Purchase cafergot 100 mg with visa
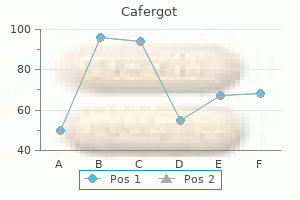
According to the mechanical hypothesis pain treatment medicine clifton springs ny order cafergot 100 mg otc, intraluminal gas enters the bowel wall under pressure through a defect in the intestinal mucosa that may result from direct trauma or increased intraluminal pressure. The plausibility of this explanation, however, is diminished by the absence of a connection between the mucosa and the cysts207 the bacterial hypothesis suggests that the cysts are caused by hydrogen-producing bacteria, either by local invasion of the intestinal wall, or by excess production of hydrogen in the colon lumen resulting from fermentation of ingested carbohydrates, followed by diffusion into an intramural gas bubble. The most common symptoms are diarrhea (68%), mucus discharge (68%), rectal bleeding (60%), and constipation (48%), although it is not always clear that the observed pneumatosis is responsible for the reported symptoms. The endoscopic appearance is of multiple cysts, which vary in size from a few millimeters to several centimeters. Because recurrences of neutropenic enterocolitis are common when chemotherapy is restarted, right hemicolectomy is recommended before chemotherapy is resumed. This uncommon disorder is characterized by multiple gasfilled cysts, which are located in the submucosa and subserosa of the intestine. Symptomatic patients may be treated successfully by breathing high-flow oxygen or by use of hyperbaric oxygen, especially in resistant cases209; high oxygen levels lead to replacement of hydrogen by oxygen within the cysts and a corresponding reduction in their size. Metronidazole also has been used to treat pneumatosis coli, supporting the bacterial theory of pathogenesis. Colonic resection is reserved for patients with complications such as intestinal obstruction or massive bleeding. Full references for this chapter can be found on expertconsultcom with each other and have a spongy consistency. On cross-section they appear shiny and honeycombed, and range in size from a few millimeters to several centimeters. Microscopically, the cysts have an endothelial lining; after they collapse, inflammation results with multinucleate giant cells and fibrosis. Subserosal cysts are surrounded by fibrous connective tissue and can produce adhesions between adjacent bowel loops. Pigments of the gastrointestinal tract: a comparison of light microscopic and electron microscopic findings. Histopathology of melanosis coli and determination of its associated genes by comparative analysis of expression microarrays. Melanosis coll; experimental observations on its production and elimination in twenty-three cases. Anthranoid laxative use is not a risk factor for colorectal neoplasia: results of a prospective case control study. Chemical colitis caused by hydrogen peroxide enema in a child: case report and literature review. Colitis due to accidental alcohol enema: clinicopathological presentation and outcome. Use of oral sodium phosphate colonic lavage solution by Canadian colonoscopists: pitfalls and complications. Long-term budesonide treatment of collagenous colitis: a randomised, double-blind, placebo-controlled trial. Low-dose budesonide for maintenance of clinical remission in collagenous colitis: a randomised, placebo-controlled, 12-month trial. Proctitis cystica profunda and radiation fibrosis in the rectum of the female Wistar rat after X irradiation: a histopathological study. Ultra-low anterior resection with coloanal anastomosis for recurrent rectal prolapse in a young woman with colitis cystica profunda. Embolotherapy of a dieulafoy lesion in the cecum: case report and review of the literature. Solitary rectal ulcer syndrome: clinical features, pathophysiology, diagnosis and treatment strategies. Fecal evacuation disorder among patients with solitary rectal ulcer syndrome: a case-control study. Behavioural therapy (biofeedback) for solitary rectal ulcer syndrome improves symptoms and mucosal blood flow. Transrectal ultrasound study of the pathogenesis of solitary rectal ulcer syndrome. Pneumatosis cystoides intestinalis and high breath H2 excretion: insights into the role of H2 in this condition. Laparoscopic rectopexy for solitary rectal ulcer syndrome without overt rectal prolapse. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. Medical treatment in the management of deep endometriosis infiltrating the proximal rectum and sigmoid colon: a comprehensive literature review. Flare-up of endometriosis induced by gonadotropin-releasing hormone agonist leading to bowel obstruction. Does Computed Tomography-based virtual colonoscopy improve the accuracy of preoperative assessment based on Magnetic Resonance imaging in women managed for colorectal endometriosis Robot-assisted surgery for the radical treatment of deep infiltrating endometriosis with colorectal involvement: short- and mid-term surgical and functional outcomes. An electron-microscopic study: demonstration of bacilliform organisms in malacoplakic macrophages. The histochemical features of the MichaelisGutmann body and a consideration of the pathophysiological mechanisms of its formation. Defect in digestion of phagocytized material due to impaired vacuolar acidification Malakoplakia: evidence for monocyte lysosomal abnormality correctable by cholinergic agonist in vitro and in vivo. Reversal of clinical and leukocyte abnormalities after withdrawal of prednisone and azathioprine. A case of pseudotumoral malakoplakia following pathologic complete response in rectal cancer. Microscopic colitis and colorectal neoplastic lesion rate in chronic nonbloody diarrhea: a prospective, multicenter study. Incidence, prevalence, and temporal trends of microscopic colitis: a systematic review and metaanalysis. The epidemiology of microscopic colitis in Olmsted County from 2002 to 2010: a population-based study. The epidemiology of microscopic colitis: a 10-year pathology-based nationwide Danish cohort study. The morphologic features of diversion colitis: studies of a pediatric population with no other disease of the intestinal mucosa. Short-chain fatty acids in the human colon: relation to gastrointestinal health and disease. Relationship between the severity of diversion colitis and the composition of colonic bacteria: a prospective study. Histological and histochemical changes in the colon mucosa after ureterosigmoidostomy or colonic conduit. Diversion colitis: histological features in the colon and rectum after defunctioning colostomy. Pathophysiology, clinical presentation and management of diversion colitis: a review of current literature. Effect of butyrate enemas on gene expression profiles and endoscopic/histopathological scores of diverted colorectal mucosa: a randomized trial. Treatment of diversion colitis with 5-aminosalicylic acid enemas: comparison with betamethasone enemas. Intraluminal irrigation with fibers improves mucosal inflammation and atrophy in diversion colitis. Endoscopic treatment of bleeding diversion pouchitis with high-concentration dextrose spray. A national snapshot of the surgical management of deep infiltrating endometriosis of the rectum and colon in France in 2015: a multicenter series of 1135 cases. Intestinal obstruction caused by endometriosis: endoscopic stenting and expedited laparoscopic resection avoiding stoma. Bowel preparation improves the accuracy of transvaginal ultrasound in the diagnosis of 85. Clinical features and treatment responses in pediatric lymphocytic and collagenous colitis. Incidence, clinical presentation, and associated factors of microscopic colitis in Northern France: a population-based study. The epidemiology of microscopic colitis: a population based study in Olmsted County, Minnesota. Decreased colorectal cancer and adenoma risk in patients with microscopic colitis. Lymphocytic ("microscopic") colitis: a comparative histopathologic study with particular reference to collagenous colitis.
Buy cafergot 100 mg low cost
Alternatively pain treatment for carpal tunnel syndrome purchase online cafergot, the operator may gently massage the submandibular gland, to express some saliva at the orifice. Conventional sialography has a failure rate of up to 14%, typically higher for submandibular sialography and usually secondary to inability to cannulate the duct. The procedure may also displace a retrievable stone to a deeper section of the gland, making its extraction difficult. In these settings, sialographic images will demonstrate an opacified salivary duct leading to a radiolucent filling defect, corresponding to the obstructing sialolith. Frequently, the main salivary duct is dilated immediately proximal to the obstructing sialolith. One may also observe luminal irregularities and focal narrowing of the main duct, indicating the presence of stenosis. Sialoadenitis and sialodochitis are consequences of several inflammatory conditions that affect the salivary glands, including sequela of viral or bacterial infections. Acute suppurative sialoadenitis affects the parotid gland with greater frequency than the submandibular gland and sialography is contraindicated during the acute phase of the illness. Such alterations of the normal ductal anatomy are readily demonstrated on conventional sialography, which reveals a beaded, sausage-shaped irregular dilatation of the involved duct, a classic imaging finding indicative of sialodochitis. Chronic sialoadenitis caused by these conditions will be seen on sialography as pruned, truncated main ducts, dilated central ducts (sialectasia), and punctate or globular intraglandular fluid collections opacifying small cavities within distorted and expanded acini. On rare occasions, while performing sialography to investigate a suspected salivary duct stenosis, sialographic findings that suggest the presence of a salivary tumor may be encountered. In these settings, the typical arborization pattern of intraglandular opacification will be distorted by the mass, causing smooth displacement of the intraglandular branches. The sialogram will reveal an area of relative paucity of branches that appear attenuated and smoothly displaced by the intraglandular tumor. Malignant lesions have a greater propensity for invading the ductal system and, on sialography, they may present as areas of absent parenchymal opacification with more irregular distortion and displacement of the adjacent ducts. Such 3D postprocessing has also been used to create virtual sialendoscopic views that serve as a screening exam of ductal anatomy in preparation for ensuing sialendoscopy or surgical intervention. This imaging modality has sensitivity and specificity comparable with more conventional imaging studies for detection of submandibular sialoliths. Considerations should be made for patient comfort given the confined space and loud noise the patient will experience. Sequences are rapidly acquired in order to avoid artifacts from repeated swallowing-related movement. In these patients, distention of the ductal lumen with contrast may be necessary and visualization of the duct is best achieved with traditional sialography. These images may be post-processed with multiplanar reconstruction for optimal assessment of the main salivary duct and proximal intraglandular branches. Dynamic imaging is performed before and after stimulation with a secretagogue to assess the quantity and rate of clearance of saliva from the duct. Clinical-radiologic issues in perineural tumor spread of malignant diseases of the extracranial head and neck. On occasion, an invasive neoplasm directly occludes the duct and this might be seen as an abrupt termination of a dilated duct or marked luminal irregularity. Patients affected by salivary gland malignancies and who have undergone surgery or radiation therapy frequently have fibrotic alteration of the remaining salivary tissue, causing distortion of the glandular architecture. In these settings, one may observe ductal strictures, sialoceles, and ductal obstructions. Apparent diffusion coefficient mapping of salivary gland tumors: prediction of the benignancy and malignancy. Positron emission tomography-computed tomography adds to the management of salivary gland malignancies. Parotid incidentaloma identified by combined 18F-fluorodeoxyglucose whole-body positron emission tomography and computed tomography: findings at grayscale and power Doppler ultrasonography and ultrasound-guided aspiration biopsy or core-needle biopsy. Clinical application of magnetic resonance sialographic 3-dimensional reconstruction imaging and magnetic resonance virtual endoscopy for salivary gland duct analysis. Facial nerve injury, wound infection, salivary fistula, or sialocele are reported after open biopsies; in addition, a curative parotid surgery can be complicated by a previous open biopsy. If malignant, the tumor type and grade are important, as selected low-grade carcinomas may not require total parotidectomy. The sensitivity and specificity in the detection of malignant neoplasms of the parotid gland were 75% and 95% and submandibular gland 91% and 94%, respectively. Interestingly, the sensitivity for submandibular gland neoplasms is higher than for parotid gland neoplasms. The high rate of falsepositives is in contrast to most studies reporting higher rates of false-negative than false-positive findings. Major complications such as tumor cell seeding or facial nerve paresis are extremely rare. The risk of cell seeding seems to be greater in other organs such as the thyroid gland (0. This enables the pathologist to apply a wider range of histochemical stains and immunohistochemical techniques, which may assist in tumor typing and grading. The examination revealed no tumor displacement in 65 cases, and in 38 cases, the needle track was not identified. The specificity of both procedures for discriminating benign from malignant lesions is quite similar. The rate of major complications such as tumor cell seeding or facial nerve paresis is low for both procedures. The pooled sensitivity and specificity in detecting malignant neoplasms were 94% and 98%, respectively. The pooled sensitivity and specificity in detecting malignant neoplasms were 90% and 99%, respectively. In two studies15,36 with more than 40 malignant parotid neoplasms, the accuracy of tumor typing was 72% and 58% and of tumor grading 73% and 78%. The sensitivity and specificity in detecting malignancy were 80% and 98%, respectively. Fine needle aspiration cytology and frozen section in the diagnosis of malignant parotid tumours. Diagnosis and management of parotid carcinoma with a special focus on recent advances in molecular biology. Preservation of the superficial lobe for deep-lobe parotid tumors: a better aesthetic outcome. Extracapsular dissection for clinically benign parotid lumps: reduced morbidity without oncological compromise. Sensitivity, specificity, and posttest probability of parotid fine-needle aspiration: a systematic review and meta-analysis. Diagnostic accuracy of fine-needle aspiration for parotid and submandibular gland lesions. Accuracy of core needle biopsy versus fine needle aspiration cytology for diagnosing salivary gland tumors. Diagnostic accuracy of fine-needle aspiration cytology and frozen section in primary parotid carcinoma. A systematic review of cases reporting needle tract seeding following thyroid fine needle biopsy. Incidence of needle tract seeding and responses of soft tissue metastasis by hepatocellular carcinoma postradiotherapy. The use of fine needle core biopsy under ultrasound guidance in the diagnosis of a parotid mass. Parotid lymphoma in west Scotland: Two-year snapshot of diagnosis, management and core issues.
Buy genuine cafergot online
When a stone has been removed from the hilum or inside the gland advanced pain treatment center edgewood ky buy cafergot once a day, medication for pain is necessary, to allow regular gland massage by the patient for a constant salivary flow. Saline rinsing of the oral cavity helps reduce inflammation and supports wound healing. Preparation and Performance of the Procedure General Requirements Before starting the operative procedure, the patient must be informed about the procedures and possible risks of the interventions. These authors normally perform sialendoscopy and the combined transoral approach under local anesthesia. The advantage of this is that no instrument is needed to open the mouth or to move the tongue. Moreover, there is more tension of the muscle in the floor of the mouth and the patient can push the gland upward into the floor of the mouth and better expose the hilum and stones. The subjective experience of discomfort and pain during the procedure was assessed as "mild" or "none" by 85% and 89%, respectively. No difference was seen between diagnostic and interventional procedures and 97% of patients would choose an operation under local anesthesia again. Straightforward cases are those with larger stones located within the middle of the floor of the mouth or in the main duct distal to the hilum. If the patient feels uncomfortable with a local anesthetic, or is a child, it can be performed under general anesthesia with trans-nasal intubation. The more difficult cases that may require general anesthesia are those with smaller impacted stones, which are not palpable within the hilum or even within the gland, when the size of the tongue is large, or the floor of the mouth is difficult to reach because of the anatomy of the mandible and teeth (deep floor of the mouth). These include intraoperative and postoperative bleeding; pain during and after the procedure, especially during swallowing; postoperative infections and sialadenitis; remaining stones within the gland or stone Endoscopy Preparation of instruments. The affected side of the floor of the mouth, as well as the oropharyngeal and laryngeal mucosa should be covered to reduce a gag response. Next, injection of a minimum of 5 mL of Ultracaine near the lingual nerve of the effected side from the hilum to the ostium in smaller increments. While dissecting in the hilum region, extra-long and slim instruments are helpful. A duct incision with scissors is performed with one branch of the scissors inserted into the duct. If the concrement is not removed by interventional sialendoscopy, the next step is to go directly ahead with a combined transoral removal. Sialendoscopy shows exactly the depth of the stone within the duct and a direct visualization within the duct system. There are different approaches, including leaving the endoscope inside the duct as a guide to find the stone illuminated in front of the endoscope. If the distance is <6 cm and the stone is within the duct or still visible near the hilum, there is a probability of >90% for safe removal. For facile dissection, open the mucosa of the floor of the mouth with scissors and follow the duct directly to where the stone is found. When necessary, open the mucosa further on laterally up to the tonsillar region (for hilar or very big stones). In cases where the concrement is located in the hilum, it is essential that the patient or an assistant pushes the submandibular gland upward toward the floor of the mouth. If the stone is not visible through the duct lumen, an incision of the duct is performed distal to the premeasured stone location and the duct is incised further into the submandibular gland to the hilum and even more proximal (submandibulotomy). The lingual nerve (green arrow) running in a deeper layer from dorsal lateral to ventral medial can be seen. The incision of the mucosa must be extended toward the tonsillar region with intraglandular impacted larger concrements. If a stone breaks into different fragments, care must be taken to completely remove all of these fragments. Rinsing with saline may help extrude smaller fragments and reduce the risk of residual and recurrent stone formation. In hilar stones, endoscopic access after stone removal is in most cases not successful due to bleeding and an open duct parenchyma. A potential better choice for searching for residual concrements is to perform an intraoperative ultrasound. Some surgeons do not marsupialize the duct and feel sialoceles or stenosis are unlikely. The anterior part of the floor of the mouth is also closed (4-0 Vicryl, P3 needle). Results and Complications the proportion of various transoral approaches reaches up to 93% of all stones. The needle is guided from the duct mucosa (blue arrow) through the mucosa of the floor of the mouth (green arrow). Authors who differentiate between distal and proximal duct stones find a higher rate of success, up to 100% for distal concrements. The more challenging stones are those in the hilar region attached to the parenchyma of the submandibular gland or patients with multiple stones. The recurrence of obstructive symptoms have a significantly higher rate in proximal stones and also in multiple stones. In the case of a partially removed stone (typically in large adherent parenchymal stones that are soft and tend to break during the procedure), there can be a return of symptoms. Other factors such as gender, age, size of stones, and palpability of stones are not related to the development of recurrent obstructive symptoms. Because of the anatomic proximity of stone and lingual nerve, the risk of an injury is higher for hilar stones. The more the lingual gland is left laterally and minimally dissected, the less the chance for generating a ranula. There is still an ongoing discussion whether it is useful to create a neo-ostium with sialodochoplasty within the floor of the mouth or not. Postoperative stenosis, reported between 0% and 5%, occurs regardless of applied technique. The authors perform a sialodochoplasty, sometimes >2 cm, to reduce the distance between the floor of the mouth and a hilar or parenchymal opening; a "submandibulotomy". Control of salivary flow in the direct postoperative course is easier to assess and it does not harm the patient. Submandibulectomy after a transoral procedure is significantly more frequent in hilar or multiple stones. Residual fragments causing obstructions may be treated by transoral stone removal or other techniques including intra- or extracorporeal lithotripsy. Residual fragments may have minimal symptoms with no indication for further treatment or gland removal. Symptomatic sialoadenitis and sialolithiasis in the English population, an estimate of the cost of hospital treatment. Long-term experience with endoscopic diagnosis and treatment of salivary gland inflammatory diseases. Complications of sialendoscopy: personal experience, literature analysis, and suggestions. Salivary simulation with ascorbic acid enhances sonographic diagnosis of obstructive sialadenitis. Intra-oral removal of stones from the hilum of the submandibular gland: report of technique and morbidity. The ductal stretching technique: an endoscopic-assisted technique for removal of submandibular stones. Transoral removal of hiloparenchymal submandibular calculi: a long-term clinical experience. Sialendoscopeassisted transoral removal of hilo-parenchymal sub-mandibular stones: surgical results and subjective scores. Factors affecting long-term outcome of transoral surgery for submandibular stones: a followup study of 125 patients.
Generic 100 mg cafergot overnight delivery
Mucous rich saliva acts more as a lubricant and protective barrier for the oral cavity treatment guidelines for pain generic cafergot 100 mg online. Also part of the epithelial compartment are contractile myoepithelial cells, which surround the acini and the ducts that directly connect to the acini. Ducts play a large role in modifying saliva before it is secreted to the oral cavity. Through the use of rodent models, the cellular and molecular processes leading to the development and functionality of secretory branching organs, such as the salivary glands, have been studied in great detail. Gland ontogenesis, development, and maturation are regulated by a series of signaling mechanisms and cellular interactions between the mesenchyme, nerves, blood vessels, and epithelium. Several recent studies have reported the presence of epithelial stem/progenitor cells, which respond to the surrounding environment to expand themselves and/or differentiate into specific cell types of functional salivaproducing gland. This type of research has significantly expanded our understanding of how organs develop and function. It also enhanced the translational concepts of manipulating signaling pathways and/or various cell types in the gland to aid patients who suffer from debilitating diseases, conditions, or syndromes that lead to loss in saliva production. While rodent models are used to analyze these processes, multiple labs have highlighted the comparison of gene expression, cell surface markers, stem cell markers, and protein expression to the human system. Here we summarize and compare our current knowledge on the embryology and physiology of the mouse and human salivary glands, and how stem/progenitor cell populations may contribute to these processes. Initial saliva by acini is generated by the transmission of water via the basement membrane and aquaporin-5 water channels. In brief, the acinar cells are concentrated in K+ and Cl- above the electrochemical equilibrium. Autonomic neuronal stimulation opens Ca+2 sensitive ion channels, allowing permeability of potassium ions to the basolateral membrane and interstitium, as well as chloride ions into the lumen of acini. The negative charge created by the Cl- draws Na+ through the tight junctions between acinar cells to the lumen. As a result of NaCl accumulation in the lumen, water moves to the lumen via osmotic pressure. While this is a brief and more commonly accepted method of ion transfer in the acinar cells, a more detailed description on additional exchange mechanisms has been previously described. Myoepithelial cells surrounding the acini can contract to push the saliva out, and aid in the movement of saliva to the connected ducts where the saliva gets modified. The second intraglandular duct, the striated duct, functions in regulating the secretion and absorption of electrolytes. Saliva is then transported to the lumen of excretory ducts, where there is a small contribution to the ion exchange. Rodent glands are similar to human glands in terms of their histologic appearance and physiologic functions. Both sympathetic and parasympathetic innervate the salivary glands with the parasympathetic system playing a dominant role. In both human and rodent glands, it was noted that the parasympathetic nerves are present at gland ontogenesis, while the sympathetic nervous system innervates the gland later when branching, cell differentiation, and lumen formation has been initiated. Hence, stimulus for glandular development, growth, vasodilation, and saliva formation and flow are mediated by parasympathetic innervation. In contrast, exocytosis, protein composition, and secretion are dependent on sympathetic innervation. While these systems have unique roles, both can have additive and synergistic effects on fluid secretion by contraction of myoepithelial cells. In brief, saliva flow is regulated by neurotransmitter receptors on the basolateral membranes of the acini and ducts. More specifically, neurotransmitter acetylcholine binds to the muscarinic cholinergic M3 receptors. This leads to the activation and binding of heterotrimeric guanine nucleotide-binding proteins. The ultimate product is formation of inositol triphosphate and the release of a second messenger, Ca+2. While Ca+2 release via acetylcholine parasympathetic stimulation induces saliva flow, beta-adrenergic sympathetic stimulation from binding of norepinephrine to beta-adrenergic receptors mediates saliva composition and exocytosis. Salivary Gland Embryogenesis Ontogenesis of all glands is initiated by interactions between epithelial cells from the oral lining and the surrounding environment (Table 2. At least in the mouse model, research revealed that the major glands are not derived from the ectoderm. After ontogenesis, both human and rodent glands follow a similar developmental pattern. Several phases of branching evoked by repetitive bud clefting and ductal elongation subsequently lead to the characteristic tree-like structure of the gland. At least in rodents, an early postnatal development still occurs where pro-acinar cells become fully functioning acini by secreting their full plethora of enzymes and proteins. Stem cells are defined by their ability to self-renew and differentiate into specialized cell types. In contrast, a progenitor cell is already more defined but still harbors some self-renewing and differentiation potential. In recent years, it has been found that multiple salivary gland epithelial stem/progenitor cells are present, and that cells can initiate a stem/progenitor celllike plasticity under several environmental changes and/or injury responses. For fetal development, the majority of information on stem/progenitor cells has been revealed via mouse genetic lineage tracings. Herein, a genetically fluorescent-labeled cell of interest is followed and all its progeny can be determined at any given time. Stem cells and signaling mechanisms that regulate embryonic epithelial outgrowth and differentiation have been extensively described before. Fetal mouse glands have also been instrumental in defining the interactions between epithelial stem/progenitor cells and the environment. Recent studies have highlighted the significance of blood vessels and innervation to gland development and stem/progenitor cell maintenance. Parasympathetic innervation is essential for the maintenance of fetal K5+ cells and their differentiation into luminal duct cells. Recent studies have also shown the necessity of endothelial cells in regulation of salivary gland epithelial patterning. Moreover, multiple studies have elucidated the crucial role of endothelial cells in cell fate, organ development and patterning. To date, little information is known about the communication between the sympathetic nerves and surrounding cell types during development. Questions remain whether the findings in fetal mouse glands are completely identical in human fetal glands. While epithelial stem/progenitor cells in fetal glands provide tremendous information on how they interact with the environment and how they differentiate, the ultimate goal, therapeutic potential of stem/progenitor cells lies within adult glands. Adult stem/progenitor cells can be used as a therapeutic tool to replace the pool of acini after irradiation and/or to replenish the loss of reservoir stem/ progenitor cells. Alternatively, adult stem/progenitor cells can be used in bioengineered glands that can aid in repair and/or replace surgically removed glands. These studies are largely promoting the translation of growth factors, stem/progenitor cells, bio-engineered glands, and gene therapy for clinical settings. Saliva mediated adherence, aggregation and prevalence in dental plaque of streptococcus mutans, streptococcus sanguis and actinomyces spp. Dose, volume, and function relationships in parotid salivary glands following conformal and intensity-modulated irradiation of head and neck cancer. Function of myoepithelial cells in salivary secretion: reevaluation of the expulsion theory. A patch-clamp study of potassium channels and wholecell currents in acinar cells of the mouse lacrimal gland. Comparing human and mouse salivary glands: a practice guide for salivary researchers. Overview of human salivary glands: highlights of morphology and developing processes.
Diseases
- Melioidosis
- Cardiomelic syndrome Stratton Koehler type
- Hypobetalipoprot?inemia, familial
- Ophthalmomandibulomelic dysplasia
- Synovitis granulomatous uveitis cranial neuropathi
- Rabson Mendenhall syndrome
- D-Glyceric acidemia
- Camptodactyly taurinuria
Order 100 mg cafergot free shipping
A history of radiation is important because of the secondary salivary effects of either radioactive iodine or external beam radiotherapy treatment for dog pain in leg order cafergot 100mg without a prescription, even though neither is associated with stone formation. A combined procedure starts with endoscopic visualization and location of the stone followed by a standard external or intraoral approach to remove the stone, avoiding removal of the involved gland (see Chapter 18). Stone fragmentation using a laser (see Chapter 22), stone fragmentation using pneumatic lithotripsy (see Chapter 23), and extracorporeal lithotripsy (see Chapter 24) are other approaches that can be considered for stones not amenable to endoscopic wire basket retrieval alone. When there is a known sialolith, general anesthesia is chosen, unless there is a patient comorbidity that precludes it. Nasal intubation offers a wider exposure of the oral cavity, but there is a risk of epistaxis, and is traditionally reserved for bilateral cases or for patients with a challenging access to the oral cavity (obese patients, large tongue, small mouth opening, tori, or large teeth). Muscle relaxation is typically used for cases performed under general anesthesia for optimal intraoral access. A single intravenous dose of perioperative antibiotic to cover the oral flora is administered. The patient is positioned supine and the bed is rotated about 100 degrees, with a set-up similar to that of routine endoscopic sinus surgery. The right arm is tucked and the left armrest is positioned next to the bed to facilitate the surgeon and the assistant on opposite sides of the patient. Oval shape oriented along the length of the duct, free-flowing movement with irrigation, and a width no <4 mm were predictors for success. Palpable anterior floor of mouth stones or stones at the papilla may be removed transorally in the office without the need for endoscopy. Stones located elsewhere along the duct or that are not palpable are better served with endoscopic localization and retrieval using endoscopic or combined techniques. Indications for Surgery Sialendoscopy should be offered in all patients with submandibular sialolithiasis who have obstructive symptoms and/or recurrent acute sialadenitis with or without abscess formation. Asymptomatic patients with incidental sialoliths are offered endoscopy versus observation and counseled on the pros and cons of each. The pros of observation is the avoidance of surgical and anesthetic complications, and the cons include the future possibility of developing sialadenitis, neck abscess, and loss of the ability to retrieve the stone endoscopically as stone size increases over time. The only relative contraindication to interventional sialendoscopy is active sialadenitis due to an increased risk of ductal injury. Equipment There is a standard set of equipment in a custom interventional sialendoscopy set, to use for each case. A monopolar cautery with a Colorado tip is available, typically at a setting of 8. Disposable equipment includes: stone baskets, guidewires, indwelling access sheaths, 60 cc syringes with tubing, and local anesthetic. We prefer the "all-in-one" Marchal Miniature Endoscope for Diagnostic and Interventional Sialendoscopy with remote eyepiece, forward zero-degree telescope, semi-rigid, outer diameter of 1. The endoscope light strength is set very low, to about 10%, to allow optimum brightness while performing sialendoscopy; too much light causes reflection off the ductal wall and a virtual white out. The scope is focused and white balancing is done using a white gauze, while operating room lights overhead provide additional light. Intraoperative Technique Exposure is obtained using a mouth prop and sweetheart retractor. An injection or forceps are not routinely performed before securing the scope in the duct, in order to avoid creating pseudo-orifices that can mimic the true orifice. Doing so in an atraumatic fashion may be the most challenging portion of the procedure. Optimal exposure is attained with a mouth prop and the assistant retracts the tongue posteriorly using a sweetheart retractor. Application of methylene blue to help make the papilla more prominent can be used if necessary. Try to avoid doing a papillotomy at the beginning of the procedure unless standard dilation techniques fail, as this prevents creation of a mucosal seal, which consequently may prevent maximum dilation of the duct by hydraulic pressure with irrigation. When the dilation technique is used, the authors typically use Schaitkin salivary punctal dilators sizes 1 through 5. The size 1 dilator is first inserted into the puncta to cannulate it and should "fall in" about 6 mm, which is the point of maximal dilation for the device. It is aimed along the direction of the duct, inferiorly, posteriorly, and laterally. The punctum dilator is used after the 4, as it allows for a better transition to the 5. The size 5 dilator on the right is a newer generation of Schaitkin dilators; unlike the illustrated older generation dilators, the size 5 has a black line on the end, marking the target depth of insertion, and it is labeled as a size 5 based on the number of black rings around its shaft. The size 2 dilator should be inserted immediately upon removal of the size 1 dilator. Next, use a tapered lacrimal punctum dilator after the size 4 dilator and lastly complete the dilation with a size 5 dilator. Dilators should not be inserted beyond 1 cm as they may push stones back or traumatize the duct (Video 17. The duct is then slowly dilated with Cook dilators using the Seldinger technique (Video 17. The sialendoscope can then be loaded onto the wire using the Seldinger technique and passed into the duct. This technique can also be used for stenosis found within the duct, which may be the location that a stone is lodged (Video 17. If the procedure is being done under sedation, the first 10 mL of irrigation has 2% lidocaine. The assistant provides slow but steady pressure to the 60 cc irrigation syringe, which can be attached via tubing to irrigation port, or if larger flow is desired, the working channel. The endoscopist adjusts the angle of the scope in the duct until the lumen is at the center of the screen (Video 17. Manual traction and pressure on the papilla helps to straighten the duct for easier navigation. Advancing a guidewire through the scope into the duct can help to straighten it and improve ductal navigation if needed. The endoscopist must be careful to avoid bending the scope on the teeth, as the scope is fragile. Keeping the lumen in the center, the endoscope is advanced until the sialolith is encountered. If the stone is noted to be free floating, that is a favorable sign for successful basket retrieval (Video 17. There are several options for wire baskets: Karl Storz baskets with 3, 4, or 6 wires, which range from 0. The 3 wire Karl Storz basket is the workhorse basket and this is typically the size we use with the Marchal 1. The closed basket is advanced through the working channel of the scope beyond the stone and then opened. To facilitate the delivery of most stones, a small papillotomy is required and performed with a Colorado tipped Bovie or 15 blade (Video 17. In cases where a stone is too big for basket retrieval, the basket may be used to help trap and locate the stone. In this situation, leave the basket in place around the stone and perform sialolithotomy. The basket can help with transoral identification of the stone as it is palpable, keeps the stone from shifting out of reach, and can be gently rocked to help demonstrate its location. Endoscopy is again performed at the end of the procedure to ensure no further stones or debris remain, and that no damage to the duct occurred. In a series of 172 patients undergoing stone retrieval, 28% of patients were found to have an additional undetected stone after initial removal of the known stone, and in 36%, strictures were diagnosed distal to the stone. If no stent is in place, the patient is instructed to massage the gland at least three times a day at home and counseled to expect mild swelling within the first 48 h. If there is a stent, patients are asked to inspect the stent for loosening or extrusion daily.
Buy generic cafergot from india
Differential diagnoses include sympathomimetic or serotinergic toxidromes pain management for uti 100mg cafergot amex, common after poisoning with amphetamines and other central nervous system stimulants, and central nervous system infection. Physostigmine given by slow intravenous push (adults Aetiology and epidemiology the most common exposure to toxic plants, particularly in the West, is in young children as they explore their environment. In other parts of the world, particularly Asia, the most common plant exposures are from self-harm in adolescents and adults, sometimes with fatal outcome. Deaths also occur after children (although rarely adults) eat poisonous plants as food, especially where there is food insecurity. Herbal medicines containing toxic principles cause accidental plant poisoning, while recreational ingestion or smoking of psychoactive plants is popular in industrialized countries. Physostigmine should be withheld if cardiotoxic agents have been co-ingested, if the patient has a bradycardia, or if there are signs of cardiac conduction abnormalities. This has caused confusion on presentation to hospital and unnecessary, expensive investigations. Hallucinogenic toxins Some plant toxins are particularly popular among abusers because of their hallucinogenic properties. Examples are tetrahydrocannabinols in cannabis Cannabis sativa, alkaloids in khat Catha edulis, mescaline in peyote Lophophora williamsii, and myristicin in nutmeg Myristica fragrans. Ayahuasca is a hallucinogenic brew made from Banisteriopsis caapi vine and Psychotria viridis leaves in South America. Treatment is symptomatic, with a calm environment and benzodiazepines as necessary. Their unpleasant taste should reduce the risk of poisoning by ingestion; nevertheless, they are sporadically confused with herbs and eaten in salads. Early symptoms are vertigo, agitation, thirst, tachycardia, hypertension, salivation, diaphoresis, vomiting, and diarrhoea. Muscle fasciculation, convulsions, hypotension, bradydysrhythmias, ascending weakness, paralysis, and coma may follow. Careful symptomatic and supportive care, including assisted ventilation, may be required. Other neurotoxins Toxins in fruit of the buckthorn or tullidora bush, Karwinskia humboldtiana, in Central America produce a flaccid, symmetric, ascending paralysis of the lower limbs. The dimeric hydroxyanthracenone peroxisomicine A1 appears to be cytotoxic but the precise mechanism of the peripheral neuropathy is not yet known. Treatment is supportive until the peripheral neuropathy resolves, with careful monitoring for impending ventilatory failure. Gelsemine in lemuan Gelsemium elegans in China and yellow jessamine G sempervirens in North America is a glycine agonist. Patients present with dizziness and eye manifestations (blurred vision, diplopia, nystagmus, ptosis), progressing to coma, seizures, and respiratory failure requiring mechanical ventilation. Cicutoxin occurs in cowbane Cicuta virosa, water hemlock C maculata, and western water hemlock C douglasii, while oenanthotoxin occurs in hemlock water dropwort Oenanthe crocata. Severe poisoning has occurred in adults eating one of these plants after mistaking it for an edible plant. These may result in hypoxia, severe metabolic acidosis, coma, circulatory instability, rhabdomyolysis, joint dislocations, and rectal prolapse. Diagnosis is typically based on the presence of recurrent seizures together with the history of plant ingestion. Treatment requires careful symptomatic and intensive care, with emphasis on combating convulsions with benzodiazepines, barbiturates, and general anaesthesia, correction of acidosis, and maintenance of urinary output. Other toxins reported to cause coma and/or seizures include coriamyrtin in Coriaria myrtifolia in the Western Mediterranean, terpenes in chinaberry Melia azedarach in South East Asia, the alkaloid dauricine in moonseed Menispermum canadense and podophylloresin in may apple Podophyllum peltatum, both in North America, strychnine in the nux vomica or strychnine tree (Strychnos nux-vomica) in South and South East Asia, and unknown toxins in Urobotrya siamensis Hiepko in South East Asia and star fruit Averrhoa carambola in patients with chronic kidney disease in East Asia. Cardiotoxic plants Aconitine Aconitine is one of the most potent plant toxins known, occurring in multiple Aconitum spp. The toxin binds to voltage-gated sodium channels causing persistent sodium influx and depolarization of cardiac and neurological tissue. Serious poisoning results from intentional ingestion of the plant, homicidal administration of aconitine in food, and from unintentional overdose of Asian herbal medications. Ingestion results in rapid onset of burning and tingling in the lips, mouth, and pharynx, followed by numbness and paraesthesia of the limbs, hypersalivation, and gastrointestinal symptoms in particular severe and protracted vomiting. Many kinds of dysrhythmias occur, but particularly ventricular ectopy leading to ventricular tachycardia and fibrillation that may be refractory to treatment. Cardiac failure and shock often develop; coma, muscular weakness, neuromuscular failure, and seizures also occur. Considering the extreme toxicity of this plant, gastrointestinal decontamination should be performed. Treatment includes optimal symptomatic and supportive care, directed at dysrhythmias and cardiac failure, including magnesium, flecainide, or lidocaine, and extracorporeal membrane oxygenation. Similar to aconitine, the toxin binds to and activates voltage-gated sodium channels on nerve, muscle, and heart cells. Where available, digitalis-specific antibodies (ovine Fab fragments) are highly effective. Where not available, management focuses on symptomatic care and treatment of hyperkalaemia. They also block Na+ channels and disrupt microtubule function, inhibiting cell division, causing central nervous system and gastrointestinal effects. Treatment involves supportive care, with extracorporeal membrane oxygenation if available. Ingestion results in severe gastrointestinal features, with abdominal pain, profuse vomiting, and diarrhoea common. Cytotoxic plants Colchicine Colchicine occurs in autumn crocus/meadow saffron Colchicum autumnale and glory lily Gloriosa superba. It binds to -tubulin, producing antimitotic effects on cells with high metabolism After an initial delay- sometimes of many hours-there is onset of intense gastrointestinal symptoms, followed by dysrhythmias, circulatory failure, seizures, central nervous system depression, and muscular weakness. There may be signs of renal and hepatic damage and, after a few days, bone marrow depression. Patients who survive the acute phase may lose their hair and develop a peripheral neuropathy. Multiple-dose activated charcoal may enhance elimination, but intensive care is crucial together with measures to encourage bone marrow recovery. Anticolchicine Fab fragments have been studied but are not yet available in clinical practice. Ricin in the castor plant Ricinus communis and abrin in jequirity bean Abrus precatorius are water-soluble proteins known as toxalbumins. Ricin is so toxic that it has been placed on the Chemical Weapons Convention List. These compounds block protein synthesis by inhibiting ribosome function, causing cell death, with the gut as the primary target organ. However, beans that have been chewed are highly toxic, with just a few sufficient to cause severe poisoning. A few hours after ingestion, severe gastroenteritis may occur with heavy fluid and electrolyte loss, resulting in renal failure, circulatory instability, and hepatic damage. After the kernels are chewed and swallowed, barriers between the cyanogenic glycoside and enzyme break down, resulting in enzymatic release of cyanide in the stomach. Cyanide poisoning from plants is unusual but, should it occur, treatment is as outlined elsewhere for cyanide (see Chapter 10. It was observed in Nigeria in the 1930s, and subsequently in other African countries. Food insecurity results in atypical ways of preparing cassava, producing small outbreaks from time to time.
Cheap 100mg cafergot fast delivery
In the case of diquat poisoning pain management in dogs and cats discount 100 mg cafergot free shipping, the urine goes a green colour in the alkaline sodium dithionite test. The outcome of paraquat poisoning can be predicted with reasonable confidence within a few hours of ingestion by relating the plasma paraquat concentration to the time after ingestion, but this assay is not readily available in Europe following the withdrawal of paraquat from the market. There is no evidence that the outcome of paraquat or diquat poisoning can be altered by any form of intervention. Symptomatic measures including antiemetics, mouth washes and analgesics are indicated, and intravenous fluids may be necessary to replace gastrointestinal losses. Carbamate insecticides Carbamate insecticides inhibit acetylcholinesterase, causing accumulation of acetylcholine at central and peripheral cholinergic nerve endings, including neuromuscular junctions. Seizures are relatively uncommon as a primary complication, because carbamate penetration into the central nervous system is limited, though they may occur secondary to hypoxia. In less substantial ingestions, cholinergic symptoms are evident within 2 h in most cases and typically resolve within 24 h. Treatment Bronchorrhoea requires removal of secretions by suction and prompt relief with intravenous atropine 2 mg (0. If these measures fail, the patient should be intubated and mechanical ventilation instituted. At present there is insufficient evidence to either recommend or advise against the use of pralidoxime in severe poisoning with carbamate insecticides. Pralidoxime seldom should need to be administered in less severe cases since carbamates have a relative short duration of action. However, if intoxication is life-threatening and unresponsive to atropine and supportive measures, pralidoxime chloride 30 mg/kg body weight by intravenous injection over 20 minutes should be given. The combination of methaemoglobinaemia and haemolysis results in varying degrees of hypoxaemia and symptoms such as general weakness, fatigue, dizziness, agitation, anxiety, confusion, and headache. Poisoning with chlorate is also commonly complicated by acute renal failure, though the underlying mechanisms are not fully understood. Haemodialysis/haemodialfiltration may remove chlorate and will also be required for the management of renal failure and hyperkalaemia. Plasmapheresis and plasma exchange or exchange transfusion have also been employed to remove chlorate, circulating free haemoglobin, and red cell stroma, but data are too limited to make a firm recommendation. They comprise an aliphatic carboxylic acid moiety attached to a chlorine- or methyl-substituted aromatic ring. These herbicides are usually formulated as salts or esters of the active compound and sometimes coformulated with the chemically related herbicides ioxynil, bromoxynil and/or dicamba. Most instances of serious poisoning have been due to deliberate ingestion, mainly in the developing world. Mechanisms of toxicity include dose-dependent cell membrane damage, chemical mimicry of acetyl coenzyme A and uncoupling of oxidative phosphorylation. Clinical features Ingestion causes nausea and vomiting which may be accompanied by burning in the mouth and throat and abdominal pain. Hypotension, which is common, is due predominantly to intravascular volume loss, although vasodilation and direct myocardial toxicity may also contribute. Coma, hypertonia, hyperreflexia, ataxia, nystagmus, miosis, hallucinations, convulsions, fasciculation, and paralysis may then ensue. Hypoventilation is commonly secondary to central nervous system Chloralose Chloralose is marketed for amateur use as cereal or paste baits containing 2 to 4% rodenticide. Clinical features Toxic amounts of chloralose cause severe central nervous system excitation with hypersalivation, increased muscle tone, hyperreflexia, opisthotonus, myoclonic jerks, and convulsions. Treatment Children who ingest small amounts of baits (amateur formulations) containing chloralose are unlikely to develop symptoms. In contrast, patients who have deliberately ingested large amounts of bait or the technical compound are likely to require admission to intensive care for management of convulsions, myoclonus, and coma. Sodium chlorate and potassium chlorate are powerful oxidizing agents that induce methaemoglobinaemia and haemolysis. Clinical features Features of chlorate toxicity may develop within as little as two hours of ingestion and are usually due to gastrointestinal irritation. Myopathic symptoms, including limb muscle weakness, loss of tendon reflexes, myotonia, and increased creatine kinase activity, have been observed. Metabolic acidosis, rhabdomyolysis, renal failure, increased aminotransferase activities, pyrexia, and hyperventilation have been reported. Treatment In addition to supportive care, urine alkalinization with high-flow urine output will enhance herbicide elimination and should be considered in all seriously poisoned patients. Haemodialysis produces similar herbicide clearances to urine alkalinization and should be considered if high-flow urine alkalinization cannot be performed for clinical reasons. This increase in motor activity, in turn, results in raised creatine kinase activity, rhabdomyolysis, hyperpyrexia, and metabolic acidosis in some cases. Less frequent complications include hyperventilation, respiratory alkalosis, minor elevation of transaminase activities, upper gastrointestinal bleeding, and mildly deranged coagulation. Glyphosate Glyphosate-containing herbicides are very popular because their mode of action is plant-specific (by inhibition of an enzyme pathway not present in mammals), they act only on contact with plant foliage and are inactivated on contact with soil. Formulations usually contain the isopropylamine salt of glyphosate, together with a surfactant. The most prominent effects are on the alimentary tract with burning in the mouth, throat, nausea, vomiting, dysphagia, and diarrhoea. Renal and hepatic impairment are also frequent and usually reflect reduced organ perfusion. Respiratory distress, impaired consciousness, pulmonary oedema, infiltration on chest radiograph, shock, arrhythmias, renal failure requiring haemodialysis, metabolic acidosis, and hyperkalaemia may supervene in severe cases and, together with advancing age and late presentation, are poor prognostic indicators. The fatality rate in case series of glyphosate concentrate ingestion is approximately 6%. Death most frequently ensues within 72 h and is related to refractory cardiovascular collapse. Methyl bromide the uses of methyl bromide (bromomethane) have gradually become restricted as it is an ozone-depleting chemical. It is currently used to fumigate mills, warehouses, shipping containers, stored products, and soil in greenhouses to eradicate pests such as woodworm and rodents that damage crops and buildings. In most countries application is now restricted to trained and licensed personnel. Methyl bromide is absorbed readily through the lungs and is excreted largely unchanged by the same route. Clinical features Inhalation causes respiratory tract irritation with shortness of breath, cough, and varying degrees of pulmonary oedema. Neurotoxicity manifests hours or days later with agitation, delirium, ataxia, intention tremor, nystagmus, dysdiadochokinesis, and hyperreflexia. Proteinuria, oliguria (due to renal tubular and cortical necrosis), and jaundice have been described. Treatment the casualty should be removed promptly from the contaminated atmosphere and undressed, as methyl bromide can penetrate clothing and rubber gloves. Systemic uptake can be quantified by measuring serum and urine bromide concentrations. Neonicotinoids Neonicotinoids are now employed widely as systemic insecticides and some (imidacloprid, dinotefuran, thiamethoxam, nitenpyram) are used as flea control agents for dogs and cats. Human poisoning with neonicotinoids is well recognized and may be severe and fatal, though the solvents and surfactants present in many formulations may also contribute to toxicity. Clinical features Poisoning with neonicotinoids is characterized by the rapid onset of symptoms including nausea and vomiting, fever, sweating, increased Metaldehyde Metaldehyde in the form of pellets is used widely for killing slugs and in some countries as a solid fuel. Clinical features Nausea, vomiting, diarrhoea, abdominal pain, agitation, dizziness, and tachycardia are common, but it is central nervous system and skeletal muscle complications that characterize the most severe toxicity. Convulsions may develop within 3 h of ingestion and recur frequently, and over days. Breathlessness, depressed respiration, cyanosis, and respiratory arrest have been reported. Bradycardia is sometimes present, but tachycardia is observed more frequently; ventricular tachycardia/fibrillation has occurred occasionally, as has cardiac arrest. Treatment In patients who are unconscious a clear airway should be established and, if ventilation is impaired, assisted ventilation should be commenced.
Purchase cafergot with mastercard
The only equipment required for the test is a new glass tube neck pain treatment quick fix order cafergot 100mg without prescription, but this may be difficult to find in modern hospitals where glass has been replaced by plastics. Patients with generalized rhabdomyolysis show a steep rise in serum creatine kinase, myoglobin, and potassium levels. Black or brown urine suggests generalized rhabdomyolysis and/or intravascular haemolysis; in both cases, positive urine sticks tests will not distinguish between blood, haemoglobin, and myoglobin. Urine should be examined for blood/haemoglobin, myoglobin, and protein, and for microscopic haematuria and red cell casts. Immunodiagnosis Specific snake venom antigens have been detected in wound swabs, aspirates or biopsies, serum, urine, cerebrospinal fluid, and other body fluids. Management of snakebite First aid the patient should be reassured and moved to the nearest hospital or dispensary as quickly, comfortably, and passively as possible. The whole patient should be immobilized, especially the bitten limb, using a splint or sling. Most traditional first aid methods are potentially harmful and should not be used. Local incisions and suction do not remove venom effectively and may introduce infection, damage tissues, and cause persistent bleeding. Vacuum extractors, potassium permanganate, and ice packs may potentiate local necrosis. Tourniquets and compression bands are potentially dangerous as they can cause gangrene, increased fibrinolysis, and bleeding in the occluded limb, peripheral nerve palsies, compartmental ischaemia, and intensification of local signs of envenoming. Pressure-immobilization (P-I) methods In animal studies, compressing superficial veins and lymphatics in the bitten limb delayed the spread of larger molecular weight toxins such as the presynaptic phospholipase A2 toxins of Australian elapid venoms. This delay might prevent development of life-threatening respiratory paralysis before the victim has had time to reach medical care. P-I is, therefore, indicated after bites by neurotoxic elapids but also, in cases of bites by unknown species, P-I should be applied immediately unless a bite by a neurotoxic elapid can, with confidence, be excluded. Although never subjected to formal clinical trials, the method was considered effective, based on anecdotal reports of delayed systemic envenoming and rapid deterioration after release of the bandage, in some cases supported by measurements of venom antigenemia. However, in practice, the technique has proved difficult to apply, even in Australia, and it is demanding on equipment and training. External compression increases intracompartmental pressure and might accentuate the local effects of some necrotic snake venoms, but animal studies found little evidence that this was deleterious and confirmed the life-saving effects of lymphatic and venous compression. A pad of whatever material is immediately available is placed directly over the bite wound and bound on very firmly with an inelastic bandage. The bitten limb is firmly bound with long, wide (4 cm) elastic bandages, starting distal to the bite site and ending at the armpit or groin. Pursuing and killing the snake is not recommended, but if the snake has been killed, it should be taken with the patient to hospital. Patients being transported to hospital should lie on their left side in the recovery position to prevent aspiration of vomit. Patients with incoagulable blood will develop haematomas after intramuscular and subcutaneous injections, and so the intravenous route should be used whenever possible except in the case of adrenaline. Respiratory distress and cyanosis should be treated by clearing the airway, giving oxygen, and, if necessary, assisted ventilation. If the patient is unconscious and no femoral or carotid pulses can be detected, cardiopulmonary resuscitation must be started immediately. Hospital treatment Clinical assessment In most cases of snakebite, uncertainties about the species and the quantity and composition of venom injected can be resolved only by admitting the patient to hospital for at least 24 h of observation. Local swelling is usually detectable within 15 min of pit viper envenoming and within 2 h of envenoming by most other vipers, but may not develop in patients bitten by some vipers, colubrids, and elapids such as kraits, coral snakes, and sea snakes. Tender enlargement of regional lymph nodes draining the bitten area is an early sign of envenoming by Viperidae and some Elapidae, notably Australasian elapids. All the tooth sockets should be examined meticulously as this is usually the first site of spontaneous bleeding: other common sites are the nose, conjunctiva, skin, and gastrointestinal tract. Persistent bleeding from venepuncture sites and other wounds implies incoagulable blood. Hypotension and shock are important signs of hypovolaemia, vasodilatation, or cardiotoxicity, seen particularly in patients bitten by North American rattlesnakes and some Viperinae Respiratory muscle power should be assessed objectively and repeatedly, for example, by measuring vital capacity. Trismus and generalized myalgia with muscle tenderness suggest rhabdomyolysis (sea snakes). Antivenom treatment In managing cases of snakebite, the most important decision is whether or not to give antivenom, the only specific antidote for envenoming. There is abundant evidence that in patients with severe envenoming, the benefits of this treatment outweigh the risks of antivenom reactions (see following paragraphs). Antivenom has reduced the mortality of systemic envenoming by Echis ocellatus in Nigeria from 20% to 3% and by C. Antivenoms are in short supply in sub-Saharan Africa and New Guinea; elsewhere, they are of variable efficacy and safety and are often used inappropriately. In the absence of systemic envenoming, local swelling involving more than half the bitten limb, extensive blistering or bruising, bites on digits, and rapid progression of swelling are indications for antivenom, especially in patients bitten by species whose venoms are known to cause local necrosis Antivenom should be given whenever there is evidence of systemic envenoming (see earlier), even if its appearance is delayed for several days after the bite. Prediction of antivenom reactions Hypersensitivity testing by intradermal or subcutaneous injection or intraconjunctival instillation of diluted antivenom was widely practised in the past. However, these tests delay the start of antivenom treatment, are not without risk, and have no predictive value for early (anaphylactic) or late (serum sickness-type) antivenom reactions, because they are not usually the result of acquired IgE-mediated type I hypersensitivity Prevention of early antivenom reactions Prophylactic antihistamines (anti-H1 and anti-H2), corticosteroids, and adrenaline have been widely used, singly or in combination, without convincing evidence of effectiveness. Hydrocortisone and promethazine were ineffective, and addition of hydrocortisone negated the benefit of adrenaline. Contraindications to antivenom Atopic patients and those who have reacted previously to equine antiserum are at increased risk of developing severe antivenom reactions. In such cases, antivenom should be given only if there is definite systemic envenoming. Reactions may be prevented or ameliorated by pretreatment with subcutaneous adrenaline (see earlier). Selection and administration of antivenom Antivenom should be given only if its stated range of specificity includes the species thought to be responsible for the bite. Whatever the stated expiry date on the ampoule, opaque solutions should be discarded, as precipitation of protein indicates loss of activity and an increased risk of reactions. However, expiry dates quoted on ampoules are often unnecessarily short, for commercial reasons; provided that the antivenom has been kept refrigerated and the solution is clear, a high proportion of its original activity is retained for 5 years or more. Polyspecific (polyvalent) antivenoms are used in many countries because of the difficulty in identifying the species responsible for bites. It is almost never too late to give antivenom while signs of systemic envenoming persist, but, ideally, it should be given as soon as it is indicated. Antivenom has proved effective up to 2 days after sea snake bites and, in patients still defibrinogenated, weeks after bites by Viperidae. In contrast, local envenoming is probably not amenable unless antivenom is given within a few hours of the bite. Few clinical trials have been performed to establish appropriate initial doses, and in most countries this is judged empirically. Intramuscular administration resulted in delayed peak concentrations (at 24 h) sixfold less than by intravenous injection. Many hospitals in the rural tropics give a standard dose of 1 to 2 ampoules to every patient who claims to have been bitten, irrespective of clinical severity. This practice squanders scarce, expensive antivenom, and exposes non-envenomed patients to the risk of reactions. Response to antivenom Often, there is marked symptomatic improvement soon after antivenom has been injected.