Cleocin 150 mg online
Some important clues into the molecular basis of tumor lymphangiogenesis have been obtained acne 415 blue light therapy 38 led bulb buy cleocin 150mg cheap. The ability of dietary factors to act as mutagens in humans was demonstrated directly in 1995. The frequency of contamination of food with aflatoxins, a fungal metabolite, parallels the incidence of hepatocellular carcinoma in various areas of the world. Dietderived nitrates can be converted by bacterial action in a hypochlorhydric stomach to nitrites and subsequently to mutagenic nitrosamines. Other dietary factors may modulate the biological potency of dietary procarcinogens. Variations in the relative and absolute amounts of dietary fats may lead to alterations in the composition of the colonic microflora and their metabolic characteristics, resulting in modulation of the production of enzymes that convert dietary constituents into potentially mutagenic compounds. Changes in dietary fiber content can alter the transit time of luminal contents in the bowel, thereby changing the duration of exposure of the mucosa to potential mutagens. Bile salt content may be an additional luminal factor that can modulate the biological effect of procarcinogens. Deconjugated bile salts may promote carcinogenesis through mucosal injury and enhanced epithelial proliferation. These mechanisms could explain well-documented correlations between the intake of various dietary constituents and the incidence of colorectal cancer in certain populations (see Chapter 127). Environmental factors play an important role in tumorigenesis insofar as they affect the progression of the underlying genetic lesions. The incidence of colorectal cancer in Japanese immigrants to the United States who consume a Western diet is much higher than that of native Japanese who consume a traditional Japanese diet. The ability to monitor billions of reactions simultaneously, so-called massively parallel sequencing, along with the ability to computationally assemble short sequence reads into a continuous long read, have revolutionized sequencing technologies. Secondly, these technologies can be applied to determine the mutational landscape of a tumor to guide treatment decisions. Another method is to subject the sample to preliminary step of enrichment, where areas of interest are extracted from the sample, using hybridization methods and primer libraries, with the goal of decreasing the complexity of the sample and increasing the number of reads possible during the sequencing reaction. With greater number of reads available, so-called reading depth, the accuracy of sequencing increases and the cost is also reduced. The most common enrichment method is to focus on the areas of the genome known to harbor genes, collectively referred to as the exome, which corresponds to about 1% of the entire genome. Missense changes are those that result in a change in the amino acid encoded by the codon. Given the normal genetic variation present in the human population, understanding whether these changes are deleterious can be quite difficult to accomplish. When the effect of such variants is not known, these are referred as "variants of unknown significance. Molecular Diagnostics Genetic testing is a powerful tool to identify high-risk families and define the cancer risk for individual family members. Today, sequencing panels that assess most of the genes associated with familial cancer syndromes are commercially available. Application of genetic testing must take into consideration the sensitivity and specificity of the assay as well as issues of patient confidentiality and potential impact on medical insurability. Because these tests rely on target enrichment, it is important to be aware of their potential limitations. For these reasons, genetic counseling is an essential component of the genetic testing process. In addition to genetic germline testing, molecular phenotyping of tumors for the purpose of guiding therapeutic decisions is important. However, their benefit has been shown only in cancers lacking activating mutations in K-ras. Testing for K-ras mutations in colorectal cancers is now standard of care before administration of such targeted therapy. For example, capture of small numbers of circulating tumor cells prior to the discovery of metastasis may yield prognostic and therapeutic benefits. Cancer and Tumor Genomics As genetic information is obtained from sequencing analysis, understanding the potential impact of the genetic changes observed becomes an important challenge. Single nucleotide variants refer to changes in a single base pair of the genetic code compared to a reference sequence. Depletion of epithelial stemcell compartments in the small intestine of mice lacking Tcf-4. The intestinal stem cell signature identifies colorectal cancer stem cells and predicts disease relapse. Identification and characterization of the familial adenomatous polyposis coli gene. Mutations in the p53 tumor suppressor gene: clues to cancer etiology and molecular pathogenesis. Germline p53 mutations in a familial syndrome of breast cancer, sarcomas, and other neoplasms. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cancer metastasis and angiogenesis: an imbalance of positive and negative regulation. Regulation of vascular endothelial growth factor by the Wnt and K-ras pathways in colonic neoplasia. Searches for ultimate chemical carcinogens and their reactions with cellular macromolecules. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. Replication errors in benign and malignant tumors from hereditary nonpolyposis colorectal cancer patients. Myeloid-derived suppressor cells: Roles in the tumor microenvironment and tumor radiotherapy. The demands on the mucosal immune system are quite distinct from their systemic counterparts. At mucosal sites, the "outside world" is typically separated from the inner world by a single layer of epithelium. The mucosal immune system exists at a number of sites, including the intestinal tract, respiratory tract (especially the upper respiratory tract), urogenital tract, mammary glands, eyes, and ears. Each of these sites encounters a distinctive array of environmental stimuli and has evolved its own set of cell populations. Nevertheless, these different compartments can interact and share some cell populations and together form a common mucosal immune system. These organisms and their products, along with ingested food, represent an enormous antigenic load that must be tolerated to maintain mucosal homeostasis. Collectively, these cells comprise the largest number of cells in the immune system. The specific characteristics and peculiarities of the mucosal immune cells reflect the unique milieu in which the cells function. To maintain mucosal homeostasis in the intestinal mucosa, one of the most important tasks of the immune system is to differentiate potentially harmful antigens such as pathogenic bacteria and toxins from products that may benefit the body such as molecules derived from food or commensal bacteria. To achieve homeostasis, unusual cell types, immunoglobulins (Igs), and secreted mediators function in a coordinated fashion. In contrast to the systemic immune system, whose focus is to act quickly within seconds of encountering a foreign antigen, the mucosal immune system is poised to respond but is predominantly tolerant,3,4 rejecting harmful antigens but allowing beneficial/harmless ones to persist without evoking harmful immune responses such as allergic reactions or inflammation. Humans have co-evolved with their microbiota and have developed multiple mechanisms of response, including intestinal epithelial cells and innate, adaptive, and regulatory immune components. Despite the persistence of the antigenic drive of the intestinal microbiota, intestinal lymphocyte effector cells fail to develop into aggressive inflammation-producing cells. Bacteria or their products play a role in this persistent state of suspended activation10 contributing to the control of inflammation in the intestinal mucosa. IgG is the most abundant isotype in the systemic immune system, but IgA is the most abundant antibody in mucosal secretions. Two IgA molecules (homodimers) are bound together by J chain (produced by plasma cells).
Purchase 150 mg cleocin overnight delivery
At a fundamental level anti-acne purchase cleocin no prescription, neoplasia arises when cell proliferation escapes the homeostatic mechanisms that maintain this process in balance with senescence and programmed cell death. Cell proliferation occurs as cells divide, a process that occurs through an orderly set of steps referred to as the cell cycle. In preparation for cell division, there is a period of biosynthetic activity called the G1 phase that is typically associated with an increase of cell size. This phase is followed by precise duplication of the genome, designated the S phase. After an intervening gap period designated as the G2 phase, mitosis occurs during the M phase. Cells may exit this cycle of active proliferation before reaching the R point and enter a quiescent phase known as G0. These proteins are expressed in specific parts of the cell cycle and regulate the G1/S and G2/M checkpoints. Thus, loss of Rb expression also accomplishes more rapid progression to S phase and is another genetic lesion seen in many tumors. During these gap phases, the cell is synthesizing proteins and metabolites, increasing its mass, and preparing for the S phase and M phase. Apoptosis Apoptosis is a form of programmed cell death that is genetically programmed and executed by specific proteases known as caspases. Apoptosis is an important mechanism that counterbalances cell proliferation; thus, escape from normal apoptotic mechanisms plays a critical role in oncogenesis. A complex interplay of proapoptotic and antiapoptotic molecules results in downstream activation of caspases that mediate cell death. The mitochondrial step is regulated by the interplay between proapoptotic (Bax, Bak) and antiapoptotic (Bcl-2, Bcl-xL) molecules. Activation of caspase-8 (downstream of death receptor) or of caspase-9 (as a result of apoptosome formation), leads to activation of executioner caspases (3 and 7) which are responsible for targeting downstream targets that are responsible for cell death. Apoptosis routinely occurs during normal development to facilitate tissue patterning. Similarly, a number of stress situations, including tissue inflammation, can trigger apoptosis. Apoptosis may also be stimulated by specific cell surface receptors belonging to the tumor necrosis factor receptor superfamily, including tumor necrosis factor R1 and Fas, which are referred to as death receptors. At the intracellular level, the last common event in all forms of apoptosis is the activation of so-called executioner caspases, caspase 3 and 7, which mediate the cleavage of a large number of downstream targets that eventually precipitate cell death. Proapoptotic signals frequently converge at the level of the mitochondria, where they destabilize the mitochondrial membrane and collapse the electrical gradient required for aerobic respiration Besides the effects that result in cellular energetics, this process leads to the release into the cytosol of proteins normally present in the intermembrane space of the mitochondria, including cytochrome c, a component of the respiratory chain. In the cytosol, cytochrome c helps in the assembly of a multiprotein complex known as the apoptosome, which contains Apaf1 and facilitates the activation of caspase 9, which can directly activate caspases 3 and 7. On the other hand, death receptors activate executioner caspases through receptor initiated intracellular signaling events that result in the upstream activation of caspase 8. The mitochondrial membrane permeabilization events that lead to apoptosome formation are controlled by proteins of the Bcl-2 family. On the one hand, Bax and Bak help form the pore, whereas Bcl-2, Bcl-xL, and Mcl-1 inhibit pore formation. The stoichiometric ratio between proapoptotic and antiapoptotic members of the Bcl-2 family can determine the balance between cell survival and cell death. Senescence Senescence is the process by which cells permanently lose their ability to divide. Associated with the exit from the cell cycle, senescence is associated with a secretory phenotype that includes a variety of proinflammatory factors. As a physiologic event, senescence limits dysregulated or excessive proliferation. However, when dysregulated, senescence can also contribute to aging and depletion of stem cells. Replicative senescence is triggered shortening of telomeres, repetitive sequences at the end of chromosomes that protect genomic integrity. This phenomenon can be routinely seen in vitro when primary cells undergo repeated rounds of replication, eventually acquiring critically short telomeres. Although progression through the cell cycle is controlled by the regulatory mechanisms just described, overall proliferation is also modulated by external stimuli. Growth factors that bind to specific transmembrane receptors on the cell surface are especially important. Also acting through transmembrane cell surface receptors, extracellular matrix and cell-cell adhesion molecules. Alterations in cell-matrix or cellcell interactions are particularly important in contributing to the invasive phenotype of malignant cells. The receptors for many peptide growth factors contain intrinsic tyrosine kinase activity within their intracellular tail. After ligand binding, tyrosine kinase activity is stimulated, leading to phosphorylation of tyrosine residues in target proteins within the cell. Most receptors also autophosphorylate tyrosine residues present in the receptors themselves to magnify signaling, and, in some cases, this also causes attenuation of their own activity to effect an intramolecular feedback regulatory mechanism. Other receptors on the cell surface possess kinase activity directed toward serine or threonine residues rather than tyrosine. These receptors also phosphorylate a variety of cellular proteins, leading to a cascade of biological responses. Multiple sites of serine and threonine phosphorylation are present on many growth factor receptors, including the tyrosine kinase receptors, suggesting the existence of significant interactions among various receptors present on a single cell. G proteins undergo a conformational change that is dependent on the presence of guanosine phosphates. Binding of growth factors and cytokines to cell surface receptors typically produces alterations in a variety of cellular functions that influence growth. However, the ligandreceptor interaction must ultimately modify one or more of the homeostatic mechanisms discussed to affect cellular proliferation. The Wnt pathway is one important example of a signaling pathway that regulates a diverse number of homeostatic mechanisms to control proliferation of intestinal epithelial cells. The destruction complex phosphorylates -catenin and targets it for degradation via the ubiquitin-proteosome pathway. In the presence of an active Wnt signal (right top), -catenin degradation is prevented and the protein is stabilized, leading to excess cytoplasmic -catenin which is translocated to the nucleus. Nuclear -catenin interacts with the Tcf-4 transcription factor to regulate the expression of many key target genes. When secreted Wnt ligands bind to cell surface receptors of the Frizzled family, the constitutive degradation of -catenin is inhibited (disheveled) which results in the nuclear accumulation of this factor, and the subsequent transcriptional activation of genes that promote cell proliferation. Inhibition of the Wnt signal in mice can be achieved by deletion of Tcf-4 or overexpression of the Wnt inhibitor Dickkopf1, which results in dramatic hypoproliferation of the intestinal epithelium. Although mutations in histones themselves are rare in cancer, mutations in the enzymes that modify histones are emerging as an important group of tumor-associated mutations. It is important to note that involvement by these pathways is not mutually exclusive. As this population grows, and particularly with the acquisition of genetic/epigenetic instability, a second round of clonal expansion occurs as a cell within this population sustains still another genetic alteration that further enhances its growth properties. This iterative process of selection, with accumulating genetic alterations, results in malignancy. Because of the nature of the clonal expansion process, once frank malignancy has developed, it is often the case that multiple clones are present in the same tumor, with a different catalog of mutations harbored among various cancer cells. Referred to as tumor heterogeneity, this ongoing process may give certain cells selection advantages. Moreover, it is hypothesized that eradication of these cells is a key therapeutic goal because failure to do so may result in relapse of disease. The basic evidence for this model is the finding that only cells with specific surface markers can repopulate the tumor in xenotransplantation experiments. This multistep nature of tumorigenesis is most directly illustrated by the changes that accrue in the development of colonic neoplasia (see Chapter 127).
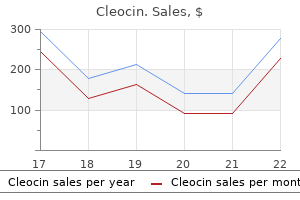
Order cleocin 150mg line
Cholestasis with Minimal Histologic Abnormalities Jaundice may accompany cholestasis in the absence of hepatic infiltration or injury to hepatocytes or cholangiocytes skin care books order genuine cleocin on-line. Several mechanisms may be responsible, including mutations in the genes that encode transport proteins involved in bile formation and conditions that interfere with the function or expression of such proteins. Patients with benign recurrent cholestasis typically present before the second decade of life with recurrent episodes of malaise and pruritus in association with jaundice; fever and abdominal pain are uncommon. When performed during an icteric episode, liver biopsy findings are generally confined to centrilobular cholestasis; portal-based inflammatory cell infiltrates are uncommon. Cholestatic episodes may last up to several months and are separated by periods of clinical remission. Although quality of life may be adversely affected, the disease does not lead to progressive liver damage, and (unlike progressive familial intrahepatic cholestasis) liver failure does not occur. A number of drugs produce histologically bland intrahepatic cholestasis (see Chapter 88). Jaundice related to the use of oral contraceptives usually develops within 2 months of initiation of therapy and is generally accompanied by pruritus; these symptoms resolve promptly with discontinuation of the drug. Anabolic steroids can produce a syndrome that is clinically indistinguishable from estrogen-induced cholestasis (see the LiverTox website). The clinical features of cholestasis associated with total parenteral nutrition (possibly related to altered enterohepatic circulation and diminished neuroendocrine stimulation of bile flow) may also resemble those related to estrogen and anabolic steroids, but progressive hepatic fibrosis has also been described. Jaundice due to intrahepatic cholestasis has been reported as a paraneoplastic phenomenon. Atypical Presentations of Cholestasis Viral hepatitis rarely may cause profound cholestasis, with pruritus and jaundice. A high level of suspicion and appropriate laboratory testing will help establish the diagnosis. Alcoholic hepatitis manifesting as fever, jaundice, abdominal pain, and leukocytosis may also be difficult to distinguish from bile duct obstruction. Jaundice in Pregnancy Several cholestatic disorders are uniquely encountered in pregnancy (see Chapter 40). Jaundice uncommonly may accompany hyperemesis gravidarum, a generally self-limited disorder of the first trimester, but liver failure is not a feature of this illness. A far more serious syndrome is acute fatty liver of pregnancy, which typically occurs in the third trimester and is associated with hepatocellular injury. Jaundice, when present, is usually accompanied by nausea, abdominal pain, and evidence of liver failure. Preeclampsia, a microvascular disorder of the third trimester, is heralded by hypertension and proteinuria and affects the liver in about 10% of cases. Jaundice in the Critically Ill Patient Establishing the cause of jaundice in the critically ill patient can present a challenge to intensivists and their consultants. The persistence of icterus can be a source of dismay and frustration to concerned relatives and other advocates for the patient, who may view jaundice as the cause rather than a manifestation of critical illness. Urgent requests for biliary drainage (in the absence of evidence of bile duct obstruction [see later]) can exacerbate the tension. Notably, even if other clinical parameters improve, there may be a lag in the resolution of jaundice. Therefore, the management of jaundice in intensive care settings requires not only a careful search for reversible causes but also a great deal of patience. A logical approach involves 4 basic steps: (1) a carefully taken patient history, thorough physical examination, and screening laboratory studies; (2) formulation of a working differential diagnosis; (3) selection of specialized tests to narrow the diagnostic possibilities; and (4) development of a strategy for treatment or further testing if unexpected diagnostic possibilities arise. A family history of jaundice or liver disease raises the possibility of hereditary hyperbilirubinemia or genetic liver disease. All clues must be interpreted with caution; for example, fever and abdominal pain accompany diseases other than biliary obstruction, and viral hepatitis may occur coincidentally in patients with a history of prior biliary surgery. Moreover, anorexia and malaise are not specific for viral hepatitis, and gallstones can develop in patients with chronic liver disease. Bile Duct Obstruction Obstructive disorders of the biliary tract include occlusion of the bile duct lumen, intrinsic disorders of the bile ducts, and extrinsic biliary compression. Choledocholithiasis the most common cause of biliary obstruction is luminal occlusion by a stone (choledocholithiasis). Three types of stones have been implicated in this process, with cholesterol gallstones responsible for the majority of cases (see Chapter 65). Cholesterol stones typically originate in the gallbladder and can migrate into the bile duct. In patients with unconjugated hyperbilirubinemia, calcium bilirubinate stones (so-called black pigment gallstones) form in the gallbladder and may also form in situ at any level of the biliary tract. Brown pigment gallstones, a distinct type of bilirubinate stone, can lead to and result from repeated bouts of cholangitis (recurrent pyogenic cholangitis), particularly in patients from certain regions of eastern Asia and in patients with prior biliary tract surgery or endoscopic intervention (see Chapter 68). Bile Duct Diseases Intrinsic narrowing of the bile ducts occurs in inflammatory, infectious, or neoplastic biliary disease. Congenital disorders of the bile ducts, including cysts and biliary atresia, are discussed in Chapter 62. Biliary strictures may also follow hepatic arterial infusion or embolization of certain chemotherapeutic compounds41 or result from surgical injury to the bile duct or hepatic artery (see Chapter 68). Initial Laboratory Studies Essential laboratory tests in the patient with jaundice include serum total bilirubin, alkaline phosphatase, aminotransferases, complete blood count, and prothrombin time (see Chapter 73). Serum alkaline phosphatase activity derives from related isoenzymes expressed on the membranes of multiple cell types; the hepatobiliary ("liver") alkaline phosphatase isoenzyme is a membrane linked protein localized predominantly on the apical poles of hepatocytes and cholangiocytes. In hepatocytes and cholangiocytes, enzymatic cleavage under physiologic conditions releases alkaline phosphatase from the apical membranes into bile; small amounts are released from the basolateral membrane into plasma as well. Biliary obstruction and intrahepatic cholestasis increase the basolateral release of alkaline phosphatase, and serum alkaline phosphatase activity increases under these conditions. Consequently, in a jaundiced patient, a predominant increase in serum alkaline phosphatase (relative to aminotransferase) activity suggests the presence of biliary tract obstruction or intrahepatic cholestasis. An increase in serum alkaline phosphatase activity (especially if aminotransferase activity is normal), however, may Extrinsic Compression Extrinsic compression of the biliary tract may result from neoplastic involvement or inflammation of surrounding viscera. Painless jaundice is a classic feature of carcinoma of the head of the pancreas (see Chapter 60). Pancreatitis may lead to biliary compression from edema or pseudocyst formation (see Chapters 58 and 59). Rarely, gallstones in the cystic duct or infundibulum of the gallbladder compress the common hepatic duct (Mirizzi syndrome) and produce jaundice. If there is diagnostic uncertainty, elevated serum activities of other proteins A predominant elevation of serum aminotransferase levels (relative to alkaline phosphatase) suggests that jaundice is due to hepatocellular injury. For example, transient biliary obstruction from choledocholithiasis may cause a brief but dramatic elevation (> 10 to 20 times normal) of serum aminotransferase activity. Leukocytosis may be a clue to the presence of biliary tract obstruction or another inflammatory disorder associated with cholestasis. The presence of anemia raises the possibility that a hemolytic disorder is responsible for jaundice, especially if isolated hyperbilirubinemia (without other abnormalities in biochemical liver tests) is detected. Thrombocytopenia is a characteristic finding in cirrhosis and appears to result from reduced synthesis of thrombopoietin, the regulator of platelet production, or from increased splenic sequestration associated with portal hypertension. Exogenously administered vitamin K will generally normalize a prolonged prothrombin time due to intrahepatic cholestasis or long-standing biliary obstruction but not due to hepatocellular injury. After endoscopic identification of the ampulla of Vater, insertion of a catheter permits contrast injection into the biliary tract; sedation and analgesia are necessary. Similarly, if there is concern about a neoplasm, biopsy and brushings for cytology can be performed. At one extreme is the asymptomatic patient with no abnormalities (other than jaundice) on physical examination. Under these conditions, if the serum alkaline phosphatase and aminotransferase activities, platelet count, and prothrombin time are normal, liver disease or biliary obstruction is highly unlikely. In this situation, further testing for specific disorders, such as an isolated defect in bilirubin metabolism or hemolysis, is warranted Alternatively, if the history, physical examination, and laboratory study results raise the possibility of biliary obstruction, hepatobiliary imaging is appropriate. Selection of the appropriate imaging study depends on the likelihood of bile duct obstruction and the diagnostic accuracy, cost, complication rate, and availability of each test (see later), especially if there is clinical urgency and therapeutic intervention at the time of the study is anticipated. The following section provides an overview with the recognition that some of the original studies concerning the performance of imaging studies in the evaluation of jaundice were performed in the 20th century. Disadvantages include dependence on the skill of the operator for the procedure and potential technical difficulty in obese patients or patients with excessive bowel gas that overlies some organs like the pancreas. When bile is aspirated, a catheter is introduced through the needle, and radiopaque contrast medium is injected.
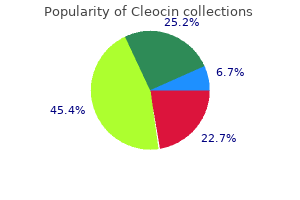
Purchase cleocin australia
They cannot be used for long periods due to their side effects skin care zarraz cleocin 150 mg with mastercard, including bone loss and hot flushes. Regarding laparoscopic and/or abdominal myomectomy, it was suggested that using a preoperative agonist might obscure the cleavage plane between the pseudocapsule and healthy myometrium. Concerns from extensive dissection of the fibroid, distortion of the pseudocapsule, and increased operative time were reported [57]. However, in a systematic review and meta-analysis, the use of an agonist prior to laparotomic and laparoscopic myomectomy had decreased intraoperative blood loss and the frequency of blood transfusions. Enucleation time for myoma and difficulty of surgery did not significantly increase with use of agonist pretreatment [58]. Fibroids and Assisted Reproduction Technology 17 Selective Progesterone Receptor Modulators the crucial role of progesterone in the development and growth of myomas has been established. These compounds exert either an agonistic or antagonistic effect on progesterone receptors. Some studies reported a significant reduction of myoma size and improvement in symptoms upon using mifepristone [64,65]. Mifepristone reduced heavy menstrual bleeding and improved quality of life, but it did not significantly reduce fibroid volume [66]. We need to establish a systematic approach to these cases and try to accomplish less invasive surgery even with the use of endoscopy. Type 1 and 2 Myomas the strategy for these myomas depends on the size, presence of anemia, and surgeon skill. Hysteroscopic myomectomy is a relatively straightforward procedure for experienced surgeons in the case of type 1 myoma, less than 3 cm, in the absence of anemia. This may induce fibroid shrinkage and enable an easier approach in the presence of a better general condition [2,70]. It was reported that type 2 myoma might significantly regress in some cases, so that they no longer disturb the endometrial cavity, and their size becomes lower than the reported detrimental cutoff size; 18 Fibroids and Reproduction therefore, surgery can be avoided [71]. Importantly, surgeon skill and preference are major determinants in dealing with type 2 myomas. Types 3 through 5 Myomas (Single or Multiple) Laparoscopic and/or abdominal myomectomy are the standard procedure. However, the decision depends on the size, number, and surgeon skill, as mentioned earlier in this chapter. In a recent Cochrane review, it was emphasized that replication of these studies is recommended before making firm conclusions. Future studies should target cost-effectiveness and identify the group of fibroid patients who would benefit from this approach [59]. In women who are desirous of pregnancy, surgery is the recommended modality, using endoscopy whenever possible. There are, however, insufficient data in the literature to ensure a good fertility potential. Medical treatment, though it has its place, is mainly for preoperative preparation and for only a limited period of time. Updates on the cytogenetics and molecular genetics of bone and soft tissue tumors: Leiomyoma. A genome-wide association study identifies three loci associated with susceptibility to uterine fibroids. The Practice Committee of the American Society for Reproductive Medicine in collaboration with the Society of Reproductive Surgeons. Gene expression studies provide clues to the pathogenesis of uterine leiomyoma: New evidence and a systematic review. Effect of fibroids on fertility in patients undergoing assisted reproduction, a structured literature review. Effect of fibroids not distorting the endometrial cavity on the outcome of in vitro fertilization treatment: A retrospective cohort study. Effect of type 3 intramural fibroids on endometrial fertilization- Intracytoplasmic sperm injection outcomes as: A retrospective cohort study. Uterine leiomyomas and their effect on in vitro fertilization outcome: A retrospective study. Is myomectomy prior to assisted reproductive technology cost effective in women with intramural fibroids Effect of intramural, subserosal, and submucosal uterine fibroids on the outcome of assisted reproductive technology treatment. Hysteroscopic endometrial ablation with the Nd:Yag laser using a nontouch technique. In: Tinelli A and Malvasi A (eds) Uterine Myoma, Myomectomy and Minimally Invasive Treatments. Hysteroscopic myomectomy respecting the pseudocapsule: the cold loop hysteroscopic myomectomy. Should the myometrial free margin still be considered a limiting factor for hysteroscopic resection of submucous fibroids The management of uterine fibroids in women with otherwise unexplained infertility. Laparoscopy versus minilaparotomy in women with symptomatic uterine myomas: Short-term and fertility results. The impact of uterine fibroid embolization on resumption of menses and ovarian function. Midterm clinical and first reproductive results of a randomized controlled trial comparing uterine fibroid embolization and myomectomy. Potential of minimally invasive procedures in the treatment of uterine fibroids: A focus on magnetic resonance-guided focused ultrasound therapy. Screening magnetic resonance imaging-based prediction model for assessing immediate therapeutic response to magnetic resonance imaging-guided high-intensity focused ultrasound ablation of uterine fibroids. Leiomyoma pseudocapsule after pre-surgical treatment with gonadotropin-releasing hormone agonists: Relationship between clinical features and immunohistochemical changes. Selective progesterone receptor modulators in reproductive medicine: Pharmacology, clinical efficacy and safety. Selective progesterone receptor modulators: A class with multiple actions and applications in reproductive endocrinology, and gynecology. Low-dose mifepristone in treatment of uterine leiomyoma: A randomised double-blind placebo-controlled clinical trial. Current management of myomas: the place of medical therapy with the advent of selective progesterone receptor modulators. Given their high prevalence, fibroids can have a significant effect on fertility outcomes, including implantation, ongoing pregnancy, live birth rate, and spontaneous abortion rate [2]. The anatomic location of a fibroid is thought to be a defining characteristic that influences the reproductive potential. Several hypotheses have been proposed to explain the relationship between fibroids and infertility. One mechanism by which fibroids may reduce fertility is through dysregulation of endometrial receptivity. Endometrial receptivity refers to a defined period in the menstrual cycle where the endometrium allows for embryo attachment and invasion, triggering a series of events that culminate in a successful pregnancy. In this chapter, we review the mechanisms by which fibroids can impact endometrial receptivity. In order for implantation to occur and a pregnancy to be established, embryo viability and endometrial receptivity need to be in synchrony, which normally occurs due to complex communication between both the embryo and the endometrium. At this stage, the embryo is referred to as a blastocyst and consists of an inner cell mass and an outer trophectoderm layer. The inner cell mass gives rise to the fetus, amnion, and vascular components of the placenta, while the trophectoderm becomes the placenta and the chorion. These signals facilitate apposition and adherence of the embryo to optimal implantation sites in the endometrium. Embryo implantation during this time frame is associated with an 85% ongoing pregnancy rate, whereas implantation on day 11 is associated with an 11% ongoing pregnancy rate [10]. The increase in vascularity and development of stromal spiral arterioles provide a substrate for embryo invasion and implantation. Optimal sites for implantation need to have sufficient depth, vascularity, and nutritional richness to support early placentation.
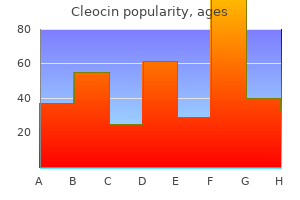
Order 150 mg cleocin amex
A swab moistened with 88% phenol is used to treat small areas until cutaneous frosting occurs acne 10 gel generic cleocin 150 mg on-line. The patient feels a burning sensation for approximately 60 seconds, which gradually decreases in intensity and can last from minutes to hours. After two sessions, 45 days apart, total elimination of residual pigmented areas is noticed. No signs of repigmentation have been seen until after one and a half years of therapy [23]. Acyclovir prophylaxis is to be given in those who have a history of herpes simplex. Phenol exerts a marked corrosive action on any tissue it comes in contact with, whether upon ingestion, inhalation, or direct contact with the skin. Its cellular uptake is both rapid and passive because of its lipophilic character, and signs of systemic toxicity develop soon after exposure. Cardiovascular shock, cardiac arrhythmias, and bradycardia as well as metabolic acidosis have been reported within 6 hours of skin-peeling procedures with phenol. After a mean followup time of 13 months, 48% showed greater than 75% depigmentation. Patients with active disease (63%) showed significantly greater depigmentation than those with stable disease (P < 0. Thirteen patients achieved excellent response, with 90% resolution of pigmentation. Follicular repigmentation may develop due to migration of perifollicular melanocytes to the epidermis, indicating that these are not destroyed by the laser therapy. Chances for relapse are higher with stable patients than those with active vitiligo [21]. Lasers are known to induce selective photothermolysis of pigmented lesions because their wavelengths are between 600 nm and 800 nm, which are absorbed easily by melanin. Because the duration of the energy pulse is shorter than the thermal relaxation time of melanosomes, no energy. The main advantages include that they are an effective, fast, and safe method with short treatment duration. They are more effective in vitiligo patients with a positive Koebner phenomenon [24]. Lasers also overcome the disadvantages of topical therapies, such as redness, burning, itching, etc. Topical therapy takes a long time, approximately 10 months, to depigment, with the possibility of only partial depigmentation and a relatively high failure rate and risk of repigmentation. With lasers, large areas can be depigmented in one sitting, as opposed to depigmentation performed using a bleaching agent. An additional advantage is that the risk of scar formation is lower due to controlled damage [21]. Bigger confluent areas of pigment on the extremities can first be treated with topical therapy. Combination therapy was seen to give better results than with any of the methods alone. If depigmentation is evident, a maximum size of 80 cm [2] can be treated in each session at an interval of 2-4 weeks under topical anesthesia. Within 3 months after each laser session, most treated areas would begin to repigment. Within 22 months, the patient was nearly clear of all pigment within the treated sites. Radmanesh [29] has demonstrated the use of cryosurgery for cost-effective rapid depigmentation that is permanent and has an excellent cosmetic result but can be done only over limited areas in each session. Inflammation develops within 24 hours of treatment, further contributing to destruction of lesions through immunologically mediated mechanisms. Mild freezing leads to a dermo-epidermal separation, which is useful in treating epidermal lesions. A 2-cm flattopped and round cryoprobe is held approximately 40 mm from the skin surface. The whole patch can be frozen with a single freeze-thaw cycle from the periphery and then by forming successive rows inward. Procedure should be terminated when a narrow (<1 mm) frost rim forms around the periphery of the cryoprobe. The rim can develop within 10-20 seconds by a cryogun connected to a container with barometric pressure above 80 kg/cm [2]. For lesions around the orbits or uneven areas of the nose, cryoprobes with smaller diameters may be required. After a week, a depigmented, unscarred, slightly atrophic, and erythematous smooth area appears. The depigmentation is permanent, although multiple sessions may be required for partially depigmented lesions, with 4- to 6-week intervals [29]. Depigmentation developed by cryotherapy is permanent and without scarring if performed by an experienced dermatologist. Many patients prefer a single short-term procedure to applying an expensive compound for 10 months or more with unpredictable effects and a considerable failure rate. A recent retrospective study that compared depigmentation in 22 patients with generalized vitiligo who had previously been treated with cryotherapy or alexandrite 755-nm laser therapy found no significant difference in depigmentation activity after one treatment [30]. Also, cryotherapy is suitable for small lesions, and a single sitting cannot be utilized for depigmenting extensive areas, unlike lasers. Imiquimod (5%) application may be followed by erythema, which gradually turns to depigmented patches over a period of 3 months. Also, depigmentation did not extend to areas that had not been treated with imiquimod [36]. The most common side effects of imiquimod are burning, itching, pain, erythema, erosions, and scabbing/crusting at the target site, which occur more frequently with twice-daily application [4]. Electron microscopy and incubation with dopa in the affected skin revealed an absence of melanosomes and melanocytes. The depigmenting effects of imatinib and imiquimod have only been reported in few studies, and randomized control trials are lacking. Hence, further studies are required on these agents and other similar molecules before they can be used as mainstream depigmenting agents. These agents have the potential to cause depigmentation but have not been used in vitiligo treatment (Table 35. The skin became darker during the discontinuation period and began lightening again once imatinib mesylate treatment was resumed. Imatinib mesylate, being a tyrosine kinase inhibitor, may interfere with the production of melanin. It is difficult to define the onset exactly, because the change is gradual within 12 weeks. Imiquimod is a novel imidazoquinolinone immune response modifier frequently used for topical treatment of anogenital warts and basal cell carcinomas [32]. These compounds were injected into animal skin as 10% and 20% solutions dissolved in 95% ethanol. Vaccines using melanoma-associated antigen were reported by many authors to produce depigmentation by eliciting an autoimmune response directed against malignant but also normal melanocytes. Ethanolic extracts of Myrica rubra dried leaves have shown good depigmenting effects in vitro and pseudo superoxide dismutase activity. In vivo studies have been recommended to evaluate their potential use as depigmenting agents [39]. Monobenzylether of hydroquinone: A retrospective study of treatment of 18 vitiligo patients and a review of the literature. Rapid repigmentation after depigmentation therapy: Vitiligo treated with monobenzyl ether of hydroquinone. Contact hypersensitivity to monobenzyl ether of hydroquinone used to treat vitiligo.
Carnosine. Cleocin.
- What is Carnosine?
- Preventing or treating complications of diabetes such as nerve damage, eye disorders, and kidney damage.
- Are there safety concerns?
- Dosing considerations for Carnosine.
- How does Carnosine work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96994
Buy discount cleocin 150 mg on-line
Life-threatening complications of nasogastric administration of polyethylene glycol-electrolyte solutions (Golytely) for bowel cleansing acne quistico generic cleocin 150mg without a prescription. Small doses of the unabsorbable substance polyethylene glycol 3350 accelerate oro-caecal transit, but slow gastric emptying in healthy subjects. Effects of bisacodyl on ascending colon emptying and overall colonic transit in healthy volunteers. Electron microscopical studies on rat intestine after long-term treatment with sennosides. The effect of an anthraquinone laxative on colonic nerve tissue: a controlled trial in constipated women. Is senna laxative use associated to cathartic colon, genotoxicity, or carcinogenicity A new technique for measuring the consistency of faeces: a report on its application to the assessment of Senokotot therapy in the elderly. Light and electron-microscopic changes in the colon of the Guinea pig after treatment with anthranoid and non-anthranoid laxatives. Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of sodium picosulfate in patients with chronic constipation. Comparison of efficacy of pharmacological treatments for chronic idiopathic constipation: a systematic review and network meta-analysis. Understanding the physics of functional fibers in the gastrointestinal tract: an evidence-based approach to resolving enduring misconceptions about insoluble and soluble fiber. Efficacy of ground flaxseed on constipation in patients with irritable bowel syndrome. Effects of linseeds on the symptoms of irritable bowel syndrome: a pilot randomised controlled trial. Magnesium hydroxide: new insights into the mechanism of its laxative effect and the potential involvement of prostaglandin E2. Paralytic ileus as a complication of iatrogenic hypermagnesaemia without renal dysfunction. Severe hypermagnesemia as a result of excessive cathartic ingestion in a child without renal failure. A 64-year-old man with abdominal pain, nausea, and an elevated level of serum creatinine. Treatment of chronic constipation with lactulose syrup: results of a double-blind study. Sorbitol intolerance: an unappreciated cause of functional gastrointestinal complaints. Cost-effective treatment of constipation in the elderly: a randomized double-blind comparison of sorbitol and lactulose. A randomized, multicenter, placebo-controlled trial of polyethylene glycol laxative for chronic treatment of chronic constipation. Comparison of efficacy and safety of two doses of two different polyethylene glycol-based laxatives in the treatment of constipation. Phenolphthalein exposure causes multiple carcinogenic effects in experimental model systems. Effect of dioctyl sodium sulfosuccinate on structure and function of rodent and human intestine. Effect of oral dioctyl sodium sulfosuccinate on intake-output studies of human small and large intestine. Severe hyperphosphatemia and hypocalcemia following the rectal administration of a phosphate-containing Fleet pediatric enema. A fatal small dose of phosphate enema in a young child with no renal or gastrointestinal abnormality. Effect of a selective chloride channel activator, lubiprostone, on gastrointestinal transit, gastric sensory, and motor functions in healthy volunteers. Guanylate cyclase Cmediated antinociceptive effects of linaclotide in rodent models of visceral pain. Linaclotide in chronic idiopathic constipation patients with moderate to severe abdominal bloating: a randomized, controlled trial. Randomized clinical trial: efficacy and safety of plecanatide in the treatment of chronic idiopathic constipation. A randomized phase iii clinical trial of plecanatide, a uroguanylin analog, in patients with chronic idiopathic constipation. Effect of tegaserod in chronic constipation: a randomized, double-blind, controlled trial. Prucalopride accelerates gastrointestinal and colonic transit in patients with constipation without a rectal evacuation disorder. Clinical trial: the efficacy, impact on quality of life, and safety and tolerability of prucalopride in severe chronic constipation-a 12-week, randomized, double-blind, placebo-controlled study. Prucalopride (Resolor) in the treatment of severe chronic constipation in patients dissatisfied with laxatives. Efficacy of prucalopride in the treatment of chronic idiopathic constipation: systematic review and meta-analysis. Safety assessment of prucalopride in elderly patients with constipation: a double-blind, placebo-controlled study. Treatment of chronic constipation with colchicine: randomized, doubleblind, placebo-controlled, crossover trial. Misoprostol in the treatment of chronic refractory constipation: results of a long-term open label trial. Efficacy and safety of subcutaneous neostigmine for ileus, acute colonic pseudo-obstruction, or refractory constipation. A randomised controlled study of the effect of cholinesterase inhibition on colon function in patients with diabetes mellitus and constipation. Pyridostigmine for the treatment of gastrointestinal symptoms in systemic sclerosis. Effect of different doses of chenodeoxycholic acid on bile-lipid composition and on frequency of side-effects in patients with gallstones. Chenodeoxycholate in females with irritable bowel syndrome-constipation: a pharmacodynamic and pharmacogenetic analysis. Relamorelin relieves constipation and accelerates colonic transit in a phase 2, placebo-controlled, randomized trial. Controlled randomised trial of visual biofeedback versus muscle training without a visual display for intractable constipation. Effect of the ingestion of a symbiotic yogurt on the bowel habits of women with functional constipation. Efficacy of traditional Chinese medicine for the management of constipation: a systematic review. A systematic review of sacral nerve stimulation mechanisms in the treatment of fecal incontinence and constipation. Physiological tests to predict long-term outcome of total abdominal colectomy for intractable constipation. Proctocolectomy with restorative ileoanal reservoir for severe idiopathic constipation. Laparoscopic-assisted compared with open total colectomy in treating slow transit constipation. Malone antegrade continence enemas for autonomic dysreflexia secondary to neurogenic bowel. Evaluation of the stapled transanal rectal resection technique with two staplers in the treatment of obstructive defecation syndrome. Stapled transanal rectal resection for outlet obstruction: a prospective, multicenter trial. Lateral division of the puborectalis muscle in the management of severe constipation. Predictors of outcome of anorectal biofeedback therapy in patients with constipation. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Prospective, randomized trial comparing four biofeedback techniques for patients with constipation. Prognostic significance of rectocele, intussusception, and abnormal perineal descent in biofeedback treatment for constipated patients with paradoxical puborectalis contraction. Effects of biofeedback on obstructive defecation-reconditioning of the defecation reflex Response to a behavioural treatment, biofeedback, in constipated patients is associated with improved gut transit and autonomic innervation.
Syndromes
- Diabetic acidosis and other forms of metabolic acidosis
- Nausea
- Lipase level
- Direct person-to-person contact
- Amount swallowed
- Eye exam
- Cardiomyopathy
- Muscle rigidity
Buy cleocin 150mg low cost
The most commonly used treatment for ulcer bleeding worldwide is epinephrine injection therapy; it is widely available skin care routine for dry skin order cleocin mastercard, easy to perform, safe, and inexpensive. Therapy with epinephrine alone seems to be more effective when used in high doses (13 to 20 mL) than in low doses (5 to 10 mL). The risk depends on whether arterial blood flow is detected before endoscopic hemostasis (Refs. Epinephrine (1:20,000) injected in 1-mL aliquots into each of 4 quadrants should be injected around clot initially, followed by piecemeal snare resection of the clot and treatment of underlying stigmata. Colonic diverticulum with active bleeding can be treated with epinephrine (1:20,000) injected into the neck or base. If a visible vessel is seen at the neck, it can be treated with multipolar electrocoagulation. Pressure is the tamponade pressure exerted en face or tangentially via the contact probe directly on the lesion. Power, pressure, and duration settings must be reduced for small, acute, or deep bleeding lesions. The rebleeding rate for ulcers with an adherent clot treated with medical therapy alone is 8% to 35%, with most large studies reporting rebleeding rates of 30% to 35%. Clean-Based Ulcers Patients with a clean-based ulcer at endoscopy after target irrigation have a rebleeding rate of less than 5%. When combination therapy is performed, coagulation is performed with a large 10 Fr multipolar probe. After epinephrine injection, the thermal probe is placed directly on the bleeding site to tamponade the site and stop the bleeding, and coagulation is applied with long (10-second) pulses and firm pressure at a low (12- to 15-W) power setting. The probe is then removed slowly from the ulcer (sometimes with gentle irrigation to prevent pulling coagulated tissue), and thermal coagulation is repeated as required to stop bleeding and flatten any underlying visible vessel. With successful endoscopic hemostasis, the rebleeding rate can be decreased to 30% with monotherapy and 15% with combination therapy (see Table 20. Alternatively, injection of epinephrine followed by hemoclip placement directly across the actively bleeding site can also be effective. Some investigators recommend that clips be placed prior to injection of epinephrine to allow placement of the clip directly on the vessel rather than on a submucosal epinephrine-filled cushion. B, After injection of epinephrine, oozing has subsided; the edge of the ulcer is seen inferior to clot. We use the same technique as that used to stop active bleeding: flattening of visible vessels using a large probe, firm pressure, and a low power setting. Coagulation or hemoclipping is performed if active bleeding, a visible vessel, or residual pedicle is seen. The combination technique decreases the rebleeding rate from up to 35% (with medical therapy alone) to 5%. Monotherapy with a thermal probe or epinephrine injection reduces the rebleeding rate to less than 5%. In patients with oozing, the bleeding arteries may be small and the outcomes are better than those in patients with active arterial bleeding. B, the nonbleeding visible vessel is injected with epinephrine, after which blanching and swelling of surrounding mucosa occur. D, After completion of treatment, the visible vessel has been coagulated and flattened. B, the clot was injected with epinephrine, followed by piecemeal snare polypectomy to trim away the clot (C-E), after which an underlying vessel was revealed (F [arrow]). If the patient has a clean-based gastric ulcer, biopsies of the ulcer edge and gastric muscosa should be considered to exclude underlying malignancy (see Chapter 53). These patients can be fed after the endoscopy and treated with oral acid suppression medication; they do not require continued hospitalization unless indicated for other medical problems. Therefore the risk of rebleeding is high, and definitive hemostasis with standard techniques is usually required in patients with varices or ulcers with major stigmata. Current guidelines recommend utilization of hemospray as a stopgap or adjunct technique. Testing for Hp Infection In a patient with a bleeding gastric or duodenal ulcer, endoscopic mucosal biopsy specimens of the normal-appearing antrum and mid-body greater curvature should be obtained to assess for the presence of Hp infection. Biopsy specimens can be obtained safely after successful endoscopic hemostasis, but bleeding reduces the sensitivity of rapid urease testing. Therefore stool antigen and other tests for Hp infection are recommended (see Chapter 52). The rebleeding rate in the omeprazole-treated group was 11% compared with 36% in the placebo-treated group (P < 0. Second-Look Endoscopy Routine repeat, or second-look, endoscopy 24 hours after initial endoscopic hemostasis, with additional endoscopic hemostasis if persistent high-risk endoscopic stigmata are found, has been proposed as a way to improve patient outcomes. Rebleeding After Endoscopic Treatment the risk of rebleeding from peptic ulcers, which started bleeding in the outpatient setting and required endoscopic hemostasis, is greatest in the first 72 hours after diagnosis and treatment. The difference between ulcer hemorrhage that starts in the outpatient setting and hemorrhage that starts in the inpatient setting is substantial (Table 20. Further studies are warranted in this high-risk group to define optimal management. A large, well-designed, randomized trial from Hong Kong found that when endoscopic hemostasis is repeated in patients with hemodynamically significant rebleeding after initial endoscopic hemostasis, 73% of patients achieve sustained hemostasis and do not require surgery. Factors that predicted failure of endoscopic retreatment included an ulcer size of at least 2 cm and hypotension on initial presentation. This new treatment has the potential to reduce the need for surgery or angiography for recurrent ulcer bleeding. Surgery should also be considered if the endoscopist does not feel comfortable treating a large or pulsating visible vessel After successful endoscopic treatment and recovery from sedation, the patient can be started on a liquid diet, with subsequent advancement of the diet. For patients who have been on and need to continue antiplatelet agents or an anticoagulant, a cardiologist or vascular physician should be consulted to help determine whether, and for how long, these agents can be held. Intermediate-Risk Stigmata Patients with flat spots and arterial blood flow detected underneath, those with oozing bleeding from an ulcer and no other stigmata Angiography, Surgery, and Over-the-Scope Hemoclips Patients with recurrent bleeding despite 2 sessions of endoscopic hemostasis can be considered for angiographic embolization or surgical therapy. Antibiotic therapy does not have to *One point signifies a healthy person; 5 points signifies high likelihood of mortality within 24 hr. In patients who are found to have an Hp-induced ulcer, confirmation of the eradication of Hp after treatment is recommended (see Chapter 52). If the patient is also positive for Hp, the organism should be eradicated with standard therapy (see Chapter 52). Endoscopy with biopsies and brushings is critical for making these diagnoses and determining the appropriate pharmacologic therapy (see Chapter 45). Ulcer Hemorrhage in Hospitalized Patients Hemorrhage from an ulcer or erosions in hospitalized patients typically falls into 2 categories. Diffuse oozing is common, and patients have a poor prognosis and high rebleeding rate, often related to impaired wound healing and multiple organ failure. The 2 main risk factors are severe coagulopathy and mechanical ventilation for longer than 48 hours. By contrast, focal inpatient ulcer hemorrhage often requires endoscopic hemostasis for severe hemorrhage In areas of the world where the population is at intermediate risk for gastric cancer, 2% to 4% of repeat upper endoscopies to confirm ulcer healing have been reported to disclose gastric cancer. It is usually located in the gastric fundus, within 6 cm of the gastroesophageal junction, although lesions in the duodenum, small intestine, and colon have been reported. The cause is unknown, and congenital and acquired (related to mucosal atrophy or an arteriolar aneurysm) causes are thought to occur (see Chapter 38). Dieulafoy lesion can be difficult to identify at endoscopy because of the intermittent nature of the bleeding; the overlying mucosa may appear normal if the lesion is not bleeding. Mallory-Weiss Tears Mallory-Weiss tears are mucosal or submucosal lacerations that occur at the gastroesophageal junction and usually extend distally into a hiatal hernia. Patients generally present with hematemesis or coffee-ground emesis and a history of nonbloody vomiting followed by hematemesis, although some patients do not recall vomiting. The tear is thought to result from increased intra-abdominal pressure, in combination with a shearing effect caused by negative intrathoracic pressure above the diaphragm, which is often related to vomiting. Mallory-Weiss tears have been reported in patients who vomit while taking a bowel purge before colonoscopy.
Buy cleocin 150 mg lowest price
The appearance may be misleading skin care 08 order genuine cleocin on-line, however, because duodenal dilatation may be caused by atony rather than mechanical obstruction. Antroduodenal and small bowel manometry may demonstrate characteristic patterns that distinguish mechanical obstruction from a motility disorder. Relief of vomiting with feeding through an enteric catheter placed across the obstruction into the proximal jejunum supports the diagnosis. The surgical technique performed most commonly is a laparoscopic proximal duodenojejunostomy; a gastrojejunostomy may not be effective because the proximal duodenum is not decompressed by this approach. A history of regular cannabis use and relief of symptoms with abstinence from cannabinoids are hallmarks of the syndrome. Rumination typically begins during or immediately following a meal and may stop when the regurgitated material becomes noticeably acidic. Rumination is relatively common in infants, typically developing between 3 and 6 months of age. There is no apparent distress, and rumination may cease with distraction or sleep. Some otherwise healthy individuals ruminate frequently without considering the practice abnormal. Some ruminators seek medical attention because of the concern that they are unable to control the process. Rumination may be diagnosed clinically in most patients with careful history taking. Achalasia, other esophageal motility disorders, gastric outlet obstruction, and gastroparesis should be excluded. High-resolution esophageal manometry and impedance testing after a meal may help distinguish rumination from other belching and regurgitation disorders. During the abrupt retrograde movement of gastric content, the gastroesophageal junction appears to move into the thorax, thereby creating a "pseudohernia" that facilitates opening of the lower esophageal sphincter. Reassurance and careful explanation of the phenomenon may allow some patients to control rumination on their own. Behavior modification is the most effective therapy and may be accomplished by teaching the patient special diaphragmatic breathing techniques or with the help of biofeedback training, because rumination and diaphragmatic contraction cannot be performed simultaneously. Further pharmacologic treatment includes baclofen (up to 10 mg orally three times daily), a -aminobutyric acid agonist that increases lower esophageal sphincter pressure and decreases the swallowing rate. Additional Tests Further testing can include blood levels of drugs and toxins (specifically digoxin, opiates, theophylline, ethanol, and carbamazepine), cultures of blood or body fluids if an infection is suspected, analysis of cerebrospinal fluid following lumbar puncture, and serologic tests for viral hepatitis, if indicated. If appropriate, blood levels of cortisol, corticotropin-releasing factor, and catecholamines can be determined. Barium contrast radiography may suggest a diagnosis of achalasia, gastroparesis, or neoplasm. Motility studies are useful for evaluating motor disorders including gastroparesis and chronic intestinal pseudo-obstruction, which are relatively uncommon but important causes of nausea and vomiting (see Chapters 50, 99, and 124). Patients with esophageal motility disorders such as achalasia and other spastic disorders may occasionally present with vomiting or regurgitation (see Chapter 44). Measurement of Gastric Emptying Radioscintigraphy is the preferred and most accurate method of assessing gastric emptying and should be performed over a 4-hour period for accurate assessment of gastric emptying. Symptoms of gastroparesis are primarily associated with delayed solid phase gastric emptying. Patients can experience heartburn or retrosternal pain after an acute bout of vomiting. By contrast, patients with chronic vomiting rarely complain of chest symptoms, and esophagitis associated with long-standing vomiting is often asymptomatic. Abrupt retching or vomiting episodes may also induce longitudinal mucosal and, rarely, transmural lacerations at the level of the gastroesophageal junction. Acute bleeding and hematemesis associated with mucosal lacerations at the gastroesophageal junction constitute the Mallory-Weiss syndrome (see Chapters 20 and 45). Boerhaave syndrome refers to spontaneous rupture of the esophageal wall, with free perforation and secondary mediastinitis and carries a high mortality rate. Multiple purpuric lesions may appear on the face and upper neck after prolonged episodes of vomiting, probably because of repetitive increases in intrathoracic pressure and rupture of blood vessels. Antroduodenal Manometry Antroduodenal manometry is the most specific physiologic test for assessing foregut motor disturbances distal to the esophagus. Intraluminal pressure changes are recorded in the antrum and proximal small bowel using a pressure-sensitive catheter. If antroduodenal manometry is abnormal, a laparoscopic full-thickness biopsy of the small bowel can be considered to diagnose genetic and acquired myogenic or neurologic causes of chronic intestinal pseudoobstruction. Spasm of the Glottis and Aspiration Pneumonia Spasm of the glottis and transient asphyxia may develop during vomiting as a result of irritation of the pharynx by acidic or bilious material. Aspiration is more likely to occur when the stomach contains food, fluid, or enteric secretions, which should be aspirated out from the stomach during endoscopy. Fluid, Electrolyte, and Metabolic Alterations Fluid, electrolyte, and metabolic abnormalities may develop rapidly after protracted vomiting. Dehydration, hypotension, hemoconcentration, oliguria, muscle weakness, and cardiac arrhythmias can result. Hypochloremic alkalosis is usually the first metabolic abnormality to develop and is due to loss of fluid, as well as of hydrogen and chloride ions. Hypokalemia results from loss of potassium ions in the vomitus and renal potassium wasting due to alkalosis. Hyponatremia may occur in severe cases because of loss of sodium and release of antidiuretic hormone in an attempt to conserve intravascular volume. Metabolic derangements, especially metabolic alkalosis with low urinary sodium excretion, may be a sign of chronic functional or selfinduced vomiting. Autonomic Function Tests Tests of autonomic function can assess sympathetic function and include the tilt table test (an orthostatic challenge to blood pressure and cardiac rate regulation) and the cold hand test (a pain reflex test in which the hand is immersed in cold water to produce vasoconstriction and a significant increase in systolic arterial pressure). Nutritional Deficiencies Nutritional deficiencies may result from reduced caloric intake or loss of nutrients in the vomitus. Regardless of cause, chronic nausea and vomiting can result in malnutrition, weight loss, and deficiency states that require supplementation (see Chapters 5 and 6). Histopathologic Studies In some patients, a further diagnostic step may involve histopathologic examination of mucosal biopsies for quantification of nerve density and morphology as evidence of autonomic neuropathy. Adequate replacement generally consists of a normal saline solution in volumes sufficient to correct deficits (and in addition to maintenance fluids) with potassium supplementation (60 to 80 mEq/24 hours). When oral intake can be resumed, glucose-containing fluids are preferred because they are easily absorbed from the intestine. Patients with long-standing chronic vomiting are at risk of developing malnutrition, so enteral or parenteral feeding should be considered when the patient is unable to resume adequate oral nutrition after 5 to 8 days. Although enteral nutrition is a good option, even orogastrojejunal catheters placed with guidewires may be dislodged during episodes of vomiting. For long-term treatment, percutaneous enteral feeding tubes or home parenteral nutrition may be required (see Chapter 6). Although domperidone is a weaker antiemetic than metoclopramide, it may be particularly useful for the management of nausea and vomiting associated with treatment with levodopa in patients with Parkinson disease, because it antagonizes the proemetic side effects of levodopa without interfering with antiparkinsonian action in brain centers protected by the blood-brain barrier. A review of domperidone use in the treatment of diabetic gastroparesis has concluded that the drug is probably useful but has not been properly evaluated by well-designed controlled trials. Phenothiazines and Butyrophenones the phenothiazines (chlorpromazine, perphenazine, prochlorperazine, promethazine, and thiethylperazine) and butyrophenones (droperidol and haloperidol) also block D2 dopaminergic receptors in addition to muscarinic M1 receptors; phenothiazines also block histamine H1 receptors. These drugs tend to induce relaxation and somnolence and are generally used parenterally or as suppositories in patients with acute intense vomiting of central origin, as in vertigo, migraine headaches, and motion sickness. They are also useful for patients with vomiting from toxic agents, from chemotherapy and after surgery. Olanzapine, a second-generation neuroleptic agent, is an attractive alternative because of its strong antinausea and antiemetic action and lack of extrapyramidal side effects. Patients who received olanzapine had significantly increased sedation, which was severe in 5% of cases, particularly at day 2 as compared with baseline. Antihistamines and Antimuscarinic Agents Antihistamines and antimuscarinic agents act primarily by blocking histamine H1 receptors (cyclizine, dimenhydramine, cinnarizine, meclizine, hydroxyzine) and muscarinic M1 receptors (scopolamine, which may be applied transdermally) at a central level. Cyclizine and diphenhydrinate are commonly used to treat motion sickness and have been shown to decrease gastric dysrhythmia, so their antiemetic effect may be mediated in part by their peripheral action. A standard antiemetic dose of cyclizine is 50 mg given 3 times daily orally or 100 mg as a suppository.
Generic cleocin 150 mg visa
Antioxidant activity and other mechanisms of thiols involved in chemoprevention of mutation and cancer acne icd 10 purchase 150mg cleocin fast delivery. Repigmentation of vitiligo lesions in a child with celiac disease after a gluten-free diet. Rapid partial repigmentation of vitiligo in a young female adult with a gluten-free diet. Whey protein rich in alpha-lactalbumin increases the ratio of plasma tryptophan to the sum of the other large neutral amino acids and improves cognitive performance in stress-vulnerable subjects. The leaching out of the pigment to lymph nodes and deeper tissues is responsible for gradual fading of the pigment over a period of few years. The deeper pigment lying within tissue microphages is also responsible for the Tyndall effect, whereby the pigment of different colors and shades eventually looks bluish gray after years. Treating melanin-devoid lesions of vitiligo using extraneous pigments is the basis of camouflage therapy, which can be temporary or permanent. Micropigmentation or dermatography is a technique used for permanent camouflaging of various medical conditions of cosmetic importance, including vitiligo. Scientific use of the age-old art of tattooing in a medical framework to produce cosmetic camouflage is called micropigmentation. Tattoos have probably been used for medical purposes since 3000 bc or more, but the term micropigmentation came into fashion in the 1980s, and its use in vitiligo also started in the same time period [4,5]. Tattooing is a process of uniform implantation of minute, metabolically inert, pigmented chemical particles or microscopic granules into the dermis through a multiple puncture technique using manually or electrically driven, closely held needles. It may be used to camouflage the depigmented skin in a lesional pattern or to create designs [2,4]. However, good matching of the tattooed skin may be achieved at the time of tattooing but it tends to become grayish blue with time. In addition, iron oxide yellow color can be obtained by using cadmium oxide, while white titanium oxide can be used to mix and match various shades required with iron oxide. Cinnabar and mercuric sulfate are red pigments which can also be used to obtain various shades by mixing and matching. The red pigments, however, have more allergenic potential than others, and iron oxide is the most versatile pigment as it can give various shades and has the least sensitizing potential [5]. Traditional tattooing implants pigment at the level of the mid dermis where the pigment particles are initially engulfed by macrophages and mononuclear cells and remain intercellular for the initial few years. Gradually the pigment becomes both intercellular and extracellular and lays in the deep dermis and superficial supporting tissue and collagen fibers. Some pigment is also taken by hair follicle, blood vessels, and the procedure can be accomplished as an office procedure under strict aseptic conditions using local anesthesia. A pigment paste is generally prepared using distilled water, normal saline, glycerin, or alcohol to obtain a reasonable consistency which does not flow. Inlaying of the pigment can be achieved by using a simple hypodermic needle for a small area of vitiligo like focal vitiligo. Motorized tattoo machines (tattoo guns) are also available commercially, which have a group of needles to inlay pigment into dermis with a back-andforth motorized movement. These sewing needles can be used as disposable needles, so the complication of reuse can be avoided [6]. The pigment shows in the tattooed area immediately, and it becomes swollen due to multiple pricks and requires prophylactic systemic and topical antibiotics and analgesics. Too much bleeding and very close pricks may lead to leaching out of the pigment along with blood and tissue fluids. The results also depend upon elasticity and laxity of the skin along with blood flow and consistency of pigment paste. Vitiligo limited to mucosal and mucocutaneous areas of lips, visible area of inside of lip, gums or gingiva, etc. Genital vitiligo involving the glans penis, shaft of the penis, scrotum, vulva, and perineal and perigenital areas, umbilicus, etc. The present evidence also indicates its use in recalcitrant lesions of vitiligo, especially over the distal digits, lips, umbilicus, hands, wrists, axillae, elbows, perianal areas, lower legs, mucosae, and mucocutaneous junctions. Micropigmentation has also been used for nipple areola reconstruction, enhancement of eyebrows and eyelashes, permanent repigmentation of achromic burn scars, reconstitution of eyebrows following recalcitrant alopecia areata, and aesthetic improvements of scars and skin grafts, especially to camouflage hairless patches. Until 1984, tattooing was mainly performed as a permanent eyeliner for enhancing eye expression. Micropigmentation or dermatography has been used in the fields of craniomaxillofacial, reconstructive, and cosmetic surgery. Tattooing has also been done with gold salts, such as 20% aurothioglucose in sesame oil for vitiligo. Others have used this procedure for implanting various earthtone color pigments to the base of the eyelash as cosmetic eyeliner. The latest Cochrane review on treatment of vitiligo, however, fails to find well-controlled studies on this the subject of micropigmentation as a treatment option for vitiligo [1]. The permanency of the procedure must be explained to the patient in no uncertain terms before carrying it out. Excellent color matching has been reported on cutaneous, mucosal, and mucocutaneous lesions, especially in dark individuals. Successful repigmentation of six cases of herpes labialis induced lip leucoderma by micropigmentation. Presentday emphasis is to reserve this procedure for therapeutic indications or as an adjunctive to surgical management of vitiligo. It is extremely helpful in coloring and concealing patches of vitiligo which at times may be stigmatic to reveal. The best patients with vitiligo for this procedure are those who do not want white skin spots and any other shade shall be acceptable for them and are looking for instant results. Looking beyond the knife: Establishing a framework for micropigmentation following breast reconstruction. This makes the patient and their family follow many different types of rituals rather than seeking medical help. Because of the huge cosmetic impact of the disease, patients tend to become depressed, which further triggers their disease condition. A study conducted on the stigmatization experience, coping, and sense of coherence in vitiligo patients supported the notion that treatment of vitiligo patients should address the emotional effects like stress, stigmatization, and depression and also include tools for psychological intervention [10]. This not only can result in better adaptation to the disease but also improved quality of life [11]. The treatment should be aimed at improving the overall quality of life and reduction in feelings of stigmatization caused by this chronic ailment. Hence debunking common myths around vitiligo with actual facts is important to the treating dermatologist as it forms a crucial part of counseling patients. Myths are popular beliefs or stories that have become associated with a person, community, or occurrence, especially when considered to illustrate a cultural ideal [12]. Many myths and misconceptions exist related to the disease and these vary from one part of the world to another. The commons ones are that the disease is not treatable, it is contagious, it is a form of leprosy, it is always hereditary, it is related to specific types of food and drinks, and it may ultimately lead to skin cancers [13]. This chapter deals with some of the most common myths prevalent about vitiligo in the society. In this autoimmune condition, depigmentation is caused by the loss of functional melanocytes from the affected area of the epidermis.