Proven 5 mg simvastatin
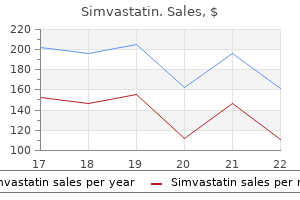
In this fashion the rectovaginal septum is palpated between the two fingers cholesterol shrimp nutrition facts order 20 mg simvastatin free shipping, and any thickness or mass is noted. The finger should also attempt to identify the uterosacral ligaments, which extend from the posterior wall of the cervix posteriorly and laterally toward the sacrum. Any thickening or nodularity of these structures may imply an inflammatory reaction or endometriosis. If the uterus is retroverted, that organ should be outlined for size, shape, and consistency at this point. Furthermore, testing a single stool specimen for fecal occult blood is also inadequate. Therefore, routine assessment of the rectum is not recommended during female pelvic exams. As noted earlier, simple inspection of the annual visit is important for both health maintenance and preventive medicine reasons. Major preventable problems must be discussed because patient behavior can make a difference. Various medical groups update recommendations for primary and preventive screening services regularly. The latter is a clearinghouse of evidence-based guidelines that allows comparison of differing recommendations, as many societies do not always agree on these guidelines. Furthermore, screening recommendations must be considered in light of local prevalence of disease and additional risk factors an individual patient might present. Obviously, patients taking an active role in changing their behavior can alter many of these factors, and physicians have the opportunity to advise them at the annual visit. Although the gynecologist may or may not function as the sole primary care provider for women, the annual visit is an opportunity to discuss patient choices, lifestyle, and habits. It offers a perfect environment to provide education about healthy lifestyle and prevention strategies to reduce harm and improve health. In 1618, an English clergyman observed, "Prevention is so much better than healing because it saves the labor of being sick. At each checkup the physician should also encourage the patient to develop an exercise program appropriate for her abilities and taking into account her overall health status and recommendations from any other health care providers. For patients who smoke, benefits of reduction and cessation should be addressed and resources provided. It is the most important modifiable risk factor associated with adverse pregnancy outcomes, and pregnancy is often a time when a woman will be motivated to quit smoking. The nonreproductive negative health effects of smoking include cancer, coronary artery disease, peripheral vascular disease, respiratory disorder, peptic ulcer disease, and osteoporosis. The five "A"s of smoking cessation are important for providers to know: ask (about use), advise (about use), assess (willingness to quit), assist (in planning and counseling), and arrange (regular contact and follow-up). Counseling strategies have been published and show that 5 to 15 minutes of motivational interviewing and problem-solving strategies will result in a 5% to 10% quit rate. More intensive options to aid in smoking cessation include pharmacotherapy with nicotine replacement, bupropion, or varenicline. It is appropriate to ask questions that assess her sexual activity and gratification and questions that detect abuse or intimidation in her life. Everyone suffers loss during his or her lifetime, and the older the patient the more likely that this is the case. Grief may be the result of a loss of a spouse or loved one, a pet, a job, a body part, or the ability to perform activities the patient has enjoyed (see Chapter 9). The patient should provide updated information about all medications/supplements that she takes. This will give the physician the opportunity to review with the patient why she is taking each one and also to assess for potential adverse drug interactions. It may also be possible to tie specific drug use to an undesirable symptom the patient may be experiencing. Muscle-strengthening activities: weight lifting, resistance bands, pushups, heavy gardening, yoga. Increasing overall time of aerobic exercise beyond the minimal recommendations further increases health benefits. Obstetrics & Gynecology Books Full 7 History, Physical Examination, and Preventive Health Care the annual visit is an opportunity for the physician to screen for a variety of illnesses affecting not only the reproductive organs but also all of the organ systems. The visit should include an interim health history and an age-appropriate physical examination. In 2013, the American College of Obstetricians and Gynecologists published online the Well-Woman Care: Assessments & Recommendations, which recommended screening examinations, immunizations, and laboratory tests for the annual visit for women in different age groups (see Table 7. Women with concurrent medical conditions such as obesity or hypertension, women with certain lifestyle choices such as tobacco use, and women with certain family history will be directed to screening that may be sooner or more frequent than that recommended for the general population. Ninety percent of breast cancers are sporadic, but 10% are due to inherited disorders. The prime findings in the history include multiple family members with breast or ovarian cancer, breast and ovarian cancer in a single individual, or early age of breast cancer onset. With women having a one out of eight chance of developing breast cancer in their lifetime, it makes sense to counsel even low-risk women about healthy lifestyle interventions that can lower their risk of cancer, including eating a healthy diet, exercising, and maintaining a normal body weight. Routine screening mammography was no longer recommended in women 40 to 49 years old. Instead, the decision about when to begin regular screening should be individualized. This received a "C," which means the organization did not recommend for or against. Reasons for this change are that while breast cancer mortality does decrease with screening in this age group, it is a small net benefit. Furthermore, there were concerns about the potential harm of mammography in terms of excess radiation exposure, excess need for additional imaging and breast biopsies (false-positive tests), and patient worries and anxiety about the testing. The recommendation does leave room for an open a discussion with the individual woman. A variety of other screening tests are recommended during annual gynecologic visits. The 2008 American College of Gastroenterology guidelines stated that the preferred test for colorectal cancer screening is colonoscopy every 10 years. A family history of polyps does not evoke earlier onset of screening unless the polyps were advanced adenomas. If a single firstdegree relative had colorectal cancer diagnosed after age 60, routine screening is recommended. Otherwise, 10 years before the age at which the family member developed colorectal cancer is the time to begin screening. Other screening tests, such as tests for hepatitis C and tuberculosis, should certainly be considered for women in high-risk groups, with comorbid medical conditions, or with certain family histories. Endometrial cancer recommendations for early detection consist of advising women at menopause of their risk factors and the symptoms of endometrial cancer. Even in women known to be at increased risk of endometrial cancer, there is insufficient evidence to recommend screening (unopposed estrogen treatment, tamoxifen therapy, late menopause, nulliparity, infertility or anovulation, obesity, hypertension, and diabetes). Women at very high risk should have an annual endometrial biopsy starting at age 35 (known hereditary nonpolyposis colorectal cancer, genetic mutation carrier, or strongly suspected carrier). Regular health exams to include the thyroid, ovaries, lymph nodes, oral cavity, and skin should be offered, but no special recommendations have been made. All women should have a Tdap booster once in their adult lifetime and in each third trimester of pregnancy to facilitate some passive immunity to the fetus against Bordetella pertussis. Pneumococcal vaccine should be offered to women with chronic lung, liver, or cardiovascular disease; diabetes; asplenia; cochlear implants; and immunocompromising conditions. In addition, women in all age groups should be offered appropriate immunizations and vaccinations when they travel to other countries. In particular, the hepatitis A vaccine should be given to women who are traveling to areas with a high or intermediate endemicity of hepatitis A, use injection drugs, have chronic liver disease, receive clotting factor concentrates, or work with primates infected with hepatitis A. In line with injury prevention, the patient should be reminded about the use of seat belts and helmets and other safety concerns mentioned earlier in this chapter.
Purchase discount simvastatin online
T2-weighted image in another patient shows small periventricular plaques (solid arrows) as well as an area of left parietal infarction (open arrow) cholesterol recipes purchase 40mg simvastatin with amex. Definition A brain abscess is a collection of infection/pus in the brain parenchyma. A brain abscess can develop due to direct spread of infection from a local infection. Less commonly, a brain abscess can develop from the hematogenous seeding of an infection from a distant site. The microorganism involved depends on the source of infection and is most commonly bacterial. Source of Infection Common Microorganisms Sinuses/dental Ears Head trauma/neurosurgical procedure Endocarditis lmmunocompromised host Streptococcus, Haemophilus, Bacteroides, Fusobacterium, and Prevote//a species Enterobacteriaceae, Pseudomonas aeruginosa, Streptococcus and Bacteroides species Staphylococcus aureus, P. Symptoms of a brain abscess are variable and include severe headache (75%) that is worse with lying flat, nausea, vomiting, drowsiness, weakness, numbness, and difficulty speaking. Other vital signs are generally normal, but if there is a systemic infection, hypotension and tachycardia may be present. Neurologic examination: No specific exam maneuvers exist for a brain abscess, but a complete neurologic examination should be performed to assess for abnormalities. Nuchal rigidity/meningismus (neck stiffness) may be present if there is rupture of the brain abscess into the ventricular system and/or coexisting meningitis. Motor/sensory/coordination: Any focal neurologic deficit may be present depending on the location of the abscess. Definition Meningitis is inflammation of the leptomeninges, which includes the dura, arachnoid, and pia mater that surround the brain and spinal cord. Meningitis is typically caused by infections and can be classified as bacterial meningitis (Table 7. Aseptic meningitis refers to meningitis in which routine bacterial cultures are negative. Aseptic meningitis may be caused by viral, fungal, and mycobacteria infections, as well as malignancy, inflammation, or drugs. Neck stiffness, headache, and fever: the differential diagnosis includes subdural/epidural empyema, brain abscess, and encephalitis. Common organisms causing meningitis Type of Infection Bacterial Microorganism Streptococcus pneumoniae, Neisseria meningitides, Haemophilus influenzae, Listeria monocytogenes (in neonates and elderly), S. Given the systemic infection, individuals may also have hypotension, tachycardia, and tachypnea. General inspection: Petechia and purpura may be present, particularly in cases of N. Special Tests Nuchal rigidity: Neck stiffness is detected with passive neck flexion (Sn 0. Kernig sign: With the patient supine and hip flexed to 90 degrees, the clinician attempts to fully extend the knees. The clinician flexes the leg at the hip and knee and then attempts to straighten the knee. Prior to the development of these symptoms, her primary care provider had diagnosed her with a viral upper respiratory tract infection. Rhinosinusitis is described by the sinuses involved (maxillary, ethmoid, frontal, or sphenoid sinuses), etiology (viral, bacterial, or fungal), presence of extrasinus involvement (complicated or uncomplicated), and aggravating factors. Furthermore, the clinical course of rhinosinusitis can be divided into five subtypes (Table 7. The majority of acute rhinosinusitis cases are caused by viral infection, specifically rhinovirus. Although rhinosinusitis occurs frequently in healthy patients, a number of local, regional, and systemic conditions may predispose a patient to developing rhinosinusitis (Table 7. Rhinitis and facial pain: the differential diagnosis includes allergic fungal rhinosinusitis, allergic rhinitis, invasive fungal rhinosinusitis, vasomotor rhinitis, trigeminal neuralgia, migraine or headache disorder, and temporomandibular joint dysfunction. Subtypes of rhinosinusitis Rhinosinusitis Task Force (2007) Clinical Classification Scheme Acute rhinosinusitis Recurrent rhinosinusitis Subacute rhinosinusitis Chronic rhinosinusitis Acute exacerbation of chronic rhinosinusitis Symptoms lasting <4 wk with complete resolution:2:4 episodes of acute rhinosinusitis per year with symptom-free intervals Symptoms lasting 4-12 wk Symptoms lasting:2:12 wk Sudden worsening of baseline chronic rhinosinusitis with return to baseline What symptoms might be observed Major symptoms of rhinosinusitis include congestion, facial pain/pressure, nasal obstruction, and purulent/colored nasal discharge. Minor symptoms include frontal headache, halitosis, dental pain, otalgia, and cough. Inspection: the anterior nasal mucosa may demonstrate edema, purulent discharge, and polyps. The oral cavity and oropharynx may demonstrate erythema from postnasal drip or poor dentition. Plain film radiography may demonstrate sinus air-fluid levels but has limited and sensitivity. Definition A retropharyngeal abscess is a suppurative infection in the potential space formed by the fascia located in the retropharynx. Retropharyngeal abscess occurs primarily in children, although it can occur in adults. Pharyngitis: the differential diagnosis includes viral pharyngitis, bacterial pharyngitis, mononucleosis, Kawasaki disease, and trauma. Symptoms of a retropharyngeal abscess include torticollis, dysphagia/anorexia, cough, trismus, and lethargy. Other potential complications include septicemia, aspiration pneumonia (abscess rupturing into airway), internal jugular vein thrombosis and thrombophlebitis, carotid artery erosion and rupture, and mediastinitis. At the level of C2, the distance from the anterior surface of the vertebrae to the posterior border of the airway should be 7 mm or less. At the level of C6, this distance should be 14 mm or less in children <15 years old and should be <22 mm in an adult. Thickened prevertebral soft tissues may be consistent with a retropharyngeal space infection. Pituitary adenomas are classified by size, with those <l cm referred to as microadenomas, and those > 1 cm referred to as macroadenomas. Pituitary adenomas may arise from any of the cell types in the anterior pituitary and can lead to excess of the hormone secreted by the involved cell type or hyposecretion of other pituitary hormones due to compression of the remainder of the gland. Pituitary adenomas develop due to clonal expansion of a cell line similar to other neoplasms. This is related to the development of genetic mutations due to genetic and environmental factors. Sellar region mass: the differential diagnosis includes craniopharyngioma (remnant of Rathke pouch, usually in children), meningioma (benign tumor of the meninges), pituitary gland hyperplasia, germ cell tumors, optic gliomas, aneurysms, and cysts. Symptoms develop due to local mass effect and/or excessive or decreased pituitary function. All pituitary tumors can cause hypofunctioning of the pituitary gland due to decreased hormone secretion from compression of the remaining pituitary gland. Vital signs: the vital signs may be affected by hormonal changes, and individuals may be hyperor hypothermic, tachy- or bradycardic, and hyper- or hypotensive, depending on the hormonal abnormalities. Special Tests Formal Humphrey visual field testing is performed to determine visual field loss. Histologically, this tumor type is highly cellular and pleomorphic with mitotic activity, microvascular proliferation, and/or necrosis. Other symptoms include nausea/vomiting (15%), memory loss (39%), personality change (27%), and visual symptoms (21 %). Cognitive impairment (39%) may be present depending on the area of the brain affected by the mass lesion. Language/motor/sensory/coordination: Any focal neurologic deficit, for example, aphasia, weak- ness, sensory deficit, and dysmetria, may be present. A stereotactic brain biopsy may also be done if the lesion is too deep for open surgery. He extends his left arm and leg to painful stimuli, but there is no movement on the right side. The primary brain injury occurs at the time of the trauma due to direct impact, acceleration-deceleration, and penetrating and blast injuries. A coup injury refers to injury in the brain at the site of impact, while contrecoup injury refers to injury on the side of the brain opposite to the impact, likely due to deceleration.
Purchase simvastatin in united states online
Bupropion appears to exert its therapeutic effect by enhancing effects of dopamine and norepinephrine foods lowering cholesterol levels effortlessly purchase simvastatin online now. It increases energy and can cause insomnia, increased anxiety, headaches, and gastrointestinal side effects. Bupropion also lowers the seizure threshold, especially at doses above 450 mg daily, and should not be used in women with a history of a seizure disorder or bulimia. Trazodone is a highly sedating serotonergic antidepressant that is used primarily at low doses (25 to 100 mg at bedtime) for insomnia. It is important to warn women that antidepressant medication can take up to 4 to 6 weeks to work, and to schedule a follow-up visit within that time to monitor treatment adherence, side effects, and therapeutic response. The mechanism for this is unclear but may be in part an increase in energy and motivation before improvement in mood. Women should be warned of this potential phenomenon and instructed to stop the medication and call the provider if this occurs. Overall, antidepressants reduce depression and risk for suicide, but this potentially serious side effect is another indication for close follow-up early in treatment. Cognitive behavioral therapy addresses the negative, distorted thinking that is characteristic of depression, such as the belief that things are bad now, have always been bad, and will always be bad, or thoughts of worthlessness and guilt. In addition, behavioral activation, or scheduling activities that provide a sense of accomplishment, mastery, or pleasure, is helpful in depression, and exercise has been shown to decrease depressive symptoms. Interpersonal therapy addresses the life changes and interpersonal challenges that contribute to depression, especially in women. These include grief, conflicts in interpersonal relationships including marital or intimate partner conflicts, transitions in roles within work or the family, and social isolation with a lack of supportive relationships. Both medication and psychotherapy are significantly more effective than placebo for treatment of major depression, with response rates varying between about 50% and 70%, depending on the patient population. Combined treatment with both psychotherapy and medication is more effective and is indicated for more severe depression. The goal of treatment for depression is complete remission, or resolution of all depressive symptoms, as even mild residual symptoms increase the risk of relapse. First, close follow-up, with visits every 1 to 2 weeks at first and then every 2 to 4 weeks, will enhance adherence and response rates. One third of people prescribed an antidepressant discontinue the medication within 30 days. Frequent visits also allow early identification of side effects that decrease adherence. Patient education about the lag in response to antidepressants and the need to take the medication every day for at least 6 to 12 months is important. If there is little response in 2 to 4 weeks, a dose increase should be considered, and only partial response at 8 weeks should prompt reassessment of the diagnosis, ensuring that the patient is taking the maximal tolerated dose of the antidepressant, and consideration of switching medications, adding an augmentation agent such as lithium, an atypical antipsychotic, or triiodothyronine (T3), or referral to a psychiatrist. Women who have had three or more episodes of major depression should be continued on maintenance antidepressant treatment. Suicide is a feared and tragic outcome of depression and other mental health conditions. Rates of suicide are highest among people aged 45 to 64 years compared with other age groups and in whites, Native Americans, and Native Alaskans compared with other ethnic groups. Risk factors for suicide include depression or other mental health disorders, substance use disorders, a prior suicide attempt, a family history of psychiatric or substance use disorders, family violence including physical or sexual abuse, access to means such as firearms in the house, and exposure to suicidal behavior by others such as family members, peers, or celebrities. This can include asking about whether the woman feels hopeless, has had thoughts that life is not worth living, or thoughts of ending her life, followed by more specific questions about whether she has made specific plans and how far she has gone to carry these out. The physician or staff should call 9-1-1 to have her taken to the nearest emergency room. Eating disorders primarily affect younger people and have their peak onset between the ages of 10 and 19. In a report from the Centers for Disease Control and Prevention (2011), 61% of female high school students reported they were trying to lose weight. In the preceding 30 days, 11% had not eaten in 24 hours or more, 5% took diet pills, powders or supplements, and 4% took laxatives or induced vomiting to avoid weight gain. Many young women with eating disorders are secretive about their disorder, do not view it as a problem, and do not seek treatment for it. Have you recently lost more than one Yes No stone (14 pounds) in a 3-month period Do you believe yourself to be fat when Yes No others say you are too thin Because the woman may not volunteer information about disordered eating, it is important to have a high index of suspicion for eating disorders. Weight loss is achieved by restricting food intake, over-exercising, self-induced vomiting, or use of laxatives, emetics, and diuretics. Anorexia is most common in white teenage girls in industrialized Western societies. Societal pressures and standards of attractiveness for women, which emphasize thinness, have long been considered to increase the risk for anorexia nervosa, and a preoccupation with dieting is common in girls at menarche. Increasing evidence indicates, however, that there is clearly a significant genetic contribution to anorexia nervosa and other eating disorders, with heritability estimates of 50% to 80%. Other risk factors include a history of childhood sexual abuse and psychological traits of low self-esteem, perfectionism, and obsessive thinking. Medical signs and symptoms associated with anorexia nervosa include bradycardia, hypotension, hypothermia, leukopenia, hair loss, skin changes, and constipation. Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health. Significantly low weight is defined as a weight that is less than minimally normal or, for children and adolescents, less than that minimally expected. Intense fear of gaining weight or becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight. This subtype describes presentations in which weight loss is accomplished primarily through dieting, fasting, and/or excessive exercise. Specify if: In partial remission: After full criteria for anorexia nervosa were previously met, Criterion A (low body weight) has not been met for a sustained period, but either Criterion B (intense fear of gaining weight or becoming fat or behavior that interferes with weight gain) or Criterion C (disturbances in self-perception of weight and shape) is still met. In full remission: After full criteria for anorexia nervosa were previously met, none of the criteria have been met for a sustained period of time. The level of severity may be increased to reflect clinical symptoms, the degree of functional disability, and the need for supervision. Recurrent, inappropriate compensatory behaviors in order to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise. The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months. Specify if: In partial remission: After full criteria for bulimia nervosa were previously met, some, but not all, of the criteria have been met for a sustained period of time. In full remission: After full criteria for bulimia nervosa were previously met, none of the criteria have been met for a sustained period of time. Specify current severity: the minimum level of severity is based on the frequency of inappropriate compensatory behaviors (see below). Mild: An average of 1-3 episodes of inappropriate compensatory behaviors per week. Moderate: An average of 4-7 episodes of inappropriate compensatory behaviors per week. Severe: An average of 8-13 episodes of inappropriate compensatory behaviors per week. Extreme: An average of 14 or more episodes of inappropriate compensatory behaviors per week. The binge-eating episodes are associated with three (or more) of the following: 1. The binge eating is not associated with the recurrent use of inappropriate compensatory behavior as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa. Specify if: In partial remission: After full criteria for binge-eating disorder were previously met, binge eating occurs at an average frequency of less than one episode per week for a sustained period of time. In full remission: After full criteria for binge-eating disorder were previously met, none of the criteria have been met for a sustained period of time.
Purchase 10mg simvastatin with mastercard
The positive predictive value of a mass with a spiculated margin is 81% and with irregular shape it is 73% cholesterol levels heart disease buy simvastatin with paypal. Subsequent breast biopsies will find 25% of clusters associated with cancer and 75% with benign disease. Clustered microcalcifications can be associated with intraductal calcifications in areas of necrotic tumor or calcifications within mucin-secreting tumors. This reporting system was devised to standardize mammographic terminology, reduce confusing interpretations, and facilitate the monitoring of outcomes. There are six assessment categories, each associated with a specific risk of cancer. Category 0 is an incomplete assessment and therefore requires additional evaluation, which may include further imaging. The image is further processed and displayed as a gray-scale image that can be displayed in multiple formats. Digital mammography has several advantages compared with conventional film screen mammography. Image manipulation through adjustments in contrast, brightness, and magnification of selected regions enables radiologists to obtain superior views. This technology makes it possible to subtract various layers of computerized imagery in order to examine suspicious areas and improve the ability to detect and diagnose breast carcinoma. Greater contrast resolution allows better screening of women with dense breasts and breast implants. With the ability to manipulate and postprocess the images, subtle abnormalities are increasingly detected. Images can be stored easily for future reference and can be sent electronically to be read at multiple viewing stations, thereby allowing double reading when necessary. The main disadvantages of digital mammography include the cost of the equipment and the reduced spatial resolution compared with film. Digital mammography has been compared with film screen mammography in various studies with little difference reported in cancer detection rates. Although there was no significant difference in overall diagnostic accuracy, digital mammography was more accurate for premenopausal and perimenopausal women. The breast cancer detection rate at 2 years was significantly higher in the full field digital mammography group compared with film screen mammography (0. In the United States, the majority of imaging centers utilize digital mammography. However, it must be noted that film mammography is an acceptable screening method for all women. The lower specificity, less than 65%, is secondary to the overlap in the enhancement pattern of benign and malignant lesions. No randomized trials exist comparing combination ultrasound and mammography versus mammography alone for screening in average-risk women. However, women with dense breasts may benefit from the addition of ultrasound to screening mammography. Ultrasound screening increased the detection of otherwise occult cancers by 37% in a study involving 3626 women age 42 to 67, with dense breasts and no visible abnormalities on mammography. In women with dense breasts as their only risk factor, the American College of Radiology recognizes that ultrasound as an addition to screening mammography may be useful for incremental cancer detection. Ultrasonography of the breast is a highly operator- and reader-dependent test with a great deal of variation among different centers. Ultrasound utilizes sound waves to image tissues and is particularly effective in differentiating cystic from solid masses. The accuracy rate of ultrasound to diagnose a cystic mass is 96% to 100%, which exceeds the combined accuracy of mammography and physical examination. Ultrasound is frequently used to guide needle aspiration, or direct core needle biopsy. In pregnant women or women younger than 30 years old with focal breast symptoms or findings, ultrasound is the first line of imaging. In summary, ultrasound should not be used as a sole imaging technique for breast disease. It is useful for contrast-enhancing lesions, for lesions close to the chest wall, and for studying the most medial and lateral aspects of the breast. It is sometimes used for preoperative wire location of a mass that is difficult to localize by mammography. The 3D image is created by taking multiple low-dose images per view along an arc over the breast. The compressed breast remains stationary while the x-ray tube rotates approximately 1 degree for each image in a 15- to 50-degree arc. The 11 to 49 acquired images are projected as cross-sectional "slices" of the breast, with each slice typically 1-mm thick. Thin slice reconstruction with tomosynthesis allows true lesions to be distinguished from spurious lesions caused by overlapping structures identified on routine mammography. Breast tomosynthesis has been approved in the United States for breast cancer screening, Obstetrics & Gynecology Books Full 15 Breast Diseases when used in combination with mammography. Friedewald and colleagues compared screening by digital mammography with digital mammography plus tomosynthesis (Friedwald, 2014). Disadvantages of tomosynthesis include increased radiation exposure and reading time. The radiation exposure is approximately double the usual radiation dose associated with mammography and can be even greater in patients with dense or thick breasts. Facilities with newer techniques that have a lower radiation dose are expensive and not widely available. This triple test has been advocated as a reliable alternative to excisional biopsy. If the physical exam, imaging findings, and cytologic evaluation of the mass all confirm the same benign process, the mass can be followed. However, if any of these assessments indicate cancer, a biopsy should be performed. The false-negative rate of triple test diagnosis approaches that of surgical biopsy, and the false-positive rate is comparable with that for frozen section. Common indications for tissue biopsy include bloody discharge from the nipple, a persistent three-dimensional mass, or suspicious mammography. Additionally, nipple retraction or elevation and skin changes, such as erythema, induration, or edema, are also indications for breast biopsy. Imaging should precede biopsy, as the inflammation and bleeding that can occur secondary to the biopsy may significantly impair needed visualization of the breast with imaging. The choice of initial biopsy methods is dependent on the lesion characteristics, including whether it is palpable, and location. The least invasive technique that is likely to produce a diagnostic specimen should be used. It is appropriate for new, wellcircumscribed, usually tender masses that are thought to be simple (not complex) cysts. If the lesion is not palpable, ultrasound guidance may be used to localize the lesion. The skin over the breast is the most sensitive area, but the breast tissue itself has few pain fibers. Some providers choose to inject a small amount of local anesthetic (1 mL of 1% lidocaine). The breast mass is secured with one hand, and the other hand introduces the needle attached to a 10- or 20-mL syringe into the mass. If the mass is found to be a cyst, the procedure can be converted into a cyst aspiration. The color of the fluid obtained via aspiration varies from clear to grossly bloody. However, if the aspirated fluid is clear, it is not necessary to submit it for cytologic evaluation, and the patient is to be reevaluated in 1 to 2 months. If the cyst recurs, imaging should be performed to confirm their benign nature and reaspiration performed under ultrasound guidance. Less than 20% of cysts recur after a single aspiration, and fewer than 10% recur after two aspirations. A biopsy should be performed on cysts that recur within 2 weeks or that necessitate more than one repeat aspiration. In cases of a solid mass, a fixed specimen is obtained and submitted for cytopathologic evaluation.
Buy discount simvastatin 10 mg
Inherited genetic abnormalities are most probably not a cause of ectopic pregnancy either cholesterol rda discount simvastatin master card. Several epidemiologic studies indicate that cigarette smoking is associated with about a twofold increased risk of ectopic pregnancy, even when the data were controlled for the presence of other risk factors. The risk of ectopic pregnancy was directly related to the number of cigarettes smoked per day, with a fourfold increased risk noted among women who smoked 30 or more cigarettes per day. Known risk factors for ectopic pregnancy, presented as odds ratios and attributable risk, are depicted in Table 17. The agglutination of the plicae (folds) of the endosalpinx produced by salpingitis can allow passage of sperm but prevent the normal transport of the larger morula. The morula can be trapped in blind pockets formed by adhesions of the endosalpinx. Its morphologic sequelae account for about half of the initial episodes of ectopic pregnancy. However, in about 40% of cases the cause cannot be determined and is presumed to be a physiologic disorder resulting from the delay of passage of the embryo into the uterine cavity. Ovulation from the contralateral ovary has been implicated as a cause of the delay of blastocyst transport, and it has been suggested that contralateral ovulation occurs in about one third of tubal pregnancies, although this has not been confirmed. Another possibility in the etiology of ectopic pregnancy is a hormonal imbalance; an elevated circulating level of either estrogen or progesterone can alter normal tubal contractility. An increased rate of ectopic pregnancies has been reported in women who conceive with physiologically and pharmacologically elevated levels of progestogens. Odds ratios for ectopic pregnancy (compared with deliveries) and attributable risks of the principal risk factors. Risk factors for ectopic pregnancy: a comprehensive analysis based on a large case-control, population-based study in France. Risk attributable to history of genital infection and tubal surgery together is 0. The risk of ectopic after acute salpingitis increased both with the number of episodes of infection and with the increasing age of the women at the time of infection. The odds ratios for ectopic pregnancy after two and after three or more episodes of chlamydial infection were 2. Endometriosis Inflammation of the fallopian tubes due to conditions such as endometriosis is a risk factor for ectopic pregnancy. Compared with women without endometriosis, women with endometriosis had two times the risk for ectopic pregnancy (relative risk 1. It is likely that adhesions between the tubal serosa and bowel or peritoneum may interfere with normal tubal motility and cause ectopic pregnancy because, as reported, 17% to 27% of women with ectopic pregnancy have had previous abdominal surgical procedures not involving the oviduct. On the other hand, neither endometriosis nor congenital anomalies of the tube have been associated with an increased incidence of ectopic pregnancy. Tubal Surgery An operative procedure on the tube itself is a cause of ectopic pregnancy whether the tube is morphologically normal, as occurs with sterilization procedures, or abnormal, as occurs with post salpingitis reconstructive surgery. The incidence of ectopic pregnancy occurring after salpingoplasty or salpingostomy procedures to treat distal tubal disease ranges from 15% to 25%, probably because the damage to the endosalpinx remains. The rate of ectopic pregnancy after reversal of sterilization procedures is lower, about 4%, because the tubes have not been damaged by infection. Women who have had a prior ectopic pregnancy, even if treated medically or by unilateral salpingectomy, are at increased risk for having a subsequent ectopic pregnancy. Of women who conceive after having one ectopic pregnancy, about 25% of subsequent pregnancies are ectopic. The rates of recurrent ectopic pregnancy after single dose methotrexate, salpingectomy and linear salpingostomy are 8%, 9. In two large series of women with ectopic pregnancy, 7% had a history of a prior ectopic pregnancy. This is likely due to abnormal tubal morphology and impaired function of the fimbriae. In an analysis of the long-term risk of pregnancy after tubal sterilization reported by Peterson and coworkers, it was found that within 10 years after the procedure, the cumulative life table probability of pregnancy was 1. These investigators reported that for all 143 pregnancies occurring after tubal sterilization, 43, or 32. Several investigators have reported that if pregnancy occurred after tubal sterilization by laparoscopic fulguration, the ectopic pregnancy rate was as high as 50%. Such fistulas can be demonstrated radiographically in about 11% of women after laparoscopic electrocoagulation. Peterson and colleagues reported that within 10 years after the sterilization procedure, twice as many women sterilized by bipolar coagulation had ectopic pregnancies than those sterilized with metal clips or silicone bands. In women who have an ectopic pregnancy after sterilization with the use of electrosurgery, because the site of the fistula usually cannot be determined clinically, salpingectomies should be carried out. Women who use this method of contraception have about twice the risk of ectopic pregnancy (7. These reports indicate that increased levels of estrogen, as well as of progesterone, interfere with tubal motility and increase the chance of ectopic pregnancy. Ectopics occur in about 1% of pregnancies that develop after in vitro fertilization and embryo transfer. The reason for this increased incidence is likely due to one or more of several factors: increased sex steroid hormone levels, the presence of proximal tubal disease (although the ratio is similar in women with normal tubes), and flushing an embryo directly into the tube. In vitro fertilization has been associated with an increased risk of ectopic pregnancy. The ectopic pregnancy rate was also noted to be associated with multiple embryo transfer. About 12% of tubal gestations occur in the isthmus and 5% to 11% in the fimbrial region. Although Breen considered pregnancies located in the cornual area of the uterus to be uterine in origin, they are in fact pregnancies implanted in the interstitial portion of the tube. A true cornual pregnancy is one located in the rudimentary horn of a bicornuate uterus, and this occurrence is quite rare. About 1 in 200 ectopic pregnancies are true ovarian pregnancies that fulfill the four criteria originally described by Spiegelburg: 1. Many women with ovarian pregnancies are believed to have a ruptured corpus luteum cyst, and the correct diagnosis was made during the surgical procedure only 28% of the time. The hemorrhagic mass (ovarian ectopic) should be located adjacent to the corpus luteum, never within it. Ovarian pregnancy is also associated with profuse hemorrhage, with 81% of reported to have a hemoperitoneum greater than 500 mL. Nevertheless, most can be successfully treated by ovarian resection and not oophorectomy. Medical management of interstitial pregnancy with high beta selective human chorionic gonadotropin. For the latter diagnosis to be made, the following three criteria originally set forth by Studdiford must be present: (1) the tubes and ovaries must be normal, with no evidence of recent or past injury; (2) there must be no evidence of a uteroplacental fistula; and (3) the pregnancy must be related only to the peritoneal surface and early enough in gestation to eliminate the possibility of secondary implantation after primary tubal nidation (Studdiford, 1942). An unusual type of primary abdominal pregnancy may implant in the spleen or liver and produce massive intraperitoneal hemorrhage. Obstetrics & Gynecology Books Full 17 Ectopic Pregnancy the prognosis for fetal survival in abdominal pregnancy is poor, found to be 11%, and is difficult to diagnose. Once the diagnosis is established, a laparotomy with removal of the fetus should be performed immediately to prevent a possible fatal hemorrhage. On occasion, when the placenta is tightly adherent to bowel and blood vessels, it should be left in the abdominal cavity. However, there may be symptoms of abdominal pain and intermittent fever for many months as well as possible partial bowel obstruction and abscess formation. Thus, it is highly desirable, if it is surgically feasible, to remove the placenta entirely. Partial removal also may result in massive hemorrhage, so the surgical approach and decision making are challenging and critical.
Fleawort (Black Psyllium). Simvastatin.
- What other names is Black Psyllium known by?
- How does Black Psyllium work?
- Are there safety concerns?
- Cancer, diarrhea, irritable bowel syndrome (IBS), and other conditions.
- Dosing considerations for Black Psyllium.
- Are there any interactions with medications?
- Improving high cholesterol.
- Constipation.
- What is Black Psyllium?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96139
Buy simvastatin 5mg on line
There are many reasons why people self-harm; only in a small proportion of cases do people who self-harm wish to bring about their own death cholesterol ratio canada discount simvastatin 10 mg with mastercard. Aggression and violence Although individuals with mental health problems are more likely to be victims of violence than perpetrators (Monahan et al. You should also ask people about their forensic history, as convictions for certain offences may give clues to their propensity towards violence. Vulnerability and neglect Certain mental health problems expose individuals to a higher risk of self-neglect. Homelessness and use of alcohol or illicit drugs also make people with mental health problems vulnerable to being abused by others. During your assessment, it is therefore important to look for signs of neglect or abuse: this could include unexpected weight loss, social withdrawal, dishevelled appearance and/or unexplained injuries. Many people with mental health problems are vulnerable due to their symptoms or wider circumstances. If you think somebody may be the victim of abuse, you must document your concerns carefully and refer appropriately to your local safeguarding team. It is therefore important to routinely ask people whether they have children and/or caring responsibilities (making a note of names and dates of birth) and seek safeguarding advice if they also present with the toxic trio features. If you fear that a child or vulnerable person is at significant risk of harm, you have a statutory duty to report this immediately; infants and children with disabilities are at particularly high risk. Nobody will ever criticise you for raising concerns about the safety of a child or vulnerable person; however, the potential consequences of ignoring such concerns do not bear thinking about. Physical health and investigations the beginning of this chapter alluded to the fact that the distinction between mental and physical health is an arbitrary one and has led to people with mental health problems being stigmatised and subjected to a host of healthcare inequalities. Mimickers Several mental health problems share symptoms with physical health conditions. Acute changes in mental state and/or impaired consciousness may also suggest an underlying physical cause. Individuals presenting with mental health symptoms should therefore undergo some basic investigations as a routine part of the assessment process. For instance, an individual with a depressive illness may present with headaches, chest pains and limb weakness. People with somatoform disorders are usually convinced that their symptoms have a physical cause and sometimes undergo a series of unnecessary physical investigations before the underlying psychological stress is identified. Somatisation is particularly prevalent among children and young adults and should always be considered when somebody presents with medically unexplained symptoms. Firstly, some psychiatric conditions have been shown to have a direct link to physical illness; for instance, being diagnosed with severe mental illness is an independent risk factor for cardiovascular disease (De Hert et al. Secondly, many of the medications used to treat mental health problems are also associated with physical ill-health; for example, some antipsychotic drugs are linked to type 2 diabetes mellitus and metabolic syndrome (Hasnain et al. Thirdly, people with mental health problems have been shown to be more likely to engage in unhealthy lifestyle behaviours, such as smoking, excessive alcohol consumption and poor diet. Health promotion Every time you conduct a mental health assessment, you should include an evaluation of physical health and a health behaviours discussion. By doing this you will also be in a position to provide health promotion and individualised advice about smoking cessation, exercise, healthy eating, health screening and access to other services, such as dentists and opticians. Specific mental health assessments Alcohol and substance misuse People who present to healthcare professionals with substance misuse problems represent only a small proportion of the people who use alcohol and/or drugs. Alcohol and substance use can therefore be seen as existing on a continuum, from abstinence and recreational use at one end to harmful use and dependence at the other. Since substance misuse remains extremely stigmatised in most cultures, it is important to adopt a nonjudgemental attitude towards people who admit to misusing alcohol and/or illicit drugs. When assessing somebody with a substance or alcohol misuse problem, it is important to determine what they are using (remember that people can become dependent on prescribed and over-the-counter medications as well as illicit drugs), how much they are using, and how often they are using them. Features of dependence include 165 Clinical examination skills for healthcare professionals cravings, tolerance (needing to use more of the substance to achieve the same effect), withdrawal symptoms and unsuccessful attempts to reduce. For instance, cocaine use is associated with euphoria, over-talkativeness, reduced appetite, confusion, paranoia, anxiety and hallucinations. In the long term, substance misuse also places individuals at increased risk of several psychiatric conditions. For instance, individuals who are alcohol dependent are more likely than the general population to develop major depression (Davidson 1995). Where possible, it is therefore advisable to assess people when they are drug-free. Eating disorders It is important to recognise and treat eating disorders early on because they are associated with impaired growth in children and high mortality rates. The two eating disorders most commonly diagnosed in the United Kingdom are anorexia nervosa and bulimia nervosa; both these conditions are driven by an intense preoccupation with food and share many of the same signs and symptoms. To assess somebody who presents with disordered eating, you should therefore enquire about their body image, eating patterns. Asking somebody what they eat in a typical day/week can also be very enlightening. Since eating disorders are associated with a large range of physical health complications, it is important to take a detailed medical history. For instance, endocrine problems associated with anorexia nervosa can cause menstrual problems (in women) and erectile dysfunction (in men). Since early detection and treatment of eating disorders improves prognosis, various assessment tools and screening tests are available for assessors to use. This questionnaire does not diagnose eating disorders but identifies people who are likely to need a more in-depth assessment. Dementia Dementia is an umbrella term for several conditions associated with a global decline in brain functioning. Assessing people with dementia can be difficult because the condition can present with a varied range of symptoms, depending on which areas of the brain have been affected. Commonly reported symptoms include memory loss, impaired judgement and difficulties using and understanding language. Asking about the chronology of these symptoms can also give an indication of the type of dementia somebody may be suffering from. It is also important to remember that delirium (an acute confusional state) can present in a similar way to dementia and should be ruled out before a diagnosis of dementia is made. This 30-point questionnaire takes approximately ten minutes to complete and examines various different areas of cognitive function. You do not need any specific equipment or training to be able to conduct this test and if somebody scores less than 24 marks out of 30 you should consider referring them for a specialist cognitive assessment. Children and young people Although many psychiatric disorders start in early life, assessing the mental health of children and young people can be difficult due to the different ways in which young 167 Clinical examination skills for healthcare professionals people communicate mental and emotional distress. When conducting a mental health assessment, it is also important to take into account the developmental stage of the child or young person you are assessing. This is particularly significant when diagnosing specific neurodevelopmental disorders such as autism or hyperkinetic disorder. Failure to meet key developmental milestones is a good indication that a child requires a more detailed investigation of their mental and physical health. Taking a detailed developmental history and close liaison with other professionals (such as school nurses and health visitors) are therefore essential aspects of the assessment process. Uncharacteristic school refusal can be one of the first indicators of mental distress in young people. Asking a child about school can therefore give a useful insight into their level of functioning. In order to uphold your responsibility to keep children safe, it is also important to ask children and young people about abuse and bullying (including cyber-bullying). As highlighted earlier in this chapter, self-harming is becoming increasingly common among young people and so asking about this should also be a routine part of your assessment. Intellectual disability Intellectual disabilities (previously known as learning disabilities or mental retardation) affect approximately 20 per 1000 people in the United Kingdom. Although 30 to 50% of people with intellectual disabilities will experience comorbid mental health problems (a higher proportion than the general population) (Smiley 2005), assessing the mental health of people with intellectual disabilities can be challenging. Firstly, it is important to be mindful of the language you use to ask questions: use short sentences where possible and avoid asking leading questions or using metaphors and/or jargon. Also, remember that some people will need longer to respond to your questions or additional support to share their symptoms. For those people who are unable to communicate verbally, you should pay attention to the non-verbal ways in which people 168 Mental health assessment express their distress. Where possible, make sure that you assess somebody with an intellectual disability in a calm and non-threatening environment; healthcare settings can be busy and loud, which may make some people with intellectual disabilities feel anxious, agitated or vulnerable.
Order 20mg simvastatin otc
The disease is rare before puberty; 98% of cases are found in reproductive-age women cholesterol medication in powder form order simvastatin from india, and most all disease regresses after menopause. The patient undergoes great emotional distress as this condition is both painful and is associated with a foul-smelling discharge. The differential diagnosis of hidradenitis suppurativa includes simple folliculitis, Crohn disease of the vulva, pilonidal cysts, and granulomatous sexually transmitted diseases. Note hyperkeratosis with extensive basal layer destruction and a dense lichenoid infiltrate at the dermoepidermal junction. It is now known to be a multisystem disease with potential Obstetrics & Gynecology Books Full 18 Benign Gynecologic Lesions involvement. The early phase of the disease involves infection of the follicular epithelium, with what first appears as a boil. Erythema, involvement of multiple follicles, chronic infections that burrow and form cysts that break open and track through subcutaneous tissue, creating odiferous and painful sinuses and fistula in the vulva. The chronic scarring, fibrosis, and hyperpigmentation with foul-smelling discharge and soiling of underclothes lead to a socially debilitating condition. Early on in the disease process there are small furuncles and folliculitis, for which topical and oral clindamycin is usually effective in the short term, usually requiring a 3-month course of antibiotics. Unfortunately, relapse is common; if treatment with long-term antibiotic therapy and topical steroids is unsuccessful, other medical therapies have included antiandrogens, isotretinoin, and cyclosporine. The treatment of refractory cases is aggressive, wide operative excision of the infected skin. Two of the most common causes of edema of the vulva are secondary reactions to inflammation or to lymphatic blockage. Vulvar edema is often recognized before edema in other areas of the female body is noted. The loose connective tissue of the vulva and its dependent position predispose to early development of pitting edema. Systemic causes of vulvar edema include circulatory and renal failure, ascites, and cirrhosis. Vulvar edema also may occur after intraperitoneal fluid is instilled to prevent adhesions or for dialysis. Local causes of vulvar edema include allergy, neurodermatitis, inflammation, trauma, and lymphatic obstruction caused by carcinoma or infection. Infectious diseases that are associated with vulvar edema include necrotizing fasciitis, tuberculosis, syphilis, filariasis, and lymphogranuloma venereum. Vulvar Pain Syndromes: Vulvar Vestibulitis, Vestibulodynia, and Dysesthetic Vulvodynia Vulvar pain, vulvodynia, is one of the most common gynecologic problems, reported by up to 16% of women in the general population (Stockdale, 2014). Vulvodynia has been defined by the International Society for the Study of Vulvovaginal Disease as vulvar discomfort, most often described as burning pain, occurring in the absence of relevant visible findings or a specific clinically identifiable, neurologic disorder (Moyal-Barracco, 2004). The disease has a wide spectrum of symptomatology and response to treatment; therefore causation is most likely multifactorial. A complete history identifying the onset of pain, other associated symptoms, duration of pain, medical and sexual history, treatments tried, allergies, and triggers for pain should be taken. Examination using cotton swab testing to identify areas of pain as well as pain intensity as described in the Vulvodynia Guideline (Haefner, 2005) is helpful to follow patients and response to treatment over time. Large populationbased studies have noted that symptoms wax and wane, with many women having spontaneous remission. Interestingly, in the control group, approximately 2% of women developed symptoms (Reed, 2008). Vulvar pain syndrome is further subdivided into two categories: vestibulodynia and dysesthetic vulvodynia. The two conditions have a significant amount of overlap, although different etiologies and clinical course. In general, vestibulodynia is found in younger women, most commonly white, with onset shortly after puberty through the mid-20s. Dysesthetic vulvodynia is most common in peri- and postmenopausal women who have rarely if ever had previous vulvar pain. The differential diagnosis of vulvar pain includes neurologic diseases, herpes simplex infection, chronic infections, abuse, pain syndromes, neoplasia, contact dermatitis, and psychogenic causes. Chronic pain is considered to be part of the vulvodynia spectrum, once the diagnoses of infection, invasive disease, and inflammation have been excluded. Severe chronic pain can be socially debilitating, and these patients have a wide spectrum of associated affective symptomatology as well. Women with vulvodynia have greater psychologic distress than women who have other vulvar problems. Importantly, these psychologic concerns must be addressed as part of the therapeutic management. Vestibulodynia involves the symptom of allodynia, which is hyperesthesia, a pain that is related to nonpainful stimuli. The diagnostic maneuver to establish the presence of allodynia is to lightly touch the vulvar vestibule with a cotton-tipped applicator. Additionally, patients with vestibulodynia experience intolerance to pressure in the vulvar region. The intolerance to pressure may be caused by tampon use, sexual activity, or tight clothing. Some authors have suggested that symptoms be present for at least 6 months prior to establishing the diagnosis. The symptoms may appear around the time of first intercourse, or within the next 5 to 15 years. Studies of women with vulvar vestibulodynia have found no increased incidence of sexual abuse compared with controls. Some even noted an increased nerve density and normal estrogen receptors compared with controls. In contrast, other investigators have noted an increase in alphaestrogen receptors. Theories regarding the etiology cite potential immunologic, and infectious factors, though no theory has been proved to date. Oral contraceptive use in younger women and hormone replacement in older women have no association with vestibulodynia. Vulvar dysesthesia, vulvodynia, is a non-localized pain that is constant (not provoked by touch), mimicking a neuralgia. Allodynia is rarely noted, and erythema is also much less common than in vulvar vestibulodynia. Dyspareunia is currently present but has usually not been present prior to the development of dysesthesia. Similar to women with vulvar vestibulodynia, there is not an increased history of sexual abuse compared with controls. Women with dysesthesia also have an increased incidence of chronic interstitial cystitis. A, Redness localized to the right Bartholin duct opening and, below it, vulvar vestibulitis. B, Discrete localized periglandular erythema in vulvar vestibulitis in a 60-year-old woman. Patients are often depressed and anxious, but this is thought to be a secondary reaction to the chronic pain. Prior to the diagnosis, one should exclude infection from atypical Candida (which may not be obvious on inspection and should be diagnosed by culture), as well as exclusion of infection by group B streptococcus. Some would recommend that prior to extensive treatment a punch biopsy should be obtained to rule out dermatitis presenting atypically, including lichen sclerosis. The therapeutic approach for these two conditions emphasizes a sensitivity to the debilitating social aspects of the problem. Similar to other chronic pain syndromes, tricyclic antidepressants or gabapentin have been found to be successful in several series. Doses of gabapentin range from 300 to 3600 mg, usually given with increasing doses every week. Most authors start at 300 mg daily, increase to 300 mg twice daily, then three times a day, then 600 mg three times per day to 900 three times per day and so on; the average affective dose is approximately 1800 mg a day. Zolnoun and coworkers reported on 61 women treated successfully for vulvar vestibulitis with 5% lidocaine ointment nightly for a period of 6 to 8 weeks (Zolnoun, 2003). In the past, women with refractory vulvar vestibulitis have been treated with surgical removal of the vulvar vestibule and reapproximation of tissue. The surgery is difficult, with a significant complication rate, but results are generally good.
Discount simvastatin 10mg
The oviduct should not be removed in these cases because it will return to normal size after the paratubal cyst is excised cholesterol in food vs in blood buy genuine simvastatin on line. In one retrospective 10-year review of 168 women with parovarian tumors, three low-grade malignant neoplasms were found. These malignancies were in women of reproductive age who had cysts greater than 5 cm in diameter with internal papillary projections. The authors cautioned that the differentiation between benign and malignant parovarian masses cannot be made by external examination of the cyst. More recent theories of epithelial ovarian carcinogenesis suggest that serous, endometrioid, and clear cell carcinomas are derived from the fallopian tube and the endometrium rather than the ovarian surface epithelium (Erickson, 2013). Paratubal cysts may grow rapidly during pregnancy, and most of the cases of torsion of these cysts have been reported during pregnancy or the puerperium. Tubal torsion usually accompanies torsion of the ovary, as they have a common vascular pedicle. The degree of tubal torsion varies from less than one turn to four complete rotations. However, it occurs also in preadolescent children, especially when part of the tube is enclosed in the sac of a femoral or inguinal hernia. Prominent intrinsic causes include congenital abnormalities, such as increased tortuosity caused by excessive length of the tube, and pathologic processes, such as hydrosalpinx, hematosalpinx, tubal neoplasms, and previous operation, especially tubal ligation. Torsion of the fallopian tube following tubal ligation is usually of the distal end. Extrinsic causes of tubal torsion are ovarian and peritubal tumors, adhesions, trauma, and pregnancy. The most important symptom of tubal torsion is acute lower abdominal and pelvic pain. The onset of this pain is usually sudden, but it may also be gradual, and the pain is usually located in the iliac fossa, with radiation to the thigh and flank. The duration of pain is generally less than 48 hours, and it is associated with nausea and vomiting in two thirds of the cases. Unless there is associated torsion of the ovary, a specific mass is usually not palpable on pelvic examination. The preoperative diagnosis of tubal torsion is made in less than 20% of reported cases. However, the number of cases diagnosed preoperatively has increased dramatically with the use of vaginal ultrasonography. Because of the severity of the pain, a wide differential diagnosis of abdominal and pelvic pathology must be considered. The differential diagnosis includes acute appendicitis, ectopic pregnancy, pelvic inflammatory disease, and rupture or torsion of an ovarian cyst. Exploratory operation determines the extent of hypoxia and the choice of operative techniques. It may be possible to restore normal circulation to the tube by manually untwisting it. The task of the clinician is to determine whether the mass should be removed or may be managed expectantly. The general factors used to consider removal include the symptoms produces by the mass, the chances that the mass is malignant, and the likelihood of spontaneous resolution. Follicular cysts are frequently multiple and may vary from a few millimeters to as large as 15 cm in diameter. A minimum diameter to be considered as a cyst is generally considered to be between 2. Follicular cysts are not neoplastic and are believed to be dependent on gonadotropins for growth. Solitary cysts may occur during the fetal and neonatal periods and rarely during childhood, but there is an increase in frequency during the perimenarcheal period. Wolf and coworkers studied 149 postmenopausal women and found simple cysts ranging in size from 0. Large solitary follicular cysts in which the lining is luteinized are occasionally discovered during pregnancy and the puerperium. Multiple follicular cysts in which the lining is luteinized are associated with either intrinsic or extrinsic elevated levels of gonadotropins. Interestingly, reproductive-age women with cystic fibrosis appear to have an increased propensity for developing individual follicular cysts. Follicular cysts are translucent, thin-walled, and are filled with a watery, clear to straw-colored fluid. If a small opening in the capsule of the cyst suddenly develops, the cyst fluid under pressure will squirt out. These cysts are situated in the ovarian cortex, and sometimes they appear as translucent domes on the surface of the ovary. Histologically the lining of the cyst is usually composed of a closely packed layer of round, plump granulosa cells, with the spindle-shaped cells of the theca interna deeper in the stroma. In many cysts the lining of granulosa cells is difficult to distinguish, having undergone pressure atrophy. The temporary disturbance in follicular function that produces the clinical picture of a follicular cyst is poorly understood. In the latter circumstance, the incompletely developed follicle fails to reabsorb follicular fluid. Some follicular cysts lose their ability to produce estrogen, and in others the granulosa cells remain productive, with prolonged secretion of estrogens. Occasionally, follicular cysts are better termed follicular hematomas, because blood from the vascular theca zone fills the cavity of the cyst. Most follicular cysts are asymptomatic and are discovered during ultrasound imaging of the pelvis or a routine pelvic examination. The patient may experience tenesmus, a transient pelvic tenderness, deep dyspareunia, or no pain whatsoever. Rarely is significant intraperitoneal bleeding associated with the rupture of a follicular cyst. However, women who are chronically anticoagulated or those with von Willebrand disease may bleed. Occasionally, menstrual irregularities and abnormal uterine bleeding may be associated with follicular cysts, which produce elevated blood estrogen levels. The syndrome associated with such follicular cysts consists of a regular cycle with a prolonged intermenstrual interval, followed by episodes of menorrhagia. Some women with larger follicular cysts notice a vague, dull sensation or heaviness in the pelvis. The initial management of a suspected follicular cyst is conservative observation. The majority of follicular cysts disappear spontaneously by either reabsorption of the cyst fluid or silent rupture within 4 to 8 weeks of initial diagnosis. However, a persistent ovarian mass necessitates operative intervention to differentiate a physiologic cyst from a true neoplasm of the ovary. There is no way to make the differentiation on the basis of signs, symptoms, or the initial growth pattern during early development of either process. Endovaginal ultrasound examination is helpful in differentiating simple from complex cysts and is also helpful during conservative management by providing dimensions to determine if the cyst is increasing in size. When the diameter of the cyst remains stable for greater than 10 weeks or enlarges, a neoplasia should be ruled out. Oral contraceptives may be prescribed for 4 to 6 weeks for young women with adnexal masses. This therapy removes any influence that pituitary gonadotropins may have on the persistence of the ovarian cyst. In one series, 80% of cystic masses 4 to 6 cm in size disappeared during the time the patient was taking oral contraceptives. However, randomized prospective trials found no difference in the rate of disappearance of functional ovarian cysts between the group that received oral contraceptives and the control group, perhaps because so many cysts will resolve spontaneously. The evaluation of an asymptomatic cyst, found incidentally, is based on the principle that the cyst should be removed if there is any suspicion of malignancy. Suspicion may develop because of history, including family history, patient age, and other nongynecologic signs and symptoms.