Discount ilosone 250mg otc
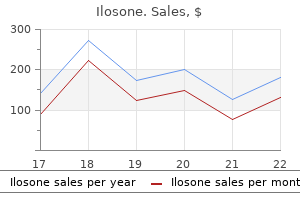
Chronic actinic damage is the most important factor symptoms food poisoning cheap ilosone 250 mg overnight delivery, particularly in pale-skinned races. In a recent series of 111 albinos from the black population of Johannesburg, approximately 23% developed skin tumors, mainly squamous cell carcinoma, particularly of the head. Viral oncoproteins exert their effects through functional inactivation of the p53 and Rb gene alike. Squamous carcinoma develops in up to 30% of patients, typically on sun-exposed skin. Immunosuppressed female patients have an increased risk of cervical intraepithelial neoplasia. In addition to arsenic (present in some insecticides, medications, and occasionally contaminating natural water supplies), a wide range of substances, especially hydrocarbons, have been incriminated. Chronic inflammation and chronic infection tumors complicating chronic infective and inflammatory (particularly scarring) conditions are now rare in developed countries. Differentiation is towards keratinization; it is therefore convenient to classify such tumors into well-differentiated, moderately differentiated, and Squamous cell carcinoma poorly differentiated variants. It is also important to remember that the tumor should be classified according to its most poorly differentiated region. Nuclear and cytoplasmic pleomorphism is more pronounced and mitotic figures (including abnormal forms) are much more commonly seen. In such instances, examination of multiple sections of tumor is frequently necessary to elicit the correct diagnosis. Squamous cell carcinoma an aid to differential diagnosis is unhelpful because many poorly differentiated squamous carcinomas express this intermediate filament, particularly spindle cell and acantholytic variants. Natural killer cells, mast cells, B lymphocytes, plasma cells, macrophages, and Langerhans cells are often present. In addition to reporting the histological subtype (see below) and degree of differentiation, a record of tumor maximum diameter and depth of invasion (measured from the granular cell layer of the surface epithelium if present) should be made. In a large series of such cases, 14% of tumors showed involvement of the perineural space, particularly spindle cell and acantholytic variants. Of particular importance is the distinction between squamous cell carcinoma and keratoacanthoma, discussed later in the chapter. Differentiation of squamous cell carcinoma from its precursor lesions depends upon examining sufficient numbers of sections to confirm the intraepidermal location of the latter conditions. In these cases, the correct diagnosis can only be made after careful examination of the surrounding tissues. Occasionally, squamous cell carcinoma may be confused with eccrine porocarcinoma, particularly as the latter may show bowenoid features. Spindled cell Microcystic adnexal carcinoma may be mistaken for an abundantly keratinizing squamous cell carcinoma, particularly if ductal differentiation is not obvious and especially if only shave or punch biopsy specimens are available. Variants of squamous cell carcinoma a number of variants of squamous cell carcinoma are of sufficient importance to merit individual attention. Clear cell and signet ring cell squamous carcinoma Clinical features Clear cell squamous carcinoma is a rare tumor that occurs primarily on the head and neck. Signet ring cell change showing compressed crescent-shaped and laterally displaced nuclei due to cytosolic glycogen accumulation is an exceedingly rare finding and this variant is also referred to as signet ring squamous cell carcinoma. Variants of squamous cell carcinoma 1125 Pathogenesis and histological features In the past, a spindled cell component in squamous carcinoma was thought to represent a pseudosarcomatous element or imply the presence of a collision tumor. On the basis of both immunohistochemistry and ultrastructural findings, this tumor is now recognized as squamous cell carcinoma showing fibroblastic and myofibroblastic differentiation. Very occasionally, a storiform growth pattern may result in confusion with dermatofibrosarcoma protuberans. Distinction from amelanotic clear cell melanoma can be difficult; numerous levels may have to be examined to find foci of more obvious squamous differentiation. If doubt remains, immunohistochemistry should readily establish the correct diagnosis. Clear cell atypical fibroxanthoma does not show cytokeratin or epithelial membrane antigen expression by immunohistochemistry and lacks squamous differentiation on morphology. More commonly, these tumors are actinically derived, present on the exposed surfaces (particularly the scalp and face), and are associated with a good prognosis, recurring infrequently and metastasizing rarely. Spindle cell squamous cell carcinoma with poor prognosis has also been reported in immunosuppressed patients following solid organ transplantation. Diagnosis in lesions such as this is often one of exclusion, and immunohistochemistry is frequently essential. Immunohistochemical studies usually disclose keratin positivity and often eMa is at least focally present. Spindle cell squamous carcinoma must be distinguished from spindle cell melanoma, cutaneous leiomyosarcoma, sarcomatous and pseudosarcomatous (carcinomatous) metastases and atypical fibroxanthoma. It accounts for approximately 7% of invasive tumors and is characterized by an increased risk of local recurrence (27. It affects the elderly with a marked male predominance and presents on sunexposed skin with a predilection for the head and neck. It is frequently ulcerated, flesh-colored, and nodular and largely confined to the head and neck. Differential diagnosis acantholytic squamous carcinoma must be distinguished from metastatic carcinoma and adenosquamous (mucoepidermoid) carcinoma of the skin. From the small number of cases reported so far, mucoepidermoid carcinoma of the skin appears to be a high-grade neoplasm commonly associated with nodal and systemic spread. Pseudovascular squamous cell carcinoma one-third of the invasive squamous cell carcinoma. Involvement of the oral cavity as well as the genital area of both vulva and penis has also been documented. Multifocality, a feature typically seen in cutaneous angiosarcoma, is not present in pseudovascular squamous cell carcinoma, and the endothelial cells lining the stromal vessels are invariably normal. Immunohistochemistry reveals keratin positivity and the majority of cells are outlined by epithelial membrane antigen. In contrast to cutaneous angiosarcoma (particularly the epithelioid variant with which this. Adenosquamous carcinoma/ mucoepidermoid carcinoma of skin Clinical features primary cutaneous squamous cell carcinoma with glandular differentiation is a rare but aggressive neoplasm that has been variably referred to as adenosquamous or mucoepidermoid carcinoma when resembling its counterpart in salivary gland. The possibility that this represents skin involvement by an underlying salivary gland tumor cannot be excluded. Glandular differentiation is appreciated as intracytoplasmic vacuoles, which coalesce to form luminal spaces. Glandular differentiation is more common in the deeper reaches and may be focal or widespread within the tumors. Nuclear pleomorphism and mitotic figures are frequent features in both the squamous as well as glandular areas. Special stains for mucin including mucicarmine or alcian blue and immunohistochemistry for Cea highlight areas of glandular differentiation. While an adnexal origin has to be considered, most authors regard this tumor as a variant of squamous cell carcinoma with divergent differentiation. Microcystic adnexal carcinoma enters the differential diagnosis but typically lacks marked cytological atypia, and mitoses are often sparse. Verrucous carcinomas occasionally arise in the sinuses of chronic osteomyelitis, at the site of chronic cutaneous tuberculosis, as a complication of ulcerative leprosy, in association with psoriasis or lichen planus, areas of scarring, dystrophic epidermolysis bullosa, chronic pressure ulcers, and hypospadiasis. Keratinization is usually massive and when accompanied by necrosis gives rise to the sinuses so characteristic of this tumor. Intraepithelial abscesses are common and a heavy chronic inflammatory cell infiltrate is often evident in the adjacent lamina propria or dermis.
Discount 250mg ilosone amex
Histological features acral lentigines are histologically identical to lentigo simplex medications japan order line ilosone. Multiple lentigines syndrome this disorder is discussed under disorders of pigmentation. Histological features actinic lentigo usually develops against a background of solar elastosis. Actinic lentigo: note the hyperkeratosis and hypergranulosis with extension of the epidermal ridges forming clublike processes. Ink spot lentigo In some examples, epidermal proliferation may lead to a reticular pattern due to the formation of anastomoses between adjacent attenuated ridges. Some (but not all) authors believe that actinic lentigo may evolve into large cell acanthoma (see tumors of the surface epithelium). Similar lesions have occasionally been described in patients, including one with systemic lupus erythematosus, following the use of sunbeds for artificial tanning. Melanocytic nuclear atypia including enlargement, pleomorphism, and hyperchromasia, multinucleation, and giant melanosomes has been described. Lesions on the scalp or face can be associated with asymmetrical growth of scalp hair or beard. A very slight chronic inflammatory cell infiltrate surrounds the vessels of the papillary dermis. In occasional lesions the reticular dermis contains large numbers of hamartomatous, irregular, enlarged smooth muscle fibers. Melanocytic nevus Melanocytic nevus (banal nevus) is a benign tumor that usually presents in childhood and adolescence. Further development results in a completely intradermal lesion called the dermal nevus. It has been estimated that the likelihood of any one nevus evolving into melanoma is roughly 1/100 000. Conjunctival junctional melanocytic nevus: there is uniform pigmentation and a regular border. In young children and adolescents in whom these lesions are at an early stage of development, increased pigmentation is to be anticipated. Clinical features Melanocytic nevi first appear in early childhood and increase in number during the second and third decades. Melanocytic nevi present a variety of features depending upon their stage of evolution. Occasionally, there are coarse hairs projecting from its surface; plucking these hairs may traumatize the dermal component of the hair follicle, resulting in granulomatous inflammation, which may cause concern to both the patient and clinician as to the possibility of malignant transformation. Nevi may become more highly pigmented under the influence of pregnancy or the oral contraceptive pill. It has the same electron microscopic appearance as a melanocyte, and identical organelles and enzyme systems; the only significant differences are that the dermal component lacks dendritic processes and with increasing depth melanin synthesis is arrested. It should, however, be noted that a shoulder can sometimes be present in a banal compound nevus, i. Compound nevi may sometimes be associated with marked hyperkeratosis, acanthosis 1160 Melanocytic nevi. The junctional nests are present at their tips, a characteristic location in banal nevi. Mitotic activity can occasionally be seen in the dermal component of an acquired melanocytic nevus (see differential diagnosis). In some dermal nevi, there may be worrying nuclear pleomorphism and hyperchromatism. In addition, they are S-100 and dopa positive and do not show Schwann cell morphology, nor do they react with antibodies to myelin basic protein. Immunohistochemical studies using endothelial cell markers are invariably negative. Differential diagnosis Distinction between a banal nevus and melanoma in the majority of cases is straightforward. Low-power examination of melanoma may reveal obvious intralesional transformation, i. Upward, intraepidermal or pagetoid spread of melanocytes is an additional feature seen in many melanomas. Caution, however, is advised when viewing sections from neonatal and even childhood nevi when nests and occasionally single cells, sometimes showing mild or even severe cytological atypia, may be identified within the upper reaches of the epidermis (see neonatal nevus). Careful inspection, however, reveals asymmetry and lack of circumscription, multiple dermal mitoses, subtle lack of maturation, and nucleolar prominence (see nevoid melanoma). Small cell melanoma cells, although often of a similar size to type B nevus cells, usually have prominent eosinophilic nucleoli and mitoses are invariably present (see small cell melanoma). Difficulties are sometimes experienced in differentiating invasive melanoma (particularly the nevoid and small cell variants) from residual benign intradermal nevus cells. In melanoma, they are usually much more numerous and often they are present throughout the thickness of the lesion. Clonal nevus Clinical features Many so-called clonal nevi (inverted type a nevi) are clinically unremarkable. One or two residual nests of nevus cells are evident in the top-left corner of the field (arrowed). Differential diagnosis the vast majority of clonal nevi most likely represent combined or deep penetrating nevi. Melanocytic nevi with a focal atypical epithelioid component (clonal nevus) share similar age, anatomic distribution, and cytological features with the deep penetrating nevus, but lack the deep extension of melanocytes. Eccrine centered nevus Clinical features eccrine centered nevus (spotted grouped pigmented nevus) is a rare variant of melanocytic nevus, and has been mainly described in the Japanese. Dermal nevus: invagination of nevus cells into the lumen of a vessel should not be confused with true vascular invasion. Distinction depends upon identification of a layer of endothelial cells covering the surface of the nevoid aggregate, as shown in this example. Their presence, however, should be viewed with considerable concern and other mitoses or additional features indicative of melanoma sought. Histological features the nevus is characterized by a striking syringocentric distribution. Melanocytic nevi at special sites Nevi at special sites usually show histological features identical to nevi seen elsewhere. Note the distinct nodule in the deeper dermis surrounded by pigment-laden melanophages. In addition, melanocytic nests show variation in shape, with frequent bizarre forms and discohesion of tumor cells within them. Focal lentiginous proliferation along the dermoepidermal junction is frequently present. Melanocytic atypia is usually mild (although occasionally severe cytological atypia is present) and random, and consists of hyperchromatic nuclei and indistinct nucleoli. Upward migration of isolated melanocytes can sometimes be seen in the central part of the lesion. Scalp nevus: lesions at this site may on occasions show cytological features that can raise concern for a diagnosis of melanoma by the unwary. Nevi in and around the ear Nevi in and around the skin of the ear demonstrating disturbing histological features are usually indistinguishable from banal nevi on clinical grounds. Upward migration of single melanocytes into the lower third of the epidermis can be seen. Nevi of the breast Nevi can occur anywhere on the breast, including in and around the nipple. Unusual histological features appear to be more common in young adults than in elderly patients. Melanocytes are enlarged with clear to dusty cytoplasm and dendritic forms Histological features peculiar histological features of nevi at flexural sites include enlarged junctional nests, variation in the size and shape of nests, confluence of nests, and diminished cohesion of melanocytes within the nests. Focal fibrosis at the tips of the rete ridges, often of the lamellar type, can be seen. Differential diagnosis Distinction from dysplastic nevus is made by the absence of the stromal response, typically seen in dysplastic nevi, including lamellar or concentric fibrosis and vascular proliferation. Acral nevus Clinical features acral palmar and plantar nevi may be symmetrical, well circumscribed, and identical to banal melanocytic or congenital nevi as seen at any other site, or they may be asymmetrical, poorly circumscribed, and a source of diagnostic difficulty, both clinically and pathologically. Mild to moderate pagetoid spread is not uncommonly present, particularly in the center of the nevus.
Buy ilosone 250 mg
Differential diagnosis pemphigus vulgaris can be readily distinguished by the clinical history and the characteristic presence of intercellular IgG deposition on direct immunofluorescence lanza ultimate treatment purchase ilosone without a prescription. Mild involvement comprises minute white or pink keratotic papules, while in more extensive disease coalescence results in larger plaques or a cobblestone surface. Pathogenesis and histological features theories of origin include ossification of branchial arch remnants, metaplastic bone formation secondary to trauma, and osteogenesis of unknown cause from pluripotent mesenchymal cells in the area. Some authors believe that cartilaginous rests of the soft palate/tonsillar area are a metaplastic phenomenon, occurring in 20% of tonsils examined. Cartilaginous choristoma Clinical features Cartilaginous choristomas present as discrete nodules, usually along the lateral border of the tongue (85% of cases) and less often on the buccal mucosa and soft palate. Cartilaginous choristoma consists of a mass of benign mature hyaline cartilage surrounded by dense perichondrium; loose myxoid tissue akin to primitive mesenchyme or even mature fat may also be present. One theory suggests that they arise from entrapped epithelial rests in the line of fusion of facial processes. Pathogenesis and histological features Heterotopic brain tissue Clinical features this uncommon condition presents in the first year of life, most often affecting the palate, tongue (especially the foramen cecum area) or oropharynx, as a result of displacement of primitive neural elements in an early stage of development or neuroglial differentiation from pluripotent cells. Histological features Mature elements of the central nervous system including astrocytes, oligodendrocytes, ependymal tissue, choroid plexus-like tissue and, rarely, neuronal tissue may all be identified. Intraoral lesions cause feeding, swallowing, and speech difficulties while extraoral variants below the myohoid muscle lead to a noticeable submental mass. Tumor-like lesions teratomas, teratoid tumors, and epignathi present as masses that may protrude from the mouth, and airway obstruction is a frequent presenting symptom; there is a female predilection and most are present at birth. Some authors consider lesions which present at sites where tonsillar tissue is normally found to be inflammatory/obstructive tonsillar reactions. In addition, cartilage, bone, muscle, adipose tissue, and even salivary glands may be present. In addition, neural, brain, lung, gastrointestinal, and respiratory tissues are sometimes present. Some cases demonstrate communication with the overlying surface epithelium, often through a narrow opening. Salivary glands and ducts may be present in the vicinity, especially floor of mouth lesions. Pathogenesis and histological features Since the thyroid anlage develops in the area of the foramen cecum and descends from there into the neck, failure to descend or persistence of remnants of the anlage which then proliferate, resulting in a noticeable mass. In most cases, a biopsy is not indicated if technetium scans are positive for thyroid tissue. Clinical features the congenital granular cell tumor presents as a pink, pedunculated mass, usually on the anterior alveolar ridge with an intact surface. Dermoid and epidermoid cysts lack the lymphoid mantle, and dermoid cysts contain adnexa in their wall. Masses and clumps of bacteria may mat together and plug tonsillar crypts, presenting as an opaque yellow mass that is not covered by epithelium and that can readily be scraped off. Tumor-like lesions 371 Gingival fibromatosis Clinical features In this condition, there is a benign, diffuse, nonhemorrhagic, and fibrotic gingival enlargement, often occurring bilaterally and involving the maxillary and mandibular gingiva, sometimes to the extent that it may reach the occlusal/ incisal edges of the teeth. Gingival fibromatosis may also be a feature of Zimmerman-Laband, ramon, rutherford, and Cross syndromes. Native fibroblasts show elevated rates of proliferation and increased synthesis of fibronectin and type I collagen. Congenital gingival leiomyomatous polyp/hamartoma has a similar clinical presentation (usually in the midline of the maxilla) but histologically contains a nonencapsulated proliferation of fusiform and spindle smooth muscle cells that, as expected, express hhF-35, smooth muscle actin, and desmin but not S-100 protein. Lymphangioma of the alveolar ridge Clinical features Lymphangioma has been identified in approximately 4% of infants, all of whom were black. Females are twice as likely to be affected as males and 74% of subjects have more than one lesion. Differential diagnosis Lymphangioma circumscriptum has an identical histology but is seen in older patients. Pathogenesis and histological features It is generally believed that a low-grade topical injury, such as occurs with the use of tobacco or coca leaves, gives rise to this condition. Ultrastructural studies show abnormal keratohyaline granules and loosely dispersed tonofilaments with fragmented organelles in the superficial degenerated cells. Smokeless tobacco keratosis presents with keratin chevrons and shows a band of coagulated and degenerate cells with anucleation similar to leukoedema. Morsicatio mucosae oris/Factitial keratosis Clinical features In morsicatio mucosae oris (pathominia mucosae oris), cheek, lip or tongue chewing habits occur either subconsciously at night or as a conscious parafunctional habit. It is usually seen in adults, is often bilateral and may involve the buccal mucosa (most common), lateral tongue and lower labial mucosa. Characteristically, the keratin is thrown into papillations with fissures and clefts, rimmed by bacteria. Ballooned and swollen superficial keratinocytes typical for leukoedema are present. Inflammation in the lamina propria is insignificant unless there is erosion and ulceration. In betel nut chewers, there is a yellowbrown pigment on the surface of the keratin and within epithelial cells, representing fragments of the betel quid. Smokeless tobacco keratosis shows sharply demarcated coagulation of the superficial cells, sometimes accompanied by hyalinized, amorphous eosinophilic material in the lamina propria. Clinical features these are white, often rough papules and plaques that occur on the crest of the alveolar ridge, in particular in the area of extracted mandibular third molars and adjacent retromolar pad. Lesions reported as alveolar ridge keratosis are any white lesion on the alveolar ridge and gingiva with no histologic connotations and include both benign and dysplastic/malignant keratotic lesions of the gingiva and alveolar ridge; they are not synonymous with benign alveolar ridge keratosis, which has the specific histologic appearance of lichen simplex chronicus. Lesions from the retromolar pad often contain stellate-shaped fibroblasts, which are normal for that area. Differential diagnosis Verrucous hyperplasia may have a similar histology and often occurs on the gingiva or alveolar ridge. Lithium carbonate (which can exacerbate psoriasis) has also been reported to precipitate migratory glossitis. Differential diagnosis Candidiasis, which must always be excluded, more typically presents with spongiotic pustules affecting only the top two to three layers of keratinocytes. Oral lesions of patients with cutaneous psoriasis are histologically indistinguishable from lesions of benign migratory glossitis. Median rhomboid glossitis is a form of oral candidiasis that occurs specifically in the midline of the tongue just anterior to the circumvallate papillae. It is unclear why this particular area of the tongue is predisposed to candidiasis. Lesions show a characteristic pale-staining surface layer of coagulated and degenerate, often anucleate, cells occasionally covered by a thin layer of parakeratin. Foreign body gingivitis Clinical features this condition occurs more often in females than in males (4:1), usually in the fifth decade. It is therefore thought that some of these cases result from such abrasives forced into the gingiva during professional dental cleaning. In one-quarter of cases, granulomatous inflammation may be seen, sometimes accompanied by foreign body and/or Langhans-type giant cells. Foreign bodies, ranging from 1 to 5 microns in diameter, are present in all cases, and 44% may be refractile. Histological features there is epithelial hyperplasia, sometimes accompanied by papillomatosis, and spongiosis. Characteristically, neutrophilic and eosinophilic abscesses are present in the connective tissue papillae at the interface, and sometimes within the epithelium itself. When positive, the staining is usually weak and represents a secondary reaction to epithelial inflammation and damage rather than a primary autoimmune phenomenon.
Generic 500mg ilosone fast delivery
It is more likely treatment hyperkalemia purchase 500 mg ilosone free shipping, however, that lesions in both men and women derive from ectopic urogenital sinus epithelium. Histological features the cyst is lined by a single layer of cuboidal or columnar nonciliated cells surrounded by a layer of smooth muscle. It arises on the upper and lateral aspect of the labium majus at the level of the insertion of the round ligament. Histological features Microscopic examination reveals a unilocular cavity lined by a single layer of flattened mesothelial cells. Histological features Biopsies from early lesions show mild to moderate epidermal hyperplasia with no cytological atypia and a variable focal lichenoid mononuclear inflammatory cell infiltrate. Larger lesions display pseudoepitheliomatous hyperplasia and often there is transition to verrucous carcinoma. It is now appreciated that histologically the two conditions are indistinguishable. It is usually a small hyperkeratotic white papule or plaque or a punched-out ulcer or erosion with a firm border. Multifocal vulval and perianal lesions are strongly associated with the oncogenic papilloma viruses, particularly hpV-16 and -18, and almost exclusively occurs in smokers. It has been suggested that hpV-positive tumors have a worse prognosis than those that are hpV negative. One study describes a distinctive triad of marked epithelial acanthosis, loss of the granular cell layer with superficial epithelial cell pallor, and multilayered parakeratosis. Lesions vary from flat to slightly elevated, and can be pearly white or moist erythematous, dark brown or black and present as macules, papules, or plaques. Basaloid lesions are monotonous and flat, whereas warty lesions are spiky and pleomorphic with prominent koilocytosis. It is not surprising that the precursor lesions of well-differentiated invasive tumors show such a high degree of differentiation. It is important to recognize this lesion because it appears to be the most frequent precursor lesion of penile carcinoma, especially of the keratinizing and well-differentiated variants. In accordance with their common pathogenesis, it is frequent to find mixtures of warty and basaloid patterns in the same specimen. We classify a lesion as either warty or basaloid when there is more than 90% predominance of one type over the other. If an associated invasive cancer is present it also shows mixed morphology of more than one subtype of invasive squamous cell carcinoma. Other exceptional and less well-studied morphologic patterns of precursor lesions include pleomorphic, spindled cell, clear cell, pagetoid and small cell. With few exceptions there is good correlation between the microscopic appearance of the preinvasive lesion and the associated invasive carcinoma. Bowenoid papulosis patients with bowenoid papulosis are younger (mean age 30 years) than those with penile cancer and present with multiple papules affecting the skin of the shaft, glans, sulcus or foreskin. Follow-up of 118 men with flat lesions showed a benign clinical course and regression in 90% of the cases in 5 years, usually within 12 months. In non-Western countries, up to 40% of patients present with inguinal lymph node metastasis and 10% with disseminated disease. In areas of high frequency, the majority of tumors are initially dignosed as invasive tumors whereas in regions of low incidence, most cases are diagnosed as in situ lesions. Invasive squamous cell carcinoma Squamous cell carcinoma arises on the mucosal surface of the penis extending from the preputial orifice to the urethral meatus, comprising the inner surface of the foreskin, coronal sulcus and glans. Distal urethral tumors, morphologically similar to some penile tumors, are not discussed in this text. In the fresh state or after fixation there may be a contrast between the white color of the tumor and the reddish, darker penile tissue. When these features predominate, there is a morphological justification for separation of the neoplasm as a special subtype of squamous cell carcinoma. Genital intraepithelial neoplasia and squamous carcinoma 499 Subtypes of squamous cell carcinoma Table 12. Lauren ackerman in 1948 in the buccal mucosa, verrucous carcinoma continues to pose diagnostic problems with other verruciform tumors sharing some of its characteristics. We have proposed a classification of verruciform neoplasms that helps to differentiate verrucous carcinoma from other similar lesions. Most tumors are unicentric but multicentric cases or association with other subtypes such as the pseudohyperplastic variant has been observed. Grossly, it is an exophytic papillomatous tumor with some variation in the configuration of the papillae, from multinodular with cobblestone morphology to filiform with a spiky appearance. Verrucous carcinoma is superficial, rarely penetrating beyond lamina propria or superficial dartos or corpus spongiosum. Histological features Microscopically, the tumor is diffusely well differentiated, resembling nomal squamous epithelium except for the presence of occasional atypical nuclei in the basal or parabasal layers. Features include papillomatosis, hyper- to orthokeratosis, acanthosis and a broad-based interface between the tumor and stroma, the latter considered pathognomonic for this tumor. Lichen sclerosus is a further frequently found associated condition and may be pathogenetically related to verrucous carcinoma. Condylomatous (warty) carcinoma Clinical features Condylomatous carcinoma is a slowly growing, verruciform low- to intermediate-grade hpV-related tumor, grossly similar to giant condyloma but with malignant histology and potential for nodal metastasis. Unlike benign condyloma, koilocytosis is not restricted to the surface epithelial cells but is also present in deep invasive portions of the tumor. Deeply invasive, high-grade condylomatous carcinoma may be associated with inguinal nodal metastasis. Koilocytosis, condylomatous papillae and jagged irregular boundaries between tumor and stroma are present in warty but not in verrucous carcinomas. Giant condylomas are broadly based noninvasive tumors with surface koilocytosis (see Table 12. Microscopically, the appearance is that of a well-differentiated papillary squamous neoplasm. Differentiating features from verrucous and condylomatous carcinoma are based on the heterogeneity of the papillae, the lack of koilocytosis and the jagged irregular interface between tumor and stroma. Low-grade squamous intraepithelial lesion and lichen sclerosus are frequently associated with papillary carcinoma. Occasional palisading at the nest periphery may be noted but it is usually not as prominent as is seen in basal cell carcinoma of the skin. Unlike other penile papillary tumors, the papillae are entirely composed of small cells simulating a transitional urothelial carcinoma. Sarcomatoid carcinoma (carcinoma with heterologous differentiation, metaplastic carcinoma) Clinical Features Sarcomatoid carcinoma is an aggressive penile neoplasm composed predominantly of spindled cells. It may arise de novo, follow a recurrence of usual squamous cell carcinoma or develop after irradiation therapy of a verrucous carcinoma. Histological features Microscopically, there are variable proportions of squamous and spindled cell carcinoma but the latter usually predominates. Immunohistochemistry is essential for tumors with little or no epithelial component and for small biopsy specimens. In our experience, cytokeratin 34betae12 and p63 appear to be the more specific and sensitive markers to categorize these tumors as epithelial. Smooth muscle actin can be focally positive; however, desmin, muscle-specific actin, myogenin and S-100 are negative. It is often multicentric and the second or third independent lesion is sometimes verrucous. We have observed similar cutaneous tumors in association with severe solar elastosis or in scars after burns. In a series of 10 cases, recurrence was noted in the glans of one patient who was circumcised for a multicentric carcinoma of the foreskin 2 years after diagnosis. Histological features Characteristic microscopic features are keratinizing nests of squamous cells with minimal atypia surrounded by a reactive stroma.
Cheap ilosone 250mg on-line
Reticulohistiocytoma Clinical features reticulohistiocytoma is a rare benign conjunctival lesion that usually occurs as an isolated skin nodule or as part of multicentric reticulohistiocytosis cold medications discount generic ilosone canada, a systemic disorder. Histological features histologically, the features of herniated fat were originally mistaken as representing pleomorphic lipoma. Floret giant cells are not uncommon in periorbital fat, as demonstrated in orbital exenteration specimens. Similarly pleomorphic, hyperchromatic cells adjacent to fibrous septa as seen in well-differentiated liposarcoma are absent. Symptoms include conjunctival masses or irritation, and, less commonly, ptosis, epiphora, blurred vision, proptosis, and diplopia. Most conjunctival lymphoid tumors are located 1292 Tumors of the conjunctiva Histological features Because differentiating between benign and malignant conjunctival lymphoid tumors by clinical examination is not possible, biopsy is necessary to establish the diagnosis. It may focally or diffusely infiltrate the substantia propria, occur on the bulbar or palpebral conjunctiva, and cause microvascular changes due to hyperviscosity (leukostasis) from markedly elevated leukemic cell counts. Conjunctival lesions have been reported as the presenting manifestation of acute leukemia in patients who were not recognized as having the condition; in other patients, conjunctival lesions have signified disease relapse. Conjunctival leukemic involvement is consistent with good visual acuity, with no reports of vision reduction associated with conjunctival infiltration; however, it has a poor prognosis, with a median survival of three months. There is an isointense mass wrapping around the right eye: A: coronal section; B: axial section at a level above the globe; C: axial section at the middle of the eye; D: sagital section showing that the bulk of the mass is more prominent inferiorly. Choristoma Choristomas are congenital lesions which represent normal tissue growing in abnormal locations. Local treatment is usually effective, but possible recurrence at extranodal sites warrants semiannual systemic evaluation. Other factors include the stage of the disease at first presentation and the lymphoma subtype. It usually contains dermal elements such as hair follicles, sebaceous glands, sweat glands, and occasionally fat tissue. Dermolipoma Clinical features Dermolipoma is a soft, yellowish tan fusiform tumor that is usually localized to the temporal or superotemporal aspect of the conjunctiva near the lateral canthus. Clinical features epibulbar osseous choristoma is a rare solitary congenital lesion that generally presents as an isolated epibulbar lesion in the superotemporal quadrant 1294 Tumors of the conjunctiva. Complex choristoma Clinical features Complex choristomas are congenital, unilateral lesions that contain tissue derived from ectoderm and mesoderm germ layers. Large, pedunculated masses protruding through the eyelid aperture have been reported. Lacrimal gland choristoma Clinical features epibulbar ectopic lacrimal gland choristoma is a simple choristomatous congenital lesion that presents as a pink, asymptomatic stromal mass, typically in the superotemporal or temporal regions of the conjunctiva. Metastatic carcinomas are fleshy, vascularized stromal tumors that are yellow or pink in color, while metastatic cutaneous melanoma may be pigmented. Conjunctival metastases are treated by excisional biopsy, radiotherapy, and chemotherapy. Metastatic and secondary tumors 1295 Secondary tumors the conjunctiva may be secondarily involved by extraocular extension of intraocular tumors and by extension of eyelid and orbital tumors. Ciliary body melanoma, extending through the sclera into the subconjunctival tissue, may simulate conjunctival melanoma. Orbital tumors, such as rhabdomyosarcoma in children, may first present in the conjunctiva. Tumors of the caruncle the caruncle (Latin caro, flesh) is a soft, pink, ovoid body about 5 mm high and 3 mm broad situated in the lacus lacrimalis medial to the plica semilunaris. Because of the histological composition of the caruncle, which includes cutaneous elements such as hair follicles, sebaceous glands, sweat glands, and accessory lacrimal tissue, the caruncle may develop lesions similar to those found in the skin, conjunctiva, or lacrimal gland. Lymphoscintigraphy, in which a radioactive isotope, such as 99mtc antimony sulfide, is injected around the site of a primary tumor, reliably identifies the lymph node basin(s) that receive lymph from that specific site. Laboratory management and gross evaluation of sentinel nodes the location of that node can then be marked on the overlying skin. Contralateral dye injections Dye drains to lateral nodes (10/10) most accurate staging technique available for melanoma. More sentinel node procedures are currently performed for breast cancer than for melanoma. Sentinel node tumor status also assists in determination of the need for immediate completion lymph node dissection. Dyeinjectedinthe lower lateral abdomen, the suprapubic are,a and the upper medial thigh passed reliably to the lateral, medial, and middle lymphnodesrespectively. Laboratory management and gross evaluation of sentinel nodes Sentinel nodes arrive at the laboratory, fixed or fresh, as a single cleanly dissected lymph node, a single node in a mass of fat or as multiple nodes embedded in fat. Larger nodes may need to be cut more extensively, but additional slices should be cut parallel to the initial cut and parallel to the meridian. Such a reagent would allow pathologists to confirm the actual status of nodes claimed to be sentinel. Drug regulations vary from country to country and widespread use of this interesting and potentially valuable technique must await the clearance of substantial regulatory hurdles. Such meetings, conducted in good faith, will usually allow the development of a mutually acceptable approach. For example, we have on occasion been willing to provide interleaved sections with one section going for histology and the next for research. Thelowerthree parts show the identical sequence,butwithcarbon particles added to the bluedye(D). Incontrastto the blue dye, the carbon particles persist in the node(EandF),confirming its sentinel status and indicate the point of entry of the afferent lymphatic where tumor cells are most likely to be detected, (B)carbonparticlesfree and within macrophages in a lymph node that receivedlymphfromthe siteofablacktattoo. Interpretation of such preparations can be challenging if the melanoma cells are few in number or small and nevocytically differentiated and the opinion of an experienced cytopathologist is likely to be necessary. Some are due to misidentification of a nonsentinel node as sentinel during lymphoscintigraphy or at surgery. In this study, additional sampling of more peripheral areas of the node did not increase the proportion of melanoma-positive lymph nodes. In choosing a protocol for sampling sentinel nodes, pathologists, in consultation with their surgical colleagues, should balance the need for accuracy with cost and workload considerations. For this reason, and to minimize delays in reporting, immunohistochemical studies are best ordered at the time of initial processing. It is important to be selective in choosing the antibodies to be used in this evaluation. Melanoma cells can be dendritic, but this morphology is usually observed in the radial growth phase of lentiginous melanomas and is exceedingly rare in vertical growth phase melanoma or metastatic melanoma. The role of immunohistochemistry in the detection of tumor in sentinel nodes 1303 A Nevocytes in lymph node capsule B Nevocytes in trabeculum of lymph node. Intheabsenceofspecial staining it may be incorrectly assumed that such cells are free within the nodal parenchyma and they may be incorrectly interpreted asmelanomametastases. C Nevocytes in arborized trabeculae of lymph node more specific for cells of melanocytic lineage than S-100 but are not expressed by the cells of up to 25% of melanomas, particularly those of metastatic melanomas. Other potential sources of false-positives are S-100-positive Schwann cells of intranodal and perinodal nerves. Distinction of these potential confounding cells is usually achieved by scrutiny of their cytology, location in or adjacent to the lymph node, and immunophenotype. The role of immunohistochemistry in the detection of tumor in sentinel nodes 1305 A B C. We have recently encountered an unusual potential cause of a false-positive interpretation of a sentinel node in patients where a small piece of melanoma is included on the slide as a positive control. In rare instances, cells from the positive control tissue may detach and float over to settle on top of the section under evaluation. Melanoma cells are usually larger than nevus cells (though the occasional nevoid melanoma may present a considerable diagnostic challenge) and are commonly located in the subcapsular sinus and deeper lymphoid tissues of the node. Unlike nevus cells, melanoma cells are seldom present in the nodal capsule other than within afferent lymphatics. Cytological features that may be used to distinguish melanoma from nevus cells include large cell size, high nuclear to cytoplasmic ratio, prominent nucleoli, and mitotic figures (especially atypical mitoses). Both melanoma and nevus cells may contain finely dispersed small granules of melanin (single melanized melanosomes that are just visible under the microscope) that indicate melanin synthesis within the cell.
Papoose Root (Blue Cohosh). Ilosone.
- Are there any interactions with medications?
- Inducing labor and menstruation, use as a laxative, stomach cramps, sore throat, hiccups, and seizures.
- What is Blue Cohosh?
- Dosing considerations for Blue Cohosh.
- How does Blue Cohosh work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96948
Cheap 250mg ilosone
At the first egress of urine from the catheter treatment brown recluse bite generic ilosone 250mg otc, the balloon is just passing through the membranous urethra. The catheter balloon still has approximately 3 to 4 cm to go before clearing the bladder neck. Inflation of the Foley balloon at any point before full insertion of the catheter might result in iatrogenic urethral injury. The male urethra is relatively fixed at the level of the urogenital diaphragm and symphysis pubis; traction downward on the penis kinks and promotes urethral folding at the level of the penile suspensory ligament. For this reason, the penis should always be held taut and upright during any urethral instrumentation, including catheterization. The catheter then needs to make only a single curve rather than a complex S-curve as it traverses into the bladder. Male Catheterization Female Catheterization the female urethra is a short (~4 cm) straight tube, usually of wide caliber, lying on top of the vagina. It must be approached between the double labia, and the urethral meatus is occasionally hidden and not obvious. If the female patient nervously adducts her legs, successful catheterization will be very difficult if not impossible. The female urethral meatus is oval but may appear as an anteroposterior slit with rather prominent margins situated directly superior to the opening of the vagina and approximately 2. The urethral meatus is directly superior to the vaginal introitus and approximately 2. The male urethra is approximately 20 cm long from the meatus to the neck of the bladder. Thus, it is essential to advance the urethral catheter to the hilt before balloon inflation to avoid urethral injury. B, In a patient with a cystocele/urethrocele or prolapsed bladder, the normal anatomy may have to be re-created for passage of a catheter. Penis Prostate A Indications Urinary catheterization and instrumentation are rarely a primary cause of urinary infection in otherwise healthy patients who urinate normally and carry small amounts of postvoid residual urine. As with any procedure, catheterization needs to be limited to those clinical situations in which the benefits outweigh the risks. Intermittent bladder catheterization in patients with neurogenic bladder dysfunction. Contraindications Urethral catheterization should be avoided when other less invasive procedures will be equally effective and informative. This will halt the advancement of a catheter, even though there is no other anatomic blockage. In the setting of a severely fractured pelvis or diastasis of the pubic symphysis, urethrogram should always precede attempts at catheterization. Check the list of contents before opening the tray because some trays do not include certain items. For most routine adult in-and-out catheterizations, a 14-Fr red rubber catheter or Foley balloon catheter is adequate. In neonates or infants, a small feeding tube taped in place produces the least amount of urethral trauma. If immediate bladder access is required in any emergency, suprapubic placement of a Foley balloon catheter using the Seldinger technique can be performed (as described in the later section on Suprapubic Cystostomy). In the uncircumcised or partially circumcised male, control of the penile foreskin is paramount to ensuring success. This will prevent the tendency for lubricant-associated normal anatomic foreskin reduction during catheterization and provide a continuously dry and sterile field. This position leaves the nondominant index finger and thumb available for manipulating the catheter. After exposing the urethral meatus in the female and the glans penis and urethral meatus in the male, use an antiseptic solution soaked into cotton balls or oversized cotton-tipped applicators to cleanse the exposed meatus and surrounding tissues. This is best done by hand but can also be done using the plastic forceps in the catheterization tray. For patients with gross hematuria, a large (20 Fr and up) threeway catheter is ideal because it allows continuous bladder irrigation and its large diameter allows the passage of blood clots. It features a semirigid curved tip that helps the catheter traverse the median lobe of the enlarged prostate gland. Your nondominant hand is now contaminated and should not let go of the penis or handle sterile equipment until the insertion has been completed. Hold the penis taut and upright with your nondominant hand while you pass the catheter into the urethra. Advance the catheter to the hilt before inflating the balloon with the recommended amount of air or water. If there is obvious resistance or patient discomfort, immediately deflate and reevaluate the position of the catheter. Affix the catheter to the thigh with tape or a catheter-specific attachment device. Rates of 1 to 2 L/hr are acceptable, provided that the amount of irrigant drained equals the amount infused. This hand is now considered contaminated and should not release the labia or handle sterile equipment throughout the procedure. If the catheter accidentally enters the vagina, it should be discarded and a new one used (to prevent iatrogenic infection). Lubricate an appropriately sized catheter (14- to 16-Fr is commonly used in adults) with viscous rather than inspissated lubricating jelly. Injection of the male urethra with 5 mL of 2% viscous lidocaine or a syringe filled with anesthetic lubricant can be helpful for topical anesthesia and urethral distention. Regardless, advise the patient of mild urethral discomfort and the potential urge to void. Gently pass the catheter by hand, or with the aid of a hemostat or plastic forceps, into the urethra and upward into the bladder. During slow, gentle passage of the catheter, be aware of the anatomic considerations discussed previously. After passing the catheter fully in all male patients, slowly inflate the balloon with 10 mL of air or tap water. Most 5-mL balloons will easily accommodate 30 to 50 mL of air or water without bursting. Obvious resistance or patient discomfort on balloon inflation should signal potential erroneous urethral positioning and mandates reevaluation. B, A gauze pad allows a firm grasp on the foreskin to prevent movement during catheterization. D, An assistant stabilizes the penile shaft with the thumb and index finger (arrow) while the operator (asterisk) spreads the redundant tissue with forceps to visualize the meatus deep within the swollen tissue and advances the catheter. It may be difficult or impossible to pass a Foley catheter in a male with a markedly edematous penis. After successful catheter passage and Foley balloon inflation, slowly withdraw the catheter until the approximation of the balloon with the bladder neck precludes further withdrawal.
Discount ilosone 250 mg on-line
Focal changes identical to those seen in Ih can be identified in a number of inflammatory processes and even in association with tumors symptoms and diagnosis purchase ilosone 250mg online. Chronic inflammation associated with lymphedema and lymphangiectasia may be the trigger for the intravascular proliferation of histiocytes. Some histiocytes have a crescentic nucleus that is pressed against the cytoplasmic membrane. Differential diagnosis the differential diagnosis includes reactive angioendotheliomatosis and intravascular lymphoma. It has been suggested that reactive angioendotheliomatosis and Ih are part of the same spectrum but this is unlikely. Morphology and immunohistochemistry should allow easy distinction between the two entities. Distinction from lupus erythematosus is extremely difficult, particularly as the lymph node changes may be identical. Distinction is based on clinicopathological correlation, immunofluorescence, and the scarcity of histiocytes and presence of plasma cells in cutaneous lesions of lupus erythematosus. Intralymphatic histiocytosis Clinical features Intravascular histiocytosis (Ih) (intravascular lymphangitis, intravascular histiocytosis) is a rare disorder with only about 36 cases described in the literature so far. In some patients there is no associated disease and in rare cases lesions develop at the sites of scars in patients with hip or knee replacement in which a metal implant has been. Langerhans cell histiocytosis multiple sites within a single system (usually bone), or present as a disseminated multisystem disease. Congenital self-healing reticulohistiocytosis (hashimotopritzker disease) is regarded by some as part of the spectrum of Langerhans cell histiocytoses, but is discussed separately. Bone and adjacent soft tissue are the most frequently affected sites, particularly the skull, femur, vertebrae, pelvic bones, and ribs. Less commonly, localized disease occurs in lymph nodes, skin, lung, brain or oral mucous membranes. Neoplastic cells are admixed with variable numbers of eosinophils and in some cases with histiocytes (including foam cells and multinucleate forms), neutrophils (often sparse), small lymphocytes, and plasma cells. In early lesions, Langerhans cells predominate along with eosinophils and neutrophils, but in later lesions there are increased foamy histiocytes and fibrosis. Lung lesions comprise a diffuse infiltrate, involving alveoli and alveolar walls, and peribronchial and subpleural deposits. Most cases can be resolved by immunohistochemistry, particularly when antibodies to langerin are available. Langerhans cell sarcoma must be differentiated from other sarcomas involving the skin, and this is usually achieved by immunohistochemistry. Most cases occur in adults, but examples in children and exceptional congenital lesions have been reported. Solitary lesions usually present as soft red nodules measuring up to 1 cm in diameter, and may be ulcerated. Most cases undergo complete or partial regression without recurrences, a more aggressive course being rare. Juvenile xanthogranuloma family the juvenile xanthogranuloma family of disorders is rare, but constitutes the most frequently encountered types of non-Langerhans cell histiocytosis. Common to all subtypes, is a proliferation of histiocytes and touton-type giants cells, with a characteristic phenotype, displaying features of both macrophage and dendritic cell differentiation. Manifestations include patients with solitary or multiple skin lesions, presentation with large deeply situated masses, and widespread disease with systemic involvement. Most patients are children with solitary or multiple skin lesions, soft tissue or visceral tumors with rare mucous membrane involvement and systemic disease. Skin is rarely involved and therefore this disease will not be discussed further herein. Other, even less frequently encountered, less well-defined, and rather more spurious entities are also best included within this family of diseases. Nevertheless, the clinical details of each will be outlined separately below, in order that the reader can relate to the pleitropic nomenclature and somewhat confused literature that surrounds these disorders. Skin lesions tend to flatten, disappearing over months to years, sometimes leaving atrophic or hypopigmented scars. Benign cephalic histiocytosis Benign cephalic histiocytosis is exceptional and presents in early childhood. Not infrequently, they later spread to affect the shoulders, proximal limbs, trunk, and pubic area. One of these involved the larynx, and the other involved the conjunctiva, gums, ears, and upper airways. Ocular involvement affecting the cornea and conjunctiva occurs in approximately 20% of patients. Juvenile xanthogranuloma family including the head, neck, upper trunk, and extremities, in decreasing order of frequency. Generalized eruptive histiocytosis and xanthoma disseminatum are proposed to be proliferations of more mature histiocytes, occurring in young adults. Middle-aged adults and the elderly are most commonly affected, the histiocytes display a fully matured spindled morphology, and the disease is progressive, resistant to treatment, and shows no tendency to spontaneous resolution. Vacuolated or lightly eosinophilic histiocytes predominate in immature lesions, scalloped and/or xanthomatized histiocytes in more mature cases, and spindled histiocytes in the most mature. Other inflammatory cells are usually present to varying degrees, particularly small lymphocytes, but also eosinophils, neutrophils, and even plasma cells can be present. Xanthomatized histiocytes predominate in papular xanthoma, and scalloped histiocytes in xanthoma disseminatum and scalloped cell xanthogranuloma. Systemic lesions more frequently lack touton-type giant cells, and spindled cells are often present and may predominate. In rosai-Dorfmann disease, the histiocytes are larger and usually paler staining, show emperipolesis, and are positive for S-100. Xanthogranulomas with a prominent spindle cell component may resemble dermatofibroma. Skin lesions are present in 9% of cases and are not uncommonly seen in the absence of lymph node and other extracutaneous disease, or systemic abnormalities. Current evidence suggests that neither hhV6 nor hhV8 is implicated in the majority of cases. Characteristically, the cytoplasm of the histiocytes appears to contain lymphocytes, red blood cells, and/or granulocytes, a feature known as emperipolesis. Involvement of other sites is rare and include the lungs, heart, liver, breast, stomach, thyroid, submandibular gland, skeletal muscle, and bone. In around 50% of patients joint symptoms remain stable or diminish over many years. Clinically, a papule or nodule measuring up to 1 cm in diameter on the skin or mucous membranes is seen. Scattered inflammatory cells, including lymphocytes, granulocytes, and plasma cells, may also be present. Cutaneous lesions represent the primary complaint in 20% of patients, and while many go on to develop joint symptoms, in some the disease remains in the skin (referred as generalized cutaneous reticulohistiocytosis). Multiple reddish-brown to yellow papules and nodules measuring from a few millimeters to 2 cm in diameter are seen. Distinction from a melanocytic lesion is made by negative staining for melanocytic markers. Nuclei are oval or elongated with vesicular or finely granular chromatin, and generally small but distinct nucleoli. Most cases appear cytologically bland, but significant atypia may be seen in some cases. Histiocytic sarcoma 1411 histiocytic sarcoma histiocytic sarcoma (hS) (histiocytic lymphoma, malignant histiocytosis) is a very rare malignant proliferation of cells displaying morphological and immunophenotypic features of mature histiocytes. Small lymphocytes, scattered between the tumor cells and forming perivascular aggregates are common. Nuclei are spindled to ovoid with finely dispersed chromatin and distinct nucleoli of small to large size.
Buy discount ilosone 250 mg line
B 534 Degenerative and metabolic diseases X-ray diffraction and infrared spectroscopy reveal a beta-pleated antiparallel configuration medications drugs prescription drugs purchase 500 mg ilosone fast delivery. Primary and myeloma-associated systemic amyloidoses Cutaneous disease occurs in up to 40% of patients with primary (due to occult plasma cell dyscrasia) and myeloma-associated systemic amyloidosis. Occasional patients present with primary systemic amyloidosis and only develop multiple myeloma later. It occurs most typically on the hands (often posttraumatic) and around the eyes, when the purpura may follow proctoscopy or vomiting. Lesions are sometimes also evident in the nasolabial folds, the neck, axillae, umbilicus, anogenital region, and within the oral cavity. Chronic paronychia, palmodigital erythematous swelling, and induration of the hands have been described. In addition to macroglossia, the tongue may be covered with waxy papules, nodules, and plaques and occasionally it is ulcerated or fissured. In mild cases the changes may be limited to the perivascular tissues, but in more extensive disease large aggregates are usually evident. Involvement of blood vessel walls, arrector pili muscles, skin adnexa, and subcutaneous fat (amyloid rings) is frequently present. In those cases associated with blistering, the vesicle appears in an intradermal or less commonly subepidermal location. Clinically normal skin shows histological evidence of amyloid deposition in up to 50% of patients. Cutaneous involvement has not been recognized as a clinical feature of secondary systemic amyloidosis. Yet in one publication it was described in eight out of nine patients with amyloidosis complicating rheumatoid arthritis. Deposits are said to be focal and abdominal subcutaneous fat has been recommended as the site that is most likely to be positive. Histological features histologically, biopsies from clinically normal skin reveal the presence of amyloid in blood vessel walls, sweat glands, and arrector pili muscle. It is characterized by episodes of fever associated with pleuritis, peritonitis, and synovitis. Histological features amyloid is seen in the dermis, around adnexal structures, surrounding elastic fibers, sometimes forming small globules, and in blood vessel walls, together with striking deposits in the dermal, subcutaneous, and serosal elastic tissue. It is characterized by urticaria, deafness, conjunctivitis, and systemic amyloidosis. Familial amyloidotic polyneuropathy Clinical features Familial amyloidotic polyneuropathy is an autosomal dominant disease in which the deposition of amyloid occurs predominantly in peripheral nerves. It may be associated with photosensitivity, short stature, and palmoplantar keratoderma. Confusion with other conditions associated with poikiloderma including poikiloderma atrophicans vasculare is possible. Pathogenesis and histological features Chronic irritation to the skin has been proposed as the cause of amyloid deposition in the macular and lichenoid variants although this has never been proven. It has been suggested that amyloid deposition in lichen amyloidosis is a consequence of scratching, as pruritus tends to be the presenting symptom even before amyloid is detected in skin biopsies. It has even been suggested that the cutaneous amyloidosis observed in patients with multiple endocrine neoplasia type 2a is secondary to notalgia paresthetica (see below). In papular or lichen amyloidosis, the histopathological changes are similar and cannot be reliably distinguished from those of the macular variant, except that the quantities deposited are greater and there is often more marked epidermal acanthosis, hypergranulosis, and hyperkeratosis. When special stains fail to demonstrate the presence of amyloid, ultrastructural studies are usually successful in detecting the presence of the protein. In earlier literature it was postulated that the amyloid might have been derived from mast cells or fibroblasts. B epidermal keratin in the deposits in both macular and lichenoid forms using monoclonal immunocytochemistry. In macular and lichenoid cutaneous amyloidosis it appears that the above disposal mechanism is either overwhelmed or nonfunctioning. It is thought that on entering the dermis, fibroblasts and macrophages convert the degenerate keratin into amyloid filaments. It would seem that despite a normal humoral response as shown by the presence of IgM and IgG in association with complement fixation, the normal cellular response whereby apoptotic keratinocytes are removed is lacking. On the basis of finding amyloid deposits immediately below the basal keratinocyte, separating its cell membrane from the lamina the amyloidoses densa in the absence of any evidence of filamentous degeneration, it has been suggested that cutaneous amyloid deposits may also be a direct secretory product of keratinocytes. Most cases of nodular amyloidosis are limited to skin and only 7% show progression to systemic amyloidosis. Histological features the histological appearances cannot be distinguished from those of systemic amyloidosis and, indeed, as in primary amyloidosis, the amyloid consists of light chain-derived aL protein. Juvenile colloid milium: there is papular thickening of the skin, particularly involving the cheeks, nose, and forehead. Characteristically, plasma cells are seen around blood vessels and at the margin of the amyloid deposits. It may also develop as a manifestation of ochronosis due to use of the skin bleaching agent hydroquinone. Induction of purpura after stroking has been described in both juvenile and adult colloid milium. Juvenile colloid milium represents a primary degenerative disorder of epidermal keratinocytes, which through the process of apoptosis are transformed into colloid bodies within the superficial dermis. With progression, filamentous transformation comes to affect the entire cell, and nuclear, cytoplasmic, and desmosomal remnants may be identified within the filamentous mass. In addition to the transformed filaments characteristic of all cytoid bodies, amyloid filaments have also been identified in juvenile colloid milium, thereby prompting the authors to classify this entity along with other amyloid-K dermatoses. Juvenile colloid milium is histochemically indistinguishable from amyloid: it is diastaseresistant, paS positive, thioflavine-t positive and shows positive staining with Congo red with apple-green birefringence. Adult colloid milium Clinical features this variant, which is much commoner than the childhood form, affects middleaged patients and shows a predilection for males. Outdoor workers are most often affected and lesions seen on sun-exposed skin are often accompanied by the features of solar elastosis, giving rise to the synonym of papular elastosis. Juvenile colloid milium: the amorphous material that characterizes this condition is of epidermal derivation. Further support for this hypothesis is given by the identification of serum amyloid p component within the colloid deposits. Induration of the oral mucosa (including the inner aspect of the lips, the gingivae, uvula, palate, and floor of the mouth) begins in childhood and is progressive, so that adults have extensive yellow infiltration. Pathogenesis and histological features the epidermis is acanthotic and occasionally papillomatous, with overlying hyperkeratosis. Intracytoplasmic inclusions, probably lysosomal in nature, have also been described. It describes subcorneal and intraepidermal acantholysis without dyskeratosis in a child with lipoid proteinosis. Despite considerable research, the precise pathogenesis of lipoid proteinosis remains an enigma. Quantitative abnormalities of dermal collagen have been clearly demonstrated, but little is known about the nature of the hyaline deposits other than that they are probably composed of an admixture of glycoproteins, glycosaminoglycans, and lipids, as may be determined by special staining techniques. It is likely that the collagen changes are not directly responsible for the accumulation of the granular hyaline material so characteristic of this disorder. Subacute or chronic skin involvement consists of skin fragility, blister formation, and progressive scarring.