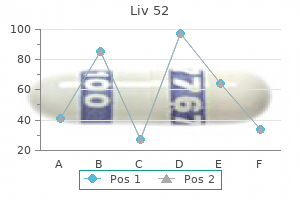
Liv 52 200ml cheap
However 2d6 medications trusted liv 52 100 ml, if disease is refractory to these drugs, an echinocandin (caspofungin, micafungin, anidulafungin) should be used. Primary opportunistic invasive nondermatophyte infections Opportunistic dermatologic infections in cancer patients can be caused by Aspergillus, Zygomycetes, Fusarium, Scedosporium, Candida, and Cryptococcus species. The portal of entry for molds is the sinopulmonary tract from where they can disseminate. A combination of cultures, histopathology, and molecular biology should be utilized for optimal diagnosis. Cultures should be interpreted with caution because these organisms are common environmental contaminants and may take weeks to grow. Primary dermatologic infection by molds and yeasts should be treated as if they represented an invasive systemic disease. If one does not have a specific fungal species diagnosis, empiric therapy with a lipid formulation of amphotericin B should be initiated to cover most possible fungal etiologies (see Appendix 31. In addition to antifungal therapy, an attempt must be made to eradicate all involved invaded and necrotic tissue: 1. The (1,3)-d-glucan assay may aid in diagnosis: (1,3)-d-glucan is produced by most fungi with the exception of Zygomycetes and Cryptococcus species. With the rising incidence of azole and echinocandin resistant invasive candidiasis, it is advisable to consider initiating echinocandin or amphotericin B lipid formulation therapy until you receive microbiologic data that allows you to "step down" the therapy. Finally, if the patient has documented (positive blood cultures) candidemia, the central venous catheter should be removed. The treatment of choice for disseminated cryptococcosis in the immunocompromised host is liposomal (or conventional) amphotericin B plus flucytosine. Cutaneous manifestations of systemic disseminated disease Aspergillus is rarely, if ever, found in the bloodstream, and skin involvement usually results from direct inoculation. The typical presentation is of rapidly developing, multiple, widespread erythematous papular or nodular painful lesions anywhere on the body with predilection for extremities. Histopathologic examination often permits distinction between Zygomycetes and other molds. Diagnosis Diagnosis of mold infections can be enhanced by serologic tests and histologic examination of (preferably) a deep skin biopsy. The Aspergillus galactomannan assay should be elevated in a patient with invasive aspergillosis, but a false-negative can result in a patient who is already on an antimold agent. The (1,3)-dglucan assay may help, which is elevated in most yeast and mold infections except invasive zygomycosis and cryptococcosis. Also, false-positive results can occur in a patient receiving piperacillintazobactam. If there is evidence of a lung lesion, bronchoscopy (with bronchoalveolar lavage fluid) should be performed. If there is sinus involvement, sinusotomy with biopsy (or scraping) should be performed. If zygomycosis cannot be ruled out, a Zygomycetes active antifungal agent should be initiated. This should be an amphotericin B lipid formulation such as amphotericin B lipid complex or liposomal amphotericin B. Amphotericin B lipid formulations, the echinocandins, and posaconazole are second-line choices. Therapy should also include the removal of any focus that is accessible and, preferably, singular. Parasitic infections In general, parasitic involvement of cutaneous structures is uncommon among cancer patients, but in an appropriate setting The prevalence in high risk cancer patients is low, likely because of the standard use of trimethoprim-sulfamethoxazole prophylaxis (for Pneumocystis (carinii) jiroveci). Histopathologic examination of involved skin demonstrated amebic trophozoites and cyst forms. Among other pathogens, Pseudomonas aeruginosa, Serratia marcescens, Enterobacter aerogenes, and Klebsiella pneumoniae were encountered less commonly. The most common sites of bacterial infections were the seborrheic regions, commonly affected by the papulopustular rash. Other sites of infection included periungual tissues, nails, trunk, and extremities. Thus, for systemic infections, an empiric regimen might consist of vancomycin, a carbapenem (imipenem or meropenem), fluconazole or an echinocandin, and acyclovir (high dose: i. This usually consists of topical corticosteroid cream and a semisynthetic tetracycline antibiotic. Clinically, moist desquamation, a more severe form of acute radiation dermatitis characterized by edema, fibrinous exudates and pain, can be associated with a bacterial superinfection. The infestation was limited to the upper chest, the area of previous irradiation, with histopathologic and immunohistochemical examination that revealed a reduced number of Langerhans cells, likely related to radiotherapy. Clinically, erysipelas manifests with a raised erythematous tender well-demarcated area with raised borders. Conclusions Oncology patients are highly susceptible to a wide spectrum of dermatologic infections, with bacterial, viral, fungal, and parasitic organisms being the topmost concerns. Individuals undergoing active treatments with chemotherapy, radiation, therapeutic transplantation, or a combination of these are particularly at risk, considering their relative immunosuppression. An impaired immune system may result in atypical or more severe manifestations and potentially lead to invasive and disseminated disease. Moreover, primary localized skin or adnexal infections may serve as a source for systemic dissemination. Thus, close vigilance and consideration of all potential infectious culprits as part of the differential diagnosis is critical in establishing an early and a correct diagnosis. Of 1877 women, those with lymphedema were twice as likely to develop cellulitis (15. Cellulitis or lymphangitis in the setting of lymphedema is usually caused by Gram-positive bacteria. Other cases of successful treatment (with trimethoprim-sulfamethoxazole, rifampin, and ketoconazole) of Acanthamoeba meningitis have been reported. Acanthamoeba isolates have been reported to be sensitive (in vitro) to pentamidine, ketoconazole, flucytosine, and amphotericin B. With improved survival, patients receiving cancer treatment are now living long enough to experience a range of late adverse events of cancer treatment. It is imperative for clinicians to continue long-term surveillance of cancer survivors and to educate them regarding possible cutaneous eruptions or lesions, as they can be a direct or indirect result of their underlying cancer or treatment. In some cases, they may herald rapidly progressive disease, so their recognition and prompt initiation of treatment can significantly affect clinical outcome. Described in this chapter are four main categories of late dermatologic conditions that can be seen in cancer patients: secondary neoplasms, cutaneous metastasis, radiation effects, and scars. Radiation-induced cutaneous neoplasms Radiation therapy has been well documented to induce both benign and malignant secondary cutaneous neoplasms (Table 32. One of the most concerning late effects of ionizing radiation is the induction of malignant diseases. In this series, there were also three cases of adnexal tumors, two malignant non-Hodgkin lymphomas, and four melanomas. The average age at irradiation Dermatologic Principles and Practice in Oncology: Conditions of the Skin, Hair, and Nails in Cancer Patients, First Edition. Patient age at diagnosis of malignancy varied from 20 to 83 years with an average of 47 years. In a report from the Childhood Cancer Survivor Study, radiation therapy was associated with a 6. The cutaneous carcinomas may occur on skin showing concurrent chronic radiation dermatitis or on skin with normal appearance but often with histopathologic changes suggestive of radiation dermatitis. When distant metastases occurred, the most common site was bone, followed by lung and distant skin. Therefore, patients who have undergone radiation treatment should be counseled regarding avoidance of future excessive sunlight. The molecular mechanisms underlying ionizing radiationinduced carcinogenesis of the skin is not clear. Cells exposed to ionizing 341 Section 5 Late Cutaneous Events from Cancer Treatment Table 32.
Buy genuine liv 52 online
These anucleate corneocytes comprise the keratinized stratum corneum medicine wheel wyoming generic liv 52 60 ml fast delivery, the lipid (ceramide) and protein (loricrin) rich surface barrier of the skin. The epidermal barrier regulates desquamation, permeation of water and environmental solubles, activity of antimicrobial peptides, and initiation of cytokine-mediated inflammation, among other critical functions. Keratinocytes throughout the epidermis are tightly intercalated through calcium-dependent cell surface adhesion molecules known as desmosomes. Immigrant cells of the epidermis include melanocytes, Langerhans cells and Merkel cells. Melanocytes are neural crestderived dendritic cells largely residing in the basal layer of the epidermis. These cells synthesize pigment and are primarily responsible for imparting color to the skin. Langerhans cells are the marrow derived dendritic antigen presenting cells of the epidermis whose cytoplasm contains characteristic racket-shaped structures known as Birbeck granules. Tumor antigens presented by Langerhans cells mount a tumor-specific immune response and, as such, these cells have been evaluated as vehicles of antitumor and vaccine therapies. Merkel cells are slow-adapting type I mechanoreceptors located in sites of high tactile sensitivity, including the lips, oral cavity, digits, and around hair follicles. Merkel cell carcinoma has been a focus of attention in dermatology and oncology given its aggressive and recalcitrant nature. This junction contains interconnecting layers of proteins (hemidesmosomes, basal lamina, lamina densa, anchoring fibrils) that secure the epidermis to the dermis and form a semipermeable barrier. Blistering Dermatologic Principles and Practice in Oncology: Conditions of the Skin, Hair, and Nails in Cancer Patients, First Edition. Oxygen and nutrition delivery, temperature and blood pressure regulation, wound repair, and immunologic progression represent just some of the roles of the cutaneous vasculature. There are two main horizontal plexuses of vessels that run through the upper and lower portions of the dermis. The vasculature tree in the skin advances from arterioles to precapillary sphincters to arterial and venous capillaries which become postcapillary venules, and ultimately venules. Lymph channels of the skin regulate interstitial pressure through resorption of released fluids and debris from vessels and tissue. Lymphatics begin as blind endings in the papillary dermis and drain into a horizontal plexus of lymph vessels that run below the papillary dermal venous plexus. Lymph flows vertically downward through the dermis to a deeper collecting plexus located at the base of the dermis. Cancer patients are susceptible to pathologic conditions involving the lymphatic vessels, including lymphedema and lymphangitis. Additionally, the importance of lymphatics in the progression and spread of cancer is now well documented. Dermis the dermis provides pliability, elasticity, and tensile strength to the skin, with a thickness ranging from 0. The connective tissue matrix of the reticular dermis is composed of interwoven bundles of densely packed helical collagen fibrils surrounded by elastic fibers. The matrix also contains glycoproteins, proteoglycans, and glycosaminoglycans that form the water binding ground substance of the dermis. The predominant cell types within the dermis include fibroblasts, macrophages, mast cells, and circulating cells of the immune system. Mesenchymally derived fibroblasts synthesize and degrade connective tissue matrix proteins which provide the structural framework for the dermis. Bone marrow derived macrophages differentiate into circulating monocytes and migrate to the dermis before differentiating further in tissue. Macrophages in the skin serve a number of important functions including antigen processing and presentation, phagocytosis, and wound healing. Mast cells are integral to the initiation of immediate-type hypersensitivity reactions in the skin Preformed histamine, which is initially confined to secretory granules within mast cells, is the major mediator of these reactions, although tryptase, chymase, carboxypeptidase, and other mast cell mediators are frequently involved. Nerves the skin contains a network of sensory and sympathetic autonomic fibers which regulate a number of critical functions in the skin. Cutaneous nerves arise segmentally from spinal nerves and follow a pattern in the skin similar to the vasculature. Pencillate sensory fibers and specialized corpuscular structures function as the receptors of touch, pain, temperature, and itch. The type and density of these receptors vary, and this accounts for the differences in sensation and acuity across body sites. After primary infection with the varicella zoster virus, the virus migrates along sensory nerve fibers to the satellite cells of dorsal root ganglia and becomes dormant. The virus may become reactivated by conditions of decreased cellular immunity and result in herpes zoster, a dermatomal eruption of grouped vesicles on an erythematous base. Subcutaneous tissue Beneath the dermis lies a layer of subcutaneous adipose tissue, also known as the panniculus, which is subject to a number of inflammatory and neoplastic disorders. The subcutaneous tissue insulates and cushions the body and serves as one of its energy reserves. It is federated with the dermis through networks of vessels, nerves, and appendages. Synthesis and storage of fat result from accumulation of lipid within adipocytes and from proliferation of existing adipocytes. Regulatory feedback signaling in this process is mediated by leptin, a hormone secreted by adipocytes. Adipocytes are organized into lobules separated by septa of fibrous connective tissue containing vessels, lymphatics, and inflammatory cells. Clear (secretory), dark (mucoid), and myoepithelial cells comprise the secretory coil to generate an ultrafiltrate of an isotonic precursor fluid in response to cholinergic stimulation. The duct reabsorbs sodium and chloride to produce hypotonic sweat which is secreted on the surface of the skin. Apocrine sweat glands the physiologic role of apocrine sweat glands in humans is unclear. These glands are found in the axillae, perineum, and areolae, and begin to secrete a milky odorless fluid around the time of puberty. Though sweat secreted by apocrine glands is odorless, it emits odor when acted upon by bacteria upon reaching the surface of the skin. Apocrine glands have a coiled structure located at the border of the deep dermis and the subcutaneous fat. This coiled structure extends upward into a straight tubular structure that drains into the mid-portion of the hair follicle and shares a common secretory opening to the surface with sebaceous glands. Sebaceous glands Sebaceous glands are composed of lobules of lipid-producing sebocytes lining sebaceous ducts associated with hair follicles throughout the body. A sebaceous gland and the associated hair follicle are termed a pilosebaceous unit. Nonhair-bearing sites including the mouth (Fordyce spots), the eyelids (meibomian glands), the nipples (Montgomery glands), and the genitals (Tyson glands) also have sebaceous glands. Only the palms and soles, which also have no hair follicles, are completely devoid of sebaceous glands. Sebaceous glands release lipids through holocrine secretion, a process in which the entire cell disintegrates to extrude its contents. Human sebum reaching the surface of the skin consists of a mixture of lipids including cholesterol, squalene, triglycerides, and free fatty acids. The hair follicle is divided into the infundibulum and the isthmus which comprise the upper portion of the follicle, as well as the suprabulbar area and the bulb which make up the lower follicle. While the upper follicle is permanent, the lower follicle regenerates with each follicular cycle. Also residing within the matrix are melanocytes which produce pigment that forms the basis of hair color. The cuticle of the hair shaft covers and protects the hair once it exits the shaft. Hair follicles perpetually cycle through three phases: anagen (growth), catagen (involution), and telogen (rest). Hairs are in the anagen phase for about 3 years, the catagen phase for a few days, and the telogen phase for about 3 months. As most hair follicles are in the anagen stage at any given time, anagen effluvium affects the majority of scalp hair.
Buy discount liv 52 on-line
At the completion of the amplification step medications 4 less canada buy discount liv 52, cells to be banked are cryopreserved until further processing for lineage commitment (see below). These protocols fit into three major categories (embryoid body formation, monolayer cultures and inductive co-cultures) (Mummery et al. Driving these progenitors further down towards a cardiomyogenic phenotype (defined by the expression of markers of the secondary and primary heart fields such as Isl-1, Tbx5, Nkx2. Although several small molecules have been reported to induce cardiac differentiation of pluripotent stem cells (reviewed in Liu et al. The transition between the activating and repressing effects of Wnt factors on cardiogenesis occurs within a very narrow time frame (Mignone et al. It is therefore important to develop similar approaches in monolayer cultures to achieve robust and scalable cardiomyocyte differentiation in well-defined growth-factor-free chemical media. In response to appropriate signals, this population was able to give rise to the three main lineages comprising heart tissue, i. This highlights the ambivalent role of pluripotency-associated transcription factors which, on the one hand, maintain pluripotency through their respective cross-inhibition but, on the other hand, also act as initiators of a given differentiation path (mesoderm in the case of Oct-4, endoderm in the case of Nanog, neuro-ectoderm in the case of Sox2). Overexpression of one of these factors disrupts this equilibrium and triggers the engagement of the cells down the ecto-, endo- or mesodermic differentiation pathway controlled by this specific factor while the others become down-regulated (Loh and Lim, 2011). As such, the degree of elasticity of the surface on which they are cultured can profoundly influence their fate. Not only the stiffness but also the microtopography or nanotopography of the culture surface may contribute to direct the cell differentiation (Kim et al. Other potentially effective approaches for facilitating cardiovascular progenitor cell differentiation include the bioengineering of three-dimensional microenvironments mimicking in vivo niches (Schenke-Layland et al. One important, and yet unsettled, issue is to determine whether it is more appropriate to transplant early mesodermal progenitors and to rely on local cardioinstructive signals of the host heart (Behfar et al. What some experimental studies have shown is that transplantation of fully mature cardiomyocytes is not more efficacious than that of cells still locked in a progenitor state (Smits et al. However these data still fail to accurately identify the optimal pre-transplantation level of differentiation of the progenitor cells. A purification phase is therefore mandatory to eliminate the non-responder cells that still demonstrate various degrees of pluripotency and as such carry the risk of uncontrolled proliferation. Several methods have been proposed either for inactivating residual pluripotent cells or for targeting their elimination during the differentiation process (reviewed in Hentze et al. Elimination of non cardiac-committed cells during the differentiation process can also be accomplished by genetic engineering if cells are transfected with an antibiotic-resistant gene driven by a cardiac promoter (typically, a neomycin-resistant gene under the control of the heavy myosin chain promoter) allowing, upon exposure to the antibiotic, killing of all but the cardiac-committed cells. More recently, an alternative non-genetic method based on distinct metabolic flows between cardiomyocytes and non-cardiomyocytes has also been reported to yield enriched populations of beating cells following exposure of human pluripotent stem cells to glucose-free conditions and lactate supplementation (Tohyama et al. However, in a clinical perspective, it seems more relevant to purify the target cell population on the basis of surface markers indicative of a cardiac commitment, of which several have been proposed (positive selection). This approach could likely be optimized by switching to a negative selection type of strategy using antibodies recognizing surface-expressed pluripotency markers like podocalyxin-like protein-1 (Choo et al. The use of large panels of surface markers should further help in defining a set of them ensuring adequate purification of the tissue-committed progenitor cell populations (Drukker et al. Because it is unlikely that a single technique can yield a 100% success rate, quality controls are critical for maximizing the safety of the procedure. In vitro, they primarily consist of checking the disappearance of pluripotency genes in the sorted cell population, which is usually done by quantitative real-time polymerase chain reaction. Additional preclinical in vivo studies are therefore mandatory to further characterize the teratoma-forming potential of the cell-based therapeutic. A common approach consists of injecting immunodeficient mice [subcutaneously in matrigel (Prokhorova et al. With the caveat that data collected in xenografted immunodeficient animals may not readily predict the tumorigenic risk in humans, these experiments still provide a benchmark for ensuring that a given batch of committed cells intended for clinical use is within the safety range, i. Biodistribution studies are therefore mandatory and, in this regard, bioluminescence is an appealing tool for monitoring cell fate over time (Su et al. The most straightforward one remains based on drugs like cyclosporine or tacrolimus. In the specific context of cellular transplantation, however, the use of these immunosuppressants raises several questions. What are the optimal dosages and is it possible to reduce them in light of (1) the depressed immune status of patients with heart failure (Calderon et al. If a new myocardial tissue is expected to be formed from the grafted cells, immunosuppression should theoretically be maintained lifelong to keep the graft viable; conversely, if cells are thought to only act paracrinally, immunosuppression can logically be given only during the period where these cells exert their secretory effects before their clearance from the host tissue, which is likely a matter of weeks, at most a few months. However, such a strategy remains fraught with serious issues like the haplotypic diversity in multiethnic societies (Fraga et al. However, the feasibility of setting such a bank has now been established in China (Lin et al. It is noteworthy that these actual population data are consistent with the previously obtained theoretical calculations (Taylor et al. However, an easier approach to implement clinically could be the induction of tolerance, which has now been achieved successfully in experimental cardiac transplantation (Bonde et al. It may therefore be more clinically relevant to target a peripheral-type of immune tolerance, which has been successfully accomplished by blockade of costimulatory molecules (Grinnemo et al. Nevertheless, although the current view is that allogeneic cells trigger an immune response that needs to be addressed, a recent study (Lauden et al. Whether this B7 family member could be used as a marker for selecting cells that are susceptible to deliver post-transplantation immunoregulatory signals is an intriguing possibility that is worth exploring. The difficulty of computing all these factors still makes such a patient-specific assumption hazardous. In our protocol, we have also selected an initially conservative dose (10 million progenitor cells). Hence, from the onset, this low initial cell retention rate inflicts a penalty to the procedure and weakens its potential efficacy. Furthermore, injection per se has several disadvantages, including poor control over cell distribution, the creation of multiple intramyocardial clusters which can cause arrhythmias (Fukushima et al. The resulting loss of cell-to-cell attachments and cell-to-matrix anchoring then sets the stage for an apoptotic-type of cell death (anoikis) (Zvibel et al. If cells are to be delivered during a cardiac surgical procedure, it makes sense to take advantage of direct control over the heart for shifting from injections to the epicardial delivery of a cell-loaded scaffold covering the infarct area to which it can be secured by the application of glue or a couple of stitches. Compared with injections, this strategy has been shown to dramatically increase early cell retention (Matsuura et al. The other technical factors to take into account are the thickness of the scaffold (which should not exceed 150 m) and its pore size, which need be optimized to allow an efficient diffusion of oxygen and nutrients within the construct while facilitating vascular infiltration and outward migration of the cells (or their derived products) towards the subepicardial layers of the heart; it is finally important that the construct be templated in a way that can promote an anisotropic bundled orientation of cardiomyocytes for enhancing function, facilitate neovascularization and reduce fibrotic reactions (Madden et al. Since there is a tissuespecific composition of extracellular matrices, those derived from the myocardium look the more appealing for heart repair (Syngelin et al. The mechanisms by which epicardially delivered scaffolds can improve postinfarct function remain elusive and might include (1) the release of cytoprotective biomolecules (Matsuura et al. Recently, decellularized ventricular extracellular matrices have also been processed in a way that enables their catheter-based delivery (Singelyn et al. In the future, it is conceivable that these tissue engineering-based techniques can be successfully combined with minimally invasive cell delivery strategies, as illustrated by the percutaneous approach to the pericardial space under fluoroscopy and intravascular ultrasound guidance (Ladage et al. Unfortunately, poor survival has been a consistent finding regardless of the cell type (Nguyen et al. Aside from the immune response to allogeneic cells, which has been discussed earlier, two factors play a major role in graft attrition: (1) ischemia due to the poor vascularization of the transplanted areas, and (2) loss of cell cohesiveness resulting from enzymatic dissociation that precedes conventional needle-based cell injections. To provide the graft with an appropriate blood supply, there are two main strategies, which are not mutually exclusive. The direct one relies on revascularization of the transplanted area whenever feasible, regardless of its modalities (angioplasty or coronary artery bypass grafting). As previously discussed, some degree of cell cohesion can be restored by incorporating cells into scaffolds which, by providing a three-dimensional template mimicking the native niche, improve cell survival compared with dissociated cells (Matsuura et al. Another benefit of scaffolds is that they can be functionalized with biomimetic peptidic motifs or control-released factors that increase patch vascularity (Miyagi et al. Regardless of the type of scaffold, the final goal is to attempt to create a microenvironment providing both mechanical support and 284 Cardiac regeneration and repair biochemical instructive cues facilitating cell adhesion, spreading and maturation (Dvir et al. In a further step, integration of gold nanowires within the scaffold has been shown to improve electrical communication between adjacent cardiac cells (Dvir et al. In brief, they rely on preconditioning, genetic manipulations or chemical treatments and share in common the objective of transplanting cells geared to better survive in an expectedly hostile environment and more effectively boost endogenous repair mechanisms (Mohsin et al. However, primarily for regulatory reasons, most of these strategies are unlikely to be applicable to patients and it is therefore important that the choice of biomimetic scaffolds or any other survival-targeted intervention takes into account key translational issues like manufacturability, scalability under Good Manufacturing Practice conditions, cost and regulatory approval with regard to safety, toxicology and biodistribution of potential degradation end products.
Order liv 52 mastercard
The second method is to use a molecular marker that is present in tumour cells but not in the adjacent tissue symptoms yeast infection women buy liv 52 with a visa. To identify a marker that has this specificity and is expressed in the majority of tumours is difficult. An advantage of haematoxylin/ eosin sections and immunohistochemistry is that the morphology of the cells can be examined and malignancy confirmed. The detection rate of micrometastases in axillary lymph nodes has been reported to range from 9% to 46%. From a literature review available at that time, the committee concluded that it was not possible to determine the significance of micrometastasis or isolated tumour cells. They noted that approximately 18% of cases are associated with other nodal (non-sentinel node) metastases. However, at present it is recommended that an intensive work-up is not justified on a population level. The committee did suggest multilevel assessment and, where resources permit, intraoperative assessment, although the results of Z0011 (see Chapter 7) suggest that some node-positive patients may not require axillary dissection and this brings the whole issue of intraoperative assessment into question. Tumour size Tumour size is one of the most powerful predictors of prognostic factor in breast cancer. It is well known that the association between increasing tumour size and increasing number of positive lymph nodes and worse outcome is highly statistically significant. Patients with smaller tumours have a better long-term survival than those with larger tumours. Estimation of tumour size has assumed particular importance since the introduction of population screening. This indicates that <15 mm may be a more realistic watershed in defining small, invasive, carcinomas of good prognosis. It is clear that pathological tumour size is a valuable prognostic factor and it has become an important quality assurance measure for breast screening. Differentiation Modern pathologists have recognised that invasive carcinomas can be divided according to their degree of differentiation. There are two ways to achieve this: (i) by allocating a histological type according to the architectural pattern of the tumour; (ii) by assigning a grade of differentiation based on semiquantitative evaluation of structural characteristics. Undoubtedly, assessment of histological type provides prognostic information in breast cancer. However, this effect is relatively small in multivariate analysis27 when compared with the prognostic value of histological grade; histological type may prove to be more useful in increasing our understanding of the biology of breast cancers. In brief, assessment of grade considers three tumour characteristics: tubule formation, nuclear pleomorphism and mitotic counts. There is a highly significant correlation between tumour grade with long-term prognosis. It has now been shown conclusively that the Nottingham method, with its more objective criteria, has excellent reproducibility when used by experienced pathologists. Tumour grade the Nottingham method (Elston and Ellis) is a modification and improvement of previously existing morphological grading systems and is able to provide greater objectivity of grade. The authors were able to demonstrate differences in survival between different individual grades (1, 2 and 3). Lymphatic and vascular invasion is considered to be a valuable surrogate for lymph node stage in cases where nodes have not been removed for examination. There were significant associations between histological grade and other clinicopathological variables of poor prognosis such as larger tumour size, positive lymph node status, vascular invasion, oestrogen receptor and androgen receptor negativity, and p53 positivity. Molecular/predictive factors Despite the overall association between molecular markers with prognosis and outcome, they are limited in their ability to capture the nuances of the complex cascade of events that drive the clinical behaviour of breast cancer. Morphological factors are unable to predict response to systemic treatments, and tumours of apparently homogeneous morphological characteristics still vary in response to therapy and have distinct outcomes. The use of strategies ranging from hormone therapy to chemotherapy and recently to novel receptor-directed therapies and vaccines relies on the expression of predictive factors by the cancer, either individually Several studies have now shown that the presence of vascular invasion correlates closely with local and regional lymph node involvement. Reproducibility is the limiting factor in its widespread adoption and routine clinical assessment. In a Nottingham study of assessing vascular invasion, the issue of reproducibility was addressed specifically. There was a 77% overall inter-observer agreement on histological features and an 85. These molecular markers are used not only to guide treatments but are also being used to monitor response and detect relapse. The Allred score categorises the percentage of cells (scored from 0 to 5) with the intensity (scored from 0 to 3) and adds these two scores to give a numerical score from 0 to 8. It is important to appreciate that all methods are subjective and, at best, semiquantitative. As these assays have become simpler, and less costly, they are now available for all patients. Progress still needs to be made in standardisation of assay technique, objectivity and reproducibility. Oestrogen and progesterone are considered to diffuse into cells, or be transported to the nucleus. The first two members of this family have been studied extensively in breast cancer. The second relies on the recognition of the receptor protein by specific antibodies. Several studies examined the correlation between assay and outcome/response and studies 26 (021)66485438 66485457 Protein levels can be quantified by Western analysis or enzyme immunoassay; however, architecture of tissue is lost in these procedures and there may be contamination by normal tissue cells or ductal carcinoma in situ. The lack of a clear picture has been attributed to several factors: lack of a standard assay (monoclonal vs. Findings from this review demonstrated a great heterogeneity of study design, levels of cut-offs for positive and negative, and, not surprisingly, differences in its prognostic value in these various studies. The predictive value of this marker for hormone resistance or responsiveness is better defined. Guidelines stress the need for stringent, reproducible and consistent criteria for testing. In studies employing various commercially available antibodies, a wide variety of sensitivity and specificity in fixed paraffin-embedded tissues is seen. Prognostic significance and association with other prognostic factors the seminal work by Slamon et al. Since then most large studies have confirmed this relationship in multivariate analysis. Several studies have also shown a reduction in response rates to hormonal therapy. However, tamoxifen was not randomised within this trial and all patients received one of three regimens of doxorubicin. The recognition of basal phenotype in these triple-negative cancers is of growing importance, with several lines of evidence supporting the view that triple-negative tumours and basal phenotype are not interchangeable but rather distinct entities. This relapse pattern has been recognised for all types of triple-negative cancers for which sufficient data exist, although the absolute relapse and survival rates differ across subtypes. Identification of histological features that could indicate a genetic predisposition would be useful in providing an insight into the function of these genes and may aid in identifying those in whom screening for genetic mutations would be useful. The genetic fingerprint provides information on normal cellular processes and morphological/phenotypic expression. When this message is altered, it forms the nidus for the development and progression of cancer. These mutations are often due to base substitutions that may directly cause a stop codon. As a result the gene is only partly transcribed and any functional protein production terminated. In solid tumours virtually all chromosomal rearrangements are unbalanced, the net result being loss or gain in certain parts of the chromosome.
Discount liv 52 100 ml visa
Therefore medicine lock box buy liv 52 120ml with mastercard, therapy is much more prolonged (48 versus 24 weeks) for genotype 1 than for 2 and 3. Although not as rapid as direct examination, it is more sensitive and much more specific. For the majority of human pathogens, culture requires only 1 to 2 days of incubation. By growing the organism, it is available for further phenotypic and genotypic analysis, such as antimicrobial susceptibility testing, serotyping, virulence factor detection, and molecular epidemiology studies. Environmental and nutritional aspect of bacterial and fungal culture Certain basic strategies are used to recover bacterial and fungal pathogens. Most bacterial and fungal cultures are performed, at least initially, at this temperature. Certain skin pathogens, such as dermato- A Primer on the Laboratory Diagnosis of Infectious Diseases 17 phytes and some Mycobacterium spp. These incubation temperatures may be used when attempting to recover a specific organism from specimens with a resident microbiota, such as feces, as few organisms other than the target organism can grow at these temperature extremes. Another important characteristic of human bacterial and fungal pathogens is the impact of the presence of oxygen on the growth of these organisms. Microbes can be divided into three major groups based on their ability to grow in the presence of oxygen. The majority of bacteria that make up the resident microbiota of the gastrointestinal and female genital tracts are anaerobic organisms. Besides temperature and oxygen, nutrients are an important third factor in the growth of microbes. They require an energy and carbon source, such as glucose; a nitrogen source, which may be ammonium salts or amino acids; and trace amounts of salts and minerals, especially iron. Some human pathogens have much more complex growth requirements, needing certain vitamins or less well-defined nutrients such as animal serum. Organisms with highly complex growth requirements are often referred to as being fastidious. A fastidious bacterium that is frequently encountered clinically is Haemophilus influenzae. Media the selection of media to be used in isolation of pathogens from clinical specimens is dependent on several factors. For example, fastidious organisms require a medium that is enriched with specific nutrients, such as animal blood, serum, or other growth factors. If the clinical specimen is obtained from a site that has a resident microbiota, certain strategies will be necessary to isolate a specific pathogen from the accompanying resident microbiota. Often in this setting, a special type of medium called selective medium is used to recover these pathogens. This is done by adding substances, such as dyes, antibiotics, or bile salts, that inhibit the growth of one group of organisms while permitting the growth of another. For example, MacConkey agar is a selective medium that contains bile salts and the dye crystal violet. These two substances are inhibitory for Grampositive organisms as well as some Gram-negative ones. MacConkey agar is an 18 A Primer on the Laboratory Diagnosis of Infectious Diseases example of a selective and differential medium. Organisms that ferment lactose are called lactose positive, and organisms that are unable to ferment lactose are called lactose negative. If Gram-negative bacilli are a component of this microbiota, than a selective-differential medium might be used as well. Certain organisms will not grow on media commonly used to culture clinical specimens, because the media may not be enriched enough or may contain inhibitory substances. When these organisms are sought, the laboratory must be notified so that special isolation medium can be used. Organism identification and susceptibility testing Once organisms are isolated, they may be identified, and in some cases susceptibility testing needs to be performed. The appearance of these colonies is often useful in determining the identity of the organism. Colonies may appear flat or raised, smooth or rough; may pit the agar; or may hemolyze red blood cells in blood-containing agar. Skilled microbiologists often have a very good idea of the identification of a microorganism based solely on its colonial appearance. In specimens that come from an area of the body with a resident microbiota, it is important to separate the colonies of organisms that may represent the resident microbiota from the colonies of organisms that may be pathogens. In patients with suspected bacterial pneumonia, a sputum specimen may be obtained. Sputum consists of secretions coughed up from the lower airways that are expectorated through the oropharynx and submitted for culture. Because they pass through the oropharynx, sputum specimens almost always contain viridans group streptococci. The appearance of colonies produced by viridans group streptococci is very similar to that produced by A Primer on the Laboratory Diagnosis of Infectious Diseases 19 S. Bacteria are typically identified on the basis of colonial morphology, Gram stain reaction, the primary isolation media on which the organism is growing, and biochemical and serologic tests of various degrees of complexity. Yeasts are identified in much the same way that bacteria are, while molds are generally identified on the basis of the arrangement of microscopic reproductive structures called conidia. First, a patient with a "strep throat" has group A streptococci recovered from his throat. Although the organism is clearly playing a role in the illness of this patient, antimicrobial susceptibility testing is not warranted. This organism is uniformly susceptible to first-line therapy-penicillin-and is susceptible more than 98% of the time to second-line therapy-the macrolide antibiotics such as erythromycin-although recent reports suggest that erythromycin resistance is becoming more frequent in this organism. Susceptibility testing is indicated because some strains are resistant to the first-line drugs used to treat this infection-semisynthetic penicillins, including oxacillin and dicloxacillin- and the second-line drug, clindamycin. In this situation, the patient may be started on empiric antimicrobial therapy until the susceptibility of the organism is known. If the organism is resistant to the agent used for empiric therapy, then the patient should be treated with an alternative antimicrobial agent to which the organism is susceptible. However, no susceptibility testing is done by the laboratory, and this practice is acceptable to the clinician caring for the patient. If the laboratory had performed the susceptibility testing without considering that this isolate was a potential contaminant, they would be validating that the isolate was clinically significant. In this setting, the laboratory should only do susceptibility testing if instructed to by the caregiver, who is in a better position to know if this organism is clinically important. All the approaches are highly standardized to ensure that the susceptibility results will be consistent from laboratory to laboratory. Screening of selected organisms for resistance to specific antimicrobial agents is one strategy that is frequently used, especially with the emergence of resistance in three organisms: S. The E-test is a plastic strip that contains a gradient of a specific antimicrobial agent. Because of their slow growth, special susceptibility testing techniques are used for the mycobacteria. Rather, they can only grow by parasitizing living animal cells (including human cells) that are maintained by continuous tissue culture. Animals such as mice, or chicken eggs, can be inoculated in an attempt to isolate certain viruses, but this approach is rarely done. Tissue culture for Chlamydia may still be attempted, especially in situations where the detection of C. Tissue culture is still an important technique for the detection of viruses in many laboratories, though laboratories are converting to molecular methods for viral detection at an increasing rate. Herpes simplex virus can be isolated from skin and genital tract lesions, often within the first 24 hours of incubation.
Myrobroma fragrans (Vanilla). Liv 52.
- What is Vanilla?
- How does Vanilla work?
- Dosing considerations for Vanilla.
- Fever, intestinal gas, and other uses.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96239
Order liv 52 cheap online
An ameba symptoms 8 weeks order 100ml liv 52, Naegleria fowleri, causes a rare and frequently fatal form of meningoencephalitis. In the United States, a number of infants who have had contact with the feces of raccoons have acquired a parasitic infection due to the raccoon roundworm, Baylisascaris procyonis. Another parasitic infection associated with eosinophilic meningitis is Angiostrongylus cantonensis, which is obtained by the ingestion of uncooked snails or slugs that are infected with this organism or by the ingestion of raw vegetables, such as in salads, that have been contaminated by infected snails or slugs. Brain abscesses occur through direct extension from a contiguous site such as an infected paranasal sinus, following head trauma, or by hematogenous spread from another infected site. Typically, patients with abscesses due to hematogenous spread have either endocarditis or a lung abscess. Septic emboli, which are small blood clots containing infectious agents, are released from the primary infection site and enter the bloodstream. The emboli lodge in capillaries in the brain, causing localized hemorrhage and producing sites for the initiation of infection which evolve into brain abscesses. The organisms most frequently causing brain abscess in immunocompetent individuals are S. In diabetic patients (especially those with ketoacidosis), rhinocerebral zygomycosis due to Mucor, Rhizopus, and other fungi within the Zygomycetes can extend from the sinuses into the brain, causing extensive necrosis. For vector-borne infections, the geographic locations at which infected arthropod vectors occur will determine where these diseases are likely to be acquired. It is worth noting that though patients may not have traveled to a region in which a particular pathogen is endemic, the pathogen, in effect, may have traveled to them. For example, there have been rare cases of malarial infections in people who were infected by mosquitoes that were imported into a malaria-free area from a malariaendemic area, such as people who acquire malaria near an international airport. While measles is efficiently transmitted from person to person by the respiratory route, the geographic range of endemicity of this disease does not include developed countries, as a result of the widespread use of the available live, attenuated vaccine. In regions of the world in which the populace has a low rate of immunization, measles in children may be common and have a mortality rate that ranges from 5 to 25%, most often due to secondary infections. This infectious complication is more common in boys than girls and is more likely to occur in children who were infected with measles when they were younger than 2 years of age. The refusal of parents to immunize their children against measles will increase disease prevalence and the likelihood of developing this rare but fatal neurologic complication. Clostridium botulinum Branching, Gram-positive bacilli, usually anaerobic Spore-forming, Grampositive bacillus Enteric Gram-negative bacilli Toxin-producing, anaerobic, Gram-positive bacillus Catalase-positive, Grampositive cocci Lactose-fermenting, Gram-negative bacillus Catalase-negative, Grampositive cocci Individuals with aspiration pneumonia Individuals with severe anthrax infection; victims of bioterrorism Neonates Brain abscess Meningitis Meningoencephalitis with abscess Infants; adults who ingest botulinum toxin; Botulism, flaccid paralysis wound botulism occurs but is not common; toxin is a potential bioterrorism agent Individuals with foreign bodies, Brain abscess Oral streptococci (Streptococcus sanguis, Streptococcus mutans, etc. Pseudomonas aeruginosa Staphylococcus aureus Streptococcus pneumoniae Fungi Aspergillus spp. The patient presented to the emergency department with altered consciousness, confusion, and agitation. On physical examination his vital signs were normal but he was confused and agitated, making a neurologic examination not possible. Over the past 2 decades, how has antimicrobial resistance changed in this organism Disseminated infections with this organism are becoming infrequent in the United States, especially in the very young and very old. What impact does this observation have on patients such as the one seen in this case Invasive infections with this organism are very common in a selected subpopulation of African-Americans. However, his history of cirrhosis of the liver, alcoholism, and diabetes put the patient at increased risk for infection. Given his presentation of altered mental status, confusion, and agitation, some type of central nervous system infection should be considered. Encephalitis is most commonly caused by viruses, with herpes simplex virus and the arboviruses being the most common. Over the years, far too many medical students have told me it is because the "bacteria use it up. In a 45-year-old patient with bacterial meningitis, the possible organisms are very limited. In patients in this age range, more than half of the cases will be due to Streptococcus pneumoniae. The Gram stain picture of Gram-positive diplococci is consistent with that organism. Without the Gram stain findings, though, Neisseria meningitidis would also need to be considered. The Gram stain findings were such that three other much less frequently encountered organisms would need to be considered and appropriate antimicrobial therapy given. Listeria monocytogenes is a Gram-positive coccobacillus and certainly might be appear like the organism on this Gram stain. Group B streptococcus (Streptococcus agalactiae) is a much more common cause of meningitis in neonates. Group A streptococcus (Streptococcus pyogenes) may also cause meningitis but is even less common. Finally, for completeness, Streptocococcus suis has been associated with adults with meningitis. This patient did not appear to be at risk for infection with this organism as it is seen primarily in people who are in close contact with hogs. There are >90 different capsular types, with 13 of those types being responsible for approximately 80 to 95% of invasive infection. Second, the surface charge of these encapsulated bacteria is such that they are not entrapped in mucus and thus are not cleared efficiently by ciliary action. It can bind to the Fc portion of IgG and activate complement, depleting it from the bloodstream; it inhibits ciliary beating, further impairing ciliary clearance; and it binds and damages type 2 pneumocytes, facilitating entry of the organism into the bloodstream in the alveolar space. If the organism is not cleared by the spleen and liver, key organs in the clearance of bacteria from the bloodstream, it can be carried to the central nervous system, where it can adhere to endothelial cells and be translocated across the blood-brain barrier. Once in the central nervous system, the organisms release a variety of bacterial products, such as cell wall lipoteichoic acid and peptidoglycan, which elicit a strong cytokine-mediated inflammatory response that is responsible of much of the tissue damage characteristic of this infection. In normal individuals, this is a rare event, because innate and adaptive immunity will kill the organism long before it reaches the meninges. Three factors are important in allowing this to occur and put this patient at increased risk for invasive disease with pneumococci: alcohol abuse, diabetes, and cirrhosis of the liver. The strongest association of these three risk factors with invasive pneumococcal infection is alcohol abuse. First, alcohol causes a decreased cough reflex, which allows this common member of the upper airway microbiota access to the bronchial and alveolar spaces. When organisms get to the alveolar space, they are more likely to survive because there is impairment in neutrophil recruitment and function. Additionally, the antimicrobial proteins lysozyme and lactoferrin have been shown to have impaired killing of pneumococcus in bronchoalvelolar lavage fluid of alcoholic patients. The problem of alcohol abuse was further magnified by the presence of diabetes in this patient. This results in impairment of neutrophil adherence, chemotaxis, phagocytosis, and bacterial killing. Finally, patients with cirrhosis of the liver have decreased complement levels because hepatic cells are a key source of complement in the body. Because complement plays a key proinflammatory role in response to infection, the lowering of complement levels results in poorer opsonophagocytic response and clearance of this organism. These two drugs were tested because they are the two most commonly used and effective agents for treatment of pneumococcal meningitis. A gradient of increasing concentration of antimicrobial is bound to the strips and when it comes in contact with the agar surface is released and "diffuses" into the agar. Because the organism was causing a central nervous system infection, the criteria for determining whether the organism is resistant to these antimicrobials are different than if it was causing pneumonia. Antimicrobials cross the blood-brain barrier at only a fraction of the level at which they will be found in the bloodstream. Starting in the late 1970s reports of penicillin G-resistant strains started to emerge. Two factors are important, one due to human activity and the other to the evolutionary power of microbial populations. By the mid-1980s, there was recognition that large amounts of antimicrobial agents were being used inappropriately to treat viral infections. What was not recognized was that this inappropriate use of antimicrobials was resulting in the emergence of commensal organisms in the microbiota that were resistant not only to penicillin G but also to many other oral antimicrobials that were also often misused, including erythromycin and trimethoprim-sulfamethoxazole. Pneumococcal strains that are resistant to all commonly used oral antimicrobials are frequently seen in children, especially in those who attend group child care, a setting in which spread and high carriage rates of drug-resistant pneumococci are common.
Syndromes
- People living with someone who has chronic health problems
- Chlorpromazine
- Medication -- ask the doctor about adjusting the dosage, changing medications, or stopping them
- 4 - 8 years: 1.0 mg/day
- Acetaminophen (Tylenol) for mild pain. Avoid drugs such as aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve, Naprosyn) which can make your symptoms worse.
- Name of the product (as well as the ingredients and strength, if known)
- Acne or minor skin infections
- Chronic renal failure
Order 200 ml liv 52 overnight delivery
The basic objective of cell therapy in heart failure is the replacement of dead cardiomyocytes by a pool of cells able to integrate electromechanically into the host myocardium and so contribute to improve its contractile function medications covered by medicaid buy cheap liv 52 100ml on-line. However, there is now compelling evidence that cells which have been tested so far, experimentally and clinically, fail to adopt a cardiomyocytic phenotype and that their putative benefits are primarily ascribed to the cardioprotective effects of the biomolecules they secrete. The experimental results obtained in animal models of myocardial infarction and summarized in this paper support the soundness of this hypothesis. The second section of the chapter describes the main translational issues that need to be addressed before the safe and efficacious clinical use of these cells. Although heart transplantation remains the only radical treatment, organ shortage still limits its widespread use. Numerous alternative options are then available, but none of them can cover the needs of the whole heart failure patient population. Hence, mechanical support under the form of destination therapy has made substantial improvements that translate into better outcomes of patients who are not eligible for transplantation (Slaughter et al. The early results of gene therapy targeting calcium handling have been encouraging but need to be confirmed (Jessup et al. Finally, despite tremendous efforts, none of the drugs trials that have been tested over the past 10 years has been successful. The recognition of a persisting gap between the number of patients with heart failure and those who could benefit from the above-mentioned therapies has led to conceptualize a novel approach based on regeneration of injured non-functional myocardium. Several chapters of this book address the various cell types that have been tested clinically to achieve this objective in the specific context of heart failure (which should be clearly distinguished from that of acute myocardial infarction or refractory angina). Of note, the positive outcomes (reduction in infarct mass) recently reported with the cardiosphere-derived cardiac cells, expanded from an endomyocardial biopsy before being re-injected intracoronarily (Makkar et al. This paracrine hypothesis has primarily stemmed from the consistent experimental observation of a sharp discrepancy between the very limited rate of persistent cell engraftment and the functional benefits of the transplantation procedure, thereby suggesting that instead of differentiating into new donor-derived cardiomyocytes, the grafted cells rather behave as biofactories, releasing a wide array of cytokines and growth factors acting on host signaling pathways. Among these pathways, angiogenesis seems to play a pivotal role but other mechanisms might also be involved such as remodeling of the extracellular matrix limiting fibrosis, reduction of apoptosis and, more hypothetically, recruitment of endogenous cardiac stem cells (Mirotsou et al. It has been shown that virtually all cells that have been tested experimentally and clinically have the ability to release these various factors (and the same factor is often secreted by several different cell types) (Mirotsou et al. However, as mentioned above, most of the clinical studies that have used cells known to feature predominantly paracrine properties have failed to yield clinically meaningful improvements. This raises the question of whether these effects are robust enough to be functionally relevant in the context of extensive areas of scarred myocardium. A negative answer to this question leads to assign an alternate, and much more challenging, role to the grafted cells, i. The other strategy that has been tested relies on the use of the so-called cardiac stem cells, the existence of which has been reported in several experimental studies (Bollini et al. However, this trial raises some methodological issues (particularly the low percentage of cells expressing markers of the myocyte, endothelial and smooth muscle cell lineages and the lack of functional comparisons between groups), which will hopefully be addressed in a future trial involving a larger number of patients. Hence, taken together, the data presented in these two papers do not allow us to conclusively establish that the benefits of the injected cells were really due to a true myocardial regeneration process and not to some paracrine effects. Indeed, the major issue associated with these cardiac stem cells is that it remains uncertain that they really persist in the human diseased heart. Our previous failure to identify such cells in myocardial biopsies taken during coronary artery bypass operations (Pouly et al. Put together, these findings suggest that although we are likely born with a pool of cardiac progenitor/ stem cells, this reservoir may become exhausted over time, an assumption supported by the experimental observation that the capacity of the mouse heart to regenerate its apex following amputation is operational shortly after birth but is lost as early as 1 week later (Porrello et al. Because the results of these rodent studies are confounded by several factors, particularly the xenogeneic setting of transplantation and the much higher heart rate of rodents compared with humans (high-rate sustained pacing is a common method for inducing heart failure in large mammals and may therefore severely compromise integration and viability of the grafted cells), we attempted to create a more clinically relevant model of non-human primate allogeneic transplantation. To this end, a closed-chest reperfused infarction model was first created in Rhesus monkeys. Two weeks after infarction, the cardiac progenitor cells were delivered by an open-chest approach (by intramyocardial injections or epicardial transfer). Two and three months later, the cardiac differentiation of the grafted progenitors was evidenced by the finding of clusters of green cells featuring a sarcomeric organization and connexin 43 expression and repopulating a large proportion of the infarct area (up to 20%). No teratoma was observed as long as the cell preparation had been purified before transplantation (Blin et al. In a similar attempt to overcome the issue raised by the rapid heart rates of mice and rats, Shiba et al. This hypothesis is supported by the ability of human cardiomyocyte progenitor cells to repair infarcted mouse myocardium without undergoing differentiation into cardiomyocytes (den Haan et al. Induced pluripotent stem cells represent an alternative variety of pluripotent cells once somatic cells (usually fibroblasts) have been reprogrammed back to an 272 Cardiac regeneration and repair embryonic-like state, from which they can be redifferentiated toward a cardiac lineage (Gai et al. In rat models, these bioengineered cells have been shown to repair myocardial infarction (Nelson et al. However, the numerous issues associated with these cells [choice of the most efficient and safest reprogramming protocol, risk of genetic and epigenetic abnormalities that may result in oncogenesis (Pera, 2011), potential for a reprogramming-induced upregulation of genes identified as self-foreign and consequently triggering rejection (Zhao et al. Importantly, both the growth kinetics and cardiomyogenic differentiation potential vary from one line to the other (Osafune et al. These parameters have to be taken into account before finalizing the choice of the line for a targeted clinical application. Another critical factor pertains to the ethical and technical conditions under which the line has been initially derived from the blastocyst. Only the most recent lines have been derived under Good Manufacturing Practice conditions but this does not necessarily preclude the use of older lines if they can be microbiologically secured and have a full sourcing and traceability record. Typically, this proliferation step is supported by mitotically inactivated feeder cells. Cultures need to be carefully inspected daily to look for the morphology of the colonies and their timely passaging when they approach confluence. Maintenance of pluripotency is regularly checked during this period by enzymatic (alkaline phosphatase) activity assay, immunostaining or real-time polymerase chain reaction (best suited for high-throughput analysis) assessing the relevant markers (such as Oct4, Nanog, Sox2, Lefty). The ability of cells to differentiate into progeny of the three germ layers in vitro and to generate teratomas in vivo is an additional common criterion for ensuring that they have remained pluripotent. Qualification of the cell bank for human use also requires extensive microbiological testing to validate the absence of pathogens that might have contaminated the cells upon their exposure to human, murine, bovine or porcine source materials. Because repeat passages [and the manner in which cells are passaged (Hentze et al. As there is not yet a consensus about the nature of the tests to be performed, we have used a rather wide combinatorial screening involving the assessment of karyotype, fluorescence in situ hybridization targeted at the chromosomes known to be at higher risk of instability and microarrays looking for genomic microrearrangements (with a particular check that cells expressed gene polymorphisms commonly found in humans, without deletion of a tumor-repressing fragment or addition of a tumor-promoting one). Finally, a meaningful assessment of these retention-enhancing and survivalenhancing strategies requires the use of tracking methods allowing the monitoring of cell fate after transplantation. Gene reporter imaging is a reliable, clinically applicable method provided the encoded gene does not adversely interfere with the differentiation/function of the engineered cells or cause a damaging immune response (Yaghoubi et al. However, safety will be eagerly scrutinized and it is clear that the occurrence of serious adverse events would have devastating consequences on the whole field. This is logical because understanding heart development and deciphering the mechanisms of action of pluripotent cells and their differentiated derivatives are mandatory to generate basic data that can then influence clinically relevant translational programs. Such a commitment, however, remains uncertain for several reasons, which include a potential reluctance of companies to work in an ethically challenging area, the geographical inhomogeneities in legislation, the difficulties in raising funds when the return on investment is still, at best, distant and the potential difficulties in securing robust intellectual property. It is likely that the first patients to benefit from this novel approach will be those who have to undergo an associated cardiac surgical procedure, although direct intramyocardial or epicardial cell/tissue transplantation is also conceivable as a stand-alone surgical procedure if it can be implemented in a minimally invasive fashion. The translation to a catheter-based approach, which would be critical to broaden the indications of the technique, will be more challenging but is not insurmountable because injectability of engineered cell products. Comparative studies of the secretomes (completed by in vivo functional experiments) should then identify the cells that release the most cardioprotective factors. At the end, if the most relevant factors could be accurately identified and characterized, one may even consider a shift in the paradigm from cell-based to protein-based or exosome-based therapy. However, the clinical applicability of this approach still remains fraught with several roadblocks primarily related to optimization of cell purification, control of immune responses, efficient transfer of cells and enhancement of their survival.
Buy 120ml liv 52 with visa
The adult bone marrow provides a broad variety of hematological progenitors in various stages of lineage commitment medications in checked baggage cheap liv 52 60ml with visa. The initial work by Till and McCulloch provided broad evidence for a clonogenic population that self-renewed, gave rise to blood cells in vitro and repopulated the bone marrow of irradiated mice (Becker et al. However, positive results have not been consistently observed, with some studies showing no benefit (Lunde et al. However, recent studies have challenged the concept that these markers can identify true endothelial cell progenitors, furthering the notion that distinct subtypes exist within previously characterized populations (Case et al. Further culture of mononuclear cells for several weeks promotes a phenotypic change with the appearance of highly proliferative clusters of cells that take on a cobblestone morphology and exhibit a very strong endothelial cell phenotype with the loss of leukocyte markers and the expression of all typical endothelial antigens (Hur et al. Interestingly, the superiority of one cell type over the other has long been a matter of speculation with as yet no head to head study of myocardial repair. This profound impairment is likely an important determinant of the rather modest nature of benefits seen in clinical trials using autologous cell therapy for post-infarct patients compared with the much more robust effects that can be demonstrated in preclinical models using cells from young, healthy animals. To circumvent this limitation, a number of advances in cell culture have been tried including the use of artificial scaffolds, genetic modification and preconditioning to enhance cell survival and activity. Early non-randomized trials demonstrated that these cells improved ejection fraction and myocardial perfusion while decreasing infarct size and adverse remodeling (Assmus et al. Although this product was well tolerated, improved cardiac function was seen only in the patients with anterior acute myocardial infarction. However, despite reduced infarct size after treatment with either cell product, neither therapy demonstrated a significant improvement in ejection fraction in this small open label trial. This may in part be attributed to a degree of adverse cardiac remodeling in this population recruited an average of 11 years since their last myocardial infarction. Observations from these studies prompted the deployment of improved candidate cell selection and culture- guided techniques to improve cell products. Ultimately, this final analysis will have important implications for the development of a practical preclinical treatment reflecting the importance of appropriate product delivery into a receptive host. In the case of both cell products, preclinical testing has formed the platform for early clinical trials. In the case of skeletal myoblasts, concerns regarding product safety with limited early evidence for clinical benefit have diminished the enthusiasm for second-generation cell products in the face of attractive more cardiogenic competitors (Bolli et al. In contrast, hematological cell products have steadily proceeded through the product development with enhanced durability and efficacy. These studies will inform directly upon the direction and necessity for future third-generation or personalized pluripotent cell therapies that loom on the very distant horizon. Adult bone marrow-derived cells for cardiac repair: a systematic review and meta-analysis. Assessment of the tissue distribution of transplanted human endothelial progenitor cells by radioactive labeling. Long-term (1 year) functional and histological results of autologous skeletal muscle cells transplantation in rat. Cytological demonstration of the clonal nature of spleen colonies derived from transplanted mouse marrow cells. Transplantation of allogeneic peripheral blood stem cells mobilized by recombinant human granulocyte colony-stimulating factor. Intermediate-term hematopoietic stem cells with extended but time-limited reconstitution potential. Skeletal myoblast transplantation through a catheter-based coronary sinus approach: an effective means of improving function of infarcted myocardium. Myocardial substitution with a stimulated skeletal muscle: first successful clinical case. Endoventricular porcine autologous myoblast transplantation can be successfully achieved with minor mechanical cell damage. Feasibility and safety of autologous myoblast transplantation in patients with ischemic cardiomyopathy. Hematopoietic cells from bone marrow have the potential to differentiate into cardiomyocytes in vitro. An in vitro analysis of myocardial potential indicates that phenotypic plasticity is an innate property of early embryonic tissue. Cardioprotective c-kit+ cells are from the bone marrow and regulate the myocardial balance of angiogenic cytokines. Autologous myoblast transplantation after myocardial infarction increases the inducibility of ventricular arrhythmias. Cardiac cell therapy: overexpression of connexin43 in skeletal myoblasts and prevention of ventricular arrhythmias. Skeletal myoblasts overexpressing relaxin improve differentiation and communication of primary murine cardiomyocyte cell cultures. Autologous skeletal myoblast transplantation in patients with nonacute myocardial infarction: 1-year follow-up. Granulocytemacrophage colony-stimulating factor to harvest circulating haemopoietic stem cells for autotransplantation. Diverse origin and function of cells with endothelial phenotype obtained from adult human blood. Viability and differentiation of autologous skeletal myoblast grafts in ischaemic cardiomyopathy. Angiomyogenesis for cardiac repair using human myoblasts as carriers of human vascular endothelial growth factor. A randomized, double-blind, placebo-controlled, dose-escalation study of intravenous adult human mesenchymal stem cells (prochymal) after acute myocardial infarction. Autologous skeletal myoblast transplantation improved hemodynamics and left ventricular function in chronic heart failure dogs. Profoundly reduced neovascularization capacity of bone marrow mononuclear cells derived from patients with chronic ischemic heart disease. Autologous intramyocardial injection of cultured skeletal muscle-derived stem cells in patients with non-acute myocardial infarction. Effects of intracoronary injection of mononuclear bone marrow cells on left ventricular function, arrhythmia risk profile, and restenosis after thrombolytic therapy of acute myocardial infarction. Characterization of two types of endothelial progenitor cells and their different contributions to neovasculogenesis. Adult bone marrow cell therapy improves survival and induces long-term improvement in cardiac parameters: a systematic review and meta-analysis. Randomized controlled trials on the therapeutic effects of adult progenitor cells for myocardial infarction: metaanalysis. Transplantation of ex vivo expanded endothelial progenitor cells for therapeutic neovascularization. Intramyocardial transplantation of autologous endothelial progenitor cells for therapeutic neovascularization of myocardial ischemia. Prospective isolation and molecular characterization of hematopoietic stem cells with durable selfrenewal potential. Skeletal myoblasts transplanted in the ischemic myocardium enhance in situ oxygenation and recovery of contractile function. Neovascularization of ischemic myocardium by human bone-marrow-derived angioblasts prevents cardiomyocyte apoptosis, reduces remodeling and improves cardiac function. Growth factors improve the in vivo migration of human skeletal myoblasts by modulating their endogenous proteolytic activity. Deterministic regulation of hematopoietic stem cell self-renewal and differentiation. Transplanted cord blood-derived endothelial precursor cells augment postnatal neovascularization. Phenotype and hematopoietic potential of side population cells throughout embryonic development. Endothelial cells promote cardiac myocyte survival and spatial reorganization: implications for cardiac regeneration. Bone marrowderived hematopoietic cells generate cardiomyocytes at a low frequency through cell fusion, but not transdifferentiation. Autologous skeletal myoblasts transplanted to ischemia-damaged myocardium in humans. Cytokines derived from cultured skeletal muscle cells after mechanical strain promote neutrophil chemotaxis in vitro. A doubleblind, randomized, controlled, multicenter study to assess the safety and cardiovascular effects of skeletal myoblast implantation by catheter delivery in patients with chronic heart failure after myocardial infarction.
Buy liv 52 60ml free shipping
Signs and symptoms include microcephaly medications before surgery 200 ml liv 52 free shipping, chorioretinitis, pneumonia, hepatitis, and rash (petechiae). Other opportunistic infections in cardiac transplant recipients include those caused by pathogens common in patients with impaired cell-mediated immunity. These infections include toxoplasmosis, Pneumocystis jirovecii pneumonia, varicella-zoster, cryptococcal pneumonia or meningitis, Listeria monocytogenes bacteremia or meningitis, Nocardia spp. As was seen with this case, cytopathologic examination of infected tissue often reveals the diagnosis. For shell vial cultures, fibroblast cells are grown as monolayers on a glass coverslip in a shell vial. The higher the number of infected cells, the more likely the patient will have clinical disease, though detection of a low number of infected cells in an asymptomatic patient may indicate a patient in the early stages of active infection. There are currently no guidelines detailing the level of viremia that should trigger therapeutic intervention, but data in the literature suggest it is ~2,000 copies/ml. In theory, primarily "free," and therefore actively replicating, virus would be present in plasma, as opposed to the cell-associated virus present latently in peripheral white cells. This theory is, of course, not absolute, so the need for clinically relevant viral thresholds for therapeutic decisions is critical. The rationale for preemptive therapy is that it is more cost-effective than prophylaxis and prevents at least some transplant patients from being exposed to potentially toxic antiviral agents. However, the consensus recommendations are to use prophylactic therapy in the most at-risk patients. Late-onset disease has been associated with higher mortality and graft rejection and is not seen with preemptive therapy. Valganciclovir is a prodrug of ganciclovir that is converted to the parent compound by intestinal and hepatic esterases. Patients who fail or cannot tolerate ganciclovir or valganciclovir therapy are usually treated with foscarnet. However, with the prophylactic strategies discussed above, resistance is becoming more of a concern. He was seen by his home health nurse, who noted shortness of breath, and trimethoprim-sulfamethoxazole was prescribed by his physician, with subsequent improvement. After discharge from the hospital, the patient began to have nausea and vomiting, as well as shortness of breath and purulent sputum. Which of the white blood cells is frequently increased in number in infections with this parasite If this organism were to invade the bloodstream or the central nervous system, how might this manifest clinically Three common types of nematode larvae pass through the lung as part of their life cycle: Ascaris lumbricoides, hookworm (Necator americanus and Ancylostoma duodenale), and Strongyloides stercoralis. Interestingly, strongyloidiasis has not been a significant problem in Vietnam War veterans, although the parasite is endemic in that country, especially in the rice-growing regions of the Mekong Delta. This patient was not a Vietnam War veteran, but as these veterans age, they may begin to manifest latent infections potentially obtained in Vietnam, such as Stronglyloides, Burkholderia pseudomallei, or Mycobacterium tuberculosis. This parasite has a highly complex life cycle, with autoinfection being a prominent feature. Two larval forms are central to its life cycle: the filariform larvae (the infective form) and the rhabditiform larvae (the initial form of the worm, which develops into the filariform larvae). The life cycle begins with filariform larvae penetrating the skin from fecally contaminated soil. The larvae migrate via the bloodstream to the lung, where they break through the wall of the alveoli, crawl out of the bronchus and up the trachea, are swallowed, and reach the duodenum. There the parasite develops into an adult worm that invades and lives beneath the intestinal wall mucosa. If feces are passed onto soil, the rhabditiform larvae either develop into filariform (infectious) larvae, and the cycle begins anew, or they develop into adult worms. These adult worms lay eggs in the soil that hatch into rhabditiform larvae and develop into filariform larvae. An important phase of the Strongyloides life cycle in hyperinfection states is the autoinfective stage. In this stage, rhabditiform larvae develop into filariform larvae in the intestinal tract. The filariform larvae then penetrate either the intestinal wall or the perianal skin, enter the bloodstream, migrate to the lung, and begin the infectious process again. It is estimated that the parasite can live for 30 or 40 years in the human gastrointestinal tract. Although the parasite may persist for many years, the parasite-host relationship appears to be kept in balance by the immune system. Infected, immunocompetent individuals frequently are asymptomatic, or they may have intermittent symptoms, which usually are gastrointestinal, including abdominal pain, diarrhea, nausea, or vomiting. A few Case 19 147 patients might have intermittent "larva currens" (racing larvae), characterized by itching and skin rash. However, when patients receive immunosuppressive therapy, the balance between host and parasite is tilted in favor of the parasite. This sharp increase in the number of parasites, with corresponding severe clinical disease due to tissue invasion by S. Patients with the hyperinfection syndrome frequently begin with worsening gastrointestinal symptoms similar to but more severe than those in symptomatic, immunocompetent individuals. These patients also may have cough, shortness of breath, wheezing, and an abnormal chest radiograph, and they can rapidly progress to respiratory failure. In addition, the larvae can migrate to other organs, including the central nervous system. Hyperinfection due to Strongyloides is of concern in patients who are organ transplant candidates because they will receive long-term immunosuppressive therapy. This therapy suppresses cell-mediated immunity, which is essential for immunoregulation of Strongyloides infection. Therefore, in patients who have lived in areas in which the nematode is endemic, such as tropical and subtropical regions of Asia and South America and the southeastern United States, screening for antibodies to Stronglyloides is routinely done prior to transplantation. If positive, the patient is treated even though the test may give false positives due to the cross-reaction with other helminths. It is important to note that serology cannot differentiate between current and prior infection, so treatment of a seropositive transplant candidate is done strictly as a precautionary measure. By comparison, stool exam in all but hyperinfection states such as occurred in this patient is insensitive and does not reliably detect low-grade infections. The use of repeated stool examination has been shown to increase the sensitivity of Strongyloides detection but not to the level of serology. The use of the agar plate culture technique has been shown to be more sensitive for the detection of S. In this method, stool is placed on sterile agar plates, and the presence of characteristic furrows due to the migration of the parasites on the surface of the agar is sought. As with many tissue-invasive parasites, eosinophil counts are increased in patients with strongyloidiasis. Although the eosinophil count was not available in this patient, the absence of eosinophilia in hyperinfection is not unusual. Patients presenting with hyperinfection are frequently receiving immunosuppressive drugs that may reduce the numbers of white cells (including eosinophils) in the blood. As mentioned previously, larvae can migrate to the central nervous system during hyperinfection. Individuals with invasion of the blood or of the central nervous system during the hyperinfection syndrome may have polymicrobial bacteremia or meningitis from which multiple species of enteric bacteria, such as Escherichia coli, Klebsiella pneumoniae, or Enterococcus spp. It is postulated that the migrating 148 Respiratory Tract Infections Strongyloides larvae are transporting enteric bacteria during their migration. Whenever enteric bacteria are recovered from cerebrospinal fluid or blood of an immunocompromised host, especially if more than one species is found, hyperinfection syndrome due to Strongyloides should be considered. Increased detection rate of Strongyloides stercoralis by repeated stool examinations using the agar plate culture method. Increased sensitivity of routine laboratory detection of Strongyloides stercoralis and hookworm by agar-plate culture. After extraction from the vehicle, he was sedated, put on a backboard with cervical collar, intubated, and transported to a level 1 trauma center.