Buy discount trileptal 150mg
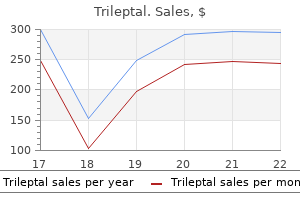
Chemotherapy medications similar to gabapentin purchase 150mg trileptal mastercard, radiation, surgery, and medications can cause disruptions in the cycle of micturition (urination) for many different physiologic reasons. For example, chemotherapy can increase fat deposits and decrease muscle mass, which increase the risk of bowel and bladder dysfunction. External radiation alters tissue viability in the surrounding area, which can affect circulation to the organs and support from muscle, fascia, ligaments, and tendons. Surgery to remove tumors, lymph nodes, or the prostate can affect bladder control through alterations of blood and lymphatic circulation, innervation, and fascial support. Edema secondary to lymphatic system compromise can increase bladder (and bowel) dysfunction. Brain, spinal cord, or pelvic surgery can affect nervous control of the bowel and bladder. Smoking contributes to constipation and is often accompanied by chronic cough, which stresses the bladder. These two findings would suggest there is a protrusion pressing on the spinal cord. Urinary incontinence in middle-aged women may be more closely associated with mechanical factors, such as childbearing, history of urinary tract infections, gynecologic surgery, chronic constipation, obesity, and exertion, than with menopausal transition. However, if incontinence is a new development from the time of the medical evaluation, the physician should be made aware of this information. It may help to introduce the subject by making a general statement such as, "Many men and women have problems with bladder control. If the client answers "yes" to any of these questions, you may want to screen further with the following questions: For Stress Incontinence Do you ever lose urine or wet your pants when you cough, sneeze, or laugh Do you lose urine or wet your pants when getting out of a chair, lifting, or exercising For overactive bladder (urge incontinence) Do you have frequent, strong, or sudden urges to urinate and cannot get to the bathroom in time However, patients/clients with chronic kidney disease leading to kidney failure may receive treatment in both inpatient and outpatient clinics for primary musculoskeletal conditions. Understanding symptoms associated with kidney disease and recognizing complications associated with dialysis shunts are imperative for the therapist. Kidney failure exists when the kidneys can no longer maintain the homeostatic balances within the body that are necessary for life. Acute renal failure refers to the abrupt cessation of kidney activity, usually occurring over a period of hours to a few days. Acute renal failure is often reversible, with return of kidney function in 3 to 12 months. It can develop slowly over a period of years or can result from an episode of acute renal failure that does not resolve. Hereditary defects of the kidneys, polycystic kidneys, and glomerular disorders, such as glomerulonephritis, can also lead to renal failure. In the elderly population, hepatotoxicity is related to drug exposure, polypharmacy and multi-drug interactions. Symptoms tend to be symmetric and more subjective than objective, such as restless legs syndrome, cramps, paresthesias, impaired vibration sense, burning feet syndrome, abnormal Achilles reflex, pruritus (itching of the skin), constipation or diarrhea, abdominal bloating, and decreased sweating. In most cases of renal failure, urine volume is significantly decreased or absent. Renal anemia is usually associated with extreme fatigue and intolerance to normal daily activities, as well as a marked decrease in exercise capacity. Treatment of renal failure involves several elements designed to replace the lost excretory and metabolic functions of this organ. From a screening perspective, the therapist must be alert to the many complications associated with chronic renal failure and dialysis. Watch for signs and symptoms of fluid and electrolyte imbalances (see Chapter 11), dehydration (see Chapter 11), cardiac arrhythmias (see Chapter 6), and depression (see Chapter 3). Cancers of the Urinary Tract Bladder Cancer Bladder cancer is a common, major public health concern that is strongly linked to cigarette smoking. Measures that have been shown to reduce the risk of developing bladder cancer include cessation of smoking, adequate intake of fluids, intake of cruciferous vegetables, limiting exposure to workplace chemicals, and prompt treatment of bladder infections. These symptoms can include blood in the urine, pain in the side that does not go away, a lump or mass in the side or abdomen, weight loss, fever, and general fatigue or feeling of poor health. These hormones control the development of the reproductive organs and other male characteristics such as body and facial hair, low voice, wide shoulders, and sexual function. Testicular cancer is relatively rare, and the average age at the time of diagnosis is 33 years. Additional risk factors include age (half of the all cases occur between the age of 20 and 34 years), race and ethnicity (Caucasian men have about a four to five times greater risk of developing testicular cancer than African American or Asian American men), and body size (several studies have reported that tall men have a somewhat higher risk of testicular cancer). The American Cancer Society states that some physicians recommend monthly self-examination of the testicles after puberty. The self-examination is best performed once each month during or after a warm bath or shower when the heat has relaxed the scrotum (see Appendix D-8 on). If cancer does arise in the second testicle, it is nearly always a new disease rather than metastasis from the first tumor. The most common place for the disease to spread is to the lymph nodes in the posterior part of the abdomen. Therefore low back pain is a frequent symptom of later stage testicular cancer (Case Example 10. If the cancer has spread to the lungs, persistent cough, chest pain, and/or shortness of breath can occur. Survivors of testicular cancer should be checked regularly by their doctors and should continue to perform monthly testicular self-examinations. Outcome even after a secondary testicular cancer is still excellent with early detection and treatment. The most common sign is a hard, painless lump in the testicle about the size of a pea. There may be a dull ache in the scrotum and the man may be aware of tender, larger breasts. Other symptoms are listed in the box Clinical Signs and Symptoms: Testicular Cancer. Pain related to a urinary tract problem can be similar to pain felt from an injury to the back, flank, abdomen, or upper thigh. The physical therapist is advised to question the client further whenever any of the signs and symptoms listed in Table 10. The therapist must ask a few screening questions to bring this kind of information to the forefront. When the physical therapist conducts a Review of Systems, any signs and symptoms associated with renal or urologic impairment should be correlated with the findings of the objective examination and combined with the medical history to provide a comprehensive report at the time of referral to the physician or other health care provider. He was sent to physical therapy by the team physician with a diagnosis of "Sciatica; L4-5 radiculopathy. During examination, the client presented with major losses of lumbar spine range of motion in all planes. There was no observable lateral shift and lumbar lordosis was not excessive or reduced. He was able to lie flat in the prone position and perform a small prone press up without increasing any of his symptoms, but he described feeling a "hard knot in my stomach" while in this position. When asked if he had any symptoms of any kind anywhere else in his body, the client replied that right after the injury, his left testicle swelled up but seemed better now. Even though the therapist thought the clinical findings supported a diagnosis of a derangement syndrome according to the McKenzie classification, there were enough red flags to warrant further investigation. The client was given an appropriate self-treatment program to perform throughout the day with instructions for self-assessment of his condition. Further diagnostic testing revealed testicular cancer as the primary diagnosis, with metastases to the abdomen causing the abdominal mass. Physical therapy was discontinued for back pain, but a new plan of care was established for exercise during cancer treatment.
Purchase trileptal 600 mg
Toxic waste products from the pancreas are released into the intestines causing irritation of the retroperitoneal space medications are administered to generic 600mg trileptal free shipping. The pancreas and low back structures are formed from the same embryologic tissue in the mesoderm. Obstruction, irritation, or inflammation of the body of the pancreas distends the pancreas, thus applying pressure on the central respiratory diaphragm. Melzack R: the McGill pain questionnaire: major properties and scoring methods, Pain 1:277, 1975. Lane P: Assessing pain in patients with advanced dementia, Nursing 34(8):17, 2004. Pola E: Onset of Berger disease after staphylococcus aureus infection: septic arthritis after anterior cruciate ligament reconstruction, Arthroscopy 19(4):E29, 2003. Merskey H, Bogduk N: Classification of chronic pain, ed 2, Seattle, 1994, International Association for the Study of Pain. Waddell G: the back pain revolution, ed 2, Philadelphia, 2004, Churchill Livingstone. Simons D, Travell J: Myofascial pain and dysfunction: the trigger point manual, ed 2, vol. Cooner E, Amorosi S: the study of pain and older Americans, New York, 1997, Louis Harris and Associates (Harris Opinion Poll). Greer S, Chambliss L, Mackler L: What physical exam techniques are useful to detect malingering Pert C: Molecules of emotion: the science behind mind-body medicine, New York, 1998, Simon & Schuster. The doctor, physician assistant, nurse, or nurse practitioner starts with inspection, followed by percussion and palpation, and finally by auscultation. In a screening assessment, the therapist may not need to perform a complete head-to-toe physical assessment. If the initial observations, client history, screening questions, and screening tests are negative, move on to the next step. In most situations, it is advised to assess one system above and below the area of complaint based on evidence supporting a regional-interdependence model of musculoskeletal impairments. For example, a shoulder problem can be caused by a problem in the stomach, heart, liver/biliary, lungs, spleen, kidneys, and ovaries (ectopic pregnancy). More specifically, consider the postmenopausal woman with a primary family history of heart disease who presents with shoulder pain that occurs 3 to 4 minutes after starting an activity and is accompanied by unexplained perspiration. Or think about the 45-year-old mother of five children who presents with scapular pain that is worse after she eats. A cardiac assessment may not be as important as a scan for signs and symptoms associated with the gallbladder or biliary system. Finally, screening and ongoing physical assessment is often a part of an exercise evaluation, especially for the client with one or more serious health concerns. Listening to the heart and lung sounds before initiating an exercise program may bring to light any contraindications to exercise. A compromised cardiopulmonary system may make it impossible and even dangerous for the client to sustain prescribed exercise levels. The use of quick and easy screening tools such as the Physical Therapist Community Screening Form for Aging Adults can help therapists identify limitations to optimal heath, wellness, and fitness in any of seven areas. With the recommendation that all individuals visit a physical therapist at least once a year to promote optimal health and wellness, evidence-based tests of this type will become increasingly available. Keep in mind (as discussed in Chapter 2) that cultural factors may dictate how the client presents himself. A few pieces of equipment in a small kit within easy reach can make the screening examination faster and easier (Box 4. Using the same pattern in screening each time will help the therapist avoid missing important screening clues. As the therapist makes a general survey of each client, it is also possible to evaluate posture, movement patterns and gait, balance, and coordination. For more involved clients the first impression may be based on level of consciousness, respiratory and vascular function, or nutritional status. Physicians may refer to this as iatrogenic delirium, anesthesia-induced dementia, or postoperative delirium. In some cases, delirium/dementia appears to be triggered by the shock to the body from anesthesia and surgery. The likelihood of delirium associated with hospitalization is much higher with hip fractures and hip and knee joint replacements,6,7 possibly attributed to older age, slower metabolism, and polypharmacy (more than four prescribed drugs at admission). Physical examination should include vital signs with oxygen concentration measured, neurologic screening, and surveillance for signs of infection. A medical diagnosis is needed to make the distinction between postoperative delirium, baseline dementia, depression, and withdrawal from drugs and alcohol. For example, inspection of the integument, limb inspection, and screening of the peripheral vascular system is important for someone at risk for lymphedema. Therapists in all settings, especially primary care therapists, can use a screening physical assessment to provide education toward primary prevention, as well as intervention and management of current dysfunctions and disabilities. A healthy individual with normal mental status will be alert, speak coherently, and be aware of the date, day, and time of day. Shock, head injury, stroke, hospitalization, surgery (use of anesthesia), medications, age, and the use of substances and/or alcohol (see discussion, Chapter 2) can cause impaired consciousness. Other factors affecting mental status may include malnutrition, exposure to chemicals, and hypothermia or hyperthermia.
Buy generic trileptal 300mg
Malfunctioning glia are important in the pathophysiology of some primary brain tumors symptoms 10 weeks pregnant order trileptal 600mg line, neurodegenerative diseases, and other neurological conditions. Furthermore, glia-targeting treatments may hold promise in treating a broad range of diseases as well as in facilitating improvement after stroke. Thus, while the developmental, structural, environmental, and repair services of glia hold far less glory than do the lofty functions of neurons, neurons cannot survive and function without glia, just as a theatrical production would grind to a halt without the stage crew and production staff. In this chapter, we learn the cell biology of neurons, glia, and their progenitor cells and then apply this understanding to a range of clinical issues such as brain tumors and neurodegenerative diseases. Immediately surrounding the neural tube is neural crest, which gives rise to most of the peripheral nervous system. Within the primordial head region of the developing embryo, neuroepithelium develops into pre-placodal ectoderm (blue), which eventually populates seven bilateral pairs of placodes (yellow), five of which give rise to sensory neurons associated with cranial nerves. Neural crest cells are motile, and they migrate to specific locations throughout the body and head of the embryo. Placodes, thickenings within the ectodermal layer, are the origin of most peripheral sensory ganglia of the head. Placodes also give rise to several non-neuronal structures such as the lens, sclera, anterior pituitary, and hair cells of the inner ear. In sum, the nervous system derives from three embryonic sources, all of which arise from ectoderm. Neural tube, neural crest, and placodes all also give rise to a number of non-neural tissues, some highly important to nervous system function. For example, patients with Waardenburg syndrome have mutations in genes that regulate neural crest development. These patients present with symptoms that appear unrelated to each other until one realizes that all derive from disruption of normal neural crest development. Predominant symptoms of Waardenburg syndrome include deafness, lack of pigment in areas of the skin and hair, blue eyes, and a facial appearance characterized by wide-set eyes, low hairline, and a uni-brow. Changes in neural crest-directed development of facial bones, muscles, and tendons produce a characteristic facial appearance. Some patients exhibit additional neurological problems such as digestive problems associated with incomplete development of the enteric nervous system. Waardenburg syndrome exemplifies developmental disorders in having an at-first-glance odd but at-second-glance coherent collection of symptoms that are related to each other solely by a shared developmental history. The daughter processes from a parent dendrite are called branches, whereas processes coming off a parent axon are called collaterals. Axons and axon collaterals communicate via synaptic terminals in the form of either bouton endings or varicosities. The appearance of varicosities resembles slightly flattened pearls on a necklace, with the axon being the metaphorical necklace. Neurons may receive an enormous number of synaptic inputs from bouton endings, varicosities, or both, throughout this field or arbor. Although the membranes of pre- and postsynaptic cells come very close to each other at classical synapses, they are separated by a narrow divide called the synaptic cleft. Note that these cartoons are not to scale but are drawn for illustrative purposes. Each of these different cellular regions plays a primary role in a different neuronal function. As is true for all cells in the body, the neuronal soma (somata is the plural) houses the nucleus, endoplasmic reticulum, Golgi apparatus, lysosomes, and other organelles that support cellular life. The rough endoplasmic reticulum in neurons is particularly active, synthesizing large quantities of proteins. Consequently, when stained with basophilic dyes, neuronal rough endoplasmic reticulum stands out prominently as Nissl substance. Staining brain sections for Nissl substance reveals the distribution of neuronal cell bodies and provides an easy and useful picture that can be used to readily identify gross changes or abnormalities in pathological specimens. Dendrites, the primary receiving zone of the neuron, receive the bulk of the input to a neuron. The entirety of the dendritic branches, from large proximal branches to thin distal ones, is called the dendritic tree or dendritic arbor. The dendritic arbor represents the receiving volume for a neuron; only synaptic terminals within the arbor may provide input to the neuron. Some, but not all, neurons have dendrites with a multitude of small protuberances called dendritic spines or simply spines. One common type of spine is knob-like in appearance with a globe-shaped head that is linked to the main dendrite by a very thin process, the neck. Inputs preferentially contact spine heads, which form a subcellular locus for changes associated with many forms of learning. The presynaptic axonal terminals contain synaptic vesicles, filled with neurotransmitter, that are released into the synaptic cleft at synaptic densities (arrows) and bind receptors on the postsynaptic dendrite. Input to the entire dendritic arbor is summed up and electrically conducted toward the soma. All input-strong or weak, fast or slow, excitatory or inhibitory-is integrated across both space (different dendritic branches) and time (see Chapter 10). If the summed electrical signal is sufficient, a neuron may then release neurotransmitter at a synaptic terminal. The bouton and dendrite are in close apposition but separated by a narrow divide called the synaptic cleft (see Box 2-1). In contrast, varicosities participate in what is a far less specific form of communication that is often termed paracrine or volume transmission. Neurotransmitter released from a varicosity may reach any postsynaptic element present within the vicinity. Regardless of the particular morphology, the essence of synaptic communication is the transfer of information from a presynaptic terminal to target, postsynaptic cells. Then, in 1873, Camillo Golgi developed a silver impregnation method, now known as the Golgi stain, which marks cells in their entirety-a great advancement over previously available somatic stains. Only a discernible number of neurons are stained (up to about 5%), enabling stained neurons to be followed and studied against a largely unstained background. Instead of a continuous, reticulated network, Cajal championed the neuron doctrine: Each neuron is an entity unto itself that closely contacts but is not continuous with other neurons. Cajal and Golgi shared the Nobel Prize in Physiology or Medicine in 1906, although Golgi never subscribed to the neuron doctrine; indeed, Golgi used his Nobel Prize lecture to argue, incorrectly, that the brain is one continuous reticulated tissue. This idea, termed the law of dynamic polarization, now accepted as the rule, holds that after traveling down the axon, information crosses over a physical divide to the dendrites and soma of another cell. This point of transfer, the place where two independent neuronal units communicate, is a synapse, a term popularized by Sir Charles Sherrington at the end of the 19th century. More important than popularizing the term "synapse," Sherrington, the first great neurophysiologist and winner of the 1932 Nobel Prize in Physiology or Medicine, recognized the potential of the synapse to integrate excitatory and inhibitory information from multiple sources. However, most neurons transfer electrical signals over long distances, and, for this, an axon is required. The axon, often referred to as a fiber, arises from a point on or close to the soma, and it is at this axon hillock that graded synaptic inputs are "translated" into the language of action potentials, all-or-none electrical potentials that can be propagated over long distances without diminution or failure. Thus, information, in the format of patterned trains of action potentials, travels down an axon to postsynaptic targets. The morphological axon and the physiological action potential are intertwined so that either both are present or both absent. The determining factor in this regard is whether neurons communicate information to distant cells: those that do have axons and action potentials. In contrast, neurons that communicate only within the immediate vicinity of the soma have neither axons nor action potentials. For example, intrinsic retinal neurons send information to nearby cells, and they lack an axon and do not fire action potentials. Axons are unique to neurons; no other cell type has as long processes as do neurons.
Order generic trileptal line
Day 1 is counted as the first day the woman experiences bleeding with her menstrual cycle treatment quadriceps tendonitis generic trileptal 600mg amex. Back pain associated with the menstrual cycle may be a regular feature for a woman, it may occur intermittently, or it may be new onset, and the woman is unaware of the link between the two until she charts her monthly cycle and correlates it with her back pain. A woman may have back pain accompanied by or alternating with sharp, bilateral, and cramping pain in the lower abdominal and/or pelvic quadrants. Tumors, masses, or even endometriosis may involve the sacral plexus or its branches, causing severe, burning pain. Risk Factors Risk factors for prostate dysfunction include advancing age, family history, ethnicity (greater risk for African American men), diet, and possibly exposure to chemicals. Not all disorders of this system occur with aging, so the therapist must remain alert for red-flag symptoms in males of any age. Clinical Presentation Back pain, changes in bladder function, and sexual dysfunction are the most common symptoms associated with male reproductive disorders. Any obstruction, growth, or inflammation of the prostate can directly affect the urethra, resulting in difficulty starting a flow of urine, continuing a flow of urine, frequency, and/or nocturia. Prostate cancer is often asymptomatic and only diagnosed when the man seeks medical assistance because of symptoms of urinary obstruction or sciatica. Sciatic pain affects the low back, hip, and leg and is caused by metastasis to the bones of the pelvis, lumbar spine, or femur. Associated symptoms may include melena, sudden moderate to high fever, chills, and changes in bowel or bladder function. Testicular cancer presents most often as a painless swelling nodule in one gonad, noted incidentally by the client or his sexual partner. This is described as a lump or hardness of the testis, with occasional heaviness or a dull, aching sensation in the lower abdomen or scrotum. Involvement of the epididymis or spermatic cord may lead to pelvic or inguinal lymph node metastasis, although most tumors confined to the testis itself will spread primarily to the retroperitoneal lymph nodes. Subsequent cephalad drainage may be to the thoracic duct and supraclavicular nodes. Hematogenous spread to the lungs, bone, or liver may occur as a result of direct tumor invasion. As discussed earlier, back pain caused by a neoplasm is typically progressive, is more pronounced at night, and may not have a clear association with activity level (as is more characteristic of mechanical back pain). The usual progression of symptoms in clients with cord compression is back pain followed by radicular pain, lower extremity weakness, sensory loss, and finally, loss of sphincter (bowel and bladder) control. Fever in anyone taking immunosuppressants is a red-flag symptom indicating a possible underlying infection. Many people with a spinal infection do not have a fever; they are more likely to have a red-flag history or risk factors. Older children can be affected, although the most common peak is after the third decade of life. Vertebral osteomyelitis is increasingly being reported as a complication of nosocomial bacteremia. Osteomyelitis also can occur after surgery, open fractures, penetrating wounds, skin breakdown and ulcers, and systemic infections. The abscess can advance anteriorly to produce an abscess that can extend to the psoas muscle producing hip pain. The most consistent clinical finding is marked local tenderness over the spinous process of the involved vertebrae with "nonspecific backache. Movement is painful and there is marked muscular guarding and spasm of the paravertebral muscles and the hamstrings. The involved vertebrae are usually exquisitely sensitive to percussion, and pain is more severe at night. A low-grade fever is most common in adults when body temperature changes do occur. Associated Signs and Symptoms Besides changes in urinary patterns, the therapist must ask about discharge from the penis, constitutional symptoms, and pain in any of the nearby soft tissue areas (groin, rectum, scrotum). Is there any blood in the urine (or change in color from yellow to orange or red) Because the therapist is not going to be treating any of these problems, any red flags should be reported to the physician. Many men are reluctant to pursue diagnosis and treatment whenever the male reproductive system is involved. Screening questions for men are a good way to elicit red-flag history, risk factors, and signs or symptoms. The therapist must follow-up with the client and make sure contact is made with the appropriate health care professional. Acute hematogenous osteomyelitis seen in children usually originates in the metaphysis of a long bone. The pain is most commonly severe enough to limit or restrict the use of the involved extremity, and fever and malaise consistent with sepsis are usual. When questioned about past medical history, the client reported a prostatectomy 22 years ago with no further problems. He was not aware of any other associated signs and symptoms but reported a recurring dermatitis that was being treated by his nurse practitioner. Clinical Presentation: the examination revealed spasm of the thoracolumbosacral paraspinal muscles bilaterally. The client reported extreme sensitivity to palpation of the spinous processes at L3 and L4; tap test reproduced painful symptoms. Hip flexion and extension reproduced the symptoms and produced additional radiating flank pain. The prescribed treatment was intravenous antibiotic therapy for 6 weeks, progressive mobilization, and a spinal brace to be provided and fitted by the physical therapist. Septic diskitis may occur following various invasive procedures, or it may be related to occult infections, urinary tract infections, septicemia, and dermatitis. Symptoms associated with postoperative disk space infection occur 2 to 8 weeks after diskectomy. Ask the parent, guardian, or caretaker of any young child with back pain if there has been a recent history of sore throat, cold, ear infection, or other upper respiratory illness. The pain can range from mild to "excruciating" and sometimes is described as "knife-like. The pain is usually made worse by activity, but unlike most other causes of back pain, it is not relieved by rest. If the condition becomes chronic, pain may radiate into the abdomen, pelvis, and lower extremities. Children present with a history of increasingly severe localized back pain often accompanied by a limp or refusal to walk. Physical examination may reveal localized tenderness over the involved disk space, paraspinal muscle spasm, and restricted lumbar motion. Half of these clients will have only musculoskeletal symptoms, without other signs of endocarditis. The early onset of joint pain and myalgia is more likely if the client is older and has had a previously diagnosed heart murmur or prosthetic valve (risk factors). Other risk factors include injection drug use, previous cardiac surgery, recent dental work, and recent history of invasive diagnostic procedures. The therapist can review history and risk factors and conduct a Review of Systems to help in the screening process. Guidelines for Immediate Medical Attention Immediate medical referral is not always required when a client presents with any one of the red flags listed in Box 14. When viewed as a whole, the history, risk factors, and any cluster of red-flag findings will guide the therapist in making a final intervention versus referral decision. Acute mechanical compression of nerves in the lower extremities, bowel, and bladder as they pass through the caudal sac may be a surgical emergency. Sudden change in blood pressure, pallor, pain, and dizziness will alert the therapist to the need for immediate medical attention. As many as 90% of affected individuals resume normal activity levels during this time.
Buy trileptal with a visa
This is especially true for clients with back pain or multiple joint pain without traumatic origin symptoms exhaustion discount 300mg trileptal with amex. If a change in position can increase or decrease the level of pain, it is likely to be a musculoskeletal problem. If, however, the client is awakened from a deep sleep by pain in any location that is unrelated to physical trauma and is unaffected by a change in position, this may be an ominous sign of serious systemic disease, particularly cancer. Stress (see also Chapter 3) By using the interviewing tools and techniques described in this chapter, the therapist can communicate a willingness to consider all aspects of illness, whether biologic or psychologic. Client self-disclosure is unlikely if there is no trust in the health professional, if there is fear of a lack of confidentiality, or if a sense of disinterest is noted. Most symptoms (pain included) are aggravated by unresolved emotional or psychologic stress. Stress may result in depression, anxiety disorders, and behavioral consequences. The effects of emotional stress may be increased by physiologic changes brought on by the use of medications or poor diet and health habits. If you have not asked any questions about assault or partner abuse, this may be the appropriate time to screen for domestic violence. These emotions may cause autonomic (branch of nervous system not subject to voluntary control) distress manifested in such symptoms as pallor, restlessness, muscular tension, perspiration, stomach pain, diarrhea or constipation, or headaches. It may be helpful to screen for anxiety-provoked hyperventilation by asking: Special Questions for Women Gynecologic disorders can refer pain to the low back, hip, pelvis, groin, or sacroiliac joint. Any woman having pain or symptoms in any one or more of these areas should be screened for possible systemic diseases. The need to screen for systemic disease is essential when there is no known cause of the pain or symptoms. Chapter 14 has a list of special questions to ask women (see also Appendix B-37 on). After the objective evaluation has been completed, the therapist can often provide some relief of emotionally amplified symptoms by explaining the cause of pain, outlining a plan of care, and providing a realistic prognosis for improvement. This may not be possible if the client demonstrates signs of hysterical symptoms or conversion symptoms (see discussion in Chapter 3). Special Questions for Men Men describing symptoms related to the groin, low back, hip, or sacroiliac joint may have prostate or urologic involvement. A positive response to any or all of the questions in Appendix B-24 on must be evaluated further. Answers to these questions correlated with family history, the presence of risk factors, clinical presentation, and any red flags will guide the therapist in making a decision regarding treatment versus referral. A careful review of the medical record for information will assist the therapist in developing a safe and effective plan of care. Use the answers from the Core Interview to recall specifics about the location, frequency, intensity, and duration of the symptoms. Recap the medical and surgical history including current illnesses, diseases, or other medical conditions; recent or past surgeries; recent or current medications; recent infections; and anything else of importance brought out by the interview process. Fluid received during surgery may affect arterial oxygenation, leaving the person breathless with minimal exertion and experiencing early muscle fatigue. Prolonged time in any one position can result in residual musculoskeletal complaints. The surgical position for men and for women during laparoscopy (examination of the peritoneal cavity) may place patients at increased risk for thrombophlebitis because of the decreased blood flow to the legs during surgery. Associated or additional problems to the primary diagnosis may be found within the record. Avoiding peak insulin levels in planning exercise schedules is discussed more completely in Chapter 11. Anemic patients may demonstrate an increased normal resting pulse rate that should be monitored during exercise. Patients with unstable blood pressure may require initial standing with a tilt table or monitoring of the blood pressure before, during, and after treatment. The questions to ask and factors to consider provide the therapist with the basic information needed to carry out appropriate physical examination procedures and to plan the intervention. In other words, does the patient know the date and the approximate time, where he or she is, and who he or she is For example, consider the client with a chief complaint of back pain who circles "yes" on the Family/Personal History form, indicating a history of ulcers or stomach problems. Obtaining further information at the first appointment by using Special Questions to Ask is necessary so that a decision regarding treatment or referral can be made immediately. This treatment-versus-referral decision is further clarified as the interview, and other objective evaluation procedures, continue. This information is not designed to make a medical diagnosis but rather to perform an accurate assessment of pain and systemic symptoms that can mimic or occur simultaneously with a musculoskeletal problem. The therapist can use the decision-making tools discussed in Chapter 1 (see Box 1. The therapist is screening to make sure that the client does indeed have a primary problem that is within the scope of a physical therapist practice. The screening steps begin with the client interview, but screening does not end there. This is especially true when progression of disease results in a changing clinical presentation, perhaps with the onset of new symptoms or new red flags after the treatment intervention has been initiated. Most of the information needed to determine the cause of symptoms is contained within the subjective assessment (interview process). The Family/Personal History form can be used as the first tool to screen clients for medical disease. The therapist is strongly encouraged to review the form with the client, entering the date and his or her own initials. Screening examinations (interview and vital signs) should be completed for any person experiencing back, shoulder, scapular, hip, groin, or sacroiliac symptoms of unknown cause. It may be necessary to explain the need to ask such detailed questions about organ systems seemingly unrelated to the musculoskeletal symptoms. Not every question provided in the lists offered in this text needs to be asked; the therapist can scan the lists and ask the appropriate questions based on the individual circumstances. When screening for domestic violence, sexual dysfunction, incontinence, or other conditions, it is important to explain that a standard set of questions is asked and that some may not apply. With the older client, a limited number of presenting symptoms often predominate-no matter what the underlying disease is-including acute confusion, depression, falling, incontinence, and syncope. A recent history of any infection (bladder, uterine, kidney, vaginal, upper respiratory), mononucleosis, influenza, or colds may be an extension of a chronic health pattern or systemic illness. The use of fluoroquinolones (antibiotic) has been linked with tendinopathies, especially in older adults who are also taking corticosteroids. Reports of dizziness, loss of balance, or a history of falls require further screening, especially in the presence of other neurologic signs and symptoms such as headache, confusion, depression, irritability, visual changes, weakness, memory loss, and drowsiness or lethargy. Consider the possibility of physical/sexual assault or abuse in anyone with an unknown cause of symptoms, clients who take much longer to heal than expected, or any combination of physical, social, or psychologic cues listed. In screening for systemic origin of symptoms, review the patient history and interview in light of the physical examination findings. The client was examined by numerous physicians, including an orthopedic specialist.
Eriodictiol (Lemon). Trileptal.
- How does Lemon work?
- Treating scurvy (as a source of vitamin C), the common cold and flu, kidney stones, decreasing swelling, and increasing urine.
- Are there safety concerns?
- Dosing considerations for Lemon.
- What is Lemon?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96546
Purchase 600mg trileptal amex
Fifty percent of clients with back pain from a malignancy have an identifiable preceding trauma or injury to account for the pain or symptoms symptoms umbilical hernia buy trileptal. Back pain may precede the development of neurologic signs and symptoms in any person with cancer. The presence of jaundice in association with any atypical presentation of back pain may indicate liver metastasis. Signs of nerve root compression may be the first indication of cancer, in particular, lymphoma, multiple myeloma, or cancer of the lung, breast, prostate, or kidney. The five most common sites of metastasis are the lymph nodes, liver, lung, bone, and brain. Lung, breast, prostate, thyroid, and the lymphatics are the primary sites responsible for most metastatic bone disease. Watch closely for early signs (dyspnea, pallor, sweating, and fatigue) of cardiopulmonary complications of cancer treatment. No reliable physical signs distinguish between benign and malignant soft tissue lesions. All soft tissue lumps that persist or grow should be reported immediately to the physician. The case study provided here is one example of how to follow up with necessary questions to rule out a systemic origin of musculoskeletal findings. A previous history of drug therapy and current drug use may be important information to obtain because prolonged use of drugs such as phenytoin (Dilantin) or immunosuppressive drugs such as azathioprine (Imuran) and cyclosporine may lead to cancer. If no, have you ever received chemotherapy, hormone therapy, or radiation therapy If yes to previous history of cancer, ask about type of cancer, date of diagnosis, stage (if known), treatment, and date of most recent follow-up visit with oncologist or other cancer specialist. Have you had a chronic cough, recurrent laryngitis, hoarseness, or any difficulty with speaking Can you think of any time during the past week when you may have bumped yourself, fallen, or injured yourself in any way Bone pain from systemic causes usually feels dull and deep and is unrelated to movement. He is seeking an evaluation on the insistence of his wife, who has noticed that his collar size has increased two sizes in the last year and that his neck looks "puffy. An appropriate lead-in to the following series of questions may be: "Because you have not seen a physician before your appointment with me, I will ask you a series of questions to find out if your symptoms require examination by a physician rather than treatment in this office. Do you have recurrent hoarseness, flu-like symptoms, or a persistent cough or cold that never seems to go away Perform a brief posture screen (general postural observations may be made while you are interviewing the client). Assess for compromise of the vertebral artery, and if negative, clear the cervical spine by using a quadrant test with overpressure. Palpate the anterior cervical spine for pathologic protrusion while the client swallows. Ask about the presence of recent change in vision, headache, numbness, or tingling into the jaw or down the arm(s). It is always recommended that the therapist give the client ongoing verbal feedback during the examination regarding evaluation results, such as: "I notice you cannot turn your head to the right as much as you can to the left-from checking your muscles and joints, it looks like muscle tightness, not any loss of joint movement. Give the client a brief summary of your findings while making your recommendations, for example, "Mr. X, I noticed today that although you do not have any ongoing neck pain, the lymph nodes in your neck and armpit are enlarged but not particularly tender. Your loss of motion while turning your head is not unusual for a person your age and certainly would not cause your neck to increase in size or shape. Given the fact that you have not seen a physician for almost 3 years, I strongly recommend that you see a physician of your choice, or I can give you the names of several to choose from. In either case, I think some medical tests are necessary to rule out any underlying medical problem. For instance, a neck x-ray examination would be recommended before physical therapy treatment is started. If the client does give the name of a physician, you may ask for written permission (disclosure release) to send a copy of your results to the physician. If you think that a problem may be potentially serious and you want this person to receive adequate follow-up without causing alarm, you may offer to let him make the appointment from your office, suggest that your secretary or receptionist make the appointment for him, or even offer to make the initial telephone contact yourself. Medical intervention was initiated and physical therapy treatment was not warranted. Name three predisposing factors to cancer that the therapist must watch for during the interview process as red flags. How do you monitor exercise levels in the oncology patient without laboratory values Whenever a therapist observes, palpates, or receives a client report of a lump or nodule, what three questions must be asked Give a general description and explanation of the changes seen in deep tendon reflexes associated with cancer. In a physical therapy practice, clients are most likely to present with signs and symptoms of metastases to the: a. When tumors produce signs and symptoms at a site distant from the tumor or its metastasized sites, these "remote effects" of malignancy are called: a. A client who has recently completed chemotherapy requires immediate medical referral if he has which of the following symptoms Fever, chills, sweating A suspicious skin lesion requiring medical evaluation has: a. He presents with exquisite right ankle pain while weight-bearing but reports no pain at night. Upon further questioning, you find he is taking ibuprofen at night before bed, which may be masking his pain. Assess for signs of fracture (edema, exquisite tenderness to palpation, warmth over the painful site). Anyone presenting with joint pain of unknown cause accompanied by multiple other signs and symptoms d. He saw his family doctor 4 weeks ago and was given diclofenac, which has not changed his symptoms. Since he last saw his physician, he has developed additional joint pain in the left knee and right shoulder. He also reports problems with his bowels but is not able to tell you exactly what is wrong. He is not taking any medications or over-the-counter drugs and does not want to see a doctor. Are there enough red flags to warrant medical evaluation before resumption of physical therapy intervention No; treatment was effective before-it is likely that he has done something to exacerbate his symptoms and needs further education about joint protection. A client with a past medical history of kidney transplantation (10 years ago) has been referred to you for a diagnosis of rheumatoid arthritis. During the examination, you notice a painless lump under the skin in the right upper anterior chest. What other symptoms should you look for as red-flag signs and symptoms in a client with this history A 55-year-old man with a left shoulder impingement also has palpable axillary lymph nodes on both sides.
Syndromes
- Swollen lymph nodes, especially in the neck and armpit
- Have you had radiation therapy or chemotherapy?
- Laxative
- Poor blood supply
- Do you feel dizzy or light-headed when standing or sitting after lying down?
- Signs of poor circulation in the hand or forearm (a bluish color, cold hands, or a swollen arm)
- Sore throat that does not get better in 1 - 2 weeks, even with antibiotics
Generic trileptal 150 mg without prescription
Are there any clusters or groups of signs and symptoms that fall into any particular category These may or may not be associated with the primary neuromusculoskeletal problem as many clients have one or more other diseases symptoms of pneumonia purchase 600mg trileptal with mastercard, illnesses, or conditions (referred to as comorbidities) with additional clinical manifestations. Client reports: Hearing and vision loss Intermittent dizziness Early morning nausea Finger/hand swelling Sleep disturbance There is not much in the report about her general health. Make a note to consider asking a few more questions about her past and current general health. The remaining symptoms noted (positive Trendelenburg gait and antalgic gait, left shoulder and knee pain) fall into the musculoskeletal category. Are there isolated groupings or clusters of signs and symptoms that fall into any of the other three diagnostic categories Documentation, communication, and medical referral will be based on the results of your evaluation using a review mechanism like the one we just completed. Diverticular Disease the terms diverticulosis and diverticulitis are used interchangeably although they have distinct meanings. Diverticulosis is a benign condition in which the mucosa (lining) of the colon balloons out through weakened areas in the wall. Someone with diverticulosis is typically asymptomatic; the diverticula are diagnosed when screening for colon cancer or other problems. Diverticulosis is very common, whereas complications resulting in diverticulitis occur in only 10% to 25% of people with diverticulosis. The diagnosis of diverticulitis is confirmed by accompanying fever, bloody stools, elevated white blood cell count, and imaging studies. She had been referred to physical therapy with the provisional diagnosis: Possible right oblique abdominis muscle tear/possible right iliopsoas muscle tear. Her history included the sudden onset of "severe pain" in the right lower quadrant with accompanying nausea and abdominal distention. Aggravating factors included hip flexion, sit-ups, fast walking, and movements such as reaching, turning, and bending. Painful symptoms could be reproduced by resisted hip or trunk flexion, and tenderness/tightness was elicited on palpation of the right iliopsoas muscle compared with the left. Screening questions for general health revealed constitutional symptoms, including fatigue, night sweats, nausea, and repeated episodes of severe, progressive pain in the right lower abdominal quadrant. Although she presented with a musculoskeletal pattern of symptoms at the time of her initial evaluation with the physician, by the time she entered the physical therapy clinic her symptoms had taken on a definite systemic pattern. She was returned for further medical follow-up, and a diagnosis of appendicitis complicated by peritonitis was established. This client recovered fully from all her symptoms following an emergency appendectomy. When the appendix becomes obstructed, inflamed, and infected, rupture may occur, leading to peritonitis. Clinical Signs and Symptoms the classic symptoms of appendicitis are pain preceding nausea and vomiting and low-grade fever in adults. The pain usually begins in the umbilical region and eventually localizes in the right lower quadrant of the abdomen over the site of the appendix. Groin and/or testicular pain may be the only symptoms of appendicitis, especially in young, healthy, male athletes. The pain comes in waves, becomes steady, and is aggravated by movement, causing the client to bend over and tense the abdominal muscles or to lie down and draw the legs up to relieve abdominal muscle tension (Case Example 8. Generalized peritonitis, whether caused by appendicitis or some other abdominal or pelvic inflammatory condition, can result in a "board-like" abdomen because of the spasm of the rectus abdominis muscles. Lean muscle mass deteriorates with aging, especially evident in the abdominal muscles of the aging population. The very old person may not present with this classic sign of generalized peritonitis because of the lack of toned abdominal muscles. In 50% of cases the appendix is retrocecal (behind the cecum) or retrocolic (behind the colon). Because the appendix develops at the descent of the colon, its final position can be posterior to the cecum or colon. These positions of the appendix are called retrocecal or retrocolic, respectively. If the individual has increased pain when the skin fold strikes the peritoneum (upon release of the skin), the test is positive for possible peritonitis. If the person being tested reacts to the pinch in an excessive fashion, he or she may have a very low pain threshold, a factor that should be taken into consideration when assessing the results. A, To assess for appendicitis or generalized peritonitis, press your fingers gently but deeply over the right lower quadrant for 15 to 30 seconds. Pain induced or increased by quick withdrawal results from rapid movement of inflamed peritoneum and is called rebound tenderness. When rebound tenderness is present, the client will have pain or increased pain on the side of the inflammation when the palpatory pressure is released. Because abdominal pain is increased uncomfortably with this test, save it for last when assessing abdominal pain during the physical examination. A positive pinch-an-inch test, or alternately, rebound tenderness, may occur with any disease or condition affecting the peritoneum (including appendicitis when it has progressed to include peritonitis). Clinical Signs and Symptoms the clinical course of most clients with acute pancreatitis follows a self-limited pattern. Symptoms can vary from mild, nonspecific abdominal pain to profound shock with coma and possible death. Abdominal pain begins abruptly in the midepigastrium, increases in intensity for several hours, and can last from days to more than a week. Pain is made worse by walking and lying supine and is relieved by sitting and leaning forward. The client may have a bluish discoloration of the periumbilical area (Cullen sign)63 as a physical manifestation of acute pancreatitis. Pathology of the head of the pancreas is more likely to cause epigastric and midthoracic pain from T5 to T9. Nausea, vomiting, weight loss, oily or fatty stools, and clay-colored or pale stools are common symptoms of chronic pancreatitis. In clients with alcohol-associated pancreatitis, the pain often begins 12 to 48 hours after an Pancreatitis Pancreatitis is an inflammation of the pancreas that may result in autodigestion of the pancreas by its own enzymes. Pancreatitis can be acute or chronic, but the therapist is most likely to see individuals with referred pain patterns associated with acute pancreatitis. Acute pancreatitis can arise from a variety of etiologic (risk) factors including, but not limited to , anatomic or functional disorders, autoimmune conditions. Chronic pancreatitis is caused by longstanding alcohol abuse, with a four-fold increase in the prevalence of pancreatitis among those with a history of alcoholism compared with those with negative history of the condition. Radiation of pain into the lumbar region is sometimes the only symptom of the disease. Sitting up and leaning forward may provide some relief, and this usually indicates that the lesion has spread beyond the pancreas and is inoperable. Other signs and symptoms include light-colored stools, constipation, nausea, vomiting, loss of appetite, weight loss, and weakness. Clients with gallstone-associated pancreatitis typically experience pain after a large meal. Manifestations involve the joints most commonly (see previous discussion of arthralgia earlier in this chapter under Arthralgia). Clinical Signs and Symptoms the clinical features of pancreatic cancer initially are nonspecific and vague, contributing to a delay in diagnosis and high mortality. Symptoms do not usually appear until the tumor obstructs nearby bile ducts or grows large enough to cause abdominal pressure or pain. The most common symptoms of pancreatic cancer are anorexia and weight loss, midepigastric pain sometimes with radiation to the midlower back region, and painless jaundice secondary to obstruction of the bile duct. The use of prednisone decreases vitamin D metabolism, impairs calcium absorption, decreases potassium supplies, and increases the nutritional requirement for protein and calories. Decreased vitamin D metabolism and impaired calcium absorption subsequently result in bone demineralization and osteoporosis.
Purchase trileptal 600mg
The orthopedic examination was consistent with a total hip replacement 6 months ago medications used for fibromyalgia purchase trileptal 150mg on line, with mild hip flexor weakness and mild loss of hip motion on the left (compared with the right). Muscle tone was increased in the lower extremities, with proprioception and deep tendon reflexes decreased in both feet (right more than left). Result: Given the history of a progressive gait disturbance, new onset of urge incontinence, and positive findings on a neurologic screening examination, this client was referred to her family physician for a medical evaluation. Basilar impression is the term used when the odontoid peg of C2 pushes up into the foramen magnum. The subsequent dislocation of the atlas on the axis can remain mobile, producing intermittent problems, or it can become fixed, producing persistent symptoms. Symmetrical shoulder girdle pain and stiffness is the most common symptom, reported in 70% to 95% of patients. Joint pain is possible, and headache, weakness, and fatigue are commonly reported. The ophthalmic arteries are affected in nearly half of all affected individuals, sometimes resulting in partial loss of vision or even sudden blindness. The client reports that she had 1 or 2 days of fever and flu-like symptoms associated with neck stiffness. The problem did not go away after the fever passed, and the symptoms gradually worsened. A month later, both shoulders were particularly worse in the morning when she was waking up. Symptoms were persisting and also waking her up at night when she was trying to change positions. She saw her primary care physician for an annual physical but did not put much emphasis on these symptoms. She again got in touch with her doctor, who referred her to physical therapy for evaluation of shoulder girdle pain. Her father had a stroke in 1991, which left him aphasic; he has hypertension and a history of coronary artery disease with coronary artery bypass graft surgery in 1975. Her desired outcome is to decrease the pain and stiffness in the shoulder area and get back to her full activities. Current medications included atenolol/chlorthalidone 50/25 daily for blood pressure management; potassium 10 mEq/L daily; aspirin 81 mg daily; calcium 1000 mg daily. The client routinely exercises using the treadmill and performs aerobic exercises three times per week. Pain: Using a Visual Analog Scale, from 0 (no pain) to 10 (worst pain imaginable), pain was rated as 8/10 in the shoulder girdle area. Posture: Mild kyphosis and a mild forward head (possible sign of osteoporosis), but otherwise unremarkable. Work, community, and leisure: Client has reported she has had difficulty getting out of bed in the morning and difficulty with sleep because it is very painful when she changes positions at night. Because of her prednisone use and the fact that she is postmenopausal, attention to management of the potential for osteoporosis must be included in the treatment plan. Even though the client was seen by the physician before referral to physical therapy, there were enough red flags to warrant consultation before beginning physical therapy intervention. Lupus can occur at any age, but it is most common in persons between the ages of 15 and 40 years; it rarely occurs in older people. Women are affected 10 to 15 times more often than men, possibly because of hormones, but the exact relationship remains unknown. Clients may differ dramatically in the relative severity and pattern of organ involvement. Common organ involvement includes cutaneous lupus, polyarthritis, nephritis, and hematologic lupus. Facial involvement is usually symmetric, and the nasolabial folds and upper eyelids are typically spared. Skin rash can also appear over the extensor surfaces of the arms, forearms, and hands/fingers. The hair may start to thin, causing an unkempt appearance referred to as lupus hair. Acute migratory or persistent nonerosive arthritis may involve any joint, but typically the small joints of the hands, wrists, and knees are symmetrically involved. One-fourth of all persons with lupus develop progressive musculoskeletal damage with deforming arthritis, osteoporosis with fracture and vertebral collapse, and osteomyelitis. Peripheral neuropathy may be motor, sensory (stocking-glove distribution), or mixed motor and sensory polyneuropathy. These may develop subacutely in the lower extremities and progress to the upper extremities. Oral corticosteroids (especially prednisone) are used to suppress the inflammation, treat the symptoms, and provide remission, but do not cure the illness. It is known to be a chronic, systemic, inflammatory disease characterized by injury to the skin, joints, kidneys, heart and blood-forming organs, nervous system, and mucous membranes. Lupus comes from the Latin word for wolf, referring to the belief in the 1800s that the rash of this disease was caused by a wolf bite. The characteristic rash of lupus (especially a butterfly rash across the cheeks and nose) is red, leading to the term erythematosus. In others, the joints, lungs, kidneys, blood, or other organs or tissues may be affected. I put weight on my right leg and felt my hip joint slip in the back with immediate pain, and I was unable to put any weight on that leg. I moved my hip around in the socket and was able to get immediate relief from the pain, but it felt like it could catch at any time. Muscle weakness 2 years ago resulted in a muscle biopsy and a diagnosis of "abnormal" muscle tissue of unknown cause. The client developed a staph infection from the biopsy, which resolved very slowly. Other past medical history included a motor vehicle accident 2 years ago, at which time her knees went through the dashboard, which left both knees "numb" for a year after the accident. Clinical Presentation: Aggravating and relieving factors from this visit fit a musculoskeletal pattern of symptoms, and objective examination was consistent with lumbar/sacroiliac mechanical dysfunction with a multitude of other compounding factors, including bilateral posterior cruciate ligament laxity, poor posture, obesity, and emotional lability. Physical therapy treatment was initiated, but a week later, when the client woke up at night to go to the bathroom, she swung her legs over the edge of her bed and experienced immediate hip and diffuse low back pain and lower extremity weakness. She went to the emergency department by ambulance and later was admitted to the hospital. She was evaluated by a neurologist (results unknown), recovered from her symptoms within 24 hours, and was released after a 3-day hospitalization. She was directed by her primary care physician to continue outpatient physical therapy services. Within 2 weeks, she experienced another middle-of-the-night acute exacerbation of symptoms. This case example is included to point out the complexity of treating a musculoskeletal condition in a client with a longterm chronic inflammatory disease process requiring years of steroidal antiinflammatory medications. Before including any resistive exercises, muscle energy techniques, or joint or selfmobilization techniques, the therapist must be aware of any clinically significant changes in bone density and the presence of developing osteoporosis. The most common symptoms associated with lupus are listed here in order of declining prevalence. Medical providers account for the clinical signs previously mentioned and interpretations of laboratory tests in the diagnostic process. Touch, vibration, and position sense are most prominently affected, and the distal limb reflexes are depressed (Case Example 12. Late scleroderma is characterized by muscle atrophy, muscle weakness, deconditioning, and flexion contractures. Similar changes occur in the small intestine, resulting in reduced motility and causing intermittent diarrhea, bloating, cramping, malabsorption, and weight loss. Inflammation and fibrosis can also affect the lungs, resulting in interstitial lung disease, a restrictive lung disease.
Buy trileptal 600 mg low cost
She had a history of uterine cancer 20 years ago and a history of breast cancer 10 years ago medications bad for your liver cheap trileptal 150mg with amex. Her family physician, oncologist, and neurologist all evaluated her before she was referred to the physical therapist. Examination by a physical therapist revealed obvious lymphadenopathy of the left cervical and axillary lymph nodes. The question for us as physical therapists in a situation like this one is how to proceed Second, the therapist must ascertain whether or not the physician is already aware of the problem and has requested physical therapy as a palliative measure. Contact with the physician will be important soon after the records are obtained, either to confirm the request as palliative therapy or to report your findings and confirm the need for medical reevaluation. If it turns out that the physician is, indeed, unaware of these physical findings, it is best to send a problem list identified as "outside the scope of a physical therapist" when returning the client to the physician. Lumps, Lesions, and Lymph Nodes the therapist should take special note of "T," which is thickening or lump in breast or elsewhere. Clients often point out a subcutaneous lesion (often a benign lipoma) and ask us to identify what it is. It can also be observed functionally when the client has difficulty getting up from sitting or climbing stairs. As the weakness progresses, the client may have trouble getting into and out of a vehicle and/or the bathtub. Respiratory muscle weakness may be seen as shortness of breath or reported as altered activity to avoid dyspnea. When making the medical referral, look for a cluster of signs and symptoms, recent trauma (including recent biopsy), or a past history of chronic fatigue syndrome, mononucleosis, and allergies. This syndrome of proximal muscle weakness is referred to as carcinomatous neuromyopathy. The most common neuromuscular manifestation is difficulty walking or going up stairs. It is accompanied by changes in two or more deep tendon reflexes (ankle jerk usually remains intact). Muscle weakness may occur secondary to cachexia, nonspecific effects of the neoplasm, or hypercalcemia, which occurs as an indirect humoral effect on bone (see the later discussion on Paraneoplastic Syndrome in this chapter). Clients with advanced cancer, multiple myeloma, or breast or lung cancer are affected most often by hypercalcemia. Sometimes questions must be directed toward function to find out this information. If a client is asked whether he or she has any muscle weakness, difficulty getting up from sitting, trouble climbing stairs, or shortness of breath, the answer may very well be "No" on all accounts. Pain Pain is rarely an early warning sign of cancer, even in the presence of unexplained bleeding. The lesion, or lesions, must be of significant size or location to create pressure and/or occlusion of normal structures; pain will be dependent on the area of the body affected. Acute and chronic cancer-related pain syndromes can occur in association with diagnostic and therapeutic interventions such as bone marrow biopsy, lumbar puncture, colonoscopy, percutaneous biopsy, and thoracentesis. Chemotherapy and radiation toxicity can result in painful peripheral neuropathies. Some individuals have very brisk reflexes under normal circumstances; others are much more hyporeflexive. Tumors (whether benign or malignant) can also press on the spinal nerve root, mimicking a disk problem. A large tumor can obliterate the reflex arc, resulting in diminished or absent reflexes. For example, a hyporesponsive patellar tendon reflex that is unchanged with distraction or repeated testing and is accompanied by back, hip, or thigh pain, along with a past history of prostate cancer, presents a different clinical picture altogether. She had just had her 6-month cancer check-up and was not scheduled to see her oncologist for another 6 months. When asked if there were any other symptoms present, she reported feeling feverish and a bit nauseous, and noted slight muscle aching. She was not aware of an elevated body temperature, although she stated she had awakened in the night feeling feverish and took some Tylenol. Upper quadrant examination was unremarkable, except for skin rash and the presence of bilateral anterior cervical adenopathy. There was a fullness of lymph node tissue without firmness or distinct nodes palpated in the axilla on the involved side. Results: this client had three red flags: recent history of cancer, skin rash, and a constitutional symptom (fever). Even though there was no external sign of local cancer recurrence and even though she was just seen by her oncologist, these new findings warranted a return visit to her physician. She was followed more closely for any cancer recurrence with more frequent testing thereafter. Integumentary Manifestations Internal cancers can invade the skin through vascular dissemination or direct extension. Metastases to the skin may be the first sign of malignancy, especially for breast or upper respiratory tract cancer. Integumentary carcinomatous metastases often present as asymmetrical, firm, skin-colored, red, purple, or blue nodules near the site of the primary tumor. The integumentary screening examination, including the assessment of common skin lesions and the nail beds, is presented in Chapter 4. During observation and inspection the therapist should be alert to any potential signs of primary skin cancer or integumentary metastases. The therapist may want to introduce the subject by saying that as health care professionals, we are trained to observe many body parts (skin, joints, posture, and so on). You notice that the client has an unusual mole (or rash or whatever has been observed), and you wonder whether this is something that has been there for years. A client with a past medical history of cancer now presenting with a suspicious skin lesion that has not been evaluated by a physician must be advised to have it evaluated as soon as possible. For any client with a previous history of cancer with surgical removal, it is always a good idea to look at the surgical site(s) for any sign of local cancer recurrence. They rarely metastasize to other parts of the body and have a nearly 100% rate of cure. Melanoma, the most serious of the skin cancers, has a 98% 5-year survival rate if localized, but only a 17% 5-year survival if it is invasive or has spread to other parts of the body. The primary warning sign for melanoma is a flat, colored, irregularly shaped lesion that can be mottled with light brown to black colors. It may turn various shades of red, blue, or white or crust on the surface and bleed. A changing mole, the appearance of a new mole, or a mole that is different or growing requires prompt medical attention. With actinic keratosis, overexposure to sunlight results in abnormal cell growth, causing a well-defined, crusty patch or bump on sun-exposed parts of the body. Clients often point out skin lesions or ask the therapist about various lumps and bumps. In addition, the therapist may observe changes in skin, skin lesions, or aberrant tissue during the visual inspection and palpation portion of the examination (see Chapter 4) that need further medical investigation. The therapist has a responsibility to report these findings to the appropriate health care professional and to make every effort to ensure client compliance with follow-up. Red, tender papules, plaques, or nodules appear on the face, extremities, and upper trunk. Most cases are idiopathic, associated with inflammatory bowel disease, or preceding upper respiratory tract infection, but some have been associated with malignancy.