Purchase betapace in india
Mannitol may also be given during some neurosurgical procedures to reduce intracranial pressure hypertension uncontrolled icd 9 code order betapace on line amex. In vascular procedures, particularly on the aorta, mannitol may be used to protect kidney function by increasing the volume of fluid entering the kidneys. Mannitol is also used in the treatment of malignant hyperthermia, a condition associated with administration of some general anesthetic agents (see Ch. If a surgical patient is hypokalemic, potential exists for cardiac arrhythmias when under general anesthesia. For detection of hypokalemia, blood chemistry analysis is performed preoperatively for all surgical patients taking diuretics. Diuretics are given intravenously in surgery during some ophthalmic, intracranial, and vascular procedures. An indwelling urinary catheter must be inserted on all surgical patients who may receive diuretics intraoperatively. Hernandez is an 85-year-old woman admitted to surgery for insertion of a hip prosthesis to treat a hip fracture. Knowing that she has a concurrent diagnosis of hypertension, which additional related items should be checked on her chart How might this situation affect the preparations going on in the surgery department What action or actions should the surgical technologist take before bringing the patient to preoperative holding Van Nguyen is a 47-year-old man admitted to surgery for repair of a retinal detachment under general anesthesia. What items should the surgical technologist have available for preoperative preparation of the patient specific to this situation Diuretics achieve their treatment goals by bringing about a negative fluid balance, mobilizing excessive extracellular fluid, and reducing excess fluid volume. When the patient receiving diuretics is scheduled for surgery, preoperative evaluations are required. The surgical first assistant must understand the physiologic effects on the body and any possible surgical complications that may arise from these medications. Hypokalemia, depletion of potassium in the blood serum, is often caused by the effects of diuretics on the kidneys. Although water and sodium are excreted from the body by the kidneys, other electrolytes, such as potassium, are also excreted. Potassium is one of the essential minerals needed by the body to maintain homeostasis. Potassium is also needed to convert blood sugar into glycogen for energy that can be stored in the muscles. Next to calcium and phosphorus, potassium is the most abundant mineral found in the body. Potassium cannot be produced by the body and must be replaced through diet or supplements. Nearly 98% of the total potassium is found inside the cells, with the remaining 2% in the blood serum. Small fluctuations in the blood serum potassium may have adverse effects in the functions of the heart, nerves, and muscles. All patients on diuretic therapy are routinely tested preoperatively for blood serum potassium levels. Potassium Levels Potassium levels in the blood serum are identified through analysis of a blood sample. In most cases, the test is part of a routine chemical analysis that also includes other minerals. Treatment of Hypokalemia Treatment of hypokalemia involves replacing the potassium with diet or a supplement to obtain and maintain a normal serum potassium level. Treatment by oral intake or a supplement is adequate for minor depletion of potassium and can be performed at home over a period of time. Because of the slow release of potassium into the system, oral replacement treatment is by far the best method for replacement without any serious side effects. Cardiac monitoring is necessary because of possible arrhythmia caused by the fluctuations of potassium levels. Dosage required for correction is based on the accepted formula that 10 mEq/L of potassium chloride will increase the blood serum level by 0. Intravenous administration of 10 mEq/h not exceeding 200 mEq/L is usually recommended for severe hypokalemia. Aldosterone Although not technically a diuretic, aldosterone does affect kidney function. Aldosterone is a mineralocorticoid hormone produced by the adrenal cortex (see Chapter 8). It increases the reabsorption of sodium and water and the secretion of potassium in the kidneys. An example is spironolactone (Aldactone), which blocks the aldosterone receptor and so lowers blood pressure. MedicineNet, Low potassium (hypokalemia) index, What is the treatment for low potassium Discuss the endocrine system and the four main groups of hormonal action effects on the body. Discuss the structure, function, and importance of the pituitary gland, thyroid gland, parathyroid glands, and adrenal glands. Explain why epinephrine is of particular interest to the surgical technologist, and identify safety practices regarding the use of epinephrine from the sterile field. Identify the two major groups of adrenal cortex hormones and the purposes of each. These diverse substances maintain homeostasis (relatively constant conditions in the body) by altering the activities of specific target cells. Functions regulated by hormones include reproduction, growth and development, and metabolism. Hormones have a wide range of actions and effects, and each hormone has a specific function at a specific location in the body. In addition to naturally occurring hormones, several synthetic hormones have been developed. Most hormones are administered as replacement therapy in the medical rather than in the surgical setting, but some hormones are used in surgery and may be administered from the sterile back table during the course of a procedure. Endocrine System Review the endocrine system works with the nervous system to relay messages to maintain homeostasis. The endocrine system communicates by sending chemical messengers (hormones) to target cells located all over the body. Hormones are produced by endocrine glands and secreted into the extracellular space. Chemical messages take longer to work than those relayed by the nervous system, but effects generally last longer. In cellular mitochondria, enzymes convert cholesterol into pregnenolone, which is not a hormone but the immediate precursor molecule to the synthesis of all steroid hormones. Steroid hormones are classified as glucocorticoids (primarily cortisol), mineralocorticoids (primarily aldosterone), estrogens, progestogens (progesterone), and androgens (male sex hormones; primarily testosterone). Amine hormones include epinephrine, norepinephrine, thyroxine (T4), and triiodothyronine (T3). The vast majority of endocrine disorders are caused by either hyposecretion or hypersecretion of hormones. Treatment for hyposecretion may include administration of hormones for supplement or replacement. Hypersecretion may be treated medically with drugs to reduce secretion or surgically by gland removal, depending on indications.
Silybum Marianum (Milk Thistle). Betapace.
- How does Milk Thistle work?
- What is Milk Thistle?
- Are there safety concerns?
- Gallbladder problems, liver disease (cirrhosis, hepatitis and other liver conditions), liver damage caused by chemicals or poisonous mushrooms, spleen disorders, swelling of the lungs (pleurisy), malaria, menstrual problems, and other conditions.
- Dosing considerations for Milk Thistle.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96178
Buy generic betapace 40mg online
A meta-analysis including 1258 patients with claudication found that cilostazol significantly increased maximal walking distance relative to placebo (50 arterial occlusion purchase betapace canada. There are, however, tolerability issues observed including gastrointestinal side effects, headache, and dizziness, which may limit or shorten use. In addition, due to safety issues with other 612 10 - Vascular Medicine Drugs phosphodiesterase inhibitors, cilostazol is contraindicated in patients with heart failure. This is not due to any harm observed with cilostazol, but rather due to a warning across the class of agents. Cilostazol does have antiplatelet and antithrombotic effects, but large outcomes trials powered for ischemic and bleeding events have not been conducted. Therefore, a personalized approach should be taken, although cilostazol is generally not prohibited in patients on more potent antithrombotic regimens. There is no dose adjustment recommended for patients with hepatic or renal impairment. Pentoxifylline is a xanthine derivative that is a competitive nonselective phosphodiesterase inhibitor. It has also been described that exposure to pentoxifylline improves blood cell deformability and reduces viscosity as well as having a modest antiplatelet effect. For the vascular patient, pentoxifylline may be used on label for claudication symptoms and is sometimes used off label for the healing of chronic venous leg ulcers. Meta-analyses have found that the individual studies are of low quality and with large variability and have concluded that the role in claudication remains uncertain. Contraindications include hypersensitivity to xanthine derivatives or recent retinal or cerebral hemorrhage, and there are cautions for patients at high risk of bleeding. Dosing is generally 400 mg every 8 hours, but the dose can be decreased to twice daily if gastrointestinal or other side effects occur. Dose modification to twice daily is also recommended for patients with a creatinine clearance less than 30 mL/min. Cilostazol and pentoxifylline are available and should be offered to appropriate patients with limiting claudication. Of the two, data supporting the efficacy of cilostazol are stronger and it is preferred as a first choice by practice guidelines. The lack of efficacy stands in contrast to that seen for angina in patients with coronary disease. These agents have been investigated as delivered both intraarterially and intramuscular. A review of 33 trials and over 4000 patients randomized to therapy or placebo showed no benefit for amputation and higher risk of adverse events. Therefore, investigations into therapies that may improve metabolic efficiency and function have been conducted. It has been hypothesized that by providing increased levels of carnitine, these agents will improve the Krebs cycle enhancing glucose and oxidative metabolism. Studies in claudicants, however, have shown no convincing benefit, and these agents remain largely investigational. Ranolazine is effective and available for reducing angina in patients with coronary artery disease. A single-center pilot study observed benefits in function versus placebo as measured by pain-free walking time. Trials of these agents have not shown convincing benefit, although there have been promising signals for validation in smaller nonrandomized studies that require validation. Drugs for Venous Thromboembolism Anticoagulant drugs are covered in detail in Chapter 8. The following chapter gives a focused review of their use in venous thromboembolism. The strategy for initial treatment, switching, and long-term treatment is determined by the patient, comorbidities, and their risk in the acute and chronic settings. Dabigatran, a direct thrombin inhibitor, has been studied in the acute setting after a 5day course of a parenteral agent and has not been studied as initial therapy. Edoxaban, an anti-Xa agent, was similarly studied after 5 days of parenteral therapy. The dose should be adjusted to 30 mg once a day for patients with a creatinine clearance between 30 mL and 50 mL per minute, patients with a body weight 60 kg, or those receiving potent inhibitors of P-glycoprotein. For patients with creatinine clearance less than 30 mL per minute, edoxaban should not be used. Parenteral agents are often the first agents utilized, particularly in the hospital setting and when intervention is considered. In cases where an oral agent is desired as the initial agent, rivaroxaban and apixaban have trial data to support that strategy. Drugs for Aortic Aneurysm and Dissection Drugs for aortic dissection and aneurysm are largely directed at blood pressure and heart rate control and are discussed in detail in Chapter 2. Options include metoprolol tartrate, which is B1 specific and has a half-life of $4 hours. For patients with significant systolic hypertension requiring more intensive blood pressure lowering, the mixed and -blocker labetalol is a common choice. Pathophysiology, clinical evaluation, and medical management of aortic dissection. Therapy should be titrated to a heart rate goal of 60 beats per minute as allowed by blood pressure. Patients who require additional blood pressure lowering generally benefit from added vasodilator therapy. Sodium nitroprusside is a preferred agent in this setting and is started at 25 g/min by continuous infusion. Doses can be titrated, but at a rate greater than 2 g/kg/min, toxicity can occur due to cyanide concentrations, and measuring thiocyanate levels should be considered to prevent this toxicity. Long-term Therapy in Aortic Dissection and Aneurysm Patients with dissection who survive to discharge should be treated with a long-acting -blocker. For patients treated with metoprolol tartrate as an inpatient, conversion to metoprolol succinate is recommended. For patients on labetalol, the longer-acting and -antagonist carvedilol can be considered. Change from short- to long-acting therapies improves adherence and avoids changes in heart rate and blood pressure associated with extended dosing intervals that go beyond drug half-life. Initial presentation is often characterized by a heightened sympathetic state requiring high doses of therapies. These may not be well tolerated as patients are followed long-term, and tapering may be required. Home blood pressure monitoring should be considered in order to optimize hemodynamic control. These findings require validation in larger trials and are not currently standard care. Typically, -blocker medications are utilized or, alternatively, nondihydropyridine calcium channel blockers. Summary: Drugs for aortic aneurysm and dissection are centered around hemodynamics to reduce aortic wall stress. In patients with concomitant atherosclerosis, antiplatelet monotherapy and lipidlowering therapies are used in accordance with practice guidelines for patients with atherosclerotic vascular disease. Drugs for Vasculitis Medical therapies for vasculitis generally fall into the class of drugs called immunosuppressive agents and should be prescribed and monitored by physicians familiar with their use. They may be given orally or parenterally, and they may be given at a high, "pulse dose" with an aim of rapidly controlling disease. Long term, however, these agents carry significant toxicity that may result in immunosuppression, weight gain, osteoporosis, and other metabolic abnormalities. Therefore, for long-term control, other agents are often used along with or instead of glucocorticoids as "steroid-sparing agents. Few randomized or comparative trials exist, and choice should be based on the patient, comorbidities, and the disease being treated.
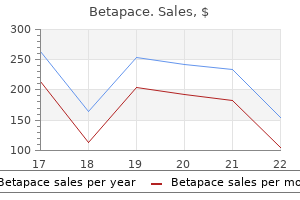
Quality 40 mg betapace
They are also used to reduce postoperative inflammation following cataract surgery blood pressure medication polygraph best buy betapace. Diagnostic Stains Staining agents (also referred to as dyes) color or mark tissue and are used as diagnostic tools in ophthalmology. These agents are instilled topically to diagnose abnormalities of the cornea and conjunctival epithelium or to locate foreign bodies. Diagnostic stains may also be used to observe the flow of aqueous humor or to demonstrate lacrimal system function. They are available as individually wrapped sterile paper strips, which are moistened with a sterile solution and applied to the anterior surface of the eye. Fluorescein sodium (Fluor-I-Strip, Ful-Glo, Fluorescite) is a nontoxic, water-soluble dye that is applied to the cornea or conjunctiva to identify denuded areas of epithelium or foreign bodies. It diagnoses corneal abrasions by staining damaged or diseased corneal tissue bright green, which is best illuminated with the aid of ultraviolet or cobalt light. Fluorescein sodium should not be used with soft contact lenses because they may absorb the dye. Rose bengal and lissamine green in 1% solutions stain devitalized cells better than fluorescein sodium. It is given intravenously outside the surgical setting to visualize the choroidal vascular network. The dye leaks slowly from these choroidal capillaries, which allows vessels in the deeper tissues to be seen (because they are not masked by the dye). As these deeper layers are visualized, tumors and other problems that may not be detectable with regular angiography at this point can be located and treated. Indocyanine green is a fluorescent, sterile, watersoluble dye that comes in powder form and must be reconstituted with sterile water. It contains sodium iodide, so caution must be used for patients with iodide allergies. List two ways in which aseptic technique is used to help to prevent infections during ophthalmic surgery. Cataracts are the leading cause of decreased vision in the United States and globally the leading cause of blindness. With surgical removal being the only treatment, cataract surgery represents the most common and successful of all surgical procedures today. A cataract is defined as an opacity or clouding of the crystalline lens of the eye. Although most cataracts are age related (senile cataract), they may be associated with other factors. The most commonly performed surgical intervention for cataracts in the United States is extracapsular extraction with phacoemulsification and intraocular lens implant. It is not uncommon for the patient to be referred for surgery before the cataract has fully matured. It is safer with less risk of complications and easier removal of the cataract before this stage. This means the perioperative team must coordinate patient preparations in a very short period. The success of surgical intervention depends on the skills and knowledge of the team. Caution Chapter 10-Ophthalmic Agents Medications that are intended for use in the eyes are potent, and one medication error can result in permanent blindness. Therefore all medications and irrigating solutions should be confirmed and labeled immediately. Conventionally, preoperative preparation for cataract extraction involved the installation of multiple drops. These may include but are not limited to a mydriatic for maximum pupil dilation that is essential for lens extraction. A short-acting mydriatic, such as phenylephrine hydrochloride (Neo-Synephrine Ophthalmic) 2. Tropicamide (Mydriacyl) 1% is a commonly used agent that causes cycloplegia (paralysis of accommodation, inhibits focusing), and it also has a mydriatic effect. Assistant Advice When topical mydriatics or cycloplegics are administered for pupil dilation preoperatively, a patient with dark irises may need a larger dose, because more pigment requires more of the medication, to achieve the desired effect. When prepping the site, povidone-iodine ophthalmic solution (Betadine Ophthalmic) 5% is used. The eye is closed, and then the area around the site is prepped the with regular povidone-iodine prep solution. Topical Method of Local Anesthesia the topical method of local anesthesia for cataract extraction has increased in popularity. A combination of anesthetic eye drops, such as tetracaine hydrochloride (Pontocaine) 0. Note the patient may be given only topical local anesthesia to the eye and valium orally to calm nervousness. Some doctors may add an antibiotic to the solution, such as vancomycin or gentamicin. A viscoelastic agent is injected into the anterior chamber to deepen and maintain the chamber and widen the pupil to facilitate the use of the phacoemulsification. After the placement of the intraocular lens implant, timolol maleate (Timoptic) 0. A miotic, such as acetylcholine chloride (Miochol-E), may be used immediately after delivery of the lens to achieve constriction of the iris. Note that gatifloxacin (Zymaxid), which is mentioned in the section on preoperative medications, may be used again. An alternative to this is a subconjunctival injection of a corticosteroid and antibiotic, such as gentamicin sulfate (Garamycin). Assistant Advice Irrigation of the eye is commonly performed during ophthalmic procedures to prevent drying of the cornea and to remove blood and debris from the operative site. This should be performed from the inner canthus to the outer canthus of the eye, to prevent the irrigation and debris from pooling. Postoperative Medications the patient is usually released within a few hours postoperatively (unless there are complications). Medications sent home with the patient will usually include the same topical antiinflammatory agent (to reduce pain and swelling) and antibiotic agents used during the surgical procedure. Advanced Practices: Learning the Language (Key Terms) Using your textbook or a standard medical dictionary, look up and write the definitions of each item. Multiple dosages of mydriatic drops may be needed to achieve pupil dilation on a patient with A. State average adult circulating volume of blood, hemoglobin, and hematocrit values. List available options for blood replacement and discuss autologous and homologous blood donation. Describe the procedure for blood replacement in surgery using donor blood from the blood bank. One of the primary goals of the surgical team is to maintain the patient in as stable a physiologic state as possible. Because fluids are essential to survival, blood and fluid replacement are two of the most common means used in surgery to assist in maintaining homeostasis. Most surgical patients will have preoperative fluid and food restrictions before surgery, so fluid replacement is usually indicated. Replacement fluids are often ordered to replenish losses caused by hemorrhage (in surgery) or vomiting and diarrhea (in the medical setting). In addition, fluids are administered topically to irrigate body tissues during surgical procedures. These irrigation solutions must be physiologically acceptable to tissues, while providing visualization, removing blood and debris, and adding medications to the surgical site. The surgical technologist will observe blood or fluid loss and replacement and assist with irrigation during surgical procedures. Fluid and Electrolyte Management Physiology Review In a healthy adult, approximately 60% of the total body weight is made up of fluids, electrolytes, and nonelectrolytes.
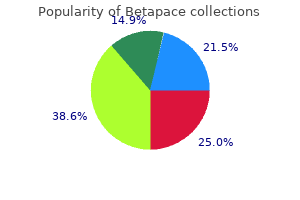
Discount 40 mg betapace otc
Therefore pulse pressure and exercise betapace 40mg with amex, it is still important to understand this eclectic group of pharmacotherapies. Antiarrhythmic Drugs Antiarrhythmic drugs are used to suppress arrhythmias with the hopes of alleviating significant symptoms or possibly to affect survival. Therefore, antiarrhythmic drugs should only be used when the suppression of arrhythmia outweighs the adverse effects of the drug. There are very few instances where antiarrhythmic drugs may actually reduce mortality and/or sudden death. Class I agents decrease phase zero of the rapid depolarization of the action potential (rapid sodium channel). In the lower panel are shown the major currents on which antiarrhythmics act, according to the Sicilian gambit. Ca-L, long-lasting calcium; I, current; If, inward funny current; Kr, rapid component of repolarizing potassium current; Ks, slow component; Na, sodium; to , transient outward. These agents can be used for treatment of either ventricular or atrial arrhythmias. There are no large-scale outcome trials to suggest that quinidine or other class I agents decrease mortality; rather there is indirect evidence that suggests increased mortality. Today, because of limited availability in some countries as well as its proarrhythmic potential, quinidine is not used as often, although its application to Brugada syndrome has led to a very small resurgence of interest in the drug. Quinidine is not often used today but can be used for the treatment of both atrial and ventricular arrhythmias. This impairs the inward sodium current and results in an unopposed Ito (transient outward potassium current) activity, which can set up Table 9. Side effects and contraindications Reduce dose by half if liver blood flow low (shock, blockade, cirrhosis, cimetidine, severe heart failure). Interactions and precautions -blockers decrease hepatic blood flow and increase blood levels. Hypotension, vertigo, dysarthria, lethargy, gingivitis, macrocytic anemia, lupus, pulmonary infiltrates. Torsades de pointes in 3% of patients which can be Interactions and precautions Digoxin level increased. Enzyme hepatic inducers are barbiturates, phenytoin, and rifampin, which induce hepatic enzymes, thereby decreasing blood levels of the drug. For atrial and ventricular arrhythmias, quinidine sulfate intermediate release can be started at 200 mg every 6 hours and cautiously titrated upward. The major side effect of quinidine is ventricular proarrhythmia and sudden death, in particular torsades de pointes. The number of culprit drugs interacting with quinidine is too numerous to list here but should always be checked when a patient is put on this drug. The result is a very rapid ventricular rate that can even degenerate to ventricular tachycardia/fibrillation and can be life-threatening. Procainamide can be used for the treatment of both atrial and ventricular arrhythmias. It is particularly useful for acute medical conversion in the emergency department. This can dramatically increase the ventricular rate of the arrhythmia and even precipitate ventricular fibrillation, which is lifethreatening. Development of either rising titers or symptoms should lead to drug discontinuation. Agranulocytosis, neutropenia, hypoplastic anemia, and thrombocytopenia can all occur in 0. Weekly blood monitoring is required for the first 3 months and then periodically thereafter. Blood counts may return back to normal within 1 month if the drug is discontinued. However, it is not a very potent antiarrhythmic for either the ventricle or atrium. The negative inotropy can be useful for patients with hypertrophic obstructive cardiomyopathy, particularly for reduction in outflow gradients. Disopyramide is more effective than both -blockers and verapamil for outflow tract gradient reduction10 and is often used prior to consideration of invasive therapy such as septal myectomy or alcohol ablation. Coadministration with pyridostigmine can alleviate the anticholinergic effects without impairing the antiarrhythmic effect. Some antiarrhythmic agents act at least in part chiefly by prolonging the action potential duration, such as amiodarone and sotalol. They also have rapid kinetics, which means they associate and dissociate from the sodium channels rapidly. They have a particular affinity for binding with inactivated sodium channels with rapid onset-offset kinetics, which may be why such drugs are more selective for sodium channels in ventricular tissue versus atrial tissue. Lidocaine acts preferentially on the ischemic myocardium and is more effective in the presence of a high external potassium concentration. Therefore, hypokalemia must be corrected for maximum efficacy (also for other class I agents). The two critical factors governing lidocaine metabolism and hence its efficacy are liver blood flow (decreased in old age and by heart failure, -blockade, and cimetidine) and liver microsomal activity (enzyme inducers). Lidocaine metabolites circulate in high concentrations and may contribute to toxic and therapeutic actions. After prolonged infusions, the half-life may be longer (up to 24 hours) because of redistribution from poorly perfused tissues. To achieve and to maintain an adequate blood level of lidocaine requires an initial bolus followed by an infusion. Often, a second bolus is required to get a steady state in addition to the infusion. Heart failure and liver failure delay metabolism of lidocaine which can increase the blood level and the accompanying danger of toxic effects. Poor liver blood flow (low cardiac output or -blockade), liver disease, or cimetidine or halothane therapy calls for halved dosage. In patients receiving cimetidine, propranolol, or halothane, the hepatic clearance of lidocaine is reduced, and toxicity may occur more readily, so that the dose should be reduced. With hepatic enzyme inducers (barbiturates, phenytoin, and rifampin), the dose needs to be increased. Combination of lidocaine with early -blockade is generally acceptable, because -blockade can reduce liver blood flow and can rarely potentiate lidocaine-associated side effects (Tables 9. If lidocaine apparently fails, consider other problems, especially concomitant hypokalemia, hypomagnesemia, severe ongoing ischemia, or other reversible underlying factors. There may have been a technical error in dosing-often people forget to bolus twice before starting the infusion.
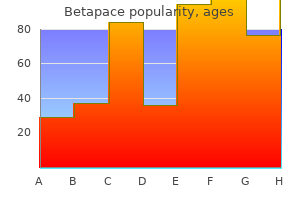
Betapace 40mg with amex
It can also result from impaction of the posterior shoulder on the maternal sacral promontory heart attack xi purchase betapace 40 mg otc. Retraction of the fetal head against the maternal perineum accompanied by difficulty in accomplishing external rotation has been called the "turtle Protocols for High-Risk Pregnancies: An Evidence-Based Approach, Seventh Edition. Even if the birthweight of the infant is over 4000 g, shoulder dystocia will only complicate 3. Risks for shoulder dystocia based on known (but not estimated) fetal weight are listed in Table 56. A prior shoulder dystocia has been shown to statistically increase the risk of recurrence. No single associated condition or combination of antenatal factors (such as excessive maternal weight gain, oxytocin use, multiparity, epidural use, precipitate or prolonged second stage of labor) prospectively allows for clinically useful positive predictive values for the antennal prediction of shoulder dystocia. Management There are no randomized clinical trials to guide physicians in the order of maneuvers that are to be performed. A single randomized trial assessing prophylactic usage of the McRoberts maneuver showed no difference in headtobody delivery times. The best available evidence shows fetal injury to be associated with all described maneuvers to relieve shoulder dystocia. The length of delay that results in permanent brain injury will depend on the condition of the fetus at the time that the shoulder dystocia is diagnosed. Most, if not all, of the commonly encountered shoulder dystocia episodes can be relieved within several minutes. Shoulder Dystocia 583 3 Additional assistance may be obtained by summoning other obstetricians, an anesthetist or anesthesiologist, additional nursing support, or a pediatrician. McRoberts position causes cephalic rotation of the pubic symphysis and flattening of the sacrum. Care should be taken to avoid prolonged or overly aggressive application of McRoberts. This pressure is usually directed posteriorly, but other described techniques have included lateral application from either side of the maternal abdomen (attempting to flex the anterior shoulder towards the chest) or alternating between sides using a rocking pressure. Posterior arm extraction replaces the biacromial diameter with the axilloacromial diameter, thereby reducing the obstructing diameter in the pelvis. Rotation of the fetal trunk to bring the posterior arm anteriorly is sometimes required. Grasping and pulling directly on the fetal arm, as well as application of pressure onto the midhumeral shaft, should be avoided as bone fracture may occur. In the Woods corkscrew maneuver, the practitioner attempts to abduct the posterior shoulder by exerting pressure onto its anterior surface. In the Rubin (reverse Woods) maneuver, pressure is applied to the posterior surface of the most accessible part of the fetal shoulder (either the anterior or posterior shoulder). If the anterior shoulder is tightly wedged underneath the symphysis pubis, it may be necessary to push the fetus slightly upward in order to facilitate the rotation. The need for cutting a generous 584 Protocol 56 episiotomy or proctoepisiotomy must be based on clinical circumstances, such as a narrow vaginal fourchette in a nulliparous patient. Pushing on the fundus serves only to further impact the anterior shoulder behind the symphysis pubis. Fundal pressure can be employed to assist with delivery of the fetal body, but only if the shoulder dystocia has already been alleviated. In this case, the anterior arm is lodged behind the symphysis pubis and/or the posterior shoulder is lodged high in the pelvis at or near the sacral promontory. Under these circumstances, consideration should be given to the following "rescue" maneuvers. This change in maternal position is thought to allow for a change in fetal position within the maternal pelvis. An attempt is now made to deliver the posterior shoulder by downward (toward the floor) traction followed by delivery of the anterior fetal shoulder by gentle upward traction. The fetal shoulder is located and grasped by sliding the first finger under the axilla and placing the thumb on top of the shoulder. The second finger is placed alongside the fetal humerus to keep the arm firmly against the body. Traction is applied directly through the fetal axilla to follow the sacral curve until the posterior shoulder appears over the perineum. Cephalic replacement (Zavanelli maneuver) the fetal head is rotated back to a prerestitution occiput anterior position and then gently flexed. Constant firm pressure is used to push the fetal head back into the vagina and cesarean delivery is subsequently performed. Shoulder Dystocia 585 Halothane or other general anesthetics, in conjunction with tocolytic agents, may be administered. Abdominal rescue A low transverse uterine incision can be performed, the anterior shoulder manually rotated into the oblique diameter by the surgeon doing the uterine incision, and vaginal delivery accomplished. Documentation Documentation of delivery maneuvers and the sequence of these maneuvers is an essential part of patient care and risk management. The use of a preprinted form listing important elements is suggested for use in cases of shoulder dystocia, regardless of apparent fetal injury at the time of delivery. Shoulder dystocia: the unpreventable obstetric emergency with empiric management guidelines. A comparison of obstetric maneuvers for the acute management of shoulder dystocia. Fatal shoulder dystocia: a review of 56 cases reported to the Confidential Enquiry into Stillbirths and Deaths in Infancy. Management of shoulder dystocia: trends in incidence and maternal and neonatal morbidity. Shoulder dystocia and associated risk factors with macrosomic infants born in California. An objective definition of shoulder dystocia: prolonged headtobody delivery intervals and/or the use of ancillary obstetric maneuvers. The number of triplet, quadruplet, and higherorder multiple births increased over 400% before peaking in recent years. The two major factors accounting for these increases are the widespread availability of assisted reproductive technologies and increasing maternal age at childbirth. Compared to singletons, multifetal pregnancies are associated with higher risks for both maternal and fetal complications. Women carrying multiples are at risk for a number of pregnancy complications in both the antepartum and postpartum period, including hyperemesis, gestational diabetes, hypertension, preeclampsia, anemia, cholestasis, hemorrhage, cesarean delivery, and postpartum depression Although multiple gestations represent only a fraction of all pregnancies in the United States, they account for a disproportionate number of infant deaths. Given the maternal and fetal risks, patients with multiple gestations require close monitoring and frequent followup throughout pregnancy as well as careful planning of mode and time of delivery. Pathophysiology Multiple gestations result either from the fertilization of multiple ova or from the division of a single fertilized ovum or early embryo into more than one fetus. The terms "monozygotic" and "dizygotic" refer to the number of ova responsible for a multiple gestation. A monozygotic pregnancy Protocols for High-Risk Pregnancies: An Evidence-Based Approach, Seventh Edition. In contrast, dizygotic pregnancies originate from the fertilization of two separate ova and are therefore genetically dissimilar. In contrast, the frequency of dizygotic twins varies by maternal age, parity, family history, maternal weight, nutritional state, race, and use of infertility drugs. In the United States, twothirds of spontaneously occurring twins are dizygotic and onethird are monozygotic. As a result of these higher gonadotropin levels, multiple ovulations can occur in a single menstrual cycle, increasing the likelihood of dizygotic twinning. Gonadotropin levels fluctuate depending on maternal age, weight, nutrition, parity, and heredity. For these reasons, both infertility treatments and advanced maternal age are associated with increased frequency of dizygotic twinning. Placentation It is clinically important to determine the placentation, chorionicity, and amnionicity of multiple pregnancies.
Cheap betapace 40 mg mastercard
Ropivacaine (Naropin) is an aminoamide local anesthetic agent released for use in 1996 blood pressure chart with age and height buy betapace 40 mg visa. This type of packaging enables the surgical technologist to fill a syringe with the agent at the sterile back table rather than requiring the circulator to hold the container for delivery to the field (see Chapter 4). Mepivacaine is used less often, because it does not have a significant advantage over lidocaine, which is used more frequently and thus is more readily available. Tech Tip For the prevention of dose-related toxicity, it is vital that the surgical technologist keep track of the amount of any local anesthetic agent used from the sterile back table. Use a sterile marking pen (see Chapter 6) to keep a running total of the volume used, so that the concentration and final total amount can be accurately reported to the anesthesia care provider. The anesthesia care provider will use this information to calculate and record the actual dose of local anesthetic administered. Excitement may or may not occur, and the patient may go from a drowsy state to unconsciousness and into respiratory arrest. Cardiovascular adverse effects are also dose-related and include hypotension, bradycardia, and ventricular arrhythmias, leading to possible cardiac arrest. Systemic toxicity of local anesthetics is most commonly caused by inadvertent intravascular injection during peripheral nerve infiltration. Quick Question Why are concentration and volume of a local anesthetic agent important when reporting the final total Regional Anesthesia Regional anesthesia is a technique used to accomplish both sensory and motor block to an entire area of the body. Regional anesthesia blocks nerves (not just nerve endings) or groups of nerves (called a plexus) at specific locations; thus it provides a larger anesthetized area. Regional blocks can affect sympathetic, sensory, and motor nerve supply, so an anesthetized limb may be immobile, as well as numb. Regional blocks are effective for many types of surgical procedures but frequently take more time to administer than a general anesthetic. Various types of regional anesthetic techniques are usually named for the nerves or areas of the body to be blocked. Although nearly any group of nerves can be blocked, we discuss only the most frequently used regional anesthetic techniques in this text. The most commonly used regional blocks are spinal and epidural, collectively referred to as central neuraxial blockade. Preoperative preparation may include administration of anxiolytics and analgesics (see Chapter 13) to minimize discomfort. The circulator usually assists the anesthesia care provider during injection of a spinal anesthetic by helping the patient to get into optimum position. The patient may be positioned laterally to facilitate correct needle placement. Thus the patient is usually instructed to curl up as much as possible, pushing his or her lower back out toward the anesthesia care provider. This position spreads the vertebral bodies apart so the spinal needle may be more easily inserted, but it is difficult for some patients, especially the elderly, to curl their backs. These patients may be assisted gently into position, with caution to avoid injury. Alternatively, patients may be in a sitting position for administration of a spinal anesthetic. The patient may sit on the operating bed with his or her back to the anesthesia care provider. Skin around the injection site area is prepped with an antiseptic agent, and a small, fenestrated sterile drape is placed over the area. Local anesthesia is injected through skin and subcutaneous tissue before insertion of a spinal needle through the ligaments and dura. The agent is injected, the needle and syringe are withdrawn, and the patient is placed in supine position. Alcohol will feel cold on an unblocked area of skin and warm or neutral on a blocked area. Another technique that may be used to assess the level of spinal anesthesia is pinprick. The patient feels a sharp pinprick on an unblocked area of skin, and a dull sensation on a blocked area. Spinal anesthesia is usually quicker to administer than an epidural and provides more intense sensory and motor blockade. If continuous spinal anesthesia is indicated, a small catheter is placed for repeated dosing. The most common local anesthetic agents used for spinal anesthesia include tetracaine, bupivacaine, and ropivacaine. Local anesthetic agents used for spinal and epidural anesthesia must be formulated as preservative-free, and this will be clearly indicated on the drug label. Dilute epinephrine may be added to prolong blockade, but it may also delay postoperative urination during recovery, so epinephrine is less frequently used for outpatient surgery. Instead, an opioid, such as fentanyl or sufentanil, may be added to prolong duration of spinal anesthesia without prolonging recovery time. Spinal anesthesia is used for procedures of the lower abdomen, perineum, and lower extremities. It is often used for transurethral resection of the prostate gland or bladder tumors, for lower leg vascular procedures (such as embolectomy), for select orthopedic procedures (such as total knee arthroplasty), and for cesarean sections. Younger, more athletic patients with lower resting heart rates have a higher risk for significant bradycardia under spinal anesthesia. Note An extreme complication of neurotoxicity attributed to the use of 5% lidocaine in spinal anesthesia is cauda equina syndrome, a paralysis of nerves resulting in lower extremity muscle weakness and impaired bowel and bladder function. Lidocaine in high concentrations (5%) is not used in spinal anesthesia because of the potential for neurotoxicity. Intrathecal catheters and pumps are used to deliver analgesics to patients with various types of chronic pain. A single injection may be administered, or a catheter may be placed for continuous infusion or repeated injections. Sedation may be given to help relieve discomfort of injection and catheter placement (except in pregnant patients because sedation would also affect the baby). When indicated for use in pediatric patients, an epidural is placed after general anesthesia is induced. Positioning, prepping, and draping for administration of an epidural anesthetic are identical to those described for a spinal anesthetic. Local anesthesia is administered at the injection site and an epidural needle is placed. A test dose of agent is administered, followed by small doses at intervals over a 1to 3-minute period. Common agents used for epidural anesthesia include lidocaine, bupivacaine, and ropivacaine. Dilute epinephrine (1:200,000) may be added to prolong duration, and small doses of opioids may be used to manage postoperative pain. Epidural anesthesia is used to relieve the pain of labor and vaginal delivery, as well as to provide anesthesia for cesarean section. A motor block will almost always be obtained with a bupivacaine concentration of 0. Epidural blocks may also be used as an adjunct to general anesthesia in select patients to minimize the amount of general anesthesia needed; they may also be used for postoperative pain control after such procedures as thoracotomy. In addition, epidural anesthesia may be administered at levels above L3 to L4-for example, at T4-T5 for thoracic analgesia. Epidural anesthesia requires greater volume of agent (typically 20 mL) than spinal (typically 1 to 2 mL) and has a slower but longer onset of action. Caudal blocks are primarily used in conjunction with general anesthesia for urologic and lower extremity surgical procedures in children for postoperative pain management. Although less common now, caudal blocks may be used for vaginal childbirth, but they are administered in the obstetric unit rather than in the surgical suite. These types of blocks may be used for procedures on distal arms and legs, the hand and fingers, and foot and toes.
Syndromes
- 1 - 3 years: 0.7 mg/day
- Trouble falling asleep on most nights
- Stool cultures to check for an infection
- Rapid drop in blood pressure
- Damage to the stomach, esophagus, liver, or small intestine. This is very rare.
- Intravenous pyelogram (IVP)
Discount betapace 40 mg with amex
Side effects are typically dose-related arteria 2013 betapace 40mg with visa, but they often improve with symptomatic support and time, without necessitating dose decrease. For patients using subcutaneous delivery devices for treprostinil, injection site pain is common occurrence, and can often be managed by rotating the infusion site. Fewer than 10% of patients may have to discontinue therapy due to injection site pain. In one observational series of patients on long-term epoprostenol, there were 119-line infections, and 70 episodes of sepsis, in 162 over an average of 3 years of follow-up. These include hypotension as well as high output heart failure, which may lead to pulmonary edema. Hyperthyroidism was more common among patients taking selexipag than placebo in a large clinical trial. Major adverse events included headache, dyspepsia, dizziness, nausea, and vomiting. In a trial of 213 patients randomized to bosentan or placebo, the incidence of abnormal liver function tests >five times the upper limit of normal. This occurred in 3% of participants taking placebo, 4% among patients taking 125 mg twice daily, but 14% among participants taking 250 mg twice daily. Macitentan is generally very well tolerated, but headache, nasopharyngitis, and anemia have been seen with higher frequency in participants taking macitentan compared with controls. In all prostanoids, the antiplatelet and antithrombotic effects might be exacerbated in patients who receive anticoagulation for other indications. There has been some concern for decreased clearance of furosemide in patients administered both epoprostenol and furosemide, but the effect was small, found in only a single study, and may be statistical aberration. Coadministration with strong inhibitors of this enzyme, such as 652 11 - Drugs for Pulmonary Hypertension gemfibrozil, is not advised due to the risk of selexipag toxicity. It should be noted, however, that the systemic blood pressure lowering effect of these agents is modest; in a preapproval hemodynamic study of healthy volunteers, administration of a high dose of sildenafil (50 mg three times daily) resulted in a systemic systolic blood pressure decrease of only 6 mmHg. Additional agents leveraging established therapeutic pathways are currently under development. High-dose calcium channel blockers were used off-label prior to approval of epoprostenol in 1995. This page intentionally left blank Index Note: Page numbers followed by f indicate figures, t indicate tables, and b indicate boxes. Discuss common categories of antibiotics used in surgery and give examples of each. Before the discovery of antimicrobial agents, surgical patients often died from postoperative wound infections. It was not known that bacteria were the cause of surgical wound infections, so there was no concept of aseptic surgical practice. Discovery of the existence of bacteria and their role in surgical wound infections eventually led to the development of modern aseptic practices (also known as sterile techniques). The incorporation of sterile techniques into surgical practice helped to reduce but not completely eliminate postoperative wound infections. The discovery of antimicrobial agents and their ability to treat surgical wound infections has saved countless lives. Although many antimicrobial agents have been developed, there has also been a dramatic increase in the number of bacterial species that are now resistant to many of these agents, causing a disturbing resurgence of deadly infections. These include antibacterials, antiprotozoals, antifungals, antiparasitics, and drugs, such as sulfa and mercury (Insight 5. Because bacteria are the cause of surgical wound infections, the only category of antimicrobial agents routinely used in surgery are antibacterials, commonly referred to as antibiotics. Make It Simple the word "antibiotic" takes its name from the Greek words anti, which means "against," and bios, which means "life. When the prefix "anti-" is combined with other root words, the meaning of these terms for medication categories becomes clearer. For example, the word anti/bacteri/al indicates pertaining to; against; bacteria, which is more precise than the more commonly used term antibiotic. Antibiotics are effective tools used to supplement the conscientious practice of sterile techniques. These agents may be administered during surgery from the sterile back table in the form of topical irrigation or application of an antibiotic ointment for surgical dressings. The use of topical antibiotic irrigation at the surgical site has been almost routine in some cases. However, the increase in antibiotic resistance has caused some discussion about the careful use of antibiotics. Caution the availability of antibiotic therapy is never considered a substitute for the consistent, mindful, and meticulous practice of sterile techniques. At this time antibiotics had yet to be discovered, but the medicinal properties of mercury were well known. Mercurials were used for the treatment of venereal diseases and also as powerful laxatives. The fact that mercury, which passed through the human digestive system more than 200 years ago, can still be detected speaks to the potency of this medication. The checklist has three sections: before the induction of anesthesia, before the skin incision, and before the patient leaves the operating room. The second section of the checklist contains a task to confirm that antibiotic administration has been accomplished within the optimal time frame. So what are these crucial agents known as antibiotics, and where do they come from Antibiotics are derived from natural chemicals (or metabolites) produced by microorganisms that inhibit the growth of other microorganisms. Microorganisms that produce antimicrobial substances include fungi (and molds, a type of fungi) and bacteria. These natural chemicals are identified, cultured, extracted, and purified for medicinal use in a pharmaceutic laboratory. Bacitracin and the polymyxins are examples of natural agents produced by bacteria of the genus Bacillus. A natural substance may be altered in the laboratory to produce semisynthetic (see Chapter 1) antibiotics, such as some penicillins and the aminoglycosides. Cephalosporins are derived from a substance produced by the mold Cephalosporium acremonium, found in the ocean near a sewage outflow. Each antibiotic in a family is similar to the original chemical but can be used to treat different types of infections because it has different properties. Other antimicrobial chemicals, such as sulfonamides and fluoroquinolones, are developed in the laboratory by chemical synthesis, and these are classified as synthetic antibacterial agents. This is a common method of determining which antibiotics are effective against a specific bacterium or fungus. Various types of antibiotic agents impregnated on paper are positioned in the culture medium, which has been inoculated with the microorganism (A). The pathogen must have a source, means of transmission, and susceptible host to cause an infection. Exogenous sources of pathogenic microbes include surgical personnel and the environment. Source of pathogenic microbe plus transmission route plus susceptible host equals infection. Caution A rare but documented example of an exogenous source of infectious microbes is various bacteria carried under artificial fingernails. Such microbes are thought to be introduced into the surgical site by glove tears commonly associated with long fingernails. Surgical instruments that are not properly cleaned before sterilization may carry viable microbes into a surgical wound and thus are another example of an exogenous source of pathogens. A specimen containing the pathogenic microorganism to be identified is swabbed onto a slide and fixed. Gram-negative bacteria lose the purple stain during decolorization, so they appear red or reddish-pink after application of safranin. A broad-spectrum antibiotic is prescribed to begin treatment, while awaiting the results of identification testing. Occasionally, during a surgical procedure, such as an incision and drainage, a sample of abscess fluid may be subjected to an immediate Gram stain process (Insight 5.
Cheap generic betapace uk
The addition of pentoxifylline to conventional therapy improves outcome in patients with peripartum cardiomyopathy blood pressure chart heart foundation betapace 40 mg low cost. Evidence of autoantibodies against cardiac troponin I and sarcomeric myosin in peripartum cardiomyopathy. The correlation between peripartum cardiomyopathy and autoantibodies against cardiovascular receptors. Activation of signal transducer and activator of transcription 3 protects cardiomyocytes from hypoxia/reoxygenation-induced oxidative stress through the upregulation of manganese superoxide dismutase. Elevated vasoinhibins may contribute to endothelial cell dysfunction and low birth weight in preeclampsia. Signal transducer and activator of transcription 3-mediated regulation of miR-199a-5p links cardiomyocyte and endothelial cell function in the heart: a key role for ubiquitin-conjugating enzymes. Activation of the neuregulin/ErbB system during physiological ventricular remodeling in pregnancy. Evaluation of bromocriptine in the treatment of acute severe peripartum cardiomyopathy: a proof-of-concept pilot study. Rationale and design of a randomized, controlled multicentre clinical trial to evaluate the effect of bromocriptine on left ventricular function in women with peripartum cardiomyopathy. Myofilament Remodeling and function is more impaired in peripartum cardiomyopathy compared with dilated cardiomyopathy and ischemic heart disease. Inhibition of cardiac myocyte apoptosis improves cardiac function and abolishes mortality in the peripartum cardiomyopathy of Galpha(q) transgenic mice. Petriea,c a Institute of Cardiovascular and Medical Sciences, University of Glasgow, Glasgow, Scotland, United Kingdom b Department of Cardiology, University Medical Center Groningen, Groningen, the Netherlands c Glasgow Royal Infirmary, Glasgow, Scotland, United Kingdom Many women present with nonspecific symptoms during or after pregnancy, and to a host of medical professionals. Shortness of breath, fatigue, and mild ankle swelling are less specific symptoms of heart failure during pregnancy, whereas orthopnea and paroxysmal nocturnal dyspnea are more specific. Any of these symptoms should prompt clinical evaluation and consideration of investigations. Thorough clinical examination is important to elucidate signs of heart failure in any peripartum woman with a potentially cardiacrelated presentation. Tachycardia, tachypnea, and extremes of blood pressure are nonspecific findings, but should point a clinician toward the possibility of cardiac dysfunction. Jugular venous distension and a third heart sound are more specific signs of heart failure. Electrocardiography the electrocardiogram is a widely available, cheap, and powerful diagnostic tool in heart failure. Most rhythm disturbances in a pregnant woman, in particular brady- or tachyarrhythmias or frequent ventricular ectopy, warrant further assessment of cardiac function. Blood tests and biomarkers As with heart failure due to other causes, routine hematological and biochemical testing can provide information about potentially reversible contributory factors, such as clinically significant anemia, and help to establish the presence of end organ damage. Some studies suggest that natriuretic peptide levels are higher in healthy pregnant women compared to nonpregnant women, though levels still fall below the upper limits of what is considered normal [5,6]. In the future, there may be a role for screening asymptomatic women looking for cardiac disease using natriuretic peptide testing, but this approach has not been validated. Higher levels of soluble fms-like tyrosine kinase 1 and serum troponin correlate inversely with myocardial recovery [10,11]. Specific blood tests, such as creatinine kinase and ferritin, can be used to investigate other causes of dilated cardiomyopathy. When positive findings do exist, they include cardiomegaly and/or features of pulmonary congestion. There is a common misconception that pregnant women should not undergo chest radiography when, in reality, the fetal radiation dose is low (< 0. Fetal radiation doses of such a low level are not associated with fetal malformation or a significant increase in risk of childhood cancers [12]. All decisions to perform investigations involving radiation should be reached in consensus with the mother. Importantly, it also excludes alternative causes of heart failure, such as primary valvular disease, a number of inherited or acquired cardiomyopathies, and congenital heart disease. The mean left ventricular ejection fraction at the time of diagnosis is around 30% [1]. Coexisting functional mitral regurgitation and right ventricular dysfunction are common, the latter being evident in up to a third of women at the time of diagnosis [1]. A comprehensive assessment of the right heart is important if advanced heart failure therapies are likely to be required. Furthermore, reduced right ventricular function has also been shown to be an independent predictor of a worse outcome [15]. In addition to assessing cardiac structure and function, echocardiography is an important tool in the identification of heart failure sequelae, such as intracardiac thrombi. Current evidence does not provide a clear answer with regards to tissue characterization in the condition, with a reported prevalence of late gadolinium enhancement ranging from 0% to 70% in two studies [16,17]. It is considered safe in pregnancy, although gadolinium contrast agent is not [18]. In breastfeeding, only a very small percentage of gadolinium enters the breast milk and virtually none is absorbed across the normal gut; therefore, cessation of breastfeeding is not routinely advised [19]. Echocardiography is the next step in investigation, prior to more advanced imaging where this is available. Patients with abnormal cardiac investigations should be referred promptly to a cardiology team for specialist management. Burden of arrhythmias in peripartum cardiomyopathy: analysis of 9841 hospitalizations. Longitudinal changes in the B-type natriuretic peptide levels in normal pregnancy and postpartum. Protection of pregnant patients during diagnostic medical exposures to ionising radiation. Myocardial damage detected by late gadolinium enhancement cardiac magnetic resonance is uncommon in peripartum cardiomyopathy. Patient characteristics Age In a retrospective study in the United States, Whitehead et al. Risk stratification in patients newly diagnosed with peripartum cardiomyopathy 23 Hemodynamic parameters In a prospective study of 100 patients from South Africa, Sliwa et al. In a further prospective study, including 206 patients from South Africa, Libhaber et al. This apparent discrepancy mainly depends on the definition of normal, particularly with regards to repolarization abnormalities. The 2 groups of patients had the same left ventricular size and systolic dysfunction at diagnosis and at discharge. Life-threatening complications include severe heart failure, cardiogenic shock, arrhythmias, thromboembolic complications, and death. Moreover, unfavorable outcomes have been reported in women with severe biventricular dysfunction [37]. Due to the rapid decline after delivery and pregnancy, and the related variability of these biomarkers, their use seems to be limited. However, a German cohort study showed that the recovery rate of patients with a positive family history of cardiomyopathy, which was present in 16. Risk stratification should gather and integrate the different parameters mentioned. Other parameters, including older age, ante-partum diagnosis, hemodynamic parameters at presentation, and cardiac biomarkers, might help refine the risk stratification. Predictors of outcome in 176 South African patients with peripartum cardiomyopathy. Pregnancyassociated cardiomyopathy: clinical characteristics and a comparison between early and late presentation. Comparison of clinical characteristics and outcomes of peripartum cardiomyopathy between African American and Non-African American women. Different characteristics of peripartum cardiomyopathy between patients complicated with and without hypertensive disorders. Phenotyping and outcome on contemporary management in a German cohort of patients with peripartum cardiomyopathy. Predictors of left ventricular recovery in a cohort of peripartum cardiomyopathy patients recruited via the internet.
Buy cheap betapace 40mg line
This method was popular for a time until transfusion reactions were recognized and reported blood pressure medication with diabetes generic betapace 40 mg on line. James Blundell performed many transfusions in the early nineteenth century (approximately half were successful), developed instruments for the process, and published his results. Since the discovery that all human blood is not alike in 1901 by Karl Landsteiner, many advances have been made in blood transfusion therapy. Currently, blood transfusions are implemented with the knowledge that blood must be compatible in type and Rh factor. The most common indication for blood replacement in surgery is hypovolemia (low circulating blood volume), seen most frequently in trauma and vascular procedures. When patients lose a certain amount of blood, they experience this syndrome, which is also called hemorrhagic or circulatory shock. The result is decreased oxygen supplied to vital organs, increased heart rate, and decreased cardiac output. This can be further complicated by the anesthetic, which may enhance the effects of hemorrhage. Other indications for blood replacement include restoration of the oxygen-carrying capacity, as seen in anemic patients or those with blood diseases, and to maintain clotting properties, as needed in patients with hemophilia. In either case, the surgeon must document the need for blood release without compatibility testing. Some of these options may not be feasible in certain cases, depending on the situation. A blood bank is responsible for collecting, processing, and releasing donor blood for use. All blood donors go through careful screening of their medical history, and those who are at risk of transmitting an infectious disease are not allowed to donate. However, it is still possible for donor blood to present some risk for transmission of bloodborne pathogens. Blood is separated during processing into components and then administered to treat specific needs. Component replacement therapy is an effective and efficient use of limited resources because a unit of donor whole blood separated into components can be used to treat several patients. Whole Blood the term whole blood indicates the blood composition has not been broken down or altered. Note In some situations involving massive trauma and severe blood loss, the replacement of blood and fluids may be as a "1:1:1 ratio. Packed cells are obtained by removing approximately 200 mL of plasma and most of the platelets from 1 unit (500 mL) of whole blood. Plasma Plasma may be administered when clotting factors are needed in addition to circulating volume. This need is frequently seen when several units of blood have been replaced because the clotting factors have been removed from donor blood. Plasma is not used for volume expansion alone because albumin and synthetic expanders are as effective and eliminate the risk of transmission of bloodborne diseases. Plasma is stored as fresh-frozen plasma to preserve clotting factors and thawed in a water bath before use. Platelets are infused to restore a more normal clotting process and to help to repair damaged blood vessels. They may also be administered prophylactically in patients who have low platelet counts, such as those receiving chemotherapy or radiation therapy or with leukemia. At room temperature, platelets must be continually gently agitated to prevent clumping. A unit of platelets is defined as the amount separated from a unit of whole blood. They do not have a blood type, so can be received from any qualified donor (or donors). Platelet-rich plasma, growth factors obtained from platelet concentrate, can be obtained from blood plasma for wound healing (Insight 11. Cryoprecipitate may be administered in surgery when massive amounts of blood have been replaced, severely impacting the normal coagulation process. It is usually given in 4 to 6 unit pools at a time rather than a single unit, and blood typing is not required. When this platelet concentrate is reintroduced into the wound, it releases growth factors that recruit and increase the reparative cells. It is used for wound healing in surgery, treatment of tendonitis, cartilage repair, cardiac care, spinal disc regeneration, and dental care. Autologous Donation Patients scheduled for elective surgical procedures in which blood loss is anticipated, such as a total hip replacement, may be allowed to donate their own blood. This can be done up to 4 days before surgery, although a much longer period of time, such as 1 month, is preferred. This process is called autologous transfusion and usually involves two units of blood. Most patients can safely donate two units of whole blood over a period of weeks just before their scheduled procedure, possibly eliminating the need for donor blood. Patients often choose this option, if available, to protect themselves from potential bloodborne disease transmission. However, some medical conditions may make autologous donation unsafe, so not all patients are eligible. Autotransfusion Another form of autologous donation used intraoperatively and postoperatively is called autotransfusion. Some are designed specifically for emergency procedures when rapid infusion is required. Blood can be collected in a suctiontype device or via bloody sponges drained into a sterile basin of saline, then aspirated into the machine. However, blood that has been exposed to collagen hemostatic agents and some medications (such as certain antibiotics) cannot be used because clotting in the machine may occur. When the canister is filled, the blood is washed in a red cell washer (usually found in the blood bank) and reinfused. In this method, the blood is sent out of the surgical department to be washed, and so there is time lost before reinfusion. Autotransfusion is performed during open heart surgery, vascular procedures, major orthopedic procedures, and some trauma procedures, such as splenectomy. Autotransfusion has several advantages over the use of donor blood, including immediate replacement of blood loss without the potential for transfusion reaction or delay for blood typing and cross-matching and no risk of transmission of bloodborne pathogens. In addition, patients with religious objections to donated blood often do not object to autotransfusion. Autotransfusion is not suitable for all patients because some trauma patients may have lost so much blood already that there is little volume left to salvage. A disadvantage of autotransfusion is that it cannot be used in the presence of cancer cells, infection, or gross contamination. Autotransfusion is generally contraindicated during cesarean section because of the presence of amniotic fluid. Autotransfusion is commonplace in most operating rooms currently, and is an effective option for replacement of blood lost during certain surgical procedures. Volume Expanders Volume expanders are used to increase the total volume of body fluid when hypovolemia occurs. One category is crystalloids, solutions that contain salts (electrolytes) and/or sugars. Another category of volume expanders is colloids, solutions that contain proteins or other substances with large molecules that increase osmolarity and do not dissolve in solution. Volume expanders can be used when donated blood or autotransfusion is not immediately available for emergency procedures. Albumin is available in concentrations of 5%, which is equal to plasma, or as a concentrated 25% in sodium chloride solution. Dextran expands plasma volume by drawing fluid from the interstitial space to the intravascular fluid space.
Betapace 40 mg online
Preinduction Phase the preinduction phase begins as the patient is admitted to the preoperative holding area and continues up to the point of administration of anesthetic agents blood pressure medication young age purchase generic betapace online. A history is obtained regarding airway issues and a physical examination is conducted to determine neck mobility and assess other factors that might indicate potential for a difficult airway. Appropriate medications are administered during this phase, as ordered by the anesthesia care provider (see Chapter 13). One goal of the preinduction phase is to have the patient arrive in the operating room calm, physiologically stable, and fully prepared for anesthesia. The preinduction phase continues as the patient is transported to the operating room and transferred to the operating room bed. The anesthesia care provider begins by attaching monitoring devices to the patient and obtaining baseline vital signs. The vital functions of all patients receiving a general anesthetic are continuously monitored (see Chapter 14). Hearing sensitivity is also heightened (hyperacusis) during induction of anesthesia. The effect of loud noises and sudden movement may be intensified during this time, inducing a stress reaction in the patient. The stress response may be characterized by unstable cardiovascular functions, which is potentially harmful to the patient. Thus the surgical technologist and all members of the surgical team must make every effort to minimize unnecessary operating room noise and movement of the patient during induction. The option of masked induction, with an inhalation anesthetic, may be chosen for children to avoid the emotional trauma of placing an intravenous catheter. Various induction agents are used to produce an unconscious state, amnesia, and analgesia. A variation of standard induction technique called neuroleptanesthesia (Insight 15. When the patient becomes unconscious, the anesthesia care provider ensures that an adequate airway is maintained. An unconscious patient requires additional support to ensure optimal respiratory function, and various methods of airway management are used to provide that support. When the patient becomes unconscious, a nasal or pharyngeal (oral) airway may be placed, as needed, to displace the tongue and facilitate air exchange through the mask. The patient may continue to breathe on his or her own (if no muscle relaxant is needed for the surgical procedure), or respirations may be controlled with the use of a ventilator or by manual ventilation (if muscle relaxants are administered). This strange-sounding term is used to indicate an anesthetic state that produces sedation and analgesia, while allowing the patient to breathe on his or her own and move on command. Also called a dissociative anesthetic state, its effects are similar to those of ketamine. Fentanyl, droperidol, and nitrous oxide are the agents used to produce neuroleptanesthesia. When indicated, this technique was used for induction of anesthesia in high-risk patients undergoing vascular procedures because of the minimal negative impact on cardiovascular and hemodynamic stability. A variation of this technique is called neuroleptic analgesia, in which pain relief is provided through the use of fentanyl and droperidol, without nitrous oxide. Thus the use of droperidol is significantly limited, and as a result the techniques of neuroleptanesthesia and neuroleptic analgesia are used rarely, if at all in current practice. In addition, many surgical procedures are of longer duration, require deep muscle relaxation, or are performed in a lateral or prone position, all of which require a more highly controlled airway. Deep muscle relaxation is achieved by the administration of neuromuscular blockers, which cause temporary relaxation of skeletal muscles including the muscles of respiration. External markings on the tube are in centimeters and are used to determine the length of tube insertion. An intubating laryngoscope (somewhat similar to an operating laryngoscope) is used to retract the tongue and lift the jaw to visualize the larynx and vocal cords. The end of the tube is placed midway between the vocal cords and the carina of the trachea (the carina is the place where the trachea bifurcates into right and left main stem bronchi), and the cuff is inflated. This development is a significant advance in technique, and it is very useful for difficult intubations. The video laryngoscope contains a microvideo camera in the laryngoscope blade that transmits images to a viewing screen. Fentanyl may be given 1 to 3 minutes before the induction agent to minimize reaction to laryngoscopy and intubation. A nonparalyzing dose of a nondepolarizing neuromuscular blocker (such as pancuronium), and a dose of succinylcholine (a depolarizing neuromuscular blocker) are administered. This technique is reserved for patients with specific conditions, such as morbid obesity, a history of difficult intubation, facial deformities, laryngeal cancer, unstable cervical spine fractures, or other conditions that may compromise the airway. Preparation for intubation before induction begins with administration of an antisialagogue (an agent to dry salivary secretions), such as glycopyrrolate (Robinul), approximately 30 minutes before intubation. Sedation is administered so that the patient can tolerate the intubation and yet continue to breathe and protect his or her own airway. Intubation may be accomplished by nasal or oral route, depending on the situation. If a nasal intubation is selected, topical vasoconstrictors (such as cocaine, oxymetazoline [Afrin], or phenylephrine) may be used intranasally to prevent bleeding (epistaxis). Additional anesthetic agents are administered during the maintenance phase, as needed, to maintain a depth of anesthesia appropriate to the surgical procedure. For example, abdominal and thoracic procedures require a much deeper level of anesthesia than superficial procedures. The patient is maintained in an unconscious state with a combination of intravenous and inhalation agents, some of which also produce amnesia and analgesia. Muscle relaxants are administered, as needed, to keep the patient immobile and facilitate retraction and visualization of the surgical site. The anesthesia care provider maintains the delicate balance of administering the appropriate agents, in the appropriate amounts, at the appropriate times, to achieve a level of anesthesia neither too deep nor too light for the surgical procedure, while maintaining a stable cardiovascular state in the patient. Indirect measures (clinical observations), such as sweating and lacrimation (the production of tears), are also considered reliable indicators of a pain response, but these signs may also indicate an insufficient depth of anesthesia. For example, an increased heart rate may be caused by hypovolemia rather than a painful stimulus. Each patient and each surgical situation present unique challenges in assessing and responding to patient needs under anesthesia. Awareness Under Anesthesia A disturbing phenomenon known as awareness under anesthesia has emerged as one of the most challenging problems in current anesthesia practice. It is important to note that dreams or fleeting perceptions on induction or emergence are not considered true awareness under anesthesia. For reasons that remain unclear, some patients do not demonstrate characteristic (measurable or observable) physiological responses to pain or have inadequate depth of anesthesia during surgery. The result is that the patient may have direct recall or explicit memory (Insight 15. When muscle relaxants are used, the patient is unable to move or speak and therefore is unable to communicate this awareness to the anesthesia care provider. Because approximately 21 million patients in the United States receive general anesthesia each year, an estimated 20,000 to 40,000 cases of awareness under anesthesia may be occurring yearly. The risk of awareness appears to be greater when it is necessary to use the lowest possible dose of anesthesia medications to avoid undesirable side effects. Patients who are hemodynamically unstable (such as trauma patients) are also at greater risk for awareness under anesthesia, as well as those undergoing cardiac and emergency obstetric procedures. Patients with a history of substance abuse and patients with chronic pain are also at greater risk. Although the extent of awareness is highly variable, approximately half of these patients report auditory recall, half report a sensation of being unable to breathe, and one third recall pain. A number of these patients reportedly go on to have posttraumatic stress disorder as a result. What we now understand about explicit and implicit memory and the number of patients who experience auditory recall (explicit memory) should motivate us to try to effect significant change in surgical team behaviors. We can no longer assume that the patient is unaffected by our conversations and comments during surgery. As surgical technologists we can support the anesthesia care providers in their efforts to bring this understanding to the attention of all surgical team members. Prevention measures include administration of midazolam for amnesia (provides anterograde amnesia only) and avoidance of the use of neuromuscular blocking agents whenever possible. Additional methods of patient monitoring have been developed to predict and prevent awareness under anesthesia.