Safe viagra gold 800 mg
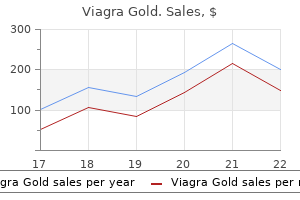
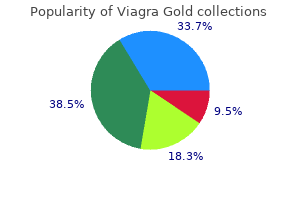
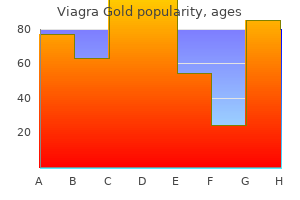
The posterior tibial artery passes downward on the back of the leg erectile dysfunction doctor nj 800 mg viagra gold overnight delivery, reaching the foot, and passes in the back of the medial malleolus. Circumflex Fibular Artery the circumflex fibular artery may arise from the anterior tibial artery. Medial Plantar Artery It is the smaller terminal plantar branch of the posterior artery. It passes along the base of the first metatarsal bone and the medial border of the first toe, anastomosing with a branch of the first metatarsal artery. This artery supplies three small superficial digital branches, joining the first, second, and third plantar arteries. Branches Muscular branches Nutrient artery of the fibula Perforating branch (through interosseous membrane) Arises 5 cm above the lateral malleolus. Communicating branch (anastomoses with the communicating branch of the posterior tibial artery). Calcaneal (terminal) branches (communicates with the calcaneal branches of the posterior tibial artery, and anterior lateral malleolar artery) Lateral Plantar Artery this artery is the largest terminal plantar branch of the posterior tibial artery. It runs lateral and distal to the base of the fifth metatarsal bone and turns medially to the area between the base of the first and second metatarsal bones, connecting with the distal aspect of the dorsal artery of the foot, completing the plantar arch. Branches Muscular branches Superficial branches Anastomotic branches-to the lateral tarsal and arcuate arteries Calcaneal branch-occasionally present Nutrient Artery of the Tibia the nutrient artery of the tibia is one of the largest nutrient arteries in the body and arises from the proximal posterior tibial artery. Plantar Arch Branches Three perforating branches Anastomoses with the dorsal metacarpal arteries Four plantar metatarsal arteries Each divides into two plantar digital arteries: distal perforating branch joining the dorsal metatarsal artery; first plantar metatarsal artery springs from the junction of the lateral plantar and dorsal artery of the foot; the digital branch for the lateral side of the fifth toe arises from the lateral plantar artery Muscular Branches these branches provide nutrition to the muscles in the back of the leg. Communicating Branch the communicating branch is the transverse artery in the back of the tibia and anastomoses with the communicating branch of the peroneal artery. Medial Malleolar Branches the medial malleolar branches are part of the malleolar network. Variations in the Arteries of the Foot There are about six variations described for the plantar arteries of the foot. Schematic drawing demonstrating the vascular and nerve structures passing under the inguinal ligament. B, Late phase of the femoral arteriography showing the companion veins of the femoral artery and branches. Note the three layers of the arterial wall; the most internal hyper-echoic, a middle layer hypo-echoic, and an external hyper-echoic layer fusing with the surrounding tissues. Schematic drawing of the popliteal artery and knee branches, including the genicular anastomotic network. Note that the circumflex fibular artery supplies a hypervascular lesion in the popliteal fossa. Anterior view of a bilateral angiogram of the popliteal arteries and main branches. A, Anterior view of an occluded popliteal artery with the prominent sural arteries. B, Lateral view of the occluded popliteal artery showing the prominent sural arteries. Anterior view of an angiogram of both popliteal arteries showing the main branches. Anterior view of an angiogram of an occluded left popliteal artery showing the prominent genicular arteries and anastomotic branches. Anterior view of a popliteal artery trifurcation showing the origins of the anterior tibial artery, posterior tibial artery, and peroneal artery. Free-standing specula may require a seventh nerve block to reduce the blepharospasm. If the nature of the offending agent is unknown or in question, use prolonged irrigation. Consult ophthalmology for all alkaline, hydrofluoric acid, and heavy metal acid injuries. Irrigation on an inpatient basis may be required for a period of 24 hours or longer, especially when the cornea is hazy or obviously thickened. Note that the magnesium contained in sparklers combines with water from tears to produce magnesium hydroxide. Treat eye damage from hair straighteners,49 phosphate-free detergents,50 and automobile air bags51 as alkaline injuries also. Measure the pH of the conjunctival fornices with a pH paper strip to check the effectiveness of irrigation. In addition to litmus paper, the pH indicator on urine multi-indicator sticks can be used. The pH indicator on urine dipsticks is conveniently closest to the handle; all the distal indicator squares can be cut off with scissors. If the pH measured in the conjunctival fornices is still abnormal after the initial irrigation, continue to irrigate. If the pH is normal after irrigation, wait 20 minutes and check it again to make sure that it remains normal, especially if alkaline contamination has occurred. Delayed changes in pH are usually the result of incomplete irrigation and inadequate swabbing of the fornices. Consider double-lid eversion with a lid elevator to expose the upper fornix for swabbing, irrigation, and pH testing. Prolonged Irrigation alkaline burns may require prolonged irrigation, and it is essential to consult ophthalmology in such cases. Then place the device carefully on the surface of the eye with the lids closed around the intravenous tubing adaptor. Attach the adaptor to intravenous tubing and provide continuous flow through the device onto the cornea and into the fornices. Complications the only significant complication from irrigation is abrasion of the cornea or the conjunctiva. This can be a mechanical injury from trying to keep the lids open in an uncooperative patient, a small corneal epithelial defect from a Morgan irrigating lens, or fine punctate keratitis from the irrigation itself. Deep or penetrating corneal injuries are likely to be a result of the caustic chemical and require emergency ophthalmologic consultation. Continue to provide slow continuous irrigation pending arrival of the ophthalmologist. Some experimental evidence suggests that massive parenteral or oral ascorbic acid supplementation may prevent the development of deep corneal injury,53 but such treatment has not gained universal acceptance. Summary Eye irrigation is easy, and complications associated with the technique are usually minimal. If any doubt exists, err on the side of irrigating the eye rather than omitting this vital procedure and risking progression of the eye injury. Frequently, the only clue is an abnormal pupil, and the extruded iris may not be appreciated as intraocular tissue. The pupil is irregular (often pear or teardrop shaped) and points toward the laceration. B, a pear-shaped pupil without protrusion of the lens is a more subtle, yet characteristic indication of a perforated globe (arrow). C, another indication of a penetrating globe injury is periorbital fat protruding from an upper eyelid laceration (arrow). Patients with penetrating injuries to the globe should be treated with systemic antibiotics (such as a combination of cefazolin and gentamicin), tetanus toxoid if indicated, and antiemetics to control vomiting (which raises intraocular pressure). Until the ophthalmologist arrives, protect the eye from further harm by keeping the patient quiet, elevating the head of the bed, and placing a protective shield over the eye. When a metal shield is not available, construct a makeshift protective shield with the material available. The protective shield helps avoid pressure on the globe and overlying tissue and assists in preventing extrusion of vitreous and other ocular contents. Extend the edges of the shield up to or beyond the bony orbital rim for this purpose. If a patient has a globe perforation, treat with systemic antibiotics (a combination of cefazolin and gentamicin is a good initial choice), tetanus toxoid, and antiemetics in doses aggressive enough to halt vomiting. That said, if the physical exam obviously suggests open globe pathology, the clinician is discouraged from this procedure, as it carries the risk of vitreous extrusion (even with minimal globe compression) with little benefit to the diagnostic evaluation.
Diseases
- Acute myeloblastic leukemia type 1
- Thrombocytopenia purpura
- Tracheobronchopathia osteoplastica
- Diabetes mellitus type 1
- Native American myopathy
- Richieri Costa Da Silva syndrome
Generic viagra gold 800 mg
The middle capsular artery arises from the renal artery or its main branches at the renal hilum erectile dysfunction books download free viagra gold 800 mg free shipping. The inferior capsular artery is uncommonly observed, but usually arises from the gonadal artery or from an inferior polar artery. There is a number of perforating capsular arteries arising from arcuate and interlobular arteries, connecting the intrarenal circulation with the larger capsular arteries. The perforating capsular arteries are usually small and enlarge only when advanced nephropathy or arterial occlusion is encountered. The pelvic arteries are small and difficult to observe either angiographically or at dissection. When there is renal artery occlusive disease, they may enlarge and may be observed as tortuous small vessels. The ureteric and pelvicoureteric arteries are also small and originate from the main renal artery or from its main branches. At the posterosuperior aspect of the testis, two branches are found on its medial and lateral surfaces, which form the tunica vasculosa after ramifying. The ureter, the perirenal fat and iliac lymph nodes, and the cremaster muscle are arterialized by the testicular artery. The ovarian arteries correspond to the testicular arteries, but follow a different path in the pelvis, to supply the ovaries, reaching the uterine broad ligament. Some branches of the gonadal artery supply the ureters, the uterine tubes, and have anastomoses with the uterine artery. The ovaries are supplied by ovarian arteries in 40% of the cases, by both uterine and ovarian arteries in 56% of cases, and by uterine arteries alone in about 4% of the cases. Dorsal Branches of the Aorta Lumbar Arteries There are usually four lumbar arteries in each side, arising from the posterior aspect of the abdominal aorta. A smaller fifth pair of lumbar arteries may arise from the middle sacral artery, but lumbar branches of the iliolumbar arteries are usually in their place. These arteries follow a posterior path over the lumbar vertebral bodies, continuing in the posterior abdominal wall. Branches Dorsal ramus Spinal branches Muscular branches the dorsal ramus of the lumbar arteries supply the dorsal muscles, joints, and skin. The spinal branches of the dorsal ramus enter the spinal canal to supply its structures and adjacent vertebra. The spinal branch of the first lumbar artery supplies the terminal spinal cord, and the others the cauda equina, meninges, and the vertebral canal. Muscular branches of the dorsal rami supply the adjacent muscles, fascia, bones, red marrow, ligaments, and joints. Testicular and Ovarian Artery the testicular and ovarian arteries arise anterolaterally from the abdominal aorta, a few centimeters below the renal arteries in 80% to 90% of the population. The ovarian or testicular arteries follow a descending path, anterior to the inferior vena cava and parallel to the gonadal vein, anteriorly to the ureter in the right side, and posterior to the left gonadal vein at the beginning, but anterior to the left ureter. Rarely the ovarian or testicular arteries arise from lumbar, adrenal, or iliac arteries. Both testicular arteries pass the deep Median Sacral Artery this is a small posterior branch of the abdominal aorta, arising from the aorta above its bifurcation that descends in the middle line, anterior to the 4th and 5th lumbar vertebra, sacrum, and coccyx. There are anastomoses with the rectum, lumbar branches of the iliolumbar artery, and the lateral sacral arteries. The common iliac arteries divide into the external iliac artery, which courses parallel to the axis of the common iliac artery, and the internal iliac artery, which is a posteromedial branch. In addition to the terminal branches, the common iliac arteries give branches to the surrounding tissues, peritoneum, psoas muscle, ureter and nerves. Occasional branches are the iliolumbar and accessory renal arteries for topic or ectopic kidneys. B, Late-phase aortography showing the bilateral nephrogram and contrast enhancement of the adrenal glands. Magnetic resonance imaging showing the abdominal aorta, the inferior vena cava (partially), and the portal and splenic veins. Schematic drawing of the celiac trunk, showing the hepatic arteries, segments (Couinaud), and the gastric and splenic circulation. A, Selective angiogram of the celiac trunk, showing the hepatic circulation, and the gastric, pancreatic, and splenic circulation. The pattern presented here is the most common and present in about 40% to 50% of the population. B, Late phase of the angiogram showing the splenic and portal veins, as well as the splenic blush and the hepatic blush. Selective angiogram of the celiac trunk, showing absence of the proper hepatic artery due to the trifurcation of the common hepatic artery into the right and left hepatic arteries and the gastroduodenal artery. Selective angiogram of the celiac trunk, showing normal distribution of the hepatic and splenic arteries. A, Selective angiogram of the celiac trunk, showing normal distribution of the arteries. The gastroduodenal artery arises directly from the bifurcation of the celiac trunk. The left gastric artery anastomoses with the right hepatic artery and courses along the lesser curvature of the stomach. Note the filling of the arteries of the fundus of the stomach and the anastomoses with the splenic arteries, as well as filling of the left gastroepiploic artery. B, Later phase of the left gastric artery injection, showing blush at the gastric wall and filling of the drainage veins, especially the left gastric vein. A, Selective injection in the left gastric artery, branch of the celiac trunk showing the gastric branches in the fundus and body of the stomach. The right gastric artery is completely opacified by the angiographic injection and the anastomosis with the hepatic artery is visible. The gastric branches of the right hepatic artery are smaller than the fundic and body branches. B, Late phase of the left gastric artery angiography showing the venous return of the fundic and body veins draining into the left gastric vein and into the portal vein (faintly opacified). Left and right gastric artery arcade, opacified by superselective catheterization and angiography of the left gastric artery. The right gastric artery is densely opacified (arrow heads) and connects with the left hepatic artery (curved arrow). Selective injection at the celiac trunk showing the normal bifurcation, with distal origin of the left gastric artery giving rise to the left hepatic artery. There is no visible dorsal pancreatic artery and the circulation of the body and tail of the pancreas is supplied mainly by the arteria pancreatica magna. Injection at the celiac trunk, showing normal bifurcation, but with an enlarged left gastric artery giving origin to the left hepatic artery. A, Selective injection at the celiac trunk showing a horizontal celiac trunk, with the replaced left hepatic artery arising from the left gastric artery. B, Late phase of the celiac injection showing the patent splenic and portal veins. Celiac injection showing occlusion of the splenic artery and development of the collateral circulation through the left gastric artery, gastric fundus arteries, short gastric arteries and with filling of the splenic artery at the hilum. There is some collateralization through pancreatic arteries on the tail and body of the pancreas, through the dorsal pancreatic artery. Celiac artery angiography showing the normal distribution of the main branches, the pancreatic branches, and the gastric and duodenal branches. Selective injection at the gastroduodenal artery, showing the duodenal and pancreatic head branches. The dorsal pancreatic artery is a branch of the common hepatic artery and is retrograde filled. Selective angiogram of the proper hepatic artery with spasm at the catheter tip (black arrow). Selective angiography at the gastroduodenal artery, showing the pancreaticoduodenal arcades and the anastomosis with the dorsal pancreatic artery and filling of the inferior pancreatic artery. Schematic drawing showing the arterial circulation of the duodenum, stomach, spleen, and greater omentum, as well as the anastomotic collaterals. Selective injection at the celiac trunk with a normal distribution of the branches. Note the dorsal pancreatic artery arising from the bifurcation of the celiac artery and that most of the arterial circulation of the pancreas arises from the dorsal pancreatic artery.
Buy cheap viagra gold 800 mg on-line
Current approaches in the treatment of relapsed and refractory acute myeloid leukemia erectile dysfunction treatment chandigarh generic viagra gold 800 mg fast delivery. Curability of patients with acute myeloid leukemia who did not undergo transplantation in first remission. Colony-stimulating factors for prevention and treatment of infectious complications in patients with acute myelogenous leukemia. Treatment of the pregnant mother with cancer: a systematic review on the use of cytotoxic, endocrine, targeted agents and immunotherapy during pregnancy. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia: time to move toward a minimal residual diseasebased definition of complete remission Modulation of splicing catalysis for therapeutic targeting of leukemia with mutations in genes encoding spliceosomal proteins. There is a slight male predominance, and Caucasians have a twofold increased risk compared with African Americans, while the highest incidence is seen in Hispanic children. Other predisposing conditions include immunodeficiency and chromosomal breakage syndromes, but most often no such underlying disorder is found. Environmental exposure risks have been suggested, but with the exception of ionizing radiation, few have been shown to be causal. Acquired chromosomal abnormalities confined to lymphoblasts are found in more than 90% of cases, including aneuploidy (most commonly hyperdiploidy) and/ or translocations that in some cases are prenatal in origin. There are several life-or organ-threatening presentations that require emergent intervention (Table 12. Routine hematopathologic analysis, immunohistochemistry, flow cytometry, cytogenetics, and molecular studies are used to define the subtype and further identify prognostic factors. Certain cytogenetic abnormalities are not apparent on routine karyotyping, and thus molecular testing may be required, most notably for t(12;21) seen in about 25% of cases in children. Lumbar puncture is required to evaluate the possibility of meningeal leukemia (Table 12. Age is a strong prognostic determinant, and outcome is inferior in infants and adults in comparison to children. Therapy is stratified based on clinicopathologic features, and treatment should be directed by physicians familiar with subtype-specific regimens. The following core recommendations are based on results of large cooperative group clinical trials. Initial induction therapy for children and most adults consists of 3 to 5 drugs given in a 28-day cycle. Various consolidation and intensification regimens are commonly employed, some of which are detailed in Table 12. Multiple consolidation/ intensification blocks are often advised for high-risk patients. These infants should be treated on age-specific protocols with certain agents dosed by weight to decrease the risk of severe toxicity. Improved outcome has been associated with the use of intensified therapy that commonly includes high-dose methotrexate, dexamethasone, and asparaginase. To minimize the risk of meningeal contamination due to traumatic lumbar puncture, spinal taps should be performed by clinicians experienced in the procedure. In addition, intrathecal chemotherapy should always be administered at the time of the initial. Radiation dose should be based on the specific indication and overall treatment regimen. In the event of significant chemotherapy-related toxicity, individual agents should be dosereduced or discontinued as clinically indicated. Individuals with Down syndrome tolerate methotrexate poorly and may require dose reduction of that agent. Importantly, patients with isolated extramedullary relapse also require systemic therapy. Attaining a second remission is critical and often times can be achieved with standard four-or five-drug reinduction regimens (Table 12. Curative salvage using standard chemotherapy and radiation is more likely in the setting of isolated extramedullary relapse. Tumor Lysis Syndrome Rapid blast lysis can result in life-threatening metabolic complications. Tumor lysis syndrome is usually seen within the first few hours to days of initiation of induction chemotherapy. Tumor lysis precautions should be started as soon as possible after diagnosis and at least 6 to 12 hours prior to the start of induction therapy. Prophylaxis and monitoring should continue until disease burden is reduced, peripheral blasts are clear, and it is apparent that no tumor lysis has developed, usually for 3 to 7 days. The following measures are indicated for all patients around initial induction therapy:39 Allopurinol: 100 mg/ m2 per dose orally, three times daily. Urate oxidase (rasburicase) is an effective alternative for management of extreme hyperuricemia, especially in the setting of renal insufficiency. Although alkalinization with sodium bicarbonate added to hydration fluids increases the solubility of uric acid, it enhances calcium-phosphate precipitation in the kidney and should be avoided, especially in the presence of hyperphosphatemia. Frequent serial laboratory monitoring is required during initiation of induction chemotherapy. Transfusions Blood transfusion should be used to prevent complications related to severe cytopenias. To decrease the risk of transfusion-associated complications, specialized products should be used. Irradiation: To reduce the risk of transfusion-associated graft-versus-host disease, all cellular blood products should be irradiated. Infection Prophylaxis Aggressive surveillance, prophylaxis, and treatment for bacterial, fungal, viral, and opportunistic infections are essential to prevent morbidity and mortality. Antifungal therapy should be initiated for neutropenic fever that persists for 5 days. Myeloid growth factor support may be employed in cases of severe fungal infection in an attempt to hasten neutrophil recovery. Chemotherapy Prophylaxis Agent-specific prophylaxis should be utilized as clinically indicated. For example, gastritis prophylaxis may be required during corticosteroid administration. Leucovorin rescue is indicated to prevent severe toxicity after high-dose methotrexate. To reduce the risk of conjunctivitis associated with high-dose Ara-C, corticosteroid or saline ophthalmic solution should be administered during and for 24 to 48 hours after treatment. Mesna should be used to prevent hemorrhagic cystitis associated with highdose ifosfamide and cyclophosphamide. Nutritional Support Nutritional status should be monitored and supplementation provided as indicated. Routine folic acid use should be avoided with methotrexate administration because it may counteract the therapeutic efficacy of folate antagonism. Psychosocial Support Multidisciplinary support for the patient and family is an important part of successful treatment. If indeterminate, repeat every 1 to 2 weeks until recovery to confirm remission or induction failure. Cardiomyopathy: To decrease the risk of cardiotoxicity, cumulative anthracycline doses are usually limited to less than 400 mg/ m2. Echocardiograms for left ventricular function determination should be performed at baseline, at completion of treatment, every 1 to 2 years after treatment until serial studies remain normal, and as clinically indicated. Neurologic toxicity: Children are at especially high risk of neurotoxicity from chemotherapy and radiation. All patients should be monitored for neurologic toxicity including neurodevelopmental dysfunction. Endocrinologic dysfunction: Patients should be monitored for endocrinopathies, including growth retardation, hypothyroidism, and infertility. Osteonecrosis: Corticosteroids, especially dexamethasone, are associated with a high incidence of osteonecrosis. Secondary malignancy: Patients should be monitored for secondary malignancies because these continue to develop even in the second decade after treatment. Acute lymphoblastic leukemia: monitoring minimal residual disease as a therapeutic principle. Should minimal residual disease monitoring in acute lymphoblastic leukemia be standard of care Augmented post-induction therapy for children with high-risk acute lymphoblastic leukemia and a slow response to initial therapy.
Discount viagra gold 800mg mastercard
Concentrations of free carnitine in the blood may be very low erectile dysfunction recovery viagra gold 800mg amex, and the excretion of carnitine esters is high. The development of tandem mass spectrometry and assay of carnitine esters of CoA containing organic acids has led to highly effective programs of expanded neonatal screening. These programs have given, for the first time, reliable data on the prevalence of 3-methylcrotonylCoA carboxylase deficiency. The incidence in the population of North Carolina was reported as one in 52,000 [33]. In Australia, incidences of one in 27,000 [34] and one in 110,000 [35] have been reported. This is another metabolic disease that appears to be common in the Amish-Mennonite populations of the United States [12]. In data from Bavaria, less than 10 percent of patients detected by screening and found to have mutations were found to develop symptoms [37]. In addition, it was concluded that none of the symptoms reported could clearly be attributed to deficiency in this enzyme. This appears to be incompatible with the fact that patients with this disease have been observed who have had clearcut organic acidemia presentations with ketoacidosis [24]. Nevertheless, on the basis of the Bavarian data, infants in Germany are no longer screened for this disease. In general, the levels of C50Hcarnitine tend to be higher in this situation than when they are provided by an affected infant. Elevated C50Hcarnitine is also found in holocarboxylase synthetase (Chapter 6) and in 3-hydroxy-3-methylglutarylCoA lyase deficiency (Chapter 50), as well as in 2-oxothiolase deficiency, where the elevated 2-methyl-2-hydroxybutyrylcarnitine shares the same mass as 3-hydroxyisovaleryl carnitine. A protein-free source of calories, vitamins, and minerals, such as Profree (Ross), may be useful. Carnitine therapy should be given to restore plasma concentrations of free carnitine and to achieve maximum excretion of carnitine esters, within the range of intestinal intolerance. The acute ketoacidotic episode is treated as in classical organic acidemia with large amounts of water and electrolyte containing bicarbonate (Chapter 1) and intravenous carnitine (300 mg/kg). If prolonged parenteral nutrition is required, formulations have been designed that exclude leucine [40]. These can be supplemented with standard parenteral solutions of amino acids, so that total restriction of any individual amino acid is not pursued for more than a few days. Isolated biotin-resistant 3-methylcrotonyl-CoA carboxylase deficiency in two sibs. Isolated biotin-resistant3-methylcrotonyl CoA carboxylase deficiency presenting with life threatening hypoglycemia. Two siblings with biotin-resistant 3-methylcrotonyl-coenzyme A carboxylase deficiency. Isolated 3-methylcrotonyl CoA carboxylase deficiency presenting as a Reye-like syndrome. The molecular basis of 3-methylcrotonylglycinuria, a disorder of leucine catabolism. Isolated biotin-resistant 3-methylcrotonyl-CoA carboxylase presenting as a clinically severe form in a newborn with fatal outcome. Isolated (biotinresistant) 3-methylcrotonyl-CoA carboxylase deficiency: four sibs devoid of pathology. Simultaneous preparation of the three biotin-containing mitochondrial carboxylases from rat liver. Isolated 3-methylcrotonyl-CoA carboxylase deficiency: evidence for an allele-specific dominant negative effect and responsiveness to biotin therapy. Potential misdiagnosis of 3-methylcrotonyl-coenzyme A carboxylase deficiency associated with absent or trace urinary 3-methylcrotonylglycine. Elevation of elevated hydroxyisovalerylcarnitine in the newborn screen by tandem mass spectrometry. The introduction of tandem mass spectrometry in to the South Australian neonatal screening program: benefits and costs. Mutation analyses by Struys and colleagues [9] led to the recognition that mutations in the dehydrogenase gene are found in patients with both mild and severe clinical disease. They refer to type I as those patients who had defective activity of the dehydrogenase enzyme and mutations in the gene. Oddly the other group, type 2 who had neither mutations nor defective activity of the enzyme, had higher levels of D-2-hydroxylglutaric acid in body fluids. Pro45Leu) were reported in siblings who had prominent facial dysmorphic features and lactic acidosis [13]. In 17 patients with the severe phenotype, manifestations were early onset: at 7 months, one [1] could not sit or roll and did not fix or follow; another [3] was cortically blind. Most of the patients classified as severe [4, 5] had little evidence of mental development. Among the patients with milder presentations, mental retardation and hypotonia were the rules, though the younger sister of one patient appeared by three years to have only speech delay, and both sisters were dysmorphic, suggesting the possibility of another etiology for the mental retardation [1]. The clinical phenotype was set out by van der Knaap and associates [4] in an international survey of 25 patients with documented D-2-hydroxyglutaric aciduria. A number of metabolic diseases, particularly organic acidemias that present in the neonatal period may be diagnosed as pyloric stenosis or similar surgical disease (see Appendix). At seven months, the head circumference in one patient at 47 cm was in the fiftieth percentile for 19 months. Macrocephaly was also present in three of the patients classified as mild [5]; and four of the severe patients became microcephalic. Macrocephaly and subdural collections of fluid are also characteristic of glutaric aciduria resulting from glutarylCoA dehydrogenase deficiency (Chapter 9), and these diseases should be considered (Appendix) before a diagnosis of nonaccidental trauma is made. Involuntary movements described have included chorea, dystonic posturing and episodic opisthotonic arching and extensor posturing [1, 3, 5]. Hypotonia has been observed in a number of patients [1, 3, 5], but there may also be hypertonia. Spasticity, increased deep tendon reflexes and positive Babinski responses have been present [1, 5]. Cardiomyopathy was found in a number of the severely affected patients, in some of whom it was clinically symptomatic. One patient had a ventricular septal defect and one had a mild coarctation of the aorta and hypertrophy of the left ventricle. A patient with severe disease displayed respiratory distress and died at 10 months of cardiogenic shock as a result of cardiomyopathy [14]. A variety of dysmorphic features have been noted in patients with this disease, including plagiocephaly, asymmetric ears, transverse palmar creases, epicanthal folds, a frontal upsweep of the hair and coarse features [1]. Facial dysmorphism has been particularly common, including a flat face, a broad nasal bridge and abnormalities of the external ears [15]. A girl with D-2-hydroxyglutaric aciduria had turricephaly, brachycephaly, a broad flat face with course features and a prominent jaw [20].
Globe Trollius (Globe Flower). Viagra Gold.
- Are there safety concerns?
- Dosing considerations for Globe Flower.
- How does Globe Flower work?
- What is Globe Flower?
- Scurvy (vitamin C deficiency) and other uses.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96647
Order viagra gold without prescription
In indolent lymphomas drugs for erectile dysfunction purchase viagra gold 800mg with mastercard, response to therapy may be slower; restaging can be performed less frequently. The rate of response may reflect tumor sensitivity to treatment and may have prognostic value. Biopsy of residual masses after therapy may be required to determine whether viable tumor is present. Response evaluation following novel biologic and immunologic therapeutics is an evolving science and consensus has not yet been reached. Disease-related features include tumor bulk, stage, number of extranodal disease sites, and histologic type and tumor histogenesis (or tumor biology). Patient-related factors include age and performance status, and whether there are comorbid conditions present that may affect the ability to administer therapy. Prognostic assessment and modeling strategies have been developed to predict the outcome based on clinical presentation. Clinical behavior is generally described as indolent, aggressive, or highly aggressive. Conventional treatment now includes chemotherapy, radiotherapy, immunotherapy, or a combination of these modalities. Novel treatments, including immunoconjugates, immune modulators, and molecularly targeted agents are now in everyday practice or the subject of current investigations. Ongoing clinical research refines how newer treatments are used and combined to augment or supplant the current standards of care. Other approaches that may also be used in patients with disease progression include fludarabine (combined with rituximab and or mitoxantrone or cyclophosphamide) and yttrium 90 ibritumomab tiuxetan radioimmunotherapy. Those with the most favorable prognosis may benefit less from early therapy whereas those with poorer prognosis may derive greater benefit from early therapy. If the toxicity of therapy creates symptoms where there are none, watchful waiting may be a better strategy. Maintenance rituximab may prolong remission (at 3 years of median follow-up, duration of remission was 23 vs. In addition, some advocate the use of radioimmunotherapy for initial disease, utilizing 131I-tositumomab. Large retrospective databases indicate that the observational strategy does not compromise survival compared to early intervention. Treatment options include bendamustine, fludarabine, and rituximab, given concurrently or sequentially. There is an interest in thalidomide and analogs, particularly lenalidomide and pomalidomide. Local therapy such as surgery or regional irradiation may yield relatively long-term disease control. Unlike other aggressive lymphomas, it is incurable and has variable reported median survivals in studies ranging from 5 to more than 12 years. In general, patients younger than 60 years are treated differently from older patients. For localized disease, many experts recommend limited cycles of chemotherapy combined with involved field radiotherapy. Salvage therapy following relapse is most effective for those whose disease remains chemotherapy sensitive. Treatment may provoke tumor lysis syndrome and prophylaxis should be used: Alkalinize the urine with D5W plus 100 mEq sodium acetate at 100 to 150 mL/ hr, add allopurinol, 600 mg, orally daily for 2 days, then 300 mg/ day orally until resolution of the tumor lysis syndrome. However, in the rituximab era, those that do relapse following rituximabinclusive therapy appear to be selected for the poorest-prognosis patients, and salvage is less successful in many cases owing to this. High-dose chemotherapy does not appear to overcome tumor resistance in the majority of cases. Graft engineering to enhance graft-versus-lymphoma benefit and to decrease graft-versus-host complications remains an active area of investigation. Studies have not consistently shown strong graft-versus-lymphoma effects in the majority of patients. It is best to once-daily combination pills because they contain pharmacokinetic boosters. Corticosteroids, alkylating agents, and bexarotene are available for topical use and are frequently utilized. Systemic multiagent chemotherapy is of limited use and reserved primarily for patients with advanced disease which has recurred and are not responding following other interventions. There are current early clinical trials findings that checkpoint inhibitors are active at least in some subsets of T-cell lymphomas and this is an area of active investigation. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano Classification. Rituximab extended schedule or retreatment trial for low-tumor burden follicular lymphoma: eastern cooperative oncology group protocol e4402. However, the limits of conventional disease markers, such as serum and urine immunofixation/ electrophoresis, have challenged the ability to precisely quantify the depth of response. Revised international staging system for multiple myeloma: a report from international myeloma working group. In the United States, age is not a sole determinant of transplant eligibility, but rather fitness, frailty, comorbidities, desire to undergo transplant, and support networks are important factors. For transplant-eligible patients, it is generally recommended that stem cell collection occur after four cycles of initial therapy due to the potential stem cell toxicity that may be associated with continuous exposure to certain classes of therapy (lenalidomide). When selecting an initial regimen, the number of drugs is not the only critical decision; rather, current comorbidities, ease of administration, availability in the country, and the balance between efficacy and toxicity must be taken into consideration. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Common side effects include peripheral neuropathy, gastrointestinal toxicity, shingles reactivation, and thrombocytopenia. Studies demonstrate that weekly and subcutaneous dosing of bortezomib yield lower peripheral neuropathy rates, allowing for increased tolerability and noninferior efficacy results. Carfilzomib Carfilzomib is an irreversible proteasome inhibitor, acting on the chymotrypsin domain of the proteasome complex. Side effects include fatigue, cytopenias, rash, diarrhea, and increased risk of thromboembolism. Although a number of different therapeutics have been tested in the maintenance setting, the most successful agent to show clinical benefit is oral lenalidomide. Of note, there was increased risk of secondary primary malignancies in patients receiving lenalidomide maintenance. The diverse array of mechanistic actions allow for synergistic combinations that have nonoverlapping toxicity profiles (Table 17. When selecting a salvage regimen, clinicians must consider the degree of aggressiveness a patient is relapsing, preexisting conditions, and toxicities. Pomalidomide Pomalidomide is a thalidomide analog that is administered daily with oral doses ranging from 1 to 4 mg and approved for patients who have received two or more prior lines of therapy (including lenalidomide and dexamethasone) and disease progression within completing 60 days of last therapy. It is administered at starting doses of 4 mg weekly and combined with lenalidomide and dexamethasone. Common side effects include diarrhea, vomiting, decreased appetite, and cytopenias. The most common side effects include infusion reactions, fatigue, thrombocytopenia, and anemia. Importantly, two practical considerations must be made when performing laboratory testing on patients receiving daratumamab. Additionally, daratumumab can comigrate with the monoclonal band on serum protein electrophoresis, resulting in a small overestimation of the m-protein. Initial doses start at 10 mg/ kg on a weekly basis for the first two cycles, and then every 2 weeks thereafter. The drug is administered with lenalidomide and dexamethasone, because single-agent activity is minimal.
Generic viagra gold 800mg otc
This lifts the epiglottis out of your field of view and allows excellent visualization of the glottis impotence icd 9 order viagra gold australia. Advance the warmed (prevents fogging) laryngeal mirror into the posterior of the oropharynx while taking care to not stimulate the posterior part of the tongue or pharynx. One or two quick sprays of benzocaine into the posterior aspect of the oropharynx is sufficient. Though rare, prolonged or repeated spraying of benzocaine can result in methemoglobinemia. Reassure the patient beforehand that although this may make the throat feel as though it is swelling or paralyzed, in actuality, it is just the numbness that accounts for the sensation. The tendency to gag can also be minimized by having the patient concentrate on breathing efforts and keep the eyes open and fixed on an object in the distance. Once the patient is anesthetized, repeat the steps described earlier and position the mirror against the soft palate. Rotate the angle of the mirror and systematically inspect the base of the tongue, valleculae, epiglottis, piriform recess, arytenoids, false and true vocal cords, and if possible, the superior aspect of the trachea. Further evaluate the anterior structure of the larynx and function of the vocal cords by having the patient say "eeee" in a high-pitched voice. This should move the epiglottis away from blocking the view of the larynx and bring the true cords together at the midline. Slide the mirror into the oropharynx with the glass surface parallel to the tongue but not touching it. Place the back of the mirror against the uvula and soft palate and smoothly lift until the larynx is visualized. In patients who cannot tolerate this procedure without gagging, apply topical anesthetic to aid in the examination. Occasionally, it may not be possible to complete the procedure because of a prominent gag reflex or patient apprehension and discomfort. Complications include traumatic abrasions and bleeding anywhere along the path of the laryngoscope or on the soft palate or pharynx if a mirror is used. In patients with head injury, there is always a slight risk of passing the scope intracranially if a basilar skull fracture has occurred; use of a soft nasal trumpet significantly reduces this risk. Laryngospasm and acute airway compromise can be induced in patients with paraglottic infections. Use a long 25- to 27-gauge needle and a 3- to 5-mL syringe for local anesthesia and a 10-mL syringe for aspiration. Avoid lateral angulation of the aspirating needle and use a needle guard to limit depth of penetration. It is rarely seen in children younger than 6 years and is the most common head and neck abscess in anyone older than 6 years. A myriad of opinions exist on the appropriate treatment method, although most agree that some form of drainage procedure is usually required and should be performed in conjunction with the administration of antibiotics and pain control medication. The palatine tonsils are located between the anterior and posterior pillars of the throat, bound in a capsule, and covered by mucosa. The superior pharyngeal constrictor muscle defines the lateral wall of the tonsil. A, Acute exudative pharyngitis is characterized by bilateral tonsillar edema, erythema, and exudate. Note that the edema is for the most part symmetric and that the uvula lies in the midline. B, A peritonsillar abscess (arrow) is characterized by asymmetric tonsillar bulging, with the uvula deviated away from the side of the abscess. The abscess is defined as a collection of pus between the tonsillar capsule, the superior constrictor muscle, and the palatopharyngeus muscle. If a rapid response to medical therapy is not seen, drainage or tonsillectomy should be performed. Approximately 50% of patients, predominately children rather than adults, will respond to medical therapy alone. Intraoral sonography may augment diagnostic accuracy and direct localization for drainage. Other contraindications can include severe trismus, coagulopathy, and inability of the patient to cooperate with the procedure. There are no data proving that antibiotics, even the correct ones in proper doses, invariably prevent the progression of tonsillitis to abscess formation. Changes in voice are common ("hot-potato voice") and caused by transient velopharyngeal insufficiency and muffled oral resonance. Although leukocytosis is often present, a complete blood count and other laboratory tests are nonspecific. Chronic conditions include leukemia, carcinoma, and tumor in the parapharyngeal space. One should administer parenteral narcotic analgesia, mild sedation, or both, before attempting aspiration. The combination of midazolam, ketamine, and glycopyrrolate is reported to be safe and effective for outpatient peritonsillar drainage in children. A myriad of opinions exist on the appropriate treatment method, although most agree that some form of drainage procedure should be performed in conjunction with the administration of antibiotics and pain control. Three options for surgical drainage include needle aspiration (most common), incision and drainage, and immediate (quinsy) tonsillectomy. Needle aspiration is relatively simple, can be performed by emergency clinicians, does not require special equipment, and is relatively inexpensive. Other benefits of needle aspiration over incision and drainage include decreased pain and trauma. Many believe that this should be the initial surgical drainage procedure for adults and children. For this reason, some authors propose admission of patients with negative aspirations and the presumed diagnosis of peritonsillar cellulitis for intravenous antibiotics and observation to prevent further morbidity. Although most studies involved hospitalization and intravenous antibiotics, selected outpatient treatment with oral antibiotics has also been successful and is usually the option chosen unless the patient appears to be in a septic state. It is usually performed after pus is obtained by needle aspiration, but occasionally it is the primary procedure. It seems most logical to first attempt needle aspiration and follow with incision and drainage only if additional pus is suspected or other extenuating circumstances are present. The success rate for incision and drainage is high, with a recurrence rate similar to or lower than that with aspiration alone. Incision and drainage and immediate tonsillectomy should be reserved for treatment failures or recurrences. These procedures can be performed in conjunction with hospital admission and administration of intravenous antibiotics or as outpatient treatment with oral antibiotics. One evidence-based review analyzed 42 articles, 5 of which were clinical studies on surgical technique. Computed tomography or ultrasound will further elucidate the diagnosis, but they are not needed in straightforward cases. For needle aspiration, you will need a light source, tongue blade, injectable (1% lidocaine with 1: 100,000 epinephrine) or topical (Cetacaine spray or 4% lidocaine) anesthetic, 3- to 5-mL syringe with a long 25-gauge needle for injection of anesthetic, and a standard or long 18- to 20-gauge needle (spinal needle) on a 10-mL syringe for aspiration (see Review Box 63. It is also helpful to have wall suction with a Frazier or Yankauer suction-tip device available. For incision and drainage, the same examination, suction, and anesthetizing equipment are required. Administer a parenteral narcotic analgesic, a mild sedative, or both before attempting aspiration. Infiltrate with 2 to 3 mL of 1% lidocaine with epinephrine via a 25- to 27-gauge needle. Use a 3- to 5-mL syringe with a long needle so it is possible to visualize the area to be injected. Displacing the tongue with a finger rather than a tongue blade may provide a better view.
Buy online viagra gold
The superior ramus anastomoses with the deep circumflex iliac artery and the ascending branch of the lateral circumflex femoral artery biking causes erectile dysfunction order viagra gold 800mg on-line. The inferior ramus anastomoses with the lateral circumflex femoral, inferior gluteal, and ascending branch of the medial circumflex femoral artery Deep Circumflex Iliac Artery. It anastomoses with the ascending branch of the lateral circumflex femoral artery and the iliolumbar and superior gluteal arteries and has a large ascending branch. It is important to be aware of the terminology employed in discussing collateral circulation. An affluent vessel is a collateral branch that arises from a patent main vessel above the obstruction or from a patent contralateral mate. An effluent vessel is a branch below the obstruction that receives blood from the affluent vessel and allows it to flow in a retrograde manner to reconstitute the occluded artery. The affluent vessel may pass blood into the effluent vessel as a continuous line, a phenomenon called inosculation, or may be connected to the effluent vessel by a network of fine vessels, forming what is called retiform anastomosis. Inosculation keeps a good flow through the anastomosis, with a heavy head of pressure, leading to refilling of the main vessels distal to the occlusion. An example of retiform anastomosis is the communication between the lumbar and iliolumbar arteries or the Winslow pathway (that is, from the intercostal and internal mammary arteries to the external iliac arteries via the epigastric arteries). An example of inosculation is between the lateral ascending branch of the arteria profunda femoris and lateral branches of the superior gluteal artery. The sciatic artery is the axial artery of the lower extremity, providing blood supply during the early stages of embryonic development. It normally regresses to form the proximal part of the inferior gluteal artery after the third month of embryologic life, after the development of the femoral artery from the external iliac artery. If the femoral system fails to develop, the sciatic artery becomes the dominant supply to the leg and the superficial femoral artery remains hypoplastic. Conversely, failure of complete involution of the sciatic artery may result in a hypoplastic sciatic artery with a normal femoral system. Aneurysm formation in the persistent sciatic artery occurs in as many as 46% of cases, and may be the first evidence of the presence of the anomaly, causing buttock pain and sometimes sciatic nerve compression with sciatic pain in the affected leg. The sciatic vein usually follows the same path as that of the artery but is less perceptible in the imaging modalities. Larger than the internal iliac arteries, they descend laterally along the medial border of the psoas major, entering the thigh posteriorly to the inguinal ligament, thereby becoming the femoral artery. Selective arteriography of the right internal iliac artery in an elderly patient showing the gluteal arteries and branches. Pelvic angiography in a patient with occlusive disease, showing the development of the collateralization in the pelvis. A, Pelvic angiography in a patient with a uterine lesion showing the enlargement of the uterine arteries. D, Selective angiography of the right internal iliac artery shows the pelvic circulation, mainly the uterine artery. E, Selective injection at the left uterine artery shows the typical vascular pattern of the enlarged uterus. A, Type I uterine artery arising as the first branch of the inferior gluteal artery, or anterior trunk. Other branches such as the internal pudendal artery may be the first branch of the inferior gluteal artery. The uterine artery, the inferior gluteal artery, and the superior gluteal artery arise at the same level as a trifurcation. The right uterine artery is the first branch of the anterior trunk, inferior gluteal artery (Type I). The left uterine artery is the first branch of the inferior gluteal artery, but not as evident (type I). The uterine artery origin is the first branch of the inferior gluteal artery (type I). The spongiosal artery is not always visible and the interruption at the bulb of the corpus spongiosum is an angiographic artifact. Selective right internal pudendal angiogram showing the classic arterial anatomy of the penis. The penile artery is the continuation of the internal pudendal artery after it gives origin to the perineal artery, and scrotal branches. The cavernosal artery is larger than usual and freely anastomoses with segments of the dorsal penile artery. B, Late phase of the angiogram showing the corpus cavernosum and corpus spongiosum. Selective angiography of the right internal iliac artery showing only the dorsal penile artery. A, Selective angiography of the right internal iliac artery shows the right dorsal penile artery and right and left cavernosal arteries filling from the right side injection. B, Right internal iliac angiography shows the dorsal penile artery and the cavernosal artery. C, Right internal iliac artery shows a small dorsal penile artery, an even smaller cavernosal artery, and a long and relatively large spongiosal artery. When flaccid, the sinusoids are smaller in capacity and the muscle has a high tonus, limiting arterial inflow. After stimulation, the sinusoidal smooth muscle relaxes and the sinusoids distend, reducing resistance to arterial flow, and obstructing the venous outflow by compressing the peripheral venules against the tunica albuginea, thereby raising the cavernosal pressure close to systolic pressure. Right internal iliac angiography showing the transverse root communication between the right and left arterial systems. Pelvic angiography showing the communications between the right and left arterial systems through the transverse root communication (A) and between medial femoral circumflex arteries or external pudendal arteries (B) in a patient with vascular disease. Pelvic angiography showing the development of anastomosis between the lumbar arteries and the internal iliac branches, due to an occlusion at the aortic bifurcation. Pelvic angiography in a patient with arterial occlusion showing the development of the lateral sacral arteries and the gluteal arteries. Right internal iliac arteriogram showing the persistent sciatic artery instead of the inferior gluteal artery. Schematic diagram of the major potential parietal pathways of collateral circulation encountered in chronic obstructive vascular disease at the abdominal and pelvic levels. Computerized tomographic angiogram of the thorax and abdomen showing the thoracoabdominal arterial anastomoses through the superior epigastric arteries and the inferior epigastric arteries, connecting with the common femoral arteries through the retiform anastomosis between the two systems. A, Anteroposterior view of a right internal iliac arteriogram in an individual with occluded right external iliac artery, with reconstitution of the arteria profunda femoris and superficial femoral artery through collateral anastomosis from lateral branches of the superior gluteal artery and lateral ascending branch of the arteria profunda femoris. B, Lateral view of the same arteriogram showing the continuation between the two systems. A, Anteroposterior view of a left internal iliac arteriogram in an individual with occluded left external iliac artery, with reconstitution of the arteria profunda femoris and the superficial femoral artery through collateral anastomosis from lateral branches of the superior gluteal artery and lateral ascending branch of the arteria profunda femoris. B, Lateral view of the same arteriogram showing the continuation of the two systems. Continued The external iliac vein is the continuation of the femoral vein; it begins at the inguinal ligament, and joins the internal iliac vein, thereby forming the common iliac vein. Tributaries Origin outside the pelvis Superior gluteal veins Inferior gluteal veins Internal pudendal veins Obturator vein Anterior to the sacrum Lateral sacral veins Origin in visceral venous plexus Middle rectal veins Rectal venous plexus Prostatic venous plexus Vesical plexus Dorsal veins of the penis and penile venous plexus Uterine plexuses Vaginal plexuses with the medial circumflex femoral and first perforating veins. They enter low in the greater sciatic foramen, joining the internal iliac vein, and connect with the superficial gluteal veins through the gluteal perforating veins. These receive veins from the penile bulb and the scrotal (or labial) and inferior rectal veins. The deep dorsal vein of the penis ends in the prostatic plexus, but is connected through that plexus to the internal pudendal veins. Obturator Vein this vein commences in the proximal adductor region and enters the pelvis through the obturator foramen, coursing a retroperitoneal path, passing between the ureter and the internal iliac artery to join the internal iliac vein. Middle Rectal Vein this vein arises from the rectal venous plexus, receiving tributaries from the bladder, prostate, and seminal vesicle. These veins enter the pelvis through the greater sciatic foramen, above the muscle piriformis, and join the internal iliac vein as a single trunk. It has an internal rectal plexus, under the rectal and anal epithelium, and an external rectal plexus outside the muscular layer.
Buy viagra gold us
Rehydration impotence diabetes buy viagra gold with a mastercard, rest, and supportive care in a cool environment are adequate therapy for heat exhaustion. The poor, urban elderly, infants, homeless, and persons with impaired mobility are at greatest risk. Highly motivated, poorly acclimatized, or unconditioned athletes and overweight military recruits are common victims, as are individuals who perform heavy physical labor in hot, humid conditions. Human immunodeficiency virus seropositivity alone was not associated with an increased risk for exertional heat-related illness. Studies of hyperthermia in patients undergoing cancer therapy have revealed that tissue sensitivity to heat is increased by relative hypoxia, ischemia, and acidosis. Although anhidrosis is described as a classic sign of heatstroke, investigations have demonstrated that cessation of sweating may be a late finding. Failure to consider the diagnosis of heatstroke in a diaphoretic patient with changes in mental status could prove disastrous. Researchers suggest that in cases of instant death, brain edema from the increased permeability of the blood-brain barrier causes raised intracranial pressure and papilledema, followed by vascular infarction and brain herniation. Coagulopathies and liver dysfunction (elevated levels of bilirubin and transaminases) occur as a consequence of thermal breakdown, consumption of serum proteins, and direct heat damage to hepatic cells. Unlike patients with hypothermia, in whom slow, gentle rewarming and supportive care often result in a favorable outcome, victims of severe heatstroke must be treated aggressively with measures designed to rapidly lower core temperature. Studies investigating precooling techniques to avoid heatstroke have been relatively unsuccessful in attenuating increases in core body temperature, and such techniques are not recommended. This results in contraction of the sarcomeres, skeletal muscle rigidity, increased skeletal muscle metabolism, elevated serum creatine kinase levels, heat production, and finally, systemic hyperthermia. Heat production in anesthetized patients can be profound with as much as a fivefold increase in oxygen consumption. The reaction is triggered by blockage of dopaminergic receptors and results in skeletal muscle spasticity, which generates excessive heat and impairs hypothalamic thermoregulation and heat dissipation. Autonomic instability is manifested as tachycardia, labile blood pressure, sweating, and incontinence. This syndrome is more likely to occur at the initiation of or after an increase in neuroleptic dosage. The syndrome may be misinterpreted as worsening of an underlying psychiatric disorder, drug intoxication. Treatment is primarily supportive in milder cases and consists of prompt recognition and withdrawal of the offending agent. Adequate sedation, usually with benzodiazepines, is essential in controlling serotonin syndrome. For the most severe cases, aggressive intensive care unit management is warranted to prevent renal failure and death. When administered as an antidote for serotonin syndrome, an initial dose of 12 mg is recommended, followed by 2 mg every 2 hours until clinical response is seen. Cyproheptadine is only available in an oral form, but it may be crushed and given through a nasogastric or orogastric tube. There has been limited success with benzodiazepines and -blockers to treat agitation in these patients. Treatment requires prompt recognition, maintenance of adequate hydration, rapid cooling, and the aggressive use of sedatives or paralyzing agents (or both) to control agitation. Importantly, the longer that psychostimulant-overdosed patients remain hyperthermic, the higher their morbidity and mortality rates. Agitation and seizures must be chemically controlled because they lead to continued generation of heat and muscle injury. The full-blown syndrome includes hyperthermia, coagulopathy, encephalopathy, and renal and hepatic dysfunction. Therapy is largely supportive and includes volume replacement with rapid cooling of the hyperthermic child while sources of bacterial infection are sought and treated. In older patients, fluid resuscitation should be monitored carefully to avoid pulmonary edema. Regarding antipyretics, there is no indication for either salicylates or acetaminophen in the setting of heatstroke because their efficacy depends on a normally functioning hypothalamus. Overzealous use of acetaminophen could potentiate hepatic damage, and salicylates may promote bleeding tendencies. Studies in animal models are based on the assumption that the fastest cooling technique is the best. Patient access, monitoring, safety, ease of use, availability, and speed are all considerations. The cooling rates achieved in various human and animal studies of heatstroke are summarized in Table 65. In addition to the cooling procedures outlined, it is imperative that the clinician institute the judicious use of sedation, muscle paralysis, or both to control agitation, suppress shivering, reduce energy expenditure, and make the patient receptive to sometimes unpleasant therapies. Immersion cooling is relatively contraindicated when cardiac monitoring of an unstable patient is required or when limited personnel make constant patient supervision impossible. Gastric lavage is also contraindicated by conditions that preclude Cooling Techniques General Considerations Heatstroke mortality is proportional to the magnitude and duration of thermal stress measured in degree-minutes. Cold peritoneal lavage is relatively contraindicated when multiple previous abdominal surgeries make placement of a lavage catheter risky. Evaporative Cooling Evaporating water is thermodynamically a much more effective cooling medium than melting ice, given an appropriate watervapor gradient. In theory, evaporative cooling should be approximately seven times more efficient than ice packing. In separate human studies, Weiner and Khogali and Wyndham and colleagues found that evaporative cooling rates were substantially greater than cooling rates with water immersion at 14. In clinical practice, ice water immersion or ice packing causes heat loss by conduction and heat consumption by the phase change of melting ice. The air must be warm but not humid because evaporation is decreased at lower temperatures. The entire body surface must be exposed to airflow and continuously moistened with water. Ideally, the patient is suspended in a mesh sling to expose the back to airflow and moisture. It maintains good peripheral perfusion and prevents shivering by warming the skin. Studies conducted in heat-stressed laying hens demonstrated superior cooling rates with ventral cooling regimes over dorsal cooling. Half the body surface, the back, will usually be unavailable for evaporative cooling. Airflow rates and temperatures are usually limited by the ambient temperature in the treatment facility and by the size and power of the fan available. These realities are reflected by the slower cooling rates achieved with evaporative cooling in a clinical setting. Procedure Complications of evaporative cooling are rare and more often a result of the underlying disorder than the cooling technique. Shivering occurs infrequently with this technique when compared with other cooling methods because the water is relatively lukewarm.
Buy viagra gold with amex
Tyrosine hydroxylase deficiency: clinical manifestations of catecholamine insufficiency in infancy erectile dysfunction medication insurance coverage purchase viagra gold online. Comparative studies on the structure of human tyrosine hydroxylase with those of the enzyme of various mammals. Localization of the human tyrosine hydroxylase gene to 11p15: gene duplication and evolution of metabolic pathways. Four novel mutations in the tyrosine hydroxylase gene in patients with infantile parkinsonism. Since then, considerable experience has been developed which has defined the clinical phenotype, the abnormal biochemistry, and the natural history of the disease [4]. This enzyme is on the metabolic pathway for methionine, and patients may be recognized by an increase in the concentration of methionine Methionine S-Adenosylmethionine S-Adenosylhomocysteine in the blood. This property forms the basis for the inclusion of homocystinuria in programs of routine newborn screening. In some patients, accumulation of methionine may give a prominent, unpleasant odor. The clinical picture regularly includes many features, like subluxation of the lenses of the eyes, which are characteristic of a disorder of connective tissue. Extreme variability of clinical presentation is a consequence of whether or not there are thrombotic events, and if so, which areas of the body suffer infarction. Variability also results from the fact that there are two distinct populations of homocystinuric patients, one of which responds to treatment with pyridoxine and one that does not [4]. Its presence may be signaled by iridodonesis, a dancing or shimmering of the iris. Subluxed lenses had previously been removed bilaterally, after which he developed glaucoma in the left eye. She had been found one year previously to have left-sided glaucoma and subluxed lenses bilaterally. Other ocular abnormalities include myopia, optic atrophy, cataracts, or retinal detachment [9]. The pigmentation of the iris may be lighter than in other family members, and the same may be true for the skin and hair. The skin may otherwise have blotchy erythema and pallor, and livido reticularis [11] is particularly common in the distal extremities, which may be quite cold and show other evidence of vascular instability. There may be posterior biconcave or fish-mouth appearance, and there may be impressive compression fractures or kyphoscoliosis [12, 13]. Presenting as developmental delay during the first years of life, intellectual disability is often the first recognized sign of homocystinuria. Thrombotic or vascular disease appears as a central pathomechanism of disease involving the nervous system. Many patients have been observed to have typical strokes, with transient or permanent hemiplegia. Psychiatric abnormalities have been observed in more than half of one series of 63 patients [14]. Three children were reported to have folate-responsive periodic behavior, including rage attacks [20, 21]. A three-year-old had episodic repetitive behavior thought to represent psychomotor seizures [20]. Adults have been diagnosed as schizophrenic or depressed [14], or to have personality disorders. Evidence of infarction has been obtained in patients presenting with hemiparesis, with or without papilledema. We, and others, have observed diffuse leukoencephalopathy as a rare finding in classical homocystinuria. Neuropathologic study has revealed occlusion of vessels, old and new thrombi, spongy degeneration, and neuronal loss [25, 26]. In the patient who died at 18 years of age with dystonia, the brain was histologically normal [16]. Cerebrovascular disease occurred in one third of 147 patients, and 32 percent of those thromboembolic events were strokes [4]. There were 11 percent peripheral arterial occlusions, 51 percent peripheral venous occlusions, and 32 of these patients had pulmonary emboli. Surgery may be especially strongly associated with thromboembolic accidents [4, 17, 25]. Medial degeneration of the vessels and intimal proliferation of both narrow vessel lumens, and initial injury is followed by the adherence of unusually sticky platelets. Acute pancreatitis has been reported [28] in two patients, one of whom developed a large pseudocyst that was drained surgically. Spontaneous pneumothorax has been reported in three patients with this disease, one of whom had two episodes [29, 30]. Homocystinuria and pregnancy have been reported [31] in 11 women (15 pregnancies), six of them pyridoxine responsive and five nonresponsive. Complications of pregnancy included pre-eclampsia in two and a venous thrombosis in a leg in one. Of 12 live-born infants, ten were normal and two had multiple anomalies, one of which was the Beckwith-Wiedemann syndrome, which were judged to be unrelated to homocystinuria. Experience has grown to more than 100 pregnancies especially with the pyridoxine-responsive form of the disorder showing that there is no significant risk of malformations in the offspring. The risk is particularly high for six weeks after delivery, while the uterus is involuting. It occurs with a frequency of one in 1800 newborns in the state of Qatar [32], one in 50,000 in Ireland and New England and one in one million in Japan; overall frequency is between one in 200,000 and 350,000. The defective enzyme may be demonstrated in cultured lymphocytes and fibroblasts, as well as in tissues such as the liver. Pyridoxine-responsive patients always have some residual activity, and increased activity of hepatic enzyme has been documented in response to treatment. Three types of enzyme were delineated: zero residual activity; reduced activity and normal affinity for pyridoxalphosphate; and reduced activity and affinity [33]. The enzyme cystathionine -synthase is a tetramer of 63 kDa [35], which undergoes post-translational proteolytic increase in activity with decrease in size to 48 kDa. In most patients, enzyme size is normal, but exceptions have been encountered [38]. There is also alternative splicing among five exons (designated -1a to -1e) in the 5-untranslated region. More than 170 mutations have been identified [42], and the functional consequences in many have been confirmed by expression systems. This, and the pyridoxine-responsive I278T, were the most common of 310 homocystinuric alleles [44]. R336C) in exon 11 is a founder mutation responsible for the high frequency of homocystinuria in the State of Qatar, 1:1800 [32]. Clinical observations, enzyme measurements and in vitro expression studies showed that this mutation completely abolishes enzyme activity and is not associated with vitamin B6 -responsiveness. Interestingly, about half of the point mutations in the coding region originate from deamination of methylcytosine in CpG dinucleotides [44], and nearly one quarter of the point mutations are found in exon 3, the most highly conserved region of the gene. Most patients have been compounds of two different mutant alleles, and most mutations are private [44]. Among compounds, a pyridoxine-responsive patient had the I278T mutation, as well as a 135-bp deletion that deleted 45 amino acids from 408 to 453 [45].