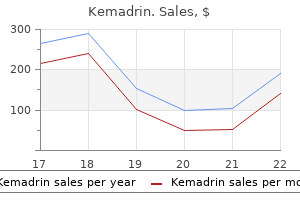
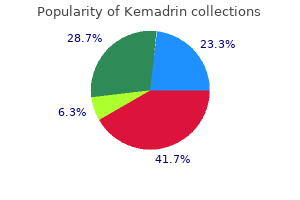
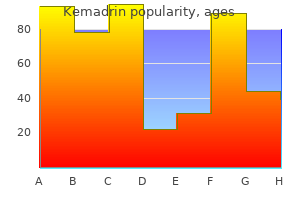
Generic kemadrin 5 mg overnight delivery
All these factors accelerate the development of interstitial fibrosis by increased extracellular matrix symptoms 32 weeks pregnant kemadrin 5mg with visa, cell infiltration, apoptosis, and accumulation of activated myofibroblasts. It has been hypothesized that changes in the intratubular dynamic forces-so-called tubular stretch-in urinary tract obstruction also are an important determinant for development of tubulointerstitial fibrosis in the kidney. Along this line, data suggest that mast cells also have the capacity to release chymase, a protease, which may limit development of tubulointerstitial fibrosis by decreasing infiltration of inflammatory cells and release of proinflammatory and profibrotic chemokines and cytokines. From multiple studies, it has been suggested that the main mechanism that is responsible for the onset of the pathophysiologic cascades is the increased pressure in the renal pelvis, which leads to increased pressure in the parenchyma and subsequently mechanical stress, which leads to activation of stretch and swelling-activated cation channels within focal adhesions of the epithelial cells, causing subsequent influx of Ca2+. Thus the process leading to kidney fibrosis is complex, and numerous processes contribute to regulating the cellular changes that are responsible for these pathophysiologic changes. However, if the studies are relevant to human obstructive nephropathy, they suggest that patients undergoing release of obstruction may benefit from therapies that block proapoptotic, proinflammatory, or profibrotic mediators or from treatments that stimulate epithelial cell growth and differentiation. These results support the view that inflammation is a crucial determinant for the onset of renal deterioration in urinary tract obstruction. However, in experimental models, obstruction in utero can cause pulmonary hyperplasia and renal impairment directly or indirectly, leading to significant morbidity and mortality. The type of intervention depends on the location of the obstruction, its degree, and its cause, as well as the presence or absence of concomitant diseases and complications, and the general condition of the patient. Calculi, the most common form of acute unilateral urinary obstruction, can usually be managed conservatively with analgesics for control of pain and intravenous fluids to increase urine flow. Ninety percent of stones smaller than 5 mm pass spontaneously, but as stones get larger, spontaneous stone passage becomes progressively less probable. Active efforts to fragment or remove the stone are indicated for persistent obstruction, uncontrollable pain, or urinary tract infection. Current possibilities for treatment include extracorporeal shock wave lithotripsy (which may require ureteral stent placement if the patient is symptomatic),308 ureteroscopy with stone fragmentation (usually with laser lithotripsy), and, in rare cases, open excision of the stone. In the past, complex stones high up in the ureter or in the renal pelvis have been difficult to remove without open surgery. Compared with adult obstructive nephropathy, fetal obstructive nephropathy is particularly devastating because renal growth and continued nephron development are impaired by the progression of fibrosis. Several studies have examined aspects of obstructive nephropathy in the newborn using a neonatal rat model of unilateral obstruction, and the pathophysiology involved in fetal urinary tract obstruction will be discussed in Chapter 73. At the time of birth, the rodent kidney is not fully developed and is representative of human renal development at approximately the midtrimester, and animal models reveal that fetal obstruction causes aberrations of morphogenesis, gene expression, cell turnover, and urine composition. It is not well known either if obstruction alone is enough to induce renal dysplasia,296,297 or if the latter results from secondary obstruction-induced mesenchymal disruption. To know the exact role of obstruction in the kidney malformation is very important clinically, because, as mentioned earlier, it is now possible to detect and potentially relieve obstruction in utero. Internal urethrotomy with direct visualization may be effective in the treatment of urethral strictures, because dilation usually has only a temporary effect. Suprapubic cystostomy may be necessary in patients with impassable urethral strictures, followed by open urethroplasty to restore urinary tract continuity, when possible. If more conservative measures such as frequent voiding or intermittent catheterization are not effective, ileovesicostomy or other forms of urinary diversion should be considered. The actual course chosen depends on the likelihood that renal function will improve with the relief of obstruction. Factors that help decide whether to operate and what form of surgical intervention to use include the age and general condition of the patient, the appearance and function of the obstructed kidney and the contralateral one, the cause of the obstruction, and the absence or presence of infection. Robotic surgery has evolved from simple extirpative surgery to complex reconstructions, including hydronephrosis, which is feasible and safe. In many cases, obstruction may be partial, so that it is difficult on the basis of the history alone to predict the outcome. In addition, imaging studies that reveal both anatomy and function of the obstructed kidney predict the extent of functional recovery poorly (see earlier), because the extent of anatomic distortion during obstruction correlates poorly with the extent of recovery once the obstruction is relieved. However, there are presently no methods available to predict reliably the functional potential recovery of an obstructed kidney. In cases of prenatal urinary tract obstruction, clinical decision making is complex because the risks of not intervening can be very high, as can the risks of prenatal surgery. Because fetal intervention can be associated with frequent complications and a high rate of fetal wastage, patients for the intervention should be carefully chosen. Fetal renal biopsy, which demonstrated a 50% to 60% success rate, correlates well with outcome and has few maternal complications. Studies demonstrate that antenatal intervention may help fetuses with the most severe forms of obstructive uropathy, otherwise usually associated with a fatal neonatal course. However, other factors, such as the presence of other illnesses and the presence or absence of urinary tract infection, play an important role as well. However, recovery of renal function in humans has been documented following release of obstruction of 69 days or longer. Chronic bilateral obstruction, as seen in benign prostatic hyperplasia, can cause chronic kidney disease, especially when the obstruction is of prolonged duration and when it is accompanied by urinary tract infections. As noted earlier, studies in experimental animals have implicated a variety of factors in chronic kidney disease due to prolonged obstruction, including excessive production of renal vasoconstrictors such as renin and angiotensin, growth factors that may enhance fibrosis. Decramer S, Wittke S, Mischak H, et al: Predicting the clinical outcome of congenital unilateral ureteropelvic junction obstruction in newborn by urinary proteome analysis. It is notable that clinically significant postobstructive diuresis usually occurs only in the setting of prior bilateral obstruction, or unilateral obstruction of a solitary functioning kidney. The mechanisms involved have been described in detail earlier and involve the combination of intrinsic damage to tubular salt, solute, and water reabsorption, as well as the effects of volume expansion, solute. When the obstruction is unilateral and there is a functioning contralateral kidney, the volume expansion, solute accumulation, and increases in natriuretic substances do not occur, and the contralateral kidney may retain salt and water, resulting in some compensation for the natriuresis and diuresis occurring in the postobstructive kidney. Management of the patient with postobstructive diuresis focuses on avoiding severe volume depletion due to salt wasting, and other electrolyte imbalances, such as hypokalemia, hyponatremia, hypernatremia, and hypomagnesemia. It usually lasts for several days to a week but may, in rare cases, persist for months. In many cases, excessive volume or fluid replacement prolongs the diuresis and natriuresis. During this period, meticulous monitoring of vital signs, volume status, urine output, and serum and urine chemistry values and osmolality is imperative. This will determine the need for ongoing replacement of salt, free water, and other electrolytes. With relief of uncomplicated obstruction, the kidney function usually returns to normal with adequate hormonal responses. Edouga D, Hugueny B, Gasser B, et al: Recovery after relief of fetal urinary obstruction: morphological, functional and molecular aspects. In Gillenwater J, Grayhack J, Howards S, et al, editors: Adult and pediatric urology, ed 2, St. Thorup J, Mortensen T, Diemer H, et al: the prognosis of surgically treated congenital hydronephrosis after diagnosis in utero. Hadas-Halpern I, Farkas A, Patlas M, et al: Sonographic diagnosis of ureteral tumors. Bolling T, Willich N, Ernst I: Late effects of abdominal irradiation in children: a review of the literature. Maeda H, Shichiri Y, Kinoshita H, et al: Urinary undiversion for pelvic actinomycosis: a long-term follow up. Emir L, Karabulut A, Balci U, et al: An unusual cause of urinary retention: a primary retrovesical echinococcal cyst. Tebyani N, Candela J, Patel H, et al: Ureteropelvic junction obstruction presenting as early satiety and weight loss. Akcay A, Altun B, Usalan C, et al: Cyclical acute renal failure due to bilateral ureteral endometriosis. Shimada K, Katsumi T, Fujita H: Appendiceal granuloma causing bilateral hydronephrosis and macroscopic haematuria. Drube J, Zurbig P, Schiffer E, et al: Urinary proteome analysis identifies infants but not older children requiring pyeloplasty. Bandin F, Siwy J, Breuil B, et al: Urinary proteome analysis at 5-year followup of patients with nonoperated ureteropelvic junction obstruction suggests ongoing kidney remodeling. Nasu K, Narahara H, Hayata T, et al: Ureteral obstruction caused by endometriosis.
Buy discount kemadrin 5mg online
Some patients have persistent symptoms jaw cancer 5mg kemadrin mastercard, severe renovascular hypertension that may be resistant to medical therapy. These patients may benefit from revascularization or nephrectomy if they suffered renal infarction, and many show improvement or complete resolution of hypertension after these procedures. Edwards and colleagues have noted adequate responses to medical management in most patients. An acute presentation is usually seen in young patients with a short history of nephrotic syndrome. In these cases, imaging reveals an enlarged kidney and pyelocalyceal irregularities. A chronic presentation is usually seen in older patients with the nephrotic syndrome who have little or no accompanying symptoms except for peripheral edema, increase in proteinuria, and gradual decline in renal function. Doppler ultrasonography can visualize the actual venous flow, increased blood velocity, and turbulence in a narrowed vein or complete cessation of flow if the lumen is totally occluded. Ultrasonography with Doppler color flow should be the initial noninvasive diagnostic study. However, sonography is highly operator dependent and has a low specificity (56%), despite a high sensitivity (85%) in experienced hands. Originally, the notching of the ureters was interpreted as representing mucosal edema; however, more detailed radiographic studies have shown indentation of the ureters by the collateral venous circulation. The Valsalva maneuver is useful during venacavography; when the intraabdominal pressure is increased, the transit of contrast agent and blood from the inferior vena cava is slowed, the proximal part of the main renal vein may be opacified, and the patency of the lumen or even the outline of the thrombus may be demonstrated. A normal renal venogram demonstrates the entire intralobular venous system to the level of the arcuate vein. In general, the use of epinephrine for better visualization of the smaller vessels is not necessary. However, in the presence of normal renal blood flow, all contrast material is washed out of the renal vein within 3 seconds or less, and occasionally only the main renal vein and major branches are visualized. In this situation, there may be uncertainty about thrombi in major or smaller branches. An imbalanced bioavailability of prothrombotic and antithrombotic factors in favor of prothrombotic factors predisposes to intravascular clotting. Impaired thrombolysis and concomitant factors such as volume depletion, hypoalbuminemia, impaired venous blood flow, and immobilization may contribute to precipitate renal vein thrombosis. An abnormal renal venogram usually demonstrates a thrombus within the lumen as a filling defect surrounded by contrast material. In the presence of partial thrombosis, extensive collateral circulation can be demonstrated. However, a low signal from the renal veins and pseudofilling defects due to slow flow, mimicking a thrombus, makes interpretation of the image difficult. An additional mechanism sustaining the procoagulant state is thrombocytosis, which has been found in a number of nephrotic adults and children. Moreover, platelets of nephrotic patients seem to display a tendency to hyperaggregability. The discovery of the association of antienolase autoantibodies with membranous nephropathy offers a tantalizing clue, because these autoantibodies could interfere with fibrinolysis. In addition to the hemostatic abnormalities associated with the nephrotic syndrome, other causative factors include amyloidosis, oral contraceptives, steroid administration, and genetic procoagulant defects. Treatment of established renal vein thrombosis can be divided into measures targeting the specific cause of the occlusion (primary renal disease, tumors, systemic disease) and those aimed at the thrombus itself and/or its complications. The latter includes volume resuscitation, dialysis as necessary, but first and primarily anticoagulation. Current management of renal vein thrombosis has shifted from surgical to medical treatment. Anticoagulation is the mainstay of therapy, and is intended to prevent further propagation of the thrombus and thromboembolic complications while permitting recanalization of occluded vessels. Systemic administration is safe and effective if no obvious contraindications exist and avoids the need for invasive procedures. The optimal duration of warfarin therapy is unknown, but given the risk of recurrence, it is reasonable to maintain anticoagulation as long as the patient is nephrotic and has significant hypoalbuminemia. Treatment with heparin warrants monitoring of the anticoagulation response and is associated with some complications, such as thrombocytopenia and osteoporosis. No randomized controlled trials have been conducted to assess the risk-benefit profile of anticoagulation therapy in patients with nephrotic syndrome. However, a Markov-based decision analysis model has found that the number of fatal emboli prevented by prophylactic anticoagulation exceeds that of fatal bleeding in nephrotic patients with idiopathic membranous nephropathy. Patients with a family history of thrombophilia might also be considered for prophylactic therapy. An alternative therapeutic approach is represented by low-dose aspirin, considering the increased platelet function in nephrotic patients. Licht C, Weyersberg A, Heinen S, et al: Successful plasma therapy for atypical hemolytic uremic syndrome caused by factor H deficiency owing to a novel mutation in the complement cofactor protein domain 15. Nathanson S, Fremeaux-Bacchi V, Deschenes G: Successful plasma therapy in hemolytic uremic syndrome with factor H deficiency. Bresin E, Daina E, Noris M, et al: Outcome of renal transplantation in patients with non-Shiga toxin-associated haemolytic uremic syndrome: prognostic significance of genetic background. Schmidtko J, Peine S, El-Housseini Y, et al: Treatment of atypical hemolytic uremic syndrome and thrombotic microangiopathies: a focus on eculizumab. Hussein M, Mooij J, Khan H, et al: Renal vein thrombosis, diagnosis and treatment. Zandman-Goddard G, Tweezer-Zaks N, Shoenfeld Y: New therapeutic strategies for systemic sclerosis-a critical analysis of the literature. Gasser C, Gautier E, Steck A, et al: Hemolytic-uremic syndrome: bilateral necrosis of the renal cortex in acute acquired hemolytic anemia. Ruggenenti P, Noris M, Remuzzi G: Thrombotic microangiopathy, hemolytic uremic syndrome, and thrombotic thrombocytopenic purpura. Galbusera M, Noris M, Remuzzi G: Thrombotic thrombocytopenic purpura-then and now. Moschcowitz E: An acute febrile pleiochromic anemia with hyaline thrombosis of the terminal arterioles and capillaries: an undescribed disease. Ruggenenti P, Galli M, Remuzzi G: Hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, and antiphospholipid antibody syndromes. Bitzan M, Richardson S, Huang C, et al: Evidence that verotoxins (Shiga-like toxins) from Escherichia coli bind to P blood group antigens of human erythrocytes in vitro. Chiurchiu C, Firrincieli A, Santostefano M, et al: Adult nondiarrhea hemolytic uremic syndrome associated with Shiga toxin Escherichia coli O157:H7 bacteremia and urinary tract infection. Trachtman H, Cnaan A, Christen E, et al: Effect of an oral Shiga toxin-binding agent on diarrhea-associated hemolytic uremic syndrome in children: a randomized controlled trial. Menne J, Nitschke M, Stingele R, et al: Validation of treatment strategies for enterohaemorrhagic Escherichia coli O104:H4 induced haemolytic uraemic syndrome: case-control study. Greinacher A, Friesecke S, Abel P, et al: Treatment of severe neurologic deficits with IgG depletion through immunoadsorption in patients with Escherichia coli O104:H4-associated haemolytic uraemic syndrome: a prospective trial. Loirat C, Niaudet P: the risk of recurrence of hemolytic uremic syndrome after renal transplantation in children. Caprioli J, Castelletti F, Bucchioni S, et al: Complement factor H mutations and gene polymorphisms in haemolytic uraemic syndrome: the C-257T, the A2089G and the G2881T polymorphisms are strongly associated with the disease. Manuelian T, Hellwage J, Meri S, et al: Mutations in factor H reduce binding affinity to C3b and heparin and surface attachment to endothelial cells in hemolytic uremic syndrome. Delmas Y, Vendrely B, Clouzeau B, et al: Outbreak of Escherichia coli O104:H4 haemolytic uraemic syndrome in France: outcome with eculizumab. Colic E, Dieperink H, Titlestad K, et al: Management of an acute outbreak of diarrhoea-associated haemolytic uraemic syndrome with early plasma exchange in adults from southern Denmark: an observational study. Szilagyi A, Kiss N, Bereczki C, et al: the role of complement in Streptococcus pneumoniae-associated haemolytic uraemic syndrome. Besbas N, Karpman D, Landau D, et al: A classification of hemolytic uremic syndrome and thrombotic thrombocytopenic purpura and related disorders. Karthikeyan V, Parasuraman R, Shah V, et al: Outcome of plasma exchange therapy in thrombotic microangiopathy after renal transplantation. Stuhlinger W, Kourilsky O, Kanfer A, et al: Letter: haemolyticuraemic syndrome: evidence for intravascular C3 activation. Noris M, Ruggenenti P, Perna A, et al: Hypocomplementemia discloses genetic predisposition to hemolytic uremic syndrome and thrombotic thrombocytopenic purpura: role of factor H abnormalities.
Purchase kemadrin 5mg without prescription
A position paper has defined the groups of patients in whom isolated kidney transplantation is extremely risky treatment 4 autism order 5mg kemadrin free shipping, where a combined kidneyliver transplantation is recommended, and those eligible to isolated kidney transplantation. Identifying complement gene abnormalities has paved the way for tailored treatments aimed at specifically hampering complement activation. Most patients treated during acute episodes achieved remission with eculizumab, including dramatic cases with severe neurologic involvement or peripheral gangrene. How long eculizumab therapy should be continued and which is the ideal treatment regimen to be administered, however, remains to be established. Conceivably, chronic lifelong treatment with eculizumab at doses able to block the complement cascade persistently might be needed to prevent disease recurrence, at least in a subgroup of patients. Reasonably, different underlying genetic defects, different clinical courses before eculizumab therapy, and different residual complement activity while on eculizumab therapy should be taken into consideration when strategies of chronic eculizumab therapy are planned. Prospective studies titrating eculizumab dosing to reliable markers of complement activation are needed to explore the possibility of gradual back titration and possible withdrawal of chronic treatment, at least in a subset of affected patients. This should reduce the risk of possible and still unknown long-term adverse effects and, considering the tremendous costs of eculizumab therapy, would have major implications for health care providers. In the pre-eculizumab era, liver transplantation had been suggested to correct the complement abnormality and prevent disease recurrence in patients with defects in genes encoding circulating complement proteins that are synthesized in the liver. The outcome, however, was complicated by early liver failure in 15% to 30% of cases. Availability of eculizumab, however, has led to reconsider this therapeutic option. Within each gene, the exons where the mutations tend to localize more frequently should be studied first. In some cases, eculizumab might have the additional benefit of reducing the risk of antibody-mediated rejection. In this context, a successful liver transplantation might allow safely withdrawing eculizumab therapy by restoring the bioavailability of liver-produced complement modulators such as factor H or factor I. On the other hand, perioperative eculizumab therapy might protect the liver from thrombotic microangiopathy and protect against early failure by preventing uncontrolled complement activation precipitated by surgical stress and revascularization damage. Thus, liver transplantation, under the umbrella of perioperative eculizumab therapy, might be a valuable option when chronic eculizumab therapy is unfeasible because of safety concerns or resource restriction. Patients with cobalamin C deficiency usually present in the early days and months of life with failure to thrive, poor feeding, and vomiting. Children may present neurologic symptoms of fatigue, delirium, psychosis, and seizures. In cases with early onset, the disease has a fulminant evolution and occasionally involves the pulmonary vasculature, but when it ensues later in childhood it may follow a more chronic course. The hallmarks of defective cobalamin C metabolism are hyperhomocysteinemia and methylmalonic aciduria, and the extremely high homocysteine levels (up to tenfold higher than normal) have been suggested to have a role in the pathogenesis of the vascular lesions. Without treatment, the disease is fatal, and some children likely die undiagnosed. Daily intramuscular administrations of hydroxycobalamin may reduce homocysteine levels and methylmalonic aciduria, whereas oral hydroxycobalamin and cyanocobalamin are ineffective. Oral betaine helps reduce serum homocysteine levels further by activating betaine homocysteine methyltransferase. Folic acid supplementation to avoid folate deficiency induced by methyltetrahydrofolate trapping and L-carnitine to increase propionyl carnitine excretion have been suggested, but their role in improving disease outcome is unclear. Intensified treatment in older children with less acute disease may achieve remission of the microangiopathic process and amelioration of the other clinical manifestations of the metabolic disorder. This protein plays a major role in primary hemostasis by forming platelet plugs at the sites of vascular injury under high shear stress. Eleven cases have been reported during treatment with clopidogrel, a new antiaggregating agent that has achieved widespread clinical use for its safety profile. The overall survival rate is 67% and is improved by early treatment withdrawal and plasma therapy. Plasma manipulation is a cornerstone in the therapy of the acute episode (see Table 35. Plasma may serve to induce remission of the disease by replacing defective protease activity. Rituximab has been also used electively to prevent relapses in patients with autoantibodies and recurrent disease. Three patients maintained a disease-free status after 29, 24, and 6 months, respectively. Studies on secretion and activity of the mutated forms of the protease have shown that most of these mutations lead to an impaired secretion from cells and, when the mutated protein is secreted, the proteolytic activity is greatly reduced. In most cases, eculizumab will achieve prompt remission of signs and symptoms of the microangiopathic process, and plasma exchange will no longer be required. However, should more exchange sessions be indicated, additional eculizumab doses should be administered shortly after each procedure because the drug is fully cleared from the circulation during the exchange. Fresh-frozen plasma, 1 or 2 L, should be exchanged daily until complete and sustained remission of the microangiopathic process has been obtained (see Table 35. Moreover, at least according to some uncontrolled reports, it also appears to be effective in patients who failed to respond to exchange with fresh- frozen plasma. The duration of remission has ranged from 9 months to 4 years, with relapses reported in approximately 10%. Dialysis is needed in 28% to 61% of patients with acute or subacute disease, with 20% to 30% recovering some kidney function after a variable period of dialytic support. The differential diagnosis includes systemic vasculitis, subacute bacterial endocarditis, polymyositis, myoglobinuric renal failure, drug-induced interstitial nephritis, and renal artery thrombosis or thromboembolism. Atheroembolic renal disease can also occur in renal allografts, with a frequency ranging from 0. The early form is usually associated with primary nonfunction, and the embolic disease is confined to the allograft. The second form is a late clinical presentation, which can arise years after transplantation in stable grafts. The disease is usually associated with precipitating factors, and in some cases shows features of a systemic disorder. Early presentation is frequently associated with poor prognosis, whereas late manifestations generally have a more benign course. The elongated clefts are actually voids where cholesterol crystals were located before fixation and staining. Note the exuberant intimal thickening and the cellular proliferation, which completely occlude the lumen. B, Electron micrograph showing needle-like clefts from atheroemboli to afferent arterioles. To reduce the risk of atheroemboli, an accurate assessment of organ donors should be done. At the time of organ procurement, manipulation of the aorta should be kept to a minimum, mobilizing the kidneys without cross-clamping the aorta, as done for living related donors. Proteinuria is present in more than 50% of patients and may occasionally be in the nephrotic range. The subsequent intravascular inflammatory reaction has been studied in experimental models of atheroembolism and in human biopsy and autopsy samples. In the chronic phase, tissue ischemia is perpetuated by marked endothelial proliferation, intimal thickening, concentric fibrosis of the vessel wall, and persistence of cholesterol crystals and giant cells in the lumens of affected arteries. Hyalinization of glomeruli, atrophy of renal tubules, and multiple wedge-shaped infarcts in the kidney result in reduced kidney size. These events induce a general inflammatory response, including the recruitment of neutrophils and macrophages to the site of crystal formation. Although these enhance local inflammation, macrophages may also contribute to crystal clearance or progressive scarring, respectively. The use of steroids is controversial and, in some series, does not appear to be beneficial, whereas in other series it has been associated with improved outcomes, independent of the doses administered. Also, the brachial approach for aortography or coronary angiography appears to be burdened by less morbidity than the femoral approach.
Kemadrin 5 mg low cost
With the addition of indices of glomerulotubular junction abnormalities and Vv(Int/cortex) medications like adderall order kemadrin 5mg otc, this increased to 92%. These structural-functional relationships are largely driven by more advanced lesions, however; structural changes are highly variable (from almost none to moderately severe) in patients without functional abnormalities. However, the relationship of renal structural changes to these low levels of albuminuria. Thus, microalbuminuria is a marker of more advanced lesions as well as other functional disturbances. Study design and renal structural-functional relationships in patients with long-standing type 1 diabetes. Through much of the natural history of diabetic nephropathy, lesions develop in complete clinical silence. This typical clinical story is best mirrored by nonlinear analyses of structural-functional relationships. There is a growing body of information, discussed elsewhere in this chapter, which supports the view that not only is glycemia a risk factor, but genetic variables also confer susceptibility or resistance to diabetic nephropathy. Mean glomerular volumes were higher in patients developing diabetic nephropathy after 25 years of type 1 diabetes compared with a group developing nephropathy after only 15 years. The number of glomeruli per kidney can vary markedly among nondiabetic individuals and among diabetic patients and it has been suggested that fewer glomeruli per kidney could be a risk factor for diabetic nephropathy. Ekinci and colleagues62 have recently described that among normoalbuminuric type 2 diabetic patients with impaired renal function, only a subset had typical diabetic glomerulopathy, whereas the remaining patients had predominantly tubulointerstitial and vascular changes. However, a study performed in type 2 diabetic white patients demonstrated a significant reduction in podocyte density in the microalbuminuric compared to the normoalbuminuric patients. The imprecise correlation between glomerular structure and renal function in patients with type 2 versus type 1 diabetes may be related to the more complex patterns of renal injury seen in type 2 diabetic patients (see earlier). Approximately 40% of patients showed atypical renal injury patterns, and these patterns were associated with a higher body mass index and less diabetic retinopathy. It is possible that the atypical manifestations of renal injury in type 2 diabetes could be related to the pathogenesis of type 2 diabetes per se. Obesity, hypertension, increased plasma triglyceride levels, decreased high-density lipoprotein cholesterol concentrations, and accelerated atherosclerosis accompany hyperglycemia in many type 2 diabetic patients. Renal dysfunction in these patients could be the consequence of hypertensive nephrosclerosis, hyperlipidemic renal vascular atherosclerosis, renal hypoperfusion due to congestive heart failure, or the synergistic effects of these multiple risk factors for renal disease, which could simulate nephropathy clinically in type 2 diabetes. The increased risk of clinical renal disease in distinct populations, such as African American, American Indian, or Hispanic patients, could represent variability in the renal consequence of one or more of these pathogenetic influences. For example, there are differences in the renal structural consequences of hypertension in African American compared with white patients. As already discussed, proteinuric type 2 diabetic patients without retinopathy may have a high incidence of atypical renal biopsy findings or other diseases. Whether healing can be induced by treatments other than cure of the diabetic state is currently unknown. The overall prevalence of microalbuminuria and macroalbuminuria is around 30% to 35% in both types of diabetes. However, the range in prevalence of diabetic nephropathy is much wider in type 2 diabetic patients. Clearly, the inability to define the onset of disease in type 2 diabetes is a confounding issue. The highest prevalence, exceeding 50%, is found in Native Americans, followed by Asians, Mexican Americans, blacks, and European white patients. Diabetic nephropathy rarely develops in patients with type 1 diabetes before 10 years after diagnosis, whereas approximately 3% of patients with newly diagnosed type 2 diabetes already have overt nephropathy. Thus, the risk of developing diabetic nephropathy is reduced for a normoalbuminuric patient who has had diabetes for longer than 30 years. Microalbuminuria has been proposed to be a marker of widespread endothelial dysfunction, which might predispose to enhanced penetrations of atherogenic lipoprotein particles into the arterial wall, and as a marker of established cardiovascular disease. Several other studies have confirmed the poor prognosis for type 1 diabetic patients with diabetic nephropathy. More recent studies have demonstrated how excess mortality in type 1 diabetes compared to the background population is almost entirely seen in patients with elevated albumin excretion. Unfortunately, this calendar effect is less well described in proteinuric type 2 diabetic patients, but data from a cohort followed from 2000 to 2010 demonstrated a 50% reduction in mortality compared to patients followed from 1983 to 2000. The lower baseline risk of death in young patients in the general population magnifies the relative risk for type 1 diabetic patients. Among European patients with type 2 diabetes, those with proteinuria had a fourfold excess of premature death compared with patients without proteinuria. Abnormalities related to well-established cardiovascular risk factors alone cannot account for this finding. However, studies in types 1 and 2 diabetic patients with diabetic nephropathy have yielded conflicting results. It has been shown that cardiac autonomic neuropathy predicts cardiovascular morbidity and mortality in type 1 diabetic patients with diabetic nephropathy. However, the demonstrated increase in filtration fraction is compatible with an enhanced transglomerular hydraulic pressure difference. Total glomerular capillary surface area is clearly increased at the onset of human diabetes. Studies of rats with experimentally induced diabetes treated with insulin have revealed hyperfiltration, hyperperfusion, enhanced glomerular capillary hydraulic pressure, reduced proximal tubular pressure, unchanged systemic oncotic pressure, and unchanged or slightly elevated Kf. It has been suggested that uric acid level is related to hypertension, metabolic syndrome, and renal disease. Consequently, more than one urine sample is needed to determine whether an individual patient has persistent microalbuminuria. For convenience, it has been recommended to use early morning spot urine samples for screening and monitoring. A normal urinary 2-microglobulin excretion rate in microalbuminuria suggests that albumin is derived from enhanced glomerular leakage rather than from reduced tubular reabsorption of protein. The transglomerular passage of macromolecules is governed by the size- and charge-selective properties of the glomerular capillary membrane and hemodynamic forces operating across the capillary wall. Alterations in glomerular pressure and flow influence the diffusive and convective driving forces for transglomerular passage of proteins. Studies using renal clearance of endogenous plasma proteins or dextrans have not detected a simple size-selective defect. Reduction in the glycocalyx above the endothelial cell may represent the first abnormality in the development of albuminuria. A close correlation between filtration fraction and urinary albumin excretion has also been shown. The demonstration that microalbuminuria diminishes promptly with acute reduction in arterial blood pressure argues that reversible hemodynamic factors play an important role in the pathogenesis of microalbuminuria. Imanishi and colleagues have demonstrated that glomerular hypertension is present in type 2 diabetic patients with early nephropathy and is closely correlated with increased urinary albumin excretion. A direct effect of insulin on increasing distal sodium reabsorption has also been demonstrated. Markers of acute tubular damage have also been investigated in relation to prediction and progression of diabetic nephropathy. However, the difference in prevalence of parental hypertension was not evident when office blood pressure measurements were used. Fluid retention is frequently observed early in the course of this kidney disease-that is, at a stage characterized by well-preserved renal function and only modest reduction in serum albumin level. Some studies have suggested that capillary hypertension, increased capillary surface area, and reduced capillary reflection coefficient for plasma proteins contribute to the edema formation, whereas the washdown of subcutaneous interstitial protein tends to prevent the progressive edema formation in diabetic nephropathy. Importantly, this rate of decline is highly variable across individuals, ranging from 2 to 20 mL/ min/yr, with a mean of about 12 mL/min/yr. Myers and colleagues have demonstrated a reduction in the number of restrictive pores resulting in loss of ultrafiltration capacity (Kf) and impairment of glomerular barrier sizeselectivity leading to progressive albuminuria and increases in urine levels of IgG in diabetic nephropathy.
Discount kemadrin 5mg with amex
The benefits of rapid acquisition include improvement in image quality treatment narcissistic personality disorder discount kemadrin on line, as a result of reduction of motion artifact; reduction of total scan time; and the ability to perform dynamic imaging. Not all implants or devices cause problems, but knowledge of the type of device is crucial for determining whether the patient can safely enter the magnet. Unlike iodinated contrast agents, the dose response to Gd-C is nonlinear; the signal intensity increases at low concentrations and then decreases at higher concentrations. Hence the collecting systems, ureters, and bladder first brighten and then darken on T1-weighted sequences as the gadolinium concentration within the urine increases. Gd-C agents have been approved for parenteral use since the 1980s and are generally well tolerated with a good safety profile. Although most Gd-C agents are clinically interchangeable, they can be differentiated on the basis of molecular stability, viscosity, and osmolality. Risk factors for adverse reactions include a history of prior reaction to Gd-C and/or iodinated contrast agents, where rates are at an eight-fold higher risk; and asthma, as well as other allergies, where rates are reported as high as 3. Because adverse reactions may occur more frequently with ionic Gd-C agents, the use of a non-ionic agent should be considered, if available. As with iodinated contrast material, hemodialysis filters Gd-C effectively, and dialysis is therefore recommended immediately after use of contrast material in patients already on hemodialysis. Burning, itching, or severe pain in involved areas or "deep bone pain" in hips and ribs has been described, as has rapid, new-onset fluctuating hypertension. Patients who may be at high risk include those over 60 years of age and those with a history of renal disease, diabetes treated with prescribed medications, and/or hypertension. Physician discretion should be used to determine the risk of Gd-C use in this patient population. This is not an absolute contraindication; however, the use of Gd-C should be at the discretion and judgment of the ordering physician. Coronal(A)andaxial (B) T2-weighted images demonstrate decreased signal intensity of the renal cortex in relation to the medullary pyramids. By taking advantage of some of these factors, diagnostic angiography and venography may be performed without the use of intravenous contrast; these sequences are sometimes called "bright-blood" sequences. The most robust sequences are based on inversion recovery, balanced steady-state free precession techniques. Although a good morphologic examination, T2-weighted urography is ultimately limited by a lack of functional information. In patients with nondilated systems, both techniques require hydration and furosemide for adequate distension of the renal collecting system. This rapid breath-hold sequence takes less than 5 seconds to obtain and is presented as a urogram-like image. The T2-weighted sequence is used as an initial survey of fluid within the collecting system. What prevents widespread clinical use, however, is the lack of consensus on optimal imaging technique and methods of data analysis. Also, hepatobiliary excretion is approximately 3%, which increases with renal insufficiency. Depth photon attenuation is corrected according to a formula relating body weight and height. The relative tubular function may be obtained by drawing renal regions of interest, corrected for background activity. Planar images are obtained in the anterior, posterior, left anterior oblique/right anterior oblique, and right posterior oblique/ left posterior oblique projections. Normal variations include dromedary hump (splenic impression on the left kidney), fetal lobulation, horseshoe kidney, crossed fused ectopy, and hypertrophied column of Bertin. The renal images also allow accurate assessment of the relative renal size, position, and axis. Prerenal and renal causes include hypotension or dehydration resulting in hypoperfusion of the kidneys and nephrotoxic drugs138 and account for more than 90% of all cases. Hydronephrosis is generally graded according to the extent of calyceal dilation and the degree of cortical thinning. The calyces appear as large, ballooned, fluid-filled structures with a dilated renal pelvis of variable size. Cortical loss is evident, with the dilated calyces approaching or reaching the renal capsule. The central echo complex is separated by the mildly distended calycesandrenalpelvis. The degree of hydronephrosis is not always correlated with the amount of obstruction. In hydronephrosis the dilated calyces have a visibly direct communication with the renal pelvis, which is also dilated. These findings, however, are nonspecific, and kidney biopsy may be required for diagnosis. The normal corticomedullary differentiation is lost with increasing cortical echogenicity. Sequential studies over time may be used to assess the progression of disease by monitoring the renal size and cortical echogenicity. The course of the dilated ureters may be followed distally to establish the site of obstruction. The cause of obstruction is frequently visible and may include pelvic tumors, distal ureteral stones, and retroperitoneal adenopathy or mass. If obstruction is not the cause, other potential causes such as cirrhosis and ascites with accompanying hepatic failure may be evident. In general, the overall size and thickness of the renal parenchyma appear to decrease with age. The density of the internal contents of the cysts may also vary as a result of hemorrhage or proteinaceous debris. A, Axial T2-weighted image demonstrates a heterogeneous renal mass with high signal intensity (arrowhead) and a structure of intermediate signal intensity adjacent to the inferior vena cava that is suspect for vascular invasion (arrow). However, this imaging pattern is nonspecific and must be interpreted in the clinical context. Obstruction can be ruled out if the clearance half-time of the renal pelvic emptying is less than 10 minutes. A slow downward slope after furosemide administration may be indicative of partial obstruction. A 17-year clinical experience at one institution proved that this protocol is useful for patients of all ages and for all indications. Nephrocalcinosis refers to diffuse or punctate renal parenchymal calcification occurring in either the medulla or cortex, usually bilaterally. Calcifications also occur in vascular structures, particularly in patients with diabetes and advanced atherosclerotic disease. Theleftkidneyhasnocontrast material in the pelvicalyceal system and contains only nonopacifiedurine. The stippled calcifications of hyperoxaluria may be found in both the cortex and the medulla, as well as in other organs, such as the heart. Nephrocalcinosis occurs in other diseases in which hypercalcemia or hypercalciuria occur, such as hyperthyroidism, sarcoidosis, hypervitaminosis D, immobilization, multiple myeloma, and metastatic neoplasms. In 70% to 75% of cases of renal tubular acidosis, there is evidence of nephrocalcinosis. The calcifications tend to be uniform and distributed throughout the renal pyramids bilaterally. With medullary sponge kidney and renal tubular ectasia, small calculi form in the distal collecting tubules, probably because of stasis. The calcifications are small, round, and within the peak of the pyramid adjacent to the calyx. Medullary sponge kidney is also associated with nephrolithiasis, because the small calculi in the distal collecting tubules may pass into the collecting systems and ureters, resulting in renal colic.
Cheap kemadrin 5mg otc
These can be extremely useful in establishing the diagnosis of hypovolemia caused by extrarenal fluid losses if there is no intrinsic renal injury and the patient is oliguric medications 7 rights purchase kemadrin 5 mg free shipping. The expected renal response of Na+ and water conservation, by enhanced renal tubular reabsorption, results in oliguria, urine specific gravity exceeding 1. In a patient who previously had undergone diuretic therapy, especially with loop diuretics, these indices may Hemoglobin. This may decrease if significant bleeding has occurred or is ongoing, but this change, which is caused by hemodilution that results from translocation of fluid from the interstitial to intravascular compartment, may take up to 24 hours. In hypovolemic situations that do not arise from bleeding, hemoconcentration is often seen, although this too is not universal, inasmuch as underlying chronic diseases that cause anemia may mask the differential loss of plasma. In that case, fractional excretion of urea from less than 30% to 35% may help in the diagnosis of hypovolemia, although the specificity of this test is rather low. Thus, tachycardia and hypotension are usually present, but the extremities are warm, which suggests that perfusion is maintained. This finding is misleading because vital organs, particularly the brain and kidneys, are underperfused as a result of the hypotension. This replacement should continue until blood pressure is corrected and tissue perfusion is restored. In the second stage of fluid replacement, the rate of administration should be reduced to maintain blood pressure and tissue perfusion. The composition of replacement fluid had been thought to be less critical than the rate of infusion. The two main categories of replacement solution are crystalloid and colloid solutions. The distribution of the solute-free compartment throughout all the fluid compartments would result in plasma dilution and reduction in the plasma Na+. Therefore, this solution should be reserved for the management of hypernatremic hypovolemia. Even in that situation, it must be remembered that volume replacement is less efficient than with isotonic saline and, early on during the treatment course, may cause plasma tonicity to fall too rapidly. In the presence of accompanying hypokalemia, especially if metabolic alkalosis is also present, volume replacement solutions must be supplemented with K+. The goals of treatment of hypovolemia are to restore normal hemodynamic status and tissue perfusion. These goals are achieved by reversal of the clinical symptoms and signs, described previously. In general, when hypovolemia is associated with a significant hemodynamic disturbance, intravenous rehydration is required. Older patients are especially vulnerable to aggressive fluid challenge, and careful monitoring is required, particularly to prevent acute left ventricular failure and pulmonary edema that result from overzealous correction. Sometimes the clinical signs do not point unequivocally to the diagnosis of hypovolemia, even though the history is strongly suggestive. Because invasive monitoring of central venous and pulmonary venous pressures has not been shown to improve outcomes in this situation,396,397 a so-called diagnostic fluid challenge can be performed. If the patient improves clinically, blood pressure and urine output increase, and no overt signs of heart failure appear over the succeeding 6 to 12 hours, then the diagnosis is substantiated and fluid therapy can be cautiously continued. Conversely, if overt signs of fluid overload appear, the fluid challenge can be stopped and diuretic therapy reinstituted. The initial calculations for replacing the fluid deficit are based on hemodynamic status. This "dogma" was recently challenged by the findings of a large prospective observational study performed in the intensive care unit setting. In this study, two periods were compared; in the control period, all patients received isotonic saline as fluid replacement, whereas during the intervention period, Hartmann solution (lactate-containing), Plasma-Lyte 148 (a balanced salt solution), or chloride-poor 20% albumin solution was administered. Because the transcapillary barrier is impermeable to these large molecules, in theory they expand the intravascular compartment more rapidly and efficiently than crystalloid solutions. Colloid solutions may be useful in the management of burns and severe trauma when plasma protein losses are substantial, and rapid plasma expansion with relatively small volumes is efficacious. However, when capillary permeability is increased, as in states of multiorgan failure or the systemic inflammatory response syndrome, colloid administration is ineffective. Moreover, randomized controlled studies in which crystalloid solutions were compared with colloid solutions have shown no survival benefit and even harm with some colloid solutions, particularly hydroxyethyl starch. In most people, increments in Na+ intake are matched by corresponding changes in Na+ excretion as a result of the actions of the compensatory mechanisms detailed earlier (see section, "Physiology"). Primary Renal Na+ Retention Treatment of relative hypovolemia is more difficult than that of absolute hypovolemia because there is no real fluid deficit. When vasodilation is more severe, vasoconstrictor agents may be needed to maintain systemic blood pressure. This can be further subclassified as caused by intrinsic kidney disease or primary mineralocorticoid excess. In contrast, in chronic kidney disease, renal tubular adaptation to salt intake is usually efficient until late stage 4 and stage 5. Primary mineralocorticoid excess or enhanced activity, in their early phases, lead to transient Na+ retention. However, because of the phenomenon of "mineralocorticoid escape," the dominant clinical expression of these diseases is hypertension. Secondary Renal Na+ Retention this occurs in low- and high-output cardiac failure and in systolic and diastolic dysfunction. Hepatic cirrhosis with portal hypertension and nephrotic syndrome are also accompanied by renal Na+ retention. The pathophysiologic process of hypervolemia is comprised of local mechanisms of edema formation and systemic factors stimulating renal Na+ retention; systemic factors can be further subclassified as abnormalities of the afferent sensing limb or efferent effector limb. Transcapillary fluid and solute transport can be viewed as consisting of two types of flow, convective and diffusive. Capillary hydraulic pressure (Pc) is under the influence of a number of factors, including systemic arterial and venous blood pressures, local blood flow, and the resistances imposed by the precapillary and postcapillary sphincters. Systemic arterial blood pressure, in turn, is determined by cardiac output, intravascular volume, and systemic vascular resistance; systemic venous pressure is determined by right atrial pressure, intravascular volume, and venous capacitance. Also, massive accumulation of fluid in the peripheral interstitial compartment (anasarca) can itself diminish venous compliance and, hence, alter overall cardiovascular performance. Net outward movement of fluid along the length of the capillary is associated with an axial decrease in Pc and an increase in c. Nevertheless, the local P continues to exceed the opposing throughout the length of the capillary bed in several tissues; thus, filtration occurs along its entire length. In view of the importance of lymphatic drainage, the lymphatic vessels must be able to expand and proliferate, and the lymphatic flow must be able to increase in response to increased interstitial fluid formation; these mechanisms help minimize edema formation. First, precapillary vasoconstriction tends to lower Pc and diminish the filtering surface area in a given capillary bed. In fact, in the absence of appropriate regulation of microcirculatory myogenic reflex, excessive precapillary vasodilation appears to account for interstitial edema in the lower extremities that is associated with some Ca2+ entry blocker vasodilators. The resulting change in the profile of Starling forces in association with increased filtration, therefore tends to mitigate further interstitial fluid accumulation. Insofar as the continued net accumulation of interstitial fluid without renal Na+ retention might result in prohibitive intravascular volume contraction and cessation of interstitial fluid formation, generalized edema is therefore indicative of substantial renal Na+ retention. In summary, all states of generalized edema reflect past or ongoing renal Na+ retention. In stark contrast, healthy individuals with the same degree of Na+ retention readily increase Na+ and water excretion. Moreover, intrinsic renal function, in the absence of underlying renal disease, is normal in edematous states. Similarly, when kidneys from patients with endstage liver disease are transplanted into patients with normal liver function, Na+ retention no longer occurs. Arterial underfilling could result from low cardiac output, peripheral arterial vasodilation, or a combination of the two. Similarly, conditions such as high-output cardiac failure, sepsis, cirrhosis, and normal pregnancy lead to peripheral arterial vasodilation and activation of arterial baroceptors.
Diseases
- Vitamin D resistant rickets
- Hyperoxaluria type 1
- Inborn renal aminoaciduria
- Arthrogryposis multiplex congenita distal
- Alopecia universalis
- Neurogenic hypertension
- Lambert Eaton myasthenic syndrome (Lambert Eaton paraneoplastic cerebellar degeneration)
- Klippel Feil syndrome recessive type
- Seow Najjar syndrome
Cheapest kemadrin
In a small number of elderly patients medicine look up drugs discount kemadrin express, generalized global sclerosis can also manifest as nephrotic proteinuria caused by undiagnosed processes that lead to renal scarring, with hypertension hastening this process. Based on limited data, recommendations for treatment of glomerular diseases are to select and tailor therapy for the elderly using the same criteria as for younger individuals. Treatment with medications requires cautious dosing and careful follow-up because drug metabolism and renal excretion are altered in the elderly, raising the risk of drug toxicity. Older individuals may experience episodes of volume overload and symptoms of heart failure, gastrointestinal bleeding, hypertension, or gradual confusion that indicate progression of renal loss. Estimates of renal function from serum creatinine levels alone may be inadequate in the elderly, given the changes in muscle mass with age. This survival advantage was lost in patients with multiple comorbid conditions, particularly in those with ischemic heart disease. Similarly, peritoneal dialysis may be an option for elderly patients who experience hemodynamic instability during hemodialysis. Elderly patients undergoing dialysis may be more prone to hypoglycemia because of prolonged insulin clearance, poor intake, and decreased sympathetic response due to other medications. Therefore, close monitoring of medications and careful attention to detect subtle changes in the clinical condition of the elderly patient undergoing dialysis are essential. Symptom relief and maintenance of independence should be considered the main goals of treatment. In 2011, 60% of kidney transplant recipients were older than 50 years, of whom 18% were older than 65 years. Delayed graft function and some decrease in allograft survival, as well as in patient survival, can be associated with increasing donor age. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: 2009annual report. Nearly half the patients age 60 or older die waiting for deceased donor transplants. In a study comparing retrospective cohorts of patients 65 years or older with those between 50 and 64 years and those younger than 50 years over 15 years, cohorts older than 50 years were found to have a higher risk of death over time. Time to death was significantly shorter for those 65 years or older who had coronary artery disease or congestive heart failure. In conclusion, with careful screening and the absence of contraindications to transplant candidacy, recipient performance status as well as discussions regarding life expectancy with and without transplantation may be more useful than age alone in the consideration of renal transplantation in the elderly patient. Coexisting illnesses in the elderly, including cerebrovascular accidents, dementia, impaired mobility, and incontinence of bladder and bowel, often are associated with poor hygiene. Bladder dystonia, changes in the pelvic musculature, prostatic enlargement, and urethral stricture can contribute to obstructive uropathy. Decreased prostatic secretions in older men may predispose to infections of the lower urinary tract. Prostatic microcalculi can harbor bacteria and become a nidus for infection in an elderly man. Decreased vaginal estrogen levels in postmenopausal women may lead to increased vaginal pH by causing relative depletion of lactobacilli and may raise the risk for bacterial colonization and infection. Pyelonephritis usually manifests as costovertebral angle tenderness, fever, and variable lower urinary tract symptoms. Dysuria, change in the character of the urine, and altered mental status were the only clinical features significantly associated with bacteriuria plus pyuria. Of these features, dysuria most effectively discriminated between those with and those without bacteriuria plus pyuria. Nearly 25% to 50% of institutionalized elderly women and 15% to 40% of institutionalized elderly men, however, are found to have asymptomatic bacteruria. For elderly patients without indwelling catheters, the minimum criterion for initiating antibiotic therapy according to consensus guidelines is acute dysuria alone or fever in the presence of at least one of the following: new or worsening urgency, frequency, suprapubic pain, gross hematuria, costovertebral angle tenderness, and urinary incontinence. For symptomatic infection in the patient with an indwelling catheter, the catheter should be removed and replaced with a new catheter before initiation of antimicrobial treatment. In relatively healthy women living in the community, however, a short course of empiric antimicrobial therapy can be effective if the patient shows typical symptoms. Treatment is continued for 10 to 14 days for pyelonephritis in both men and women. The initial treatment for chronic bacterial prostatitis is the use of a prostatepenetrating antimicrobial agent. A first-line regimen is nitrofurantoin 50 or 100 mg or trimethoprim-sulfamethoxazole, one half a regularstrength tablet daily or every other day at bedtime. Storz P: Reactive oxygen species-mediated mitochondria-tonucleus signaling: a key to aging and radical-caused diseases. Lavu S, et al: Sirtuins-novel therapeutic targets to treat ageassociated diseases. They may be solitary, or multiple and bilateral and generally have little clinical significance. Mulkerrin E, et al: Aldosterone responses to hyperkalemia in healthy elderly humans. Miya M, et al: Age-related decline in label-retaining tubular cells: implication for reduced regenerative capacity after injury in the aging kidney. Kurella Tamura M, et al: Functional status of elderly adults before and after initiation of dialysis. Melk A, et al: Cell senescence in rat kidneys in vivo increases with growth and age despite lack of telomere shortening. Jiang S, et al: Age-related change in kidney function, its influencing factors, and association with asymptomatic carotid atherosclerosis in healthy individuals-a 5-year follow-up study. Corman B, et al: Effect of feeding on glomerular filtration rate and proteinuria in conscious aging rats. Remuzzi A, et al: Angiotensin converting enzyme inhibition ameliorates glomerular filtration of macromolecules and water and lessens glomerular injury in the rat. Zoja C, et al: Renal protective effect of angiotensin-converting enzyme inhibition in aging rats. Ferder L, et al: Decreased glomerulosclerosis in aging by angiotensin-converting enzyme inhibitors. Inserra F, et al: Renal interstitial sclerosis in aging: effects of enalapril and nifedipine. Liangos O, et al: Epidemiology and outcomes of acute renal failure in hospitalized patients: a national survey. McLachlan M, Wasserman P: Changes in sizes and distensibility of the aging kidney. Tauchi H, Tsuboi K, Okutomi J: Age changes in the human kidney of the different races. Wang X, et al: Age, kidney function, and risk factors associate differently with cortical and medullary volumes of the kidney. Baert L, Steg A: Is the diverticulum of the distal and collecting tubules a preliminary stage of the simple cyst in the adult Gagliano N, et al: Age-dependent expression of fibrosis-related genes and collagen deposition in rat kidney cortex. Basso N, et al: Protective effect of the inhibition of the reninangiotensin system on aging. Sataranatarajan K, et al: Molecular events in matrix protein metabolism in the aging kidney. Hill C, et al: Basal and stimulated nitric oxide in control of kidney function in the aging rat. Sonaka I, Futami Y, Maki T: L-arginine-nitric oxide pathway and chronic nephropathy in aged rats. Adler S, et al: Oxidant stress leads to impaired regulation of renal cortical oxygen consumption by nitric oxide in the aging kidney. Hogan M, Cerami A, Bucala R: Advanced glycosylation endproducts block the antiproliferative effect of nitric oxide: role in the vascular and renal complications of diabetes mellitus. Baylis C: Sexual dimorphism in the aging kidney: differences in the nitric oxide system. He C, et al: Dietary glycotoxins: inhibition of reactive products by aminoguanidine facilitates renal clearance and reduces tissue sequestration. Menini S, et al: Deletion of p66Shc longevity gene protects against experimental diabetic glomerulopathy by preventing diabetesinduced oxidative stress.
Discount kemadrin generic
This report constitutes a proof of principle for the role of the 24-hydroxylase in D-dependent calcium stones but it is difficult to determine whether these alleles predispose to urolithiasis in the general population symptoms 5 days after conception buy kemadrin us. It was proposed that the postprandial inhibition of renal tubular calcium reabsorption is due to differences in insulin levels in hypercalciuric stone formers. B,Theactualfraction(%)ofdistallydeliveredcalcium that was excreted decreased with increasing distal delivery, and stone formers lie above normal subjects at a comparable distal delivery. This study is at variance with a previous report that used insulin extracted from islets rather than recombinant insulin and that showed significant insulin-induced hypercalciuria. Citrate is freely filtered, and approximately 10% to 35% of filtered citrate is excreted in urine; however, this varies tremendously, depending mainly on acid-base status. The reabsorption of citrate predominantly occurs from the proximal convoluted tubule and, to a lesser extent, the proximal straight tubule. Oxalate is a dicarboxylic acid and, in mammals, is an end product of hepatic metabolism. Oxalate balance consists of ingestion and endogenous production versus intestinalandurinaryexcretion. A number of other metabolic precursors of oxalate metabolism, including by-products of the breakdown of ascorbic acid, fructose, xylose, and hydroxyproline, potentially contribute to oxalate production. There is a wide variation in estimated intake of oxalate, ranging from 50 to 1000 mg/day. It was proposed that the main fraction of oxalate is absorbed in the small intestine, since most oxalate is absorbed during the first 4 to 8 hours after the consumption of oxalate-rich foods,358,366,379,380 and 5 hours of intestinal transit time is required for nutrients to move from the stomach to the colon. Nevertheless, it has also been suggested that the colon also participates, but to a lesser extent, in oxalate absorption. However, it has been proposed that at a low gastric pH, part of the dietary oxalate is converted into small hydrophobic molecules that could possibly diffuse through the lipid bilayer,381-384 thereby increasing urinary oxalate excretion. The anion exchange transporter Slc26a6 has been shown to be involved in intestinal oxalate transport. Furthermore, in vivo studies in Slc26a6 null mice on a controlled oxalate diet showed increased plasma oxalate concentration, decreased fecal oxalate excretion concentration, and high urinary oxalate excretion. These results suggest that diminished net oxalate secretion in the gut is responsible for net oxalate absorption; this results in a rise in plasma oxalate concentration, elevated urinary oxalate excretion and bladder stones, and Yasue-positive crystals in the kidney. However, the influence of this putative anion exchange transporter on intestinal oxalate absorption- specifically, its role in kidney stone formation in humans- has not yet been demonstrated. Studies with exogenous radiolabelled oxalate in normal humans have shown that renal excretion accounts for most of the disposal of oxalate. Oxalate is not significantly protein-bound and is freely filtered at the glomerulus. With impaired kidney function, plasma oxalate concentration steadily increases, exceeds its saturation in the blood, and therefore enhances the risk of systemic tissue oxalate deposition, including kidney damage. Radiolabeled oxalate studies398,399 have demonstrated oxalate secretion, while endogenous renal oxalate clearance assessments using direct measurements of serum and urine oxalate have demonstrated net reabsorption. In slc26a6 null mice, the high serum oxalate appears to be driven mostly by hyperoxalemia rather than by renal leak of oxalate. A national private insurance claim database from 2002 to 2006 supported the notion that gastric banding is not associated with increased kidney stone risk. This disease is severe and is associated with frequent stone recurrence and impaired kidney function. Enteric hyperoxaluria due to inflammatory bowel disease, jejunoileal bypass, and modern bariatric surgeries for morbid obesity are the most common causes of hyperoxaluria in clinical practice. A comparison of Oxalate and calcium are both important in raising CaOx supersaturation in urine. Normal urine is often supersaturated with CaOx because the solubility of CaOx in an aqueous solution is limited to approximately 5 mg/L at a pH of 7. Considering that normal urine volume ranges from 1 to 2 L/day, normal urinary excretion is more than 40 mg. In most cases, one can surmise that normal urine is supersaturated with CaOx salt. However, under normal conditions, the blood is undersaturated with respect to CaOx. Over the past 4 decades, the average CaP content of stones has progressively increased. It has been suggested that urinary pH elevation plays the most important role in the transformation of CaOx to CaP. A retrospective study of 62 patients found that high urinary pH was the primary physiologic abnormality in those in whom CaOx transformed to CaP. This has been supported by experimental evidence demonstrating the presence of macromolecules Hyperuricosuria can be due to genetic, metabolic, or dietary factors. The disease manifestations commonly present during childhood; however, they remain silent until puberty. It has been shown that one third of the stones are composed of uric acid, an incidence is higher than the incidence of 8% to 10% reported in the general population. Ectopic fat is termed steatosis, and the ill effects of steatosis are termed lipotoxicity,489-494 which is the consequence of the accumulation of toxic metabolites such as acyl coenzyme A (acyl CoA), diacylglycerol, and ceramide. In about 3% of patients with clinical cystinuria, there are no mutations in the two candidate loci. The current belief is that all cases of classic and isolated cystinuria are due to mutations in system b0,+. In contrast, clearance of cationic amino acids is only partly affected (40 to 60 mL/min/1. The prevalence is reported to be highest in individuals of Libyan Jewish descent (1: 2500). A history of parental consanguinity may or may not be present because compound heterozygotes can come from apparently unrelated marriage partners. The features that raise suspicion are family history of cystinuria, staghorn calculi, positive nonquantitative screening test with sodium nitroprusside (>75 mg/L, 0. Poor cystine solubility and precipitation can sometimes lead to misleadingly low results, so alkalinization of collected urine is often required. These problems led to the development of a solid-phase assay, which is reliable in the presence of thiol drugs. These stones are rapidly growing, branch and enlarge, and fill the renal collecting system to form staghorns. The nature of these stones to grow rapidly, recur, and cause morbidity and mortality has led to the term stone cancer. Chronic urinary stasis or infections predispose to struvite stones so that older age, neurogenic bladder, indwelling urinary catheters, and urinary tract anatomic abnormalities are all predisposing factors. Whether a stone will dissolve with prolonged antibiotic is dependent on the amount of carbonate apatite. While many bacteria (gram-negative and gram-positive), Mycoplasma, and yeast species can produce urease, most urease-producing infections are caused by Proteus mirabilis. Colony counts may be low so the laboratory should be instructed to identify any bacteria and determine sensitivities, no matter how low the number of colony-forming units. If routine urinary cultures are negative but a urease producer is suspected, the laboratory should be specifically instructed to culture for Mycobacterium or Ureaplasma urealyticum, which are also urease-positive. Xanthine stones are present in about one third of subjects with classic xanthinuria, which is an inborn error in metabolism inherited as an autosomal recessive trait. Xanthinuria should be suspected if a patient has significant hypouricemia and hypouricosuria in the presence of radiolucent stones. Xanthine stones may also be acquired following allopurinol treatment in patients with significant hyperuricemia such as Lesch-Nyhan syndrome and in those undergoing chemotherapy for myeloproliferative disorders. Acquired causes may be iatrogenic with the use of medications or may be caused by toxins or other diseases. The results showed that those with high exposure had an increased incidence of urolithiasis. The group of children with kidney stones was reported to be significantly younger than those without. Metabolic workups did not disclose any evidence of hypercalciuria, and the stones were radiolucent, indicating that these stones were related to melamine ingestion. The challenges include phenocopy, multiple loci, locus heterogeneity, and lack of an intermediate phenotype in clinical databases.
Discount kemadrin 5mg line
Jamieson A in treatment 2 generic kemadrin 5 mg visa, et al: Clinical, biochemical and genetic features of five extended kindred with glucocorticoid-suppressible hyperaldosteronism. Kotelevtsev Y, et al: Hypertension in mice lacking 11betahydroxysteroid dehydrogenase type 2. Estevez R, et al: Barttin is a Cl- channel beta-subunit crucial for renal Cl- reabsorption and inner ear K+ secretion. Vargas-Poussou R, et al: Functional characterization of a calciumsensing receptor mutation in severe autosomal dominant hypocalcemia with a Bartter-like syndrome. Riccardi D, et al: Localization of the extracellular Ca2+/polyvalent cation-sensing protein in rat kidney. Peters M, et al: Clinical presentation of genetically defined patients with hypokalemic salt-losing tubulopathies. Lu M, Wang W: Two types of K(+) channels are present in the apical membrane of the thick ascending limb of the mouse kidney. Dave S, Honney S, Raymond J, et al: An unusual presentation of cystic fibrosis in an adult. Woywodt A, Herrmann A, Haller H, et al: Severe hypokalaemia: is one reason enough Iida R, Otsuka Y, Matsumoto K, et al: Pseudoaldosteronism due to the concurrent use of two herbal medicines containing glycyrrhizin: interaction of glycyrrhizin with angiotensin-converting enzyme inhibitor. Farese S, et al: Glycyrrhetinic acid food supplementation lowers serum potassium concentration in chronic hemodialysis patients. Pradervand S, et al: Dysfunction of the epithelial sodium channel expressed in the kidney of a mouse model for Liddle syndrome. Hannila-Handelberg T, et al: Common variants of the beta and gamma subunits of the epithelial sodium channel and their relation to plasma renin and aldosterone levels in essential hypertension. Brochard K, et al: Phenotype-genotype correlation in antenatal and neonatal variants of Bartter syndrome. Komhoff M, et al: Cyclooxygenase-2 expression is associated with the renal macula densa of patients with Bartter-like syndrome. Colussi G, et al: A thiazide test for the diagnosis of renal tubular hypokalemic disorders. Loffing J, et al: Thiazide treatment of rats provokes apoptosis in distal tubule cells. Nijenhuis T, et al: Enhanced passive Ca2+ reabsorption and reduced Mg2+ channel abundance explains thiazide-induced hypocalciuria and hypomagnesemia. Panichpisal K, Angulo-Pernett F, Selhi S, et al: Gitelman-like syndrome after cisplatin therapy: a case report and literature review. Dorup I, Clausen T: Correlation between magnesium and potassium contents in muscle: role of Na(+)-K+ pump. Jaeger P, Karlmark B, Giebisch G: Ammonium transport in rat cortical tubule: relationship to potassium metabolism. Parisi A, et al: Complex ventricular arrhythmia induced by overuse of potassium supplementation in a young male football player. Nagasaki A, Takamine W, Takasu N: Severe hyperkalemia associated with "alternative" nutritional cancer therapy. Moreno M, Murphy C, Goldsmith C: Increase in serum potassium resulting from the administration of hypertonic mannitol and other solutions. Hirota K, et al: Two cases of hyperkalemia after administration of hypertonic mannitol during craniotomy. Magnus Nzerue C, Jackson E: Intractable life-threatening hyperkalaemia in a diabetic patient. Sirken G, Raja R, Garces J, et al: Contrast-induced translocational hyponatremia and hyperkalemia in advanced kidney disease. Eiro M, Katoh T, Watanabe T: Use of a proton-pump inhibitor for metabolic disturbances associated with anorexia nervosa. Allon M, Dunlay R, Copkney C: Nebulized albuterol for acute hyperkalemia in patients on hemodialysis. Bellevue R, Dosik H, Spergel G, et al: Pseudohyperkalemia and extreme leukocytosis. Sevastos N, et al: Pseudohyperkalemia in patients with increased cellular components of blood. Sangkabutra T, et al: Impaired K+ regulation contributes to exercise limitation in end-stage renal failure. Yamamoto T, Fukuyama J, Hasegawa K, et al: Isolated corticotropin deficiency in adults. Morimoto S, et al: Selective hypoaldosteronism with hyperreninemia in a diabetic patient. Agmon D, Green J, Platau E, et al: Isolated adrenal mineralocorticoid deficiency due to amyloidosis associated with familial Mediterranean fever. Koren-Michowitz M, et al: Early onset of hyperkalemia in patients treated with low molecular weight heparin: a prospective study. Fischer E, et al: Prolonged zona glomerulosa insufficiency causing hyperkalemia in primary aldosteronism after adrenalectomy. Espinosa G, et al: Adrenal involvement in the antiphospholipid syndrome: clinical and immunologic characteristics of 86 patients. Mayo J, Collazos J, Martinez E, et al: Adrenal function in the human immunodeficiency virus-infected patient. Sebastian A, Schambelan M, Lindenfeld S, et al: Amelioration of metabolic acidosis with fludrocortisone therapy in hyporeninemic hypoaldosteronism. Sebastian A, Schambelan M: Amelioration of type 4 renal tubular acidosis in chronic renal failure with furosemide. Chan R, et al: Renin-aldosterone system can respond to furosemide in patients with hyperkalemic hyporeninism. Elisaf M, Terrovitou C, Tomos P, et al: Severe hyperkalaemia after cotrimoxazole administration in a patient with hyporeninaemic hypoaldosteronism. Antoniou T, et al: Trimethoprim-sulfamethoxazole-induced hyperkalemia in patients receiving inhibitors of the reninangiotensin system: a population-based study. Antoniou T, et al: Trimethoprim-sulfamethoxazole and risk of sudden death among patients taking spironolactone. Fralick M, et al: Co-trimoxazole and sudden death in patients receiving inhibitors of renin-angiotensin system: population based study. Pitt B, et al: Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. Akcay A, Yavuz T, Semiz S, et al: Pseudohypoaldosteronism type 1 and respiratory distress syndrome. Bonny O, et al: Functional expression of a pseudohypoaldosteronism type I mutated epithelial Na+ channel lacking the poreforming region of its alpha subunit. Oishi M, et al: A case of hyperkalemic distal renal tubular acidosis secondary to tacrolimus in living donor liver transplantation. Higgins R, et al: Hyponatraemia and hyperkalaemia are more frequent in renal transplant recipients treated with tacrolimus than with cyclosporin. Pei Y, Richardson R, Greenwood C, et al: Extrarenal effect of cyclosporine A on potassium homeostasis in renal transplant recipients. Muto S, Tsuruoka S, Miyata Y, et al: Effect of trimethoprimsulfamethoxazole on Na and K+ transport properties in the rabbit cortical collecting duct perfused in vitro. Alvestrand A, Wahren J, Smith D, et al: Insulin-mediated potassium uptake is normal in uremic and healthy subjects. De Wolf A, Frenette L, Kang Y, et al: Insulin decreases the serum potassium concentration during the anhepatic stage of liver transplantation. Mandelberg A, et al: Salbutamol metered-dose inhaler with spacer for hyperkalemia: how fast Allon M, Shanklin N: Effect of bicarbonate administration on plasma potassium in dialysis patients: interactions with insulin and albuterol. Furuya R, Kumagai H, Sakao T, et al: Potassium-lowering effect of mineralocorticoid therapy in patients undergoing hemodialysis. Emmett M, et al: Effect of three laxatives and a cation exchange resin on fecal sodium and potassium excretion. Gruy-Kapral C, et al: Effect of single dose resin-cathartic therapy on serum potassium concentration in patients with end-stage renal disease.
Buy kemadrin 5mg cheap
Follow-up data on the study patients were accumulated through late 1998 (median follow-up medicine 257 order 5mg kemadrin with mastercard, 8 years). At last report, 17 patients (7%) were classified as having complete responses and 20 (8%) as having partial responses. Despite publication of promising data by several groups, follow-up trials conducted by the Cytokine Working Group did not confirm the promise of cytokine combination therapy. Most adverse effects, especially the flu-like symptoms, tend to diminish with time during long-term therapy. Later studies have suggested that the antitumor effects of interferon are quite limited. This entire surface may be affected by carcinogenic influences, a characteristic that may help explain the multiplicity in time and place of "urothelial" tumors, which some have termed polychronotropism. Tumors of the upper tract are twice as common in men, generally occur in patients older than 65 years, and are usually unilateral. Long-term exposure to the analgesic phenacetin has been associated with the development of renal pelvic tumors. Although most tumors of the upper tract are transitional cell carcinomas, which account for more than 90% of lesions, squamous carcinomas also occur, usually in the setting of chronic infections with kidney stones. Exfoliative cytologic analysis commonly has positive findings, as in bladder cancers. A positive cytologic result in the presence of a filling defect of the renal pelvis or ureter confirms the diagnosis. Results of retrograde pyelography with brush biopsy of suspicious lesions may also yield the diagnosis of cancer. If there is still uncertainty about the diagnosis after pyelography, including a retrograde evaluation, ureteroscopy may be performed to further evaluate the filling defect or obstruction. Because of the difficult access to some tumors of the upper tract, clinical staging is problematic. Histologic grade of biopsy specimens can be used to predict pathologic stage of disease. Lymphatic metastases usually indicate that more widespread metastatic disease is or will be present. For high-stage and high-grade lesions that have infiltrated into the renal parenchyma, the surgical treatment of choice is nephroureterectomy and removal of a cuff of bladder that encompasses the ipsilateral ureteral orifice. This approach is generally required because of the high likelihood of local recurrence in the bladder at the ureterovesical junction or in the distal ureter. Chemotherapy status was not associated with any significant cancer-specific or overall survival differences. Nevertheless, definitions of regional templates for lymphadenectomy in this disease have been developed. Initial response rates may vary depending on prognostic factors, but long-term survival is poor. Another consideration is neoadjuvant chemotherapy in high-risk/locally advanced disease because of the risk to the patient of renal insufficiency after nephroureterectomy and the resultant inability to receive optimal adjuvant chemotherapy. Fibrosarcomas are the most common and have a poor prognosis as a result of typically late presentation and the presence of locally advanced involvement into the renal vein or metastatic disease at presentation. Other, rarer sarcoma variants that may occur are leiomyosarcoma, rhabdomyosarcoma, osteogenic sarcoma, and liposarcoma. Other genetic abnormalities have suggested the presence of other abnormal chromosomal locations. In contrast to these differentiated structures, undifferentiated or sarcomatoid lesions can also occur and are associated with a worse prognosis. Removal of all gross tumors should be attempted and justifies the radical resection that is often required. All patients receive at least two-drug chemotherapy with dactinomycin and vincristine; those with more advanced disease receive additional doxorubicin, cyclophosphamide, and etoposide with abdominal radiation (1080 Gy) and possibly radiation to the chest (1200 Gy). Specific recommendations regarding the exact protocols to be used are determined by the operative findings, the histologic subtype of the tumor, and whether there was evidence of tumor spillage during the resection. Not only is chemotherapy administered after surgery, but neoadjuvant chemotherapy can diminish the size of the primary tumor and cause regression of metastatic lesions as well as reduce tumors in patients with stage 5 disease (bilateral disease). Before the extensive use of chemotherapy, the survival rate for patients with stage 2 or 3 tumors was less than 45%. Now, cure rates approaching 80% to 90% are routinely achieved; survival rates of 92% to 97% are obtainable in earlier stages of disease. As these excellent results continue to accumulate, treatment programs aimed at lessening treatment duration and minimizing long-term consequences, such as induction of second tumors, continue to be evaluated. Such programs include the more selective use of radiation therapy and a decrease in the duration of chemotherapy. Hematuria, anemia, hypertension, and/or acute severe abdominal pain may also be present. Abdominal ultrasonography is an important diagnostic test to further evaluate the mass and its anatomic extension, which may include inferior or superior extension into the vena cava. Multimodality Treatment High cure rates have been achieved with the concerted effort of multimodality teams performing surgery, radiation therapy, and chemotherapy. Overall survival analysis with a follow-up period in excess of more than 10 years. Rixe O, Billemont B, Izzedine H: Hypertension as a predictive factor of Sunitinib activity. Kondo T, Nakazawa H, Ito F, et al: Impact of the extent of regional lymphadenectomy on the survival of patients with urothelial carcinoma of the upper urinary tract. Halpenny D, Snow A, McNeill G, et al: the radiological diagnosis and treatment of renal angiomyolipoma-current status. Brescia A, Pinto F, Gardi M, et al: Renal hemangiopericytoma: case report and review of the literature. Upreti L, Dev A, Kumar Puri S: Imaging in renal lymphangiectasia: Report of two cases and review of literature. Ozmen M, Deren O, Akata D, et al: Renal lymphangiomatosis during pregnancy: Management with percutaneous drainage. Wadhwa P, Kumar A, Sharma S, et al: Renal lymphangiomatosis: Imaging and management of a rare renal anomaly. Battaglia M, Ditonno P, Mancini V, et al: Long-term follow-up of peripelvic renal multicystic lymphangiectasia. Michal M, Hes O, Bisceglia M, et al: Mixed epithelial and stromal tumors of the kidney. The basic cytological and histopathological elements and their use for diagnostics. Delahunt B: Sarcomatoid renal carcinoma: the final common dedifferentiation pathway of renal epithelial malignancies. Delahunt B: Advances and controversies in grading and staging of renal cell carcinoma. Pignot G, Elie C, Conquy S, et al: Survival analysis of 130 patients with papillary renal cell carcinoma: Prognostic utility of type 1 and type 2 subclassification. Ortmann M, Vierbuchen M, Fischer R: Sialylated glycoconjugates in chromophobe cell renal carcinoma compared with other renal cell tumors. Lornoy W, Becaus S, de Vleeschouwer M, et al: Renal cell carcinoma, a new complication of analgesic nephropathy. Hajj P, Ferlicot S, Massoud W, et al: Prevalence of renal cell carcinoma in patients with autosomal dominant polycystic kidney disease and chronic renal failure. Zbar B, Brauch H, Talmadge C, et al: Loss of alleles of loci on the short arm of chromosome 3 in renal cell carcinoma. Heimann P, El Housni H, Ogur G, et al: Fusion of a novel gene, rcc17, to the tfe3 gene in t(x;17)(p11. Bruder E, Passera O, Harms D, et al: Morphologic and molecular characterization of renal cell carcinoma in children and young adults. Latif F, Tory K, Gnarra J, et al: Identification of the Von HippelLindau disease tumor suppressor gene.