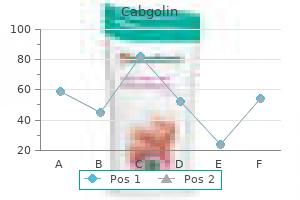
Order cheap cabgolin line
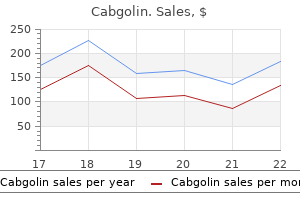
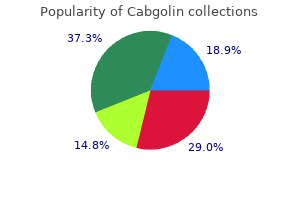
Transplant Tourism Practice of transplantation during which transplant resources are diverted to a recipient from another country medications hair loss cabgolin 0.5 mg online. The declaration distinguishes between "travel for transplantation" and "transplant tourism. When organ trafficking, commercialism, and diversion of resources undermine the ability of a host country to provide transplant services for its own population, it becomes unethical transplant tourism (Table 159. Induction strategies include conventional immunosuppressive agents and/or the use of antibodies directed against T-cell antigens, such as anti-thymocyte globulin and/or total body radiation in the case of bone marrow transplants. Maintenance immunotherapy is less potent and is used to prevent acute and late rejection of the transplanted organ (Table 159. Data show an impressive increase in 1-year allograft survival after kidney transplantation. Kidney transplant recipients require relatively minimal immunosuppression, liver and heart transplant recipients require moderate amounts, and those who undergo small bowel and lung transplantation require higher levels. Pre-travel counseling and vaccination can help reduce morbidity in this population. Only 16 patients (7%) developed illness after traveling that required medical attention. Travelers who fell ill were more likely to have traveled to Central and South America, Africa, the Middle East, and South and Southeast Asia; experienced longer trip durations; and visited family and relatives. Malaria should also be considered in transplant recipients whose donors were from endemic areas. In a comprehensive review of parasitic infections in transplant recipients, the majority of the malaria cases were attributed to the allografts (77. Screening of donors who have visited endemic areas before organ donation is suggested. Treatment does not change in transplant patients, with the caveat that anti-malarial medications interact with some immunosuppressants. This is possibly due to the long cold preservation time of the kidneys, resulting in lower burden of parasites transmitted, in addition to the lower immunosuppression required in renal transplants. Given the low incidence of disease and sub-optimal screening tests, primary prophylaxis is not recommended. All cases were treated with liposomal amphotericin, with a 30% relapse rate after 1 to 8 months; one recipient died. This predominance is thought to be due to the higher number of kidney transplants. High doses of immunosuppressive drugs are a significant risk factor in the development of disease. The majority were treated with amphotericin, with a relapse rate of 25% within 1 year of treatment. Only one third of patients had the classic triad of leishmaniasis at the time of diagnosis, emphasizing the importance of a high index of suspicion in this population. Reactivation of chronic Strongyloides infection is usual, although cases of donor-derived infection are reported. In severe cases, the presence of gram-negative bacteremia could be a clue; this can occur as parasites migrate from the intestinal tract to the bloodstream. In severe cases, addition of albendazole/thiabendazole has been used with equivocal results. Among 27 cases of donor-derived infections, over 50% were in kidney transplant and all had received tacrolimus. Leishmaniasis affects men three times more than women, and older transplant recipients are at higher risk. De novo transmission by infected sandfly and blood- or organ-derived transmission has been reported. Leishmaniasis is known for the triad of persistent fever, pancytopenia, and hepatosplenomegaly, although in transplant recipients the presentation is atypical. Transmission by transplantation of cyst-containing organ or ingestion of undercooked meat is reported. Currently, screening of donors and recipients is not mandatory but is recommended by most experts. Chemoprophylaxis is effective in the following circumstances: in individuals who seroconvert, when there is discordant serology between donors and recipients, and in heart transplant recipients. These recipients tended to acquire infection shortly after engraftment with rapid progression to disseminated disease. Transplant recipients are infected through organ transplantation, blood transfusion, or reactivation of chronic disease, although post-transplant de novo infections have been reported. The risk of Chagas disease is highest during the first year after transplantation. Clinical presentation is similar to acute organ rejection, characterized by fever, rash, gastrointestinal symptoms, and myocarditis in heart transplants. For other organs, there is no consensus and the decision is made on a case-by-case basis. Clinical and laboratory surveillance of chronically infected recipients is recommended. In endemic areas, chagasic cardiomyopathy is the most common reason for heart transplantation. The implications of Istanbul declaration on organ trafficking and transplant tourism. Mycophenolate mofetil: effects on cellular immune subsets, infectious complications, and antimicrobial activity. Patient-reported quality of life after allogeneic hematopoietic cell transplantation or chemotherapy for acute leukemia. International travel patterns and travel risks for stem cell transplant recipients. Donor-derived Plasmodium vivax infection following volunteer unrelated bone marrow transplantation. Plasmodium vivax malaria after autologous bone marrow transplantation: an unusual complication. Risk factors, clinical features and outcomes of visceral leishmaniasis in solid-organ transplant recipients: a retrospective multicenter case-control study. Donor-derived strongyloidiasis infection in solid organ transplant recipients: a review and pooled analysis. Toxoplasma prophylaxis in haematopoietic cell transplant recipients: a review of the literature and recommendations. Molecular diagnosis of toxoplasmosis in immunocompromised patients: a 3-year multicenter retrospective study. Risk factors, clinical features, and outcomes of toxoplasmosis in solid-organ transplant recipients: a matched case-control study. Screening and treatment of chagas disease in organ transplant recipients in the United States: recommendations from the chagas in transplant working group. Some have theorized that abnormal sensations experienced by patients (as if something was crawling on the skin) lead to the conviction that parasites are present (that something really is crawling on the skin). Stress can also exacerbate somatic complaints, and the stress induced by the severity of the perceived illness may augment symptoms further. Such findings must be interpreted with caution, however, given the small number of patients studied and the lack of comparison with age-matched normal controls. Patients with delusional disorders do not meet the diagnostic criteria for schizophrenia or other psychiatric disorders. Specifically, hallucinations, disorganized speech, schizophrenic behavior, and other "negative" symptoms are absent,3 although hallucinations that are secondary to the delusional theme. Similarly, anxiety or depression secondary to the delusional disorder may be present. Recently a single group of investigators published several studies from a small number of patients with Morgellons that described histologic and electron microscopic findings of skin samples that included the presence of spirochetes; they proposed that the condition may be related to Borrelia burgdorferi infection.
Buy discount cabgolin line
The patient experiences no symptoms and there will be no or only very minor changes in the laboratory values medications canada cabgolin 0.5 mg otc. Anemia occurs late in the course of chronic blood loss because the body stores of iron are depleted. Most of the iron in hemoglobin is continually recycled as old blood cells are removed in the liver and spleen. When there is chronic bleeding, iron cannot be recovered from the red blood cells, and the bone marrow uses up its store of iron. Iron and blood products can be administered to return laboratory values to normal, but the source of the chronic blood loss must also be discovered. A careful menstrual history and checking stool for occult (not visible to the naked eye) blood uncovers the two most common causes of chronic blood loss. The red blood cells remaining in the anemic blood are normochromic and normocytic. Within a few days, an elevated reticulocyte count heralds the stepped up production and release of new cells from the bone marrow. Blood lost does not need to be replaced unless the amount is such that hemodynamic effects, such as shock, occur. Chronic blood loss is the slow loss of small amounts of blood over a period of time, most commonly the result of excessive menstrual bleeding or bleeding from the gastrointestinal tract. Hemolysis may be caused by production of defective red blood cells that are destined to a short life, or by events that affect normal cells after they are released from the bone marrow. Destruction and recycling of red blood cells results in increased production of bilirubin. The transportation of this pigment to the liver for excretion is often manifested by an elevation of serum bilirubin and by mild jaundice. The bone marrow, which is stimulated by the anemia to produce more erythrocytes, becomes hyperplastic and releases more immature erythrocytes than normal, causing reticulocytosis. Laboratory abnormalities will additionally include free hemoglobin in the blood and urine, and a decrease in serum haptoglobin, a serum protein that binds free hemoglobin. In fact, administration of iron and transfusion therapy can lead to iron overload, with excessive iron deposition in tissues. These include genetic diseases, immune-mediated destruction of red blood cells, premature destruction of red blood cells in the spleen, and mechanical injury to red blood cells by rough surfaces in the bloodstream. Sickle cell anemia is one of several genetic abnormalities of hemoglobin structure caused by an altered sequence of amino acids in the globin molecule. The diseases produced by these genetic defects are called hemoglobinopathies, and the abnormal hemoglobin is designated by a letter or name of a place where it was first described. Sickle cell anemia occurs in persons with two genes for hemoglobin S (the homozygous state). Persons with one hemoglobin S gene (the heterozygous state) are said to carry the sickle "trait". Hemoglobin S is a genetic abnormality predominantly of black people; overall, about 10% of blacks are heterozygous carriers, and about 1% are homozygous and experience symptoms of the disease. Specifically, they collapse into a half-moon, or sickle shape, under conditions of stress. This change in red blood cell shape can be precipitated by changes in temperature (particularly exposure to cold, such as swimming in cold water), dehydration, changes in altitude, exercise, and mental stress. The abnormally "sickle"-shaped cells are not only more susceptible to rupture and premature death, but also tend to sludge and obstruct small blood vessels. Vascular obstructions are particularly common in the spleen and bone, where they produce multiple small infarcts over a period of years. Patients with sickle cell anemia often live reasonably well with their anemia except during periods of so-called crisis, when more cells become sickled, leading to abdominal and bone pain from small infarcts and jaundice from the increased breakdown of red blood cells. Hemoglobin is composed of two alpha and two beta globin molecules linked together. Alteration of the genes coding for the alpha or beta molecules results in deficient production of adult hemoglobin, and subsequently decreased iron-carrying capacity in the blood. There is a compensatory increase in a type of hemoglobin found in the fetus (hemoglobin F) or in a type of hemoglobin found normally in small amounts (hemoglobin A2). Thalassemia is most common in Mediterranean countries and some parts of Africa and Southeast Asia. The severity of the disease varies from asymptomatic anemia resembling iron-deficiency anemia, to severe, life-threatening hypoxia and congestive heart failure. Since hemoglobin is not assembled at a normal rate, but the body is absorbing and recycling iron normally, the patient may develop iron overload, which can damage the heart, liver, and endocrine systems. This is an even greater danger if the patient receives blood transfusions as part of their therapy. Iron chelation, or removal of iron by administration of drugs that bind iron for transport out of the body, is often indicated, especially in severe forms of the disease. Red blood cells with abnormal hemoglobin are removed in the spleen, so the patient may develop hypersplenism, which in turn removes even more red blood cells. Finally, the bone marrow undergoes hyperplasia in an effort to step up production of red blood cells. This affects the structure of bone, not only making it thin and prone to fracture, but causing deformities, especially in bones rich in hematopoietic tissue, such as the skull and facial bones. Treatment for thalassemia is supportive, in other words, aimed at mitigating the adverse effect of anemia, with iron chelation, judicious blood transfusions, and removal of the spleen. Prenatal, and sometimes even premarital, screening in endemic areas is effective at reducing the number of children born with this disease. Bone marrow transplantation is currently the only known "cure," and used only as a measure of last resort in patients who have severe forms of the disease. The abnormal red blood cells are spherical rather than the normal flat, biconcave disks. As they filter through the spleen, they are more easily removed than are normal cells. This is an example of a dominant disease that is perpetuated because its relatively mild nature and prolonged course allow persons with the disease to reach maturity and reproduce. These patients have a mutant enzyme that becomes deficient in older red blood cells, allowing oxidants to damage the cell membrane and produce hemolysis. Discontinuance of the drug and normal replacement by young red blood cells end the hemolytic episode. Males are much more prone to develop anemia because most affected females are heterozygous carriers. The disease can be prevented by screening high-risk individuals (black males) for the defect and then avoiding exposure to oxidant drugs. In contrast, immune-mediated hemolytic anemia is caused by destruction of red blood cells by the immune system. Specifically, antibodies specific to antigens on the surface of red blood cells cause complement activation and subsequent lysis of the red blood cells within the vascular system or the spleen. Certain drugs, such as antibiotics, and medications used for Parkinson disease may also induce antibodies to red blood cells. The Coombs test and flow cytometry can detect the presence of antibodies attached to the surface of red blood cells in immune and autoimmune hemolytic anemias. Hypersplenism is most commonly caused by chronic passive congestion of the spleen. This results when venous outflow from the spleen is obstructed, usually because of obstruction of the portal venous system, as occurs, for example, with cirrhosis of the liver. The venous congestion causes the spleen to enlarge and secondarily to remove more blood cells than normal, thus producing a type of extravascular hemolytic anemia. The condition is suspected in a patient with cirrhosis and enlarged spleen, leukopenia (decreased white blood cells) and thrombocytopenia (decreased platelets) along with anemia. Prosthetic heart valves, rough atherosclerotic plaques, and disseminated intravascular thrombosis can cause mechanical destruction of red blood cells as these flow past. The blood smear will show the fractured cells which are called schizocytes or helmet cells. The blood smear will also show reticulocytes, as the bone marrow accelerates the release of red blood cells to compensate for loss of the fractured ones. Anemias with Decreased Red Blood Cell Production the bone marrow may fail to put out enough red blood cells if it has an inadequate supply of nutrients to produce red blood cells, if its function is suppressed by the presence of chronic disease, or if the bone marrow tissue is insufficient in amount. As already discussed in the context of chronic blood loss anemia, iron deficiency can be caused by loss of iron, or by inadequate dietary intake of iron.
Diseases
- Alopecia mental retardation syndrome
- Deafness X-linked, DFN3
- Cerebro reno digital syndrome
- Chromosome 15q, tetrasomy
- Complex 2 mitochondrial respiratory chain deficiency
- Short stature deafness neutrophil dysfunction
- Doyne honeycomb retinal dystrophy
- Gaucher disease type 3
Discount 0.5mg cabgolin visa
Terminal urine microscopy (for ova) and serology for schistosomiasis should be performed in those returning from Africa medications at 8 weeks pregnant best buy cabgolin. If initially negative, stool microscopy should be performed on a total of up to three occasions, and serology should be repeated at 3 months if it was first taken less than 12 weeks after the time of probable exposure. If initial investigations are negative, attention should be paid to the possibility of other parasitic, non parasitic and non-infectious causes. Fever and/or Respiratory Symptoms Katayama Syndrome this occurs during acute schistosomiasis infection 2 to 9 weeks after exposure. Empiric treatment should be given when this presentation is accompanied by a history of freshwater exposure in Africa: praziquantel 20 mg/kg in two doses 6 hours apart and oral prednisolone 20 mg/day for 5 days. Praziquantel is relatively ineffective against immature stages of schistosomiasis, so treatment should be repeated at 6 to 8 weeks. Diagnosis Treatment Name Picture Ancylostoma duodenale/ Necator americanus Worldwide Concentrated stool microscopy Albendazole 400 mg single dose (mebendazole 500 mg single dose). Praziquantel 20 mg/kg, 2 doses 6 h apart Loa loa (eye worm) Onchocerca volvulus Africa (Central and West predominantly) (river blindness, onchocerciasis) Africa (S. Dec, diethylcarbamazine; pair, puncture, aspiration of cyst contents, injection of a substance toxic to the immature "scolices," and re-aspiration. It presents similarly to Katayama syndrome, with fever, urticaria, wheeze, and dry cough. Diagnosis is clinical, as symptoms occur before eggs can be detected in the stool. Trichuris infection is usually asymptomatic, but heavy infections can cause morbidity in children, including anemia, dysentery, and rectal prolapse. Ascaris and hookworm are treated with a single dose of albendazole 400 mg; trichuriasis requires albendazole 400 to 800 mg twice daily for 3 days. In immunocompromised individuals, strongyloides can present decades after exposure as hyper-infestation syndrome6 with paralytic ileus and gram-negative sepsis. This condition is due to uncontrolled replication of the parasite and is life threatening. Diagnosis of strongyloides infection can be difficult: serology is usually the most sensitive test, and stool microscopy is often negative. The reverse applies in the hyper-infestation syndrome, where stool samples contain abundant larvae but serology may be negative and eosinophilia absent. Stool culture (performed in specialist laboratories) is recommended in cases where diagnosis is difficult or the danger of missing strongyloides is high. Migrants from all tropical regions should be screened for strongyloides before starting treatment with immunosuppressive drugs. Schistosomiasis is diagnosed by serology and microscopy of either nitrocellulose-filtered terminal urine (S. Hydatid Hydatid disease is most often seen in individuals returning from sheep-rearing areas, especially the Middle East, although it also occurs in North and East Africa, Asia, Europe, and the Americas. Affected individuals are usually asymptomatic; eosinophilia, right upper quadrant pain, and fever can indicate cyst leakage or infection. The presence of peripheral eosinophilia usually suggests a leakage of cyst contents, often into the biliary system. Surgical and percutaneous intervention carry a risk of anaphylaxis and cyst dissemination, and should be performed in specialist centers. Soil-Transmitted Helminths (Geohelminths) these have a worldwide distribution but are most prevalent in the tropics. Hookworm may present with a transient itch and maculopapular rash, followed weeks later by nausea, vomiting, diarrhea, and abdominal pain. They are diagnosed by stool microscopy (low sensitivity in fasciola infection) and serology, and treated with triclabendazole (Fasciola) and praziquantel (Opisthorchis and Clonorchis). The most common cause of eosinophilic meningitis is Angiostrongylus cantonensis, the rat lung worm. This occurs in the Caribbean, Hawaii, and Southeast Asia, and is acquired after the ingestion of larvae in undercooked snails, prawns, crabs, or frogs. It presents with severe acute headache, meningism, visual disturbance, paresthesias, and cranial nerve palsies. It is acquired by consuming inadequately cooked fish, frog, snake, or chicken and presents with a severe meningoencephalitis and myelitis, which can be fatal. Involvement of the spinal cord, usually with paraplegia, is more widely reported with S. Dermatologic Presentations Filariasis: Onchocerciasis, Lymphatic Filariasis, and Loa loa the major filariases are onchocerciasis, lymphatic filariasis (W. Onchocerciasis, or river blindness, occurs around fast-flowing rivers mainly in Africa. It presents with an itchy rash, which over a long period can develop into a "leopard skin" pattern of hypopigmented patches and nodules. Migration of microfilariae within the eye results in keratitis, anterior uveitis, and choroidoretinitis, with eventual blindness. Lymphatic filariasis has a worldwide tropical distribution, although it is most common in Africa. Presentation is with fever, lymphangitis, and lymphedema that can include the scrotum. In routine practice, day bloods (taken around midday) for microscopy of filtered blood are often adequate. Onchocerciasis can be diagnosed by microscopy of skin snips (shallow snips of skin are taken, then incubated in saline before microscopy), or if microfilariae are seen on slit lamp examination of an affected eye. Treatment is associated with significant risks and should be carried out in specialist centers. Screening for schistosomiasis, filariasis, and strongyloidiasis among expatriates returning from the tropics. The changing etiology of eosinophilia in migrants and returning travelers in the Hospital for Tropical Diseases, London 2002 to 2015: An observational study. Schistosomiasis presenting in travellers: a 15 year observational study at the Hospital for Tropical Diseases, London. Chronic Strongyloides stercoralis infection in former British Far East prisoners of war. Utility of history, examination and laboratory tests in screening those returning to Europe from the tropics for parasitic infection. A comparative trial of a single-dose ivermectin versus three days of albendazole for treatment of Strongyloides stercoralis and other soil-transmitted helminth infections in children. Barnett Some screening tests should be performed routinely for all immigrants, based upon prevalence of these conditions, availability and accuracy of screening tests, existence of effective interventions once these conditions are identified, and the potential risk that not identifying these conditions poses to both the immigrant and their contacts (Box 156. The majority of newly identified cases of hepatitis B in the United States are in the foreign-born. Some information may not be revealed until development of a trusting relationship with health professionals, particularly when immigrants have experienced traumatic experiences or are unfamiliar with the U. Laboratory screening tests include complete blood count with differential (identifies anemia, possible hemoglobinopathy, eosinophilia, or other blood abnormality), urinalysis (identifies hematuria, proteinuria, or glucosuria), and lead levels for children. Immigrants should be offered the same age-appropriate screening and immunizations that are given to U. Stool for ova and parasites is no longer needed for refugees who undergo pre-departure treatment for soil-transmitted helminths, but may be appropriate for immigrants not treated before departure or who are symptomatic.
Order cabgolin 0.5 mg without a prescription
Larvae are coughed up treatment arthritis order cabgolin 0.5 mg with mastercard, swallowed, pass through the esophagus and stomach, and arrive in the small intestine before molting to become adults. Hookworms ingest blood, lyse red cells, and then degrade hemoglobin through an ordered cascade of hemoglobin-digesting proteases. During the first few decades of the 20th century, hookworm infection was common in the rural southeastern United States, but it has been eliminated as a public health problem after urbanization, consistent shoe-wearing, and economic development. Clinical Features the clinical features of hookworm infection correspond to its life cycle and the intensity of infection. Cutaneous larva migrans is a related condition caused by skin penetration of animal hookworms, classically A. They are most frequently seen on the lower extremities, followed by the buttocks and anogenital area, although the trunk and upper extremities may be affected. Epidemiology Approximately 800 million people are infected worldwide, with the largest number of cases in sub-Saharan Africa, Asia, and tropical regions of the Americas. Severe cases of hookworm anemia and hypoalbuminemia are accompanied by cardiovascular changes. Gastrointestinal Manifestations Epigastric pain and tenderness occur early in the intestinal phase. Patient Evaluation, Diagnosis, and Differential Diagnosis Hookworm disease should be considered in any patient from an endemic area who presents with anemia, eosinophilia, or both. Direct fecal examination in saline or an iodine solution detects persons with more than 1200 eggs per gram of stool. For epidemiologic studies, it may be necessary to perform quantitative fecal egg counts, which roughly correlate with the number of hookworms in the intestine. On physical examination, the mucous membranes, conjunctivae, and skin appear pale. A yellowishgreen hue (chlorosis) that results in a sallow complexion can be seen in heavy infections. Anemia is often accompanied by eosinophilia, and, in severe cases, protein loss and hypoalbuminemia. Treatment the therapy of hookworm disease is treatment with an oral antihelminthic agent. In resource-poor countries where hookworm is endemic, the drugs are usually administered as part of mass treatment programs, either on child health days or through schoolbased deworming programs on an annual or more frequent basis. Benzimidazole agents, albendazole or mebendazole, have been first-line treatments. However, in a systematic review and meta-analysis, the cure rate of single-dose oral albendazole (400 mg) was 72% compared with 15% for single-dose mebendazole (500 mg). Triple-dose therapy with either agent is more effective than single dose, with albendazole providing higher cure rates than mebendazole. Benzimidazoles are teratogenic and embryotoxic in high doses in laboratory animals. Therefore in children older than 1 year but under 2 years, albendazole should be given at one-half the dose (200 mg). The latter are usually older males; veterans who have lived in endemic tropical areas; and those with underlying malignant, metabolic, pulmonary or renal disease. However, the life cycle can occur completely in the soil (free-living cycle) or completely in the host (internal or external autoinfection). Autoinfection is the basis of persistent infection and hyperinfection in patients receiving corticosteroids. These larvae have slender bodies and notched tails that distinguish them from hookworm larvae. The L3 migrate through the lungs and ascend the airways to the trachea and epiglottis before being swallowed to complete their life cycle in the small intestine. In the intestine, adult female worms, eggs, and larvae are found in the superficial sub-mucosa and in the mucosal crypts, causing mechanical trauma, mucous discharge, and microscopic ulceration but usually minimal inflammation. Progressive involvement may lead to edema; flattened villi; malabsorption; and even ulceration, enteritis, and secondary bacterial invasion. It is this larval stage that is characteristically found in the stool or the upper small bowel. Under favorable soil conditions, rhabditiform larvae transform into infective L3 within 24 hours after fecal passage. Under selected conditions, the autoinfective process may become dysregulated, leading to a large number of L3 penetrating the gut, cycling through the lungs, and re-entering the intestine, leading to hyperinfection, secondary bacteremias, and bacterial meningitis. Immunosuppressive drug therapies, especially corticosteroids, are associated with hyperinfection. Other conditions are hematologic malignancies, solid organ transplantations, and autoimmune disorders, although corticosteroids are used for treatment of many of these. In some patients with hyperinfection, the migrating larvae can develop to adult worms in ectopic sites. In external autoinfection, L3 larvae can develop in the colorectal area and penetrate the perianal skin, resulting in pruritic creeping eruption, or larva currens and external autoinfection. During pregnancy, treating the anemia of hookworm disease with both anti-helminthic drugs and iron therapy is superior to either treatment alone. An experimental vaccine to prevent hookworm infection and re-infection is under development. It is unusual among helminths in its ability to multiply within the host and maintain a persistent infection for years (autoinfection). Epidemiology Strongyloidiasis has a patchy, widespread distribution through warm, wet, tropical, and sub-tropical areas. In temperate regions, it is encountered in institutions where sanitary facilities are poor or in moist conditions. The difficulties in diagnosing strongyloidiasis have contributed to a limited understanding of the global prevalence and disease burden. The classically recognized triad of symptoms is larva currens, abdominal pain, and diarrhea. There is an endemic focus in southeastern Kentucky and in Appalachia, where most patients are usually white, male, older than 50 years, and from lower socioeconomic backgrounds. Cough, shortness of breath, wheezing, fever, transient pulmonary infiltrates, and eosinophilia are infrequent but may be encountered with the migration of larvae through the lungs. When adult worms develop and penetrate the mucosa in the small bowel, non-specific aching or epigastric abdominal pain and diarrhea can develop. With heavy infections, vomiting, malabsorption, steatorrhea, weight loss, edema, or a paralytic ileus with edema in the small bowel wall may be seen. In external autoinfection, there is a pruritic maculopapular rash or rapidly migrating linear urticaria called larva currens that is usually seen on the buttocks. Hyperinfection Syndrome Gastrointestinal signs and symptoms are common; they include crampy abdominal pain, bloating, watery diarrhea, and constipation. Patients can develop an ileus and small bowel obstruction, with diffuse tenderness and hypoactive bowel sounds. There is a high mortality, often with gram-negative enteric bacterial infection secondary to extensive larval spread from the intestine. All immunodiagnostic methods can cross-react with other nematode helminth infections. The safety of ivermectin in young children (<15 kg) and in pregnancy has not been established. Albendazole should be taken with a fatty meal to promote absorption; ivermectin should be taken on an empty stomach and with water. Immunocompromised patients with hyperinfection syndrome should be treated until clinical signs resolve. Because the autoinfective life cycle requires at least 2 weeks, some investigators recommend that treatment and screening should continue until fecal cultures have been negative for 2 weeks. For patients who cannot take or absorb oral medications, a veterinary parenteral formulation of ivermectin has been used.
Buy 0.5 mg cabgolin with visa
Define medicine 10 day 2 times a day chart quality cabgolin 0.5 mg, describe, and be able to use in context all the words in bold print in this chapter. The trachea branches into bronchi, which in turn branch into bronchioles of decreasing diameter. Review of Structure and Function the main function of the lungs is to transfer oxygen from the atmosphere to the blood, and carbon dioxide from the blood to the atmosphere. The lungs also serve as a filter of air and blood; like the kidney and liver, they are involved in the detoxification and excretion of toxins and metabolites. To carry out its main function, air must be moved from the atmosphere to the terminal units of the lung; this process is called ventilation, and gas must pass across tissue from air to blood or from blood to air, a process called gas exchange or diffusion. Anatomy the ventilatory pathway is treelike, with the trachea as the trunk, branching bronchi as limbs, and terminal air sacs called alveoli (sing. Movement of air in the tracheobronchial tree is brought about by muscular movement of the rib cage and diaphragm and elastic recoil of the lungs. Smooth muscle in the bronchial wall controls the diameter of the bronchi and thus the resistance to air flow. A cluster of alveoli with their associated respiratory bronchioles form an acinus. They consist of capillaries, a scant amount of connective tissue, and epithelial lining cells called Type I pneumocytes. Type I pneumocytes have very thin cytoplasm, much like an endothelial cell, and make up the inner lining of the alveolus. The endothelium of the capillary and epithelium of the Type I pneumocyte share basement membranes in areas, so gases diffuse over a very short distance. The other cell in the alveolus is the macrophage, which scavenges foreign particles that are aspirated into alveoli. Macrophages are also present within the connective tissue of the lung, for example, around, bronchioles. The pulmonary connective tissue contains a molecule that is particularly essential to its function, called elastin. This property affords the lung considerable elasticity: as the alveoli become distended with air during inspiration, the elastin fibers stretch, and their recoil helps propel the air out of the lung. The acinus is composed of a respiratory bronchiole, alveolar duct, and the cluster of alveoli that receive air from that duct. Instead, in two dimensions, the lung looks like a sheet of polygonal spaces enclosed by very thin alveolar walls. Normal pH is required to maintain the structural integrity of proteins in the extracellular fluid and on the surfaces of cells. If these are changed, basic and essential cell functions, such as maintenance of the Na+/K+ gradient across the cell membrane, are compromised, and cells consequently undergo injury and death. It is a weak acid that is easily soluble in water, and readily dissociates into either bicarbonate and H+ (acid), or carbon dioxide (base) and water, depending on whether there is an excess of acid or base in the environment. The mucus traps inhaled particles, and the cilia convey the mucus upward toward the mouth, from whence it is swallowed. When excessive material accumulates in the bronchi, the cough reflex helps expel it. Protection of the air spaces is provided by the specialized epithelial lining of the bronchial tree called the mucociliary escalator. When excessive mateO O rial accumulates in the bronchi, the cough Carbon dioxide Water Carbonic acid Bicarbonate reflex helps expel it. In the context of the discussion of lung diseases, however, the central chemoreceptors in the brainstem are the most important. Respiratory alkalosis can happen with hyperventilation, or if someone suddenly ascends to high altitudes and increases the rate of breathing to maintain oxygenation. Respiratory acidosis can complicate many of the diseases discussed in this chapter. This is not only due to acidosis but also increased work of breathing, as the chronically elevated respiratory rate leads to muscle fatigue and caloric consumption. Symptoms of respiratory alkalosis include lightheadedness, confusion, tingling in the hands and feet and around the mouth, and, if severe, syncope or fainting. These may be inflammatory diseases that adhere the lung to the chest wall so that it cannot fully deflate during exhalation because it is tethered to the rib cage, or muscular diseases that inhibit the action of the diaphragm or chest muscles so that the lungs cannot fully expand, or diseases affecting the connective tissue of the lung and destroying its elasticity, such as pulmonary fibrosis. Obstructive lung diseases are those that prevent the outflow of air through the bronchial tree so that air becomes trapped within the distal branches. Examples of obstructive lung diseases are chronic obstructive pulmonary disease, in which the bronchi are obstructed by thick mucus, and asthma, in which narrowing of the bronchi occurs through contraction of bronchial smooth muscle. Before we turn our attention to descriptions of diseases, a few definitions are in order. The following conditions are not diseases in themselves but manifestations of other processes in the lung. Either there is external pressure on the lung causing it to deflate, or there is obstruction of a bronchus with secondary resorption of the air distal to the obstruction. External pressure can be applied to the lung from substances accumulating in the pleural cavity. Air, transudative or exudative fluid, lymph, and blood can fill and distend the pleural space in various medical and traumatic conditions. Mucus distal to obstruction cannot be carried proximally and accumulates, becoming a nidus for infection. Bronchiectasis can occur in a variety of conditions-for example, following viral pneumonia, cystic fibrosis, tuberculosis, or aspiration of a foreign body. The treatment of bronchiectasis requires, treatment of the underlying cause of the obstruction, antibiotics or anti-inflammatory medications, and, if it is confined to a single location and the inflammation does not clear, surgical removal of the affected segment of lung. Two major processes result in consolidation: infection, which fills the alveoli with an inflammatory exudate including white blood cells, fluid, hemorrhage and necrotic debris, and cancer, which fills the alveoli with malignant cells and induces progressive scarring of the tissue. Consequently, the incidence of lung cancer in women has also gone up, to the point that currently, lung cancer accounts for more deaths in women than breast cancer does. In contrast, in some nations, such as Scandinavian countries, the social "ban" on women smoking (at least in public) during the same time period has been quite strong, and consequently the incidence of lung cancer in women is low. The lung is also the site of several serious diseases that are not necessarily related to cigarette smoking. The term pneumonitis is used in a less specific sense to indicate inflammation of the lung usually limited to the interstitium, in other words, the connective tissue of the alveolar walls, or surrounding bronchioles. Pneumonitis may result from a viral infection, but it may also be a hypersensitivity reaction to inhaled organic dusts, such as mold particles or bird droppings, or a reaction to radiotherapy or drugs such as certain antibiotics or chemotherapeutic agents. Pneumonitis affects the alveolar walls, causing them to swell, and thereby hinders diffusion of gases across them. In chronic cases, pneumonitis can result in irreversible scarring and severe restrictive lung disease. Asthma is a nondestructive lung disease that is most common in children and young adults. The smooth muscle of bronchioles constricts, in response to a particular stimulus, impeding the flow of air from the lungs. Asthma may be an allergic reaction to inhaled pollens or dusts, but it may also be triggered by cold, exercise, or cigarette smoke. In the lungs, the genetic aberration results in the production of thicker than normal mucus in the airways.
Syndromes
- Uses more words and understands simple commands
- Feeling tired during the day or falling asleep during the day
- EMG or nerve conduction studies
- Slow or rapid heart rate
- Allow the child opportunities to make choices and have some control in his or her life. This is particularly important, because research shows that the more people feel they have control over a situation, the better their response to stress will be.
- Barium swallow
Cabgolin 0.5 mg online
The risk is dose-dependent: the higher the exposure medications beta blockers cheap cabgolin 0.5mg overnight delivery, the more likely it is that a second cancer may develop. For example, patients who underwent radiation therapy for advanced breast cancer may develop angiosarcoma of the breast years after the initial treatment. Ultraviolet light from sunlight is a form of radiation to which we are exposed all the time. These arise most commonly in fair-skinned individuals because melanin, the pigment that imparts a dark color to skin, is protective against the ionizing effect of ultraviolet light. Squamous and basal cell carcinomas of the skin typically develop in older individuals on sun-exposed areas, such as the face and ears. The strongest risk factor for the development of melanoma of the skin is a history of blistering sunburns, and the incidence of melanoma is highest in fair-skinned individuals living in sunny locations (Florida, Australia) or engaged in occupations where they are exposed to ionizing radiation from the sun, such as fishing and farming. Not many microorganisms have been identified that cause cancers in humans, but there is no doubt that they can do so. Only one bacterium, Helicobacter pylori (which infects the mucosa of the stomach and causes gastritis), has been identified as a carcinogen in humans, but several oncogenic viruses are known. Some of these cancers are preceded by many years of low-grade, chronic inflammation, which appears also to play a role in carcinogenesis. Moreover, there is geographic variation in the development of virally induced cancers. However, the incidence rate of Burkitt lymphoma is much higher in certain areas of Africa than in the United States. Other, as yet not understood, factors are obviously involved in the induction of viral carcinogenesis. Many familial cancer syndromes have been identified and more are discovered every year. In these syndromes, an inherited genetic mutation puts patients at risk of developing cancer at a younger age than typical for that cancer type, because they already have sustained a "first hit" in their genome. In fact, even in a single gene, the location of the exact mutation that disables the resultant protein can be variable. For example, in retinoblastoma, the mutation can vary from a single base pair substitution, to insertions of a few base pairs, to large deletions. Finally, the genes involved in driving cancer in familial settings are not necessarily those that are most important in their sporadic counterparts. The Natural History of Cancer Cancers have a long life history, most of which occurs before there is any lesion that can be clinically detected. The multiple genetic "hits" required to turn a normal cell into a neoplastic growth capable of invading and metastasizing develop over years. The earliest "hits" may not result in a changed phenotype: if they were examined microscopically, the cells would look normal. Features of atypia include enlarged nuclei, decreased amounts of cytoplasm, irregular nuclear placement in a cell, multiple nucleoli, large nucleoli, and frequent mitotic figures. The nuclei of the cells are arranged at the periphery of the glands, and a droplet of mucin distends the cytoplasm toward the luminal surface. In the colonic carcinoma in B, the cells are no longer arranged in a regular pattern, the nuclei are overlapping one another and have irregular shapes and sizes, and the cells do not contain mucin droplets. A neoplastic clone may be atypical in appearance but still localized to its tissue of origin. Dysplastic cells have acquired some of the genetic alterations necessary for the development of overt malignancy, but they do not necessarily become malignant. Dysplasias can range from low grade, or exhibiting minimal atypia, to high grade, or exhibiting the amount of atypia one would expect to see in an invasive lesion. High-grade dysplasias are considered to be in situ lesions, or cancers that are still "in place. Tubular adenomas of the colon that show a high degree of atypia are designated as having high-grade dysplasia, but in the breast we use the term "carcinoma in situ. At this stage of development of neoplasia, surgical excision of the lesion would be curative: the cells have not yet spread beyond their site of origin, so removal of the neoplastic clone prevents the development of overt malignancy. While we tentatively consider in situ or high grade dysplastic lesions to have malignant potential, they are not per se malignant: they do not have the ability to invade or metastasize. To invade, malignant cells must be able to elaborate enzymes that destroy the basement membrane and the underlying connective tissue. The basal cells are tethered to a very thin basement membrane (not seen at this magnification), that separates the epithelium from the underlying connective tissue. The epithelium is hypercellular in comparison to normal, and the basal layer is greatly expanded, occupying about half the width of the epithelium. There is still a sharp demarcation between the epithelium and the underlying connective tissue. Epithelial cells have broken through the basement membrane and are present in detached clusters that have invaded deeply into the connective tissue. Sometimes, they provoke proliferation of fibrous tissue, so the lesion becomes very firm. The central areas of the tissue may become necrotic due to inadequate oxygenation. In addition, the neoplastic cells destroy the normal structures that were present. They may destroy the epithelial lining of a mucosal surface, resulting in ulceration. Invasion is a local process: the cells have moved from their site of origin in a continuous fashion into adjacent tissue. Indeed, small, relatively localized invasive cancers can be cured with surgical excision. The larger the tumor gets and the farther it grows into adjacent tissues, however, the less likely is it that surgical excision will be curative. This is because some of the malignant subclones will have developed the ability to metastasize, or to move to distant sites of the body in a noncontiguous fashion. First, the malignant cells must have acquired the ability to invade into neighboring tissue, as already described. This requires the production of enzymes capable of digesting basement membrane and extracellular proteins. The malignant cells must then be able to grow through the wall of a vessel, either a blood vessel or a lymphatic capillary. The granular red and yellow tissue at either end of the specimen is the marrow cavity of the bone. Note the irregular margins of the sarcoma where it is growing diffusely through the marrow space. The Natural History of Cancer of additional enzymes capable of breaking apart the basement membrane to which endothelial cells are anchored, and the junctions between the cells of the vessel wall and the vessel lining. Circulating lymphocytes and monocytes recognize the tumor emboli as "foreign" and rapidly clear them from the circulation. If the embolus is capable of surrounding itself with a platelet coat, however, it evades immune detection because it is hidden from the immune cells. The flow of blood can carry the tumor cell or cluster of cells, which is called a "tumor embolus," to distant sites. The tumor embolus then must adhere again to the vessel wall, at a distant site, and migrate back out of it. This is the inverse of the process of intravasation, and referred to as extravasation. Finally, the tumor cells must be able to establish themselves in the new location. This may require the ability to stimulate growth of its own blood supply, or angiogenesis. If a neoplasm demonstrates invasion or metastatic growth at the time of clinical detection, it is by definition malignant.
Generic cabgolin 0.5 mg free shipping
Invasion of virgin jungle during construction of new highways and irrigation and hydroelectric schemes has led to an increased incidence of snakebite in Brazil and Sri Lanka medications valium buy cabgolin 0.5mg on-line. On rare occasions, snakebite or injection of snake venom has been used for recreational purposes, suicide, or homicide. In snake-infested areas, boots, socks, and long trousers should be worn for walks in undergrowth or deep sand, and a light and walking stick should always be carried at night. Collecting firewood; dislodging logs and boulders with bare hands; pushing sticks or fingers into burrows, holes, and crevices; climbing rocks and trees covered with dense foliage; and swimming in overgrown lakes and rivers are particularly hazardous activities. Sleeping on the ground carries a risk of nocturnal krait bites in South Asia and of spitting cobra bites in Africa, but well-tucked-in mosquito nets are protective. Attempting to *Scientific (Latin) names are important because they are used internationally to describe the range of specificity of antivenoms. Specific antivenoms are manufactured for the treatment of envenoming by all these species (see Table 137. Various substances toxic to snakes, such as insecticides and methylbromide, have been used to keep human dwellings free of these animals. Cardiovascular and Autopharmacologic Toxins Some venoms release vasodilating autacoids such as histamine and kinins. Sarafotoxins from the venom of the Israeli burrowing asp (Atractaspis engaddensis) are similar to physiologic endothelins. They are potent vasoconstrictors of the coronary arteries and delay atrioventricular conduction. The venom duct opens within a sheath at the base of the fang, and venom is conducted toward the tip in a partially or completely closed groove or fang canal. Venomous snakes can inject doses of venom lethal to their natural prey at each of 10 or more consecutive strikes. Whether the dose can be adjusted according to the size of the prey or the intention of the snake is controversial. The high proportion of bites without envenoming ("dry bites") reported for species such as Calloselasma rhodostoma (>50%) or Pseudonaja spp. There is no support for the popular belief that snakes are less dangerous after they have eaten. The snake uses only a small fraction of the content of its venom gland at each strike. Variation in Venom Composition Venom composition varies enormously from species to species but also within a single species throughout its geographic range, at different seasons of the year, and ontogenically as the snake matures. Pharmacology When snakes bite people, venom is inoculated subcutaneously or intramuscularly. Smaller Mw elapid neurotoxins are rapidly absorbed into the bloodstream, whereas larger Mw phospholipase A2 presynaptic toxins and viperid enzymes are taken up more slowly through the lymphatics, sometimes causing visible lymphangitis and enlarged, painful lymph nodes. Continuing absorption of venom from the depot injected at the site of the bite may explain delayed or recurrent envenoming after an initial therapeutic response to antivenom. Redistribution of venom toxins into the vascular compartment may occur as a result of antivenom treatment. Most venoms are concentrated and bound in the kidney, and some components are eliminated in the urine. Crotaline venoms are selectively bound in the lungs, concentrated in the liver, and excreted in bile, whereas polypeptide neurotoxins, such as -bungarotoxin, are tightly bound at neuromuscular junctions. Central nervous system effects of venoms, such as drowsiness, remain controversial. Non-enzymatic polypeptide toxins and non-toxic proteins such as nerve growth factor are abundant. Viperid venoms have metalloproteinases, endopeptidase, arginine ester hydrolase, and kininogenase, as well as thrombin-like factor X and prothrombinactivating enzymes responsible for the anti-hemostatic effects of envenoming. They damage mitochondria, erythrocytes, leukocytes, platelets, peripheral nerve endings, skeletal muscle, vascular endothelium, and other membranes and produce presynaptic paralysis, opiate-like sedative effects, and the autopharmacologic release of histamine. Snakebite is usually a terrifying experience, especially for those who believe that all bites are rapidly fatal. Thus patients who are bitten but not envenomed may feel flushed and breathless, with constriction of the chest and a thumping pulse, palpitations, sweating, and effects of hyperventilation, such as dizziness, syncope, acroparesthesia, and carpo-pedal spasms. Such symptoms dominate many accounts of snakebites written by the victims and are falsely attributed to neurotoxicity. Misguided traditional pre-hospital treatments can result in swelling and ischemia of limbs whose circulation is occluded by tourniquets, bleeding or sensory loss resulting from local incisions, vomiting and other side effects caused by ingested herbal remedies, smarting eyes and conjunctivitis from instillation of plant juices, and bronchospasm from insufflation of oils. Rarely, snakebite may precipitate vasovagal collapse, angina pectoris, myocardial infarction, or cardiac arrhythmia. Necrotoxins A variety of venom myotoxic and cytolytic factors contribute to local tissue necrosis at the site of the bite. In other cases, digestive hydrolases, hyaluronidase, polypeptide cytotoxins (Elapidae), and, perhaps, secondary effects of inflammation are involved. Neurotoxins Postsynaptic (-)neurotoxins, such as -bungarotoxin and cobrotoxin, are three-finger fold polypeptides that bind to acetylcholine receptors on the motor end plate. Presynaptic (-)neurotoxins, such as -bungarotoxin, crotoxin, taipoxin, and notexin, are phospholipases A2 that prevent release of acetylcholine at the neuromuscular junction and damage the nerve endings irreparably so that recovery will depend on the growth of new synapses. Myotoxic phospholipases A2 in venoms of Elapidae, notably sea snakes and some Australasian, American, and Asian terrestrial elapids, and Viperidae can cause generalized rhabdomyolysis. General Symptoms and Signs the evolution of symptoms and signs of envenoming depends on the nature of the venom, the dose, and the site of injection. The earliest symptom is usually pain-felt immediately, but krait and sea snake bites may be painless. Usually, however, death comes hours after an elapid bite and days after a viper bite. Other symptoms include weakness, rigors, sweating, spontaneous bleeding, neurotoxic effects such as fasciculations or myokymia (Cr. Tender swelling spreads from the site of the bite, and there is early painful enlargement of lymph nodes draining the bitten area. Bullaecaused by Viperidae bites frequently dry up and slough without the development of necrosis. A pale, anesthetic, demarcated area of skin smelling of putrefaction signals the appearance of necrosis. Necrotic tissue is vulnerable to secondary infection by bacteria, including Clostridium tetani and other anaerobes. Massive swelling of the bitten limb and adjacent areas of the trunk indicates increased permeability leading to extravasation of circulating volume; a swollen limb can accommodate several liters of blood/plasma. Peri-oral and labial paresthesias and an abnormal metallic taste are common early symptoms after bites by Southern Pacific (Cr. Themost common sites of hemorrhage are intracerebral, gastrointestinal, retroperitoneal, and genito-urinary, including uterine bleeding in pregnant women. Oozing from sites of venipunctures or other recent trauma suggests that the blood is uncoagulable. Hemorrhagic and thrombotic (ischemic) strokes are an important cause of death and morbidity. Hypotension and Shock Early syncope can occur as part of the autopharmacologic syndrome after bites by vipers, Australasian elapids, and burrowing asps. A few species of vipers also produce neurotoxic effects, for example, South American Cr. Typically, neurotoxic symptoms develop early, but after krait and coral snakebites there may be a delay of 10 or more hours. Symptoms include vomiting, headache, paresthesia, hyperacusis, diplopia, blurred vision, heaviness of the eyelids, and difficulty in speaking. The levator palpebrae superioris and extraocular muscles are the most sensitive to neuromuscular blockade, and in some patients, the only feature of envenoming is bilateral ptosis and ophthalmoplegia. Paralyzed patients are fully conscious unless they are hypoxemic (respiratory failure) or hypotensive (circulatory failure). Generalized Rhabdomyolysis Envenoming by sea snakes,9 some Australasian elapids, Daboia russelii, and Cr.
Cabgolin 0.5mg otc
The route of infection is the basis of classification of the two major types of osteomyelitis kapous treatment discount 0.5 mg cabgolin with visa. Hematogenous osteomyelitis involves spread of the causative organism through the blood to localize in one bone and set up a focus of infection. The site of entry of the organism is often a skin infection, which may go unnoticed. The organism is usually Staphylococcus aureus, and the site of the osteomyelitis is usually the metaphysis of a long bone, near but not involving the epiphysis. The purulent infection may produce sinuses or channels of inflammation from the site of infection in the bone to the skin. These continually drain pus, and in very severe or prolonged cases, bits of necrotic bone may also exit through the sinus. The necrotic bone at the site of infection must be removed surgically, because antibiotics will not be effective against bacteria lurking in dead bone. The clinical Osteoporosis Osteopenia and osteoporosis both refer to quantitative decrease in bone mineralization. The difference between the two terms is that osteoporosis is more severe and is more likely to result in pathologic fracture. Osteopenia can be demonstrated by a special type of radiographic procedure called dual-energy X-ray absorptiometry, which measures how much of each of two X-ray beams with different amounts of energy are absorbed by bone. The result of this study is not a conventional X-ray image, but rather a number, or T-score, that relates the measured bone density to normal values. In the laboratory, bone health is indicated by serum levels of calcium, phosphorus, and alkaline phosphatase. Conditions that cause metabolic breakdown of bone typically cause elevated alkaline phosphatase levels and altered calcium and phosphorus levels. However, these tests are not sensitive for osteopenia or the type of osteoporosis that occurs in postmenopausal women. Bone mineral density reaches its peak in the early 30s and begins to decline after this point. In women, there is a direct relationship between estrogen levels and bone Specific Diseases mineralization. After menopause, when estrogen production by the ovaries ceases, bone resorption by osteoclasts far outstrips bone mineralization, with a net decrease in bone strength. Whereas most osteoporosis occurs in postmenopausal women, it may occur in older men, in patients on long-term corticosteroid therapy, and in those subject to prolonged bed rest. Persons with large bones are less affected than persons with small bones, and physically active people, especially those who engage in weight-bearing activities such as jogging, hiking, weight-lifting, or stair climbing, develop osteoporosis at a slower rate. Obviously, estrogen is necessary for maintaining bone, and lack of exercise induces resorption of bone simply because it is not being used. However, lack of dietary calcium and interference of normal calcium metabolism by diseases such as chronic renal failure, hyperparathyroidism, excess corticosteroids, hyperthyroidism, inadequate intake of vitamin D, and certain intrinsic diseases of bone such as Paget disease, can all result in osteoporosis. Other risk factors include smoking, eating disorders, female sex, white or Asian race, and other diseases the patient may have that affect bone, such as rheumatoid arthritis. Once developed, reversion back to normal bone thickness is very difficult if not impossible to achieve. Therefore, prevention of the development of the disease is most important, and this must be done years (decades) before the disease is likely to become manifest. Therapies that have been directed at this goal include increased calcium intake, vitamin D supplements, estrogens in menopausal women, testosterone in men with low levels, exercise, bisphosphonates (agents that inhibit bone resorption by osteoclasts), and calcitonin (a thyroid hormone that also inhibits bone resorption). Unfortunately, in most instances, preventive treatment is not employed, and complications are treated as they develop. The most common complications of osteoporosis are compression fractures of vertebrae and hip fractures. Hip fracture is a severe acute illness that is often fatal or leads to permanent disability, particularly in frail older women. Osteomalacia and Rickets Osteomalacia and rickets are relatively rare conditions characterized by softening of bone. They differ from osteoporosis in that there is inadequate deposition of calcium and phosphorus, rather than accelerated absorption of bone. The majority of cases are secondary to poor intake or poor utilization of vitamin D, with consequent imperfect deposition of calcium and phosphorus in bone. It occurs most often in the middle-aged to older adult and is estimated to be present in 20 million persons in the United States. The lesion consists of erosion of the articular joint cartilage, with subsequent deformity of the cartilage and of the bone, resulting in stiffness and decreased motion. This pattern of involvement, plus a typical X-ray picture, helps distinguish degenerative from rheumatoid arthritis. The joint lesions, characterized by pain, stiffness, and deformity, are caused by inflammation of the synovial lining. As the inflammation extends on to the joint surface, it destroys cartilage and produces a layer of granulation tissue called a pannus, which induces destruction of the underlying cartilage and resorption of bone. Eventually, the entire joint surface may be destroyed and replaced by fibrous tissue, resulting in ankylosis, or joint rigidity. Rheumatoid arthritis is three times more common in women than in men, and the overall prevalence is nearly 2% of the population. The disease varies in severity from mild joint stiffness to distortion and ankylosis of many joints, with almost total loss of function. The joint spaces, or the spaces between the tibia, femur, and patella, are narrowed, and the edges of the bones are blurry, indicating erosion and reactive sclerosis of the articular surfaces of the bone. The contour of the patella is quite irregular and large osteophytes, or "spurs," are growing from its edges. Many patients with severe rheumatoid arthritis also have chronic inflammation and vasculitis involving other organs such as the heart, muscle, lungs, skin, and blood vessels. As with most autoimmune diseases, the exact etiology of rheumatoid arthritis is not known. Most people with rheumatoid arthritis have antibodies against a particular region on the immunoglobin G (IgG) molecule: in other words, they produce an antibody against an antibody. Immune complexes form in serum and synovium, but they are not thought to be critical in stimulating the inflammatory response. Rheumatoid factor can be measured in serum and is a marker of disease activity, but it can also be present in other diseases and even in individuals without rheumatoid arthritis. The disease usually develops over months and years, with gradual involvement of additional joints. The disease can also wax and wane, with periods of severe arthritis followed by periods of remission. Severe joint deformities can be corrected by surgically replacing them with prostheses. Ankylosing spondylitis is an inflammatory arthritis predominantly involving the spine and sacroiliac joints. Excess uric acid is deposited in many tissues, particularly joints, causing painful arthritis. Formerly, gout was called the "disease of kings" because it can be caused by excess consumption of wine and red meat, and it was associated with a gluttonous lifestyle. Gout occurs almost exclusively in men older than the age of 30 years and clinically manifests with bouts of painful arthritis. Ganglion cysts are often associated with continued trauma and may be painful, although they usually arise insidiously as a simple swelling. The most common malignant tumors are metastatic cancers from sites such as the breast, lung, prostate, and kidney, as well as multiple myeloma and lymphomas. The most common primary malignant neoplasms of bone-osteosarcoma and Ewing sarcoma-are diseases of children and young adults. Paget Disease of Bone Paget disease, or osteitis deformans, is a localized or multifocal enlargement of bone of unknown cause that affects about 2% of the population, typically in persons older than 40 years of age. Initially, the affected bone may be more porous, but there is a gradual haphazard bony proliferation leading to some deformity of the bone and occasionally to pathologic fracture.
Purchase cabgolin 0.5mg fast delivery
This abnormal gene will be present in all the cells of the new individual and will be passed to subsequent generations by the germ cells medicine 834 purchase cheapest cabgolin. Thus, abnormal genes can pass from one generation to the next or can arise by new mutations in germ cells. Mutations can also occur in nongerm cells (somatic cells), but the effects are limited to the individual and not transmitted to the next generation. Each genetic trait is influenced by two genes, one on each of the paired chromosomes. One of the alleles of a pair may be dominant over the other-that is, it determines how the genetic trait is expressed. A recessive gene results in an abnormal trait only when both alleles are defective. Some of the genes on the female, or X, chromosome are not present on the Y chromosome, so a gene on the X chromosome is expressed in a dominant fashion in a male, whereas it is recessive in a female. Genes that are located on the X or Y chromosomes are called sex-linked, while those occurring on any of the other chromosomes are called autosomal. Although it is the genes that carry the blueprints for cellular structure and function, the genetic makeup alone does not determine how genes are expressed. Sometimes an abnormal dominant gene or pairs of abnormal recessive genes do not produce an abnormal trait. An abnormal trait may be expressed differently in individuals with an identical genotype for the alleles responsible for the trait. Defects in these genes can lead to mitochondrial genetic diseases, which primarily affect the nervous system and muscles. Paternal imprinting silences certain genes that are derived from the father so that only the maternal allele is expressed. For all these reasons, the phenotype-the physical and functional manifestation of genetic traits-is not simply a reflection of the genotype. It is dependent on a complex interplay between genes, the environment, and other factors that together influence how a gene will be expressed. The cells undergo rapid mitotic division during this stage and are therefore very sensitive to cytotoxic and mutagenic insults, such as poor nutrition, infection, various chemicals, including pharmaceutical agents, toxins such as alcohol, and radiation exposure. During the embryonic period, the fertilized egg is transformed into a fetus with a body structure and organs. Obviously, abnormalities in chromosome number and structure will have an adverse effect on this tightly controlled developmental sequence. Most spontaneous abortions occurring during this period involve embryos with severe chromosomal abnormalities. The fetal period spans the time from the eighth week after fertilization to birth. This period is primarily one of growth and maturation of organs and tissues, and results in an individual who can survive and grow without the direct support of the maternal blood supply. The lungs, kidneys, liver, and brain require the longest time to reach maturation. Fetal growth depends not just on a sound chromosomal makeup but also on a healthy uterine environment. Maternal diseases that interfere with blood supply to the placenta can result in stunted growth or intrauterine fetal demise; intrauterine infections can cause severe damage to developing fetal tissues; abnormal implantation of the placenta and true knots in the umbilical cord can jeopardize blood flow to the fetus; and amniotic bands can wrap around fetal body parts and cause asymmetric development or even infarction. These abnormalities are called congenital: they are present at birth, but not necessarily genetic in origin. The first 8 weeks is the embryonic period, and the rest of the time is the fetal period. Because it is difficult, in most pregnancies, to ascertain when fertilization occurred, pregnancies are practically dated in reference to the last menstrual period, or roughly fertilization plus 2 weeks. Gestational age makes the embryo/fetus roughly 2 weeks older than it actually is, and makes pregnancy 40 weeks long rather than 38. The perinatal period is defined as the period from 2 weeks before birth to 4 weeks after birth. The major event of the perinatal/neonatal period is adjustment to life outside the womb. Kidney and liver function increases at this time to meet the demands formerly met by the placenta and the flow of blood from the mother. Functional derangements of the heart, lungs, kidney, and liver that had not interfered with fetal development may manifest at this stage of life. Major events during this period include growth, development of motor and intellectual functions, and development of immunologic defenses against foreign substances. The period of childhood covers the period from infancy to puberty and is primarily one of growth and refinement of motor and intellectual functions. Abnormalities of development may be the result of altered genetic structure or environmental effects, or a combination of the two. The interaction of genetic and environmental factors is complex, and for any particular Definitions disease may not be well understood. We use the term developmental abnormality in a broad sense to refer to diseases that affect normal maturation. Most abnormal genes are acquired at the time of fertilization, but most genetic diseases do not manifest until sometime after birth. Monogenetic (single-gene) defects encompass the classic genetic diseases in which a single abnormal gene is responsible for the disease and can be traced through family trees. Polygenetic (multiple-gene) or complex gene defects involve more than one abnormal gene and sometimes interaction with environmental factors for their expression. Inheritance patterns of multiple-or complex gene defects are not clear-cut, but there is some tendency for these diseases to occur in families. Chromosomal diseases are defined by microscopically visible structural changes in chromosomes. Chromosomal diseases often result in genetic abnormalities so severe as to preclude reproduction and transmission of the abnormality. Gordana Raca, Department of Pathology and Laboratory Medicine, University of Wisconsin School of Medicine and Public Health. Genetic and chromosomal diseases may also not manifest until sometime after birth. Familial diseases are diseases in which several family members have the same genetically or chromosomally based disease. Many individuals with genetic diseases do not have a family history of the disease either because it is recessive. In the latter situation, the disease can be classified as both congenital and familial. The abnormality appears in a parent of each involved individual; half the children of a parent with the trait will inherit it. Frequency and Significance of Developmental Abnormalities Approximately 2% of newborns have congenital anomalies. The causes of these anomalies can roughly be estimated as follows: 65% unknown, 20% genetic, 5% chromosomal, and 10% environmental. The overall frequency of genetic diseases is difficult to establish because of the delayed onset of some types and the variable effects of environmental factors on their expression. Monogenetic Diseases Monogenetic diseases are classified according to whether the abnormal gene is located on an autosome or sex chromosome, and whether it is dominant or recessive. Thus, there are four possible modes of inheritance: autosomal recessive, autosomal dominant, sex-linked recessive, and sex-linked dominant. Many of the thousands of types of genetic diseases are incompletely penetrant (not all persons with the affected genes will have the disease) and many are variably expressed (not all persons will have the disease to the same severity). Most genetic diseases are uncommon or rare; yet, when taken in aggregate, most families are influenced by some type of multifactorial genetic disease. Huntington disease, a devastating disease causing destruction of neurons in the brain, is an example of an autosomal dominant disease with complete penetrance. Because it is a dominant trait, the offspring of an affected individual have a 50% chance of inheriting the defective gene, and because it is completely penetrant, if they inherit the gene, they will develop manifestations. Unfortunately, manifestations of Huntington disease do not develop until the individual has reached middle age and has most likely already had children, so the gene has already been transmitted to the next generation. Cystic fibrosis and sickle cell anemia are examples of autosomal recessive diseases.
Cheap generic cabgolin canada
Colon cancer may come to attention with constipation medications versed discount cabgolin 0.5mg, and patients with pancreatic cancer may present with jaundice because of back-up of bile that cannot flow through the occluded bile duct. Infection is another complication of obstruction, because blockage of any lumen leads to accumulation of secretions that are good culture media for bacteria. It is such a large spaceoccupying lesion that is has pushed the remaining white matter against the ventricle, essentially causing it to collapse, and has pushed the midline structures to the left. The portion of bowel proximal to the colon cancer becomes dilated, resulting in excruciating abdominal pain. In addition, with hematologic malignancies, the white blood cells may be deficient in phagocytic ability. Inadequate nutrition in the terminally debilitated cancer patient also impacts the ability of the immune system to function properly. Because lymphocyte quantity and quality are often deficient in neoplastic disease, cell-mediated immunity may be particularly impaired. Immune deficiency is manifested by the occurrence of unusual infections caused by fungi, protozoa, viruses, and bacteria that are ordinarily not pathogenic in normal hosts. Major mechanisms include blood loss caused by hemorrhage, bone marrow replacement by neoplastic cells, and decreased production of red blood cells resulting from the effects of chemotherapeutic drugs or radiation on bone marrow. This radiograph of the hip shows a large lytic (destructive) lesion involving the ischium of the pelvis and extending into the acetabulum. The patient likely has severe pain in the hip, and is susceptible to developing a fracture through the weakened bone. Hemorrhage Cancers on mucosal surfaces or the skin may ulcerate and bleed, leading to either acute or chronic blood loss. Inapparent blood in feces (occult blood) can be detected by a simple chemical test during a routine examination. Cancers of the lung, breast, and prostate are especially likely to metastasize to bone. Multiple myeloma, a neoplastic proliferation of plasma cells, is a primary cancer of bone marrow that commonly destroys adjacent bone. Another mechanism by which a neoplasm can cause pathologic fracture is by induction of osteoporosis. The interplay of a variety of mechanisms produces infections in patients with cancer. At the local level, erosion or ulceration of epithelial surfaces by a tumor allows entry of microorganisms through impaired defenses. Obstruction results in pooling of secretions and their subsequent colonization by organisms. Hormone Production A few neoplasms secrete hormones that lead to specific clinical manifestations. Benign neoplasms of the endocrine glands most commonly cause overproduction of hormones. The chest of this man has a "skin and bones" appearance because subcutaneous tissue and muscle has atrophied in the setting of a chronic, wasting disease. For example, male or female patients with a pituitary adenoma may suddenly begin to produce milk due to release of the hormone prolactin by the tumor. Tumors of the endocrine islets of pancreas can over produce insulin, for example, which induces hypoglycemia. Other neoplasms, such as small cell carcinoma of the lung may produce hormones in sufficient quantity to cause clinical effects. Manifestations of aberrant and uncontrolled hormone production by a malignant neoplasm are called paraneoplastic syndromes. The test must be able to detect disease when it is present and not when it is absent. No laboratory test in medicine is absolutely accurate: each has a known rate at which it gives a false result. These results are either false positives (the patient is identified as having the disease when s/he actually does not), or false negatives (the patient has the disease but it was not detected by the test). Ideally, a screening test would never yield a false positive or a false negative result, but such a test does not exist. Even the Pap smear for cervical cancer, which is one of the most effective screening tools available, has a false negative rate of approximately 50%. Everyone in the population must be screened in order for the test to provide a survival benefit. If the screening test were available only to a small subset of patients, it would obviously not detect "everyone" with the disease, and therefore the test would fall short of fulfilling the purpose of screening. In fact, universal screening, in which truly "everyone" is tested for the disease, is often not feasible or necessary. The only screening test we have currently that has a high detection rate for lung cancer is radiography, but this is expensive and exposes the patient to radiation, which in itself is harmful. Therefore, routine screening for lung cancer by radiography is not performed on patients who have never smoked: the yield of a positive test in this population is not sufficient to warrant the risks involved. On the other hand, screening the population of patients who have ever smoked (currently or in the past) is of high yield, because this is the population that has the highest incidence of the disease. For similar reasons, the population of patients that should be screened is carefully chosen for most cancer screening tests: colonoscopy for adults beginning at the age of 50, mammography for women beginning age 40, but earlier in women with a family history of breast or ovarian cancer, and so forth. You can see the enormity of the problem with a little math: if a test costs $1 per person, and it will be administered to the U. If the patient presents with symptoms, or has abnormalities detected on physical examination or screening exams, additional tests are performed to better delineate the process. The diagnosis is confirmed by pathologic examination of tissue or fluid removed from the lesion. A pathologic diagnosis is required to confirm that the growth is malignant and to identify the histologic nature of the disease. The lump may be a benign growth such as a fibroadenoma, or an inflammatory nodule that formed subsequent to trauma, or it may be a preinvasive neoplasm, an invasive carcinoma, or, very rarely, a sarcoma. Each of these different types of pathologic processes requires a different treatment approach, and obviously has very different prognostic implications for the patient. Discovery of cancer, especially in older adults, often occurs when a physician sees the patient for some other disease. Physicians may detect asymptomatic cancer of the breast, prostate, or testis by palpation, and they can inspect the skin for malignant melanoma and carcinoma. In addition, as already discussed, cancers are ideally diagnosed when they are still small, or when they are still in a premalignant stage, but they rarely cause symptoms at an early stage of growth. Small and localized cancers can be detected by screening procedures: simple and cheap tests that are geared at detecting abnormalities that could indicate the presence of cancer and prompt definitive testing if positive. The purpose of screening is to identify people with a disease when it is still in its early stages and treatable. Moreover, the test needs to be performed periodically, in order to catch new incidences of disease, so that would be a quarter of a million dollars spent every year for that screening procedure. For all screening tests, the cost must be balanced against the benefit of detection: an expensive screening test is not necessarily a good investment. Colonoscopy, the screening test performed for colon cancer, is also relatively safe, but quite uncomfortable. It is billed as an outpatient procedure, but is quite involved: the "colon prep," whereby the colonic contents are purged so adherent fecal material does not obstruct the view of the colonic mucosa, is in and of itself unpleasant; the procedure itself requires some degree of anesthesia, to reduce discomfort as the colonoscopy tube is carefully slipped up through the length of the colon, and recovery from the anesthesia precludes most patients returning to work that day. While it exposes the patient to minimal risk, the inconvenience involved is the factor most commonly cited for why patients skip getting the test. Radiographic tests for lung or breast cancer expose the patient to ionizing radiation. With these tests, the risk of the procedure needs to be balanced against the risk that the patient actually has cancer. In the case of most cancers, the intent of screening is to find the cancer at a stage when it can still be cured with surgery. It is easier to treat cancer at the pre-invasive or very early invasive stage than it is in the late stages of the disease, when cancers would otherwise come to attention because of the symptoms they cause. Prostate cancer grows very slowly and is therefore not readily amenable to radiation therapy or chemotherapy. Surgery (prostatectomy) carries significant risk of side effects (urinary incontinence and sexual impotence). Longitudinal studies have shown that "watchful waiting," or surveillance for progression of prostate cancer, affords men with low-grade cancer similar survival outcomes to aggressive interventions. The next most common cancers are prostate cancer and breast cancer: for the former, a very good screening test is available, but there is no effective cure; for the latter, the screening test involves an imaging procedure that can only be performed at a medical center, is costly, uncomfortable, and exposes the patient to radiation risk.