Isoptin 240mg lowest price
Fibrous bands from adjacent portal tracts eventually join and dissect the parenchyma into irregular micronodules blood pressure heart rate purchase 240mg isoptin with mastercard. By this stage there is marked hemosiderin deposition with heavy pigment staining of the hepatocytes, bile duct epithelium, ductules, and mesenchymal cells of the fibrous septa and vessels. Regeneration is not usually prominent, but regenerative nodules offer striking contrast to the remaining parenchyma by their lack of stainable iron, so-called iron-free foci [125]. Ultrastructurally, the mitochondria have a dense matrix with separation of the membranes of the cristae. Acute ischemic injury typically produces zone 3 ("centrilobular") coagulative necrosis, similar to that seen in severe injury from certain toxins, such as acetaminophen overdose or mushroom poisoning. Ischemic injury may follow shock, left-sided heart failure, or right-sided failure associated with hypotension [130,131]. Clinically, the presentation may mimic viral hepatitis (ischemic hepatitis) [132]. Liver cells that have undergone coagulative degeneration are shrunken, have an intensely eosinophilic cytoplasm, and show nuclear pyknosis or lysis. Clearing of the dead hepatocytes leads to condensation of reticulin fibers and fibrosis in some cases. Mild portal fibrosis with some periductal fibrosis and reduction in portal vein diameter is a frequent finding in elderly individuals. Often there will be areas in the liver in which vascular structures appear close together, indicating that the acini have atrophied. Macronodular cirrhosis is present with large nodules separated by bands of scar tissue. A variety of patterns of cirrhosis can develop in the later stages but a macronodular type is the most common. Regenerative foci lack identifiable copper, so an absence of stainable copper in a cirrhotic biopsy, particularly if the sample is small, does not rule out Wilson disease. On the other hand, a large amount of copper in a cirrhotic liver is strongly suggestive of Wilson disease. Vascular disorders Vascular patterns of injury Certain patterns of injury in the liver are typical, if not pathognomonic, of a vascular disease. Congestion, atrophy, and coagulative necrosis are all findings that suggest a vascular component to the underlying disorder. The entire hepatic parenchyma is replaced by hyperplastic nodules separated by atrophic liver cell plates. The tissue is fibrotic, and there are portal areas and ductules, but hepatocytes are missing, presumably because of chronic ischemia. Venous outflow obstruction the terminal hepatic venules ("central veins"), intercalated ("sublobular") veins, hepatic veins, and inferior vena cava form the venous outflow tract, but only the terminal hepatic venules and intercalated veins are commonly sampled by liver biopsy. Obstruction of any portion of the outflow tract can be followed by changes in other vessels, such as sinusoidal dilatation and, rarely, thrombosis of the portal venules. Chronic congestive heart failure or constrictive pericarditis can mimic outflow tract obstruction when severe. Many of the changes resemble those of congestive heart failure, but differ by showing variability of involvement among acini, particularly well visualized with open (wedge) biopsy specimens. Those acini with acute changes show severe sinusoidal dilatation and congestion, most pronounced in zone 3. Erythrocytes in the congested areas are packed into the spaces of Disse and crowd the degenerating hepatocytes. The terminal hepatic venules and intercalated veins can show thrombosis, recanalized thrombi. Zone 3 fibrosis can follow either type of injury and can link adjacent terminal hepatic venules. The efferent vein has a markedly narrowed lumen because of intimal thickening with extravasation of erythrocytes. An organizing thrombus in a large intercalated vein (V) is associated with severe sinusoidal dilatation and congestion and necrosis of zone 3 of the surrounding acini. The caudate lobe is often uninvolved because of its separate venous drainage and can undergo compensatory hypertrophy. Intimal edema is followed by the subendothelial deposition of reticulin and collagen fibers and progressive narrowing of the lumen. With progressive fibrosis of the walls, the veins become difficult to identify, appearing as small Sinusoidal lesions Dilatation of sinusoids is a frequent finding in liver biopsy specimens and is often a nonspecific reaction to systemic disease. Chronic congestive heart failure leads to the gradual development of dilatation and congestion of sinusoids and finally to atrophy of hepatocytes, predominantly in zone 3, with secondary fibrosis [130,131]. A characteristic type of periportal (zone 1) sinusoidal dilatation sometimes follows the use of oral contraceptives [137]. The change affects all acini, unlike the focal sinusoidal dilatation seen sometimes near hepatic masses. Panacinar sinusoidal dilatation can be found in sickle cell disease; the dilated sinusoids are packed with masses of sickled erythrocytes. Variable dilatation, lacking any particular zonal localization, can be associated with other disorders, notably neoplasms and granulomatous diseases. Sinusoidal dilatation of the liver may be a systemic manifestation of a number of neoplasms. Peliosis hepatis is characterized by scattered lakes of blood of varying sizes, which appear to represent an extreme degree of localized sinusoidal dilatation. The pathogenesis of the process is now considered to be due to endothelial injury that allows blood to accumulate in the spaces of Disse with a resultant formation of cavities. In the past, peliosis was recognized as a complication of debilitating disorders, such as tuberculosis and malignancies, and was discovered at autopsy as an incidental finding. Currently, the most frequent cause is therapy with androgenic/anabolic corticosteroids [139]. Varying degrees of sinusoidal dilatation can be present near some of the lesions, but the term peliosis hepatis should not be used for simple sinusoidal dilatation. Thrombosis of sinusoids with deposition of fibrin thrombi is unusual, but it happens in some diseases. Patients with toxemia of pregnancy usually have no evidence of liver disease; those who do frequently have deposits of fibrin in periportal sinusoids [141]. Occasionally, the deposits are associated with coagulative-type hepatocellular necrosis. Disseminated intravascular coagulation can be associated with a similar pattern of injury, but the sinusoidal fibrin deposition need not be restricted to the periportal areas. Collagen is deposited in the space of Disse along with laminin, forming basement membranes and leading to capillarization of the sinusoids. Sinusoidal fibrosis is prominent in zone 3 of the acinus in the early stages of alcoholic hepatitis. Amyloidosis Patients with amyloidosis frequently have hepatic involvement, and liver biopsy has been advocated as a means of establishing the diagnosis. There are at least 11 chemical types of amyloid precursor proteins that can form deposits in various tissues and interfere with organ function. The Masson stain shows collagen of the fibrous septa enveloping and traversing the fragments. Cirrhosis Cirrhosis is defined as a diffuse process characterized by fibrosis and conversion of the normal liver architecture into structurally abnormal nodules [143]. Three basic morphologic categories are recognized on the basis of the size of the cirrhotic nodules. The micronodular type includes those cases in which almost all nodules are less than 3 mm in diameter. In the macronodular type, most nodules are greater than 3 mm in diameter and usually show striking variation in size.
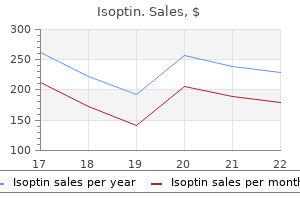
Purchase isoptin on line
Bando K blood pressure 58 over 38 purchase discount isoptin line, Kobayashi J, Kosakai Y, et al: Impact of Cox-Maze procedure on outcome in patients with atrial fibrillation and mitral valve disease. Bando K, Kobayashi J, Hirata M, et al: Early and late stroke after mitral valve replacement with a mechanical prosthesis: risk factor analysis of a 24-year experience. Ad N, Henry L, Hunt S, et al: the outcome of the Cox-Maze procedure in patients with previous percutaneous catheter ablation to treat atrial fibrillation. Gaita F, Riccardi R, Caponi D, et al: Linear cryoablation of the left atrium versus pulmonary vein cryoisolation in patients with permanent atrial fibrillation and valvular heart disease: correlation of electroanatomic mapping and long-term clinical results. Albage A, Peterffy M, Kallner G: Learning what works in surgical cryoablation of atrial fibrillation: results of different application techniques and benefits of prospective follow-up. Tada H, Ito S, Naito S, et al: Long-term results of cryoablation with a new cryoprobe to eliminate chronic atrial fibrillation associated with mitral valve disease. La Meir M, Gelsomino S, Lorusso R, et al: the hybrid approach for the surgical treatment of lone atrial fibrillation: One-year results employing a monopolar radiofrequency source. Zembala M, Filipiak K, Kowalski O, et al: Minimally invasive hybrid ablation procedure for the treatment of persistent atrial fibrillation: one year results. Nevertheless, in a select group of patients, surgical ablation is still an important option for treating refractory ventricular arrhythmias. Of these 295, 144 patients (49%) had heart disease categorized as nonischemic based on the lack of a prior infarct and absence of coronary disease. Six had dilated cardiomyopathy and 2 had longstanding hypertrophic cardiomyopathy. This was impossible to target effectively by percutaneous catheter ablation from the endocardium or epicardium. The original technique used resection of the dyskinetic/akinetic scarred myocardial tissue (aneurysmectomy) with only modest success (~40%) for longterm arrhythmia control. This resulted in the development of subendocardial resection (removing tissue up to a depth of 2-4 mm in the area surrounding the dense aneurysm). This method was adequate for identifying critical components of the reentrant circuit in patients with healed infarcts. However, in these instances, the cardiac temperatures on bypass need to be maintained in the normothermic range. Furthermore, if cryothermy is used for ablation, then the most effective lesions are created on a cooled, cardioplegia-arrested heart. However, it is impossible to sustain ventricular arrhythmias during cold cardioplegia. The loss of autonomic tone as well as the effects of various anesthetic agents coupled with under-filled hearts can make this hard. This precluded the need for additional arrhythmia induction or mapping during open-heart surgical ablation. Thus, cryolesions delivered on the endocardial surface could be palpated from the epicardial aspect and vice versa. Lesion Creation: Energy Sources Several energy sources have been used to create effective lesions during surgical ablation of ventricular arrhythmias. The standard duration of cryoapplication with this unit is for a maximum of 3 minutes and comprises both the cooling and thawing phases. The best results are achieved under cold cardioplegia, which allows the probe to achieve the lowest tissue temperatures. The malleable probe can be configured into various shapes, which is helpful for ablating at different cardiac locations and surfaces. Because the entire length of the probe cools during energy application, care has to be taken to avoid making contact of the proximal end of probe with critical cardiac structures. Furthermore, creating lesions using resistive heating may not be as effective in cooled hearts. Thus, cold cardioplegia is essential for effective cryothermy during surgical ablation of ventricular arrhythmias. However, as was pointed out earlier, this usually requires a beating heart setup or euthermic cardiac temperatures. An alternative method to assess ablation efficacy may be to evaluate physical properties of the targeted tissue. Effective lesions should also result in alteration in the electrical properties of the tissue. Thus, inability to capture the ablated site at high pacing outputs can serve as an end point for effective lesion creation. In some situations in which lesions are delivered across reentrant channels, one can test for the presence of postablation conduction block across the targeted channel. However, beyond this period, pericardial adhesions may form and then epicardial access can be challenging. For all of these reasons, procedure-related complications are not uncommon in this group of patients. These include infection, altered mentation, worsening heart failure, prolonged inotropic support, persistent hypoxemia, and arrhythmias. However, if these arrhythmias become sustained then patients may need extra corporeal membrane oxygenation support or a ventricular assist device to maintain end-organ perfusion. In these instances, consideration should also be given to percutaneous catheter ablation. For sustained ventricular arrhythmias that remain refractory to all of these interventions, cardiac transplantation may be the only remaining option. The latter is an effective strategy in patients with nonischemic cardiomyopathy in whom the scar is patchy and not easily identifiable visually during open heart surgery. In the remaining six patients, the median time from surgery to discharge was 7 days (range, 5 to 11 days). However, over a 5-year period, there was a steady decline in survival so that at the fifth year, 25% of the subjects had died. It is possible that hybrid rooms, which are capable of supporting percutaneous interventions and open-heart surgical procedures, may help accomplish this. Development of energy sources and platforms that can create effective lesions without the need for cold cardioplegia is also highly desirable because it will enhance the ability to ablate during an ongoing arrhythmia. This can provide a more rigorous and easily reproducibly end point of arrhythmia termination during lesion creation and inability to induce the targeted arrhythmia afterward. Another improvement in the surgical ablation technique would be the ability to map and ablate ventricular arrhythmias using a less invasive approach (without median sternotomy). Although this approach is successful for treating refractory ventricular arrhythmias in patients with both ischemic and nonischemic cardiomyopathies, it is highly invasive. A major challenge during surgical ablation is the ability to reproducibly induce and map the clinical arrhythmia. Until this is accomplished, surgical ablation will remain the treatment of last resort in the management of ventricular arrhythmias. Wellens F, Geelen P, Demirsoy E, et al: Surgical treatment of tachyarrhythmias due to post infarction left ventricular aneurysm with endoaneurysmorrhaphy and cryoablation. Michowitz Y, Mathuria N, Tung R, et al: Hybrid procedures for epicardial catheter ablation of ventricular tachycardia: value of surgical access. First results of hybrid surgical-electrophysiological approach for atrial fibrillation. Lindblom D, Albage A, Sartipy U: Surgery for ventricular tachycardia in patients undergoing surgical ventricular restoration. Pirk J, Bytesnik J, Kautzner J, et al: Surgical ablation of ventricular tachycardia guided by mapping in sinus rhythm: long term results. Mathuria N, Michowitz Y, Shivkumar K: Hybrid surgical procedures for epicardial ventricular tachycardia ablation: an update. Maximal stimulation current, pulse width, and operation algorithm of the CardioFit System are controlled by wireless communication and are used noninvasively to adjust the stimulation algorithm and settings for optimal outcome of therapy in each individual case. This focus gave rise to beneficial drugs such as angiotensin-converting enzyme inhibitors, -adrenergic receptor blockers, and aldosterone antagonists. Recognition that alteration in cardiac vagal efferent activity through peripheral cardiac nerve stimulation can produce bradycardia and can modify ventricular contractile function provided added support to this approach. Acetylcholine neurotransmission activates M2 muscarinic receptors located in the heart, where they act to slow the heart rate down to normal sinus rhythm after stimulatory actions of the sympathetic nervous system by slowing the speed of depolarization.
Quality 120 mg isoptin
However arteria iliaca comun order isoptin mastercard, defective glucuronidation is a more common mechanism that results in reduced bilirubin clearance and consequent unconjugated hyperbilirubinemia. Higher neonatal bilirubin levels that predispose to kernicterus occur in the face of profound prematurity, Gilbert syndrome (see later), hemolysis, or both. Familial hyperbilirubinemias Familial unconjugated hyperbilirubinemias the spectrum of familial unconjugated hyperbilirubinemias is indicated in Box 5. Conjugated hyperbilirubinemia Conjugated hyperbilirubinemias typically reflect abnormalities in hepatocellular excretion of conjugated bilirubin or in biliary tract obstruction. In both disorders, general hepatocellular function is preserved and liver chemistries other than the bilirubin concentration are typically normal. Far more common is the defective bilirubin excretion that occurs with a broad spectrum of hepatobiliary diseases. Less often the mutation occurs in exon 1 and the loss of glucuronidation capacity is largely limited to bilirubin conjugation (type 1b). Although survival has been extended with the advent of phototherapy, those who survive beyond early childhood remain at substantial risk for late-onset bilirubin encephalopathy, the onset of which often follows after even mild febrile illnesses. This mutant Wistar strain of rats was initially described by Gunn in 1938 as having chronic nonhemolytic unconjugated hyperbilirubinemia [166]. Bilirubin glucuronyltransferase activity is undetectable in livers of affected rats [167]. Depending on the severity of the molecular defect, either basal or phenobarbital-stimulated enzyme activity is sufficient in most cases to prevent the development of kernicterus. Clinically relevant neurological sequelae can, however, be precipitated in the setting of intercurrent illnesses, fasting, or any other factor that temporarily raises the serum bilirubin concentration significantly above baseline. The average curve for each group was calculated by computer from the mean values, for the group, of the intercompartmental rate constants () of a compartmental model of bilirubin metabolism. Gilbert syndrome Gilbert syndrome resides at the other end of the spectrum of disorders of bilirubin conjugation. Originally described in 1901 [175], this condition occurs with a phenotypic prevalence of approximately 8% in the general population and is characterized by a mild, unconjugated hyperbilirubinemia at levels that rarely exceed 4 mg/dL, otherwise normal liver function, and hepatic histology that is also normal other than a modest increase in lipofuscin pigment in some cases. Other than mild icterus in some patients, physical examination is also unremarkable. It has been suggested that additional variables, such as mild hemolysis (reported in up to 50% of Gilbert patients) or a separate defect in bilirubin uptake [176,179,180,182], might be among the factors enhancing phenotypic expression. Such missense mutations, which result in a Gilbert syndrome phenotype, have thus far been reported only from Japan [183]. If a phenotypic reduction in bilirubin clearance is taken as the operational definition of Box 5. The diagnosis of Gilbert syndrome is most often made clinically on the basis of a mild, unconjugated hyperbilirubinemia in the absence of other causes. Provocation tests such as a 48-hour fast or the intravenous administration of nicotinic acid augment the bilirubinemia of Gilbert syndrome patients and normal controls by a similar proportion, and are of limited value in establishing a diagnosis of Gilbert syndrome (reviewed in [65]). Bilirubin levels in simple Gilbert syndrome in adults are never sufficiently elevated to pose a risk of neurological damage. No significant toxicity has been ascribed to any of these pharmacokinetic abnormalities. Although a third disorder that had been termed hepatic storage disease [193] was also included in this group, more recent evidence indicates that these patients have Rotor syndrome. They are clinically benign but establishment of a precise diagnosis is important to differentiate them from other more serious disorders and to save patients from unnecessary anxiety or surgical intervention. There are several additional familial disorders characterized by conjugated hyperbilirubinemia in association with cholestasis. These include benign recurrent intrahepatic cholestasis and the progressive familial intrahepatic cholestases described later. Aside from jaundice, physical examination is normal in most cases, but an occasional patient may be found to have hepatosplenomegaly [195,196]. Mild constitutional symptoms similar to those observed in Gilbert syndrome (vague abdominal pain, fatigue, and weakness) are common [195,196]. However, as in Gilbert syndrome, these symptoms may be related to the anxiety associated with prolonged diagnostic testing. Subclinical cases often become manifest during pregnancy or in association with the initiation of oral contraceptive therapy [197]. In the majority of patients with intact gallbladders, this organ was visualized approximately 90 minutes after injection; in all cases, isotopic activity had reached the intestine within 1 hour of injection. However, in a patient with Rotor syndrome, as well as in jaundiced patients with hepatocellular disease, administration of 99m Tc-lidofenin resulted in no visualization of the liver, gallbladder, or biliary tract and no accumulation of radioactivity in the intestine over 24 hours of observation. The kidneys visualized intensely in these latter conditions, indicating selective excretion of the radionuclide by this route [227]. Uncommon on a worldwide basis, the disorder is highly prevalent (1: 1300) among Iranian Jews [196]. Light microscopy reveals no scarring, hepatocellular necrosis, or distortion of zonal architecture. Instead, the characteristic feature is the accumulation of a coarsely granular pigment, most pronounced in the centrilobular zones.
Purchase genuine isoptin on-line
Ketoacidosis in pregnancy carries a 50% fetal mortality blood pressure going up generic isoptin 120mg, but maternal hypoglycaemia, although highly undesirable, is relatively well tolerated by the fetus. Neonatal problems Maternal diabetes, especially when poorly controlled, is associated with fetal macrosomia. The infant of a diabetic mother is more susceptible to hyaline membrane disease than non-diabetic infants of similar maturity. The mechanism is as follows: maternal glucose crosses the placenta, but insulin does not; the fetal islets hypersecrete to combat maternal hyperglycaemia, and a rebound to hypoglycaemic levels occurs when the umbilical cord is severed. The same approach is used in the emergency situation, with the exception that a separate variable-rate insulin infusion may be needed to bring blood glucose under control before surgery. Gestational diabetes has been estimated to complicate about 7% of all pregnancies, with wide variation due to differences between populations and diagnostic criteria. Women with a previous history of gestational diabetes, older or overweight women, those with a history of large for gestational age babies and women from certain ethnic groups are at particular risk, but many affected women are not in any of these categories. For this reason some advocate screening of all pregnant women on the basis of random plasma glucose testing in each trimester and by oral glucose tolerance testing if the glucose concentration is, for example, 7 mmol/L or more. This has added to the controversy concerning the appropriate cut-off levels for screening and intervention, since the benefits of intervention are marginal at lower glucose levels, while labelling a mother as diabetic may have unwanted consequences such as a higher rate of caesarean section. Those who meet the diagnostic criteria for diabetes at first presentation are treated with insulin. Treatment for the remainder is with diet in the first instance, although most patients require insulin cover at some stage during pregnancy (target levels: fasting <4. Many oral agents cross the placenta and are usually avoided because of the potential risk to the fetus, although metformin has been used with success when healthcare facilities are limited. Gestational diabetes has been associated with all the obstetric and neonatal problems described above for preexisting diabetes, except that there is no increase in the rate of congenital abnormalities. Gestational diabetes typically remits after delivery but signals an increased risk of type 2 diabetes in later life; maintaining a low bodyweight and keeping physically active reduce this risk. True type 1 diabetes may develop, and swift diagnosis is essential to prevent the development of ketoacidosis. Hospital admission is required if the patient is symptomatic, or has ketonuria or a markedly elevated blood glucose level. Frequent biochemical hypoglycaemia lowers the glucose level at which symptoms develop. A common error is to increase the dose when a patient needs more frequent injections to overcome a problem of timing. These include pituitary insufficiency, adrenal insufficiency and premenstrual insulin sensitivity. Recurrent ketoacidosis this usually occurs in adolescents or young adults, particularly girls. A combination of chaotic food intake and insulin omission, whether conscious or unconscious, is now regarded as the primary cause of this problem. It almost always occurs in the context of considerable psychosocial problems, particularly eating disorders. This area needs careful and sympathetic exploration in any patient with recurrent ketoacidosis. Other causes include: Unstable diabetes this term is used to describe patients with recurrent ketoacidosis and/or recurrent hypoglycaemic coma. Of these, the largest group is made up of those who experience recurrent severe hypoglycaemia. For example, a once-daily regimen may cause hypoglycaemia during the afternoon or evening and pre-breakfast hyperglycaemia due to insulin deficiency. Unsuspected infections, including urinary tract infections and tuberculosis, may be present. By this stage, endogenous insulin secretion is negligible in the great majority of patients. Pancreatic cells are still present in undiminished numbers, but the glucagon response to hypoglycaemia is virtually absent. Long-term patients are thus subject to fluctuating hyperinsulinaemia owing to erratic absorption of insulin from injection sites, and lack a major component of the hormonal defence against hypoglycaemia. In this situation adrenaline (epinephrine) secretion becomes vital, but this too may become impaired in the course of diabetes. Loss of adrenaline (epinephrine) secretion has the inhibition of hepatic glycogenolysis and gluconeogenesis by insulin Depletion of hepatic glycogen reserves by malnutrition, fasting, exercise or advanced liver disease Impaired gluconeogenesis. Symptoms may also remit on treatment with a somatostatin analogue (octreotide or lanreotide). Certain massive tumours, especially sarcomas, may produce hypoglycaemia owing to the secretion of insulin-like growth factor-1. Peripheral glucose uptake is accelerated by high insulin levels and by exercise, but these conditions are normally balanced by increased hepatic glucose output. Postprandial hypoglycaemia If frequent venous blood glucose samples are taken following a prolonged glucose tolerance test, about one in four subjects will have at least one value below 3 mmol/L. The arteriovenous glucose difference is quite marked during this phase, so that very few are truly hypoglycaemic in terms of arterial (or capillary) blood glucose content. Later work showed a poor correlation between symptoms and biochemical hypoglycaemia. Even so, a number of otherwise normal people occasionally become pale, weak and sweaty at times when meals are due, and report benefit from advice to take regular snacks between meals. Postprandial hypoglycaemia sometimes occurs after gastric surgery, owing to rapid gastric emptying and mismatching of nutrient absorption and insulin secretion. Most are sporadic but some patients have multiple tumours arising from neural crest tissue (multiple endocrine neoplasia). The classic presentation is with fasting hypoglycaemia, but early symptoms may also develop in the late morning or afternoon. Recurrent hypoglycaemia is often present for months or years before the diagnosis is made, and the symptoms may be atypical or even bizarre; the presenting features in one series are given in Table 20. Common misdiagnoses include psychiatric disorders, particularly pseudodementia in elderly people, epilepsy and cerebrovascular disease. This is satisfied when: Symptoms are associated with fasting or exercise Hypoglycaemia is confirmed during these episodes Glucose relieves the symptoms. The diagnosis is confirmed by the demonstration of hypoglycaemia in association with inappropriate and excessive insulin secretion. Hypoglycaemia is demonstrated by: Measurement of overnight fasting (16 hours) glucose and insulin levels on three occasions. About 90% of patients with insulinomas will have low glucose and non-suppressed (normal or elevated) insulin levels. A prolonged 72-hour supervised fast if overnight testing is inconclusive and symptoms persist. Hepatic and renal causes of hypoglycaemia the liver can maintain a normal glucose output despite extensive damage, and hepatic hypoglycaemia is uncommon. The kidney has a subsidiary role in glucose production (via gluconeogenesis in the renal cortex), and hypoglycaemia is sometimes a problem in terminal renal failure. Hereditary fructose intolerance occurs in 1 in 20 000 live births and can cause hypoglycaemia (see p. Autonomous insulin secretion is demonstrated by lack of the normal feedback suppression during hypoglycaemia. This may be shown by measuring insulin, C-peptide or proinsulin during a spontaneous episode of hypoglycaemia. Treatment of insulinoma the most effective therapy is surgical excision of the tumour, but insulinomas are often very small and difficult to localize. Endocrine causes of hypoglycaemia Deficiencies of hormones antagonistic to insulin are rare but well-recognized causes of hypoglycaemia. Quinine may produce severe hypoglycaemia in the course of treatment for falciparum malaria.
Buy isoptin with mastercard
Ketonaemia is confirmed by centrifuging a blood sample and testing the plasma with a dipstick that measures ketones arrhythmia recognition quiz 120 mg isoptin with amex. Patients have a total body potassium deficit of 350 mmol, although initial plasma levels may not be low. Insulin therapy leads to uptake of potassium by the cells with a consequent fall in plasma K+ levels. A patient with healthy kidneys will rapidly compensate for the metabolic Emergency Box 20. Ketonuria: measure urine ketone levels where plasma ketone measurements are not available. Continue insulin with dose adjusted according to hourly blood glucose test results. Special measures Subsequent management Note: the regimen of fluid replacement set out above is a guide for patients with severe ketoacidosis. Excessive fluid can precipitate pulmonary and cerebral oedema; inadequate replacement may cause renal failure. Fluid replacement must therefore be tailored to the individual and monitored carefully throughout treatment. Relatively modest doses of insulin lower blood glucose by suppressing hepatic glucose output rather than by stimulating peripheral uptake, and are therefore much less likely to produce hypoglycaemia. Insulin and glucose together both inhibit gluconeogenesis, and thus ketone production, and are needed to metabolize ketones into less harmful substances. Short-acting insulin is given as an intravenous infusion where facilities for adequate supervision exist or as hourly intramuscular injections. The subcutaneous route is avoided because subcutaneous blood flow is reduced in shocked patients. Two common markers of infection are misleading: fever is unusual even when infection is present, and polymorpholeucocytosis is present even in the absence of infection. If infection is suspected, broad-spectrum antibiotics are started once the appropriate cultures have been taken. Subsequent management Intravenous glucose and insulin are continued until the patient feels able to eat and keep food down. The drip is then taken down and a similar amount of insulin is given as four injections of soluble insulin subcutaneously at meal times and a dose of intermediate-acting insulin at night. Sliding-scale regimens are unnecessary and may even delay the establishment of stable blood glucose levels. The mortality of diabetic ketoacidosis is around 5%, and is increased in older patients. Its treatment is incomplete without a careful enquiry into the causes of the episode and advice as to how to avoid its recurrence. Hyperosmolar hyperglycaemic state this condition, in which severe hyperglycaemia develops without significant ketosis, is the metabolic emergency characteristic of uncontrolled type 2 diabetes. Patients present in middle or later life, often with previously undiagnosed diabetes. Common precipitating factors include consumption of glucose-rich fluids, concurrent medication such as thiazide diuretics or steroids, and intercurrent illness. The hyperosmolar hyperglycaemic state and ketoacidosis represent two ends of a spectrum rather than two distinct disorders (Box 20. The extreme dehydration characteristic of hyperosmolar hyperglycaemic state may be related to age. Old people experience thirst less acutely, and more Problems of management 1020 Hypotension. Plasma expanders (or whole blood) are therefore given if the systolic blood pressure is below 80 mmHg. A bladder catheter is inserted if no urine is produced within 2 h, but routine catheterization is not necessary. It is essential to pass a nasogastric tube to prevent aspiration, since gastric stasis is common and carries the risk of aspiration pneumonia if a drowsy patient vomits. This is a rare, but serious complication and has mostly been reported in children or young adults. These include hypoglycaemia and hypokalaemia, due to loss of K+ in the urine from osmotic diuresis. Overenthusiastic fluid replacement may precipitate pulmonary oedema in the very young or the very old. Hyperchloraemic acidosis may develop in the course of treatment since patients have lost a large variety of negatively charged electrolytes, which are replaced with chloride. It can be measured directly, or can be calculated approximately from the formula: Osmolality = 2(Na + + K +) + glucose + urea. For instance, in the example of severe ketoacidosis given above: Osmolality = 2(140 + 5) + 30 + 8 = 328 mOsm / kg and in the example of the hyperosmolar hyperglycaemic state: Osmolality = 2(155 + 5) + 50 + 15 = 385 mOsm/kg. In the example of ketoacidosis the anion gap is 40, and in the example of the hyperosmolar hyperglycaemic state, the anion gap is 25. This will be shown by a rising plasma chloride and persistence of a low bicarbonate even though the anion gap has returned to normal. In addition, the mild renal impairment associated with age results in increased urinary losses of fluid and electrolytes. Endogenous insulin levels are sufficient to inhibit hepatic ketogenesis, but insufficient to inhibit hepatic glucose production. The following are consequences of hyperglycaemia and may play a role: Clinical features the characteristic clinical features on presentation are dehydration and stupor or coma. Evidence of underlying illness such as pneumonia or pyelonephritis may be present, and the hyperosmolar state may predispose to stroke, myocardial infarction or arterial insufficiency in the lower limbs. Investigations and treatment these are (with some exceptions) according to the guidelines for ketoacidosis. It can be measured directly or calculated as (2(Na+ + K+) + glucose + urea), all in mmol/L. Many patients are extremely sensitive to insulin, and the glucose concentration may plummet. Low-molecularweight heparin should be given to counter the increased risk of thromboembolic complications associated with this condition. This leads to an accumulation of advanced glycosylated end-products causing injury and inflammation via stimulation of pro-inflammatory factors. The metabolism of glucose by increased intracellular aldose reductase leads to accumulation of sorbitol and fructose. These growth factors are released by ischaemic tissues and cause endothelial cells to proliferate. It has been proposed that all of the above mechanisms stem from a single hyperglycaemia-induced process of overproduction of superoxide by the mitochondrial electron chain. This paradigm offers an integrated explanation of how complications of diabetes develop. Unlike ketoacidosis, the hyperosmolar hyperglycaemia state is not an absolute indication for subsequent insulin therapy, and survivors may do well on diet and oral agents. For example, people with diabetes in Japan are less likely than European patients to develop atherosclerosis, but more likely to develop it than non-diabetic Japanese. Lactic acidosis Lactic acidosis may occur in diabetic patients on biguanide therapy. The risk in patients taking metformin is extremely low provided that the therapeutic dose is not exceeded and the drug is withheld in patients with advanced hepatic or renal dysfunction. Patients present in severe metabolic acidosis with a large anion gap (normally <17 mmol/L), usually without significant hyperglycaemia or ketosis. Several large trials have shown that intensive glucoselowering treatment of diabetes has a relatively minor effect upon cardiovascular risk. Since the effect of other cardiovascular risk factors is enhanced in diabetes, it is vital to tackle all cardiovascular risk factors together in diabetes, and not just to focus on glucose levels.
Aspidosperma quebracho-blanco (Quebracho). Isoptin.
- Dosing considerations for Quebracho.
- What is Quebracho?
- How does Quebracho work?
- Asthma, lung disorders, cough, high blood pressure, spasms, fluid retention, menstrual cramps, fever, increasing sex drive, and other conditions.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96400
Cheap 240mg isoptin with visa
The major sites of bilirubin production are the spleen and other compartments of the reticuloendothelial system blood pressure chart age 70 buy discount isoptin 40 mg on line, which degrade the hemoglobin of senescent and injured red blood cells. Stereo-specific opening of the heme macrocycle at the -bridge carbon by the microsomal enzyme heme oxygenase results in the formation of equimolar amount of biliverdin and carbon monoxide. Biliverdin is subsequently reduced to bilirubin by the enzyme biliverdin reductase. Quantitative aspects of bilirubin production In normal human subjects, bilirubin production averages 4 mg/kg body weight per day (6 mol/kg body weight per day) [25]. In normoblastic hemolytic anemias, the bone marrow can increase red blood cell production as much as eight-fold [31], leading to a corresponding increase in the component of bilirubin production derived from erythrocytes [27]. Under these conditions, the amount of bilirubin derived from ineffective erythropoiesis in the marrow may increase in absolute terms, but the proportion of bilirubin production due to ineffective erythropoiesis remains unchanged [27]. Increased bilirubin production also occurs in disorders of heme biosynthesis, including the hereditary erythropoietic porphyrias and lead poisoning [27,28,32]. Finally, administration of phenobarbital and other drugs increases the turnover of heme enzymes, notably hepatic cytochrome P450 isoforms, with a resulting increase in bilirubin production [29,30,33] (see later). This configuration allows the formation of internal hydrogen bonds between the propionic acid side-chain on the B ring and polar groups on the D ring, and between the propionic acid on the C ring and polar groups on the A ring [36]. Although bilirubin is frequently depicted as a linear tetrapyrrole, these hydrogen bonds in fact fix the molecule in a rigid, "ridge tile" configuration [37]. The early labeled peak of stercobilin is derived from ineffective erythropoiesis and the turnover of heme enzymes; the late peak reflects the death of senescent erythrocytes. The observed specific activity of hemoglobin protoporphyrin is less than that predicted from the continued availability of labeled glycine for hemoglobin synthesis as determined from the hippuric acid curve. Finally, under certain conditions in vitro, the two nonidentical halves of the bilirubin molecule can dissociate and then reassemble at random [42]. However, only the (4Z,15E) and (4E,15E) photoisomers, which are formed and readily excreted without conjugation during phototherapy of neonatal jaundice [34,35,44,45], are of clinical significance. As an otherwise insoluble molecule, bilirubin formed in the periphery is transported to the liver tightly bound to albumin, at concentrations that far exceed its solubility in protein-free aqueous solutions [50,51]. Adult human albumin has one high-affinity binding site for bilirubin and at least one class of lower affinity sites. Experimental measurements of the affinity of bilirubin for albumin have varied considerably with the methods employed [50], but estimates of a Kd for the high-affinity site have been in the micromolar range by several different approaches [50,52,53]. The determination of these estimates has been based on the assumption that the affinity of bilirubin for albumin is constant, and is independent of the albumin concentration. Under this assumption, until the bilirubin: albumin molar ratio in the circulation exceeds 1: 1, virtually all of the bilirubin present would be bound to the high-affinity site on albumin, and the unbound bilirubin concentration would remain extremely small. This small, unbound bilirubin concentration [54] is, nevertheless, considered to be an important driving force for hepatocellular bilirubin uptake (see later). Under this model, if the 1: 1 molar ratio of bilirubin to albumin is exceeded, the unbound bilirubin concentration increases rapidly with further increases in total bilirubin. Similar neurotoxicity may, rarely, occur in adolescents and adults who develop sufficiently high concentrations of unconjugated bilirubin to exceed the critical 1: 1 bilirubin: albumin molar ratio [59]. This is, in fact, the only clinically significant potential toxicity of hyperbilirubinemia. Since a normal albumin concentration is 4 g/dL (600 mol/L), and a 1 mg/dL bilirubin concentration represents 17. The oxygen functions on the A and D rings are depicted as the lactam tautomers, and the bridge carbons at positions 5 and 15 are shown in the Z configuration. In this configuration they and their attached hydrogens project toward the substituted positions on the adjacent pyrrole rings, just as in the protoporphyrin ring from which bilirubin is derived. Rings A and B lie in one plane, and C and D lie in another, with the interplanar angle being approximately 98. In the Z configuration, the meso hydrogen at position 5 is trans to the A-ring lactam hydrogen, while in the E configuration it is cis. In the 4E,15Z configuration, the A-ring nitrogen and oxygen groups are not spatially available to form hydrogen bonds with the C12 propionic acid side-chain. If a plane is erected perpendicular to the page along the 4,5 double bond (illustrated by the dashed lines), the B ring may be together adults only at bilirubin concentrations at or in excess of 35 mg/dL. In catabolic states in which hypoalbuminemia exists, however, the 1: 1 ratio may be exceeded at much lower bilirubin concentrations, for example, less than 17 mg/dL in the presence of an albumin concentration of 2 g/dL. Efficient transfer of bilirubin from blood to bile is dependent on normal sinusoidal architecture, plasma membrane transport processes and intracellular binding and conjugation. However, the most rapid changes in affinity reportedly occur at quite low albumin concentrations, with only relatively minor further changes occurring as the albumin concentration is increased above 150 mol/L [61]. Thus, the impact of this new observation on bilirubin:albumin binding within the physiologic range of albumin concentrations, and hence on the risk of kernicterus, has yet to be definitely determined, and may be very small. The resulting increase in the free bilirubin concentration may, at least theoretically, increase the risk of kernicterus in susceptible individuals. Transfer of bilirubin from blood to bile involves four distinct but interrelated steps: hepatocellular bilirubin uptake, binding to specific intracellular cytosolic proteins, conjugation with glucuronic acid, and canalicular excretion. In this setting, bilirubin dissociates from albumin and traverses the hepatocyte plasma membrane into the cell. Recent studies have also identified a purely passive, nonsaturable bilirubin uptake process, but its relative magnitude compared with the saturable process remains to be determined [76]. Accordingly, many questions remain regarding the mechanism(s) underlying hepatocellular bilirubin transport. This is of interest in part because of another single report that long-chain fatty acids, another class of organic anions tightly bound to albumin in the circulation and long believed to be exported from cells by passive diffusion, are in fact exported from adipocytes by facilitated transport, mediated by an as yet uncharacterized protein transporter [78]. Kinetic analyses suggest that binding to these proteins is not involved in the initial process of cellular bilirubin uptake, but does increase net bilirubin sequestration by decreasing bilirubin efflux from the cytosol back into the space of Disse [80]. Bilirubin glucuronidation the aqueous insolubility of bilirubin reflects the rigid, highly ordered, molecular structure conferred by internal hydrogen bonding, which prevents solvent access to polar components of the molecule. Subsequent conjugation with glucuronic acid residues disrupts this internal hydrogen bonding, rendering the resulting monoglucuronide and diglucuronide conjugates highly soluble in aqueous solutions. In the neonatal period, the presence of increased levels of intestinal -glucuronidase [102,109] may result in the presence of appreciable amounts of unconjugated bilirubin within the distal small intestine and upper colon. Absorption from these sites can give rise to a significant enterohepatic circulation of unconjugated bilirubin [99,102,110], which has been implicated as a contributing factor to physiologic jaundice of the newborn and to the further increase in plasma bilirubin concentrations seen in neonates with intestinal obstruction, delayed passage of meconium, or fasting [101]. Efforts to reduce unconjugated hyperbilirubinemia in such situations by interrupting the enterohepatic circulation of unconjugated bilirubin with the use of agents such as oral agar, charcoal, or cholestyramine have had at best limited and inconsistent success [101,102,113]. Bilirubin in the urine Because of its very tight binding to albumin, the free fraction of unconjugated bilirubin in plasma is too small to permit efficient ultrafiltration at the glomerulus. Consequently, unconjugated bilirubin never appears in urine no matter what its plasma concentration. A small degree of tubular reabsorption has been demonstrated, but tubular secretion apparently does not occur [118,119]. The presence of bilirubin in the urine is an absolute indicator of conjugated hyperbilirubinemia.
Buy cheap isoptin 40 mg
A rise in plasma creatinine is a late feature that progresses inevitably to renal failure hypertension teaching for patients order isoptin without a prescription, although the rate of progression may vary widely between individuals. Diagnosis the urine of all diabetic patients should be checked regularly (at least annually) for the presence of protein. Once proteinuria is present, other possible causes should be considered (see below), but once these are excluded, a presumptive diagnosis of diabetic nephropathy can be made. For practical purposes this implies inevitable progression to end-stage kidney disease, although the time course can be markedly slowed by early aggressive antihypertensive therapy. Clinical suspicion of a non-diabetic cause of nephropathy may be provoked by an atypical history, the absence of diabetic retinopathy (usually but not invariably present with diabetic nephropathy) and the presence of red-cell casts in the urine. Renal biopsy should be considered in such cases, but is rarely necessary or helpful. Ischaemic lesions Arteriolar lesions, with hypertrophy and hyalinization of the vessels, can occur in patients with diabetes. Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes mellitus. Management the management of diabetic nephropathy is similar to that of other causes of chronic kidney disease, with the following provisos: Aggressive treatment of blood pressure with a target below 130/80 mmHg has been shown to slow the rate of deterioration of renal failure considerably. These drugs should also be used in normotensive patients with persistent microalbuminuria. Insulin sensitivity increases and drastic reductions in insulin dosage may be needed. Associated diabetic retinopathy tends to progress rapidly, and frequent ophthalmic supervision is essential. The earliest functional change in diabetic nerves is delayed nerve conduction velocity; the earliest histological change is segmental demyelination, caused by damage to Schwann cells. In the early stages axons are preserved, implying prospects of recovery, but at a later stage irreversible axonal degeneration develops. Symmetrical mainly sensory polyneuropathy this is often unrecognized by the patient in its early stages. Involvement of the hands is much less common and should prompt a search for non-diabetic causes. Complications include unrecognized trauma, beginning as blistering due to an ill-fitting shoe or a hot-water bottle, and leading to ulceration. Involvement of motor nerves to the small muscles of the feet gives rise to interosseous wasting. Unbalanced traction by the long flexor muscles leads to a characteristic shape of the foot, with a high arch and clawing of the toes, which in turn leads to abnormal distribution of pressure on walking, resulting in callus formation under the first metatarsal head or on the tips of the toes and perforating neuropathic ulceration. The hands show small-muscle wasting as well as sensory changes, but these signs and symptoms must be differentiated from those of the carpal tunnel syndrome, which occurs with increased frequency in diabetes and may be amenable to surgery. Management of end-stage disease is made more difficult by the fact that patients often have other complications of diabetes such as blindness, autonomic neuropathy or peripheral vascular disease. Vascular shunts tend to calcify rapidly and hence chronic ambulatory peritoneal dialysis may be preferable to haemodialysis. The failure rate of renal transplants is somewhat higher than in non-diabetic patients. A segmental pancreatic or islet graft is sometimes performed under cover of the immunosuppression needed for the renal graft, and this has been shown to improve survival as well as offering freedom from insulin injections. Diabetic neuropathy Diabetes can damage peripheral nervous tissue in a number of ways. The vascular hypothesis postulates occlusion of the vasa nervorum as the prime cause. This seems likely in isolated mononeuropathies, but the diffuse symmetrical nature of the common forms of neuropathy implies a metabolic cause. Since hyperglycaemia leads to increased formation of sorbitol and fructose in Schwann cells, accumulation of these sugars may disrupt function and structure. The patient describes burning or crawling pains in the feet, shins and anterior thighs. These symptoms are typically worse at night, and pressure from bedclothes may be intolerable. It may present at diagnosis or develop after sudden improvement in glycaemic control. A more chronic form, developing later in the course of the disease, is sometimes resistant to almost all forms of therapy. Neurological assessment is difficult because of the hyperaesthesia experienced by the patient, but muscle wasting is not a feature and objective signs can be minimal. Explanation and reassurance about the high likelihood of remission within months may be all that is needed. A warm foot with a bounding pulse is sometimes seen in a polyneuropathy as a result of peripheral vasodilatation. Gastrointestinal tract Vagal damage can lead to gastroparesis, often asymptomatic, but sometimes leading to intractable vomiting. Implantable devices which stimulate gastric emptying, and injections of botulinum toxin into the pylorus (to partly paralyse the sphincter), have each shown benefit in cases of this previously intractable problem. Autonomic diarrhoea characteristically occurs at night accompanied by urgency and incontinence. Diarrhoea and steatorrhoea may occur owing to small bowel bacterial overgrowth; treatment is with antibiotics such as tetracycline. Mononeuritis and mononeuritis multiplex (multiple mononeuropathy) Any nerve in the body can be involved in diabetic mononeuritis; the onset is typically abrupt and sometimes painful. Isolated palsies of nerves to the external eye muscles, especially the third and sixth nerves, are more common in diabetes. A characteristic feature of diabetic third nerve lesions is that pupillary reflexes are retained owing to sparing of pupillomotor fibres. Lesions are more likely to occur at common sites for external pressure palsies or nerve entrapment. Bladder involvement Loss of tone, incomplete emptying and stasis (predisposing to infection) can occur, and may ultimately result in an atonic, painless, distended bladder. Treatment is with intermittent self-catheterization, permanent catheterization if that fails and prophylactic antibiotic therapy for those prone to recurrent infection. The first manifestation is incomplete erection which may in time progress to total failure; retrograde ejaculation also occurs in patients with autonomic neuropathy. Erectile dysfunction in diabetes has many causes including anxiety, depression, alcohol excess, drugs. Phosphodiesterase type-5 inhibitors (sildenafil, tadalafil, vardenafil, avanafil), which enhance the effects of nitric oxide on smooth muscle and increase penile blood flow, are used in those who do not take nitrates for angina. Alternatives for those who fail to improve with a phosphodiesterase inhibitor, who dislike the side-effects (headache and a green tinge to vision the next day) or those in whom it is contraindicated, are: Diabetic amyotrophy this condition is usually seen in older men with diabetes. Presentation is with painful wasting, usually asymmetrical, of the quadriceps muscles or occasionally in the shoulders. Diabetic amyotrophy is usually associated with periods of poor glycaemic control and may be present at diagnosis. Autonomic neuropathy Asymptomatic autonomic disturbances can be demonstrated on testing in many patients (Box 20. It affects both the sympathetic and parasympathetic nervous systems and can cause disabling postural hypotension. The cardiovascular system Vagal neuropathy results in tachycardia at rest and loss of sinus arrhythmia. At a later stage, the heart may become denervated (resembling a transplanted heart). Side-effects include priapism which needs urgent treatment should erection last more than 3 hours Vacuum devices.
Best purchase isoptin
Epidemiology enrique heart attack buy isoptin 240 mg cheap, risk factors, and disease associations Changes consistent with pulmonary hypertension were found in 0. More recently, retrospective studies in liver transplantation candidates have found a prevalence ranging from 3. Elevated portal pressure is critical for the development of pulmonary hypertension [60]. Liver injury and/or portal hypertension trigger the production of cytokines and vasoactive mediators that increase vascular shear stress as is proposed for hepatopulmonary syndrome. Physical examination reveals jugular venous distention, a loud pulmonary component of the second heart sound, and a systolic murmur resulting from tricuspid regurgitation. Electrocardiographic abnormalities are similar to those seen in primary pulmonary hypertension and include evidence of right atrial enlargement, right ventricular hypertrophy, right axis deviation, and/or right bundle branch block. Radiographic findings are generally subtle, but in advanced cases a prominent main pulmonary artery or cardiomegaly due to prominent right cardiac chambers may occur. Other causes of elevated pulmonary pressures and/or right heart failure, including left ventricular dysfunction, volume overload, and chronic obstructive lung disease, have to be excluded. The presence of Chapter 14: Pulmonary Manifestations of Liver Disease 361 pulmonary hypertension is suggested by an increased estimated pulmonary artery systolic pressure (derived from measuring the velocity of the tricuspid regurgitant jet), pulmonary valve insufficiency, right atrial enlargement, and/or right ventricular hypertrophy or dilatation [80]. However, anticoagulants and calcium channel blockers are not recommended due to their potential to increase bleeding and portal pressure, respectively. The use of -adrenergic blockers for the prevention of variceal bleeding should be considered, with caution given the potential for cardiac depression [85]. The risk-benefit ratio of -blocker therapy should be considered, along with alternative approaches to secondary bleed prophylaxis. However, most therapeutic interventions are described in case reports and retrospective analysis. No controlled trials have been undertaken and whether medical therapy impacts survival is unknown. Survival in pulmonary hypertension correlates with the severity of right-sided cardiac dysfunction as assessed by the degree of elevation in the right-sided cardiac pressures and the degree of decline in the cardiac output [81]. International Liver Transplant Society Practice Guidelines: Diagnosis and management of hepatopulmonary syndrome and portopulmonary hypertension. Use of macroaggregated albumin lung perfusion scan to diagnose hepatopulmonary syndrome:a new approach. Hepatopulmonary syndrome in inferior vena cava obstruction responding to cavoplasty. Prevalence of hepatopulmonary syndrome in cirrhosis and extrahepatic portal venous obstruction. Structural and pathologic changes in the lung vasculature in chronic liver disease. Exhaled nitric oxide and impaired oxygenation in cirrhotic patients before and after liver transplantation. Nitric oxide production by the e alveolar compartment of the lungs in cirrhotic patients. Practice guidelines: diagnosis and management of hepatopulmonary syndrome and portopulmonary hypertension. Endothelin-1 in the rat bile duct ligation model of hepatopulmonary syndrome: correlation with pulmonary dysfunction. Analysis of pulmonary heme oxygenase1 and nitric oxide synthase alterations in experimental hepatopulmonary syndrome. Endothelin-1 stimulation of endothelial nitric oxide synthase in the pathogenesis of hepatopulmonary syndrome. The role of endothelin-1 and the endothelin B receptor in the pathogenesis of experimental hepatopulmonary syndrome. The role of receptor tyrosine kinase activation in cholangiocytes and pulmonary vascular endothelium in experimental hepatopulmonary syndrome. Frequency, clinical characteristics, and respiratory parameters of hepatopulmonary syndrome. Cost-effectiveness of screening for hepatopulmonary syndrome in liver transplant candidates. Pulse oximetry is a poor screening test for hepatopulmonary syndrome in liver transplant candidates. Use of macroaggregated albumin lung perfusion scan to diagnose hepatopulmonary syndrome: a new approach. Ancient remedies revisited: does Allium sativum (garlic) palliate the hepatopulmonary syndrome Novel presentation and approach to management of hepatopulmonary syndrome with use of antimicrobial agents. Prevalence and severity of hepatopulmonary syndrome and its influence on survival in cirrhotic patients evaluated for liver transplantation. Defining and characterizing severe hypoxemia after liver transplantation in hepatopulmonary syndrome. Successful liver transplantation in patients with mild to moderate pulmonary hypertension. Portopulmonary hypertension in candidates for liver transplantation: diagnosis at evaluation comparing Doppler echocardiography with cardiac catheterization and incidence on the waiting list. Prevalence of spontaneous portosystemic shunts in patients with portopulmonary hypertension and effect on treatment. Significant improvement of portopulmonary hypertension after 1-week terlipressin treatment. Portopulmonary hypertension: imatinib as a novel treatment and the emory experience with this condition. Effectiveness of phosphodiesterase-5 inhibitor therapy for portopulmonary hypertension. Long-term follow-up of portopulmonary hypertension patients after liver transplantation. Successful outcomes following living donor liver transplantation for portopulmonary hypertension. Living-donor liver transplantation for moderate or severe porto-pulmonary hypertension accompanied by pulmonary arterial hypertension: a single-centre experience over 2 decades in Japan. Outcomes of liver transplantation for porto-pulmonary hypertension in model for end-stage liver disease era. Genetic risk factors for portopulmonary hypertension in patients with advanced liver disease. Clinical predictors of pulmonary hypertension in patients undergoing liver transplant evaluation. Echocardiography for the detection of portopulmonary hypertension in liver transplant candidates: an analysis of cutoff values. A careful history and physical examination, ascitic fluid analysis, and imaging tests usually provide definitive diagnoses regarding the cause(s) of ascites and complications, such as spontaneous bacterial peritonitis. Treatment of patients with ascites is dependent on the cause(s) of fluid formation. Ascitic fluid forms in the setting of cirrhosis due to intrahepatic portal hypertension, splanchnic vasodilatation, and renal retention of sodium and water. Most patients with cirrhosis and ascites have physical findings that raise suspicion for liver disease, including vascular spiders, palmar erythema, and abdominal wall collaterals. Abdominal paracentesis with ascitic fluid analysis is crucial in detecting the cause of ascites formation and potential infection. Antibiotic strategies should be adapted to the site of acquisition of infection and to local epidemiology. Specific subgroups of cirrhotic patients at high risk for spontaneous infections benefit from antibiotic prophylaxis. Diet combined with spironolactone with or without furosemide in single morning doses can control the fluid in >90% of compliant patients. The efficacy of automated low-flow pump systems in patients with refractory ascites is currently under investigation.