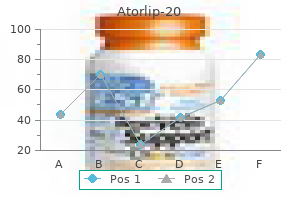
Generic atorlip-20 20 mg fast delivery
Galati and colleagues (2008) reported 23 children with urachal remnants cholesterol ratio score buy discount atorlip-20 20mg line, of which 10 underwent excision because of symptomatic problems. In their treatment protocol, asymptomatic remnants are managed with physical and sonographic examination. They found that spontaneous resolution with nonoperative management is likely with remnants in patients younger than 6 months. However, if symptoms persist or the remnant fails to resolve after age 6 months, they recommend excision. Vesicourachal diverticulum (3% to 5%) Patent Urachus Patent urachus is explained by nondescent of the bladder or, more commonly, failure of the epithelial-lined urachal canal to obliterate (Gearhart, 2002). Bladder obstruction during fetal development has been blamed for the urachus remaining tubular. The fact that urachal patency is often absent with severely obstructed bladders in utero, however, casts doubt on this theory. Additionally, only up to 14% of patients with a patent urachus have postnatal confirmation of in utero bladder obstruction (Schrenck and Campbell, 1972; Mesrobian et al, 1997). It seems possible that obliteration of the urachus may be independent from the level of bladder distention. Therefore retubularization, rather than primary patency, might be the cause for urinary drainage from the umbilicus. Chapter138 BladderAnomaliesinChildren 3177 Patent urachus would manifest as a Meckel diverticulum connected to the umbilicus. These structures can be very difficult to differentiate from an umbilical-urachus sinus because no connection to the bladder or bowel can be seen on sinugram. However, the surgical approach to both anomalies requires the complete excision of all tissue. Unlike urachal structures, omphalomesenteric remnants can show gastric or small bowel mucosa on histologic examination. However, the fluid-filled cyst can drain through the umbilicus or into the bladder intermittently. Urachal cysts are found more commonly in the distal part of the urachus and manifest more commonly in adults than in infants or children (Cilento et al, 1998). These cells can become infected; Staphylococcus aureus has been identified as the most common organism (Mesrobian et al, 1997). Once infected, urachal cysts can manifest as umbilical abscess formation or bladder infections. Additional symptoms include localized lower abdominal pain, voiding symptoms, or even a painful and palpable mass. The diagnosis is confirmed by ultrasound, demonstrating the localized cyst between the anterior abdominal wall and the peritoneum. If unrecognized, the infected cyst can perforate into the bladder (Maruschke et al, 2003) or peritoneal cavity. This can cause peritonitis and formation of an enteric fistula (Ohgaki et al, 2003; Quek et al, 2003). Treatment consists of draining the infected cyst, followed by complete excision of the urachal remnant structures. The rectus fascia is incised in a longitudinal fashion, muscles spread apart, and the dome of the distended bladder identified. The dissection continues extraperitoneally toward the umbilicus until the previously incised umbilical portion is free and can be pulled into the surgical field. A bladder cuff including the urachal insertion is marked and excised using electrocautery. This can be done even in children younger than 6 months of age (Fahlenkamp et al, 1995; Cadeddu et al, 2000; Khurana and Borzi, 2002). Khurana and Borzi (2002) described their laparoscopic experience with 4 children between 5 months and 10 years and found the procedure to be safe in children of all ages. Technically, they suggested a three-port approach, with the camera port in the midline between the umbilicus and the xiphoid and two working ports on either side in the upper quadrant. Early in their series they inserted the camera port at the umbilicus with working ports into the right and left upper abdomen. Later they preferred to place the camera into the left lower abdominal wall, with 2-mm working ports at the left lower and upper abdomen for better visualization of the urachus at the umbilicus. They reported no intraoperative or postoperative complications, no recurrences, and a median operating time of 35 minutes. The advantage of the laparoscopic technique is the good visualization of the course of the urachus and the bladder dome. However, the laparoscopic techniques require an intra-abdominal approach and pose the potential risk for spilling infected or malignant material into the abdominal cavity. Vesicourachal Diverticulum the urachus obliterates almost completely, except at the level of bladder apex. These lesions are usually nonsymptomatic and found incidentally on nonrelated radiographic workups. Although the diverticulum can enlarge in the case of urinary obstruction, this rarely causes problems because they tend to have a large opening and drain into the bladder well. Stone formation and urinary tract infections have been reported, especially in the case of a narrowed neck causing the need for intervention. Conservative treatment with observation is justified in asymptomatic cases because of possible spontaneous resolution. BladderDiverticulum Bladder diverticula are caused by infravesical obstruction, iatrogenic after bladder surgery, or as a congenital defect. Independent from the cause, all diverticula develop as herniation of bladder mucosa between defects of bladder smooth muscle fibers. The neck of the resulting diverticulum depends on the size of the muscular defect. In adult males the incidence tends to be much higher because of the higher occurrence of infravesical obstruction. The Umbilical-Urachus Sinus In the umbilical-urachus sinus, the urachus obliterates at the bladder level but remains open at the umbilical site, causing a continuously draining sinus. The caudal part of the urachus is filled with desquamated epithelial cells, and no connection to the bladder can be identified. Primary diverticula arise as a localized herniation of bladder mucosa through the ureteral hiatus between the intravesical ureter and the roof of the ureteral hiatus. These primary diverticula are also known as congenital diverticula and are most likely caused by a congenitally deficient bladder wall. Some authors have implied an isolated defect in the Waldeyer sheet; however, congenital diverticula often occur on one side only and a unilateral defect seems unlikely (Stephens, 1963). Congenital diverticula are often found in children with generalized connective tissue diseases such as Ehlers-Danlos, Williams elfin-facies, or Menkes syndrome (Babbitt et al, 1979; Daly and Rabinovitch, 1981; Levard et al, 1989). These diverticula can be resected if symptomatic; however, because of the impaired healing in patients with connective tissue disease, recurrence and wound healing complications are more common. Secondary paraureteral diverticula are acquired and develop as a result of existing infravesical obstruction. The resulting increased infravesical pressure forces the bladder mucosa to bulge between the muscle fibers. These diverticula are usually just one of many pop-off mechanisms that can occur throughout the bladder. These diverticula also can be caused by weakening in the bladder muscle by infection (Barrett et al, 1976) or development of a muscular defect after bladder surgery (Sheu et al, 1998). In both types of paraureteral diverticula, the Waldeyer sheet eventually becomes damaged as the diverticulum expands in size. The increasing diverticulum pulls the intravesical ureter out of its anchored position, causing dysfunction of the ureterovesical junction. Eventually, the enlarged diverticulum can become responsible for ureteral obstruction.
Buy atorlip-20 online
Revision rates range between 7% and 18% cholesterol ratio 2.7 buy atorlip-20 20mg without a prescription, secondary to lead migration, faulty connection, and infection. These agents act by reducing the frequency and intensity of uninhibited detrusor contractions during the filling phase of the bladder, resulting in an increase in the functional bladder capacity and compliance. Typically, moderate-tolarge amounts of urinary leakage are triggered by laughing alone. It should be emphasized that the incontinence episodes are invariably significant and often the entire bladder volume is drained. Giggle incontinence has a significant adverse effect on the social life, and this is often why medical assistance is sought. Underactive Bladder As the name suggests, underactive bladder describes a child who is required to raise intra-abdominal pressure to initiate, maintain, and complete voiding. Obviously, this requires appropriate counseling and thoughtful guidance of both patient and caregiver, especially in the child who is neurologically intact. Pollakiuria (Extraordinary Daytime Urinary Frequency) this is a disorder characterized by a very high daytime frequency of micturition (sometimes as high as 50 times per day). It is commonly seen in prepubertal girls, and the typical history is that of wetting of undergarments approximately 10 to 15 minutes after a normal void. Reassurance and postural modification to ensure complete vaginal emptying is the only treatment required. In fact, most experts in the field would estimate the proportion of children with enuresis that are truly monosymptomatic to represent fewer than half of all bedwetting children (Franco et al, 2013). Obviously one begins with a thorough history and physical examination, along with the appropriate laboratory and imaging studies. If comorbid behavioral disorders are present, these should be addressed by an appropriate provider. EpidemiologyandNaturalHistory Enuresis is a common problem, with an estimated 7 million children in the United States alone with this condition. According to a recent large longitudinal study in the United Kingdom, at least 20% of children in the first grade occasionally wet the bed and 4% wet the bed two or more times per week (Butler and Heron, 2008). In a study of almost 11,000 children in the United States, the prevalence of enuresis in boys at 7 and 10 years of age was 9% and 7%, respectively, and in girls at those ages, 6% and 3%, respectively (Byrd et al, 1996). It is currently generally accepted that in the West approximately 15% of children will have some degree of nighttime wetting at 5 years of age, with a spontaneous resolution rate of approximately 15% per year (Forsythe and Redmond, 1974). Consequently, at 15 years of age only 1% to 2% of teenagers will still wet the bed (Klackenberg, 1981). It has also been shown that the longer the enuresis persists, the lower the probability is that it will resolve spontaneously (Forsythe and Redmond, 1974; Bakker et al, 2002). Enuresis seems to be more common in boys than in girls, with most reports revealing a 2: 1 ratio. Genetics Enuresis has a complex and multifactorial pathophysiology with a strong genetic underpinning (von Gontard et al, 1998a; Schaumburg et al, 2008). When one or both parents have a history of prolonged nighttime wetting, approximately 43% and 77%, respectively, of the offspring are affected (Bakwin, 1973). When neither parent has a history of nocturnal enuresis, only 15% of offspring are affected (Bakwin, 1973). Linkage of enuresis to markers on chromosomes 12, 13, and 22 has been reported, with autosomal dominant inheritance and high penetrance suggested; however, a major gene locus has yet to be identified (Eiberg et al, 1995, Eiberg 1998; Arnell et al,1997). Family and twin studies suggest locus heterogeneity and poor phenotype-genotype correlation (von Gontard et al, 2011b). The identification of these genes certainly lifts the burden of guilt from children who have enuresis and helps to dispel the theory that enuresis is behavioral in origin and completely under their control. In children and adolescents without enuresis, the diurnal pattern of urine production results in a relative reduction in nocturnal diuresis to approximately 50% of daytime levels (Rittig et al, 1995, 2010). This contention is rooted in the fact that most children eventually attain nocturnal dryness regardless of what intervention is used and even if enuresis is left untreated. Put very simply, the three organ systems implicated in the pathogenesis of enuresis include the bladder. Yeung and associates found that nearly half of treatment failures with standard therapy. In addition, urodynamic Arousal and Sleep Regardless of whether the child has detrusor overactivity and/or nocturnal polyuria, neither observation explains why a child with enuresis is unable to awaken from sleep to void before a wetting episode. Given that both bladder distention and detrusor contractions are robust arousal stimuli (Koyama et al, 1998), it is curious that an enuretic child will not wake up during the night to the sensation of a full or contracting bladder. This situation is often experienced by family members of patients exposed to alarm therapy as parents awaken from sleep while their enurectic child will sleep through the alarm. This was illustrated by a study in which bladder capacity was measured in the awake state as well as under general anesthesia in children with enuresis and compared with functional bladder capacity among controls (Troup et al, 1971). Compared with control children, the average volume of urine voided by enuretic children in the awake state was reduced. Whether this situation is a result of reduced nocturnal functional bladder capacity or nocturnal detrusor overactivity, however, may not be critical because the treatment strategy employed would largely be the same. Given the self-limiting nature of enuresis, one treatment option is to observe and allow the natural history to follow its predetermined course. The decision about when to start treatment generally should be guided by the degree of concern and motivation on the part of the child rather than the parents. For the child, nocturnal enuresis usually becomes significant when it interferes with his or her ability to socialize with peers. Treatment probably should be delayed if it seems that the parents are more interested in treatment than the child and the child is unwilling or unable to assume some responsibility for the treatment program. One important point to ask about is the presence of nocturia; this would suggest that the child is not extremely difficult to arouse from sleep. The fundamental goal of behavioral therapy is much like the treatment of daytime urinary incontinence and centers around the practice of good bladder and bowel habits. Highsugar and caffeine-based drinks should be avoided, particularly in the evening hours. Isolated nighttime fluid restriction, without compensatory increase in daytime fluid consumption, may prevent the child from meeting his or her daily fluid requirement and is usually unsuccessful. An individualized program with a series of realistic goals between appointments and monthly follow-up to sustain motivation improves the outcome (Glazener and Evans, 2004). Children in whom one first-line treatment has failed should be offered the other, and for those in whom both have failed, second- and third-line treatments can be tried, either alone or in combination. The response is more gradual and sustained than for desmopressin, with approximately two thirds of children becoming dry during active treatment and nearly half remaining dry after treatment completion (Glazener et al, 2005). After the alarm goes off, only the child should turn off the alarm, get up, and finish voiding in the toilet. We often remind parents that at the initiation of therapy, the child may fail to awaken and that parents should wake the child when the alarm sounds. The child being fully awake and cognizant of what is happening is critical to the success of alarm therapy. Adverse effects of alarms include alarm failure, false alarms, disruption of the lives of other family members, and lack of adherence because of difficulty using the alarm (Glazener et al, 2005). Children who do not continue to improve after 6 weeks of alarm training are unlikely to become completely dry with this technique (Taylor and Turner, 1975), and alternative interventions may be warranted. Children who relapse after discontinuation of the alarm usually can achieve a rapid secondary response because of preconditioning as a result of the first treatment program (Tuncel et al, 2008). It is available in the United States in oral (crushable) tablets and in sublingual and intranasal spray formulations.
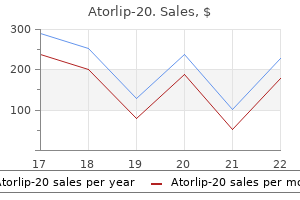
Buy atorlip-20 australia
Vesicoureteral reflux in infants with prenatal hydronephrosis confirmed at birth: racial differences cholesterol lowering food brands order atorlip-20 20mg otc. Impact of early screening for reflux in siblings on the detection of renal damage. Ibuprofen combined with antibiotics suppresses renal scarring due to ascending pyelonephritis in rats. New contralateral vesicoureteral reflux after unilateral ureteral reimplantation: predictive factors and clinical outcomes. Pyelonephritic scarring in 213 patients with upper and lower urinary tract infections: long-term followup. Renal cortical abnormalities in siblings of index patients with vesicoureteral reflux. Resolution of vesicoureteral reflux in completely duplicated systems: fact or fiction Vesicoscopic ureteral reimplantation: a minimally invasive technique for the definitive repair of vesicoureteral reflux. Lack of major involvement of human uroplakin genes in vesicoureteral reflux: implications for disease heterogeneity. The pelvic plexus and antireflux surgery: topographical findings and clinical consequences. The evolution of vesicoureteral reflux management in the era of dextranomer/hyaluronic acid copolymer: a Pediatric Health Information System database study. Local tissue reaction to the subureteral injection of glutaraldehyde cross-linked bovine collagen in humans. Endoscopic injection of glutaraldehyde cross-linked bovine dermal collagen for correction of vesicoureteral reflux. Outcome of antibiotic prophylaxis cessation in patients with persistent vesico-ureteral reflux who initially presented with a febrile urinary tract infection. Acute pyelonephritis and sequelae of renal scar in pediatric first febrile urinary tract infection. Renin-angiotensin system polymorphisms in Taiwanese primary vesicoureteral reflux. Virulence-associated traits in Escherichia coli causing first and recurrent episodes of urinary tract infection in children with or without vesicoureteral reflux. Development of Macroplastique bolus calcification detected during long term follow-up after injection for vesico-ureteral reflux. The management of children with vesicoureteral reflux and ureteropelvic junction obstruction. Relationship among vesicoureteral reflux, P-fimbriated Escherichia coli, and acute pyelonephritis in children with febrile urinary tract infection. Polytef (Teflon) migration after periurethral injection: tracer and x-ray microanalysis techniques in experimental study. Migration and granulomatous reaction after periurethral injection of polytef (Teflon). Society of Nuclear Medicine procedure guideline for renal cortical scintigraphy in children, version 3. Complications of pregnancy after childhood reimplantation for vesicoureteral reflux: an update with 25 years of followup. Increased renal echogenicity: a sonographic sign for differentiating between obstructive and nonobstructive etiologies of in utero bladder distention. Adverse reactions of nitrofurantoin, trimethoprim and sulfamethoxazole in children. Prospective long-term analysis of nerve-sparing extravesical robotic-assisted laparoscopic ureteral reimplantation. Clinical and radiographic results of endoscopic injection for vesicoureteral reflux: defining measures of success. Computational model for predicting the chance of early resolution in children with vesicoureteral reflux. The cost-effectiveness of endoscopic injection of dextranomer/hyaluronic acid copolymer for vesicoureteral reflux. Vesicoureteral reflux diagnosed in adulthood: incidence of urinary tract infections, hypertension, proteinuria, back pain and renal calculi. Newly diagnosed contralateral reflux after successful unilateral endoscopic correction: is it due to the pop-off mechanism Long-term followup of children treated with dextranomer/hyaluronic acid copolymer for vesicoureteral reflux. Angiotensin converting enzyme inhibitors and reflux nephropathy: 2-year follow-up. Reflux nephropathy and hypertension: correlation with the progression of renal damage. Retrograde catheterization of the ureter after antireflux plasty by the Cohen technique of transverse advancement. Vesicoureteral reflux after ureteroneocystostomy: indications for postoperative voiding cystography. Extravesical ureteral reimplantations for the correction of primary reflux can be done as outpatient procedures. Severe vesicoureteral reflux and chronic renal failure: a condition peculiar to male gender Pregnancies in women with and without renal scarring after urinary infections in childhood. Postoperative hospitalization of children undergoing cross-trigonal ureteroneocystostomy. Outcome of pregnancy in an Oxford-Cardiff cohort of women with previous bacteriuria. Endoscopic treatment of vesicoureteral reflux with Coaptite: the first 50 patients. Normal and abnormal development of the ureter in the human embryo: a mechanistic consideration. What is the fate of the refluxing contralateral kidney in children with multicystic dysplastic kidney Incidence of contralateral vesicoureteral reflux following unilateral extravesical detrusorrhaphy (ureteroneocystostomy). Expanded polytetrafluoroethylene patch in hernia repair: a review of clinical experience. Is it reasonable to observe patients with persistent vesico-ureteral reflux after failed first endoscopic injection Embryology and genetics of primary vesicoureteric reflux and associated renal dysplasia. Clinical characteristics of primary vesicoureteral reflux in infants: multicenter retrospective study in Japan. A comparison of calcium hydroxyapatite and dextranomer/hyaluronic acid for the endoscopic treatment of vesicoureteral reflux. Color flow Doppler sonography: a reliable alternative to voiding cystourethrogram in the diagnosis of vesicoureteral reflux in children. A comparative study of endoscopic trigonoplasty for vesicoureteral reflux in children and in adults. Features of primary vesicoureteric reflux detected by investigation of foetal hydronephrosis. Constipation: a cause of enuresis, urinary tract infection and vesico-ureteral reflux in children. Extracellular matrix degradation and reduced nerve supply in refluxing ureteral endings. Resistive index in febrile urinary tract infections: predictive value of renal outcome. Enhanced detection of vesicoureteral reflux in infants and children with use of cyclic voiding cystourethrography. Cyclic voiding cystourethrography: is vesicoureteral reflux missed with standard voiding cystourethrography Vesicoureteral reflux associated renal damage: congenital reflux nephropathy and acquired renal scarring. Vesicoureteral reflux in infants with isolated antenatal hydronephrosis [comment]. Renal scarring following reflux and nonreflux pyelonephritis in children: evaluation with 99m technetiumdimercaptosuccinic acid scintigraphy. Ascending renal infections: with special reference to the reflux of urine from the bladder into the ureters as an etiological factor in its causation and maintenance. Febrile urinary tract infections in children with an early negative voiding cystourethrogram after treatment of vesicoureteral reflux with dextranomer/hyaluronic acid.
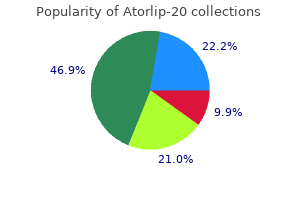
Buy atorlip-20 20 mg
Most surgeons now preserve the native bladder as long as it is widely opened to prevent a narrow-mouthed anastomosis cholesterol test vhi buy generic atorlip-20 20 mg, which can result in the augmentation segment behaving as a diverticulum. The incision is carried from a point several centimeters cephalad to the bladder neck anteriorly to a position just above the trigone posteriorly. Such an incision allows a technically easier anastomosis to the bowel segment and leaves the native bladder to add to the overall capacity. A greater circumference for the anastomosis can be provided if need be, by opening the bladder in a stellate fashion with a second transverse incision into the two bladder halves. There have been reports of penile or perineal pain Ileocystoplasty Goodwin and associates (1959) were among the first to demonstrate the numerous ways to anastomose a patch of ileum to the native bladder after the ileum was detubularized and reconfigured to achieve the most spheric shape possible. A 20- to 40-cm segment of ileum at least 15cm from the ileocecal valve is removed and opened on its antimesenteric border. Technique A segment of ileum at least 15 to 20 cm proximal to the ileocecal valve should be selected. The isolated segment should be 20 to 40 cm in length depending on patient size, native bladder capacity, and the desired final capacity. This would require creation of an ileal nipple valve to prevent reflux as in the Kock or hemi-Kock pouch; this type of construction may require up to 60 cm of small intestine. The segment to be used should have an adequate mesentery to reach the native bladder without tension. After selection of the appropriate segment, the mesentery is cleared from the bowel at either end for a short distance to create a window. The bowel is divided at those ends, and a hand-sewn ileoileostomy or stapled anastomosis is performed. The mesenteric window at the bowel anastomosis is closed to prevent an internal hernia. The suture line should approximate the full thickness of ileum to ileum while inverting the mucosa. The anastomosis of the ileum to native bladder is easily done when started posteriorly. The anastomosis may be done in a one- or two-layer fashion, always using absorbable suture and inverting the mucosa to the lumen. Permanent sutures should never be used for any cystoplasty because they serve as a nidus for stone formation. A suprapubic tube is brought through the native bladder when possible and secured. A drain is placed near the bladder and brought out of the pelvis through a separate stab incision. It should be removed promptly if not draining urine, particularly in neurogenic patients with a ventriculoperitoneal shunt. The appendix may be removed with a small cuff of cecal wall and tunneled into the native bladder or a tenia of the cecal segment to provide a continence mechanism. If the appendix is not to be used, an appendectomy is performed with standard ileocecocystoplasty. Presently, cecocystoplasty is an uncommon operative procedure and will not be discussed because it has largely been replaced by various forms of ileocecocystoplasty. With this technique, the cecum is opened, reconfigured, and used to augment the bladder alone, leaving a segment of ileum to reach the ureters or create a continent abdominal wall stoma. Conversely, the ileal segment can be opened and used as a patch on the cecal segment before augmentation cystoplasty. Ileocecal Valve the ileocecal segment has been used extensively in the adult population undergoing reconstruction and bladder replacement. It has been used less frequently in children because the majority of patients undergoing augmentation cystoplasty do so for neurogenic dysfunction affecting both bladder and bowel. Removal of the ileocecal valve in such children can result in intractable diarrhea (Gonzalez and Cabral, 1987; King, 1987). Antireflux tunnels can easily be performed into the tenia of the cecum when necessary. Again for the short ureter, a tail of ileum can be left intact to bridge the gap and the imbricated ileocecal valve used for antireflux. The same imbrication technique can be used to create a continent abdominal wall stoma similar to that used in the Indiana Pouch (Cain and Husmann, 1994; Cain et al, 1999). Technique Many modifications of the technique exist, but all start with mobilization of the cecum and right colon by incising the peritoneum along the white line of Toldt up to the hepatic flexure. As with all intestinal cystoplasties, before division of the bowel segment, it should be noted that it will reach the bladder without tension. In the typical ileocecal augmentation, the ileal and cecal segments are of equivalent length such that the borders of the open segment can be anastomosed and then folded on themselves to form a cup cystoplasty. The anastomosis of the reconfigured segments is done in either a one- or two-layer closure with absorbable suture. The opening should be left large enough to provide a wide anastomosis to the bivalved bladder. If more volume is necessary, the ileal segment can be significantly longer, allowing it to be folded before anastomosis to the cecum. The Mainz ileocecocystoplasty uses an ileal segment twice the length of the cecal segment. The mesenteric window is closed, and a suprapubic tube is placed through the native bladder and secured through the abdominal wall. SigmoidCystoplasty Use of the sigmoid colon for augmentation cystoplasty was first reported by Lemoine in 1912 (Charghi et al, 1967), and it continues to be used commonly. Because of the strong unit contractions of the sigmoid, it is imperative to detubularize and reconfigure the segment to provide maximal compliance and disruption of contractions. After identification of this blood supply, the surgeon must ensure that the segment can reach the bladder without tension. The remainder of the abdominal cavity Appendix One potential advantage of ileocecocystoplasty is the presence of the appendix. The segment easily fits on the bivalved bladder in either the sagittal or coronal plane. A slightly longer segment of sigmoid may be necessary for effective reconfiguration in this manner. A B Gastrocystoplasty Two basic techniques exist for use of stomach in bladder augmentation. With their technique, the left gastroepiploic artery is always used as a vascular pedicle. If the right gastroepiploic artery is dominant and the left vessel ends high of the greater curvature, a strip of body along the greater curvature from the left gastroepiploic artery to the antrum is maintained and provides adequate blood supply (Leong, 1988). Continuity of the upper gastrointestinal tract is restored with a Billroth I gastroduodenostomy. Technique Using Body A gastric wedge based on the midportion of the greater curvature may be used (Adams et al, 1988). The gastric segment used in this technique is made up mainly of body and consequently has a higher concentration of acid-producing cells. The wedge-shaped segment of stomach includes both the anterior and posterior wall. The segment used may be 10 to 20 cm along the greater curvature depending on patient age and size as well as the needed volume. The incision into the stomach is stopped just short of the lesser curvature to avoid injury to branches of the vagus nerve controlling the gastric outlet. Branches of the left gastric artery just cephalad to the apex of this incision are suture ligated in situ before incision to avoid significant bleeding. Branches of the gastroepiploic artery to the antrum on the right or to the high corpus on the left are divided to provide mobilization of the gastroepiploic pedicle. In order that the eventual pedicle is long enough to reach the bladder, the appropriate segment may be higher on the greater curvature if the right vessel is used as a pedicle or lower if based on the left. The segment and pedicle may be passed through windows in the transverse mesocolon and mesentery of the distal ileum and carefully secured to the posterior peritoneum. Despite consideration for an adequate pedicle length, on occasion the gastric segment initially may not reach the bladder without tension.
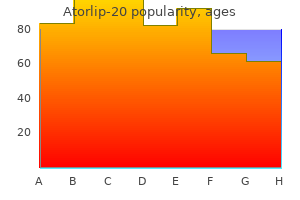
Order atorlip-20 20mg mastercard
The original modification described by Zaontz and colleagues (1987) for the extravesical procedure included incision of the detrusor distal to the ureteric orifice for 5 to 10 mm with advancement of the ureter using two vest sutures cholesterol values normal order atorlip-20 australia. Leissner and colleagues (2001) demonstrated that this particular aspect of the procedure may be responsible for injury to the bladder innervation at the trigonal area and may be the lead cause of urinary retention in bilateral extravesical reimplants. Therefore, to avoid damage to the nerves, this maneuver should be avoided unless there is a paraureteral diverticulum that requires repair simultaneously (Jayanthi et al, 1995). In those cases, dissection of the detrusor distal to the ureter should be carried out in a limited fashion. Once creation of the submucosal tunnel is complete, the bladder is decompressed before reapproximation of the detrusor. The ureter is positioned in the new tunnel, and the detrusor reapproximated using interrupted 3-0 polyglactin sutures. To achieve alignment of the tunnel, it is best to place the most proximal suture first at the new ureteral hiatus and to leave it untied and tagged on a mosquito snap. Tension applied to this suture straightens and elevates the detrusor flaps, allowing the surgeon to reapproximate the detrusor without risk for injury to the ureter or the mucosa. The adventitia of the ureter may be incorporated in one or two of these sutures to stabilize the tunnel and prevent a diverticulum from forming at the most distal or proximal portion of it. At the completion of the suture line, the caliber of the hiatus should be tested with a right-angle clamp to ensure absence of any constriction or compression of the ureter. The course of the ureter is reinspected to ensure absence of any kinks in the retroperitoneum or any bulging of the mucosa at either end of the tunnel. A Foley catheter is left for 24 to 48 hours; some authors recommended not leaving a catheter at all (Marotte and Smith, 2001). If an epidural caudal catheter is inserted for postoperative analgesia, it should be discontinued 6 to 12 hours before removal of the Foley catheter. Chapter137 VesicoureteralReflux 3165 2001), the success rate with uncomplicated ureteroneocystostomy approaches 100% (Bisignani and Decter, 1997; Bomalaski et al, 1997b; El-Ghoneimi et al, 1999; Barrieras et al, 2000; Grossklaus et al, 2001). This recommendation should be individualized on the basis of the family situation and the expertise of the center performing the surgery. Some families have followed reflux for several years and are anxious to know with certainty that the reflux has resolved. However, the lower success rate for high-grade reflux would still support complete postoperative studies in most cases. After ureteroneocystostomy, the presence of minimal ureteral dilation and low-grade hydronephrosis on early postoperative ultrasonography is not unusual (Bomalaski et al, 1997b; Barrieras et al, 2000). Indeed, this common finding should argue against performing such studies too early after surgery. On the other hand, persistence of this dilation beyond 3 months or its progression should be further investigated (Aboutaleb et al, 2003). As discussed previously, children with renal scarring should have their blood pressure measured at every visit with their family physician. In the report by Barrieras and colleagues (2000), 49 of 723 renal units had reflux at 3 months, 11 of which were contralateral. Persistent reflux at 1 year was more common in patients who had highgrade reflux preoperatively. Two thirds of those with persistent reflux at 1 year (12 of 18) were from that group. Contralateral Reflux the issue of contralateral reflux has been the subject of several reports in the literature over the past 15 years, most of which are retrospective (Hubert et al, 2014). Minevich and colleagues (1998b) and Burno and colleagues (1998) noted a low incidence of contralateral reflux after unilateral extravesical detrusorrhaphy in 5. These patients were analyzed according to grade of initial reflux, presence of a Hutch diverticulum or duplex system, and the surgical technique employed to correct the reflux. No difference was noted among the various surgical techniques, but there was a significant trend toward development of contralateral reflux with the higher grades of ipsilateral corrected reflux and correction of reflux in duplex systems. They concluded that the distortion of the contralateral hemitrigone was not a responsible factor for contralateral reflux but rather the severity (grade 5) of reflux, and the presence of a duplex system put patients at risk for development of contralateral reflux postoperatively. As a result of these outstanding outcomes, several centers have evaluated the need for postoperative invasive imaging. In a large study by Barrieras and colleagues (2000), 723 renal units were evaluated. They refuted the existence of the pop-off mechanism accounting for new contralateral reflux in their series because the risk for new contralateral reflux did not correlate with the preoperative reflux grade (grades 4 and 5). Sparr and colleagues (1998) reviewed a series of 143 patients on conservative management and initially diagnosed with unilateral reflux but subsequently developed metachronous contralateral reflux. Contralateral reflux appeared in 33%, suggesting a different cause for the appearance of contralateral reflux unrelated to surgical correction. Prophylactic bilateral reimplantation for unilateral reflux, to avoid contralateral reflux, is not warranted on the basis of the high spontaneous resolution rates (Burno et al, 1998). Recommendations for management of contralateral reflux range from observation in the majority of cases to intervention for control of clinical pyelonephritis episodes. In asymptomatic children, younger than 4 to 5 years of age, prophylactic antibiotics are warranted for postoperative contralateral reflux, particularly if one is to be consistent with the medical therapy for the previous ipsilateral reflux. In a recent report by Hubert and colleagues (2014) from Boston, new contralateral reflux was observed in 10% of the children (18% grade 1, 70% grade 2, and 12% grade 3). Younger age (<6 years) and low observed bladder capacity (<50% of predicted capacity) were significant predictors of contralateral reflux on multivariable analysis. Follow-up cystography documented resolution of contralateral reflux in almost 80% at a median of 21. Suprahiatal Twists of the ureter and ischemia result from poor handling of the ureter and are the most common causes of suprahiatal obstruction. Hiatus At the point of entry into the new hiatus, angulation of the ureter occurs, most commonly as a result of a hiatus that is positioned too lateral or anterior such that when the bladder fills, the ureter becomes carried laterally and anteriorly, resulting in the "high reimplant" phenomenon. This situation may resolve spontaneously but on occasion requires stenting or repeat surgery. Tunnel A submucosal tunnel that is not adequately developed can lead to compression of the ureter causing obstruction within the tunnel. The submucosal tunnel is obviously more difficult to develop in an abnormal bladder such as the valve or neuropathic bladder. Developing a smooth, capacious, submucosal tunnel can be quite challenging because of the irregularities created by the muscular hypertrophy, trabeculation, and cellule formation. Ischemia to the ureter and the submucosal tunnel is another important factor that results from improper handling of the ureter, leading to its devascularization. Significant obstruction in the submucosal tunnel can be overcome by balloon dilation and stenting for a time. Orifice the anastomosis of the ureter to the bladder and the new hiatal position is an important technical aspect of the reimplant procedure. The most vulnerable point for obstruction is the apex of the ureteral spatulation. The apical sutures must be placed with the utmost care to ensure an adequate orifice caliber. If the submucosal tunnel is of adequate length, endoscopic unroofing of the distal few millimeters, including the orifice, may relieve the obstruction while maintaining the antireflux mechanism. Obstruction It is not unusual to detect a mild-to-moderate degree of hydronephrosis in the early postoperative period by ultrasonography (see earlier discussion). Acute postoperative obstruction may be related to technical issues such as twisting or kinking of the ureter in its new tunnel, intramural blood clots, or extramural compression by submucosal hematoma or edema at the site of anastomosis. Progressive, significant obstructions usually become apparent in the first 2 weeks after surgery. The children typically present with symptoms of acute ureteral obstruction, including acute abdominal pain, nausea, and vomiting. Although infection is less common, if it occurs it is quite significant in the obstructed system. The diagnosis is readily made on ultrasonography, and the severe hydroureteronephrosis is confirmed by delayed function and excretion on renal scintigraphy. In the more significant cases, drainage of the system either by retrograde insertion of a double-J stent or a percutaneous nephrostomy tube may be necessary.
Indian Head (Echinacea). Atorlip-20.
- Preventing vaginal yeast infections when used with a medicated cream called econazole (Spectazole).
- Are there safety concerns?
- What is Echinacea?
- What other names is Echinacea known by?
- Is Echinacea effective?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96942
Order atorlip-20 online now
Until 16 weeks of gestation definition of cholesterol in nutrition cheap 20 mg atorlip-20 visa, the amniotic fluid is mainly consistent with placental transudate, at which time it changes to predominantly fetal urine (Takeuchi et al, 1994). The umbilical cord should contain two arteries and one vein without evidence of a fluid-filled urachus (Bronsthein et al, 1990). It is difficult to classify bladder anomalies because of the large variety of possible malformations, the relatively low incidence of the anomalies, and the common association with other congenital anomalies. The pubic bones mark the anterior border and the rectosigmoid the posterior border. If the bladder is dilated, the condition can be due to obstruction or caused by incomplete emptying of the bladder without evidence of a mechanical obstruction. Dilated Fetal Bladder In the first trimester, the fetal bladder is considered dilated if larger than 7 mm on ultrasound. If, on subsequent ultrasounds, the bladder continues to retain urine and shows no evidence of urine cycling, concern regarding obstruction should be raised. If the amniotic fluid does not increase, this may indicate the progression to oligohydramnios. Determination of the sex of the child is very important because of the male gender predominance of certain conditions and diseases such as posterior urethral valves or prune belly syndrome. It can be difficult to distinguish in utero if the dilation is due to obstruction. In a retrospective study, Kaefer and coworkers (1997) described 15 patients with marked bladder dilation in utero, 8 with and 7 without obstruction. All of the patients with obstruction presented with moderate-to-severe oligohydramnios and a marked increase in renal echogenicity, whereas all but one of the nonobstructed bladders had normal amniotic fluid levels and regular renal echogenicity. Therefore fetuses with nonobstructive dilation appear to pass enough urine to maintain renal function and adequate amniotic fluid levels throughout the pregnancy (Mandell et al, 1992). Dilation Caused by Obstruction Urethral Anomalies and External Bladder Outlet Obstruction. Dilations of the fetal bladder caused by anatomic obstructions are mostly due to urethral anomalies or external obstruction. Urethral anomalies include congenital urethral strictures, anterior and posterior urethral valves, and urethral atresia. Compression of the bladder outlet region can be due to obstructing syringoceles, a sacrococcygeal teratoma or pelvic neuroblastoma, an anterior sacral myelomeningocele, or rectum anomalies. The observed bladder changes are due to mechanical obstruction and affect bladder development at a critical time, which can lead to bladder wall hypertrophy and remodeling (Pagon et al, 1979; Beasley et al, 1988; Stephens and Gupta, 1994). Affected patients do not demonstrate any sign of obstruction on postnatally performed voiding studies or cystoscopic evaluations, except when urethral atresia is also present. In this case the presentation is similar to that in patients with posterior urethral valve. However, it is possible that the largely distended bladder, as in prune belly syndrome, is caused by a transient obstruction in utero, and in some cases the presence of urethral atresia has been noted with prune belly syndrome. Another possibility for the distention is the presence of neurologic disorders leading to an inability to empty the bladder in utero. Congenital Megacystis the term megacystis is often used to describe any condition leading to a distended fetal bladder in utero, without referring to the cause of the dilation. Even the describing authors recognized that surgical interventions at the bladder neck level did not change the future outcome. Therefore the observed reflux is not an after effect of obstruction but rather the cause of the bladder dilation from continuous recycling of the urine between the upper tract and bladder (Harrow, 1967). Congenital megacystis is defined currently as a dilated, thinwalled bladder with a wide and poorly developed trigone. The wide-gaping ureteral orifices are displaced very laterally, causing massive reflux. Bladder contractility is normal, although a majority of the urine refluxes into the ureters with each void. Most patients are recognized prenatally and should be placed on prophylactic antibiotics after birth (Mandell et al, 1992). Correcting the reflux often restores normal voiding dynamics and should be performed after 6 months of age. Reduction cystoplasty can be performed but is usually unnecessary (Burbige et al, 1984). Anterior urethral valves also have been associated with megacystis, with improvement after valve resection (Confer et al, 2010). Congenital megacystis has been recognized in association with microcolon-intestinal hypoperistalsis syndrome. The syndrome can be identified on antenatal ultrasound by the appearance of a largely dilated bladder. It has been reported mostly in females and is usually considered lethal (Srikanth et al, 1993; Lashley et al, 2000). So far only 10 patients have lived beyond the first year of life, and almost all need total parental nutrition. Once identified after birth, the distended bladder requires drainage by intermittent catheterization or vesicostomy placement. Long-term data concerning the urinary tract are not available because of the short life span of the patients (Bloom and Kolon, 2002). Nondilated or Absent Fetal Bladder To truly diagnose an absent fetal bladder on ultrasound, the examination has to be repeated after 15 to 20 minutes to rule out that the fetus has not simply emptied the bladder. Bladder exstrophy conditions are characterized by the presence of a bladder template only. Therefore it can be suspected in the absence of regular bladder filling during fetal ultrasound. Bladder exstrophy can be distinguished from bladder agenesis by the bladder template on the lower abdominal wall, which, along with the amniotic fluid level, remains normal throughout the pregnancy (Mirk et al, 1986; Gearhart et al, 1995). The bladder can be hypoplastic as a result of inadequate filling or storing of urine during fetal life. Although the bladder is formed during fetal development and can be detected on antenatal ultrasound throughout pregnancy, it never reaches an adequate capacity. Some of these bladders grow once the malformation is corrected; however, later bladder augmentation is often required to reach adequate capacity (Gearhart, 2002). The division of the cloaca into the urogenital sinus and the anorectum apparently is regular, because the hindgut is usually normal. Therefore the defect can be due to either atrophy of the cranial part of the urogenital sinus or failure to incorporate the mesonephric ducts and ureters into the trigone (Krull et al, 1988). The absence of the bladder is often associated with neurologic, orthopedic, or other urogenital anomalies such as renal dysplasia or agenesis or absence of the prostate, seminal vesicles, penis, and vagina (Aragona et al, 1988). It is a very rare anomaly; only 16 live births have been reported in the 45 known cases in the English literature. All but 2 were female (Adkes et al, 1988; Gopal et al, 1993; Di Benedetto et al, 1999). In surviving infants, the diagnosis can be confirmed by retrograde ureteronephrograms via the ectopic openings. Renal function can be preserved after creation of a ureterosigmoidostomy or external stoma (Glenn, 1959; Berrocal et al, 2002). They are commonly associated with severe anomalies, are often the cause for oligohydramnios, and can require fetal or immediate postnatal intervention to prevent fetal demise. However, most patients are diagnosed postnatally because of symptomatic disease or during workup for a nonrelated disease. Malformations listed in the prenatally detected group usually severely affect fetal development, are often associated with other malformations, and require prenatal or postnatal interventions. Postnatally detected defects, on the other hand, usually do not affect fetal development and generally can be treated with conservative measures or a single surgical intervention. Bladder anomalies in the infant or child are suspected in cases of urinary tract infections, hematuria, voiding difficulties, anatomic malformations and masses, or umbilical site drainage. UrachalAnomalies Understanding the embryologic development of the urachus and its unique location is the key to understanding congenital urachal anomalies. This space is lined by the obliterated umbilical arteries, with its base on the anterior dome of the bladder and the tip directed toward the umbilicus. It has a diameter of 8 to 10 mm and can connect with one or both obliterated umbilical arteries. An inner layer consists of either transitional or cuboidal epithelial cells surrounded by a layer of connective tissue.
Syndromes
- Chemical munitions
- Hiccups after swallowing
- Eat a nutritious diet with enough calories.
- Removal of the entire colon and the rectum is called a proctocolectomy.
- Tumor, such as acoustic neuroma
- Redness of the skin (erythema), which spreads to cover most of the body
- Bleeding
- Fecal incontinence
- Cold cone biopsy
- Rye bread
Cheap atorlip-20 20 mg mastercard
The most recent series supports this finding in low-grade reflux but notes that high-grade reflux into lower pole ureters in females is more prone to breakthrough infection and scarring and therefore may warrant more aggressive management (Afshar cholesterol chart europe buy atorlip-20 20mg fast delivery, 2005; Estrada et al, 2009). Although contralateral renal growth often displays compensatory hypertrophy, one study observed somewhat less compensatory hypertrophy by 1 year of age (Zerin and Leiser, 1998) than may be expected if contralateral reflux is absent (5. In a retrospective study of 46 children with solitary renal agenesis, the rate of contralateral renal pathology was 46%. The presence of active reflux appears to present a risk factor for the affected mother. In 1958, Hutch described a higher incidence of pyelonephritis during pregnancy in 23 women with a history of reflux and recurrent bacteriuria (Hutch, 1952, 1961). Heidrick and colleagues (1967) evaluated 321 women with cystography either during the last trimester or within 30 hours after delivery. The incidence of pyelonephritis was 33% in women with reflux compared with less than 5% in women without reflux. Finally, cystograms performed 4 to 6 months postpartum in 100 women with a history of asymptomatic bacteriuria during pregnancy showed reflux in 21%. Bacteriuria was easier to clear in patients without reflux (67%) than in those with reflux (33%) (Williams and Hulme-Moir, 1970). They found that women with a history of prior infections had a high incidence of bacteriuria during pregnancy, whereas those with renal scarring and persistent reflux were more prone to develop acute pyelonephritis. In a similar study, the outcome of pregnancy was assessed in 88 women with previous bacteriuria. Women with normal kidneys and reflux also had an increased risk for hypertension during the last trimester (McGladdery et al, 1992). Pregnant women with bilateral renal scars were also shown to have a higher incidence of preeclampsia than those with unilateral scarring (24% vs. In a large study of 158 women with reflux nephropathy, pregnancy was uneventful in patients with normal blood pressure and renal function, whereas the risks for fetal demise and accelerated maternal renal disease were increased in women with impaired renal function (Jungers, 1996). However, they were not at a higher risk for miscarriage than the general population. In a larger study of 77 pregnancies in 41 women whose ureters had been reimplanted, Bukowski (1998) and colleagues reported that the incidence of pyelonephritis during pregnancy was slightly higher than in the general population but that the fetus and mother were at significant risk when renal scarring or hypertension was present. Although these studies may at first suggest a limited benefit to reimplantation during a subsequent pregnancy, several factors must be borne in mind. Also, bladder dynamics change during pregnancy as a result of increasing uterine size. Finally, it is not known whether formerly refluxing renal units in such adult patients carry a latent predisposition or heightened susceptibility to pyelonephritis during the pregnancy as a consequence of previous postinfection damage during childhood and/or any inherent reflux-associated dysmorphism, both of which would persist despite surgery at the bladder level. Nevertheless, in keeping with the more recent emphasis on preexisting renal status when considering reflux management, at least one meta-analysis of the respectively. In another study, 19 cases of contralateral reflux were observed in 51 patients with ipsilateral renal agenesis (Song et al, 1995). Reflux repair or persistence was documented in 9 and 7 patients, respectively, with spontaneous resolution observed in only 3 patients. The gross inefficiency of the bladder that expels urine to both the exterior and the upper tracts results in gradual bladder dilation as the refluxed urine returns to the bladder. This perpetuates marked ureteral dilation, leading to the radiographic appearance of massive hydroureter and a thin-walled enlarged bladder (Burbige et al, 1984). The phenomenon is referred to as the megacystis-megaureter association or syndrome. It is more frequent in males, and the differentiation from posterior valves is crucial (Kaefer et al, 1997). Although the latter is due to an obstructive lesion, megacystis-megaureter is a nonobstructive condition akin to cardiac dilation by regurgitation from incompetent valves. Voiding studies will readily demonstrate an open posterior urethra and differentiate megacystis-megaureter from posterior valves or prune-belly syndrome. Vesicostomy can temporize by eliminating the residual urine volume and establishing safe drainage of the upper tracts until ureteral reimplantation can be performed. Treatments aimed at improving an already patent bladder outlet are contraindicated, risk infection, and fail to correct the primary cause. A period of bladder rehabilitation by strict attention to emptying in the postoperative period (Koefoot et al, 1981) usually will result in a return to normal bladder volume and contractile behavior. This suggests that potentially normal underlying bladder physiology can be realized if the propensity for reflux is corrected. No precise common genetic insult has been determined to explain such associations. PregnancyandReflux the morphology of the urinary tract is altered with the onset of pregnancy and increases throughout gestation (Beydoun, 1985). Bladder tone decreases because of edema and hyperemia, changes that predispose the patient to bacteriuria. In addition, urine volume increases in the upper collecting system as the physiologic dilation of pregnancy evolves. The slower drainage that results can enhance the growth of organisms and increase the significance of a pregnancy and reflux association also suggests that the presence of renal scarring, and not the presence or absence of reflux, is the principal factor driving morbidity during pregnancy in such women (Hollowell, 2008). When combined with the known physiologic renal and bladder changes during pregnancy, it is reasonable to speculate that such kidneys may carry a heightened predisposition to pyelonephritis. Those with uncorrected reflux appear to be particularly at risk and should have their reflux corrected before pregnancy to minimize maternal and fetal morbidity. Because of the difficulty in predicting an outcome for this subset of patients, most clinicians recommend surgical correction for girls with reflux that persists beyond puberty, although there has been a trend toward discontinuation of prophylactic antibiotics in older girls with active reflux. Long-term follow-up studies of these patients through puberty are unavailable (see later discussion). Chapter137 VesicoureteralReflux 3153 1992), and 85% of grade 2 (Edwards et al, 1977). This belies the fact that lower urinary tract dynamics may also play a role in mitigating spontaneous resolution. Grade 3 reflux will resolve in approximately 50% of cases (Duckett, 1983; McLorie et al, 1990). Very few cases of higher grade reflux (grades 4 and 5, and bilateral grade 3) will resolve spontaneously. Analyses from several sources, including the International Reflux Study in Children, support a uniformly low prevalence of resolved high-grade reflux with no more than 25% (Weiss et al, 1992b) and as little as 9% (Skoog et al, 1987) of patients demonstrating spontaneous resolution. It is possible no real difference exists in resolution rates in high-grade reflux (Tamminen-Mobius et al, 1992). Considering the fact that any given reflux grade is assigned on the basis of a dynamic voiding study, the possibility for variability by at least one grade, especially in assigning higher grades to reflux, is quite real. Thus attempting to discriminate true differences in resolution rates for grades 3 and higher reflux may not be particularly clinically relevant. ResolutionbyAge the age at which reflux begins or is first encountered will play a more potent role in the management of the patient with reflux than the grade itself. It is self-evident that if reflux is a congenital disorder with an inherent tendency to resolve spontaneously over time, it will (1) be most prevalent in neonates and young children, and (2) demonstrate the greatest tendency to resolve in this group. Conversely, in any analysis, if reflux is truly primary, is encountered in an older child, and has been present since birth, it already has demonstrated a propensity to persist and therefore is self-selected for reflux, which is unlikely to resolve (Skoog et al, 1987). Interpretation of more recent follow-up studies (Connolly et al, 2001) suggest that diagnosis at age 5, as well as in infancy, is associated with a similar resolution rate (20% per year), regardless of age. However, as stated at the outset, it must be remembered that resolution 5 years after age 5 implies reflux has required 10 years to resolve versus resolution 5 years after birth. Moreover, the observation by McLorie and colleagues (1990) that high-grade reflux in patients presenting after birth showed no difference in resolution rates between subjects younger and older than 1 year of age may reflect the generally poor resolution rate of high-grade reflux to begin with. These principles likely underlie the observation that when reflux resolves, it often does so within the first few years of life. The study by Skoog and colleagues (1987) observed that 30% to 35% of subjects resolved their reflux each year. In the study by McLorie and coworkers (1990), 92% of resolved grade 3 reflux occurred within 4 years. There is a tendency to ascribe a benefit to the observation of interval reduction in grade. Clearly then, what constitutes reflux resolution depends on the period over which resolution is sought.
Atorlip-20 20mg without a prescription
More exstrophy cells migrated than control cells cholesterol medication starts with l 20mg atorlip-20, although it is not known if this movement is organized or directional. In a second study, Suson and colleagues (2012) showed that enhanced exstrophy smooth muscle cell migration was a result of excess transforming growth factor-1 signaling but was independent of increases in intracellular calcium concentration. In a recent report by Stec and colleagues (2012a), 674 patients were reviewed; 462 were found to have had ultrasound examination. The most common malformation was a duplicated collecting system (6); others included hypoplastic or absent kidney (3), pelvic kidney (2), ureteropelvic junction obstruction (1), and multicystic dysplastic kidney. The peritoneal pouch of Douglas between the bladder and the rectum is enlarged and unusually deep, forcing the ureter down laterally in its course across the true pelvis. The distal segment of the ureter approaches the bladder from a point inferior and lateral to the orifice, and it enters the bladder with little or no obliquity. Therefore, reflux in the closed exstrophy bladder occurs in 100% of patients, and reimplantation surgery is required at bladder neck reconstruction. If excessive outlet resistance is gained at the time of either initial closure or combined epispadias and bladder exstrophy closure, and recurrent infections are a problem even with suppressive antibiotics, ureteral reimplantation or Deflux injections are required before bladder neck reconstruction. Because there is probably a common embryologic origin for all of these defects, they all share many or some of the defects noted in the three major components of the complex-skeletal, urinary, and genital. The presence of a characteristic musculoskeletal defect of the exstrophy anomaly with no major defect in the urinary tract has been named pseudoexstrophy (Marshall and Muecke, 1968). Predominant characteristics include an elongated, low-set umbilicus and divergent rectus muscles that attach to the separated pubic bones. In this variant, the mesodermal migration has been interrupted in its superior aspect only, thus wedging apart the musculoskeletal elements of the lower abdominal wall without obstructing the formation of the genital tubercle. In the superior vesical fissure variant of the exstrophy complex, the musculature and skeletal defects are exactly the same as those in classic exstrophy; however, the persistent cloacal membrane ruptures only at the uppermost portion, and a superior vesical fistula results that actually resembles a vesicostomy. In a large review of an exstrophy database of over 815 patients, Lowentritt and colleagues (2005) reported 25 exstrophy complex variants, of which six were cloacal exstrophy variants. Continence rates after bladder neck repair were compatible with classic exstrophy. Three cases were reported by Arap and Giron (1986) in which the patients had classic musculoskeletal defects, and two of the three were continent. Of the two male patients, one had an associated complete epispadias and the other had a completely normal penis. Therefore the external genital manifestations in exstrophy variants can be quite variable. In addition to pseudoexstrophy, superior vesical fissure, and duplicated exstrophy, isolated occurrences of a fourth entity, covered exstrophy, have been reported (Cerniglia et al, 1989). A common factor in these patients is the presence of musculoskeletal defect associated with classic exstrophy but no significant defect of the urinary tract. Chandra and associates (1999) reported a covered exstrophy with incomplete duplication of the bladder. However, in cases of covered exstrophy (Narasimharao et al, 1985; Cerniglia et al, 1989), there has been an isolated ectopic bowel segment present on the inferior abdominal wall near the genital area, which can be either colon or ileum with no connection with the underlying gastrointestinal tract and only epispadias in the male. A patient seen at our institution had the standard appearance of most split symphysis variants, and one could actually see the bladder through a thin membrane of lower abdominal skin. There are two different forms of bladder duplication: anteroposterior duplication and side-by-side duplication. The former form is considered a duplicate exstrophy with a patch of everted bladder mucosa on the anterior abdominal wall and a second bladder lying in the pelvis. The mainstay of treatment has been resection of the ectopic mucosa and closure of the abdominal wall defect. The other form of duplication involves patients who have two separately formed bladder halves in a left-right orientation with a midline septum between the bladders containing muscle. Variants are rare, but it is important to recognize the different appearances at birth, because the initial treatment will greatly influence the long-term outcome. Two patient groups had better outcomes than those with classic presentations-superior vesical fissure and skin-covered cloacal exstrophy. Because the sphincter is intact, patients with superior vesical fissure went through regular toilet training and became continent without the need for a later bladder neck procedure. Many reports of exstrophy variants include these patients, leading to the wrong belief that all patients with variants perform better than those with bladder exstrophy. Lowentritt and colleagues (2005) suggest that other than superior vesical fissure, all variants should be managed with formal exstrophy closure at birth and followed in the same manner as their classic presentations. PrenatalDiagnosis Even with modern ultrasound modalities, the prenatal diagnosis of bladder exstrophy is often difficult to delineate. Ultrasound evaluation of the fetus by means of high-resolution real-time units allows a thorough survey of the fetal anatomy, even during routine obstetric ultrasound examinations (Gearhart et al, 1995a). In these reviews, the absence of a normal fluid-filled bladder on repeated examinations suggested the diagnosis, as did a mass of echogenic tissue on the lower abdominal wall (Mirk et al, 1986; Verco et al, 1986). The main reason for the prenatal diagnosis of bladder exstrophy is so that the parents can be counseled regarding the risks and benefits and other aspects of the condition. After appropriate counseling, arrangements can be made for delivery of the baby in a specialized exstrophy center where immediate reconstruction of the exstrophy can occur. Delivery in a specialized exstrophy center allows the parents to be exposed to the expertise of multiple disciplines, including the all-important psychological support these parents need when a child with a birth defect of this magnitude is delivered. Four to 6 days before bladder closure, bilateral iliac osteotomies were performed. The continence procedure was limited to freeing the fibers from the intrasymphyseal band and wrapping this band around the urethra at the time of closure to increase outlet resistance. The initial staged approach to functional bladder closure included three separate stages: bladder and abdominal wall closure; bladder neck reconstruction and antireflux procedure; and later epispadias repair. This approach was recommended for most cases of exstrophy reconstruction beginning in the early 1970s (Cendron, 1971; Jeffs et al, 1972; Williams and Keaton, 1973). Although this procedure was successful, it has been modernized in the last 15 years to include bladder closure, abdominal wall closure, and posterior urethral closure well onto the penis in the newborn period with bilateral innominate and vertical iliac osteotomy, if indicated; epispadias repair at 6 months to 1 year of age; and bladder neck reconstruction along with antireflux procedure at age 4 to 5 years, when the child has achieved an adequate bladder capacity for bladder neck reconstruction and is motivated to participate in a postoperative voiding program (Gearhart and Jeffs, 1998). Other methods of treatment of the newborn with bladder exstrophy have been offered. Grady and Mitchell (1999) proposed combining bladder exstrophy closure with penile repair in the newborn period. Baka-Jakubiak (2000) recommended newborn exstrophy closure alone and combined bladder neck reconstruction and epispadias repair when the child reaches a satisfactory age for participation in a voiding program. Kelly (1995) has recommended a staged repair in which no osteotomy is used and a second-stage "radical soft-tissue mobilization" is performed before later urethral repair. Schrott and colleagues (1984) recommended bladder closure, ureteral reimplantation, epispadias repair, and bladder neck reconstruction in the newborn period. Lastly, Stein and coworkers (1999) recommended ureterosigmoidostomy in the newborn period with abdominal wall and bladder closure. Chapter139 Exstrophy-EpispadiasComplex 3193 special interest and experience in managing the exstrophy spectrum. An exstrophy support team should be available and should include a pediatric orthopedic surgeon, pediatric anesthesiologist, social workers, nurses with special interest in bladder exstrophy, and a child psychiatrist or psychologist with expertise and experience in genital anomalies. The Association for the Bladder Exstrophy Community is available and has a website for parents and family members to obtain further information about the bladder exstrophy condition. Cardiopulmonary and general physical assessment measures can be carried out in the first few hours of life. Well-done ultrasound studies are usually sufficient to provide evidence of renal structure, function, and drainage, even in the first few hours of life before the patient undergoes closure of the exstrophy defect. In these days of modern transportation, no child is ever more than a few hours away from a neonatal center with full diagnostic and consultative services. During travel the bladder should be protected by a plastic membrane, as in the nursery, to prevent damage to the delicate newborn bladder mucosa. Selection of Patients for Immediate Closure Successful treatment of exstrophy with functional closure demands that the potential for success in each child be carefully considered at birth by an experienced exstrophy surgeon. The size and the functional capacity of the detrusor muscle are important considerations for the eventual success of functional closure. Correlation between apparent bladder size and the potential bladder capacity must not be confused.
Buy atorlip-20 on line
Woodhouse (1999) believed that although prophylactic surgery may be helpful cholesterol levels post heart attack discount atorlip-20 online american express, once prolapse occurs, anterior fixation is insufficient to correct uterine prolapse in the exstrophy patient. Woodhouse recommends fixing both sides of the uterus from the cervix to the top of the uterus bilaterally to the presacral ligaments. Mathews and coauthors (2003a) reported on a large series of girls and women with the exstrophy complex. All girls older than 18 years indicated that they had normal sexual desire, and many were sexually active. Some patients indicated that they restricted sexual activity because of the cosmetic appearance of their external genitalia. Mons plasty is therefore very important to obtain a cosmetically pleasing appearance either in infancy or in adolescence because hair-bearing skin and fat should be used to cover the midline defect. It certainly can be done in adolescence with the use of rhomboid flaps, as popularized by Kramer and colleagues (1986). Sporadic instances of pregnancy or the initiation of pregnancy by males with bladder exstrophy have been reported. Only 3 of 68 men in one study (Bennett, 1973) and 4 of 72 in another (Woodhouse et al, 1983) had successfully fathered children. Milking the urethra in an antegrade fashion from proximal to distal has provided pregnancy in some cases (Woodhouse, 1999). In a large series of 2500 patients with exstrophy and epispadias (Shapiro et al, 1985), there were 38 males who had fathered children. Hanna and Williams (1972) compared semen analyses in men who had undergone primary closure and ureterosigmoidostomy. A normal sperm count was found in only 1 of 8 men after functional closure and in 4 of 8 men with diversion. The difference in observed fertility potential is probably attributable to iatrogenic injury to the verumontanum during functional closure or bladder neck reconstruction. Retrograde ejaculation may also account for low sperm counts after functional bladder closure. In a long-term study from our institution, Ben-Chaim and associates (1996) found that 10 of 16 men reported they ejaculated a few cubic centimeters of volume, 3 ejaculated only a few drops, and 3 had no ejaculation. Semen analysis was obtained in 4 patients: 3 had azoospermia and 1 had oligospermia. In another large series by Stein and colleagues (1994) from Germany, the authors found that none of the patients who had reconstruction of the external genitalia could ejaculate normally, nor had they fathered children. Five patients who did not undergo reconstruction had normal ejaculation, and 2 had fathered children. The conclusion was that male patients with genital reconstruction and closure of the urethra demonstrated high risk of infertility. In a large study of successful primary closure from a large exstrophy center by Ebert and colleagues (2008), sperm parameters were poor in 18 of 21 patients and follicle-stimulating hormone was increased in 25% of patients (Ebert et al, 2009). Ebert and colleagues (2010) reported on 17 adult men with bladder exstrophy undergoing the Erlangen approach single-stage procedure. At a mean follow-up of 19 years, 15 had bladder preservation and 12 were voiding per urethra. The potential for normal sperm counts was greater in patients who underwent only a single bladder neck procedure. However, the ultimate outcome would be better measured by how these children adjust overall in society. The severe nature of the exstrophy disorder could predict that this birth defect could have substantial psychological implications. Multiple hospitalizations may interfere with the ability to be like other children. Concerning the potential medical and psychological implications of this anomaly, children born with exstrophy may be at increased risk for difficulties. Formerly, there was a limited amount of information in the literature concerning this condition and its treatment and whether or not it has a deleterious effect on children and their families. Montagnino and coworkers (1998) evaluated younger children who performed more poorly and had disturbed behavior, specifically in skills related to function in school. Children who achieved continence after the age of 5 years were more likely to have problems with acting-out behavior. There were no differences in adjustment based on male or female sex, bladder versus cloacal exstrophy, type of continence strategy, or gender reassignment versus no reassignment. The conclusions of this long-term study were that children with exstrophy do not have clinical psychopathology (Montagnino et al, 1998). There was acting-out behavior rather than depression or anxiety, suggesting that improved outcomes may be achieved through a focus on normal adaptation rather than potential psychological stress. In addition, earlier achievement of continence through reconstructive efforts is potentially of psychological benefit. This work was further supported by Catti and colleagues (2006), who found that QoL in adults was better in those who were continent with a good body image. Reiner (1999) studied 42 children with exstrophy and presented preliminary results suggesting that these patients tend to have more severe behavioral and developmental problems than children with other anomalies, significant body distortion, and self-esteem problems. Reiner has recommended early intervention with the exstrophy patient and family and continuation with long-term psychiatric support into adult life. In a study from Europe, Feitz and associates (1994) found a more positive picture when they evaluated 11 women and 11 men with exstrophy, of whom 9 women (82%) and 10 men (91%) did not manifest any clinical levels of psychological stress. With the use of structured instruments and appropriate evaluation and interviews, Reiner and Gearhart (2006) indicated that all 20 patients evaluated met criteria for at least one anxiety disorder. Older patients experienced waning of anxiety associated with peer discovery of incontinence after successful surgical reconstruction, and all noted intensified sexual activity with age. Data from Reiner and colleagues (2008) from a large series of male patients revealed that 14% experienced suicidal ideation. As they became older, 31% experienced this phenomenon; a few attempted adolescent or early adulthood suicide, and 1 succeeded. These findings underline the importance of screening patients for psychopathology as they age. In an important study by Lee and colleagues (2006), females were found to have more close friendships, fewer disadvantages in relation to healthy peers, and more partnerships than males. There were no gender differences in adjustment within educational and professional careers, which overall were very good. Ebert and colleagues (2005) reviewed by questionnaire a group of 100 exstrophy adolescents. All patients were heterosexual and almost 50% were sexually active, but almost 60% expressed anxiety about sexual activity. The most important finding was that 94% of patients expressed an interest in psychological assistance, underlining the importance of early childhood intervention. TheFemalePatient Krisiloff and colleagues (1978) reported on 45 women with bladder exstrophy who successfully delivered 49 normal offspring. The main complication after pregnancy was cervical and uterine prolapse, which occurred frequently. Burbage and coworkers (1986) described 40 women ranging from 19 to 36 years of age who were treated in infancy for bladder exstrophy; 14 pregnancies in 11 of these women resulted in 9 normal deliveries, 3 spontaneous abortions, and 2 elective abortions. Spontaneous vaginal deliveries were performed in those women, and cesarean sections were performed in women with functional bladder closures to eliminate stress on the pelvic floor and to avoid traumatic injury to the urinary sphincter mechanism (Krisiloff et al, 1978). With modern reconstructive techniques, successful pregnancies have been reported in female patients who have undergone continent urinary diversion (Kennedy et al, 1993). Giron and colleagues (2011) reported on 14 women who had undergone successful reconstruction and had 22 pregnancies. Seventeen pregnancies resulted in healthy newborns, 1 premature delivery of an infant who did well, 4 spontaneous abortions caused by genital prolapse, and 1 postpartum demise. After delivery, 3 mothers had temporary urinary incontinence, 1 mother had a vesicocutaneous fistula, and 7 women (50%) had genital prolapse. In a larger report on 52 women with bladder exstrophy, Deans and colleagues (2012) reported on reproductive outcomes.