation. Laparoscopy still remains the gold standard for both the diagnosis and assessment of the extent of the disease. It may be preferable to perform a planning laparoscopy before embarking on definitive therapy, particularly in cases of pouch of Douglas obliteration. This system is best used in assessing the infertile patient and may underrepresent the severity of disease, particularly in the situation of intestinal endometriosis. Many other conditions may mimic, or be mimicked by, endometriosis as a result of its wide distribution within the female pelvis. Although the clinician might suspect the primary condition to be endometriosis, other differentials should be considered, including pelvic inflammatory disease, primary dysmenorrhoea, appendicitis and other gastrointestinal diseases. When pelvic masses are present, benign and malignant disease of the uterus and ovaries must be considered in the differential diagnosis. Bilateral endometriomas adherent to back of uterus with resultant pouch of Douglas obliteration. The rectum was drawn into the back of the uterus and a bowel probe was unable to be passed. Menorrhagia is not a common feature of pelvic endometriosis but can be associated with adenomyosis (endometrial glands infiltrating deep into the uterine muscle). If there is obvious severe disease but the patient is asymptomatic, then the decision to treat is questionable. If the patient is trying to conceive, surgical treatment is usually necessary as many of the medications used will also be contraceptive. Patients with severe endometriosis are best managed in multidisciplinary units accustomed to dealing with the disease. Denote appearance of superficial implant types as red [(R), red, red-pink, flamelike, vesicular blobs, clear vesicles], white [(W), opacifications, peritoneal defects, yellow-brown], or black [(B), black, hemosiderin deposits, blue]. Source: American Society for Reproductive Medicine, Revised Classification of Endometriosis. Conservative surgery may involve peritonectomy when multiple lesions are removed or ovarian cystectomy. Severe disease involving the pouch of Douglas, rectosigmoid or bladder may require collaboration with colorectal or urology specialists. The incidence of recurrence after surgery is variable: up to 50% of women diagnosed with endometriosis may require surgery again to improve symptom control. Five per cent of patients will report persistent symptoms of endometriosis after pelvic clearance. It is not always possible or prudent to remove all of the disease and a recurrence is inevitable in the most severe cases when treated conservatively. The resulting lower level of prostaglandin leads to less vigorous contractions of the uterus and, therefore, less discomfort. Suppresses ovulation, reduces growth of endometrial tissue, down-regulates cell proliferation, increases apoptosis of ectopic endometrium. Also indirect via decrease in endogenous oestrogen through inhibition of the hypothalamopituitary axis. Androgenic side effects can be extremely troublesome-hirsutism, acne, irreversible voice deepening. Bone mineral density is negatively affected so add-back therapy with oral norethisterone or hormone replacement therapy is recommended. Aromatase inhibitors block the local biosynthesis of oestrogen in the endometriotic lesions and lead to a decrease in symptoms. Down-regulate the hypothalamopituitary axis, leading to a hypo-oestrogenic state and improvement in symptoms of endometriosis. It is known that pregnancy has a slowing effect on this disease but the effect is not permanent. Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain: a systematic review. Surgical treatment of endometriosis-associated infertility: meta-analysis compared with survival analysis. Revised American Society for Reproductive Medicine classification of endometriosis. Recurrent pain after hysterectomy and bilateral salpingooophorectomy for endometriosis: evaluation of laparoscopic excision of residual endometriosis. Prevalence and anatomical distribution of endometriosis in women with selected gynaecological conditions: results from a multicentric Italian study. Peritoneal endometriosis, ovarian endometriosis and adenomyotic nodules of the rectovaginal septum are three different entities. Peritoneal endometriosis: new aspects in two dimensional and three dimensional evaluation. Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Endometriosis and infertility: a laparoscopic survey of endometriosis among fertile and infertile women. Outpatient laparoscopy for abdominal and pelvic pain in the United States 1994 through 1996. The two most common complaints are of a breast lump or lumpiness and breast pain (mastalgia). While the majority of breast lumps in women under 40 years of age are benign, breast cancer is the most common cancer diagnosed in women worldwide and 1 in 8 Australian women will be diagnosed with breast cancer by age 85. The 5-year relative survival from breast cancer is now 89%; the 10-year relative survival is 83%. The amount of fat surrounding the mammary gland determines the size of the breast. The breast position on the anterior thoracic wall is consistent between women and extends vertically from the second to the sixth rib and transversely from the lateral border of the sternum to the midaxillary line. Note that the axillary tail of the breast (axillary tail of Spence) extends towards the axilla and clinical assessment must include this portion of the breast. Fibrous, suspensory ligaments of Cooper anchor the breast to the overlying dermis as well as the underlying fascia and also help support the glandular architecture of the breast. A retromammary space or bursa exists between the pectoralis major fascia and the posterior capsule. The nipple is contiguous with the areola, a circle of pigmented skin that surrounds the nipple. The nipple contains multiple openings of the lactiferous ducts and is composed of circular smooth muscle fibres that compress during lactation or erect the nipple in response to stimulation. Other glands under the areola form small elevations (tubercles of Montgomery) that may enlarge with pregnancy. Each lactiferous duct dilates just prior to the nipple, forming the lactiferous sinus. Breast milk is produced by the alveoli, which form grape like clusters at the base of each lobule. Additional arterial blood supply also occurs from the lateral thoracic arteries, which branch from the axillary artery, and the posterior intercostal arteries, which come directly from the thoracic portion of the aorta and run in the intercostal spaces. Breast venous drainage occurs mainly to the axillary vein, with some additional drainage via the internal thoracic vein. More than 75% of lymph drains superiorly and laterally to the axillary lymph nodes, especially from the lateral breast. The axillary lymph nodes are divided into several different bundles (apical, lateral, central, pectoral or anterior and subscapular or posterior), which can be thought of as a pyramid in distribution. Some lymph will drain medially and superiorly to the parasternal and mediastinal nodes while less common drainage includes cross-mammary (to the contralateral breast) or into deep pathways including subpectoral and subdiaphragmatic. Fibrous septa enclose each lobe in a separate compartment and limit the spread of infection.
Hytrin 2 mg fast delivery
Internationally pulse pressure nursing generic 1mg hytrin visa, the dosage of mifepristone has varied between 200 and 800 mg; however, in Australia only one product is available, marketed by Marie Stopes. Misoprostol is a prostaglandin analogue, originally developed for peptic ulcer, and can be given sublingually, buccally or vaginally. Many models of delivering this service have been developed including day stay, outpatient and home-based care. Medical termination of pregnancy Oral mifepristone 200 mg is followed by misoprostol 24 to 48 hours later and then subsequent, repeat doses of Misoprostol 400 mcg as needed up to five doses. The average length to delivery is 12 hours, with considerable variation depending on the gestation. The surgery is referred to as dilation and evacuation (D & E) and requires greater cervical dilation-up to 18 mm at times. Therefore, cervical ripening becomes crucial, with 24-plus hours required to achieve this. Misoprostol can be used, while trials have revealed mifepristone also to be a successful adjuvant. Laminaria, a type of highly absorbent seaweed, can be inserted into the cervix under local anaesthetic the day prior to surgery, with the expanded rods removed just prior to evacuation. A 2-week follow-up is recommended to assess physical and emotional recovery and ensure contraceptive needs are met. Features suggestive of endometritis include fever, pain and temperature increase +/ offensive discharge. Features suggestive of retained products of conception include pain and bleeding, with possible ultrasound evidence of retained products of conception. This has a very low incidence and is primarily associated with ascending pelvic infection. The incidence has decreased with the advent of suction curettage and is treated by dividing the adhesions hysteroscopically. Recently, a hand-generated suction aspirator has been developed for areas where suction equipment or electricity is not available. Misoprostol (oral or vaginal) is used as a prelude to soften the uterine cervix, thereby decreasing perforation risk and blood loss. A delay of 1 to 3 hours is preferable prior to surgery where, after prep and drape, the cervix is grasped and gently dilated from 6 to 10 mm depending on gestation. There is no definite lower gestational limit for the procedure, but care needs to be taken not to miss the gestational sac with gestations of less than 7 weeks. At these gestations both surgical and medical terminations are associated with higher rates of bleeding and blood transfusion. Surgical methods are more associated with cervical tears or uterine trauma, while medical methods are associated 464 · Chapter 53 Contraception, Sterilisation and Abortion · such as regret or depression post-termination, and that women generally report improvement on qualityof-life scales. Post-abortion contraception and its effects on repeat abortion rates in Auckland, New Zealand. Depot-medroxyprogesterone acetate injection (depo-Provera): a highly effective contraceptive option with proven long-term safety. Effect of levonorgestrel releasing intrauterine device on hormonal profile and menstrual pattern after-long term use. Symptoms may include discharge, discomfort, itch, pain (including dyspareunia), burning sensation, odour or any combination of these. Signs may be florid or subtle and include vaginal discharge, inflamed cervix, vulval redness, swelling, or the presence of ulcers, skin fissures and lymphadenopathy. In order to ascertain the diagnosis and therefore manage the infection appropriately, history, examination and laboratory tests need to be performed. Vaginal discharge is one of the most common symptoms in obstetric and gynaecological practice. Upper genital tract infection Infections of the upper genital tract involve the endocervix, uterus and fallopian tubes. Clinical features may include discharge, pelvic pain and sometimes abnormal uterine bleeding. Tubal damage may result, with the possibility of chronic pelvic pain and/or infertility. With puberty, the oestrogen levels rise and physiological vaginal discharge is cyclically produced. Cervical mucus secretion is scant in the follicular phase of the menstrual cycle; clear, profuse and like egg white at ovulation; and then returns to minimal in the luteal phase. The Billings method of contraception relies on the recognition and charting of these changes. This squamous epithelium on the ectocervix may be the source of increased physiological discharge. An ectropion is more commonly seen when the oestrogen levels are increased, such as during pregnancy or on the combined oral contraceptive pill. Around the time of the menopause, oestrogen levels reduce as do lactobacilli, resulting in an increasing pH. This alkaline environment favours mixed bacteria including bowel commensals but candidiasis becomes less likely. Candida in the absence of other stimulants such as oestrogen or steroids should raise the possibility of diabetes in this age group. Oestrogen deficiency also results in thinning of the epithelial layer and atrophic vaginitis ensures. It is a common finding in the reproductive age group and may be physiological as previously discussed or pathological. These infections usually involve the cervix or vagina and will be discussed in detail. It can be profuse, watery (in the rare case of fallopian tube tumour) or scant and blood stained. Endometriosis of the cervix or vaginal vault may produce a cyclical brown or bloody discharge. A retained tampon is an important cause of foreign body infection and will not be identified unless the woman is properly examined with a speculum. A further complication may be toxic shock syndrome, due to the release of Staphylococcus aureus toxins, and may present with fever, rash, vomiting, diarrhoea and collapse. Early pregnancy-related complications may present with bleeding or discharge, as can retained products of conception. Desquamative vaginitis is a poorly understood condition characterised by a purulent vaginal discharge and large numbers of parabasal cells (exfoliated immature epithelial cells) are seen on vaginal Gram stain. Erosive autoimmune dermatosis such as lichen planus may present with a vaginal discharge as well as pain or scarring. This may be amplified if they are concerned regarding judgment or lack of understanding of their sexual behaviour. Sexual history taking should be appropriately performed by healthcare providers in any branch of medicine, but is particularly pertinent in the field of obstetrics and gynaecology. Age should be noted as Chlamydia trachomatis is more common in those younger than 30 years of age. Direct questioning regarding genital symptoms include vaginal discharge, its amount, character (colour, consistency and odour), whether it is intermittent or continuous, association with the menstrual cycle or sexual activity. Enquire regarding dyspareunia, abdominal pain and difficulties with micturition or defecation. In particular, ask about recent treatments including self-medicated over-the-counter preparations, as they may modify symptoms, signs and laboratory findings. Include a history of blood transfusion, intravenous drug use and blood-borne viruses. With particular reference to a sexual history, ask the easy questions first such as: `When did you last have sex? Therefore, obtaining a history alone is insufficient for accurate diagnosis, and hence examination and laboratory testing are necessary. Ensure that this is performed in a safe, private environment and in a respectful manner.
Order discount hytrin on line
Congenital herpes simplex virus infection: two unique cutaneous presentations associated with probable intrauterine transmission arrhythmia loading order 1 mg hytrin visa. While it may appear benign initially, progression to central nervous system disease and/or disseminated (multi-organ) disease can occur. Pustules may be present from birth in the condition of congenital candidal infection, or appear later particularly with Staphylococcus aureus skin infection. The differential diagnosis needs to include the much more common condition, erythema toxicum, which is described earlier. Congenital dermal melanocytosis (Mongolian spot) is the most frequently encountered newborn pigmented lesion. It presents as a large pigmented macule with indefinite borders, often distributed over the lower back. It appears as a red area on the upper eyelids, root of nose, upper lip and/or nape of neck. These lesions are benign, often fade with time but nonetheless may case maternal anxiety. A capillary malformation (port-wine stain or naevus flammeus) is a deep vascular naevus, usually found on the face, often in the distribution of a division of the trigeminal nerve. Although commonly benign, there is a rare but important risk of associated neuroepileptic syndromes. It becomes larger for several months and then regresses spontaneously, usually by 3 years of age. Treatment is necessary if the haemangioma distorts tissue such as the eyelid or airway. Occasionally, very large haemangioma leave redundant skin or scar tissue after regressing. Large haemangiomas (often separately classified) may be associated with platelet destruction and thrombocytopenia (Kasabach Merritt phenomenon). Fat necrosis is an indurated area of skin where pressure has been applied over a protracted period. While not always warranted for the common and benign skin issues, a paediatric or dermatological opinion may assist families to decide on a desired course of action. Following this general examination, the systematic examination moves to the hands, followed by the arms, head, face, neck, thorax, abdomen, hips, legs and feet. This has the advantage that, unlike a systems-oriented approach to examination, there will be little need to backtrack during the examination. It can be accomplished in a relatively short time without undue disturbance to the newborn and it is unlikely that abnormalities will be missed. A caveat to this approach includes auscultation of the heart early in the examination. In this instance, a more settled and quiet neonate will better facilitate cardiac auscultation. Treatment with oral propranolol (utilising the anti-angiogenesis effect of Я-agonists) is increasingly being administered. Often supernumerary digits are found joined to the ulnar side of the hand by a thin pedicle of tissue without bone (post-axial polydactyly). Ligature in the immediate newborn period is associated with complications and no longer recommended. Pre-axial (radial) polydactyl may be associated with syndrome diagnoses and warrants further assessment. The cardiovascular examination, which is undertaken when the thorax is examined, may be initiated by palpation of the brachial artery during examination of the arm. GraspandMororeflexes this is an opportune time to elicit the grasp and Moro reflexes and check head control when pulled from supine. Pulling the newborn from the wrists allows an assessment of head control to be made. In this starting position, the lower back, buttocks and legs remain on the cot surface. This may suggest abnormalities of connective tissue, or be part of a syndromic diagnosis. Acquiredpathology Failure of normal spontaneous movement or failure to move symmetrically may suggest a fracture of the humerus or clavicle after a difficult delivery or the presence of a deep tissue or bone infection. The proportionally shorter legs and arms seen in this infant are consistent with achondroplasia. Abnormalities of the Moro reflex occur symmetrically if there is central nervous system depression or neuromuscular disease, or unilaterally in conditions such as fracture of the clavicle or a brachial plexus injury. Remember, a watchful mother is often nearby and reassurance and explanation is required prior to conducting the Moro assessment. Elicitation of these reflexes, along with a general appraisal of tone, strength, level of activity and alertness, form an appropriate neurological screening examination. The finding of macrocephaly, usually defined as a head circumference > 97th percentile for gestational age, requires that hydrocephalus be ruled out as a possible cause by cranial ultrasound imaging. Shapeandmoulding A newborn cranial vault is made up of distinct separate bones or plates. There may be overlapping of the individual cranial vault bones due to moulding, facilitating movement through the birth canal. The triangle-shaped posterior fontanelle can often be hard to palpate in the immediate postnatal period (due to movement and moulding of the separate cranial vault bones). However, appropriate paediatric follow-up over time may prevent unnecessary cranial radiation. Extra-cranialswellingsorhaematomas Classification of extra-cranial fluid collections or haematomas is important based on the various causes and blood-fluid collections that can occur along certain anatomical planes. Caputs are characterised by tissue oedema and are often associated with cranial vault moulding. They can be due to prolonged engagement in the birth canal or vacuum-assisted delivery. Cephalohaematomas rarely expand after birth; they may completely resolve, or calcify leaving a minor convexity to the cranial vault. A subgaleal haemorrhage occurs due to shearing of blood vessels outside of the periosteum, below the epicranial aponeurosis (galea aponeurotica). They can occur spontaneously, but vacuum-assisted delivery increases the risk significantly. If a cranial swelling is evident, close observation is required, especially after an instrumental delivery. If a subgaleal haemorrhage is suspected, regular cardiovascular monitoring and prompt senior neonatal advice is required. Spina bifida is a much more common type of neural tube defect 608 Chapter 66 Assessment of the Neonate involving failure of fusion of the neural tube, usually the lower spine. Increasing awareness of the role that folate supplementation plays in preventing neural tube defects, including mandatory folate fortification of flour and bread (common in many jurisdictions around the world; commenced in Australia in 2009), has decreased the overall prevalence of neural tube defects. Several syndromes are associated with underdevelopment of the auricle or a low positioning (low-set ears) of the auricle on the head. Low-set is defined as when the top of the ear helix falls below a horizontal line that is imaged through the middle of the eyes and outer canthus. Pre-auricular pits or skin tags may be benign, familial or associated with deficits of auditory acuity. Unilateral tearing suggests a blocked tear duct, which almost always resolves spontaneously. Pupillary reflexes to light should be present and elicited (both directly and consensually) in the term newborn. Bilateral cleft lip and palate may be associated with a more generalised midline defect with abnormalities of the brain and pituitary gland. The roof of the mouth should be inspected to detect a cleft but must also be palpated to exclude a sub-mucosal defect of the palate. Excessive secretions should alert the examiner to the possibility of a problem with deglutition (inability to swallow): oesophageal atresia, central neurological depression or neuromuscular disease. A ranula presents as a mass beneath the tongue and is due to partial blockage of the submandibular duct. Other oral lesions are rare; however, if present they may warrant further expert opinion because they may be derived from the thyroid gland, be tumours or interfere with the patency of the airway. If there is nothing abnormal between the light of the ophthalmoscope and the retina then a bright orange-red view is obtained through the pupil. Provided the remainder of the examination is normal, this common finding is often attributable to a prolonged birth or difficult extraction.
Generic hytrin 1 mg free shipping
There is less experience with proton pump inhibitors in early pregnancy but they are commonly prescribed in late pregnancy for refractory cases not responding to other medication blood pressure below normal buy hytrin with a mastercard. It may be aggravated by dehydration with excessive vomiting in early pregnancy, iron supplementation and any relative immobility. Endometriosis, haemoperitoneum from any cause (uterine rupture, splenic artery aneurysm rupture, hepatic rupture). The pain is usually lateral to the uterus, in the groin and overlying the round ligament, which can be palpated as a tender cord. The pain is usually unilateral and is more often left-sided, perhaps associated with dextrorotation of the uterus bringing the left ligament into apposition with the peritoneum of the left anterior abdominal wall. The pain is often initiated or accentuated by sudden movement (standing up, bending, coughing, sneezing). Excessive straining may aggravate haemorrhoids and is intuitively unwise if there is any reason to suspect cervical insufficiency. Increase of dietary fibre (bran, green vegetables, dried fruit) should be the focus of therapy. The woman troubled with constipation should become familiar with the fibre content of specific foods and also what is effective for her. Suitable agents would include bulkproducing compounds (Fybogel, Metamucil, Normacol), magnesium hydroxide (milk of magnesia) and lactulose. Stimulant laxatives such as senna (Senokot) are also safe in pregnancy and may be appropriate. Treatment Treatment is to rest in a position of comfort and take analgesia with paracetamol. Usually the condition abates completely within 2 to 3 weeks, although hypertrophy and stretching of the ligaments continue. Known presence of a fibromyoma is extremely helpful in making the diagnosis, as is point tenderness over an area of the uterus in the context of an obviously healthy fetus. It is best to think of the differential diagnosis in terms of the likely organ involved and then secondarily what might cause pain at that location. Round ligament pain, miscarriage or labour, red degeneration of a fibromyoma, placental abruption, chorioamnionitis. Treatment After exclusion of more sinister causes, treatment is conservative with simple analgesia. They are most 204 Chapter 26 Common Problems in Pregnancy commonly completely asymptomatic but the woman may recognise a palpable tightness of the uterus that may be associated with mild discomfort. Sometimes Braxton Hicks contractions are more significant and the woman needs to briefly stop what she was doing. Management Braxton Hicks contractions require only an explanation and a reminder of the signs of labour. Threatened preterm labour and spurious labour are, by definition, retrospective diagnoses and will not generally be distinguishable from genuine labour until they are observed over time and labour is found not to eventuate. Recurrent spurious labour at term is a risk factor for adverse perinatal outcome and should be managed with increased fetal surveillance and consideration given to induction of labour. For example, bronchitis is probably more common, which may have implications for women who suffer from bronchial asthma (see Ch 17). Although there is a strong hereditary tendency, each pregnancy makes the condition worse. The fullness related to vulval varicosities may create alarm in the patient but a strong postural dependence (only apparent on standing) makes diagnosis relatively easy and the woman can be reassured that complete resolution is extremely likely in the puerperium. Thrombophlebitis (thrombosis) occurs in 5% of women with varicose veins, usually in the puerperium. Haemorrhage will occur if the vein is damaged and bleeding can be profuse but, being of low pressure, is readily controlled by direct pressure. If a varix in the leg is bleeding, the woman must lie down, elevate the leg and have pressure applied to the bleeding site. Significant bleeding may eventuate during delivery if an episiotomy incision or tear involves vulval or vaginal varicose veins. The main aggravating factors are constipation (see above) and prolonged pushing down during the second stage of labour. The former is usually associated with the passage of a hard motion, and is rarely severe. If prolapse is immediately recurrent, repeated replacement is obviously unhelpful. The veins will improve after pregnancy but this can take several months and not usually right back to the pre-pregnancy state. The following strategies may minimise worsening of lower limb varicose veins in pregnancy. An understanding of the incompetence of the perforating veins will make it obvious that exercise will aggravate the condition. Swimming will not have the same effect as the lower limb venous pressure will be less and therefore becomes the preferred mode of exercise for these women. Support stockings may be helpful but a tight roll occluding veins at the top of the stocking should be avoided. Intrapartum Care should be taken at the time of delivery to minimise laceration to varicosities. In extreme cases, a midline episiotomy may be considered, recognising the attendant risk of sphincter damage. Any haemorrhage from damaged vulval varices should be controlled by simple pressure until medical assistance is obtained. A low-molecular-weight heparin may speed resolution, as may anti-inflammatory drugs. Oedematous painful haemorrhoids in association with a sutured episiotomy that has probably been sutured too tight, leading to oedema of the suture line. Chapter 26 Common Problems in Pregnancy examination is performed when the woman reports bleeding and if bleeding persists after pregnancy, further investigation with sigmoidoscopy is indicated to exclude other bowel pathology. The condition is managed largely by increasing the rest periods, with the legs well elevated; diuretics are contraindicated. A similar phenomenon can occur with the lateral cutaneous nerve of the thigh and is known as meralgia paraesthetica. It is due to the increased venous pressure consequent on both the arteriovenous shunt through the placenta and extrinsic compression of the great veins by the uterus. Only very rarely is surgery needed during pregnancy to relieve the pressure by incising the fibrous roof of the tunnel. Analgesics can be used as needed-most commonly paracetamol but with codeine or even morphine if necessary. Investigation is required if the attacks are frequent, severe or persistent or are associated with localising neurological symptoms or signs. In late pregnancy, syncope can be induced by pressure on the inferior vena cava by the gravid uterus, the supine hypotensive syndrome. Therefore, it is not surprising that a majority of pregnant women complain of a backache or sense of strain in the lower back, most commonly to one side or the other. Although a relationship between fainting and fetal sequelae is not established, anaphylaxis and other examples demonstrate that the fetus is exquisitely sensitive to sustained maternal hypotension. Often this is maximal around mid-pregnancy, implying a hormonal basis as much as a mechanical one. Supine hypotension is avoided by advising women and their carers of the inadvisability of lying supine (on the back) for any length of time during the third trimester. While this could be true, it would appear more likely that sleep apnoea poses the greater risk and the woman that develops supine hypotension during sleep is most likely to experience discomfort and instinctively move to a more suitable position. Rest is the most important form of treatment, particularly avoiding activities that aggravate the condition. Very often the pain is worse at night, following increased activity during the day. Every patient with the condition must be made aware of the mechanism and the obvious imperative of avoiding weightbearing exercise.
Cheap hytrin 2 mg line
Treatment is conservative with abstinence of sexual activity until completely resolved blood pressure medication gynecomastia purchase hytrin overnight. Anticoagulation and antiplatelet medications have not been shown to be of benefit. Microscopically, it is composed both of epithelial structures similar to renal tubules and stroma comprising nonspecific spindle cells. The differential diagnosis for these tumors includes cystic nephroma and cystic partially differentiated nephroblastoma. This technique utilizes an elliptical incision that preserves the umbilicus and thickens and strengthens the anterior abdominal wall. Full-thickness resection of skin from the central abdomen is performed, and the anterior wall is sutured in a double-breasted fashion preserving vascularity and the umbilicus. A novel technique for reconstruction of the abdominal wall in the prune belly syndrome. Infection occurs after breakage of the skin and characteristically begins as a small papule. When mature, it is a discrete 25 mm smooth, dome-shaped, pearly or flesh-colored nodule that is often umbilicated. A review of 199 patients undergoing Monti ileovesicostomy at a single institution reported a revision rate of 8. Patients present with a distinct facial phenotype, mental retardation, epilepsy, agenesis of corpus callosum, and congenital heart defects. Roughly 50% of patients have genitourinary anomalies with hypospadias being the most prominent (52%). Bifid scrotum, vesicoureteral reflux and micropenis are rare but have been reported. Based on their less well-developed spikes than seen on jackstones; the spikes possess more of a mamillated appearance. If complete androgen insensitivity occurs, the child will appear to have a normal female phenotype and the testes are located internally. Many children are diagnosed at the time of hernia repair as infants or not diagnosed until puberty during an evaluation for primary amenorrhea. This repeat surgery can be difficult due to formation of scar tissue in the corpora. Another option is to remove the prosthesis, perform a copious antibiotic washout of the corpora cavernosa with an antibiotic solution, then place a ``tutor' cylinder inside the corpora to prevent shortening and scarring. Another approach to the management of an infected penile prosthesis is the Mulcahy protocol. This involves complete removal of the infected part of the prosthesis and all other components followed by the use of the specific Mulcahy salvage procedure outlined below with reinsertion of a new penile prosthesis in the same sitting with a reported success rate of 85%. Patients receiving hemodialysis and deferoxamine are at particular risk for disseminated disease. The procedure was initially described to treat rectal prolapse by securing the rectum to the fixed vagina, and the same logic has been used to correct vaginal prolapse by fixing it to the rectum. This is a normal finding in patients who have undergone bladder replacement surgery using bowel segments. Mucosuria can be a symptom of mucinous adenocarcinoma of the urinary tract, most commonly of the urachus however mucin producing tumors of the prostate and renal pelvis have been reported. Other sources of mucin production in the bladder include invasive colorectal cancer and colovesical fistulas. Mucin-producing tumors and tumor-like lesions involving the prostate: A comprehensive review. Patients present with cryptorchidism and hernia, and the persistent mullerian structures are found within the hernia sac. Ё Increasing evidence is mounting that persistent mullerian structures are at risk for malignant Ё transformation. Hyperparathyroidism is the most common presentation of this syndrome, but overall this is a rare cause of hyperparathyroidism in the general population. The management of mumps orchitis is supportive (bedrest, scrotal support, analgesics) with resolution in about 7 days. The incidence of cervicothoracic vertebral defects, especially from C5T1, is 80%. Other abnormalities may include Sprengel deformity, upper limb defects, and moderately frequent rib anomalies. Persistent Mullerian duct syndrome: lessons learned from Ё managing a series of eight patients over a 10-year period and review of literature regarding malignant risk from the Mullerian remnants. The contents of the cysts consist of either clear to yellow fluid or thick myxomatous gel. Cystic nephroma presents in a bimodal age distribution of 3 mo2 yr (2:1 male-tofemale) and in adulthood (8:1 female-to-male). Children usually present with a palpable mass and adults with pain, hematuria, or infection. The nephromas contain noncommunicating cysts with thin septa separating the cysts. The most simple muscle flaps are local and regional flaps where blood supply of the muscle is not interrupted when the flap is repositioned to its new location. Pedicle and micro vascular free flaps are more complicated forms of tissue transfer that are finding new indications in reconstructive urologic procedures. Tissue transfer has become increasingly used in centers for complex repair of fistula disease following radiation. In addition, clinical study has shown latissimus dorsi transferred to acontractile detrusor tissue with microsurgical coaptation of the thoracodorsal nerve to low intercostal nerves innervating the rectus abdominus has restored voluntary voiding in patients with detrusor areflexia. The classic triad involves marrow plasmacytosis, lytic bone lesions, and a serum and/or urine M component. Hypercalcemia is the most common cause, but hyperuricemia is also present and a likely cause. There may be tubular precipitation of light-chain proteins (myeloma kidney), urinary obstruction due to uric acid or calcium-containing stones, or recurrent pyelonephritis. Renal failure is rare but has been reported after the use of contrast agents in patients with multiple myeloma. The rectus abdominis myocutaneous flap: Modifications, complications, and sexual function. However, it may be a cause of chronic prostatitis in men or urgency and frequency in women. Renal failure is initially manifested by oliguria and followed later by a polyuric state. Mycoplasma genitalium is associated with symptomatic and asymptomatic nongonococcal urethritis in men. Myoglobin is released into the serum following massive muscle necrosis (rhabdomyolysis) from crush, compartment syndrome, electrical injury, toxins, malignant hyperthermia, and other causes, and imparts a cola-like color to the urine. Diagnosis is made by electrophoresis separation and radioimmunoassay of urinary myoglobin. Serum creatinine kinase is elevated, and there is an absence of red cells in the urine. Painful myofascial trigger points and pain sites in men with chronic prostatitis/chronic pelvic pain syndrome. Genital mycoplasmas: Mycoplasma genitalium, Mycoplasma hominis, and Ureaplasma species. Pelvic floor trigger points refer pain to the vagina, vulva, perineum, rectum, and bladder. Irritative symptoms (eg, urinary urgency, vulvovaginal burning, rectal fullness) may be more prominent than pain. Pelvic floor physical therapy (manual myofascial release, stretching, and strengthening) is useful for many patients. More severe cases may require trigger point injections (bupivacaine), gabapentin, or botulinum toxin if muscle spasm can be identified. Common applications are for skin coverage during ilioinguinal node dissections for penile cancer, closure of urinary fistulae, and reconstruction after Fournier gangrene: r Rectus abdominis flap: the blood supply of the rectus abdominis is the superior and deep inferior epigastric vessels. The deep superior epigastric vessels are not utilized as a vascular pedicle for the free flap because of their smaller caliber and a greater amount of skin can be transferred by relying on the interior epigastric pedicle. It can be utilized either as a muscle flap or myocutaneous flap and leaves the patient without any functional deficit. The nerve supply to the gracilis muscle is a branch of the obturator nerve, and its blood supply is a single artery from the profunda femoral system.
Diseases
- Viljoen Smart syndrome
- Carcinophobia
- Lee Root Fenske syndrome
- Chromosome 5, trisomy 5q
- Familial ventricular tachycardia
- Pachydermoperiostosis
- Choroido cerebral calcification syndrome infantile
Purchase hytrin 2 mg fast delivery
Surgery to evert the nipple may interfere with breastfeeding or result in nipple hypersensitivity hypertension va disability rating buy discount hytrin 1 mg on-line. Breast involution occurs slowly from the age of 30, unless a woman becomes pregnant. The breast stroma is replaced by fat, which allows dropping and a softer contour but is also less radio-dense. Changes in the glandular breast tissue increase the formation of small cysts (microcysts), fibrosis and glandular tissue (adenosis). A systematic approach needs to be used to ensure all areas of the breast are examined, including the axillary tail that extends into the armpit. Any discrete lesion should be assessed for size, mobility in relation to skin and deeper tissues, tenderness, overlying skin change, contour and consistency. If the primary complaint is of pain, the underlying chest wall must be examined as many complaints of breast pain actually emanate from the underlying chest wall. Locations within the breast are usually described in terms of the four quadrants (upper outer, upper inner, lower outer, lower inner) and the axillary tail. She should raise her arms to the ceiling, then place her hands on her hips, while the practitioner looks for skin dimpling that may only be seen with elevated arms or pectoralis major contraction. The two views obtained of each breast are the oblique view and the craniocaudal view. Mammography aids delineation of any masses, as well as showing microcalcification and parenchymal distortion. The dense fibrofatty breast tissue in women under 35 years of age Chapter 59 Breast Disorders age. The majority of breast lumps require histopathological confirmation of their benign or malignant nature and most women will want reassurance that their symptoms are not due to breast cancer. Cytology has a non-diagnostic sample rate of around 13%, a false-positive rate of up to 0. Biopsy In a core biopsy, local anaesthetic is injected and a 14-gauge needle or specific core biopsy mechanical gun (vacuum-assisted biopsy 8 or 11 gauge) is used to remove a more significant piece of breast tissue. Usually three or more core biopsies are taken to ensure adequate tissue sampling and its sensitivity increases to > 95% when used with image guidance. The cancer detection rate of clinical examination and mammography improves with increasing patient age. High-frequency sound waves tend to show benign lesions with distinct borders, whereas carcinomas tend to have indistinct outlines. While not definitive, colour flow Doppler ultrasound can aid diagnosis, with malignant lesions tending to have greater blood flow. This can be unequivocally diagnosed as benign and will explain a clinical or radiologic well-defined mass in the breast. They account for 10 to 15% of all symptomatic breast lumps but 60% of breast lumps in women 20 years of age. Fibroadenomas are categorised into common, giant (> 5 cm) or juvenile (occurring in adolescents). Fibroadenomas tend to calcify and 20% of women will have more than one fibroadenoma of the breast. Over a 2-year period, 25% will increase, 50% will involute or disappear completely and 25% will remain unchanged. Cytology is appropriate in small fibroadenomas in young woman but anything larger requires several core biopsies. Any rapidly growing fibroma or a fibroma > 4 cm should be excised to ensure it is not a phyllodes tumour, which has a malignant potential and is difficult to differentiate clinically from a fibroadenoma. Pathologically, this group of lesions can be divided into sclerosing adenosis, radial scars and complex sclerosing lesions. This is the only benign breast condition associated with an increased risk of breast cancer if the cells show atypia (relative risk up to fivefold). Up to 3% of woman with breast cysts will be found to have a breast cancer; however, the majority are incidental findings from breast imaging, unrelated to the underlying cyst. All women with nipple discharge should have a careful clinical examination and mammography if > 35 years of age. If the discharge is from a single duct, it should be checked for haemoglobin as up to 10% of these patients with moderate to large amounts of blood in their nipple discharge will have an underlying malignancy. If a woman desires preservation of breastfeeding ability then localised (versus total) duct excision should be considered. Low-fat diets, progesterone, evening primrose oil and -linoleic acid have contradicting or poor-quality evidence to support their use in managing mastalgia. Bromocriptine, a dopamine agonist, is no longer recommended due to its significant side effect profile (including headaches and vertigo). Luteal phase danazol is superior to placebo but obviously has androgenic side effects. Luteal phase tamoxifen is also effective but at the cost of menopausal side effects. In lactating women, ongoing expressing or breastfeeding from the affected breast should be strongly encouraged, with adequate lactational support. If the infection persists despite adequate treatment with flucloxacillin, culture from aspiration or drainage is likely to be helpful. Periareolar infection occurs in women in their third decade and is strongly associated with smoking. Central breast pain, nipple discharge, a mass and nipple retraction to the side of the infection are common features. Treatment is with antibiotics and aspiration/ incision and drainage; however, up to one-third of women will experience a fistula (as the underlying diseased duct has not been removed). Peripheral non-lactating breast abscesses are rare and the patient may be immunosuppressed. Rarely, non-lactating breast infections can be associated with ductal carcinoma in situ, hence mammography is recommended after symptom resolution in women > 35 years of age. Other breast infections include skin-associated infections (such as cellulitis post-mastectomy or radiation treatment), infected sebaceous cysts, hidradenitis suppurativa, tuberculosis, and self-inflicted trauma and consequent infection. It is also common that pain experienced in the breast is actually referred pain from the chest wall and it is important to differentiate the two as they are managed differently. Note that breast pain with normal clinical examination and imaging is actually a very rare symptom of breast cancer. True mastalgia (pain in the breast tissue itself) is thought to be due to hormonal modulation and there are different theories as to the cause (oestrogen or prolactin excess, progesterone deficiency or increased breast hormone receptor sensitivity). Older terminology divides cancers into ductal and lobular; however, better understanding shows that all breast cancers arise from the duct lobular unit and so this terminology, while still in use, has been largely superseded. Treatment options involve wide local excision +/- radiotherapy if < 4 cm affected area or mastectomy if > 4 cm. Survival rates are equivalent; however, conservative surgery has a higher recurrence rate. Special types of breast cancer are: tubular mucinous cribriform papillary medullary classic lobular. Occasionally lymphomas or sarcomas occur in the breast as well as phyllodes tumours (rare fibroepithelial tumours that range from benign to malignant). It can be converted into a clinical stage of 0 to 4 based largely on tumour size and axillary lymph node status. All patients should have a full blood examination and liver function test in addition to imaging. If these bloods are abnormal or if there is more advanced primary disease at presentation, the patient should have liver and bone imaging for any metastases that would alter primary management. If there is no mass lesion, wide local excision and postoperative radiotherapy is recommended. Risk doubles every decade until menopause, when it slows; however, 40% of all breast cancers are still found in women > 70 years of age. Undergoing menopause > 55 years of age doubles the risk of breast cancer compared to a woman who underwent menopause at 45 years of age. Breast cancer risk is also doubled in women who have their first child after 30 years of age versus 20 years of age.
Buy 5mg hytrin
Importantly heart attack white sea remix discount hytrin amex, it should be established whether the relative with the cancer is still living to assess the possibility of genetic cancer screening. Other issues are diabetes, particularly if the patient has polycystic ovarian syndrome, endometriosis, clots and cardiovascular disease. It should be ascertained whether the patient lives alone or with someone 354 Chapter 44 Gynaecological History and Examination it tends to occur. If the patient is postmenopausal, has there been any bleeding more than a year after her last period, which qualifies it as postmenopausal bleeding? Pelvic pain Dysmenorrhoea should be elicited, and the relationship between it and the period. If the patient does have dysmenorrhoea, has it been present since menarche or is this a new occurrence? Does she need to take any medications for the pain and does she need to alter her activities because of the pain, especially taking time off work or school? In addition to dysmenorrhoea, the patient should be asked if she has any dyschezia (pain with bowel movements, especially during the period) or dysuria. Pain with intercourse (dyspareunia) should be discussed, and if present, it should be established whether the patient has pain all the time or only in certain positions, and whether the pain is on deep or superficial penetration. From this history and examination, a problem list can be generated to ensure that each issue is addressed separately. Bowel and bladder function An assessment should be made regarding bowel and bladder function, especially enquiring as to the presence of constipation, diarrhoea, blood or mucous and/or symptoms of bladder problems including dysuria, frequency, nocturia, urgency, haematuria and incontinence. If there is incontinence, it should be elicited whether it is stress or urge incontinence, or insensible incontinence. Not every gynaecological patient will be examined vaginally and in general, no patient who has not been sexually active should be examined vaginally. Then a breast examination will be undertaken with consent, followed by examination for the thyroid; if there is any suggestion of a prolactinoma, then a neurological exam for visual fields should be undertaken. A general inspection of the abdomen should be undertaken, assessing for scars and hair distribution, and palpating for masses and tenderness. The patient is asked to lie on her back with her knees bent and her feet together. The external genitalia are inspected, particularly for hair growth pattern, evidence of oestrogen deficiency, any masses or change in skin colour or ulceration. A bimanual exam should then be performed with one hand on the lower abdomen and the other hand palpating the organs through the vagina. The presence of any nodules should be assessed in the pouch of Douglas to indicate the presence of severe endometriosis. Most people will produce physiological discharge which will change throughout the cycle. Typically, it will be thin discharge in the first part of the cycle, become stringy and long around mid-cycle and then become short and clumpy post-ovulation. Discharge that is green, offensive smelling or white and flocculent can indicate pathology. Information about itchiness of the vulva should be elicited, including whether or not it is accompanied by vulval and/or vaginal pain. Contraception and fertility Contraception is an important part of the gynaecological discussion. It is important to note when the last Pap smear was and whether there have been any abnormalities with past smears. Other system review If any issues are elicited in the general questioning, then some accessory questions may need to be asked. If a patient has amenorrhoea/oligomenorrhoea, assessment should be made as to the cause. If required at the gynaecological examination, a pipelle sample can be taken and this will be discussed further in Ch 45. Screening and education opportunities can be divided into two distinct age group categories: premenopausal and postmenopausal Table 44. The patient is much more likely to disclose all the important information and leave feeling well treated. Non-invasive gynaecological investigations are divided into blood tests, microbiological, cytological, histological and imaging modalities. Invasive gynaecological investigations comprise hysteroscopy and laparoscopy with attendant biopsy. The investigations requested are not exhaustive and will of course need to be tailored to the relevant history and examination findings. It is important to note that up to 80% of chlamydial infection in women is asymptomatic2 and can lead to ectopic pregnancy, infertility and chronic pelvic pain3. This rate has more than tripled over the past decade, increasing from 130 notifications per 100 000 in 2001. There is no screening test currently available for ovarian cancer which meets these criteria. Infectious vaginitis is one of the most common presentations in women seeking gynaecological care and includes three types of vaginal infections-bacterial vaginosis, candidiasis and trichomonas-with prevalence rates of 22 to 50%, 17 to 39%, and 4 to 35% respectively. Positive cultures for yeasts and Gardnerella vaginalis, without the accompanying microscopic features as above, usually indicate the presence of these organisms as normal flora. Additionally, an endocervical brush should be used in peri- and postmenopausal women where the transformation zone of the cervix is in the endocervical canal. Gram-stained smear of urethral exudate showing intracellular gram-negative diplococci that are characteristic of gonorrhoea. If lubricant must be used, it should be applied sparingly on the outer portion of the speculum so as not to contaminate the sample. It is a minimally invasive way of assessing the uterus, tubes, ovaries, cul-desac and kidneys, and can be performed abdominally or vaginally. A complete pelvic ultrasound evaluation may entail both a transabdominal and transvaginal examination. Three-dimensional ultrasonography is finding some use in the evaluation of gynaecologic disease. Endovaginal transducers use high-frequency probes and allow the transducer to be placed closer to the structures being studied. This means that the images produced have a better resolution, but the transducer does not provide a full view of the pelvis. It is also more invasive, and thus not suitable for all patients, especially those who have not been sexually active. The transabdominal approach uses a lower-frequency probe and is more suitable for the abdominal organs, such as the kidneys, and the pregnant uterus. This approach results in a broader view of the pelvis, albeit with images that suffer from attenuation and lower spatial resolution. A full bladder provides an acoustic window and optimal view (because sound travels better through water), displaces loops of bowel and aligns the uterus with its long axis parallel to the abdominal wall. The slide should be fixed immediately by spraying from a distance of 20 cm to avoid air drying of the specimen, which may compromise the sample. The accuracy of the assessment will depend on both the experience and training of the operator, and the resolution of the machine. The ultrasound is part of the first-line investigation of abnormal vaginal bleeding (including heavy menstrual bleeding and intermenstrual bleeding), pelvic pain or pelvic mass. It is also the investigation of choice to investigate early-pregnancy bleeding or pregnancy of unknown origin. A comprehensive pelvic ultrasound report should comment on the orientation of the uterus, the thickness of the endometrial lining, the myometrium, the presence of adenomyosis or fibroids and the position of these, the mobility and size of the ovaries, and the presence of ovarian cysts and whether they are simple cysts or contain septae or solid components. A pelvic ultrasound is best performed in the first half of the menstrual cycle in order to minimise the endometrial thickness, so structures abutting the lining of the uterus are more clearly seen. If the endometrial lining is poorly delineated, then a saline infusion sonohysterogram could be requested. The ultrasound specialist introduces a small amount of saline into the endometrial cavity through the cervix, which is particularly useful in assessing for the presence or absence of polyps. Rinse the spatula as quickly as possible into the PreservCyt Solution vial by swirling the spatula vigorously in the vial 10 times. Obtain an adequate sampling from the endocervix using an endocervical brush device. Rinse the brush as quickly as possible into the PreservCyt Solution by rotating the device in the solution 10 times while pushing against the PreservCyt vial wall.
Generic hytrin 2mg free shipping
During the course of asphyxia there is an apnoeic period during which heart attack effects generic 2 mg hytrin with visa, with appropriate general measures such as tactile stimulation, the newborn will spontaneously commence respiration. If the asphyxia has been more prolonged or severe, such measures will never be effective in causing spontaneous respirations to commence: the so-called secondary apnoea. In this case, only after assisted respiration (resuscitation) has been provided and hypoxia and acidosis reversed will spontaneous respirations commence. Importantly, there is no way of knowing in advance (or during resuscitation) whether the newborn is in a period of primary or secondary apnoea. These definitions, while assisting in animal and scientific explanations of asphyxia, do not assist in the real-world delivery room. No Prevent heat loss Ensure open airway Stimulate Yes Stay with mother Routine care: Prevent heat loss Ongoing evaluation No No Laboured breathing or persistent cyanosis? Most babies who do not require active resuscitation will achieve a clear airway unaided. Routine suction is not recommended although excessive oral secre tions may be suctioned under visualisation. Pro longed or vigorous suction may cause bradycardia, by stimulating pharyngeal vagal receptors. If the baby has not commenced adequate spontane ous respirations (remains apnoeic or has slow, gasping or weak selfventilatory efforts), commence assisted ventilation (positive pressure ventilation). This is most commonly achieved with the use of a tightfitting mouthandnose mask, attached to one of the follow ing devices: 588 a. Guedel airway or laryngeal mask) are rarely necessary and prompt improvement in cardiorespiratory function nearly always ensures with adequate ventilation with one of these three devices. Irrespective of which device is used, the primary aim is to achieve adequate ventilation of the lungs. Adequate lung ventilation is assessed by visual inspection of the chest wall movement, which should match that which would occur with normal neonatal respirations. Higher pressures are sometimes required; however, this may result in Chapter 64 Neonatal Physiology: Adaptation and Resuscitation General equipment · Firm, padded resuscitation surface · Overhead warmer · Light for the area · Clock with timer in seconds · Warmed towels or similar covering · Polyethylene bag or sheet, big enough for a baby less than 1500 g birthweight · Stethoscope, neonatal size preferred · Pulse oximeter plus neonatal probe. Equipment for airway management · Suction apparatus and suction catheters (Size 6 French [Fr], 8 Fr and either 10 Fr or 12 Fr) · Oropharyngeal airways (sizes 0 and 00) · Intubation equipment: o Laryngoscopes with infant blades (00, 0, 1) o Spare bulbs, and ba eries o Endotracheal tubes (sizes 2. NeoPuff), or o Flow-inflating bag with a pressure safety valve and manometer and o Self-inflating bag (approximately 240 mL) with a removable oxygen reservoir · Medical gases: o Source of medical oxygen (reticulated and/or cylinder, allowing flow rate of up to 10 L/min) with flow meter and tubing o Source of medical air o Air/oxygen blender · Feeding tubes for gastric decompression. Given that respiratory depression is often the primary issue being treated, adequate ventilation is central to neonatal resuscitation. Direct airway, and hence lung ventilation, can be achieved with the use of a laryngeal airway mask or via an endotracheal tube. The devices listed previ ously can then be attached directly to the laryngeal airway or endotracheal tube to assist in ventilation. However, intubation is rarely required if one appro priately uses a mask and one of the devices listed. Failure of adequate cardiorespiratory function at this point often relates to issues around potential airway obstruction or inadequate ventilation. Adrenaline is the only drug recommended in neonatal resuscitation, although it is rarely required. Adrenaline should only be considered if clear attention, reassessment and establishment of adequate ventilation and chest com pressions do not result in an increase in heart rate. Endo tracheal administration of adrenalin (one requires a tenfold dose) is a further option, but remains controversial. For example, fluid volume expansion may be considered, especially if one sus pects that severe shock is due to fetal blood loss. This may necessitate-in the first instance-the adminis tration of a crystalloid volume expander; that is, 0. Impor tantly, in the absence of severe blood loss, some animal studies have shown deleterious effects of fluidbolus when used in neonatal resuscitation. The Apgar score If present, the severity of birth depression can be ascer tained by a number of clinical methods. The Apgar score comprises assessment of five items: heart rate, respira tory effort, muscle tone, colour and reflex response. The Apgar score is based on the degree of cardiorespiratory and neurological depression present, ventilatory resuscitation commences in air. The use of peripheral oxygen monitoring is recommended, espe cially in the context of laboured breathing and/or when resuscitating a newborn requires assisted ventilation. The use of air/oxygen mixtures allows for the titration of inspired oxygen in order to avoid over oxygenation. Initial resuscitation in 100% oxygen is not recommended; adverse outcomes including delay to establish normal respiratory state have been shown. Importantly, the ability to use air/oxygen mixtures during the resuscitation is now almost universal. Very occasionally, when the heart rate remains < 60 bpm, and despite adequate assisted ventilation, chest compressions are then required. The ratio of compressions to ventilatory breaths in neonates differs from the ratios listed in resuscitation guide lines for infants, children and adults. Chapter 64 Neonatal Physiology: Adaptation and Resuscitation and is measured at 1 and 5 minutes after birth. It is com monly measured in all babies at birth regardless of whether or not birth depression is present. A normal Apgar score is 7 to 10; a score of 4 to 6 demonstrates moderate depression and a score of 0 to 3 demonstrates severe depression. The Apgar score is useful in assessing the adequacy of resuscitation and, in some studies, has been shown to have a degree of prognostic value. Approx imately 9% of babies with an Apgar score at 5 minutes or less than 7 will have some neurological disability com pared to around 2% in the remaining population. The umbilical artery pH best reflects the metabolic state of the fetus and a pH below 7. While both Apgar scores and cord pH sampling have limitations in predicting longterm neurological outcome, in cases where birth depression is suspected both are often obtained and documented. In the event of a prolonged neonatal resuscitation, thought should be given to the cessation of resuscitation. Newborns can be resuscitated, and survive without disability, despite an Apgar score of 0 at 1 minute. General consensus is to consider ceasing resuscitation if the heart rate is undetected and remains so for 10 minutes. Clear and open discussion among the resuscitation team, as well as with the family, should guide decisions regarding starting or ceasing resuscitation. Response to resuscitation In the vast majority of cases of resuscitation, the newborn responds to adequate assisted ventilation and hence restoration of cardiorespiratory function. Subsequent increase in heart rate and improvement in cardiovascular status often ensures purely with effective ventilatory resuscitation. Ongoing research, both in Australia and internation ally, occurs to better facilitate evidencebased resuscitation guidelines (see Box 64. If there has been a significant hypoxic event and/or extensive neonatal resuscitation, clear guidelines exist to assess and offer treatment to these newborns in the immediate postnatal period. This includes post resuscitation therapeutic hypothermia, which is discussed in Chapter 69. Lastly, there may be situations where families choose not to resuscitate a newborn; for example, in extreme prematurity or in cases with known severe congenital anomalies. Conversely, lack of response to a prolonged resuscitation ultimately requires a decision to stop treat ment (see Box 64. Association of Apgar score at five minutes with longterm neurologic disability and cognitive function in a prevalence study of Danish conscripts. In Australia, various states and territories offer neonatal resuscitation training. Additionally, the Australian Resuscitation Council updates and reviews neonatal (and other) resuscitation guidelines. Routine care should: allow maternalinfant bonding promptly detect illness or abnormality of the newborn actively facilitate and support breastfeeding. Newborns should be maintained in a thermal environment that is appropriately warm, while avoiding under- or overheating. The arrival of a new member into the family causes many changes that can be the source of both joy and stress. Vitamin K is often administered intramuscularly at this time in order to prevent haemorrhagic disease of the newborn (see Chapter 74).
Hytrin 2 mg overnight delivery
If these are normal and there is no other explanation prehypertension warsaw 2014 order hytrin mastercard, imaging of the pituitary may be required. If there is any doubt regarding uterine or obstructive causes, a progesterone challenge test may be performed to determine if a normally oestrogenised endometrium is responsive to progesterone withdrawal, and will confirm the existence of a patent outflow tract. Lower genital tract obstruction Cryptomenorrhoea is a term that may be used to describe the situation where menstruation is occurring normally but is not revealed due to obstruction to menstrual flow. Accumulation of menstrual fluid may occur in the vagina (haematocolpos), the uterus (haematometra) and tubes (haematosalpinges). Increased retrograde menstruation into the peritoneal cavity may cause severe endometriosis in a young woman. Sometimes the obstruction is only on one side of a completely or partially duplicated system, resulting in features of obstructed menstrual flow (pain, mass) but with menstruation still occurring-through the patent side. Cervical obstruction to menstrual flow may be due to congenital cervical atresia or cervical stenosis as a consequence of surgery or cancer. At a vaginal level, a complete vaginal septum or area of atresia will prevent menstrual flow, as will an imperforate hymen at the introitus. Treatment Treatment may involve restoration of a normal body weight, a reduction in psychological stressors or normalisation of exercise patterns. However, ovulation induction may be ill-advised if, for example, a low body weight meant that pregnancy was potentially dangerous for both mother and child. Symptoms of endocrine disorders should be sought such as galactorrhoea, cold intolerance, acne and hirsutism. Neurological examination should focus on eliciting bitemporal hemianopia as a sign of a pituitary neoplasm. Chapter 49 Amenorrhoea, Hyperprolactinaemia and Ovulation Induction Hypothalamic: hyperprolactinaemia this condition is discussed later in this chapter. Functions of prolactin include aiding breast development in preparation for lactation, as well as directly facilitating milk production with high serum levels present during pregnancy and lactation. Assessment Investigation should include a karyotype, presence of autoantibodies and evaluation of the anatomy using ultrasound. Drug induced: especially drugs which antagonise dopamine action and hence interfere with the dopamine mediated inhibition of prolactin release. Microprolactinomas (microadenomas) are associated with lower serum prolactin levels (up to 3000 mU/L) while macroprolactinomas (macroadenomas) with a diameter greater than 10 mm can be associated with much higher levels. Nonprolactin-secreting tumours may also cause a raised prolactin by causing compression of the pituitary stalk that interrupts the passage of dopamine from the hypothalamus. All women with signs or virilisation should be investigated for possible androgen secreting tumours. Patients with only polycystic ovaries on ultrasound should be reassured that it is a normal finding. Women who want to conceive but are anovulatory can use clomiphene citrate to induce ovulation. Hirsutism is a relatively common finding in women: 20% will have noticeable hair on the upper lip and in 5% it is also present on the chin and/or side of the face. Other androgen-sensitive areas that may be involved include the chest, upper back and lower abdomen. There is often considerable psychological disturbance and sometimes social withdrawal. Signs of more excessive androgen increase are androgenic alopecia (male-pattern balding), clitorimegaly and voice deepening. These signs and symptoms should prompt a more detailed evaluation, in particular for an androgen-secreting tumour of the ovary or adrenal gland. Vellus is soft, fine and non-pigmented, while terminal hair is coarse and pigmented. In androgen-sensitive areas (upper lip, face, chest, abdomen, back and buttocks), terminal hair can predominate if androgen levels are sufficient or if pilosebaceous glands are sensitive enough to the circulating androgens. It is common for women to have some hair growth in androgen-sensitive areas; 25% of Caucasian women have terminal hair on the upper lip, 10% have terminal hair on the chin, 5% have sideburns and many have periareolar hair. Its distribution and density is largely genetically determined, with the major factors being the number of androgen receptors in the skin and the amount of circulating free androgen. Generally, women with idiopathic hirsutism have androgen levels that are mildly elevated or at the upper end of normal and by definition there is no identifiable cause. Under the influence of the enzyme 5-alpha-reductase, both androstenedione and testosterone are converted to dihydrotestosterone, especially in the skin; dihydrotestosterone is particularly active in stimulating the pilosebaceous follicle. Some women with mild hirsutism may be especially distressed, while others with mild symptoms may be partially treating themselves with cosmetic measures. It is important therefore to assess the level of patient distress on history, and to treat the patient on the basis of this. Idiopathic hirsutism is uncommon is SouthEast Asian women, but more common in Mediterranean, subcontinental and Middle Eastern women. It may be related to androgenic medications such as anabolic steroids, danazol and phenytoin. Ovarian hyperthecosis Ovarian hyperthecosis is seen typically in postmenopausal women, and is caused by the luteinisation of nests of theca cells within the ovarian stroma. Women present with slow onset of hirsutism and acne, often with signs of virilisation. The treatment is bilateral oophorectomy after consideration of other potential causes. The pathogenesis is multifactorial, but elevated androgens have a role by stimulating the growth of sebaceous glands and augmenting sebum productions. The use of antiandrogen medications can see a reduction in the amount of acne lesions present. Examination the most important aspect of clinical examination is to look for signs of virilisation, which could indicate an androgen-secreting tumour, and signs suggestive of endocrine disorders that can lead to hirsutism. The FerrimanGallwey score is a system that can be used to classify the physical extent of androgen-sensitive hair. Being an objective score system, it is poor at assessing a condition that is subjectively experienced by patients. Clinically significant hirsutism should be investigated to elucidate a possible cause Table 50. A young woman with inflammatory papules of acne vulgaris and significant hirsutism. Investigation Serum total testosterone Investigation finding Normal value = idiopathic hirsutism Mild elevation suggests an ovarian source. This is a complicated procedure, and in postmenopausal women, or women whose families are complete, bilateral oophorectomy may be more sensible. Laser hair removal is easily available commercially, and will reduce hair, but with regrowth expected after 12 months. Similarly, electrolysis is readily available at beauty salons, and is theoretically permanent; however, if performed incorrectly (as is common) regrowth will occur, and ongoing hyperandrogenism will also lead to more growth of hair. These methods should be discussed with patients, together with medical treatments, allowing them to decide the level of treatment required. These actions are all irrespective of the type of progesterone in the pill, so inexpensive preparations should be trialled first. More expensive preparations containing cyproterone acetate or drospirenone, which have additional anti-androgenic properties, can be tried if the patient is unhappy with the side effects or response. It is worth trialling treatment for 6 months, given that hair turnover is slow, meaning it will take months to see any benefit. For women who fail to achieve an adequate response, an anti-androgen medication should be added. Two are commonly used in Australia-spironolactone and cyproterone acetate-and both are equally effective. Normal ovaries on ultrasound probably excludes an androgen-secreting ovarian tumour as well, although these are very uncommon and sometimes tumours invisible to ultrasound can secrete significant amounts of androgen. Serum androgen levels are useful to guide the need for further investigation, especially given that clinical signs (such as the FerrimanGallwey score) correlate poorly with serum androgen levels. Generally, in the absence of signs of virilisation and with normal or subtly raised androgen levels, no more investigations are required to diagnose idiopathic hirsutism or exclude more serious diagnoses.