Buy fluoxetine discount
All contacts of persons with multidrug-resistant tuberculosis or extensively drug-resistant tuberculosis should have 2 years of follow-up regardless of treatment menstrual cramps during pregnancy buy fluoxetine online from canada. Persons with a positive tuberculin skin test (5 mm or more of induration) and fibrotic lesions suggestive of old tuberculosis on chest radiographs who have no evidence of active disease and no history of treatment for tuberculosis should receive 9 months of isoniazid or 4 months of rifampin (with or without isoniazid). Pregnant or breastfeeding women with latent tuberculosis should receive either daily or twice-weekly isoniazid with pyridoxine (vitamin B6). Patients receiving treatment for latent tuberculous infection should be evaluated once a month to assess for symptoms and signs of active tuberculosis and hepatitis and for adherence to their treatment regimen. Routine laboratory testing during treatment is indicated for those with abnormal baseline laboratory tests and for those at risk for developing liver disease. Treatment of latent tuberculous infection substantially reduces the risk that infection will progress to active disease. Targeted testing with the tuberculin skin test or interferon gamma release assays is used to identify persons who are at high risk for tuberculosis and who stand to benefit from treatment of latent infection. In general, patients with a positive tuberculin skin test or interferon gamma release assay who are at increased risk for exposure or disease are treated. It is essential that each person who meets the criteria for treatment of latent tuberculous infection undergo a careful assessment to exclude active disease. A history of past treatment for tuberculosis and contraindications to treatment should be sought. Patients suspected of having tuberculosis should receive one of the recommended multidrug regimens for active disease until the diagnosis is confirmed or excluded. Some close contacts of persons with active tuberculosis should be evaluated for treatment of latent tuberculous infection despite a negative tuberculin skin test reaction (less than 5 mm induration). These include immunosuppressed persons and those who may develop disease quickly after tuberculous infection. These organisms are not considered communicable from person to person, have distinct laboratory characteristics, and are often resistant to most antituberculous medications (Chapter 33). Vaccination of health care workers should be considered on an individual basis in settings in which a high percentage of tuberculosis patients are infected with strains resistant to both isoniazid and rifampin, in which transmission of such drug-resistant M tuberculosis and subsequent infection are likely, and in which comprehensive tuberculous infectioncontrol precautions have been implemented but have not been successful. Almost all properly treated immunocompetent patients with tuberculosis can be cured. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: treatment of drugsusceptible tuberculosis. Extensively drug-resistant tuberculosis: principles of resistance, diagnosis, and management. Less common symptoms include malaise, dyspnea, fever, hemoptysis, and weight loss. Parenchymal opacities on chest radiograph, most often thin-walled cavities or multiple small nodules associated with bronchiectasis. Bronchial washings are considered to be more sensitive than expectorated sputum samples; however, their specificity for clinical disease is not known. Diagnostic criteria in immunocompetent persons include the following: positive culture results from at least two separate expectorated sputum samples; or positive culture from at least one bronchial wash; or a positive culture from pleural fluid or any other normally sterile site. Diagnostic criteria are less stringent for patients with severe immunosuppression. For patients with severe fibrocavitary disease, streptomycin or amikacin is added for the first 2 months. The optimal duration of treatment is unknown, but therapy should be continued for 12 months after sputum conversion. Medical treatment is initially successful in about two-thirds of cases, but relapses after treatment are common; long-term benefit is demonstrated in about half of all patients. Surgical resection is an alternative for the patient with progressive disease that responds poorly to chemotherapy; the success rate with surgical therapy is good. A daily regimen of rifampin, isoniazid, and ethambutol for at least 18 months with a minimum of 12 months of negative cultures is usually successful. Rapidly growing mycobacteria (M abscessus, M fortuitum, M chelonae) are generally resistant to standard antituberculous therapy. Imaging errs es ook b ook b Chest radiographic findings include infiltrates that are progressive or persist for at least 2 months, cavitary lesions, and multiple nodular densities. Progression of pulmonary infiltrates during therapy or lack of radiographic improvement over time are poor prognostic signs and also raise concerns about secondary or alternative pulmonary processes. First, clinical disease may never develop in some patients, particularly asymptomatic patients with few organisms isolated from single specimens. Second, the spectrum of clinical disease severity is very wide; in patients with mild or slowly progressive symptoms, traditional chemotherapeutic regimens using a combination of agents may lead to drug-induced side effects worse than the disease itself. The investigators monitored the participants after screening for an average of 12 years. Invasive diagnostic evaluations were uncommon and were associated with a low complication rate (1. Since the groups were randomized and well matched, lung cancer incidence should have been identical. Many, perhaps most, of these lung cancers will never cause clinical disease and represent overdiagnosis. There is no evidence of benefit in a mixed population screened with chest radiography. The frequency of malignancy in surgical series ranges from 10% to 68% depending on patient population. Benign neoplasms, such as hamartomas, account for less than 5% of solitary nodules. The goals of evaluation are to identify and resect malignant tumors in patients who will benefit from resection while avoiding invasive procedures in benign disease. The task is to identify nodules with a sufficiently high probability of malignancy to warrant biopsy or resection or a sufficiently low probability of malignancy to justify observation. Symptoms alone rarely establish the cause, but clinical and imaging data can be used to assess the probability of malignancy. Smokers are at increased risk, and the likelihood of malignancy increases with the number of cigarettes smoked daily. Patients with a prior malignancy have a higher likelihood of having a malignant solitary nodule. The first and most important step in the imaging evaluation is to review old imaging studies. Comparison with prior studies allows estimation of doubling time, which is an important marker for malignancy. Rapid progression (doubling time less than 30 days) suggests infection while long-term stability (doubling time greater than 465 days) suggests benignity. The appearance of a smooth, well-defined edge is characteristic of a benign process. Benign lesions tend to have dense calcification in a central or laminated pattern. Malignant lesions are associated with sparser calcification that is typically stippled or eccentric. Cavitary lesions with thick (greater than 16 mm) walls are much more likely to be malignant. The probabilities in parentheses below represent guidelines only and should not be interpreted as prescriptive. In the case of solitary pulmonary nodules, a continuous probability function may be grouped into three categories. In patients with a low probability (less than 5%) of malignancy (eg, age under 30, lesions stable for more than 2 years, characteristic pattern of benign calcification), watchful waiting is appropriate. Patients with a high probability (greater than 60%) of malignancy should proceed directly to resection following staging, provided the surgical risk is acceptable. In general, the bronchoscopic yield for nodules that are less than 2 cm and peripheral is low, although complications are generally rare.
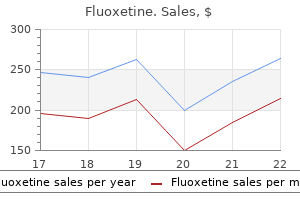
Purchase genuine fluoxetine on-line
It is usually considered benign when it occurs in acute myocardial infarction women's health clinic lawrenceburg tn purchase fluoxetine overnight, but the ischemia that induces it may also cause ventricular tachycardia and ventricular fibrillation. Sudden death occurs more frequently (presumably as a result of ventricular fibrillation) when ventricular premature beats occur in the presence of organic heart disease but not in individuals with no known cardiac disease. Exercise generally abolishes premature beats in normal hearts, and the rhythm becomes regular. Ventricular tachycardia is a frequent complication of acute myocardial infarction and dilated cardiomyopathy but may occur in chronic coronary disease, hypertrophic cardiomyopathy, mitral valve prolapse, myocarditis, and in most other forms of myocardial disease. It can also be a consequence of atypical forms of cardiomyopathies, such as arrhythmogenic right ventricular cardiomyopathy. However, ventricular tachycardia can also occur in patients with structurally normal hearts. In nonacute settings, most patients with ventricular tachycardia have known or easily detectable cardiac disease, and the finding of ventricular tachycardia is an unfavorable prognostic sign. In patients with structurally normal hearts, the prognosis is generally benign and syncope is uncommon. The etiology is often triggered activity from the right or left ventricular outflow tract and acute treatment with a short-acting intravenous beta-blocker may terminate the episode. If the patient is tolerating the rhythm, amiodarone 150 mg as a slow intravenous bolus over 10 minutes, followed by an infusion of 1 mg/min for 6 hours and then a maintenance infusion of 0. If the ventricular tachycardia recurs, supplemental amiodarone infusions of 150 mg over 10 minutes can be given. Symptoms and Signs Patients may be asymptomatic or experience syncope or milder symptoms of impaired cerebral perfusion. Sustained ventricular tachycardia-Patients with symptomatic or sustained ventricular tachycardia in the absence of a reversible precipitating cause (acute myocardial infarction or ischemia, electrolyte imbalance, medication toxicity, etc) are at high risk for recurrence. Catheter ablation has a high success rate in these patients who fail initial medical treatment. Beta-blockers are the mainstay for medical treatment of ventricular tachycardia in patients with structural heart disease. Amiodarone is generally preferred in patients with structural heart disease but sotalol may be considered as well. Laboratory Findings Ventricular tachycardia can occur in the setting of hypokalemia and hypomagnesemia. Cardiac markers may be elevated when ventricular tachycardia presents in the setting of acute myocardial infarction or as a consequence of underlying coronary disease and demand ischemia. Differentiation of Aberrantly Conducted Supraventricular Beats From Ventricular Beats errs es ook b ook b Ventricular tachycardia is either nonsustained (three or more consecutive beats lasting less than 30 seconds and terminating spontaneously) or sustained. When ventricular fibrillation occurs in the initial 24 hours after infarction, long-term management is no different from that of other patients with acute infarction. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. Sudden death risk in syncope: the role of the implantable cardioverter defibrillator. Wearable cardioverter-defibrillator therapy for the prevention of sudden cardiac death. These may be symptomatic (usually experienced as light-headedness) or asymptomatic. In general, treatment of the underlying cardiac disease is indicated rather than treatment of the arrhythmia itself. The causative rhythm in most cases is ventricular fibrillation, which is usually preceded by ventricular tachycardia except in the setting of acute ischemia or infarction. A disproportionate number of sudden deaths occur in the early morning hours and this suggests that there is a strong interplay with the autonomic nervous system. Sudden death may be the initial manifestation of coronary disease in up to 20% of patients and accounts for approximately 50% of deaths from coronary disease. Because the rate is often similar to the sinus rate, fusion beats and alternating rhythms are common. It occurs commonly in acute infarction and following reperfusion with thrombolytic medications. The incidence of associated ventricular fibrillation is much less than that of ventricular tachycardia with a rapid rate, and treatment is not indicated unless there is hemodynamic compromise or more serious arrhythmias. It may occur in the presence (Jervell-Lange-Nielsen syndrome) or absence (Romano-Ward syndrome) of congenital deafness. Specific genetic mutations affecting membrane potassium and sodium channels have been identified and help delineate the mechanisms and susceptibility to arrhythmia. Long-term treatment with beta-blockers (particularly nadolol) has been shown to be effective. The management of torsades de pointes differs from that of other forms of ventricular tachycardia. Increasing the heart rate, whether by infusion of beta-agonist (dopamine or isoproterenol) or temporary atrial or ventricular pacing, is an effective approach that can both break and prevent the rhythm. These rhythms are often caused or exacerbated by medications (digitalis, calcium channel blockers, beta-blockers, sympatholytic agents, antiarrhythmics), and agents that may be responsible should be withdrawn prior to making the diagnosis. Another presentation is of recurrent supraventricular tachycardias (paroxysmal reentry tachycardias, atrial flutter, and atrial fibrillation), associated with bradyarrhythmias ("tachy-brady syndrome"). The long pauses that often follow the termination of tachycardia cause the associated symptoms. Sick sinus syndrome occurs most commonly in elderly patients and is frequently seen in patients with concomitant atrial fibrillation. The pathologic changes are usually nonspecific, characterized by patchy fibrosis of the sinus node and cardiac conduction system. Sick sinus syndrome may rarely be caused by other conditions, including sarcoidosis, amyloidosis, Chagas disease, and various cardiomyopathies. Because these symptoms are either nonspecific or are due to other causes, it is essential that they be demonstrated to coincide temporally with arrhythmias. Patients may be asymptomatic or may complain of weakness or dyspnea if the rate is less than 35 beats/min; symptoms may occur at higher rates if the left ventricle cannot increase its stroke output. During periods of transition from partial to complete heart block, some patients have ventricular asystole that lasts several seconds or longer. Patients with episodic or chronic infranodal complete heart block require permanent pacing, and temporary pacing is indicated if implantation of a permanent pacemaker is delayed. Permanent pacing does not reduce mortality but may alleviate symptoms and improve quality of life in carefully selected patients. A standardized nomenclature for pacemaker generators is used, usually consisting of four letters. The first letter refers to the chamber that is stimulated (A = atrium, V = ventricle, D = dual, for both). The second letter refers to the chamber in which sensing occurs (also A, V, or D). The third letter refers to the sensory mode (I = inhibition by a sensed impulse, T = triggering by a sensed impulse, D = dual modes of response). The fourth letter refers to the programmability or rate modulation capacity (usually P for programming for two functions, M for programming more than two, and R for rate modulation). A dual-chamber multiple programmable pacemaker that senses and paces in both chambers is the most physiologic approach to pacing patients who remain in sinus rhythm. In patients with single-chamber ventricular pacemakers, the lack of an atrial kick may lead to the so-called pacemaker syndrome, in which the patient experiences signs of low cardiac output while upright. Pulse generators are also available that can increase their rate in response to motion or respiratory rate when the intrinsic atrial rate is inappropriately low. Follow-up after pacemaker implantation, usually by telephonic monitoring, is essential. All pulse generators and lead systems have an early failure rate that is now well below 1% and an expected battery life varying from 6 to 10 years.
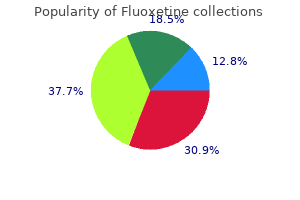
Order fluoxetine now
In other instances menstrual knee pain proven fluoxetine 20 mg, hyperplasia of all or part of the gallbladder wall may be so marked as to give the appearance of a myoma (adenomyomatosis). Hydrops of the gallbladder results when acute cholecystitis subsides but cystic duct obstruction persists, producing distention of the gallbladder with a clear mucoid fluid. Occasionally, a stone in the neck of the gallbladder may compress the common hepatic duct and cause jaundice (Mirizzi syndrome). Xanthogranulomatous cholecystitis is a rare, aggressive variant of chronic cholecystitis characterized by grayish-yellow nodules or streaks, representing lipid-laden macrophages, in the wall of the gallbladder and often presents with acute jaundice. Cholelithiasis with chronic cholecystitis may be associated with acute exacerbations of gallbladder inflammation, bile duct stone, fistulization to the bowel, pancreatitis and, rarely, carcinoma of the gallbladder. A technically successful surgical procedure in an appropriately selected patient is generally followed by complete resolution of symptoms. In severe cases, a fluoroquinolone such as ciprofloxacin, 250 mg intravenously every 12 hours, plus metronidazole may be given. Because of the high risk of recurrent attacks (up to 10% by 1 month and over 30% by 1 year), cholecystectomy-generally laparoscopically- should be performed within 24 hours of admission to the hospital for acute cholecystitis. Compared with delayed surgery, surgery within 24 hours is associated with a shorter length of stay, lower costs, and greater patient satisfaction. If nonsurgical treatment has been elected, the patient (especially if diabetic or elderly) should be watched carefully for recurrent symptoms, evidence of gangrene of the gallbladder, or cholangitis. In high-risk patients, ultrasound-guided aspiration of the gallbladder, if feasible, percutaneous cholecystostomy, or endoscopic insertion of a stent or nasobiliary drain into the gallbladder may postpone or even avoid the need for surgery. Immediate cholecystectomy is mandatory when there is evidence of gangrene or perforation. Surgical treatment of chronic cholecystitis is the same as for acute cholecystitis. If indicated, cholangiography can be performed during laparoscopic cholecystectomy. Long-term outcomes of endoscopic gallbladder stenting in high-risk surgical patients with calculous cholecystitis (with videos). In refractory cases, surgical sphincteroplasty or removal of the cystic duct remnant may be considered. Emptying of the gallbladder may be markedly reduced on gallbladder scintigraphy following injection of cholecystokinin; cholecystectomy may be curative in such cases. Histologic examination of the resected gallbladder may show chronic cholecystitis or microlithiasis. Duloxetine for the treatment of patients with suspected sphincter of Oddi dysfunction: a pilot study. The persistence of symptoms in this group of patients suggests the possibility of an incorrect diagnosis prior to cholecystectomy, eg, esophagitis, pancreatitis, radiculopathy, or functional bowel disease. Pain may also be associated with dilatation of the cystic duct remnant, neuroma formation in the ductal wall, foreign body granuloma, or traction on the bile duct by a long cystic duct. The clinical presentation of right upper quadrant pain, chills, fever, or jaundice suggests biliary tract disease. Biliary pain associated with elevated liver biochemical tests or a dilated bile duct in the absence of an obstructing lesion suggests sphincter of Oddi dysfunction. Endoscopic sphincterotomy is most likely to relieve symptoms in patients with a sphincter disorder or stenosis, although many patients continue to have some pain. In some cases, treatment with a calcium channel blocker, long-acting nitrate, phosphodiesterase inhibitor (eg, vardenafil), duloxetine, or tricyclic antidepressants or possibly injection of the sphincter with botulinum toxin may be beneficial. The rate of psychosocial comorbidity with sphincter of Oddi dysfunction does s errs ook e ook e/eb e/eb /t. Cholangitis should be suspected with fever followed by hypothermia and gram-negative shock, jaundice, and leukocytosis. Symptoms and Signs About 15% of patients with gallstones have choledocholithiasis (bile duct stones). The percentage rises with age, and the frequency in elderly people with gallstones may be as high as 50%. Bile duct stones usually originate in the gallbladder but may also form spontaneously in the bile duct after cholecystectomy. The risk is increased twofold in persons with a juxtapapillary duodenal diverticulum. Biliary pain results from rapid increases in bile duct pressure due to obstructed bile flow. The addition of altered mental status and hypotension (Reynolds pentad) signifies acute suppurative cholangitis and is an endoscopic emergency. According to the Tokyo guidelines (2006), the diagnosis of acute cholangitis is established by the presence of either (1) the Charcot triad or (2) two elements of the Charcot triad plus laboratory evidence of an inflammatory response (eg, elevated white blood cell count, C-reactive protein), elevated liver biochemical test levels, and imaging evidence of biliary dilatation or a cause of obstruction. Hepatomegaly may be present in calculous biliary obstruction, and tenderness is usually present in the right upper quadrant and epigastrium. Bile duct obstruction lasting more than 30 days results in liver damage leading to cirrhosis. In a population-based study from Denmark, acute cholangitis was reported to be a marker of occult gastrointestinal cancer. If the likelihood that obstruction is caused by a stone is high (bile duct diameter greater than 6 mm, bile duct stone seen on ultrasonography, serum bilirubin greater than 4 mg/dL [68. Bilirubinuria and elevation of the serum bilirubin are present if the bile duct remains obstructed; levels commonly fluctuate. Not uncommonly, serum amylase elevations are present because of secondary pancreatitis. When extrahepatic obstruction persists for more than a few weeks, differentiation of obstruction from chronic cholestatic liver disease becomes more difficult. Prolongation of the prothrombin time can result from the obstructed flow of bile to the intestine. Next in frequency are neoplasms of the pancreas, ampulla of Vater, or bile duct or an obstructed stent placed previously for decompression of an obstructing tumor. Extrinsic compression of the bile duct may result from metastatic carcinoma (usually from the gastrointestinal tract or breast) involving porta hepatis lymph nodes or, rarely, from a large duodenal diverticulum. Gallbladder cancer extending into the bile duct often presents as obstructive jaundice. Hepatocellular jaundice can usually be differentiated by the history, clinical findings, and liver biochemical tests, but liver biopsy is necessary on occasion. Recurrent pyogenic cholangitis should be considered in persons from Asia (and occasionally elsewhere) with intrahepatic biliary stones (particularly in the left ductal system) and recurrent cholangitis. A bile duct stone in a patient with cholelithiasis or cholecystitis is usually treated by endoscopic sphincterotomy and stone extraction followed by laparoscopic cholecystectomy within 72 hours in patients with cholecystitis and within 2 weeks in those without cholecystitis. An alternative approach, which is also associated with a shorter duration of hospitalization in patients at intermediate risk for choledocholithiasis, is laparoscopic cholecystectomy and bile duct exploration. For patients older than 70 years or poor-risk patients with cholelithiasis and choledocholithiasis, cholecystectomy may be deferred after endoscopic sphincterotomy because the risk of subsequent cholecystitis is low. Aminoglycosides should not be given for more than a few days because the risk of aminoglycoside nephrotoxicity is increased in patients with cholestasis. Regimens that include drugs active against anaerobes are required when a biliaryenteric communication is present. If sphincterotomy cannot be performed, the bile duct can be decompressed by a biliary stent or nasobiliary catheter. Once decompression is achieved, antibiotics are generally continued for at least another 3 days. Elective cholecystectomy can be undertaken after resolution of cholangitis, unless the patient remains unfit for surgery. This procedure is generally reserved for patients with coagulopathy because the risk of bleeding is lower with balloon dilation than with sphincterotomy. Choledocholithiasis discovered at laparoscopic cholecystectomy may be managed via laparoscopic or, if necessary, open bile duct exploration or by postoperative endoscopic sphincterotomy. Operative findings of choledocholithiasis are palpable stones in the bile duct, dilatation or thickening of the wall of the bile duct, or stones in the gallbladder small enough to pass through the cystic duct.
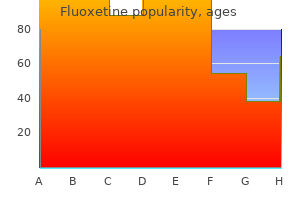
Order fluoxetine 10 mg with visa
The physical and laboratory abnormalities related to deficiencies of vitamins or minerals are discussed in Chapter 29 menstrual itching discount fluoxetine 10 mg overnight delivery. Chronic Infections es kerrs oo k eb oo e//eb me Chronic parasitic infections may cause diarrhea through a number of mechanisms. Pathogens most commonly associated with diarrhea include the protozoans Giardia, Entamoeba histolytica, and Cyclospora as well as the intestinal nematodes. Strongyloidiasis and capillariasis should be excluded in patients from endemic regions, especially in the presence of eosinophilia. Bacterial infections with C difficile and, uncommonly, Aeromonas and Plesiomonas may cause chronic diarrhea. Systemic Conditions Chronic systemic conditions, such as thyroid disease, diabetes, and collagen vascular disorders, may cause diarrhea through alterations in motility or intestinal absorption. Physical examination should assess for signs of malnutrition, dehydration, and inflammatory bowel disease. Because chronic diarrhea is caused by so many conditions, the subsequent diagnostic approach is guided by the relative suspicion for the underlying cause, and no specific algorithm can be followed in all patients. Prior to embarking on an extensive evaluation, the most common causes of chronic diarrhea should be considered, including medications, irritable bowel syndrome, and lactose intolerance. The clinician should establish whether the diarrhea is continuous or intermittent, its relationship to meals, and whether it occurs at night or during fasting. The stool appearance may suggest a malabsorption disorder (greasy or malodorous), inflammatory disorder (containing blood or pus), or a secretory process (watery). The presence of abdominal pain suggests irritable bowel syndrome or inflammatory bowel disease. Serologic tests for neuroendocrine tumors- Secretory diarrheas due to neuroendocrine tumors are rare but should be considered in patients with chronic, highvolume watery diarrhea (greater than 1 L/day) with a normal osmotic gap that persists during fasting. Breath test-The diagnosis of small bowel bacterial overgrowth is suggested by a noninvasive breath tests (glucose or lactulose); however, a high-rate of false-positive test results limits the utility of these tests. A definitive diagnosis of bacterial overgrowth is determined by aspirate of small intestinal contents for quantitative aerobic and anaerobic bacterial culture; however, this procedure is not available at most centers. Anemia occurs in malabsorption syndromes (folate, iron deficiency, or vitamin B12) as well as inflammatory conditions. Hypoalbuminemia is present in malabsorption, protein-losing enteropathies, and inflammatory diseases. Increased erythrocyte sedimentation rate or C-reactive protein suggests inflammatory bowel disease. Routine stool studies-Stool sample should be analyzed for ova and parasites, electrolytes (to calculate osmotic gap), qualitative staining for fat (Sudan stain), occult blood, and leukocytes or lactoferrin. Parasitic infections (Giardia, E histolytica, Cryptosporidia, and Cyclospora) may be diagnosed with stool antigen assays or microscopy with special stains. Alternatively, stool molecular diagnostic tests are available that screen for a panel of pathogens, providing results within 5 hours. As discussed previously, an increased osmotic gap suggests an osmotic diarrhea or disorder of malabsorption. The presence of fecal leukocytes or lactoferrin may suggest inflammatory bowel disease. Endoscopic examination and mucosal biopsy-Most patients with chronic persistent diarrhea undergo colonoscopy with mucosal biopsy to exclude inflammatory bowel disease (including Crohn disease and ulcerative colitis), microscopic colitis, and colonic neoplasia. Upper endoscopy with small bowel biopsy is performed when a small intestinal malabsorptive disorder is suspected (celiac disease, Whipple disease) from abnormal laboratory studies or a positive fecal fat stain. Loperamide: 4 mg orally initially, then 2 mg after each loose stool (maximum: 16 mg/day). Diphenoxylate with atropine: One tablet orally three or four times daily as needed. Codeine and deodorized tincture of opium: Because of potential habituation, these drugs are avoided except in cases of chronic, intractable diarrhea. Octreotide: this somatostatin analog stimulates intestinal fluid and electrolyte absorption and inhibits intestinal fluid secretion and the release of gastrointestinal peptides. Further Studies If the cause of diarrhea is still not apparent, further studies may be warranted. A fecal fat determination in excess of 10 g/24 h confirms a malabsorptive disorder. Volume status to determine severity of blood loss; hematocrit is a poor early indicator of blood loss. In the United States, the mortality rate for nonvariceal upper gastrointestinal bleeding has declined steadily over the past 20 years to 2. Mortality is higher in patients who are older than age 60 years and in patients in whom bleeding develops during hospitalization. Patients seldom die of exsanguination but rather of complications from an underlying disease. The most common presentation of upper gastrointestinal bleeding is hematemesis or melena. Although hematochezia generally suggests a lower bleeding source (eg, colonic), severe upper gastrointestinal bleeding may present with hematochezia in 10% of cases. Upper gastrointestinal bleeding is self-limited in 80% of patients; urgent medical therapy and endoscopic evaluation are obligatory in the rest. Patients with bleeding more than 48 hours prior to presentation have a low risk of recurrent bleeding. Bleeding usually arises from esophageal varices and less commonly gastric or duodenal varices or portal hypertensive gastropathy. Approximately 25% of patients with cirrhosis have medium to large esophageal varices, of whom 30% experience acute variceal bleeding within a 2-year period. Due to improved care, the hospital mortality rate has declined over the past 20 years from 40% to 15%. Gastric Neoplasms Gastric neoplasms result in 1% of upper gastrointestinal hemorrhages. Vascular anomalies are found throughout the gastrointestinal tract and may be the source of chronic or acute gastrointestinal bleeding. They have a bright red stellate appearance and occur throughout the gastrointestinal tract but most commonly in the right colon. The Dieulafoy lesion is an aberrant, large-caliber submucosal artery, most commonly in the proximal stomach that causes recurrent, intermittent bleeding. Erosive Gastritis Because this process is superficial, it is a relatively unusual cause of severe gastrointestinal bleeding (less than 5% of cases) and more commonly results in chronic blood loss. Erosive Esophagitis Severe erosive esophagitis due to chronic gastroesophageal reflux may rarely cause significant upper gastrointestinal bleeding, especially in patients who are bed bound long-term. Peptic ulcers account for 40% of major upper gastrointestinal bleeding with an overall mortality rate of less than 5%. In North America, the incidence of bleeding from ulcers is es kerrs oo k eb oo e//eb me m 604 H. In the absence of continued bleeding, the hemoglobin should rise approximately 1 g/dL for each unit of transfused packed red cells. Transfusion of blood should not be withheld from patients with massive active bleeding regardless of the hemoglobin value. In patients with severe gastrointestinal bleeding, it is desirable to transfuse blood before the hemoglobin reaches 7 g/dL to prevent decreases below that level occurring from hemodilution with fluid resuscitation.
Buy cheap fluoxetine online
The major adverse reactions include intravascular volume depletion weird women's health issues order fluoxetine mastercard, prerenal azotemia, and hypotension. Hypokalemia, particularly with accompanying digitalis therapy, is a major problem. Less common side effects include skin rashes, gastrointestinal distress, and ototoxicity (the latter more common with ethacrynic acid and possibly less common with bumetanide). The oral potassium-sparing agents are often useful in combination with the loop diuretics and thiazides. Their diuretic potency is only mild and not adequate for most patients with heart failure, but they may minimize the hypokalemia induced by more potent agents. Side effects include hyperkalemia, gastrointestinal symptoms, and kidney dysfunction. These medications spare loss of potassium, they have some diuretic effect (especially at higher doses), and they also improve clinical outcomes, including survival. Patients with refractory edema may respond to combinations of a loop diuretic and thiazide-like agents. Metolazone, because of its maintained activity with chronic kidney disease, is the most useful agent for such a combination. Extreme caution must be observed with this approach, since massive diuresis and electrolyte imbalances often occur; 2. In many cases this is necessary only once or twice a week, but dosages up to 10 mg daily have been used in some patients. Within several days (for those with the markers of higher risk) or at most 2 weeks, patients should be questioned about symptoms of hypotension, and both kidney function and potassium levels should be monitored. Some patients exhibit increases in serum creatinine or potassium, but they do not require discontinuation if the levels stabilize-even at values as high as 3 mg/dL and 5. Kidney dysfunction is more frequent in patients with diabetes, older patients, and those with low systolic pressures, and these groups should be monitored more closely. This has led to a strong recommendation that stable patients (defined as having no recent deterioration or evidence of volume overload) with mild, moderate, and even severe heart failure should be treated with a beta-blocker unless there is a noncardiac contraindication. In this study, one death was prevented for every 13 patients treated for 1 year-as dramatic an effect as has been seen with a pharmacologic therapy in the history of cardiovascular medicine. Thus, patients with chronic heart failure should be treated with extended-release metoprolol succinate, bisoprolol, or carvedilol but not shortacting metoprolol tartrate. Because even apparently stable patients may deteriorate when beta-blockers are initiated, initiation must be done gradually and with great care. Patients should be instructed to monitor their weight at home as an indicator of fluid retention and to report any increase or change in symptoms immediately. Before each dose increase, patients should be seen and examined to ensure that there has not been fluid retention or worsening of symptoms. If heart failure worsens, this can usually be managed by increasing diuretic doses and delaying further increases in beta-blocker doses, though downward adjustments or discontinuation is sometimes required. Carvedilol, because of its beta-blocking activity, may cause dizziness or hypotension. This can usually be managed by reducing the doses of other vasodilators and by slowing the pace of dose increases. Hyperkalemia was uncommon in severe heart failure clinical trial patients who received high doses of diuretic as maintenance therapy; however, hyperkalemia in patients taking spironolactone appears to be common in general practice. For some patients, cost will be a barrier to use, although analyses have shown that sacubitril/valsartan is cost effective. Beta-blockers-Beta-blockers are part of the foundation of care of chronic heart failure based on their lifesaving benefits. It is lower in patients with kidney dysfunction, in older patients, and in those with smaller lean body mass. Amiodarone, quinidine, propafenone, and verapamil are among the medications that may increase digoxin levels up to 100%. Digoxin may induce ventricular arrhythmias, especially when hypokalemia or myocardial ischemia is present. Once an appropriate maintenance dose is established, subsequent levels are usually not indicated unless there is a change in kidney function or medications that affects digoxin levels or a significant deterioration in cardiac status that may be associated with reduced clearance. The nitrates are moderately effective in relieving shortness of breath, especially in patients with mild to moderate symptoms, but less successful-probably because they have little effect on cardiac output-in advanced heart failure. Nitrate therapy is generally well tolerated, but headaches and hypotension may limit the dose of all agents. This is minimized by intermittent therapy, especially if a daily 8- to 12-hour nitrate-free interval is used, but probably develops to some extent in most patients receiving these agents. Transdermal nitroglycerin patches have no sustained effect in patients with heart failure and should not be used for this indication. Hydralazine-Oral hydralazine is a potent arteriolar dilator; when used as a single agent, it has not been shown to improve symptoms or exercise tolerance during longterm treatment. The combination of nitrates and oral hydralazine produces greater hemodynamic effects. The major side effect is gastrointestinal distress, but headaches, tachycardia, and hypotension are relatively common. Ivabradine-Ivabradine inhibits the If channel in the sinus node and has the specific effect of slowing sinus rate. It is approved by the European Medicines Agency for use in patients with a heart rate of 75 beats per minute or more. In a trial of patients with chronic angina, ivabradine did not reduce cardiovascular events, and there may have been more events with ivabradine (than placebo) in patients with symptomatic angina. Combination of medical therapies-Optimal management of chronic heart failure involves using combinations of proven life-saving therapies. Nitrates-Intravenous vasodilators (sodium nitroprusside or nitroglycerin) are used primarily for acute or severely decompensated chronic heart failure, especially when accompanied by hypertension or myocardial ischemia. If neither of the latter is present, therapy is best initiated and adjusted based on hemodynamic measurements. However, this risk appears to be primarily in patients who are in atrial fibrillation, who have had thromboemboli, or who have had a large recent anterior myocardial infarction. In general, these patients should receive warfarin for 3 months following the myocardial infarction. Biventricular pacing (resynchronization)-Many patients with heart failure due to systolic dysfunction have abnormal intraventricular conduction that results in dyssynchronous and hence inefficient contractions. Antiarrhythmic therapy-Patients with moderate to severe heart failure have a high incidence of both symptomatic and asymptomatic arrhythmias. Beta-blockers, because of their marked favorable effect on prognosis in general and on the incidence of sudden death specifically, should be initiated in these as well as all other patients with heart failure (see Beta-Blockers, above). For patients with systolic heart failure and atrial fibrillation, a rhythm control strategy has not been shown to improve outcome compared to a rate control strategy and thus should be reserved for patients with a reversible cause of atrial fibrillation or refractory symptoms. Statin therapy-Even though vascular disease is present in many patients with chronic heart failure, the role of statins has not been well defined in the heart failure population. Strategies to prevent clinical deterioration, such as case management, home monitoring of weight and clinical status, and patient adjustment of diuretics, can prevent rehospitalizations and should be part of the treatment regimen of advanced heart failure. Involvement of a multidisciplinary team (rather than a single physician) and in-person (rather than just telephonic) communication appear to be important features of successful programs. More severe sodium restriction is usually difficult to achieve and unnecessary because of the availability of potent diuretic agents. Exercise training improves activity tolerance in significant part by reversing the peripheral abnormalities associated with heart failure and deconditioning.
Buy fluoxetine online
Nonantibiotic prophylactic strategies menopause help purchase online fluoxetine, including probiotics, bile acids, and statins, are under study. Hepatorenal syndrome-Hepatorenal syndrome occurs in up to 10% of patients with advanced cirrhosis and ascites. It is characterized by (1) azotemia (increase in serum creatinine level of greater than 0. Oliguria, hyponatremia, and a low urinary sodium concentration are typical features. Hepatorenal syndrome is diagnosed only when other causes of acute kidney injury (including prerenal azotemia and acute tubular necrosis) have been excluded. Urinary neutrophil gelatinase-associated lipocalin levels (normal, 20 ng/mL) and other biomarkers may help distinguish hepatorenal syndrome (105 ng/mL) from chronic kidney disease (50 ng/mL) and other causes of acute kidney injury (325 ng/mL). Type I hepatorenal syndrome is typically associated with at least doubling of the serum creatinine to a level greater than 2. Continuous venovenous hemofiltration and hemodialysis are of uncertain value in hepatorenal syndrome. Liver transplantation is the ultimate treatment of choice, but many patients die before a donor liver can be obtained. Type 1 hepatorenal syndrome is often irreversible in patients with a systemic infection. The 3-month probability of survival in cirrhotic patients with hepatorenal syndrome (15%) is lower than that for renal failure associated with infections (31%), hypovolemia (46%), and parenchymal kidney disease (73%). Gram-positive cocci are the most common isolates in patients who have undergone an invasive procedure such as central venous line placement, and the frequency of enterococcal isolates is increasing. Alternative choices include ceftriaxone, amoxicillin-clavulanic acid, and levofloxacin (in patients not receiving fluoroquinolone prophylaxis). Oral ofloxacin, 400 mg twice daily for 7 days, or, in a patient not already taking a fluoroquinolone for prophylaxis against bacterial peritonitis, a 2-day course of intravenous ciprofloxacin, 200 mg twice daily, followed by oral ciprofloxacin, 500 mg twice daily for 5 days, may be effective alternative regimens in selected patients. A carbapenem has been recommended for patients with hospital-acquired spontaneous bacterial peritonitis, which is increasingly caused by multidrug-resistant organisms. Supplemental administration of intravenous albumin (which may have anti-inflammatory effects in addition to expanding plasma volume) prevents further renal impairment and reduces mortality, particularly in patients with a serum creatinine greater than 1 mg/dL (83. The overall mortality rate is high-up to 30% during hospitalization and up to 70% by 1 year. Another model predictive of mortality includes the blood urea nitrogen, white blood cell count, Child-Pugh score, and mean arterial pressure. Patients with cirrhosis and septic shock have a high frequency of relative adrenal insufficiency, which if present requires administration of hydrocortisone. In survivors of bacterial peritonitis, the risk of recurrent peritonitis may be decreased by long-term ciprofloxacin (eg, 500 mg orally once per day) or norfloxacin (400 mg orally daily; no longer available in the United States) or trimethoprim-sulfamethoxazole (eg, one double-strength tablet once per day). In cases of recurrent peritonitis, the causative organism is often resistant to fluoroquinolones and may become multidrug resistant in some cases. In high-risk cirrhotic patients without prior peritonitis (eg, those with an ascitic protein less than 1. In patients hospitalized for acute variceal bleeding, intravenous ceftriaxone (1 g per day), followed by oral trimethoprim-sulfamethoxazole (one double-strength es kerrs oo k eb oo e//eb /t. Hepatic encephalopathy-Hepatic encephalopathy is a state of disordered central nervous system function resulting from failure of the liver to detoxify noxious agents of gut origin because of hepatocellular dysfunction and portosystemic shunting. The clinical spectrum ranges from day-night reversal and mild intellectual impairment to coma. Patients with covert (formerly minimal) hepatic encephalopathy have no recognizable clinical symptoms but demonstrate mild cognitive, psychomotor, and attention deficits on standardized psychometric tests and an increased rate of traffic accidents. The stages of overt encephalopathy are (1) mild confusion, (2) drowsiness, (3) stupor, and (4) coma. Ammonia is the most readily identified and measurable toxin but is not solely responsible for the disturbed mental status. Bleeding into the intestinal tract may significantly increase the amount of protein in the bowel and precipitate encephalopathy. The diagnosis is based primarily on detection of characteristic symptoms and signs, including asterixis. A smartphone app called EncephalApp using the "Stroop test" (asking the patient to name the color of a written word rather than the word itself, even when the word is the name of a different color) has proved useful for detecting covert hepatic encephalopathy. Gastrointestinal bleeding should be controlled and blood purged from the gastrointestinal tract. The value of treating patients with covert hepatic encephalopathy is uncertain; probiotic agents may have some benefit. Lactulose, a nonabsorbable synthetic disaccharide syrup, is digested by bacteria in the colon to short-chain fatty acids, resulting in acidification of colon contents. Lactulose also leads to a change in bowel flora so that fewer ammonia-forming organisms are present. When given orally, the initial dose of lactulose for acute hepatic encephalopathy is 30 mL three or four times daily. Coagulopathy-Hypoprothrombinemia caused by malnutrition and vitamin K deficiency may be treated with vitamin K (eg, phytonadione, 5 mg orally or intravenously daily); however, this treatment is ineffective when synthesis of coagulation factors is impaired because of hepatic disease. In such cases, correcting the prolonged prothrombin time requires large volumes of fresh frozen plasma (see Chapter 14). Continued use of lactulose after an episode of acute encephalopathy reduces the frequency of recurrences. The ammonia-producing intestinal flora may also be controlled with an oral antibiotic. The nonabsorbable agent rifaximin, 550 mg orally twice daily, is preferred and has been shown as well to maintain remission of and reduce the risk of rehospitalization for hepatic encephalopathy over a 24-month period, with or without the concomitant use of lactulose. Patients who do not respond to lactulose alone may improve with a course of an antibiotic added to treatment with lactulose. Zinc deficiency should be corrected, if present, with oral zinc sulfate, 600 mg/day in divided doses. Sodium benzoate, 5 g orally twice daily, ornithine aspartate, 9 g orally three times daily, and L-acyl-carnitine (an essential factor in the mitochrondrial transport of long-chain fatty acids), 4 g orally daily, may lower blood ammonia levels, but there is less experience with these drugs than with lactulose. Flumazenil is effective in about 30% of patients with severe hepatic encephalopathy, but the drug is short-acting and intravenous administration is required. Use of special dietary supplements enriched with branched-chain amino acids is usually unnecessary except in occasional patients who are intolerant of standard protein supplements. Relative contraindications include age over 70 years, morbid obesity, portal and mesenteric vein thrombosis, active alcohol or drug abuse, severe malnutrition, and lack of patient understanding. Combined liver-kidney transplantation is indicated in patients with associated kidney failure presumed to be irreversible. The major impediment to more widespread use of liver transplantation is a shortage of donor organs.
Purchase 10mg fluoxetine fast delivery
On auscultation breast cancer north face order discount fluoxetine on-line, there are characteristic midsystolic clicks that may be multiple and emanate from the chordae or redundant valve tissue. If leaflets fail to come together properly, the clicks will be followed by a late systolic murmur. As the mitral regurgitation worsens, the murmur is heard more and more throughout systole. Whether sudden cardiac death presumably due to ventricular arrhythmias is more frequent in patients with mitral valve prolapse remains controversial. Often associated with skeletal changes (straight back, pectus excavatum, and scoliosis) or hyperflexibility of joints. Diagnostic Studies the diagnosis is primarily clinical and confirmed echocardiographically. If palpitations are an issue, an ambulatory monitor is often helpful to distinguish atrial from ventricular tachyarrhythmias. Selective serotonin reuptake inhibitors have also been used, especially if orthostatic hypotension or anxiety is associated with mitral valve prolapse; results have been mixed. Afterload reduction has not been shown to change prognosis when mitral regurgitation is present. Mitral valve repair is strongly favored over valve replacement, and its efficacy has led many to recommend intervention earlier and earlier in the course of the disease process. Mitral repair may include shortening of chordae, chordae transfers, wedge resection of redundant valve tissue, the insertion of a mitral annular ring to reduce the annular size, or some combination of these techniques. Stitching the middle of the leaflets together to create a double-orifice mitral valve is also used at times (Alfieri procedure) and can be performed percutaneously (MitraClip). A controversial hyperadrenergic syndrome has also been described (especially in young females) that may be responsible for some of the noncardiac symptoms observed. Some patients with mitral prolapse have findings of a systemic collagen abnormality (Marfan or Ehlers-Danlos syndrome). In many persons, the "degenerative" myxomatous mitral valve clearly leads to long-term sequelae and is the most common cause of mitral regurgitation in developed countries. Endocarditis prophylaxis is no longer recommended for most patients with mitral valve prolapse regardless of the degree of mitral regurgitation. A variety of percutaneous techniques and devices have been tried with some success, although results suggest that surgical repair is generally more durable. Epidemiology and pathophysiology of mitral valve prolapse: new insights into disease progression, genetics, and molecular basis. Floppy mitral valve/mitral valve prolapse syndrome: beta-adrenergic receptor polymorphism may contribute to the pathogenesis of symptoms. In mild or moderate cases where the valve is still pliable, an ejection click may precede the murmur and the closure of the valve (S2) is preserved. The characteristic systolic ejection murmur is heard at the aortic area and is usually transmitted to the neck and apex. In some cases, only the high-pitched components of the murmur are heard at the apex, and the murmur may sound like mitral regurgitation (the so-called Gallaverdin phenomenon). A delayed upstroke, though, is an unreliable finding in older patients with extensive arteriosclerotic vascular disease and a stiff, noncompliant aorta. A dilated ascending aorta, primarily due to an intrinsic defect in the aortic root media, may accompany the bicuspid valve in about half of these patients. Coarctation of the aorta is also seen in a number of patients with congenital aortic stenosis. Offspring of patients with a bicuspid valve have a much higher incidence of the disease in either the valve, the aorta, or both (up to 30% in some series). A second pathologic process, degenerative or calcific aortic stenosis, is thought to be related to calcium deposition due to processes similar to those that occur in atherosclerotic vascular disease. Approximately 25% of patients over age 65 years and 35% of those over age 70 years have echocardiographic evidence of aortic valve thickening (sclerosis). Certain genetic markers are associated with aortic stenosis (most notably Notch 1), so a genetic component appears a likely contributor, at least in some patients. Aortic stenosis has become the most common surgical valve lesion in developed countries, and many patients are elderly. Angina pectoris frequently occurs in aortic stenosis due to underperfusion of the endocardium. The common underlying measure of severe aortic stenosis is an aortic valve area of less than 1. In the same situation, super-severe aortic stenosis is defined as a mean gradient of greater than 55 mm Hg or peak aortic velocity greater than 5 m/sec by Doppler. Low flow (low output) in these situations is defined by an echocardiographic stroke volume index of less than 35 mL/min/m2. If the aortic valve area can be made to increase and a mean gradient of greater than 40 mm Hg cannot be demonstrated by inotropic challenge, the presumption is that the low gradient is due to an associated cardiomyopathy and not the aortic valve stenosis. Intervention is indicated in supersevere aortic stenosis even without demonstrable symptoms (grade C) and in any of the other situations when es kerrs oo k eb oo e//eb /t. The chest radiograph may show (1) a normal or enlarged cardiac silhouette, (2) calcification of the aortic valve, and (3) dilation or calcification (or both) of the ascending aorta. Likewise, the echocardiography/Doppler can estimate the stroke volume index used to define the low-flow state when the valve area is small but the gradient is less than 40 mm Hg. Cardiac catheterization mostly provides an assessment of the hemodynamic consequence of the aortic stenosis, and the anatomy of the coronary arteries. Catheterization data can be important when there is a discrepancy between symptoms and the echocardiography/Dopper information of aortic stenosis severity. In younger patients and in patients with high aortic gradients, the aortic valve need not be crossed at catheterization. Stress testing can be done cautiously in patients in whom the aortic stenosis severity does not match the reported symptoms in order to confirm the reported clinical status. For this reason, a Heart Valve Team approach bringing together invasive and noninvasive cardiologists, radiologists, anesthesiologists, and cardiac surgeons is mandatory; clinical factors (such as frailty) and anatomic features (such as a calcified aorta, vascular access, etc) can affect the decision making. Medical therapy to reduce the progression of disease has not been effective to date. None revealed any benefit on the the progression of aortic stenosis or on clinical outcomes despite the association of aortic stenosis with atherosclerosis. Efforts to reduce stenosis progression by blockage of the renin-angiotensin system have also been ineffective. In young and adolescent patients, percutaneous balloon valvuloplasty still has a small role. There are also times when asymptomatic aortic stenosis should undergo intervention. Following the onset of heart failure, angina, or syncope, the prognosis without surgery is poor (50% 3-year mortality rate). Medical treatment may stabilize patients in heart failure, but intervention is indicated for all symptomatic patients with evidence of significant aortic stenosis. The surgical mortality rate for valve replacement is low, even in older adults, and ranges from 2% to 5%. This low risk is due to the dramatic hemodynamic improvement that occurs with relief of the increased afterload. Mortality rates are substantially higher when there is an associated ischemic cardiomyopathy. In patients with a bicuspid aortic valve, there is an associated ascending aortic aneurysm in about half. It is also appropriate to intervene when the maximal aortic root size is greater than 5. The aortic valve may be replaced at the same time if at least moderate aortic stenosis is present or may be either left alone or repaired (valve sparing operation). In general, mechanical aortic valves are less subject to thrombosis than mechanical mitral valves. These devices are fundamentally stents with a trileaflet bioprosthetic valve constructed within them.