Order 30 mg vytorin amex
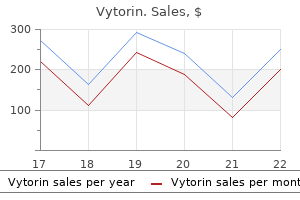
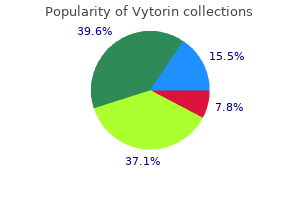
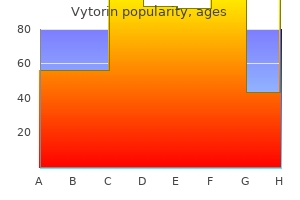
Keywords: buccal defects cholesterol quantitation kit buy vytorin 30mg line, oral vestibular reconstruction the arterial supply of the buccal regions is derived from the buccal branch of the internal maxillary artery as well as the facial artery. Sensory innervation is supplied by branches of the maxillary and mandibular branches of the trigeminal nerve. The parotid duct exits from the anterior aspect of the parotid gland and courses superficial to the masseter muscle. In simple terms, the buccal mucosa serves as a passive barrier that helps enclose the oral cavity and, in conjunction with the action of the lips, prevents leakage of saliva and other oral contents. The ability to seal the oral cavity is also necessary to generate a positive air pressure gradient for plosive speech and a negative pressure gradient for sucking. The muscles of facial expression, in addition to accomplishing their namesake, are involved in the transit of food during mastication and deglutition. Facial reanimation, as it pertains to the buccal region, is therefore an important consideration for reconstruction of buccal defects that involve the facial musculature and nerve branches. Specific techniques for facial reanimation, however, are beyond the scope of this chapter. One of the most common functional consequences of surgical resection and reconstruction for buccal cancer is the development of trismus, defined as a mouth opening limited to 35 mm or less. In addition, native buccal mucosa has a high degree of inherent elasticity that is difficult to replicate through any form of tissue transfer. By itself, trismus may contribute to difficulty with oral intake, chewing, swallowing, speaking, as well as dental issues from poor oral hygiene. Functionally, the buccal region plays a crucial role in oral phase swallowing, speech, mastication, and facial movement. Facial expression, along with the contour of the face and appearance of the oral commissure, can also introduce aesthetic complexities in reconstruction. Successful reconstruction of the buccal region is aimed at restoring a barrier that encloses the oral cavity while supporting the functional and aesthetic components listed above. Each of these elements must be considered in characterizing a defect and planning for an appropriate reconstruction the muscles of facial expression in the buccal region include the orbicularis oris, risorius, zygomaticus major and minor, buccinator, and depressor anguli oris. Squaquara et al classify the size of intraoral defects into small (4 cm diameter), medium (7 cm diameter), and large (> 7 cm diameter). However, with increasing defect diameter and soft-tissue involvement, the risk of trismus increases. For large and complex defects, free tissue transfer remains the most versatile option for reconstruction, although it is not without its drawbacks. However, it provides minimal bulk and can retract substantially, making it unsuitable for medium or large defects. It is designed just anterior to the parotid duct and consists of mucosa, submucosa, part of the buccinator muscle, the facial artery, and a rich submucous venous plexus. These flaps are generally versatile and reliable, but require a second-stage surgery, as the flap pedicle tethers the tongue and must be divided after the initial inset. During the postoperative period, trauma to the pedicle can occur from the teeth, as well as excessive movement of the tongue. Dysarthria is also a potential sequela, although this can usually be avoided if the mobility of the tongue tip is maintained. The use of a posteriorly based buccinator musculomucosal flap has also been reported. Excessive harvesting of buccal mucosa, however, may result in trismus as well as damage to the parotid duct. Both flaps can be harvested either as muscle alone or as a musculocutaneous flap, and are based off of the submental artery. The submental flap is designed across the midline in the submental area, and can be used to reconstruct full-thickness defects of the cheek. If skin is included, the patient should be counseled on the potential for development of intraoral hair. In contrast, the island platysma flap is designed over a hairless area at the distal aspect of the sternocleidomastoid muscle. The superior trapezius flap is unique in that its blood supply is unaffected by neck dissection. The lateral island trapezius flap is the least reliable of the three trapezius flaps. It may be used to reconstruct the lateral oral cavity although its primary use is for external defects of the lateral and anterior neck. The venous drainage for this flap occurs through the superficial cervical veins, rather than the venae comitantes of the transverse cervical artery. Given the thin size of the pedicle, the supraclavicular flap may be tunneled into the buccal defect with minimal donor site morbidity and better cosmesis compared to the pectoralis major and trapezius flaps. However, the thyrocervical trunk must be preserved and remain undamaged by prior or concurrent neck dissection. Furthermore, limitations in pedicle length and variations in vascular anatomy may limit its reach to the buccal area. Facial artery ligation does not appear to affect the viability of the flap, as its arterial supply is derived from multiple vessels. A superiorly based flap is typically used for defects centered above the occlusal line, whereas an inferiorly based flap is used for defects centered below. The trapezius can be harvested as one of a combination of three different flaps: the superior trapezius flap based off of paraspinous perforators, the 20. In addition, patients with multiple comorbidities may not be suitable candidates to undergo microvascular free tissue transfer. These factors are exacerbated in patients who undergo postoperative radiation therapy. The prevalence of trismus is estimated to be over 25% in patients who have undergone conventional radiation therapy and over 30% in patients who have undergone concurrent chemoradiation. Trismus in the setting of radiation therapy can be caused by direct contracture of the buccal soft tissue as well as scarring of the muscles of mastication within the field of radiation. Nonoperative management of trismus includes physical therapy exercises, the use of a tongue depressor plate, mechanical stretching aids, pentoxifylline, or injection of steroids, fibrinolytic agents, or botulinum toxin. Surgical management usually entails a combination of scar release, masticatory muscle myotomy, coronoidectomy, and microvascular free tissue transfer. Free tissue transfer is especially important to create long-lasting improvement in mouth opening, as it introduces healthy, nonirradiated, and well-perfused tissue. Key Points Reconstruction of the buccal region following tumor resection poses a unique challenge with important aesthetic and functional considerations. Reconstructive options range from healing by secondary intention to microvascular free tissue transfer. Ablation of buccal cancer and functionality buccal reconstruction using an individuation anterolateral thigh flap. Intra oral reconstruction with buccal fat pad: recent applications of autologous tissue transplantation as a local flap. The lateral tongue flap: a salvage option for reconstruction of buccal recurrences. Use of the posteriorly based lateral tongue flap in the repair of palatal fistulae. Systematic review of the platysma myocutaneous flap for head and neck reconstruction. Superiorly or inferiorly based "islanded" nasolabial flap for buccal mucosa defects reconstruction. Extended supraclavicular fasciocutaneous island flap based on the transverse cervical artery for head and neck reconstruction after cancer ablation. Application of various flaps to intraoral reconstruction of buccal defects after resection of buccal mucosa carcinoma. Comparison of radial forearm free flap, pedicled buccal fat pad flap and split-thickness skin graft in reconstruction of buccal mucosal defect. Reconstruction of full-thickness buccal defects with folded radial forearm free flaps: a retrospective clinical study. Microsurgical reconstruction of the oral cavity with free flaps from the anterolateral thigh and the radial forearm: a comparison of perioperative data from 161 cases. Reconstruction of soft-tissue defects of the head and neck: radial forearm flap or anterolateral thigh flap
Cheap vytorin 20 mg with mastercard
The prognosis is inversely related to gestational age: the earlier the oligohydramnios occurs cholesterol biosynthesis buy vytorin 30 mg cheap, the worse the outcome. Expected Outcome: When oligohydramnios occurs in term or postterm pregnancies, it is associated with fetuses that do not tolerate labor well (five-fold to seven-fold increase in rate of cesarean delivery). Specific Measures: Amnioinfusion (the introduction of normal saline via an intrauterine catheter placed through the partially dilated cervix during labor) has been used to reduce the incidence of umbilical cord compression during labor. A randomized clinical trial of the intrapartum assessment of amniotic fluid volume: amniotic fluid index versus the single deepest pocket technique. Prophylactic amnioinfusion for intrapartum oligohydramnios: a meta-analysis of randomized controlled trials. Perinatal outcome and amniotic fluid index in the antepartum and intrapartum periods: a metaanalysis. Amniotic fluid index versus single deepest vertical pocket as a screening test for preventing adverse pregnancy outcome. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Steroid therapy to accelerate fetal lung maturation has been advocated for patients remote from term. Oxytocin, methylergonovine maleate (Methergine), and prostaglandin (E2) therapy to assist with uterine contraction after delivery. Contraindications: -Mimetic agents should not be used if there is significant maternal blood loss or hypotension. Significant bleeding from the placental site may result in maternal compromise, and extensive measures (including hysterectomy) to achieve control must be taken. Approximately 35% of infants whose mothers require transfusion require transfusion themselves. Internal (concealed) bleeding External bleeding Obstruction of cervix by presenting part Section through placenta in premature separation showing nodular ischemia and infarction above clots. Imaging: Ultrasound may show signs of a retroplacental clot or collection of blood, but absence does not rule out abruption. Expected Outcome: Small abruption may be managed conservatively; larger separations may jeopardize mother and fetus and frequently require immediate delivery. Pathologic Findings Bleeding into the decidua basalia with hematoma formation, leading to progressive separation of the placenta and pressure necrosis. Acute anemia, evidence of clotting activation and consumption, histologically normal placenta. Specific Measures: Fetal and uterine activity monitoring, monitoring of maternal condition (pulse, blood pressure, pulse oxygenation), expedited delivery when significant separation has occurred. Often there is insufficient time for any more than the most basic information and counseling. An international contrast of rates of placental abruption: an age-period-cohort analysis. Incidence of placental abruption in relation to cigarette smoking and hypertensive disorders during pregnancy: a meta-analysis of observational studies. Risk factors for preeclampsia, abruptio placentae, and adverse neonatal outcomes among women with chronic hypertension. Contraindications: Tocolytics should not be used until a diagnosis is established. Imaging: Amniotic fluid index calculated by adding the vertical depths of the largest pockets of amniotic fluid in each quadrant of the uterus (average at term = 12. Specific Measures: Indomethacin therapy has been shown to be of help in some patients. Therapeutic amniocentesis may be used to transiently relieve maternal symptoms and in some cases allow prolongation of the gestation. Administration of steroids to accelerate fetal lung maturation as indicated by gestational age and risk for preterm delivery. Contraindications: Aspirin-sensitive asthma, inflammatory bowel disease, or ulcers. Precautions: Use of nonsteroidal antiinflammatory agents has been associated with premature closure of the ductus arteriosus. Possible Complications: Premature labor and delivery (40%), abruptio placentae, maternal pulmonary compromise, umbilical cord prolapse, uterine atony. Expected Outcome: Mild to moderate increases in fluid are not associated with significant risk. Association of isolated polyhydramnios at or beyond 34 weeks of gestation and pregnancy outcome. Outcome of children born out of pregnancies complicated by unexplained polyhydramnios. Ultrasound abnormalities of the amniotic fluid, membranes, umbilical cord, and placenta. Medication to suppress lactation has little value, and recommendations for its use have been withdrawn. Single dose cabergoline versus bromocriptine in inhibition of puerperal lactation: randomised, double blind, multicentre study. The effect of hollyhock (Althaea officinalis L) leaf compresses combined with warm and cold compress on breast engorgement in lactating women: a randomized clinical trial. Special Tests: Beck Depression Inventory or the 10-item Edinburgh Postnatal Depression Scale may be used to screen for depression. Precautions: Use in pregnancy must be carefully weighed versus the potential effects (teratogenic) on the fetus. Some agents are associated with delayed cardiac conduction and disturbances in rhythm. Interactions: Virtually all agents may produce fatal interactions with monoamine oxidase inhibitors or antiarrhythmic medications. Monoamine oxidase inhibitors can also adversely interact with vasoconstrictors, decongestants, meperidine, and other narcotics. Alternative Therapy Electroshock therapy may still play a role in the treatment of major depression and mania in those who do not respond to other therapies or are at high risk for suicide. For those with a history of prior postpartum depression, prophylactic treatment with antidepressants is associated with a reduced rate of recurrence. Possible Complications: Progressive loss of function, impaired bonding, marital discord, infanticide or suicide. Recurrence rates are approximately 50% after a single episode, 70% after two episodes, and 90% with three or more episodes. The association between pregnancy processes, preterm delivery, low birth weight, and postpartum depressions-The need for interdisciplinary integration. Hospitalization is required for all but the most benign conditions (mild gestational hypertension, stable chronic hypertension with normal fetal growth).
Syndromes
- Avoid taking salt substitutes if you are asked to eat a low-salt diet
- The spot where the wart is may be lighter or darker than the other skin. Rarely, warts are black.
- Dementia
- Damage to the nerves in the spinal cord, especially if the person moves during the test
- A tumor in the middle ear
- Jaundice
- Headaches
- See how far cancer has spread
Order vytorin 30mg on-line
Complications in the postoperative period can include wound infection and orocutaneous fistulas cholesterol medication comparison order vytorin 20mg. Severe soft tissue edema after large resections with free tissue transfer can cause airway obstruction, such that a tracheostomy should be considered at the time of surgery in select patients. In the longer term, extensive resections can result in significant swallowing difficulties due to impaired tongue mobility and tethering, and decreased sensation if the lingual or glossopharyngeal nerves were resected. Speech articulation may be affected for the same reasons, and velopharyngeal insufficiency can result from soft palate resection. It is usually treated conservatively with hyperbaric oxygen therapy; however, surgical resection with reconstruction may be required. Postradiation therapy patients are also at risk for dental caries and periodontal disease, and should be routinely evaluated by dental providers familiar with radiation therapy-related dental sequelae. Recommended treatment is complete surgical resection, followed by radiation therapy for all but small lowgrade tumors. Advances in molecular genetics have greatly enhanced our understanding of salivary gland tumor biology, and hold future promise for improved diagnostic accuracy and the development of targeted therapeutics and other novel treatments. Key Points Oral cavity salivary gland malignancies are rare and include a remarkable diversity of histopathologic tumor types. Mucoepidermoid carcinoma and adenoid cystic carcinoma are the most common histopathologic types of minor salivary gland malignancies in the oral cavity. The treatment for oral cavity salivary gland malignancies is surgical resection with postoperative radiation for high-risk tumors. Neck dissection is indicated for clinically evident cervical lymph node metastases. Elective neck treatment with either neck dissection or radiation therapy may be considered for high-risk tumors. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Preface. Long-term follow-up of over 1000 patients with salivary gland tumours treated in a single centre. A prognostic index for predicting lymph node metastasis in minor salivary gland cancer. Prognostic factors and occult nodal disease in mucoepidermoid carcinoma of the oral cavity and oropharynx: An analysis of the National Cancer Database. Diet and other risk factors for cancer of the salivary glands:a population-based case-control study. Radiationinduced salivary gland tumors: a report of 18 cases and a review of the literature. Mucoepidermoid carcinoma postradioactive iodine treatment of papillary thyroid carcinoma: unique presentation and putative etiologic association. Minor salivary gland mucoepidermoid carcinoma in children and adolescents: a case series and review of the literature. Intraoral minor salivary gland tumors: a review of 75 cases in a Libyan population. Staging and follow-up of high-grade malignant salivary gland tumours: the role of traditional versus functional imaging approaches-A review. Pitfalls in the biopsy diagnosis of intraoral minor salivary gland neoplasms: diagnostic considerations and recommended approach. Comparison of ultrasound-guided core biopsy versus fine-needle aspiration biopsy in the evaluation of salivary gland lesions. Ultrasound-guided core needle biopsy of salivary gland lesions: a systematic review and meta-analysis. Quantitative diffusion-weighted magnetic resonance imaging in the evaluation of parotid gland masses: a study with histopathological correlation. Positron emission tomography-computed tomography adds to the management of salivary gland malignancies. The role of molecular testing in the differential diagnosis of salivary gland carcinomas. Polymorphous low-grade adenocarcinoma of the head and neck: a population-based study of 460 cases. Histopathological grading of adenoid cystic carcinoma of the head and neck: analysis of currently used grading systems and proposal for a simplified grading scheme. Long-term outcomes of surgery followed by radiation therapy for minor salivary gland carcinomas. Postoperative irradiation of minor salivary gland malignancies of the head and neck. Radical treatment strategies improve the long-term outcome of recurrent atypical meningiomas. Mucoepidermoid carcinoma of minor salivary glands: report of 17 cases with follow-up. Is it necessary to resect bone for low-grade mucoepidermoid carcinoma of the palate Polymorphous low-grade adenocarcinoma: a case series and determination of recurrence. Nineteen-year oncologic outcomes and the benefit of elective neck dissection in salivary gland adenoid cystic carcinoma. Systemic therapy in metastatic salivary gland carcinomas: a pathology-driven paradigm Systemic therapy in the management of metastatic or locally recurrent adenoid cystic carcinoma of the salivary glands: a systematic review. Salivary duct carcinoma: an aggressive salivary gland malignancy with opportunities for targeted therapy. Predictors of speech and swallowing function following primary surgery for oral and oropharyngeal cancer. Dysphagia in head and neck cancer patients treated with radiation: assessment, sequelae, and rehabilitation. A review of dental treatment of head and neck cancer patients, before, during and after radiotherapy: part 2. A review of dental treatment of head and neck cancer patients, before, during and after radiotherapy: part 1. Schmitt Summary In addition to squamous cell carcinoma, several other rare tumors can arise in the oral cavity. Detection of these other tumors often requires a high index of suspicion and careful pathologic review. Prior radiation is one known risk factor for oral cavity sarcoma, most commonly osteosarcoma. The latency period between radiation and development of osteosarcoma of the mandible is usually 10 years or more. These tumors are rare and can often be mistaken for squamous cell carcinoma, so a proper pathologic diagnosis is critical. Most of these uncommon malignancies are treated with comprehensive surgical resection, except for lymphomas and some sarcomas. Some of these lesions arise de novo, but evolution of a benign pigmented lesion into a melanoma has also been reported. Sarcomas involving the mandible or maxilla may present with loss or mobility of teeth. While most oral melanomas are primary lesions, they can also metastasize to the oral cavity from other sites. Similarly, patients with oral lymphomas may have a solitary oral lesion or disseminated disease, requiring extensive imaging and bone marrow biopsy for staging. For lesions involving the maxilla or mandible with bony destruction noted on imaging, osteosarcoma and lymphoma should be in the differential diagnosis. However, reconstructive surgery may be necessary in cases where lymphoma has caused substantial destruction of bone.
Generic 30mg vytorin mastercard
Quality of life considerations in head and neck cancer: United Kingdom National Multidisciplinary Guidelines cholesterol test nil by mouth order genuine vytorin. Nutrition impact symptoms and associated outcomes in post-chemoradiotherapy head and neck cancer survivors: a systematic review. Werning Summary Our increased understanding of lip cancer has undergone an incremental evolution that permits head and neck cancer specialists to improve the treatment outcomes for our patients. Recognition that the biological behavior of lip cancer differs based on its origin from the wet or dry vermilion is essential to accordingly modify treatment and optimize outcomes. Keywords: actinic cheilitis, mucosal lip, dry vermilion In cross-section, the lip is a three-layered structure comprising the skin, orbicularis oris muscle, and lining intraoral mucosa. The vermilion region, or the true lip, has a rich vascular plexus that underlies a thin epithelial architecture that gives the vermilion its unique aesthetic appearance. The vermilion zone of the lip is covered by orthokeratinized stratified squamous epithelium that is firmly attached to the underlying orbicularis oris muscle, whereas the intraoral labial mucosa is nonkeratinized. The transition between the intraoral lining mucosa and the wet vermilion is termed the wet line. However, cancers arising from the dry vermilion and the vermilion border are now designated as extraoral and are staged as cutaneous cancers. Alterations in their appearance or function can adversely impact self-esteem, societal acceptance, and quality of life. We are generally unaware of the aesthetic and functional importance of the lips until they are altered, but when they are altered, the impact can be life-changing. As the point of transition between the skin of the face and the oral cavity, the lips are exposed to environmental agents that cause both skin cancer and oral cancer. Over the past decade, refinements in our understanding of the natural history and biological behavior of lip cancer have helped characterize the differences in diagnosis, management, and outcomes between cancers of the extraoral, or dry vermilion lip, and of the intraoral wet mucosal lip. This review compares and contrasts the treatment for and prognosis of cancers that arise from the mucosal lip and the dry vermilion. In contrast, Eastern and Southeast Asia and sub-Saharan Africa had the lowest incidence rates. The incidence of lip cancer in the United states, based on data compiled by the Globocan Project, is between 0. Greater than 98% of the diagnosed lip cancers occur in the Caucasian population, and more than 60% of these are diagnosed in individuals older than 60 years of age. The boundaries of the upper cutaneous lip extend superiorly to the nostril sill and alar base, and laterally to the melolabial, or nasolabial sulcus. The upper lip is comprised of three aesthetic subunits: two lateral subunits, which extend from each philtral ridge to the melolabial sulcus, and the centrally located philtrum. In contrast, the lower cutaneous lip has one aesthetic unit that extends inferiorly to the labiomental crease. The cutaneous portion of the upper and lower lips terminates at the white roll, where the curvature of the vermilion creates a clearly delineated border. Fishermen, farmers, foresters, and concrete workers who work outside have markedly higher incidence rates of lip cancer. However, epidemiologic evidence in support of this association is limited because the incidence rates of mucosal lip cancer and oral mucosal cancers in tobacco users have not been analyzed separately. Moreover, the association between chronic alcohol use and lip cancer has not been rigorously evaluated, so the causative role of alcohol use has been extrapolated from epidemiologic investigations of oral cancer patients and is largely presumptive. Solid organ transplant recipients on immunosuppressive agents such as cyclosporine A and azathioprine have a risk of developing lip cancer that is 20 times greater than the general population. The lips demonstrate atrophic changes with increased prominence of vertical folds, patchy color variegation, and obscuration of the vermilion border. Clinically, actinic cheilitis has a varied appearance, but is frequently characterized by areas of desiccation with a scaly appearance and rough surface texture, atrophic changes, and an increase in the prominence of vertical folds, or fissuring. Color variegation is frequently present with patchy areas of leukoplakia, erythroplakia, or erythroleukoplakia. Biopsy of the most concerning area should be performed whenever clinical examination is consistent with actinic cheilitis. In the cases where carcinoma in situ or invasion is identified, biopsies of other less concerning areas along the surface of the lip may help clarify the indicated treatment. The exclusion of invasive cancer at the time of biopsy is of paramount importance since many of the treatment modalities that are used for actinic cheilitis ablate the epithelial surface in lieu of formal excision. However, choosing the most appropriate area for biopsy may be challenging because areas with a homogeneous appearance have been shown to demonstrate heterogeneous histologic changes. Treatment is clearly indicated whenever the risk of evolution to malignancy is high, but excision or ablation may be optional if the risk of malignant progression is low, and may be based on patient factors, such as cosmetic concerns or patient discomfort. Vermilionectomy, or the lip shave, remains the standard by which the efficacy of other techniques must be compared since vermilionectomy is the only excisional procedure. Numerous other techniques have been used with varying success rates, including cryosurgery, 5-fluorouracil, imiquimod, photodynamic therapy, trichloroacetic acid chemical peel, electrodessication, carbon dioxide laser ablation, diclofenac, and dermabrasion. The medical history should be reviewed for conditions or medications that cause immunosuppression, as well as the use of photosensitizing antihypertensive medications. Documentation of the extent of sun exposure and the amount of tobacco and alcohol use is essential to identify possible etiologies. Lip cancer is usually detected in its early stages due to its conspicuous anatomic location. Cancers arising from the dry vermilion that arise from areas involved by actinic cheilitis tend to be slow growing. Surface changes that are thought to be due to actinic cheilitis may in fact be involved by early invasive cancer that remains undiagnosed until vermilionectomy is performed. Subtle actinic-appearing changes, if untreated, may slowly progress to a raised irregular exophytic lesion, an indurated subcutaneous/submucosal lesion, or an ulcerated lesion. The involved mucosa may have a patchy appearance with areas of normal-appearing mucosa. Biopsy of a necrotic central ulceration may result in a false-negative biopsy result, so biopsy of viable tissue surrounding the central ulceration is preferred. Clinical evaluation requires careful inspection of the surface anatomy of the lip to characterize any changes of the dry and wet vermilion. Examination for mottling, color and textural changes, fissuring, ulcerations, induration, and obscuration of the vermilion border and normal lip anatomy should be performed. Incisional or punch biopsy is preferred over shave biopsy, which could lead to the incorrect diagnosis of a noninvasive in situ lesion. Physical examination of the lip and neck is sufficient for smaller lesions, whereas axial imaging should be considered for lesions measuring more than 2 cm in diameter. Information pertaining to retrograde perineural involvement of the trigeminal nerve and mandibular marrow invasion is ideally assessed with magnetic resonance imaging. While the updated staging criteria reflect our current understanding of lip cancer, they will also result in stage migration that limits our ability to extrapolate treatment outcomes from the existing peer-reviewed literature to the updated stage groups. Most retrospective case series document metastasis rates of less than 15% in lesions measuring 4 cm or less. Zitsch et al documented cervical metastasis in 7% of patients 2 cm or less in diameter versus 16% in larger cancers. A large retrospective review of 1,036 lip cancers found that 31% of cancers involving the commissure metastasized to the cervical 13. Wider tumor-free margins are essential to maximize local control and to minimize the need for adjuvant radiotherapy with or without chemotherapy. Individuals who wear removable dentures must be counseled that postoperative microstomia may prevent their use. Careful preoperative assessment with inspection and palpation permits the surgeon to appreciate the three-dimensional nature of the cancer, the planned resection, and the resultant soft-tissue defect. Lip cancer resection should be performed en bloc with the intent to achieve negative, or clear, margins during the initial resection. The excision of lip cancers with 10-mm mucosal margins that are immersed in 10% buffered formalin shrink by 41 to 47. Resection of the lip cancer and vermilionectomy of the entire lower lip was performed. Reconstruction was achieved with a circumoral Estlander flap and a labial mucosal advancement flap to reconstruct the vermilion.
Cheap 20mg vytorin with amex
Loss of any or all of the graft will dictate that the wound will heal by secondary intention cholesterol levels beer vytorin 20mg otc. This leads to contraction of the wound leading to pathological contracture, which is an ongoing problem without an easy solution. To ensure complete take of the buccal skin graft, a tie-over bolster should be used. The graft is secured at the mucosal margins with interrupted chromic or other absorbable sutures. It is desirable to augment the bolster with through-and-through buccal mattress sutures, usually done with chromic sutures. The sutures can be tied on the skin over a cotton dental roll or a piece of petrolatum gauze rolled into a sausage shape. This will avoid necrosis on the skin and the sutures will increase complete contact of the graft with the bed and insure excellent take of the graft. Initially the buccal surface will be deeply indented in the area of resection, but will fill in over time. The laminated nature of the cheek will need to be resected and an adequate reconstruction cannot be accomplished with local tissue. A composite resection of buccal mucosa, buccinator, and skin will require a complex reconstruction. Based on size, the defect may require a "folded" flap to give internal lining and skin coverage. The flap will be insensate and will not animate and with the loss of the buccinator there will be a tendency for the patient to be unable to mobilize the food bolus onto the occlusal surface. The use of pedicled local and regional flaps for reconstruction of larger defects of the buccal tissues is for the most part of historical significance. For patients who cannot tolerate the prolonged surgical time associated with free tissue transfers, temporalis muscular flaps and pectoralis major myocutaneous flaps have been described and can be used in selected circumstances. A frozen section margin of the duct should be sent to pathology while preparing the repositioning of the structure. The duct can be freed up to the anterior border of the masseter and cannulated with a lacrimal probe or other instrument. It should be opened longitudinally for a few millimeters to give a "fish-mouth" effect, opening the drainage of the duct and avoiding a stricture. A stent, angiocatheter, or other soft pliable device should be placed and sutured into the cheek. All patients should be counseled prior to treatment that physical therapy and speech and swallowing therapy will be an ongoing process that will require their active participation in an effort to return the patient to a full and active life. Trismus is a common sequela of treatment requiring ongoing stretching and swallowing therapy. In patients who are clinically N0, observation, elective neck dissection, sentinel node biopsy, or elective neck radiation have all been employed. However, locoregional recurrence rates are higher in patients who undergo observation compared to elective neck dissection, ranging from 25 to 100% versus 7 to 33%, with corresponding statistically significant differences in overall survival. Patients with advanced-stage buccal cancer have a higher incidence of occult nodal metastasis, and should undergo elective neck dissection at the time of primary site surgery. The incidence of nodal metastases in level V is reported at less than 5% and most patients will require postoperative radiation therapy. Because of the high recurrence rates associated with buccal cancer, postoperative radiation therapy is recommend for all but favorable early-stage disease. Adjuvant treatment for oral cancer is covered in more detail in Chapter 35 and 36. Treatment is primarily surgical and often requires reconstruction and adjuvant therapy. Early, aggressive swallowing rehabilitation is advised to mitigate late dysphagia. The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012. Clinicopathologic evaluation of prognostic factors for squamous cell carcinoma of the buccal mucosa. Prognostic factors in patients with buccal squamous cell carcinoma: 10-year experience. Squamous cell carcinoma of tongue and buccal mucosa: clinico-pathologically different entities. Positive surgical margins in early stage oral cavity cancer: an analysis of 20,602 cases. Cancer of the buccal mucosa: are margins and T-stage accurate predictors of local control Squamous cell carcinoma of the buccal mucosa: outcomes of treatment in the modern era. Malignant transformation of oral submucous fibrosis: overview of histopathological aspects. Malignant transformation of oral lichen planus and oral lichenoid lesions: a meta-analysis of 20095 patient data. Potentially malignant disorders revisited-The lichenoid lesion/proliferative verrucous leukoplakia conundrum. What is the role of elective neck dissection in the treatment of patients with buccal squamous cell carcinoma and clinically negative neck findings Outcome and cervical metastatic spread of squamous cell cancer of the buccal mucosa, a retrospective analysis of the past 25 years. Carcinoma of the buccal mucosa: analysis of clinical presentation, outcome and prognostic factors. Skin involvement and ipsilateral nodal metastasis as a predictor of contralateral nodal metastasis in buccal mucosa cancers. Predictors of locoregional recurrence in early stage buccal cancer with pathologically clear surgical margins and negative neck. Head and neck cancer: major changes in the American Joint Committee on Cancer Eighth Edition cancer staging manual. Oral cavity squamous cell carcinoma: role of pretreatment imaging and its influence on management. Patterns of cervical lymph node metastases from squamous carcinomas of the upper aerodigestive tract. Setting the stage for 2018: how the changes in the American Joint Committee on Cancer/Union for International Cancer Control Cancer Staging Manual Eighth Edition impact radiologists. Definitive chemoradiation for locallyadvanced oral cavity cancer: a 20-year experience. In-continuity neck dissection: long-term oncological outcomes in squamous cell carcinoma of the buccal mucosa. A retrospective analysis of squamous carcinoma of the buccal mucosa: an aggressive subsite within the oral cavity. Buccal mucosa elasticity influences surgical margin determination in buccal carcinoma resection. Clinicopathological study of surgical margins in squamous cell carcinoma of buccal mucosa. Post-operative radiotherapy in carcinoma of buccal mucosa, a prospective randomized trial. Systematic review of the current evidence in the use of postoperative radiotherapy for oral squamous cell carcinoma. Surgery versus surgery and postoperative radiotherapy in squamous cell carcinoma of the buccal mucosa: a comparative study. Eisele, and Carole Fakhry Summary Reconstruction of the buccal region following tumor resection poses a unique challenge with important aesthetic and functional considerations. The buccal region plays a major role in mouth opening, chewing, swallowing, speech, as well as facial movement. The optimal reconstructive technique is largely based on the size of the primary defect. Smaller defects may be closed primarily or with a local flap, while larger defects may require a regional or free flap to preserve function. Trismus is one of the most common sequelae following buccal tumor resection and reconstruction, especially in patients who have undergone or are planned to undergo radiation therapy. There are multiple nonoperative as well as operative treatments for trismus, with microvascular free tissue transfer playing an important role in creating long-lasting improvement in mouth opening. Trismus secondary release surgery and microsurgical free flap reconstruction after surgical treatment of head and neck cancer.
Best vytorin 20mg
However cholesterol tests over the counter discount 20mg vytorin with mastercard, although LrFs offer the ability to close large defects with robust, vascularized tissue, without the need for microvascular expertise, they still suffer from a few shortcomings and lack the adaptability that is offered by free flaps. Specifically, they can be limited by the length and degree of rotation of their vascular pedicle and may be affected by defect size and location. It can be raised as a superiorly14 or inferiorly based flap13 with the limits of the harvest being the inferior and superior gingival sulci. The key step is to identify the facial artery and this can be done at the anterior or posterior incision of the flap. The artery lies deep to the buccinator muscle and the flap is harvested in a plane deep to the artery. The artery must stay attached to the more superficial tissues to maintain vascularity and the venous drainage is based on submucosal venous plexus. The pedicle can be ligated between from 13 and 21 days after inset; however, techniques have been described to tunnel the pedicle to avoid needed ligation. If it is too large to close primarily, it can be left to granulate or closed using a buccal fat pad transposition flap. Submental Island Flap the submental island flap is a commonly used regional flap for reconstruction of the oral cavity. However, if level I is shown to be clinically negative for disease, the submental island flap can still be used and the harvest of the flap allows for an appropriate level Ia and Ib neck dissection without compromising the flap pedicle. Although variations in harvest technique are described, the general steps are as follows:9,11,12 the skin paddle is designed to fit the necessary defect. The skin incision through the inferior edge of flap is performed and subplatysmal flaps are elevated. The facial artery is found as it traces over the mandible and then the submental arteries are identified branching off the facial and are traced to the anterior belly of the digastric. The level I neck dissection can be completed, preserving the facial and submental vessels. The anterior flap incision can be made and the mandibular attachment of the anterior belly of the digastric can be divided to help protect the pedicle. The depth of the flap dissection is to the mylohyoid muscle with branches of the submental artery supplying the mylohyoid needing to be ligated. Once the flap is elevated, if necessary, any remaining nodal contents can be cleared carefully from the adjacent pedicle before being rotated into oral cavity for inset. Supraclavicular Island Flap the supraclavicular island flap is a popular LrF being used with increased frequency by head and neck surgeons and has shown application in floor of mouth reconstruction. It can be located in the triangle created by the sternocleidomastoid muscle, clavicle, and external jugular vein. The artery can then be marked out heading laterally over the supraclavicular fossa eventually crossing the clavicle. The length of the skin that can be taken has been described to extend reliably up to 5 cm past the most distal portion of the pedicle Doppler signal. Using the triangle previously mapped out as a fulcrum point, a gauze or something similar can be used to estimate the length of flap needed to reach the defect site. The distal portion of the flap can be raised supra- or subfascially to the fascia overlying the deltoid muscle. The flap is raised up in this plane up to the pedicle found medial to the inferolateral border of the trapezius muscle. The superficial plane of dissection above the clavicle is in the supraplatysmal plane to avoid injury to the contributing vascularity. Next the skin paddle is raised with the underlying platysma, raising a subplatysmal flap. The external jugular vein is ligated distally and left attached to the platysma to allow for retrograde venous drainage and ideally the submental branches of the facial artery and vein are left in continuity with the flap to allow for optimal vascularity. The disadvantages of using the flap for floor of mouth defects are that it can only be used on smaller defects, it is not an option for dentulous patients, and that a second-stage pedicle takedown procedure is required. The flap is raised in the same manner as one would for reconstructing facial defects. The portion of the flap that is in the tunnel is de-epithelized in order to avoid buried epithelium. This can be used to obliterate any submental dead space resulting from the resection. Free Tissue Closure Free tissue transfer is the most complex reconstructive option for floor of mouth defects. Although there are no definite indications for free-flap reconstruction, common reasons include the following: large defects with minimal remaining mobile floor of mouth mucosa attached to the fixed gingiva, resection after radiation failure, or composite reconstruction resulting in a through-and-through defect into an associated neck dissection wound. Many options exist for free-flap reconstruction, each with their own advantages and disadvantages. Generally, when reconstructing the floor of the mouth a flap should be chosen that has a thin and pliable skin paddle, a decent length vascular pedicle, and the option of incorporating soft tissue into the flap to add bulk. The two most common soft-tissue flaps used to reconstruct the floor of the mouth are the radial forearm and anterolateral free flap. This tissue can also be utilized to increase the bulk to the reconstruction in patients undergoing a partial glossectomy as a part of their resection. The associated donor site is typically closed with a split- or full-thickness skin graft, with primary closure of the proximal incision. It offers the possibility of a large, modifiable skin paddle with soft-tissue bulk and a pedicle length of 8 cm. However, in defects limited to the floor of the mouth, this increased bulk can sometimes be detrimental and may even limit tongue mobility and cause mass effect on the oral and oropharyngeal airway. An additional disadvantage is the potential for variability of the perforator vascular supply that can result in an increased challenge with harvest. In thin patients such as those in the East Asian population where it was initially described,30 the skin can be appropriately thin. It should also be noted that the skin paddle is often thinner with less subcutaneous fat in the distal portion of the leg, while thicker more proximally. Therefore, the skin paddle could be designed to incorporate the distal skin, if perforating vessel anatomy allows. The pedicle, based on the radial artery, associated venae comitantes, and the cephalic vein, is fairly long, which allows access to vessels on both sides of the neck if needed. One disadvantage is that the ulnar nerve and artery are closely related, with the artery giving multiple branches to vascularize the nerve. Such a design can be used for defects involving the floor of the mouth as well as the adjacent ventral or lateral tongue to optimize mobility of the anterior tongue. While these flaps can provide versatile options for a large variety of bony and soft-tissue defects, the thickness of skin on the back make them less ideal for this type of repair. Moreover, due to the location on the shoulder, the ability to perform a two-team approach to optimize efficiency is more limited. For limited resections with primary closure or wounds left open to granulate without communication to the neck wound, patients can be allowed to start an oral diet immediately postoperatively. Often full liquids or a soft mechanical diet is ideal to start, advancing when appropriate. In such instances, chlorhexidine mouth rinse can be used three times daily and after food to provide topical antibacterial coverage. In instances where a split-thickness skin graft is used, a xeroform bolster can be placed to keep the graft flush with the underlying wound bed. These patients should be maintained on a liquid diet or with a nasogastric tube for nutrition, with regular antibiotic mouth rinse. The bolster can then be removed in the office around 1 week postoperatively, at which time the diet can be slowly advanced. For regional or free tissue transfer repair, patients should be covered with 24 hours of perioperative systemic antibiotic coverage for gram-positive, gram-negative, and anaerobic organisms. Following this initial period, if the suture line remains intact, they should be assessed by a speech and swallowing team regarding the safety for starting oral intake. Such reconstructions are more prone to contracture than skin-containing free flaps. Downsides of the fascia-only flap have been shrinkage and contracture of the flap.
Glucerite (Glycerol). Vytorin.
- What other names is Glycerol known by?
- Dosing considerations for Glycerol.
- Are there safety concerns?
- Constipation, when used rectally as a suppository.
- Treating stroke when used intravenously.
- Helping with weight loss, when taken by mouth.
- How does Glycerol work?
- What is Glycerol?
- Improving exercise performance when taken by mouth.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96054
Purchase vytorin uk
Bleeding is most common in the early postoperative period and usually warrants operative exploration and control of hemorrhage foods lower bad cholesterol fast buy cheap vytorin 30 mg on-line. Chyle leaks can occur on the right side because of interruption of the right accessory lymphatic duct. Surgical management of the neck adds the benefit of pathologic evaluation and staging of the neck and identification of high-risk pathologic features. Radiation therapy is usually started within 4 to 6 weeks after surgical therapy, as delays beyond 6 weeks have worse outcome. Postoperative radiation therapy is indicated when two or more histologically positive lymph nodes are identified. There is some controversy regarding this, given studies that reported surgery only for N1 disease had regional recurrence rates from 16 to 25%. This suggest that postoperative radiation therapy may be beneficial and deserves multidisciplinary discussion. Combination therapy certainly has improved efficacy when compared to either modality alone. Furthermore, there is also evidence that the addition of chemotherapy to radiation therapy may improve locoregional control and overall survival for these patients. Imaging evaluation of the neck should be used routinely as it can significantly help with identification of neck disease or suspicious cervical lymph nodes. N + neck disease requires surgical treatment with therapeutic neck dissection and potential consideration of adjuvant radiation therapy and chemotherapy based on high-risk pathologic characteristics. Elective versus therapeutic radical neck dissection in epidermoid carcinoma of the oral cavity: results of a randomized clinical trial. Elective versus therapeutic neck dissection in early carcinoma of the oral tongue. Supraomohyoid neck dissection in the treatment of T1/T2 squamous cell carcinoma of oral cavity. Effectiveness of selective neck dissection for management of the clinically negative neck. Elective neck treatment versus observation in patients with T1/T2 N0 squamous cell carcinoma of oral tongue. Elective neck dissection in early-stage oral squamous cell carcinoma -does it influence recurrence and survival Elective neck dissection for the management of the N0 neck in early cancer of the oral tongue: need for a randomized controlled trial. Based on evaluation of high-risk pathologic factors, patients may also require postoperative radiation therapy if not chemotherapy. For nonsurgical patients, radiation therapy is an option, but tumor response and control rates are poor. However, because current methods to assess the risk for occult metastasis are insufficiently accurate and prone to underestimation of actual risk, limited number of studies favor elective treatment of the N0 neck due to better overall locoregional control and survival. Key Points Neck disease significantly affects overall disease-free patient survival, and appropriate evaluation and treatment are critical in oral cavity malignancies. Elective neck dissection in patients with stage T1-T2N0 carcinoma of the anterior tongue. Does elective neck dissection in T1/T2 carcinoma of the oral tongue and floor of the mouth influence recurrence and survival rates Head and neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. Elective neck dissection versus observation in the treatment of early oral tongue carcinoma. Elective neck dissection and survival in patients with squamous cell carcinoma of the oral cavity and oropharynx. Improved survival for patients with clinically T1/T2, N0 tongue tumors undergoing a prophylactic neck dissection. Selective neck dissections for squamous carcinoma of the upper aerodigestive tract: patterns of regional failure. Frequency and therapeutic implications of "skip metastases" in the neck from squamous carcinoma of the oral tongue. The incidence of micrometastases in neck dissection specimens obtained from elective neck dissections. The incidence of lymph node micrometastases in patients pathologically staged N0 in cancer of oral cavity and oropharynx. Importance of the treatment package time in surgery and postoperative radiation therapy for squamous carcinoma of the head and neck. Assessment of cervical lymph node metastasis with different imaging methods in patients with head and neck squamous cell carcinoma. Staging of cervical lymph nodes in oral squamous cell carcinoma: adding ultrasound in clinically lymph node negative patients may improve diagnostic work-up. American Head and Neck Society, American Academy of Otolaryngology-Head and Neck Surgery. Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Objective comparison of shoulder dysfunction after three neck dissection techniques. Clinicopathological analysis of elective neck dissection for N0 neck of early oral tongue carcinoma. Association of postoperative radiotherapy with survival in patients with N1 oral cavity and oropharyngeal squamous cell carcinoma. The extent of neck disease after regional failure during observation of the N0 neck. Tumor thickness influences prognosis of T1 and T2 oral cavity cancer-but what thickness Histopathological and lymphangiogenic parameters in relation to lymph node metastasis in early stage oral squamous cell carcinoma. Elective neck irradiation for squamous cell carcinoma of the head and neck: analysis of time-dose factors and causes of failure. Surgical treatment of early oral carcinoma-results of a prospective controlled multicenter study. Early stage carcinoma of oral tongue: prognostic factors for local control and survival. The origin of regional failure in oral cavity squamous cell carcinoma with pathologically negative neck metastases. Diagnostic efficacy of sentinel lymph node biopsy in early oral squamous cell carcinoma: a meta-analysis of 66 studies. Occult metastases detected by sentinel node biopsy in patients with early oral and oropharyngeal squamous cell carcinomas: impact on survival. Sentinel lymph node biopsy accurately stages the regional lymph nodes for T1-T2 oral squamous cell carcinomas: results of a prospective multi-institutional trial. Postoperative urinary tract infection and short-term outcomes and costs in head and neck cancer surgery. Impact of secondary lymphedema after head and neck cancer treatment on symptoms, functional status, and quality of life. First bite syndrome: a complication of surgery involving the parapharyngeal space. Management of chyle leak after head and neck surgery: review of current treatment strategies. Treatment results of postoperative radiotherapy on squamous cell carcinoma of the oral cavity: coexistence of multiple minor risk factors results in higher recurrence rates. Perineural invasion: independent prognostic factor in oral cancer that warrants adjuvant treatment. Cervical lymph node metastases: incidence and implications of extracapsular carcinoma. Association of time between surgery and adjuvant therapy with survival in oral cavity cancer.
Purchase vytorin with american express
The role of positron emission tomography and computed tomography fusion in the management of early-stage and advanced-stage primary head and neck squamous cell carcinoma cholesterol/hdl ratio blood test purchase vytorin 30 mg otc. Impact of [18F]-2-fluorodeoxyglucosepositron emission tomography/computed tomography on previously untreated head and neck cancer patients. Effect of induction chemotherapy on speech and swallowing function in patients with oral tongue cancer. Long-term functional outcomes after resection of tongue cancer: determining the optimal reconstruction method. Pre-mental foramen mandibulotomy for resecting tumors of tongue base and parapharyngeal space. A proposal to redefine close surgical margins in squamous cell carcinoma of the oral tongue. Dynamic optical contrast imaging as a novel modality for rapidly distinguishing head and neck squamous cell carcinoma from surrounding normal tissue. Prospective randomized study of selective neck dissection versus observation for N0 neck of early tongue carcinoma. Tumor thickness influences prognosis of T1 and T2 oral cavity cancer: but what thickness Neck treatment of patients with early stage oral tongue cancer: comparison between observation, supraomohyoid dissection, and extended dissection. Prospective evaluation of the quality of life of oral tongue cancer patients before and after the treatment. Risk factors predicting aspiration after free flap reconstruction of oral cavity and oropharyngeal defects. Subtotal glossectomy preserving half the tongue base prevents taste disorder in patients with tongue cancer. Quality of life in patients treated for cancer of the oral cavity requiring reconstruction: a prospective study. Vosler Summary Reconstruction of the oral tongue is essential for restoration of speech and swallowing function following resection of both benign and malignant tumors. This article outlines the pertinent anatomy, principles of reconstruction, and the reconstructive options based on the location and size of the ablative defect. Locoregional and free-flap reconstruction options and functional outcomes of each flap are discussed. Keywords: tongue reconstruction, locoregional flaps, free flaps, oral tongue resection, articulation, swallow function overlying the abdomen, and palpation of the skin and muscle overlying the latissimus dorsi muscle are performed to determine the best potential free-flap donor site. Diagnostic imagining is imperative for comprehensive determination of tumor involvement and tumor thickness. The body of the tongue is divided into dorsal and ventral components in the axial plane, and into lateral halves in the sagittal plane separated by the median sulcus. The posterior aspect of the oral tongue is the terminal sulcus, indicated by the circumvallate papillae. There are four intrinsic muscles of the tongue: superior longitudinal, inferior longitudinal, transverse, and vertical muscles. The extrinsic muscles include the genioglossus, hyoglossus, styloglossus, and palatoglossus. These muscles originate outside the tongue and insert within it to change tongue position. Deep to the extrinsic muscles is the mylohyoid muscle, which provides a diaphragm for the oral cavity contents. While it is not a muscle of the tongue, involvement of the mylohyoid and removal for safe oncologic margin affects the reconstructive design due to the potential for ptosis of the oral cavity contents postoperatively. Extirpation of benign and, more often, malignant tumors is the indication for reconstruction in the majority of cases. The type of reconstruction depends on the type and extent of the tumor, involvement of other subsites of the oral cavity and oropharynx, and patient factors including comorbid conditions, body habitus, and prior radiation therapy. Overall, the goal of reconstruction is to close the oral defect and restore volume to the oral tongue to assist with articulation and swallowing. Tumor location is an important consideration for tongue reconstruction, as removal of tumors of the tip of the oral tongue tends to produce more difficulties with articulation than tumors involving the lateral tongue. Size of the tumor and involvement of other oral cavity or oropharyngeal subsites will influence the decision of the type and extent of reconstruction. Finally, prior radiation therapy of the oral cavity and neck will limit the use of local and regional flaps, thus limiting the reconstructive options. Physical examination of the oral cavity should consist of determining the location of the tumor, involvement of adjacent subsites such as the floor of the mouth, mandibular alveolus, retromolar trigone, and base of tongue, and estimation of the depth of the tumor. The ipsilateral buccal mucosa is evaluated for the presence of tumor and scars for consideration of regional flap reconstruction. The laxity of cervical skin, the presence of scars from prior surgeries or injuries, and radiation fibrosis should be assessed to determine the feasibility of local and regional flap reconstruction. For anticipated defects greater than 50% of the oral tongue, or if multiple subsites are involved, free-flap reconstruction is preferred. The lingual arteries travel deep to the styloglossus muscle traveling superomedially and then altering course traveling anteroinferiorly. The main branches of the lingual artery are the dorsal lingual artery, the deep lingual, and the sublingual arteries. The dorsal lingual artery supplies the base of the tongue, while the latter two supply the oral tongue. Knowledge of the vascular anatomy of the tongue is important for both the ablative surgeon and the reconstructive surgeon. Adequate hemostatic control of the dorsal lingual artery is imperative to prevent potential catastrophic hemorrhage postoperatively. The sensory innervation of the tongue via the lingual nerve is a more important consideration for the 129 Reconstruction of the Oral Tongue reconstructive surgeon if there is a plan for tongue sensory reinnervation. However, too much tissue rearrangement results in impaired function with no correction for the loss of tongue volume. There are many regional pedicled flaps and free flaps that are available for defects spanning one-third to one-half of the oral tongue. The regional pedicled flaps include the submental artery island flap, facial artery myomucosal flap, supraclavicular artery island flap, temporalis muscle flap, and the pectoralis major myocutaneous flap. Pectoralis major myocutaneous pedicled flaps can also be used, but are generally reserved for salvage cases. Often, small benign and malignant lesions can be left to heal by secondary intention. Small defects in the ventral tongue and floor of mouth should not be allowed to heal by secondary intention, as there is the potential risk of scarring and tethering of the tongue. Defects that leave a large surface area of the tongue exposed but not large enough to produce a significant reduction of tongue volume greater than approximately one-third of the tongue2 can be partially or completely closed primarily with absorbable sutures. Mobilization of local tongue mucosa and musculature with a local flap is also an option to aid in closure. These are comprehensively described by Chepeha et al, and are summarized in the following text. Not an option for dentate patients due to pedicle compromise See above Good regional option with little donor site morbidity. Generally reserved as a salvage option or patients with significant comorbidities Good for midsize defect with thin fasciocutaneous flap. Donor site morbidity due to skin graft and healing issues Limited donor site morbidity. May have too much subcutaneous tissue for appropriate reconstruction based on patient body habitus Potential postoperative ileus and hernia Perforator difficult to identify; may have to convert to latissimus dorsi free flap, which increases volume significantly See above Usually a good option for subtotal and total glossectomies given adequate volume available Limited donor site morbidity. Potential donor site morbidity if radial nerve injured See above Potential for motor innervation. There is limited use of this flap in the literature Potential for motor innervation. Overcorrect for the eventual volume loss due to scar and atrophy over time, as well as the further decrease in volume if adjuvant radiation therapy is planned. Expect an approximately 20% reduction in size with no radiation therapy, and approximately 40% reduction with radiation therapy.
Purchase vytorin american express
Traditional teaching held that surgical repair should be delayed when the injury was diagnosed between roughly days 7 and 14 after ureteric injury cholesterol jones vytorin 30 mg with amex, the time when maximal oedema and inflammation at the site of repair was believed to occur. If there has been a delay in recognition of a ligature injury to the ureter, it is probably safer to remove the affected segment of the ureter and perform a uretero-ureterostomy. Generally speaking, the stent is maintained in position for somewhere between 3 and 6wk (no hard and fast rules). Associated head, chest, intra-abdominal (spleen, liver, mesentery of the bowel), pelvic (bladder, urethra, vagina, rectum), and genital injuries are common, and these injuries and massive blood loss from torn pelvic veins and arteries account for the substantial (20%) mortality after pelvic fracture. Some hospitals perform retrograde urethrography only when blood is present at the meatus; others do this in all pelvic fracture patients where the pubic rami have been disrupted. If there is no blood present at the meatus, a gentle attempt at urethral catheterization may be made. It has been suggested that this could convert a partial urethral rupture into a complete rupture. If the retrograde urethrogram demonstrates a normal urethra, proceed with another attempt at catheterization, using plenty of lubricant. Instability suggests a greater degree of trauma to the pelvis and increases the likelihood of serious associated injuries. In addition, fixation of an unstable fracture reduces blood loss, mortality, hospital stay, leg length discrepancy, and long-term disability; makes nursing care easier; and reduces analgesic consumption. Stability can be defined according to the Tile classification system of pelvic ring fractures (Table 11. The pubic rami fracture and overlap, and the ilium and sacral wings may be fractured. Nerves and vessels are not stretched, but the urethra is more likely to be damaged by scissor-like action of overlapping pubic rami. Radiological determination of stability Based on inlet (for anteroposterior displacement) and outlet views (for vertical displacement) of the pelvis, with the X-ray beam being angled accordingly. Sixty per cent of pelvic fracture bladder ruptures are extraperitoneal, 30% intraperitoneal, and 10% combined extraperitoneal and intraperitoneal. Ten to 20% of patients with a pelvic fracture and bladder rupture also have a posterior urethral rupture (Box 11. The urethral rupture will prevent a cystogram from being done, so direct inspection of the bladder is required to establish the presence/absence of a bladder injury. The high-riding prostate is said to be a classic sign of posterior urethral rupture. Conversely, what may be thought to be a normal prostate in a normal position may actually be a palpable pelvic haematoma. Simultaneous bladder and prostato membranous urethral rupture from external trauma. Use at least 400ml of contrast in an adult, and 60ml plus 30ml per year of age in children up to a maximum of 400ml in children. A whisper of contrast from a posterior perforation may be obscured by a bladder distended with contrast. Intraperitoneal Usually repaired surgically to prevent complications from leakage of urine into the peritoneal cavity. Spontaneous rupture after bladder augmentation Spontaneous bladder rupture occasionally occurs months or years after bladder augmentation and usually with no history of trauma. Male posterior urethral injuries the great majority of posterior urethral injuries are an associated injury following pelvic fracture, and their diagnosis and initial management are discussed on E p. Immediate (within 48h) open repair of posterior urethral injuries is associated with a high incidence of urethral strictures (70%) and subsequent restenosis after stricture repair, incontinence (20%), and impotence (40%). The surrounding haematoma and tissue swelling make it difficult to identify structures and to mobilize the two ends of the urethra to allow tension-free anastomosis. In the majority of posterior urethral injuries, treatment should be deferred for 3 months to allow the oedema and haematoma to completely resolve. As this occurs, the two distracted ends of the urethra come closer together, thereby reducing the amount of mobilization that the surgeon has to do. Immediate repair is indicated where there is an open wound, as long as the urethral ends are close. Urethral injuries in females Rare because the urethra is short and its attachments to the pubic bone are weak, such that it is less prone to tearing during pubic bone fracture. When they do occur, such injuries are usually associated with rectal or vaginal injuries. In developing countries, prolonged labour can cause ischaemic injury to the urethra and bladder neck, leading to urethrovaginal or vesicovaginal fistula formation. History and examination the patient usually presents with difficulty in passing urine and frank haematuria in the context of a straddle injury. Blood may be present at the end of the penis and a haematoma around the site of the rupture. Confirming the diagnosis and subsequent management Retrograde urethrography delineates the extent of urethral injury. Urinary diversion (urethral or suprapubic catheter) prevents further extravasation of urine, and antibiotics may reduce the likelihood of superadded infection. Anterior urethral contusion Typical history: blood at the meatus, no extravasation of contrast on retrograde urethrogram. Pass a small-gauge urethral catheter (12Ch in an adult), and remove a week or so later. Partial rupture of anterior urethra leak of contrast from the urethra, with retrograde flow into the bladder. Seventy per cent heal without stricture formation (primary closure can be difficult because of oedema and haematoma at the site of injury and can convert a short area of urethral injury into a longer one). Give a broad-spectrum antibiotic to prevent infection of extravasated urine and blood. Suprapubic catheterization (percutaneously) is preferred over urethral catheterization, because a partial rupture can be converted to a complete rupture. Complete rupture of anterior urethra leak of contrast from the urethra on retrograde urethrogram, no filling of the posterior urethra or bladder. Remember, as the urethra passes through the pelvic floor (the membranous urethra), there is a normal narrowing and similarly, the prostatic urethra is narrower than the bulbar urethra. Penetrating partial and complete anterior urethral injuries Knife or gunshot wound: primary. Immediate surgical repair of anterior urethral injuries is only done in the context of penile fracture or where there is an open wound. Most in civilian practice are blunt, a blow forcing the testicle against the pubis or the thigh. Bleeding occurs into the parenchyma of the testis, and if sufficient force is applied, the tunica albuginea of the testis (the tough fibrous coat surrounding the parenchyma) ruptures, allowing extrusion of the seminiferous tubules. Penetrating injuries occur as a consequence of gunshot and knife wounds and from bomb blasts; associated limb. Where bleeding is confined by the tunica vaginalis, a haematocele is said to exist. Intraparenchymal (intratesticular) haemorrhage and bleeding beneath the parietal layer of the tunica vaginalis will cause the testis to enlarge slightly. The testis may be under great pressure as a consequence of the intratesticular haemorrhage confined by the tunica vaginalis. The force is usually sufficient to rupture the tunica albuginea and tunica vaginalis, and the seminiferous tubules and blood extrude into the layers of the scrotum. The resulting scrotal haematoma can be very large, and the bruising and swelling so caused may spread into the inguinal region and lower abdomen. Testicular ultrasound in cases of blunt trauma A normal parenchymal echo pattern suggests there is no significant testicular injury. A tender, palpable defect may be felt over the site of the tear in the tunica albuginea.
Best buy for vytorin
The Maternal-Fetal Medicine Units cesarean registry: Chorioamnionitis at term and its duration-relationship to outcomes ldl cholesterol calc definition cheap 20 mg vytorin amex. Use of C-reactive protein as a predictor of chorioamnionitis in preterm prelabour rupture of membranes: a systematic review. Oral clindamycin and histologic chorioamnionitis in women with abnormal vaginal flora. Acute and chronic chorioamnionitis and the risk of perinatal human immunodeficiency virus-1 transmission. Gentamicin and clindamycin therapy in postpartum endometritis: the efficacy of daily dosing versus dosing every 8 hours. Preterm premature rupture of membranes: diagnosis, evaluation and management strategies. High renal plasma flow and diffusion rates that exceed tubular reabsorption result in a physiologic glucosuria of approximately 300 mg/day. This physiologic glucosuria, combined with the poor correlation between urinary glucose and blood glucose levels, makes the urinary glucose screening useless to detect or monitor diabetes during pregnancy (once the standard). The use of these classifications makes comparisons of published data meaningful and may help to predict the relative risk to the pregnant mother and fetus. Gestational diabetes is reversible, although these patients have a greater incidence of glucose intolerance in subsequent pregnancies or with aging. Because of the increased risk for fetal anomalies, a determination of maternal serum -fetoprotein and early ultrasonographic studies are of great importance for these patients. Antenatal testing and active management of late pregnancy and labor induction are all indicated for selected patients with diabetes. When there is an estimated fetal weight of 4500 g or more, cesarean delivery may be considered because it may reduce the likelihood of permanent brachial plexus injury in the infant. To diagnose and manage disturbances of glucose metabolism to minimize the risk associated with diabetes in mothers and fetuses. Diabetes and pregnancy have profound effects on each other, making a familiarity with the interactions between mother, fetus, and the diabetic process a requirement to provide optimal care. Patients with type 1 diabetes are at greater risk for maternal complications (diabetic ketoacidosis, glucosuria, hyperglycemia, polyhydramnios, preeclampsia, pregnancy-induced hypertension, preterm labor, retinopathy, urinary tract infections, postpartum uterine atony). Other fetal complications include fetal demise, polyhydramnios, hyperbilirubinemia, hypocalcemia, hypoglycemia, macrosomia, polycythemia, prematurity, respiratory distress syndrome, and spontaneous abortion. Objectives of Management: To return serum glucose levels to as close to normal as possible through a combination of diet, exercise, oral hypoglycemic agents, and insulin (for selected patients). For the established patient with diabetes, this teaching is directed to the need for tighter control and more frequent monitoring. The woman with newly diagnosed diabetes requires general instruction about her disease and the unique aspects of diabetes during pregnancy. With respect to the fetus, the goal of treatment is to reduce the likelihood of macrosomia and its consequences. The upper limit of normal for such a test is 130 mg/dL (A screening test threshold of 140 mg/dL has 10% less sensitivity than a threshold of 130 mg/dL but fewer false-positive results; either threshold is acceptable). Approximately15% of patients have an abnormal screening test, and approximately the same proportion have an abnormal 3-hour test. For a 3-hour glucose tolerance test, the patient must ingest a minimum of 150 g/day of glucose for the 3 days preceding the test. If two or more values are abnormal, the diagnosis of gestational diabetes may be made. Studies indicate that screening may be omitted for selected individuals who are very low risk by selection criteria (see Box 224. This anti-insulin effect is sufficient to tip borderline patients into a diabetic state or prompt readjustments in the insulin dosage used by patients with insulin-dependent diabetes. Screening for gestational diabetes mellitus by a model based on risk indicators: a prospective study. A comparison of glyburide and insulin in women with gestational diabetes mellitus. Different strategies for diagnosing gestational diabetes to improve maternal and infant health. Gestational Diabetes Screening: the International Association of the Diabetes and Pregnancy Study Groups Compared With Carpenter-Coustan Screening. Jelly beans as an alternative to a fifty-gram glucose beverage for gestational diabetes screening. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. No safe level of exposure has been demonstrated, although sporadic use of less than 1 oz of alcohol per day has not been associated with the syndrome. Alcohol use among pregnant and nonpregnant women of childbearing age - United States, 1991-2005. Possible Complications: Higher rate of spontaneous miscarriage in heavy users of alcohol. Expected Outcome: Infants affected by fetal alcohol syndrome vary from mildly to profoundly mentally retarded. Systematic review of effects of lowmoderate prenatal alcohol exposure on pregnancy outcome. Alcohol abuse and other substance use disorders: ethical issues in obstetric and gynecologic practice. Because of the large size of some molar pregnancies and a tendency toward uterine atony, concomitant oxytocin administration is advisable and blood for transfusion must be immediately available, should it be needed. Oxytocin or methylergonovine maleate (Methergine) is used to help contract the uterus during surgical evacuation. Primary or recurrent malignant trophoblastic disease is generally treated with chemotherapy (methotrexate, actinomycin D, chlorambucil, or cyclophosphamide [Cytoxan], singly or in combination). Possible Complications: Gestational trophoblastic neoplasia is notable for the possibility of malignant transformation, although fewer than 10% of patients develop malignant changes. In general, the larger or more advanced the molar pregnancy, the greater the risk of pulmonary complications, bleeding, trophoblastic emboli, or fluid overload during evacuation. Expected Outcome: Approximately 80% of molar pregnancies follow a benign course after an initial therapy. The prognosis for patients with primary or recurrent malignant trophoblastic disease is generally good (>90% cure rate). The theca lutein cysts often found in molar pregnancies may take several months to regress after evacuation of the uterine contents. Fewer than 5% of patients will require hysterectomy to achieve a cure for choriocarcinoma. Methotrexate with citrovorum factor rescue for nonmetastatic gestational trophoblastic neoplasms. These patients have no higher rate of abortions, stillbirths, congenital anomalies, prematurity, or other complications of pregnancy with future gestations. The placenta from any subsequent pregnancies should be sent for histologic evaluation.