Buy generic promethazine 25 mg
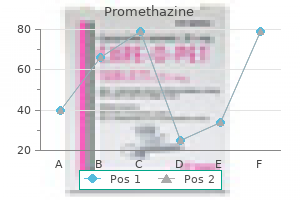
In muscular arteries allergy shots on nhs discount promethazine 25 mg free shipping, the tunica intima also contains a layer of thin elastic connective tissue. The tunica media, or middle layer, consists of smooth muscle cells arranged circularly around the blood vessel. It also contains variable amounts of elastic and collagen fibers, depending on the size and type of the vessel. In muscular arteries, a layer of elastic connective tissue forms the outer margin of the tunica media. The tunica adventitia (ad-ventish a) is composed of dense connective tissue adjacent to the tunica media; the tissue becomes loose connective tissue toward the outer portion of the blood vessel wall. Cardiovascular Capillaries Blood flows from arterioles into capillaries, which branch to form networks (figure 13. Blood flow through capillaries is regulated by smooth muscle cells called precapillary sphincters located at the origin of the branches. Capillary walls consist of endothelium (en-do-the le-um), which is a layer of simple squamous epithelium surrounded by delicate loose connective tissue. The thin walls of capillaries facilitate diffusion between the capillaries and surrounding cells. Capillaries branch without changing their diameter, which is approximately the same as the diameter of a red blood cell (7. Red blood cells flow through most capillaries in single file and are frequently folded as they pass through the smaller-diameter capillaries. Capillary networks are more numerous and more extensive in the lungs and in highly metabolic tissues, such as the liver, kidneys, skeletal muscle, and cardiac muscle, than in other tissue types. Veins Blood flows from capillaries into venules and from venules into small veins. Venules (ven oolz) have a diameter slightly larger than that of capillaries and are composed of endothelium resting on a delicate connective tissue layer (see figure 13. The 352 Chapter 13 Tunica adventitia Tunica adventitia Tunica media (elastic tissue and smooth muscle) Connective tissue Endothelium and basement membrane Tunica media Tunica intima Connective tissue Endothelium and basement membrane (g) Large veins. The tunica media is thin but can regulate vessel diameter because blood pressure in the venous system is low. Elastic arteries recoil when stretched, which prevents blood pressure from falling rapidly. Tunica adventitia Elastic connective tissue Smooth muscle Elastic connective tissue Connective tissue Endothelium and basement membrane (b) Muscular arteries. Tunica media Tunica adventitia Tunica media Tunica intima Connective tissue Endothelium and basement membrane (f) Small and medium veins. Tunica intima Cardiovascular Tunica adventitia Tunica intima Tunica media Tunica intima (c) Arterioles. All three tunics are present; the tunica media consists of only one or two layers of circular smooth muscle cells. Only the tunica intima resting on a delicate layer of dense connective tissue is present. Walls consist of only a simple endothelium surrounded by delicate loose connective tissue. Arteriole Precapillary sphincters Capillaries Capillary network media contains a continuous layer of smooth muscle cells, and the connective tissue of the tunica adventitia surrounds the tunica media (see figure 13. The three thin but distinctive tunics make up the wall of the medium-sized and large veins. The tunica media contains some circular smooth muscle and sparsely scattered elastic fibers. The predominant layer is the outer tunica adventitia, which consists primarily of dense collagen fibers (see figures 13. The connective tissue of the tunica adventitia determines the degree to which they can distend. Veins having diameters greater than 2 mm contain valves, which allow blood to flow toward the heart but not in the opposite direction (figure 13. Each valve consists of folds in the tunica intima that form two flaps, which are similar in shape and function to the semilunar valves of the heart. There are many valves in medium-sized veins and more valves in veins of the lower limbs than in veins of the upper limbs. This prevents blood from flowing toward the feet in response to the pull of gravity. Blood flow decreases when the precapillary sphincters constrict and increases when they dilate. The tunica the pulmonary circulation is the system of blood vessels that carries blood from the right ventricle of the heart to the lungs and back to the left atrium of the heart. Blood from the right ventricle is pumped into a short vessel called the pulmonary (pul mo-nar-e) trunk (figure 13. The pulmonary trunk then branches into the right and left pulmonary arteries, which extend to the right and left lungs, respectively. As a consequence, venous pressure is greater than normal in the veins of the lower limbs and can result in edema (swelling) of the limb. For example, stand- Varicose Veins the blocked veins can prevent blood from flowing through the capillaries that are drained by the veins. Four pulmonary veins (two from each lung) exit the lungs and carry the oxygen-rich blood to the left atrium. Cardiovascular systemiC CirCulAtion: Arteries Learning Outcome After reading this section, you should be able to 13. The part of the descending aorta that extends from the diaphragm to the point at which it divides into the two common iliac (il e-ak) arteries is called the abdominal (ab-dom i-nal) aorta (figure 13. An arterial aneurysm (an u-rizm; a dilation) is a localized dilation of an artery that usually develops in response to trauma or a congenital (existing at birth) weakness of the artery wall. Rupture of a large aneurysm in the aorta is almost always fatal, and rupture of an aneurysm in an artery of the brain causes massive damage to brain tissue and even death. The first vessel to branch from the aortic arch is the brachiocephalic (bra ke-o-se-fal ik; vessel to the arm and head) artery. This short artery branches at the level of the clavicle to form the right common carotid (ka-rot id) artery, which transports blood to the right side of the head and neck, and the right subclavian (sub-kla ve-an; beneath the clavicle) artery, which transports blood to the right upper limb (see figures 13. Instead, both the left common carotid and the left subclavian arteries branch directly off the aortic arch (see figures 13. The left common carotid artery transports blood to the left side of the head and neck, and the left subclavian artery transports blood to the left upper limb. The common carotid arteries extend superiorly along each side of the neck to the angle of the mandible, where they branch into internal and external carotid arteries. The base of each internal carotid artery is slightly dilated to form a carotid sinus, which contains structures important in monitoring blood pressure (baroreceptors). The external carotid arteries have several branches that supply the structures of the neck, face, nose, and the systemic circulation is the system of blood vessels that carries blood from the left ventricle of the heart to the tissues of the body and back to the right atrium. Oxygen-rich blood from the pulmonary veins passes from the left atrium into the left ventricle and from the left ventricle into the aorta. Aorta All arteries of the systemic circulation branch directly or indirectly from the aorta (a-or ta). The aorta is usually considered in three parts-the ascending aorta, the aortic arch, and the descending aorta; the last segment is further divided into the thoracic aorta and the abdominal aorta (figure 13. The ascending aorta is the part of the aorta that passes superiorly from the left ventricle. The right and left coronary arteries arise from the base of the ascending aorta and supply blood to the heart (see chapter 12). Three major arteries, which carry blood to the head and upper limbs, originate from the aortic arch: the brachiocephalic artery, the left common carotid artery, and the left subclavian artery (figure 13. After passing from the right atrium to the right ventricle, blood is pumped into the pulmonary trunk. The internal carotid arteries pass through the carotid canals and contribute to the cerebral arterial circle (circle of Willis) at the base of the brain (figure 13.
Promethazine 25 mg otc
Severe atherosclerosis is more prevalent in some families than in others allergy testing shots purchase promethazine with mastercard, which suggests a genetic influence. Some evidence suggests that a low-fat diet, mild exercise, and relaxation activities slow the progression of atherosclerosis and may even reverse it to some degree. Atherosclerosis greatly increases resistance to blood flow because the deposits narrow the inside diameter of the arteries. The added resistance hampers normal circulation to tissues and greatly increases the work the heart must perform. Furthermore, the rough atherosclerotic plaques attract platelets, which adhere to them and increase the chance of thrombus formation. Their walls become thicker, and consequently the efficiency of capillary exchange decreases. Veins tend to develop patchy thickenings in their walls, resulting in narrowing in these areas. The tendency to develop varicose veins increases with age (see Clinical Impact earlier in this chapter), as does the tendency to develop hemorrhoids (varicose veins of the rectum or anus) because some veins increase in diameter due to weakening of the connective tissue in their walls. There is a related increase in the development of thromboses and emboli, especially in veins that are dilated or those in which blood flow is sluggish. Cardiovascular 380 Chapter 13 3 4 Actions Reactions Atrial natriuretic mechanism: Cardiac muscle cells detect increased atrial blood pressure; secretion of atrial natriuretic hormone increases. Blood pressure (normal range) 1 Start here 6 Cardiovascular Homeostasis Disturbed: Blood pressure decreases. Reactions Effectors Respond: Vasoconstriction increases peripheral resistance to blood flow. AnsWer to leArn tO PrediCt After reading the Clinical impact "Circulatory shock" in this chapter, we learned that circulatory shock is inadequate blood flow throughout the body and that septic shock is one type of circulatory shock. Large, elastic arteries have many elastic fibers but little smooth muscle in their walls. They carry blood from the heart to smaller arteries with little decrease in pressure. They undergo vasodilation and vasoconstriction to control blood flow to different regions of the body. Arterioles, the smallest arteries, have smooth muscle cells and a few elastic fibers. They undergo vasodilation and vasoconstriction to control blood flow to local areas. The circulatory system can be divided into the pulmonary vessels and the systemic vessels. The circulatory system carries blood; exchanges nutrients, waste products, and gases; transports hormones; regulates blood pressure; and directs blood flow. The heart pumps blood through elastic arteries, muscular arteries, and arterioles to the capillaries. Blood returns to the heart from the capillaries through venules, small veins, medium-sized veins, and large veins. The tunica intima, the innermost layer, consists of endothelium, a basement membrane, and connective tissue. The tunica media, the middle layer, contains circular smooth muscle and elastic fibers. Capillaries consist of only endothelium and are surrounded by a basement membrane and loose connective tissue. Small veins are venules covered with a layer of smooth muscle and a layer of connective tissue. Medium-sized and large veins contain less smooth muscle and fewer elastic fibers than arteries of the same size. Veins of the Upper Limbs the deep veins are the brachial, axillary, and subclavian; the superficial veins are the cephalic, basilic, and median cubital. Veins of the Thorax the left and right brachiocephalic veins and the azygos veins return blood to the superior vena cava. The pulmonary trunk carries oxygen-poor blood from the heart to the lungs, and pulmonary veins carry oxygen-rich blood from the lungs to the left atrium of the heart. Veins from the kidneys, adrenal glands, and gonads directly enter the inferior vena cava. Veins from the stomach, intestines, spleen, and pancreas connect with the hepatic portal vein, which transports blood to the liver for processing. The brachiocephalic, left common carotid, and left subclavian arteries branch from the aortic arch to supply the head and the upper limbs. The common carotid arteries divide to form the external carotids (which supply the face and mouth) and the internal carotids (which supply the brain). Blood pressure is a measure of the force exerted by blood against the blood vessel walls. Blood pressure can be measured by listening for Korotkoff sounds produced as blood flows through arteries partially constricted by a blood pressure cuff. Arteries of the Upper Limbs the subclavian artery continues as the axillary artery and then as the brachial artery, which branches to form the radial and ulnar arteries. Pressure and Resistance In a normal adult, blood pressure fluctuates between 120 mm Hg (systolic) and 80 mm Hg (diastolic) in the aorta. If blood vessels constrict, resistance to blood flow increases, and blood flow decreases. Thoracic Aorta and Its Branches the thoracic aorta has visceral branches, which supply the thoracic organs, and parietal branches, which supply the thoracic wall. Abdominal Aorta and Its Branches the abdominal aorta has visceral branches, which supply the abdominal organs, and parietal branches, which supply the abdominal wall. Blood pressure, capillary permeability, and osmosis affect movement of fluid across the wall of the capillaries. Arteries of the Lower Limbs the common iliac arteries give rise to the external iliac arteries, and the external iliac artery continues as the femoral artery and then as the popliteal artery in the leg. Blood flow through a tissue is usually proportional to the metabolic needs of the tissue and is controlled by the precapillary sphincters. The nervous system is responsible for routing the flow of blood, except in the capillaries, and for maintaining blood pressure. Epinephrine and norepinephrine released by the adrenal medulla alter blood vessel diameter. The baroreceptor reflex changes peripheral resistance, heart rate, and stroke volume in response to changes in blood pressure. The heart releases atrial natriuretic hormone when atrial blood pressure increases. Atrial natriuretic hormone stimulates an increase in urine production, causing a decrease in blood volume and blood pressure. The baroreceptor, chemoreceptor, and adrenal medullary reflex mechanisms are most important in short-term regulation of blood pressure. Hormonal mechanisms, such as the renin-angiotensin-aldosterone system, antidiuretic hormone, and atrial natriuretic hormone, are more important in long-term regulation of blood pressure. Epinephrine released from the adrenal medulla as a result of sympathetic stimulation increases heart rate, stroke volume, and vasoconstriction. Reduced elasticity and thickening of arterial walls result in hypertension and decreased ability to respond to changes in blood pressure. Name, in order, all the types of blood vessels, starting at the heart, going to the tissues, and returning to the heart. What is the function of valves in blood vessels, and which blood vessels have valves Name the major arteries that branch from the aorta and deliver blood to the vessels that supply the heart, the head and upper limbs, and the lower limbs. Name the arteries that supply the major areas of the head, upper limbs, thorax, abdomen, and lower limbs. Describe the changes in blood pressure, starting in the aorta, moving through the vascular system, and returning to the right atrium. Define pulse pressure, and explain what information can be determined by monitoring the pulse.
Discount promethazine 25 mg without a prescription
The systemic blood pressure can decrease enough that the blood flow to the brain decreases allergy medicine gastritis 25mg promethazine for sale. Decreased blood flow to the brain results in a reduced O2 level in the brain tissue, causing dizziness. If the amount of amino acids is excessive, ammonia or keto acids, the breakdown products of amino acid metabolism, can accumulate to toxic levels. Ammonia is toxic, so it is converted in the liver to urea, which is carried by the blood to the kidneys and eliminated. The heat raises body temperature, which is resisted by the dilation of blood vessels in the skin and by sweating. No, this approach does not work because he is not losing stored energy from adipose tissue. In the sauna, he gains heat, primarily by convection from the hot air and by radiation from the hot walls. The loss of water will make him thirsty, and he will regain the lost weight from drinking fluids and eating foods containing water. Because the water is cool, raising the water to body temperature requires the expenditure of energy. The body also conserves heat by constricting blood vessels in the skin (producing pale skin) and by reducing sweat loss (producing dry skin). When the fever breaks-that is, "the crisis is over"-heat is lost from the body to lower body temperature to normal. This is accomplished by dilation of blood vessels in the skin (producing flushed skin) and increased sweat loss (producing wet skin). The rate of urine production increased over the next 2 hours, and the urine was dilute. The water he consumed increased his blood volume and decreased the concentration (osmolality) of his blood. The sodium chloride increased the concentration (osmolality) of his blood without affecting the volume of blood. The excessive sweating results in a reduced blood volume and the blood has a greater than normal concentration (osmolality). Excessive urine production, low blood pressure, high plasma K+ levels, but not high plasma Na+ levels, result. The Na+ attract water molecules from the peritubular capillaries into the nephron, which results in a greater than normal urine volume. The loss of water in the urine reduces the blood volume and therefore reduces the blood pressure. Because aldosterone causes Na+ reabsorption from the nephron and K+ secretion into the nephron, K+ accumulate in the plasma. The following all decrease the blood pressure in the glomerular capillaries and therefore decrease the glomerular filtration rate: decreased blood pressure and increased sympathetic stimulation that constricts the renal arteries and the afferent arterioles. Blocking the nephron causes the capsule pressure in the nephron to increase, so that it is equal to the pressure in the glomerular capillaries, which reduces the filtration rate. The increased plasma protein concentration attracts water by osmosis and therefore reduces the tendency for water to pass from the glomerulus to Bowman capsule. The rate and depth of respiration increase because a decreased body fluid pH stimulates the respiratory center. The decrease in the body fluid pH causes the kidneys to secrete additional H+ into the nephron. The increased concentration of H+ in the body fluids caused the pH of the body fluids to decrease. The kidneys are more powerful regulators of body fluid pH, but they require several hours to become maximally active. Since Martha lost fluid from her body and she consumed no fluid, the concentration of her body fluids increased and her blood volume decreased. In addition, the progesterone acts on the endometrium of the uterus to cause its maximum development. Therefore, progesterone secretion reaches its maximum levels and the endometrium reaches its greatest degree of development during the secretory phase of the menstrual cycle. Progesterone is not secreted in large amounts until the corpus luteum is formed after ovulation. The corpus luteum secretes progesterone in increasing quantities and small amounts of estrogen as the corpus luteum develops. A drug that blocks the effect of progesterone on its target tissues will cause the tissue to respond as if no progesterone were present. The progesterone affects the endometrium of the uterus and, in response, the endometrium becomes prepared for implantation. If a drug that blocks progesterone is taken by a woman who is pregnant, the effect will be to cause the endometrium to slough. The corpus luteum of the ovary secretes progesterone until the end of the first 3 months of pregnancy; prior to the third month of pregnancy, the placenta begins to secrete progesterone. The placenta becomes the primary source of progesterone after the third month of pregnancy. During menopause, estrogen and progesterone are produced by the ovary in only small amounts. It has just completed the "budding" period; limb buds and other "buds" have just formed (see table 20. A high fever during this period could prevent neural tube closure in the embryo, so that the newborn baby may have neural tube defects, such as anencephaly (open neural tube in the area of the brain, resulting in absence of the upper brain) or spina bifida (open spinal cord resulting from failure of the neural tube to close in that area). Surges of prolactin are stimulated by the process of suckling and are required to maintain milk production. Drugs that inhibit prolactin release will cause the breast to cease milk production after a few days. Because dimpled cheeks are dominant, a person with dimpled cheeks may have a genotype of Dd (D being the dominant gene for dimples and d being the normal gene). If two Dd, dimpled people have a child, there is a 25% probability that the child would not have dimples (dd). To be able to roll their tongue into a tube, both mother and son need to have only one dominant gene. It is also possible that his father is a tongue roller, but there is no proof for either hypothesis. A female must have the genotype XhXh to have hemophilia, whereas because males have only one X chromosome, a single hemophilia gene will cause them to have the disorder (XhY). In this chapter, you learned that in order to keep body temperature near its set point, the control center (the hypothalamus), receives input from thermoreceptors in the skin. The hypothalamus would then instruct the effectors (the sweat glands), to produce sweat if body temperature had risen too high. So, for this question, you can predict that swimming in cool water would prevent the hypothalamus from stimulating the sweat glands to produce sweat. The next part of the question asks what would happen if this mechanism was not sufficient to maintain normal body temperature. In other words, if you were swimming in cool water, the thermoreceptors would cause the hypothalamus to initiate shivering. Simply preventing sweating was insufficient to keep body temperature from dropping out of its normal range. If shivering continued to be ineffective, the body would conserve heat through loss of consciousness and severe hypothermia could set in. To answer this question, you must first recall the major difference between negative-feedback mechanisms and positive-feedback mechanisms. Negative feedback returns a variable to its set point while positive feedback keeps a variable different from its set point. When you are thirsty your impulse is to drink something, thereby adding fluid to your body.
| Comparative prices of Promethazine | ||
| # | Retailer | Average price |
| 1 | Alimentation Couche-Tard | 426 |
| 2 | Advance Auto Parts | 369 |
| 3 | Big Lots | 581 |
| 4 | Meijer | 852 |
| 5 | Nordstrom | 488 |
| 6 | Family Dollar | 476 |
| 7 | Target | 543 |
| 8 | 7-Eleven | 932 |
| 9 | Dick's Sporting Goods | 155 |
Discount promethazine 25 mg line
During their development allergy treatment in toddlers cheap promethazine online, red blood cells lose their nuclei and most of their organelles. Red Function the primary functions of red blood cells are to transport oxygen from the lungs to the various tissues of the body and to help transport carbon dioxide from the tissues to the lungs. Oxygen transport is accomplished by hemoglobin, which consists of four protein chains and four heme groups. Each heme contains one iron atom, which is necessary for the normal function of hemoglobin. Hemoglobin picks up oxygen in the lungs and releases oxygen in other tissues (see chapter 15). Hemoglobin that is bound to oxygen is bright red, whereas hemoglobin without bound oxygen is a darker red. Stem cells form proerythroblasts (pro-erithro-blastz; pro-, before + erythro-, red + blastos, germ), which give rise to the red blood cell line (see figure 11. After each cell division, the new cells change and become more like mature red blood cells. In the later divisions, the newly formed cells manufacture large amounts of hemoglobin. After the final cell division, the cells lose their nuclei and become completely mature red blood cells. Consequently, a lack of folate, vitamin B12, or iron can interfere with normal red blood cell production. Typical causes of low blood oxygen are decreased numbers of red blood cells, decreased or defective hemoglobin, diseases of the lungs, high altitude, inability of the cardiovascular system to deliver blood to tissues, and increased tissue demand for oxygen, as occurs during endurance exercises. Thus, when oxygen levels in the blood decrease, the production of erythropoietin increases, which increases red blood cell production. Conversely, if blood oxygen levels rise, less erythropoietin is released, and red blood cell production decreases. Women need more dietary iron than men do because women lose iron as a result of menstruation. Although oxygen is the primary molecule that binds to hemoglobin, other molecules can also bind to hemoglobin. Carbon monoxide, a gas produced by the incomplete combustion of hydrocarbons, such as gasoline, is one example. It binds to the iron in hemoglobin about 210 times more readily than does oxygen and does not tend to unbind. Nausea, headache, unconsciousness, and death are possible consequences of prolonged exposure to carbon monoxide. Carbon dioxide is produced in tissues and transported in the blood to the lungs, where it is removed from the blood (see chapter 15). Approximately 70% of the carbon dioxide in blood is transported in the form of bicarbonate ions. When red blood cells become old, abnormal, or damaged, they are removed from the blood by macrophages located in the spleen and liver (figure 11. Within the macrophage, the globin part of the hemoglobin molecule is broken down into amino acids that are reused to produce other proteins. The iron released from heme is transported in the blood to the red bone marrow and used to produce new hemoglobin. The heme molecules are converted to bilirubin (bil-i-roo bin), a yellow pigment molecule. Bilirubin is normally taken up by the liver and released into the small intestine as part of the bile (see chapter 16). If the liver is not functioning normally, or if the flow of bile from the liver to the small intestine is hindered, bilirubin builds up in the circulation and produces jaundice (jawn dis; jaune, yellow), a Blood 303 Decreased blood oxygen Increased blood oxygen yellowish color to the skin. After it enters the intestine, bilirubin is converted by bacteria into other pigments. Some of these pigments give feces their brown color, whereas others are absorbed from the intestine into the blood, modified by the kidneys, and excreted in the urine, contributing to the characteristic yellow color of urine. When the components of blood are separated from one another, white blood cells as well as platelets make up the buffy coat, a thin, white layer of cells between plasma and red blood cells (see figure 11. White blood cells are larger than red blood cells, and each has a nucleus (table 11. Although white blood cells are components of the blood, the blood serves primarily as a means of transporting these cells to other body tissues. White blood cells can leave the blood and travel by ameboid (a-meboyd; like an ameba) movement through the tissues. In this process, the cell projects a cytoplasmic extension that attaches to an object. Two functions of white blood cells are (1) to protect the body against invading microorganisms and other pathogens and (2) to remove dead cells and debris from the tissues by phagocytosis. Red Blood Cell Production Aged, abnormal, or damaged red blood cells in response to decreased blood oxygen, the kidneys release erythropoietin into the general circulation. Cardiovascular 1 In macrophages, the globin part of hemoglobin is broken down to individual amino acids (red arrow) and metabolized or used to build new proteins. Those containing large cytoplasmic granules are granulocytes (gran u-lo-sitz; granulo-, granular), and those with very small granules that cannot be seen easily with the light microscope are agranulocytes (a-gran u-lo-sitz; a-, without). Neutrophils (noo tro-filz; neutro-, neutral + philos, loving), the most common type of white blood cells, have small cytoplasmic granules that stain with both acidic and basic dyes (figure 11. Their nuclei are commonly lobed, with the number of lobes varying from two to four. Dead neutrophils, cell debris, and fluid can accumulate as pus at sites of infections. Basophils (baso-filz; baso-, base), the least common of all white blood cells, contain large cytoplasmic granules that stain blue or purple with basic dyes (table 11. Basophils release histamine and other chemicals that promote inflammation (see chapters 4 and 14). Eosinophils (e-o-sin o-filz) contain cytoplasmic granules that stain bright red with eosin, an acidic stain. Eosinophils are involved in inflammatory responses associated with allergies and asthma. In addition, chemicals from eosinophils are involved in destroying certain worm parasites. Lymphocytes (limfo-sitz; lympho-, lymph) are the smallest of the white blood cells (table 11. The lymphocytic cytoplasm consists of only a thin, sometimes imperceptible ring around the nucleus. Their diverse activities involve the production of antibodies and other chemicals that destroy microorganisms, contribute to allergic reactions, reject grafts, control tumors, and regulate the immune system. After they leave the blood and enter tissues, monocytes enlarge and become macrophages (mak ro-fa-jez; macro-, large + phago, to eat), which phagocytize bacteria, dead cells, cell fragments, and any other debris within the tissues. In addition, macrophages can break down phagocytized foreign substances and present the processed substances to lymphocytes, causing activation of the lymphocytes (see chapter 14). Predict 3 Based on their morphology, identify each of the white blood cells shown in figure 11. Platelets Platelets are minute fragments of cells, each consisting of a small amount of cytoplasm surrounded by a cell membrane (see figure 11. They are produced in the red bone marrow from megakaryocytes (meg-a-kar e-o-sitz; mega-, large + karyon, nucleus), which are large cells (see figure 11. Small fragments of these cells break off and enter the blood as platelets, which play an important role in preventing blood loss. When a blood vessel is damaged, blood can leak into other tissues and interfere with normal tissue function, or blood can be lost from the body. The body can tolerate a small amount of blood loss and can produce new blood to replace it. Fortunately, when a blood vessel is damaged, loss of blood is minimized by three processes: vascular spasm, platelet plug formation, and blood clotting.
Best purchase promethazine
It is appropriate to use when there is no desire to anesthetize the stable patient to perform a diagnostic subxyphoid pericardial window or when the ultrasound machine is broken or unavailable allergy quick dissolve strips discount promethazine 25 mg free shipping. Any 10 mm Hg increase in central venous pressure over time in the relaxed supine patient receiving only maintenance intravenous fluids should prompt a median sternotomy or thoracotomy. A pericardiocentesis has a therapeutic effect in the patient with cardiac tamponade and hemodynamic instability. However, the diagnostic sensitivity of this maneuver in the stable patient with a small tamponade has always been questioned. An open surgical subxyphoid pericardial window is performed under general anesthesia and mandates a bloodless operative approach. Also, it is used in many centers around the world when nonsurgeon or surgeon-performed ultrasound is unavailable or when there is not acceptable accuracy. The operative approach is through a 5 cm to 10 cm midline incision starting on the xyphoid process, which may be excised as needed for exposure. The linea alba is divided, and extraperitoneal dissection is performed bluntly in a superior direction toward the pericardium. Exposure is enhanced by lifting the xiphoid process (if still in place) and the lower sternum up with one medium Richardson retractor or two Army-Navy retractors. Once cardiac pulsations are palpated, the inferior pericardial sac is grasped with two long Allis clamps, and a 2-cm vertical pericardiotomy is made between the clamps. Patients who manifest progressive hemodynamic deterioration during the subxyphoid pericardial window should undergo left anterolateral thoracotomy and opening of the pericardium through that approach. Some centers choose to wash blood out of the pericardial sac after a positive window in the reasonably stable patient and to observe for further bleeding without opening the pericardial sac further. The rationale for this approach is that pericardial wounds only or wounds that injure the cardiac wall superficially (epicardium and outer myocardium) may have stopped bleeding by the time the pericardial window has been performed. This maneuver can also diagnose intracardiac lesions such as septal defects or valvular injuries and can also calculate an ejection fraction. Unfortunately, the majority of penetrating cardiac injuries come to the emergency department on weeknights or weekends when the specialists who perform formal transthoracic or transesophageal ultrasounds are not available. Additionally, the sedation required to properly perform transesophageal echocardiography would be contraindicated in the unstable patient with this injury scenario. Over the past 15 years, reports have been documented that transthoracic echocardiography performed in the emergency center by surgeons or specialists in emergency medicine using a 3. This usually results in a clear view of the apex of the heart, the pericardium, and the left lobe of the liver. The beating heart in this real-time ultrasound approach should lie immediately adjacent to the liver. Should tamponade be present, a black stripe will separate the beating heart from the liver. The black or anechoic stripe with an ultrasound density that is the same as blood in the inferior vena cava represents blood outside the heart or represents a tamponade. The ultrasound probe is next placed in a horizontal direction in the 4th or 5th left parasternal space to obtain a coronal view of the same cardiac structures. In the study by Rozycki et al, 246 patients with penetrating thoracic wounds were evaluated by surgeon-performed ultrasound. A follow-up study by Rozycki et al in 313 patients with penetrating precordial or transthoracic wounds resulted in 289 true-negative examinations, two false-positive examinations, and 22 true-positive examinations. Finally, Rozycki et al completed a multicenter study in which emergency pericardial sonograms were performed by ultrasound technicians, cardiologists, or surgeons. The accuracy (97%), specificity (97%), and sensitivity (100%) were equivalent to those reported in the previous study from Grady Memorial Hospital. Arrhythmias such as sinus tachycardia, premature atrial or ventricular contractions, and heart block are the most common manifestations of blunt cardiac injury. When an operation for another injury is indicated in a patient with blunt cardiac injury, not including cardiac rupture, the prognosis is generally excellent. In the report by Flancbaum et al, 19 patients with blunt cardiac injury had an emergency operation, including 15 on the day of admission. The duration of anesthesia was 6 hours, and there were no cardiac-related complications or deaths. The same incision(s) would be used in the operating room for agonal patients or for those having gone into cardiac arrest particularly following transmediastinal gunshot wounds. These incisions allow for expedited control of hemorrhage from cardiac perforation(s) and for cross-clamping of the descending thoracic aorta. The anterolateral thoracotomy approach may also be kept separate from any abdominal midline incision needed to address intraabdominal injury. The median sternotomy is performed in the operating room in patients who are more hemodynamically stable and who have solitary anterior stab wounds. In such patients, multiple cardiac perforations are unlikely and cross-clamping of the descending thoracic aorta is usually not needed. Pericardiotomy Opening of the left chest via an anterolateral thoracotomy requires a Finochietto retractor after which a longitudinal left lateral pericardiotomy can be performed anterior to the left phrenic nerve. In obese patients where fat obscures the phrenic nerve, the accompanying pericardial-phrenic vessels mark the location. Even if the pericardium is difficult to grab with a forceps secondary to distention of the sac with blood, the surgeon should resist performing a pericardiotomy with a scalpel. This is a particularly dangerous as right-sided tamponade from a wound to the atrium or ventricle may push the heart to the left so that it lies immediately underneath or abuts the left pericardial sac. In this position, the left anterior descending coronary artery is at risk of injury if a scalpel is passed too deep while opening the pericardium. A better technique is to lift the pericardium with a toothed forceps and to open the sac with the tip of a straight Mayo scissors. Once it has been opened, the pericardium generally lifts away from the surface of the heart allowing the incision to be extended in a superior direction until the pericardial fold on the great vessels is reached. The longitudinal left pericardiotomy is completed in an inferior direction until the left hemidiaphragm is reached. This pericardial incision is made at a right angle to the left lateral pericardiotomy and extends to 1 cm anterior to the right phrenic nerve. In patients undergoing a bilateral anterolateral thoracotomy, either the pericardiotomy described above or the midline pericardiotomy described below can be used. After a median sternotomy and insertion of a Finochietto retractor, the epicardial fat and the anterior extensions of the parietal pleura are swept laterally with the fingers over laparotomy pads. This maneuver exposes the anterior surface of the pericardial sac which is grasped with toothed forceps and opened in a midline longitudinal direction from the great vessels to the diaphragm. Control of Hemorrhage from the Heart (Table 9-2) After the pericardiotomy is performed, blood and thrombus are removed from the pericardial sac manually and with irrigation and suction. A rapid inspection of the anterior surface of the heart and great vessels is performed. A profoundly hypotensive patient may not tolerate inspection of the posterior aspect of the heart, which requires elevation of the apex. Lifting the heart to inspect the underside compresses or kinks the vena cava, restricting right-sided filling. This maneuver also carries with it a risk of sucking air into an open Table 9-2 Techniques for the General Surgeon to Control Hemorrhage from a Cardiac Perforation or Rupture Atrium/ventricle Atrium/ventricle Atrium Lateral atrium adjacent to pericardium or atrium adjacent to ventricle Atrium/ventricle Ventricle Large ventricular hole or multiple chamber wounds Finger Stapler Satinsky vascular clamp row of Allis clamps Foley balloon catheter Crossed mattress sutures Inflow (superior vena cava/ inferior vena cava) occlusion 3-mg intravenous adenosine to induce 10 to 20 seconds asystole. With left ventricular perforation, air has the potential to rapidly move into the coronary arteries causing an air embolism and cardiac arrest. As such, manual palpation of the posterior surface of the heart without elevation of the apex is all that is advised until the patient is resuscitated with a relatively normal blood pressure. Palpation of a posterior defect or jet of blood as a ventricle contracts mandates leaving the finger in place for control of hemorrhage until the aforementioned status can be reached. Once the patient has been stabilized and the surgeon is ready to lift the apex of the heart to inspect the posterior aspect, he or she should notify the anesthesia team so that they are aware and can assist in managing any associated hypotension. If there is bleeding from this posterior aspect of the heart that will require prolonged elevation and/or suturing, the surgeon should consider placing a cross-clamp on the descending thoracic aorta to preserve central pressure and cerebral circulation. A finger or compression with fingers will control hemorrhage from cardiac perforation or cardiac rupture in 95% to 96% of patients. This is because patients with larger defects die at the scene or in transit and are generally not alive to undergo operation.
Promethazine 25mg free shipping
Thoracic wounds in the cardiac box or those with a transmediastinal trajectory that might have injured the superior vena cava should prompt placement of resuscitation lines into the common femoral veins allergy symptoms icd 9 cheap promethazine 25 mg free shipping. Initial application of this hypotensive resuscitation strategy allots for the fact that needless administration of any fluid aimed at achieving an arbitrary systolic blood pressure may lead to or worsen bleeding that had otherwise nearly stopped. Emergency center thoracotomy for resuscitation and control of hemorrhage is indicated in a highly selected group of patients. This maneuver also referred to as resuscitative thoracotomy is performed in hospitals that do not have an operating room in or immediately adjacent to the emergency department. Reasonable indications to perform an emergency center thoracotomy are as follows3,4: 1. Deteriorating shock or cardiac arrest after care has been initiated in the emergency center. Uncontrolled hemorrhage from the thoracic inlet or emanating from a tube thoracostomy tube 4. Need for open cardiac massage or occlusion of the descending thoracic aorta before laparotomy in the operating room 6. Need for open cardiac massage or clamping of thoracic aorta when countershock or closed chest cardiac massage is ineffective. Strong contraindications for the use of resuscitative thoracotomy include penetrating trauma with no signs of life in the field and blunt trauma with no signs of life on arrival in the emergency center. When a penetrating right thoracic wound is present and the patient is agonal on arrival, a bilateral anterolateral thoracotomy. If intrapleural exsanguination from a suspected injury to a subclavian vessel is believed to be present, an anterolateral thoracotomy at a higher intercostal space is appropriate. The primary goal of either a unilateral anterolateral or bilateral anterolateral thoracotomy is to control hemorrhage from a wound to the heart, to a great vessel, or to the lung or to release a cardiac tamponade. Whether suture repair of the injured organ or vessel is appropriate in the emergency department will depend on the following factors: (1) the magnitude of the injury; (2) the success of temporary hemorrhage control maneuvers; (3) the quality of lighting, and (4) the availability of instruments and sutures. An additional and important goal of resuscitative thoracotomy is to cross-clamp the descending thoracic aorta to maintain any remaining central aortic pressure and perfusion to the coronary and carotid arteries. One must be mindful in these scenarios that applying a cross-clamp to the descending thoracic aorta is more difficult through the higher left-sided thoracotomy incisions. Thoracic aortic clamping is performed by first lifting the posterolateral edge of the left lung out of the hemithorax. Once the mediastinal pleura over the descending thoracic aorta and vertebral bodies is visualized, it is opened with scissors. Because of the cost and low survivability of emergency center thoracotomy, the technique has been used more selectively in recent years. The overall reported survival rate of 7% to 10% is somewhat deceptive as it includes patients with penetrating cardiac wounds who have a significantly better outcome. A more recent report on 283 patients undergoing emergency department thoracotomy for penetrating injury to the heart and great vessels documented worse outcomes including a survival rate of 24% in patients with stab wounds and only 3% in those with gunshot wounds. For patients with penetrating wound(s) that may involve the heart, arch, or great vessels who are hemodynamically normal, it is appropriate to image the thorax to better characterize the presence and location of injury. Standard transfemoral digital subtraction aortography may also be useful and augmented with retrograde angiography of the axillary and subclavian vessels via brachial artery or basilica vein access in the upper extremity. In women, the left breast is retracted superiorly and the incision is made at the midaspect of the left hemithorax. The Finochietto retractor is placed with the handle facing the left side of the patient. Hill of Montgomery, Alabama, is credited with the first successful delayed repair of a stab wound to the left ventricle in the United States in 1902. Only rapid transport to a trauma center or acute care hospital will save the lives of patients with repairable cardiac injuries and signs of life in the field. This is because therapeutic procedures such as pericardiocentesis, an open pericardial window, or an emergent anterolateral thoracotomy are not performed in the prehospital setting in the United States or during military conflicts. Having used the tip of an aortic clamp to spread the pleura above and below the mid-descending thoracic aorta, the surgeon is using the left index finger to encircle the aorta and pull it to the left so that the clamp can be applied to under direct vision. B, Atrial wounds are repaired over a Satinsky clamp, while ventricular wounds are repaired by sewing under a finger and under adjacent coronary arteries. C, Patients with profound hypotension, electromechanical dissociation, or asystole undergo two-handed internal cardiac massage. In this study, blunt cardiac injury was determined to have an overall mortality of 89%. In contrast, patients with gunshot wounds present with cardiac tamponade (20%), intrapleural hemorrhage (80%), or both. Cardiac tamponade is caused by blood in an intact pericardial sac, which compresses the atria and impairs venous return. While blood pressure decreases by as much as 10 mm Hg with inspiration secondary to a decrease in left ventricular stroke volume, this decrease may be 15 mm Hg or more in the setting of cardiac tamponade. In the setting of tamponade there is a simultaneous progressive rise in central venous pressure secondary to the impaired venous return. In this scenario, patients often present with a dusky or deathlike appearance that is noticeable regardless of race. If the diagnosis of cardiac tamponade is delayed, myocardial ischemia and continuing decreases in cardiac output occur. This spiral leads to cardiovascular collapse and cardiac arrest in minutes in patients with wounds or ruptures of the ventricles. In patients with wounds or ruptures of the atria, compression of the hole by the extravasated blood in the pericardium may stop further hemorrhage and progressive tamponade. The main hemodynamic finding in such patients is a progressive rise in central venous pressure to 20 mm Hg to 30 mm Hg with profound hypotension or a cardiac arrest as the terminal event. The diagnosis of a compressed atrial wound may go undiagnosed for 12 or more hours until clinical suspicion prompts a pericardial ultrasound, a pericardial window, a sternotomy, or a thoracotomy. Hemorrhage from the injured heart into a pleural cavity most often results from a gunshot wound in the cardiac box or one with a transmediastinal trajectory. Depending on the hemodynamic status of the patient, an early resuscitative thoracotomy, and not diagnostic tests, will be necessary. Measurement of central venous pressure is invasive, time consuming, and may not confirm the diagnosis of cardiac tamponade immediately. When a finger is not successful in controlling bleeding or when more definitive control is needed, the techniques in Table 9-2 may be applied. Disposable skin staplers with long rotating heads have been used to quickly close atrial or ventricular defects for over 2 decades. The safest policy is to buttress any ventricular repair with Teflon pledgets in the operating room in patients who stabilize after the initial hemorrhage control and resuscitation maneuvers. Elevation of an atrial wound with the fingers, forceps, or Allis clamps will frequently allow placement of a Satinsky vascular clamp under the perforation. Atrial wounds or ruptures in the lateral aspect adjacent to the pericardium or anteriorly or posteriorly adjacent to the ventricle cannot be controlled with a Satinsky. With these injuries, Allis clamps grabbing both sides of the defect are placed in a row similar to the method described for wounds to the vena cava for the past 100 years. Use of a Foley balloon catheter to control hemorrhage from a difficult cardiac location after a penetrating wound was first described in 1966. On rare occasions, the length of a ventricular laceration will lead to exsanguinating hemorrhage that will preclude the use of the stapler or the balloon catheter. With manual compression of the defect, a horizontal mattress suture is rapidly placed on either side of the defect, the two ends on each side are placed in the hands, and the hands holding the suture ends are crossed. This should prevent exsanguination as a continuous over-and-over suture row or a row of staples is placed. A temporary closure as described would then be buttressed with Teflon pledgets in the operating room. Because few trauma surgeons are familiar with the bimanual technique for control of hemorrhage from the heart described over a century ago by Ernst Ferdinand Sauerbruch (1875-1951), the related technique of inflow occlusion is used occasionally to control major hemorrhage from the heart. Harken (1910-1983) as a technique to slow the heart and to allow for removal of intracardiac foreign bodies.
Discount promethazine 25mg line
Adrenal androgens increase female sexual drive but normally have little effect in males allergy index denver cheap promethazine online mastercard. The pancreas secretes insulin in response to elevated levels of blood glucose and amino acids. Insulin increases the rate at which many tissues, including adipose tissue, the liver, and skeletal muscles, take up glucose and amino acids. The pancreas secretes glucagon in response to reduced blood glucose and increases the rate at which the liver releases glucose into the blood. Some membrane-bound receptors are associated with membrane proteins called G proteins. Second-messenger systems act rapidly because they act on already existing enzymes and produce an amplification effect. The testes secrete testosterone, and the ovaries secrete estrogen and progesterone. Secretions from the anterior pituitary are controlled by hormones that pass through the hypothalamic-pituitary portal system from the hypothalamus. Hormones secreted from the posterior pituitary are controlled by action potentials carried by axons that pass from the hypothalamus to the posterior pituitary. Pineal Gland the pineal gland secretes melatonin, which may help regulate the onset of puberty by acting on the hypothalamus. Hormones secreted by cells in the stomach and intestine help regulate stomach, pancreatic, and liver secretions. The prostaglandins are hormones that have a local effect, produce numerous effects on the body, and play a role in inflammation. The placenta secretes human chorionic gonadotropin, estrogen, and progesterone, which are essential to the maintenance of pregnancy. Thyroid Gland the thyroid gland secretes thyroid hormones, which control the metabolic rate of tissues, and calcitonin, which helps regulate blood Ca2+ levels. Parathyroid Glands the parathyroid glands secrete parathyroid hormone, which helps regulate blood Ca2+ levels. What are the major functional differences between the endocrine system and the nervous system List the major differences between intracellular and intercellular chemical signals. List the intercellular chemical signals that are classified on the basis of the cells from which they are secreted and their target cells. Describe the mechanisms by which membrane-bound receptors produce responses in their target tissues. Describe the mechanisms by which intracellular receptors produce responses in their target tissues. Compare the means by which hormones that can and cannot cross the cell membrane produce a response. What makes one tissue a target tissue for a hormone and another not a target tissue Describe how secretions of the anterior and posterior pituitary hormones are controlled. What are the functions of the thyroid hormones, and how is their secretion controlled What happens when too large or too small an amount of the thyroid hormones is secreted Explain how calcitonin, parathyroid hormone, and vitamin D are involved in maintaining blood Ca2+ levels. List the hormones secreted from the adrenal gland, give their functions, and compare the means by which the secretion rate of each is controlled. What is the effect if too little insulin is secreted or the target tissues are not responsive to insulin Based on these observations, describe the mechanism by which the membranebound receptor is most likely to produce a response to the hormone. Aldosterone and antidiuretic hormone play important roles in regulating blood volume and concentration of blood. The response to one of these hormones is evident within minutes, and the response to the other requires several hours. Biceps Benny figured that if a small amount of a vitamin was good, a lot should be better, so he began to take supplements that included a large amount of vitamin D. Predict the effect of vitamin D on his blood Ca2+ levels and on the secretion of hormones that regulate blood Ca2+ levels. Explain how the blood levels of glucocorticoids, epinephrine, insulin, and glucagon change after a person has gone without food for 24 hours. However, over the last few days she had started experiencing significant abdominal pain. Blood has always fascinated humans, and throughout history they have speculated about its function. Some societies consider blood the "essence of life" because the uncontrolled loss of it can result in death. Many cultures around the world, both ancient and modern, believe blood has magical qualities. For example, people of a noble bloodline are sometimes described as "blue bloods," whereas criminals are said to have "bad" blood. People commonly say that anger causes their blood to "boil," whereas fear makes it "curdle. Blood performs many functions essential to life and can reveal much about our health. Carbon dioxide, produced by cells, is carried in the blood to the lungs, from which it is expelled. The blood transports Module 9 Cardiovascular system ingested nutrients, ions, and water from the digestive tract to cells, and the blood transports the waste products of the cells to the kidneys for elimination. Many substances are produced in one part of the body and transported in the blood to another part, where they are modified. For example, the precursor to vitamin D is produced in the skin (see chapter 5) and transported by the blood to the liver and then to the kidneys for processing into active vitamin D. Then the blood transports active vitamin D to the small intestine, where it promotes the uptake of calcium. Another example is lactate produced by skeletal muscles during anaerobic respiration (see chapter 7). The blood carries many of the hormones and enzymes that regulate body processes from one part of the body to another. The osmotic composition of blood is also critical for maintaining normal fluid and ion balance. Warm blood is transported from the interior of the body to the surface, where heat is released from the blood. Certain cells and chemicals in the blood constitute an important part of the immune system, protecting against foreign substances, such as microorganisms and toxins. When blood vessels are damaged, blood clotting protects against excessive blood loss. When tissues are damaged, the blood clot that forms is also the first step in tissue repair and the restoration of normal function (see chapter 4). Blood is a type of connective tissue that consists of a liquid matrix containing cells and cell fragments. The liquid matrix is the plasma (plaz ma), and the cells and cell fragments are the formed elements (figure 11. The plasma accounts for slightly more than half of the total blood volume, and the formed elements account for slightly less than half. Unlike the fibrous proteins found in other connective tissues, such as loose connective tissue, plasma contains dissolved proteins.
Purchase generic promethazine on-line
However allergy shots alcohol cheap 25 mg promethazine with mastercard, promising reports on their efficacy have been registered from the terminal stages of the war in Afghanistan and anecdotal cases of civilian trauma. Despite successes associated with the development of a small number of junctional hemorrhage control devices, further research is needed to develop approaches or tools to control noncompressible torso and junctional hemorrhage at the point of injury and in the acute, out-of-hospital phase of care. If a single tourniquet is not successful in controlling extremity hemorrhage, a second tourniquet should be applied to increase the effective tourniquet width. Kragh and others from the United States Army Institute of Surgical Research reported that the application and use of tourniquets to control extremity bleeding before the onset of shock resulted in lower mortality than application of tourniquets after the onset of hemodynamic instability. In a clinical series of 428 tourniquets applied on 309 severely injury limbs, the incidence of nerve palsy was 1. There was no association with vascular thrombosis, myonecrosis, rigor, pain, fasciotomy, or renal failure. Reports from those wars and clinical experience of the editors suggest that the vast majority of tourniquets applied during the wars in Afghanistan and Iraq were in place for 2 hours or less. Clearly tourniquet application and the potential adverse effects of complete limb ischemia for longer periods of time in future military or civilian scenarios will need to be reappraised. TibialLevelInjuries Tibial vascular injury may be the result of penetrating or blunt trauma and is most commonly associated with fracture of the tibia or fibula. In cases in which control of bleeding is difficult, exploration of the vascular injury with ligation of the vessel or placement of a temporary vascular shunt may be necessary before fracture reduction and stabilization. However, in most instances, fracture reduction or traction and stabilization can be performed promptly and results in restoration of perfusion to the leg and foot. The surgical scrub and draping of the patient should be from the umbilicus to the toes of both lower extremities. Preparing the operative field to include the umbilicus and lower abdomen allows for retroperitoneal exposure and control of the iliac vessels if needed. Preparation of the contralateral lower extremity allows one to use saphenous vein from the noninjured extremity as conduit for vascular reconstruction if needed. Also, access to the contralateral femoral artery may be useful to perform percutaneous, transluminal arteriography of the injured lower extremity either as a pre- or completion step using an "up and over" approach. In rare cases, having access to the contralateral femoral artery can be useful as a source of inflow. Regardless of anatomic level, lower extremity vascular reconstruction begins with exposure of the injured segment. Depending on the experience of the surgeon and the anatomic location of the injury, this may be preceded by obtaining remote proximal arterial control. Frequently junctional or proximal femoral vascular injuries require control at an uninjured segment such as the iliac artery through a retroperitoneal exposure. Injuries in the popliteal fossa and those at the tibial trifurcation may also benefit from inflow control at a proximal, uninjured segment. In contrast, superficial femoral injuries in the thigh and those below the tibial trifurcation can often be controlled by extending any penetrating wounds and exploring the injured area directly. Once the injured segment of vessel(s) has been exposed and controlled, assessment should be made as to the extent of injury and adequacy of distal perfusion. The spectrum of vascular trauma ranges from vessel contusion with degrees of thrombosis to transection with a missing segment. In considering management strategies, one must remember that ligation is a viable option in many scenarios. In other words management of lower extremity vascular trauma does not always require vascular reconstruction and restoration of flow through the injured segment. For example, injury of a tibial artery or a branch of the superficial femoral or profunda femorus arteries can often be ligated without compromising viability of the extremity. In these instances, redundant or collateral circulation often exists, which will keep the limb viable, even with a degree of ischemia, without repair of the injured vessel. Viability in these scenarios is most reliably predicted by assessment of capillary refill and with the presence of an arterial Doppler signal distal to the injury. Vessel ligation, with or without primary amputation, may also be a prudent damage control option in patients with a severely mangled extremity or those with a constellation of other life-threatening injuries or physiology. If reconstruction of lower extremity vascular injury is planned, standard operative techniques should be used regardless of anatomic level. Care must be taken to ensure that this compartment is identified separately from the lateral compartment through the lateral leg incision. Opening of the anterior compartment exposes the muscles and anterior neuromuscular bundle, as well as the intermuscular septum, which separates the anterior and the lateral compartments. Both sides of this septum should be visualized assuring that both the anterior and the lateral compartments have been opened widely. In instances of isolated lower extremity vascular trauma with limited softtissue damage, use of full-dose heparin before and during the vascular reconstruction is often possible. In contrast, patients with lower extremity vascular trauma who also have torso or head injuries or larger, complex soft-tissue wounds are not able to receive systemic heparin. As such, while preferable in all cases, the use of anticoagulation is a judgment call made by the operative surgeon in close communication with the anesthesia, neurosurgical, and other specialty providers. When considering the use of heparin, one should recognize and make use of the benefit of limited amounts of local and regional heparin that can be used on and infused proximal and distal to the segment undergoing repair. Intraluminal platelet aggregate and thrombus must be removed directly using forceps or with a Fogarty thromboembolectomy catheter and diluted amounts of heparin flush. As mentioned, this same dilute heparin should be gently instilled proximal and distal to the controlled vascular segment to reduce the incidence of thrombus formation during assessment and repair. Lower extremity vascular reconstruction generally consists of primary repair, patch angioplasty, or placement of an in-situ interposition graft. Bypass with ligation of the intervening injured segment is another option that may be used with popliteal and tibial level arterial injuries. Regardless of the method, fine monofilament suture and surgical loupe magnification are central to most attempts at vascular reconstruction. Lateral arteriorrhaphy (or venorrhaphy) is a method of primary repair that can be pursued if the vessel diameter will not be narrowed with this approach. In most instances of extremity trauma, this type of lateral wall repair is not possible because the vessels are small by nature. If 50% or more of the vessel wall is uninjured, patch angioplasty using autologous vein or other synthetic material may be an option to allow repair and to prevent narrowing of the lumen. End-to-end anastomosis is another form of primary repair that can be used if the vessel is transected sharply. In order for primary, end-to-end repair to be possible, the vessel must approximate without tension. Because extremity vessels are elastic and frequently spasm and retract in the setting of trauma, it is the exception that the edges will come together in a satisfactory manner. In these cases and in those where a segment of vessel has been transected with a missing segment, performance of an interposition graft is required. Reversed saphenous vein is generally preferred as the conduit in instances where an interposition graft is required. Autologous vein is especially recommended in contaminated cases such as those with an open or penetrating mechanism. Experience from the wars in Afghanistan and Iraq has demonstrated the effectiveness of saphenous vein as the conduit of choice for lower extremity vascular trauma. However, this same experience has highlighted challenges associated with the dismounted complex blast injury pattern that often results in one or more severely mangled lower extremities. In these cases, most if not all of the saphenous vein is injured or absent and therefore is not able to be used as conduit. In these scenarios, creative use of temporary vascular shunts or synthetic conduits has been shown to be effective in the short term and midterm. Seventynine percent of these remained patent long enough to allow the patient to be stabilized and to be evacuated to a level 5 facility in the United States. In many instances, the patient then underwent a more deliberate evaluation, reoperation, and resection of the synthetic conduit in favor of remaining autologous vein.