Buy generic septra online
Clinical Correlate: Because the round ligament terminates in the labia majora symptoms of colon cancer discount septra 480mg free shipping, inguinal hernias can rarely present as labial masses. In pregnancy, varicosities of the round ligament can readily be mistaken for inguinal hernias. Posteriorly, the labia minora may be united by a small fold of the skin called the frenulum of the labia. It is the term applied to the mons pubis and labia majora, and the structures that lie between the labia. Mons pubis the mons pubis is a rounded, median elevation lying anterior and inferior to the pubic bone. The suspensory ligament of the vagina attaches to the subcutaneous tissue of the mons pubis. Labia majora the labia majora are two large folds of skin that run downward and backward from the mons pubis. These elongated folds enclose between them the median pudendal cleft and are largely filled with subcutaneous fat. The lateral part joins the corresponding one from the opposite side to form the prepuce of the clitoris. Clinical Correlate: Partial or complete removal of the labia minora and/or majora due to female genital mutilation is increasingly seen in the United States. Recent reports estimate that up to 507,000 females in the United States have undergone or are at risk for genital cutting. It contains the orifices of the urethra, vagina, and ducts of the greater vestibular glands. The external urethral orifice (meatus) is located about 2 cm or more behind the glans clitoris and immediately in front of the vaginal orifice. The vaginal orifice is considerably larger than the urethral one and is also a median cleft. Its appearance and size depend upon the condition of the hymen, which is a thin fold of mucous membrane that partially or sometimes wholly occludes the vaginal orifice. The parts of the labia minora lying anterior to the clitoris form the prepuce of the clitoris, whereas the parts lying posterior to it form the frenulum. The clitoris consists mainly of erectile tissue and is capable of enlargement like the penis as a result of engorgement with blood. It is composed of two corpora cavernosa which form the body of the clitoris, which is about 2. The corpora cavernosa are enclosed by a fibrous envelope and are separated from each other by an incomplete septum. The body of the clitoris separates posteriorly into two crura, each of which is attached to its respective ischiopubic ramus. It also is composed of erectile tissue and, like the glans of the penis, is covered by sensitive epithelium. The suspensory ligament of the clitoris connects the organ to the front of the pubic symphysis. Bulbs of the vestibule the bulbs of the vestibule are two elongated masses of erectile tissue, one lying at each side of the vaginal opening under the bulbospongiosus muscle. They are narrow in front where they unite with each other to form a thin strand which is connected to the underside of the glans clitoris. The duct of each gland opens into the groove between the labium minus and the attached margin of the hymen. During sexual intercourse, the greater vestibular glands are compressed and secrete mucus which lubricates the vagina. There are many smaller, lesser vestibular glands on each side of the vestibule which open between the urethral and vaginal orifices. Ascending infections have been described with bartholin abscess in pregnant women. The infections are typically polymicrobial with Escherichia coli being the most common isolate. When incising a bartholin abscess, the incision should be made at, or proximal to , the hymen. It extends from the symphysis pubis, anteriorly, to the sacrum and the tip of the coccyx, posteriorly, with an ischial tuberosity on each lateral side. Its superior limit is the pelvic diaphragm consisting of the levator ani and coccygeus muscles. It is restricted to the region immediately around and between the anal and vaginal orifices. The perineum is divided into two parts, the urogenital region and the anal region. The urogenital region is anterior to an imaginary horizontal line joining the midpoints of the two ischial tuberosities. The perineal body or tendinous center of the perineum is a fibromuscular mass that is located in the median plane between the anal canal and the lower vagina. It contains smooth and skeletal muscle fibers bound with elastic and collagenous tissue. Attached to it are the superficial and deep transverse perineal, the bulbospongiosus, the levator ani, and the anal sphincter muscles. The anal sphincter muscles include an external sphincter, which is a thick ring of predominately striated muscle, and an internal anal sphincter. The internal sphincter is found deep to the external sphincter and extends approximately 1 cm superior to external sphincter, along the anal canal. The superficial and deep perineal fasciae and the superior and inferior fasciae of the urogenital diaphragm blend with it. Clinical Correlate: Lacerations or episiotomies in the midline may involve the anal sphincter and the rectum. Command of the anatomy in this region is imperative to safely and successfully repair these defects. Particular attention should be placed to restoring the both the internal and external anal sphincters, if involved, as they perform roles in anal continence. Urogenital region the urogenital region contains the external genital organs and the associated muscles and glands. All of the muscles in the superficial compartment are supplied by the perineal branch of the pudendal nerve. Bulbospongiosus muscle this muscle arises from the tendinous center of the perineum and passes forward around the lower part of the vagina covering the bulb of the vestibule. It is inserted partly into the side of the pubic arch and partly into the dorsum and body of the clitoris. Clinical Correlate: this muscle is often disrupted in second degree vaginal lacerations and mediolateral episiotomies. Ischiocavernosus muscle this muscle originates from the inner surface of the ramus of the ischium and inserts on the lower and medial aspects of the crus of the clitoris. It helps to maintain erection of the clitoris by compressing the crus and thus retarding the flow of blood from the clitoris. Superficial transverse perineal muscle this muscle arises from the lower part of the inner surface of the ramus of the ischium adjacent to the tuberosity and inserts into the tendinous center of the perineum. Deep perineal compartment the deep compartment is enclosed between the superior and inferior layers of fascia of the urogenital diaphragm. Deep transverse perineal muscle this muscle arises from the inner surface of the ramus of the ischium. Its anterior fibers insert into the lateral wall of the vagina, and its posterior fibers insert into the tendinous center of the perineum. Sphincter urethrae muscle this muscle arises from the inner surface of the inferior ramus of the pubis. Most of its fibers insert into the lateral wall of the vagina, but a few pass in front of the urethra and between the urethra and vagina. Since the urethra and vagina are fused inferiorly, the fibers of the sphincter urethrae muscle do not surround the urethra completely. The superior fascia of the urogenital diaphragm is indistinct, but the inferior fascia is relatively dense and strong. The deep compartment contains the internal pudendal vessels, the dorsal nerve of the clitoris, and branches of the perineal nerve that supply the two muscles located there. The anal canal passes through the pelvic diaphragm and opens onto the surface of the perineum as the anus.
Buy septra 480mg with mastercard
The drug of choice should be one that covers Gram-positive and Gram-negative bacteria ok05 0005 medications and flying buy 480 mg septra amex. This dose may need to be increased in obese patients; this is discussed further below. Several new studies have attempted extending the spectrum of antibiotics to include coverage for Ureaplasma and Mycoplasma with the addition of azithromycin, doxycycline, or metronidazole and have found reductions in infection rates and duration of hospital stay; however, more studies are needed to identify if this difference is significant. However, this is a controversial topic due to the unknown effects of antibiotics on neonatal outcome and has led institutions to administer the antibiotics 424 Prevention of surgical site infections Microorganisms associated with cesarean section. Staphylococcus aureus Staphylococcus epidermidis Escherichia coli Enterococci Staphylococci Streptococci Enterococci Lactobacilli Diphtheroids E. A meta-analysis including 10 studies and 5041 women showed administration of prophylactic antibiotics prior to incision halved the risk of endometritis and wound infection as opposed to women who received antibiotics after cord clamping. In cases of severe penicillin allergies, such as anaphylaxis, angioedema, respiratory distress, or urticaria, clindamycin with an aminoglycoside, such as gentamicin, is an appropriate alternative. More randomized controlled trials are required for the development of an algorithm or guidelines. Currently, there are no evidence-based recommendations for antibiotic prophylaxis. However there are several risks associated with cervical cerclage placement, including chorioamnionitis, preterm premature rupture of membranes, preterm delivery, displacement of sutures, and cervical lacerations. Transabdominal cerclage placement also has additional risks that normally exist for abdominal surgery. Cerclage placement is contraindicated in patients who exhibit signs of labor or chorioamnionitis. The risk of developing intraamniotic infection is increased in patients with emergency, indicating cerclage placement; however, no recommendations currently exist for the use of antibiotic prophylaxis. In patients with cerclage placement due to history or ultrasound finding, the risk of developing intra-amniotic infection is rare and no antibiotic prophylaxis is indicated. Therefore, it is recommended that cord traction be used as the method of delivering the placenta during a cesarean. Some physicians prescribe them because of the proximity of the incision to the rectum and the potential of transmitting bacteria from the rectum to the laceration. Of those who received antibiotics and returned for a 2-week postpartum check as required for the study (n = 49), 8. Due to the high dropout rate, these results are difficult to generalize to the population. Cesarean hysterectomy is performed for several indications including, uncontrolled postpartum hemorrhage, abnormal placentation, uterine rupture, leiomyoma, cervical laceration, invasive cervical cancer, or ovarian neoplasia. In recent years, the predominant reason for cesarean hysterectomy has been abnormal placentation, followed by uterine atony and uterine rupture. The morbidities associated with this procedure include blood transfusion, fever, perinatal death, bladder injuries, wound infection, disseminated intravascular coagulation, and postoperative ileus. In patients, where placental accreta disorders are detected in the intrapartum period, preparations are made in anticipation of these risks and lead to decreased blood loss, less requirement for transfusion, and less disruption of the urinary tract system. In cases where the procedure is performed as an emergency, blood loss prior to the procedure compounds the blood loss associated with the procedure itself. However, additional doses may be administered when there is a blood loss greater than 1500 mL or if the procedure is longer than 4 hours. As part of that initiative, data were collected to study the different maternal behaviors, health conditions, and experiences for women in the United States who had a live birth. Prevalence was noted to be higher among women aged 20 years old or greater, and among black and Hispanic women. With evidence showing increased rates of woundrelated complications in obese pregnant women, recommendations for wound infection prevention include antibiotic prophylaxis with consideration for a higher dosage. Most hospital institutions have 2 g cefazolin dosing as the standard recommended higher dose. Adequate antibiotic levels at the incision site in pregnant obese patients are affected by a greater volume of distribution and increased glomerular filtration rate. Another small study showed 4 g cefazolin dosing provided increased antibiotic concentrations in adipose but it did not study whether it decreased infection rates. Other methods appropriate for infection prevention include closure of the subcutaneous layers with plain suture when it is greater than 2 cm for prevention of wound separation and its associated complications. Several studies have also examined drainage systems in conjunction with subcutaneous closure in reducing wound infection and found no difference. National Action Plant to Prevent Health Care-Associated Infections: Road Map to Eelimination. Comparison of bacteria on new, disposable, laundered, and unlaundered hospital scrubs. Disposable surgical face masks for preventing surgical wound infection in clean surgery. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings. Gloves, extra gloves or special types of gloves for preventing percutaneous exposure injuries in healthcare personnel. Influence of double-gloving on manual dexterity and tactile sensation of surgeons. Blunt versus sharp suture needles for preventing percutaneous exposure incidents in surgical staff. Glove perforations with blunt versus sharp surgical needles in Caesarean delivery: A randomized control trial. The use of blunt needles does not reduce glove perforations during obstetrical laceration repair. Role of blunt suture needle in episiotomy repair at uncomplicated vaginal deliveries in reducing glove perforation rate: A randomized controlled trial. Effect of hand cleansing with antimicrobial soap or alcohol-based gel on microbial colonization of artifical fingernails worn by health care workers. Pathogenic organisms associated with artificial fingernails worn by healthcare workers. Candida osteomyelitis and diskitis after spinal surgery: An outbreak that implicates artificial nail use. A prolonged outbreak of Pseudomonas aeruginosa in a neonatal intensive care unit: Did staff fingernails play a role in disease transmission Preoperative hair removal and surgical site infections: Network metaanalysis of randomized controlled trials. Skin preparation for the prevention of surgical site infection: Which agent is best The forgotten role of alcohol: A systematic review and meta-analysis of the clinical efficacy and perceived role of chlorhexidine in skin antisepsis. Reduction of surgical site infections in low transverse cesarean section at a university hospital. Traffic flow in the operating room: An explorative and desriptive study on air quality during orthopedic trauma implant surgery. Risk factors for particulate and microbial contamination of air in operating theatres. Implementation of a bundle of care to reduce surgical site infections in patients undergoing vascular surgery. Measuring intraoperative interference from distraction and interruption observed in the operating theatre. Microbiology of explanted suture segments from infected and noninfected surgical patients. Early versus delayed dressing removal after primary closure of clean and clean-contaminated surgical wounds. Early versus delayed post-operative bathing or showering to prevent wound complications. Surgical staples compared with subcuticular suture for skin closure after cesarean delivery: A randomized controlled trial.
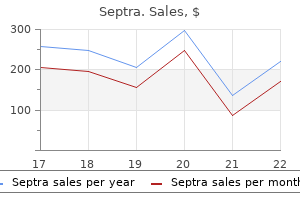
Purchase septra 480mg fast delivery
The uterus that has accommodated a previous pregnancy is usually slightly larger than the one that has not medications post mi buy line septra. By the end of the second month of gestation, the uterus triples in size and changes from the typical flat pear shape to a rounded form, a shape it retains throughout the second trimester. Because of the rapid increase in size and weight during the second month, the uterus may assume exaggerated positions of anteflexion, retrocession, and retroversion. It contacts the anterior abdominal wall and displaces the intestines laterally and superiorly. Midway through pregnancy (20 weeks gestation), the fundus is at the level of the umbilicus. At the beginning of the third trimester, the uterus assumes an ovoid shape, the vertical axis increasing more rapidly than either the transverse or anteroposterior axis. Rotation to the right is considered to result from the pressure of the sigmoid colon in the left side of the pelvic cavity. Occasionally, rotation of the uterus to the left occurs when there is a pelvic or lower abdominal mass on the right side. In the supine position, the uterus lies backward, resting upon the aorta and inferior vena cava. The myometrium during pregnancy the wall of the uterus is composed of a thin outer covering of peritoneum (serosa), a thick, intermediate layer of variable proportions of muscle and connective tissue (myometrium), and an inner mucosal layer (endometrium). The body of the uterus contains the most muscle, with the content of muscle fibers diminishing below as the cervix is approached. The cervix is composed mainly of connective tissue and only about 10% muscle fiber. This interlacing network of muscle fibers is in the middle layer that forms the main part of the uterine wall. Bundles of smooth muscle contained in the supportive ligaments interlace and blend with the middle layer. The inner layer of muscle consists of circularly arranged, sphincter-like fibers at the isthmus and, at the orifices of the tubes, it is continuous with the inner portion of the inner circular layer of the tube. Two muscle bundles, the fasciculi cervicoangulares, are present at the lateral aspect of the uterus, bridging the cervix and fundus. The bundles may serve as a system for conduction or coordination of muscle contraction. Uterine enlargement during pregnancy involves stretching and marked hypertrophy of the muscle layer. At term the body of the uterus weighs over 1000 g compared to approximately 70 g in the nongravid state. Since mitotic activity is rarely observed in the myometrium, the smooth muscle cells are considered to undergo hypertrophy rather than hyperplasia. The new muscle cells which do form likely originate from growth of the media of the myometrial arteries and veins. During the second and third trimesters, the increased uterine size is caused mainly by the pressure exerted by the expanding conceptus. Thinning of the uterine wall may be exaggerated in multigravid women, during multiple pregnancy and in hydramnios. The musculature in the wall of the isthmus must dilate during labor rather than contract and, after the second month, makes up the major portion of the lower uterine segment. It is poorly defined during the early weeks of pregnancy when the area feels softer than either the body or cervix. During the second trimester, the isthmus becomes incorporated into the body of the uterus and the isthmic canal becomes part of the uterine cavity. This condition persists until the middle of the last trimester, when a transverse linear depression appears in the junction region. It is sometimes referred to as the physiologic contraction ring, which rises to a higher level during labor. After delivery the ring appears as a marked constriction between the body and the cervix. The cervix of the gravid uterus the size of the cervix in relation to the body of the uterus varies with age and parity. The cervix is twice the size of the body in a young child, about equal in nulliparous women, and about one-third the size of the body in a multiparous woman. It is composed mainly of collagen-rich connective tissue and only approximately 10% is muscle. Two of the earliest signs of pregnancy are cervical softening and cyanosis caused by increased vascularity and edema. Soon after conception, the cervical glands secrete a very thick mucus into the cervical canal, forming a plug that closes off the canal during the gestation period. In the nonpregnant state, the glands usually comprise only a small fraction of the cervical mass. They undergo such remarkable proliferation during pregnancy that by term they make up approximately one-half its mass. There is no appreciable change in the muscle content of the cervix during pregnancy. The incompetent cervix dilates painlessly during the second or early third trimester, resulting in rupture of the membranes, followed by the delivery, usually, of a previable fetus. Previous cervical trauma from such procedures as dilation, curettage, and cauterization appears to be a major causative factor. The ratio of muscle to collagen has been reported to change, resulting in more abundant muscle fibers. The cervical canal is slightly expanded in its middle and opens into the vagina through the external os. The point where the lower end of the isthmic canal widens into the cervical canal is known as the histologic internal os, as it is the point where an abrupt microscopic change occurs in the mucosa. The uterine cavity in the gravid condition enlarges as the myometrium hypertrophies. Initially, its rate of enlargement is greater than the growth rate of the conceptus. Later, during the early part of the second trimester, the uterine cavity becomes completely filled by the rapidly expanding conceptus. Uterine enlargement is not symmetric but is sometimes most marked in the fundus and other times in the body below the tubes. Its canal runs from the superior angle of the uterine cavity to the ovary and gradually increases in diameter as it courses laterally. When straightened, the tube in the nongravid state measures approximately 10 cm long. The intramural portion passes through the uterine wall and has the smallest lumen diameter (1 mm or less). It continues laterally into a broad, sometimes tortuous, portion called the ampulla. Finger-like fimbriae extend from the periphery of the infundibulum surrounding the abdominal ostium. The wall of the uterine tube is made up of three layers: an outer serosa, an intermediate smooth muscle layer (myosalpinx), and an inner mucosal lining (endosalpinx). The endosalpinx is arranged into longitudinal folds that become highly branched in the ampullary segment. Each ovary measures approximately 4 cm long, 2 cm wide, and 1 cm thick and usually has a grayishpink color and a puckered, uneven surface. Its long axis is nearly vertical, with the upper pole located close to the uterine tube and the lower pole nearer the uterus. Its posterior border is free, but its anterior border is attached to the broad ligament by a short, two-layered fold of peritoneum, the mesovarium, through which vessels and nerves pass to the hilum of the ovary. However, in the multiparous woman, it may lie anywhere against the lateral pelvic wall and sometimes in the rectouterine pouch.
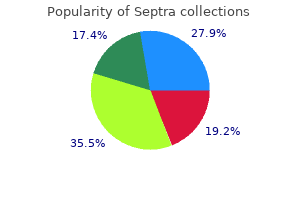
Purchase septra us
An alternative 9 medications that can cause heartburn generic 480 mg septra with mastercard, highly effective, and time-proven maneuver is somewhat more involved and requires careful observance of a series of steps. This approach stipulates that: (1) extraction of the retained arm should be carried out in the space provided by the sacrum; (2) the right arm should be extracted with the right hand and the left arm with the left hand; (3) the arm should be brought out in front of the fetus and never behind the body; and (4) any traction or pressure exerted upon the arm must be directed against a joint, usually at the elbow. When the tendency of the rotation is such that the left shoulder is anterior and the right one is posterior, the legs of the fetus are grasped with the left hand, and, with a semicircular swing, they are lifted up to rest against the right inguinal area of the mother. The index and middle fingers of the right hand are inserted into the vagina over the perineum in such a manner that they follow the shoulder and upper arm and reach out for the elbow joint of the right arm. With pressure and traction upon the joint, the arm is swept out under the body in the space provided by the curve of the sacrum. Now the left hand is introduced into the vagina and the index and middle fingers sweep out the left arm in the same manner as described before. This procedure is highly useful for the prevention, as well as for the correction, of extension of the arm above the head. By the same token, rotation of the body in the wrong direction is likely to result in extension of the arm and difficulties with delivery of the head. Thus, by definition, this is "assisted breech delivery", part of the expected process when breech delivery is an elective procedure. Several excellent methods are available, probably equally satisfactory in experienced hands. It was through the contributions of Levret, Smellie, and Veit that it achieved great popularity during the last three centuries. In the absence of spontaneous delivery up to and including the shoulders and the arms, the Mauriceau maneuver (as well as the other comparable techniques) follows the extraction of the arms immediately. Note that the left hand simply supports the body of the fetus while the right one is used for traction. The purpose of this hold is not traction (in fact, traction should be avoided very carefully), but flexion of the fetal head in order to permit the passage of the most favorable diameter of the vertex through the pelvis. With flexion of the fetal head carefully maintained throughout the traction, as the occiput is felt to clear the resistance offered by the symphysis, the direction of the pull is changed gradually until, in the course of upward traction, the nose, forehead, and cranium are borne over the perineum. Alternatively, when the perineum does not offer resistance, it may precede the delivery of the head. Occasionally, in cases of multiparous women with lax perineal structures, breech delivery may be done without perineal incision. A simple and effective method for the delivery of the head is that recommended by Bracht. Even more than other procedures, this one mandates that the bladder be emptied immediately before the delivery. The technique requires the cooperation of two persons, one who handles the fetus and another who exercises pressure over the lower abdomen of the mother upon the fetal head. In Germany, where the technique enjoys particular popularity, the role of the person exercising pressure above the symphysis is perceived as the crucial one. Therefore, it is generally the attending physician who applies the pressure and the assistant, or assisting midwife, who holds and delivers the fetus. In general, the procedure is considered suitable for the completion of spontaneous birth, but not for one that requires partial or complete extraction. Accordingly, those attending should refrain from any action until the fetus is delivered up to the neck. If necessary, the arms are brought down with one of the earlier discussed methods. The assistant simply supports the body of the fetus in such a manner that with the birth of the upper body, the trunk is lifted up first to the level of and then above the symphysis. When the full delivery of the body is accomplished, with two fists placed over the symphysis, the physician applies firm, continuous pressure against the head of the fetus. Under constant pressure and elevation of the body by the attending physician or the assistant, the fetus is delivered finally in a head-down position. In the practice of many European obstetricians, the Bracht maneuver is the first-line procedure. They resort to the Mauriceau maneuver on those rare occasions when the procedure fails. Before the application of forceps to the aftercoming head, the fetus must be held by an assistant with some degree of extension at the neck. Some operators prefer to assume a kneeling position before introducing the left blade upward and diagonally across the introitus along the mento-occipital line of the fetal head. A large episiotomy is essential so that during the introduction of the forceps blade, extension of the head is avoided. Before locking the forceps, it is important to be certain that the blades have been inserted with sufficient depth to have a good purchase on the fetal head. These forceps are designed to prevent injury to the fetal neck, to decrease compression of the fetal head, and to give the needed axis traction. The index finger of the inside hand ensures flexion of the head and is not used for traction. External version 339 Nuchal arms Nuchal arms are a significant complication during breech delivery that may be prevented to a large degree. It has been shown that umbilicus-to-mouth delivery times of up to 240 seconds (4 minutes) are usually associated with 5-minute Apgar scores of 7 or greater. If nuchal arms are present, the infant should be raised or lowered in the direction opposite to the nuchal arm and flexed over the opposite groin or buttocks of the mother. The trunk is then rotated so that the opposite nuchal arm is swept along the chest wall and the splinting maneuver repeated. The rule of delivering left arm with left hand and right arm with right hand must be remembered. During this procedure, no part of the fetal body other than the leg is delivered spontaneously. The operator places a hand in the birth canal, locates by palpation both or at least one of the fetal feet, and delivers the lower extremities by gentle traction. The fetal thighs are next grasped as in partial breech extraction and the fetal torso is delivered to the scapulae. The anesthesiologist in the delivery room may be called upon to administer general anesthesia during total breech extraction in the absence of sufficient maternal pain relief. Hardly ever used in connection with elective delivery of singleton fetuses presenting by the breech, the technique is favored by some obstetricians for the delivery of the second twin, sometimes after the performance of an internal version. If there is a choice, the upper foot is to be grasped when the fetal abdomen or chest is presenting, whereas the extraction of the lower limb is preferable when the presenting area is the fetal back. This promotes anterior rotation of the back and prevents anterior rotation of the chin and its earlier mentioned sequelae. In the absence of a choice, the leg that can be reached easiest is to be used for traction. Occasionally, it is possible to grasp both lower limbs, a circumstance that facilitates the procedure. The conclusion of internal version is identical with that of breech extraction as described earlier in this chapter. Internal uterine manipulations carry the risks of uterine rupture and cervical damage as well as that of colporrhexis. Therefore, exploration of the uterine cavity after the delivery of placenta and thorough inspection of the cervix and the vaginal vault are integral parts of the total operative procedure. Although, even relatively recently, internal version and extraction have been used widely for the delivery of the second twin presenting as a vertex, such a stressful fetal manipulation is rarely justifiable. Spontaneous vertex delivery usually follows artificial rupture of the membranes; if not, delivery can be accomplished with the vacuum extractor. Thus, transverse lie of the second twin is probably the only good reason for internal version and extraction in modern obstetrics. It consists of three steps: (1) introduction of the hands, (2) grasping the lower extremity or extremities, and (3) version of the body.
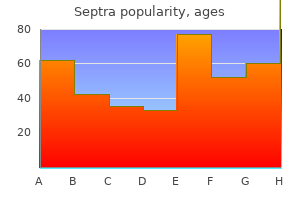
Purchase generic septra on line
On the ground of a large international study which involved a variety of obstetric centers with differing professional standards medicine to stop vomiting septra 480 mg for sale, Hannah et al. The latter complication along with a variety of others that occur with increased frequency after abdominal deliveries, such as placenta previa, placenta accreta, premature labor, and in utero fetal death, imposes substantial risks upon future siblings of babies delivered by the abdominal route. A randomized study which compared elective cesarean section with protocol-managed labor in frank breech fetuses at term found significant maternal morbidity when breech infants were delivered by cesarean section, with no dramatic improvement in the neonatal outcome. When the opportunity arises for a selective trial of labor, the obstetrician must possess the skills necessary to conduct delivery vaginally. It is advisable to discuss the risks and benefits of the available options with the patient before any relevant decision making. Although usually less conducive to birth trauma than a vaginal breech delivery, abdominal extraction of the fetus presenting by the breech can involve considerable technical difficulties. Since the lower uterine segment is often uneffaced, it may be difficult to cut a long enough transverse uterine incision for the delivery of the aftercoming head. Delay in completing the delivery process may cause fetal hypoxia, and undue force used during traction may result in traumatic injury. For this reason, careful inspection of the contemplated incision site is important. When necessary, there should be no hesitation to apply a lower segment vertical incision in order to minimize the risks of these complications and the incision can extend toward the fundus as necessary. If this opportunity has been forfeited, extension of the incision in an inverted "T" fashion may resolve the problem at the expense of leaving behind a weak and vulnerable scar in case of future pregnancy. Extension of the incision into a long classical incision may be the only solution in such instances. In cases of premature cesarean breech delivery, when the lower uterine segment is not developed, a lower segment transverse incision may be insufficient to deliver the head. The manipulative procedures to be described evolved decades and even centuries ago as a result of extensive application in everyday practice. With regard to elective breech delivery, one must remember the importance of certain precautionary measures6: (1) labor should not be induced, (2) oxytocin should not be used for uterine stimulation, (3) the second stage should not extend beyond 60 minutes, (4) the estimated fetal weight should not exceed 3600 g. Vaginal breech delivery may occur spontaneously or may require partial or complete breech extraction. Personnel critical to a safe vaginal delivery in breech presentation include: (1) an obstetrician skilled in the appropriate techniques; (2) an assistant to support the weight of the fetal body as the aftercoming head is delivered or, when needed, provide suprapubic pressure on the descending fetal head to maintain flexion; (3) a pediatrician to resuscitate the neonate if required; (4) an anesthesiologist to provide pain relief during the delivery; (5) appropriate nursing support; and (6) operating room personnel scrubbed and gowned for instant cesarean section. Based solely on the mode of vaginal delivery, the best perinatal outcome has been found in association with spontaneous birth. The more complicated the procedure and manipulation needed for vaginal breech delivery, the greater the perinatal morbidity and mortality risk. The expulsion of the legs precedes the emergence of the buttocks in partial or complete breech presentations. As the fetal buttocks distend the perineum, episiotomy usually is required to prevent undue delay and maternal perineal lacerations. As the fetal body descends to the umbilicus, the physician supports, but does not place traction on, the fetal torso. It is important to allow sufficient time for spontaneous delivery, bearing in mind, however, that once the body is expelled to the scapula, the umbilical cord becomes compressed between the head and the bony pelvis. Assisted breech delivery In the process of birth, the delivery of the fetal body occurs relatively quickly once the breech has emerged through the pelvic outlet and the trunk has begun its rotation. This important factor is bound to be lost or reduced if conduction or general anesthesia is used. Interference prior to the delivery of the trunk, whether elective or indicated, increases the risks involved with the delivery of the head. In most instances, the need exists for providing assistance with the delivery of the aftercoming head. The various maneuvers that facilitate this process will be discussed in some detail in the following sections. Despite favorable cephalopelvic proportions, the premature fetus is liable to be stressed excessively or suffer birth injuries due to its fragile physical structure. Additional risks are introduced by the fact that the relative diameters of the breech, as compared with the head, are small, and the presenting part can pass through the cervix at a lesser degree of dilation than that required for the passage of the head. Thus, chances are high that the powerful musculature of the cervix will prevent delivery of the caput for a prolonged period of time. On rare occasions, the normal rotation of the fetus is reversed and the chin instead of the occiput rotates toward the symphysis after the delivery of the body. In this situation, the chin interlocks with the symphysis; a collision which is bound to deflex the head. Ideally, the malrotation should be prevented by facilitating the anterior rotation of the back before the full delivery of the trunk. This can be begun by an external maneuver; a fist over the symphysis displaces the chin toward one side. The effort is to be completed internally; a hand inserted into the vagina tries to rotate the occiput toward the desired direction. If this maneuver fails, as it often does, the "reverse Prague maneuver" is the last resort. One hand grasps the fetal extremities and brings them, with gentle force, toward the abdomen of the mother. Since the use of some force is likely to be required under these exceedingly unfavorable circumstances, the maneuver involves considerable fetal risks. In contemporary practice, "abdominal rescue"35 seems to be the preferable approach. Partial breech extraction Partial breech extraction involves the spontaneous delivery of the fetus to the umbilicus and the employment of obstetric maneuvers thereafter for delivery of the upper torso, shoulders, arms, and aftercoming head. Although partial breech extraction may be necessary in some instances, the advisability of waiting until spontaneous delivery of the body up to the shoulder blades has been accomplished cannot be overemphasized. External version can result in up to 70% reduction in the incidence of breech presentation at term. It was successful in 68% of the cases, and all of these presented in labor subsequently with vertex presentations. Nulliparity, maternal obesity, engagement of the breech, and uterine anomaly tended to reduce the success rate of external version. In the control group, only 18% of the presenting breeches converted to vertex beyond week 37 of the pregnancy. Transient fetal heart rate decelerations were noted during version in 36% of the attempts (24% of successes and 63% of failures). External cephalic version is less successful in cases of frank breech, where the splinting action of the extended fetal legs makes version difficult to perform. Other complications of external version include fetal distress; twisting, knotting, or laceration of the cord; placental separation; uterine rupture; premature labor; premature rupture of the membranes; and spinal cord transection in utero. Parity, sufficient amniotic fluid, and unengaged presenting part are conducive to a successful version. It is recommended that the external version procedure be carried out according to a prearranged protocol. The availability of at least one assistant for the performance of the procedure is considered essential. For the performance of external version, the patient should take nothing by mouth for at least 6 hours before the procedure. It is considered advantageous by some to spread fine talc powder over the abdomen in order to facilitate the maneuver. As mentioned earlier, the performance of a nonstress test at the end of the procedure is indicated in order to avoid overlooking fetal distress resulting from the version. After the exact position of the fetus has been established by ultrasound, the physician performing the procedure positions himself/herself in such a manner that he/she faces the fetus. The procedure itself begins with the operator lifting out the presenting breech from the pelvis and elevating it as high as possible without the use of undue force.
Order septra with visa
Improved clinician experience and knowledge treatment 12mm kidney stone cheap 480mg septra otc, as well as advancements in infertility management, have also resulted in some novel clinical scenarios. However, if there are apparent problems with the singleton, then keeping the twins is the next best option. Many of these women, for both medical and social reasons, desire a singleton pregnancy. In a series of triplets from the late 1990s, we observed that the average age of patients reducing to twins was 37 years, and to a singleton 41 years. As a reduction to a singleton has become more common, the age difference between those women reducing to twins and those to a singleton has vanished. Not unexpectedly, there are frequently differences in opinion among couples as to the preferability of twins versus singleton, or even as to the total number desired, which sometimes is greater than twins for one member of the couple. Outcomes have continually improved because of the following reasons: (1) improved understanding of the clinical issues involved; (2) decrease in the proportion of extremely higher-order multiples. The most notable shift has been the movement from questions of mortality to questions 90 Fetal reduction and selective termination of morbidity. This appears to be linked to an increase in the age of patients undergoing fertility treatments and a decrease in the number of presenting fetuses. Currently, with decreasing starting numbers, improved ultrasound visualization, enhanced understanding of zygosity, and a select cohort of experienced practitioners accounting for a high proportion of reductions performed, preterm deliveries are decreased to about 4%. Actually, there are two parallel but independent trends: fewer lower- and middle-class teenage mothers delivering (and having terminations) and more women postponing childbearing for a wide variety of reasons to their thirties and forties. The latter is, of course, the 35 30 25 20 15 10 5 0 Quints Quads Before group that mostly applies to our discussion here. As a consequence of the shift to older patients, many of whom already had previous relationships and children, there is an increased desire by these patients to have only one additional child. In the 1980s, most of our procedures were performed between 9 and 10 weeks with decisions based principally on basic ultrasound and fetal position. Waiting for a full karyotype has been problematic because of the long time interval to get the results, as well as the fact that there may be a 1% error rate in matching incorrectly the karyotype results with the corresponding fetus. Occasionally, fetal abnormalities are found for the first time even in the third trimester, which poses medical, ethical, and legal issues. We recently published that in pregnancies with ultrasonographically normal fetuses, 3. This may be more practical for patients reducing twins to a singleton who live locally but it may be less Introduction 93 practical for higher-order numbers and patients traveling from too far. We have observed a number of instances in which errors have occurred resulting in babies born with conditions for which screening had been performed. In the vast majority of cases, the major determining factor in deciding which fetus or fetuses to reduce is based on chromosomal risk. Recently, we evaluated a couple with triplets who were both cystic fibrosis carriers. Using appropriate probes, we were able to determine that two of the fetuses were carriers, and one was affected, which was subsequently reduced. Historically, we perceived a significant bias among those patients who were interested and who mostly expressed a preference for males. Because of such bias, we refused to let gender be a factor with the rare exception of genetic diseases with gender discordancy. Of course, in X-linked disorders, the males are at risk, thus making females the safer option. Over the past 15 years, however, we noticed a shift to requests coming from all ethnic groups and a perceived equalization of gender preferences. In the early 2000s, our ethics consultant, John Fletcher, PhD, encouraged us to consider, and we have adopted, the following approach. First, a detailed ultrasound examination is performed in search for a fetus with a "potential problem. Patients are told that there will be a nongender disclosing "poker faced" discussion when the results are obtained. For patients reducing to twins, the overwhelming preference is for one of each; for those reducing to a singleton, it is essentially a 50/50 split (Table 8. In the past few years, we have seen several gay male couples, using surrogate carriers with egg donation, when both partners fertilized the eggs. Our older data suggested that after 16 weeks, the loss rate of the survivor was increased, but our experience now shows even after 20 weeks, the outcomes of the normal twin are generally improved by reduction of the abnormal twin. It is usually not possible to determine prospectively the risk of damage to the remaining twin. Even so, there always is the possibility of some vascular connection between the two. The primary focus of research and care continues to be on the advancement of fertilization strategies and techniques that offer greater control in lowering the probabilities of such higher-order multifetal pregnancies. However, in our view, the proportion of patients desiring reduction from twins to singleton will steadily increase over the next several years, and this option may be presented to all patients. With a gradual decrease in starting fetal numbers, the emphasis has somewhat shifted to the prevention of serious morbidity, i. The efficacy of reduction for triplets or more has long been accepted by all but the most conservative of commentators. The medical data now also show that the reduction of twins to a singleton improves outcomes. Selective first trimester termination in octuplet and quadruplet pregnancies: Clinical and ethical issues. Technology in American Health Care: Policy Direction for Effective Evaluation and Management. Effect of age on decisions about the number of embryos to transfer in assisted conception: A prospective study. Neonatal encephalopathy and cerebral palsy: Defining the pathogenesis and pathophysiology. The cost of prematurity: Hospital charges at birth and frequency of rehospitalizations and acute care visits over the first year of life: A comparison by gestational age and birth weight. Neurologic and developmental disability at six years of age after extremely preterm birth. Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low birth weights in the 1990s. Multifetal pregnancy reduction by transvaginal puncture: Evaluation of the technique used in 134 cases. Attitudes on the ethics of abortion, sex selection & selective termination among health care professionals, ethicists & clergy likely to encounter such situations. Risk factors for adverse outcomes in spontaneous versus assisted conception in twin pregnancies. Obstetric and neonatal risk of pregnancies after assisted reproductive technology: A matched control study. Perinatal outcomes of in vitro fertilization twins: A systematic review and meta analysis. Triplets: Outcomes of expectant management versus multifetal reduction for 127 pregnancies. A comparative study of multifetal pregnancy reduction from triplets to twins in the first versus early second trimesters 96 Fetal reduction and selective termination 35. Conjoined twins in a triplet pregnancy: Early prenatal diagnosis with three-dimensional ultrasound and review of the literature. The multiple gestation epidemic: the role of the assisted reproductive technologies. Infertility patients and their partners: Differences in the desire for twin gestations. Prenatal diagnosis in twin gestations: A comparison between second-trimester amniocentesis and first-trimester chorionic villus sampling.
Diseases
- Macular degeneration, polymorphic
- Congenital cystic adenomatoid malformation
- Mohr syndrome
- Sonoda syndrome
- Neuroma biliary tract
- Malignant hyperthermia susceptibility type 4
Buy generic septra 480mg
Head deviation in progressive supranuclear palsy: enhanced vestibulo-collic reflex or loss of resetting head movements Voluntary medicine shoppe buy 480mg septra mastercard, spontaneous and reflex blinking in patients with clinically probable progressive supranuclear palsy. Clinical analysis of blepharospasm and apraxia of eyelid opening in patients with parkinsonism. Progressive supranuclear palsy affects both the substantia nigra pars compacta and reticulata. Pathological overlap in cases of parkinsonism associated with neurofibrillary tangles. A study of recent cases of postencephalitic parkinsonism and comparison with progressive supranuclear palsy and Guamanian parkinsonism-dementia complex. Neurodegenerative disorders with extensive tau pathology: a comparative study and review. Pathological inclusion bodies in tauopathies contain distinct complements of tau with three or four microtubule-binding repeat domains as demonstrated by new specific monoclonal antibodies. Evidence of a founder effect in families with frontotemporal dementia that Harbor the tau+16 splice mutation. Mutation in the tau exon 10 splice site region in familiar frontotemporal dementia. Cholinergic imaging in corticobasal syndrome, progressive supranuclear palsy and frontotemporal dementia. Incidence of progressive supranuclear palsy and multiple system atrophy in Olmsted County, Minnesota, 1976 to 1990. Population based mortality and quality of death certification in progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome). Pure akinesia with gait freezing: a third clinical phenotype of progressive supranuclear palsy. Autopsy-proven progressive supranuclear palsy presenting as behavioral variant frontotemporal dementia. Atypical progressive supranuclear palsy underlying progressive apraxia of speech and nonfluent aphasia. Clinical and neuropathologic features of progressive supranuclear palsy with severe pallido-nigroluysial degeneration and axonal dystrophy. Developing therapeutic approaches to tau, selected kinases, and related neuronal protein targets. Differential regulation of microtubule dynamics by three- and four-repeat tau: implications for the onset of neurodegenerative disease. Expression of separate isoforms of human tau protein: correlation with the tau pattern in brain and effects on tubulin polymerization. The tau gene A0 polymorphism in progressive supranuclear palsy and related neurodegenerative diseases. Association of an extended haplotype in the tau gene with progressive supranuclear palsy. Stefansson H, Helgason A, Thorleifsson G, Steinthorsdottir V, Masson G, Barnard J, et al. The distribution and most recent common ancestor of the 17q21 inversion in humans. Linkage disequilibrium fine mapping and haplotype association analysis of the 81 94. Linkage disequilibrium fine-mapping and haplotype association analysis of the tau gene in progressive supranuclear palsy and corticobasal degeneration. Identification of common variants influencing risk of the tauopathy progressive supranuclear palsy. The Search for a Cause: An Anthropological Perspective of a Neurological Disease in Guam, Micronesia. European journal of neurology: the official journal of the European Federation of Neurological Societies. Randomized placebo-controlled trial of sodium valproate in progressive supranuclear palsy. Davunetide in patients with progressive supranuclear palsy: a randomised, doubleblind, placebo-controlled phase 2/3 trial. Mitochondrial dysfunction in cybrid lines expressing mitochondrial genes from patients with progressive supranuclear palsy. Short-term effects of coenzyme Q10 in progressive supranuclear palsy: a randomized, placebo-controlled trial. A clinicopathological study of vascular progressive supranuclear palsy: a multi-infarct disorder presenting as progressive supranuclear palsy. Retrospective study of drug response in 87 patients with progressive supranuclear palsy. Neurotherapeutics: the journal of the American Society for Experimental NeuroTherapeutics. Inhibition of glycogen synthase kinase-3 by lithium correlates with reduced tauopathy and degeneration in vivo. The current diagnostic criteria are those from a 2005 consensus conference [1] (Table 9. Either in clinical or research settings, it is not always possible to identify clearly the time of onset of one symptom. Higher prevalence has been reported in studies conducted in Europe compared to Japan [9], including a prevalence among dementia patients of 30. Incidence increased with age and was higher in men than in women, especially after 60 years of age [13]. The frequency of Lewy body pathology at autopsy may be considerably higher than the prevalence of the clinical disorder the Honolulu Study of Aging, which is a population-based study, showed that about 12. Thus, Lewy body pathology may exist in an asymptomatic or preclinical form, but the lag between the appearance of preclinical Lewy body pathology and the eventual appearance of clinical manifestations is not known. Executive dysfunction and visuospatial dysfunction are the most prominent cognitive deficits, with impairments in learning and short-term memory loss more variable [17, 18]. Cognitive fluctuations may be recurrent with pronounced variations in alertness and attention; however, they may not always be present [1]. Cognitive fluctuations represent the intersection of the disorder of the control of attention and concentration with the disorder of maintenance of wakefulness. Visual hallucinations are far more common than auditory ones, although the latter occasionally occur. Other psychiatric symptoms such as delusions and depression may also be present in the disease [24]. For some patients, the tendency to wish to sleep up to 20 hours per day is the major determinant of impaired quality of life in the disease. It is encoded by a gene on chromosome 4 [1] and seems to be localized specifically in presynaptic terminals [34]. The function of -synuclein is not totally understood; however, it seems to play a role in synaptic vesicle production. When aggregated it is insoluble, depositing in the brain and becoming the main component of the fibrils constituting Lewy bodies [35]. The mechanism underlying the dysregulation of -synuclein and the subsequent development of Lewy bodies is still unknown. It is also possible that the presence of Lewy bodies in the brain is a normal response of the neurons to toxic fibrils that have been formed by dysfunctional proteosomes [24]. The common locations for Lewy bodies and Lewy neurites are the brainstem (substantia nigra and locus coeruleus), limbic structures and basal forebrain (amygdala, nucleus basalis, transentorhinal cortex, and cingulate gyrus), and neocortex (frontal, temporal, and parietal). However, the early appearance of dementia seems to suggest that cortical involvement might sometimes occur earlier than the Braak staging system would predict. There have been variable reports on the relationship of the number of Lewy bodies to the severity of clinical symptoms, some reporting weak relationships [38, 39] and others a stronger one [40, 41]. The presence of Lewy bodies in the temporal lobes is related to the generation of complex hallucinations [42]. Ultimately, synaptic loss and not Lewy bodies is the key correlate of cognitive impairment [43]. The number of the neurofibrillary tangles correlates with the clinical features to some extent.
Order 480 mg septra
Percutaneous fetoscopic patch closure of human spina bifida aperta: Advances in fetal surgical closure techniques may obviate the need for early postnatal neurosurgical intervention treatment spinal stenosis order septra 480 mg line. Elective cesarean delivery and long-term motor function or ambulation status in infants with meningomyelocele. First-trimester cystic hygroma: Relationship of nuchal translucency thickness and outcomes. Technical aspects and effectiveness of percutaneous fetal therapies for large sacrococcygeal teratomas: Cohort study and a literature review. A systematic, yet empathetic approach to the diagnosis, evaluation, and management, regardless of gestational age, is crucial. In the United States, stillbirth affects 1 in 160 pregnancies, resulting in 26,000 stillbirths annually. Most states report fetal deaths at 20 weeks or greater if gestational age is known or a birth weight greater than or equal to 350 g if the gestational age is unknown. However, racial disparity is evident, with the fetal mortality rate in non-Hispanic white women being 4. Other sonographic signs include absent fetal motion, abnormal head shape due to overlapping skull bones, and reduced or absent amniotic fluid. Prior to obtaining ultrasound confirmation, stillbirth may be suspected from a variety of clinical signs and symptoms. These include decreased or absent fetal movements, decreased fundal height, vaginal bleeding, inability to auscultate the fetal heart by transabdominal Doppler, and possibly elevated maternal serum -fetoprotein. There is a "stillness" within the uterine cavity, with no motion other than the pulsation of the maternal aorta. After confirming the absence of cardiac activity, it is important that the mother be included in confirming the diagnosis of stillbirth. She should be allowed to visualize the screen after localizing the fetal heart with the ultrasound transducer kept still so as not to create motion artificially. This helps to eliminate the doubt surrounding the diagnosis and to reduce subsequent denial. Often, women are immediately asked when the last time fetal movement was experienced. This question is likely to elicit strong feelings of guilt that she did not seek medical attention in a timely fashion and does little to assist the medical team in making a diagnosis; it should be avoided, if possible. First, it aids the parents in understanding what led to the demise of their fetus, and in doing so often alleviates selfimposed guilt. Second, if the cause of death is found, the parents may be counseled appropriately as to the recurrence risks of the specific condition. Third, for conditions which may recur, subsequent pregnancies may be managed with closer fetal surveillance and possible therapeutic interventions. Because the causes of stillbirth are many, a systematic diagnostic approach addressing potential maternal, fetal, and placental factors is most beneficial (Table 17. This tool spanned six categories, including maternal medical conditions; obstetric complications; maternal or fetal hematologic conditions; fetal genetic, structural, and karyotypic abnormalities; placental infection, fetal infection, or both; and placental pathological findings. The purpose of this was to identify conditions of interest that might be a potential cause of stillbirth. These conditions can then be further classified into "probable cause of death" or "possible cause of death. For example, the presence of histologic chorioamnionitis alone is not a possible cause of death unless there is documented funisitis. Maternal A careful maternal history and physical examination is part of the diagnostic evaluation of fetal death. Women should be asked about underlying medical conditions, obstetric history, current pregnancy history, medication or substance use, potentially infectious exposures, trauma, and family history. It is extremely important to question the mother carefully so as not to induce blame. The approximate gestational age at which death occurred can be estimated by fetal long bone. While the calvarium and intracranial anatomy are assessed, the biparietal diameter is not used to date the age at death, since soon after death the head becomes quite compressible, resulting in underestimation of the gestational age. The long bones, on the other hand, will remain relatively unchanged for several weeks. Congenital anomalies and the presence of hydrops should be sought in all cases of stillbirth. However, care should be exercised not to confuse postmortem ultrasound findings. Since chromosomal abnormalities are significant causes of stillbirth at all gestational ages, chromosomal analysis with karyotype and microarray is indicated. This 224 Evaluation and management of stillbirth information is best obtained by amniocentesis or chorionic villus sampling at the time of diagnosis. For this reason, viable tissue may not be available at birth for cytogenetic analysis. On the other hand, fetal cells floating in the amniotic fluid may survive for days after fetal death,11 making amniocentesis the preferred method of obtaining a specimen for cytogenetic analysis. If amniocentesis is not performed, other acceptable specimens for cytogenetic analysis include a placental block from below the umbilical cord insertion site, a segment of umbilical cord, or internal fetal tissue (costochondral junction or patella). If the fetus is delivered intact, photographs and radiographs should be taken and kept on file, particularly if unusual or dysmorphic features are found. Once the benefits of such an examination are pointed out to them, consent can usually be obtained. Even when a fetal anomaly has been identified by ultrasound, autopsy has been shown to add information affecting the risk of recurrence in 27% of cases. Postmortem fetal magnetic resonance imaging is also a feasible adjunct in cases of maternal refusal to conventional autopsy, particularly in diagnosing intracranial anomalies. The placenta may be abnormally thickened in cases of erythroblastosis fetalis and certain infections. A retroplacental clot, increased placental thickness, subchorionic hematoma, or intra-amniotic blood may be visualized in cases of abruption. After delivery, placental cultures for aerobic and anaerobic bacteria, Listeria monocytogenes, and ureaplasma and mycoplasma may be sent. The placenta should always be examined histologically for evidence of thrombi, infarcts, inflammation, villitis, parasitic infestation, etc. Gross examination of the umbilical cord and placenta can identify circumvallate placentation, velamentous cord insertions, abnormal twisting, and/or thrombosis of the umbilical cord. For example, the presence of a nuchal cord alone is not a probable cause of stillbirth unless there is evidence of umbilical cord occlusion or fetal hypoxia. Stillbirth in multiple gestations Death of one fetus in a multiple gestation deserves special attention. Although the exact incidence of this event is unknown, it complicates approximately 0. Outcome is influenced by gestational age at the time of the demise and by chorionicity. First-trimester fetal demise does not appear to adversely affect the outcome of the surviving twin. In addition, monochorionic gestations are at risk of multiorgan ischemic damage, multicystic encephalomalacia, and neurologic sequelae in the surviving cotwin. Since the timing of this insult is most likely at the time of the demise, immediate delivery has not been shown to alter outcomes. Attempts should be made to determine chorionicity, as this determines the risk to the surviving fetus. Both twins should be examined for the presence of structural abnormalities, and karyotyping of both fetuses by amniocentesis should be considered. At previable gestations, both expectant management and pregnancy termination are options.
Effective 480 mg septra
Chorionic mosaicism: Association with fetal loss but not with adverse perinatal outcome symptoms gluten intolerance order septra cheap online. Risk of fetal mosaicism when placental mosaicism is diagnosed by chorionic villus sampling. A comparison of chorionic villi sampling and amniocentesis: Acceptability of procedure and maternal attachment to pregnancy. Over a century ago, initial reports of extracting amniotic fluid from the gravid uterus appeared for the treatment of polyhydramnios. Amniocentesis was performed in the 1930s to identify the placental location and for the purpose of pregnancy termination by the instillations of dye and hypertonic saline, respectively. However, the utility of this genetic test has evolved with the result of novel screening algorithms and with the advent of noninvasive screening technologies. Amniocentesis is a safe and accurate procedure and can be selectively performed by the clinician to identify conditions after collecting amniocytes. Midtrimester amniocentesis continues to be the most common procedure performed in invasive prenatal diagnosis. If a structural fetal anomaly is identified on ultrasound evaluation, further invasive diagnostic testing and genetic counseling should be offered to the patient. Fetal cells exfoliated from gastrointestinal and urogenital tracts, from the skin, and from the amnion are used for genetic analysis. Amniocentesis performed at this gestational age yields greater than 99% diagnostic accuracy. Due to the significant recent advances in ultrasound visualization and laboratory techniques, efforts have been made to shift prenatal diagnosis into the first trimester of pregnancy to provide parents with an earlier diagnosis. It usually is indicated at various late gestational ages depending on the maternal, fetal, and obstetric conditions that are involved. A variety Technique of amniocentesis 57 of diagnostic laboratory tests are available to determine the relative concentrations of the surfactant-active phospholipids. Some clinicians, in contrast, utilize the presence of phosphatidylglycerol in amniotic fluid as the definitive test to ensure fetal pulmonary maturity. A myriad of other tests, including the foam stability, lamellar body counting, surfactant-to-albumin ratio, and infrared spectroscopy tests, may also be performed by various reference laboratories on amniotic fluids obtained by amniocentesis. Since the widespread availability of rhesus immunoglobulin (RhoGam), the prevalence of this condition has substantially decreased to one to six cases per 1000 live births. Invasive diagnostic technologies, such as amniocentesis, have been regularly used historically in the management of pregnancies complicated by alloimmunization. However, with the advent of noninvasive ultrasound technology, an indirect methodology for evaluation for fetal well-being can be ascertained with evaluation of the fetal middle cerebral peak-systolic velocity Doppler waveforms. In situations where the appropriate ultrasound expertise for noninvasive evaluation for fetal anemia is available, amniocentesis with spectophotometric examination of the amniotic fluid can be used to assess for fetal anemia. Since most amniocenteses are performed for genetic reasons today, such counseling is best done by a genetic counselor. This time will also allow for a discussion regarding the risks and benefits involved in the amniocentesis procedure itself. An ultrasound evaluation should also be performed prior to the procedure to document the viability, number, complete fetal anatomic survey, gestational age, and position of the fetus(es) and to identify the placental location. Only clinicians familiar with its indications and technique should perform amniocentesis. Thus, transabdominal amniocentesis is the approach of choice for this prenatal diagnostic technique. Initially, transabdominal amniocentesis was performed without ultrasound guidance. The possibility of continuous ultrasound guidance during amniocentesis was first reported in the early 1980s. Continuously monitored amniocentesis resulted in a lower number of dry and bloody taps of the first needle insertion, a decrease in the number of patients requiring multiple attempts, and a reduction in the number of spontaneous losses following the procedure. Sterile gel can then be applied to the abdomen for improved sonographic visualization of the intrauterine environment. After the initial ultrasonic evaluation, the obstetrician locates an appropriate site for the needle insertion. Some would argue that this is an unnecessary step because the site of the initial needle insertion may change if the fetus moves; therefore, the anesthetic would have to be applied to another site. In addition, this may actually increase patient discomfort because an extra skin puncture would be required. We prefer to use a 22-gauge needle to minimize maternal discomfort and maintain uterine quiescence if possible. However, some clinicians prefer a 20-gauge spinal needle to the 22-gauge because of the decreased resistance to amniotic fluid flow, increased resistance to bending, and more echogenic visibility of the tip on realtime ultrasound. Needle guidance can adequately be performed with a linear or curvilinear transducer, and great care must be taken to ensure that the echogenic needle tip is always visualized by the clinician, and does not go outside the beam of the ultrasound. In addition, minimal pressure should be applied to the transducer so as not to distort the spatial relationship between the maternal abdomen and uterine cavity. After meticulous asepsis of the maternal abdomen is completed and the puncture site has been selected after ultrasonic evaluation, the spinal needle is introduced into the maternal skin. After dermal and uterine penetration, the amniotic sac is perforated, with a characteristic "pop" or loss of resistance being perceived by the obstetrician. During this time, careful attention is paid to continuous visualization of the needle tip. Upon confirmation of appropriate entry into the amniotic cavity, the needle stylet should be removed. Maternal cell contamination is much more pronounced in women with anterior placentas than in posterior placentation. Some investigators have evaluated different techniques of amniocentesis and their impact on maternal cell contamination; one study found no difference between amniocentesis technique and maternal cell contamination. This "dry tap" is not uncommon in early gestation and may result from a tenting of the membranes. The first technique involved withdrawing the needle tip back into the myometrium and reinserting it with a forceful thrust. The amount of amniotic fluid to be aspirated depends on the indication for the procedure. If large quantities of amniotic fluid are being removed in cases of polyhydramnios to alleviate maternal symptoms, a gravitational drainage system, multiple syringe aspirations, or a negative-pressure vacuum bottle aspiration system can be used safely to remove amniotic fluid at a rate of 89 mL/minute. After obtaining the appropriate volume of amniotic fluid, the stylet should be reinserted and the needle removed under continuous ultrasound visualization. If no fluid is obtained after more than two attempts, the patient should be offered the opportunity to repeat the procedure after 1 week. Fetal cardiac activity should be verified after the completion of the amniocentesis, whether successful or not. The patient can be discharged after the appropriate postprocedural counseling is completed and the results of the indirect Coombs test are confirmed. The clinician can instill 1 mL of a dilute indigo carmine dye solution (1 mL indigo carmine/9 mL normal saline) into the first gestational sac after amniotic fluid has been removed. In this manner, with sampling of the second sac, the amniotic fluid should be clear and colorless. Methylene blue dye is contraindicated for this purpose because of the potential for fetal hemolysis. This technique usually requires two different skin puncture wounds under continuous ultrasound guidance.
Generic septra 480 mg visa
Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term symptoms quitting smoking purchase septra with a visa. Peripartum complications with cesarean delivery: A review of Maternal-Fetal Medicine Units Network publications. Practices to reduce surgical site infections among women undergoing cesarean section: A review. Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections. Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section. Different classes of antibiotics given to women routinely for prevention infection at cesarean section. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Impact of extendedspectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Timing of intravenous prophylactic antibiotics for preventing pospartum infectious morbidity in women undergoing cesarean delivery. Antibiotic prophylaxis for thirdand fourth-degree perineal tear during vaginal birth. Antibiotic prophylaxis for prevention of postpartum perineal wound complications: A randomized controlled trial. Prophylactic antibiotics for manual removal of retained placenta in vaginal birth. The frequency and complication rates of hysterectomy accopanying cesarean delivery. Emergency peripartum hysterectomy: Incidence, indications, risk factors and outcome. The effect of maternal obesity on outcomes in patient undergoing tertiary or higher cesarean delivery. Effects of maternal obesity on tissue concentrations of prophylactic cefazolin during cesarean delivery. Plasma and tissue cefazolin concentrations in obese patients undergoing cesarean delivery and receiving differing 100. Suture closure of subcutaneous fatand wound disruptionafter cesarean delivery: A meta-analysis. Role of subcutaneous closure in preventing wound complications after cesarean delivery with Pfannestiel incision: A randomized clinical trial. Subcutaneous tissue, reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Prophylactic subcutaneous drainage for prevention of wound complications after cesarean delivery-A meta-analysis. In a subsequent pregnancy, complications can occur during the antenatal period such as bleeding from a placenta previa and/or abnormally adherent placenta or even uterine rupture. Regardless of the gestational age many of these complications can be catastrophic for both mother and neonate. Notwithstanding this argument in the literature one can find terms such as "cesarean ectopic," "cesarean section ectopic pregnancy," and others. A niche is defined as an anechoic defect in the anterior low myometrium in the area of the prior incision. It is usually referred to as a dehiscence mainly when there is a large and total defect without covering myometrium. The typical sonographic appearance of the niche is that of a triangle with the apex pointing toward the myometrial/bladder interphase. Several descriptions for large niches have been used such as "the niche penetrating to a depth of at least 50% or 80% of the anterior myometrium," or "the remaining myometrial thickness is 2. The shape of the niches or dehiscence can vary from triangular, round, or oval, at times it may be extensive and reaching the anterior uterine wall or the area below the bladder in the shape of a fistulous connection between the uterine cavity and the uterine surface. Since the prevalence of niches is relatively high one can speculate that the possibility of the blastocyst implanting in or on the niche is all too realistic. A line is drawn from an opening in the center of the ectocervix (external cervical os) to the external surface of the uterine fundus. The sensitivity, specificity, and positive and negative predictive values for the cervix-to-sac-center in the study were 93%, 98. In a cervical pregnancy, the placenta and the entire gestational sac containing an embryo/fetus are present centrally within the endocervical canal below the level of the internal os. The cervical canal and the cervix are dilated and barrel-shaped while the uterine cavity is empty. Nonetheless, it can provide information regarding the precise location of the gestational sac, its vascularity, and the volume of the gestational sac. These quantitative blood flow measurements can be used to serially monitor the healing process of treated cases. There were numerous articles discussing severe bleeding, shock, uterine rupture, and hysterectomies in patient reaching only the second trimester. Based upon the above severe complications and dismal outcomes patients were counseled almost exclusively for termination of the pregnancy to avoid life-threatening complications resulting from the abnormal implantation into the scar. There is typically an urgency to terminate the pregnancy as soon as the decision to terminate is reached. The reason is that as the pregnancy is allowed to grow larger and further in gestation, it may cause more complications at the time of the treatment (Table 32. In addition, with deeper placental invasion, there is progressive and faulty invasion of the placenta into the scar, resulting in an abnormal and at times deeply invading placentation, typically referred to as placenta accreta. Ten of the twelve nonviable pregnancies were treated with conservative management and all resolved without any severe and long-lasting complications. Ten patients elected to continue the pregnancy, of which five had significant second-trimester complications, three had uterine rupture, one had uterine dehiscence and bulging membranes, and all five eventually needing a hysterectomy. However, 3 of the 10 patients who continued the pregnancy delivered a viable baby by elective cesarean section, but all three had a hysterectomy. All 33 (100%) cases managed with transvaginally guided local intragestational sac injection resolved without the need for hysterectomy. Among the 10 patients that opted to continue the pregnancy 4 (40%) delivered a viable neonate and 5 (50%) had second-trimester complications resulting in hysterectomy. One of the patients had a gravid hysterectomy due to second-trimester complications (cervical shortening and severe bleeding); pathology confirmed placenta percreta in this case. All nine patients underwent hysterectomy for an abnormally adherent placenta and the pathology confirmed placenta percreta in all nine cases. However, after extensive counseling patients decide to continue the pregnancy and there is growing evidence that under certain circumstances and precautions taken this is possible. The gestational sac with a live embryo and yolk sac at 6 5/7 weeks is seen anterior in close proximity to the bladder (arrow). The gestational and yolk sac are seen "tucked" in the niche and in very close proximity to the bladder (b). Histology of the uteri in nearly all of the above cases confirmed the presence of the adherent placenta. In the literature there are numerous treatment options, some of which are associated with significant rates of complications (Table 32. Complications were defined first and foremost as the immediate or delayed need for a secondary treatment. Other most common indications for the secondary treatments were failure to stop the heart rate by a primary treatment, blood loss requiring transfusion of greater than 200 mL, shock, and hemoperitoneum. Secondary treatments included surgical interventions such as laparoscopy, hysteroscopy, laparotomy, hysterectomy, or procedures that required general or regional anesthesia or embolization of the uterine arteries. Among all of the treatment modalities, three were identified to have the largest complications rates: dilation and curettage (D&C) alone or in combination with any other treatment had a complication rate of 61. Using color flow Doppler the vascularity of the placenta is seen in the area of the prior scar in very close proximity to the bladder (long arrow).