Cheap generic anafranil canada
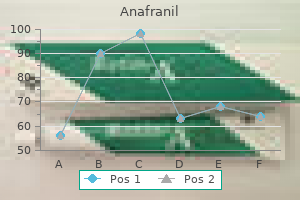
Among the 51 infants delivered vaginally mood dysregulation disorder dsm 5 generic anafranil 25 mg, there were 4 deaths, 3 of which were the result of tentorial tears. Pelvimetry performed with computed tomography exposes the fetus to substantially less radiation and is performed with greater facility in most hospitals than conventional x-ray pelvimetry. This will continue to occur despite the increasing practice of planned cesarean delivery for all patients with a term breech presentation. In a study by Zatuchni and Andros,199 clinical screening of patients with breech presentations at term identified mothers who safely accomplished a vaginal delivery. On admission to the hospital in labor, patients were evaluated according to a "diagnostic index" (Table 43-11). Skillful, atraumatic delivery, regardless of the route of birth, is essential in keeping infant morbidity to a minimum. Milner203 showed that application of forceps to the after-coming head was associated with a reduced rate of neonatal mortality from breech delivery. The well-illustrated publication by Piper and Bachman,204 describing the use of the forceps designed by Piper and presenting in detail the method of breech delivery, should be standard reading for all physicians planning to assist in the vaginal delivery of a breech presentation. Even when the delivery is cesarean, forceps should be available (use of Piper forceps is not necessary), and they should be applied through the uterine incision to the after-coming head if there is any difficulty with its extraction. Calvert205 found that infants in breech presentation born by cesarean section had a higher incidence of birth asphyxia than a comparable group of infants in cephalic presentation born by cesarean. A uterine incision does not ensure an atraumatic delivery of an infant, especially one in a breech presentation. External Version External version substantially reduces the incidence of term breech presentation. Complications that require immediate delivery, including placental separation and umbilical cord compression, occur in 1% to 2% of patients. The procedure is performed late in gestation and with cesarean delivery capability available, so that prompt delivery can be accomplished if persistent umbilical cord compression or premature separation of the placenta occurs. Tocolytic medications have been used in most series to prevent uterine contractions during the procedure, and the evidence shows that their use improves the success rate of external version. In addition to a reduced morbidity risk for mother and infant, the cost savings are substantial. After successful external version, patients had significantly higher rates of instrumental delivery and emergency cesarean delivery. The higher risk of operative delivery was the result of an increase in several major indications: fetal heart rate abnormalities, failure of labor to progress, and failed induction of labor. It is apparent that external cephalic version, even when successful, does not eliminate all of the risks inherent in breech presentation. The method of pain control for a vaginal breech delivery is another controversial issue. Conduction anesthesia has been used with good results,200 and a case can be made that it prevents the mother from pushing uncontrollably in the second stage and allows for an easier and more comfortable application of the Piper forceps to the after-coming head. However, in a study of 643 singleton term breech presentations, epidural analgesia was associated with longer duration of labor, increased need for augmentation of labor with oxytocin, and a significantly higher rate of cesarean delivery in the second stage of labor. Because the fetal abdomen and the insertion of the umbilical cord are in the lower uterine segment during the late first stage and the second stage of labor, significant variable decelerations are more likely to be encountered than with cephalic presentation. For this reason, membranes should be left intact as long as possible, to provide some hydraulic protection against umbilical cord compression. Vaginal breech deliveries are more often associated with significant fetal acidosis than cephalic presentations. The use of oxytocin for induction of labor or augmentation of abnormal labor in a breech presentation is controversial. In the randomized, controlled trial by Hannah and associates,184 a disproportionate number (64%) of the perinatal deaths in the intended vaginal delivery arm occurred in labors that were induced or augmented with oxytocin. The procedure should be performed in a hospital in which cesarean delivery can be accomplished if unrelenting fetal distress occurs. A real-time ultrasonographic scan is performed to confirm the breech presentation; to detect multiple gestation, oligohydramnios, or fetal abnormalities; and to measure fetal dimensions. After a reactive nonstress test, a tocolytic drug is administered (terbutaline sulfate, 0. One person can elevate and laterally displace the breech while a second person manipulates the fetal head in the opposite direction. Mineral oil on the abdomen facilitates movement of the hands during the procedure. The fetal heart rate should be monitored intermittently with Doppler or real-time scanning. Fetal bradycardia occurs in about 20% of cases but almost always subsides after the manipulation ceases. External fetal heart rate monitoring is continued for 1 hour, after which the patient is discharged. Premature rupture of the membranes (30%) and placenta previa (10%) are also more common in transverse lie than in longitudinal presentation. These accidents typically happen unexpectedly, when spontaneous rupture of the membranes occurs outside the hospital setting. In such cases, the patient is usually admitted to the hospital with a severely asphyxiated or dead fetus. Management of the patient with a confirmed diagnosis of transverse lie depends on the length of the gestation, the size of the fetus, the position of the placenta, and whether the membranes have ruptured. If the patient is in labor with a transverse lie and the expected fetal weight and gestational age are below those compatible with a reasonable (10%) chance of survival, no intervention is necessary beyond attempts to stop labor in the interest of increasing fetal weight and maturity before delivery. A fetus of this size (usually <600 g) eventually is delivered vaginally in shoulder presentation (conduplicato corpore) without undue trauma to the mother. If the gestational age or expected fetal weight is such that the chance for neonatal survival, in the absence of severe asphyxia or trauma, is greater than 10%, cesarean delivery is usually necessary, especially if the membranes are ruptured or placenta previa is present. The role of external version in the management of transverse lie is highly controversial. Moreover, there is the possibility that spontaneous version to a longitudinal lie will occur with additional growth and maturity of the fetus or with the onset of contractions. In 102 cases so managed, 86 patients delivered vaginally, with only 1 case of cord prolapse and no perinatal deaths. Most authorities advise a low vertical or classic uterine incision in such cases, although Cruikshank and White217 found an extraordinarily high maternal morbidity rate (severe intraperitoneal infection, 21%; maternal death, 8. The low transverse incision often suffices in cases of a back-up transverse lie, and the high transverse incision described by Durfee219 can be used in cases of a back-down shoulder presentation. Finally, a technique of intra-abdominal version to allow the use of a low transverse incision has been described. However, uterine incision should always be chosen with the primary purpose of abdominal delivery in mind. About 50% of such diagnoses are not made until the second stage of labor; many of the deflection problems detected early in labor correct themselves spontaneously as labor progresses. With the exception of anencephaly, which almost always results in a face presentation, fetal anomalies do not seem to account for deflection problems in labor. Friedman3 found that face presentation, contrary to generally held clinical impressions, did not appear to affect the course of labor significantly in either nulliparas or multiparas. Brow presentation, in contrast, was associated with abnormalities of descent and longer second stage of labor compared with vertex presentation in matched controls. This is not surprising, because in brow presentation the largest dimension of the head, the mento-occipital diameter, must negotiate the inlet of the pelvis. Consequently, successful descent, rotation, and delivery of a brow presentation in the term infant depend on conversion to either a face or a vertex presentation. Moreover, it is often the delay in labor associated with this conversion that results in a more careful assessment of fetal position and the recognition of a brow presentation. Perinatal mortality rates for brow and face presentations are higher than for vertex presentations, but the differences can be accounted for by fetal anomalies (anencephaly), prematurity, and asphyxia and trauma associated with manipulation during vaginal delivery. Awareness and diagnosis of deflection problems are enhanced by an emphasis on careful vaginal examination and a description of the position and characteristics of the presenting fetal part as an essential element in labor monitoring. If, on vaginal examination, the lambdoid sutures and posterior fontanelle cannot easily be identified as occupying a central position in the pelvis, an abnormal presentation or deflection of a cephalic presentation must be suspected.
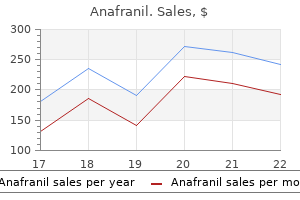
Discount anafranil 10 mg on-line
Although pulmonary disease predominates in early-onset disease anxiety erectile dysfunction buy anafranil now, meningitis may also be present. Late-onset disease may result in localized infections involving the middle ear, sinuses, conjunctiva, breasts, lungs, bones, joints, or skin. The swab should initially be incubated in a nutrient broth and then subcultured on selective blood agar. The specimen is first incubated in selective broth (enriched sample), and then the nucleic acid amplification test is applied. The sensitivity of the test is excellent, ranging from 93% to 100%, with specificity in the range of 93% to 99%. The enrichment process may require up to 24 hours, negating the time-saving advantage of the rapid test. However, when the nucleic acid amplification test is performed on a nonenriched specimen, the sensitivity drops to 63% to 94% and the specificity to 65% to 97%. Moreover, this testing methodology is somewhat complex and is not yet available in all hospitals 24 hours a day, 7 days a week. The diagnosis should be suspected if the clinical manifestations occur in the setting of a risk factor for infection. In most instances, however, treatment must be initiated before the availability of culture results. In these cases, a broad-spectrum approach for empirically treating the mother with chorioamnionitis or puerperal sepsis and the neonate with sepsis is required. Alternative drugs for patients with a contraindication to penicillin are a cephalosporin in those not at risk for immediate penicillin hypersensitivity or vancomycin in patients who are at risk. The frequency of resistance to erythromycin is now so high (25% to 30%) that it should not be used under any circumstances for prophylaxis. Strategies can be classified as antepartum, intrapartum, neonatal, and immunologic. Antepartum Strategies Antepartum strategies to reduce maternal carrier rates generally have been unsuccessful owing to recolonization and therefore are not recommended. Intrapartum Strategies Intrapartum strategies have been the most attractive to date from both clinical and cost-effectiveness perspectives. In cases of onset of labor or rupture of membranes earlier than 37 weeks with "significant risk for imminent preterm delivery," treat as follows: a. The dose is 2 g intravenously initially, followed by 1 g every 4 hours until delivery. If not at high risk for anaphylaxis: the drug of choice is cefazolin, 2 g intravenously, then 1 g every 8 hours until delivery. However, even administration less than 4 hours before delivery may still achieve therapeutic concentrations of antibiotics in fetal serum. Fetuses exposed to antibiotics for less than 4 hours actually had higher serum concentrations than those exposed for longer than 4 hours. Another caveat involves the technique used for collection of the screening culture. However, two thirds of women report at least mild pain associated with collection of the rectal sample. Although initial reports were encouraging, most trials in low-birth-weight infants have not found this approach to be effective. Such a vaccine would need to be polyvalent to cover all serotypes involved in early-onset sepsis. In the adult, typical lesions are vesicular or ulcerative, involving only the skin and mucous membranes. On the other hand, because of an incompletely developed immune system, the newborn is subject to systemic, and frequently lethal, disease. However, both viruses can cause either genital or oropharyngeal lesions, which are indistinguishable clinically. Its clinical manifestations include severe local symptoms, with lesions lasting 3 to 6 weeks, regional adenopathy, constitutional symptoms, and, in a small percentage of cases, viral meningitis. Because the antibody response is directed against epitopes within areas of homology in the glycoprotein G expressed by each viral type, there is some cross-reactivity. Therefore, the presentation is more similar to recurrent episodes than to first-episode primary genital herpes. Recurrent genital herpes infections are much milder and shorter, with lesions lasting 3 to 10 days. The shortened course of infection reflects the preexisting presence of antibody to the viral serotype causing the recurrent infection. Transplacental infection of the fetus resulting in congenital infection is a rare complication of maternal infection. Exact estimates of its frequency are subject to error, because up to 50% of infants with culture-proven fatal disease do not show typical lesions on the skin or mucous membranes. In addition, application of treatment recommendations probably has decreased the incidence of neonatal disease. Neonatal herpes is acquired perinatally from an infected lower maternal genital tract, most commonly during a vaginal delivery. In a study by Brown and colleagues,259 only those women with very recent infection. The risk is considerably lower (1% to 2%) among women with recurrent, clinically evident infection. In one study, the incidence of infection in infants born vaginally to women with asymptomatic recurrent infection was 0 in 34 cases. In a referral nursery, 70% of mothers of infected infants had asymptomatic infections. Among infants with disseminated herpes, the risk of death or serious sequelae exceeds 40%, even with antiviral therapy. With primary infection, tender inguinal adenopathy, fever, and other constitutional symptoms may occur. The frequency of clinically detectable recurrences varies widely among individuals, but about 50% of patients have recurrent disease within 6 months. Recurrences are milder, with fewer lesions, fewer constitutional symptoms, and a shorter course (usually 3 to 10 days). Furthermore, making the diagnosis of genital herpes has social and future implications. The "gold standard" diagnostic test to detect the presence of herpesvirus infection has been the viral culture. The virus grows rapidly, and most positive cultures are identifiable at 48 to 72 hours. Culture of vesicular fluid has the highest yield, and the sensitivity of culture decreases with increasing duration of active lesions. The diagnosis of herpes infection can be made using the Tzanck smear or the Pap smear. Newer IgG assays that are specific to the respective glycoprotein G of each type now allow clinicians to distinguish between these infections. Many women find that frequent bathing, followed by thorough drying of the affected area with a hair dryer, provides temporary relief. Acyclovir, 400 mg orally three times daily, is highly effective for treatment of primary or recurrent infection. When used twice daily, acyclovir also is highly effective in reducing the frequency of recurrent infection. Suppressive therapy with acyclovir has been demonstrated to be safe and effective for 6 years or longer. The appropriate dose of valacyclovir for treatment of infection is 1000 mg twice daily. Accordingly, cesarean delivery is recommended when typical herpes lesions are present at labor, regardless of the time since membrane rupture. Seventeen women had positive antepartum cultures, but none was positive at delivery. Brown and colleagues259 published a cohort study that included more than 40,000 women. However, we believe that acyclovir should be the drug of choice for suppression of recurrent genital herpes during the third trimester, because this drug has been the most extensively studied. Current recommendations for prenatal and intrapartum care include the following: 1. Serial cultures beginning at 34 to 36 weeks are not recommended for asymptomatic women with a history of herpes infection.
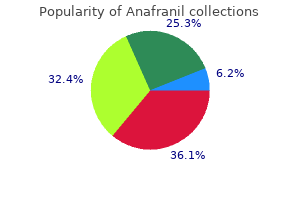
Generic anafranil 75mg otc
As might be expected depression quiz buzzfeed anafranil 10 mg on line, placenta previa and previa accreta are a cause of preterm birth due to the need for iatrogenic preterm delivery. We plan for delivery at 34 to 35 weeks after maternal corticosteroid administration. This strategy is supported by a decision analysis comparing various gestational ages with and without amniocentesis before delivery. The placenta is allowed to remain in situ while the surgeons proceed to a total abdominal hysterectomy. This may require very complex surgical technique and planning, and a pelvic surgeon capable of wide resection of the lower uterine segment and parametrial areas should be available, as well as ample transfusion capability. It is estimated that vasa previa affects between 1 in 1275 and 1 in 8333 pregnancies. It may also result from the presence of a bilobed or succenturiate placenta, with the connecting vessels similarly overlying the cervix. In addition to a succenturiate placenta83 and velamentous insertion, other risk factors include a low-lying placenta observed in the second trimester,84 multiple gestation, and in vitro fertilization. Vaginal bleeding is followed by fetal distress and death if emergent delivery cannot be effected in time. Because the entire fetal cardiac output passes through the cord, it can take less than 10 minutes for total exsanguination to occur. Electronic fetal monitoring may show an initial tachycardia, rapidly followed by decelerations, bradycardia, and a preterminal sinusoidal rhythm. Occasionally, fetal vessels have reportedly been felt through the membranes during vaginal examination or visualized on amnioscopy; such observations are really only of historical interest in modern practice. It is now well established that vasa previa may be diagnosed prenatally with the use of ultrasound. Gray-scale ultrasound can identify placental cord insertion in most cases, but color or power Doppler makes the process easier and should be used. More importantly, in cases in which vasa previa was detected prenatally, there were no fetal deaths from the condition. A recent retrospective, multicenter study showed newborn survival rates of 97% in prenatally detected cases of vasa previa and a fetal loss rate of 56% in cases not identified before the commencement of labor. A, Transabdominal power Doppler identifies the umbilical cord possibly overlying the cervix. Although transvaginal three-dimensional power Doppler provides an excellent means of visualizing the entire lower uterine segment for the evaluation of vasa previa, similar information may be obtained by careful use of a two-dimensional vaginal probe. Such imaging combined with maternal positional change, the use of the Trendelenburg position, and gentle manual elevation of the fetal presenting part aid in visualizing the fetal vessels. The latter technique is particularly useful because the vessels may be compressed by the presenting part and therefore difficult to visualize. A decision analysis comparing 11 strategies for delivery timing concluded that delivery at 34 to 35 weeks best balanced the risk of prematurity with the risk of neonatal mortality. Public and professional awareness has been heightened by such organizations as the International Vasa Previa Foundation However, a high index of suspicion by the attending physician and a meticulous approach to diagnosis provide the best opportunity for a favorable outcome. Subchorionic Hemorrhage Subchorionic hemorrhage is not generally considered to be part of the spectrum of placental abruption. It occurs in the first half of pregnancy and manifests with bleeding only, rather than the more dramatic clinical presentation seen with placental abruption. It is disconcerting to women who have the experience, and it is associated with increased risk of adverse pregnancy outcomes. In 2010, a retrospective review of 63,966 pregnancies revealed subchorionic hemorrhage in 1081 (1. There was also a slightly higher risk of premature membrane rupture and preterm delivery, although the absolute risks remained low. It is a particularly hazardous condition associated with significant maternal and fetal morbidity and mortality. Abruption sufficient to cause fetal death occurs in about 1 of every 420 deliveries. There has been an increase of almost 25% in the rate of clinically detected abruption in the United States in recent decades, with a disproportionate increase seen among African-American women. The hemorrhage dissects the decidua apart, with loss of the corresponding placental area for gaseous exchange and provision of fetal nutrition. The process may be self-limited or ongoing with further dissection of the decidua. Dissection can lead to external bleeding if it reaches the placental edge and tracks down between the fetal membranes; circumferential dissection leading to near-total separation of the placenta can occur, particularly with concealed abruption. The underlying event in many cases of abruption is thought to be vasospasm of abnormal maternal arterioles. Some cases may result from venous hemorrhage into areas of the decidua that have become necrotic secondary to thrombosis. Abruption may also occur secondary to acute shearing forces affecting the placentadecidua interface, such as those that occur with trauma- particularly rapid deceleration injuries (motor vehicle accidents) and the sudden decompression of an overdistended uterus that occurs with membrane rupture in polyhydramnios or delivery of a multiple gestation. As the abruption process continues, loss of placental function results in fetal hypoxia possibly ending in fetal death. Bleeding into the myometrial tissue can lead to a Couvelaire uterus which becomes atonic and increases the risk of uterine hemorrhage after delivery. Risk Factors and Associations for Abruption the most important risk factor for abruption is a history of abruption in a prior pregnancy. Chronic hypertension is associated with a fivefold increase in risk, which rises to eightfold with superimposed preeclampsia. Perhaps the most readily preventable risk factor for abruption is cigarette smoking. Substance abuse is closely linked to abruption: Any agent that causes vasospasm or transient severe hypertension may be causative. There has been substantial interest in the possible association between thrombophilic disorders and abruption. Some retrospective studies of abruption have found increased rates of thrombophilia. Women with vaginal bleeding or contractions after a motor vehicle accident should be observed for at least 24 hours; those who are asymptomatic can safely be discharged after 6 hours of monitoring. These tests include maternal first- and second-trimester serum screening for aneuploidy. Even at that level, a positive test had poor predictive value and was not associated with increased risk of abruption. The classic presentation is that of vaginal bleeding, usually accompanied by abdominal (uterine) pain. If bleeding is present, the amount is often a poor guide to the degree of separation, because there is usually a mixed picture of apparent and concealed hemorrhage. Fetal compromise is a common finding, and if more than 50% of the placenta is involved, fetal death is likely. Massive concealed abruption often manifests with severe pain, a hard uterus, and a dead fetus; such a picture may occur in association with severe preeclampsia or recent use of a vasoactive drug such as cocaine. Abruption may precipitate preterm labor, and it should always be considered in the differential diagnosis for a patient in apparent idiopathic preterm labor. Although ultrasonography is an integral part of the diagnostic approach to late pregnancy bleeding, its utility is primarily for the exclusion of placenta previa as the cause of hemorrhage. In early acute abruptions, blood and clot retained within the uterus appear as hyperechoic or isoechoic collections relative to placental echogenicity. An acute abruption with obvious vaginal bleeding, in which little or no blood is retained within the uterus, may have no specific sonographic findings. Cardiotocography is an integral part of the evaluation for late pregnancy bleeding. Abruption is commonly accompanied by uterine contractions that may not be appreciated clinically, particularly after trauma. Kleihauer-Betke testing is of no diagnostic value in abruption: It may be negative with proven abruption141,142,157 or positive when no abruption has occurred. Its only value in this setting is to guide Rh immune globulin dosing in Rh-negative women who are thought to have sustained an abruption.
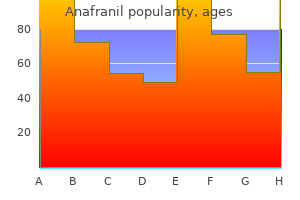
75 mg anafranil free shipping
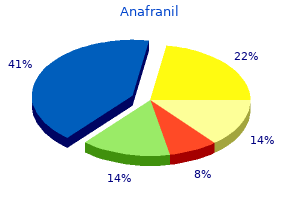
Bacteria also may reach the amniotic cavity from extragenital sources such as the urinary tract or periodontal tissue depression nutrition purchase anafranil with paypal. Risk factors for clinical chorioamnionitis are largely obstetric conditions in patients experiencing protracted labor. The most common organisms found in the amniotic fluid of women with chorioamnionitis are Bacteroides species (25%), G. This organism rarely is isolated in cases of clinical chorioamnionitis, and no significant antibody changes to C. Usual laboratory indicators of infection, such as positive stains for organisms or leukocytes and positive cultures, are found much more frequently than is clinically evident infection. Diagnosis typically is based on the signs of maternal fever, maternal or fetal tachycardia, uterine tenderness, foul odor of the amniotic fluid, and peripheral blood leukocytosis. Because peripheral blood leukocytosis occurs commonly in normal labor, a high white blood cell count (>15,000/mL) supports, but is not diagnostic of, infection. Direct examination of the amniotic fluid, via amniocentesis or aspiration through an intrauterine pressure catheter, may provide important diagnostic information. Positive Gram staining of amniotic fluid for bacteria or leukocytes occurs significantly more often in women with clinical chorioamnionitis than in matched controls. If the amniotic fluid glucose concentration is greater than 20 mg/ dL, the likelihood of a positive culture is less than 2%. If the glucose level is less than 5 mg/dL, the likelihood of a positive culture rises to approximately 90%. Gibbs and colleagues170 reported on a policy in which cesarean delivery was performed only for standard obstetric indications and not for the presence of clinical chorioamnionitis alone. The mean time from diagnosis to delivery was between 3 and 5 hours, and more than 90% of patients were delivered within 12 hours after diagnosis. No critical interval from diagnosis of chorioamnionitis to delivery could be identified. Three studies demonstrated a significant advantage for intrapartum rather than immediate postpartum antibiotic treatment (Table 51-5). In a nonrandomized trial, Sperling and coworkers175 reported a lower incidence of neonatal sepsis when antibiotic treatment was begun at the time of diagnosis, compared with treatment begun immediately after delivery. Gilstrap and colleagues176 found an almost fourfold reduction in neonatal sepsis with use of intrapartum treatment (5. In a randomized trial, Gibbs and colleagues177 used ampicillin (2 g intravenously every 6 hours) plus gentamicin (1. In addition, clindamycin was used after umbilical cord clamping if cesarean delivery was performed, because of the high failure rate of ampicillin and gentamicin alone in women delivered abdominally. Maternal outcome was improved, and confirmed neonatal sepsis was decreased by intrapartum treatment. The duration of postpartum antibiotic therapy needed for patients with clinical chorioamnionitis was addressed in a randomized clinical trial by Edwards and Duff. Failure to add a drug with specific anaerobic coverage will result in an unacceptably high rate of treatment failure, exceeding 20%. Short-Term Outcome Since 1979, reports from systematically collected data on the outcome of mothers and neonates in pregnancies complicated by intra-amniotic infection have shown a vastly improved perinatal outcome compared with older studies. Maternal outcome has been excellent, with no deaths, few cases of septic shock, and rare pelvic abscesses. The cesarean delivery rate has been increased twofold to threefold in all studies, usually because of dystocia. Perinatal mortality has been increased in cases of clinical chorioamnionitis, but little of the excess mortality can be attributed to infection per se. Among term infants born after clinical chorioamnionitis, perinatal mortality has been less than 1%. Cerebrospinal fluid cultures were negative in all 49 infants sampled, and there was no clinical evidence of meningitis. Chest radiographs were interpreted as "possible" pneumonia in 20% and as "unequivocal" pneumonia in only 4%. There was no significant difference in the frequency of low Apgar scores between the chorioamnionitis group and the control group. Preterm neonates born to mothers with clinical chorioamnionitis experience a higher frequency of complications than do those born to mothers without this disorder. Garite and Freeman180 observed that the perinatal death rate was significantly higher in 47 preterm neonates with chorioamnionitis than in 204 uninfected neonates with similar birth weights (13% versus 3%, P <. The group with chorioamnionitis also included a significantly higher number with respiratory distress syndrome (34% versus 16%, P <. Patients with clinical chorioamnionitis are more likely to require cesarean delivery, often for uterine dysfunction, inadequate uterine response to oxytocin, or abnormal labor progress even when uterine activity is adequate. The combination of prematurity and chorioamnionitis increases the risk of serious sequelae in the neonate. Long-Term Outcome There is increasing evidence that intrauterine infection is associated with increased risks of respiratory distress syndrome, periventricular leukomalacia, and cerebral palsy. This "fetal inflammatory response syndrome" has been likened to the systemic inflammatory response syndrome in adults. Several studies have linked maternal infection with cerebral palsy and with cystic necrosis of the white matter in preterm and term infants. Collectively, these observations have aroused renewed interest in the importance of the long-term effects of intrauterine infection, as well as strategies to avoid their serious complications. Chlorhexidine vaginal washes during labor185,186 and selected infection-control measures168 have been ineffective. Use of a screeningbased strategy (which results in more women receiving antibiotics) compared with a risk-based strategy produces lower rates of chorioamnionitis. Although episiotomy and vaginal laceration repair are commonly performed after a vaginal delivery, infection is an infrequent complication. Shy and Eschenbach196 classified episiotomy infections according to the extent of the structures involved. Signs are local edema and erythema with exudate; more extensive findings should raise the suspicion of a deeper infection. Drainage alone usually is adequate, but appropriate antibiotics should be given if there is marked superficial cellulitis or isolation of group A streptococci. Wounds involving the external anal sphincter or rectal mucosa may be repaired after the field is free of infection. When the tissue appears healthy (usually after about 1 week or longer), a definitive repair can be undertaken. For fourth-degree lacerations, a bowel preparation should be given before the repair. Such repair is an attractive option compared with the delay of 2 to 3 months recommended in older literature. Skin findings are variable but initially include edema and erythema without clear borders. As the infection progresses, either loss of sensation or hyperesthesia may develop. Associated findings include marked hemoconcentration, although often after fluid replacement the patient is anemic. Traditionally, this infection has been associated with group A streptococci, but anaerobic bacteria also play an important role. Indications for surgical exploration include extension beyond the labia, unilateral or markedly asymmetric edema, signs of systemic toxicity or deterioration, and failure of the infection to resolve within 24 to 48 hours. At surgery, necrotizing fasciitis may be recognized by separation of the skin from the deep fascia, absence of bleeding along incision lines, and a serosanguineous discharge. It often is the result of a myotoxin elaborated by Clostridium perfringens, but it occasionally can result from an extension of necrotizing fasciitis. Clinicians should recognize that not all vulvar edema in the puerperum signifies serious perineal infection. In fact, most cases of vulvar edema result from less serious causes, such as hematoma, prolonged bearing-down in labor, generalized edema from preeclampsia, allergic reactions, or trauma.
Purchase 75mg anafranil mastercard
In this circumstance depression symptoms test nhs order anafranil on line, a repeat procedure is undertaken 48 hours later to normalize the fetal hematocrit. Hydrops typically reverses after one or two intravascular transfusions; placentomegaly is the last feature of the hydropic state to reverse. At our center, we use empiric intervals of 10 days, 2 weeks, and then every 3 weeks for the second, third, and subsequent procedures. Other experts recommend that the interval be calculated on the basis of an anticipated decline in fetal hemoglobin of 0. The procedure-related loss is 10-fold increased compared with procedures undertaken later in gestation. Ruma and colleagues48 used immunomodulation in a series of nine patients, seven of whom had experienced a previous perinatal loss. The larger target of the peritoneal cavity is more easily accessible than the umbilical vessels at these early gestations. Fox and coworkers49 reported a series of six pregnancies with a previous perinatal loss rate of 66%. Hyaline membrane disease and the need for neonatal exchange transfusions for the treatment of hyperbilirubinemia were common. Finally, the administration of maternal oral phenobarbital may be considered in the 7 to 10 days before delivery. This has been proposed to induce hepatic maturity to allow improved conjugation of bilirubin. One retrospective study has demonstrated a reduction in the need for neonatal exchange transfusions for hyperbilirubinemia. In the largest series reported to date-740 procedures in 254 fetuses treated at a national referral center in the Netherlands between 1988 and 2001-the overall perinatal survival was 89%. Similarly, a series of 284 transfusions in 84 pregnancies in Stockholm over a 20-year period revealed an overall survival of 92%. These infants are born with a virtual absence of reticulocytes, and their red cell mass is almost entirely composed of donor red cells. Because exchange transfusion is rarely required, passively acquired maternal antibodies remain in the neonatal circulation for weeks. This results in a 1- to 3-month period in which up to 75% of these infants may need "top-up" red cell transfusions. Threshold-for-transfusion hematocrit values of less than 30% in the symptomatic infant or less than 20% in the asymptomatic infant have been suggested. Recombinant erythropoietin has been attempted in these infants with minimal effect on their reticulocytosis. In a series of 16 hydropic fetuses who survived to 10 years of age, two of the infants (12. This compared with an incidence of cerebral palsy in the general Dutch population of 0. In a multivariate regression analysis including only preoperative risk factors, only severe hydrops fetalis was independently associated with neurodevelopmental impairment (odds ratio = 11. The study group was found to have evidence of a 10% decrease in left ventricular mass and a 9% decrease in left atrial area. The authors speculated that these findings may result from the prenatal effects of anemia on cardiomyocyte proliferation and differentiation, predisposing these children to adult cardiac disease. The latter two products are purified by ion-exchange chromatography and can therefore be administered by either the intravenous or the intramuscular route. All current products undergo micropore filtration to eliminate viral transmission. When compared with plasma-derived anti-D antibodies, a similar dosage-dependent rate of erythrocyte clearance of RhD red cells from the circulation of volunteers was noted. Severe maternal sensitization does occasionally occur before 28 weeks, and by not performing the antibody screen, the clinician loses the opportunity to detect a potentially salvageable anemic fetus. The RhD antigen is expressed on the fetal red blood cell as early as 38 days after conception. If the rosette is positive, a Kleihauer-Betke stain or fetal cell stain using flow cytometry is performed. In addition, RhD sensitization would limit the availability of blood products if the patient later required a transfusion. The "Weak D" Dilemma Monoclonal typing sera are now routinely used for RhD typing. Many of the weak D and D variants cannot be detected unless a Coombs phase is performed during the typing procedure. Although not systematically studied, this practice has the potential to reduce the chance for alloimmunization in cases of rare RhD phenotypes. In this case, current practice is to employ the indirect Coombs test in the RhD typing, which will detect most partial RhDs and RhD variants. Such a practice prevents the potential for alloimmunization in RhD-negative individuals should they receive a blood unit from these atypical donors. Szczepura and colleagues70 conducted a cost analysis of mass testing to target antenatal anti-D prophylaxis in England and Wales. A recent national first-trimester screening program in the Netherlands found that non-RhD antibodies occurred in 1 in 304 pregnancies. In one series, more than half of pregnant patients had a history of a previous blood transfusion. Anti-RhC, -RhE, and -Rhe Antibodies against the rhesus antigens C, E, and e are usually found at a low titer in conjunction with anti-RhD antibody. Consultation with a blood bank pathologist should be undertaken to clarify whether anti-RhG is present. K1 is found on the red cells of 9% of whites and 2% of blacks, with virtually all antigen-positive individuals being heterozygous (Table 36-3). These gene frequencies are calculated to yield approximately a 5% risk for an affected fetus in the Kell alloimmunized pregnancy if the paternal antigen status and zygosity are unknown. Because the majority of cases of alloimmunization are the result of transfusion (blood is not routinely cross-matched for the Kell in the United States), the first step in the treatment of these patients should be to determine the paternal Kell type. The Kell antibody is noted to cause fetal anemia by two distinct mechanisms-fetal splenic sequestration of sensitized red cells and suppression of the fetal erythropoiesis. Anti-M and Anti-N Anti-M and anti-N are naturally occurring IgM antibodies that typically are cold agglutinins. Four candidate peptides were developed that represented significant epitopes for helper T cells; these were then administered intranasally to the immunized mice. A blunted antibody response was noted when the mice were rechallenged with the purified RhD protein. An antibody screen should be undertaken at the first prenatal visit in all pregnancies. In the first alloimmunized pregnancy, maternal titers can be used to guide the need for fetal surveillance. Giannakoulopoulos X, Sepulveda W, Kourtis P, et al: Fetal plasma cortisol and beta-endorphin response to intrauterine needling [see comments], Lancet 344:77, 1994. Giannakoulopoulos X, Teixeira J, Fisk N, et al: Human fetal and maternal noradrenaline responses to invasive procedures, Pediatr Res 45:494, 1999. Detti L, Oz U, Guney I, et al: Doppler ultrasound velocimetry for timing the second intrauterine transfusion in fetuses with anemia from red cell alloimmunization, Am J Obstet Gynecol 185:1048, 2001. Tiblad E, Kublickas M, Ajne G, et al: Procedurerelated complications and perinatal outcome after intrauterine transfusions in red cell 568. Kenny-Walsh E: Clinical outcomes after hepatitis C infection from contaminated anti-D immune globulin. Stasi R: Rozrolimupab, symphobodies against rhesus D, for the potential prevention of hemolytic disease of the newborn and the treatment of idiopathic thrombocytopenic purpura, Curr Opin Mol Ther 12:734, 2010. Ramsey G: Inaccurate doses of R immune globulin after Rh-incompatible fetomaternal hemorrhage: survey of laboratory practice, Arch Pathol Lab Med 133:465, 2009. In the past, most cases of hydrops fetalis were caused by severe erythroblastosis from Rh alloimmunization.
Buy cheap anafranil 75 mg on-line
This approach to gating depression internet test order anafranil with american express, first described in 1996,147,148 has become widely commercialized as spatiotemporal image correlation. In contrast, real-time approaches use specialized probes to image the fetal heart as a volume, acquiring the entire fetal heart (or a portion thereof) virtually instantaneously. The volume data do not require reconstruction, and they do not require gating algorithms (as do reconstructive techniques) to view cardiac motion. Real-time approaches make the most sense for imaging the fetal heart, given their quick acquisition time (2 seconds), relative resistance to artifact derived from random fetal motion, and lack of a need for cardiac gating. After volume data have been acquired, via either reconstructive or real-time techniques, volume data sets may be reviewed interactively, displaying any plane,71,149 rendered volume,69,71,164,165 or sweep of interest and allowing precise quantitative measurements of ventricular size and function. The Future Within the next 10 years, 3D imaging of the fetal heart is likely to become far more common. The embryology of certain defects is described briefly; more detailed descriptions may be found elsewhere. Because of the complexity of various forms of fetal structural heart defects, as well as their common association with maternal or extracardiac fetal disease, a multidisciplinary team. Normally, during embryonic development, bilateral umbilical veins course along each side of the fetal liver, carrying oxygenated blood from the placenta to the fetal heart. Rarely, the right umbilical vein fails to involute and appears later in gestation as a persistent umbilical vein. The fetus is typically found to have a large, unobstructed vein connecting from the cordal insertion site directly to the right atrium. The finding of a persistent right umbilical vein should prompt a detailed evaluation for other structural defects, cardiac and extracardiac, as well as an evaluation of cardiac function. All cases deserve neonatal clinical and echocardiographic follow-up, although if the anomaly is isolated, the infant typically does well, as the persistent umbilical vein involutes after occlusion of the cord at delivery. Normally, during embryogenesis, the right-sided superior vena cava forms from the right anterior cardinal vein and the right common cardinal vein. The azygos vein returns deoxygenated blood to the right atrium via the superior vena cava. Using both 2D and low-velocity color flow sagittal imaging, the azygos vein can be seen longitudinally, located posterior to the aorta and coursing superiorly and anteriorly. Such cases represent variations of normal and do not require any intervention, either prenatally or after birth. However, given the strong association with polysplenia-related abnormalities, all cases deserve neonatal echocardiographic follow-up. Normally, during embryonic development, the common pulmonary vein evolves to form not only four separate pulmonary veins but also much of the left atrium itself. As with abnormalities of systemic venous return, both 2D and color flow imaging play important roles in the diagnosis of anomalous pulmonary venous return. Anomalous pulmonary venous return frequently occurs in association with other structural cardiac defects, commonly in association with heterotaxy. Postnatally, this vein may appear radiographically like a sword, or scimitar; hence, the name of the syndrome. Color flow imaging may demonstrate such anomalously draining right-sided pulmonary venous return. Commonly, a collateral vessel arising from the descending aorta supplies a separate part of the right lung. Further evaluation may demonstrate a collateral vessel arising from the descending aorta and supplying a portion of the right lung. The fetus with scimitar syndrome may have minimal or no right heart disproportion but frequently presents with dextrocardia or mesocardia. Typically, surgery for scimitar syndrome can be postponed beyond the neonatal period or even beyond infancy. Other than having the potential for development of pulmonary hypoplasia, arrhythmias, and infection, most affected infants do well. Color flow imaging may demonstrate anomalously draining right-sided pulmonary veins. Sinus venosus defects do not generally require intervention during infancy; ultimately, however, closure of the defect is required, with baffling of the right-sided pulmonary venous drainage to the left atrium. Prognosis is usually excellent, but some patients have residual pulmonary venous obstruction or atrial arrhythmias. The descending vein, which is typically partially obstructed in the liver, should be evaluated with color flow imaging. For this reason, delivery should be performed at facilities prepared to manage such high-risk cases. Prenatally, the aortic isthmus normally shunts flow between the right and left heart distributions. The foramen ovale allows oxygenated blood flow to stream from the right atrium to the left atrium, and the ductus arteriosus directs the majority of right ventricular output toward the fetal body, away from the high-resistance pulmonary circuit. Postnatally, the ductus arteriosus closes via constriction, and the foramen ovale closes via pressure-related closure of a one-way valve or flap door. Thus, the normal fetus has a right-to-left atrial shunt, as well as a patent ductus arteriosus, but never a communication between right and left ventricles. During the second and third trimesters, the flap of the foramen ovale (septum primum) becomes progressively more aneurysmal and more deviated into the left atrium. In some cases, the flap appears more aneurysmal than normal for gestational age, or the foramen itself appears to occupy a greater proportion of the atrial septum than normal. In such cases, a detailed evaluation for associated cardiac abnormalities, such as right heart obstruction in the case of excessive deviation, should be performed. If the foramen ovale does appear abnormal prenatally, particularly in association with other cardiac abnormalities or other risk factors for fetal heart disease, elective postnatal echocardiography would be prudent. Moreover, the right-sided pulmonary veins can occasionally be demonstrated to drain anomalously to the superior vena cava on 2D and color flow imaging. Ostium primum defects result from failure of fusion of the septum primum with the endocardial cushions. The most reliable and consistent prenatal sonographic finding is absence of the lower, inferior portion of the atrial septum. First, these defects carry an increased risk for trisomy 21,25,32 so karyotype analysis may be indicated. Isolated defects generally do not require neonatal intervention, but they uniformly require surgical repair, usually during the first 5 years of life. Long-term prognosis is usually excellent, although abnormalities of the mitral valve can rarely persist and may require additional medical or surgical attention. Color flow imaging helps confirm the diagnosis, but spectral Doppler evaluation should also be performed. Small or moderate muscular defects may close prenatally or within a few years after delivery. Large muscular defects manifest in infancy with tachypnea and failure to thrive and may require surgical closure during the first year of life. Because muscular defects occur in a heavily trabeculated portion of the ventricular septum, effective surgical closure can be difficult to achieve. The long-term prognosis is usually excellent unless delayed surgery has allowed the development of pulmonary vascular disease. The membranous septum resides anteriorly a small distance beneath the aortic valve. Small defects may be missed, although color flow imaging and spectral Doppler evaluation are helpful for both prenatal detection and confirmation. Long-term prognosis is usually excellent unless irreversible damage to the aortic valve has occurred. Subarterial defects may reside predominantly under the aortic valve (subaortic) or under the pulmonary valve (subpulmonary). These defects almost invariably require surgical correction within the first year of life. The prognosis, although generally good, relates in part to associated cardiac abnormalities and to any residual aortic or pulmonary pathology.
Cheap anafranil express
Several parameters have been suggested to indicate poor prognosis depression test had order 10mg anafranil with mastercard, such as a high weight ratio of the acardiac twin to the pump twin,158 a rapid increase in the acardiac mass,159 and small differences in the umbilical artery Doppler values. The risk of miscarriage is higher if a breach of the membranes is performed before obliteration of the coelomic cavity. In 8 (33%) of 24 cases, spontaneous fetal death of the pump twin occurred before the planned intervention. In the half of the cases that exhibited spontaneous cessation of blood flow to the acardiac twin, 85% of the co-twins died or suffered brain damage. For those pregnancies that do reach 16 weeks, early prophylactic intervention rather than later intervention may preclude the technical difficulties of achieving arrest of flow in larger and often hydropic acardiac masses, as well as cardiac failure. For later procedures, umbilical cord coagulation and needle-based intrafetal coagulation techniques are both suitable treatment options. The largest experience with fetoscopic laser coagulation for this indication was by Hecher and coworkers (N = 60), who reported an 80% survival rate. Intrafetal coagulation techniques constitute a good alternative and may be the preferred method when access is difficult because of a short umbilical cord or placental location. The pathophysiology includes excessive transfer of fluid into the amniotic cavity from an increased tumoral vascular area, venous obstruction or functional insufficiency within the placenta, and fetal heart failure. Heart failure may result from the combination of a hyperdynamic fetal circulation or mass return of poorly oxygenated blood from the nonfunctional placental area, anemia, and hypoalbuminemia. The most frequent cause of fetal loss cited in the literature is prematurity, followed by fetal heart failure and hydrops. Poor prognostic factors include tumor size, polyhydramnios, cardiac failure, and location close to the umbilical cord insertion. Beyond the point of ex utero viability, delivery is the treatment of choice, except in the case of anemia, when transfusion may be attempted. Before viability, in utero therapy can be offered in cases of "imminent" or evident fetal heart failure consisting of intrauterine fetal transfusion168,169 with or without interruption of the vascular supply, documented by either ultrasound-guided170-171 or endoscopic166,176-178 techniques. These cells can differentiate into embryonic tumors (mature and immature teratomas) or extraembryonic tumors (choriocarcinomas and yolk sac teratomas). Other, less frequent teratoma locations are the anterior mediastinum, pineal area, retroperitoneal area, neck, stomach, and vagina. Extension forms the anatomic basis for the classification by the American Academy of Pediatrics, Surgical Section (Box 35-2), but this is a descriptive surgical classification that does not provide prognostic information regarding the likely prenatal or postnatal course. Chorioangioma Chorangiomas are hamartomas of the primitive chorionic mesenchyme that arise from angioblastic tissue. They occur in 1% of microscopically examined placentas and as such are the most common nontrophoblastic placental tumor. In rare cases, preterm labor develops, usually linked to the occurrence of polyhydramnios. Less common causes of anemia are hemorrhage within the tumor or into the amniotic fluid. Postnatal surgery for resection of the lesion has a low mortality and morbidity in skilled hands. Bond and coworkers183 determined that 10 of 10 hydropic fetuses and 9 of 9 with placentomegaly died (Tables 35-10 and 35-11). It would seem logical that tumor size would also be related to the risk of cardiac failure. Westerburg and colleagues190 could not confirm that tumor size was predictive of demise, but the highest death risk occurred in fetuses with the most highly vascularized tumors, regardless of size. They divided cases into three groups based on clinical and ultrasound presentation, in a way comparable to what was suggested by Westerburg earlier (see Table 35-11). Larger, faster-growing tumors with significant effect on cardiac function (group 2, N = 21) led to earlier delivery and a greater incidence of polyhydramnios. Eleven of these 21 infants died in the neonatal period (52%), but 8 (72%) of the 11 who died were nonhydropic. Survivors from this group had significant morbidity, such as intraventricular hemorrhage, pulmonary hypertension (and other steal syndromes), and acute renal failure, and three infants had a rectal perforation or sepsis requiring colostomy. A good prognosis in cases with smaller tumors and those with less circulatory impact was confirmed in another study from the Harris Birthright Centre (London). The long-term outcome (average, 39 months) was excellent, with one child having constipation. There were 12 fetal interventions including laser ablation (n = 4, all for hydrops), alcohol sclerosis (n = 3, all for hydrops), cystocentesis (n = 2, to facilitate delivery), and amniodrainage (n = 2, polyhydramnios), and vesicoamniotic shunt (n = 1, fetal bladder obstruction). Although 9 of the 12 fetuses with prenatal intervention survived until birth (mean gestational age at birth, 33 weeks), 6 of the 7 cases with hydrops at presentation resulted in fetal or neonatal demise. Larger or more vascular tumors (no cutoff has been defined) should be followed more carefully, with measurements of tumor size and amniotic fluid volume and with Doppler studies of cardiovascular function and tumor vascularity. The method of delivery should be altered only when direct trauma to the sacral tumor or dystocia is feared. Currently, prenatal intervention is done based on the presence of presumed risk factors for fetal death, such as hydrops or other signs of heart decompensation. Interventions include drainage of polyhydramnios, correction of fetal anemia, and shunting of secondary urinary obstruction. Successful bladder shunting was first reported (at 28 weeks) by Jouannic, and since then by others. In one study, one fetus required cardiac resuscitation during the procedure, probably because of hemorrhage. Four days later, that fetus developed ductus arteriosus constriction, was delivered at 27. One survivor had rectal stenosis from the use of the stapler on the stalk, and other morbidities as well, which were believed to be related to embolic events that may have occurred during surgery. One long-term survivor developed chronic lung disease, probably as a result of prematurity (27. Recently, they also proposed that fetuses be delivered early in selected cases with gestational age greater than 27 weeks when fetal surgery is not possible. Speculations about gas embolization, hyperkalemia from tissue necrosis, hemorrhage, and hyperthermia have been made. In tumors with mature features on histology (most being endodermal stromal tumors), recurrences occurred in fewer than 20% and were usually successfully treated with adjuvant chemotherapy. Only 1 of the 24 patients with an immature teratoma had benign recurrence (mature teratoma). De Backer and colleagues reviewed 70 cases, almost one third with late postnatal diagnoses; 84% were treated by surgery only. Five patients (7%) had recurrence, all with malignancy in the secondary tumor, and two of these patients died. For instance, in utero bladder rupture and urinary tract obstruction have been reported. Also, functional rectal and urinary problems may be more frequent when a considerable portion of the tumor is in the pelvis, which might elongate the pelvic plexus and sacral nerves. The morbidity in the third group was mainly related to postoperative scarring or local infection. Urologic sequelae were most common (>40%), and this may have been related to tumor growth as well as to surgical trauma during removal. The anatomic extent of the tumor has neither direct prenatal prognostic value nor oncologic prognostic significance. However, cases exhibiting large tumor size, a fast growth pattern, and high tumor vascularization appear to have a poorer outcome. The development of hydrops is particularly ominous, but that may be a late sign for fetal intervention. A decision for prenatal intervention in the previable period is probably best made on the basis of a combination of indicators, such as signs pointing to cardiac failure or indicating an increased chance of early delivery. The embryology and molecular and genetic mechanisms behind the disease are beyond the scope of this chapter but are excellently reviewed elsewhere. Relative or severe hypoplasia of both lungs may ensue, with fewer airway branches and abnormal pulmonary vessels as well as reduced lung compliance. This causes postnatal ventilatory insufficiency and pulmonary hypertension, and the fetus may die before the defect can be surgically repaired. Survivors may have several morbidities, such as bronchopulmonary dysplasia and persistent pulmonary hypertension, gastroesophageal reflux, and feeding problems; less frequently, they have thoracic deformations after successful repair. The existence of abdominal viscera in the thorax may be identified by the presence of peristalsis.